Drug overdose deaths in the United States are a substantial public health issue. The number of annual reported drug overdose deaths increased roughly 3-fold, from 23 500 in 2002 to 70 200 in 2017.1,2 Of even greater concern, during this same period, the number of opioid-related overdose deaths increased 4-fold, from 11 900 in 2002 to 47 600 in 2017.2
From 2016 to 2017, rates of opioid-related overdose deaths rose from 42 400 to 47 600, an increase of 12%. Also during this period, death rates associated with cocaine and psychostimulants increased by 34.4% (from 3.2 to 4.3 per 100 000 population) and 33.3% (from 2.4 to 3.2 per 100 000 population), respectively, likely contributing to the rise in overall drug overdose deaths.1 On the other hand, the number of overdose deaths related to either prescription opioids (which include buprenorphine, codeine, hydrocodone, hydromorphone, meperidine, methadone, morphine, oxycodone, oxymorphone, and tramadol) or heroin did not increase.1
Estimates based on provisional data for 2018 from the Centers for Disease Control and Prevention (CDC) explain these findings. Of an estimated 48 000 overall opioid-related overdose deaths in 2018, 28 400 deaths involved nonmethadone synthetic opioids, the most common of which was illicitly manufactured fentanyl.3 This trend is concerning because illicitly manufactured drugs commonly contain additional pharmacologically active components. These components are added during the illicit manufacturing process to either increase the bulk of the product or enhance the potency of the primary active component, are known as adulterants or cutting agents, and can themselves be toxic.4
In this Executive Perspective, we review data on the opioid crisis and describe recent US and global trends in the role of toxic adulterants and other pharmacologically active components in illicitly manufactured street drugs. We also highlight the role of toxic adulterants in opioid-related overdose deaths, chronic illicit drug abuse, and other public health issues. Finally, based on the information provided, we propose that clinicians increase attention to the potential role of toxic adulterants when evaluating and treating patients involved in drug abuse, overdose death, and addiction and that future public and personal health responses to the opioid epidemic emphasize building awareness and knowledge about the presence and dangers of toxic adulterants. In this way, we can further highlight the need to aggressively decrease the supply of illicitly manufactured drugs.
A Closer Look at the Opioid Crisis
Addressing the US opioid crisis involves taking an in-depth look at data on legal opioid prescribing, licit and illicit use of opioids by patients for pain and addiction, and overdose deaths. According to data from the 2017 National Survey on Drug Use and Health, the misuse of prescription opioids is declining.5 CDC also notes that the overall national opioid-prescribing rate declined from 255 million in 2012 to 191 million in 2017.6 However, despite these trends, the number of overdose deaths involving illicitly manufactured opioids (eg, fentanyl and fentanyl analogues) is increasing.7 Similarly, in a 2017 analysis of 20 states by CDC, nonmethadone synthetic opioids were detected in about 60% of opioid-related overdose deaths in 15 states, which represented a 45% overall increase from the previous year.1 These data highlight the concern that illicitly manufactured opioids have become the main drivers of the nation’s opioid crisis, and they prompt a call to action for both clinicians and public health professionals.
Other evidence also suggests that the current opioid epidemic is more complex than was originally recognized, in large part because it involves far more than the previously described drugs (eg, fentanyl, prescription opioids).8 It is becoming clear that the fentanyl and fentanyl analogues associated with overdoses are produced in clandestine laboratories rather than in commercial pharmaceutical laboratories.7 These drugs are then sold on the street as a powder, spiked on blotter paper or film, and then mixed with or substituted for heroin or as tablets that mimic other, less potent opioids. This illicitly manufactured fentanyl is now being mixed with counterfeit pharmaceutical pills, heroin, and cocaine.9,10 At the same time, the Drug Enforcement Administration (DEA) reported that the cocaine supply in 2017 had reached its highest level since 2007.11 National data also suggest that in 2017, cocaine use had its most significant increase since 2009.5 Because cocaine is increasingly being added to illicitly manufactured fentanyl, these cocaine-related trends are likely complicating and amplifying adverse outcomes of the opioid crisis.
At the same time, illicitly manufactured drugs can increasingly contain various other pharmacologically active components, in addition to cocaine and heroin.4 These additional components or ingredients are typically added in illicit noncommercial laboratories and are commonly known as cutting agents or adulterants. These adulterants come from a wide range of pharmacological categories, and many are toxic when ingested alone or in combination with other drugs. The presence of these adulterants in street drugs adds yet another layer of complexity to the US opioid crisis.
The problem of adulterants is exacerbated by the fact that most commercially available toxicological analyses identify a limited number of adulterants in illicit drug samples. Consequently, adulterants often go undetected, and their presence tends to be underreported.4 The effects of this limitation manifest in various settings. For example, in 2016 in the United States, only an estimated 15% of death certificates with overdose listed as a cause of death specified the types of drugs involved in the overdose,1 despite recommendations by the National Association of Medical Examiners that certifiers should list all drugs involved in overdose deaths.12 An analysis of National Vital Statistics System Multiple Cause of Death mortality files from 2008-2010 showed that states with centralized medical examiner systems were able to specify a higher percentage of the drugs involved in overdose deaths than states with other systems, such as county/district examiners, decentralized county coroners, or a mix of decentralized systems.13 A related problem is that, for various reasons, including a lack of adequate time and resources, many state crime laboratories, emergency departments, and medical examiners in the United States do not routinely test for adulterants, unless requested to do so.14
Ultimately, medical examiners and public health departments, clinicians, emergency departments, and substance abuse treatment centers are best served by having a complete list of the drugs present in each patient’s system.15 Comprehensive toxicological data are essential for diagnosis and, thus, for clinical care and public health surveillance of fatal and nonfatal drug overdoses. Thus, more complete toxicology panels, including those that test for a variety of adulterants, need to be both available and used in these settings to help address this aspect of the opioid epidemic.
Global Trends in the Role of Adulterants
Since 2015, the US Department of State has partnered with Colombo Plan, an independent intergovernmental organization based in Sri Lanka, to gain additional insight into the characteristics of the opioid- and other illicit drug-related overdose epidemics and to identify toxic adulterants that are used in the manufacture of illicit drugs in the United States and other regions of the world.16 Colombo Plan scientists have traveled to Argentina, Brazil, Ecuador, Peru, and South Africa to collect street drug samples and urine samples from street drug users, and the samples are tested using Raman and Fourier transform spectroscopy, immunoassays, and liquid chromatography/mass spectrometry.17 In these samples, they identified adulterants such as aminopyrine, diltiazem, dipyrone, levamisole, and phenacetin. These findings are similar to the findings of a 2016 DEA Special Testing and Research Lab report, which demonstrated that most South American heroin imported into the United States contained adulterants, including aminopyrine, diltiazem, and phenacetin, as well as acetaminophen, caffeine, diphenhydramine, quinine, and xylazine.18
The presence of toxic adulterants in street drugs worldwide appears to be magnifying the danger of these drugs to those who use them. Colombo Plan scientists reported that adulterants were likely related to additional local health problems identified in the regions tested.17 For example, emergency departments and drug treatment centers in South America and Africa have reported severe health effects from suspected adulterants added to street drugs, including renal and liver problems, blood disorders, infectious diseases, respiratory depression, and cardiac arrest.19
Emerging US Trends in the Role of Adulterants
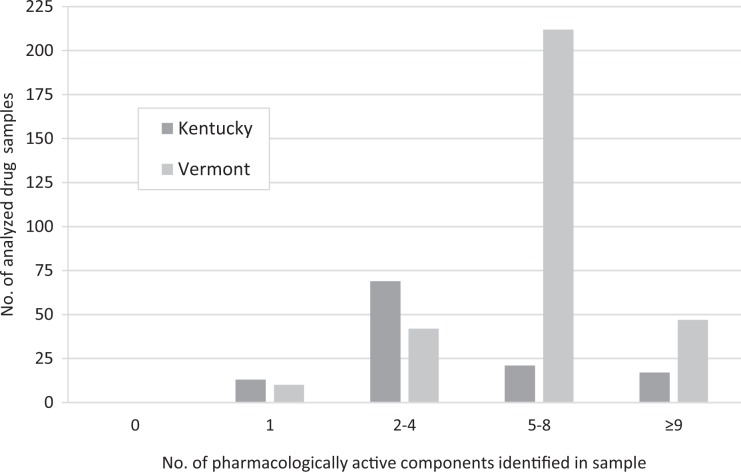
In 2017, Colombo Plan scientists partnered with NMS Labs (Horsham, PA) to test street drug samples of opioid and cocaine from Vermont and Kentucky to determine whether adulterants similar to those found overseas were also appearing in the United States.20 Using quadrupole time-of-flight mass spectrometry, a technology not routinely found in forensic or clinical laboratories, they identified multiple additional pharmacologically active components in most of the drug samples. A total of 301 of 311 (97%) samples collected in Vermont and 107 of 120 (89%) samples collected in Kentucky contained multiple additional pharmacologically active components (Figure). As many as 9 or more additional components, including fentanyl, were identified in 47 (15%) samples from Vermont and 17 (14%) samples from Kentucky. In addition to fentanyl, the additional components included adulterants (eg, acetaminophen, aminopyrine, diltiazem, diphenhydramine, dipyrone, levamisole, phenacetin, quetiapine, and others), controlled drugs (eg, cocaine, heroin), and impurities from the heroin-manufacturing process (eg, acetyl codeine, noscapine, papaverine; Table).
Figure.
Number of pharmacologically active components identified in street drug samples from Vermont (n = 311) and Kentucky (n = 120), 2017.20 Illicitly manufactured drugs commonly contain additional pharmacologically active components that are added during the manufacturing process, some of which are known as adulterants or cutting agents. Colombo Plan Secretariat scientists, in conjunction with NMS Labs (Horsham, PA), used quadrupole time-of-flight mass spectrometry to test opioid and cocaine samples for adulterants and other pharmacologically active components and found that all street drug samples contained ≥1 additional toxic adulterant, fentanyl, another controlled drug, or an impurity from the heroin-manufacturing process. Of the 311 samples collected in Vermont, 301 (97%) contained >1 additional pharmacologically active component, 259 (83%) contained ≥5 additional components, and 47 (15%) contained ≥9 additional components. Of the 120 samples collected in Kentucky, 107 (89%) contained >1 additional pharmacologically active component, 38 (32%) contained ≥5 additional components, and 17 (14%) contained ≥9 additional components.
Table.
Example lists of pharmacologically active components detected in 4 of 431 seized opioid and cocaine street drug samples from Kentucky and Vermont, 2017
| Category | Vermont Sample #156 | Vermont Sample #160 | Kentucky Sample #26 | Kentucky Sample #105 |
|---|---|---|---|---|
| Controlled drugs |
|
|
|
|
| Fentanyl |
|
|
|
|
| Adulterants |
|
|
|
|
| Impurities from the heroin-manufacturing process |
|
|
|
|
Abbreviations: 4-ANPP, 4-anilino-N-phenethyl-4-piperidinone; 6-MAM, 6-monoacetylmorphine.
Similarly, a report from the Florida Drug-Related Outcomes Surveillance and Tracking System at the University of Florida indicated that more than 90% of decedents with opioid-related overdose deaths in Florida in 2017 also had other, nonopioid, toxic components in their systems. Among those whose deaths were caused by opioids, such as fentanyl or heroin, an average of 2 or 3 additional nonopioid pharmacologically active components were also involved. Furthermore, as many as 11 additional components were identified in the systems of several decedents during autopsy.21
Most toxic adulterants detected in street drug samples in the United States, either alone or in combination with other pharmacologically active components, have also been implicated as possible causes of adverse health outcomes, including death. Health issues reported in the United States to be related to these adulterants include anemia, bone marrow damage, cancers, cardiac arrhythmias, hemolytic uremic syndrome, leukopenia, multifocal inflammatory leukoencephalopathy, neutropenia, and renal failure.22,23 Yet the danger lies not only in the direct toxicity of these adulterants but also in their unpredictability and their potential for unknown or unanticipated synergistic reactions with the opioid or other nonopioid components, all of which increase the risk for adverse health consequences, including death.4
Building Awareness and Knowledge of Toxic Adulterants Among Clinicians and the Public Health Community
The opioid crisis is one of the worst public health crises ever faced in the United States.24 To date, efforts to respond to the opioid crisis have focused primarily on limiting opioid prescriptions and reducing the supply of illicitly manufactured fentanyl.8 However, our analysis of trends in the United States and other regions of the world suggests that increased emphasis should be placed on the presence of toxic adulterants and other dangerous pharmacologically active components in street drugs. Mounting evidence suggests that overdoses, severe health consequences, and even death can occur as a result of the toxic and potentially synergistic effects of multiple toxic adulterants in combination with illicitly manufactured drugs of abuse.22,25-27
Moving forward, physicians and other clinicians in emergency departments, urgent care centers, primary care settings, and substance abuse treatment facilities will need to be increasingly aware of the role of toxic adulterants in how patients who take street drugs present. They will also need to be increasingly mindful that toxic adulterants can cause unusual drug interactions, complications, and medical conditions, all of which may increase the risk of opioid-related overdose and death. Also, because health care providers and patients are best served by having a complete list of the drugs present in a patient’s system, more complete toxicology panels, including those that test for a variety of adulterants, need to be available and used. Failure to recognize and identify toxic adulterants is likely to hinder timely and appropriate treatment, including life-saving measures.
In addition, public health professionals can work to build awareness and knowledge about the presence and dangers of toxic adulterants, particularly in populations most at risk for seeking illicit drugs. They can also continue to advocate for more comprehensive analyses of street drugs and their compositions, including toxic adulterants. Data from these analyses will provide a better understanding of the various factors that play a role in overdose deaths and will help identify emerging trends in the role of adulterants in the opioid epidemic.
Greater awareness and understanding of the developing role of toxic adulterants in the US opioid crisis is needed. Improved recognition of and knowledge about toxic adulterants could help clinicians take a more well-informed approach with their patients and guide public health professionals in formulating additional policies and programs to address the crisis.
Acknowledgments
The authors gratefully acknowledge NMS Labs and Colombo Plan for providing case sample data used in this work and Ms Chanya Liv for her efforts to this work.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors declared the following financial supports for the research, authorship, and/or publication of this article: Funding for the global toxic adulterant project was provided by the US Department of State, Bureau of International Narcotics & Law Enforcement Affairs and the Colombo Plan Secretariat.
ORCID iD: Joshua Montgomery, MPH  https://orcid.org/0000-0001-8490-3685
https://orcid.org/0000-0001-8490-3685
References
- 1. Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths—United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152):1419–1427. doi:10.15585/mmwr.mm675152e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention. About multiple cause of death, 1999-2017. https://wonder.cdc.gov/mcd-icd10.html. Published December 2018 Accessed January 21, 2019.
- 3. Ahmad FB, Escobedo LA, Rossen LM, Spencer MR, Warner M, Sutton P. 2018 provisional drug overdose death counts. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Published 2019 Accessed May 13, 2019.
- 4. Cole C, Jones L, McVeigh J, Kicman A, Syed Q, Bellis M. Adulterants in illicit drugs: a review of empirical evidence. Drug Test Anal. 2011;3(2):89–96. doi:10.1002/dta.220 [DOI] [PubMed] [Google Scholar]
- 5. Bose J, Hedden SL, Lipari RN, Park-Lee E. Key Substance Use and Mental Health Indicators in the United States: Results From the 2017 National Survey on Drug Use and Health. HHS Pub. No. SMA 18-5068, NSDUH Series H-53 Rockville, MD: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics; 2019. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.pdf. Accessed September 20, 2019. [Google Scholar]
- 6. Centers for Disease Control and Prevention. U.S. opioid prescribing rate maps. https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html. Updated October 2018. Accessed August 8, 2019.
- 7. US Department of Justice, Drug Enforcement Administration, Strategic Intelligence Section. 2018 national drug threat assessment report. https://www.dea.gov/sites/default/files/2018-11/DIR-032-18%202018%20NDTA%20final%20low%20resolution.pdf. Published October 2018 Accessed February 15, 2019.
- 8. DuPont RL. The opioid epidemic is an historic opportunity to improve both prevention and treatment. Brain Res Bull. 2018;138:112–114. doi:10.1016/j.brainresbull.2017.06.008 [DOI] [PubMed] [Google Scholar]
- 9. Kandel DB, Hu MC, Griesler P, Wall M. Increases from 2002 to 2015 in prescription opioid overdose deaths in combination with other substances. Drug Alcohol Depend. 2017;178:501–511. doi:10.1016/j.drugalcdep.2017.05.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McCall Jones C, Baldwin GT, Compton WM. Recent increases in cocaine-related overdose deaths and the role of opioids. Am J Public Health. 2017;107(3):430–432. doi:10.2105/AJPH.2016.303627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Drug Enforcement Administration, Strategic Intelligence Section. DEA Intelligence Brief. Colombian cocaine production expansion contributes to rise in supply in the United States. DEA-DCI-DIB-014-17. https://ndews.umd.edu/sites/ndews.umd.edu/files/dea-colombian-cocaine-production_expansion-contributes-to-rise-in-us-supply2.pdf. Published August 2017 Accessed February 15, 2019.
- 12. Davis GG, National Association of Medical Examiners and American College of Medical Toxicology Expert Panel on Evaluating and Reporting Opioid Deaths. Complete republication: National Association of Medical Examiners position paper: recommendations for the investigation, diagnosis, and certification of deaths related to opioid drugs. J Med Toxicol. 2014;10(1):100–106. doi:10.1007/s13181-013-0323-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Warner M, Paulozzi LJ, Nolte KB, Davis GG, Nelson LS. State variation in certifying manner of death and drugs involved in drug intoxication deaths. Acad Forensic Pathol. 2013;3(2):231–237. doi:10.23907/2013.029 [Google Scholar]
- 14. Slavova S, O’Brien DB, Creppage K, et al. Drug overdose deaths: let’s get specific. Public Health Rep. 2015;130(4):339–342. doi:10.1177/003335491513000411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wu AH, McKay C, Broussard LA, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines: recommendations for the use of laboratory tests to support poisoned patients who present to the emergency department. Clin Chem. 2003;49(3):357–379. [DOI] [PubMed] [Google Scholar]
- 16. US Department of State, Bureau for International Narcotics and Law Enforcement Affairs. International narcotics control strategy report. Volume 1: drug and chemical control. https://www.hsdl.org/?view&did=809034. Published March 2018 Accessed August 7, 2019.
- 17. Fiorentin TR, Fogarty M, Limberger RP, Logan BK. Determination of cutting agents in seized cocaine samples using GC-MS, GC-TMS and LC-MS/MS. Forensic Sci Int. 2019;295:199–206. doi:10.1016/j.forsclint.2018.12.016 [DOI] [PubMed] [Google Scholar]
- 18. Drug Enforcement Administration, Intelligence Programs Section. DEA Intelligence Report. 2016 Heroin Domestic Monitor Program. The Heroin Signature Program and Heroin Domestic Monitor Program 2014 Reports. DEA-DCW-DIR-051-16. Washington, DC: US Department of Justice; 2016. https://www.hsdl.org/?view&did=802102. Accessed December 3, 2018. [Google Scholar]
- 19. United Nations Office on Drugs and Crime. 2017 Global Synthetic Drugs Assessment. Vienna, Austria: United Nations Office on Drugs and Crime; 2017. https://www.unodc.org/documents/scientific/Global_Drugs_Assessment_2017.pdf. Accessed March 4, 2019. [Google Scholar]
- 20. Fiorentin TR, Krotulski AJ, Martin DM, et al. Detection of cutting agents in drug-positive seized exhibits within the United States. J Forensic Sci. 2019;64(3):888–896. doi:10.1111/1556-4029 [DOI] [PubMed] [Google Scholar]
- 21. Wang Y, Goldberger BA, Delcher C. Florida drug-related outcomes surveillance and tracking system. http://frost.med.ufl.edu/frost. Published 2019 Accessed May 5, 2019.
- 22. Gold MS. Deadly adulterants: new dangers of illicit drugs. The Sober World Magazine. https://www.thesoberworld.com/2017/07/01/deadly-adulterants-new-dangers-of-illicit-drugs. Published July 1, 2017 Accessed January 21, 2019.
- 23. Phillips KA, Hirsch GA, Epstein DH, Preston KL. Cardiac complications of unwitting co-injection of quinine/quinidine with heroin in an intravenous drug user. J Gen Intern Med. 2012;27(12):1722–1725. doi:10.1007/s11606-012-2089-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. DuPont RL. A new narrative to understand the opioid epidemic. J Glob Drug Policy Pract. 2018;12(1):1–22. https://www.dfaf.org/wp-content/uploads/2018/11/Opioid-Narrative-3.pdf. Accessed January 16, 2019. [Google Scholar]
- 25. Ribeiro M, Trevizol AP, Frajzinger R, et al. Adulterants in crack cocaine in Brazil. Trends Psychiatry Psychother. 2019;41(2):186–190. doi:10.1590/2237-6089-2017-0143 [DOI] [PubMed] [Google Scholar]
- 26. Akhgari M, Etemadi-Aleagha A, Jokar F. Street level heroin, an overview on its components and adulterants. Neuropathol Drug Addict Subst Misuse. 2016;1:867–877. doi:10.1016/B978-0-12-800213 -1.00081-X [Google Scholar]
- 27. US Department of Health and Human Services. Report on pain management best practices: updates, gaps, inconsistencies, and recommendations. https://www.hhs.gov/ash/advisory-committees/pain/reports/index.html. Published May 2019 Accessed September 30, 2019.