In chronic cocaine users, there remains the potential for extensive sinonasal necrosis, leading to the complication known as a cocaine-induced midline destructive lesion (CIMDL).1 One of the most challenging aspects of CIMDL is its ability to mimic vasculitic disorders, given the capacity of adulterated cocaine to cause elevation to antineutrophil cytoplasmic antibody (ANCA) titers.1
Institutional Review Board
Institutional review board approval is not required for case reports at our institution, per MedStar Health Research Institutional Review Board guidelines.
Case
A 33-year-old man, with a history of cocaine abuse, presented with 4 weeks of nasal obstruction, dysphagia, otalgia, and worsening nasal bridge deformity. Endoscopy revealed extensive mucosal devitalization of the oropharynx ( Figure 1 ), as well as complete necrosis of the nasal corridor with limited identifiable landmarks ( Figure 2 ). Furthermore, extensive nasopharyngeal destruction was noted with involvement of the eustachian tube orifices bilaterally (Video 1). Computer tomography (CT) scan was performed with findings in concordance with extensive bony destruction of the nasal cavity as well as multiple small pulmonary nodules. Laboratory analysis revealed leukocytosis as well as elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Furthermore, urine toxicology revealed the presence of cocaine metabolites, which, in the setting of elevated cytoplasmic ANCA (c-ANCA) titers, raised the possibility of levamisole-induced vasculitis. Given the presence of pulmonary nodules, the patient underwent biopsy of the sinonasal lesions to rule out systemic vasculitides, but tissue specimens ultimately did not meet the diagnostic criteria for vasculitis. The patient was counseled on cocaine cessation but unfortunately eloped soon thereafter and was lost to follow-up.
Figure 1.
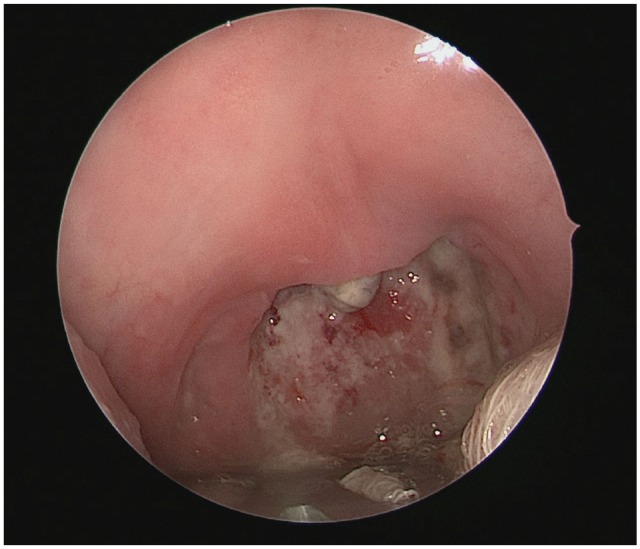
Oropharyngeal endoscopy demonstrating necrotic, insensate mucosa of uvula and posterior oropharyngeal wall.
Figure 2.
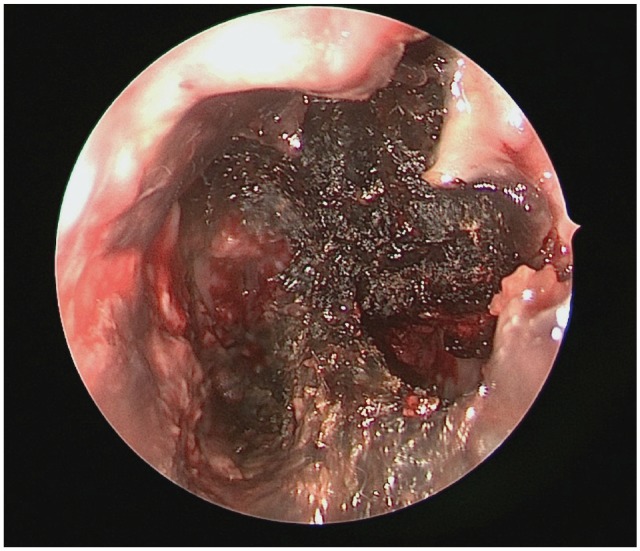
Nasal endoscopy demonstrating extensive nasal cavity necrosis with diffuse inspissated clot and large septal defect.
Discussion
Pseudovasculitis is a nonspecific term given to a broad array of disease processes that clinically and serologically mimic vasculitis but do not display the typical histopathological findings of a true vasculitis. Of note, cocaine is frequently contaminated with exogenous substances that elicit elevated ANCA titers, making differentiation from true vasculitides particularly challenging.1
Levamisole is a synthetic imidazothiazole antihelminthic agent originally developed in the 1970s and used in various rheumatologic and oncologic applications for its immunomodulatory effects. Its use was curtailed in the late 1990s following recognition of severe adverse reactions, including cutaneous skin lesions, agranulocytosis, thrombocytopenia, and arthritis.1 Despite these concerns, its use as an additive has gained popularity in the illegal drug market, owing to its ease of use a bulking agent and ability to potentiate and enhance stimulant effects of various narcotic drugs.2 According to the Centers for Disease Control and Prevention, at least 70% of illicit cocaine used in the United States is contaminated with levamisole.
Levamisole-associated CIMDL is often strongly suspected in individuals presenting with extensive sinonasal necrosis, but definitive diagnosis can prove problematic, especially in those individuals who do not readily admit to cocaine use or have a family history of vasculitic disease. Several clues can aid in accurate diagnosis. In particular, the degree of local destruction is much more substantial in CIMDL compared to systemic entities, such as granulomatosis with polyangiitis (GPA).2 In addition, histological analysis is a critical element in definitive diagnosis, with pathognomonic features such as stromal granulomas, leukocytoclasis, presence of giant cells, and deep microabscesses favoring GPA over CIDML.3 Unfortunately, although these criteria may aid in diagnosis, approximately 50% of nasal biopsies are nondiagnostic in patients with GPA.4
In regards to laboratory testing, serological assessment may prove beneficial. It is generally recognized that c-ANCA is predominantly elevated in GPA, whereas elevated p-ANCA is more suggestive of CIMDL.5 The exact mechanism in which levamisole leads to upregulation of ANCA is not completely understood, but it is thought to act as a haptan, triggering an immune response and upregulation of antibody formation.3 Direct testing for levamisole is completed via mass spectrometry and provides a definitive diagnosis but is not routinely conducted secondary to low availability in the clinical setting and relatively short half-life of levamisole.2
Overall, management of CIMDL is clinically challenging. Conservative measures such as serial debridements, regular saline douches, and topical antibiotics may slow progression of disease but will not reverse existing damage. Definitive management relies on complete abstinence from cocaine use but, in practice, is difficult to achieve in individuals with addiction problems, given barriers to substance abuse rehabilitation and treatment compliance.3
Author Contributions
Adnan S. Hussaini, lead author, substantial contribution to conception, analysis, and acquisition, article drafting, final approval, accountability for the work; Cara K. Black, contributing author, substantial contribution to conception, article drafting, final approval, accountability for the work; Sonya Malekzadeh, senior author, substantial contribution to conception and analysis, article drafting, final approval, accountability for the work, Gregory J. Milmoe, senior author, substantial contribution to conception and acquisition, article drafting, final approval, accountability for the work.
Disclosures
Competing interests: None.
Sponsorships: None.
Funding source: None.
Footnotes
No sponsorships or competing interests have been disclosed for this article.
Supplemental Material: Additional supporting information is available at http://journals.sagepub.com/doi/suppl/10.1177/2473974X19894239
References
- 1. Sayadi L, Laub D. Levamisole-induced vasculitis. Eplasty. 2018;18:ic5. [PMC free article] [PubMed] [Google Scholar]
- 2. Trimarchi M, Bussi M, Sinico RA, Meroni P, Specks U. Cocaine-induced midline destructive lesions—an autoimmune disease? Autoimmun Rev. 2013;12:496-500. [DOI] [PubMed] [Google Scholar]
- 3. Trimarchi M, Gregorini G, Facchetti F, et al. Cocaine-induced midline destructive lesions: clinical, radiographic, histopathologic, and serologic features and their differentiation from Wegener granulomatosis. Medicine (Baltimore). 2001;80:391-404. [DOI] [PubMed] [Google Scholar]
- 4. Del Buono EA, Flint A. Diagnostic usefulness of nasal biopsy in Wegener’s granulomatosis. Hum Pathol. 1991;22:107-110. [DOI] [PubMed] [Google Scholar]
- 5. Lawrence LA, Jiron JL, Lin HS, Folbe AJ. Levamisole-adulterated cocaine induced skin necrosis of nose, ears, and extremities: case report. Allergy Rhinol (Providence). 2014;5:132-136. [DOI] [PMC free article] [PubMed] [Google Scholar]


