Abstract
Background
This review is one in a series of Cochrane reviews investigating pain management for childbirth. These reviews all contribute to an overview of systematic reviews of pain management for women in labour, and share a generic protocol. This review updates an earlier version of the review of the same title.
Objectives
To examine the effectiveness and safety of hypnosis for pain management during labour and childbirth.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register (30 September 2015) and the reference lists of primary studies and review articles.
Selection criteria
Randomised controlled trials (RCTs) and quasi‐RCTS comparing preparation for labour using hypnosis and/or use of hypnosis during labour, with or without concurrent use of pharmacological or non‐pharmacological pain relief methods versus placebo, no treatment or any analgesic drug or technique.
Data collection and analysis
Two review authors independently extracted data and assessed trial quality. Where possible we contacted study authors seeking additional information about data and methodology.
Main results
We included nine trials randomising a total of 2954 women. The risk of bias in trials was variable, there were several well‐designed large trials and some trials where little was reported about trial design. Although eight of the nine trials assessed antenatal hypnotherapy, there were considerable differences between these trials in timing and technique. One trial provided hypnotherapy during labour. In this updated review we compared hypnosis interventions with all control groups (main comparison) and also with specific control conditions: standard care (nine RCTs), supportive counselling (two RCTs) and relaxation training (two RCTs).
In the main comparison, women in the hypnosis group were less likely to use pharmacological pain relief or analgesia than those in the control groups, (average risk ratio (RR) 0.73, 95% CI 0.57 to 0.94, eight studies, 2916 women; very low‐quality evidence; random‐effects model). There were no clear differences between women in the hypnosis group and those in the control groups for most of the other primary outcomes. There were no clear differences for sense of coping with labour (MD 0.22, 95% CI ‐0.14 to 0.58, one study, 420 women; low‐quality evidence) or spontaneous vaginal birth (average RR 1.12, 95% CI 0.96 to 1.32, six studies, 2361 women; low‐quality evidence; random‐effects model). There were no clear differences for satisfaction with pain relief (measured on a seven‐point scale two weeks postnatally) for women in the hypnosis group who also received pethidine (MD 0.41, 95% CI ‐0.45 to 1.27; one study, 72 women), Entonox (MD 0.19, 95% CI ‐0.19 to 0.57; one study, 357 women), self‐hypnosis (MD 0.28, 95% CI ‐0.32 to 0.88; one study, 160 women), or epidural (MD ‐0.03, 95% CI ‐0.40 to 0.34; one study, 127 women), but a slight benefit in favour of hypnosis was seen for women who received water immersion (MD 0.52, 95% CI 0.04 to 1.00; one study, 174 women (all low‐quality evidence). There were no clear differences for satisfaction with pain relief when it was measured as the number of women who reported they had adequate pain relief (risk ratio (RR) 1.06, 95% confidence interval (CI) 0.94 to 1.20, one study, 264 women; low‐quality evidence). It should be noted that for pharmacological pain relief and spontaneous vaginal birth, there was evidence of considerable statistical heterogeneity, which could not be fully explained by subgroup analysis.
For this review's secondary outcomes, no clear differences were found between women in the hypnosis group and women in the control groups for most outcomes where data were available. There was mixed evidence regarding benefits for women in the hypnosis group compared with all control groups for pain intensity, satisfaction with childbirth experience and postnatal depression. For each of these outcomes, data from more than one trial were available for analysis but could not be combined due to differences in measurement methods. There was evidence that fewer women in the hypnosis group stayed in hospital for more than two days after the birth but this finding was based on one small study (RR 0.11, 95% CI 0.02 to 0.83). No clear differences between women in the hypnosis group and the control groups were found for the other secondary outcomes where data were available.
In the comparisons of hypnosis with specific types of control conditions: standard care, supportive counselling and relaxation training, there were no clear differences found between women in the hypnosis group and those in the standard care control groups or the relaxation control groups for the primary outcomes. Compared with the women in the supportive counselling control group, women in the hypnosis group were less likely to use pharmacological analgesia (average RR 0.48, 95% CI 0.32 to 0.73, two studies, 562 women). They were also more likely to have a spontaneous vaginal birth (RR 2.42, 95% CI 1.43 to 4.07), although this finding was based on the results of one small study. Overall these new comparisons displayed much less statistical heterogeneity than the comparison including all control groups.
Authors' conclusions
There are still only a relatively small number of studies assessing the use of hypnosis for labour and childbirth. Hypnosis may reduce the overall use of analgesia during labour, but not epidural use. No clear differences were found between women in the hypnosis group and those in the control groups for satisfaction with pain relief, sense of coping with labour or spontaneous vaginal birth. Not enough evidence currently exists regarding satisfaction with pain relief or sense of coping with labour and we would encourage any future research to prioritise the measurement of these outcomes. The evidence for the main comparison was assessed using GRADE as being of low quality for all the primary outcomes with downgrading decisions due to concerns regarding inconsistency of the evidence, limitations in design and imprecision. Further research is needed in the form of large, well‐designed randomised controlled trials to assess whether hypnosis is of value for pain management during labour and childbirth.
Keywords: Female; Humans; Pregnancy; Analgesia, Obstetrical; Analgesia, Obstetrical/methods; Hypnosis; Hypnosis/methods; Labor Pain; Labor Pain/psychology; Labor Pain/therapy; Labor, Obstetric; Labor, Obstetric/psychology; Length of Stay; Patient Satisfaction; Randomized Controlled Trials as Topic; Time Factors
Plain language summary
Hypnosis for pain management during labour and childbirth
What is the issue?
Women's experiences of pain in labour are variable and complex. Techniques such as hypnosis have been proposed as ways to help women cope with pain during labour. Hypnosis represents an aspect of conscious awareness similar to daydreaming and involves focusing attention inwards and increased responsiveness to suggestions. Suggestions are verbal and non‐verbal communications, that may influence perceptions (such as the way contractions are experienced), mood or behaviour. During childbirth women may use hypnosis in a range of ways; to promote relaxation, as a means of dissociating from pain or to change their perceptions, for example, perceIving contractions as a way to get closer to birthing their baby rather than an experience of pain and suffering more usually associated with injury and disability. Women can be guided into hypnosis by a practitioner during labour or individuals can learn self‐hypnosis during pregnancy, for subsequent use during labour. This training on how to use hypnosis during the pregnancy is sometimes supplemented by audio recordings of hypnotic suggestions.
Why is it important?
Childbirth is a major physical, emotional and social event in a woman's life. The experience and management of pain during labour are important issues for many women.
What evidence did we find?
We included nine trials that randomised 2954 women to hypnosis or to control groups receiving; standard care, relaxation training or supportive counselling. In eight trials the women were trained in self‐hypnosis during pregnancy for later use during labour. In the other trial, the hypnotherapist was present during the woman's labour.
There were no clear differences between women in the hypnosis group and those in the control groups in terms of the number of normal deliveries, women's satisfaction with the method of pain relief or women's sense of coping with labour. However, fewer women in the hypnosis group used pain relief medication for labour. Epidural use did not differ between the groups. All the evidence for these outcomes was found to be of low quality. The studies measured a range of other outcomes and no consistent differences were found.
What does this mean?
Hypnosis may reduce the overall use of pain medication during labour, but does not seem to reduce the use of epidurals. Women using hypnosis are no more likely to have a normal vaginal birth. There is currently not enough evidence to say whether hypnosis helps women feel more satisfied about their pain relief in labour, nor whether it improves their sense of coping with labour. Further high‐quality research is needed and should include assessment of women's satisfaction with pain relief and sense of coping in labour. Our conclusions about the impact hypnosis has on pain during labour and childbirth may change with future, high‐quality research.
Summary of findings
Summary of findings for the main comparison. Self‐hypnosis or hypnotherapy versus all for management of pain during labour and childbirth.
| Self‐hypnosis or hypnotherapy versus all for management of pain during labour and childbirth | ||||||
| Patient or population: pregnant women Setting: Australia, Denmark, UK, USA Intervention: self‐hypnosis or hypnotherapy Comparison: standard care (including supportive counselling, relaxation) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with all | Risk with Self‐hypnosis or hypnotherapy | |||||
| Use of pharmacological pain relief/anaesthesia | Study population | average RR 0.73 (0.57 to 0.94) | 2916 (8 studies) | ⊕⊝⊝⊝ very low1, 2 | ||
| 608 per 1000 | 444 per 1000 (347 to 572) | |||||
| Moderate | ||||||
| 673 per 1000 | 491 per 1000 (384 to 633) | |||||
| Satisfaction with pain relief (number of women who reported that they felt they had adequate pain relief) |
Study population | RR 1.06 (0.94 to 1.20) | 264 (1 study) | ⊕⊕⊝⊝ low3,4 | ||
| 773 per 1000 | 820 per 1000 (727 to 928) | |||||
| Satisfaction with pain relief (reported 2 weeks postnatal) ‐ Pethidine Seven‐point scale: 7 = most satisfaction |
The mean satisfaction with pain relief score was 4 in the control group | The mean satisfaction with pain relief score in the hypnosis group was 0.41 points more (1.27 higher to 0.45 lower) | 72 (1 study) | ⊕⊕⊝⊝ low3,4 | Higher score indicates more satisfaction with pain relief | |
| Satisfaction with pain relief (reported 2 weeks postnatal) ‐ Entenox Seven‐point scale: 7 = most satisfaction |
The mean satisfaction with pain relief score was 4.07 in the control group | The mean satisfaction with pain relief score in the hypnosis group was 0.19 points more (0.57 higher to 0.19 lower) | 357 (1 study) | ⊕⊕⊝⊝ low3,4 | Higher score indicates more satisfaction with pain relief | |
| Satisfaction with pain relief (reported 2 weeks postnatal) ‐ Self‐hypnosis Seven‐point scale: 7 = most satisfaction |
The mean satisfaction with pain relief score was 4.04 in the control group | The mean satisfaction with pain relief score in the hypnosis group was 0.28 points more (0.88 higher to 0.32 lower) | 160 (1 study) | ⊕⊕⊝⊝ low3,4 | Higher score indicates more satisfaction with pain relief | |
| Satisfaction with pain relief (reported 2 weeks postnatal) ‐ Epidural Seven‐point scale: 7 = most satisfaction |
The mean satisfaction with pain relief score was 6.55 in the control group | The mean satisfaction with pain relief score in the hypnosis group was 0.03 points lower (0.34 higher to 0.40 lower) | 127 (1 study) | ⊕⊕⊝⊝ low3,4 | Higher score indicates more satisfaction with pain relief | |
| Satisfaction with pain relief (reported 2 weeks postnatal) ‐ Water immersion Seven‐point scale: 7 = most satisfaction |
The mean satisfaction with pain relief score was 4.94 in the control group | The mean satisfaction with pain relief score in the hypnosis group was 0.52 points higher (1.00 higher to 0.04 higher) | 174 (1 study) | ⊕⊕⊝⊝ low3,4 | Higher score indicates more satisfaction with pain relief | |
| Coping in labour | The mean coping in labour score was 5.29 in the control group | The mean coping in labour score in the hypnosis group was 0.22 points higher (0.14 fewer to 0.58 more) | 420 (1 study) | ⊕⊕⊝⊝ low3,4 | Coping in labour was measured on a seven‐point scale where 0 = extremely dissatisfied and 7 = extremely satisfied | |
| Spontaneous vaginal birth | Study population | average RR 1.12 (0.96 to 1.32) | 2361 (6 studies) | ⊕⊕⊝⊝ low5, 6 | ||
| 619 per 1000 | 693 per 1000 (594 to 817) | |||||
| Moderate | ||||||
| 560 per 1000 | 627 per 1000 (538 to 739) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 Inconsistency: considerable heterogeneity evident ‐ I2 = 91% (‐2)
2 Design limitations: four of eight studies are at high/unclear risk for selection bias (‐1)
3 Design limitations: the one study contributing data had design limitations to do with lack of blinding of participants for this subjective outcome (‐1)
4 Imprecision: only one study with a small sample size (‐1)
5 Inconsistency: substantial heterogeneity evident ‐ I2 = 73% (‐1)
6 Design limitations: three of six studies are at high/unclear risk for selection bias; three of six studies are at high risk for detection bias (‐1)
Background
This review was one in a series of Cochrane reviews examining pain management for childbirth. These reviews all contribute to an overview of systematic reviews of pain management for women in labour (Jones 2012), and share a generic protocol (Jones 2011).
Description of the condition
Women's experiences of pain during labour are complex phenomena. Although almost all women report some pain during childbirth, their sensory and affective perceptions can vary widely (Lowe 2002). For example, some women describe the sensations of labour as more akin to extreme muscular exertion from physical activity, some as productive pain which signals that their baby's birth is closer, some compare it with intense period pain and others describe it as agony or like torture (Green 1998; Lundgren 1998; McCutcheon‐Rosegg 1996). There have also been reports that occasionally women experience no labour pain and give birth unexpectedly (Gaskin 2003). A range of physiological and psychosocial factors have been identified, which attempt to explain labour pain and its variability (Lowe 2002).
Traditionally, labour pain has been defined similarly to acute pain, "a complex constellation of unpleasant sensory, perceptual and emotional experiences and certain associated autonomic, physiologic, emotional and behavioural responses" (Bonica 1990a). However, unlike other acute pain, which can usually be attributed to pathological processes, labour pain does not signal harm or pathology and is considered a normal part of birth (Lowe 2002). The physiological processes thought to cause pain during labour include uterine contractions dilating the cervix in the first stage of labour and the stretching of the vagina and pelvic floor as the baby descends during the second stage of labour (Bonica 1990b). Although pain intensity has been found to increase with the frequency of contractions and greater cervical dilatation, these patterns are not consistent across women (Melzack 1984). Physical factors such as maternal positioning have also been found to affect pain, with women randomised to upright positions in the first stage of labour less likely to use epidural analgesia than women randomised to recumbent positions (Lawrence 2013).
Psychosocial factors including anxiety, fear, feelings of self‐efficacy, coping skills and social support have also been shown to have a relationship with women's experiences of labour and labour pain (Hodnett 2013; Lowe 2002). For example, anxiety and fear of pain have been positively correlated with reported pain levels during labour (Lowe 2002). By contrast, women were less likely to use pain medications if they had a continuous support person for labour, and women's confidence in their ability to cope has also been associated with reduced pain perception (Hodnett 2013; Lowe 1989). Historically, Dick‐Read 1947 made a influential theoretical contribution to the literature on psychological factors in labour. His cyclical "fear‐tension‐pain syndrome" linked women’s feelings of fear and anxiety to muscular tension and pain in childbirth (Dick‐Read 1947). In this model, high levels of maternal fear led to increased muscular tension, causing increased pain which in turn further heightened the woman’s level of fear (Dick‐Read 1947). This theory has been explicitly incorporated into a range of childbirth education programs, including the hypnosis‐oriented program developed by Mongan 2005. Many antenatal education programs seek to reduce maternal anxiety and increase confidence.
The measurement of pain generally and the measurement of labour pain in particular is challenging given the subjective nature of the experience and the complex interpretations involved. Indeed, there is evidence that the way pain is measured can affect the way it is interpreted by individuals (Chooi 2011; Chooi 2013). Studies have also shown low levels of agreement between the subjective assessments of pain by patients and the estimates of medical staff (for example, Trentin 2001). Given these challenges, more objective measures such as use of pharmacological pain relief can be usefully supplemented with a range of subjective measures of pain experience.
Description of the intervention
A wide range of methods for pain management are currently used by women during childbirth (Caton 2002). Commonly, these include pharmacological methods such as epidural analgesia and/or physical methods such as water immersion (Caton 2002). The use of psychological methods for comfort in childbirth has a very long history and forms of verbal suggestion were reportedly used for this purpose in Egyptian and Chinese societies (Bonica 1990b). The term 'hypnosis' was proposed by James Braid in the 1840s and it has been reported that the technique was soon adopted as a method of pain relief for childbirth (Platonov 1960).
There is considerable academic debate about whether hypnosis represents "a distinct state of consciousness" or whether it is a normal state, where "social influence combines with a set of cognitive‐behavioural skills to heighten suggestibility" (Gamsa 2003). However, the core components of hypnosis are generally described as involving "narrowed focus of attention, reduced awareness of external stimuli, absorption in hypnotic suggestions, increased responsiveness to hypnotic suggestions, and usually, though not always, deep relaxation" (Gamsa 2003). Suggestions are "verbal and non‐verbal communications" that can be used to influence perceptions, mood or behaviour (Cyna 2004; Cyna 2009 ). In the context of childbirth, suggestions may focus on increasing feelings of safety, relaxation and comfort, reframe the experience from one of pain to achievement, as well as potentially developing sensations of anaesthesia such as numbing.
There are two main methods for providing hypnosis interventions for childbirth: hypnotherapy delivered in‐person by a practitioner; and self‐hypnosis, where the practitioner teaches the mother how to induce a "state of consciousness similar to meditation which results in failure of normally perceived experiences reaching conscious awareness" (Cyna 2004). Self‐hypnosis can be taught to women individually or in groups, and can be supplemented with audio recordings for use at home. For example, in one US trial, groups of 15 pregnant women had one‐hour hospital‐based training sessions each week for six weeks (Harmon 1990). The women were also given audio recordings of the hypnotic induction for daily practice leading up to the birth (Harmon 1990). The benefits of teaching women self‐hypnosis before labour include the promotion of women's active participation and sense of control for managing anxiety and discomfort (Martin 2001). Alternatively, an example of hypnotherapy for childbirth guided by a practitioner was a trial in Philadelphia, where a trained medical student provided hypnosis to women in active labour in hospital (Rock 1969). This method of delivering the intervention was chosen as it was considered to be less time consuming than antenatal training and more predictable results were expected (Rock 1969).
How the intervention might work
There is promising evidence that hypnosis may be effective in reducing acute pain across a range of settings, including burns treatment and other invasive medical procedures (Montgomery 2000; Patterson 2003). A meta‐analysis of 18 studies of experimentally induced and clinical pain found that hypnotic analgesia provided a moderate to large analgesic effect for both types of pain (Montgomery 2000). Although most of the participants were reported to be randomly assigned to treatment or control conditions, most of the trials included in the analysis were small (Montgomery 2000), and there was no explicit assessment of potential sources of selection, attrition and selective reporting bias in the trials. Patterson 2003 also reported that several well‐designed controlled trials supported the efficacy of hypnosis for acute pain in a large review of hypnosis and clinical pain. This review provided more detailed information about each trial, but again did not explicitly assess all potential sources of bias.
Neuro‐imaging studies have provided evidence about the nature of neuro‐physiological changes during hypnosis generally and during hypnotically‐induced analgesia (Faymonville 2000; Maquet 1999). A positron emission tomography and magnetic resonance imaging study found hypnosis reduced pain experienced from hot, noxious stimuli and that the process was "mediated by the anterior cingulate cortex" (Faymonville 2000). Both the affective and sensory aspects of pain perception were reduced when participants used hypnosis (Faymonville 2000). Hypnosis has also been used to selectively alter the degree of unpleasantness of hot, noxious stimuli without changing the perceived intensity of the pain in a study designed to differentiate the cortical areas involved in the affective and sensory dimensions of pain (Rainville 1997).
In the context of pain management for childbirth, hypnosis is often considered alongside other non‐pharmacological methods as focused on the affective aspects of the pain experience, such as reducing anxiety, fear, muscular tension as well as enhancing mood and increasing the woman's sense of control (Simkin 2004). However, there have been case reports of hypnosis used as the only analgesia for surgical procedures, including caesarean section, for highly hypnotisable individuals (for example, Kroger 1957).
Hypnotisability refers to the degree to which individuals follow suggestions during hypnosis and a number of scales have been constructed to measure and predict hypnotic suggestibility (Gamsa 2003). Some studies have found that highly hypnotisable individuals experienced greater pain relief than those who scored low on hypnotisability scales (Harmon 1990; Stam 1984), although other studies did not replicate this finding (Rock 1969; Samko 1975). Hypnotisablity may not be a stable characteristic with evidence that the ability to control pain can improve with repeated use of hypnoanalgesia (Lewis 1992) and that the physiological and hormonal changes associated with pregnancy may affect individuals' responsiveness to hypnosis (Alexander 2009). For example, one study found that women were more hypnotisable when pregnant (Alexander 2009). This study used a repeated‐measures design with 37 women and found a large, clinically meaningful effect (d = 0.84) for increased hypnotisability during pregnancy. Measured on the Creative Imagination Scale (CIS) (Barber 1979), which has a maximum score of 40, the women's mean CIS score when pregnant was 23.5 (standard deviation (SD) 6.9), compared with a mean CIS score of 18.7 (SD 6.6) when the women were between 14 and 28 months postpartum (Alexander 2009).
The safety of hypnosis for pregnant women was considered in an earlier systematic review (Cyna 2004). There were no reports of adverse effects attributed to the hypnosis intervention in the reviewed trials (Cyna 2004). However, two previously published reports of individual maternal mental disturbances, specifically antenatal psychotic symptoms and treatable postnatal anxiety and compulsive behaviour, were noted (Cyna 2004). The current review will also note any reports of adverse events.
Why it is important to do this review
A range of pharmacological methods of pain management for labour exist; however, not all methods are routinely available across international maternity care settings. Some methods, such as parenteral opioids and epidural, have also been associated with increased risks of adverse maternal effects and increased rates of other medical intervention (Anim‐Somuah 2011; Ullman 2010). The Australian and New Zealand College of Anaesthetists recommends consideration of non‐pharmacological options before pharmacological options for pregnant women as pain medications generally cross the placenta (McIntyre 2010). Hypnosis has been recognised by organisations including the British Medical Association, the American Medical Association and the British Psychological Society as an effective clinical tool (AMA Council on Mental Health 1958; BMA Working Party 1955; BPS Working Party 2001). Like other non‐pharmacological methods of pain management for childbirth, hypnosis can be used autonomously by women in labour and may enhance feelings of self‐confidence, mastery and well‐being (Simkin 2004). Hypnosis interventions appear to be acceptable to some pregnant women with at least two programs widely available for community‐based preparation in high‐income countries (Howell 2009; Mongan 2005).
An earlier Cochrane review of complementary and alternative therapies for pain management in labour found that women taught self‐hypnosis used less pharmacological analgesia and were more satisfied with pain management in labour than women randomised to control conditions (Smith 2006). The authors concluded that hypnosis may be beneficial as a method of pain management in labour but noted that only a small number of women had been studied (Smith 2006). This review updates the evidence in a stand‐alone review.
Objectives
To assess the effectiveness and safety of hypnosis for pain management during labour and childbirth.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and quasi‐randomised controlled trials.
Types of participants
Pregnant women. (This included women in high‐risk groups, e.g. preterm labour or following induction of labour. We planned to use subgroup analysis to assess any possible differences in the effects of hypnosis for these groups where data were available.)
Types of interventions
Preparation for labour using hypnosis and/or use of hypnosis during labour, with or without concurrent use of pharmacological or non‐pharmacological pain‐relief methods versus placebo, no treatment or any analgesic drug or technique.
This review is one in a series of Cochrane reviews examining pain management in labour. These reviews contribute to an overview of systematic reviews of interventions for pain management in labour (Jones 2012), and share a generic protocol (Jones 2011). The current list is as follows.
Placebo/no treatment
Hypnosis (this review)
Biofeedback (Barragán 2011)
Intracutaneous or subcutaneous sterile water injection (Derry 2012)
Immersion in water (Cluett 2009)
Aromatherapy (Smith 2011a)
Relaxation techniques (yoga, music, audio) (Smith 2011c)
Acupuncture or acupressure (Smith 2011b)
Massage, reflexology and other manual methods (Smith 2012)
Transcutaneous electrical nerve stimulation (TENS) (Dowswell 2009)
Inhaled analgesia (Klomp 2012)
Opioids (Ullman 2010)
Non‐opioid drugs (Othman 2012)
Local anaesthetic nerve blocks (Novikova 2012)
Epidural (including combined spinal epidural) (Anim‐Somuah 2011; Simmons 2012)
Types of outcome measures
The protocol for this review was formulated prior to the development of the generic protocol (Jones 2011), the outcome measures include both outcomes that were originally planned as well as all outcomes specified in the generic protocol.
Primary outcomes
Use of pharmacological pain relief or anaesthesia at any time during labour and childbirth (as defined by trialists)
Satisfaction with pain relief (as defined by trialists)
Sense of coping with labour (as defined by trialists)
Spontaneous vaginal birth
Secondary outcomes
Pain intensity (as defined by trialists)
Maternal pain score as measured by visual analogue pain scores or verbal numerical rating scores
Severe pain experienced during the birth (as defined by trialists), measured in labour or postnatally
Sense of control in labour (as defined by trialists)
Satisfaction with childbirth experience (as defined by trialists)
Birth experience worse than expected
Effect (negative) on mother/baby interaction
Breastfeeding at discharge from hospital
Assisted vaginal birth
Caesarean section
Admission to special care baby unit/neonatal intensive care unit (as defined by trialists)
Apgar score less than seven at five minutes
Poor infant outcomes at long‐term follow‐up (as defined by trialists)
Cost (as defined by trialists)
Use of epidural/neuroaxial block as additional analgesia
Preterm birth
Induction of labour
Augmentation of labour with oxytocin
Length of labour (as defined by trialists)
Perineal trauma (defined as episiotomy and incidence of tear ‐ greater than first degree)
Primary postpartum haemorrhage (> 500 mL)
Need for postpartum blood transfusion
Postnatal depressive symptoms (as defined by trialists)
Number of maternal days in hospital after the birth
Number of neonatal days in hospital after the birth
Any other incidences or adverse events, e.g. post‐dural puncture headache; maternal/neonatal death; maternal mental disturbance
Search methods for identification of studies
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group (PCG).
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co‐ordinator (30 September 2015).
The Register is a database containing over 20,000 reports of controlled trials in the field of pregnancy and childbirth. For full search methods used to populate the Pregnancy and Childbirth Group’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link to the editorial information about the Cochrane Pregnancy and Childbirth Group in The Cochrane Library and select the ‘Specialized Register ’ section from the options on the left side of the screen.
Briefly, the Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Search results are screened by two people and the full text of all relevant trial reports identified through the searching activities described above is reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth Group review topic (or topics), and is then added to the Register. The Trials Search Co‐ordinator searches the Register for each review using this topic number rather than keywords. This results in a more specific search set which has been fully accounted for in the relevant review sections (Included and Excluded).
Searching other resources
We searched the reference lists of all available primary studies and review articles and planned to contact the primary authors of known studies to seek other published or unpublished trials.
We did not apply any language or date restrictions.
Data collection and analysis
For methods used in the previous version of this review, seeMadden 2012.
For this update, the following methods were used for assessing the five reports that were identified as a result of the updated search.
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Selection of studies
Two review authors (KM, LJ) independently assessed for inclusion all the potential studies identified as a result of the search strategy. We resolved any disagreement through discussion or, if required, we consulted a third review author.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted a third review author. Data were entered into Review Manager software (RevMan 2014) and checked for accuracy.
When information regarding any of the above was unclear, we contacted authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors (KM, LJ) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreement was resolved by discussion or by involving a third assessor.
When information regarding any of the above was unclear, we planned to contact authors of the original reports to provide further details.
(1) Sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number); or
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal the allocation to control or intervention groups prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth); or
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding was unlikely to affect the results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
low, high or unclear risk of bias for outcome assessors.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we re‐included missing data in our analyses. We assessed methods as:
low risk of bias (e.g. where there were no missing data or where reasons for missing data were balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; 'as treated' analysis done with substantial departure of intervention received from that assigned at randomisation); or
unclear risk of bias.
(5) Selective reporting bias (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it was clear that all of the study’s prespecified outcomes and all expected outcomes of interest to the review were reported);
high risk of bias (where not all the study’s prespecified outcomes were reported; one or more reported primary outcomes were not prespecified; outcomes of interest were reported incompletely and so could not be used; the study failed to include results of a key outcome that would have been expected to have been reported); or
unclear risk of bias.
(6) Other sources of bias (checking for bias due to problems not covered in (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias. For example, where there was a potential source of bias related to a specific study design or where a trial was stopped early due to some data‐dependent process.
We assessed whether each study was free of other problems that could put it at risk of bias and categorise as:
low risk of other bias;
high risk of other bias; or
unclear whether there was a risk of other bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered it was likely to impact on the findings. We explored the impact of the level of bias through undertaking sensitivity analyses, seeSensitivity analysis.
Assessment of the quality of the evidence using GRADE
For this update we assessed the quality of the evidence using the GRADE approach as outlined in the GRADE Handbook in order to assess the quality of the body of evidence relating to the following outcomes for the main comparisons (self‐hypnosis or hypnotherapy versus all).
Use of pharmacological pain relief or anaesthesia at any time during labour and childbirth (as defined by trialists)
Satisfaction with pain relief (as defined by trialists)
Sense of coping with labour (as defined by trialists)
Spontaneous vaginal birth
We used the GRADEpro Guideline Development Tool to import data from Review Manager 5.3 (RevMan 2014) in order to create a ’Summary of findings’ table. A summary of the intervention effect and a measure of quality for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
For continuous data, we used the mean difference if outcomes were measured in the same way between trials. In future updates, if appropriate, we will use the standardised mean difference to combine trials that measured the same outcome, but used different methods.
Ordinal data
For ordinal data measured on scales (e.g. pain measured on visual analogue scales), we planned to analyse as continuous data and express the intervention effect as a difference in means or standardised difference in means. For ordinal data (e.g. satisfaction with pain relief) measured on shorter ordinal scales (e.g. excellent, very good, good), we planned to analyse as dichotomous data by combining categories (e.g. excellent and very good) and express the intervention effect using risk ratios.
Unit of analysis issues
Cluster‐randomised trials
No cluster‐randomised trials were included in this update. In future updates, if identified and eligible, we will include cluster‐randomised trials in the analyses along with individually‐randomised trials. We will adjust either their sample sizes or standard errors using the methods described in the Handbook [Section 16.3.4 or 16.3.6] using an estimate of the intra cluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity analysis to investigate the effects of the randomisation unit.
Cross‐over trials
Cross‐over trials are not a suitable study design for inclusion in this review.
Multiple treatment groups
In order to overcome unit‐of‐analysis errors for studies that include multiple relevant treatment arms, we combined groups to create single pair‐wise comparisons. For example, in Werner 2013, there were three randomised groups: a hypnosis, a relaxation and a usual care group. In the overall comparison for hypnosis versus all, we combined the dichotomous and continuous data from the relaxation and usual care group into one single group. We used the methods outlined in the Cochrane Handbook [Chapter 16.5, 7.7.3.8].
Dealing with missing data
For included studies, we noted levels of attrition. We planned to explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using Sensitivity analysis.
For all outcomes we carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses, and analysed all participants in the group to which they were allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if an I² was greater than 30% and either a Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity.
Assessment of reporting biases
Had there been 10 or more studies in the meta‐analysis, we planned to investigate reporting biases (such as publication bias) using funnel plots. We planned to assess funnel plot asymmetry visually. If asymmetry was suggested by a visual assessment, we planned to perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where trials were examining the same intervention, and the trials' populations and methods were judged sufficiently similar. If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. We treated the random‐effects summary as the average of the range of possible treatment effects and discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we did not combine trials.
Where we used random‐effects analyses, we have presented the results as the average treatment effect with its 95% confidence interval, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
We investigated substantial heterogeneity using subgroup analyses and sensitivity analyses. We considered whether an overall summary was meaningful, and if it was, used random‐effects analysis to produce it.
We planned to carry out the following subgroup analyses, but it was only possible to carry out subgroup analysis for five of the subgroups (in bold below).
Spontaneous labour versus induced labour.
Primiparous/nulliparous versus multiparous.
Term versus preterm birth.
Continuous support in labour versus no continuous support.
Trimester (first versus second versus third trimester; first and second trimester versus third trimester) at commencement of hypnosis sessions.
Number of hypnosis sessions (less than four versus four or more).
Method of hypnosis intervention delivery (one‐to‐one versus group classes, audio CD versus no audio CD, hypnosis preparation prior to labour versus practitioner‐assisted hypnosis in labour).
Maternal anxiety levels (high versus low).
Maternal hypnotisability (high versus low).
We restricted subgroup analysis to the primary outcomes.
We assessed subgroup differences by interaction tests available within RevMan (RevMan 2014). We reported the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
Sensitivity analysis
We carried out sensitivity analysis to explore the effect of trial quality for primary outcomes in the review. Where there was risk of bias associated with a particular aspect of study quality (e.g. inadequate allocation concealment), we explored this by sensitivity analyses.
Results
Description of studies
SeeCharacteristics of included studies; Characteristics of excluded studies.
Results of the search
We identified a total of 24 reports (11 studies) from the search strategy. Six of these reports were identified in an updated search conducted in September 2015. A total of nine studies (22 reports) reporting data on 2954 women were included in this review. Two studies were excluded (seeCharacteristics of excluded studies).
Included studies
Study design
All nine studies were parallel design (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Rock 1969; Werner 2013) comparing self‐hypnosis or hypnotherapy with a control group or groups. Two studies were quasi‐randomised controlled trials (Harmon 1990; Rock 1969). Five studies had two groups (Downe 2015; Fisher 2009; Freeman 1986; Harmon 1990; Rock 1969), two studies had three groups (Cyna 2011; Werner 2013), and two studies had two randomised groups plus another 'comparison' group (Martin 2001; Mehl‐Madrona 2004), but only the data from the two randomised groups were considered as part of this review. The control groups consisted of the following: standard care (including routine childbirth education classes) (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Rock 1969; Werner 2013), relaxation training (Harmon 1990), relaxation and mindfulness training (Werner 2013); supportive counselling (Martin 2001) and supportive psychotherapy (Mehl‐Madrona 2004). For this update it was decided to conduct separate comparisons for the different types of control group, comparing hypnosis with: standard care (Comparison 2), supportive counselling (Comparison 3), and relaxation training (Comparison 4). For the purposes of the review, the control groups supportive counselling (Martin 2001) and supportive psychotherapy (Mehl‐Madrona 2004) were judged to be similar enough to be combined as supportive counselling. Similarly, the control groups relaxation training (Harmon 1990) and relaxation and mindfulness training (Werner 2013) were judged to be similar enough to be combined as relaxation training. One study used two methods of delivering the hypnosis training (Cyna 2011).
Sample sizes
Sample size in the included studies ranged from 38 (Fisher 2009) to 1222 (Werner 2013).
Study location
Five of the studies were conducted in the USA (Fisher 2009; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Rock 1969), two in the UK (Downe 2015; Freeman 1986), one in Australia (Cyna 2011), and one in Denmark (Werner 2013).
Participants
Five studies recruited both nulliparous and multiparous women (Cyna 2011; Fisher 2009; Martin 2001; Mehl‐Madrona 2004; Rock 1969) and four studies recruited only nulliparous women (Downe 2015; Freeman 1986; Harmon 1990; Werner 2013). One study only recruited women aged 18 years or younger (Martin 2001). For further information about inclusion and exclusion criteria for each study, seeCharacteristics of included studies.
Types of intervention
In eight studies the intervention was antenatal hypnosis training (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Werner 2013) which was taught in group classes (Cyna 2011; Downe 2015; Fisher 2009; Harmon 1990; Werner 2013) or during individual consultations (Freeman 1986; Martin 2001; Mehl‐Madrona 2004). In one study, the intervention was hypnosis provided during labour (Rock 1969). One trial had two intervention groups as well as the usual care control group (Cyna 2011). In one intervention group, women listened to 'live' hypnosis in antenatal classes led by a hypnotherapist and a hypnosis audio CD was provided for home practice (Cyna 2011). In the other intervention group, women listened to the same hypnosis audio CD at antenatal classes led by a nurse without training in hypnosis and were also provided with the audio CD for home practice (Cyna 2011). The live hypnosis intervention is similar to the other antenatal self‐hypnosis trials so has been included in the main comparisons and all subgroup comparisons for this review. A separate set of comparisons for the nurse/CD group versus control has been reported as Comparison 5 and for a subgroup comparison regarding method of hypnosis.
The hypnosis intervention began in the first or second trimester of pregnancy in one study (Mehl‐Madrona 2004), in the second trimester in one study (Martin 2001), and in the third trimester in five studies (Cyna 2011; Downe 2015; Freeman 1986; Harmon 1990; Werner 2013). The intervention began during labour in one study (Rock 1969). It was not clear when in the pregnancy the intervention began in one study (Fisher 2009). One study provided two 90‐minute intervention sessions at approximately 32 weeks' and 35 weeks' gestation (Downe 2015). Four studies involved weekly intervention sessions (Cyna 2011; Freeman 1986; Harmon 1990; Werner 2013). In one study these sessions started at 32 weeks' gestation and continued until the birth (Freeman 1986), and in one study a series of six weekly classes were scheduled (Harmon 1990). In two studies there were three‐weekly intervention sessions (Cyna 2011; Werner 2013), for one of these trials, the sessions started as closely as possible to 37 weeks' gestation (Cyna 2011). In four studies women were also provided with an audio recording for daily practice at home (Cyna 2011; Downe 2015; Harmon 1990; Werner 2013). In one study there were four intervention sessions spanning approximately eight weeks (Martin 2001). One study reported that women could attend for hypnotherapy as often as desired (subject to therapist availability) (Mehl‐Madrona 2004). It was not clear how many intervention sessions were provided for one study (Fisher 2009). In the study where hypnosis was provided during labour, the hypnotherapist was a medical student who also performed routine labour assessments (Rock 1969). The hypnotic induction took an average of 20 minutes and it was reported that the total time added by the hypnotic procedures was 45 minutes longer than with usual care (Rock 1969).
Outcome measures
The following primary outcomes were reported upon in the studies: use of pharmacological pain relief or anaesthesia during labour and childbirth (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Rock 1969; Werner 2013); satisfaction with pain relief (Cyna 2011; Downe 2015); sense of coping with labour (Cyna 2011; Downe 2015; Fisher 2009) spontaneous vaginal birth (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Werner 2013).
The following secondary outcomes were reported upon in the studies: pain intensity (Downe 2015; Freeman 1986; Harmon 1990; Werner 2013); maternal pain score (Cyna 2011); satisfaction with the childbirth experience (Cyna 2011; Freeman 1986; Werner 2013); birth experience worse than expected (Werner 2013); breastfeeding at hospital discharge (Cyna 2011; Downe 2015; Werner 2013); assisted vaginal birth (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Werner 2013); caesarean section (Cyna 2011; Downe 2015; Fisher 2009; Martin 2001; Mehl‐Madrona 2004; Werner 2013); admission to special care baby unit/neonatal intensive care unit (Cyna 2011; Downe 2015; Martin 2001; Werner 2013); Apgar score (Cyna 2011; Fisher 2009; Harmon 1990; Mehl‐Madrona 2004; Werner 2013); use of epidural (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Mehl‐Madrona 2004; Rock 1969; Werner 2013); preterm birth (Werner 2013); length of labour (Cyna 2011; Downe 2015; Freeman 1986; Harmon 1990; Martin 2001; Werner 2013); perineal trauma (Werner 2013); induction of labour (Cyna 2011; Downe 2015; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Werner 2013); augmentation of labour with oxytocin (Cyna 2011; Downe 2015; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Werner 2013); primary postpartum haemorrhage (Cyna 2011; Mehl‐Madrona 2004; Werner 2013); cost (Downe 2015); need for postpartum blood transfusion (Cyna 2011; Downe 2015); postnatal depressive symptoms (Cyna 2011; Downe 2015; Harmon 1990; Mehl‐Madrona 2004; Rock 1969; Werner 2013); number of maternal days in hospital after the birth (Martin 2001); any other adverse events (maternal side effects, newborn resuscitation) (Cyna 2011; Downe 2015; Mehl‐Madrona 2004).
Excluded studies
We excluded two studies, one where the hypnotherapeutic programme was not used for pain management during labour and childbirth (Guse 2006) and one which did not use hypnosis as an intervention and did not appear to be a randomised or quasi‐randomised controlled trial (Hao 1997) (seeCharacteristics of excluded studies for further details).
Risk of bias in included studies
SeeFigure 1; Figure 2, for further details regarding 'Risk of bias' assessment.
1.
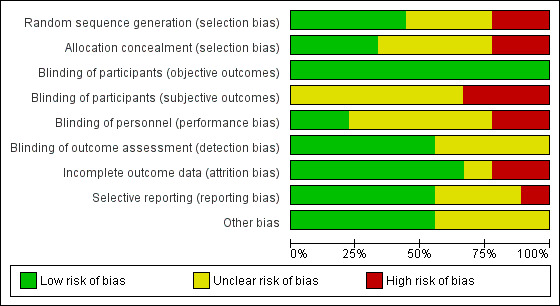
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
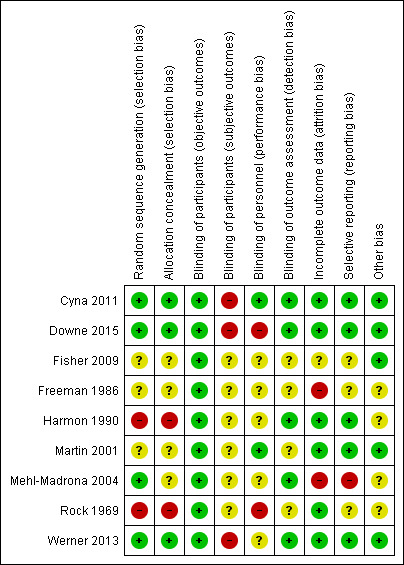
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Three of the nine trials (Cyna 2011; Downe 2015; Werner 2013) had a low risk of bias for both random sequence generation and allocation concealment: they all used computer‐based random number generators and concealed allocation using centralised allocation via telephone (Cyna 2011), via a password protected participant management database (Downe 2015), and by an interactive voice response system (Werner 2013). Two trials were quasi‐randomised trials and therefore were at high risk of selection bias (allocated based on hospital number in Rock 1969 and the month the woman was due in Harmon 1990). In three trials, method of randomisation and allocation concealment were not reported and so they were assessed as unclear for selection bias (Fisher 2009; Freeman 1986; Martin 2001). In one study (Mehl‐Madrona 2004), risk of bias was low for random sequence generation (computer‐based random number generator), but the method for allocation concealment was not reported and so allocation concealment was assessed as unclear.
Blinding
Blinding of participants is difficult for hypnosis interventions but four trials reported that women were not told which group they were allocated to (Cyna 2011; Harmon 1990; Martin 2001; Rock 1969). We considered that participants knowledge of their group allocation may have an impact on subjective outcomes (such as satisfaction with pain relief) but was unlikely to have an impact on objective outcomes (such as spontaneous vaginal birth). We assessed risk of bias separately for subjective and objective outcomes where studies reported that blinding of participants had been attempted. All studies were rated as low risk of bias for objective outcomes as lack of blinding is unlikely to have an impact on objective outcomes. Three studies (33%) were rated as unclear risk of bias for subjective outcomes (Harmon 1990; Martin 2001; Rock 1969) as women were not told their group allocation, but there was no reporting about whether blinding was successful. Only one trial (11%) reported data about the success of blinding for participants (Cyna 2011). This trial was rated at high risk of bias for subjective outcomes as results showed that none of the women in the control group believed they were in a hypnosis group and more than 70% of women in the two intervention groups believed they were in a hypnosis group (Cyna 2011). Two trials (22%) did not attempt to blind women to their group allocations (Downe 2015; Werner 2013) so were rated at high risk of bias for subjective outcomes. Three studies (33%) were rated as unclear risk of bias for blinding of participants for subjective outcomes (Fisher 2009; Freeman 1986; Mehl‐Madrona 2004) as they did not report whether any attempt was made to blind the women to their group allocation.
It is not possible for personnel providing hypnosis interventions to be blinded to the intervention but it is possible for personnel caring for a woman in labour to be blinded so assessment of blinding of personnel in this review relates to blinding of the personnel who cared for the woman during labour. Blinding of personal was assessed as low risk of bias in two studies (Cyna 2011; Martin 2001) (22%) and at high risk of bias for two trials (Downe 2015; Rock 1969) (22%). The risk of bias was unclear in the remaining studies (56%) as there was either no reporting of whether personnel were blinded to group allocation (Fisher 2009; Freeman 1986; Harmon 1990; Mehl‐Madrona 2004), or the blinding that was attempted was only partially effective (Werner 2013).
Blinding of outcome assessment was at low risk of bias in five studies (Cyna 2011; Downe 2015; Harmon 1990; Mehl‐Madrona 2004; Werner 2013) (56%) and unclear in the remaining studies (44%). Two studies did not report whether outcome assessors were blinded to group allocation (Fisher 2009; Freeman 1986), and in two studies it was unclear from what was reported whether outcome assessors were blinded (Martin 2001; Rock 1969).
Incomplete outcome data
Six of the trials (67%) were rated as low risk of bias for incomplete outcome data (Cyna 2011; Downe 2015; Harmon 1990; Martin 2001; Rock 1969; Werner 2013). In one trial the intervention was provided in labour and no losses of participants were reported (Rock 1969). In one study all primary and secondary outcomes for eligible trial participants were analysed using the intention‐to‐treat principle (Cyna 2011). In one trial one woman was excluded following randomisation after becoming ineligible for inclusion in the study (Harmon 1990). Similarly, in one trial five women were excluded (four from the hypnosis group and one from the relaxation group) due to not meeting the inclusion criteria (Werner 2013). In one trial three women randomised in error were withdrawn, two requested withdrawal and three were lost to follow‐up, these losses were reported to be balanced across groups and unlikely to be related to the intervention (Downe 2015). Similarly, in another trial the reasons for the five participants lost to follow‐up were unlikely to have been related to the intervention or were balanced between groups (three moved out of the geographic area and one from each group did not complete the research protocol) (Martin 2001). Two trials were assessed as high risk of bias (Freeman 1986; Mehl‐Madrona 2004) (22%). In Freeman 1986, losses appeared to be related to the intervention, four participants from the hypnosis condition were excluded as they did not attend for hypnosis. In the other trial, women from the hypnosis group were excluded from data analysis if they were diagnosed with a range of mental illnesses, but it was unclear whether women from the control group were excluded on the same basis (Mehl‐Madrona 2004). In the remaining study risk of bias for incomplete outcome data was unclear (11%) as there was no reporting of how many participants were lost to follow‐up (Fisher 2009).
Selective reporting
Five of the trials (56%) were rated as low risk of bias for selective outcome reporting (Cyna 2011; Downe 2015; Harmon 1990; Martin 2001; Werner 2013). In two trials all of the outcomes listed in the trial registration were reported or provided (Cyna 2011; Downe 2015), in two trials all of the outcomes listed in the hypotheses were reported (Harmon 1990; Martin 2001), and in one trial all but one from a long list of outcomes were reported or provided (Werner 2013). One study (11%) was assessed as being at high risk of bias (Mehl‐Madrona 2004) as not all of the outcomes outlined in the study were fully reported. In the remaining three studies (33%) risk of bias for was unclear (Fisher 2009; Freeman 1986; Rock 1969) as one report was a conference abstract so detailed data were not reported (Fisher 2009) and two studies reported narrative descriptions with P values without frequency data for one outcome (Freeman 1986; Rock 1969).
Other potential sources of bias
Five of the trials (56%) were rated as being at low risk of bias for other bias (Cyna 2011; Downe 2015; Fisher 2009; Martin 2001; Werner 2013) based on balance in demographic characteristics of participants at baseline and no other issues of concern identified. In the remaining four studies (44%) risk of bias was unclear (Freeman 1986; Harmon 1990; Mehl‐Madrona 2004; Rock 1969) as little or no demographic data were reported for the intervention and control groups.
Effects of interventions
See: Table 1
Comparison 1 ‐ Self‐hypnosis or hypnotherapy versus any other intervention or control
Primary outcomes
Use of pharmacological pain relief or anaesthesia during labour and childbirth
All nine studies measured this outcome (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Rock 1969; Werner 2013), but one study did not report any numerical data so could not be included in the analysis (Fisher 2009). Two studies (Harmon 1990; Rock 1969) reported the use of tranquillizers but these were not considered to be pain relief for the purposes of this review. Therefore, the data for Harmon 1990 and Rock 1969 used in this outcome relate to the use of narcotics only. One study (Freeman 1986) combined women who used the inhaled analgesic Entonox with those who used no analgesia so only those who were reported as using pethidine and/or epidural were included as using pharmacological pain relief or anaesthesia.
Women in the hypnosis group were less likely to use pharmacological pain relief or anaesthesia during labour and childbirth, (average risk ratio (average RR) 0.73, 95% confidence interval (CI) 0.57 to 0.94, eight studies, 2916 women; very low‐quality evidence). There was substantial statistical heterogeneity: I² = 91%, Tau² = 0.10, Chi² test for heterogeneity P < 0.01, and so we used a random‐effects model, Analysis 1.1. It is likely that the Harmon 1990 and Mehl‐Madrona 2004 trials contributed to the high level of heterogeneity. The Harmon 1990 trial was a quasi‐randomised controlled trial so is subject to a high risk of selection bias. The other quasi‐randomised controlled trial (Rock 1969) also favoured hypnosis but not as strongly as the Harmon 1990 or Mehl‐Madrona 2004 trials. For the Mehl‐Madrona 2004 trial, it is not clear whether the timing of the intervention and/or some other characteristic of the trial explains the result strongly favouring the intervention.
1.1. Analysis.
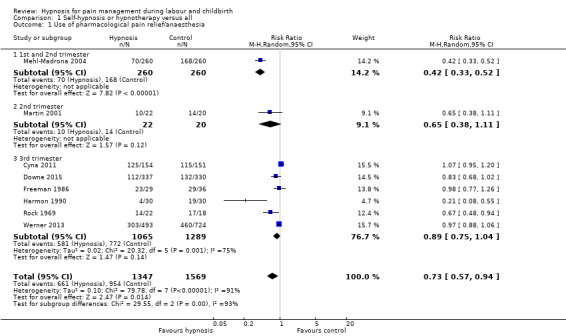
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 1 Use of pharmacological pain relief/anaesthesia.
Subgroup analysis indicated that there may have been an interaction between the trimester at commencement of hypnosis sessions and use of pharmacological analgesia (test for subgroup differences P < 0.01, I² = 93.2%, (Analysis 1.1). In one trial (n = 520), women commenced hypnosis in the first or second trimester (RR 0.42, 95% CI 0.33 to 0.52). In one trial (n = 42), women commenced hypnosis in the second trimester (RR 0.65, 95% CI 0.38 to 1.11). In six trials (n = 2354), women commenced hypnosis in the third trimester (average RR 0.89, 95% CI 0.75 to 1.04). Thus, the use of pharmacological analgesia may have been lower when women commenced hypnosis in the first or second trimester. However, data were only available for one trial where the intervention was provided in the first or second trimester (Mehl‐Madrona 2004) so, as noted above, it is not clear whether the result was related to the timing of the intervention and/or some other characteristic of the trial.
As noted, one trial had a second intervention; this group of women listened to an audio CD of hypnosis as part of antenatal sessions with a nurse without training in hypnotherapy (Cyna 2011). This group will be referred to as the 'nurse/audio CD group'. No clear difference was found in the proportion of women who used pharmacological pain relief or analgesia in the nurse/audio CD group compared with the control group (RR 1.01, 95% CI 0.89 to 1.15, one study, 294 women), Analysis 5.1.
5.1. Analysis.
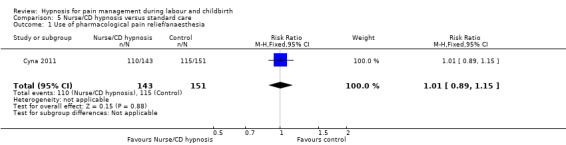
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 1 Use of pharmacological pain relief/anaesthesia.
Satisfaction with pain relief
Two studies reported on this outcome (Cyna 2011; Downe 2015). The data were reported in different ways in the two studies and so could not be combined in one analysis. In one study Cyna 2011, there was no clear difference identified between the hypnosis and control group in the proportion of women who reported that they received adequate pain relief (RR 1.06, 95% CI 0.94 to 1.20, one study, 264 women; low‐quality evidence), Analysis 1.2. The other study (Downe 2015), reported satisfaction with pain relief for specific pain relief methods and found no clear difference in satisfaction according to a postnatal questionnaire two weeks postpartum for pethidine (mean difference (MD) 0.41, 95% CI ‐0.45 to 1.27, 72 women; low‐quality evidence), Entonox (MD 0.19, 95% CI ‐0.19 to 0.57, 357 women; low‐quality evidence), self‐hypnosis (MD 0.28, 95% CI ‐0.32 to 0.88, 160 women; low‐quality evidence), epidural (MD ‐0.03, 95% CI ‐0.40 to 0.34; low‐quality evidence), although women in the hypnosis group who had water immersion reported being more satisfied (MD 0.52, 95% CI 0.04 to 1.00, 174 women; low quality evidence), Analysis 1.3. Satisfaction was measured on a seven‐point scale, with seven indicating most satisfaction.
1.2. Analysis.
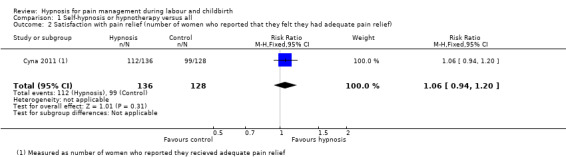
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 2 Satisfaction with pain relief (number of women who reported that they felt they had adequate pain relief).
1.3. Analysis.
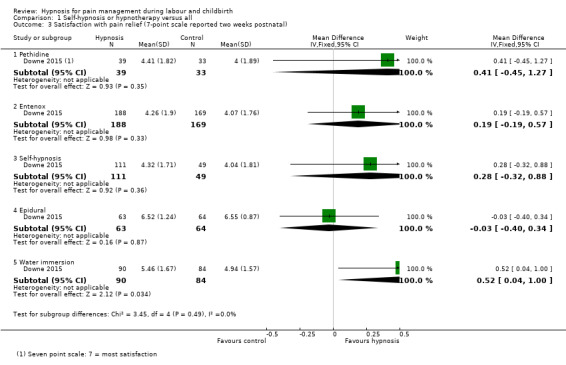
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 3 Satisfaction with pain relief (7‐point scale reported two weeks postnatal).
There was also no clear difference in the proportion of women who reported they received adequate pain relief between the nurse/CD group and the control group (RR 0.91, 95% CI 0.78 to 1.05, one study, 259 women), Analysis 5.2.
5.2. Analysis.
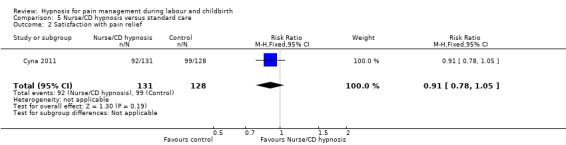
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 2 Satisfaction with pain relief.
Sense of coping with labour
Three studies reported on this outcome (Cyna 2011; Downe 2015; Fisher 2009), but two of the studies did not report data in a way that could be analysed for the review (Cyna 2011; Fisher 2009). Cyna 2011 reported women's perceptions of coping with childbirth postnatally prior to their discharge from hospital stating that there was no clear difference in median interquartile ranges (IQR) 7 (3) versus 8 (3) on a 10‐point scale. Fisher 2009 reported: "a greater ability to cope during childbirth after hypnosis course completion compared to the conventional group. However, after delivery, the hypnosis group recalled relatively poorer intrapartum coping skills (P = 0.02)".
One study (Downe 2015) measured coping on a seven‐point scale and did not find a difference between women in the hypnosis group and those in the control group (MD 0.22, 95% CI ‐0.14 to 0.58, one study, 420 women; low‐quality evidence), Analysis 1.4.
1.4. Analysis.
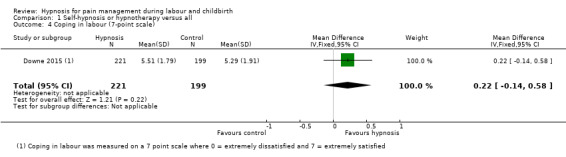
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 4 Coping in labour (7‐point scale).
Spontaneous vaginal birth
Eight studies reported on this outcome (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Werner 2013), but data were only available for analysis from six studies (Cyna 2011; Downe 2015; Freeman 1986; Harmon 1990; Martin 2001; Werner 2013). One trial did not report numerical data for this outcome (Fisher 2009) and one trial reported data grouped as 'uncomplicated births' and 'complicated births' (Mehl‐Madrona 2004). Although the uncomplicated births group only included spontaneous vaginal births, the complicated births group included both spontaneous vaginal births and surgically‐assisted births. This meant that the overall number of spontaneous vaginal births could not be calculated (for example, if a woman had a spontaneous vaginal birth followed by a postpartum haemorrhage she was included in the complicated birth group) (Mehl‐Madrona 2004).
No clear difference was found between the hypnosis and control group in the proportion of women having a spontaneous vaginal birth (average RR 1.12, 95% CI 0.96 to 1.32, six studies, 2361 women; low‐quality evidence). There was substantial statistical heterogeneity: I² = 73%, Tau² = 0.02, Chi² test for heterogeneity P < 0.01, and so we used a random‐effects model, Analysis 1.5. It is likely that the Martin 2001 trial contributed to the high level of heterogeneity. This trial included only women aged 18 years or younger and involved hypnosis preparation for labour provided one‐on‐one from the second trimester. It is not clear which, if any, of these factors may help explain the heterogeneity.
1.5. Analysis.
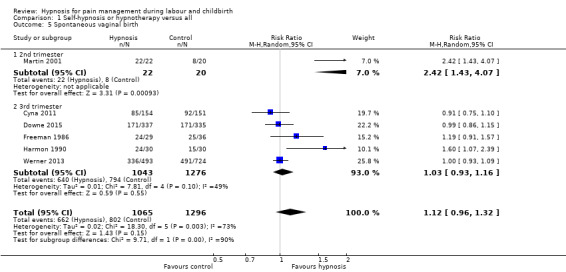
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 5 Spontaneous vaginal birth.
Subgroup analysis indicated that there may have been an interaction between trimester at commencement of hypnosis sessions and spontaneous vaginal birth (test for subgroup differences P = 0.002, I² = 89.7%, Analysis 1.5). In one trial (n = 42), women commenced hypnosis in the second trimester (RR 2.42, 95% CI 1.43 to 4.07). In five trials (n = 2319), women commenced hypnosis in the third trimester (average RR 1.03, 95% CI 0.93 to 1.16). Thus, the likelihood of spontaneous vaginal birth may have been greater when women commenced hypnosis in the second trimester. However, data were only available for one trial where the intervention was provided in the second trimester (Martin 2001) so it is not clear whether the result was related to the timing of the intervention and/or some other characteristic of the trial.
There was no clear difference in the proportion of women who had a spontaneous vaginal birth between those in the nurse/audio CD group compared with those in the control group (RR 0.96, 95% CI 0.80 to 1.16, one study, 294 women), Analysis 5.3.
5.3. Analysis.
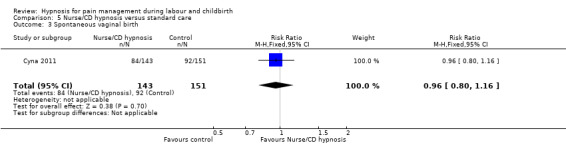
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 3 Spontaneous vaginal birth.
Secondary outcomes
Pain intensity
Four studies reported on this outcome (Downe 2015; Freeman 1986; Harmon 1990; Werner 2013), but data were only available for analysis from two studies (Downe 2015; Harmon 1990). In the one study no numerical data were reported but it was noted that there was no clear difference between the two groups in terms of efficacy of pain relief on a linear analogue scale (Freeman 1986). In one study (Werner 2013) data were reported as medians (Mdn) and IQR at specific points in the labour for women who received epidural analgesia and women who did not receive epidural. No clear differences were found between intervention and control groups for any specific point in the labour
In one study the mean pain score in the hypnosis group was lower than the mean pain score in the control group according to the present pain intensity scale of the McGill Pain Questionnaire, (where, 0 = No pain, 1 = Mild, 2 = Discomforting, 3 = Distressing, 4 = Horrible, 5 = Excruciating), (MD ‐0.70, 95% CI‐1.03 to ‐0.37, one study, 60 women), Analysis 1.6. However, in the other study (Downe 2015), no clear difference was found for memory of labour pain reported at two weeks postnatally on a 100‐point scale as "Worst imaginable" (MD 0.05, 95% CI ‐4.14 to 4.24, one study, 430 women) Analysis 1.7 or as "Completely unbearable" (MD ‐0.26, 95% CI ‐4.92 to 4.40, one study, 429 women) Analysis 1.7.
1.6. Analysis.
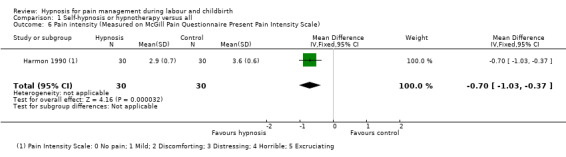
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 6 Pain intensity (Measured on McGill Pain Questionnaire Present Pain Intensity Scale).
1.7. Analysis.
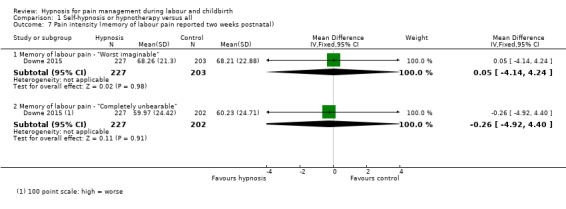
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 7 Pain intensity (memory of labour pain reported two weeks postnatal).
Maternal pain score as measured by visual analogue pain scores of verbal numerical rating scales
One study reported on this outcome (Cyna 2011), but the results were reported as Mdn and IQR (as is appropriate for ordinal level data) so was not in a format suitable for analysis as part of the review. However, no clear differences were reported between the scores for the hypnosis group (Mdn 8, IQR 2), the control group (Mdn 8, IQR 2) and the nurse/CD only group (Mdn 8, IQR 2).
Severe pain experienced during the birth, measured in labour or postnatally
None of the studies reported data for this outcome.
Sense of control in labour
None of the studies reported data for this outcome.
Satisfaction with the childbirth experience
Three studies reported on this outcome (Cyna 2011; Freeman 1986; Werner 2013). One study measured this outcome as the number of women who reported being "very satisfied" (score 8 to 10 on linear analogue scale) with labour (Freeman 1986), one trial measured it as the number of women who reported the birth as a positive experience (Cyna 2011), and one trial measured satisfaction on a continuous scale using the Wijmas Delivery Experience Questionaire (Werner 2013).
For the dichotomous data no clear difference was found for satisfaction with the childbirth experience between women in the hypnosis group and women in the control group (average RR 1.36, 95% CI 0.52 to 3.59, two studies, 370 women). There was substantial statistical heterogeneity: I² = 87%, Tau² = 0.43, Chi² test for heterogeneity P < 0.01, and so we used a random‐effects model, Analysis 1.8. As there were only two trials, it is not clear which differences between the trials could explain this heterogeneity, for example, the Freeman 1986 trial was much smaller, the hypnosis intervention began earlier in the pregnancy and involved more sessions than the Cyna 2011 trial.
1.8. Analysis.
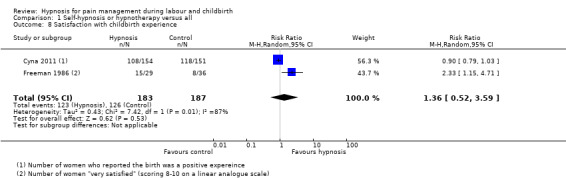
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 8 Satisfaction with childbirth experience.
For the continuous data, women in the hypnosis group were found to have a more positive experience of childbirth (MD ‐4.40, 95% CI ‐7.22 to ‐1.58, one study, 1126 women), Analysis 1.9 (lower scores represent a more positive experience).
1.9. Analysis.
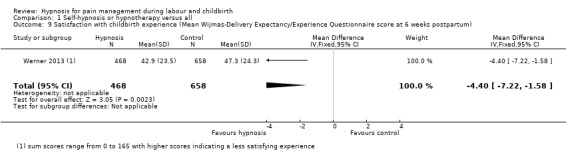
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 9 Satisfaction with childbirth experience (Mean Wijmas‐Delivery Expectancy/Experience Questionnaire score at 6 weeks postpartum).
No clear difference was found between the nurse/audio CD group and the control group for satisfaction with the childbirth experience (RR 0.94, 95% CI 0.83 to 1.07, one study, 294 women), Analysis 5.4.
5.4. Analysis.
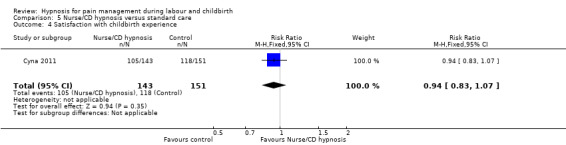
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 4 Satisfaction with childbirth experience.
Birth experience worse than expected
Only one study reported on pain influence on birth experience in a negative direction (Werner 2013). The data were not reported in a format that could be included in the analysis, but no clear difference was found for median scores for the hypnosis group 2 (IQR 5), relaxation group 2 (5) and standard care group 2 (4).
Effect (negative) on mother/baby interaction
None of the studies reported data for this outcome.
Breastfeeding at discharge
Three studies reported on breastfeeding (Cyna 2011; Downe 2015; Werner 2013), however there were some differences in the time point when breastfeeding was reported. The Cyna 2011 trial reported at discharge from hospital, the Downe 2015 trial reported at six weeks postnatally and the Werner 2013 trial reported at one month or more. No clear difference was found in the proportion of women who reported any breastfeeding between the hypnosis group and the control group (average RR 1.01, 95% CI 0.98 to 1.06, three studies, 1826 women), Analysis 1.10. There was also no clear difference between the nurse/audio CD group and the control group for this outcome (RR 1.01, 95% CI 0.98 to 1.04, one study, 294 women), Analysis 5.5.
1.10. Analysis.
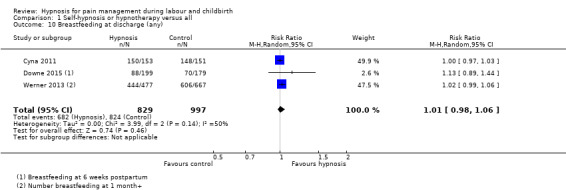
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 10 Breastfeeding at discharge (any).
5.5. Analysis.
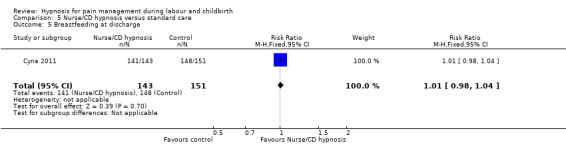
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 5 Breastfeeding at discharge.
Assisted vaginal birth
Eight studies measured this outcome (Cyna 2011; Downe 2015; Freeman 1986; Fisher 2009, Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Werner 2013) but data were only available for analysis from six studies (Cyna 2011; Downe 2015; Freeman 1986; Harmon 1990; Martin 2001; Werner 2013). One study did not report numerical data for this outcome (Fisher 2009) and one study grouped assisted vaginal births within a complicated birth group which included a range of complications as outlined above (Mehl‐Madrona 2004).
No clear difference was found in the proportion of women who had assisted vaginal births between the women in the hypnosis group and those in the control group (average RR 0.80, 95% CI 0.63 to 1.03, six studies, 2363 women). There was moderate statistical heterogeneity: I² = 32%, Tau² = 0.03, Chi² test for heterogeneity P = 0.19, so we used a random‐effects model, Analysis 1.11. It does not appear that any individual trial was responsible for this heterogeneity.
1.11. Analysis.
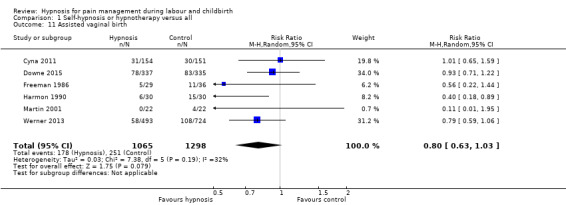
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 11 Assisted vaginal birth.
No clear difference was found between women in the nurse/audio CD group and women in the control group for assisted vaginal birth (RR 1.20, 95% CI 0.78 to 1.85, one study, 294 women), Analysis 5.6.
5.6. Analysis.
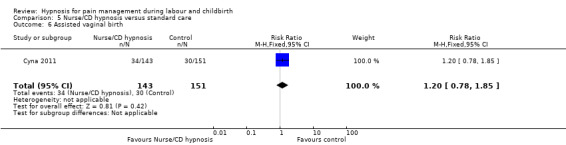
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 6 Assisted vaginal birth.
Caesarean section
Six studies reported upon this outcome (Cyna 2011; Downe 2015; Fisher 2009; Martin 2001; Mehl‐Madrona 2004; Werner 2013), but one study did not report numerical data so was not able to be included in the analysis (Fisher 2009). No clear difference was found in the proportion of women who had a caesarean section between those in the hypnosis group and the control group (average RR 0.90, 95% CI 0.60 to 1.34, five studies, 2756 women). There was substantial statistical heterogeneity: I² = 79%, Tau² = 0.14, Chi² test for heterogeneity P < 0.01, and so we used a random‐effects model, Analysis 1.12. It is likely that the Martin 2001 trial contributed to the high level of heterogeneity. This trial included only women aged 18 years or younger and involved hypnosis preparation for labour provided one‐on‐one from the second trimester. It is not clear which, if any, of these factors may help explain the heterogeneity.
1.12. Analysis.
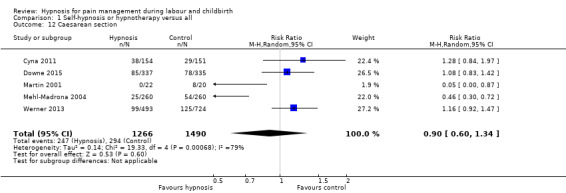
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 12 Caesarean section.
There was no clear difference between women in the nurse/audio CD group and women in the control group for caesarean section (RR 0.91, 95% CI 0.56 to 1.48, one study, 294 women), Analysis 5.7.
5.7. Analysis.
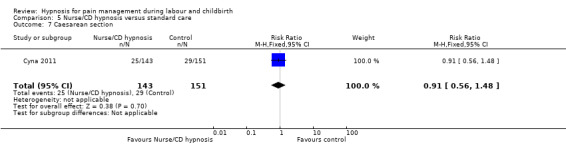
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 7 Caesarean section.
Admission to special care baby unit/neonatal intensive care unit
Four studies reported on this outcome (Cyna 2011; Downe 2015; Martin 2001; Werner 2013). No clear difference was found for admissions to the neonatal intensive care unit for babies born to the mothers in the hypnosis group compared with babies born to mothers in the control group (average RR 1.06, 95% CI 0.86 to 1.30, four studies, 2233 women). There was little statistical heterogeneity: I² = 16%, Tau² = 0.01, Chi² test for heterogeneity P = 0.31, so we used a fixed‐effect model, Analysis 1.13.
1.13. Analysis.
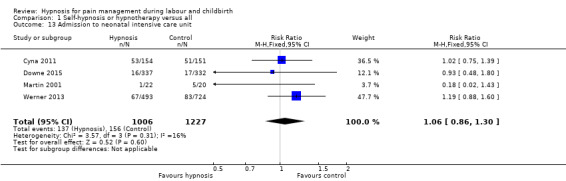
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 13 Admission to neonatal intensive care unit.
There was no clear difference between women in the nurse/audio CD group and women in the control group for babies admitted to the neonatal intensive care unit (RR 0.93, 95% CI 0.67 to 1.29, one study, 294 women), Analysis 5.8.
5.8. Analysis.
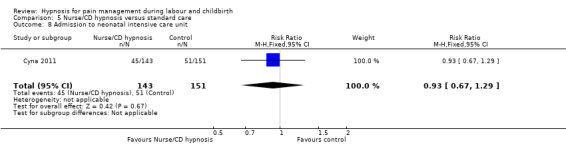
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 8 Admission to neonatal intensive care unit.
Apgar score less than seven at five minutes
Five studies reported on this outcome (Cyna 2011; Fisher 2009; Harmon 1990; Mehl‐Madrona 2004; Werner 2013), but two trials did not report numerical data so were unable to be included in the analysis (Fisher 2009; Mehl‐Madrona 2004).
No clear difference was found in the proportion of babies who had Apgar scores less than seven at five minutes between the women in the hypnosis group and the control group (average RR 1.02, 95% CI 0.28 to 3.71, three studies, 1582 women). There was little statistical heterogeneity: I² = 0%, Tau² = 0.00, Chi² test for heterogeneity P = 0.45, so we used a fixed‐effect model, Analysis 1.14.
1.14. Analysis.
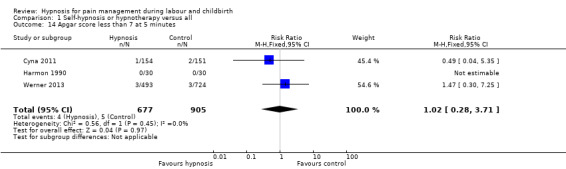
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 14 Apgar score less than 7 at 5 minutes.
There was also no clear difference between women in the nurse/audio CD group and women in the control group for this outcome (RR 0.53, 95% CI 0.05 to 5.76, one study, 294 women), Analysis 5.9.
5.9. Analysis.
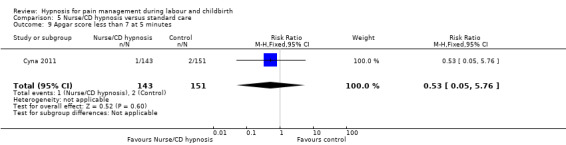
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 9 Apgar score less than 7 at 5 minutes.
Poor infant outcomes at long‐term follow‐up
None of the studies reported data for this outcome.
Use of epidural/neuroaxial block
Seven studies reported on this outcome (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Mehl‐Madrona 2004; Rock 1969; Werner 2013), but one trial did not report numerical data so was not able to be included in the analysis (Fisher 2009).
No clear difference was found in the proportion of women having an epidural between the hypnosis and control group (average RR 0.81, 95% CI 0.51 to 1.27, six studies, 2817 women). There was substantial statistical heterogeneity: I² = 92%, Tau² = 0.24, Chi² test for heterogeneity P < 0.01, and so we used a random‐effects model, Analysis 1.15. It appears that the Mehl‐Madrona 2004 trial was responsible for the high level of heterogeneity. This trial provided unlimited one‐on‐one hypnotherapy commencing in the first or second trimester and was judged to be at high risk of attrition bias. It is not clear which of these factors, if any, contributed to the results strongly favouring hypnosis.
1.15. Analysis.
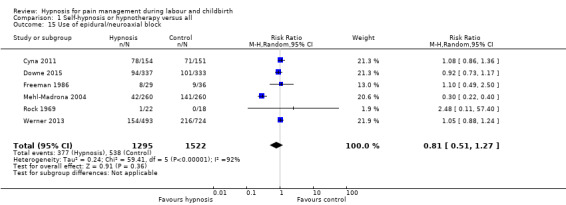
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 15 Use of epidural/neuroaxial block.
There was no clear difference found between women in the nurse/audio CD group and the control group for use of epidural/neuroaxial block (RR 0.94, 95% CI 0.73 to 1.20, one study, 294 women), Analysis 5.10.
5.10. Analysis.
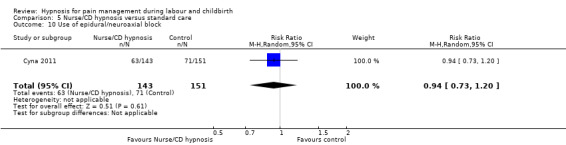
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 10 Use of epidural/neuroaxial block.
Preterm birth
One study reported on this outcome (Werner 2013). No clear difference was found in the proportion of preterm births between women in hypnosis group and the control groups (RR 0.96, 95% CI 0.56 to 1.65, one study, 1217 women), Analysis 1.16.
1.16. Analysis.
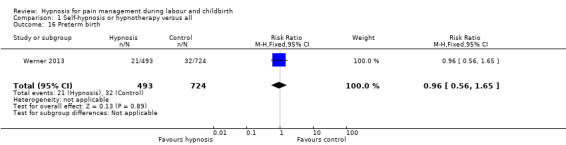
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 16 Preterm birth.
Length of labour
Six studies reported on this outcome (Cyna 2011; Downe 2015; Freeman 1986; Martin 2001; Harmon 1990; Werner 2013). Four trials did not report data in a format that could be included in the review (Cyna 2011; Freeman 1986; Martin 2001; Werner 2013). One of these trials reported that women in the hypnosis group had longer labours (Freeman 1986). The other trials reported no clear differences between the hypnosis and control groups. For (Cyna 2011), no clear difference ‐ median (IQR) of 8 (7.3) hours for hypnosis versus 7.4 (6.7) hours for control women. For Werner 2013 no clear differences between the intervention and control groups for vaginal births in duration of first stage of labour (P = 0.35), second stage of labour (P = 0.35) or for emergency caesarean births (P = 0.17). The other trial reported that no differences were found in the perceived hours of each stage of labour between the groups (Martin 2001).
In the two studies where data were available, no clear difference was found between the mean length of labour for women in the hypnosis group or control group, (MD ‐93.78, 95% CI ‐233.43 to 45.87, two studies, 559 women). There was substantial statistical heterogeneity: I² = 92%, Tau² = 9291.75, Chi² test for heterogeneity P < 0.001, and so we used a random‐effects model, Analysis 1.17 . As there were only two trials, it is not clear whether differences in the interventions or trial designs would explain this heterogeneity. However, Harmon 1990 was a quasi‐randomised controlled trial so is subject to a high risk of selection bias.
1.17. Analysis.
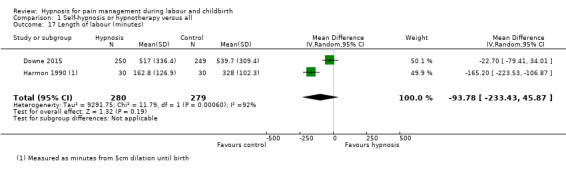
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 17 Length of labour (minutes).
Perineal trauma (episiotomy and incidence of tear ‐ greater than first degree)
One study reported on this outcome (Werner 2013). No clear difference was found in the proportion of women who experienced perineal trauma between those in the hypnosis group and the control groups (RR 0.91, 95% CI 0.80 to 1.03, one study, 1217 women), Analysis 1.18.
1.18. Analysis.
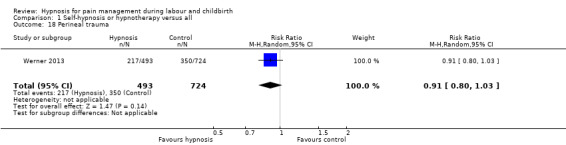
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 18 Perineal trauma.
Induction of labour
Six studies reported on this outcome (Cyna 2011; Downe 2015; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Werner 2013), but two studies could not be included in the analysis as they reported induction and augmentation data combined (Martin 2001; Mehl‐Madrona 2004). Both of those studies reported that women in the hypnosis group had less induction or augmentation, two of the 22 women in the hypnosis compared with six of the 20 women in the Martin 2001 trial and 22 of the 260 women in the hypnosis group compared with 72 of the 260 women in the control group in the Mehl‐Madrona 2004 trial.
No clear difference was found in the proportion of women whose labour was induced between the hypnosis group and the control group (average RR 0.98, 95% CI 0.77 to 1.25, four studies, 2247 women). There was substantial statistical heterogeneity: I² = 59%, Tau² = 0.02, Chi² test for heterogeneity P = 0.06, and so we used a random‐effects model, Analysis 1.19. It appears that the Harmon 1990 trial is likely to be responsible for the high level of heterogeneity, it was a quasi‐randomised controlled trial so is subject to a high risk of selection bias.
1.19. Analysis.
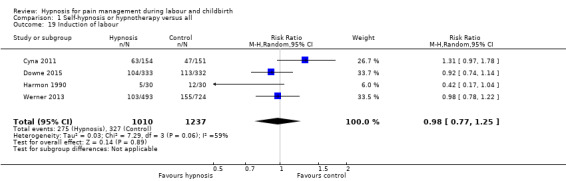
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 19 Induction of labour.
There was no clear difference found between women in the nurse/audio CD group and women in the control group for induction of labour (RR 0.97, 95% CI 0.68 to 1.36, one study, 294 women), Analysis 5.11.
5.11. Analysis.
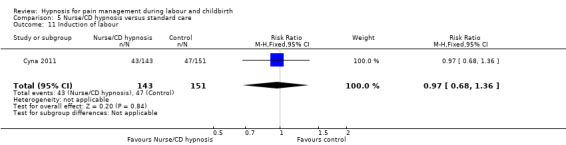
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 11 Induction of labour.
Augmentation with oxytocin
Six studies reported on this outcome (Cyna 2011; Downe 2015; Harmon 1990; Martin 2001; Mehl‐Madrona 2004; Werner 2013) but three studies could not be included in the analysis. Two of the studies reported induction and augmentation data combined as noted above (Martin 2001; Mehl‐Madrona 2004). One of the trials reported induction data separately as well as overall use of oxytocics but did not provide data for augmentation alone (Harmon 1990). That study reported that nine of the 30 women in the hypnosis group used oxytocics at some stage in labour compared with 29 of 30 women in the control group (Harmon 1990).
No clear difference was found in the proportion of women who had their labour augmented between those in the hypnosis group and the control group (average RR 0.97, 95% CI 0.88 to 1.08, three studies, 2165 women). There was little statistical heterogeneity: I² = 0%, T² = 0.07, Chi² test for heterogeneity P = 0.96, so we used a fixed‐effect model, Analysis 1.20.
1.20. Analysis.
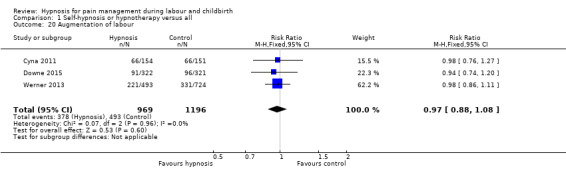
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 20 Augmentation of labour.
There was also no clear difference found between women in the nurse/audio CD group and women in the control group for this outcome (RR 1.06, 95% CI 0.82 to 1.36, one study, 294 women), Analysis 5.12.
5.12. Analysis.
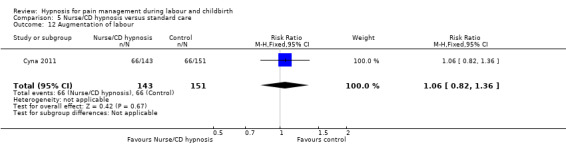
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 12 Augmentation of labour.
Primary postpartum haemorrhage (greater than 500 mL)
Three studies reported on this outcome (Cyna 2011; Mehl‐Madrona 2004; Werner 2013), but data from one study were reported in a combined 'complicated birth' category so could not be included in the analysis (Mehl‐Madrona 2004).
No clear difference was found in the proportion of women who had a primary postpartum haemorrhage between the hypnosis group and the control group (average RR 1.12, 95% CI 0.59 to 2.15, two studies, 1522 women). There was substantial statistical heterogeneity: I² = 75%, T² = 0.17, Chi² test for heterogeneity P = 0.04, so we used a random‐effects model, Analysis 1.21.
1.21. Analysis.
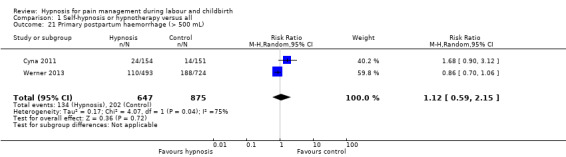
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 21 Primary postpartum haemorrhage (> 500 mL).
There was also no clear difference found between women in the nurse/audio CD group and women in the control group for this outcome (RR 1.66, 95% CI 0.88 to 3.12, one study, 294 women), Analysis 5.13.
5.13. Analysis.
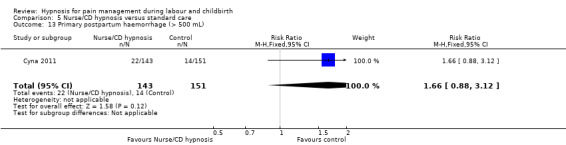
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 13 Primary postpartum haemorrhage (> 500 mL).
Cost (as defined by trialists)
One study reported data on this outcome (Downe 2015). No clear difference was found between the cost (in pounds sterling) for the hypnosis group and the control group (MD 4.83, 95% CI ‐257.78 to 267.44, one study, 672 women) Analysis 1.22.
1.22. Analysis.
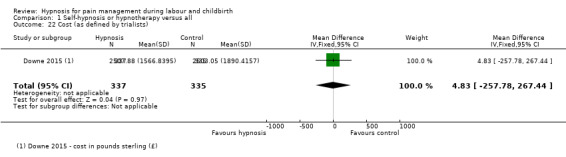
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 22 Cost (as defined by trialists).
Need for postpartum blood transfusion
Two trials reported on this outcome (Cyna 2011; Downe 2015). No clear difference was found in the proportion of women who needed a postpartum blood transfusion between those in the hypnosis group and the control group (RR 1.30, 95% CI 0.55 to 3.04, two studies, 827 women). There was little statistical heterogeneity: I² = 25%, T² = 0.25, Chi² test for heterogeneity P = 0.25, we used a fixed‐effect model, Analysis 1.23.
1.23. Analysis.
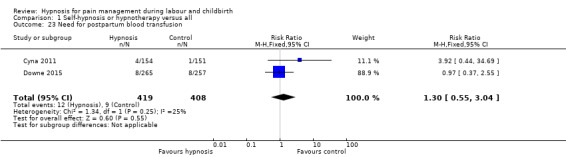
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 23 Need for postpartum blood transfusion.
There was also no clear difference found between women in the nurse/audio CD group and women in the control group although there was a trend towards women in the nurse/audio CD group being more likely to need a postpartum blood transfusion (RR 7.39, 95% CI 0.92 to 59.33, one study, 294 women), Analysis 5.14.
5.14. Analysis.
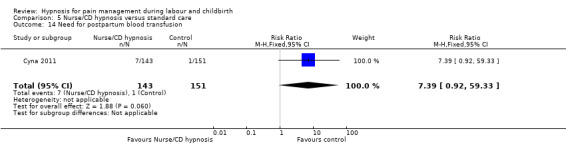
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 14 Need for postpartum blood transfusion.
Postnatal depressive symptoms
Six studies reported on this outcome (Cyna 2011; Downe 2015; Harmon 1990; Mehl‐Madrona 2004; Rock 1969; Werner 2013), but data were not available in a suitable format for analysis from two trials. The author of one trial advised that women were followed up at one month and that "there were no cases of significant post‐partum depression during that month in either group" but it was not clear how many participants were able to be contacted for this follow‐up (Mehl‐Madrona 2004). The other trial reported mean T scores on the Minnesota Multiphasic Personality Inventory (MMPI) Depression scale for high and low hypnotic susceptibility groups for the intervention and control groups. It was reported that there was an interaction effect of hypnosis with susceptibility P < 0.05 and that only the highly susceptible, hypnotically‐trained women had lower MMPI depression scale scores (Harmon 1990).
One of the trials (Rock 1969), had no events in either group. No clear difference was found in the proportion of women who reported post‐natal depressive symptoms between those in the hypnosis group and the control group (RR 1.06, 95% CI 0.77 to 1.47, three studies, 1562 women). There was little statistical heterogeneity: I² = 0%, T² = 0.00, Chi² test for heterogeneity P = 0.48, so we used a fixed‐effect model, Analysis 1.24.
1.24. Analysis.
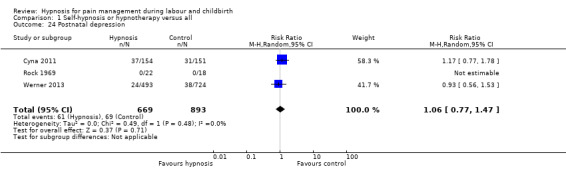
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 24 Postnatal depression.
One trial reported continuous data using the Edinburugh Postnatal Depression Scale (EPDS) (Downe 2015). Women in the hypnosis group had slightly better EPDS scores than those in the control group (MD ‐0.21, 95% CI ‐0.28 to ‐0.15, one study, 376 women), Analysis 1.25.
1.25. Analysis.
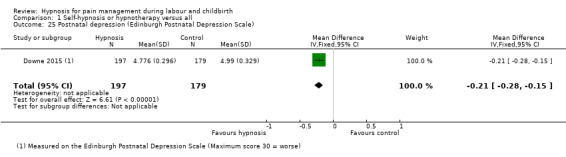
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 25 Postnatal depression (Edinburgh Postnatal Depression Scale).
There was also no clear difference found between women in the nurse/audio CD group and women in the control group for this outcome (RR 0.82, 95% CI 0.51 to 1.32, one study, 294 women), Analysis 5.15.
5.15. Analysis.
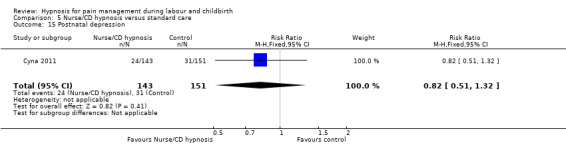
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 15 Postnatal depression.
Number of maternal days in hospital after the birth
One study reported on this outcome (Martin 2001). There were fewer women in the hypnosis group compared with the control group, who stayed in hospital for more than two days after the birth, (RR 0.11, 95% CI 0.02 to 0.83, one study, 42 women), Analysis 1.26.
Number of neonatal days in hospital after the birth
None of the studies reported data for this outcome.
Any other adverse events (maternal side effects, newborn resuscitation)
Three studies reported data that have been included for this outcome (Cyna 2011; Downe 2015; Mehl‐Madrona 2004). One study reported on newborn resuscitations (Mehl‐Madrona 2004). No clear difference was found in the proportion of babies who received resuscitation as newborns between women in the hypnosis group and those in the control group (RR 0.67, 95% CI 0.11 to 3.96, one study, 520 women), Analysis 1.27.
1.27. Analysis.
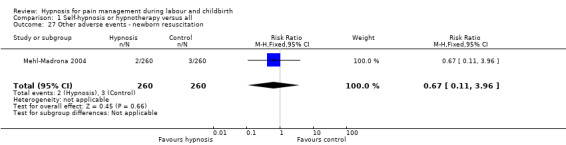
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 27 Other adverse events ‐ newborn resuscitation.
One study reported on maternal readmissions to hospital, neonatal readmissions to hospital and maternal admissions to the high dependency unit or intensive care unit (Cyna 2011). No clear difference was found in the proportion of women who were readmitted to hospital between those in hypnosis group and the control group (RR 1.56, 95% CI 0.62 to 3.90, one study, 267 women), Analysis 1.28. There was also no clear difference found between women in the nurse/audio CD group and women in the control group for this outcome (RR 1.14, 95% CI 0.43 to 3.06 one study, 266 women), Analysis 5.16.
1.28. Analysis.
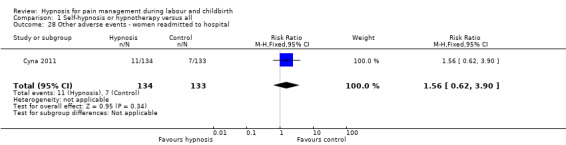
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 28 Other adverse events ‐ women readmitted to hospital.
5.16. Analysis.
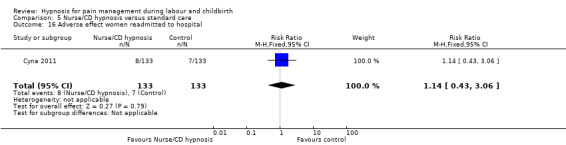
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 16 Adverse effect women readmitted to hospital.
No clear difference was found in the proportion of babies who were readmitted to hospital between women who were in the hypnosis group and those in the control group (RR 1.39, 95% CI 0.64 to 3.02, one study, 267 women), Analysis 1.29, or between women in the nurse/audio CD group and women in the control group (RR 0.90, 95% CI 0.38 to 2.14, one study, 266 women), Analysis 5.17.
1.29. Analysis.
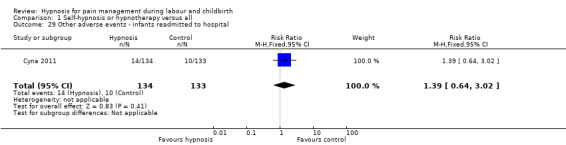
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 29 Other adverse events ‐ infants readmitted to hospital.
5.17. Analysis.
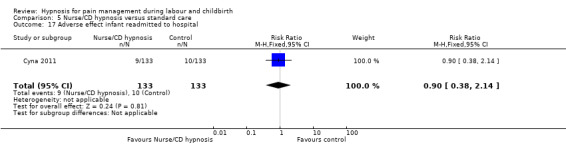
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 17 Adverse effect infant readmitted to hospital.
No clear difference was found in the proportion of women who were admitted to the high dependency or intensive care unit between women in the hypnosis group and those in the control group (RR 1.47, 95% CI 0.25 to 8.68, one study, 305 women), Analysis 1.30. There was also no clear difference found between women in the nurse/audio CD group and women in the control group for this outcome (RR 3.70, 95% CI 0.78 to 17.50, one study, 294 women), Analysis 5.18.
1.30. Analysis.
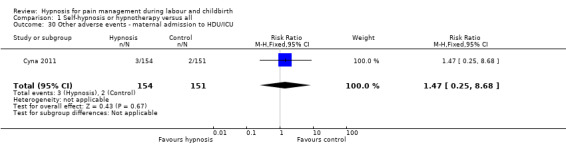
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 30 Other adverse events ‐ maternal admission to HDU/ICU.
5.18. Analysis.
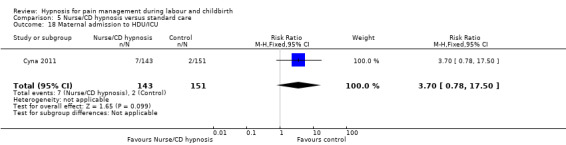
Comparison 5 Nurse/CD hypnosis versus standard care, Outcome 18 Maternal admission to HDU/ICU.
One study reported on stillbirths (Downe 2015). No clear difference was found in the number of babies who were stillborn between the hypnosis group and the control group (RR 2.91, 95% CI 0.30 to 27.79, one study, 522 women), Analysis 1.31.
1.31. Analysis.
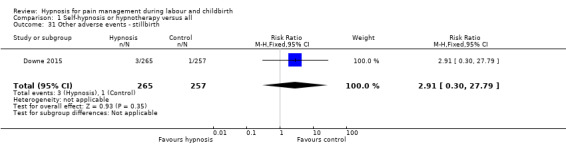
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 31 Other adverse events ‐ stillbirth.
Comparison 2 ‐ Self‐hypnosis or hypnotherapy versus standard care
Primary outcomes
Use of pharmacological pain relief or anaesthesia during labour and childbirth
Six studies measured this outcome (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Rock 1969; Werner 2013), but one study did not report any numerical data so could not be included in the analysis (Fisher 2009). One study (Rock 1969) reported the use of tranquillizers but these were not considered to be pain relief for the purposes of this review. Therefore, the data for Rock 1969 used in this outcome relate to the use of narcotics only. One study (Freeman 1986) combined women who used the inhaled analgesic Entonox with those who used no analgesia so only those who were reported as using pethidine and/or epidural were included as using pharmacological pain relief or anaesthesia.
No clear difference was found in the use of pharmacological pain relief or anaesthesia during labour and childbirth for those using hypnosis compared with those receiving standard care (average RR 0.94, 95% CI 0.83 to 1.07, five studies, 1800 women). There was substantial statistical heterogeneity: I² = 60%, Tau² = 0.01, Chi² test for heterogeneity P < 0.04, and so we used a random‐effects model, Analysis 2.1. It is likely that the Rock 1969 trial contributed to the high level of heterogeneity. The Rock 1969 trial was a quasi‐randomised controlled trial so is subject to a high risk of selection bias. This trial also provided individual hypnotherapy to women during labour so it is not clear whether these factors and/or some other characteristic of the trial explains the result favouring the intervention.
2.1. Analysis.
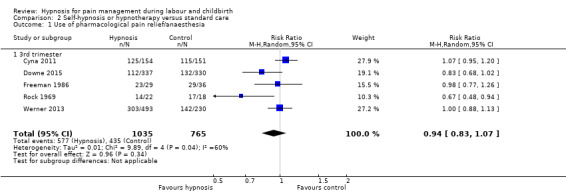
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 1 Use of pharmacological pain relief/anaesthesia.
Satisfaction with pain relief
Two studies reported on this outcome (Cyna 2011; Downe 2015). The data were reported in different ways in the two studies and so could not be combined in one analysis. There was no clear difference identified between the hypnosis and control group in the proportion of women who reported that they received adequate pain relief (RR 1.06, 95% CI 0.94 to 1.20, one study, 264 women), Analysis 2.2. One study (Downe 2015) reported satisfaction with pain relief for specific pain relief methods and found no clear difference in satisfaction according to a postnatal questionnaire two weeks postpartum for pethidine (MD 0.41, 95% CI ‐0.45 to 1.27, 72 women), Entonox (MD 0.19, 95% CI ‐0.19 to 0.57, 357 women), self‐hypnosis (MD 0.28, 95% CI ‐0.32 to 0.88, 160 women), epidural (MD ‐0.03, 95% CI ‐0.40 to 0.34), although women in the hypnosis group who had water immersion reported being more satisfied (MD 0.52, 95% CI 0.04 to 1.00), Analysis 2.3. Satisfaction was measured on a seven‐point scale, with seven indicating most satisfaction.
2.2. Analysis.
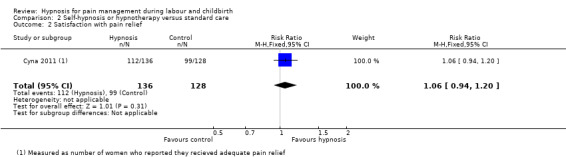
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 2 Satisfaction with pain relief.
2.3. Analysis.
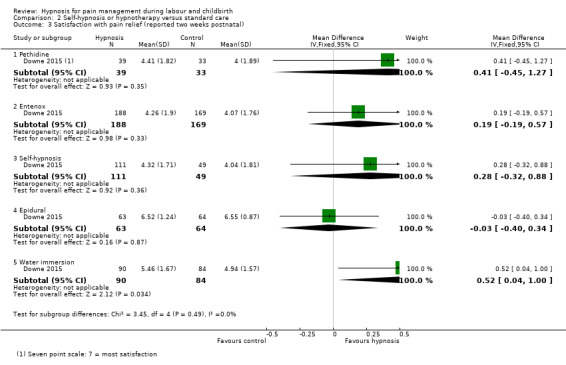
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 3 Satisfaction with pain relief (reported two weeks postnatal).
Sense of coping with labour
Three studies reported on this outcome (Cyna 2011; Downe 2015; Fisher 2009), but two of the studies did not report data in a way that could be analysed for the review (Cyna 2011; Fisher 2009). Cyna 2011 reported women's perceptions of coping with childbirth postnatally prior to their discharge from hospital stating that there was no clear difference in median IQR 7(3) versus 8(3) on a 10‐point scale. Fisher 2009 reported: "a greater ability to cope during childbirth after hypnosis course completion compared to the conventional group. However, after delivery, the hypnosis group recalled relatively poorer intrapartum coping skills (P = 0.02)".
One study (Downe 2015) measured coping on a seven point scale did not find a difference between women in the hypnosis group and those in the control group (MD 0.22, 95% CI ‐0.14 to 0.58, one study, 420 women), Analysis 2.4.
2.4. Analysis.
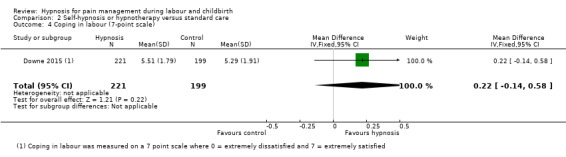
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 4 Coping in labour (7‐point scale).
Spontaneous vaginal birth
Five studies reported on this outcome (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Werner 2013), but data were only available for analysis from four studies (Cyna 2011; Downe 2015; Freeman 1986; Werner 2013). One trial did not report numerical data for this outcome (Fisher 2009).
No clear difference was found between the hypnosis and standard care group in the proportion of women having a spontaneous vaginal birth (average RR 0.99, 95% CI 0.91 to 1.07, four studies, 1765 women). There was little statistical heterogeneity: I² = 0%, Tau² = 0.00, Chi² test for heterogeneity P < 0.45, so we used a fixed‐effect model, Analysis 2.5.
2.5. Analysis.
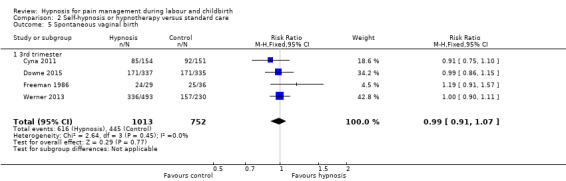
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 5 Spontaneous vaginal birth.
Secondary outcomes
Pain intensity
Three studies reported on this outcome (Downe 2015; Freeman 1986; Werner 2013), but data were only available for analysis from one study (Downe 2015). In the one study no numerical data were reported but it was noted that there was no clear difference between the two groups in terms of efficacy of pain relief on a linear analogue scale (Freeman 1986). In one study (Werner 2013), data were reported as Mdn and IQR at specific points in the labour for women who received epidural analgesia and women who did not receive epidural.
No clear difference was found for memory of labour pain reported at two weeks postnatally on a 100‐point scale as "Worst imaginable" (MD 0.05, 95% CI ‐4.14 to 4.24, one study, 430 women) Analysis 2.6 or as "Completely unbearable" (MD ‐0.26, 95% CI ‐4.92 to 4.40, one study, 429 women) Analysis 2.6.
2.6. Analysis.
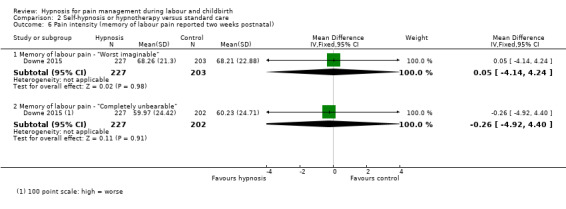
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 6 Pain intensity (memory of labour pain reported two weeks postnatal).
Maternal pain score as measured by visual analogue pain scores of verbal numerical rating scales
One study reported on this outcome (Cyna 2011), but the results were reported as Mdn and IQR (as is appropriate for ordinal level data) so was not in a format suitable for analysis as part of the review. However, no clear differences were reported between the scores for the hypnosis group (Mdn 8, IQR 2) and the standard care group (Mdn 8, IQR 2).
Satisfaction with the childbirth experience
Three studies reported on this outcome (Cyna 2011; Freeman 1986; Werner 2013). One study measured this outcome as the number of women who reported being "very satisfied" (score 8 to 10 on linear analogue scale) with labour (Freeman 1986), one trial measured it as the number of women who reported the birth as a positive experience (Cyna 2011), and one trial measured satisfaction on a continuous scale using the Wijmas Delivery Experience Questionaire (Werner 2013).
For the dichotomous data, no clear difference was found for satisfaction with the childbirth experience between women in the hypnosis group and women in the control group (average RR 1.36, 95% CI 0.52 to 3.59, two studies, 370 women). There was substantial statistical heterogeneity: I² = 87%, Tau² = 0.43, Chi² test for heterogeneity P < 0.01, and so we used a random‐effects model, Analysis 2.7. As there were only two trials, it is not clear which differences between the trials could explain this heterogeneity, for example, the Freeman 1986 trial was much smaller, the hypnosis intervention began earlier in the pregnancy and involved more sessions than the Cyna 2011 trial.
2.7. Analysis.
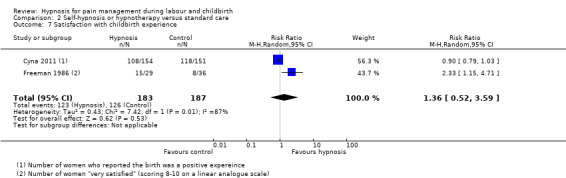
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 7 Satisfaction with childbirth experience.
For the continuous data women in the hypnosis group were found to have a more positive experience of childbirth (MD ‐4.60, 95% CI ‐8.34 to ‐0.86, one study, 678 women), Analysis 2.8 (lower scores represent a more positive experience).
2.8. Analysis.
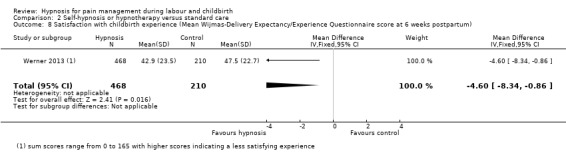
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 8 Satisfaction with childbirth experience (Mean Wijmas‐Delivery Expectancy/Experience Questionnaire score at 6 weeks postpartum).
Breastfeeding at discharge
Three studies reported on breastfeeding (Cyna 2011; Downe 2015; Werner 2013), however there were some differences in the time point when breastfeeding was reported. The Cyna 2011 trial reported at discharge from hospital, the Downe 2015 trial reported at six weeks postnatally and the Werner 2013 trial reported at one month or more. No clear difference was found in the proportion of women who reported any breastfeeding between the hypnosis group and the control group (average RR 1.02, 95% CI 0.96 to 1.08, three studies, 1380 women), Analysis 2.9.
2.9. Analysis.
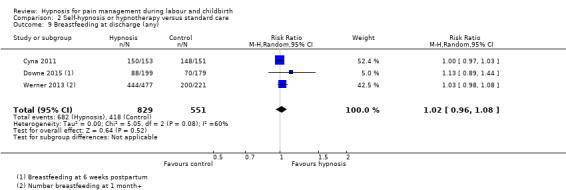
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 9 Breastfeeding at discharge (any).
Assisted vaginal birth
Five studies measured this outcome (Cyna 2011; Downe 2015; Freeman 1986; Fisher 2009; Werner 2013), but data were only available for analysis from four studies (Cyna 2011; Downe 2015; Freeman 1986; Werner 2013). One study did not report numerical data for this outcome (Fisher 2009).
No clear difference was found in the proportion of women who had assisted vaginal births between the women in the hypnosis group and those in the standard care group (RR 0.88, 95% CI 0.72 to 1.06, four studies, 1765 women). There was little statistical heterogeneity: I² = 0%, Tau² = 0.00, Chi² test for heterogeneity P = 0.56, so we used a fixed‐effect model, Analysis 2.10.
2.10. Analysis.
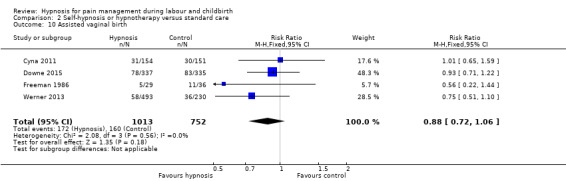
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 10 Assisted vaginal birth.
Caesarean section
Four studies reported upon this outcome (Cyna 2011; Downe 2015; Fisher 2009; Werner 2013), but one study did not report numerical data so was not able to be included in the analysis (Fisher 2009). No clear difference was found in the proportion of women who had a caesarean section between those in the hypnosis group and the control group (RR 1.17, 95% CI 0.97 to 1.42, three studies, 1700 women). There was little statistical heterogeneity: I² = 0%, Tau² = 0.00, Chi² test for heterogeneity P = 0.73, so we used a fixed‐effect model, Analysis 2.11.
2.11. Analysis.
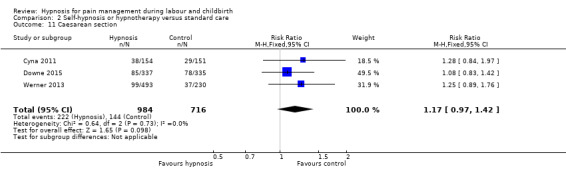
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 11 Caesarean section.
Admission to special care baby unit/neonatal intensive care unit
Three studies reported on this outcome (Cyna 2011; Downe 2015; Werner 2013). No clear difference was found for admissions to the neonatal intensive care unit for babies born to the mothers in the hypnosis group compared with babies born to mothers in the control group (average RR 1.44, 95% CI 0.67 to 3.12, three studies, 1697 women). There was significant statistical heterogeneity: I² = 83%, Tau² = 0.38, Chi² test for heterogeneity P = 0.002, so we used a random‐effects model, Analysis 2.12. It is likely that the Werner 2013 trial contributed to the high level of heterogeneity. It is not clear which characteristics of this trial might help explain the heterogeneity as all three trials were large, well‐designed trials using similar methods.
2.12. Analysis.
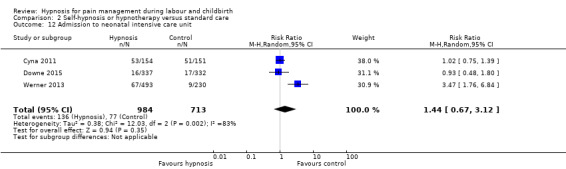
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 12 Admission to neonatal intensive care unit.
Apgar score less than seven at five minutes
Three studies reported on this outcome (Cyna 2011; Fisher 2009; Werner 2013), but one trial did not report numerical data so was unable to be included in the analysis (Fisher 2009).
No clear difference was found in the proportion of babies who had Apgar scores less than seven at five minutes between the women in the hypnosis group and the standard care group (RR 0.86, 95% CI 0.18 to 4.19, two studies, 1028 women). There was little statistical heterogeneity: I² = 0%, Tau² = 0.00, Chi² test for heterogeneity P = 0.53, so we used a fixed‐effect model, Analysis 2.13.
2.13. Analysis.
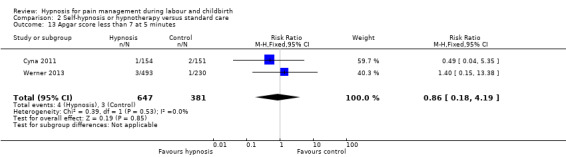
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 13 Apgar score less than 7 at 5 minutes.
Use of epidural/neuroaxial block
Six studies reported on this outcome (Cyna 2011; Downe 2015; Fisher 2009; Freeman 1986; Rock 1969; Werner 2013), but one trial did not report numerical data so was not able to be included in the analysis (Fisher 2009).
No clear difference was found in the proportion of women having an epidural between the hypnosis and the standard care group (average RR 1.02, 95% CI 0.89 to 1.16, five studies, 1803 women). There was little statistical heterogeneity: I² = 0%, Tau² = 0.00, Chi² test for heterogeneity P = 0.86, we used a random‐effects model, Analysis 2.15.
2.15. Analysis.
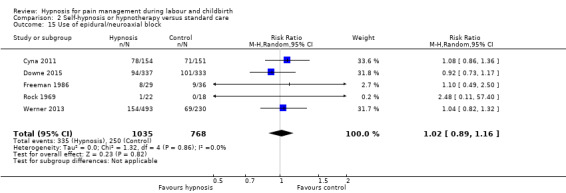
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 15 Use of epidural/neuroaxial block.
Preterm birth
One study reported on this outcome (Werner 2013). No clear difference was found in the proportion of preterm births between women in hypnosis group and the control groups (RR 0.98, 95% CI 0.47 to 2.05, one study, 723 women), Analysis 2.14.
2.14. Analysis.
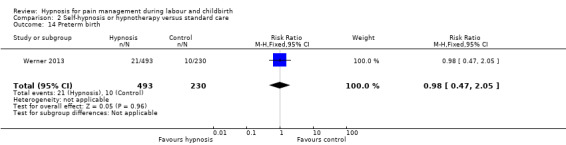
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 14 Preterm birth.
Length of labour
Four studies reported on this outcome (Cyna 2011; Downe 2015; Freeman 1986; Werner 2013). Three trials did not report data in a format that could be included in the review (Cyna 2011; Freeman 1986; Werner 2013). One of these trials reported that women in the hypnosis group had longer labours (Freeman 1986). The other trials reported no clear differences between the hypnosis and control groups. For Cyna 2011, no clear difference ‐ median (IQR) of 8 (7.3) hours for hypnosis versus 7.4 (6.7) hours for control women.
In the study where data were available, no clear difference was found between the mean length of labour (minutes) for women in the hypnosis group or the standard care group (MD ‐22.70, 95% CI ‐79.41 to 34.01, one study, 499 women) Analysis 2.16.
2.16. Analysis.
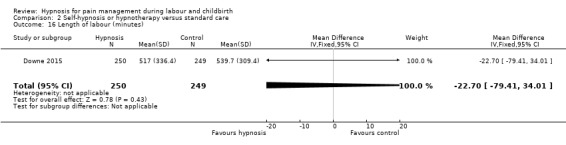
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 16 Length of labour (minutes).
Perineal trauma (episiotomy and incidence of tear ‐ greater than first degree)
One study reported on this outcome (Werner 2013). No clear difference was found in the proportion of women who experienced perineal trauma between those in the hypnosis group and the control groups (RR 0.92, 95% CI 0.78 to 1.09, one study, 723 women), Analysis 2.17.
2.17. Analysis.
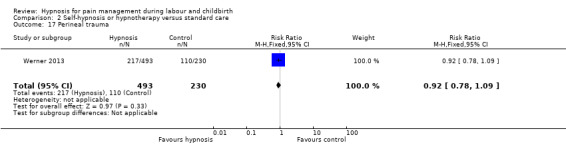
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 17 Perineal trauma.
Induction of labour
Three studies reported on this outcome (Cyna 2011; Downe 2015; Werner 2013). No clear difference was found in the proportion of women whose labour was induced between the hypnosis group and the standard care group (average RR 1.04, 95% CI 0.84 to 1.28, three studies, 1693 women). There was some statistical heterogeneity: I² = 45%, Tau² = 0.02, Chi² test for heterogeneity P = 0.16, therefore we used a random‐effects model, Analysis 2.18. It is not clear which of the trials is responsible for this heterogeneity.
2.18. Analysis.
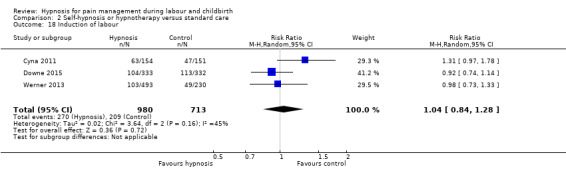
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 18 Induction of labour.
Augmentation with oxytocin
Three studies reported on this outcome (Cyna 2011; Downe 2015; Werner 2013). No clear difference was found in the proportion of women who had their labour augmented between those in the hypnosis group and the standard care group (RR 1.02, 95% CI 0.89 to 1.15, three studies, 1671 women). There was little statistical heterogeneity: I² = 0%, Tau² = 0.00, Chi² test for heterogeneity P = 0.63, so we used a fixed‐effect model, Analysis 2.19.
2.19. Analysis.
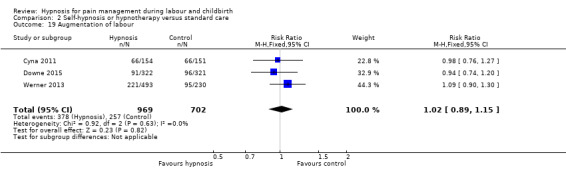
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 19 Augmentation of labour.
Primary postpartum haemorrhage (greater than 500 mL)
Two studies reported on this outcome (Cyna 2011; Werner 2013). No clear difference was found in the proportion of women who had a primary postpartum haemorrhage between the hypnosis group and the standard care group (average RR 1.14, 95% CI 0.60 to 2.15, two studies, 1028 women). There was substantial statistical heterogeneity: I² = 73%, Tau² = 0.16, Chi² test for heterogeneity P = 0.06, so we used a random‐effects model, Analysis 2.20. As there were only two large, well‐designed trials it is not clear what might explain this heterogeneity.
2.20. Analysis.
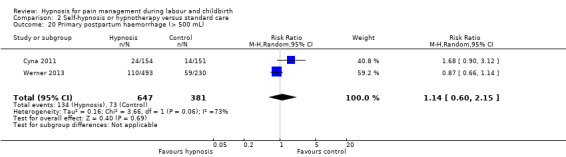
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 20 Primary postpartum haemorrhage (> 500 mL).
Cost (as defined by trialists)
One study reported data on this outcome (Downe 2015). No clear difference was found between the cost (in pounds sterling) for the hypnosis group and the standard care group (MD 4.83, 95% CI ‐257.78 to 267.44, one study, 672 women) Analysis 2.21.
2.21. Analysis.
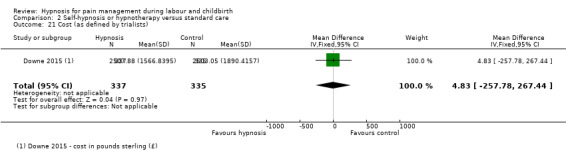
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 21 Cost (as defined by trialists).
Need for postpartum blood transfusion
Two trials reported on this outcome (Cyna 2011; Downe 2015). No clear difference was found in the proportion of women who needed a postpartum blood transfusion between those in the hypnosis group and the standard care group (RR 1.30, 95% CI 0.55 to 3.04, two studies, 827 women). There was little statistical heterogeneity: I² = 25%, Tau² = 0.25, Chi² test for heterogeneity P = 0.25, we used a fixed‐effect model, Analysis 2.22.
2.22. Analysis.
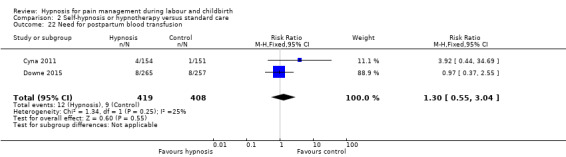
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 22 Need for postpartum blood transfusion.
Postnatal depressive symptoms
Four studies reported on this outcome (Cyna 2011; Downe 2015; Rock 1969; Werner 2013). One of the trials (Rock 1969), had no events in either group. No clear difference was found in the proportion of women who reported postnatal depressive symptoms between those in the hypnosis group and the standard care group (RR 1.15, 95% CI 0.80 to 1.66, three studies, 1068 women). There was little statistical heterogeneity: I² = 0%, Tau² = 0.00, Chi² test for heterogeneity P = 0.92, we used a fixed‐effect model, Analysis 2.23.
2.23. Analysis.
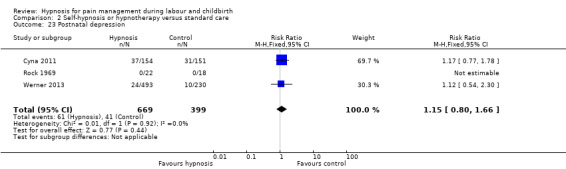
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 23 Postnatal depression.
One trial reported continuous data using the EPDS (Downe 2015). Women in the hypnosis group had slightly better EPDS scores than those in the control group (MD ‐0.21, 95% CI ‐0.28 to ‐0.15, one study, 376 women), Analysis 2.24.
2.24. Analysis.
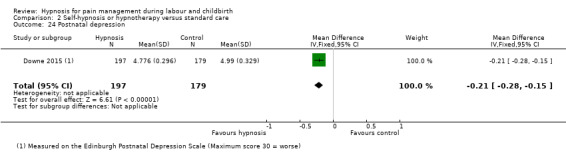
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 24 Postnatal depression.
Any other adverse events (maternal side effects, newborn resuscitation)
Two studies reported data that have been included for this outcome (Cyna 2011; Downe 2015). One study reported on maternal readmissions to hospital, neonatal readmissions to hospital and maternal admissions to the high dependency unit or intensive care unit (Cyna 2011). No clear difference was found in the proportion of women who were readmitted to hospital between those in hypnosis group and the standard care group (RR 1.56, 95% CI 0.62 to 3.90, one study, 267 women), Analysis 2.25.
2.25. Analysis.
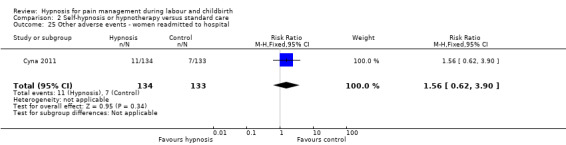
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 25 Other adverse events ‐ women readmitted to hospital.
No clear difference was found in the proportion of babies who were readmitted to hospital between women who were in the hypnosis group and those in the standard care group (RR 1.39, 95% CI 0.64 to 3.02, one study, 267 women), Analysis 2.26.
2.26. Analysis.
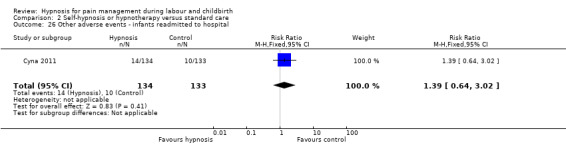
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 26 Other adverse events ‐ infants readmitted to hospital.
No clear difference was found in the proportion of women who were admitted to the high dependency or intensive care unit between women in the hypnosis group and those in the standard care group (RR 1.47, 95% CI 0.25 to 8.68, one study, 305 women), Analysis 2.27.
2.27. Analysis.
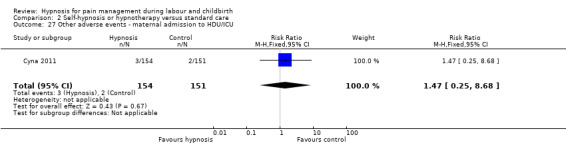
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 27 Other adverse events ‐ maternal admission to HDU/ICU.
One study reported on stillbirths (Downe 2015). No clear difference was found in the number of babies who were stillborn between the hypnosis group and the standard care group (RR 2.91, 95% CI 0.30 to 27.79, one study, 522 women), Analysis 2.28.
2.28. Analysis.
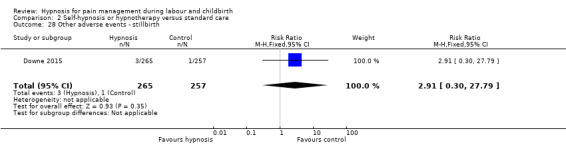
Comparison 2 Self‐hypnosis or hypnotherapy versus standard care, Outcome 28 Other adverse events ‐ stillbirth.
Comparison 3 ‐ Self‐hypnosis or hypnotherapy versus supportive counselling
Primary outcomes
Use of pharmacological pain relief or anaesthesia during labour and childbirth
Both studies measured this outcome (Martin 2001; Mehl‐Madrona 2004). Women in the hypnosis group were less likely to use pharmacological pain relief or anaesthesia during labour and childbirth than women who received supportive counselling, (average RR 0.48, 95% CI 0.32 to 0.73, two studies, 562 women). There was substantial statistical heterogeneity: I² = 56%, Tau² = 0.06, Chi² test for heterogeneity P = 0.13, therefore we used a random‐effects model, Analysis 3.1. As there were only two trials it is not clear which characteristics of the studies might explain this heterogeneity.
3.1. Analysis.
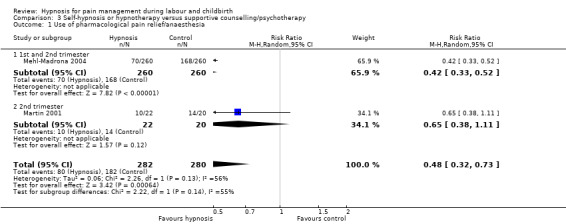
Comparison 3 Self‐hypnosis or hypnotherapy versus supportive counselling/psychotherapy, Outcome 1 Use of pharmacological pain relief/anaesthesia.
Spontaneous vaginal birth
Both studies also reported on this outcome (Martin 2001; Mehl‐Madrona 2004), but data were only available for analysis from one study (Martin 2001). The Mehl‐Madrona 2004 trial reported data grouped as 'uncomplicated births' and 'complicated births', which meant data could not be included in the analysis. Although the uncomplicated births group only included spontaneous vaginal births, the complicated births group included both spontaneous vaginal births and surgically‐assisted births. This meant that the overall number of spontaneous vaginal births could not be calculated (for example, if a woman had a spontaneous vaginal birth followed by a postpartum haemorrhage she was included in the complicated birth group) (Mehl‐Madrona 2004).
More women in the hypnosis group had a spontaneous vaginal birth than those in the supportive counselling group (RR 2.42, 95% CI 1.43 to 4.07, one study, 42 women), Analysis 3.2.
3.2. Analysis.
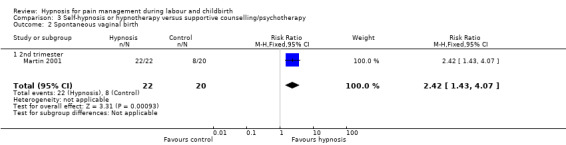
Comparison 3 Self‐hypnosis or hypnotherapy versus supportive counselling/psychotherapy, Outcome 2 Spontaneous vaginal birth.
Secondary outcomes
Assisted vaginal birth
Both studies measured this outcome (Martin 2001; Mehl‐Madrona 2004) but data were only available for analysis from one study (Martin 2001). As noted above, the Mehl‐Madrona 2004 study grouped assisted vaginal births within a complicated birth group, which included a range of complications so could not be included in the analysis. No clear difference was found in the proportion of women who had assisted vaginal births between the women in the hypnosis group and those in the supportive counselling group (RR 0.11, 95% CI 0.01 to 1.95, one study, 44 women), Analysis 3.3.
3.3. Analysis.
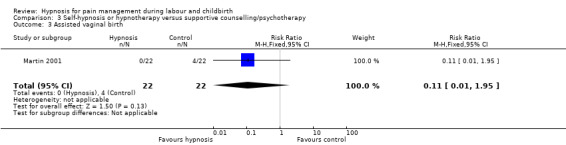
Comparison 3 Self‐hypnosis or hypnotherapy versus supportive counselling/psychotherapy, Outcome 3 Assisted vaginal birth.
Caesarean section
Both studies reported on this outcome (Martin 2001; Mehl‐Madrona 2004). No clear difference was found in the proportion of women who had a caesarean section between those in the hypnosis group and the supportive counselling group (average RR 0.24, 95% CI 0.03 to 1.78, two studies, 562 women). There was substantial statistical heterogeneity: I² = 58%, Tau² = 1.42, Chi² test for heterogeneity P = 0.12, so we used a random‐effects model, Analysis 3.4. Again, as there were only two trials it is not clear which characteristics of the studies might explain this heterogeneity.
3.4. Analysis.
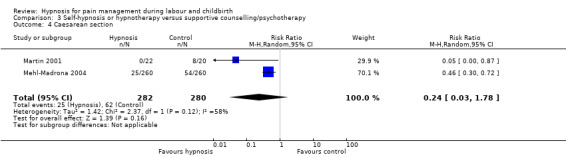
Comparison 3 Self‐hypnosis or hypnotherapy versus supportive counselling/psychotherapy, Outcome 4 Caesarean section.
Admission to special care baby unit/neonatal intensive care unit
One study reported on this outcome (Martin 2001). No clear difference was found for admissions to the neonatal intensive care unit for babies born to the mothers in the hypnosis group compared with babies born to mothers in the supportive counselling group (RR 0.18, 95% CI 0.02 to 1.43, one study, 42 women), Analysis 3.5.
3.5. Analysis.
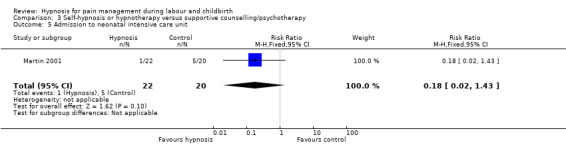
Comparison 3 Self‐hypnosis or hypnotherapy versus supportive counselling/psychotherapy, Outcome 5 Admission to neonatal intensive care unit.
Apgar score less than seven at five minutes
One study measured this outcome (Mehl‐Madrona 2004) but did not report numerical data so could not be analysed.
Use of epidural/neuroaxial block
One study reported on this outcome (Mehl‐Madrona 2004). It found women in the hypnosis group were less likely to have an epidural than women in the supportive counselling group (RR 0.30, 95% CI 0.22 to 0.40, one study, 520 women), Analysis 3.6.
3.6. Analysis.
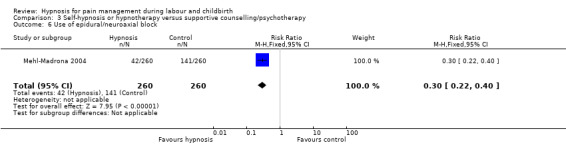
Comparison 3 Self‐hypnosis or hypnotherapy versus supportive counselling/psychotherapy, Outcome 6 Use of epidural/neuroaxial block.
Length of labour
One study reported on this outcome (Martin 2001), but did not report data in a format that could be analysed in the review. That study reported no clear differences were found in the perceived hours of each stage of labour between the groups (Martin 2001).
Number of maternal days in hospital after the birth
One study reported on this outcome (Martin 2001). There were fewer women in the hypnosis group compared with the supportive counselling group, who stayed in hospital for more than two days after the birth, (RR 0.11, 95% CI 0.02 to 0.83, one study, 42 women), Analysis 3.7.
3.7. Analysis.
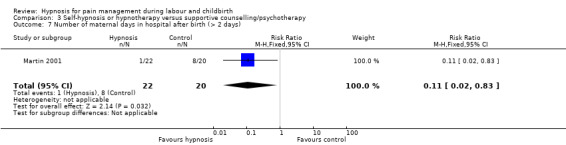
Comparison 3 Self‐hypnosis or hypnotherapy versus supportive counselling/psychotherapy, Outcome 7 Number of maternal days in hospital after birth (> 2 days).
Any other adverse events (maternal side effects, newborn resuscitation)
One study reported data for newborn resuscitation that have been included for this outcome (Mehl‐Madrona 2004). No clear difference was found in the proportion of babies who received resuscitation as newborns between women in the hypnosis group and those in the control group (RR 0.67, 95% CI 0.11 to 3.96, one study, 520 women), Analysis 3.8.
3.8. Analysis.
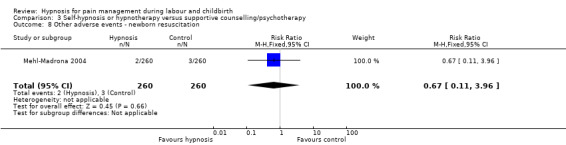
Comparison 3 Self‐hypnosis or hypnotherapy versus supportive counselling/psychotherapy, Outcome 8 Other adverse events ‐ newborn resuscitation.
Comparison 4 ‐ Self‐hypnosis or hypnotherapy versus relaxation
Primary outcomes
Use of pharmacological pain relief or anaesthesia during labour and childbirth
Both studies measured this outcome (Harmon 1990; Werner 2013). No clear difference was found between the hypnosis and relaxation groups in the proportion of women who used pharmacological pain relief of anaesthesia (average RR 0.48, 95% CI 0.11 to 2.17, two studies, 1047 women). There was substantial statistical heterogeneity: I² = 90%, Tau² = 1.07, Chi² test for heterogeneity P = 0.002, so we used a random‐effects model, Analysis 4.1. As there were only two studies, it is not clear which characteristics of the trials were responsible for this heterogeneity. The Harmon 1990 trial was a quasi‐randomised trial so is subject to a high risk of selection bias.
4.1. Analysis.
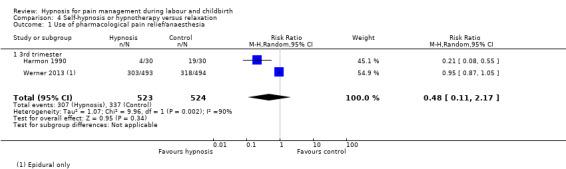
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 1 Use of pharmacological pain relief/anaesthesia.
Spontaneous vaginal birth
Both studies also reported on this outcome (Harmon 1990; Werner 2013). No clear difference was found between the hypnosis and the relaxation group in the proportion of women having a spontaneous vaginal birth (average RR 1.22, 95% CI 0.78 to 1.90, two studies, 1047 women). There was substantial statistical heterogeneity: I² = 80%, Tau² = 0.09, Chi² test for heterogeneity P = 0.03, so we used a random‐effects model, Analysis 4.2.
4.2. Analysis.
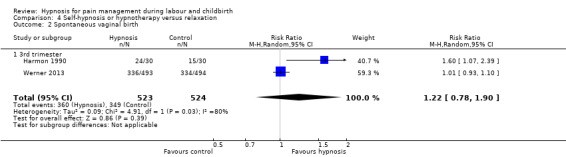
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 2 Spontaneous vaginal birth.
Secondary outcomes
Pain intensity
Both studies reported on this outcome (Harmon 1990; Werner 2013), but data were only available for analysis from the Harmon 1990 trial. In the Werner 2013 study data were reported as Mdn and IQR at specific points in the labour for women who received epidural analgesia and women who did not receive epidural. No clear differences were found between intervention and control groups for any specific point in the labour, but results were not presented separately for the relaxation and standard care group, but presented as a combined group.
In the Harmon 1990 study, the mean pain score in the hypnosis group was lower than the mean pain score in the control group according to the present pain intensity scale of the McGill Pain Questionnaire, (where, 0 = No pain, 1 = Mild, 2 = Discomforting, 3 = Distressing, 4 = Horrible, 5 = Excruciating), (MD ‐0.70, 95% CI‐1.03 to ‐0.37, one study, 60 women), Analysis 4.3.
4.3. Analysis.
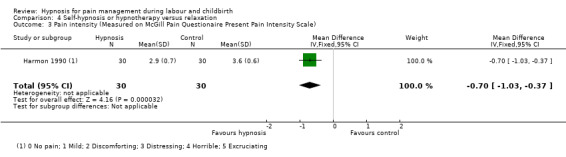
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 3 Pain intensity (Measured on McGill Pain Questionaire Present Pain Intensity Scale).
Satisfaction with the childbirth experience
One study reported on this outcome and measured satisfaction on a continuous scale using the Wijmas Delivery Experience Questionaire (Werner 2013).
Women in the hypnosis group were found to have a more positive experience of childbirth (MD ‐4.30, 95% CI ‐7.45 to ‐1.15, one study, 916 women), Analysis 4.4 (lower scores represent a more positive experience).
4.4. Analysis.
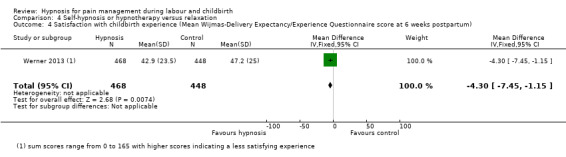
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 4 Satisfaction with childbirth experience (Mean Wijmas‐Delivery Expectancy/Experience Questionnaire score at 6 weeks postpartum).
Breastfeeding at discharge
One study reported on breastfeeding (Werner 2013) (at one month or more postnatally). No clear difference was found in the proportion of women who reported any breastfeeding between the hypnosis group and the relaxation group (RR 1.02, 95% CI 0.98 to 1.06, one study, 923 women), Analysis 4.5.
4.5. Analysis.
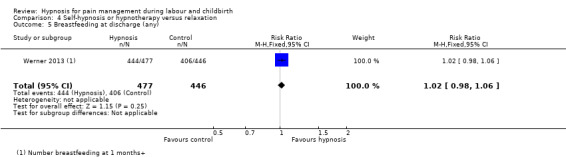
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 5 Breastfeeding at discharge (any).
Assisted vaginal birth
Both studies measured this outcome (Harmon 1990; Werner 2013). No clear difference was found in the proportion of women who had assisted vaginal births between the women in the hypnosis group and those in the relaxation group (average RR 0.63, 95% CI 0.32 to 1.21, two studies, 1047 women). There was substantial statistical heterogeneity: I² = 61%, Tau² = 0.15, Chi² test for heterogeneity P = 0.11, we used a random‐effects model, Analysis 4.6.
4.6. Analysis.
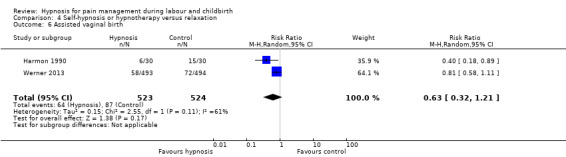
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 6 Assisted vaginal birth.
Caesarean section
One study reported upon this outcome (Werner 2013). No clear difference was found in the proportion of women who had a caesarean section between those in the hypnosis group and the relaxation group (RR 1.13, 95% CI 0.87 to 1.46, one study, 987 women), Analysis 4.7.
4.7. Analysis.
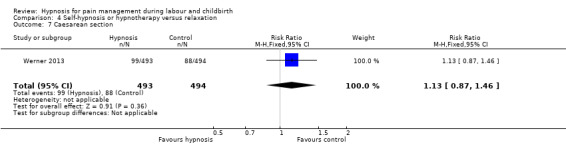
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 7 Caesarean section.
Admission to special care baby unit/neonatal intensive care unit
One study reported on this outcome (Werner 2013). No clear difference was found for admissions to the neonatal intensive care unit for babies born to the mothers in the hypnosis group compared with babies born to mothers in the relaxation group (RR 0.91, 95% CI 0.67 to 1.23, one study, 987 women), Analysis 4.8.
4.8. Analysis.
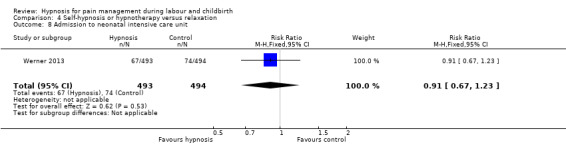
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 8 Admission to neonatal intensive care unit.
Apgar score less than seven at five minutes
Both studies reported on this outcome (Harmon 1990; Werner 2013). One study had no events for either group (Harmon 1990). No clear difference was found in the proportion of babies who had Apgar scores less than seven at five minutes between the women in the hypnosis group and the relaxation group (RR 1.50, 95% CI 0.25 to 8.96, two studies, 1047 women), Analysis 4.9.
4.9. Analysis.
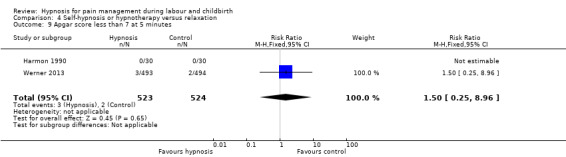
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 9 Apgar score less than 7 at 5 minutes.
Use of epidural/neuroaxial block
One study reported on this outcome (Werner 2013). No clear difference was found in the proportion of women having an epidural between the hypnosis and relaxation group (average RR 1.05, 95% CI 0.87 to 1.27, one study, 987 women), Analysis 4.10.
4.10. Analysis.
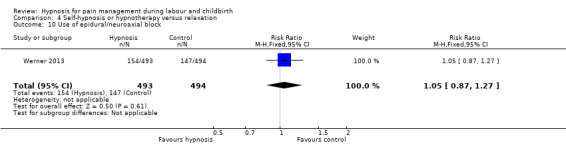
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 10 Use of epidural/neuroaxial block.
Preterm birth
One study reported on this outcome (Werner 2013). No clear difference was found in the proportion of preterm births between women in hypnosis group and the relaxation groups (RR 0.96, 95% CI 0.53 to 1.72, one study, 987 women), Analysis 4.11.
4.11. Analysis.
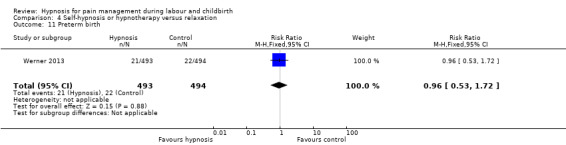
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 11 Preterm birth.
Length of labour
Both studies measured this outcome (Harmon 1990; Werner 2013). The Werner 2013 trial did not report data in a format that could be included in the review but found no clear differences between the intervention and control groups for vaginal births in duration of first stage of labour (P = 0.35), second stage of labour (P = 0.35) or for emergency caesarean births (P = 0.17), but they did not present the data separately for the two control groups (relaxation and standard care).
The other study found that women in the hypnosis group had shorter labours than those in the relaxation group (RR ‐165.20, 95% CI ‐223.53 to ‐106.87, one study, 60 women), Analysis 4.12.
4.12. Analysis.
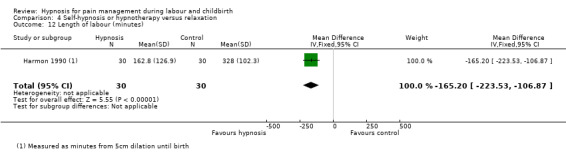
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 12 Length of labour (minutes).
Perineal trauma (episiotomy and incidence of tear ‐ greater than first degree)
One study reported on this outcome (Werner 2013). No clear difference was found in the proportion of women who experienced perineal trauma between those in the hypnosis group and the relaxation group (RR 0.91, 95% CI 0.79 to 1.04, one study, 987 women), Analysis 4.13.
4.13. Analysis.
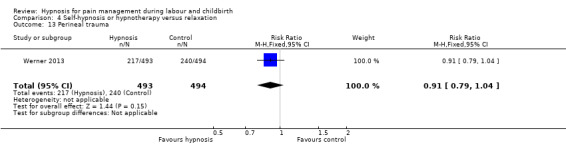
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 13 Perineal trauma.
Induction of labour
Both studies reported on this outcome (Harmon 1990; Werner 2013). No clear difference was found in the proportion of women whose labour was induced between the hypnosis group and the relaxation group (average RR 0.72, 95% CI 0.32 to 1.59, two studies, 1047 women). There was moderate statistical heterogeneity: I² = 68%, Tau² = 0.24, Chi² test for heterogeneity P = 0.08, so we used a random‐effects model, Analysis 4.14.
4.14. Analysis.
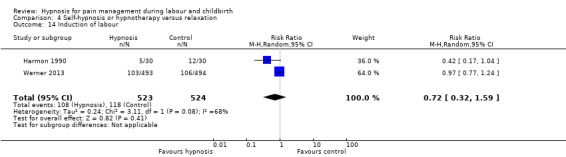
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 14 Induction of labour.
Augmentation with oxytocin
Both studies measured this outcome (Harmon 1990; Werner 2013). Data from the Harmon 1990 could not be analysed because it reported induction data separately as well as overall use of oxytocics but did not provide data for augmentation alone (Harmon 1990). It was reported that nine of the 30 women in the hypnosis group used oxytocics at some stage in labour compared with 29 of 30 women in the control group (Harmon 1990).
No clear difference was found in the proportion of women who had their labour augmented between those in the hypnosis group and the relaxation group (RR 0.94, 95% CI 0.82 to 1.07, one study, 987 women), Analysis 4.15.
4.15. Analysis.
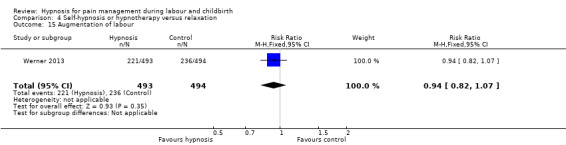
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 15 Augmentation of labour.
Primary postpartum haemorrhage (greater than 500 mL)
One study reported on this outcome (Werner 2013). No clear difference was found in the proportion of women who had a primary postpartum haemorrhage between the hypnosis group and the relaxation group (RR 0.85, 95% CI 0.68 to 1.07, one study, 987 women), Analysis 4.16.
4.16. Analysis.
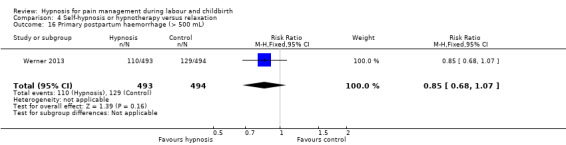
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 16 Primary postpartum haemorrhage (> 500 mL).
Postnatal depressive symptoms
One study reported on this outcome (Werner 2013). No clear difference was found for the number of women with EPDS scores of greater than 13 at 6 weeks postpartum (RR 0.86, 95% CI 0.51 to 1.46, one study, 987 women), Analysis 4.17.
4.17. Analysis.
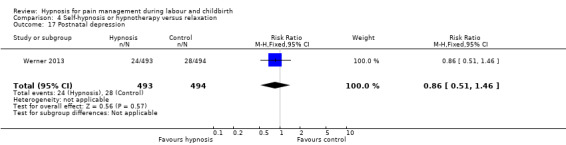
Comparison 4 Self‐hypnosis or hypnotherapy versus relaxation, Outcome 17 Postnatal depression.
Subgroup analysis ‐ Analyses 6 to 11
A relatively large number of subgroup analyses were planned to investigate potential sources of heterogeneity. Some of these analyses were specified by the generic protocol (Jones 2011) and others were specific to this review. Three of the subgroup analyses specified in the generic protocol (spontaneous labour versus induced labour; term versus preterm birth; and continuous support in labour versus no continuous support) were not applicable for this review as the hypnosis intervention was generally provided during the antenatal period rather than during labour. Those subgroups divided participants according to characteristics that occurred after randomisation and therefore were not baseline characteristics for this intervention. In addition, no data were available for the prespecified subgroup analysis of maternal anxiety levels (high versus low) so this was not performed. All subgroup analyses were prespecified although the groupings for trimester and audio CD were amended to include all available data.
Subgroup analyses were restricted to the primary outcomes and data were only available for two outcomes, use of pharmacological pain relief or analgesia and spontaneous vaginal birth. For use of pharmacological pain relief or analgesia, the following subgroup analyses did not explain the heterogeneity: nulliparous versus multiparous women (P = 0.38) Analysis 6.1; group versus one‐to‐one hypnosis sessions (P = 0.23) Analysis 8.1; hypnosis plus audio CD/tape versus hypnosis no audio CD/tape versus nurse/audio CD only (P = 0.45) Analysis 9.1; hypnosis preparation for labour versus hypnosis during labour (P = 0.67) Analysis 10.1; and high versus low hypnotisability (P = 0.81) Analysis 11.1. Similarly, these subgroups did not explain the heterogeneity for spontaneous vaginal birth: nulliparous versus multiparous women (P = 0.85) Analysis 6.2; group versus one‐to‐one hypnosis sessions (P = 0.20) Analysis 8.2; hypnosis plus audio CD/tape versus hypnosis no audio CD/tape versus nurse/audio CD only (P = 0.41) Analysis 9.2; and high versus low hypnotisability (P = 0.85) Analysis 11.2.
6.1. Analysis.
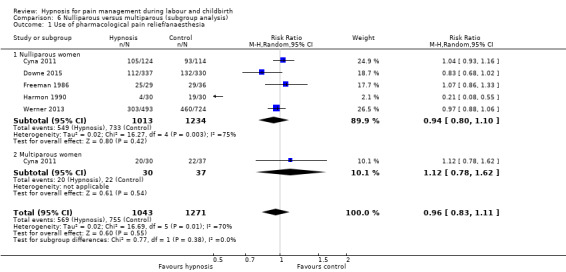
Comparison 6 Nulliparous versus multiparous (subgroup analysis), Outcome 1 Use of pharmacological pain relief/anaesthesia.
8.1. Analysis.
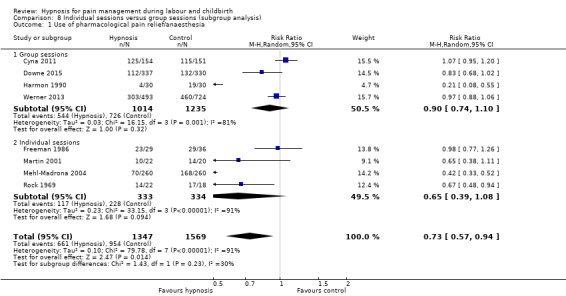
Comparison 8 Individual sessions versus group sessions (subgroup analysis), Outcome 1 Use of pharmacological pain relief/anaesthesia.
9.1. Analysis.
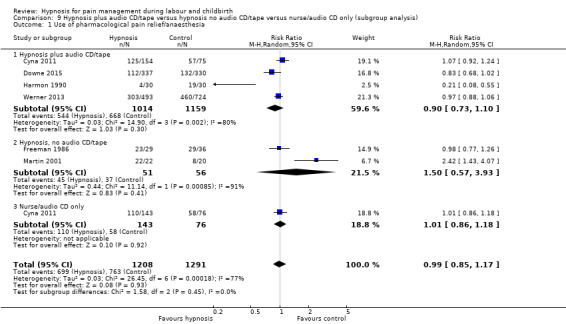
Comparison 9 Hypnosis plus audio CD/tape versus hypnosis no audio CD/tape versus nurse/audio CD only (subgroup analysis), Outcome 1 Use of pharmacological pain relief/anaesthesia.
10.1. Analysis.
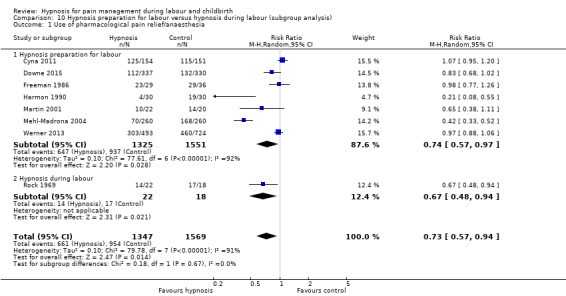
Comparison 10 Hypnosis preparation for labour versus hypnosis during labour (subgroup analysis), Outcome 1 Use of pharmacological pain relief/anaesthesia.
11.1. Analysis.
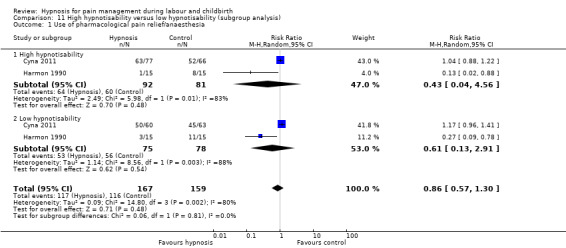
Comparison 11 High hypnotisability versus low hypnotisability (subgroup analysis), Outcome 1 Use of pharmacological pain relief/anaesthesia.
6.2. Analysis.
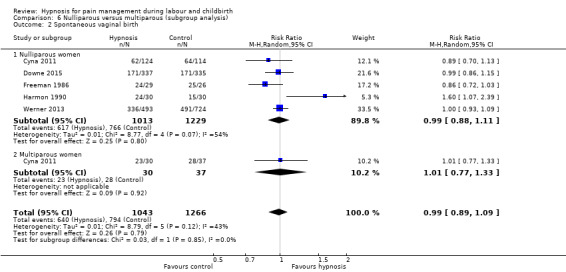
Comparison 6 Nulliparous versus multiparous (subgroup analysis), Outcome 2 Spontaneous vaginal birth.
8.2. Analysis.
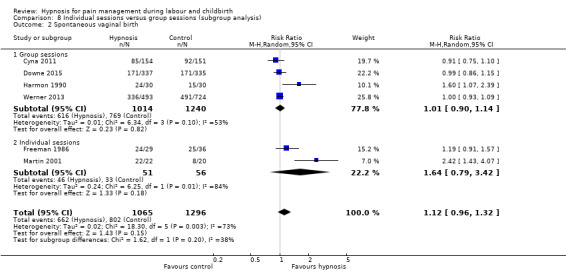
Comparison 8 Individual sessions versus group sessions (subgroup analysis), Outcome 2 Spontaneous vaginal birth.
9.2. Analysis.
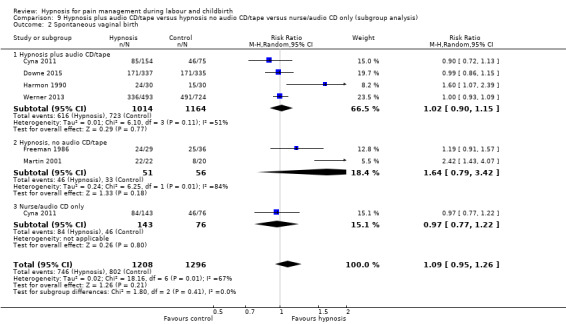
Comparison 9 Hypnosis plus audio CD/tape versus hypnosis no audio CD/tape versus nurse/audio CD only (subgroup analysis), Outcome 2 Spontaneous vaginal birth.
11.2. Analysis.
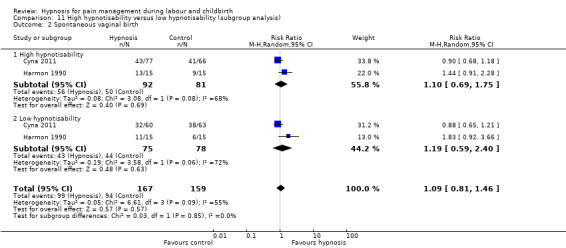
Comparison 11 High hypnotisability versus low hypnotisability (subgroup analysis), Outcome 2 Spontaneous vaginal birth.
As noted in the main results, there may be interactions between trimester at commencement of hypnosis sessions and use of pharmacological analgesia (P < 0.001) Analysis 1.1, and spontaneous vaginal birth (P = 0.002) Analysis 1.5. The use of pharmacological analgesia may be lower when women commenced hypnosis in the first or second trimester and the likelihood of spontaneous vaginal birth may be greater when women commenced hypnosis in the second trimester. However, these interactions should be interpreted with particular caution as each relied on the results of a single study.
The interaction tests also suggested that there may be a subgroup difference between the number of hypnosis sessions (less than four sessions versus four or more sessions) for both use of pharmacological pain relief (Test for subgroup differences: Chi² = 3.28, df = 1 (P = 0.07), I² = 69.5%) , Analysis 7.1 and spontaneous vaginal birth (Test for subgroup differences: Chi² = 5.12, df = 1 (P = 0.02), I² = 80.5%) Analysis 7.2. The number of hypnosis sessions may therefore have an impact on use of pharmacological pain relief and spontaneous vaginal birth and could be a possible source of the heterogeneity between studies. However, particular caution should be exercised in interpreting these results as the trials providing less than four sessions were all large, well‐designed trials, whilst the trials offering four or more sessions were small with much less information available about trial design and quality, Analysis 7.1, Analysis 7.2.
7.1. Analysis.
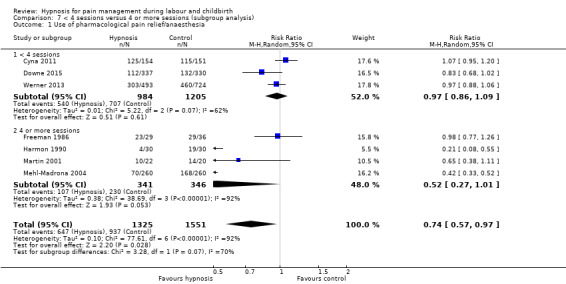
Comparison 7 < 4 sessions versus 4 or more sessions (subgroup analysis), Outcome 1 Use of pharmacological pain relief/anaesthesia.
7.2. Analysis.
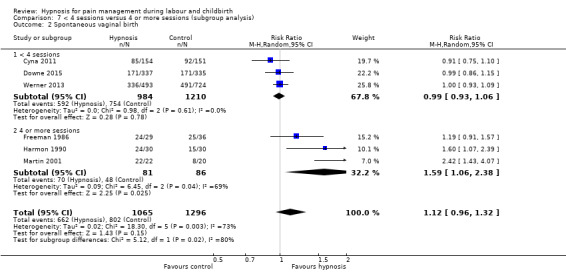
Comparison 7 < 4 sessions versus 4 or more sessions (subgroup analysis), Outcome 2 Spontaneous vaginal birth.
Subgroup comparisons generally should be treated with caution as such comparisons are observational in nature and are subject to the limitations of any observational investigation (Higgins 2011). It should also be noted that there was substantial statistical heterogeneity within the subgroups for both commencement of hypnosis in the third trimester and for four or more sessions of hypnosis. For example, for use of pharmacological analgesia within the third trimester subgroup I² = 75%, T² = 0.02, Chi² test for heterogeneity P < 0.001. There were a lack of data for the other subgroups with only one study able to be included in each group, Analysis 1.1. This increases the caution which should be used in interpreting the results of these subgroup analyses.
Sensitivity analysis
Sensitivity analysis was undertaken for the primary outcomes by excluding the two quasi‐randomised controlled trials (Harmon 1990; Rock 1969) as these were at high risk of bias for selection bias. With the quasi‐randomised studies included, women in the hypnosis group were found to be less likely to use pharmacological pain relief or anaesthesia during labour and childbirth than those in the control groups, (average RR 0.73, 95% CI 0.57 to 0.94, eight studies, 2916 women), Analysis 1.1. The result just crossed the line of no effect when the quasi‐randomised controlled trials were excluded for this outcome (average RR 0.80, 95% CI 0.62 to 1.03, six studies, 2816 women), although the same trend for a reduction in the use of pharmacological pain relief was observed in the hypnosis group.
Only one of the quasi‐randomised controlled trials provided data for the spontaneous vaginal birth outcome (Harmon 1990). The results with this trial included, found no clear difference between women in the hypnosis group and women in the control group (average RR 1.12, 95% CI 0.96 to 1.32, six studies, 2361 women), Analysis 1.5. Similarly, no clear difference was found when the Harmon 1990 trial was excluded (average RR 1.07, 95% CI 0.92 to 1.24, five studies, 2301 women).
No data from the quasi‐randomised controlled trials were available for the other primary outcomes.
Discussion
Summary of main results
We included nine trials randomising a total of 2954 women. The quality of the trials were quite variable, with several well‐designed large trials and some trials where very little was known about the trial design. For the primary outcomes, no clear differences were found between women in the hypnosis group and those in the control groups regarding satisfaction with pain relief, sense of coping with labour or spontaneous vaginal birth. Women in the hypnosis group may be less likely to use pharmacological pain relief or analgesia than those in the control groups. However, there was evidence of substantial heterogeneity for this outcome and it was assessed as being very low quality according to GRADE criteria. Sensitivity analysis indicated that this result did not reach statistical significance if the quasi‐randomised trials were removed from the analysis.
For secondary outcomes, no clear differences were found between women in the hypnosis group and women in the control group for most outcomes where data were available. There was mixed evidence regarding benefits for women in the hypnosis group compared with all control groups for pain intensity, satisfaction with childbirth experience and postnatal depressive symptoms. For each of these outcomes, data from more than one trial was available for analysis but could not be combined due to differences in measurement methods. For pain intensity one study of 60 women found those in the hypnosis group had lower mean pain scores than those in the control group, but another study of 429 women did not find a difference for memory of labour pain as "Worst imaginable" or as "Completely unbearable". For satisfaction with childbirth experience, two studies reported dichotomous data. When combined, no clear difference was found for satisfaction with the childbirth experience between women in the hypnosis group and women in the control group (370 women). One study of 1126 women reported continuous data and women in the hypnosis group were found to have a more positive experience of childbirth. For postnatal depressive symptoms, no clear difference was found between those in the hypnosis group and the control group for the three studies that used dichotomous measures (1562 women). However, another trial of 376 women reported continuous data using the Edinburugh Postnatal Depression Scale (EPDS) and found that women in the hypnosis group had slightly better (lower) EPDS scores than those in the control group. There was evidence that fewer women in the hypnosis group stayed in hospital for more than two days after the birth, but this finding was based on a single study which included a small number of women. No clear differences between women in the hypnosis group and the control groups were found for breastfeeding at hospital discharge, assisted vaginal birth, caesarean section, admission to special care baby unit/neonatal intensive care unit, Apgar score, use of epidural, preterm birth, length of labour, perineal trauma, induction of labour, augmentation of labour with oxytocin, primary postpartum haemorrhage, cost, need for postpartum blood transfusion or any other adverse events (newborn resuscitation, maternal admission to the high dependency/intensive care unit, maternal or newborn readmission to hospital or stillbirth). No data were available in a format suitable for analysis for the other outcome measures.
This updated review compared hypnosis interventions with all control groups (reported above) and also compared hypnosis with specific types of control conditions: standard care, supportive counselling and relaxation training. For the primary outcomes, no clear differences were found between women in the hypnosis group and those in the standard care control groups or the relaxation control groups. Compared with the women in the supportive counselling control group, women in the hypnosis group were less likely to use pharmacological analgesia and were more likely to have a spontaneous vaginal birth, although this finding was only based on the results of one small study. Overall, these new comparisons displayed much lower statistical heterogeneity than the comparison including all control groups.
Overall completeness and applicability of evidence
Five of the trials were undertaken in the USA, two trials in the UK, one in Australia and one in Denmark. Four of the trials included a large number of randomly assigned participants; 1222 women in the largest trial (Werner 2013), 680 in Downe 2015, 520 in Mehl‐Madrona 2004 and 448 for the other large trial (Cyna 2011). The other trials reported data for less than 70 participants (Fisher 2009; Freeman 1986; Harmon 1990; Martin 2001; Rock 1969), and two of these studies were quasi‐randomised controlled trials (Harmon 1990; Rock 1969). Inclusion and exclusion criteria were reported. Generally, trials included low‐risk nulliparous and multiparous women. Most studies involved teaching women self‐hypnosis in group classes or individual consultations and this reflects clinical practice. Some studies did not provide detailed descriptions of the hypnotic suggestions used but five of the studies (Cyna 2011; Harmon 1990; Martin 2001; Werner 2013) did provide sufficient information about the intervention to be generalisable in other settings. One study provided a detailed economic analysis which did not find a difference in the cost of pregnancy, labour and postnatal care for the hypnosis and standard care groups when the cost of the hypnosis intervention was included in the antenatal costs. This is useful information for organisations considering implementing such programs. Only one study reported the number of women who were approached to consider participating in the trial (3554 women) compared with the number who were recruited and randomised (1222 women) (Werner 2013). More data like this would assist in assessing the generalisability of the findings. One study did report data regarding 50 potentially eligible women who expressed some interest in the trial but eventually declined to participate (Cyna 2011). Most of the women (58%) did not state their reason, 24% indicated they felt their pregnancy was too advanced to attend sessions, 14% reported they definitely wanted hypnosis and 4% reported being too tired to attend all sessions (Cyna 2011).
Not all studies reported detailed demographic data for participants. One study specifically recruited teenage women (Martin 2001). Only one study compared participants with the general population of pregnant women (Cyna 2011). In that study, more than 55% of participants reported they had a tertiary education, a much higher proportion than the average among the pregnant population of that state generally (Cyna 2011). The author noted "This study population was more highly educated and older than the general pregnant population of South Australia which may have affected the generalisability of our study findings" (Cyna 2011). Another study was able to compare the demographic characteristics of participants with women who were invited to participate in the trial but did not respond (Werner 2013). Compared with the study participants, women who did not respond to the invitation were more likely to be born outside the country where the trial was conducted and were more likely to report being a smoker.
There was wide variation in the number of hypnosis sessions included in the intervention and the gestation when sessions commenced. This was explored as part of the subgroup comparisons which indicated that hypnosis earlier in pregnancy or involving more sessions may be beneficial. It is clinically plausible that hypnosis preparation earlier in the pregnancy and involving a greater number of sessions may be beneficial, particularly for self‐hypnosis. Self‐hypnosis is a skill, which can be learned, and in this context it is a skill which needs to be applied under the physical and psychological challenges of labour. There also is some evidence that hypnotic response can improve with repeated sessions (Lewis 1992). These results should be treated with caution due to the observational nature of subgroup comparisons. However, in addition, it is worth noting that the studies also reported very wide variations in women's actual attendance and practice of the techniques. For example, in one trial, in addition to attending six prenatal training sessions, participants reported practicing with an audio‐recording a mean number of 28 times individually and five times as a couple (Harmon 1990). By comparison, another study reported that "Only 26.0% of women in the Hypnosis Group and 30.8% in the CD group actually complied with all parts of the intervention, – i.e. they attended all sessions and listened at least once to each of the four CDs" (Cyna 2011). The two most recent trials reported good attendance rates, 85% of women in the hypnosis group attended all three training sessions in the Werner 2013 trial and the same percentage attended both training sessions in the Downe 2015 trial. Women in the Downe 2015 trial also reported practicing at home a median of 24 times, or approximately three times per week. These observations may be useful in planning future trials or for women interested in preparing for labour using hypnosis when considering issues of timing and practice.
Although the interventions were clinically heterogeneous, we considered it reasonable to combine the studies as the interventions were considered to be sufficiently similar to produce meaningful results. Random‐effects analysis was used when statistical heterogeneity was high, as planned and outlined in the methods section. Potential trial features, which may account for the very substantial heterogeneity in this review, were noted in the results. However, as single trials were often the source of the heterogeneity it was difficult to attribute this to any particular feature of the trial. Based on the current evidence, we cannot reliably identify the sources of most of the heterogeneity in this review.
Quality of the evidence
The 'Risk of bias' figures (Figure 1; Figure 2) indicate that the risk of bias was generally unclear for several trials. Three trials were large, well‐designed trials and were generally at low risk of bias (Cyna 2011; Downe 2015; Werner 2013). Those trials measured a large number of outcomes and found very few differences in between women in the hypnosis group and those in the control groups. Two of the trials (Harmon 1990; Rock 1969) were quasi‐randomised trials so were at high risk of selection bias. Both of these trials found that women in the hypnosis group were less likely to use pharmacological pain relief compared with those in the control group. Previous analysis of studies comparing findings of trials with adequate allocation concealment and trials with inadequate or unclear concealment of allocation (including quasi‐randomised trials) found no clear difference in four studies and larger estimates of effect in trials with inadequate allocation concealment in five studies (Odgaard‐Jensen 2011). Overall, it was concluded that predictions could not be made about the likely magnitude or even the direction of possible selection biases for such studies (Odgaard‐Jensen 2011).
Rates of follow‐up were moderate to high, considering that the intervention was conducted antenatally in all but one trial (Rock 1969). Where losses to follow‐up occurred, they generally did not appear to be related to the intervention. Blinding of participants was attempted in some studies (Cyna 2011; Harmon 1990; Martin 2001; Rock 1969), but only one study reported data on the success of this blinding (Cyna 2011). Given the difficulty of blinding participants to the intervention, risk of bias was assessed separately for subjective outcomes where lack of blinding may affect results (such as satisfaction with pain relief) and objective outcomes where lack of blinding is not likely to affect results (such as spontaneous vaginal birth). It is not possible to blind the therapist who provides the hypnotic intervention, but it is possible to blind medical personal who care for the woman during labour and outcome assessors for objective clinical outcomes. Five studies reported that outcome assessors were blinded to group allocation (Cyna 2011; Downe 2015; Harmon 1990; Mehl‐Madrona 2004; Werner 2013) and medical personal were blinded in two studies (Cyna 2011; Martin 2001). One study assessed the success of blinding medical personal and found the midwives were able to guess the group allocation for 32% of women in the hypnosis group and 58% of women in the relaxation training control group (Werner 2013).
Most of the studies included in this review were small, with less than 100 participants in each trial arm (Fisher 2009; Freeman 1986; Harmon 1990; Martin 2001; Rock 1969). Research into the effect of small studies on meta‐analyses of osteoarthritis trials found that small studies generally showed greater treatment effects than studies with at least 100 participants in each arm of the trial (Nuesch 2010), although it is not clear if this would apply more broadly.
There was a lack of consistency in the outcomes measured by the studies and there were several outcomes where information was only available from one study. This lack of data makes it difficult to fully assess any treatment effect from hypnosis for pain management for labour and birth. Authors of several studies were contacted to provide additional methodological information and results.
In this update, we have assessed the quality of the evidence using the GRADE approach as outlined in the GRADE Handbook for the primary outcomes analysed in the main comparison of self‐hypnosis or hypnotherapy versus all. The evidence was assessed as being of very low or low quality for the primary outcomes (pharmacological pain relief; spontaneous vaginal birth; satisfaction with pain relief; coping in labour). For the two outcomes, satisfaction with pain relief and coping in labour, reasons for downgrading included concerns regarding lack of blinding of subjective outcomes and evidence being derived from single studies with small sample sizes. For the other two outcomes, use of pharmacological pain relief and spontaneous vaginal birth, the main reasons for downgrading were due to: inconsistency in terms of the high level of statistical heterogeneity observed in both analyses, which could not be fully explained by subgroup analysis; and also concerns regarding limitations in design for selection and detection bias. See Table 1.
Potential biases in the review process
We attempted to minimise bias during the review process by having two people assess the eligibility of studies, assess risk of bias and extract data with a third person involved to check or review each area. We attempted to be as inclusive as possible in our search.
Agreements and disagreements with other studies or reviews
One other systematic review of hypnosis for pain management for labour and birth has been conducted (Cyna 2004). The original review of Complementary and alternative therapies for pain management in labour included hypnosis (Smith 2006), and this was later split into individual therapies and hypnosis was reviewed as a single intervention review (Madden 2012). This current review updates (Madden 2012). All reviews concluded that hypnosis may be beneficial for pain management in childbirth but noted that further large, high‐quality studies were needed as the number of women studied was small.
Authors' conclusions
Implications for practice.
There are still only a relatively small number of studies assessing the use of hypnosis for labour and childbirth. Hypnosis may reduce the overall use of analgesia during labour, though not epidural use. Further high‐ quality research is needed to more fully assess its clinical usefulness for pain management in maternity care.
Implications for research.
It is pleasing to note that the reporting on the most recent trials provided more detailed information so accurate assessments of bias could be made (for example, more explicit explanation of randomisation and blinding processes). Reporting on the training and length of experience of the hypnotherapist may also be of value. The inclusion of economic analysis in a recent trial is also pleasing, it would be useful for future trials to include such measures.
Evaluation of hypnosis interventions in institutions with and without an 'on demand' epidural service with a cost‐benefit analysis to be incorporated into the design of future studies is recommended. It may also be useful for trialists to consider the timing and number of hypnosis sessions included in the intervention.
What's new
| Date | Event | Description |
|---|---|---|
| 30 September 2015 | New citation required but conclusions have not changed | In this update, the conclusions remain largely the same, although there is now more evidence to suggest that hypnosis may result in less use of pharmacological pain relief or analgesia. |
| 30 September 2015 | New search has been performed | Search updated. Two trials have been included (Downe 2015; Werner 2013) and one trial (previously awaiting assessment) has now been excluded (Hao 1997) in this update. Methods updated to incorporate a 'Summary of findings' table and comparisons restructured to include separate comparisons for the different types of control group (all types of control; standard care; supportive counselling; relaxation). |
Acknowledgements
We gratefully acknowledge Research Associate Mohammad Othman for his work in assessing studies for inclusion and risk of bias as well as conducting data extraction and entry for the original review. We also gratefully acknowledge Shanshan Han for completing the translation and extraction of relevant information on a trial that was originally reported in Chinese for this update. We would also like to thank the staff in the Editorial Office of Cochrane Pregnancy and Childbirth, Liverpool, UK.
We would also like to thank Soo Downe and Anette Werner for providing additional data from their trials (Downe 2015; Werner 2013), to be included in this updated review.
As part of the pre‐publication editorial process, the original review was commented on by three peers (an editor and two referees who are external to the editorial team), a member of the Pregnancy and Childbirth Group's international panel of consumers and the Group's Statistical Adviser.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of their employers, the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Data and analyses
Comparison 1. Self‐hypnosis or hypnotherapy versus all.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of pharmacological pain relief/anaesthesia | 8 | 2916 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.57, 0.94] |
| 1.1 1st and 2nd trimester | 1 | 520 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.33, 0.52] |
| 1.2 2nd trimester | 1 | 42 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.38, 1.11] |
| 1.3 3rd trimester | 6 | 2354 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.75, 1.04] |
| 2 Satisfaction with pain relief (number of women who reported that they felt they had adequate pain relief) | 1 | 264 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.94, 1.20] |
| 3 Satisfaction with pain relief (7‐point scale reported two weeks postnatal) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Pethidine | 1 | 72 | Mean Difference (IV, Fixed, 95% CI) | 0.41 [‐0.45, 1.27] |
| 3.2 Entenox | 1 | 357 | Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.19, 0.57] |
| 3.3 Self‐hypnosis | 1 | 160 | Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.32, 0.88] |
| 3.4 Epidural | 1 | 127 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.40, 0.34] |
| 3.5 Water immersion | 1 | 174 | Mean Difference (IV, Fixed, 95% CI) | 0.52 [0.04, 1.00] |
| 4 Coping in labour (7‐point scale) | 1 | 420 | Mean Difference (IV, Fixed, 95% CI) | 0.22 [‐0.14, 0.58] |
| 5 Spontaneous vaginal birth | 6 | 2361 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.96, 1.32] |
| 5.1 2nd trimester | 1 | 42 | Risk Ratio (M‐H, Random, 95% CI) | 2.42 [1.43, 4.07] |
| 5.2 3rd trimester | 5 | 2319 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.93, 1.16] |
| 6 Pain intensity (Measured on McGill Pain Questionnaire Present Pain Intensity Scale) | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐1.03, ‐0.37] |
| 7 Pain intensity (memory of labour pain reported two weeks postnatal) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Memory of labour pain ‐ "Worst imaginable" | 1 | 430 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐4.14, 4.24] |
| 7.2 Memory of labour pain ‐ "Completely unbearable" | 1 | 429 | Mean Difference (IV, Fixed, 95% CI) | ‐0.26 [‐4.92, 4.40] |
| 8 Satisfaction with childbirth experience | 2 | 370 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.52, 3.59] |
| 9 Satisfaction with childbirth experience (Mean Wijmas‐Delivery Expectancy/Experience Questionnaire score at 6 weeks postpartum) | 1 | 1126 | Mean Difference (IV, Fixed, 95% CI) | ‐4.40 [‐7.22, ‐1.58] |
| 10 Breastfeeding at discharge (any) | 3 | 1826 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.98, 1.06] |
| 11 Assisted vaginal birth | 6 | 2363 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.63, 1.03] |
| 12 Caesarean section | 5 | 2756 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.60, 1.34] |
| 13 Admission to neonatal intensive care unit | 4 | 2233 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.86, 1.30] |
| 14 Apgar score less than 7 at 5 minutes | 3 | 1582 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.28, 3.71] |
| 15 Use of epidural/neuroaxial block | 6 | 2817 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.27] |
| 16 Preterm birth | 1 | 1217 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.56, 1.65] |
| 17 Length of labour (minutes) | 2 | 559 | Mean Difference (IV, Random, 95% CI) | ‐93.78 [‐233.43, 45.87] |
| 18 Perineal trauma | 1 | 1217 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.80, 1.03] |
| 19 Induction of labour | 4 | 2247 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.77, 1.25] |
| 20 Augmentation of labour | 3 | 2165 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.88, 1.08] |
| 21 Primary postpartum haemorrhage (> 500 mL) | 2 | 1522 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.59, 2.15] |
| 22 Cost (as defined by trialists) | 1 | 672 | Mean Difference (IV, Fixed, 95% CI) | 4.83 [‐257.78, 267.44] |
| 23 Need for postpartum blood transfusion | 2 | 827 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.55, 3.04] |
| 24 Postnatal depression | 3 | 1562 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.77, 1.47] |
| 25 Postnatal depression (Edinburgh Postnatal Depression Scale) | 1 | 376 | Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.28, ‐0.15] |
| 26 Number of maternal days in hospital after birth (> 2 days) | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.02, 0.83] |
| 27 Other adverse events ‐ newborn resuscitation | 1 | 520 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.11, 3.96] |
| 28 Other adverse events ‐ women readmitted to hospital | 1 | 267 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.56 [0.62, 3.90] |
| 29 Other adverse events ‐ infants readmitted to hospital | 1 | 267 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.39 [0.64, 3.02] |
| 30 Other adverse events ‐ maternal admission to HDU/ICU | 1 | 305 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.25, 8.68] |
| 31 Other adverse events ‐ stillbirth | 1 | 522 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [0.30, 27.79] |
1.26. Analysis.
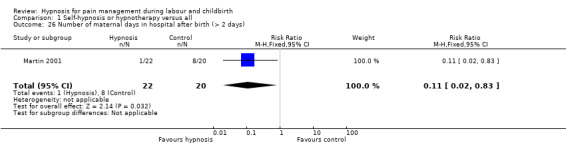
Comparison 1 Self‐hypnosis or hypnotherapy versus all, Outcome 26 Number of maternal days in hospital after birth (> 2 days).
Comparison 2. Self‐hypnosis or hypnotherapy versus standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of pharmacological pain relief/anaesthesia | 5 | 1800 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.83, 1.07] |
| 1.1 3rd trimester | 5 | 1800 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.83, 1.07] |
| 2 Satisfaction with pain relief | 1 | 264 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.94, 1.20] |
| 3 Satisfaction with pain relief (reported two weeks postnatal) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Pethidine | 1 | 72 | Mean Difference (IV, Fixed, 95% CI) | 0.41 [‐0.45, 1.27] |
| 3.2 Entenox | 1 | 357 | Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.19, 0.57] |
| 3.3 Self‐hypnosis | 1 | 160 | Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.32, 0.88] |
| 3.4 Epidural | 1 | 127 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.40, 0.34] |
| 3.5 Water immersion | 1 | 174 | Mean Difference (IV, Fixed, 95% CI) | 0.52 [0.04, 1.00] |
| 4 Coping in labour (7‐point scale) | 1 | 420 | Mean Difference (IV, Fixed, 95% CI) | 0.22 [‐0.14, 0.58] |
| 5 Spontaneous vaginal birth | 4 | 1765 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.91, 1.07] |
| 5.1 3rd trimester | 4 | 1765 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.91, 1.07] |
| 6 Pain intensity (memory of labour pain reported two weeks postnatal) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Memory of labour pain ‐ "Worst imaginable" | 1 | 430 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐4.14, 4.24] |
| 6.2 Memory of labour pain ‐ "Completely unbearable" | 1 | 429 | Mean Difference (IV, Fixed, 95% CI) | ‐0.26 [‐4.92, 4.40] |
| 7 Satisfaction with childbirth experience | 2 | 370 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.52, 3.59] |
| 8 Satisfaction with childbirth experience (Mean Wijmas‐Delivery Expectancy/Experience Questionnaire score at 6 weeks postpartum) | 1 | 678 | Mean Difference (IV, Fixed, 95% CI) | ‐4.60 [‐8.34, ‐0.86] |
| 9 Breastfeeding at discharge (any) | 3 | 1380 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.96, 1.08] |
| 10 Assisted vaginal birth | 4 | 1765 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.72, 1.06] |
| 11 Caesarean section | 3 | 1700 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.97, 1.42] |
| 12 Admission to neonatal intensive care unit | 3 | 1697 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.67, 3.12] |
| 13 Apgar score less than 7 at 5 minutes | 2 | 1028 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.18, 4.19] |
| 14 Preterm birth | 1 | 723 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.47, 2.05] |
| 15 Use of epidural/neuroaxial block | 5 | 1803 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.89, 1.16] |
| 16 Length of labour (minutes) | 1 | 499 | Mean Difference (IV, Fixed, 95% CI) | ‐22.70 [‐79.41, 34.01] |
| 17 Perineal trauma | 1 | 723 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.78, 1.09] |
| 18 Induction of labour | 3 | 1693 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.84, 1.28] |
| 19 Augmentation of labour | 3 | 1671 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.89, 1.15] |
| 20 Primary postpartum haemorrhage (> 500 mL) | 2 | 1028 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.60, 2.15] |
| 21 Cost (as defined by trialists) | 1 | 672 | Mean Difference (IV, Fixed, 95% CI) | 4.83 [‐257.78, 267.44] |
| 22 Need for postpartum blood transfusion | 2 | 827 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.55, 3.04] |
| 23 Postnatal depression | 3 | 1068 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.80, 1.66] |
| 24 Postnatal depression | 1 | 376 | Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.28, ‐0.15] |
| 25 Other adverse events ‐ women readmitted to hospital | 1 | 267 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.56 [0.62, 3.90] |
| 26 Other adverse events ‐ infants readmitted to hospital | 1 | 267 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.39 [0.64, 3.02] |
| 27 Other adverse events ‐ maternal admission to HDU/ICU | 1 | 305 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.25, 8.68] |
| 28 Other adverse events ‐ stillbirth | 1 | 522 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [0.30, 27.79] |
Comparison 3. Self‐hypnosis or hypnotherapy versus supportive counselling/psychotherapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of pharmacological pain relief/anaesthesia | 2 | 562 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.32, 0.73] |
| 1.1 1st and 2nd trimester | 1 | 520 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.33, 0.52] |
| 1.2 2nd trimester | 1 | 42 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.38, 1.11] |
| 2 Spontaneous vaginal birth | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.42 [1.43, 4.07] |
| 2.1 2nd trimester | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.42 [1.43, 4.07] |
| 3 Assisted vaginal birth | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.01, 1.95] |
| 4 Caesarean section | 2 | 562 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.03, 1.78] |
| 5 Admission to neonatal intensive care unit | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.02, 1.43] |
| 6 Use of epidural/neuroaxial block | 1 | 520 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.22, 0.40] |
| 7 Number of maternal days in hospital after birth (> 2 days) | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.02, 0.83] |
| 8 Other adverse events ‐ newborn resuscitation | 1 | 520 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.11, 3.96] |
Comparison 4. Self‐hypnosis or hypnotherapy versus relaxation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of pharmacological pain relief/anaesthesia | 2 | 1047 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.11, 2.17] |
| 1.1 3rd trimester | 2 | 1047 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.11, 2.17] |
| 2 Spontaneous vaginal birth | 2 | 1047 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.78, 1.90] |
| 2.1 3rd trimester | 2 | 1047 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.78, 1.90] |
| 3 Pain intensity (Measured on McGill Pain Questionaire Present Pain Intensity Scale) | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐1.03, ‐0.37] |
| 4 Satisfaction with childbirth experience (Mean Wijmas‐Delivery Expectancy/Experience Questionnaire score at 6 weeks postpartum) | 1 | 916 | Mean Difference (IV, Fixed, 95% CI) | ‐4.30 [‐7.45, ‐1.15] |
| 5 Breastfeeding at discharge (any) | 1 | 923 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.98, 1.06] |
| 6 Assisted vaginal birth | 2 | 1047 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.32, 1.21] |
| 7 Caesarean section | 1 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.87, 1.46] |
| 8 Admission to neonatal intensive care unit | 1 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.67, 1.23] |
| 9 Apgar score less than 7 at 5 minutes | 2 | 1047 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.25, 8.96] |
| 10 Use of epidural/neuroaxial block | 1 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.87, 1.27] |
| 11 Preterm birth | 1 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.53, 1.72] |
| 12 Length of labour (minutes) | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐165.2 [‐223.53, ‐106.87] |
| 13 Perineal trauma | 1 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.79, 1.04] |
| 14 Induction of labour | 2 | 1047 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.32, 1.59] |
| 15 Augmentation of labour | 1 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.82, 1.07] |
| 16 Primary postpartum haemorrhage (> 500 mL) | 1 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.68, 1.07] |
| 17 Postnatal depression | 1 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.51, 1.46] |
Comparison 5. Nurse/CD hypnosis versus standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of pharmacological pain relief/anaesthesia | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.89, 1.15] |
| 2 Satisfaction with pain relief | 1 | 259 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.78, 1.05] |
| 3 Spontaneous vaginal birth | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.80, 1.16] |
| 4 Satisfaction with childbirth experience | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.83, 1.07] |
| 5 Breastfeeding at discharge | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.98, 1.04] |
| 6 Assisted vaginal birth | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.78, 1.85] |
| 7 Caesarean section | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.56, 1.48] |
| 8 Admission to neonatal intensive care unit | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.67, 1.29] |
| 9 Apgar score less than 7 at 5 minutes | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.05, 5.76] |
| 10 Use of epidural/neuroaxial block | 1 | 294 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.73, 1.20] |
| 11 Induction of labour | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.68, 1.36] |
| 12 Augmentation of labour | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.82, 1.36] |
| 13 Primary postpartum haemorrhage (> 500 mL) | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.66 [0.88, 3.12] |
| 14 Need for postpartum blood transfusion | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.39 [0.92, 59.33] |
| 15 Postnatal depression | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.51, 1.32] |
| 16 Adverse effect women readmitted to hospital | 1 | 266 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.43, 3.06] |
| 17 Adverse effect infant readmitted to hospital | 1 | 266 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.9 [0.38, 2.14] |
| 18 Maternal admission to HDU/ICU | 1 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.70 [0.78, 17.50] |
Comparison 6. Nulliparous versus multiparous (subgroup analysis).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of pharmacological pain relief/anaesthesia | 5 | 2314 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.83, 1.11] |
| 1.1 Nulliparous women | 5 | 2247 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.80, 1.10] |
| 1.2 Multiparous women | 1 | 67 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.78, 1.62] |
| 2 Spontaneous vaginal birth | 5 | 2309 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.89, 1.09] |
| 2.1 Nulliparous women | 5 | 2242 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.88, 1.11] |
| 2.2 Multiparous women | 1 | 67 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.77, 1.33] |
Comparison 7. < 4 sessions versus 4 or more sessions (subgroup analysis).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of pharmacological pain relief/anaesthesia | 7 | 2876 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.57, 0.97] |
| 1.1 < 4 sessions | 3 | 2189 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.86, 1.09] |
| 1.2 4 or more sessions | 4 | 687 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.27, 1.01] |
| 2 Spontaneous vaginal birth | 6 | 2361 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.96, 1.32] |
| 2.1 < 4 sessions | 3 | 2194 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.93, 1.06] |
| 2.2 4 or more sessions | 3 | 167 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [1.06, 2.38] |
Comparison 8. Individual sessions versus group sessions (subgroup analysis).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of pharmacological pain relief/anaesthesia | 8 | 2916 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.57, 0.94] |
| 1.1 Group sessions | 4 | 2249 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.74, 1.10] |
| 1.2 Individual sessions | 4 | 667 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.39, 1.08] |
| 2 Spontaneous vaginal birth | 6 | 2361 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.96, 1.32] |
| 2.1 Group sessions | 4 | 2254 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.90, 1.14] |
| 2.2 Individual sessions | 2 | 107 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [0.79, 3.42] |
Comparison 9. Hypnosis plus audio CD/tape versus hypnosis no audio CD/tape versus nurse/audio CD only (subgroup analysis).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of pharmacological pain relief/anaesthesia | 6 | 2499 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.85, 1.17] |
| 1.1 Hypnosis plus audio CD/tape | 4 | 2173 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.73, 1.10] |
| 1.2 Hypnosis, no audio CD/tape | 2 | 107 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [0.57, 3.93] |
| 1.3 Nurse/audio CD only | 1 | 219 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.86, 1.18] |
| 2 Spontaneous vaginal birth | 6 | 2504 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.95, 1.26] |
| 2.1 Hypnosis plus audio CD/tape | 4 | 2178 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.90, 1.15] |
| 2.2 Hypnosis, no audio CD/tape | 2 | 107 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [0.79, 3.42] |
| 2.3 Nurse/audio CD only | 1 | 219 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.77, 1.22] |
Comparison 10. Hypnosis preparation for labour versus hypnosis during labour (subgroup analysis).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of pharmacological pain relief/anaesthesia | 8 | 2916 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.57, 0.94] |
| 1.1 Hypnosis preparation for labour | 7 | 2876 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.57, 0.97] |
| 1.2 Hypnosis during labour | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.48, 0.94] |
| 2 Spontaneous vaginal birth | 2 | 1889 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.93, 1.08] |
| 2.1 Hypnosis preparation for labour | 2 | 1889 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.93, 1.08] |
| 2.2 Hypnosis during labour | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
10.2. Analysis.
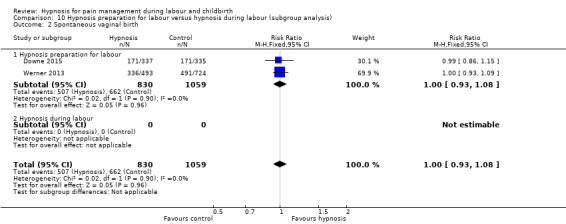
Comparison 10 Hypnosis preparation for labour versus hypnosis during labour (subgroup analysis), Outcome 2 Spontaneous vaginal birth.
Comparison 11. High hypnotisability versus low hypnotisability (subgroup analysis).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of pharmacological pain relief/anaesthesia | 2 | 326 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.57, 1.30] |
| 1.1 High hypnotisability | 2 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.04, 4.56] |
| 1.2 Low hypnotisability | 2 | 153 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.13, 2.91] |
| 2 Spontaneous vaginal birth | 2 | 326 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.81, 1.46] |
| 2.1 High hypnotisability | 2 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.69, 1.75] |
| 2.2 Low hypnotisability | 2 | 153 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.59, 2.40] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cyna 2011.
| Methods | Randomised controlled trial of parallel design conducted in Women's and Children's Hospital, Adelaide, Australia. | |
| Participants | "Inclusion criteria: women > 34 and < 39 weeks' gestation, with a singleton, viable fetus, vertex presentation, who are not in active labour and who are planning a vaginal birth. Exclusion criteria: previous hypnosis preparation for childbirth; poor understanding of English requiring a translator; women who are already enrolled in another pregnancy trial where analgesia requirements are an outcome measure; active psychological or psychiatric problems such as: active depression requiring treatment by a psychiatrist; schizophrenia; prior psychosis; severe intellectual disability. Also women with pain caused by specific pathological entities such as: congenital neuromuscular disorders; spina bifida; metastatic disease; osteoporosis; rheumatoid arthritis; fractures." |
|
| Interventions | Intervention Group 1 (n = 154): "antenatal hypnosis training in preparation for childbirth administered by a qualified hypnotherapist with the use of audio compact discs on hypnosis for re‐enforcement". Intervention Group 2 (n = 143): "antenatal hypnosis training in preparation for childbirth using audio compact discs on hypnosis administered by a nurse with no training in hypnotherapy". Controls (n = 151): "participants continue with their usual preparation for childbirth with no additional intervention" (no treatment). The hypnosis interventions were provided in 3 sessions to groups of up to 10 women. The sessions commenced "as closely as possible to 37 weeks' gestation". |
|
| Outcomes | "Use of pharmacological analgesia (nitrous oxide; opioids; epidural); use of oxytocics; mode of delivery; Apgar score less than seven at five minutes; admission to HDU/ICU; adverse effects for women (PPH => 600 mL blood transfusion; death; ICU admission); adverse effects for infants (meconium‐stained liquor; admission to neonatal unit); overall experience of pain during labour and childbirth ‐ birth experience was worse/better, same as expected; whether birth rated as positive or negative experience; how well coped with labour/childbirth (postpartum questionnaire); length of labour; length of neonatal nursery stay; length of maternal stay; number women breastfeeding at discharge, 6‐week and 6‐month follow‐up; Edinburgh Postnatal Depression Scale and Spielberger anxiety scales repeated at 6 weeks and 6 months. Hypnotisability was also measured using the Creative Imagination Scale (CIS) with high hypnotisability defined as a score greater than or equal to 23 and low hypnotisability defined as a score < 23." | |
| Notes | Principal investigator contacted on 19/8/2011 and replied "The Cyna trial is complete and it has been written up and accepted in part as a PhD thesis. We are currently preparing the paper for submission to a journal". Update January 2012 ‐ the digital thesis is now available online. The principal investigator has also provided additional data and information about methodology as requested. Update September 2015 ‐ the results of the trial have also been published in BJOG. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "computer‐generated random number sequence.” The author provided additional detail that "Study participants were stratified for parity and randomised in (unspecified) blocks of 15 by a computer random number generator." |
| Allocation concealment (selection bias) | Low risk | “we were provided with group allocation via telephone at the Department of Public Health for the first 6 months of the study and then by a password‐protected computer database program.” “The randomization sequence was inaccessible to research assistants involved in recruiting potential trial participants.” The author provided additional detail that "Allocation concealment was assured by using a computer database assignment to one of three groups, which was only revealed after patient identifiers had been entered." |
| Blinding of participants (objective outcomes) | Low risk | Participant: "All participants were informed that they may or may not appreciate which group they are in, as we believed that some women might think that the baseline testing for hypnotisability was the intervention. However, we did expect that most women allocated to usual care would probably realise they were not in an intervention group. An assessment of blinding was determined by asking participants if they thought they were in a control or intervention group in the final post‐partum questionnaire." 110 of 134 in the hypnosis believed they were in the hypnosis arm of the trial, 98 of 133 women in the CD believed they were in the hypnosis and 0 of 133 of women in the control of the trial believed they were in the hypnosis. High risk of bias for subjective outcomes (such as satisfaction with pain relief) and low risk of bias for objective outcomes (such as spontaneous vaginal birth). |
| Blinding of participants (subjective outcomes) | High risk | Participant: "All participants were informed that they may or may not appreciate which group they are in, as we believed that some women might think that the baseline testing for hypnotisability was the intervention. However, we did expect that most women allocated to usual care would probably realise they were not in an intervention group. An assessment of blinding was determined by asking participants if they thought they were in a control or intervention group in the final post‐partum questionnaire." 110 of 134 in the hypnosis group believed they were in the hypnosis arm of the trial, 98 of 133 women in the CD arm believed they were in the hypnosis arm and 0 of 133 of women in the control arm of the trial believed they were in the hypnosis arm. High risk of bias for subjective outcomes (such as satisfaction with pain relief) and low risk of bias for objective outcomes (such as spontaneous vaginal birth). |
| Blinding of personnel (performance bias) | Low risk | Clinician: confirmed with the author that clinicians caring for the women in labour were blinded to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “All data were collected and analysed by researchers who were unaware of the participants’ group allocation.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 190 women not randomised, (50 declined to participate and 140 did not meet eligibility criteria) 137 were excluded after randomisation due to protocol violations (see below). All other women analysed at birth. 48 women lost to follow‐up at 6 week follow‐up (live hypnosis group = 20, audio CD hypnosis group = 10, control group = 18). 138 women were excluded due to protocol violations 1 in active labour, 137 gestation less than or equal to 34 weeks at randomisation due to human error at the point of randomisation. The author provided additional detail that "After completing nearly two years of recruitment, we became aware that some women, who were ineligible for participation, had been inadvertently randomised, outside our eligibility criteria, prior to 34 weeks' gestation. We therefore planned to continue to recruit women to the study until our initial planned sample size of eligible women had been reached. Only those women who met all eligibility criteria for inclusion were analysed." "All primary and secondary outcomes of trial participants fulfilling all eligibility criteria were analysed using the 'Intention‐to‐treat' principle." |
| Selective reporting (reporting bias) | Low risk | All outcomes listed in trial registration reported except maternal rating of control during labour and breastfeeding rates at discharge from hospital (and breastfeeding at 6 months) ‐ data provided by the author. Additional secondary outcomes not listed in trial registration also reported. |
| Other bias | Low risk | "Our analyses of baseline data shows that the randomisation with stratification for parity produced comparable groups with the exception of the incidence of women with a history of depression, and an EPDS score > 12 being increased in the Hypnosis Group. The distribution of all other participants’ baseline demographic data across the three groups, such as mothers’ use of complementary therapies during their pregnancy, age, weight and country of birth, were also comparable." |
Downe 2015.
| Methods | "Multi‐site, pragmatic, non‐blinded RCT based on intention to treat." | |
| Participants | "680 women were randomised." "Participants were 27‐32 weeks' gestation at the time of randomisation, could read and understand English, were not on medication for hypertension or psychological illness, and were not planning an elective caesarean section. Birth partners were eligible to take part if they returned a consent form." | |
| Interventions | Intervention: "The intervention group received self‐hypnosis training in addition to usual care. Two 90‐minute group sessions were offered, 3 weeks apart, at around 32 and 35 weeks gestation". "Participants were invited to attend group sessions at their local Trust, with or without their intended birth companion. They were also advised to listen to a 26‐minute self‐hypnosis CD daily (recorded by VM) until the birth of the baby, and to complete logs of this practice, and of other antenatal educational activities. Fifteen midwives were trained in hypnosis techniques by the same trainers (though at different times). All hypnosis midwives were visited by a member of the research team at least once during a self‐hypnosis session to ensure fidelity to the intervention protocol.” Total number randomised: n = 340. Control/Comparison intervention: “Those randomised to this group continued with usual care only”. Total number randomised: n = 337. |
|
| Outcomes |
"Primary outcome measure Use of epidural analgesia for labour pain relief. Secondary outcome measures The secondary outcome measures assessed covered four domains. 1. Measures of the hypothesised mechanism of effect of the intervention · Anxiety and fear about labour (and changes in these measures over time) 2. Impact of the mechanism of effect (fear and anxiety) · Mode of labour onset · Length of labour · Use of any pharmacological pain relief 3. Outcomes associated with the use of pharmacological pain relief in labour · Method of infant feeding (breastfeeding at 6 weeks postnatal) · Mode of birth · Postnatal recollection of pain during labour 4. Measures of morbidity and of well‐being in the postnatal period · Clinical morbidity · Psychological morbidity · Satisfaction with childbirth · Preferences relating to hypnosis Secondary outcomes The main outcome of the economic analysis was the Incremental Cost Effectiveness Ratio (ICER), based on resource use per quality‐adjusted life year (QALY), measured using the EQ‐5D instrument. This assesses health status on five dimensions (mobility, self‐care, ability to undertake usual activities, pain, anxiety/depression). Three specific phases of resource utilisation were assessed: the activities undertaken during the antenatal period, an inventory of the resources required during labour, and services required as part of post‐partum admissions. Full details of the cost effectiveness analysis conducted alongside this clinical trial will be reported separately." 7‐point scale used for measure of satisfaction with pain relief at 2 weeks postpartum. |
|
| Notes | The author was contacted with a request for additional data in March 2015 and these were provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “We used a computer‐generated sequence on a 1:1 basis, without stratification or blocking.” |
| Allocation concealment (selection bias) | Low risk | “The allocation was uploaded automatically to the participant management database, accessible by password to the research team, to allow for session allocation for the intervention group.” |
| Blinding of participants (objective outcomes) | Low risk | “Blinding to randomisation was not possible for participants or the hypnosis trainers." Lack of blinding unlikely to effect objective measures. |
| Blinding of participants (subjective outcomes) | High risk | “Blinding to randomisation was not possible for participants or the hypnosis trainers." |
| Blinding of personnel (performance bias) | High risk | Author advised that personnel caring for the women in labour were not blinded to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Outcomes data were collected by staff that did not know group allocation, and returned separately to the CTU, for data linkage." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Minimal loss of women, "680 women were randomised, three in error (who were withdrawn). Two women requested withdrawal and three were lost to follow up. Data are therefore available for 672 women (337 intervention and 335 control)". None were excluded from analysis. Losses were balanced across groups and not likely to be related to the intervention. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported in published paper or provided as unpublished data. Further publications planned. |
| Other bias | Low risk | Baseline characteristics appear similar between the groups, apart for education – (% GCSE or below) – slightly more women had achieved GCSEs in the hypnosis group 21% versus 16.3% in the control group. See table 2 – baseline characteristics. |
Fisher 2009.
| Methods | Randomised controlled trial conducted in a USA hospital setting. | |
| Participants | 38 women participated in this trial, 17 in the intervention group and 21 in the control group. Inclusion criteria: "patients interested in childbirth preparatory courses". | |
| Interventions | Intervention group received hypnobirthing course while the control group received standard childbirth preparation course. | |
| Outcomes | "Coping skills" "route of delivery; birthweight, Apgar scores; intrapartum and postpartum epidural and analgesic use." | |
| Notes | This is an abstract of poster presentation and so information was very limited. Principal investigator contacted on 17/1/12 seeking further information about methodology and outcome data no reply to date ‐ September 2015. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised – no further details. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants (objective outcomes) | Low risk | Not reported, but lack of blinding unlikely to have an impact. |
| Blinding of participants (subjective outcomes) | Unclear risk | Not reported. |
| Blinding of personnel (performance bias) | Unclear risk | Not reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported. |
| Selective reporting (reporting bias) | Unclear risk | Only an abstract and so word limit on reporting of data – no numerical data reported. |
| Other bias | Low risk | Abstract reports that the "The groups were similar with respect to age, parity, and gestational age at course enrollment". |
Freeman 1986.
| Methods | Randomised controlled trial conducted in St George's Hospital Medical School, London, UK. | |
| Participants | 65 women participated in this trial, 29 in the intervention group and 36 in the control group. Inclusion criteria: "normal pregnancy and a desire to avoid epidural anaesthesia". | |
| Interventions | In the intervention group women "attended routine weekly antenatal classes". They "were also seen individually every week from 32 weeks' gestation" where they received "hypnosis regarding relaxation and pain relief. Patients were encouraged to imagine warmth or anaesthesia in 1 hand and shown how to transfer this to the abdomen". In the control group women "attended routine weekly antenatal classes". |
|
| Outcomes | Pain intensity (linear analogue scale); satisfaction with childbirth experience (“very satisfied" with labour (score 8‐10 on linear analogue scale); assisted vaginal birth; use of additional analgesia (epidural, pethidine); spontaneous vaginal birth; length of labour, duration of pregnancy. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned – no other detail. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants (objective outcomes) | Low risk | Not reported, but lack of blinding unlikely to have an impact. |
| Blinding of participants (subjective outcomes) | Unclear risk | Not reported. |
| Blinding of personnel (performance bias) | Unclear risk | Not reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 17 excluded after randomisation due to: pre‐eclampsia (1), breech presentation (3), caesarean section (9), failed to attend for hypnosis (4). |
| Selective reporting (reporting bias) | Unclear risk | Did not report pain efficacy data ‐ but short report so limit on reporting of data. |
| Other bias | Unclear risk | No baseline characteristics table. |
Harmon 1990.
| Methods | Quasi‐randomised controlled trial conducted in a USA hospital setting. | |
| Participants | 60 women participated in this trial, 30 in each arm. Inclusion criteria: "women ranging in age from 18 to 35 years, nulliparous, married, white, during the end of the second trimester of pregnancy. No reported history of (1) psychiatric hospitalisation, (2) depression during pregnancy, or (3) obstetric risk (e.g. miscarriage, pre‐eclampsia, diabetes, etc.). The study did accept women with borderline hypertension". | |
| Interventions | Experimental group: antenatal preparation was "conducted over six 1‐hour weekly sessions". Participants in the hypnosis group "heard the live hypnotic induction during Session 1 and heard the taped induction at the beginning of Sessions 2‐6". Women were then given 2 trials of an IPT using the dominant arm. Women were also given a cassette tape recording of the hypnotic induction and told to practice daily. Control group: "antenatal preparation was "conducted over 6 1‐hour weekly sessions". Control participants "listened to the control tape at the beginning of each treatment session". Women were then given 2 trials of the same IPT. Women were "given a cassette tape recording of 'Practice for Childbirth'" and told to practice daily. "Control tapes contained standard neuromuscular relaxation exercises in which women were asked to let go of tension in sequential muscle groups." Antenatal preparation began "in the early portion of the third trimester" and the sessions included up to 15 women. Both groups attended 6 childbirth education classes provided by their physicians. |
|
| Outcomes | Pain intensity (measured on the McGill Pain Questionaire Present Pain Intensity Scale where 0 = No pain, 1 = Mild, 2 = Discomforting, 3 = Distressing, 4 = Horrible, 5 = Excruciating); postnatal depressive symptoms (Depression scores on Minnesoto Mulitphasic Personality Inventory (MMPI) Depression Scale); Apgar score < 7 at 5 minutes; length of labour; spontaneous vaginal birth; use of pharmacological pain relief; caesarean section. Hypnotisability was also measured using the Harvard Group Scale of Hypnotic Susceptibility. High hypnotisability was defined as a score greater than or equal to 7 and low hypnotisability was defined as a score < 7. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised controlled trial ‐ "Assignment to one of the two treatment groups (hypnosis or control) was based solely on the month the woman was expected to deliver". |
| Allocation concealment (selection bias) | High risk | Quasi‐randomised controlled trial ‐ "Assignment to one of the two treatment groups (hypnosis or control) was based solely on the month the woman was expected to deliver". |
| Blinding of participants (objective outcomes) | Low risk | “Subjects were not informed that there were two treatment conditions; all were told that they would be receiving additional specialized childbirth training.” |
| Blinding of participants (subjective outcomes) | Unclear risk | Women not told their group allocation but there was no reporting about whether blinding was successful. |
| Blinding of personnel (performance bias) | Unclear risk | Not reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “blind ratings” noted as part of discussion of shortcomings of previous studies where the outcomes were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 women excluded because each had 1 or more pre‐treatment scores > 70 on the MMPI and 1 woman excluded due to caesarean section. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported upon. |
| Other bias | Unclear risk | No baseline demographic characteristics table presented. |
Martin 2001.
| Methods | Randomised controlled trial conducted in Alachua County Public Health Unit, Gainseville Florida, USA. | |
| Participants | 42 women participated in this trial 22 in the intervention group and 20 in the control group. Inclusion criteria: "teenage patients (18 years or younger at the time of conception)... before the end of their 24th week of pregnancy". | |
| Interventions | Experimental group received "childbirth preparation in self‐hypnosis that incorporated information on labour and delivery". Control group received "supportive counselling designed to control for interpersonal contact and social support and to provide an opportunity for discussion about pregnancy issues of concern to the patient". A retrospective comparison group of 24 women who received no specialised training was included in the study but has not been considered as part of this review as the women were not randomly assigned to the comparison group. The intervention was a 4‐session sequence provided to women on a 1‐to‐1 basis. |
|
| Outcomes | Caesarean section; spontaneous vaginal birth; assisted vaginal birth; admission to SCBU/NICU; number of maternal days in hospital after the birth; use of pharmacological pain relief, induction or augmentation with Pitocin. | |
| Notes | Information requested: email sent to authors requesting additional information on methods and clarification on definitions for outcomes (types of surgical intervention; complications; reason for hospital stay). No response to date but a copy of the PhD thesis reporting on the study has been obtained. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “randomly assigned” |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants (objective outcomes) | Low risk | “Both groups of patients received the standard prenatal treatment protocol from the medical staff, nurse practitioners, and hospital staff, all of whom were blind to group assignment.” |
| Blinding of participants (subjective outcomes) | Unclear risk | Women not told their group allocation but there was no reporting about whether blinding was successful. |
| Blinding of personnel (performance bias) | Low risk | “Both groups of patients received the standard prenatal treatment protocol from the medical staff, nurse practitioners, and hospital staff, all of whom were blind to group assignment.” |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Complications and other data “were entered in subjects’ records by obstetric staff who were unaware of the study."...“Statistical analysis was based on a simple count of the presence or absence of complications in the medical record by researchers (the researchers were not blinded to the patient’s study assignment)" not clear who made outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5 participants chose not to participate in the study prior to randomisation. Following randomisation there was a loss of 5 participants (3 moved out of the area before the birth and 1 from each group did not complete the research protocol) ‐ losses seem fairly balanced between groups and not likely to be related to the intervention. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported upon. |
| Other bias | Low risk | "There were no statistically significant differences between the groups for racial group and relationship status, the groups were also comparable for age, educational background and parity." |
Mehl‐Madrona 2004.
| Methods | Randomised study conducted in 3 locations: San Francisco, California; Tucson, Arizona; and Burlington, Vermont, USA. "10 years were required to recruit and treat 520 women (because of the limitations of how many patients could be treated at one time for free)." | |
| Participants | 520 women participated in this study. The number of participants in each arm of the study was not reported although subsequently confirmed by the author as 260 in each group. Exclusion criteria: "women in the third trimester of pregnancy, pregnant women with diagnosed high‐risk conditions, pregnant women with a DSM‐IV psychiatric diagnosis". | |
| Interventions | Hypnosis group: hypnosis sessions 1‐to‐1 with the author. Control group: "further discussion of issues that arose during the assessment (supportive psychotherapy) 1‐to‐1 with the author’s graduate psychology intern". A 'matched' comparison group, which received no specialised treatment, was included in the study but has not been considered as part of this review as the women were not randomly assigned. Women could attend for hypnotherapy or supportive psychotherapy as often as desired (subject to therapist availability). |
|
| Outcomes | Caesarean section; maternal side effects (complicated birth); newborn resuscitation; epidural use; use of pharmacological pain relief; maternal depression; low Apgar scores; primary PPH; labour induction or augmentation with oxytocin. | |
| Notes | Information requested: email sent to author requesting additional information on methods and number of participants in each arm. Response received by AMC in 2006 and 2012. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants (objective outcomes) | Low risk | Not reported, but lack of blinding unlikely to have an impact. |
| Blinding of participants (subjective outcomes) | Unclear risk | Not reported. |
| Blinding of personnel (performance bias) | Unclear risk | Not reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "An obstetrician and 2 midwives who were blind to the existence of the study reviewed each case to assess outcome variables." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | “19 subjects refused hypnosis, but were included in the hypnosis group anyway, under an intention to treat design....Ninety‐nine subjects declined an additional interview with the graduate intern... Once hypnosis was underway the author excluded from data analysis any patient who he came to diagnose with an anxiety disorder, major depressive disorder, specific axis II personality disorder (axis II traits were acceptable), a psychotic disorder, dysthymic disorder, cyclothymia, or other major affective disorder.” No details were reported regarding the number of women who were excluded from the hypnosis and control groups. |
| Selective reporting (reporting bias) | High risk | Apgar score and PPH not reported upon. Induction and augmentation with oxytocin not reported numerically. |
| Other bias | Unclear risk | No baseline characteristics. |
Rock 1969.
| Methods | Single‐centre quasi‐randomised controlled trial at Temple University Obstetrical Servlce, Philadelphia, Pennsylvania, USA. | |
| Participants | 40 women in labour “Patients were selected from the wards of the Temple University Obstetrical Service, and they were selected by the following criteria: a) the patients were believed to be at term; b) as far as could be ascertained, no obstetrical or other abnormalities existed; c) the patients were believed to be in labour; and d) labour had not progressed beyond 4 cm of cervical dilation". | |
| Interventions | Hypnosis group: hypnosis with suggestions for comfort, relaxation and anaesthesia provided by a medical student who sat by the woman. The medical student also undertook routine medical observations and examinations. Control: a medical student sat by the woman and undertook routine medical observations and examinations (usual care). |
|
| Outcomes | Use of pharmacological analgesia, pain intensity, use of epidural/neuroaxial block as additional analgesia, postnatal depressive symptoms. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised controlled trial ‐ "the patient was assigned, at any hour of the day or night, to either the experimental (hypnotic) or control group if she met the criteria for the study. If the last digit of the hospital history number was odd, the patient was assigned to the experimental group; if the digit was even, the patient was assigned to the control group." |
| Allocation concealment (selection bias) | High risk | Quasi‐randomised controlled trial with an attempt to conceal allocation "in order to eliminate any bias in assigning patients to either the experimental or the control group, history number was concealed until after the patient had been examined and the decision had been made that she met all the criteria for the study." |
| Blinding of participants (objective outcomes) | Low risk | "After the patient was assigned to the experimental group, the hypnotist began the procedure by telling her that he would help her with her labour. The patient was not told that she was to be hypnotized; she was not asked if she wished to be helped." |
| Blinding of participants (subjective outcomes) | Unclear risk | Women not told their group allocation but there was no reporting about whether blinding was successful. |
| Blinding of personnel (performance bias) | High risk | The hypnosis intervention was provided by main care provider for labour so high risk of bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Some outcomes were assessed by the hypnotist, some by a resident and postpartum outcomes were assessed by a co‐author who had not been present in the labour room and who was not previously known to the woman. Unclear if the resident and/or co‐authors were blind to women's group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intervention was provided during labour and no losses were noted. |
| Selective reporting (reporting bias) | Unclear risk | Results mainly reported in the narrative and only tabulated for the experimental group. Only reports results for pain as a P value "patients in the experimental group rated their experience as less painful" (P < 0.01). |
| Other bias | Unclear risk | Baseline characteristics for patients not presented ‐ narrative report on groups being comparable for ages, despite differences in parity ‐ no other detail. |
Werner 2013.
| Methods | The trial was "randomised, controlled, single‐blinded" and "used a three‐arm group design consisting of an intervention group, an active comparison group, and a control group receiving ordinary antenatal care". | |
| Participants | A total of 1222 women were randomised. "... no chronic diseases, uncomplicated pregnancy, nulliparous, older than 18 years, and able to understand and speak Danish." | |
| Interventions | Intervention: "The hypnosis group attended three 1‐hour classes on self‐ hypnosis for childbirth held over three consecutive weeks. A test for hypnotic susceptibility was conducted during the first session... The programme included three audiorecordings including a 20‐minute section especially meant for labour". Total number randomised: n = 497. "The active comparison group (named ‘the relaxation group’...) also attended three antenatal classes, each lasting 1 hour. The programme was taught by the same midwives as in the intervention group and included a variety of body awareness, relaxation and mindfulness techniques. This course also included audiorecordings for homework and labour." Total number randomised: n = 495. "The usual care group received only ordinary antenatal care, which included a nuchal translucency scan at about 12 weeks of gestation, an anomaly scan at about 19 weeks of gestation, four to five visits at the midwifery clinics, and a tour of the birth department." Total number randomised: n = 230. |
|
| Outcomes | "The primary endpoint was the use of epidural analgesia during birth. Self‐reported pain was examined as a secondary outcome." Onset of birth (preterm birth; PROM or PPROM) Duration of childbirth
Mode of delivery
Intervention
Child
Postpartum outcomes
"Baseline information and data on self‐reported pain were collected by questionnaire. The first questionnaire was completed at recruitment and included among others: The Ten‐item Perceived Stress Scale, the World Health Organization (WHO)‐5 Wellbeing questionnaire and the following questions about expectancy for labour and labour pain on an 11‐point Likert scale: How do you expect you will experience the pain intensity during labour? To what extent do you expect the labour pain will influence your birth experience in a negative way? To what extent do you expect the labour pain will influence your birth experience in a positive way? How do you expect you will experience the childbirth in general? (Five‐point Likert scale) Six weeks postpartum, the women completed a second questionnaire that included information about their pain experience during labour and delivery. The participants only completed the specific questions about the pain experience if it was relevant. On 11‐point Likert scales (scores: 0–10), they rated the level of perceived pain intensity at the end of the first stage of labour, during the second stage of labour, and just before receiving epidural analgesia, if relevant. They were also asked to what extent their labour pain influenced their birth experience positively and negatively, their perceived level of calmness, and whether they had experienced sufficient pain relief during birth. The Wijmas Delivery Expectancy/Experience Questionnaire, version A (W‐DEQ A) and version B (W‐DEQ B) were used to assess the childbirth experience. This instrument is a well‐validated tool. W‐DEQ A measures fear, confidence, and expectations concerning the upcoming childbirth and W‐DEQ B evaluates the same aspects of the actual childbirth experience." |
|
| Notes | The author was contacted in May 2015 and provided additional data including a copy of her PhD dissertation on the trial. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The participants were randomly allocated to either an intervention group (n = 497), an active comparison group (n = 495), or a control group (n = 230) using a computer‐generated interactive voice‐response telephone randomisation system. The randomisation programme used the participant’s unique personal identification number, which ensured that the participant could only be randomised once." |
| Allocation concealment (selection bias) | Low risk | "The participants were randomly allocated to either an intervention group (n = 497), an active comparison group (n = 495), or a control group (n = 230) using a computer‐generated interactive voice‐response telephone randomisation system. The randomisation programme used the participant’s unique personal identification number, which ensured that the participant could only be randomised once." Comment: presumably the use of an Interactive Voice Response Randomization System meant that assignment could not be foreseen. |
| Blinding of participants (objective outcomes) | Low risk | No blinding, but, lack of blinding unlikely to effect objective measures. |
| Blinding of participants (subjective outcomes) | High risk | No blinding. |
| Blinding of personnel (performance bias) | Unclear risk | "The midwives assisting the birth were blinded to the allocated treatment as the participants were told not to inform the staff about their type of training. The effectiveness of this blinding was investigated by asking the midwife to estimate the woman’s allocate treatment immediately after the delivery. We received 699 (59.8%) forms from the midwives on their estimation of the women’s allocated treatment." "The accuracy of the midwives estimation was highest in the relaxation group (58.4%) and lowest in the hypnosis group (31.5%)." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Information about the participant’s allocated treatment was removed from the data set, so that data management could be performed without knowledge of the participant’s allocated treatment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 excluded from hypnosis group and 1 excluded from relaxation group after randomisation due to not meeting inclusion criteria. "Information was available for all participants with respect to baseline characteristics and the primary outcome: use of epidural analgesia. The overall response rate for the questionnaire 6 weeks postpartum was high (97.0% in the control group and 98.4% in the two intervention groups)." |
| Selective reporting (reporting bias) | Low risk | A few outcomes specified in the protocol have not been reported in any of the 3 reports of the trial or the PhD dissertation: infection during birth and 6 weeks postpartum (mother and child); child’s condition and well‐being at 6 months follow‐up. Comment: a request for further information was sent to the first author who provided additional data, including the PhD dissertation. The 2 missing outcomes are a very small proportion of the many reported for the trial and were not considered to put the trial at significant risk of reporting bias. |
| Other bias | Low risk | Baseline characteristics similar between the 3 groups, apart for education – where control group had fewer women who had no higher education – 17 (3.5% hypnosis group compared to 10, 2.0 % in relaxation group compared to only 2, 0.9% in care as usual group) – reported in 2 reports. |
DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders 4th edition EPDS: Edinburgh Postnatal Depression Scale HDU: high dependency unit ICU: intensive care unit IPT: ischaemic pain task MMPI: Minnesota Multiphasic Personality Inventory NICU: neonatal intensive care unit PPH: postpartum haemorrhage PPROM: preterm premature rupture of membranes PROM: premature rupture of membranes SCBU: special care baby unit
Characteristics of excluded studies [ordered by study ID]
Differences between protocol and review
The protocol stated that we would exclude quasi‐randomised trials. We revised this decision to include quasi‐randomised controlled trials due to the small number of trials available for inclusion in the original review. This decision also ensured that the current review is consistent with the inclusion criteria used for the earlier review of complementary and alternative therapies for pain management in labour which included hypnosis (Smith 2006).
The planned subgroup comparisons for trimester (first versus second versus third trimester; first and second trimester versus third trimester) at commencement of hypnosis was revised to; first and second trimester versus second trimester versus third trimester as all trials could be included in this format within the one comparison.
The planned subgroup comparison for method of hypnosis intervention delivery (audio CD versus no audio CD) was revised to; hypnosis plus audio CD versus hypnosis no audio CD versus nurse/audio CD only to include data from all groups where audio CDs were used.
For the 2015 update, the comparisons were restructured to include separate comparisons for the different types of control group, comparing hypnosis with: standard care (Comparison 2), supportive counselling (Comparison 3) and relaxation training (Comparison 4). In this update (2015), the control groups supportive counselling (Martin 2001) and supportive psychotherapy (Mehl‐Madrona 2004) were judged to be similar enough to be combined as supportive counselling. Similarly, the control groups relaxation training (Harmon 1990) and relaxation and mindfulness training (Werner 2013) were judged to be similar enough to be combined as relaxation training. A 'Summary of findings' table has been added.
Contributions of authors
K Madden: screened papers for eligibility; carried out quality appraisal, data extraction and data entry; wrote to authors of papers for additional information; entered data into RevMan; carried out data analysis; updated description of studies and effects of interventions sections; re‐wrote final draft of review.
AM Cyna: conceived the review topic, contributed to writing the draft manuscript.
P Middleton: reviewed the draft update, provided advice on statistical analysis and methodology.
M Matthewson: commented on drafts.
L Jones: screened papers for eligibility; carried out quality appraisal, data extraction and data entry; checked data in RevMan; produced the 'Summary of findings' table; reviewed drafts of review.
Sources of support
Internal sources
University of Liverpool, UK.
External sources
-
Nursing and Allied Health Scholarship and Support Scheme (NAHSSS), Australia.
K Madden has been supported by a scholarship from the NAHSSS funded by the Department of Health and Ageing. The views expressed in this review do not necessarily represent those of the NAHSSS, its Administrator, Services for Australian Rural and Remote Allied Health (SARRAH) and/or the Australian Government Department of Health and Ageing.
-
National Institute for Health Research, UK.
Cochrane‐NHS Engagement Project No: 10/4000/02
The above project supported Leanne Jones's involvement as author in the original review (2012)
Declarations of interest
K Madden used hypnosis during the births of her two children. She is employed as a psychologist with St Helen's Private Hospital and as a Grassroots Community Development Worker with MI Fellowship. Until October 2015 she offered private calmbirth® childbirth education classes in Hobart, these classes included psychological strategies for comfort. She has also received payment for giving professional development talks to midwives and doulas about calmbirth® classes.
Philippa Middleton ‐ none known.
AM Cyna conducted the Hypnosis Antenatal Training for Childbirth (HATCh) randomised controlled trial that is included in this review. None of the study assessors were involved in the HATCh trials but AM Cyna was K Madden's secondary supervisor for honours and was the secondary supervisor for a masters thesis which was based on the original Cochrane review. M Matthewson was the primary supervisor for the masters thesis but had no involvement with the HATCh trial.
Mandy Matthewson is employed by the University of Tasmania and has also received payment Private Practice at Salamanca Psychology, Hobart. She was also the primary supervisor for K Madden's masters thesis which was based on the original Cochrane review.
Leanne Jones is employed by the University of Liverpool as an Associate Editor with Cochrane Pregnancy and Childbirth. Her employment is supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. She had no involvement with the editorial processes for this review update.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Cyna 2011 {published and unpublished data}
- Cyna A. Hypnosis antenatal training for childbirth (HATCh): a randomised controlled trial (ongoing trial). ClinicalTrials.gov (http://www.clinicaltrials.gov/ct2/show/NCT00282204) (accessed January 13, 2011) 2006. [DOI] [PMC free article] [PubMed]
- Cyna A, Andrew M, Robinson J, Crowther C. Antenatal hypnosis training for childbirth: a randomised controlled trial. Anaesthesia and Intensive Care 2010;38(6):111‐2. [Google Scholar]
- Cyna A, Crowther C, Robinson J, Andrew M, Antoniou G, Baghurst P. Hypnosis antenatal training for childbirth: a randomised controlled trial. BJOG: an international journal of obstetrics and gynaecology 2013;120(10):1248‐59. [DOI] [PubMed] [Google Scholar]
- Cyna AM. The HATCh Trial: Hypnosis Antenatal Training for Childbirth (PhD thesis) (http://digital.library.adelaide.edu.au/dspace/bitstream/2440/69216/1/02whole.pdf). Adelaide, Austraila: The University of Adelaide, 2011. [Google Scholar]
- Cyna AM, Andrew MI, Robinson JS, Crowther CA, Baghurst P, Turnbull D, et al. Hypnosis antenatal training for childbirth (HATCh): a randomised controlled trial. BMC Pregnancy and Childbirth 2006;6:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyna AM, Andrew MI, Whittle C. Hypnosis antenatal training for childbirth (HATCh): Intervention Scripts 1 and 4. Australian Journal of Clinical and Experimental Hypnosis 2007;35(1):83‐94. [Google Scholar]
Downe 2015 {published and unpublished data}
- Downe S. Self‐hypnosis for intrapartum pain management (ship) trial. ISRCTN Registry (http://www.isrctn.com/) [accessed 10 September 2015] 2011.
- Downe S. The SHIP trial ‐ a randomised controlled trial of self‐hypnosis during labour. http://www.midirs.org/development/MIDIRSEssence.nsf/articles/F329431A7FF3E593802578A90052BFA5 (accessed 14 December 2011). ISRCTN27575146 2011.
- Downe S, Finlayson K, Melvin C, Spiby H, Ali S, Diggle P, et al. Self‐hypnosis for intrapartum pain management in pregnant nulliparous women: a randomised controlled trial of clinical effectiveness. BJOG: an international journal of obstetrics and gynaecology 2015;122(9):1226‐34. [DOI: 10.1111/1471-0528.13433] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fisher 2009 {published data only}
- Fisher B, Esplin S, Stoddard G, Silver R. Randomized controlled trial of hypnobirthing versus standard childbirth classes: patient satisfaction and attitudes towards labor. American Journal of Obstetrics and Gynecology 2009;201(6 Suppl 1):S61‐S62. [Google Scholar]
Freeman 1986 {published data only}
- Freeman RM, Macaulay AJ, Eve L, Chamberlain GVP. Randomised trial of self hypnosis for analgesia in labour. British Medical Journal 1986;292:657‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harmon 1990 {published data only}
- Harmon TAM. Hypnotic Analgesia in Childbirth [PhD thesis]. Milwaukee: The University of Wisconsin‐ Milwaukee, 1982. [Google Scholar]
- Harmon TM, Hynan MT, Tyre TE. Improved obstetric outcomes using hypnotic analgesia and skill mastery combined with childbirth education. Journal of Consulting & Clinical Psychology 1990;58:525‐30. [DOI] [PubMed] [Google Scholar]
Martin 2001 {published data only}
- Martin AA. The effects of hypnosis and supportive counselling on the labor processes and birth outcomes of pregnant adolescents [PhD thesis]. Gainesville: University of Florida, 1987. [Google Scholar]
- Martin AA, Schauble PG, Rai SH, Curry RW Jr. The effects of hypnosis on the labor processes and birth outcomes of pregnant adolescents. Journal of Family Practice 2001;50(5):441‐3. [PubMed] [Google Scholar]
Mehl‐Madrona 2004 {published data only}
- Mehl‐Madrona LE. Hypnosis to facilitate uncomplicated birth. American Journal of Clinical Hypnosis 2004;46(4):299‐312. [DOI] [PubMed] [Google Scholar]
Rock 1969 {published data only}
- Rock NL, Shipley TE, Campbell C. Hypnosis with untrained, nonvolunteer patients in labor. International Journal of Clinical and Experimental Hypnosis 1969;17(1):25‐36. [DOI] [PubMed] [Google Scholar]
Werner 2013 {published and unpublished data}
- Werner A. Antenatal Hypnosis Training ‐ the Effect on Pain Expereince, Duration of Birth and other Birth Outcomes (PhD thesis). Aarhus University, 2013. [Google Scholar]
- Werner A. The effect of mental training on childbirth measured on pain experience and other birth outcomes. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 5 September 2015] 2009.
- Werner A, Uldbjerg N, Zachariae R, Nohr EA. Effect of self‐hypnosis on duration of labor and maternal and neonatal outcomes: a randomized controlled trial. Acta Obstetricia et Gynecologica Scandinavica 2013;92(7):816‐23. [DOI] [PubMed] [Google Scholar]
- Werner A, Uldbjerg N, Zachariae R, Rosen G, Nohr E. Self‐hypnosis for coping with labour pain: a randomised controlled trial. BJOG: an international journal of obstetrics and gynaecology 2013;120(3):346‐53. [DOI] [PubMed] [Google Scholar]
- Werner A, Uldbjerg N, Zachariae R, Wu CS, Nohr EA. Antenatal hypnosis training and childbirth experience: a randomized controlled trial. Birth 2013;40(4):272‐80. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Guse 2006 {published data only}
- Guse T, Wissing M, Hartman W. The effect of a prenatal hypnotherapeutic programme on postnatal maternal psychological well‐being. Journal of Reproductive and Infant Psychology 2006;24(2):163‐77. [Google Scholar]
Hao 1997 {published data only}
- Hao TY, Li YH, Yao SF. Clinical study on shortening the birth process using psychological suggestion therapy. Zhonghua Hu Li Za Zhi 1997;32(10):568‐70. [PubMed] [Google Scholar]
Additional references
Alexander 2009
- Alexander B, Turnbull D, Cyna A. The effect of pregnancy on hypnotizability. American Journal of Clinical Hypnosis 2009;52(1):13‐22. [DOI] [PubMed] [Google Scholar]
AMA Council on Mental Health 1958
- American Medical Association Council on Mental Health. Hypnosis. Journal of the American Medical Association 1958;168(1):57. [Google Scholar]
Anim‐Somuah 2011
- Anim‐Somuah M, Smyth RMD, Jones L. Epidural versus non‐epidural or no analgesia in labour. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD000331.pub3] [DOI] [PubMed] [Google Scholar]
Barber 1979
- Barber TX, Wilson SC. The Barber Suggestibility Scale and the Creative Imagination Scale: experimental and clinical applications. American Journal of Clinical Hypnosis 1979;21(2‐3):84‐108. [DOI] [PubMed] [Google Scholar]
Barragán 2011
- Barragán Loayza IM, Solà I, Juandó Prats C. Biofeedback for pain management during labour. Cochrane Database of Systematic Reviews 2011, Issue 6. [DOI: 10.1002/14651858.CD006168.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
BMA Working Party 1955
- Psychological Medicine Group Committee of the British Medical Association. Medical use of hypnotism. British Medical Journal 1955;1(4920):190‐3. [Google Scholar]
Bonica 1990a
- Bonica JJ, editor. Definitions and taxonomy of pain. The Management of Pain. 2nd Edition. Malvern: Lea & Febiger, 1990:18‐27. [Google Scholar]
Bonica 1990b
- Bonica JJ, McDonald JS. The pain of childbirth. In: Bonica JJ editor(s). The Management of Pain. 2nd Edition. Malvern: Lea & Febiger, 1990:1313‐43. [Google Scholar]
BPS Working Party 2001
- British Psychological Society Working Party. The Nature of Hypnosis. A report prepared by a Working Party at the request of The Professional Affairs Board of The British Psychological Society. Leicester: British Psychological Society, 2001. [Google Scholar]
Caton 2002
- Caton D, Corry MP, Frigoletto FD, Hopkins DP, Lieberman E, Mayberry L, et al. The nature and management of labor pain: executive summary. American Journal of Obstetrics and Gynecology 2002;186(5 Suppl 1):1‐15. [DOI] [PubMed] [Google Scholar]
Chooi 2011
- Chooi CSL, Nerlekar R, Raju R, Cyna AM. The effects of positive or negative words when assessing postoperative pain. Anaesthesia and Intensive Care 2011;39(1):101‐6. [DOI] [PubMed] [Google Scholar]
Chooi 2013
- Chooi CS, White A, Tan SGM, Cyna AM. Pain vs comfort scores after Caesarean section: a randomized trial. British Journal of Anaesthesia 2013;110(5):780‐7. [DOI] [PubMed] [Google Scholar]
Cluett 2009
- Cluett ER, Burns E. Immersion in water in labour and birth. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD000111.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cyna 2004
- Cyna AM, McAuliffe GL, Andrew MI. Hypnosis for pain relief in labour and childbirth: a systematic review. British Journal of Anaesthesia 2004;93(4):505‐11. [DOI] [PubMed] [Google Scholar]
Cyna 2009
- Cyna AM, Andrew MI, Tan SGM. Communication skills for the anaesthetist. Anaesthesia 2009;64(6):658‐65. [DOI] [PubMed] [Google Scholar]
Derry 2012
- Derry S, Straube S, Moore RA, Hancock H, Collins SL. Intracutaneous or subcutaneous sterile water injection compared with blinded controls for pain management in labour. Cochrane Database of Systematic Reviews 2012, Issue 1. [DOI: 10.1002/14651858.CD009107.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dick‐Read 1947
- Dick‐Read G. Childbirth Without Fear: The Principle and Practice of Natural Childbirth. London: Heinemann Medical, 1947. [Google Scholar]
Dowswell 2009
- Dowswell T, Bedwell C, Lavender T, Neilson JP. Transcutaneous electrical nerve stimulation (TENS) for pain management in labour. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD007214.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Faymonville 2000
- Faymonville ME, Laureys S, Degueldre C, DelFiore G, Luxen A, Franck G, et al. Neural mechanisms of antinociceptive effects of hypnosis. Anesthesiology 2000;92(5):1257‐67. [DOI] [PubMed] [Google Scholar]
Gamsa 2003
- Gamsa A. Hypnotic analgesia. In: Melzack R, Wall PD editor(s). Handbook of Pain Management: A Clinical Companion to Wall and Melzack's Textbook of Pain. Sydney: Churchill Livingstone, 2003:521‐31. [Google Scholar]
Gaskin 2003
- Gaskin IM. Ina May's Guide to Childbirth. New York: Bantam Dell, 2003. [Google Scholar]
Green 1998
- Green J, Coupland V, Kitzinger J. Great Expectations: A Prospective Study of Women's Expectations and Experiences of Childbirth. 2nd Edition. Cheshire: Books for Midwives Press, 1998. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 (updated March 2011). The Cochrane Collaboration 2011. Available from www.cochrane‐handbook.org.
Hodnett 2013
- Hodnett ED, Gates S, Hofmeyr GJ, Sakala C. Continuous support for women during childbirth. Cochrane Database of Systematic Reviews 2013, Issue 7. [DOI: 10.1002/14651858.CD003766.pub5] [DOI] [PubMed] [Google Scholar]
Howell 2009
- Howell, M. Effective Birth Preparation. Headley Down: Intuition UN, 2009. [Google Scholar]
Jones 2011
- Jones L, Dou L, Dowswell T, Alfirevic Z, Neilson JP. Pain management for women in labour: generic protocol. Cochrane Database of Systematic Reviews 2011, Issue 6. [DOI: 10.1002/14651858.CD009167] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2012
- Jones L, Othman M, Dowswell T, Alfirevic Z, Gates S, Newburn M, et al. Pain management for women in labour: an overview of systematic reviews. Cochrane Database of Systematic Reviews 2012, Issue 3. [DOI: 10.1002/14651858.CD009234.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Klomp 2012
- Klomp T, Poppel M, Jones L, Lazet J, Nisio M, Lagro‐Janssen ALM. Inhaled analgesia for pain management in labour. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD009351.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kroger 1957
- Kroger WS, DeLee ST. Use of hypnoanesthesia for cesarean section and hysterectomy. Journal of the American Medical Association 1957;163(6):442‐4. [DOI: 10.1001/jama.1957.82970410001009] [DOI] [PubMed] [Google Scholar]
Lawrence 2013
- Lawrence A, Lewis L, Hofmeyr GJ, Styles C. Maternal positions and mobility during first stage labour. Cochrane Database of Systematic Reviews 2013, Issue 10. [DOI: 10.1002/14651858.CD003934.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewis 1992
- Lewis DO. Hypnoanalgesia for chronic pain: the response to multiple inductions at one session and to separate single inductions. Journal of the Royal Society of Medicine 1992;85:620‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lowe 1989
- Lowe NK. Explaining the pain of active labour: the importance of maternal confidence. Research Nursing and Health 1989;12(4):237‐45. [DOI] [PubMed] [Google Scholar]
Lowe 2002
- Lowe NK. The nature of labor pain. American Journal of Obstetrics and Gynecology 2002;186(5 Suppl 1):16‐24. [DOI] [PubMed] [Google Scholar]
Lundgren 1998
- Lundgren I, Dahlberg K. Women's experience of pain in childbirth. Midwifery 1998;14:105‐10. [DOI] [PubMed] [Google Scholar]
Maquet 1999
- Maquet P, Faymonville ME, Degueldre C, Delfiore G, Luxen A, Franck G, et al. Functional neuroanatomy of hypnotic state. Biological Psychiatry 1999;45(3):327‐33. [DOI] [PubMed] [Google Scholar]
McCutcheon‐Rosegg 1996
- McCutcheon‐Rosegg S, Ingraham E, Bradley RA. Natural Childbirth the Bradley Way. Revised. New York: Plume, 1996. [Google Scholar]
McIntyre 2010
- McIntyre PE, Schug SA, Scott DA, Visser EJ, Walker SM, editors. Acute Pain Management: Scientific Evidence. 3rd Edition. Melbourne: ANZCA & FPM, 2010. [Google Scholar]
Melzack 1984
- Melzack R, Kinch R, Dobkin P, Lebrun M, Taezner P. Severity of labour pain: influence of physical as well as psychologic variables. Canadian Medical Association Journal 1984;130(5):579‐84. [PMC free article] [PubMed] [Google Scholar]
Mongan 2005
- Mongan MF. HypnoBirthing: The Mongan Method. 3rd Edition. Deerfield Beach: Health Communications, 2005. [Google Scholar]
Montgomery 2000
- Montgomery GH, Duhamel KN, Redd WH. A meta‐analysis of hypnotically induced analgesia: how effective is hypnosis?. International Journal of Clinical and Experimental Hypnosis 2000;48(2):138‐53. [DOI] [PubMed] [Google Scholar]
Novikova 2012
- Novikova N, Cluver C. Local anaesthetic nerve block for pain management in labour. Cochrane Database of Systematic Reviews 2012, Issue 4. [DOI: 10.1002/14651858.CD009200.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nuesch 2010
- Nuesch E, Trelle S, Reichenback S, Rutjes AWS, Tschannen B, Altman DG, et al. Small study effects in meta‐analyses of osteoarthritis trial: meta‐epidemiological study. BMJ 2010;341:c3515. [DOI: 10.1136/bmj.c3515] [DOI] [PMC free article] [PubMed] [Google Scholar]
Odgaard‐Jensen 2011
- Odgaard‐Jensen J, Vist GE, Timmer A, Kunz R, Akl EA, Schunemann H, et al. Randomisation to protect against selection bias in healthcare trials. Cochrane Database of Systematic Reviews 2011, Issue 4. [DOI: 10.1002/14651858.MR000012.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Othman 2012
- Othman M, Jones L, Neilson JP. Non‐opioid drugs for pain management in labour. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD009223.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Patterson 2003
- Patterson DR, Jensen, M. Hypnosis and clinical pain. Psychological Bulletin 2003;129(4):495‐521. [DOI] [PubMed] [Google Scholar]
Platonov 1960
- Platonov K. Psychotherapeutic methods and their application in painless childbirth: Lectures for obstetricians. In: Nikolaev AP, Vel'vovskii IZ, Velvovsky I editor(s). Painless Childbirth through Psychoprophylaxis. Moscow: Foreign Languages Publication House, 1960. [Google Scholar]
Rainville 1997
- Rainville P, Duncan GH, Price DD, Carrier B, Bushnell C. Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science 1997;277:968‐71. [DOI: 10.1126/science.277.5328.968] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Samko 1975
- Samko MR, Schoenfeld LS. Hypnotic susceptibility and the Lamaze childbirth experience. American Journal of Obstetrcis and Gynecology 1975;121:631‐6. [DOI] [PubMed] [Google Scholar]
Simkin 2004
- Simkin P, Bolding A. Update on nonpharmacologic approaches to relieve labor pain and prevent suffering. Journal of Midwifery & Women's Health 2004;49(6):489‐504. [PUBMED: 15544978] [DOI] [PubMed] [Google Scholar]
Simmons 2012
- Simmons SW, Taghizadeh N, Dennis AT, Hughes D, Cyna AM. Combined spinal‐epidural versus epidural analgesia in labour. Cochrane Database of Systematic Reviews 2012, Issue 10. [DOI: 10.1002/14651858.CD003401.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2006
- Smith CA, Collins CT, Cyna AM, Crowther CA. Complementary and alternative therapies for pain management in labour. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD003521.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2011a
- Smith CA, Collins CT, Crowther CA. Aromatherapy for pain management in labour. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD009215] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2011b
- Smith CA, Collins CT, Crowther CA, Levett KM. Acupuncture or acupressure for pain management in labour. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD009232] [DOI] [PubMed] [Google Scholar]
Smith 2011c
- Smith CA, Levett KM, Collins CT, Crowther CA. Relaxation techniques for pain management in labour. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD009514] [DOI] [PubMed] [Google Scholar]
Smith 2012
- Smith CA, Levett KM, Collins CT, Jones L. Massage, reflexology and other manual methods for pain management in labour. Cochrane Database of Systematic Reviews 2012, Issue 2. [DOI: 10.1002/14651858.CD009290.pub2] [DOI] [PubMed] [Google Scholar]
Stam 1984
- Stam HJ, McGrath PA, Brooke RI. The effects of a cognitive‐behavioral treatment program on temporo‐mandibular pain and dysfunction syndrome. Psychosomatic Medicine 1984;46(6):534‐45. [DOI] [PubMed] [Google Scholar]
Trentin 2001
- Trentin L, Visentin M, Marco R, Zanolin E. Prevalence of pain in a public hospital: correlation between patients and caregivers. Journal of Headache and Pain 2001;2(2):73‐8. [DOI: 10.1007/PL00012189] [DOI] [Google Scholar]
Ullman 2010
- Ullman R, Smith LA, Burns E, Mori R, Dowswell T. Parenteral opioids for maternal pain management in labour. Cochrane Database of Systematic Reviews 2010, Issue 9. [DOI: 10.1002/14651858.CD007396.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Madden 2012
- Madden K, Middleton P, Cyna AM, Matthewson M, Jones L. Hypnosis for pain management during labour and childbirth. Cochrane Database of Systematic Reviews 2012, Issue 11. [DOI: 10.1002/14651858.CD009356.pub2] [DOI] [PubMed] [Google Scholar]


