Abstract
Purpose
To define a distraction distance (pull length) cut-off that would differentiate those patients with hip microinstability and those without the disorder, called the Pull-Out Test.
Methods
In total, 100 consecutive patients undergoing hip arthroscopy were included in the study. Patients were separated into a hip microinstability group (HMI) and non-hip microinstability group (NHI) based on the results of Beighton's score, the abduction–extension–external rotation test, hip extension–external rotation examination, and the prone instability test. Inclusion criteria were patients with an magnetic resonance imaging-proven labral tear who did not respond to conservative treatment and underwent hip arthroscopy. Exclusion criteria included those patients undergoing revision hip arthroscopy, had a previous surgery on the ipsilateral hip, or had severe arthritis in the hip. The Pull-Out Test was performed before surgery with the hip in 30° of abduction and the foot in 30° of external rotation. A blinded examiner places gross axial traction on the leg until a firm end point is reached. The distraction distance between the femoral head and acetabulum is the pull length.
Results
In total, 32 patients made up the HMI group whereas 68 patients were in the NHI group. The average pull length for the NHI group was 0.9 ± 0.1 cm and 1.7 ± 0.4 cm for the HMI group (P < .001). Subtracting the standard deviation from the HMI group average, when defined a cut off for hip microinstability as 1.3 cm. Using this value, we found the Pull-Out Test to have a sensitivity of 0.91 and specificity of 0.96. The positive predictive value for the Pull Test was 0.91 and the negative predictive value 0.97.
Conclusions
The Pull-Out Test is a useful test in identifying and confirming the presence of hip microinstability in patients undergoing hip arthroscopy. A pull-length of 1.3 cm or greater is consistent with the presence of microinstability with a specificity of 94% and a sensitivity of 96%.
Level of Evidence
Level IV, diagnostic, case-control study.
Hip arthroscopy for the treatment of femoroacetabular impingement and labral tears demonstrates good results in the literature.1, 2, 3, 4, 5, 6, 7, 8, 9 However, as our understanding of hip mechanics improves, it appears some hips not as stable as once believed.10 The bony acetabulum covers 170° of the femoral head and is oriented with 48° ± 4° of lateral cephalad tilt in the coronal plane and 21° ± 5° of anterior tilt in the sagittal plane.11, 12 The bony acetabular architecture of the hip covers more of the posterior hip as compared with the anterior hip, causing the soft-tissue structures of the anterior hip to play a greater role in stability.9 The major stabilizing soft-tissue structures of the anterior hip are the labrum and hip capsule. The hip capsule is a complex structure made up of the iliofemoral (y-ligament of Bigelow), ischiofemoral, and pubofemoral ligaments. Loss of hip capsule integrity can lead to dysfunction of the hip joint and poor outcomes following hip arthroscopy.13, 14, 15 Capsular closure after hip arthroscopy has shown improved outcomes compared with partial closure.16
In addition to iatrogenic hip instability following hip arthroscopy, hip instability may be present in the native hip before surgery. Hip instability can cause hip pain along with intra-articular pathologies that contribute to pain originating from the hip joint.9, 17, 18, 19 Hip instability can be categorized into gross instability and microinstability. High-energy injuries can lead to hip dislocations and gross hip instability.9 Microinstability of the hip is a relatively new clinical entity that may cause hip pain in young athletes.17 Microinstability is defined as motion of the hip joint beyond physiologic range leading to pain with or without the sensation of joint unsteadiness.20 Considered factors that contribute to hip microinstability include ligamentous or capsular laxity and muscular weakness of the hip and pelvic region.17 Sporting activities associated with repetitive hip joint rotation and axial loading are considered factors in the development of hip microinstability.9, 20 In the setting of intra-articular pathology such as labral tears, surgical intervention in a patient with microinstability may be necessary if conservative treatment fails.17, 21 The described surgical treatment for microinstability in the absence of severe dysplasia is capsular plication.11, 17, 22 This tightens the capsule, leading to less volume within the hip joint, subsequently decreasing the micromotion of the femoral head within the joint.
Although effective treatments for hip microinstability have been described, the diagnosis of this disorder remains elusive.23 To optimize outcomes in patients with microinstability, it is paramount the surgeon identifies the presence of the disorder either before surgery or intraoperatively. No definitive preoperative test, including history, physical examination, or radiologic findings can clearly identify hip microinstability. Several physical examination maneuvers have been described to help identify patients with hip microinstability, including the Beighton criteria, Dial examination, abduction–hyperextension and external rotation (AB-HEER), prone-instability, and the hyperextension-ER (HEER) tests.9, 17, 24, 25 These physical examination maneuvers show good specificity and sensitivity, but a more reliable and reproducible confirmatory test would be helpful.26
Shibata et al.27 described a dynamic hip examination using traction before hip arthroscopy to help identify patients with hip microinstability. The test relies on the number of turns of traction it takes for a patient to distract well enough to perform hip arthroscopy.27 This method relies on the use of a specific traction device and cannot be used universally with all surgical setups. A test that can be universally used regardless of traction device to confirm the presence of hip microinstability would eliminate this difficulty in confirming diagnosis.
We describe a confirmation test for hip microinstability, known as the Pull-Out Test, where the anterior structures are placed on maximum tension and gross manual traction is placed on the operative leg. The distraction distance between the femoral head and acetabulum is then measured to determine the distraction distance. The purpose of this study was to define a distraction distance (pull length) cut-off that would differentiate those patients with hip microinstability and those without the disorder, called the Pull-Out Test. We hypothesized there would be a significant increase in hip distraction distance (pull length) in patients with preoperatively diagnosed hip microinstability by physical examination versus those patients with negative preoperative testing for microinstability.
Methods
The study was conducted from September 2017 until June 2018 and concluded once 100 participants were available for the study. One hundred consecutive patients undergoing hip arthroscopy by a single surgeon were included in the study. All participants consented to participate, and the study was approved by institutional review board. Inclusion criteria for the study included any patients undergoing hip arthroscopy with magnetic resonance imaging–proven labral tears who had not responded to more than 3 months of conservative treatment, including formal physical therapy. Exclusion criteria included those patients undergoing revision hip arthroscopy, previous ipsilateral fracture, and any patient with advanced osteoarthritis with a Tönnis grade >1.
Chart review was performed to obtain patient demographics. Each patient's alpha-angle, lateral center-edge angle, and Tönnis grade were measured using preoperative plain radiographs. A Beighton score and physical examination were performed and documented. Preoperative hip examinations included the flexion–adduction–external rotation examination, flexion–abduction and external rotation, and hip range of motion. In addition, 3 physical examination maneuvers described in the literature to specifically identify hip microinstability were performed at the patient's preoperative visit. These tests included the AB-HEER, HEER, and the prone instability test. The AB-HEER test was first described by Domb et al.25 and is performed with the patient in the lateral decubitus position with the affected extremity up. The leg is then abducted 30°, hyperextended, and externally rotated with anterior pressure placed on the posterior greater trochanter area using the examiner's hand. The test is positive when the maneuver elicits pain in the anterior hip. The HEER test is performed with the patient supine with their legs hanging over the foot of the bed.17 The hip is then placed in extension and external rotation while the contralateral hip is placed in flexion. Reproduction of the patient's anterior hip pain is considered a positive test for hip microinstability. The prone instability test is performed with the patient in the prone position.24 The hip is externally rotated while the examiner places anterior force on the posterior aspect of the greater trochanter. Reproduction of the anterior hip pain constitutes a positive test. A patient that had a positive test in any 1 of the 3 microinstability tests was placed into the hip microinstability group (HMI). Patients who did not have pain with any of the maneuvers were placed in the non-hip microinstability group (NMI).
All patients enrolled in the study underwent conventional hip arthroscopy. The procedures were performed with the patient in the lateral decubitus position using a Smith & Nephew Lateral Hip Distractor (Andover, MA) with a well-padded traction boot under general anesthesia with complete muscular relaxation. The patient was placed on a bean bag for support and their bony prominences were well padded with gel pads. The nonoperative leg was left free on the operative table with a gel pad under the fibular head to protect the peroneal nerve.
Pull-Out Test
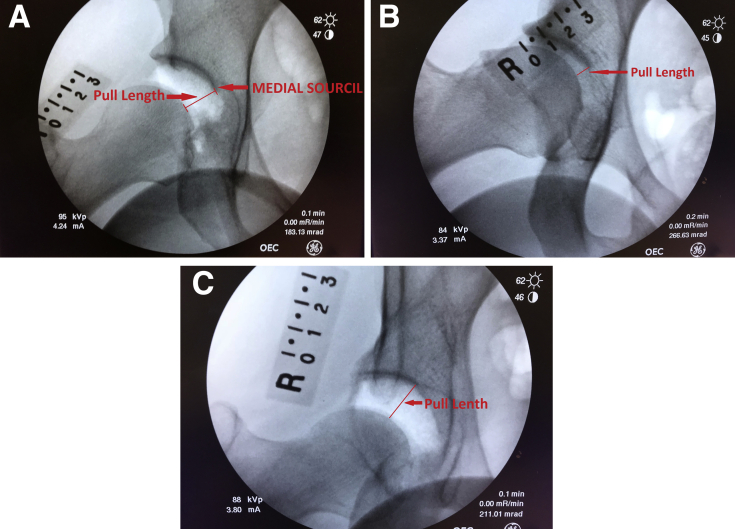
The Pull-Out Test is performed with the patient in the lateral decubitus position for this study but could be done in the supine position depending on surgeon preference. A 3-cm radiographic marker with 10-mm markings was taped over the anterior superior iliac spine before prepping and draping. A large C-arm was positioned in the anteroposterior position and a scout shot taken to confirm appropriate positioning and rotation of the hip and pelvis. The operative leg is then abducted 30° and placed in 30° of extension (Fig 1A). The foot is then externally rotated 30° (Fig 1B). Manual traction is then placed on the leg until a solid end-point is appreciated and no further gross distraction is possible (Fig 2). At this point, the gross traction is locked and second anteroposterior image of the operative hip is taken with the radiographic marker present in the image. The pull-length was the amount of distraction of the femoral head out of the acetabulum measured at the medial most aspect of the sourcil straight down to the femoral head (Fig 3 A-C).
Fig 1.
The Pull Test. (A) The Pull-Out Test is performed with the patient in the lateral decubitus position in this example. Under general anesthesia with full relaxation, the right leg is abducted 30°. A C-arm is placed in the anteroposterior position. (B) The leg is placed in 30° of extension and the foot is externally rotated 30° to put maximum tension on the anterior capsule.
Fig 2.
The Pull-Out Test is completed with the examiner placing an axial pull on the right leg using gross traction until a firm end-point is reached. A fluoroscopic image is obtained at this point and the distraction distance is measured.
Fig 3.
(A) Anteroposterior fluoroscopic image of the right hip during the Pull-Out Test. The pull length is measured from the medial sourcil down to the femoral head. (B) A Pull Test image in a patient without hip microinstability. The distance measures 0.6 cm. (C) A Pull-Out Test that is positive with a pull length of 1.7 cm, which exceeds the cut off found in the study of 1.3 cm.
The pull-length was measured directly on the C-arm screen using length measuring software when available. In situations in which measuring software was not available, the calibrated radiographic marker was used to measure the length. The length between the acetabulum and the femoral head was measured with a caliper directly on the C-arm screen. One centimeter was then measured on the radiographic marker. The measured length of distraction was divided by the measured length of 1 cm to determine the pull-length. The Pull Test was performed twice on each patient, once by the operating surgeon and once by the assistant. The assist performing the test varied from case to case and included residents and nurse practitioner first-assistants. Both pull-lengths were measured by the surgeon. The 2 pull-lengths were averaged creating the final pull-length that was used for the study. The examiners were blinded to the physical examination findings at the time of surgery.
Once testing was completed, the radiographic marker was removed, and fine traction was placed on the leg, if necessary, to create roughly 1.5 cm of hip distraction. Anterior and anterolateral portals were created under fluoroscopic guidance. Hip arthroscopy was then performed through an interportal capsulotomy repairing the labrum with suture anchors and performing femoral osteoplasty if the patient had an alpha-angle of 55° or more on preoperative Dunn views. Patients in the NMI group underwent capsular closure following the procedure using 2 or 3 FiberWire (Arthrex, Naples, FL) sutures passed in a simple interrupted fashion using a Slingshot suture passer (Stryker, Denver, CO) to close the interportal capsulotomy. Patients in the HMI group underwent capsular plication. Capsular plication was performed with the hip in 30° of flexion. The suture was passed through the proximal limb of the capsule anteriorly and then through the distal limb of the capsule roughly 2 cm distal to the cut edge. This was repeated 2 more times posteriorly. The large bite of capsule distally allowed for overlapping of the edges when the sutures were tied creating a plication of the capsule.28
All 100 patients were grouped into the HMI group or the NHI group based on the results of the AB-HEER, HEER, and prone instability tests performed preoperatively. The mean pull-lengths and their corresponding standard deviation of both the HMI and NHI groups were calculated. The mean pull-length of the HMI group minus the standard deviation for the group represented the cut-off value for the presence of hip microinstability. An a priori power analysis was conducted using a power of 80%, an expected difference of 10 mm, standard deviation of 15 mm, and an alpha of 0.05 giving a 90-patient sample size. Using this cut off, specificity, sensitivity, positive predictive value, and negative predictive value of the test were determined. In addition, as the data collected were continuous, an intraclass correlation coefficient was calculated. The Student t test was used to compare differences in demographic factors, physical examination findings, radiologic measurement, and the mean pull lengths between HMI and NHI groups. A P value of ≥ .05 was considered statistically significant.
Results
Of the 100 patients, 32 tested positive for hip microinstability using the 3 preoperative tests designed to identify hip microinstability and made up the HMI group. The other 68 did not test positive for hip microinstability and were placed in the NMI group. Demographics of each group are shown in Table 1. There was no difference between the 2 groups with regards to side of procedure or age. Regarding sex, the HMI group was made up of 28 female and 4 male patients, whereas the NMI group had 30 female and 38 male patients (P < .01). Height and body mass index were not statistically different between the 2 groups. Table 2 summarizes the physical examination findings between the 2 groups. The HMI group had statistically greater internal rotation and external rotation compared with the NHI group. The HMI group mean Beighton score was 5.16 ± 2.33 versus 0.88 ± 2.2 in the NHI group (P < .001). Of the 32 patients who tested positive for hip microinstability, 24 had a Beighton score greater than 4 and 8 had a score of 3 or less. In the patients who tested negative for hip microinstability by physical examination, 11 had Beighton scores of 4 or greater and 57 had Beighton scores of 3 or less. A positive Dial examination was found in 67% of the HMI group and 20% of the NHI group (P = .004). The alpha angle and Tönnis grade between the 2 groups were similar; however, the center-edge angle of the HMI group was significantly less than in the NHI group (P = .04). Radiographic findings are presented in Table 3. Seven of the patients in the HMI group had dysplasia, whereas no patient in the NMI group had dysplasia.
Table 1.
Patient Demographics
| HMI Group | NMI Group | |
|---|---|---|
| Side | 19 right/13 left | 36 right/32 left |
| Age | 31.8 ± 17.5 | 39.4 ± 13.3 |
| Sex* | 4 male/28 female | 38 male/30 female |
| Height | 169.1 ± 7.6 cm | 172.8 ± 7.6 cm |
| Weight* | 66.9 ± 17.8 kg* | 77.8 ± 16.6 kg |
| BMI | 23 ± 5.9 | 25.8 ± 4.8 |
NOTE. There was no significant difference between the 2 groups except for sex and weight, which had a P value ≤ .05 (represented by *).
BMI, body mass index; HMI, hip microinstability group; NMI, non-hip microinstability group.
Table 2.
Physical Examination Findings of Patients
| HMI Group | NMI Group | |
|---|---|---|
| Internal rotation* | 43.3 ± 10.2° | 27.2 ± 14.1° |
| External rotation* | 70.3 ± 14.3° | 50.3 ± 19.6° |
| Dial examination* | 22 positive/10 negative | 14 positive/54 negative |
| Beighton score* | 5.2 | 0.9 |
NOTE. Physical examination findings were significantly different between the 2 groups (*represents P ≤ .05).
HMI, hip microinstability group; NMI, non-hip microinstability group.
Table 3.
Radiologic Findings of Study Subjects
| HMI Group | NMI Group | |
|---|---|---|
| Alpha Angle | 54.3 ± 7.7° | 58 ± 6.8° |
| CEA* | 25.5 ± 5.6° | 30.6 ± 7° |
| Tönnis grade | 0.33 | 0.68 |
NOTE. Cam lesion size was not significantly different between the 2 groups, but the CEA in the HMI group was significantly lower than the NMI group (*P ≤ .05).
CEA, center-edge angle; HMI, hip microinstability group; NMI, non-hip microinstability group.
The mean pull-length was 0.9 ± 0.1 cm in the NHI group and 1.7 ± 0.4 cm in the HMI group (P < .001). The range for the pull-length of the NHI group was 0.5 to 1.5 cm. The HMI pull-length range was 0.9 to 2.5 cm. Using the mean pull-length for the HMI group and subtracting the standard deviation, we found that the cut off for positive microinstability of the Pull-Out Test was 1.3 cm. Using this cutoff, we found that the sensitivity of the Pull-Out Test was 0.94, whereas specificity was 0.96. Positive predictive value was 0.91 and negative predictive value was 0.97 using our classification of hip microinstability described previously (Table 4).
Table 4.
Test Statistics: Sensitivity, Specificity, PPV, and NPV
| Sensitivity | 0.94 |
| Specificity | 0.96 |
| PPV | 0.91 |
| NPV | 0.97 |
NPV, negative predictive value; PPV, positive predictive value.
Discussion
Using the intraoperative “Pull-Out Test,” we found that a pull length of 1.3 cm identifies those patients with microinstability with a sensitivity of 94% and a specificity of 96%. Microinstability of the hip is recognized as a source of pain and disability in patients without arthritic changes in the hip.26 However, no consistent objective criteria for the diagnosis of the disorder or clear quantitative findings confirming the presence of hip microinstability exist. Currently, the diagnosis is based on a thorough history, physical examination, and radiographic examination of the hip. Dynamic imaging can be performed including axial traction or placing the hip in positions of apprehension, but these images are difficult to obtain logistically and can be painful for the awake patient. In this study, we described the Pull-Out Test, a dynamic test that is performed just before hip arthroscopy that can help identify patients with hip microinstability or confirm their diagnosis. The Pull-Out Test is performed by placing the hip in 30° of abduction, extension, and external rotation, and then placing gross traction on the leg until a firm end point is felt. By measuring the distraction present in this position, confirmation of microinstability can be made.
The anterior structures of hip including the labrum and capsule function to stabilize the hip. Cadaveric studies have shown the anterior aspect of the labrum to withstand the greatest tensile strain in the hip.29, 30, 31 The hip capsule also plays a major role in hip stability. The capsule is made up of 3 ligaments including the iliofemoral, pubofemoral, and ischiofemoral ligaments. The strongest of the 3 ligaments and the primary ligament of the anterior hip capsule is the iliofemoral ligament (y-ligament of Bigelow), which restricts extension and is a static restraint of the hip when it is in full extension.10, 32 Hewitt et al.32, 33 showed that the iliofemoral ligament is stiffer and withstands greater force than the other 2 hip capsule ligaments. Insufficiency of the iliofemoral ligament has been proposed as a major factor leading to hip microinstability.34 The pubofemoral ligament also helps control external rotation of the hip in extension in concert with the iliofemoral ligament.35 Cadaveric studies have shown placing the hip into extension, external rotation, and abduction places the highest tensile strain through the anterior capsule and labrum.29, 30, 31 The Pull-Out Test was designed to put maximum tension on the anterior structures stabilizing the hip by positioning the hip in extension, external rotation and abduction and then placing maximum manual traction on the hip to determine the distraction length between the femoral head and acetabulum. Increased distraction of the hip in this position points to dysfunction of these anterior hip structures consistent with hip microinstability.
The diagnosis of hip microinstability is typically made with a combination of clinical and physical examination findings. In our study, patients in the HMI group had significantly greater internal and external rotation of the hip compared with the patients in the NHI group. This finding was expected, since a known risk factor for hip microinstability is hyperlaxity.9, 17 The Beighton score has commonly been used to identify patients with generalized ligamentous laxity.36 In our study, the Beighton score was significantly greater in the HMI group compared with the NHI group. However, 25% of patients in the HMI had a Beighton score of 3 or less, which is considered normal in terms of laxity.36 If based on the Beighton score alone, these patients would not have been considered to have hip microinstability, and plication of their capsule would not have been performed. However, all 8 of the patients in the HMI group with Beighton scores of 3 or less had positive Pull-Out Tests. This confirms the Pull-Out Test may be able to identify those patients with microinstability who do not have gross ligamentous laxity.
Several physical examination maneuvers have been described to aid in identifying hip microinstability including the log roll test, dial Examination, abduction–hyperextension–external rotation test, prone instability test, and the hyperextension–external rotation test.17, 24, 25 Hoppe et al.26 studied the effectiveness of 3 physical examination tests in identifying hip microinstability. The study compared the abduction–hyperextension–external rotation test, prone instability test, and the hyperextension–external rotation test. The study found the AB-HEER test to most accurately identify hip instability with a sensitivity of 80.6% and specificity of 89.4%. The prone instability test had a sensitivity of 33.9% and a specificity 97.9%. The HEER test showed a sensitivity of 71% and specificity of 85.1%. The Pull-Out Test's sensitivity of 94% was greater than any of these 3 physical examination tests, and its specificity of 96% was similar to the specificity achieved by the prone instability test, which had the greatest specificity of all the 3 tests studied. The high sensitivity and specificity of the Pull-Out Test makes it an effective confirmatory test to identify hip microinstability.
Shibata et al.27 described a test similar to the Pull-Out Test to confirm the presence of hip microinstability. The test determined hip microinstability based on the number of turns of traction necessary to distract the hip using a MIS Hip Interventions table (Maquet, Wayne, NJ). A hip that required less than 10 turns of fine traction was considered to have microinstability. The study also determined hip microinstability by venting the hip with a spinal needle and releasing traction. Any hip with residual widening of the medial joint of more than 3 mm after traction was released was considered positive for hip microinstability. These tests are a useful tool in confirming the presence of hip microinstability but are limited to the use of a specific traction device and cannot be used universally with all distractors. The Pull Test relies on direct measurement of the distraction distance and can be reproduced on any of the available traction devices on the market. The medial sourcil was chosen as the reference point on the acetabulum to measure distraction distance because it is a reproducible point that is present in all hips. The sourcil is the radio-dense subchondral bone of the weight-bearing dome of the acetabulum. The lateral edge was not used since it is not always easy to determine depending on the clarity of the radiograph or the presence of osteoarthritis. In addition, the presence of lateral osteophytes or an os acetabuli can make it difficult to measure hip distraction accurately using the lateral edge. The medial sourcil is less affected by the presence of arthritis and osteophytes of the hip and is easy to identify on radiographs, making it a reproducible point on the acetabulum to measure the distraction distance.
Limitations
The study has inherent limitations. The major limitation of this study is the lack of a confirmatory test to identify hip microinstability. Placing patients in the HMI and NMI groups was dependent on 3 physical examination findings meant to identify microinstability. Unfortunately, none of these physical examination maneuvers are 100% sensitive or specific for identifying patients with hip microinstability. A patient who tested positive for any of the 3 tests was considered positive for hip microinstability. Another option would have been to only place patients in the HMI group if they tested positive in multiple tests. However, this would have led to a very small population in the HMI group. A second limitation to the study is the small number of patients in the HMI group compared with the NMI group. However, this represents the typical distribution of hip microinstability present in the population. The power of the study was appropriate to identify statistical differences between the 2 study populations pointing to an appropriate number of patients in each group.
Another limitation is the fact the study was conducted using the lateral position. Lateral position was chosen for the study due to the senior author's preferred position for hip arthroscopy. The concept behind the Pull-Out Test is to place the anterior hip capsule on tension by abducting, extending, and externally rotating the hip. This position can be obtained in either the lateral or supine position. Although the senior author has used the Pull-Out Test in both the lateral and supine positions to confirm hip microinstability, the pull-length of 1.3 cm has not been formally tested in the supine position. Repeating the study in the supine position would be helpful to confirm the findings in this study in addition to variation in examiners individual strengths during assessment. In addition, individual patient's habitus may change measurements as measurements are performed by laying a ruler external to the patient. Finally, the outcomes of the hip arthroscopies performed in this study were not reported. A future study looking at the outcomes of patients with hip microinstability determined by the Pull-Out Test would be helpful in confirming the usefulness of the test.
Conclusions
The Pull-Out Test is a useful test in identifying and confirming the presence of hip microinstability in patients undergoing hip arthroscopy. A pull-length of 1.3 cm or greater is consistent with the presence of microinstability with a specificity of 94% and a sensitivity of 96%.
Footnotes
The authors report the following potential conflict of interest or source of funding: A.C.: Arthrex (Consultant and Speakers Bureau), Desert Mountain Medical (consultant fees), Trice Medical (consultant fees), Stryker (educational conference, residents), and Smith and Nephew (educational grant). Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Alradwan H., Philippon M.J., Farrokhyar F., et al. Return to preinjury activity levels after surgical management of femoroacetabular impingement in athletes. Arthroscopy. 2012;28:1567–1576. doi: 10.1016/j.arthro.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 2.Byrd J.T. Femoroacetabular impingement in athletes: Current concepts. Am J Sports Med. 2014;42:737–751. doi: 10.1177/0363546513499136. [DOI] [PubMed] [Google Scholar]
- 3.Byrd J.T., Jones K.S. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2003;19:1055–1060. doi: 10.1016/j.arthro.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 4.Byrd J.W., Jones K.S. Hip arthroscopy in athletes: 10-year follow-up. Am J Sports Med. 2009;37:2140–2143. doi: 10.1177/0363546509337705. [DOI] [PubMed] [Google Scholar]
- 5.Byrd J.T., Jones K.S. Hip arthroscopy for labral pathology: Prospective analysis with 10-year follow-up. Arthroscopy. 2009;25:365–368. doi: 10.1016/j.arthro.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Byrd J.T., Jones K.S. Prospective analysis of hip arthroscopy with 10-year followup. Clin Orthop Rel Res. 2010;468:741–746. doi: 10.1007/s11999-009-0841-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Larson C.M., Giveans M.R., Taylor M. Does arthroscopic FAI correction improve function with radiographic arthritis? Clin Orthop Rel Res. 2011;469:1667–1676. doi: 10.1007/s11999-010-1741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nepple J.J., Byrd T.J., Siebenrock K.A., Prather H., Clohisy J.C. Overview of treatment options, clinical results, and controversies in the management of femoroacetabular impingement. J Am Acad Orthop Surg. 2013;21:S53–S58. doi: 10.5435/JAAOS-21-07-S53. [DOI] [PubMed] [Google Scholar]
- 9.Boykin R.E., Anz A.W., Bushnell B.D., Kocher M.S., Stubbs A.J., Philippon M.J. Hip instability. J Am Acad Orthop Surg. 2011;19:340–349. doi: 10.5435/00124635-201106000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Fuss F.K., Bacher A. New aspects of the morphology and function of the human hip joint ligaments. Am J Anat. 1991;192:1–13. doi: 10.1002/aja.1001920102. [DOI] [PubMed] [Google Scholar]
- 11.Philippon M.J. The role of arthroscopic thermal capsulorrhaphy in the hip. Clin Sports Med. 2001;20:817–830. doi: 10.1016/s0278-5919(05)70287-8. [DOI] [PubMed] [Google Scholar]
- 12.Köhnlein W., Ganz R., Impellizzeri F.M., Leunig M. Acetabular morphology: Implications for joint-preserving surgery. Clin Orthop Rel Res. 2009;467:682–691. doi: 10.1007/s11999-008-0682-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 14.Bogunovic L., Gottlieb M., Pashos G., Baca G., Clohisy J.C. Why do hip arthroscopy procedures fail? Clin Orthop Rel Res. 2013;471:2523–2529. doi: 10.1007/s11999-013-3015-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clohisy J.C., Nepple J.J., Larson C.M., Zaltz I., Millis M., Members AN of CHOR (ANCHOR) Persistent structural disease is the most common cause of repeat hip preservation surgery. Clin Orthop Rel Res. 2013;471:3788–3794. doi: 10.1007/s11999-013-3218-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frank R.M., Lee S., Bush-Joseph C.A., Kelly B.T., Salata M.J., Nho S.J. Improved outcomes after hip arthroscopic surgery in patients undergoing t-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: A comparative matched-pair analysis. Am J Sports Med. 2014;42:2634–2642. doi: 10.1177/0363546514548017. [DOI] [PubMed] [Google Scholar]
- 17.Kalisvaart M.M., Safran M.R. Microinstability of the hip—it does exist: Etiology, diagnosis and treatment. J Hip Preserv Surg. 2015;2:123–135. doi: 10.1093/jhps/hnv017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shindle M.K., Ranawat A.S., Kelly B.T. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med. 2006;25:309–326. doi: 10.1016/j.csm.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Smith M.V., Sekiya J.K. Hip instability. Sports Med Arthrosc Rev. 2010;18:108–112. doi: 10.1097/JSA.0b013e3181de0fff. [DOI] [PubMed] [Google Scholar]
- 20.Shu B., Safran M.R. Hip instability: Anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30:349–367. doi: 10.1016/j.csm.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 21.Bolia I., Chahla J., Locks R., Briggs K., Philippon M.J. Microinstability of the hip: A previously unrecognized pathology. Muscles Ligaments Tendons J. 2016;6:354. doi: 10.11138/mltj/2016.6.3.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalisvaart M.M., Safran M.R. Hip instability treated with arthroscopic capsular plication. Knee Surg Sports Traumatol Arthrosc. 2017;25:24–30. doi: 10.1007/s00167-016-4377-6. [DOI] [PubMed] [Google Scholar]
- 23.Dangin A., Tardy N., Wettstein M., May O., Bonin N. Microinstability of the hip: A review. Orthop Traumatol Surg Res. 2016;102:S301–S309. doi: 10.1016/j.otsr.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 24.Domb B.G., Stake C.E., Lindner D., El-Bitar Y., Jackson T.J. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: Two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41:2591–2598. doi: 10.1177/0363546513499154. [DOI] [PubMed] [Google Scholar]
- 25.Domb B.G., Brooks A.G., Guanche C. Wolters Kluwer/Lippincott Williams and Wilkins; Philadelphia: 2010. Physical examination of the hip. Hip and pelvis injuries in sports medicine; pp. 62–70. [Google Scholar]
- 26.Hoppe D.J., Truntzer J.N., Shapiro L.M., Abrams G.D., Safran M.R. Diagnostic accuracy of 3 physical examination tests in the assessment of hip microinstability. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117740121. 2325967117740121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shibata K.R., Matsuda S., Safran M.R. Is there a distinct pattern to the acetabular labrum and articular cartilage damage in the non-dysplastic hip with instability? Knee Surg Sports Traumatol Arthrosc. 2017;25:84–93. doi: 10.1007/s00167-016-4342-4. [DOI] [PubMed] [Google Scholar]
- 28.Friel N., Ukwuani G., Nho S.J. Current techniques in treating femoroacetabular impingement: Capsular repair and plication. Am J Orthop. 2017;46:49–54. [PubMed] [Google Scholar]
- 29.Crawford M.J., Dy C.J., Alexander J.W., et al. The 2007 Frank Stinchfield Award: The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Rel Res. 2007;465:16–22. doi: 10.1097/BLO.0b013e31815b181f. [DOI] [PubMed] [Google Scholar]
- 30.Dy C.J., Thompson M.T., Crawford M.J., Alexander J.W., McCarthy J.C., Noble P.C. Tensile strain in the anterior part of the acetabular labrum during provocative maneuvering of the normal hip. J Bone Joint Surg Am. 2008;90:1464–1472. doi: 10.2106/JBJS.G.00467. [DOI] [PubMed] [Google Scholar]
- 31.Safran M.R., Giordano G., Lindsey D.P., et al. Strains across the acetabular labrum during hip motion: A cadaveric model. Am J Sports Med. 2011;39(1 suppl):92–102. doi: 10.1177/0363546511414017. [DOI] [PubMed] [Google Scholar]
- 32.Hewitt J., Guilak F., Glisson R., Vail T.P. Regional material properties of the human hip joint capsule ligaments. J Orthop Res. 2001;19:359–364. doi: 10.1016/S0736-0266(00)00035-8. [DOI] [PubMed] [Google Scholar]
- 33.Hewitt J.D., Glisson R.R., Guilak F., Vail T.P. The mechanical properties of the human hip capsule ligaments. J Arthroplasty. 2002;17:82–89. doi: 10.1054/arth.2002.27674. [DOI] [PubMed] [Google Scholar]
- 34.Bedi A., Galano G., Walsh C., Kelly B.T. Capsular management during hip arthroscopy: From femoroacetabular impingement to instability. Arthroscopy. 2011;27:1720–1731. doi: 10.1016/j.arthro.2011.08.288. [DOI] [PubMed] [Google Scholar]
- 35.Martin H.D., Savage A., Braly B.A., Palmer I.J., Beall D.P., Kelly B. The function of the hip capsular ligaments: A quantitative report. Arthroscopy. 2008;24:188–195. doi: 10.1016/j.arthro.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 36.Beighton P., De Paepe A., Danks D., et al. International nosology of heritable disorders of connective tissue, Berlin, 1986. Am J Med Genet. 1988;29:581–594. doi: 10.1002/ajmg.1320290316. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.