Abstract
Pancreatitis is an inflammatory disease of the pancreas characterized by acute and chronic condition as well as varying duration and severity. Acute pancreatitis (AP) is a severe abdominal inflammation, characterized by parenchymal edema, necrosis with occasional presence of pseudocysts, abscess, hemorrhage, and inflammatory cell infiltration. Its disease spectrum varies from mild edematous to severe disease with fatal complications. Pancreatic acinar cells are very susceptible to inflammation during an episode of AP attack. It is believed that some initiating factors can lead to the premature transformation of inactive pro-proteases into active proteases within the pancreas. The active proteases degrade a number of cellular proteins such as the structural protein F-actin, thus leading to the collapse and malfunction of acinar and pancreatic damage, a process known as autodigestion of the pancreas.
Keywords: Acute pancreatitis, Chronic pancreatitis, Cystic fibrosis, Cystic fibrosis transmembrane conductance regulator, Pancreatic cancer, Brucein D, Type 1 diabetes mellitus, Type 2 diabetes mellitus, Gestational diabetes, Maturity onset diabetes of the young
Pancreatitis
Pancreatitis is an inflammatory disease of the pancreas characterized by acute and chronic condition as well as varying duration and severity. Acute pancreatitis (AP) is a severe abdominal inflammation, characterized by parenchymal edema, necrosis with occasional presence of pseudocysts, abscess, hemorrhage, and inflammatory cell infiltration (Chan & Leung, 2007a). Its disease spectrum varies from mild edematous to severe disease with fatal complications. Pancreatic acinar cells are very susceptible to inflammation during an episode of AP attack. It is believed that some initiating factors can lead to the premature transformation of inactive pro-proteases into active proteases within the pancreas. The active proteases degrade a number of cellular proteins such as the structural protein F-actin, thus leading to the collapse and malfunction of acinar and pancreatic damage, a process known as autodigestion of the pancreas (Singh et al., 2001).
Etiology and Prognosis
Some AP-triggering environmental toxins are known to directly affect pancreatic acinar cells, leading to rupture and necrosis, and eventually an extensive inflammatory response. Epidemiological studies have revealed that the morbidity rate of the disease depends on which regions are examined, ranging from 50 to 800 cases per 1,000,000 people annually. Actually, AP is more prevalent in Caucasian than in Asian populations. The incidence rate is 700–800 and 150–420 per million annually in the USA and UK, respectively (Banks, 2002); however, it is just 106–205 per million annually in Japan (Sekimoto et al., 2006). Similar studies in China and Hong Kong have been inconsistent. In 2007, there were only 1976 patients with AP admitted to hospital from 15 Chinese tertiary care centres during the period from 1990 to 2005 (Bai et al., 2007). Despite this discrepancy, there are an increasing number of individuals with AP, probably due to life-style changes and increased exposure to risk factors in recent decades.
The diagnosis of AP entails several characteristic clinical features, such as abdominal pain at the upper epigastric region, vomiting, and elevation of plasma pancreatic enzyme levels, such as α-amylase and lipase. Hyperstimulation or pancreatic lesions might account for leakage of pancreatic enzymes into circulation. It should be emphasized that elevated levels of plasma pancreatic enzymes are a commonly used indicator for AP, though they do not generally reflect the degree of disease severity. It is noted that the elevation of plasma α-amylase tends to be cleared most rapidly from the circulation and it is the first enzyme to fall during resolution of AP. In view of this fact, if a patient with AP presents more than a few days after onset of abdominal pain, serum amylase can be normal or only slightly elevated. In this case, serum lipase is however cleared less rapidly and thus this enzyme is more likely to remain elevated in patients whose onset of symptoms is several days earlier. In addition, serum amylase levels can also be elevated in non-AP conditions such as pancreatic duct obstruction, pancreatic cancer, appendicitis, bowel obstruction and renal failure. On the other hand, measurement of serum C-reactive peptide and interleukin-6 (IL-6) provides additional information, particularly within 48 h of the onset of AP symptoms (Davies & Hagen 1997). For further evaluations, approaches such as ultrasonography and computed tomography imaging are more effective and reliable; these diagnostic procedures offer a better understanding of the cause of the disease, including the presence of gallstones or dilatation of the common bile duct.
In the clinical setting, about 80% of AP can be etiologically determined while the remaining cases are classified as idiopathic or without a known cause. Alcoholism and gallstone obstruction (choledocholithiasis) are the two major causes of the disease, accounting for about 35 and 45% of AP cases, respectively. Other causes of AP, to name but a few, include drug uses, trauma, genetic and infection. The cardinal feature of alcoholism-induced AP is characterized by the formation of proteinaceous plugs in bile ducts thus activating proteolytic enzymes and leading to pancreatic autodigestion. Gallstone obstruction-induced AP is, however, due mainly to gallstone formation which results in blockage of ampulla of Vater and thus reflux of biliary and pancreatic juices into pancreatic ducts, eventually leading to pancreatic inflammation. Different countries and regions have various proportions of pancreatitis caused by alcoholism and gallstones. Alcoholism is a major cause in some regions while gallstones may be a major cause in others. A similar incidence rate between these two etiological factors has also been reported (Gullo et al., 2002). However, it should be noted that the risk of acute alcoholic pancreatitis and acute gallstone-induced pancreatitis is around 2–3% and 0.63–1.48%, respectively, suggesting that these two risk factors can not fully account for the incidence of AP. In fact, idiopathic pancreatitis accounts for the third most common cause of AP clinically. Other risk factors including hyperlipidemia, viral infection (HIV, mumps and hepatitis B), and endoscopic retrograde cholangiopancreatiography (ERCP), as well as surgical procedures and medications may be implicated in the development of AP (Chan & Leung, 2007a).
The AP recurrence rate is relatively high. A cohort study in Sweden reported that about 21% of AP patients suffer a recurrence, with nearly 70% of them exhibiting a second episode within three months of the first episode (Andersson et al., 2004). A similar follow-up study conducted in Japan indicated an overall recurrence rate of 37% (Sekimoto et al., 2006). If choledocholithiasis is not treated properly, the recurrence rate of gallstone-induced pancreatitis could reach 32–61% (Delorio et al., 1995). Patients with alcoholism-induced pancreatitis and idiopathic pancreatitis have been reported to have relapse rates of around 46 and 3.2%, respectively, indicating that recurrence varies in an etiology-dependent manner (Pelli et al., 2000).
Some patients may gradually develop chronic pancreatitis (CP) if recurrent AP is not well controlled. Basic research studies have revealed that repeated episodes of AP result in a progressive development to CP. The so-called “necrosis-fibrosis theory” hypothesizes that residual pancreatic damage, especially necrosis, can gradually lead to parenchymal destruction and fibrosis replacement (Ammann & Muellhaupt, 1994). It is believed that repeated acinar injury leads to activation of pancreatic stellate cells (PSCs). The activated PSCs secrete fibrogenic factors, thus triggering progressive substitution of functional exocrine pancreas and subsequent development of CP (Leung & Chan, 2009). It should be emphasized that AP and CP are two distinct diseases with discrete features in terms of pancreatic morphology and clinical outcome. Patients with AP usually exhibit pancreatic swelling (edematous or necrotic cell death), while the pancreata of CP patients usually undergoes atrophy and apoptosis. In AP, the damage is confined to the exocrine pancreas and exocrine dysfunction leads to pancreatic exocrine insufficiency; meanwhile, CP or repeated episode of AP attack causes endocrine dysfunction that emerges from advanced stage of CP, notably in the form of pancreatic fibrosis which accounts for not only pancreatic exocrine but also endocrine insufficiency, the latter being attributable to impaired glucose tolerance or diabetes.
Mortality is the major complication of severe AP. The overall mortality rate of AP lies between 7.5 and 20%, depending on the diagnostic criteria chosen and the age of the patients. Most patients are susceptible to death within the first few weeks after the onset of symptoms. Early mortality is associated with the development of systemic inflammatory response syndrome (SIRS), aggravated by multiple organ dysfunction syndrome (MODS). In this context, death is generally due to local complications, notably occurrence of infection resulting from pancreatic necrosis. The clinical parameters of MODS include dyspnea, shock, bleeding tendency, and elevated blood urea (Sekimoto et al., 2006). In terms of organ failure, pulmonary dysfunction is commonly observed. Acute respiratory distress syndrome (ARDS) is usually the primary manifestation of AP-associated complications and is believed to trigger MODS (Bosma & Lewis, 2007). On the other hand, the development of ARDS may further exacerbate the severity of pancreatitis since hypoxia is a well-known enhancer of inflammatory responses. Undoubtedly, the more organs that fail, particularly if the liver and kidney are involved, the higher the mortality rate is (McFadden, 1991). The mortality rate in AP-induced ARDS surges when renal failure has ensued. Actually, there is a close association between pancreatic necrosis and development of SIRS as well as MODS. It is believed that necrotizing pancreatitis causes the release of overwhelming pro-inflammatory mediators and, subsequently, over-activates inflammatory responses, leading to SIRS and distant organ lesions and thus death ensues.
Treatments
Although AP has been studied for decades, promising and effective therapy is still not available. In most cases, patients develop mild, self-limiting AP, requiring no special treatment or surgery. Traditional approaches are generally palliative and nonspecific including analgesic (opiate) administration for pain relief, intravenous fluids for volume depletion and nothing by mouth for pancreatic rest. By doing so, the patients may be discharged from the hospital within weeks. However, around 20% of patients develop severe AP, concomitant with lethal complications that bring the mortality rate up to 20–25% in these patients, compared with 1–3% in a mild attack. In such cases, patients should be monitored under intensive care unit and surgery should be justified in such case as gallstone-induced AP.
Enteral/parentenal nutrition, antibiotic treatment, surgical removal of necrotic tissue, and some surgical manipulations such as cholecystectomy are the first-line treatment modalities for clinical AP (Makola et al., 2007). However, many such treatments are rather passive in nature (e.g. enteral/parentenal nutrition) while others are invasive (e.g. surgical management). Most of these treatments are targeted for the complications of the disease (e.g. sepsis or pain management) rather than the primary insults. In view of this fact, clinicians are in search of new effective alternatives for curing AP. Potential therapeutic approaches derived from basic research include, but are not limited to, the protease inhibitor gabexate, the anti-secretagogue agent octreotide, the anti-inflammatory drug lexipafant, and an antioxidant regimen. Unfortunately, thus far, these potential therapeutic methods have yielded unsatisfactory or marginal results and warrant further extensive investigation (Chan & Leung, 2007a; Leung & Chan, 2009).
Emerging data from basic research have shed some lights on potential therapeutic strategies against AP, such as cyclooxygenase (COX)-2 inhibition, substance P antagonism, and heat shock protein (HSP) activation. COX-2 expression has been found to be up-regulated in caerulein-induced pancreatitis in both mice (Song et al., 2002) and rats (Zhou et al., 2004). Treatment with specific COX-2 inhibitors, such as celecoxib and NS-398, could alleviate pancreatic injury (Song et al., 2002). Genetic knock-out of COX-2 leads to resistance against experimental pancreatic injury and its associated lung injury (Song et al., 2002). In addition, the expression of substance P, the physiological agonist of neurokinin 1 receptor (NK1R), has been shown to be upregulated during experimental pancreatitis, thus implicating its role in AP-induced lung injury (Bhatia et al., 1998; Lau et al., 2005a); a pharmacological antagonist for its receptor was also protective against caerulein-induced pancreatitis and associated lung damage (Lau et al., 2005a). On the other hand, the chaperon protein and HSP have also been closely linked with AP pathogenesis; secreatagogue and arginine-induced pancreatitis was shown to provoke pancreatic HSP protein expression and HSP induction was shown to be protective against experimental pancreatitis (Tashiro et al., 2001). Last but not least, we have shown that angiotensin II, the vasoactive peptide, is crucial in mediating pro-inflammatory responses during AP (Chan & Leung, 2007b). The novel roles of angiotensin II and its type 1 receptor (AT1R) blockade and thus its clinical relevance to pancreatic inflammation will be further discussed in 10.1007/978-90-481-9060-7_10. Potential pathogenetic factors of acute pancreatitis implicated and discussed above in the pathogenesis of AP are summarized in Fig. 3.1.
Fig. 3.1.
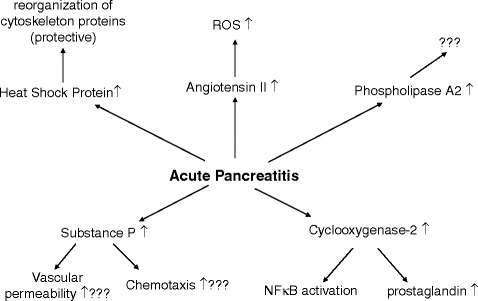
Schematic diagram illustrating the simplified relationship between AP pathophysiology and some novel biological factors (modified from Chan & Leung, 2007a)
Cystic Fibrosis
Cystic fibrosis (CF) is an autosomal recessive disease commonly found about once in every 25,000 births in the Caucasian population while it occurs rare in native Africans and Asians. The disease is a result of a genetic defect leading to abnormal sodium chloride and water movement across the epithelial membranes. Where such membranes line the pancreatic duct and small respiratory airways, they produce dense and viscous mucus that cannot be properly cleared, thus causing pancreatic insufficiency and pulmonary disorder. The genetic defect involves a particular membrane protein expressed in the epithelial cells, called cystic fibrosis transmembrane conductance regulator (CFTR). Mutations in the CFTR are categorized into five groups according to their repercussion on CFTR protein synthesis and its chloride channel function. Class I or stop codon mutations result in truncated non-functional CFTR; Class II mutations consist of aberrantly folded CFTR protein that is degraded by the cell quality control system; Class III mutations lead to defective regulation of the CFTR protein; Class IV mutations cause defective chloride conductance; and Class V mutations interfere with normal transcription, thereby reducing the amount of normal CFTR (Proesmans et al., 2008).
Etiology and Prognosis
One of the genetic mutations of CF gene is due to a single mutation (amino acid 508) located on the long arm of chromosome 7 that codes for the CFTR protein. This genetic defect is characterized by abnormalities in exocrine gland function that result in altered ion composition and increased viscosity of epithelial cell secretions. The affected tissues include the secretory cells of the sweat glands, salivary glands, small intestine, lungs, vas deferens, and the exocrine pancreas (Voynow & Scanlin, 2005). CF is manifested by elevated electrolyte concentrations, reduced ion permeability, and impaired luminal ion secretion upon stimulation by secretagogues (Tucker et al., 2003). Thus, the defect in perturbed salt and water transport leads to secondary alterations of pancreatic, intestinal and pulmonary functions. Pancreatic exocrine insufficiency is clinically obvious in 85–90% of CF patients (Baker et al., 2005).
As mentioned, CFTR is expressed in various cell types, including the pancreas. It is comprised of two membrane-spanning domains and two nucleotide-binding domains separated by a regulatory R domain. The two membrane-spanning domains form a low-conductance chloride channel pore. It is regulated by ATP binding and hydrolysis at the nucleotide-binding domains following initial phosphorylation of the R domain. CFTR functions as a chloride channel in the apical membrane of epithelial cells that regulate ion transport (Schwiebert et al., 1999). It has inhibitory effects on apical Na+ permeability across epithelia while activating non-CFTR chloride channels. Owing to the widespread presence of CFTR throughout the body, CF is a multisystem disorder affecting many organs, especially the gastrointestinal tract, pancreas and lungs.
Failure of the function of CFTR results in impaired chloride transport at the apical surface of epithelial cells and dysregulation of other transporters, such as the chloride-coupled bicarbonate transport and sodium channel activity (Reddy et al., 1999; Choi et al., 2001). The aqueous medium of the intestinal lumen becomes hyper-viscous in CP patients due to excessive and abnormal intestinal mucoprotein (Forstner et al., 1984). In the pancreas, these viscous secretions cause luminal obstruction of pancreatic ducts, leading to acinar cell destruction, fibrosis, and ultimately pancreatic exocrine insufficiency which is characterized by a decrease or absence of digestive enzymes and concomitant with maldigestion and malabsorption of nutrients. In view of the close interaction between exocrine and endocrine pancreas, patients with CF usually develop with pancreatic exocrine along with endocrine insufficiency as manifested by other pancreatic conditions such as acute and chronic AP, pancreatic surgery and pancreatic cancer (Czako et al., 2009). The pathophysiology of lung disease in CF is more complex than that of pancreatic disease. A major finding is that the airway mucus is thick and viscous as a result of insufficient fluid secretion into the airway. The lung epithelium secretes fluid in a mechanism that requires CFTR while absorbing fluid that requires apical ENaC sodium channels. In patients with CF, the reduced activity of CFTR shifts the balance more toward absorption, and a thick mucous layer is generated that inhibits the ciliary clearance of foreign bodies. The result is an increased rate and severity of infections and thus inflammatory processes that contributes to the destructive process in the lung (Ingbar et al., 2009). In contrast, the levels of salivary secretion are normal or raised while lingual lipase levels are elevated (Guy-Crotte et al., 1996). Although CF is the most common lethal genetic disease in Caucasians, there is often a delay between the onset of symptoms and definitive diagnosis. Blood spot CF screening tests can be performed in newborn babies. A definitive diagnostic sweat test will then be given if the screening suggests CF. About one in five people with CF are diagnosed at birth when their gut is blocked by extra thick meconium.
Treatments
The conventional treatment of CF is usually palliative, alleviating signs and symptoms and treating organ dysfunction, including replacement of pancreatic enzymes, vitamin and nutritional supplements, airway clearance techniques, daily physiotherapy and antibiotics for pulmonary infections (Davis et al., 1996; Ramsey, 1996).
Despite advances in treatment, there remains no cure for CF. It has become apparent that there is a need for a more effective and convenient therapy. New therapies directed at the basic defect represent the only potential approach to truly treating CF. The identification of the gene responsible for CF (CFTR protein), in 1989, provided insight into a potential treatment for CF. Gene therapy, the transfer of a normal copy of the CFTR gene into the lungs of CF patients, has been proposed as an attractive alternative to the conventional approach (Riordan, 2008; Ratjen, 2007). Genes are most commonly transferred into cells through viruses and liposomes. Viruses have evolved to enter the cells of the body efficiently. Scientists have harnessed this property for gene therapy by inserting a copy of the therapeutic gene of interest into the virus, which then directs it into the cell. The adenovirus is an example of a virus that has been used extensively for gene therapy. On the other hand, liposomes are fatty substances that naturally adhere to the surface of cells, thus facilitating entry into cells. The CF gene could potentially be transferred into the airway cells; however, considerable challenges lie ahead, particularly with regard to efficiency of gene transfer and persistence of transferred gene expression (Atkinson, 2008). The field is moving forward rapidly, particularly pertaining to the development of better virus and liposome vectors. Apart from the aforementioned state-of-the-art methodology, there are a number of potential drugs which are emerging for the treatment of CF and are in clinical trials. They include some anti-bacterial formulations, anti-inflammatory agents, ion channel modulating agents, and agents that correct the underlying gene defect (Jones & Helm, 2009). The pathogenetic pathways and common symptoms of CF are briefly summarized in Fig. 3.2.
Fig. 3.2.
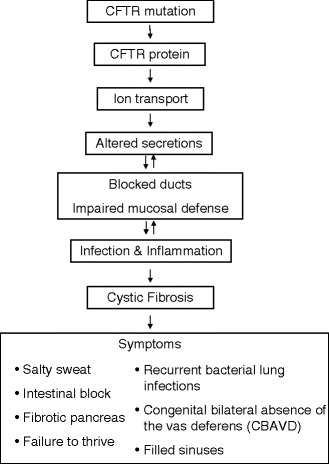
The pathogenesis of cystic fibrosis disease and its common signs and symptoms
Pancreatic Cancer
Etiology and Prognosis
Pancreatic cancer is a deadly malignant disease with an extremely high mortality rate in humans. It is classified into tumours arising from the pancreatic exocrine tissue (ductal adenocarcinoma) and pancreatic endocrine tissue (insulinoma, glucagonoma, gastrinoma and VIPoma), as well as atypical neoplasms (lymphomas, mesotheliomas and sarcomas) (Hruban & Adsay, 2009). It is the fourth leading cause of cancer in the United States, with an estimated 37,680 new cases and 34,290 deaths in 2008 (Jemal et al., 2008). Ductal adenocarcinoma accounts for approximately 80% of all pancreatic cancers (Lewis, 2006). Only 23% of patients with pancreatic cancer of exocrine origin will survive for 1 year, while about 4% will survive for 5 years. In contrast, pancreatic endocrine tumours are relatively rare accounting for less than 2% of pancreatic neoplasms. In this section, we thus focus on the ductal adenocarcinoma as an example of pancreatic cancer for further discussion below.
The risk of developing pancreatic cancer is much higher beyond the age over 50 and is more prevalent in males. Risk factors include family history, cigarette smoking, a diet rich in fat and meat, and exposure to chemicals. In addition, patients with diabetes mellitus, chronic pancreatitis and gastric surgery are more susceptible to the disease (Dunphy, 2008). Diagnosis of pancreatic cancer in an early stage is extremely difficult, mainly due to the nonspecific symptoms and the lack of accurate diagnostic tests. Hence, more than 80% of patients with pancreatic cancer are diagnosed only in advanced or late tumour stages (stage II–IV), often when the tumours metastasize without a recourse of tumour resection (Canto, 2008). Furthermore, the propensity for tumour metastasis and intrinsic resistance to conventional chemo-radiation treatments renders pancreatic cancer very difficult to handle clinically. Surgical resection of localized tumours is the only potentially curative option available for pancreatic cancer patients (Ozawa et al., 2001). Unfortunately, pancreatic cancer is a highly aggressive cancer and, with the late diagnosis that characterizes many cases, only about 10–15% of patients are considered suitable for the surgical option. There are two standard resection procedures, including resection of the pancreatic head and of the left-side pancreatic tissues. In the case of a local advanced tumour, a total pancreatectomy may be chosen for particular patients (Loos et al., 2008a). Pancreatic surgery has significantly improved and the associated postoperative morbidity and mortality have decreased markedly over the last three decades. Despite these advances, the prognosis for patients with pancreatic cancer remains poor and this poor prognosis is the reason for pancreatic cancer’s high mortality rate.
Treatments
Complete surgical resection of the tumour is only possible in 10–25% of patients with pancreatic cancer, while about half of them are subjected to adjuvant therapies. Chemotherapy with 5-fluorouracil (5-FU), cisplatin, oxaliplatin, mitomycin C, and doxorubicin in mono- or combination treatments are the major options for pancreatic cancer. In the case of locally unresectable or metastatic adenocarcinoma, chemotherapy was found to enhance overall 1-year survival, but not to appreciable improve long-term (5-year) survival (Loos et al., 2008b). In 1996, gemcitabine was approved as the standard chemotherapeutic agent in monotherapy or combination therapy for locally advanced and metastatic pancreatic cancer (Barton-Burke, 1999; Hui & Reitz, 1997). Gemcitabine has been reported to improve survival and alleviate disease-related symptoms (Almhanna & Kim, 2008). Single chemotherapy with gemcitabine is considered the standard for patients with advanced pancreatic cancer along with other drugs including 5-FU. Meanwhile, targeted therapies inhibiting specific pathways for the growth and progression of malignant tumors are under intensive investigations. The epidermal growth factor receptor (EGFR) mediated pathway is one of the most promising targets for the treatment. In over 90% of cases, EGFR is over-expressed to stimulate pancreatic tumour growth (Lemoine et al., 1992). Indeed, the EGFR tyrosine inhibitor erlotinib has been shown to increase median survival and, in 2005, the U.S. FDA approved the use of erlotinib in combination with gemcitabine for treating locally advanced, unresectable, or metastatic pancreatic cancer (Danovi et al., 2008). Gene therapy using antisense oligonucleotides or ribozymes could also correct a genetic defect or mutation. For example, K-ras and p53 tumour suppressor gene mutations are found in about 70% of pancreatic cancer and have been predominant targets in preclinical gene therapy studies (Danovi et al., 2008).
Despite these recent advances, treatment of pancreatic cancer remains difficult and relatively ineffective due to its intrinsic broad resistance to cytotoxic drugs. Some recent studies have focused on the transcription factor nuclear factor kappa B (NF-κB), which is proposed to be a central determinant in the induction and manifestation of chemo-resistance in pancreatic cancer cells. Since constitutive activation of NF-κB is a hallmark of pancreatic cancer accounting for profound chemo-resistance, suppression of NF-κB activity might be a useful strategy for increasing sensitivity towards cytostatic drug treatment (Sebens et al., 2008). However, solid tumors apparently exhibit comprehensive protection from induction of apoptosis, so pharmacological inhibition of NF-κB only appears to be insufficient. Thus, NF-κB inhibition should be used as a chemo-sensitizing adjuvant in combination with other cytostatic drugs.
Several new immunotherapies have been developed for potential treatment of pancreatic cancer. Chemotherapy, which reduces tumour cells by preferentially poisoning proliferating cells, is not a cancer cure per se. Immunotherapy, however, could potentially eliminate quiescent tumour (stem) cells. Although immunotherapy is in the early stage of development and has not yet replaced conventional chemotherapy, it may in the future be an additional approach in fighting cancer and eradicating tumour stem cells (Schulenburg et al., 2006). Table 3.1 summarizes the different forms of pancreatic tumours that arise from exocrine and endocrine origins, together with their characteristics and the current treatments.
Table 3.1.
A brief summary of classification, characteristics and current treatments of exocrine and endocrine tumors of the pancreas
| Origin | Types | Characteristics | Treatments |
|---|---|---|---|
| Pancreatic exocrine tumors | Adenocarcinoma | The most common type of pancreatic cancer, accounting for 75% of all pancreas cancer; nearly all of these are ductal adenocarcinoma; cause back pain when tumor grow large and invade nerves | Surgical resection: pancreaticoduodenectom, total pancreatectomy and distal pancreatectomy |
| Acinar cell carcinoma | Rare cancerous tumor produces excessive amounts of digestive enzymes. Unusual skin rashes, joint pain and increased increased eosinophils level | First-line chemotherapy: Gemcitabine | |
| Adenosquamous carcinoma | Similar to adenocarcinoma that it forms glands, but it flattens as it grows. It can mimic other types of cancer that show squamous differentiation | Second line chemotherapy: 5-flourouracil (5-Fu), irinotecan, celecoxib, cisplatin and oxaliplatin | |
| Giant cell tumor | Extremely rare and is not aggressive as adenocarcinomas. It has unusually large cells | Combined therapy: ICM-C225 + Gem, erlotinib + Gem | |
| Intraductal papillary-mucinous neoplasm (IPMN) | Rare but very distinctive tumor. It grows along the pancreatic duct and appears to be a fingerlike projection into the duct | ||
| Mucinous cystadenocarcinoma | Rare, cystic, fluid-containing pancreas tumor and can develop into cancer over time. The space within the spongy tumor is filled with a think fluid called mucin | Radiation therapy and chemoradiotherapy | |
| Pancreatoblastoma | Rare malignant tumor occurs primarily in children, and called pancreatic cancer of infancy | ||
| Pancreatic endocrine tumor | Insulinoma | Produce large amounts of insulin which result in hypoglycemia |
Surgical resection Chemotherapy: Streptozocin, dacarbazine, doxorubicin and 5-Fu Combination therapy |
| Glucagonoma | Produce excessive amounts of glucagon which result in severe dermatitis, mild diabetes, stomatitis, anemia, and weight loss |
Distal pancreatectomy Standard chemotherapy: streptozocin and dacarbazine Octreotide: Reduce elevated glucagon levels, and control the hyperglycemia and dermatitis |
|
| Gastrinoma | Release large quantities of the hormone gastrin into the blood stream leading to severe duodenal ulcers and persistent diarrhea |
Surgical resection Chemotherapy: Proton pump inhibitors, like lansoprazole, pantoprazole esomeprasole, in high doses to control hypersecretion of gastric acid |
|
| VIPoma | Releasing large amounts of the hormone VIP into the blood stream. Symptoms include watery diarrhea, hypokalemia, and either achlorhydria or hypochlorhydria. |
Surgical excision Chemotherapy: Octreotide to reduce circulating VIP levels and control diarrhea No specific chemotherapy for VIPoma patients |
|
| Somatostatinoma | Less common, releasing large quantities of the hormone somatostatin into the blood stream | Combination treatment with intravenous 5-FU and streptozotocin or doxorubicin and 5-FU |
Alternative Approach Using Traditional Chinese Medicine
Based on herbal medicine knowledge that has accrued over centuries, traditional Chinese medicine provides a potential approach for alternative treatments to pancreatic cancer. Chinese herbal extracts have been extensively investigated in various clinical trials of anti-tumour studies, including studies of leukemia, lung, ovarian, breast and pancreatic cancers. Indeed, a number of Chinese herbs have been identified as having anti-cancer properties (Wang et al., 2005). For example, Curcumin has been reported to possess a wide range of beneficial properties, including anti-inflammatory, antioxidant, chemopreventive and chemo-therapeutic activities. Curcumin influences multiple signalling pathways, including the following: cell survival pathways regulated by NF-κB, Akt, and growth factors; Nrf2-dependent cytoprotective pathways; and matrix metallo-proteinase-dependent metastatic and angiogenic pathways (Park et al., 2005; Zheng & Chen, 2004). Additionally, the traditional Chinese medicinal Brucea javanica was recently shown to exhibit various biological activities such as anti-malarial (O’Neill et al., 1987), anti-inflammatory (Hall et al., 1983), and hypoglycaemic effects (NoorShahida et al., 2009), thus implicating its clinical use for the treatment of various diseases.
Brucea javanica is a shrub of about 3-meter height. The fruit of Brucea javanica, or Ya Dan Zi in Chinese (meaning crow bile fruit), contains oils (glyceroltrileate, oleic acid, linoleic acid), alkaloids, quassinoids, bursatol, brucein A, B, C, D, E, F and H etc (Fig. 3.3). In term of cancer, extracts or compounds from Brucea javanica, particularly brucein D, have anti-proliferative and cytotoxic effects on a number of cancer cell types; they include, but are not limited to, the lung, liver, breast and oesophageal cancers (Lau et al., 2005b). In our laboratory, we have recently performed preliminary screening tests on nine commonly used Chinese herbal medicines for anti-pancreatic cancer activities. Among these, an ethanolic extract of Brucea javanica fruit has also been identified to possess potent cytotoxicity that induced marked apoptosis in several human pancreatic cancer cell lines, including PANC-1, SW1990 and CAPAN-1 while exhibiting less cytotoxic action on Hs68 cells (a human foreskin fibroblast cell line); specifically, it produced chromatin condensation and fragmentation as well as activation of the proteolytic cleavage of caspase 3 in these human pancreatic cancer cell lines (Lau et al., 2008). Furthermore, brucein D, a quassinoid compound found abundantly in Brucea javanica fruit, displayed potent anti-proliferative activity and induced apoptosis in PANC-1 cells through activation of the p-38 mitogen-activated protein kinase (MAPK) signal transduction pathway (Lau et al., 2009). Both intrinsic and extrinsic apoptotic pathways are activated following p38-MAPK phosphorylation and, ultimately, the effector caspase 3 is activated, causing irreversible apoptotic cell death in pancreatic cancer cells. On the other hand, Brucein D treatment depletes intracellular glutathione levels in PANC-1 cells, while triggering activation of the NADPH oxidase isoforms p22phox and p67phox, and increasing superoxide generation. Although intracellular reactive oxygen species and NADPH oxidase activities can be inhibited by the presence of an antioxidant (e.g. N-acetyl cysteine), inhibition of NF-κB activity in brucein D-treated cells appears to be independent of ROS changes (Lau et al., 2010). These results suggest that brucein D elicits apoptosis in pancreatic cancer cells by activating the redox-regulated p38 MAPK signalling pathway and reducing anti-apoptotic activity through inhibition of NF-κB activation.
Fig. 3.3.
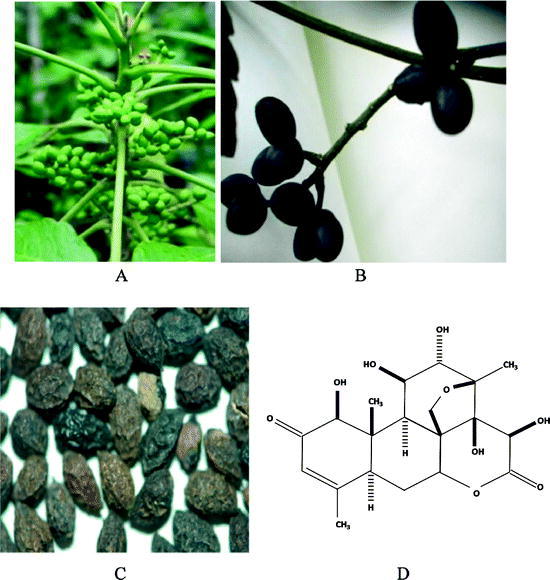
Photographs of Brucea javanica. (a) The plant. (b) The fruit. (c) The dry fruit. (d) Chemical structure of brucein D
Taken the above substantial data together, these findings provide experimental evidence that supports the potential use of traditional Chinese medicinal such as Brucea javanica fruit extract, in the treatment of pancreatic cancer and, more importantly, brucein D is a promising candidate compound for further development into a mechanism-driven anti-pancreatic cancer agent. A schematic presentation of the proposed mechanism(s) by which brucein D induces MAPK-mediated apoptosis and NF-κB-mediated survival in PANC-1 cells is presented in Fig. 3.4.
Fig. 3.4.
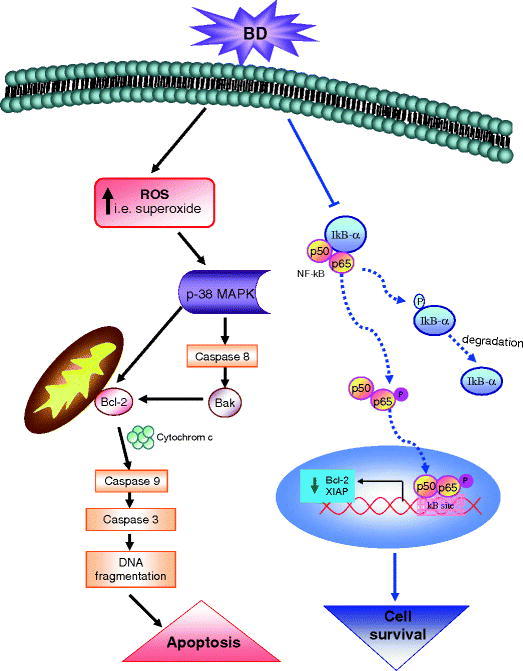
A schematic presentation of the proposed mechanism (s) by which brucein D induces apoptosis and anti-apoptosis in PANC-1 cells
Diabetes Mellitus
Etiology and Prognosis
Blood glucose concentration has a normal range of 3.8–7 mmol/l (70–125 mg/dl). When the body is not able to maintain normal glucose status, glucose cannot enter into cells to supply them with energy. Prolonged high blood glucose levels, a state known as hyperglycemia, ultimately leads to diabetes mellitus. The American Diabetes Association (ADA, 2009) distinguishes among normoglycemia, impaired glucose tolerance (IGT, also known as pre-diabetes), and overt diabetes mellitus based on fasting plasma glucose (FPG) levels and 2-h oral glucose tolerance test (OGTT) results as follows: normoglycemia is FPG <6.0 mmol/l (110 mg/dl) and 2-h OGTT <7.7 mmol/l (140 mg/dl); IGT is FPG levels ≥6.0 mmol/l (110 mg/dl) but <7.0 mmol/l (125 mg/dl), and 2-h OGTT ≥7.8 mmol/l (140 mg/dl) but <11.1 mmol/l (200 mg/dl); and overt diabetes mellitus is FPG ≥7.0 mmol/l (125 mg/dl) and 2-h OGTT >11.1 mmol/dl (200 mg/dl). Individuals with impaired FPG or IGT are generally euglycemic and have normal or near normal glycated hemoglobin levels (HbA1c, normal range 3.5–5.5%), but may progress to overt diabetes without treatment. Diabetes is often concomitant with chronic complications such as nephropathy, retinopathy and neuropathy which in turn can lead to end-stage renal failure, blindness and diabetic foot, respectively.
Diabetes mellitus is classified as type 1 (T1DM), type 2 (T2DM), gestational diabetes (GDM), and other specific types, based on its specific pathogenesis (American Diabetes Association, 2009). According to the definition of the World Health Organization (WHO), the two major types, namely T1DM and T2DM, account for approximately 10 and 90% of diabetics, respectively. T1DM (also previously known as insulin-dependent or juvenile diabetes) results from an absolute deficiency of insulin secretion from pancreatic β-cells. Most of the T1DM incidence is due to immune-mediated disease with autoimmune features, such as the presence of islet cell antibodies (e.g., islet cell antigen, islet cell surface antigen, GAD65 and GAD67). T1DM pathogenesis is thought to involve both genetic susceptibility and environmental factors. T2DM results from relative insulin deficiency and insulin resistance (also previously known as non-insulin dependent or adult-onset diabetes). While the etiology of T2DM is multifactorial, it is associated with strong genetic and environmental factors (e.g., single-diabetes gene, diet, physical inactivity and obesity). In the former case, one form of T2DM called maturity onset diabetes of the young (MODY) has been attributed to dysfunction of a single gene. MODY is an autosomal dominant genetic disease which leads to metabolic abnormality, notably defective insulin secretion. Based on the influence of specific single gene concerned, it is divided into various forms, such as MODY1, MODY2, MODY3, MODY 4 etc, depending on which particular gene is involved. For example, if the defective gene occurs in the hepatocyte nuclear factor 4α (HNF 4α) and pancreatic duodenal homeobox factor-1 (PDX-1), they are called MODY 1 and MODY 4, respectively (Table 3.2).
Table 3.2.
Some examples of single recessive dominant genes as exemplified by maturity onset diabetes of the young (MODY) which is associated with metabolic syndrome disorder as observed in T2DM
| Gene | Type of MODY | Genetic defect | Metabolic disorder | Clinical features |
|---|---|---|---|---|
| Hepatocyte nuclear factor 4α | MODY 1 | Autosomal dominant | Impaired insulin secretion | Rare and progressive form of early onset disease |
| Glucokinase | MODY 2 | Autosomal dominant | Impaired insulin secretion | Mild and relatively stable early onset disease |
| Hepatocyte nuclear factor 1α | MODY 3 | Autosomal dominant | Impaired insulin secretion | Progressive form of early onset disease |
| Pancreatic duodenal homeobox factor-1 | MODY 4 | Autosomal dominant | Impaired insulin secretion | Early onset disease |
| Mitochondrial DNA | – | Maternal DNA | Impaired insulin secretion | Diabetes associated with deafness |
| Insulin | – | Autosomal dominant | Defective insulin production | Very rare |
| Insulin receptor | – | Autosomal dominant or recessive | Impaired insulin signaling pathway | Severe insulin resistance |
Some confusion has arisen from the above classification scheme. For example, some patients with severe T2DM may also require insulin therapy in order to maintain euglycemic control. In addition, age is no longer a classification criterion. Though most commonly observed before the age of 30, T1DM can develop at any age (Eisenbarth, 2007). Meanwhile, T2DM once supposed to develop later in life, can also occur in young people (Song & Hardisty, 2008). In any case, loss of beta-cell mass over time is a common feature of both T1DM and T2DM, leading to impaired glucose tolerance, hyperglycemia and overt diabetes (Butler et al., 2003). On the other hand, GDM is defined as any degree of glucose intolerance with an onset during pregnancy (American Diabetes Association, 2009). The cause of GDM remains ambiguous, but placental hormones produced during pregnancy may reduce sensitivity to insulin. Repeated GDM over multiple pregnancies may increase the incidence of permanent diabetes. On the other hand, the remaining ∼1% of cases, termed secondary diabetes, are considered complications of other conditions or medications. Secondary diabetes is usually temporary, unless due to total pancreatectomy. Conditions associated with secondary diabetes include disorders that impair pancreatic functions, such as hemochromatosis, chronic pancreatitis, cystic fibrosis, and pancreatic trauma, as well as drugs such as beta blockers, glucocorticoids, antiretrovirals, opiates, and alcohol. Table 3.3 summarizes some cardinal features and that distinguish T1DM from T2DM.
Table 3.3.
Some key features in term of etiology, metabolic feature and clinical presentation that distinguish T1DM from T2DM
| Type | T1DM | T2DM |
|---|---|---|
| Etiology | ||
| • Autoimmune features |
Yes (e.g. islet cell antigens, GAD65 & 67) Moderate |
No Very strong (e.g. MODY) |
| • Genetic susceptibility | Viruses, diet and stress | Physical inactivity |
| • Environmental factors | ||
| Metabolic features | ||
| • Insulin deficiency | Severe | Moderate |
| • Insulin resistance | Moderate | Severe |
| • Diabetic ketoacidosis | Yes | No |
| Clinical presentation | ||
|
• Age of onset • Body weight • Body mass index |
Most occur < 40 years old Commonly decrease Mostly <25 |
Most occur > 40 years Sometimes decrease Mostly >25 |
Treatments
The incidence of diabetes is ever increasing globally in terms of mortality and morbidity (Wild et al., 2004). Unfortunately, adequate preventive and curative management for diabetes is lacking. Most treatments are intended to slow or prevent disease progression and complications (Reimann et al., 2008). Ideally, T1DM treatment should be focused on β-cell regeneration and early intervention (Meier, 2008). While T1DM may be incurable, its onset and progression may be delayed. Insulin therapy remains the mainstay treatment of T1DM since glycemic control is crucial for preventing chronic complications. Hypoglycemia remains the major disadvantage of insulin injection treatment. Physiologically, prevention of β-cell loss would be a more direct treatment. In this context, recent studies have proposed novel approaches, such as immunoregulatory techniques, to deal with autoimmune β-cell destruction (Phillips et al., 2008). In addition, pancreatic or renal-pancreatic transplantation together with long-term immunosuppressive drugs can be an affective treatment course for T1DM (Stratta & Alloway, 1998). Although islet β-cell transplantation has been performed experimentally in animals and human patients, its major obstacle and practicability for clinical use are due to the very limited availability of islets (Shapiro et al., 2006). In order to resolve this issue, a stem cell-based approach to islet cell transplantation is promising and may someday circumvent this problem as well as providing a cure but not only treatment for T1DM. In this regard, hyperglycemia has been completely reversed in some cases as reported recently (Voltarelli et al., 2007). Additional information on current research concerning pancreatic stem cells, with particular focus of the novel roles of RAS in this area, will be discussed in 10.1007/978-90-481-9060-7_9.
As far as T2DM is concerned, improvements of insulin secretion and/or insulin sensitivity along with reduction of chronic complications are the major considerations in T2DM treatment (Stumvoll et al., 2005). Key preventive strategies include primary prevention, decreasing risk factors, and enhancing β-cell function and cell mass (Reimann et al., 2008). Life-style changes, such as reducing obesity and increasing physical activity can reduce the risk of developing T2DM and related complications (Pan et al., 1997; Gillies et al., 2007). Pharmacological interventions, such as oral hypoglycemic drugs, are the most effective means of therapy, when diet, exercise and change of life style are not sufficient (Torgerson et al., 2004). There are three major categories of oral anti-diabetic drugs currently available based on the two primary causes of T2DM: insulin sensitizers that enhance insulin sensitivity of peripheral tissues at the levels of skeletal muscle, adipose tissue and liver; β-cell secretagogues that improve β-cell secretion, function and cell mass; and α-glucosidase inhibitors that delay or inhibit carbohydrate absorption from the intestine. Apart from these classes of drugs, some novel treatment modalities and novel candidate drugs such as combination drugs and RAS blockers, respectively, the later being fully discussed in 10.1007/978-90-481-9060-7_8, provide significant and effective approaches for treating T2DM. Current treatments of oral hypoglycaemic drugs and some combination therapy for T2DM, and their proposed mechanisms involved are briefly tabulated in Table 3.4.
Table 3.4.
Currently and potentially used oral hypoglycemic medications and proposed mechanisms for the management of T2DM
| Major class of drugs | Site of actions and proposed mechanisms | Some specific drugs |
|---|---|---|
| β-cell secretagogues | ||
| Sulfonylureas |
• Act on the pancreas • Enhance β-cell secretion by acting on the ATP-dependent potassium channel • Use with or without insulin but hypoglycemia |
– Tolbutamide Glipizide Meglitinides Nateglinide – Exenatide, Liraglutide; – Sitagliptin, Vidagliptin; |
| GLP-1 analogues/DPP-IV inhibitors/Amylin analogue |
• Act on the pancreas • Enhance β-cell secretion and/or cell mass • Do not cause weight gain but GI side effects |
– Synthetic amylin |
| α-glucosidase inhibitors |
• Act on the gastrointestinal tract • Lower blood glucose by delaying the digestion and absorption of carbohydrates • Do not cause weight gain and hypoglycemia but concomitant with gas, bloating and diarrhea |
– Acarbose – Miglitol |
| Insulin sensitizers | ||
| Biguanides |
• Act primarily on the liver • Decrease liver’s glucose production and slightly increase muscle glucose uptake • Do not cause weight gain and hypoglycemia while inducing nausea, diarrhea or loss of appetite |
– Metformin – Metformin (extended release) – Metformin (liquid) |
|
Thiazolidinediones (TZDs) |
• Act on the peripheral tissues • Decrease insulin resistance at the muscle & liver levels • Improve cholesterol and triglyceride status while but cause weight gain |
– Pioglitazone – Rosiglitazone – Troglitazone |
| RAS blockers |
• Act on the pancreas and the peripheral tissues • Improve β-cell function, structure and/or insulin resistance |
– ACEIs (Ramipril) – ARBs (Losartan, Valsartan) |
| Combination drugs |
• Act on different tissue-organ levels • Potential advantages and disadvantages for each drug in the combination listed separately above |
– Metformin + TZD, – Metformin + DPP-IV inhibitor, – TZD + Sulfonylurea |
RAS, Renin-angiotensin system; ACEIs, Angiotensin-converting enzyme inhibitors; ARBs, Angiotensin receptor blockers; GLP-1, Glucagon-like peptide-1; DPP-IV, Dipeptidyl peptidase IV.
References
- Almhanna K, Kim R. Second-line therapy for gemcitabine-refractory pancreatic cancer: is there a standard? Oncology. 2008;22:1176–1183. [PubMed] [Google Scholar]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2009;32(Suppl 1):S62–S67. doi: 10.2337/dc09-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammann RW, Muellhaupt B. Progression of alcoholic acute to chronic pancreatitis. Gut. 1994;35:552–556. doi: 10.1136/gut.35.4.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson R, Andersson B, Haraldsen P, Drewsen G, Eckerwall G. Incidence, management and recurrence rate of acute pancreatitis. Scand J Gastroenterol. 2004;39:891–894. doi: 10.1080/00365520410007061. [DOI] [PubMed] [Google Scholar]
- Atkinson TJ. Cystic fibrosis, vector-mediated gene therapy and relevance of toll-like receptors: a review of problems, progress, and possibilities. Curr Gene Ther. 2008;8:201–207. doi: 10.2174/156652308784746468. [DOI] [PubMed] [Google Scholar]
- Bai Y, Liu Y, Jia L, Jiang H, Ji M, Huang K, Zou X, Li Y, Tang C, Guo X, Peng X, Fang D, Wang B, Yang B, Wang L, Li Z. Severe acute pancreatitis in China: etiology and mortality in 1976 patients. Pancreas. 2007;35:232–237. doi: 10.1097/MPA.0b013e3180654d20. [DOI] [PubMed] [Google Scholar]
- Baker SS, Borowitz D, Baker RD. Pancreatic exocrine function in patients with cystic fibrosis. Curr Gastroenterol Rep. 2005;7:227–233. doi: 10.1007/s11894-005-0039-4. [DOI] [PubMed] [Google Scholar]
- Banks PA. Epidemiology, natural history, and predictors of disease outcome in acute and chronic pancreatitis. Gastrointest Endosc. 2002;56:S226–S230. doi: 10.1016/S0016-5107(02)70016-3. [DOI] [PubMed] [Google Scholar]
- Barton-Burke M. Gemcitabine: a pharmacologic and clinical overview. Cancer Nurs. 1999;22:176–183. doi: 10.1097/00002820-199904000-00011. [DOI] [PubMed] [Google Scholar]
- Bhatia M, Saluja AK, Hofbauer B, Frossard JL, Lee HS, Castagliuolo I, Wang CC, Gerard N, Pothoulakis C, Steer ML. Role of substance P and the neurokinin 1 receptor in acute pancreatitis and pancreatitis-associated lung injury. Proc Natl Acad Sci USA. 1998;95:4760–4765. doi: 10.1073/pnas.95.8.4760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosma KJ, Lewis JF. Emerging therapies for treatment of acute lung injury and acute respiratory distress syndrome. Expert Opin Emerg Drugs. 2007;12:461–477. doi: 10.1517/14728214.12.3.461. [DOI] [PubMed] [Google Scholar]
- Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes. 2003;52:102–110. doi: 10.2337/diabetes.52.1.102. [DOI] [PubMed] [Google Scholar]
- Canto MI. Screening and surveillance approaches in familial pancreatic cancer. Gastrointest Endosc Clin N Am. 2008;18:535–553. doi: 10.1016/j.giec.2008.05.012. [DOI] [PubMed] [Google Scholar]
- Chan YC, Leung PS. Acute pancreatitis: animal models and recent advances in basic research. Pancreas. 2007;34:1–14. doi: 10.1097/01.mpa.0000246658.38375.04. [DOI] [PubMed] [Google Scholar]
- Chan YC, Leung PS. Angiotensin II type 1 receptor-dependent nuclear factor-kappaB activation-mediated proinflammatory actions in a rat model of obstructive acute pancreatitis. J Pharmacol Exp Ther. 2007;323:10–18. doi: 10.1124/jpet.107.124891. [DOI] [PubMed] [Google Scholar]
- Choi JY, Muallem D, Kiselyov K, Lee MG, Thomas PJ, Muallem S. Aberrant CFTR-dependent HCO3− transport in mutations associated with cystic fibrosis. Nature. 2001;410:94–97. doi: 10.1038/35065099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czako L, Hegyi P, Rakonczay Z, Wittmann T, Otsuki M. Interactions between the endocrine and exocrine pancreas and their clinical relevance. Pancreatology. 2009;9:351–359. doi: 10.1159/000181169. [DOI] [PubMed] [Google Scholar]
- Danovi SA, Wong HH, Lemoine NR. Targeted therapies for pancreatic cancer. Br Med Bull. 2008;87:97–130. doi: 10.1093/bmb/ldn027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies MG, Hagen PO. Systemic inflammatory response syndrome. Br J Surg. 1997;84:920–935. doi: 10.1002/bjs.1800840707. [DOI] [PubMed] [Google Scholar]
- Davis PB, Drumm M, Konstan MW. Cystic fibrosis. Am J Respir Crit Care Med. 1996;154:1229–1256. doi: 10.1164/ajrccm.154.5.8912731. [DOI] [PubMed] [Google Scholar]
- Delorio AV, Vitale GC, Jr, Reynolds M, Larson GM. Acute biliary pancreatitis. The roles of laparoscopic cholecystectomy and endoscopic retrograde cholangiopancreatography. Surg Endosc. 1995;9:392–396. doi: 10.1007/BF00187157. [DOI] [PubMed] [Google Scholar]
- Eisenbarth GS. Update in type 1 diabetes. J Clin Endocrinol Metab. 2007;92:2403–2407. doi: 10.1210/jc.2007-0339. [DOI] [PubMed] [Google Scholar]
- Dunphy EP. Pancreatic cancer: a review and update. Clin J Oncol Nurs. 2008;12:735–741. doi: 10.1188/08.CJON.735-741. [DOI] [PubMed] [Google Scholar]
- Forstner J, Wesley A, Mantle M, Kopelman H, Man D, Forstner G. Abnormal mucus: nominated but not yet elected. J Pediatr Gastroenterol Nutr. 1984;3(Suppl 1):S67–S73. doi: 10.1097/00005176-198400031-00012. [DOI] [PubMed] [Google Scholar]
- Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT, Khunti K. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ. 2007;334:299. doi: 10.1136/bmj.39063.689375.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gullo L, Migliori M, Oláh A, Farkas G, Levy P, Arvanitakis C, Lankisch P, Beger H. Acute pancreatitis in five European countries: etiology and mortality. Pancreas. 2002;24:223–227. doi: 10.1097/00006676-200204000-00003. [DOI] [PubMed] [Google Scholar]
- Guy-Crotte O, Carrere J, Figarella C. Exocrine pancreatic function in cystic fibrosis. Eur J Gastroenterol Hepatol. 1996;8:755–759. [PubMed] [Google Scholar]
- Hall IH, Lee KH, Imakura Y, Okano M, Johnson A. Anti-inflammatory agents. III. Structure-activity relationships of brusatol and related quassinoids. J Pharm Sci. 1983;72:1282–1284. doi: 10.1002/jps.2600721111. [DOI] [PubMed] [Google Scholar]
- Hruban RH, Adsay NV. Molecular classification of neoplasms of the pancreas. Hum Pathol. 2009;40:612–623. doi: 10.1016/j.humpath.2009.01.008. [DOI] [PubMed] [Google Scholar]
- Hui YF, Reitz J. Gemcitabine: a cytidine analogue active against solid tumors. Am J Health Syst Pharm. 1997;54:162–170. doi: 10.1093/ajhp/54.2.162. [DOI] [PubMed] [Google Scholar]
- Ingbar DH, Bhargava M, O’Grady SM. Mechanisms of alveolar epithelial chloride absorption. Am J Physiol. 2009;297:L813–L815. doi: 10.1152/ajplung.00324.2009. [DOI] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- Jones AM, Helm JM. Emerging treatments in cystic fibrosis. Drugs. 2009;69:1903–1910. doi: 10.2165/11318500-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Lau HY, Wong FL, Bhatia M. A key role of neurokinin 1 receptors in acute pancreatitis and associated lung injury. Biochem Biophys Res Commun. 2005;327:509–515. doi: 10.1016/j.bbrc.2004.12.030. [DOI] [PubMed] [Google Scholar]
- Lau FY, Chui CH, Gambari R, Kok SH, Kan KL, Cheng GY, Wong RS, Teo IT, Cheng CH, Wan TS, Chan AS, Tang JC. Antiproliferative and apoptosis-inducing activity of Brucea javanica extract on human carcinoma cells. Int J Mol Med. 2005;16:1157–1162. [PubMed] [Google Scholar]
- Lau ST, Lin ZX, Leung PS. Role of reactive oxygen species in brucein D-mediated p38 mitogen-activated protein kinase and nuclear factor κB signaling pathways in human pancreatic adenocarcinoma cells. Br J Cancer. 2010;102:583–593. doi: 10.1038/sj.bjc.6605487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau ST, Lin ZX, Liao YH, Zhao M, Cheng CH, Leung PS. Brucein D induces apoptosis in pancreatic adenocarcinoma cell line PANC-1 through the activation of p38-mitogen activated protein kinase. Cancer Letters. 2009;281:42–52. doi: 10.1016/j.canlet.2009.02.017. [DOI] [PubMed] [Google Scholar]
- Lau ST, Lin ZX, Zhao M, Leung PS. Brucea javanica fruit induces cytotoxicity and apoptosis in pancreatic adenocarcinoma cell lines. Phytother Res. 2008;22:477–486. doi: 10.1002/ptr.2344. [DOI] [PubMed] [Google Scholar]
- Lemoine NR, Hughes CM, Barton CM, Poulsom R, Jeffery RE, Kloppel G, Hall PA, Gullick WJ. The epidermal growth factor receptor in human pancreatic cancer. J Pathol. 1992;166:7–12. doi: 10.1002/path.1711660103. [DOI] [PubMed] [Google Scholar]
- Leung PS, Chan YC. Role of oxidative stress in pancreatic inflammation. Antioxid Redox Signal. 2009;11:135–165. doi: 10.1089/ars.2008.2109. [DOI] [PubMed] [Google Scholar]
- Lewis BC. Development of the pancreas and pancreatic cancer. Endocrinol Metab Clin. 2006;35:387–404. doi: 10.1016/j.ecl.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Loos M, Kleeff J, Friess H, Buchler MW. Approaches to localized pancreatic cancer. Curr Oncol Rep. 2008;10:212–219. doi: 10.1007/s11912-008-0033-8. [DOI] [PubMed] [Google Scholar]
- Loos M, Kleeff J, Friess H, Buchler MW. Surgical treatment of pancreatic cancer. Ann N Y Acad Sci. 2008;1138:169–180. doi: 10.1196/annals.1414.024. [DOI] [PubMed] [Google Scholar]
- Makola D, Krenitsky J, Parrish CR. Enteral feeding in acute and chronic pancreatitis. Gastrointest Endosc Clin N Am. 2007;17:747–764. doi: 10.1016/j.giec.2007.07.010. [DOI] [PubMed] [Google Scholar]
- McFadden DW. Organ failure and multiple organ system failure in pancreatitis. Pancreas. 1991;6(Suppl 1):S37–S43. doi: 10.1097/00006676-199101001-00007. [DOI] [PubMed] [Google Scholar]
- Meier JJ. Beta cell mass in diabetes: a realistic therapeutic target? Diabetologia. 2008;51:703–713. doi: 10.1007/s00125-008-0936-9. [DOI] [PubMed] [Google Scholar]
- NoorShahida A, Wong TW, Choo CY. Hypoglycemic effect of quassinoids from Brucea javanica (L.) Merr (Simaroubaceae) seeds. J Ethnopharmacol. 2009;124:586–591. doi: 10.1016/j.jep.2009.04.058. [DOI] [PubMed] [Google Scholar]
- O’Neill MJ, Bray DH, Boardman P, Chan KL, Phillipson JD, Warhurst DC, Peter W. Plants as sources of antimalarial drugs. Part 4. Activity of Brucea Javanica fruits against chloroquine-resistant Plasmodium falciparum in vitro an against Plasmodium berghei in vivo. J Nat Prod. 1987;50:41–48. doi: 10.1021/np50049a007. [DOI] [PubMed] [Google Scholar]
- Ozawa F, Friess H, Kunzli B, Shrikhande SV, Otani T, Makuuchi M, Buchler MW. Treatment of pancreatic cancer: the role of surgery. Dig Dis. 2001;19:47–56. doi: 10.1159/000050653. [DOI] [PubMed] [Google Scholar]
- Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, Hu ZX, Lin J, Xiao JZ, Cao HB, Liu PA, Jiang XG, Jiang YY, Wang JP, Zheng H, Zhang H, Bennett PH, Howard BV, Diabetes Study. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20:537–544. doi: 10.2337/diacare.20.4.537. [DOI] [PubMed] [Google Scholar]
- Park SD, Jung JH, Lee HW, Kwon YM, Chung KH, Kim MG, Kim CH. Zedoariae rhizoma and curcumin inhibits platelet-derived growth factor-induced proliferation of human hepatic myofibroblasts. Int Immunopharmacol. 2005;5:555–569. doi: 10.1016/j.intimp.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Pelli H, Sand J, Laippala P, Nordback I. Long-term follow-up after the first episode of acute alcoholic pancreatitis: time course and risk factors for recurrence. Scand J Gastroenterol. 2000;35:552–555. doi: 10.1080/003655200750023840. [DOI] [PubMed] [Google Scholar]
- Phillips B, Giannoukakis N, Trucco M. Dendritic cell mediated therapy for immunoregulation of type 1 diabetes mellitus. Pediatr Endocrinol Rev. 2008;5:873–879. [PubMed] [Google Scholar]
- Proesmans M, Vermeulen F, De Boeck K. What is new in cystic fibrosis: from treating symptoms to correction of the basic defect. Eur J Pediatr. 2008;167:839–849. doi: 10.1007/s00431-008-0693-2. [DOI] [PubMed] [Google Scholar]
- Ramsey BW. Management of pulmonary disease in patients with cystic fibrosis. N Engl J Med. 1996;335:179–188. doi: 10.1056/NEJM199607183350307. [DOI] [PubMed] [Google Scholar]
- Ratjen F. New pulmonary therapies for cystic fibrosis. Curr Opin Pulm Med. 2007;13:541–546. doi: 10.1097/MCP.0b013e3282efbc56. [DOI] [PubMed] [Google Scholar]
- Reddy MM, Light MJ, Quinton PM. Activation of the epithelial Na+ channel (ENaC) requires CFTR Cl– channel function. Nature. 1999;402:301–304. doi: 10.1038/46297. [DOI] [PubMed] [Google Scholar]
- Reimann M, Bonifacio E, Solimena M, Schwarz PE, Ludwig B, Hanefeld M, Bornstein SR. An update on preventive and regenerative therapies in diabetes mellitus. Pharmacol Ther. 2008;121:317–331. doi: 10.1016/j.pharmthera.2008.11.009. [DOI] [PubMed] [Google Scholar]
- Riordan JR. CFTR function and prospects for therapy. Annu Rev Biochem. 2008;77:701–726. doi: 10.1146/annurev.biochem.75.103004.142532. [DOI] [PubMed] [Google Scholar]
- Schulenburg A, Ulrich-Pur H, Thurnher D, Erovic B, Florian S, Sperr WR, Kalhs P, Marian B, Wrba F, Zielinski CC, Valent P. Neoplastic stem cells: a novel therapeutic target in clinical oncology. Cancer. 2006;107:2512–2520. doi: 10.1002/cncr.22277. [DOI] [PubMed] [Google Scholar]
- Schwiebert EM, Benos DJ, Egan ME, Stutts MJ, Guggino WB. CFTR is a conductance regulator as well as a chloride channel. Physiol Rev. 1999;79:S145–S166. doi: 10.1152/physrev.1999.79.1.S145. [DOI] [PubMed] [Google Scholar]
- Sebens S, Arlt A, Schafer H. NF-kappaB as a molecular target in the therapy of pancreatic carcinoma. Recent Results Cancer Res. 2008;177:151–164. doi: 10.1007/978-3-540-71279-4_17. [DOI] [PubMed] [Google Scholar]
- Sekimoto M, Takada T, Kawarada Y, Hirata K, Mayumi T, Yoshida M, Hirota M, Kimura Y, Takeda K, Isaji S, Koizumi M, Otsuki M, Matsuno S. Japan guidelines for the management of acute pancreatitis: epidemiology, etiology, natural history, and outcome predictors in acute pancreatitis. J Hepatobiliary Pancreat Surg. 2006;13:10–24. doi: 10.1007/s00534-005-1047-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro A, Ricordi C, Hering B, Auchincloss H, Lindblad R, Robertson R, Secchi A, Brendel M, Berney T, Brennan D, Cagliero E, Alejandro R, Ryan E, DiMercurio B, Morel P, Polonsky K, Reems J, Bretzel R, Bertuzzi F, Froud T, Kandaswamy R, Sutherland D, Eisenbarth G, Segal M, Preiksaitis J, Korbutt G, Barton F, Viviano L, Seyfert-Margolis V, Bluestone J, Lakey J. International trial of the Edmonton protocol for islet transplantation. N Engl J Med. 2006;355:1318–1330. doi: 10.1056/NEJMoa061267. [DOI] [PubMed] [Google Scholar]
- Singh VP, Saluja AK, Bhagat L, van Acker GJ, Song AM, Soltoff SP, Cantley LC, Steer ML. Phosphatidylinositol 3-kinase-dependent activation of trypsinogen modulates the severity of acute pancreatitis. J Clin Invest. 2001;108:1387–1395. doi: 10.1172/JCI12874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song AM, Bhagat L, Singh VP, Van Acker GG, Steer ML, Saluja AK. Inhibition of cyclooxygenase-2 ameliorates the severity of pancreatitis and associated lung injury. Am J Physiol. 2002;283:G1166–G1174. doi: 10.1152/ajpgi.00370.2001. [DOI] [PubMed] [Google Scholar]
- Song SH, Hardisty CA. Early-onset Type 2 diabetes mellitus: an increasing phenomenon of elevated cardiovascular risk. Expert Rev Cardiovasc Ther. 2008;6:315–322. doi: 10.1586/14779072.6.3.315. [DOI] [PubMed] [Google Scholar]
- Stratta R, Alloway R. Pancreas transplantation for diabetes mellitus: a guide to recipient selection and optimum immunosuppression. BioDrugs. 1998;10:347–357. doi: 10.2165/00063030-199810050-00002. [DOI] [PubMed] [Google Scholar]
- Stumvoll M, Goldstein BJ, van Haeften TW. Type 2 diabetes: principles of pathogenesis and therapy. Lancet. 2005;365:1333–1346. doi: 10.1016/S0140-6736(05)61032-X. [DOI] [PubMed] [Google Scholar]
- Tashiro M, Schäfer C, Yao H, Ernst SA, Williams JA. Arginine induced acute pancreatitis alters the actin cytoskeleton and increases heat shock protein expression in rat pancreatic acinar cells. Gut. 2001;49:241–250. doi: 10.1136/gut.49.2.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torgerson JS, Hauptman J, Boldrin MN, Sjostrom L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004;27:155–161. doi: 10.2337/diacare.27.1.155. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Spock A, Spicer SS, Shelburne JD, Bradford W. Inspissation of pancreatic zymogen material in cystic fibrosis. Ultrastruct Pathol. 2003;27:323–335. doi: 10.1080/716100784. [DOI] [PubMed] [Google Scholar]
- Voltarelli J, Couri C, Stracieri A, Oliveira M, Moraes D, Pieroni F, Coutinho M, Malmegrim K, Foss-Freitas M, Simoes B, Foss M, Squiers E, Burt R. Autologous nonmyeloablative hematopoietic stem cell transplantation in newly diagnosed type 1 diabetes mellitus. JAMA. 2007;297:1568–1576. doi: 10.1001/jama.297.14.1568. [DOI] [PubMed] [Google Scholar]
- Voynow JA, Scanlin TF. Cystic fibrosis. In: Panitch HB, editor. Pediatric Pulmonology. Philadelphia, PA: Elsevier Mosby; 2005. [Google Scholar]
- Wang X, Wang SH, Gou H. The progress in the experimental studies of anticancer Chinese herbal compounds. Chin J Exp Trad Med Form. 2005;11:71–73. [Google Scholar]
- Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- Zheng S, Chen A. Activation of PPARgamma is required for curcumin to induce apoptosis and to inhibit the expression of extracellular matrix genes in hepatic stellate cells in vitro. Biochem J. 2004;384:149–157. doi: 10.1042/BJ20040928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou ZG, Yan WW, Chen YQ, Chen YD, Zheng XL, Peng XH. Effect of inducible cyclooxygenase expression on local microvessel blood flow in acute interstitial pancreatitis. Asian J Surg. 2004;27:93–98. doi: 10.1016/S1015-9584(09)60320-1. [DOI] [PubMed] [Google Scholar]


