Abstract
Objective:
To examine trends in mental health (MH) visits to pediatric emergency departments (EDs) and identify whether ED disposition varies by presence of a hospital inpatient psychiatric unit (IPU).
Study Design:
Cross-sectional study of 8,479,311 ED visits to 35 children’s hospitals from 2012 to 2016 for patients aged 3 to 21 years with a primary MH or non-MH diagnosis. Multivariable generalized estimating equations and bivariate Rao-Scott chi-square tests were used to examine trends in ED visits and ED disposition by IPU status, adjusted for clustering by hospital.
Results:
From 2012 to 2016, hospitals experienced a greater increase in ED visits with a primary MH vs. non-MH diagnosis (50.7% vs. 12.7% cumulative increase, P<.001). MH visits were associated with patients who were older, female, white non-Hispanic, and privately insured compared with patients of non-MH visits (all P<.001). 44% of MH visits in 2016 had a primary diagnosis of depressive disorders or suicide or self-injury, and the increase in visits was highest for these diagnosis groups (depression: 109.8%; suicide or self-injury: 110.2%). Among MH visits, presence of a hospital IPU was associated with increased hospitalizations (34.6% vs. 22.5%, P<.001) and less transfers (9.3% vs. 16.2%, P<.001).
Conclusion:
The increase in ED MH visits from 2012 to 2016 was four times greater than non-MH visits at US children’s hospitals, and was primarily driven by patients diagnosed with depressive disorders and suicide or self-injury. Our findings have implications for strategic planning in tertiary children’s hospitals dealing with a rising demand for acute MH care.
Keywords: pediatric mental health, emergency department, suicide or self-injury, depression, discharge disposition
Introduction
National recommendations for pediatric emergency care include strengthening the capacity to address mental health (MH) emergencies as well as timely transfer to inpatient psychiatric care.1 During the last decade, pediatric emergency department (ED) use for MH conditions has risen dramatically,2–7 and EDs are increasingly serving as a “safety net” for youth in crisis.8,9 ED visits with a primary or secondary diagnosis of suicidal ideation or suicide attempt are rising in children’s hospitals across the United States (US),10,11 but trends for other MH conditions have not been well described. The rise in pediatric ED use for MH conditions is straining the capacity of overcrowded EDs.6 MH visits are longer, more likely to be triaged to urgent evaluation, and result in more admissions, transfers, and readmissions compared to non-MH visits. 3,12–14 Acute care of pediatric MH conditions in the ED often requires assessment of a broad spectrum of mental and substance use disorders, psychotropic medication treatment regimens, and underlying contextual factors, presenting a unique challenge for ED clinicians without psychiatric training.15
Pediatric ED clinicians face many barriers when connecting patients to specialized MH care.16 Patients who need inpatient care often require a transfer to another facility, with many children enduring long ED wait times due to the national shortage of inpatient psychiatric beds.17 Hospitals with inpatient psychiatric units (IPUs) may provide quicker access to acute MH care and improved coordination of care across the ED and MH clinical teams. Indeed, the one single-hospital study on this topic found that having an IPU was associated with shorter ED length of stay and higher rates of hospitalization.16 To date, no national study has evaluated whether the presence of an IPU in a tertiary care children’s hospital impacts rates of transfer or hospitalization for patients presenting to an ED with MH conditions.
To address this knowledge gap, using a large administrative database including 35 tertiary care children’s hospitals we sought to: 1) describe four-year trends in pediatric ED visits for primary MH vs. non-MH conditions overall and by specific MH condition; 2) describe variation in sociodemographic characteristics, medical complexity, and ED disposition by MH diagnosis status; and 3) identify whether ED disposition for patients with a primary MH condition varies by presence of a hospital IPU. Together these findings can inform strategic planning of pediatric ED resources in children’s hospitals by identifying priority clinical populations and describing the impact of an IPU on ED disposition for patients with a primary MH condition.
Methods
Study Design and Data Source
This study was a cross-sectional analysis of the Pediatric Health Information System (PHIS), an administrative database containing hospitalization data from 35 tertiary care US children’s hospitals. All PHIS hospitals are members of the Children’s Hospital Association (Lenexa, KS). Data quality and reliability are assured jointly by the Children’s Hospital Association, participating hospitals, and Truven Health Analytics (New York, NY).18 Each record in PHIS represents a single discharge and contains administrative data, including demographic characteristics, billing information, and procedures and diagnoses classified by the International Classification of Disease, Ninth or Tenth Revision, Clinical Modification (ICD-9-CM/ICD-10-CM).
Study Population
We examined all ED visits for patients aged 3 to 21 years from 2012 to 2016 from 35 hospitals with discharge and billing data for the entire study period. Similar to other studies, we restricted the study sample to visits for patients aged 3 to 21 years to focus on pediatric visits most likely to require acute MH care.5,6,19
Classification of MH diagnoses
The primary reason for ED visit was determined using ED discharge diagnosis codes. MH conditions were classified into diagnosis categories using ICD-9-CM or ICD-10-CM codes based on a scheme previously developed to identify pediatric MH conditions from hospital discharge data.20 A visit was categorized as a primary MH visit if the primary discharge diagnosis was for a MH condition or met a validated definition for suicide attempt.21 All other visits were categorized as a primary non-MH visit.
Patient and Hospital Characteristics
Characteristics assessed for the primary MH and non-MH groups included age, sex, race/ethnicity, insurance type, medical complexity using the chronic condition indicator (CCI) system, the complex chronic condition (CCC) classification system,22 and ED disposition. For ED MH visits an ED disposition of admission included admission to a medical or psychiatric bed within the same hospital, and an ED disposition of transfer included both transfer to a psychiatric unit in another hospital or transfer to a free-standing psychiatric facility. A hospital was categorized as having an IPU if they submitted any records to PHIS with psychiatric unit bed charges. Billing codes were used to identify whether a hospital had an IPU available for the entire study period or a portion of the study period.
Statistical Analysis
We assessed associations of patient demographic and clinical characteristics by primary diagnosis group and age group using bivariate Rao-Scott chi-square tests, accounting for hospital clustering. We used traditional chi-square tests to assess associations by the presence of an IPU, since presence of an IPU is clustered at the hospital level. To assess aggregate trends in the growth of ED visits within subgroups we used linear, multivariable regression. Multivariable models were derived using generalized estimating equations to account for clustering of data within hospitals. The linear generalized estimating equation models contained a random effect for hospital, fixed effects for population factors that may influence the growth trends (e.g., total pediatric population, number of US pediatric ED visits, total number of children living in poverty),23 and interaction terms for primary diagnosis group and year. An interaction term between primary diagnosis group and year was used to compare the adjusted growth over time among patients visiting for primary MH or non-MH concerns. Cumulative growth was calculated as the percent change between 2012 and 2016. Subgroup analyses were performed on MH ED visits by specific MH condition, hospitals with IPUs for the full study period, and hospitals without IPUs for the full study period. Two hospitals added an IPU during the study period and were excluded from the trends analysis comparing IPU vs. non-IPU hospitals. All hospitals were included in chi-square analyses. P values <0.05 were considered statistically significant, and all analyses were performed with SAS, version 9.4 (SAS Institute, Inc, Cary, NC). This study of de-identified data was reviewed and deemed exempt by the Institutional Review Board at Children’s Minnesota.
Results
ED Visits for MH vs. Non-MH Conditions
We identified 8,479,311 ED visits that met inclusion criteria. Among these, 245,256 (2.9%) were primary MH visits,which represented 180,558 individual patients. Of patients with MH ED visits, 4.8% had 3 or more visits in a one-year period. The rate of increase of ED visits for MH conditions from 2012 to 2016 was significantly greater than the increase in visits for non-MH conditions (50.7% vs. 12.7%, p<0.001). The rate of increase in ED visits for MH conditions differed by diagnosis (Figure 1). Three MH conditions increased by more than 100%, with an over 8 times greater cumulative rise than non-MH visits (Table 1). Visits with a diagnosis of depressive disorder rose 109.8% (6,792 visits in 2012 to 14,253 in 2016); visits for suicide or self-injury rose 110.2% (5,425 in 2012 to 11,406 in 2016); and visits with a diagnosis of trauma and stressor-related disorders rose 114.8% (1,253 in 2012 to 2,692 in 2016). Depressive disorders and suicide or self-injury represented almost a third of MH visits in 2012 (31.5%), and grew to 43.9% of visits by 2016.
Figure 1.
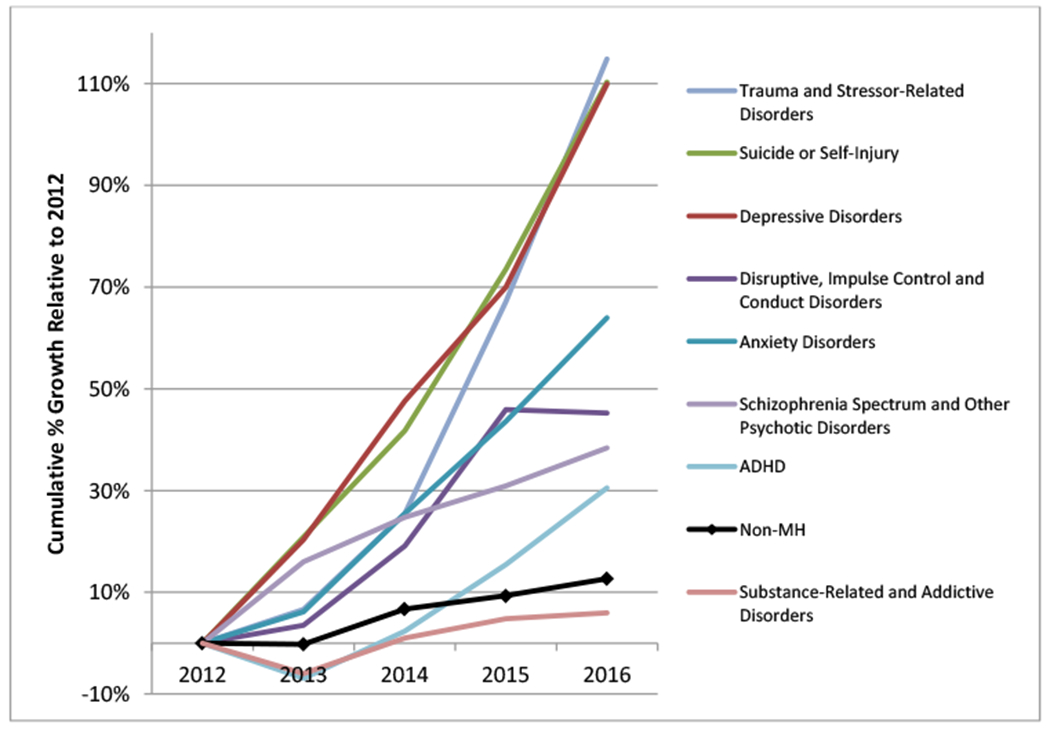
Cumulative % Growth from 2012 to 2016 for Primary MH vs. Primary Non-MH ED visits
Table 1.
Cumulative % Growth from 2012 to 2016 by Type of ED Visit and Specific MH Diagnosis Groups
| ED Visits in 2012 N | ED Visits in 2016 N | Cumulative % Growth 2012 to 2016 | p-value | |
|---|---|---|---|---|
| Non-MH ED Visit | 1,555,956 | 1,755,511 | 12.7% | - |
| MH ED Visit | 38,829 | 58,503 | 50.7% | <0.001a |
| Top MH Diagnosis Groups | ||||
| Depressive disorders | 6,792 | 14,253 | 109.8% | <0.001 |
| Suicide or self-injury | 5,425 | 11,406 | 110.2% | <0.001 |
| Disruptive, impulse control and conduct disorders | 5,416 | 7,864 | 45.2% | <0.001 |
| Anxiety disorders | 3,303 | 5,415 | 63.9% | <0.001 |
| Trauma and stressor-related disorders | 1,253 | 2,692 | 114.8% | 0.013 |
| Substance-related and addictive disorders | 1,757 | 1,862 | 6.0% | 0.038 |
| Schizophrenia spectrum and other psychotic disorders | 1,177 | 1,629 | 38.4% | <0.001 |
| ADHD | 1,053 | 1,374 | 30.5% | 0.051 |
MH=mental health; ED=emergency department; ADHD=attention deficit hyperactivity disorder.
P-value for comparison between cumulative % growth for MH vs. non-MH ED visits.
Sociodemographic characteristics and ED disposition varied among ED patients depending on whether or not the primary diagnosis was a MH condition. Among pediatric ED visits for a primary MH condition, patients were more likely to be older, female, white non-Hispanic, and privately insured compared to youth seen in the ED for a non-MH visit (all p<.001, Table 2). Compared with non-MH ED visits, nearly three times as many patients visiting the ED with a primary MH condition were admitted (31.0% vs. 11.4%, p<.001), and over 22 times as many were transferred (11.3% vs. 0.5%, p<.001). There was no significant difference in medical complexity between MH and non-MH ED visits.
Table 2.
Characteristics of ED Visits for Pediatric Patients Overall and by Presence of a Primary MH Diagnosis from 2012 to 2016
| Characteristic | All patients (N = 8,479,311) n (%) |
Primary MH diagnosisa (N = 245,256) n (%) |
Primary non-MH diagnosis (N = 8,234,055) n (%) |
|---|---|---|---|
| Age, y | |||
| 3-7 | 3,835,865 (45.2) | 20,980 (8.6) | 3,814,885 (46.3) |
| 8-12 | 2,363,983 (27.9) | 65,802 (26.8) | 2,298,181 (27.9) |
| 13-17 | 1,997,177 (23.6) | 151,038 (61.6) | 1,846,139 (22.4) |
| 18-21 | 282,286 (3.3) | 7,436 (3.0) | 274,850 (3.3) |
| Sex | |||
| Male | 4,363,745 (51.5) | 112,194 (45.8) | 4,251,551 (51.6) |
| Female | 4,114,475 (48.5) | 132,942 (54.2) | 3,981,533 (48.4) |
| Race/ethnicity | |||
| White/NH | 3,223,535 (38.0) | 128,118 (52.2) | 3,095,417 (37.6) |
| Black/NH | 2,390,985 (28.2) | 57,157 (23.3) | 2,333,828 (28.3) |
| Hispanic | 2,047,776 (24.2) | 37,007 (15.1) | 2,010,769 (24.4) |
| Other | 817,015 (9.6) | 22,974 (9.4) | 794,041 (9.6) |
| Payer | |||
| Government | 5,263,303 (62.1) | 133,764 (54.5) | 5,129,539 (62.3) |
| Commercial | 2,638,725 (31.1) | 98,142 (40.0) | 2,540,583 (30.9) |
| Self-pay | 368,021 (4.3) | 7,626 (3.1) | 360,395 (4.4) |
| Other | 137,383 (1.6) | 3,105 (1.3) | 134,278 (1.6) |
| Missing | 71,879 (0.8) | 2,619 (1.1) | 69,260 (0.8) |
| Chronic Conditions | |||
| CCC | 471,809 (5.6) | 10,515 (4.3) | 461,294 (5.6) |
| Physical CCI | 962,063 (11.3) | 25,810 (10.5) | 936,253 (11.4) |
| No CCC or Physical CCI | 7,045,439 (83.1) | 208,931 (85.2) | 6,836,508 (83.0) |
| ED Disposition | |||
| Admitted | 1,011,503 (11.9) | 75,969 (31.0) | 935,534 (11.4) |
| Discharged | 7,221,525 (85.2) | 133,964 (54.6) | 7,087,561 (86.1) |
| Transfer | 65,296 (0.8) | 27,803 (11.3) | 37,493 (0.5) |
| Against Medical Advice | 76,465 (0.9) | 934 (0.4) | 75,531 (0.9) |
| Died | 857 (0.0) | 20 (0.0) | 837 (0.0) |
| Other | 103,665 (1.2) | 6,566 (2.7) | 97,099 (1.2) |
MH=mental health; NH=non-Hispanic; CCC=complex chronic condition; CCI=chronic condition indicator.
For primary MH diagnosis (Yes vs. No) all differences significant at P < .001 with the exception of chronic conditions (p=0.10).
ED Visits for MH Conditions at IPU vs. Non-IPU Hospitals
Of the 35 freestanding children’s hospitals in our cohort, 14 (40%) had an IPU for the duration of the study period. Two hospitals added an IPU during the study period and were excluded from trend analysis. The majority of patients with a MH visit were treated at a hospital with an IPU (69.8%). Likelihood of having an IPU was significantly associated with hospital size; only 15.4% of hospitals with less than 15,000 admissions in 2016 had an IPU, whereas over half (63.6%) of hospitals with greater than 15,000 admissions had an IPU (p=0.006). However, the cumulative percentage increase in MH visits at hospitals with an IPU was similar to the increase in MH visits in hospitals with no IPU (47.1% vs. 40.5%, p=0.22).
Patients visiting a hospital with an IPU for a MH condition were more likely to be older, male, white non-Hispanic, and privately insured compared to youth visiting a hospital without an IPU (all p<.001, Table 3). MH visits to a hospital with an IPU were more likely to result in admission compared to visits to non-IPU hospitals (34.6% vs. 22.5%, P<0.001), and we found a corresponding decrease in likelihood of transfer at IPU vs. non-IPU hospitals (9.2% vs. 16.2%, p<0.001). Combined admission and transfer rates were higher at IPU vs. non-IPU hospitals (43.8% vs. 38.7%).
Table 3.
Characteristics of ED Visits with a Primary MH Diagnosis by Presence of a Hospital IPU from 2012 to 2016
| Patient characteristic | Inpatient Psychiatric Unit (N = 171,153) n (%) |
No Inpatient Psychiatric Unita (N = 74,103) n (%) |
|---|---|---|
| Age, y | ||
| 3-7 | 13,241 (7.7) | 7,739 (10.4) |
| 8-12 | 46,392 (27.1) | 19,410 (26.2) |
| 13-17 | 106,661 (62.3) | 44,377 (59.9) |
| 18-21 | 4,859 (2.8) | 2,577 (3.5) |
| Sex | ||
| Male | 79,047 (46.2) | 33,147 (44.7) |
| Female | 92,012 (53.8) | 40,930 (55.3) |
| Race/ethnicity | ||
| White/NH | 91,795 (53.6) | 36,323 (49.0) |
| Black/NH | 38,519 (22.5) | 18,638 (25.2) |
| Hispanic | 24,732 (14.5) | 12,275 (16.6) |
| Other | 16,107 (9.4) | 6,867 (9.3) |
| Payer | ||
| Government | 91,373 (53.4) | 42,391 (57.2) |
| Commercial | 71,335 (41.7) | 26,807 (36.2) |
| Self-pay | 4,616 (2.7) | 3,010 (4.1) |
| Other | 1,786 (1.0) | 1,319 (1.8) |
| Chronic Conditions | ||
| CCC | 6,968 (4.1) | 3,547 (4.8) |
| Physical CCI | 18,980 (11.1) | 6,830 (9.2) |
| No CCC or Physical CCI | 145,205 (84.8) | 63,726 (86.0) |
| ED Disposition | ||
| Admitted | 59,264 (34.6) | 16,705 (22.5) |
| Discharged | 91,328 (53.4) | 42,636 (57.5) |
| Transfer | 15,801 (9.2) | 12,002 (16.2) |
| Against Medical Advice | 654 (0.4) | 280 (0.4) |
| Died | 8 (0.0) | 12 (0.0) |
| Other | 4,098 (2.4) | 2,468 (3.3) |
NH=non-Hispanic; CCC=complex chronic condition; CCI=chronic condition indicator.
All differences significant at P < .001.
ED Disposition by Specific Condition and Presence of an IPU
The proportion of MH ED visits resulting in transfer compared to admission differed between hospitals with and without an IPU by specific MH condition. Patients visiting IPU hospitals who had a diagnosis of depressive disorders were almost three times as likely to be admitted compared to patients who visited non-IPU hospitals (47.5% vs. 17.6%, p<.001, Table 4), while those visiting with disruptive, impulse control and conduct disorders were twice as likely to be admitted at IPU hospitals (27.7% vs. 11.6%, p<.001). The likelihood of patient transfer was significantly lower at IPU vs. non-IPU hospitals for the top MH conditions with the exclusion of anxiety disorders. Patients with a diagnosis of suicide or self-injury had the highest transfer rate at both types of hospitals, although the percentage of patients transferred was significantly lower at IPU vs. non-IPU hospitals (36.9% vs. 53.7%, p<.001). Patients with depressive disorders were the next most likely to be transferred, with transfers also less likely at IPU vs. non-IPU hospitals (16.0% vs. 30.9%, p<.001). Finally, we found that patients with depressive disorders had a higher overall combined admission/transfer rate at IPU vs. non-IPU hospitals (63.5% vs. 48.5%), resulting in lower rates of discharge at IPU hospitals (36.5% vs. 51.5%, p<.001). In contrast, patients visiting for suicide or self-injury had a lower combined admission/transfer rate at IPU vs. non-IPU hospitals (69.5% vs. 88.6%), resulting in higher rates of discharge at IPU hospitals (30.7% vs. 11.4%, p<.001).
Table 4.
Disposition for ED MH Visits Overall and by Presence of an IPU for the 5 Most Common Diagnosis Categories from 2012 to 2016
| Hospital IPU |
|||
|---|---|---|---|
| Overall | Yes a | No | |
| N (%) | N (%) | N (%) | |
| Depressive disorders | |||
| N | 50,788 | 43,230 | 7,558 |
| Hospitalization | 21,863 (43.0) | 20,534 (47.5) | 1,329 (17.6) |
| Transfer | 9,261 (18.2) | 6,923 (16.0) | 2,338 (30.9) |
| Dischargedb | 19,664 (38.7) | 15,733 (36.5) | 3,891 (51.5) |
| Suicide or self-injury | |||
| N | 40,493 | 21,687 | 18,806 |
| Hospitalization | 13,587 (33.6) | 7,026 (32.4) | 6,561 (34.9) |
| Transfer | 18,098 (44.7) | 7,997 (36.9) | 10,101 (53.7) |
| Discharged | 8,808 (21.8) | 6,664 (30.7) | 2,144 (11.4) |
| Disruptive, impulse control and conduct disorders | |||
| N | 33,244 | 24,728 | 8,516 |
| Hospitalization | 7,847 (23.6) | 6,859 (27.7) | 988 (11.6) |
| Transfer | 4,743 (14.3) | 2,689 (10.9) | 2,054 (24.1) |
| Discharged | 20,654 (62.1) | 15,180 (61.4) | 5,474 (64.3) |
| Anxiety disorders | |||
| N | 21,113 | 12,622 | 8,491 |
| Hospitalization | 1,944 (9.2) | 1,557 (12.3) | 387 (4.6) |
| Transfer | 797 (3.8) | 535 (4.2) | 262 (3.1) |
| Discharged | 18,374 (87.0) | 10,530 (83.4) | 7,842 (92.4) |
| Trauma and stressor-related disorders | |||
| N | 8,947 | 7,851 | 1,096 |
| Hospitalization | 3,105 (34.7) | 2,868 (36.5) | 237 (21.6) |
| Transfer | 649 (7.3) | 527 (6.7) | 122 (11.1) |
| Discharged | 5,193 (58.0) | 4,456 (56.8) | 737 (67.3) |
All differences significant at P < .001.
Category includes patients who left against medical advice, died, or other, but vast majority of patients were discharged (95%).
Discussion
From 2012 to 2016, the increase in ED visits to US children’s hospitals for MH conditions far outpaced the increase in visits for non-MH conditions. Depressive disorders and suicide or self-injury represented 44% of primary MH visits in 2016, and the increase in visits for these two MH conditions was almost 8 times that of non-MH visits. Patients visiting hospitals with an IPU for primary MH concerns were significantly more likely to be admitted, and thus significantly less likely to require transfer compared to patients visiting non-IPU hospitals. For the most common diagnosis group, depressive disorders, patients were nearly three times as likely to be admitted and half as likely to be transferred when visiting IPU hospitals. Combined admission/transfer rates also differed by IPU status. For all but one of the top five diagnosis groups, MH visits at IPU hospitals were more likely to result in either a hospital admission or a transfer to an inpatient unit. Our findings have several implications for strategic planning in tertiary children’s hospitals.
Findings from this study confirm continued growth in MH-related ED visits using a large national dataset of tertiary care children’s hospitals across the US. While multiple studies have previously documented the dramatic rise in pediatric ED visits for MH conditions overall,2–7 the only other study that stratified growth by individual MH condition was limited to data through 2012.3 In addition, for this study time period, depressive disorders, suicide or self-injury, and trauma and stressor-related disorders were the primary drivers of the substantial cumulative rise in ED MH visits in children’s hospitals. MH ED visits were also more likely among adolescents and females. Together, these findings are consistent with prior studies that found increases in ED visits specifically for suicide or self-injury in US youth,3,10,11,24,25 and an increase in prevalence of major depression, particularly among female adolescents.26,27 Priority populations for quality improvement interventions in the pediatric ED include youth with major depression or acute suicidal ideation or self-harm. Interventions to improve care may include development of standardized approaches to ED-based suicide and major depression screening, child psychiatric emergency care, and clinician decision support tools for ED disposition and child safety monitoring.
For hospitals considering opening an IPU, our results provide valuable information on the influence an inpatient unit has on patient disposition from the ED. We found that patients visiting IPU hospitals were more likely to be admitted and thus less likely to be transferred to another facility. A previous study by Sheridan et al. found that in two tertiary pediatric EDs in close proximity, patients with ED visits for MH conditions in a hospital with an IPU were more likely to be hospitalized compared to patients visiting a hospital with no IPU.16 Our study adds to these findings by including data from 35 tertiary children’s hospitals across the US, and by comparing transfer rates at IPU vs. non-IPU hospitals. Our findings also highlight important differences in combined admission and transfer rates by specific diagnosis group. We found a higher combined admission/transfer rate for visits for depressive disorders at IPU vs. non-IPU hospitals. In contrast, we found a lower combined admission/transfer rate for visits for suicide or self-injury at IPU vs. non-IPU hospitals. A possible explanation for these results include improved access to on-site MH providers at IPU hospitals including psychiatrists, psychologists and social workers who can assist with ED disposition planning through safety assessment and plans for follow-up care. For patients visiting for suicide or self-injury, the lower combined admission/transfer rate at IPU hospitals may indicate increased comfort with accurately assessing the risk for ongoing self-harm due to access to an on-site multidisciplinary MH team, allowing for more discharges.
Less than half of the hospitals in our cohort had an IPU during the study period indicating a national lack of access to inpatient psychiatric care within tertiary children’s hospitals. In addition, at IPU hospitals nearly 1 in 10 patients still required transfer for inpatient psychiatric care. While we do not know the exact numbers of inpatient beds available in IPU hospitals, these results suggest that even hospitals with an IPU cannot accommodate the full demand for admissions due to limited inpatient bed capacity.28 These findings are consistent with a national shortage of inpatient psychiatric beds which is associated with prolonged ED stays and often results in discharge after long ED stays due to reduction in the MH crisis or frustration with waiting for an available bed.29 There is limited research on the impact of discharge after long ED stays in pediatric patients, but ED revisit rates are higher for adult patients who had a psychiatric bed request in place prior to being discharged.29 More than half of the children with a MH visit were discharged from the ED, but the proportion was lower in IPU hospitals. Future research should examine the clinical severity and complexity of youth discharged after a MH ED visit to estimate the extent of unmet need for inpatient psychiatric care.
Adequate access to timely inpatient psychiatric care is crucial for those experiencing a MH crisis, and our results show variation in access by presence of an IPU. While it may be expected that increased admission rates at IPU hospitals would correspond with lower transfer rates, these results have important implications for quality of care and overall healthcare costs. A transfer can result in discontinuity of care, while also resulting in the boarding of patients in the ED, keeping labor-intensive patients under the watch of providers while occupying beds that could be used by other patients. While adding an IPU is not a feasible option for all hospitals, those that have the capacity could justify the addition of inpatient beds to not only improve overall patient experience by providing more timely access to MH care, but also to potentially reduce costs due to a reduction in expensive transfers and avoidance of unnecessary hospitalizations. There are multiple other ways to further integrate MH care into EDs and hospitals, including the use of training programs to help increase clinician skill and comfort level, investment in MH and behavior specialists to increase the capacity for evaluation and treatment initiation, and low cost options including telemedicine-based approaches or innovative smartphone applications.30
This study has several limitations. We used an administrative dataset and were therefore limited to the information recorded by hospitals and submitted to PHIS. The diagnoses recorded may not have identified the correct MH condition, and there are likely differences in coding practices across sites that could have impacted the primary diagnosis given in the ED. While all ED MH visits were categorized into MH diagnosis groups, 28% of patients had a MH diagnosis code that was not categorized into one of our main 8 MH diagnosis groups. Our analysis was at the level of ED visits and not individual patients as our study objectives focused on hospital systems. We only focused on primary diagnosis, and did not take into account patients with secondary MH diagnoses or patients with undiagnosed MH conditions since comorbid MH diagnoses are rarely coded in the ED setting. Since we categorized MH condition using the primary diagnosis, we may have underestimated the rates of ED visits for depressive disorders and suicide or self-harm, such as for patients with a primary diagnosis of a trauma-related injury or overdose related to suicide or self-harm if the MH diagnosis was not coded by the clinical team. There were no standardized criteria to indicate a child’s need for transfer or hospitalization, and we do not know the ultimate disposition of patients after they were transferred. Our rates of transfer may be underestimated as we only recorded transfers directly from the ED, while not accounting for transfers occurring after brief admissions to the hospital. A considerable proportion of patients were admitted at non-IPU hospitals (22.5%), likely due to an immediate need for stabilization; 21.5% of patients were ultimately transferred, likely due to a lack of onsite specialized inpatient psychiatric treatment programs. When examining hospitalizations we could not differentiate between admission to a medical or psychiatric bed. While billing data allowed us to determine the presence or absence of an IPU, we were not able to determine bed size or capacity of these units. Our study sample was limited to tertiary care children’s hospitals, and thus, our findings may not be generalizable to non-children’s hospitals. In addition, we only included hospitals that contributed billing data to PHIS continuously throughout the study period, and our study sample may not be generalizable to all tertiary care children’s hospitals. There were some coding changes during the transition from ICD-9 to ICD-10 that could have impacted our results, but the consistency of trends over time in our analysis, along with a recent study concluding similar validity in recording clinical condition information,31 argues for validity of the ICD coding classification scheme.
Conclusion
The rise in MH ED visits substantially exceeded non-MH visits in pediatric patients from 2012 to 2016. Our findings show that the dramatic increase is primarily driven by youth requiring acute care for depressive disorders and suicide or self-injury, underscoring the need for hospitals and EDs to identify strategies to address these priority populations. We found significant differences in hospitalization and transfer rates depending on presence of an IPU, which may indicate improved access to inpatient psychiatric care and greater opportunity to coordinate disposition planning with an on-site multidisciplinary MH team. More research will be needed to fully understand the benefits a hospital IPU provides for patients and health systems. Specifically, future studies should examine whether the presence of an IPU leads to more timely and effective care of acute MH conditions as well as reduced costs through reduction of repeat ED visits or psychiatric hospitalizations.
What’s New.
The dramatic rise in pediatric mental health emergency department visits is being primarily driven by visits with a primary diagnosis of depression or suicide or self-injury, and there are significant differences in patient hospitalization and transfer rates depending on presence of an inpatient psychiatric unit.
Acknowledgments
Funding Source: No funding was secured for this study.
Dr. Doupnik was supported by grant K23MH115162 from the National Institute of Mental Health, and sponsor had no role in study design, data collection, analysis or interpretation, writing of the report, or decision to submit the report for publication.
Footnotes
Potential Conflict of Interest and Corporate Sponsors: None
References
- 1.American Academy of Pediatrics CoPEM, American College of Emergency P, Pediatric C. Care of children in the emergency department: guidelines for preparedness. Pediatrics. 2001;107(4):777–781. [DOI] [PubMed] [Google Scholar]
- 2.Rogers SC, Mulvey CH, Divietro S, Sturm J. Escalating Mental Health Care in Pediatric Emergency Departments. Clin Pediatr (Phila). 2017;56(5):488–491. [DOI] [PubMed] [Google Scholar]
- 3.Mapelli E, Black T, Doan Q. Trends in Pediatric Emergency Department Utilization for Mental Health-Related Visits. J Pediatr. 2015;167(4):905–910. [DOI] [PubMed] [Google Scholar]
- 4.Sheridan DC, Spiro DM, Fu R, et al. Mental Health Utilization in a Pediatric Emergency Department. Pediatr Emerg Care. 2015;31(8):555–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simon AE, Schoendorf KC. Emergency Department Visits for Mental Health Conditions Among US Children, 2001-2011. Clin Pediatr (Phila). 2014;53(14):1359–1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nadler A, Avner D, Khine H, Avner JR, Fein DM. Rising Clinical Burden of Psychiatric Visits on the Pediatric Emergency Department. Pediatr Emerg Care. 2018. [DOI] [PubMed] [Google Scholar]
- 7.Pittsenbarger ZE, Mannix R. Trends in pediatric visits to the emergency department for psychiatric illnesses. Acad Emerg Med. 2014;21(1):25–30. [DOI] [PubMed] [Google Scholar]
- 8.Dolan MA, Fein JA. Pediatric and adolescent mental health emergencies in the emergency medical services system. Pediatrics. 2011;127(5):e1356–1366. [DOI] [PubMed] [Google Scholar]
- 9.Larkin GL, Beautrais AL, Spirito A, Kirrane BM, Lippmann MJ, Milzman DP. Mental health and emergency medicine: a research agenda. Acad Emerg Med. 2009;16(11):1110–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Plemmons G, Hall M, Doupnik S, et al. Hospitalization for Suicide Ideation or Attempt: 2008-2015. Pediatrics. 2018;141(6). [DOI] [PubMed] [Google Scholar]
- 11.Burstein B, Agostino H, Greenfield B. Suicidal Attempts and Ideation Among Children and Adolescents in US Emergency Departments, 2007–2015. JAMA Pediatr. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newton AS, Ali S, Johnson DW, et al. Who comes back? Characteristics and predictors of return to emergency department services for pediatric mental health care. Acad Emerg Med. 2010;17(2):177–186. [DOI] [PubMed] [Google Scholar]
- 13.Mahajan P, Alpern ER, Grupp-Phelan J, et al. Epidemiology of psychiatric-related visits to emergency departments in a multicenter collaborative research pediatric network. Pediatr Emerg Care. 2009;25(11):715–720. [DOI] [PubMed] [Google Scholar]
- 14.Case SD, Case BG, Olfson M, Linakis JG, Laska EM. Length of stay of pediatric mental health emergency department visits in the United States. J Am Acad Child Adolesc Psychiatry. 2011;50(11):1110–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chun TH, Mace SE, Katz ER, et al. Evaluation and Management of Children and Adolescents With Acute Mental Health or Behavioral Problems. Part I: Common Clinical Challenges of Patients With Mental Health and/or Behavioral Emergencies. Pediatrics. 2016;138(3). [DOI] [PubMed] [Google Scholar]
- 16.Sheridan DC, Johnson KP, Fu R, Spiro DM, Hansen ML. Impact of an Inpatient Psychiatric Unit on Pediatric Emergency Mental Health Care. Pediatr Emerg Care. 2017;33(1):1–4. [DOI] [PubMed] [Google Scholar]
- 17.Bastiampillai T, Sharfstein SS, Allison S. Increase in US Suicide Rates and the Critical Decline in Psychiatric Beds. JAMA. 2016;316(24):2591–2592. [DOI] [PubMed] [Google Scholar]
- 18.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA. 2011;305(7):682–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Doupnik SK, Lawlor J, Zima BT, et al. Mental Health Conditions and Medical and Surgical Hospital Utilization. Pediatrics. 2016;138(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zima BT, Rodean J, Hall M, Bardach NS, Coker TR, Berry JG. Psychiatric Disorders and Trends in Resource Use in Pediatric Hospitals. Pediatrics. 2016;138(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Callahan ST, Fuchs DC, Shelton RC, et al. Identifying suicidal behavior among adolescents using administrative claims data. Pharmacoepidemiol Drug Saf. 2013;22(7):769–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berry JG, Hall M, Hall DE, et al. Inpatient growth and resource use in 28 children’s hospitals: a longitudinal, multi-institutional study. JAMA Pediatr. 2013;167(2):170–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mercado MC, Holland K, Leemis RW, Stone DM, Wang J. Trends in Emergency Department Visits for Nonfatal Self-inflicted Injuries Among Youth Aged 10 to 24 Years in the United States, 2001-2015. JAMA. 2017;318(19):1931–1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cutler GJ, Flood A, Dreyfus J, Ortega HW, Kharbanda AB. Emergency Department Visits for Self-Inflicted Injuries in Adolescents. Pediatrics. 2015;136(1):28–34. [DOI] [PubMed] [Google Scholar]
- 26.Weiss AJ, Barrett ML, Heslin KC, Stocks C. Trends in Emergency Department Visits Involving Mental and Substance Use Disorders, 2006-2013: Statistical Brief #216. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD)2006. [Google Scholar]
- 27.Mojtabai R, Olfson M, Han B. National Trends in the Prevalence and Treatment of Depression in Adolescents and Young Adults. Pediatrics. 2016;138(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Conrad HB, Hollenbach KA, Gehlbach DL, Ferran KL, Barham TA, Carstairs KL. The Impact of Behavioral Health Patients on a Pediatric Emergency Department’s Length of Stay and Left Without Being Seen. Pediatr Emerg Care. 2018;34(8):584–587. [DOI] [PubMed] [Google Scholar]
- 29.Lee S, Harland KK, Swanson MB, et al. Safety of reassessment-and-release practice for mental health patients boarded in the emergency department. Am J Emerg Med. 2018;36(11):1967–1974. [DOI] [PubMed] [Google Scholar]
- 30.Doupnik SK, Esposito J, Lavelle J. Beyond Mental Health Crisis Stabilization in Emergency Departments and Acute Care Hospitals. Pediatrics. 2018;141(5). [DOI] [PubMed] [Google Scholar]
- 31.Quan H, Li B, Saunders LD, et al. Assessing validity of ICD-9-CM and ICD-10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43(4):1424–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]


