Abstract
Antibiotic resistance in Streptococcus pneumoniae (pneumococcus), the main pathogen responsible for community-acquired pneumonia (CAP), meningitis, bacteremia, and otitis media, is a major concern for clinicians. This pathogen is associated with high rates of morbidity and mortality, especially among children under 2 years old, immunocompromised persons, and the elderly population. The major anti-pneumococcus agents are β-lactams and macrolides, with fluoroquinolones ranking third. The emergence of antibiotic-resistant pneumococcus due to overuse of antibiotics is a global concern. While the discovery of novel classes of antibiotics for the pneumococcus is at a standstill, significant progress in reducing the problem of resistance is associated with antibacterial vaccines. Nevertheless, the World Health Organization recently considered drug-resistant S. pneumoniae as ranking among the 12 bacteria, for which there is an urgent need for new treatments. A challenge is to slow the evolution of new strains that are resistant to the vaccines.
Introduction
Antibiotic resistance is a direct result of antibiotic consumption [1, 2]. In the United States, it is estimated that antibiotic resistance is responsible for more than 2 million infections and 23,000 deaths each year, with a direct cost of $20 billion and additional productivity losses of $35 billion [3, 4]. Data from Europe showed that approximately 25,000 deaths are attributable to antibiotic-resistant infections, with a related cost of $1.5 billion annually [5]. The use of antibiotics in primary care is high; the most frequent indications for their use are respiratory tract infections [6].
Streptococcus pneumoniae (pneumococcus) is the leading cause of community-acquired pneumonia and is considered to be a major cause of death of children under 5 years old worldwide. In a recent report on global antibiotic resistance, published by the World Health Organization (WHO) in 2014, pneumococcus was considered to be one of the nine bacteria of international concern [7]. Other infections caused by pneumococcus include bacteremia , otitis media, and meningitis. In bacterial meningitis, pneumococcus is associated with mortality rates ranging from 16% to 37%. About 30–50% of adult survivors present permanent residual symptoms [8, 9]. The study by Van Boeckel et al. [10], regarding global antibiotic consumption from 2000 to 2010, reported that it grew by more than 30%, from approximately 50 billion to 70 billion standard units. Penicillins, cephalosporins, and macrolides were the three most consumed antibiotics in 2010. The three countries that consumed the most antibiotics in 2010 were India with 13 billion standard units, China with 10 billion, and the United States with 7 billion standard units (a standard unit is the number of doses sold; the IMS Health database identifies a dose as a pill, capsule, or ampoule).
Resistance of pneumococcus against ß-lactams and macrolides is a major concern worldwide. For example, in Southern European countries, the prevalence of this resistance may be above 20% [11, 12]. The increased utilization of antibiotics, the dissemination of several resistant clones, the ability of pneumococcus to undergo serotype replacement and capsular switching, and the horizontal transmission of antibiotic resistance genes make this pathogen very difficult to control. This chapter summarizes currently available information regarding pneumococcal antibiotic resistance.
Basis of Antimicrobial Resistance in Streptococcus pneumoniae
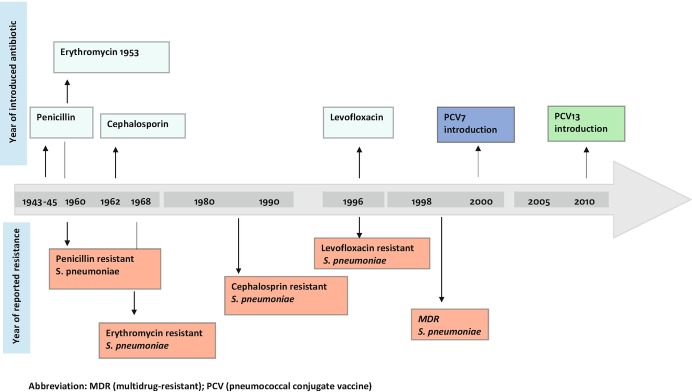
The nasopharyngeal carriage rate of pneumococcus is higher in children, mainly during the first years of life (nasopharyngeal carriage rates range from 20% to 50% in healthy children). In contrast, with the healthy adult population, nasopharyngeal carriage rates range from 5% to 30%. Transmission of pneumococcus from children to household contacts or adults is the principal cause of nasopharyngeal carriage and the spread of antibiotic-resistant clones. Pneumococcus undergoes genetic transformation and can acquire DNA from other streptococci; during asymptomatic nasopharyngeal carriage , selection of resistant pneumococcus occurs especially in children, because they carry pneumococcus more often and for longer periods. Moreover, children are more frequently exposed to antibiotics. Interestingly, the use of fluoroquinolones in children is limited, because in animal models using young animals, development of articular cartilage damage in weight-bearing joints has been described [13, 14]. This adverse effect may explain why the rate of pneumococcus resistance to fluoroquinolones remains low. A direct correlation has been reported between the use of the fluoroquinolone antibiotics and prevalence of fluoroquinolone resistance in pneumococcus [15–18]. Table 2.1 describes the principal mechanisms of resistance to this antibiotic class by pneumococcus; Fig. 2.1 shows the timeline of antimicrobial resistance of pneumococcus.
Table 2.1.
Basis of antimicrobial resistance in Streptococcus pneumoniae
| Antibiotic | Effect | Mechanism resistance | Risk factors |
|---|---|---|---|
| ß-lactam | Inhibit the final steps of peptidoglycan synthesis (cell wall) by binding to high-molecular-weight penicillin-binding proteins (PBPs) | Alteration of the cell wall PBP, resulting in decreased affinity for penicillin | Previous antibiotic use of ß-lactam antibiotics in the last 3–6 months |
| Prior hospitalization in the last 3 months | |||
| Attendance in a day-care center | |||
| Residence in long-term care facilities | |||
| Chronic pulmonary disease mainly chronic obstructive pulmonary disease (COPD) | |||
| Human immunodeficiency virus (HIV) infection | |||
| Macrolides | Inhibit protein synthesis by binding 23S ribosomal target sites in bacteria |
Target site (ribosomal) alteration by an enzyme that methylates 23S rRNA subunits and is encoded by the ermB (erythromycin-resistance methylase) gene: high level of macrolide resistance and complete cross-resistance to macrolide lincosamide streptogramin B type Active efflux pumps encoded by the mefE or mefA (macrolid efflux) gene: low-level of resistance only to macrolides |
Previous hospital admission |
| Resistance to penicillin | |||
| Previous use of macrolides | |||
| Recurrent otitis media | |||
| Cases related to serotypes such serotype 6A, 6B, 14, 23F, 19F | |||
| Attendance in day-care centers | |||
| Fluoroquinolones | Inhibit DNA synthesis by interacting with intracellular drug targets, DNA gyrase, and topoisomerase IV | Spontaneous point mutations in the quinolone resistance-determining region (QRDR) | Prior use of fluoroquinolones |
| Chronic obstructive pulmonary disease (COPD) | |||
| Residence in a long-term center | |||
| Elderly persons | |||
| Cerebrovascular disease |
Fig. 2.1.
Timeline of antibiotic resistance of Streptococcus pneumoniae. Abbreviation: MDR multidrug-resistant, PCV pneumococcal conjugate vaccine
Penicillin and ß-Lactam-Resistant Streptococcus pneumoniae
β-lactam antibiotics include penicillins, cephalosporins, and carbapenems. These compounds inhibit the final steps of peptidoglycan (cell wall) synthesis by binding to high-molecular-weight penicillin-binding proteins (PBPs). These antibiotics have a broad spectrum of activity against Gram-positive and Gram-negative bacteria. β-lactam antibiotics are considered to be time-dependent killers, meaning that increasing concentration significantly above the minimal inhibitory concentration (MIC) does not increase killing. The compounds have efficacy when concentrations are approximately four times the MIC of the microorganism. To determine the efficacy of β-lactam antibiotics , the preferred pharmacodynamic parameter is time (T) > MIC. For the majority of β-lactams, effectiveness is achieved at T > MIC for more than 40–50% of the dosing interval [19].
Amino acid alterations of the cell wall PBP result in decreased affinity for penicillin, which is the main mechanism of penicillin resistance. Several PBPs have been identified, including 1a, 1b, 2x, 2a, 2b, and 3. Alterations to the properties of PBPs are brought about by transfer of portions of the genes encoding the PBPs from other streptococcal species, resulting in mosaic genes [20].
The Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) define penicillin resistance of pneumococcus via empirical breakpoint determination [21]. Breakpoints established by the CLSI in 2012 for pneumococci defined penicillin resistance as:
Infections other than meningitis: susceptible < 2 μg/ml, intermediate < 4 μg/ml, and resistant ≥ 8 μg/ml
: susceptible ≤ 0.06 μg/ml, intermediate ≥ 0.12 μg/ml, and resistant ≥ 2 μg/ml
The breakpoints for penicillin susceptibility are based on three criteria: microbiological data, pharmacokinetic/pharmacodynamics of β-lactam antibiotics, and clinical outcome of pneumococcal infections. In a patient treated with a dose of intravenous penicillin, the levels achieved in the lung will be 100 times greater than those reached in the brain. Thus, use of low concentrations of β-lactam for pneumococcal infections, such as otitis media or meningitis, could lead to treatment failure. In contrast, with pulmonary infections the levels of β-lactam reached are generally sufficient to clear infection. Therefore, treating the same pathogen will require different doses of a given β-lactam depending on the site of infection. Likewise, we must considerer pneumococcal resistance in different sites of infection differently, and breakpoints for resistance will be different.
Macrolide Resistance in Streptococcus pneumoniae
Macrolides inhibit bacterial protein synthesis by binding to the 23S rRNA component of the 50S ribosomal subunit in bacteria. There are two main mechanisms of macrolide resistance in pneumococcus. One involves target-site (ribosomal) alteration by an enzyme that methylates 23S rRNA, an enzyme that is encoded by the ermB (erythromycin-resistance methylase) gene. The resistance phenotype is called MLSB (macrolide, lincosamide, streptogramin B type) and is responsible for a high level of macrolide resistance. In a low proportion of cases, ermB gene variation that modifies the binding site for macrolides and lincosamides confers complete cross-resistance to clindamycin [22].
The second mechanism of resistance involves active efflux pumps encoded by the mefE or mefA (macrolide efflux) genes. These mutations result in low-level resistance to macrolides but not to the other two agents. The mefA gene is predominant in Europe, whereas mefB gene predominates in North America.
The relative frequency of the two macrolide resistance mechanisms varies by geographic region [23–36] (Table 2.2): in European countries, approximately 90% of the isolates of pneumococcus presented the MLSB phenotype, which is associated with high levels of macrolide resistance, whereas in North America between 50% and 65% of the resistant pneumococcus isolates contained efflux mutations that were associated with lower levels of macrolide resistance [12]. In Asian countries, strains that showed both mechanism of resistance are a major concern, with between 12% and 40% of the resistant isolates displaying both mechanisms [31, 37–40]. In South American countries, isolates reporting both mechanisms vary between 4% and 20% [34, 41]. Worldwide resistance to macrolides in pneumococcus has increased recently and is associated with the extensive global use of macrolides, principally for community-acquired respiratory tract infections.
Table 2.2.
Worldwide genotype distribution of macrolide resistance in Streptococcus pneumoniae
| Country/year of study | No of isolates tested | % genotype distribution | Reference |
|---|---|---|---|
| Europe | |||
| Turkey – 2008–2009 | 80 |
44% ermB 11% mefA 44% ermB + mefA |
Sirekbasan et al. [23] |
| Spain – 1999–2007 | 187 |
90% ermB 9% mefE 1% mefA |
Calatayud et al. [24] |
| Greece – 2005–2009 | 1105 (carriers) |
29% ermB 24% ermB + mefE 42% mefE 5% mefA |
Grivea et al. [25] |
| Belgium – 2007–2009 | 249 |
90% ermB 2% mefE 3% ermB + mefE |
Lismond et al. [26] |
| North America | |||
| Canada– 1998–2004 | 865 |
47% mefA 43% ermB 6% ermB + mefA |
Wierzbowsk et al. [27] |
| USA – 2007 | 4535 |
18% ermB 62% mef (A/E) gene 15% mef (A/E) + ermB |
Hawkins et al. [28] |
| Asia | |||
| Lebanon − 2010–2015 | 132 |
38% ermB 29% mef (A/E) 31% mef (A/E) + ermB |
El Ashkar et al. [29] |
| Japan – 2013–2014 | 960 |
76% ermB 32% mef (A/E) 11% mef (A/E) + ermB |
Kawaguchiya et al. [30] |
| Iran | 186 |
44% ermB 16% mef (A/E) 40% mef (A/E) + ermB |
Azadegan et al. [31] |
| South Korea – 2008–2009 | 2184 |
49% ermB 20% mefA 30% mefA + ermB |
Kim et al. [32] |
| South America | |||
| Colombia – 1994–2011 | 225 |
98% ermB 2% ermB + mef E |
Ramos et al. [33] |
| Argentina – 2009–2010 | 126 |
77% mefA 19% ermB 4% mefA + ermB |
Reijtman et al. [34] |
| Africa | |||
| Morocco – 2007–2014 | 655 |
90% ermB 6% mef E 35 ermB + mefE |
Diawara et al. [35] |
| Tunisia – 1998–2004 | 100 |
88% ermB 12% mefA |
Rachdi et al. [36] |
Fluoroquinolone Resistance in Streptococcus pneumoniae
Fluoroquinolones inhibit DNA synthesis by forming drug-enzyme-DNA complexes with DNA gyrase and topoisomerase IV. The main mechanism of resistance to fluoroquinolones is mediated by amino acid substitutions in these two essential enzymes. As with other bacteria, resistant pneumococcus exhibits spontaneous point mutations in a region of GyrA (gyrase) and ParC (topoisomerase IV) called the quinolone resistance-determining region (QRDR). Some pneumococci may also exhibit an efflux-mediated mechanism, although the clinical significance is unclear. The presence of dual mechanisms of resistance has been reported in strains having high levels of resistance, often from cases of treatment failure [12, 42, 43]. In some cases multiple mutations in the target proteins accumulate [44], which supports the idea that repeated antimicrobial challenge gradually erodes the effectiveness of fluoroquinolones.
Resistance to Other Antibiotics
Currently, the European Respiratory Society (ERS)/European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines recommend the use of tetracyclines (broad-spectrum bacteriostatic antibiotics that act by binding to the 30S ribosomal subunit and thereby inhibit bacterial protein synthesis) as a first choice for treatment of lower respiratory infections [45]. On the other hand, the American Thoracic Society (ATS)/Infectious Disease Society of America (IDSA) [46] recommends doxycycline for healthy patients with pneumococcal community-acquired pneumonia with low risk of drug-resistant pneumococcus and for patients with penicillin allergy [46].
The ribosomal protection protein (RRP) , which binds to the ribosome and forces the drug from its binding site, is the main resistance mechanism of pneumococcus to tetracycline and doxycycline. This form of resistance is mediated by an alteration in the tetM gene. In 2012 a study by Dönhöfer et al. showed that TetM can directly remove and release tetracycline from the bacterial ribosome by an interaction between domain IV of the 16S rRNA and the tetracycline binding site [47].
Due to the increase in resistance of pneumococcus to several antibiotics over the last decade and several reported cases of treatment failure, vancomycin, a glycopeptide antibiotic that acts by inhibiting proper cell wall synthesis, was added to the standard antibiotic treatment for pneumococcal meningitis. There are several reports about treatment failure with vancomycin due to the emergence of vancomycin-tolerant pneumococcus. However, there is no report of vancomycin-resistant pneumococcus.
Tolerant pneumococcus survives but does not replicate during therapy with antibiotics. When antibiotic therapy is finished, pneumococci are able to resume growth. This phenomenon is associated with a reduction of autolysin activity, which is part of an endogenous bacterial cell-death pathway [48].
Multidrug-Resistant (MDR) Streptococcus pneumoniae
It is estimated that the worldwide prevalence of multidrug-resistant (MDR) S. pneumoniae is high, ranging from 36% in Asia to 15% in Europe [12, 49], although the prevalence is geographically variable. Multidrug resistance in pneumococcus is defined as resistance to three or more antibiotic classes. Pneumococcus MDR generally involves reduced susceptibility to β-lactams, macrolides, tetracyclines, and sulfonamides; resistance to quinolones in MDR pneumococcus is less frequent.
The majority of MDR strains of pneumococcus are derived from resistant genetic clones, with a few clones dominating the pneumococcus isolates on a worldwide basis [49]. Data from European studies show that the MDR phenotype is most frequent among serotypes 1, 14, 15A, 19A, 19F, and 23F [50]. In the United States and Canada, however, the most frequent serotypes associated with MDR pneumococcus are 15A, 15B, 15C, 22F, 23A, 33F, and 35B [51–54]. Studies from Asian countries report that 11A, 15A, 19A, and 19F are the serotypes most frequently associated with MDR pneumococcus [53, 55, 56]. In African countries, 19A and 19F are the most frequently associated with MDR pneumococcus [57]. Collectively these data indicate that the spread of MDR pneumococcus globally has high variability among countries. The introduction of conjugate pneumococcal vaccines contributed to the large reduction of the burden of pneumococcal disease and the reduction of antimicrobial resistance in S. pneumoniae . Nevertheless, the emergence of non-vaccine serotypes that show multidrug resistance is a major concern.
Risk Factors for Infection by Drug-Resistant Pneumococcus
Several studies identify factors associated with an increased risk of infection by pneumococcus resistant to the most frequently used antibiotics. The three main factors are host factors (age, comorbidities), environmental factors (geographic regions with high population density and proximity to high-resistance regions, day-care centers with children, long-term nursing facilities with elderly persons), and factors related to the use of antibiotics (previous antibiotic therapy, duration of antibiotic therapy).
Risk Factors Related to Penicillin Resistance
The use of a β-lactam antibiotic in the previous 3–6 months is the main risk factor associated with penicillin-resistant pneumococcal infection [12, 21, 58–60]. A study by Ruhe et al. [61] regarding the duration of previous antibiotic treatment and its association with penicillin-resistant bacteremic infection revealed that the risk depends on the class of prior antibiotic exposure and the duration of therapy. The study analyzed 303 patients with pneumococcal bacteremia. In 98 (32%) cases of bacteremia caused by penicillin-non-susceptible S. pneumoniae, statistical analysis showed that the use of β-lactams, sulfonamides, and macrolides within the last 1–6 months before presentation was associated with penicillin-non-susceptible S. pneumoniae bacteremia (p < 0.05). In a second study with the same bacteremic population, Ruhe et al. [62] identified 33 (11%) cases of bacteremia caused by high-level resistant S. pneumoniae. In these cases, three risk factors for high-level penicillin-resistant pneumococcal infection were identified: β-lactam antibiotic use in the previous 6 months, previous residence in a risk area (defined as stays in day-care facilities, prisons, homeless shelters, nursing homes, or other long-term care facilities), and respiratory tract infection in the previous year.
Age extremes (<5 years or > 65 years) are a recognized risk factor for penicillin-resistant pneumococcal infections [12, 17, 63]. As pointed out above, nasopharyngeal carriage of pneumococcus in healthy children ranges from 20% to 50%, and in the healthy adult population, nasopharyngeal carriage rates range from 5% to 30% [64, 65]. Consequently, it is not difficult to understand why several studies have shown that day-care centers are a risk factor for colonization and infection of children due to penicillin-resistant pneumococcus [66–68]. Similarly, institutionalized adults, especially those older than 65 years of age , have increased risk for penicillin-resistant pneumococcal infections [69]. Moreover, the presence of specific comorbidities, such as human immunodeficiency virus (HIV) and chronic pulmonary disease, especially chronic obstructive pulmonary disease (COPD), is a recognized risk factor for penicillin-resistant pneumococcal infection [58].
Several studies have addressed the association between antibiotic consumption and resistance selection . A study by van Eldere et al. [70], concerning the impact of antibiotic usage in ambulatory patients in Belgium, involved 14,448 Streptococcus pneumoniae isolates collected between 1994 and 2004. This work showed a modest relationship between consumption and resistance; additional factors were high population density and proximity to high-resistance regions, particularly for the development of multiple resistances in pneumococcus. In this Belgian population, the highest levels of resistance were to erythromycin, followed by resistance to tetracycline and penicillin; the highest prevalence of co-resistance to two antibiotics was for erythromycin-tetracycline.
In 2001 the prevalence of non-susceptibility to erythromycin in the Belgium study peaked at 36.7% and stayed mostly stable until 2004. Prevalence of non-susceptibility to tetracycline reached its highest level (31.7%) in 2000; penicillin non-susceptibility hit 17.7% in 2000 and declined to 11.6% in 2004. The prevalence of co-resistance to erythromycin-tetracycline was 26.7% in the period 2002–2003 and decreased slightly to 25.9% in 2004.
The overall antibiotic consumption in Belgium was 26.4 DID (daily doses per 1000 inhabitants per day) in 1995 and decreased slightly to 23.3 DID in 2004. The most frequently consumed antibiotics were broad-spectrum penicillins (9 DID in 2000 to 6.4 DID in 2004). Macrolides showed a similar pattern (6 DID in 2000 to 4.5 DID in 2004) as did cephalosporins (4.7 DID in 2000 to 3.7 DID in 2004). Tetracycline was the second most prescribed class in 1995, but usage declined in 2004 to 1.9 DID. Overall, consumption and resistance were roughly parallel.
Another study concerned antimicrobial drug use in ambulatory care and resistance trends in Europe [71] for 21 countries during the period 2000–2005. The work showed that variation in consumption coincided with the prevalence of resistance at the country level [71]. Antimicrobial drug use decreased (>15%) in Bulgaria, Czech Republic, France, and Germany, but it increased (>15%) in Croatia, Denmark, Greece, and Ireland. The most widely used antibiotics were penicillins (including broad-spectrum penicillins). Macrolides were the second most widely used category; the third consisted of cephalosporins, monobactams, and carbapenems. Fluoroquinolones occupied the fourth position. Four (France, Luxemburg, Belgium, and Portugal) of the six countries reporting the highest antimicrobial usage (Greece, France, Luxembourg, Portugal, Croatia, and Belgium) also reported the highest resistance proportions.
An interesting, small, case-controlled study about penicillin dust exposure with pharmaceutical workers in Tehran (Iran) reported that the workers in the penicillin production line carried a greater percentage of resistant pneumococcus [72]. The study included 60 cases (workers on a penicillin production line) and 60 controls (workers in food production), and data were obtained via survey, air sampling, and throat swab. In the penicillin production line arm of the study, the mean overall concentrations of penicillin dust were 6.6 mg/m3, while it was 4.3 mg/m3 in the food production line (p = 0.001). S. pneumoniae was detected in 45% (27) individuals in the dust-exposed group, 92.6% of which showed penicillin resistance. In the control group, S. pneumoniae was detected in 35% of the subjects, while 71.4% of the S. pneumoniae-positive cases were drug resistant (p = 0.014).
Risk Factors Related to Macrolide Resistance
Recent therapy by macrolides is the main risk factor for macrolide-resistant nasal colonization and pneumococcal infection [1, 12, 73, 74]. The study by Dias et al. [75], which evaluated the role of antimicrobial and vaccine use in the trends of resistance to penicillin and erythromycin in Portugal from 1994 to 2004, found that the use of macrolides was the main factor associated with an increase of penicillin and erythromycin non-susceptible isolates among adults (p < 0.01) and erythromycin non-susceptible isolates among children (p = 0.006). The study also suggested that the heptavalent vaccine is failing to reduce antimicrobial resistance, possibly due to the increased consumption of azithromycin (p = 0.04). Other works showed that there is an increased risk of macrolide-resistant infection in cases related to certain pneumococcus serotypes, in particular 6A, 6B, 11A, 14, 23F, and 19F [76, 77].
Other important risk factors are age below 5 years [78–81], attendance in a day-care center [82–84], middle ear infection [85–87], and nosocomial acquisition [26]. As with β-lactams, there is strong evidence correlating the prevalence of macrolide resistance of pneumococcus and overall macrolide consumption within specific geographic areas [70, 71, 88].
Risk Factors Related to Fluoroquinolone Resistance
Previous exposure to fluoroquinolones is considered the main risk factor for fluoroquinolone resistance [89–92]. Other risk factors, reported worldwide, are COPD, nosocomial acquisition, and residence in a nursing home [43, 93, 94]. A retrospective review of cases of invasive pneumococcal infections in adults in Spain reported that residence in public shelters (OR 26.13, p = 0.002), previous hospitalization (OR 61.77, p < 0.001), human immunodeficiency virus (HIV) infection (OR 28.14, p = 0.009), and heavy smoking (OR 14.41, p = 0.016) are risk factors associated with acquiring an infection by levofloxacin-resistant pneumococci [95–97].
Risk Factors Related to Multidrug-Resistance
The reported risk factors for multidrug-resistant pneumococcal infection are extremes in age (< 2 years and > 65 years), presence of co-morbidities, such as chronic heart disease, chronic lung disease, chronic liver disease, chronic renal disease, prior exposure, especially repeated exposure, to antibiotic therapy in the previous 3 months, and being an immunosuppressed host [21, 46, 49, 66, 98–100]. Also, infections with pneumococcal serotypes such as 6A/B, 19A, 19F, 15A, 35B, 23A, 22F, and 33F were risk factors. Of these, the strongest risk factor is repeated exposure to antibiotic therapy. Figure 2.2 provides a schematic explanation for how antibiotic resistance arises and spreads in bacterial populations. We conclude that the increasing prevalence of multidrug-resistant strains complicates treatment options for S. pneumoniae infections and in some cases resistance leads to treatment failure.
Fig. 2.2.
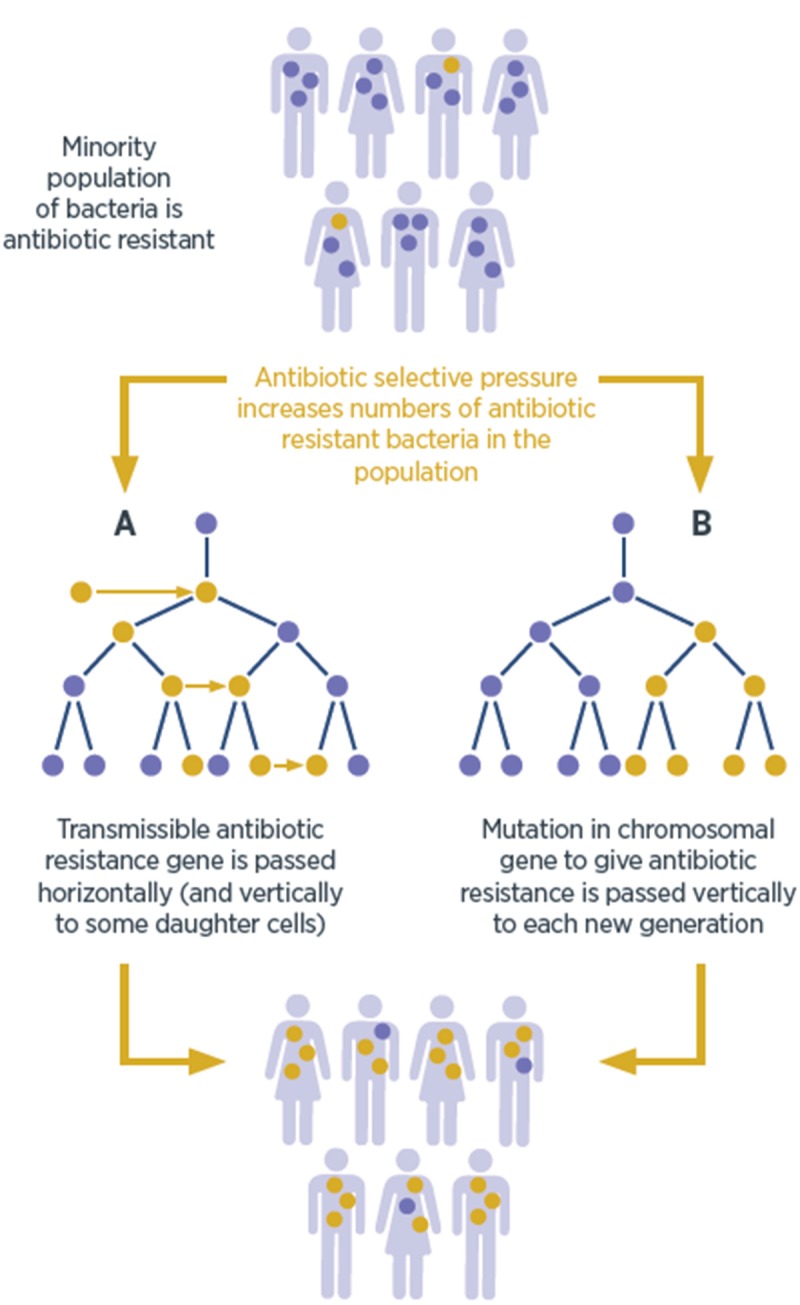
How antibiotic resistance arises and spreads in bacterial population. (Figure reproduced by the permission of the author: Laura Piddock and Victoria Wells. Longevity Bulletin: Antimicrobial Resistance, Chapter 3: How antimicrobial resistance emerges. Issue 8, May 2016)
Pneumococcal Serotypes and Antibiotic Resistance
There are 98 reported pneumococcal serotypes (capsule type); 92 were identified using the Quellung method, and the additional serotypes were identified using molecular techniques [101–103]. These serotypes are grouped into 48 serogroups based on their antigenic similarities [104]. Several epidemiological studies suggest that relationships exist between specific serotypes/serogroups and the age of the host, site of infection, comorbidities, geographic region, pneumococcal invasiveness, and disease severity [105–108]. As pointed out above, serotype differences also relate to antimicrobial resistance. The differing behavior among serotypes may reflect differences in nasopharyngeal carriage , with the highest rates in children, especially in the first year of life. As pointed out above, risk factors for nasopharyngeal carriage in children include winter season, age below 6 years, presence of younger siblings, and attendance in day-care centers. In adults, risk factors for nasopharyngeal carriage include cigarette smoking, asthma, and acute upper respiratory infection [64, 109, 110].
Colonization in children may persist for a mean of 4 months, but it is much shorter in adults, usually 2–4 weeks [16]. This long period of carriage and the frequent exposure to antibiotics by children explain why they are considered the main source of resistant strains of pneumococcus [99].
Global Resistance Trends
In recent decades there has been a global acceleration in pneumococcal antibiotic resistance that coincides with the increased use of antibiotics [2]. The report, Antibiotic Resistance Threats in the United States, 2013 [111], highlights the importance of drug-resistant pneumococcus. This report covers bacteria causing severe human infections and the antibiotics used to treat those infections. The main objective of this report was to provide an overview of the complex problem of antibiotic resistance and to encourage immediate action to keep the situation from getting worse. In this report the CDC prioritized bacteria into one of three categories: urgent threats, serious threats, and concerning threats. Drug-resistant S. pneumoniae was considered to be a serious threat. Pathogens in this category require prompt and sustained action.
Navarro et al. [112], in a 2010 surveillance report on invasive pneumococcal disease in 26 EU/EEA countries, considered isolates with MIC ≥ 0.12 mg/L as non-susceptible to penicillin (this cutoff value is for meningeal isolates and is the most widely used for surveillance studies). The highest rates of non-susceptibility to penicillin were found in Romania (42.2%), Cyprus (36.4%), and France (27.5%). The highest rates of non-susceptibility to cefotaxime were found in Romania (23.8%) and Ireland (9.3%).
The European Antimicrobial Surveillance, published in 2014, showed that of the 10,456 invasive pneumococcal disease cases reported by 28 EU/EEA countries, Romania, Spain, and Croatia showed the highest rates of non-susceptibility to penicillin (47%, 28%, and 26%, respectively, for these countries). The lowest rates were reported for Cyprus, Belgium, and the Netherlands, at 0%, 1.3%, and 2.1%, respectively [95]. We note that these surveillance data might not be strictly comparable among all countries, as the clinical breakpoints used to determine penicillin susceptibility differed, depending on guidelines used and the site of infection [113]. Nevertheless, the striking differences likely reveal key differences in antimicrobial use.
Rates of macrolide resistance range widely, from 20% to 90%. This variability is likely related to geographical differences [114–116]. A US surveillance study by Jones et al. [114] reported that 56% of isolates (from 19,000 samples analyzed) showed macrolide resistance. The 2014 European Report of antimicrobial resistance showed that Romania, Slovakia, and Malta (48%, 41%, and 38%, respectively) reported the highest rates of non-susceptibility to macrolides; the lowest rates were reported for Cyprus (0%), Latvia (4.1%), and the Netherlands (4.3%) [113]. A recent Spanish study of 643 patients with community-acquired pneumonia found that 22% had macrolide-resistant pneumococcus and 98% of those showed high-level resistance [117].
The rate of fluoroquinolone resistance of pneumococcus in the United States and Europe remains low (<1% and <3%, respectively) [12, 113, 118, 119]. One study, the Antimicrobial Resistance Surveillance in Europe [113], reported resistance data for 30 European countries from the period 2009 to 2012 for 8 bacterial pathogens as invasive isolates (blood and cerebrospinal fluid). Twenty-four European countries reported susceptibility data for fluoroquinolones in 6263 isolates (57% of all reported pneumococcus isolates). Among these, 5.2% were resistant to fluoroquinolones, and 4.4% of the fluoroquinolone-resistant isolates were also penicillin non-susceptible. Similarly, an American study by Jones et al. [114], which was a 14-year longitudinal (1998–2011) survey of S. pneumoniae that analyzed 18,911 isolates (collected from community-acquired respiratory tract infections, bacteremias, and pneumonia), reported only 1.2% non-susceptibility to fluoroquinolones (levofloxacin). In contrast, Asian countries reported higher levels, from 10% to 12%. For example, a study from Hong Kong that analyzed antimicrobial resistance data for S. pneumoniae from the period 2001–2007, using samples from respiratory tissue, wounds, blood, and other fluids, reported that 11% had reduced susceptibility to levofloxacin [32, 120]. Similarly, a prospective surveillance study of 2184 S. pneumoniae isolates collected from patients with pneumococcal infections from 60 hospitals in 11 Asian countries from 2008 to 2009 reported resistance to fluoroquinolones at 1.7%, 0.4%, 1.5%, and 13.4% for levofloxacin, moxifloxacin, gatifloxacin, and ciprofloxacin, respectively (Kim et al. [91]). Isolates from Taiwan (6.5%) and South Korea (4.6%) showed the highest rates of levofloxacin resistance.
Impact of Vaccines on Resistance
Two types of pneumococcal vaccines are currently available: the polyvalent pneumococcal polysaccharide vaccine (PPV) and the pneumococcal conjugate vaccine (PCV).
The PPV23 vaccine includes 23 purified capsular polysaccharide antigens of Streptococcus pneumoniae (1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19A, 19F, 20, 22F, 23F, and 33F); it was licensed in the United States in 1983. PPV23 induces antibodies primarily through a T-cell-independent immune response that enhances phagocytosis, thereby killing the bacterium [121]. The immune system of young children does not produce an adequate response to the polysaccharide capsule; consequently, the vaccine is not used in this age group.
The pneumococcal conjugate vaccine 7-valent ( PCV7) , which included seven pneumococcal sertotypes (4, 6B, 9V, 14, 18C, 19F, and 23F), was introduced in the United States in 2000. It is recommended for infants and young children. This vaccine is highly effective in preventing invasive disease, with percentages of efficacy of about 90%. The routine use of PCV7 has resulted not only in a tremendous reduction in invasive pneumococcal infections in children but also decreased rates of pneumococcal disease in adults.
Also, after 4 years of the introduction of PCV7 in the United States, the incidence of invasive pneumococcal disease caused by penicillin-non-susceptible S. pneumoniae and multidrug-resistant S. pneumoniae decreased. In 1999, the rate of invasive disease caused by penicillin-non-susceptible strains was 6.3 cases per 100,000 – it decreased to 2.7 cases per 100,000 in 2004. Similarly, in 1999 the rate of cases caused by strains not susceptible to multiple antibiotics was 4.1 cases per 100,000 and decreased to 1.7 cases per 100,000 in 2004 [122]. The study by Whitney et al. [123] demonstrated that the PCV7 vaccine prevents invasive disease in both healthy and chronically ill children. Despite the success of PCV7, studies have noted an increase in the incidence of invasive pneumococcal disease ( IPD) caused by non-vaccine serotypes , such as 1, 3, 5, 6A, 6C, 7F, 12F, 19A, and 22F [124]. These serotypes are related to penicillin-non-susceptible clones. The emergence of serotype 19A, which correlates with high-level penicillin and multidrug resistance, is a main concern globally [125]. This serotype presents a dual macrolide-resistance phenotype (erm B and mefA).
A new 13-valent pneumococcal polysaccharide-protein conjugate vaccine ( PCV13) was approved by the Food and Drug Administration in February 2010 for the prevention of IPD in infants and young children. PCV13 contains capsular polysaccharides from serotypes 1, 3, 4,6A, 7F, 9 V, 14, 18C, 19A, 19F, and 23F. In March 2010, the Advisory Committee for Immunization Practices (ACIP) recommended that PCV13 replace PCV7 for the vaccination of children. New studies show a similar reduction in IPD following the introduction of the PCV13 vaccine, as seen previously with the PCV7 vaccine. The study by Moore et al. [126] analyzed IPD cases (33,688 cases, of which 89% contained serotyping results) during July 2004–June 2013 and classified as being caused by the PCV13 serotypes against which PCV7 has no effect (PCV13/nonPCV7). The work found a reduction in IPD in adults associated with PCV13 introduction in children. In all adult age groups, PCV13/nonPCV7-type IPD (especially serotypes 19A and 7F) declined by 58–72%, which was comparable to that observed early after PCV7 introduction. The PCV13 led to overall reductions of IPD of 12–32% [126]. However, the phenomenon of serotype replacement, which is thought to be caused by non-vaccine serotypes (NVT) that occupy nasopharyngeal natural niches vacated after pneumococcal vaccination, is again observed with pneumococcal serotypes 11A, 15A, 23B, and 35B, the most frequent serotypes. Serotypes 15A and 23B show a high proportion of penicillin non-susceptibility [127].
Impact of Antibiotic Resistance on Outcome
The relationship between antibiotic resistance of pneumococci and clinical outcome is an important consideration for clinicians, because treatment failure related to antimicrobial resistance is not clear-cut. There are several factors that influence clinical outcome in pneumococcal infections, such as comorbidities (host factors) and invasiveness of the pneumococcus serotype (virulence of the microorganism) that contribute to poor outcome [12].
β-Lactam Resistance and Clinical Implications
The relevance of penicillin-resistant to clinical outcome in cases of pneumococcal community-acquired pneumonia (CAP) is controversial. Several studies showed that treatment failure in CAP cases does not occur when appropriate therapy and doses are used, even in those patients infected with non-susceptible strains and treated with β-lactams. For example, in 2010 a Spanish study analyzed 1041 patients with pneumococcal pneumonia in which 114 (11%) presented septic shock. The main risk factors were current smoking, chronic corticosteroid therapy, and serotype 3 pneumococcus. No difference was found regarding genotypes or patterns of antibiotic resistance between patients with or without septic shock [128]. Similarly, a study by Morgandon et al. [129], concerning severe pneumococcal pneumonia in patients admitted to intensive care units (ICU), reported that risk factors for mortality were age, male sex, and renal replacement therapy. Comorbidities, macrolide administration, concomitant bacteremia , or penicillin susceptibility did not influence outcome in these cases. These studies suggest that the outcome with community-acquired pneumococcal pneumonia is probably associated with the clinical presentation of pneumonia rather than the antibiotic resistance of the pneumococcus strain. A plausible explanation is that antibiotic concentrations achieved in the lung are usually higher than the pneumococcal MIC for more than 40–50% of the dosing interval, even with resistant strains. It will now be interesting to determine whether infection by strains having a very high level of resistance to β-lactams (MIC ≥ 16 μg/ml) correlates with clinical failure with pneumonia patients.
A different situation is seen with pneumococcal otitis media or meningitis when treated with a β-lactam – treatment failure is associated with resistant strains. The speculation is that treatment failure is due to the difficulty in obtaining sufficiently high antibiotic levels at these sites of infection. For this reason, most guidelines recommend the use of concomitant vancomycin for patients with pneumococcal meningitis until the pneumococcal MIC for a β-lactam is known [130].
Macrolide Resistance and Clinical Implications
The high rate of macrolide resistance in pneumococcus is a major concern worldwide. Reports of treatment failure in cases of otitis media , meningitis, pneumonia, and bacteremic pneumonia are in the literature [12, 131] for patients who had infections caused by macrolide-resistant strains. For this reason, monotherapy with macrolides is not recommended as an empirical treatment in any infection caused by pneumococcus.
Much less information is available for the relationship between macrolide-resistant Streptococcus pneumoniae and clinical outcome than with patients treated with β-lactams. A recent work by Cillóniz et al. [117] concerning the effect of macrolide resistance on the presentation and outcome of 643 patients with CAP reported that 22% were macrolide resistant. They found no evidence suggesting that patients hospitalized for macrolide-resistant S. pneumoniae pneumonia were more severely ill upon presentation or had worse clinical outcomes if they were treated with guideline-compliant regimens, including β-lactams, versus noncompliant regimens. A randomized prospective trial is needed to determine whether there is a relationship between macrolide resistance and poor outcome in patients with severe community-acquired pneumonia with whom β-lactam-macrolide combination therapy might improve outcome.
Fluoroquinolone Resistance and Clinical Implications
Treatment failure has been observed with patients treated with fluoroquinolones who had infections caused by fluoroquinolone-resistant strains [43, 132]. However, the global rates of fluoroquinolone resistance remain low [32, 99, 114, 118, 133], making correlation between resistance and outcome statistically marginal. In a 2013 study, Kang et al. [134] evaluated the impact of levofloxacin resistance on 136 adult patients with invasive pneumococcal disease (IPD). In this work, pneumonia was the most frequent disease (68%), followed by primary bacteremia (11%) and meningitis (11%). The rate of levofloxacin resistance in invasive pneumococcal isolates was 3.7% (5/136) of the isolates. The overall 30-day mortality rate was 26.5% (36/136). In univariate analysis, the factors associated with 30-day mortality in patients with IPD were corticosteroid use, presentation with septic shock, and development of acute respiratory distress syndrome (ARDS). The authors found an association between levofloxacin resistance and increased mortality, although statistical significance was not reached (p = 0.083). However, multivariate analysis revealed that presentation with septic shock, corticosteroid use, development of ARDS, and levofloxacin resistance were independent factors associated with 30-day mortality.
Several worldwide reports about antimicrobial resistance in pneumococcus noted that in countries where the rates of β-lactam resistance and macrolide resistance are high, the prevalence of fluoroquinolone resistance is also high [70, 114]. It may be that in those situations the consumption of fluoroquinolones is also high.
Future Considerations
Pneumococcal infections and antimicrobial resistance remain a global health problem.
Since global antibiotic consumption contributes to the emergence of antibiotic-resistant bacteria such as S. pneumoniae, one approach for reducing the problem is to reduce the need for antibiotics through better public health. Changing social norms about how and when to use antibiotics is central to preserving antibiotic effectiveness in all countries. For example we should avoid the use of antibiotics in agriculture and the food industry. The study by Boeckel el al., concerning global trends in antimicrobial use in food animals, reported that the demand for meat globally has led to antibiotic consumption in animals to rise by 70% over the past decade.
The pneumococcus is unusual because vaccines are available. The pediatric pneumococcal conjugate vaccine has had a striking effect on vaccinated children and even non-vaccinated children and adults for the pneumococcal serotypes included in the vaccine. However, non-vaccine serotypes have emerged and are now associated with high-level antimicrobial resistance. Therefore, continuous surveillance programs are needed to determine optimal empiric treatment for a given locality. Surveillance programs are also needed to control the impact of pneumococcal campaigns on serotype distribution, emergence of non-vaccine serotypes, and antimicrobial resistance.
Not all members of an antibiotic class are equally effective against the pneumococcus. Some have a lower MIC than others, and some kill more rapidly. At approved doses, some reach infected tissues more effectively than others. These properties need to be carefully defined to guide clinical use. For example, with compounds that induce mutagenic responses, rapid killing is likely to be important. Additional insight may emerge from geographical locations that use particular derivatives and have very high rates of resistance. A clear example of this is the resistance of pneumococcus to macrolides. In Europe the main resistance mechanism is the ribosomal mutation that confers high resistance to macrolides, whereas in the United States, the dominant mechanism of resistance is active efflux, which confers low levels of resistance to macrolides. These data suggest the importance of clinical studies in different geographical areas before recommending particular antibiotics. A completely different question is how to slow transmission among young children and elderly persons in long-term care facilities. Solutions may involve reducing antimicrobial consumption, the main driver of newly acquired resistance.
Continued surveillance to quantify pneumococcal resistance is also needed to detect the emergence of new strains exhibiting high-level resistance to penicillin. Moreover, we need to better understand the clinical relevance and impact of antibiotic resistance on pneumococcal infections, since there is not always a clear relationship between resistance and treatment failure.
Major Points
Streptococcus pneumoniae remains an important pathogen worldwide. Pneumococcal infections are related to high rates of morbidity and mortality especially in young children, older adults, and immunocompromised persons.
Worldwide pneumococcal infections remain a big challenge for physicians because of its resistance to penicillin and increasing resistance to macrolides.
Efforts to reduce antibiotic consumption should be encouraged by educational programs and guidelines for healthcare professionals.
The best way to prevent pneumococcal infection is by the implementation of conjugate pneumococcal vaccinations.
It is important to monitor the evolution of pneumococcal disease, focusing on serotype replacement.
Studies focusing on the development of new vaccine designs should be addressed in order to avoid serotype replacement.
Contributor Information
I. W. Fong, Phone: +11+1(416) 864-5746, FAX: +11+1(416) 864-7854, Email: fongi@smh.ca
David Shlaes, Email: shlaesaac@gmail.com.
Karl Drlica, Phone: +119738543360, FAX: +119738543101, Email: drlicaka@njms.rutgers.edu.
References
- 1.Goossens H. Antibiotic consumption and link to resistance. Clin Microbiol Infect. 2009;15(Suppl 3):12–15. doi: 10.1111/j.1469-0691.2009.02725.x. [DOI] [PubMed] [Google Scholar]
- 2.Bell BG, Schellevis F, Stobberingh E, Goossens H, Pringle M. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis. 2014;14:13. doi: 10.1186/1471-2334-14-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frieden T, Center for Disease Control. Antibiotic Resistance Threats in the United States 2013. US: U.S. Department of Health and Human Service, Center for Disease Control and Prevention; 2013.
- 4.Solomon SL, Oliver KB. Antibiotic resistance threats in the United States: stepping back from the brink. Am Fam Physician. 2014;89(12):938–941. [PubMed] [Google Scholar]
- 5.Anon. The bacterial challenge: time to react. EMEA-ECDC Technical Report 2009. 2009.
- 6.Adriaenssens N, Coenen S, Versporten A, Muller A, Vankerckhoven V, Goossens H. European Surveillance of Antimicrobial Consumption (ESAC): quality appraisal of antibiotic use in Europe. J Antimicrob Chemother. 2011;66(Suppl 6):vi71–vi77. doi: 10.1093/jac/dkr459. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO) Antimicrobial resistance: global report on surveillance 2014. Geneva: World Health Organization; 2014. [Google Scholar]
- 8.Weisfelt M, van de Beek D, Spanjaard L, Reitsma JB, de Gans J. Clinical features, complications, and outcome in adults with pneumococcal meningitis: a prospective case series. Lancet Neurol. 2006;5(2):123–129. doi: 10.1016/S1474-4422(05)70288-X. [DOI] [PubMed] [Google Scholar]
- 9.van de Beek D, de Gans J, Tunkel AR, Wijdicks EF. Community-acquired bacterial meningitis in adults. N Engl J Med. 2006;354(1):44–53. doi: 10.1056/NEJMra052116. [DOI] [PubMed] [Google Scholar]
- 10.Van Boeckel TP, Gandra S, Ashok A, et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis. 2014;14(8):742–750. doi: 10.1016/S1473-3099(14)70780-7. [DOI] [PubMed] [Google Scholar]
- 11.Linares J, Ardanuy C, Pallares R, Fenoll A. Changes in antimicrobial resistance, serotypes and genotypes in Streptococcus pneumoniae over a 30-year period. Clin Microbiol Infect. 2010;16(5):402–410. doi: 10.1111/j.1469-0691.2010.03182.x. [DOI] [PubMed] [Google Scholar]
- 12.Lynch JP, III, Zhanel GG. Streptococcus pneumoniae: does antimicrobial resistance matter? Semin Respir Crit Care Med. 2009;30(2):210–238. doi: 10.1055/s-0029-1202939. [DOI] [PubMed] [Google Scholar]
- 13.Choi SH, Kim EY, Kim YJ. Systemic use of fluoroquinolone in children. Korean J Pediatr. 2013;56(5):196–201. doi: 10.3345/kjp.2013.56.5.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bradley J. S., Jackson M. A. The Use of Systemic and Topical Fluoroquinolones. PEDIATRICS. 2011;128(4):e1034–e1045. doi: 10.1542/peds.2011-1496. [DOI] [PubMed] [Google Scholar]
- 15.Arason VA, Kristinsson KG, Sigurdsson JA, Stefansdottir G, Molstad S, Gudmundsson S. Do antimicrobials increase the carriage rate of penicillin resistant pneumococci in children? Cross sectional prevalence study. BMJ. 1996;313(7054):387–391. doi: 10.1136/bmj.313.7054.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dagan R. Impact of pneumococcal conjugate vaccine on infections caused by antibiotic-resistant Streptococcus pneumoniae. Clin Microbiol Infect. 2009;15(Suppl 3):16–20. doi: 10.1111/j.1469-0691.2009.02726.x. [DOI] [PubMed] [Google Scholar]
- 17.Hogberg L, Geli P, Ringberg H, Melander E, Lipsitch M, Ekdahl K. Age- and serogroup-related differences in observed durations of nasopharyngeal carriage of penicillin-resistant pneumococci. J Clin Microbiol. 2007;45(3):948–952. doi: 10.1128/JCM.01913-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fenoll A, Granizo JJ, Aguilar L, et al. Temporal trends of invasive Streptococcus pneumoniae serotypes and antimicrobial resistance patterns in Spain from 1979 to 2007. J Clin Microbiol. 2009;47(4):1012–1020. doi: 10.1128/JCM.01454-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Owens RC, Jr, Shorr AF. Rational dosing of antimicrobial agents: pharmacokinetic and pharmacodynamic strategies. Am J Health Syst Pharm. 2009;66(12 Suppl 4):S23–S30. doi: 10.2146/090087d. [DOI] [PubMed] [Google Scholar]
- 20.Jensen A, Valdorsson O, Frimodt-Moller N, Hollingshead S, Kilian M. Commensal streptococci serve as a reservoir for beta-lactam resistance genes in Streptococcus pneumoniae. Antimicrob Agents Chemother. 2015;59(6):3529–3540. doi: 10.1128/AAC.00429-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cilloniz C, Ardanuy C, Vila J, Torres A. What is the clinical relevance of drug-resistant pneumococcus? Curr Opin Pulm Med. 2016;22(3):227–234. doi: 10.1097/MCP.0000000000000262. [DOI] [PubMed] [Google Scholar]
- 22.Shortridge VD, Doern GV, Brueggemann AB, Beyer JM, Flamm RK. Prevalence of macrolide resistance mechanisms in Streptococcus pneumoniae isolates from a multicenter antibiotic resistance surveillance study conducted in the United States in 1994–1995. Clin Infect Dis. 1999;29(5):1186–1188. doi: 10.1086/313452. [DOI] [PubMed] [Google Scholar]
- 23.Sirekbasan L, Gonullu N, Sirekbasan S, Kuskucu M, Midilli K. Phenotypes and genotypes of macrolide-resistant streptococcus pneumoniae. Balkan Med J. 2015;32(1):84–88. doi: 10.5152/balkanmedj.2015.15169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calatayud L, Ardanuy C, Tubau F, et al. Serotype and genotype replacement among macrolide-resistant invasive Pneumococci in adults: mechanisms of resistance and association with different transposons. J Clin Microbiol. 2010;48(4):1310–1316. doi: 10.1128/JCM.01868-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grivea IN, Sourla A, Ntokou E, Chryssanthopoulou DC, Tsantouli AG, Syrogiannopoulos GA. Macrolide resistance determinants among Streptococcus pneumoniae isolates from carriers in Central Greece. BMC Infect Dis. 2012;12:255. doi: 10.1186/1471-2334-12-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lismond A, Carbonnelle S, Verhaegen J, et al. Antimicrobial susceptibility of Streptococcus pneumoniae isolates from vaccinated and non-vaccinated patients with a clinically confirmed diagnosis of community-acquired pneumonia in Belgium. Int J Antimicrob Agents. 2012;39(3):208–216. doi: 10.1016/j.ijantimicag.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 27.Wierzbowski AK, Nichol K, Laing N, et al. Macrolide resistance mechanisms among Streptococcus pneumoniae isolated over 6 years of Canadian Respiratory Organism Susceptibility Study (CROSS) (1998 2004) J Antimicrob Chemother. 2007;60(4):733–740. doi: 10.1093/jac/dkm273. [DOI] [PubMed] [Google Scholar]
- 28.Hawkins PA, Chochua S, Jackson D, Beall B, McGee L. Mobile elements and chromosomal changes associated with MLS resistance phenotypes of invasive pneumococci recovered in the United States. Microb Drug Resist. 2015;21(2):121–129. doi: 10.1089/mdr.2014.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.El Ashkar S, Osman M, Rafei R, et al. Molecular detection of genes responsible for macrolide resistance among Streptococcus pneumoniae isolated in North Lebanon. J Infect Public Health. 2017;10(6):745–748. doi: 10.1016/j.jiph.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 30.Kawaguchiya M, Urushibara N, Aung MS, et al. Emerging non-PCV13 serotypes of noninvasive Streptococcus pneumoniae with macrolide resistance genes in northern Japan. New Microbes New Infect. 2016;9:66–72. doi: 10.1016/j.nmni.2015.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Azadegan A, Ahmadi A, Lari AR, Talebi M. Detection of the efflux-mediated erythromycin resistance transposon in Streptococcus pneumoniae. Ann Lab Med. 2015;35(1):57–61. doi: 10.3343/alm.2015.35.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim SH, Song JH, Chung DR, et al. Changing trends in antimicrobial resistance and serotypes of Streptococcus pneumoniae isolates in Asian countries: an Asian Network for Surveillance of Resistant Pathogens (ANSORP) study. Antimicrob Agents Chemother. 2012;56(3):1418–1426. doi: 10.1128/AAC.05658-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramos V, Duarte C, Diaz A, Moreno J. Mobile genetic elements associated with erythromycin-resistant isolates of Streptococcus pneumoniae in Colombia. Biomedica. 2014;34(Suppl 1):209–216. doi: 10.1590/S0120-41572014000500023. [DOI] [PubMed] [Google Scholar]
- 34.Reijtman V, Gagetti P, Faccone D, et al. Macrolide resistance in Streptococcus pneumoniae isolated from Argentinian pediatric patients suffering from acute otitis media. Rev Argent Microbiol. 2013;45(4):262–266. doi: 10.1016/S0325-7541(13)70034-8. [DOI] [PubMed] [Google Scholar]
- 35.Diawara I, Zerouali K, Katfy K, et al. Phenotypic and genotypic characterization of Streptococcus pneumoniae resistant to macrolide in Casablanca, Morocco. Infect Genet Evol. 2016;40:200–204. doi: 10.1016/j.meegid.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 36.Rachdi M, Boutiba-Ben Boubaker I, Moalla S, et al. Phenotypic and genotypic characterization of macrolide resistant Streptococcus pneumoniae in Tunisia. Pathol Biol (Paris) 2008;56(3):125–129. doi: 10.1016/j.patbio.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 37.Reinert RR, Filimonova OY, Al-Lahham A, et al. Mechanisms of macrolide resistance among Streptococcus pneumoniae isolates from Russia. Antimicrob Agents Chemother. 2008;52(6):2260–2262. doi: 10.1128/AAC.01270-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ma X, Yao KH, Xie GL, et al. Characterization of erythromycin-resistant Streptococcus pneumoniae isolates causing invasive diseases in Chinese children. Chin Med J (Engl) 2013;126(8):1522–1527. [PubMed] [Google Scholar]
- 39.Zhou L, Yu SJ, Gao W, Yao KH, Shen AD, Yang YH. Serotype distribution and antibiotic resistance of 140 pneumococcal isolates from pediatric patients with upper respiratory infections in Beijing, 2010. Vaccine. 2011;29(44):7704–7710. doi: 10.1016/j.vaccine.2011.07.137. [DOI] [PubMed] [Google Scholar]
- 40.Geng Q, Zhang T, Ding Y, et al. Molecular characterization and antimicrobial susceptibility of Streptococcus pneumoniae isolated from children hospitalized with respiratory infections in Suzhou, China. PLoS One. 2014;9(4):e93752. doi: 10.1371/journal.pone.0093752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Caierao J, Hawkins P, Sant’anna FH, et al. Serotypes and genotypes of invasive Streptococcus pneumoniae before and after PCV10 implementation in southern Brazil. PLoS One. 2014;9(10):e111129. doi: 10.1371/journal.pone.0111129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fuller JD, McGeer A, Low DE. Drug-resistant pneumococcal pneumonia: clinical relevance and approach to management. Eur J Clin Microbiol Infect Dis. 2005;24(12):780–788. doi: 10.1007/s10096-005-0059-x. [DOI] [PubMed] [Google Scholar]
- 43.Fuller JD, Low DE. A review of Streptococcus pneumoniae infection treatment failures associated with fluoroquinolone resistance. Clin Infect Dis. 2005;41(1):118–121. doi: 10.1086/430829. [DOI] [PubMed] [Google Scholar]
- 44.Urban C, Rahman N, Zhao X, et al. Fluoroquinolone-resistant Streptococcus pneumoniae associated with levofloxacin therapy. J Infect Dis. 2001;184(6):794–798. doi: 10.1086/323086. [DOI] [PubMed] [Google Scholar]
- 45.Woodhead M, Blasi F, Ewig S, et al. Guidelines for the management of adult lower respiratory tract infections--full version. Clin Microbiol Infect. 2011;17(Suppl 6):E1–59. doi: 10.1111/j.1469-0691.2011.03672.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society Consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–S72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Donhofer A, Franckenberg S, Wickles S, Berninghausen O, Beckmann R, Wilson DN. Structural basis for TetM-mediated tetracycline resistance. Proc Natl Acad Sci U S A. 2012;109(42):16900–16905. doi: 10.1073/pnas.1208037109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moscoso M, Domenech M, Garcia E. Vancomycin tolerance in Gram-positive cocci. Environ Microbiol Rep. 2011;3(6):640–650. doi: 10.1111/j.1758-2229.2011.00254.x. [DOI] [PubMed] [Google Scholar]
- 49.Van BF, Reinert RR, Appelbaum PC, Tulkens PM, Peetermans WE. Multidrug-resistant Streptococcus pneumoniae infections: current and future therapeutic options. Drugs. 2007;67(16):2355–2382. doi: 10.2165/00003495-200767160-00005. [DOI] [PubMed] [Google Scholar]
- 50.Sheppard C, Fry NK, Mushtaq S, et al. Rise of multidrug-resistant non-vaccine serotype 15A Streptococcus pneumoniae in the United Kingdom, 2001 to 2014. Euro Surveill. 2016;21(50):3042. [DOI] [PMC free article] [PubMed]
- 51.Richter SS, Diekema DJ, Heilmann KP, Dohrn CL, Riahi F, Doern GV. Changes in pneumococcal serotypes and antimicrobial resistance after introduction of the 13-valent conjugate vaccine in the United States. Antimicrob Agents Chemother. 2014;58(11):6484–6489. doi: 10.1128/AAC.03344-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Golden AR, Rosenthal M, Fultz B, et al. Characterization of MDR and XDR Streptococcus pneumoniae in Canada, 2007–13. J Antimicrob Chemother. 2015;70(8):2199–2202. doi: 10.1093/jac/dkv107. [DOI] [PubMed] [Google Scholar]
- 53.Golden AR, Adam HJ, Zhanel GG. Invasive Streptococcus pneumoniae in Canada, 2011–2014: Characterization of new candidate 15-valent pneumococcal conjugate vaccine serotypes 22F and 33F. Vaccine. 2016;34(23):2527–2530. doi: 10.1016/j.vaccine.2016.03.058. [DOI] [PubMed] [Google Scholar]
- 54.Olarte L, Kaplan SL, Barson WJ, et al. Emergence of Multidrug-resistant Pneumococcal Serotype 35B among U.S. Children. J Clin Microbiol. 2017;55(3):724–34. [DOI] [PMC free article] [PubMed]
- 55.Nakano S, Fujisawa T, Ito Y, et al. Serotypes, antimicrobial susceptibility, and molecular epidemiology of invasive and non-invasive Streptococcus pneumoniae isolates in paediatric patients after the introduction of 13-valent conjugate vaccine in a nationwide surveillance study conducted in Japan in 2012–2014. Vaccine. 2016;34(1):67–76. doi: 10.1016/j.vaccine.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 56.Elshafie S, Taj-Aldeen SJ. Emerging resistant serotypes of invasive Streptococcus pneumoniae. Infect Drug Resist. 2016;9:153–160. doi: 10.2147/IDR.S102410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bahy RH, Hamouda HM, Shahat AS, Yassin AS, Amin MA. Emergence of neoteric serotypes among multidrug resistant strains of Streptococcus pneumoniae prevalent in Egypt. Jundishapur J Microbiol. 2016;9(4):e30708. doi: 10.5812/jjm.30708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Aspa J, Rajas O, Rodríguez de Castro F, et al. Drug-resistant pneumococcal pneumonia: clinical relevance and related factors. Clin Infect Dis. 2004;38(6):787–798. doi: 10.1086/381886. [DOI] [PubMed] [Google Scholar]
- 59.Pallares R, Gudiol F, Linares J, et al. Risk factors and response to antibiotic therapy in adults with bacteremic pneumonia caused by penicillin-resistant pneumococci. N Engl J Med. 1987;317:18–22. doi: 10.1056/NEJM198707023170104. [DOI] [PubMed] [Google Scholar]
- 60.Tsai HY, Lauderdale TL, Wang JT, et al. Updated antibiotic resistance and clinical spectrum of infections caused by Streptococcus pneumoniae in Taiwan: emphasis on risk factors for penicillin nonsusceptibilities. J Microbiol Immunol Infect. 2013;46(5):345–351. doi: 10.1016/j.jmii.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 61.Ruhe JJ, Hasbun R. Streptococcus pneumoniae bacteremia: duration of previous antibiotic use and association with penicillin resistance. Clin Infect Dis. 2003;36(9):1132–1138. doi: 10.1086/374556. [DOI] [PubMed] [Google Scholar]
- 62.Ruhe JJ, Myers L, Mushatt D, Hasbun R. High-level penicillin-nonsusceptible Streptococcus pneumoniae bacteremia: identification of a low-risk subgroup. Clin Infect Dis. 2004;38(4):508–514. doi: 10.1086/381197. [DOI] [PubMed] [Google Scholar]
- 63.Mollendorf CV, Cohen C, De Gouveia L, et al. Factors associated with ceftriaxone nonsusceptibility of Streptococcus pneumoniae: analysis of South African national surveillance data, 2003 to 2010. Antimicrob Agents Chemother. 2014;58(6):3293–3305. doi: 10.1128/AAC.02580-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bogaert D, de Groot R, Hermans PW. Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis. 2004;4(3):144–154. doi: 10.1016/S1473-3099(04)00938-7. [DOI] [PubMed] [Google Scholar]
- 65.Gritzfeld JF, Wright AD, Collins AM, et al. Experimental human pneumococcal carriage. J Vis Exp. 2013;(72):50115. [DOI] [PMC free article] [PubMed]
- 66.Vasoo S, Singh K, Hsu LY, et al. Increasing antibiotic resistance in Streptococcus pneumoniae colonizing children attending day-care centres in Singapore. Respirology. 2011;16(8):1241–1248. doi: 10.1111/j.1440-1843.2011.02036.x. [DOI] [PubMed] [Google Scholar]
- 67.Jain A, Kumar P, Awasthi S. High nasopharyngeal carriage of drug resistant Streptococcus pneumoniae and Haemophilus influenzae in North Indian schoolchildren. Trop Med Int Heal. 2015;10:234–239. doi: 10.1111/j.1365-3156.2004.01379.x. [DOI] [PubMed] [Google Scholar]
- 68.Dunais B, Bruno-Bazureault P, Carsenti-Dellamonica H, Touboul P, Pradier C. A decade-long surveillance of nasopharyngeal colonisation with Streptococcus pneumoniae among children attending day-care centres in south-eastern France: 1999–2008. Eur J Clin Microbiol Infect Dis. 2011;30(7):837–843. doi: 10.1007/s10096-011-1154-9. [DOI] [PubMed] [Google Scholar]
- 69.Nuorti JP, Butler JC, Crutcher JM, et al. An outbreak of multidrug-resistant pneumococcal pneumonia and bacteremia among unvaccinated nursing home residents. N Engl J Med. 1998;338:1861–1868. doi: 10.1056/NEJM199806253382601. [DOI] [PubMed] [Google Scholar]
- 70.Van Eldere J, Mera RM, Miller LA, Poupard JA, Amrine-Madsen H. Risk factors for development of multiple-class resistance to Streptococcus pneumoniae Strains in Belgium over a 10-year period: antimicrobial consumption, population density, and geographic location. Antimicrob Agents Chemother. 2007;51(10):3491–3497. doi: 10.1128/AAC.01581-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.van de Sande-Bruinsma N, Grundmann H, Verloo D, et al. Antimicrobial drug use and resistance in Europe. Emerg Infect Dis. 2008;14(11):1722–1730. doi: 10.3201/eid1411.070467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Farshad Ali Asghar, Enferadi Mojtaba, Bakand Shahnaz, Jamshidi Orak Rouhangiz, Mirkazemi Roksana. Penicillin dust exposure and penicillin resistance among pharmaceutical workers in Tehran, Iran. International Journal of Occupational and Environmental Health. 2016;22(3):218–223. doi: 10.1080/10773525.2016.1201238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hare KM, Leach AJ, Morris PS, et al. Impact of recent antibiotics on nasopharyngeal carriage and lower airway infection in Indigenous Australian children with non-cystic fibrosis bronchiectasis. Int J Antimicrob Agents. 2012;40(4):365–369. doi: 10.1016/j.ijantimicag.2012.05.018. [DOI] [PubMed] [Google Scholar]
- 74.Metlay JP, Fishman NO, Joffe MM, Kallan MJ, Chittams JL, Edelstein PH. Macrolide resistance in adults with bacteremic pneumococcal pneumonia. Emerg Infect Dis. 2006;12(8):1223–1230. doi: 10.3201/eid1208.060017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dias R, Canica M. Trends in resistance to penicillin and erythromycin of invasive pneumococci in Portugal. Epidemiol Infect. 2008;136(7):928–939. doi: 10.1017/S0950268807009405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Baek JY, Kim SH, Kang CI, et al. Prevalence of antimicrobial resistant Streptococcus pneumoniae serotype 11A isolates in Korea, during 2004–2013, due to the increase of multidrug-resistant clone, CC166. Infect Genet Evol. 2016;38:122–125. doi: 10.1016/j.meegid.2015.12.018. [DOI] [PubMed] [Google Scholar]
- 77.Zhou L, Ma X, Gao W, et al. Molecular characteristics of erythromycin-resistant Streptococcus pneumoniae from pediatric patients younger than five years in Beijing, 2010. BMC Microbiol. 2012;12:228. doi: 10.1186/1471-2180-12-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pan F, Han L, Huang W, et al. Serotype distribution, antimicrobial susceptibility, and molecular epidemiology of Streptococcus pneumoniae Isolated from children in Shanghai, China. PLoS One. 2015;10(11):e0142892. doi: 10.1371/journal.pone.0142892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hadjipanayis A, Efstathiou E, Alexandrou M, et al. Nasopharyngeal Pneumococcal Carriage among Healthy Children in Cyprus Post Widespread Simultaneous Implementation of PCV10 and PCV13 Vaccines. PLoS One. 2016;11(10):e0163269. doi: 10.1371/journal.pone.0163269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vanderkooi OG, McConnell A, Church DL, Kellner JD. Antimicrobial susceptibility of invasive and lower respiratory tract isolates of Streptococcus pneumoniae, 1998 to 2007. Can J Infect Dis Med Microbiol. 2009;20(4):e139–e144. doi: 10.1155/2009/413749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Matsumoto A, Hosoya M, Kawasaki Y, Katayose M, Kato K, Suzuki H. The emergence of drug-resistant Streptococcus pneumoniae and host risk factors for carriage of drug-resistant genes in northeastern Japan. Jpn J Infect Dis. 2007;60(1):10–13. [PubMed] [Google Scholar]
- 82.Grivea IN, Priftis KN, Giotas A, et al. Dynamics of pneumococcal carriage among day-care center attendees during the transition from the 7-valent to the higher-valent pneumococcal conjugate vaccines in Greece. Vaccine. 2014;32(48):6513–6520. doi: 10.1016/j.vaccine.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 83.Zuccotti G, Mameli C, Daprai L, et al. Serotype distribution and antimicrobial susceptibilities of nasopharyngeal isolates of Streptococcus pneumoniae from healthy children in the 13-valent pneumococcal conjugate vaccine era. Vaccine. 2014;32(5):527–534. doi: 10.1016/j.vaccine.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 84.Korona-Glowniak I, Siwiec R, Malm A. Resistance determinants and their association with different transposons in the antibiotic-resistant Streptococcus pneumoniae. Biomed Res Int. 2015;2015:836496. doi: 10.1155/2015/836496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ding Y, Geng Q, Tao Y, et al. Etiology and epidemiology of children with acute otitis media and spontaneous otorrhea in Suzhou, China. Pediatr Infect Dis J. 2015;34(5):e102–e106. doi: 10.1097/INF.0000000000000617. [DOI] [PubMed] [Google Scholar]
- 86.Abdelnour A, Arguedas A, Dagan R, et al. Etiology and antimicrobial susceptibility of middle ear fluid pathogens in Costa Rican children with otitis media before and after the introduction of the 7-valent pneumococcal conjugate vaccine in the National Immunization Program: acute otitis media microbiology in Costa Rican children. Medicine (Baltimore) 2015;94(2):e320. doi: 10.1097/MD.0000000000000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pumarola F, Mares J, Losada I, et al. Microbiology of bacteria causing recurrent acute otitis media (AOM) and AOM treatment failure in young children in Spain: shifting pathogens in the post-pneumococcal conjugate vaccination era. Int J Pediatr Otorhinolaryngol. 2013;77(8):1231–1236. doi: 10.1016/j.ijporl.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 88.Arason VA, Sigurdsson JA, Erlendsdottir H, Gudmundsson S, Kristinsson KG. The role of antimicrobial use in the epidemiology of resistant pneumococci: a 10-year follow up. Microb Drug Resist. 2006;12(3):169–176. doi: 10.1089/mdr.2006.12.169. [DOI] [PubMed] [Google Scholar]
- 89.Ho PL, Tse WS, Tsang KW, et al. Risk factors for acquisition of levofloxacin-resistant Streptococcus pneumoniae: a case-control study. Clin Infect Dis. 2001;32(5):701–707. doi: 10.1086/319222. [DOI] [PubMed] [Google Scholar]
- 90.Kang CI, Song JH, Kim SH, et al. Risk factors for levofloxacin-nonsusceptible Streptococcus pneumoniae in community-acquired pneumococcal pneumonia: a nested case-control study. Eur J Clin Microbiol Infect Dis. 2014;33(1):55–59. doi: 10.1007/s10096-013-1928-3. [DOI] [PubMed] [Google Scholar]
- 91.Kim ES, Hooper DC. Clinical importance and epidemiology of quinolone resistance. Infect Chemother. 2014;46(4):226–238. doi: 10.3947/ic.2014.46.4.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kuster SP, Rudnick W, Shigayeva A, et al. Previous antibiotic exposure and antimicrobial resistance in invasive pneumococcal disease: results from prospective surveillance. Clin Infect Dis. 2014;59(7):944–952. doi: 10.1093/cid/ciu497. [DOI] [PubMed] [Google Scholar]
- 93.Wolter N, Du Plessis M, Von Gottberg A, De Gouveia L, Klugman KP. Molecular characterization of emerging non-levofloxacin-susceptible pneumococci isolated from children in South Africa. J Clin Microbiol. 2009;47(5):1319–1324. doi: 10.1128/JCM.02280-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ben-David D, Schwaber MJ, Adler A, et al. Persistence and complex evolution of fluoroquinolone-resistant Streptococcus pneumoniae clone. Emerg Infect Dis. 2014;20(5):799–805. doi: 10.3201/eid2005.130142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Isea-Pena MC, Sanz-Moreno JC, Esteban J, Fernandez-Roblas R, Fernandez-Guerrero ML. Risk factors and clinical significance of invasive infections caused by levofloxacin-resistant Streptococcus pneumoniae. Infection. 2013;41(5):935–939. doi: 10.1007/s15010-013-0481-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kupronis BA, Richards CL, Whitney CG. Invasive pneumococcal disease in older adults residing in long-term care facilities and in the community. J Am Geriatr Soc. 2003;51(11):1520–1525. doi: 10.1046/j.1532-5415.2003.51501.x. [DOI] [PubMed] [Google Scholar]
- 97.Vanderkooi OG, Low DE, Green K, Powis JE, McGeer A. Predicting antimicrobial resistance in invasive pneumococcal infections. Clin Infect Dis. 2005;40(9):1288–1297. doi: 10.1086/429242. [DOI] [PubMed] [Google Scholar]
- 98.Thabit AK, Crandon JL, Nicolau DP. Antimicrobial resistance: impact on clinical and economic outcomes and the need for new antimicrobials. Expert Opin Pharmacother. 2015;16(2):159–177. doi: 10.1517/14656566.2015.993381. [DOI] [PubMed] [Google Scholar]
- 99.Song JH, Dagan R, Klugman KP, Fritzell B. The relationship between pneumococcal serotypes and antibiotic resistance. Vaccine. 2012;30(17):2728–2737. doi: 10.1016/j.vaccine.2012.01.091. [DOI] [PubMed] [Google Scholar]
- 100.Thummeepak R, Leerach N, Kunthalert D, Tangchaisuriya U, Thanwisai A, Sitthisak S. High prevalence of multi-drug resistant Streptococcus pneumoniae among healthy children in Thailand. J Infect Public Health. 2015;8(3):274–281. doi: 10.1016/j.jiph.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 101.Jin P, Kong F, Xiao M, et al. First report of putative Streptococcus pneumoniae serotype 6D among nasopharyngeal isolates from Fijian children. J Infect Dis. 2009;200(9):1375–1380. doi: 10.1086/606118. [DOI] [PubMed] [Google Scholar]
- 102.Oliver MB, van der Linden MP, Kuntzel SA, Saad JS, Nahm MH. Discovery of Streptococcus pneumoniae serotype 6 variants with glycosyltransferases synthesizing two differing repeating units. J Biol Chem. 2015;290(44):26474–26475. doi: 10.1074/jbc.A113.480152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Calix JJ, Porambo RJ, Brady AM, et al. Biochemical, genetic, and serological characterization of two capsule subtypes among Streptococcus pneumoniae Serotype 20 strains: discovery of a new pneumococcal serotype. J Biol Chem. 2012;287(33):27885–27894. doi: 10.1074/jbc.M112.380451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jauneikaite E, Tocheva AS, Jefferies JM, et al. Current methods for capsular typing of Streptococcus pneumoniae. J Microbiol Methods. 2015;113:41–49. doi: 10.1016/j.mimet.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 105.Brueggemann AB, Peto TE, Crook DW, Butler JC, Kristinsson KG, Spratt BG. Temporal and geographic stability of the serogroup-specific invasive disease potential of Streptococcus pneumoniae in children. J Infect Dis. 2004;190(7):1203–1211. doi: 10.1086/423820. [DOI] [PubMed] [Google Scholar]
- 106.Browall S, Backhaus E, Naucler P, et al. Clinical manifestations of invasive pneumococcal disease by vaccine and non-vaccine types. Eur Respir J. 2014;44(6):1646–1657. doi: 10.1183/09031936.00080814. [DOI] [PubMed] [Google Scholar]
- 107.Sjostrom K, Spindler C, Ortqvist A, et al. Clonal and capsular types decide whether pneumococci will act as a primary or opportunistic pathogen. Clin Infect Dis. 2006;42(4):451–459. doi: 10.1086/499242. [DOI] [PubMed] [Google Scholar]
- 108.Henriques-Normark B, Blomberg C, Dagerhamn J, Battig P, Normark S. The rise and fall of bacterial clones: Streptococcus pneumoniae. Nat Rev Microbiol. 2008;6(11):827–837. doi: 10.1038/nrmicro2011. [DOI] [PubMed] [Google Scholar]
- 109.Meropol SB, Stange KC, Jacobs MR, Weiss JK, Bajaksouzian S, Bonomo RA. Bacterial colonization and antibiotic resistance in a prospective cohort of newborn infants during the first year of life. Open Forum Infect Dis. 2016;3(4):ofw221. doi: 10.1093/ofid/ofw221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Boken DJ, Chartrand SA, Goering RV, Kruger R, Harrison CJ. Colonization with penicillin-resistant Streptococcus pneumoniae in a child-care center. Pediatr Infect Dis J. 1995;14(10):879–884. doi: 10.1097/00006454-199510000-00012. [DOI] [PubMed] [Google Scholar]
- 111.Centers for Disease Control and Prevention (CDC). Antibiotic Resistance Threats in the United States. 2013.
- 112.Navarro TA, Dias JG, Quinten C, et al. European enhanced surveillance of invasive pneumococcal disease in 2010: data from 26 European countries in the post-heptavalent conjugate vaccine era. Vaccine. 2014;32(29):3644–3650. doi: 10.1016/j.vaccine.2014.04.066. [DOI] [PubMed] [Google Scholar]
- 113.European Centre for Disease Prevention and Control (ECDC). Antimicrobial resistance surveillance in Europe 2012. 2012.
- 114.Jones RN, Sader HS, Mendes RE, Flamm RK. Update on antimicrobial susceptibility trends among Streptococcus pneumoniae in the United States: report of ceftaroline activity from the SENTRY Antimicrobial Surveillance Program (1998–2011) Diagn Microbiol Infect Dis. 2013;75(1):107–109. doi: 10.1016/j.diagmicrobio.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 115.Jenkins SG, Farrell DJ. Increase in pneumococcus macrolide resistance, United States. Emerg Infect Dis. 2009;15(8):1260–1264. doi: 10.3201/eid1508.081187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Xiao Y, Wei Z, Shen P, et al. Bacterial-resistance among outpatients of county hospitals in China: significant geographic distinctions and minor differences between central cities. Microbes Infect. 2015;17(6):417–425. doi: 10.1016/j.micinf.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 117.Cilloniz C, Albert RK, Liapikou A, et al. The effect of macrolide-resistance on the presentation and outcome of patients hospitalized for Streptococcus pneumoniae pneumonia. Am J Respir Crit Care Med. 2015;191(11):1265–1272. doi: 10.1164/rccm.201502-0212OC. [DOI] [PubMed] [Google Scholar]
- 118.Pletz MW, van der Linden M, von Baum H, Duesberg CB, Klugman KP, Welte T. Low prevalence of fluoroquinolone resistant strains and resistance precursor strains in Streptococcus pneumoniae from patients with community-acquired pneumonia despite high fluoroquinolone usage. Int J Med Microbiol. 2011;301(1):53–57. doi: 10.1016/j.ijmm.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 119.Jacobs E, Dalhoff A, Korfmann G. Susceptibility patterns of bacterial isolates from hospitalised patients with respiratory tract infections (MOXIAKTIV Study) Int J Antimicrob Agents. 2009;33(1):52–57. doi: 10.1016/j.ijantimicag.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 120.Ho PL, Cheng VC, Chow KH. Decreasing prevalence of levofloxacin-resistant Streptococcus pneumoniae in Hong Kong, 2001 to 2007. J Antimicrob Chemother. 2009;63(4):836–838. doi: 10.1093/jac/dkp038. [DOI] [PubMed] [Google Scholar]
- 121.Vila-Corcoles A, Ochoa-Gondar O. Preventing pneumococcal disease in the elderly: recent advances in vaccines and implications for clinical practice. Drugs Aging. 2013;30(5):263–276. doi: 10.1007/s40266-013-0060-5. [DOI] [PubMed] [Google Scholar]
- 122.Kyaw MH, Lynfield R, Schaffner W, et al. Effect of introduction of the pneumococcal conjugate vaccine on drug-resistant Streptococcus pneumoniae. N Engl J Med. 2006;354(14):1455–1463. doi: 10.1056/NEJMoa051642. [DOI] [PubMed] [Google Scholar]
- 123.Whitney CG, Pilishvili T, Farley MM, et al. Effectiveness of seven-valent pneumococcal conjugate vaccine against invasive pneumococcal disease: a matched case-control study. Lancet. 2006;368(9546):1495–1502. doi: 10.1016/S0140-6736(06)69637-2. [DOI] [PubMed] [Google Scholar]
- 124.Gertz RE, Jr, Li Z, Pimenta FC, et al. Increased penicillin nonsusceptibility of nonvaccine-serotype invasive pneumococci other than serotypes 19A and 6A in post-7-valent conjugate vaccine era. J Infect Dis. 2010;201(5):770–775. doi: 10.1086/650496. [DOI] [PubMed] [Google Scholar]
- 125.Reinert R, Jacobs MR, Kaplan SL. Pneumococcal disease caused by serotype 19A: review of the literature and implications for future vaccine development. Vaccine. 2010;28(26):4249–4259. doi: 10.1016/j.vaccine.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 126.Moore MR, Link-Gelles R, Schaffner W, et al. Effect of use of 13-valent pneumococcal conjugate vaccine in children on invasive pneumococcal disease in children and adults in the USA: analysis of multisite, population-based surveillance. Lancet Infect Dis. 2015;15(3):301–309. doi: 10.1016/S1473-3099(14)71081-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.van der Linden M, Perniciaro S, Imohl M. Increase of serotypes 15A and 23B in IPD in Germany in the PCV13 vaccination era. BMC Infect Dis. 2015;15:207. doi: 10.1186/s12879-015-0941-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Garcia-Vidal C, Ardanuy C, Tubau F, et al. Pneumococcal pneumonia presenting with septic shock: host- and pathogen-related factors and outcomes. Thorax. 2010;65(1):77–81. doi: 10.1136/thx.2009.123612. [DOI] [PubMed] [Google Scholar]
- 129.Mongardon N, Max A, Bougle A, et al. Epidemiology and outcome of severe pneumococcal pneumonia admitted to intensive care unit: a multicenter study. Crit Care. 2012;16(4):R155. doi: 10.1186/cc11471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kaplan SL, Mason EO., Jr Management of infections due to antibiotic-resistant Streptococcus pneumoniae. Clin Microbiol Rev. 1998;11(4):628–644. doi: 10.1128/cmr.11.4.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Schroeder MR, Stephens DS. Macrolide resistance in Streptococcus pneumoniae. Front Cell Infect Microbiol. 2016;6:98. doi: 10.3389/fcimb.2016.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Endimiani A, Brigante G, Bettaccini AA, Luzzaro F, Grossi P, Toniolo AQ. Failure of levofloxacin treatment in community-acquired pneumococcal pneumonia. BMC Infect Dis. 2005;5:106. doi: 10.1186/1471-2334-5-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kim L, McGee L, Tomczyk S, Beall B. Biological and epidemiological features of antibiotic-resistant Streptococcus pneumoniae in pre- and post-conjugate vaccine eras: a United States perspective. Clin Microbiol Rev. 2016;29(3):525–552. doi: 10.1128/CMR.00058-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kang CI, Song JH, Kim SH, et al. Association of levofloxacin resistance with mortality in adult patients with invasive pneumococcal diseases: a post hoc analysis of a prospective cohort. Infection. 2013;41(1):151–157. doi: 10.1007/s15010-012-0299-5. [DOI] [PubMed] [Google Scholar]