Abstract
Children less than 6 years have the greatest risk for accidental ingestion and poisoning.
Keywords: Poisoning, Iron ingestion, Head trauma, Drowning, Wounds, Puncture wounds, Animal and human bites, Status epilepticus, Burns, Resuscitation
Poisoning
Background
Children less than 6 years have the greatest risk.
Adolescent exposure either intentional or occupational
Plant ingestions either substance experimentation or attempted self-harm
The website http://www.aapcc.org contains useful information about poison centers
Prevention of poisoning
Child-resistant packaging
Anticipatory guidance in well child care
Poison proofing child’s environment, e.g., labeling and locked cabinets
Parents to utilize online sources and contact poison control emergency number
Carbon monoxide detectors
Maintenance of fuel-burning appliances
Yearly inspection of furnaces, gas pipes, and chimneys
Car inspection for exhaust system
No running engine in a closed garage
Avoid indoor use of charcoal and fire sources
Evaluation of unknown substance
Call poison control center, describe the toxin, read the label, and follow the instruction
Pattern of toxidrome
Amount of exposure, number of pills, number of the remaining pills, amount of liquid remaining
Time of exposure
Progression of symptoms
Consider associated ingestions and underlying medical conditions
General measures for toxic exposures
Emergency department evaluation in ingestion of a large or potential toxic doses
Wash the skin with soap and water
Activated charcoal absorb the substances and decreases bioavailability
-
Activated charcoal is ineffective in the following; CHEMICaL:
- Caustics
- Hydrocarbons
- Ethanol (alcohols)
- Metals
- Iron
- Cyanide
- Lithium
Ipecac no longer used, and induction of emesis is contraindicated in hydrocarbons and caustics
-
Gastric lavage
- Contraindicated in hydrocarbons, alcohols and caustics
- It can be used if life-threatening ingestion within 30–60 min
Whole bowel irrigation
Anticholinergic Ingestion
Agents
Diphenhydramine, atropine, Jimsonweed (Datura Stramonium), and deadly night shade (Atropa Belladonna)
Background
Jimson weed and deadly night shade produce anticholinergic toxins, e.g., atropine, scopolamine, and hyoscyamine
Common garden vegetables in the solanum genus, including tomatoes, potatoes, and eggplants.
Cause anticholinergic symptoms
Clinical presentation (anticholinergic symptoms)
Dry as a bone: Dry mouth, decrease sweating, and urination
Red as a beet: Flushing
Blind as a bat: Mydriasis, blurred vision
Mad as a hatter: Agitation, seizures, Hallucinations
Hot as a hare: Hyperthermia
Bloated as a Toad (ileus, urinary retention)
Heart runs alone (tachycardia)
Management
Activated charcoal
Physostigmine may be indicated to treat severe or persistent symptoms
Carbamazepine Ingestion
Mild ingestion
Central nervous system (CNS) depression
Drowsiness
Vomiting
Ataxia
Slurred speech
Nystagmus
Severe intoxication
Seizures
Coma
Respiratory depression
Treatment
Activated charcoal
Supportive measures
Charcoal hemoperfusion can be effective for severe intoxication
Clonidine
Antihypertensive medication with α-2 adrenergic receptor blocking ability
Commonly used in children with attention deficit hyperactivity disorder (ADHD)
A dose as small as 0.1 mg can cause toxicity in children
Common symptoms
Lethargy
Miosis
Bradycardia
Hypotension but it may cause hypertension
Apnea
Treatment
Supportive care, e.g., intubation, atropine, dopamine as needed
Electroencephalogram (EEG), blood gases
Toxicity usually resolve in 24 h
Opiates
Common opiates
Morphine, heroin, methadone, propoxyphene, codeine, meperidine
Most cases are drug abuse
Symptoms
Common triad of opiate poisoning (pinpoint pupil, coma, respiratory depression)
Drowsiness to coma
Miosis
Change in mood
Analgesia
Respiratory depression
Hypotension with no change in heart rate (HR)
Decreased gastrointestinal (GI) motility
Nausea and vomiting
Abdominal pain
Treatment
Airway, breathing, and circulation (ABCs)
Intubation if necessary
Naloxone as needed
Phenothiazine Ingestion
Common drugs
Promethazine (Phenergan), prochlorperazine, and chlorpromazine
Symptoms
Hypertension
Cogwheel rigidity
Dystonic reaction (spasm of the neck, tongue thrusting, oculogyric crisis)
CNS depression
Treatment
Charcoal
Manage blood pressure
Diphenhydramine for dystonic reaction
Foxglove (Digitalis) Ingestion
Source
Foxglove plants.
Produces cardioactive glycosides.
They are also found in lily of the valley (Convallaria).
Clinical presentation
Similar to digoxin toxicity
Hyperkalemia
CNS depression
Cardiac conduction abnormalities
Treatment
Digoxin-specific antibody fragments can be lifesaving
Seeds (Cherries, Apricots, Peaches, Apples, Plums) Ingestion
Amygdalin is contained in seeds and produces hydrogen cyanide which is a potent toxin
Inhibition of cellular respiration and can be lethal
Mushrooms Ingestion
Ingestion of mushrooms also may have fatal consequences in species that harbor amatoxins (Amanita) and related compounds
Clinical presentation
Nausea, vomiting, and diarrhea; delayed onset (6 h)
A second latent period is followed by acute and possibly fulminant hepatitis beginning 48–72 h after ingestion
Management
Activated charcoal
Whole bowel irrigation
Supportive care, including liver transplant if necessary, is the mainstay of therapy
Acetaminophen Ingestion
Background
The single toxic acute dose is generally considered to be > 200 mg/kg in children and more 7.5–10 g in adult and can cause hepatic injury or liver failure
Any child with history of acute ingestion of > 150 mg/kg of acetaminophen should be referred for assessment and measurement of acetaminophen level
Clinical presentation
-
First 24 h
- Asymptomatic or nonspecific signs
- Nausea, vomiting, dehydration, diaphoresis, and pallor
- Elevation of liver enzyme
-
24–72 h after ingestion
- Tachycardia and hypotension
- Right upper quadrant pain with or without hepatomegaly
- Liver enzyme is more elevated
- Elevated prothrombin time (PT) and bilirubin in severe cases
-
3–4 days post ingestion
- Liver failure
- Encephalopathy, with or without renal failure
- Possible death from multi-organ failure or cerebral edema
-
4–14 days post ingestion
- Complete recovery or death
Management
Measure serum acetaminophen level 4 h after the reported time of ingestion
Acetaminophen level obtained < 4 h after ingestion cannot be used to estimate potential toxicity
Check acetaminophen level 6–8 h if it is co-ingested with other substance slow GI motility, e.g., diphenhydramine
-
Rumack–Matthew nomogram (Fig. 1)
- Plot 4-h value of a single acute ingestion
- Risk of hepatotoxicity possible if 4-h level is equal or greater than 150 mcg/ml. If fall on upper line (200 mcg/ml at 4 h) hepatotoxicity is probable
-
Assess the liver function
- Obtain hepatic transaminases level, renal function tests, and coagulation parameters
If acetaminophen level > 10 μg/ml even with normal liver function, start the N-acetylcysteine (NAC)
If acetaminophen level is low or undetectable with abnormal liver function, NAC should be given
Patients with a history of potentially toxic ingestion more than 8 h after ingestion should be given the loading dose of NAC and decision to continue treatment should be based on acetaminophen level or liver function test
NAC therapy is most effective when initiated within 8 h of ingestion
Liver transplant if severe hepatotoxicity
Consult poison control center at 1-800-222-1222
Fig. 1.
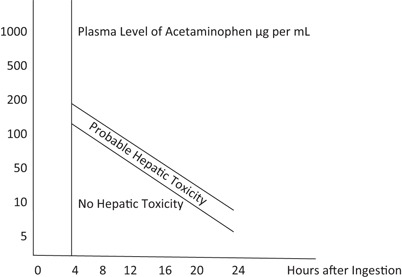
Rumack–Mathew nomogram for acetaminophen poisoning. (Adapted from Rumack BH, Mathew H. Acetaminophen poisoning and toxicity. Pediatrics 55:971–876, 1975)
Ibuprofen Ingestion
Background
Inhibit prostaglandin synthesis
May cause GI irritation, ulcers, decrease renal blood flow, and platelet dysfunction
Dose > 400 mg/kg can cause seizure and coma
Dose < 100 mg/kg usually does not cause toxicity
Clinical presentation
Nausea, vomiting and epigastric pain
Drowsiness, lethargy, and ataxia may occur
Anion gap metabolic acidosis, renal failure, seizure and coma may occur in severe cases
Management
Activated charcoal
Supportive care
Salicylic acid Ingestion
Products contain an aspirin
Baby aspirin
Regular aspirin at home includes: Anti-diarrheal medications, topical agents, e.g., keratolytics and sport creams
Toxic dose
Refer to emergency departments for ingestions > 150 mg/kg
Ingestion of > 200 mg/kg is generally considered toxic, > 300 mg/kg is more significant toxicity, > 500 mg/kg is potentially fatal
Clinical presentation
Acute salicylism; nausea, vomiting, diaphoresis, and tinnitus
Tachypnea, hyperpnea, tachycardia, and altered mental status can be seen in moderate toxicity
Hyperthermia and coma are seen in severe acetylsalicylic acid toxicity
Diagnosis
Classic blood gas of salicylic acid toxicity is respiratory alkalosis, metabolic acidosis, and high anion gap
Check serum level every 2 h until it is consistently down trending
Management
Initial treatment is gastric decontamination with activated charcoal, volume resuscitation, and prompt initiation of sodium bicarbonate therapy in the symptomatic patients
Goal of therapy includes a urine pH of 7.5–8.0, a serum pH of 7.5–7.55, and decreasing salicylate levels
Tricyclic Antidepressants Ingestion
Toxicity
Tricyclic antidepressants (TCAs) can cause significant toxicity in children even with ingestion of 1–2 pills (10–20 mg/kg)
Clinical presentation
It gives the clinical feature of anticholinergic toxidrome; delirium, mydriasis, dry mucous membrane, tachycardia, hyperthermia, hypotension, and urinary retention
Cardiovascular and CNS symptoms dominate the clinical presentation
Most common cardiac manifestations; widening of QRS complex, premature ventricular contractions, ventricular arrhythmia
Refractory hypotension is poor prognostic indicator, and is the most common cause of death in TCAs toxicity
Electrocardiography
A QRS duration > 100 ms identifies patients who risk for seizures and cardiac arrhythmia
An R wave in lead aVR of > 3 mm is independent predictor of toxicity
Electrocardiography (ECG) parameter is superior to measured serum of TCAs
Management
Stabilization of patient is the most important initial step specially protecting the airway, and ventilation support as needed, activated charcoal in appropriate patients
Obtain ECG as soon as possible
ECG indication for sodium bicarbonate therapy include: QRS duration > 100 ms, ventricular dysrhythmias and hypotension
Caustic Ingestion
Background
Strong acid and alkalis < 2 or > 12 pH can produce severe injury even in small-volume ingestion
Patient can have significant esophageal injury without visible oral burns.
Clinical presentation
Pain , drooling, vomiting, and abdominal pain
Difficulty in swallowing, or refusal to swallow
Stridor, and respiratory distress are common presenting symptoms
Esophageal stricture caused by circumferential burn and require repeated dilation or surgical correction
Management
Emesis and lavage are contraindicated
Endoscopy should be performed within 12–24 h in symptomatic patients, or on basis of history and characteristics of ingested products
Organophosphate and Insecticide Exposure
Clinical presentation
DUMBBELLS - Diarrhea, Urination, Miosis, Bradycardia, Bronchospasm, Emesis, Lacrimation, Lethargy, Salivation, and Seizures
Management
Wash all exposed skin with soap and water and immediately remove all exposed clothing
Fluid and electrolyte replacement, intubation, and ventilation, if necessary
Antidote is atropine and pralidoxime
Hydrocarbon Ingestion
Products contain hydrocarbon substances
Mineral spirits, kerosene, gasoline, turpentine, and others
Clinical presentation
Aspiration of small amount of hydrocarbons can lead to serious, and potentially, life-threatening toxicity
Pneumonitis is the most important manifestation of hydrocarbon toxicity
Benzene is known to cause cancer, most commonly acute myelogenous leukemia
Inhalants can cause dysrhythmias and sudden death including toluene, propellants, volatile nitrite, and the treatment is beta blocker
Management
Emesis and lavage are contraindicated
Activated charcoal should be avoided due to risk of inducing vomiting
Observation and supportive care, each child who is not symptomatic should be observed for at least 4–6 h in Emergency department (ED)
Neither corticosteroids or prophylactic antibiotics have shown any clear benefits
Methanol Ingestion
Toxicity primarily caused by formic acid
Clinical presentation
Drowsiness, nausea, and vomiting
Metabolic acidosis
Visual disturbances; blurred and cloudy vision, feeling being in snow storm, untreated cases can lead to blindness
Management
Methanol blood level and osmolar gap may be used as surrogate marker
IV fluids, glucose and bicarbonate as needed for electrolyte imbalances/dehydration
Fomepizole is the most preferred antidote for both methylene and ethylene glycol. Ethanol can be used if Fomepizole is unavailable
If > 30 ml methanol ingested, consider hemodialysis
Ethylene Glycol Ingestion (Antifreeze)
Clinical presentation
Nausea, vomiting, CNS depression, anion gap metabolic acidosis
Hypocalcemia, renal failure due to deposition of calcium oxalate crystals in the renal tubules
Management
Osmolar gap can be used to estimate ethylene glycol level
IV fluids, glucose and bicarbonate as needed for electrolyte imbalances/dehydration
Fomepizole the most preferred antidote for both methylene and ethylene glycol. Ethanol can be used if Fomepizole is unavailable
Carbon Monoxide Poisoning
Sources of CO
Wood-burning stove, old furnaces, and automobiles
Clinical presentation
Headache , malaise, nausea, and vomiting are the most common flu or food poisoning like early symptoms
Confusion, ataxia, syncope, tachycardia, and tachypnea at higher exposure
Coma, seizure, myocardial ischemia, acidosis, cardiovascular collapse, and potentially death in severe cases
Management
Evaluate for COHb level in symptomatic patients; arterial blood gas with CO level, creatine kinase in severe cases, and ECG in any patient with cardiac symptoms
100 % oxygen to enhance elimination of CO, use until CO < 10 % and symptoms resolve
Severely poisoned patient may benefit from hyperbaric oxygen specially if COHb > 25 %, significant CNS symptoms, or cardiac dysfunction
Iron Ingestion
Background
It is a common cause of pediatric poisoning.
Ingestion of > 60 mg/kg/dose is toxic
Clinical presentation
-
Gastrointestinal stage (30 min−6 h)
- Nausea, vomiting, and abdominal pain
- Hematemesis, and bloody diarrhea in severe cases
-
Stability stage (6–24 h)
- No symptoms: Patient must be observed during this stage
-
Systemic toxicity within (48 h)
- Cardiovascular collapse
- Severe metabolic acidosis
Hepatotoxicity and liver failure (2–3 days)
Gastrointestinal and pyloric scarring (2–6 weeks)
Management
-
Abdominal X-ray
- May show the pill
- Chewable and liquid form vitamins usually not visible
Serum iron < 300 mcg/dl in at hours is nontoxic
Iron blood level > 500 mcg/dl is toxic
Treatment
Chelation with IV deferoxamine if serum iron > 500 mcg/dl (Table 1)
Table 1.
Common antidotes for poisoning
| Poison | Antidote |
|---|---|
| Acetaminophen | N-Acetylcysteine (mucomyst) |
| Anticholinergics | Physostigmine |
| Benzodiazepines | Flumazenil |
| β-blockers | Glucagon |
| Calcium channel blockers | Insulin and calcium salts |
| Carbon monoxide | Oxygen |
| Cyanide | Nitrates |
| Digitalis | Digoxin-specific fragments antigen-binding(Fab) antibodies |
| Ethyleneglycol and methanol | Fomepizole |
| Iron | Deferoxamine |
| Isoniazid (INH) | Pyridoxine |
| Lead and other heavy metals, e.g., mercury and arsenic | BAL (dimercaprol) |
| Methemoglobinemia | Methylene blue |
| Opioids | Naloxone |
| Organophosphates | Atropine and pralidoxime |
| Salicylates | Sodium bicarbonate |
| Sulfonylureas | Octreotide |
| Tricyclic antidepressants | Sodium bicarbonate |
Head Trauma
Most head trauma are not serious and require only observation.
Physical signs of possible serious injuries
-
Basilar skull fracture
- Raccoon eyes
- Battle’s sign
- Hemotympanum
-
Temporal fracture
- Potential middle meningeal artery injury
- Hearing loss
- Facial paralysis
- Cerebrospinal fluid (CSF) otorrhea
- Facial paralysis
Scalp swelling or deep lacerations
Pupillary changes
-
Retinal hemorrhage and bruises
- In infant indicate possible abuse
Indication for head CT scan
Change in mental status
Loss of consciousness more than 1 min
Acute skull fracture
Bulging fontanelle
Signs of basilar skull fracture
Focal neurological sign
Seizures
Irritability
Persistent vomiting
Management of head trauma
Protection of airway if unresponsive or Glasgow Coma Scale less than 8
Intracranial pressure (ICP) monitoring
Maintain cerebral perfusion pressure at 40 mmHg
IV mannitol or 3 % saline if increased ICP
Mild hyperventilation
Control hyperthermia
Consult neurosurgery
Drowning
Drowning is a major cause in head injuries and death
-
Initial peak
- Toddler age group
-
Second peak
- Male adolescents
-
Children younger than 1 year of age
- Often drown in bathtubs, buckets, and toilets
-
Children 1–4 years of age
- Likely drown in swimming pools where they have been unsupervised temporarily (usually for < 5 min)
- Typical incidents involve a toddler left unattended temporarily or under the supervision of an older sibling
-
Adolescent and young adult age groups (ages 15–24 years)
- Most incidents occur in natural water
Approximately 90 % of drowning occur within 10 yards of safety
Parent should be within an arm’s length of a swimming child (anticipatory guidance)
Mechanism of injury
Initial swallowing of water
Laryngospasm
Loss of consciousness
Hypoxia
Loss of circulation
Ischemia
CNS injury (the most common cause of death)
Acute respiratory distress syndrome (ARDS) may develop
-
Salt water drowning classically associated with:
- Hypernatremia
- Hemoconcentration
- Fluid shifts and electrolyte disturbances are rarely seen clinically
-
Fresh water drowning classically associated with:
- Hyponatremia and hemodilution
- Hyperkalemia
- Hemoglobinuria and renal tubular damage
-
Management of drowning and near drowning
- Cardiopulmonary resuscitation (CPR) at the scene
- Admit regardless of clinical status
- All children with submersion should be monitored in the hospital for 6–8 h
- If no symptoms develop can be discharged safely
- 100 % oxygen with bag and mask immediately
- Nasogastric tube for gastric decompression
- Cervical spine immobilization if suspected cervical injuries
- Positive end expiratory pressure (PEEP) and positive pressure ventilations in case of respiratory arrest
- Continuous cardiac monitoring
- Bolus of normal saline or Ringer’s lactate
- Vasopressors
- Defibrillation if indicated
Wounds
General principles of wound care
The time and mechanism of injury because these factors relate to subsequent management options.
Accidental or non-accidental trauma
The timing of the injury may affect management (lacerations > 8–24 h old may not be repaired depending on location).
Acute wounds often can be repaired primarily
Older wounds may require delayed primary closure or healing by secondary intention
Hemostasis
Persistent bleeding despite direct pressure can be controlled with the careful application of a tourniquet above the injury
The use of tourniquets may lead to ischemia, and the need for a tourniquet can indicate a more severe soft tissue or vascular injury that may require surgery
Blood pressure cuff inflated to suprasystolic pressures is effective
-
Local infiltration with lidocaine containing epinephrine; except:
- Digits
- Ears
- Nose
- Penis
Wound cleaning
Decontamination of the wound is the most important step in preventing infectious complications.
Irrigation.
Removal of foreign material from the wound is essential to minimize the risk of infection
Dressings
Once the wound has been evaluated, decontaminated, and repaired, an appropriate dressing should be applied
Topical antibiotic ointments (e.g., bacitracin) and an occlusive dressing (moist wound heals better)
Dressings can be left in place for 24–48 h and then changed once or twice daily
Wounds that cross joints may require splinting or bulky dressings to minimize movement and tension on the wound
Prophylaxis
All children who have cutaneous wounds should have their tetanus status reviewed and appropriate prophylaxis administered
Empiric use of antibiotics is not indicated except bites
Puncture Wounds
Background
Most are plantar puncture wounds from nails, punctures also can occur in other parts of the body.
Immediate evaluation should assess for any life-threatening injuries, especially for puncture wounds of the head, neck, chest, and abdomen
Particular attention should be paid to wound depth, possible retained foreign bodies, and risk of infection
Evaluation
Timing and mechanism of the injury
Puncture wounds that are older than 6 h, occur from bites, have retained foreign body or vegetative debris, or extend to a significant depth have a higher risk of infection
Radiography may help identify a retained foreign body or fracture
Ultrasonography is a convenient, radiation-free, and highly sensitive modality for identifying retained foreign bodies
Management
Most puncture wounds can be managed in the outpatient setting with an antibiotic, dressing and warm soaks
Most infected puncture wounds are caused by S. aureus or S. pyogenes, and respond to oral antibiotics
Infected puncture wounds that result from a nail through a tennis shoe should be evaluated for possible pseudomonas aeruginosa infection
Additional imaging and intravenous antibiotics may be necessary to treat more serious infections, including cellulitis, abscess, osteochondritis, and osteomyelitis
Surgical consultation for potential debridement or retained foreign body removal should be considered for wounds refractory to medical management
Lacerations
Laceration is a traumatic disruption to the dermis layer of the skin
The most common anatomic locations for lacerations are the face (~ 60 %) and upper extremities (~ 25 %)
Evaluation
An evaluation for life-threatening injuries is the first priority
Ongoing bleeding that may cause hypovolemic shock
Applying direct pressure usually is successful
Sphygmomanometer may be used for up to 2 h on an extremity
Ring tourniquet on a digit for up to 30 min to help control ongoing blood loss
Lacerations of the neck should be evaluated for deeper structural injuries
If developmentally appropriate, two-point discrimination at the finger pads provides the best assessment of digital nerve function
It is critical to identify foreign material within the laceration
Anesthetics and anxiolysis
The use of the topical anesthetic LET (4 % Lidocaine, 1:2000 Epinephrine, and 0.5 %Tetracaine) has been shown to be effective and to reduce length of stay
LET usually is effective 20–30 min after application to a laceration site on the face but often needs twice that amount of time to be effective elsewhere
Blanching of the site after application most often indicates achievement of effective anesthesia
A local anesthetic also may be used to prepare for placement of sutures
Closure of lacerations
Dermabond: It is critical that the laceration be dry and well approximated to avoid application below the epidermal surface, which may cause the wound to gape open or lead to a “Dermabond Oma”
Evenly spaced suture placement: The general rule is sutures should be spaced the same distance as they are placed from the wound edge. For irregular wound shapes, approximate the midpoint of the wound first and then work laterally
Lip lacerations
Lip laceration require special care if the injury crosses the vermilion border
It is essential to approximate the vermilion border with a suture. Failure to do so may result in a poor cosmetic outcome
An infraorbital or mental nerve block along the lower gum line may be considered to reduce tissue distortion for lip lacerations, including those through the vermilion border
Lacerations of the nail bed
It may be painful and produce anxiety for the child and parent
A digital nerve block should be applied to provide adequate analgesia for this injury
If the nail has been removed during the injury, the nail bed should be repaired with absorbable sutures by using a reverse cutting needle
The nail should be placed under the eponychium (cuticle) to preserve this space
If a nail is not available, a small piece of sterile aluminum foil from the suture pack may be used as a substitute for 3 weeks
If possible, a small hole can be placed in the nail plate to allow for drainage and to avoid a subungual hematoma
The nail can be secured with tissue adhesive and tape adhesive
Approximately half of all nail bed injuries are associated with a fracture of the distal phalanx
No evidence that antimicrobial prophylaxis reduces the rate of infection
Most hand surgeons recommend a 3- to 5-day course of antibiotic (e.g., cephalexin)
Wrapping dressings too tightly around the digit should be avoided because this may cause tissue ischemia and infarction
Daily dressing changes are recommended to evaluate the wound
Removal times for sutures (sutures removed before 7 days are unlikely to leave suture tracks)
Face 3–5 days
Scalp 5–7 days
Trunk 5–7 days
Extremities 7–10 days
Joints 10–14 days
Animal and Human Bites
Dog Bites
Dog bite causes a crushing-type wound.
Extreme pressure of dog bite may damage deeper structures such as bones, vessels, tendons, muscle, and nerves.
Cat Bites
The sharp pointed teeth of cats usually cause puncture wounds and lacerations that may inoculate bacteria into deep tissues
Infections caused by cat bites generally develop faster than those of dogs
Other Animals
Foxes, raccoons, skunks, and bats exposure are a high risk for rabies
Human Bites
Three general types of injuries can lead to complications:
Closed-fist injury
Chomping injury to the finger
Puncture-type wounds about the head caused by clashing with a tooth
Common bacteria involved in bite wound infections include the following:
Dog bites
Staphylococcus species
Eikenella species
Pasteurella species
Cat bites
Pasteurella species
Bacteroides species
Human bites
Eikenella Corrodens
Staphylococcus, Streptococcus
Staphylococcus aureus is associated with some of the most severe infections
-
Human bites can transmit the following organism:
- Hepatitis B, hepatitis C, herpes simplex virus (HSV), and syphilis
Clinical presentation
Time and location of event
Type of animal and its status (i.e., health, rabies vaccination history, behavior,)
Circumstances surrounding the bite (i.e., provoked or defensive bite versus unprovoked bite)
Location of bites (most commonly on the upper extremities and face)
Laboratory
Fresh bite wounds without signs of infection do not need to be cultured
Infected bite wounds should be cultured to help guide future antibiotic therapy
CBC and blood culture if clinically required.
Imaging studies
Radiography is indicated if any concerns exist that deep structures are at risk (e.g., hand wounds, deep punctures, crushing bites, especially over joints)
Management
-
Debridement and removing devitalized tissue
- It is an effective means of preventing infection
-
Irrigation
- In general, 100 ml of irrigation solution per centimeter of wound is required with normal saline
-
Primary closure
- It may be considered in limited bite wounds that can be cleansed effectively (this excludes puncture wounds, i.e., cat bites)
- Other wounds are best treated by delayed primary closure
-
Facial wounds
- Because of the excellent blood supply, are at low risk for infection, even if closed primarily.
- The risk of infection must be discussed with the patient prior to closure
General management of bites
Fresh bite wounds without signs of infection do not need to be cultured
Infected bite wounds should be cultured to help guide future antibiotic therapy
Local public health authorities should be notified of all bites and may help with recommendations for rabies prophylaxis
Consider tetanus and rabies prophylaxis for all wounds
Antibiotic therapy
All human and animal bites should be treated with antibiotics.
The choice between oral and parenteral antimicrobial agents should be based on the severity of the wound and on the clinical status of the victim
Oral Amoxicillin–Clavulanate is an excellent choice for empirical oral therapy for human and animal bite injuries
Parenteral Ampicillin–Sulbactam is the drug of choice in severe cases
If patient is allergic to penicillin, clindamycin in combination with trimethoprim/sulfamethoxazole can be given
Antirabies treatment may be indicated for the following: If stray dog, not captured and dog not provoked prior to attack not captured, or known dogs found to have rabies within 10 days of bite, or any dog or animal proven to have rabies.
Snake Bites
Background
-
Most snakebites are non poisonous and are delivered by non poisonous species.
- North America is home to 25 species of poisonous snakes
- Characteristics of most poisonous snakes
- Triangular head
- Elliptical eyes
- Pit between the eyes and nose
- For example, rattlesnakes, cotton mouth and copperh eads
- Few snakes with round head are venomous, e.g., coral snakes (red on yellow bands)
Clinical presentation
-
Local manifestation
- Local swelling, pain, and paresthesias may be present
- Soft pitting edema that generally develops over 6–12 h but may start within 5 min
- Bullae
- Streaking
- Erythema or discoloration
- Contusions
-
Systemic toxicity
- Hypotension
- Petechiae, epistaxis, hemoptysis
- Paresthesias and dysesthesias—Forewarn neuromuscular blockade and respiratory distress (more common with coral snakes).
- The time elapsed since the bite is a necessary component of the history
- Determine history of prior exposure to antivenin or snakebite. (this increases risk and severity of anaphylaxis).
- Assessment of vital signs, airway, breathing, and circulation
Laboratory
CBC with differential and peripheral blood smear
Coagulations profile
Fibrinogen and split products
Blood chemistries, including electrolytes, blood urea nitrogen (BUN), creatinine
Urinalysis for myoglobinuria
Arterial blood gas determinations and/or lactate level for patients with systemic symptoms
Radiography
Baseline chest radiograph in patients with pulmonary edema
Plain radiograph on bitten body part to rule out retained fang
Management
Prehospital care
Monitor vital signs and airway
Restrict activity and immobilize the affected area
Immediately transfer to definitive care
Do not give antivenin in the field
Indication for antivenom
Hemodynamic or respiratory instability
Abnormal coagulation studies
Neurotoxicity, e.g., paralysis of diaphragm
Evidence of local toxicity with progressive soft tissue swelling
Antivenom is relatively specific for snake species against which they designed to protect
There is no benefit to administer antivenom to unrelated species due to risk of anaphylaxis and expenses as well
Orthopedic consultation
Surgical assessment focuses on the injury site and concern for the development of compartment syndrome
Fasciotomy is indicated only for those patients with objective evidence of elevated compartment pressure
Bitten extremities should be marked proximal and distal to the bite and the circumference at this location should be monitored every 15 min to monitor for progressive edema and compartment syndrome
Black Widow Spider Bite
Background
Black spider with bright-red or orange abdomen
Neurotoxin acts at the presynaptic membrane of the neuromuscular junction, and decreased reuptake of acetylcholine and severe muscle cramping
Clinical presentation
Pricking sensation that fades almost immediately
Uncomfortable sensation in the bitten extremity and regional lymph node tenderness
A “target” or“ halo” lesion may appear at the bite site
Proximal muscle cramping, including pain in the back, chest, or abdomen, depending on the site of the bite
Dysautonomia that can include nausea, vomiting, malaise, sweating, hypertension , tachycardia, and a vague feeling of dysphoria
Management
-
Analgesics should be administered in doses sufficient to relieve all pain
- Oral medications may be tried for minor pain
- Intravenous opioid analgesics , such as morphine or meperidine, should be administered to all patients who are experiencing significant pain
- Benzodiazepines are adjunctive to the primary use of analgesics
Hydration and treatment of severe hypertension
-
Hypertension
- Frequently, adequate analgesia alleviates hyperten sion
- Dangerous hypertension is rare, but if it is present despite adequate analgesia, nitroprusside or antivenin should be considered
Brown Recluse Spider
Background
Dark, violin-shaped mark on the thorax
Venom causes significant local skin necrosis
Clinical presentation
Almost painless bite, and only rarely is a spider recovered
Erythema, itching, and swelling begin 1 to several hours after the bite
Central ischemic pallor to a blue/gray irregular macule to the development of a vesicle
The central area may necrose, forming an eschar
Induration of the surrounding tissue peaks at 48–96 h
Lymphadenopathy may be present
The entire lesion resolves slowly, often over weeks to months
Management
Tetanus status should be assessed and updated
Signs of cellulitis treated with an antibiotic that is active against skin flora
Treatment is directed at the symptoms
Scorpion Stings
Background
The only scorpion species of medical importance in the USA is the Arizona bark scorpion ( Centruroides Sculpturatus).
Toxins in its venom interfere with activation of sodium channels and enhance firing of axons.
Clinical presentation
Local pain is the most frequent symptom
Usually no local reaction
-
In small children
- Uncontrolled jerking movements of the extremities
- Peripheral muscle fasciculation, tongue fasciculation, facial twitching, and rapid disconjugate eye movements
- May misdiagnosed as experiencing seizures
-
Severe reaction
- Agitation
- Extreme tachycardia
- Salivation
- Respiratory distress
Management
Maintenance of a patent airway and mechanical ventilation in severe cases
-
Victims may be managed solely with supportive care:
- Analgesia and sedation
- Airway support and ventilation
- Supplemental oxygen administration
Antivenin therapy also may obviate or reduce the need for airway and ventilatory support
Status Epilepticus
Status epilepticus (SE) is defined as a seizure that lasts more than 30 min
Treatment of SE should be based on an institutional protocol, such as the following :
Management
-
Initial management
- Attend to the ABCs before starting any pharmacologic intervention
- Place patients in the lateral decubitus position to avoid aspiration of emesis and to prevent epiglottis closure over the glottis
- Make further adjustments of the head and neck if necessary to improve airway patency
- Immobilize the cervical spine if trauma is suspected
- Administer 100 % oxygen by facemask
- Assist ventilation and use artificial airways (e.g., endotracheal intubation) as needed
- Suction secretions and decompress the stomach with a nasogastric tube
- Carefully monitor vital signs, including blood pressure
- Carefully monitor the patient’s temperature, as hyperthermia may worsen brain damage
- In the first 5 min of seizure activity, before starting any medications, try to establish IV access and to obtain samples for laboratory tests and for seizure medications
- Infuse isotonic IV fluids plus glucose at a rate of 20 ml/kg/h (e.g., 200 ml D5NS over 1 h for a 10-kg child)
- In children younger than 6 years, use intraosseous (IO) infusion if IV access cannot be established within 5–10 min
-
Laboratory
- Finger stick blood glucose
- If serum glucose is low or cannot be measured, give children 2 ml/kg of 25 % glucose
- If the seizure fails to stop within 4–5 min, prompt administration of anticonvulsants may be indicated
- BMP and other lab depending on the history and physical examination
-
Anticonvulsant medication: Selection can be based on seizure duration as follows:
- 6–15 min: Lorazepam (0.05–0.1 mg/kg IV or IO slowly infused over 2–5 min); or diazepam per rectum at 0.5 mg/kg, not to exceed 10 mg
- 16–35 min: Phenytoin (Dilantin) or fosphenytoin (15–20 mg or PE/Kg max 1500 mg), not to exceed infusion rate of 1 mg/kg/min; do not dilute in D5 W; if unsuccessful, phenobarbital 15–20 mg/kg IV; increase infusion rate by 100 mg/min; phenobarbital may be used in infants before phenytoin
- 45–60 min: Pentobarbital anesthesia (patient already intubated); or midazolam, loading dose 0.1–0.3 mg/kg IV followed by continuous IV infusion at a rate of 0.1–0.3 mg/kg/h
- Pentobarbital anesthesia is administered as follows:
- Loading dose: 5–7 mg/kg IV
- May repeat 1-mg/kg to 5-mg/kg boluses until EEG exhibits burst suppression; closely monitor hemodynamics and support blood pressure as indicated
- Maintenance dose: 0.5–3 mg/kg/h IV; monitor EEG to keep burst suppression pattern at 2–8 bursts/min
- Other specific treatments may be indicated if the clinical evaluation identifies precipitants of the seizures. Selected agents and indications are as follows:
- Naloxone—0.1 mg/kg/dose, IV preferably (if needed may administer IM or SQ) for narcotic overdose
- Pyridoxine—50–100 mg IV/IM for possible dependency, deficiency, or isoniazid toxicity
- Antibiotics—If meningitis is strongly suspected, initiate treatment with antibiotics prior to CSF analysis or CNS imaging
Burns
First-degree burn
Superficial, dry, painful to touch, and heals in less than 1 week
Second-degree burn
Partial thickness and pink or possibly mottled red
Exhibits bullae or frank weeping on the surface
Usually is painful unless classified as deep and heals in 1–3 weeks
Second-degree burns commonly are caused by scald injuries and result from brief exposure to the heat source
Third-degree burn
It is the most serious
Pearly white, charred, hard, or parchment-like
Dead skin (eschar) is white, tan, brown, black, and occasionally red
Superficial vascular thrombosis can be observed
Electrical burns
Superficial burns can be associated with deep tissue injuries and complications
-
Complications of electric burns
- Cardiac arrhythmia
- Ventricular fibrillation
- Myocardial damage
- Myoglobinuria
- Renal failure
- Neurologic damage can develop up to 2 years following an electrical burn
- Guillain–Barré syndrome
- Transverse myelitis
- Amyotrophic lateral sclerosis
- Paresis
- Paralysis
- Eye injuries
- Cataracts are the most common complications
- Fractures and joint dislocation can occur
Management
The superficial burn wound that extends to less than 10 % total body surface area (TBSA) usually can be treated on an outpatient basis unless abuse is suspected
-
Cotton gauze occlusive dressing to protect the damaged skin from bacterial contamination:
- Eliminate air movement over the wound (thus reducing pain)
- Decrease water loss
- Dressings are changed daily
-
Topical antimicrobial agent should be applied to the wound prior to the dressing for prophylaxis, e.g., silver sulfadiazine
- Silver sulfadiazine has activity against Staphylococcus aureus, Escherichia coli, Klebsiella spp, Pseudomonas aeruginosa, Proteus spp, and Candida albicans
- The primary adverse effect of silver sulfadiazine is leukopenia, which occurs in 5–15 % of treated patients
Application of various wound membrane dressings can promote healing with less painful wound dressing changes
Initial treatment of a child who has extensive burns
Fluid resuscitation to prevent shock
Early excision and grafting of the burn wound coupled with early nutrition support
Identification of airway involvement due to inhalation injury
Measures to treat sepsis
-
Fluid Administration
- Once the nature and extent of injury are assessed, fluid resuscitation is begun.
- Two large-bore intravenous catheters
-
Parkland Formula for fluid requirements
- ◦ 4 ml/kg/day for each percent of body surface area (BSA) burned
- The first half of the fluid load is infused over the first 8 h post-burn
- The remainder is infused over the ensuing 16 h
- The infusion rates should be adjusted to maintain a urine flow of 1 ml/kg per hour
- During the second 24 h, fluid administration is reduced 25–50 %
Resuscitation
ABCs
Stabilize airway, be sure it is patent
Place on oxygen, determine if patient requires assisted ventilations
Chest compressions if no heartbeat or if < 60 bpm (< 80 in infants and not increasing with ventilation)
IV fluids 20 ml/kg normal saline or lactated ringers
Shock
Goals—improve tissue perfusion, improve metabolic imbalance, restore end-organ function.
-
Types
- Hypovolemic—dehydration, blood loss
- Distributive—anaphylaxis, neurogenic, sepsis
- Cardiogenic—poor cardiac function
- Obstructive—cardiac tamponade, tension pneumothorax
-
Treatment
- Position—trendelenburg may be helpful
- Oxygen
- IV access
- Fluid resuscitation—20 ml/kg bolus crystalloid if not improving after 2–3 boluses consider packed red blood cells (PRBC) may use less fluid in cardiogenic shock
- Vasopressors if refractory to fluids
- Warm shock (septic)—norepinephrine
- Normotensive shock—dopamine
- Hypotensive shock—epinephrine
- Adrenal insufficiency—fluid refractory and pressor dependent shock should make you suspect adrenal insufficiency
- If suspected give hydrocortisone 2 mg/kg (100 mg max)
- Septic shock—antibiotics
- Anaphylaxis—epinephrine, diphenhydramine, H2 blockers and steroids
-
Monitoring
- Cardiopulmonary status
- Temperature
- Mental status
- Urine output
- Labs help with end-organ function assessment and for sepsis evaluation
Tachycardias with Pulse
-
Sinus—narrow complex, determine cause and treat accordingly
-
Causes 4 H’s and 4 T’s plus pain
- ◦ Hypoxemia, hypovolemia, hypothermia, hypo/hype rkalemia–metabolic
- ◦ Tension pneumothorax, tamponade, toxins, throm boembolism
-
-
Supraventricular— > 220 infants and > 180 children, usually narrow complex, no p waves, consistent rate
- Adenosine if stable 0.1 mg/kg (6 mg max) if unsuccessful 0.2 mg/kg (12 mg max), rapid push
- Synchronized cardioversion if unstable 0.5–1 J/kg increase to 2 J/kg (Fig. 2)
-
Ventricular tachycardia—wide complex tachycardia—sharks tooth appearance
- Establish cause and treat if stable
- Synchronized cardioversion 0.5–1 J/kg if unsuccessful 2 J/kg
- Amiodarone 5 mg/kg, lidocaine and procainamide are other options
-
Torsades de pointes—ventricular tachycardia with oscillating amplitudes
- IV Magnesium 25–50 mg/kg (max 2 g) if cardiovascularly stable
- Defibrillation if unstable 2 J/kg increase to 4 J/kg if lower dose unsuccessful
Fig. 2.
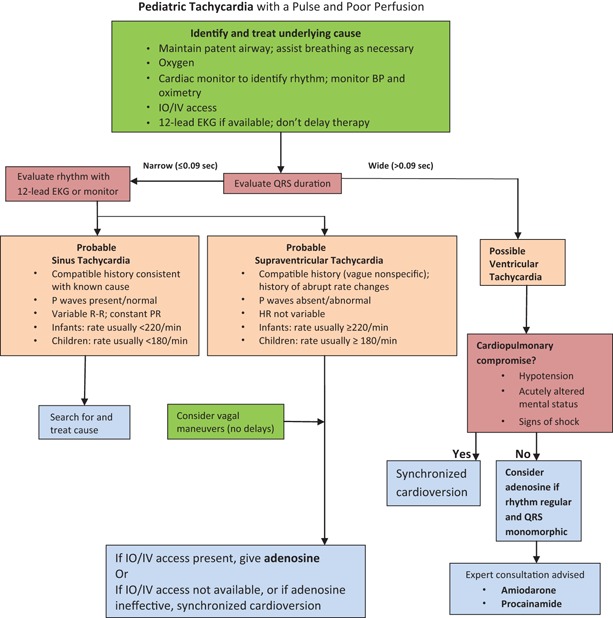
Pediatric advance life support tachycardia algorithm. HR heart rate, IV intravenous, IO intraosseous, EKG electrocardiogram. (Kleinman ME et al. American Heart Association guideline for cardiopulmonary resuscitation and emergency cardiovascular care, part 14. Circulation 2010, 122, suppl. 3, pp. S876–S908, Fig. 3, p. S888)
Tachycardia without Pulse
-
Asystole—no electrical activity will look like flat line on monitor
- CPR and epinephrine 0.1 ml/kg (1:10,000)
-
Pulseless electrical activity (PEA)—may look like sinus tachycardia but with no pulse (no ventricular contractions)
- CPR and epinephrine 0.1 ml/kg (1:10,000)
-
Ventricular tachycardia (without pulse) or ventricular fibrillation
- CPR
- Defibrillate 2 J/kg increase to 4 J/kg if initial unsuccessful
- Add epinephrine after second defibrillation if unsuccessful
- Defibrillation followed by epinephrine each round every 3–5 min
- Amiodarone and lidocaine can be considered after epinephrine attempted
-
Bradycardia—most common pre-arrest rhythm in children with hypotension, hypoxemia and acidosis (Fig. 3)
-
Sinus bradycardia
- ◦ Maybe non-pathologic in case of well conditioned individuals like athletes
- ◦ Causes include: hypothermia, hypoglycemia , hypoxia, hypothyroidism, electrolyte imbalance, toxic ingestion, head injury with raised ICP
- ◦ Treatment—identify cause and treating that condition
- ◦ HR < 60 bpm in a child who is a well-ventilated patient, but showing poor perfusion, chest compression should be initiated
- ◦ If HR remains below 60 despite adequate ventilation and oxygenation, then epinephrine or atropine (0.02 mg/kg—0.1 mg min and 0.5 mg max) should be given
- ◦ Symptomatic bradycardia unchanged by above may require pacing
-
-
AV mode blocks
-
First degree—prolonged PR interval
- ◦ Generally asymptomatic
-
Second degree—2 types
-
◦ Type 1—Wenckebach
- ▪ Progressive PR prolongation until no QRS propagated
-
◦ Type 2—regular inhibition of impulse
- ▪ Usually every other P results in QRS
- Third degree—complete dissociation between P and QRS
-
Reversible causes of cardiac arrest (Fig. 4)
- ◦ Hypovolemia
- ◦ Hypoxia
- ◦ Hydrogen ion (acidosis)
- ◦ Hypoglycemia
- ◦ Hypo-/hyperkalemia
- ◦ Tension pneumothorax
- ◦ Tamponade cardiac
- ◦ Toxins
- ◦ Thrombosis, pulmonary
- ◦ Thrombosis, coronary
-
-
Fig. 3.
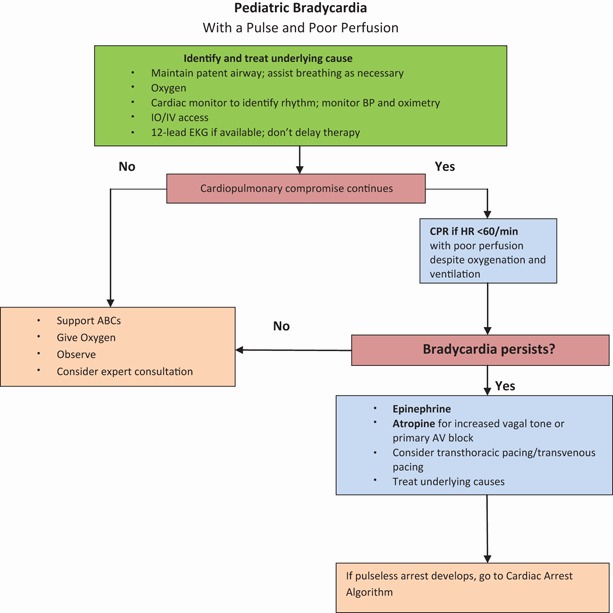
Pediatric advance life support bradycardia algorithm. IV intravenous, IO intraosseous, ABCs airway, breathing, and circulation, AV atrioventricular (conductor), EKG electrocardiogram, HR heart rate, BP blood pressure, CPR cardio-pulmonary resuscitation. (Kleinman ME et al. American Heart Association guideline for cardiopulmonary resuscitation and emergency cardiovascular care, part 14. Circulation 2010, 122, suppl 3, pp. S876–S908, Fig. 2, p. S887)
Fig. 4.
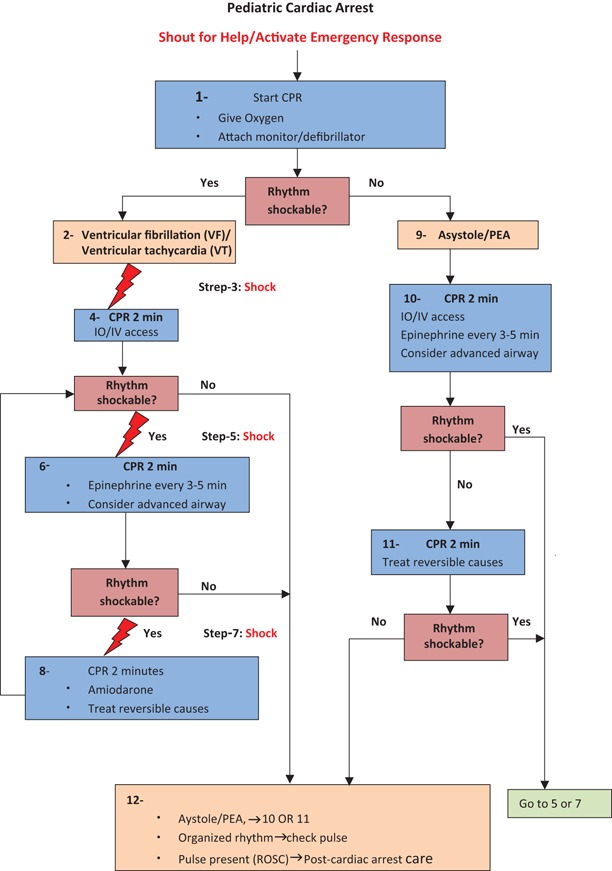
Pediatric advance life support bradycardia algorithm. ROSC return of spontaneous circulation, IV intravenous, IO intraosseous, CPR cardio-pulmonary resuscitation. (Kleinman ME et al. American Heart Association guideline for cardiopulmonary resuscitation and emergency cardiovascular care, part 14. Circulation 2010, 122, suppl 3, pp. S876–S908, Fig. 1, p. S885)
Contributor Information
Osama Naga, Email: osamanaga@yahoo.com.
Steven L. Lanski, Email: steven1.lanski@tenethealth.com.
Osama Naga, Email: osama.naga@ttuhsc.edu.
Suggested Readings
- 1.Graeme KA. Toxic plant ingestions. Wilderness medicine. 5. Philadelphia: Mosby; 2007. [Google Scholar]
- 2.O’Donnell KA, Ewald MB. Poisoning. In: Kliegman RM, Stanton BF, St. Geme JW, Schor NF, Behrman RE, editors. Nelson Text book of pediatrics. 19. Philadelphia: Elsevier Saunders; 2011. pp. 250–47. [Google Scholar]
- 3.Wingert WA, Chan L. Rattlesnake bites in southern California and rationale for recommended treatment. West J Med. 1988;148:37. [PMC free article] [PubMed] [Google Scholar]
- 4.Clark RF, Kestner SW, Vance MV. Clinical presentation and treatment of black widow spider envenomation: a review of 163 cases. Ann Emerg Med. 1992;21:782–7. doi: 10.1016/S0196-0644(05)81021-2. [DOI] [PubMed] [Google Scholar]
- 5.Wright SW, Wrenn KD, Murray L, Seger D. Clinical presentation and outcome of brown recluse spiderbite. Ann Emerg Med. 1997;30:28–32. doi: 10.1016/S0196-0644(97)70106-9. [DOI] [PubMed] [Google Scholar]
- 6.Curry SC, Vance MV, Ryan PJ. Envenomation by the scorpion Centruroides Sculpturatus. J ToxicolClinToxicol. 1984;21:417–49. doi: 10.3109/15563658308990433. [DOI] [PubMed] [Google Scholar]
- 7.Epilepsy Foundation of America. ’. s Working Group on Status Epilepticus Treatment of convulsive status epilepticus. Recommendations of the Epilepsy Foundation of America’s Working Group on Status Epilepticus. JAMA. 1993;270:854–9. doi: 10.1001/jama.1993.03510070076040. [DOI] [PubMed] [Google Scholar]
- 8.Herndon DN. Total burn care. 2. London: Saunders; 2002. [Google Scholar]
- 9.Nichols DG, Yaster M. Golden hour: handbook of pediatric advanced life support. St Louis: Mosby; 1996. [Google Scholar]
- 10.Chameides L, Samson RA. Pediatric advanced life support. Dallas: American Heart Association; 2012. [Google Scholar]


