Abstract
Psoriasis is a chronic, common, inflammatory skin disease. The classic skin lesions can be described as sharply demarcated, scaly, erythematous plaques often found on the extensor surfaces. Several variants of psoriasis have also been described, including palmoplantar, pustular, erythrodermic, and guttate forms. Although psoriasis is usually diagnosed clinically, characteristic histologic findings include hyperkeratosis, parakeratosis, and acanthosis of the epidermis with dilated blood vessels and a lymphocytic infiltrate. Psoriasis is an immune-mediated disease, and although the etiology is not fully understood, genetic and environmental factors have been implicated. Importantly, psoriasis is associated with a number of systemic complications and comorbidities that have a high impact on affected patients.
Keywords: Psoriasis, Diagnosis, Histopathology, Erythrodermic psoriasis, Guttate psoriasis, Pustular psoriasis
Introduction and Epidemiology
Psoriasis is a common, chronic inflammatory skin disease that is characterized by the formation of sharply demarcated, scaly, erythematous plaques. It is a prevalent disease, both in the USA and globally. According to the large population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis (MAPP) survey, the prevalence of psoriasis ranges from 1.4% in Spain to 3.3% in Canada, with an overall prevalence of 1.9%. The prevalence in the USA is slightly higher than the average at 2.2% [1]. Worldwide, the prevalence has been found to vary both geographically and among different ethnic groups within the same region and is overall reported at higher rates in locations distant from the equator [2, 3].
Psoriasis can present at any age. However, the disease onset appears to follow a bimodal distribution, peaking around 20–30 years of age and again around 50–60 years of age [4]. A family history of the disease is common. Approximately 30% of patients have a first-degree relative with psoriasis, and the risk of psoriasis increases with the number of affected relatives a patient has [5]. Some studies suggest that this bimodal distribution represents two distinct forms of psoriasis; compared to patients whose psoriasis presents later in life, patients with early onset psoriasis are much more likely to possess a genetic marker that is highly associated with psoriasis and to have a parent with psoriasis. Earlier onset psoriasis is also associated with more severe disease [4]. In most cases, the disease waxes and wanes throughout a patient’s life, and spontaneous remission without treatment is unlikely [6].
The plaques of psoriasis can be disfiguring and severely pruritic and/or painful. Itching is often the most bothersome symptom of psoriasis [1]. Quality of life can be substantially affected, and many psoriasis patients report a significant social and emotional burden along with the negative impact of psoriasis on their physical well-being [7, 8]. Functional disability due to psoriasis is comparable or even greater compared to those seen in other serious diseases including cancer, depression, and heart disease [9].
In the MAPP survey, there was a 2-year median delay from symptom onset to time of diagnosis. In terms of disease severity, approximately 30% of psoriasis patients and 50% of those with both psoriasis and psoriatic arthritis rated their disease as severe. Despite this, nearly half of psoriasis patients had not seen a physician in the past year, and many were on either no treatment or topical therapy alone. One of the reasons for this undertreatment was lack of tolerability or efficacy of available oral or biologic agents [1]. These statics highlight the importance of improving disease detection and the need for improved therapeutic choices.
Associated Conditions and Complications
In recent years, the impact of psoriasis has been found to extend beyond the skin, and psoriasis has been found to be associated with a variety of systemic conditions. Approximately 75% of patients will have at least one comorbid condition, and many will have multiple comorbidities [10]. The association is thought to be due to the chronic inflammatory changes and elevated proinflammatory cytokines found in psoriasis that lead to a systemic inflammatory state.
The most well-recognized associated condition is psoriatic arthritis, a seronegative inflammatory arthritis. The exact proportion of patients with psoriasis who will develop psoriatic arthritis is unknown but is estimated to be <10 to 40%. Psoriatic arthritis typically occurs in patients who have had preexisting skin findings of psoriasis for 5–12 years; however, approximately 20% of patients will present with joint symptoms first [1, 11]. The most common presentation of psoriatic arthritis is polyarticular peripheral arthritis but can vary widely with peripheral and/or axial, monoarticular, or polyarticular patterns. The severity of psoriatic arthritis can also vary drastically among individuals but does not necessarily correlate with the severity of skin findings. At its most severe, the arthritis can be erosive and deforming (arthritis mutilans) [11]. Even among psoriasis patients without a diagnosis of psoriatic arthritis, 50% report joint pain [10]. Given the high prevalence and disease burden of psoriatic arthritis, it is important to screen for arthritis symptoms in every patient with psoriasis at each visit [11].
Of notable concern, psoriasis is also associated with an increased risk of cardiovascular disease. Psoriasis patients are more likely to have cardiovascular risk factors including diabetes mellitus (especially type 2), obesity, hyperlipidemia, hypertension, and tobacco and alcohol abuse [12–14]. However, psoriasis patients have been found to have an increased risk of myocardial infarction even after controlling for these cardiovascular risk factors, signifying that psoriasis itself may be an independent risk factor for cardiovascular disease. The risk of cardiovascular disease appears to be highest in patients with more severe psoriasis at a younger age [15, 16]. Other significant associated conditions include depression, autoimmune diseases, Parkinsonism, and cancers, such as skin cancers and lymphomas [6, 17, 18].
Overview of Pathogenesis
The pathophysiology of psoriasis is characterized by excessive epidermal growth and altered keratinocyte differentiation. The underlying pathogenesis is multifactorial and complex with genetic, immunologic, and environmental contributions. Certain environmental triggers are thought to disrupt the homeostasis of the skin immune system in genetically predisposed individuals [19]. Medications implicated in the induction and exacerbation of psoriasis include angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), antimalarials, lithium, and nonsteroidal anti-inflammatory drugs [20–22]. Despite the association with ACE inhibitors and ARBs, a population-based case-control study found that beta-blockers and other anti-hypertensives are not associated with psoriasis [23]. Other potential triggers include infections (i.e., human immunodeficiency virus [HIV] and streptococcus) and trauma to the skin (the Koebner phenomenon) [20, 24].
In recent years, a variety of genes have been identified that predisposes an individual to psoriasis, many of which involve mediators of immune signaling pathways, emphasizing the importance of the immune system in the pathogenesis of psoriasis [25–28]. Early genetic linkage studies identified a major genetic determinant of psoriasis in the susceptibility-1 locus (PSORS1) of the major histocompatibility complex (MHC). Later, the human leukocyte antigen (HLA)-Cw6 was identified as the diseased allele at PSORS1 [26]. In recent years, genome-wide association studies have identified 63 genes that account for approximately 28% of the heritability of psoriasis. These genes include those of inflammatory interleukins and immune mediators [27]. In particular, a review of single-nucleotide polymorphism (SNP) analyses from multiple studies has shown an association between psoriasis and the loci for the T-helper type 2 (Th2) pathway (including interleukin [IL]-4 and IL-13), the T-helper type 17 (Th17) pathway (including subsets of IL-12 and IL-23), innate immune signaling pathways for nuclear factor kappa-light-chain-enhancer of activated B cells (NFkB) and interferons (IFN), and adaptive immune pathways involving CD8 T cells [28].
Although early research focused on aberrant keratinocyte activity as the primary cause of psoriasis, more recent studies have shown that psoriasis is an immune-mediated disease, as the skin inflammation of psoriasis is dependent on immune cells and their cytokines [29]. This has been supported by the genetic studies mentioned above. Abnormal activation of inflammatory mediators from the innate and adaptive immune systems has been implicated in the pathogenesis of psoriasis. Involved cells include keratinocytes, dendritic cells, and T cells, and important inflammatory mediators include tumor necrosis factor (TNF)-α, IL-17, IL-12, and IL-23 [30]. Recent advances in understanding the underlying inflammatory mechanisms have been pivotal in the development of new and more efficacious targeted therapies such as TNF-α, IL-12 and/or -23, and IL-17 inhibitors.
Diagnosis
Psoriasis is a clinical diagnosis, and a skin biopsy is usually not necessary for classic presentations of the disease. The characteristic lesions are sharply demarcated, scaly, erythematous plaques. The plaques may be pruritic and/or painful. They can be ovoid, round, or irregular in morphology and are often symmetrically distributed. When the xerotic scale is removed with scraping, points of fine bleeding may be seen (the “Auspitz sign”). Lesions may develop at sites of trauma or injury, known as the Koebner phenomenon.
The plaques are most frequently found on the extensor surfaces (elbows and knees), the scalp, and the intergluteal cleft. The palms and soles may be affected in the variants of palmoplantar psoriasis and palmoplantar pustulosis. Other forms of psoriasis include generalized pustular, guttate, erythrodermic, and inverse psoriasis.
The extent and severity of psoriasis can be measured using the Psoriasis Area and Severity Index (PASI), which includes evaluations of body surface area (BSA) involvement, erythema, induration, and scaling. This generates a severity score ranging from 0 to 72 [31]. Although more commonly used in clinical trials than in the context of clinical practice, the PASI can be a useful measurement in assessing response to a given treatment . For example, PASI-75 indicates that the patient’s psoriasis has improved by 75% or greater from baseline. The Physician Global Assessment (PGA) is another simplified measurement tool that rates the severity of psoriasis at a single point in time [32]. It is important to note that one of the limitations of the PASI and PGA is that there can be high interobserver variability.
In addition to assessing the severity of psoriasis, it is also important to include evaluations of subjective symptoms and quality of life burden. Furthermore, given the high probability of systemic comorbidities, including arthritis and cardiovascular, metabolic, and psychiatric disorders, patients should be screened for such conditions and have an established primary care physician who can help manage the patient’s overall health.
Clinical Characteristics of Psoriasis and Its Variants
Plaque Psoriasis
Also known as psoriasis vulgaris, plaque psoriasis is the most common form of psoriasis, accounting for 80–90% of cases [33]. The lesions are characteristically well-defined, erythematous, scaly plaques and often have the distribution detailed above (elbows, knees, scalp, intergluteal cleft) (Figs. 1.1, 1.2, 1.3, 1.4, and 1.5). The plaques vary in size, and patients may present with only a few lesions or with widely generalized disease. Lesions are often symmetrically distributed. Mild to moderate disease, classified as involving less than 10% of the BSA, represents approximately 80% of cases of plaque psoriasis. The remainder of patients have moderate to severe disease and may have involvement of the majority of the BSA [6].
Fig. 1.1.

Plaque psoriasis: classic morphology characterized by a sharply demarcated, erythematous plaque with silver scale
Fig. 1.2.

Plaque psoriasis: this lesion is less severe with mild scaling but is diagnostic for psoriasis
Fig. 1.3.

Plaque psoriasis: this patient has widespread involvement of the majority of the body surface area
Fig. 1.4.

Scalp psoriasis: scaling is prominent with notable background erythema
Fig. 1.5.

Scalp psoriasis: severe scaling involving the periauricular region
Palmoplantar psoriasis is characterized by erythematous, desquamative plaques in the acral distribution (Fig. 1.6). Palmoplantar psoriasis can be an isolated entity or may coexist in the context of plaque psoriasis [34].
Fig. 1.6.

Palmoplantar psoriasis: notable severe scaling and erythema on the palmer surface of the distal finger
Guttate Psoriasis
Guttate psoriasis presents with the sudden appearance of many small (1–10 mm) erythematous papules, often covered with fine scale (Figs. 1.7 and 1.8). It is found more commonly in children and young adults and represents less than 2% of psoriasis cases [6]. The lesions of guttate psoriasis are widely disseminated, particularly on the proximal extremities and trunk. Lesions may also be found on the face [35]. Guttate psoriasis can occur in patients with and without a history of plaque psoriasis. It is associated with group A beta-hemolytic streptococcal infections, which often precedes the skin findings by 2–3 weeks [6]. This disease is often self-limiting in nature and can resolve spontaneously or with treatment [17]. Some patients with guttate psoriasis can go on to develop chronic guttate psoriasis or chronic plaque psoriasis [36].
Fig. 1.7.

Guttate psoriasis: widespread small, erythematous papules generalized over the entire body surface area
Fig. 1.8.

Guttate psoriasis: a close-up image showing the characteristic fine scale
Generalized Pustular Psoriasis
Generalized pustular psoriasis is characterized by the formation of sterile pustules on a background of erythematous skin, which are widespread and can be generalized (Figs. 1.9 and 1.10). The etiology remains unclear; however, administration of certain medications, including lithium and nonsteroidal anti-inflammatory drugs, may precede the onset of pustular psoriasis [24]. Other precipitating factors include infection and abrupt cessation of systemic corticosteroids [17]. Generalized pustular psoriasis may follow a mild and chronic course or appear severely and acutely (von Zumbusch type). Pustules can coalesce , and the whole body may be involved, including mucosal areas [37].
Fig. 1.9.

Pustular psoriasis: pustules on a background of erythema. Desquamation is also prominent here
Fig. 1.10.

Pustular psoriasis: severe erythema and desquamation are present
Given the widespread involvement, these patients can lose the skin’s protective function. Loss of the thermoregulatory function of the skin may cause fever or hypothermia. Fluid loss through the skin can result in volume depletion, dehydration, and even shock. There can be significant loss of electrolytes, iron, and protein through the skin. Patients with acute generalized pustular psoriasis often meet systemic inflammatory response syndrome (SIRS) criteria on presentation, and associated lab abnormalities include neutrophilia, leukocytosis up to 30,000 WBC/μL, elevated erythrocyte sedimentation rate (ESR), and elevated liver function tests [37]. Most importantly, these patients lose the protective function of the skin against the entry of pathogens, leaving them susceptible to bacteremia. There are multiple reports of staphylococcal sepsis and death in patients with generalized pustular psoriasis [38–40]. Another potential fatal complication is the development of aseptic neutrophilic pneumonitis, which can lead to acute respiratory distress syndrome (ARDS) [37]. Severe cases of generalized pustular psoriasis therefore necessitate admission to the burn unit or intensive care unit (ICU). Treatment of generalized pustular psoriasis with rapidly acting agents like cyclosporine can reduce the need for hospitalization.
Palmoplantar Pustulosis
Unlike generalized pustular psoriasis, pustular psoriasis can be limited to the palms and soles, referred to as palmoplantar pustulosis. This disease is characterized by recurrent eruptions of sterile pustules on the palmar and plantar surfaces [34] (Figs. 1.11 and 1.12). Although this form is not life-threatening as in generalized pustular psoriasis, it is a debilitating condition with high morbidity, as patients can have severe pain. Patients with psoriasis on the hands and feet have been found to have a worse quality of life than patients with extensive involvement on the trunk [41, 42]. Palmoplantar pustulosis typically presents between 30 and 40 years of age, and the palmar lesions typically precede plantar involvement by a few months [43]. Notably, the majority of patients are female, with a female to male ratio of 9:1. Palmoplantar pustulosis is also highly associated with smoking with 95% of patients having a previous or current smoking history [17]. Roughly 25% of palmoplantar psoriasis patients will also have a diagnosis of chronic plaque psoriasis, although genetic studies indicate that they are distinct entities [25].
Fig. 1.11.

Palmoplantar pustulosis: a severe case on the plantar surface
Fig. 1.12.

Palmoplantar pustulosis: a mild case on the palmar surface
Erythrodermic Psoriasis
Erythrodermic psoriasis is another potentially life-threatening form of psoriasis associated with the loss of skin function. In addition to being one of the most severe forms of psoriasis, it is also one of the rarest, affecting only 1% of psoriasis patients [44]. Among patients with a history of psoriasis who presents with erythroderma, the erythroderma is due to the preexisting psoriasis in only 20% of patients [45]. Even in patients with known psoriasis, it is important to consider other possible causes of erythroderma, of which there are many (see section “Differential Diagnosis”).
In erythrodermic psoriasis, the skin over the entire body surface area is inflamed, erythematous, and scaly. Desquamation may occur (Figs. 1.13, 1.14, and 1.15). Although erythrodermic psoriasis can develop over time in patients with chronic plaque psoriasis, it may also occur suddenly in patients without a previous psoriasis history [6]. It can be precipitated by antimalarial drugs, the rapid discontinuation of either topical or systemic corticosteroids, overexposure to sun or UV light, and infections [35]. As in generalized pustular psoriasis, the loss of thermoregulatory and barrier functions of the skin can lead to fever, hypothermia, fluid loss, dehydration , and shock [6]. Patients are also at a high risk of sepsis and even death, especially staphylococcal sepsis [46].
Fig. 1.13.

Erythrodermic psoriasis: widespread erythroderma covers the majority of the body surface area
Fig. 1.14.

Erythrodermic psoriasis: a close-up of the face shows erythema with areas of desquamation
Fig. 1.15.

Erythrodermic psoriasis: severe erythema can be observed
Inverse Psoriasis
Inverse psoriasis, also known as intertriginous or flexural psoriasis , affects 3–7% of psoriasis patients [47]. It involves the skinfolds, including the axillae, genital regions, and inframammary and inguinal creases. The face can also be involved. These lesions are less likely to be scaly given the high moisture in these areas and mainly present as shiny, erythematous plaques [6] (Fig. 1.16). Fissuring and superimposed bacterial or fungal infections may occur. Histologically, there is no difference between inverse and plaque psoriasis, and thus the two are differentiated on clinical presentation alone [47]. Notably, psoriasis patients with palmar involvement are approximately five times more likely to have inverse psoriasis than classic plaque psoriasis [48].
Fig. 1.16.

Inverse psoriasis: an erythematous plaque in the axilla with minimal to no scale
Nail Changes
Nail changes can occur in any type of psoriasis. Among patients with psoriasis, fingernail changes occur in 50% of patients and toenail changes occur in 35% of patients. Nail changes are common in psoriatic arthritis patients, occurring in up to 90% of cases [6]. Many of the structures within the nail unit can be affected, resulting in a broad range of clinical presentations, include pitting, onycholysis, “oil drop” spots, discoloration, splinter hemorrhages, and subungual hyperkeratosis (Fig. 1.17).
Fig. 1.17.

Onychody-strophy due to psoriasis: findings include nail yellowing, onycholysis, and subungual hyperkeratosis
Pitting is the most common nail finding in psoriasis. These superficial depressions in the nail plate are caused by psoriatic lesions within the nail matrix, resulting in parakeratotic foci in the nail plate that slough off upon exposure to the environment. “Oil drop” or “salmon-colored” spots represent psoriatic lesions that are completely contained within the nail bed of the affected nail. If the lesion involves the hyponychium, onycholysis can occur. Subungual hyperkeratosis results in the raising of the nail plate off the nail bed secondary to deposits of cells underneath the nail plate that have not undergone desquamation. Leukonychia and onychorrhexis (longitudinal ridges and splinting) may also be seen in the nail plate. Splinter hemorrhages occur secondary to rupture of capillaries in the dermis of the nail bed. A variety of other dystrophic nail changes may also be found. Nail psoriasis is particularly difficult to treat and is often a persistent condition [49].
Differential Diagnosis
The differential diagnosis of psoriasis is broad, depending on the patient’s presentation. When the skin findings are characteristic with erythematous, sharply demarcated, scaling plaques found symmetrically on the extensor surfaces, the diagnosis is straightforward. Involvement of the skin in the periumbilical region and gluteal cleft and nail findings are clues to the diagnosis of psoriasis. However, the variants of psoriasis and atypical cases may present more diagnostic difficulty.
Common conditions on the differential diagnosis for plaque psoriasis include atopic dermatitis, nummular dermatitis, lichen simplex chronicus, pityriasis rosea, pitryiasis rubra pilaris, and tinea. If clinical diagnosis is unclear, a biopsy may be helpful. Drug reactions may also result in erythemato-papulosquamous psoriasiform eruptions. If this is a consideration, the presence of bright red lesions with intense pruritus and eosinophilia point more toward a drug eruption [35]. Mycosis fungoides can also present as inflammatory papulosquamous lesions and can be misdiagnosed as psoriasis.
In the differential diagnosis for scalp psoriasis, seborrheic dermatitis or tinea capitis may be considered. The lesions of psoriasis can be distinguished by the findings of well-demarcated, xerotic plaques with silvery scale, which may advance beyond the border of the hairline. Tinea can be distinguished from psoriasis by fungal culture, potassium hydroxide (KOH) preparation of skin scrapings, or histologically if a biopsy is performed [35, 45]. Palmoplantar psoriasis can also be confused with lichen simplex chronicus, lichen planus, secondary syphilis, hand dermatitis, or contact dermatitis. Clinical presentations of these conditions usually have distinct characteristics, but in unclear cases, a biopsy may be necessary to distinguish these conditions [35, 50].
Pustular psoriasis on the palms and the soles can resemble dyshidrotic eczema, irritant dermatitis, folliculitis, or allergic contact dermatitis. Infectious causes should also be ruled out. Work up may include cultures, KOH preparation, PAS or GRAM stains, and patch testing [35, 43]. Generalized pustular psoriasis may be mistaken for Stevens-Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN) given the widespread erythema and desquamation [37]. Another important differential diagnosis is that of acute generalized exanthematous pustulosis (AGEP), a febrile drug eruption also characterized by small sterile pustules on an erythematous base. The short latency period between drug administration and the skin reaction can help differentiate this from pustular psoriasis. Biopsy findings can also be helpful [35]. Subcorneal pustulosis is another consideration, but clinical and histological clues often help to differentiate the two [35].
The differential diagnosis for guttate psoriasis includes lymphomatoid papulosis, pityriasis rosea, pityriasis lichenoides chronica, tinea versicolor, and secondary syphilis, although these conditions often have distinctive presentations [35].
It is important to distinguish erythrodermic psoriasis from the other causes of generalized erythroderma, including drug reactions, atopic dermatitis, congenital ichthyoses, bullous dermatoses, cutaneous T cell lymphoma, and pityriasis rubra pilaris. If present, a prior personal or family history of psoriasis can be very helpful. Identifying the underlying etiology of erythroderma is difficult, and in many cases, even with biopsies and other tests, the cause is never identified [35].
In cases of inverse psoriasis, the differential diagnosis often includes fungal and bacterial infections. KOH examination of skin scrapings, Wood’s lamp examination, and bacterial cultures are useful to rule out infections. Intertrigo secondary to skin friction can also be very similar in appearance to inverse psoriasis. Other causes of intertriginous plaques include Hailey-Hailey disease, flexural Darier disease, extra-mammary Paget’s disease, Langerhans cell histiocytosis, and glucagonoma syndrome. These conditions may be differentiated by clinical and histological findings, lab abnormalities, and systemic symptoms [35, 47].
The nail findings of psoriasis have a broad differential diagnosis. Pitting, a common feature of psoriatic nail disease, can also be seen in alopecia areata and contact dermatitis. However, the pitting seen in psoriasis is usually deeper than that seen in the other conditions. Oil spots can be seen in other inflammatory diseases, including systemic lupus erythematosus (SLE). Subungual hyperkeratosis can be seen in onychomycosis, pityriasis rubra pilaris, contact dermatitis, or with trauma. A positive KOH or nail culture would suggest onychomycosis; however, it is important to note that onychomycosis and nail psoriasis can occur concurrently. Lastly, onycholysis is also a feature of many other systemic, infectious, traumatic, or congenital syndromes [35].
Histopathology
As previously stated, a skin biopsy is not usually necessary to diagnose psoriasis. However, in the event that a biopsy is deemed necessary, certain key features can be seen. Classic histopathological findings of plaque psoriasis include hyperkeratosis, parakeratosis, loss of the granular cell layer, epidermal acanthosis, dilated and tortuous vasculature, and a leukocytic infiltrate [35]. The histology of uninvolved skin will be normal [17].
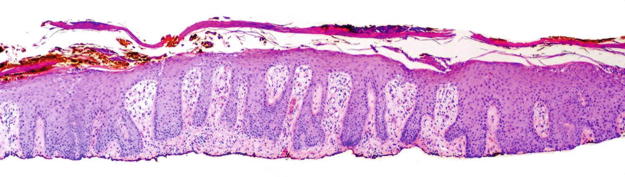
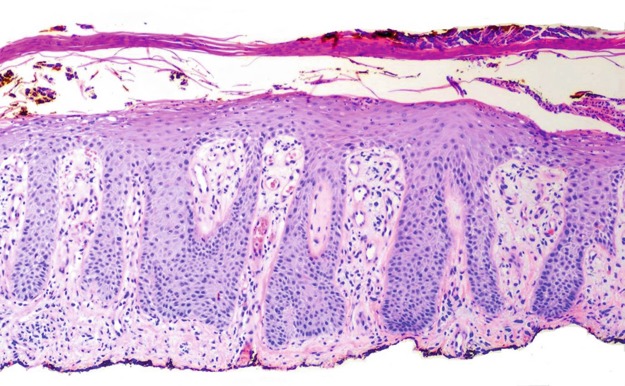
Hyperproliferation and impaired differentiation of keratinocytes are the two key features that lead to the skin findings of psoriatic plaques. This can be seen histologically as epidermal thickening (hyperkeratosis) with regularly elongated rete ridges [51]. The rete ridges display increased thickening toward the tips , resulting in a club-like appearance (Fig. 1.18). The capillaries of the interdigitating dermal papillae will be dilated and tortuous (Fig. 1.19). Fine fibrillary collagen bundles can also be seen in the papillae. The suprapapillary plate is thinned, particularly in the stratum spinosum and stratum granulosum [45]. Terminal differentiation begins in the granular cell layer of the epidermis, which is absent in the areas subajacent to the observed parakeratosis. The stratum corneum therefore develops from keratinocytes that have not undergone normal differentiation, leading to the finding of parakeratosis (aberrant retention of nuclei in the stratum corneum) [45, 52] (Fig. 1.20). Orthokeratosis (hyperkeratosis without parakeratosis) is also often seen, alternating with areas of parakeratosis . Another finding related to hyperproliferation includes increased mitoses in the basal and suprabasal layer [45]. A mononuclear leukocytic infiltrate can be seen in the epidermis and dermis consisting of predominately lymphocytes [51].
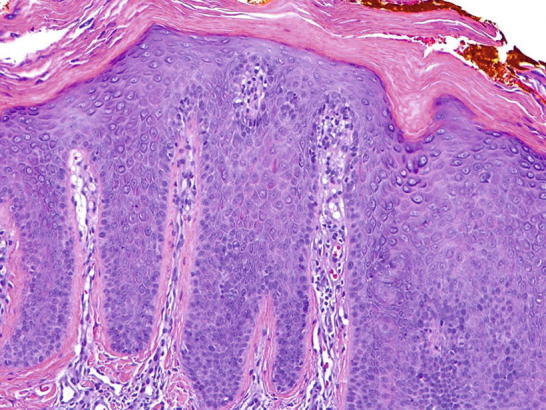
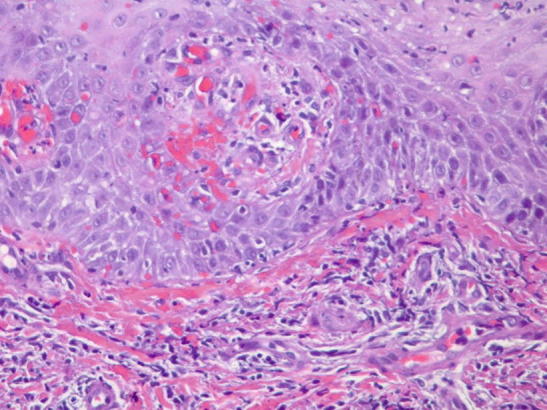
Fig. 1.18.
Histological findings of plaque psoriasis: epidermal hyperkeratosis and elongated, clubbed rete ridges are seen
Fig. 1.19.
Histological findings of plaque psoriasis: elongated, club-like rete ridges are visualized, along with dilatation and ectasia of the interdigitating dermal capillaries
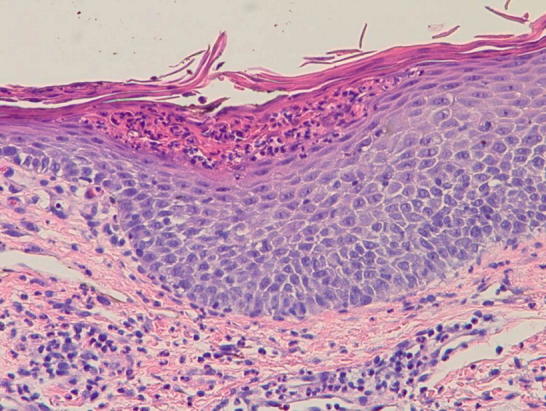
Fig. 1.20.
Histological findings of plaque psoriasis: classic findings include hyperkeratosis, acanthosis, and parakeratosis of the epidermis
Two key histological markers of psoriasis are the findings of foci of neutrophils in the parakeratotic stratum corneum, otherwise known as “ Munro’s microabscesses,” and spongiform neutrophilic micropustules in the spinous layer of the epidermis, termed “spongiform pustules of Kogoj” [45, 51] (Figs. 1.21 and 1.22). Munro’s microabscesses are found commonly and can be seen in 75% of cases [45]. These features, along with dilated and tortuous dermal capillaries, are diagnostic for psoriasis, especially when combined with the findings detailed above [45].
Fig. 1.21.
Histological findings of plaque psoriasis: scattered collections of neutrophils are present within the stratum corneum, forming Munro’s microabscesses
Fig. 1.22.
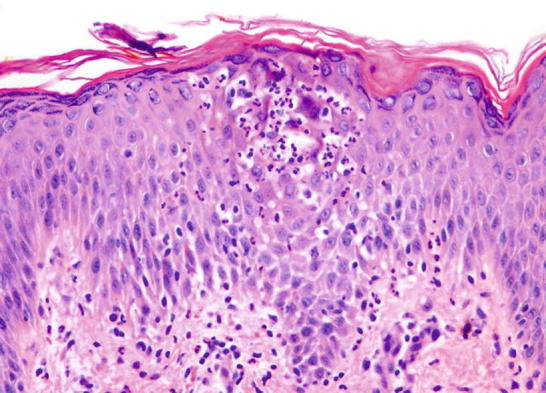
Histological findings of plaque psoriasis: neutrophils replace keratinocytes in the epidermis, forming a classic spongiform pustule of Kogoj
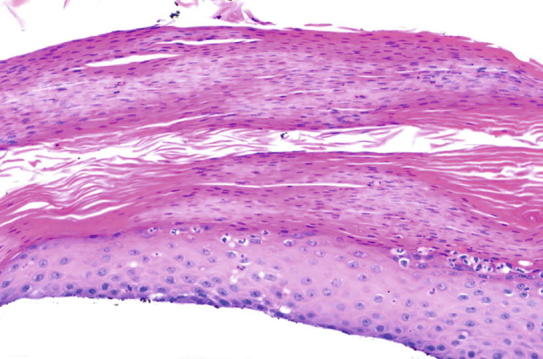
It is important to note that the histopathologic features will vary depending on the stage of the lesion that is biopsied, and the histology described above for a typical psoriatic lesion may not be found in all cases. For example, biopsy of a very early lesion may show predominantly dermal changes including a mild perivascular lymphocytic infiltrate, along with dilation and minimal tortuosity of the vasculature, in a background of a slight edema and spongiosis [45]. Once the lesion evolves, further changes can be seen, including mild epidermal hyperplasia, mounds of parakeratosis, ectatic superficial dermal vasculature, neutrophilic exocytosis, and Munro’s microabscesses with nearby hypogranulosis [45]. Conversely, a resolving plaque may show a decrease in neutrophils, less parakeratosis and orthokeratosis, and a reforming granular cell layer. Key findings that may lead to the correct diagnosis in resolving psoriasis lesions include residual epidermal hyperplasia and dermal capillary dilatation and tortuosity [45] (Fig. 1.23).
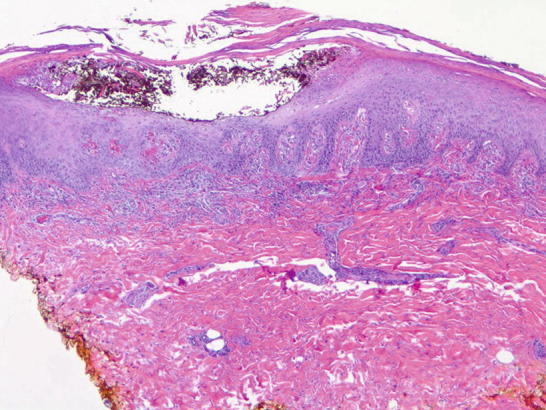
Fig. 1.23.
Histological findings of a partially treated psoriasis plaque: telangiectasias and ectatic vessels are still present. Thinning of the suprapapillary plate can be seen, along with some residual thickening of the epidermis. The neutrophilic infiltrate is less prominent compared to active psoriasis lesions
The histopathology of pustular psoriasis is characterized by sterile intraepidermal pustules. These are analogous to the spongiform pustules of Kogoj but are larger than those seen in other forms of psoriasis. A mixed inflammatory infiltrate may be seen in the dermis (Figs. 1.24, 1.25, and 1.26). Munro’s microabscesses can also form from neutrophils that have made their way up to the stratum corneum (Fig. 1.27). In acute cases, the neutrophilic infiltrate occurs before any epidermal hyperplasia is seen, and thus the histologic changes associated with chronic plaque psoriasis will not be visualized [45].
Fig. 1.24.
Histological findings of pustular psoriasis with a prominent intraepidermal pustule
Fig. 1.25.
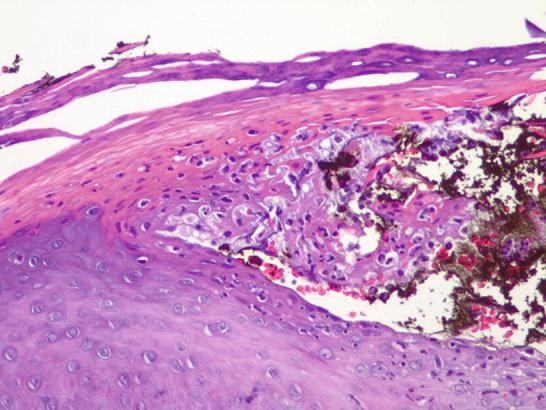
Histological findings of pustular psoriasis: a spongiform pustule of Kogoj is observed near the intraepidermal pustule
Fig. 1.26.
Histological findings of pustular psoriasis: a mixed inflammatory infiltrate is seen in the dermis
Fig. 1.27.
Histological findings of pustular psoriasis: a subcorneal collection of neutrophils is present. A mixed inflammatory infiltrate is seen in the dermis
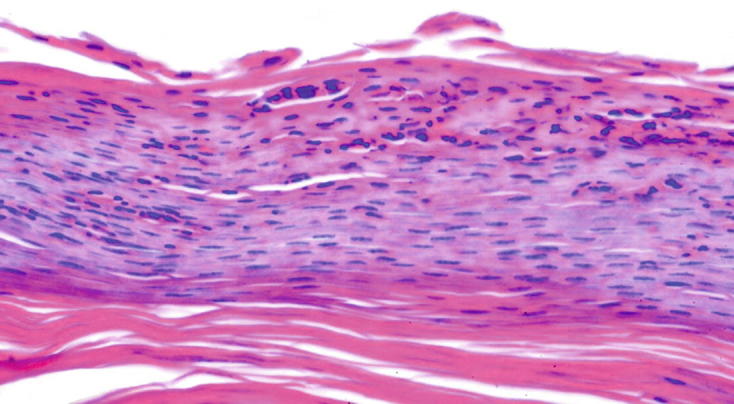
In erythrodermic psoriasis, common histological changes include absence of the stratum corneum and an even more notable dilation of the dermal vasculature than that seen in plaque psoriasis. Some of the changes seen in early plaque psoriasis lesions may also be visualized. Overall, this is a difficult diagnosis to make, as the histological findings may be nonspecific. Often, multiple biopsies are required [45].
The histology of palmoplantar psoriasis is characterized by multiple foci of alternating parakeratosis and orthokeratosis with an inflammatory infiltrate [50]. Palmoplantar pustulosis will show similar findings to those seen in generalized pustular psoriasis including epidermal sterile pustules. Other features that are typically seen in plaque psoriasis may also be seen, including mild acanthosis and parakeratosis [43].
Contributor Information
Tina Bhutani, Email: tina.bhutani@ucsf.edu.
Wilson Liao, Email: wilson.liao@ucsf.edu.
Mio Nakamura, Email: mio.nakamura@ucsf.edu.
Grace W. Kimmel, Email: grace.kimmel@mssm.edu
References
- 1.Lebwohl MG, Bachelez H, Barker J, Girolomoni G, Kavanaugh A, Langley RG, Paul CF, Puig L, Reich K, van de Kerkhof PC. Patient perspectives in the management of psoriasis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis Survey. J Am Acad Dermatol. 2014;70(5):871–881.e871–830. doi: 10.1016/j.jaad.2013.12.018. [DOI] [PubMed] [Google Scholar]
- 2.Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70(3):512–516. doi: 10.1016/j.jaad.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 3.Parisi R, Symmons DP, Griffiths CE, Ashcroft DM. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133(2):377–385. doi: 10.1038/jid.2012.339. [DOI] [PubMed] [Google Scholar]
- 4.Henseler T, Christophers E. Psoriasis of early and late onset: characterization of two types of psoriasis vulgaris. J Am Acad Dermatol. 1985;13(3):450–456. doi: 10.1016/S0190-9622(85)70188-0. [DOI] [PubMed] [Google Scholar]
- 5.Andressen C, Henseler T [Inheritance of psoriasis. Analysis of 2035 family histories]. Hautarzt. 1982;33(4):214–7. [PubMed]
- 6.Menter A, Gottlieb A, Feldman SR, van Voorhees AS, Leonardi CL, Gordon KB, Lebwohl M, Koo JYM, Elmets CA, Korman NJ, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: Section 1. Overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics. J Am Acad Dermatol. 2008;58(5):826–850. doi: 10.1016/j.jaad.2008.02.039. [DOI] [PubMed] [Google Scholar]
- 7.Krueger G, Koo J, Lebwohl M, Menter A, Stern RS, Rolstad T. The impact of psoriasis on quality of life: results of a 1998 National Psoriasis Foundation patient-membership survey. Arch Dermatol. 2001;137(3):280–284. [PubMed] [Google Scholar]
- 8.Pariser D, Schenkel B, Carter C, Farahi K, Brown TM, Ellis CN. A multicenter, non-interventional study to evaluate patient-reported experiences of living with psoriasis. J Dermatolog Treat. 2016;27(1):19–26. doi: 10.3109/09546634.2015.1044492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rapp SR, Feldman SR, Exum ML, Fleischer AB, Jr, Reboussin DM. Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol. 1999;41(3 Pt 1):401–407. doi: 10.1016/S0190-9622(99)70112-X. [DOI] [PubMed] [Google Scholar]
- 10.Lebwohl MG, Kavanaugh A, Armstrong AW, Van Voorhees AS. US perspectives in the Management of Psoriasis and Psoriatic Arthritis: patient and physician results from the population-based multinational assessment of psoriasis and psoriatic arthritis (MAPP) survey. Am J Clin Dermatol. 2016;17:87–97. doi: 10.1007/s40257-015-0169-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gottlieb A, Korman NJ, Gordon KB, Feldman SR, Lebwohl M, Koo JYM, Van Voorhees AS, Elmets CA, Leonardi CL, Beutner KR, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: Section 2. Psoriatic arthritis: overview and guidelines of care for treatment with an emphasis on the biologics. J Am Acad Dermatol. 2008;58(5):851–864. doi: 10.1016/j.jaad.2008.02.040. [DOI] [PubMed] [Google Scholar]
- 12.Sommer DM, Jenisch S, Suchan M, Christophers E, Weichenthal M. Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis. Arch Dermatol Res. 2006;298(7):321–328. doi: 10.1007/s00403-006-0703-z. [DOI] [PubMed] [Google Scholar]
- 13.Herron MD, Hinckley M, Hoffman MS, Papenfuss J, Hansen CB, Callis KP, Krueger GG. Impact of obesity and smoking on psoriasis presentation and management. Arch Dermatol. 2005;141(12):1527–1534. doi: 10.1001/archderm.141.12.1527. [DOI] [PubMed] [Google Scholar]
- 14.Higgins Alcohol, smoking and psoriasis. Clin Exp Dermatol. 2000;25(2):107–110. doi: 10.1046/j.1365-2230.2000.00588.x. [DOI] [PubMed] [Google Scholar]
- 15.Gelfand JM, Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB. RIsk of myocardial infarction in patients with psoriasis. JAMA. 2006;296(14):1735–1741. doi: 10.1001/jama.296.14.1735. [DOI] [PubMed] [Google Scholar]
- 16.Mallbris L, Akre O, Granath F, Yin L, Lindelöf B, Ekbom A, Ståhle-Bäckdahl M. Increased risk for cardiovascular mortality in psoriasis inpatients but not in outpatients. Eur J Epidemiol. 2004;19(3):225–230. doi: 10.1023/B:EJEP.0000020447.59150.f9. [DOI] [PubMed] [Google Scholar]
- 17.Griffiths CEM, Barker JNWN. Pathogenesis and clinical features of psoriasis. The Lancet. 2007;370(9583):263–271. doi: 10.1016/S0140-6736(07)61128-3. [DOI] [PubMed] [Google Scholar]
- 18.Sheu J-J, Wang K-H, Lin H-C, Huang C-C. Psoriasis is associated with an increased risk of parkinsonism: a population-based 5-year follow-up study. J Am Acad Dermatol. 2013;68(6):992–999. doi: 10.1016/j.jaad.2012.12.961. [DOI] [PubMed] [Google Scholar]
- 19.Mahil SK, Capon F, Barker JN. Update on psoriasis immunopathogenesis and targeted immunotherapy. Semin Immunopathol. 2016;38(1):11–27. doi: 10.1007/s00281-015-0539-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Basavaraj KH, Ashok NM, Rashmi R, Praveen TK. The role of drugs in the induction and/or exacerbation of psoriasis. Int J Dermatol. 2010;49(12):1351–1361. doi: 10.1111/j.1365-4632.2010.04570.x. [DOI] [PubMed] [Google Scholar]
- 21.Gilleaudeau P, Vallat VP, Carter DM, Gottlieb AB. Angiotensin-converting enzyme inhibitors as possible exacerbating drugs in psoriasis. J Am Acad Dermatol. 1993;28(3):490–492. doi: 10.1016/S0190-9622(08)81761-6. [DOI] [PubMed] [Google Scholar]
- 22.Marquart-Elbaz C, Grosshans E, Lipsker D, Lipsker D. Sartans, angiotensin II receptor antagonists, can induce psoriasis. Br J Dermatol. 2002;147(3):617–618. doi: 10.1046/j.1365-2133.2002.48848.x. [DOI] [PubMed] [Google Scholar]
- 23.Brauchli YB, Jick SS, Curtin F, Meier CR. Association between beta-blockers, other antihypertensive drugs and psoriasis: population-based case-control study. Br J Dermatol. 2008;158(6):1299–1307. doi: 10.1111/j.1365-2133.2008.08563.x. [DOI] [PubMed] [Google Scholar]
- 24.Schleicher SM. Psoriasis: pathogenesis, assessment, and therapeutic update. Clin Podiatr Med Surg. 2016;33(3):355–366. doi: 10.1016/j.cpm.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 25.Asumalahti K, Ameen M, Suomela S, Hagforsen E, Michaëlsson G, Evans J, Munro M, Veal C, Allen M, Leman J, et al. Genetic analysis of PSORS1 distinguishes guttate psoriasis and palmoplantar pustulosis. J Investig Dermatol. 2003;120(4):627–632. doi: 10.1046/j.1523-1747.2003.12094.x. [DOI] [PubMed] [Google Scholar]
- 26.Nair RP, Stuart PE, Nistor I, Hiremagalore R, Chia NVC, Jenisch S, Weichenthal M, Abecasis GR, Lim HW, Christophers E, et al. Sequence and haplotype analysis supports HLA-C as the psoriasis susceptibility 1 gene. Am J Hum Genet. 2006;78(5):827–851. doi: 10.1086/503821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsoi LC, Stuart PE, Tian C, Gudjonsson JE, Das S, Zawistowski M, et al. Large scale meta-analysis characterizes genetic architecture for common psoriasis associated variants. Nat Commun. 2017;24(8):15392. doi: 10.1038/ncomms15382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elder JT, Bruce AT, Gudjonsson JE, Johnston A, Stuart PE, Tejasvi T, Voorhees JJ, Abecasis GR, Nair RP. Molecular dissection of psoriasis: integrating genetics and biology. J Investig Dermatol. 2010;130(5):1213–1226. doi: 10.1038/jid.2009.319. [DOI] [PubMed] [Google Scholar]
- 29.Eberle Franziska C., Brück Jürgen, Holstein Julia, Hirahara Kiyoshi, Ghoreschi Kamran. Recent advances in understanding psoriasis. F1000Research. 2016;5:770. doi: 10.12688/f1000research.7927.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim J, Krueger JG. The immunopathogenesis of psoriasis. Dermatol Clin. 2015;33(1):13–23. doi: 10.1016/j.det.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 31.Fredriksson T, Pettersson U. Severe psoriasis—oral therapy with a new retinoid. Dermatology. 1978;157(4):238–244. doi: 10.1159/000250839. [DOI] [PubMed] [Google Scholar]
- 32.Langley RG, Ellis CN. Evaluating psoriasis with psoriasis area and severity index, psoriasis global assessment, and lattice system physician's global assessment. J Am Acad Dermatol. 2004;51(4):563–569. doi: 10.1016/j.jaad.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 33.Nestle FO, Kaplan DH, Barker J. Psoriasis. N Engl J Med. 2009;361(5):496–509. doi: 10.1056/NEJMra0804595. [DOI] [PubMed] [Google Scholar]
- 34.Raposo I, Torres T. Palmoplantar psoriasis and palmoplantar pustulosis: current treatment and future prospects. Am J Clin Dermatol. 2016;17(4):349–358. doi: 10.1007/s40257-016-0191-7. [DOI] [PubMed] [Google Scholar]
- 35.Lisi P. Differential diagnosis of psoriasis. Reumatismo. 2007;59(Suppl 1):56–60. [PubMed] [Google Scholar]
- 36.Martin BA, Chalmers RG, Telfer NR. HOw great is the risk of further psoriasis following a single episode of acute guttate psoriasis? Arch Dermatol. 1996;132(6):717–718. doi: 10.1001/archderm.1996.03890300147032. [DOI] [PubMed] [Google Scholar]
- 37.Varman KM, Namias N, Schulman CI, Pizano LR. Acute generalized pustular psoriasis, von Zumbusch type, treated in the burn unit. A review of clinical features and new therapeutics. Burns. 2014;40(4):e35–e39. doi: 10.1016/j.burns.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 38.Matsubara M, Komori M, Koishi K, Yasuno H, Ueda K, Seto Y, Nonomura K. Generalized pustular psoriasis and bacteremia. J Dermatol. 1983;10(6):525–529. doi: 10.1111/j.1346-8138.1983.tb01176.x. [DOI] [PubMed] [Google Scholar]
- 39.Augey F, Renaudier P, Nicolas JF. Generalized pustular psoriasis (Zumbusch): a French epidemiological survey. Eur J Dermatol. 2006;16(6):669–673. [PubMed] [Google Scholar]
- 40.Sharkey MP, Muir JB. Staphylococcal scalded skin syndrome complicating acute generalized pustular psoriasis. Australas J Dermatol. 2002;43(3):199–201. doi: 10.1046/j.1440-0960.2002.00595.x. [DOI] [PubMed] [Google Scholar]
- 41.Pettey AA, Balkrishnan R, Rapp SR, Fleischer AB, Feldman SR. Patients with palmoplantar psoriasis have more physical disability and discomfort than patients with other forms of psoriasis: implications for clinical practice. J Am Acad Dermatol. 2003;49(2):271–275. doi: 10.1067/S0190-9622(03)01479-8. [DOI] [PubMed] [Google Scholar]
- 42.Sampogna F, Tabolli S, Söderfeldt B, Axtelius B, Aparo U, Abeni D, investigators IDIMPRoVE Measuring quality of life of patients with different clinical types of psoriasis using the SF-36. Br J Dermatol. 2006;154(5):844–849. doi: 10.1111/j.1365-2133.2005.07071.x. [DOI] [PubMed] [Google Scholar]
- 43.Yamamoto T. Extra-palmoplantar lesions associated with palmoplantar pustulosis. J Eur Acad Dermatol Venereol. 2009;23(11):1227–1232. doi: 10.1111/j.1468-3083.2009.03296.x. [DOI] [PubMed] [Google Scholar]
- 44.Goeckerman WH, O'Leary PA. Erythroderma psoriaticum: a review of twenty-two cases. J Am Med Assoc. 1932;99(25):2102–2105. doi: 10.1001/jama.1932.02740770032007. [DOI] [Google Scholar]
- 45.Murphy M, Kerr P, Grant-Kels JM. The histopathologic spectrum of psoriasis. Clin Dermatol. 2007;25(6):524–528. doi: 10.1016/j.clindermatol.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 46.Green MS, Prystowsky JH, Cohen SR, Cohen JI, Lebwohl MG. Infectious complications of erythrodermic psoriasis. J Am Acad Dermatol. 1996;34(5:911–914. doi: 10.1016/S0190-9622(96)90078-X. [DOI] [PubMed] [Google Scholar]
- 47.Syed ZU, Khachemoune A. Inverse psoriasis. Am J Clin Dermatol. 2011;12(2):143–146. doi: 10.2165/11532060-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 48.Fransson J, Storgards K, Hammar H. Palmoplantar lesions in psoriatic patients and their relation to inverse psoriasis, tinea infection and contact allergy. Acta Derm Venereol. 1985;65(3):218–223. [PubMed] [Google Scholar]
- 49.Jiaravuthisan MM, Sasseville D, Vender RB, Murphy F, Muhn CY. Psoriasis of the nail: anatomy, pathology, clinical presentation, and a review of the literature on therapy. J Am Acad Dermatol. 2007;57(1):1–27. doi: 10.1016/j.jaad.2005.07.073. [DOI] [PubMed] [Google Scholar]
- 50.Aydin O, Engin B, Oğuz O, İlvan Ş, Demirkesen C. Non-pustular palmoplantar psoriasis: is histologic differentiation from eczematous dermatitis possible? J Cutan Pathol. 2008;35(2):169–173. [PubMed] [Google Scholar]
- 51.Raychaudhuri SK, Maverakis E, Raychaudhuri SP. Diagnosis and classification of psoriasis. Autoimmun Rev. 2014;13(4–5):490–495. doi: 10.1016/j.autrev.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 52.Lowes MA, Bowcock AM, Krueger JG. Pathogenesis and therapy of psoriasis. Nature. 2007;445(7130):866–873. doi: 10.1038/nature05663. [DOI] [PubMed] [Google Scholar]