Abstract
This chapter provides the reader with a concise outline of the topics required for general pediatric board examination, respiratory component. Basic diagnostic testing is reviewed. Common upper airway problems, lower airway issues, and parenchymal diseases are covered. Congenital malformations and common diseases of the lung are reviewed. The physiology of extrapulmonary problems is reviewed. Sleep disordered breathing and the evaluation of apneas and ALTE/SIDS are also discussed. Hints regarding physiology, clinical features, diagnostic testing, and management are present with references to national guidelines and resources.
Keywords: Pediatric pulmonology, Congenital malformations of the lung, Cystic fibrosis, Asthma, Bronchiolitis, Bronchopulmonary dysplasia, Aspiration, Pneumonia, Bronchiectasis, Primary ciliary dyskinesia
Diagnostic Testing for Respiratory Conditions
Pulmonary Function Testing (PFT)
-
Lung volumes and capacities are defined
-
Four volumesRV residual volume
- ◦ ERV expiratory reserve volume
- ◦ TV tidal volume
- ◦ IRV inspiratory reserve volume
-
Capacities are sums of volumes
- ◦ TLC total lung capacity (all four volumes)
- ◦ IC inspiratory capacity (TV + IRV)
- ◦ FRC functional residual capacity (RV + ERV)
- ◦ VC vital capacity (RV + ERV + TV)
-
Spirometry
- ◦ Forced or slow-maneuver breathing from TLC to RV capturing VC
- ◦ Displays volume exhaled and flow rates for the process
- ◦ Interpreted to show obstruction (low flows), restriction (low volumes) or mixed process (Fig. 1)
-
◦ Measurement of RV
- ▪ Impossible with spirometry
-
▪ Gained by
- Plethysmography, most accurate
- Nitrogen wash out, less accurate if obstructive process present
-
Fig. 1.
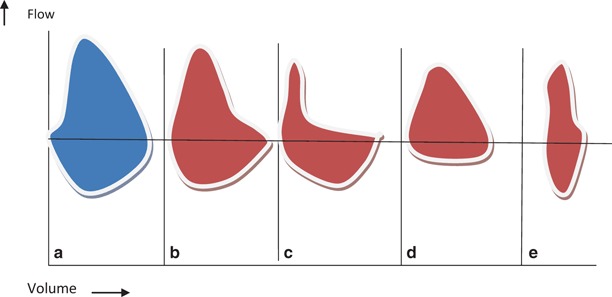
Flow volume loop configurations in normal and different pulmonary disorders. Loop above line is expiratory loop; loop below line is inspiratory. a Normal, b early small airway obstruction, c chronic obstructive disease, d variable extrathoracic large airway obstruction, e.g., vocal cord pathologies, e restrictive diseases
Oximetry
PaO2—partial pressure of arterial oxygen.
SpO2—saturation pulse correlated showing percentage of binding sites of hemoglobin with oxygen attached.
-
These are related via the oxyhemoglobin dissociation curve which is S shaped.
- Oxygen saturation shifts to the left with alkalosis, hypocarbia and hypothermia, shifting to the right with increased temperature, acidosis, hypercarbia and increased 2,3 DPG. A shift to the left means oxygen binds more avidly to the hemoglobin, to the right less so.
Oximetry readings are affected by dyes, nail polish, high-intensity light, impaired perfusion, artificial nails, methemoglobin, and carboxyhemoglobin. It is less accurate at low saturations or with motion.
SpO2 and PaO2 are not equal. It is important to obtain a blood gas to understand acid–base balance and carbon dioxide as well as saturation in sick patients, especially those supported on supplemental oxygen which can improve saturation and falsely reassure a caregiver.
Blood gas analysis
Capillary blood gas can give representation of arterial sample if heel is adequately warmed and perfusion is excellent.
Blood gases will be inaccurate if permitted to remain warm outside of the body and delays in reading occur since WBC metabolism will continue consuming oxygen and generating waste products leading to increased acidosis.
Imaging the chest
-
Radiation basics
- mSv is a milliSievert unit which reflects the ionizing radiation from plain films, fluoroscopy, and CT imaging
- A single chest X-ray (CXR) provides 0.1 mSv = background radiation on the earth in 10 days time
-
A standard helical CT of newborn chest 1.7 mSv to 5.4 mSv in an adult-sized teenager
- ◦ Low-dose protocols can halve these numbers
- ◦ Ultra-low dose protocols are as low as 0.14 mSv and useful for children likely to require multiple CT during a lifetime
-
Suggested modalities for various issues
- Plain CXR: suspected vascular ring, pneumonia
- Plain expiratory or decubitus views: suspected foreign body
- Plain decubitus: pleural fluid, pneumothorax
- Virtual bronchoscopy: persistent anomalies of tracheobronchial tree
- Ultrasound: pleural effusion, complicated pneumonia
- CT scan: chest wall structure, lung abscess, airspace disease, bronchiectasis , anterior or middle mediastinal masses, complicated pneumonia, asthma complications
- PET scan: anterior, middle mediastinal masses
- MRI: posterior mediastinal mass, pulmonary vascular bed, rings, new programs to better visualize the lung and spare radiation being evaluated
Upper airway obstruction
Early increase in PCO2 and proportionate decrease in PO2 and responds well to supplemental oxygen initially
Intrapulmonary airway obstruction
Mild: decrease PCO2, normal to decreased PO2
Moderate: Normal PCO2, decrease PO2 moving toward failure
Severe: increase PCO2 and decrease PO2
Supplemental oxygen will support patient, but imperative to monitor carbon dioxide as well
Alveolar interstitial pathology
Diffusion defects occur and cause poor transit of oxygen with desaturation first at exercise and then also at rest
R–L shunt
Early decrease in PO2
Normal or low PCO2, high PCO2 if fatigue develop
-
Testing with 100 % oxygen helps to define this issue
- Response to supplemental oxygen is fair to poor depending on shunt volume
Stridor
Background
Stridor is an abnormal, high-pitched sound.
Produced by turbulent airflow through a partially obstructed airway.
The timing of the sound can help to localize the narrowing. Because the extrathoracic airway collapses with inspiration any swelling/obstruction in this location will cause inspiratory stridor. Glottic obstruction/right at the cords will produce a to-and-fro noise. Subglottic will produce noise first on exhalation.
Could be supraglottic, glottic subglottic, and/or trachea.
Differential diagnosis of acute stridor
Laryngotracheobronchitis or croup (see amplified discussion)
Foreign body aspiration (see amplified discussion)
Bacterial tracheitis (see amplified discussion)
-
Retropharyngeal abscess
- Children younger than 6 years
- Abrupt onset of high fevers, difficulty swallowing, refusal to feed, sore throat, hyperextension of the neck, and respiratory distress
-
Peritonsillar abscess
- Adolescents and preadolescents
- Severe throat pain, trismus, and trouble swallowing or speaking
-
Spasmodic croup, also termed acute spasmodic laryngitis
- Occurs most commonly in children aged 1–3 years
- May be associated with GI reflux
-
Allergic reaction or anaphylaxis
- History of allergy
- Other organ involvement, e.g., itchiness or hives
Epiglottitis (see amplified discussion)
Differential diagnosis of chronic stridor
-
Laryngomalacia
-
Background
- ◦ The most common cause of inspiratory stridor in the neonatal period and early infancy
- ◦ Accounts for up to 75 % of all cases of stridor
-
Clinical presentation
- ◦ Exacerbated by crying or feeding
- ◦ Placing the patient in a prone position with the head elevated improves the stridor
- ◦ Supine position worsens the stridor
-
Diagnosis
- ◦ Flexible laryngoscopy can confirm the diagnosis but may miss tracheal abnormalities
- ◦ If moderate to severe obstruction, difficulty in feeding and breathing, unable to gain weight then use flexible bronchoscopy to r/o other associated airway anomalies
-
Management
- ◦ Laryngomalacia is usually benign and self-limiting and improves as the child reaches age 1–2 years
- ◦ Careful observation and growth monitoring for most patients
- ◦ Surgical correction or supraglottoplasty may be considered in severe cases
-
-
Vocal cord abnormalities
- The second most common cause of stridor in infants
- Unilateral vocal cord paralysis can be congenital or secondary to birth or surgical trauma, such as cardiothoracic surgery.
- Patients with a unilateral vocal cord paralysis present with a weak cry and biphasic stridor that is louder when awake and improves when lying with the affected side down.
- Bilateral vocal cord paralysis (BVCP) is a more serious entity and usually present with high-pitched biphasic stridor that may progress to severe respiratory distress.
- Bilateral vocal cord paralysis can be associated with CNS abnormalities, such as Arnold–Chiari malformation, tumors, or increased intracranial pressure.
- Diagnosis: flexible laryngoscopy, if BVCP get MRI of the head
- Management: pulmonary consultation, if traumatic should improve in 6 months and if has not then unlikely to do so.
- Bilateral cord paralysis may need tracheostomy
-
Laryngeal webs
- Laryngeal webs are caused by an incomplete recanalization of the laryngeal lumen during embryogenesis
- Weak cry and biphasic stridor
- Surgery can be curative if significant obstruction occurs
-
Laryngeal hemangiomas
- Fifty percent accompanied by cutaneous hemangiomas in the head and neck .
- Patients usually present with inspiratory or biphasic stridor that may worsen as the hemangioma enlarges.
- Diagnosis: flexible bronchoscopy or direct exam
- Treatment: propranolol for months to years by center with expertise (dermatology and pulmonary/ENT)
-
Laryngeal papillomas
- Usually secondary to vertical transmission of the human papilloma virus (genital warts) during the birth process.
- Papillomas are the most common cause of respiratory neoplasm in children
- HPV 6 and 11 are the most commonly associated with laryngeal disease
- Sixty percent are born to mother with condyloma accuminata
- Produce chronic hoarseness in infants
- Most are solitary and occur in larynx
- Thirty percent in other areas of respiratory tract
-
Treatment
- ◦ Surgical removal is repeatedly required (mean 4× annually)
- ◦ Other therapies, laser, antivirals under evaluation
-
Vocal nodules
- They are the most common cause of chronic hoarseness in children
- Caused by voice abuse or misuse, can be exacerbated by GER
- Voice rest, therapy or behavioral therapy may be effective
- Usually resolves by early teen
- Surgery is rarely required
-
Subglottic stenosis (SGS)
- Inspiratory or biphasic stridor
- Could be congenital subglottic stenosis (rare and usually associated with other genetic syndromes and conditions) or acquired due to airway instrumentation or prolonged intubation (more common)
-
Tracheomalacia
-
Background
- ◦ Expiratory wheezing secondary to airway cartilage floppiness, and airway narrowing/collapse during expiration
- ◦ Can be associated with esophageal atresia or tracheoesophageal fistula
-
Causes
- ◦ Congenital
- ◦ Associated with high ventilator pressure during mechanical ventilation in premature infants
-
Clinical presentation
- ◦ Expiratory wheezing
- ◦ Honking cough
- ◦ Apnea, cyanosis and hypoxia in severe cases “death spells”
- ◦ Supine position and crying make it worse
- ◦ Prone position makes it better
-
Cough
Background
Cough receptors in airway mucosa, most common cause is asthma, also resides in pharynx, paranasal sinus, stomach, and external auditory canal
Source of cough may need to be sought beyond the lung
Family history of atopy, allergic rhinitis, asthma or malabsorption
Types of cough and the associations
Staccato or paroxysmal: pertussis, cystic fibrosis (CF) , FB, chlamydia, mycoplasma
Followed by whoop is pertussis
All day but never during sleep: psychogenic or habit
Barking, brassy: croup, psychogenic, tracheomalacia, tracheitis, epiglottitis, and laryngeal involvement
Abrupt onset: Foreign body aspiration and pulmonary embolism
Follows exercise: exercise-induced asthma
Accompanies eating or drinking: aspiration, GERD, tracheoesophageal fistula
Throat clearing: postnasal drip and habit
Productive: infection and bronchiectasis
Night cough: sinusitis and asthma
Seasonal: asthma and allergic rhinitis
Immunosuppressed: bacterial pneumonia, PCP, TB, mycobacterium avium intracellulare, and cytomegalovirus
Failure to thrive: CF
Dyspnea: hypoxia and hypercarbia
Animal exposure: Chlamydia psittaci (birds), Yersinia pestis (rodents), Francisella tularensis (rabbits), Q-fever (sheep, cattle), hantavirus (rodents), and histoplasmosis (pigeon)
Geographic: Histoplasma (Mississippi, Missouri, Ohio River Valley), Coccidioidomycosis (Southwest), and Blastomycosis (North and Midwest)
Work days only, clearing in off days: occupational
Any child with cough > 6 weeks should be tested for CF
Sputum
Very purulent; bronchiectasis
Eosinophilia; asthma
Combinations of cough
Cough–Anemia; hemosiderosis
Cough-Trial of bronchodilator; diagnostic for asthma if responsive
Cough–Ichthyosis; asthma
Cough–Nasal polyp; CF
Chronic cough > 3 weeks
Screen: sweat test for CF, spirometry for asthma, complete blood count (CBC) with diff
Management: based on etiology, use consultants for complicated diagnoses
Clubbing of Digits or Hypertrophic Pulmonary Osteodystrophy
Causes
The most common cause is cyanotic heart disease
Most common pulmonary cause is CF, and bronchiectasis
Biliary cirrhosis
Infective endocarditis
Normal variant as familial trait
Diagnosis
Obliteration of the angle between the proximal nail and soft tissue of the digit
In normal, person will have diamond-shaped space when placing the distal phalangeal joints in mirror-like fashion
Hemoptysis
Background
Hemoptysis is coughing blood (hematemesis is vomiting blood)
Differential diagnosis of hemoptysis
Upper airway (nasopharyngeal bleeding), e.g., epistaxis or nosebleed which is very common
Gastrointestinal bleeding
Bronchitis
Bronchiectasis
Airway trauma
Foreign body
Lung abscess
Pneumonia, e.g., TB
Mycetoma or fungal ball
Idiopathic pulmonary hemosiderosis
Arteriovenous malformation
Pulmonary embolism
Pulmonary endometriosis in female adolescents
Goodpasture syndrome (GS)
Systemic lupus erythematosus (SLE)
Wegener granulomatosis (WG)
Churg–Strauss syndrome (CSS)
Polyarteritis Nodosa
Management
Examination of the nose and throat (The most common cause of hemoptysis and/or hematemesis in children is epistaxis).
Rule out infectious causes.
It is important to obtain a urinalysis and kidney function tests to rule out renal involvement.
Refer to pulmonologist or Otolaryngology (ENT) depending on the cause.
Croup
Background
Most common cause is parainfluenza viral infection
Causes subglottic narrowing
Common between 3 months and 3 years of age
Spasmodic croup is similar but without viral prodrome or other identifiable cause
Clinical presentation
Upper respiratory tract infection (URI) with or without low-grade fever
Croup can be associated with fever 39–40 °C
Barking cough
Brassy cough
Inspiratory stridor
Retraction, hypoxia, and respiratory distress in severe cases
Child may prefer to sit or be held upright
Diagnosis
It is a clinical diagnosis, and radiograph is not necessary in typical cases.
Steeple sign on frontal CXR common though occasionally absent.
Steeple sign can present in normal person as normal variant.
Mild: no stridor at rest, Moderate: stridor at rest, no agitation, and Severe: persistent stridor, agitation possibly lethargy.
Management
Reassurance, observation, and adequate hydration always required.
Dexamethasone, 0.6 mg/kg oral steroid is very beneficial in mild croup (decreasing edema and need for hospitalization).
Oxygen and racemic epinephrine (1/1000 5 ml or 0.5 ml of 2.25 %) in moderate to severe cases.
Racemic epinephrine does not cause rebound worsening of obstruction; however, patient may worsen when drug effect subsides thus a 2-h close observation following dosing is important.
Racemic epinephrine should be used cautiously in patients with left ventricular outlet obstruction.
Helium–oxygen (Heliox) may be effective in children with severe croup.
Admit for severe distress, hypoxia, and inability to feed/drink, requiring two or more nebulized racemic epinephrine treatments.
Consult pediatric pulmonary/ENT if prolonged course (multiple days) .
Endotracheal intubation should not be delayed until patient becomes restless and cyanotic.
Use endotracheal tube less 0.5–1 mm smaller in size.
Intubation more likely for bacterial tracheitis and epiglottitis and rare in croup, if intubation is required consider measles or influenza A.
Bacterial Tracheitis
Background
The most common cause is Staphylococcus aureus, , also Moraxella catarrhalis, and Streptococcus bacteria
Mean age is 4 years (range 4 weeks to 13 years, typically 2 years)
Clinical presentation
Brassy and barking cough, similar to croup but the patient has high fever and looks very toxic, with respiratory distress and stridor.
Patient may lie flat and does not have drooling or dysphagia associated with epiglottitis.
Rapid progression and purulent secretion to obstruct airway may mandate early endotracheal intubation.
Failure to respond to racemic epinephrine or corticosteroids.
Management
Intubation especially younger patients; 50–60 % do not need intubation.
High fever, purulent airway secretions, absence of finding in epiglottitis.
X-ray is not needed, but may show the classic finding of pseudomembrane detachment in the trachea.
Humidification and careful suctioning of the ET Tube are important.
Antistaphylococcal treatment, e.g., nafcillin or vancomycin.
Prognosis is excellent.
Complications can include toxic shock, septic shock, pulmonary edema, ARDS, and subglottic stenosis.
Common Cold
General considerations
Change in color or consistency in nasal secretions is common during the course of illness does not indicate sinusitis.
Presence of polymorphonuclear leukocytes in nasal secretions does not indicate bacterial superinfection.
Bacterial culture is indicated only if Group A streptococcus, Bordetella pertussis, or nasal diphtheria is suspected.
Codeine, dextromethorphan hydrobromide, has no effect on cough from cold.
Guaifenesin is not an antitussive agent.
First-generation antihistamine reduces rhinorrhea by 25–30 %, via its anticholinergic effect; therefore, using second-generation antihistamine is not helpful.
Conditions that mimic the common cold
Allergic rhinitis—prominent itching and sneezing, and nasal eosinophils (Nasal smear may be useful if allergic rhinitis is suspected)
Nasal foreign body—unilateral foul-smelling secretions, and bloody nasal secretions
Sinusitis—presence of fever, headache , facial pain, periorbital edema, persistence of rhinorrhea > 14 days
Streptococcosis—nasal discharge that excoriates the nares
Pertussis—viral prodrome with prolonged persistent staccato cough
Congenital syphilis—persistent rhinorrhea with onset in the first 3 months of life
Acute Bronchiolitis
Background
Viral bronchiolitis is the most common lower respiratory tract infection in infants and children who are 2 years of age and younger .
Respiratory syncytial virus (RSV) responsible for more than 50 % of acute bronchiolitis.
Other causes: human metapneumovirus, parainfluenza virus, adenovirus, influenza, rhinovirus, and mycoplasma.
Risk factors for persistent wheezing include:
Maternal asthma
Maternal smoking
Persistent rhinitis
Eczema at < 1 year of age
Clinical presentation
Nasal congestion, rhinorrhea, and cough.
Tachypnea or elevated respiratory rate is the earliest and most sensitive vital sign change.
Nasal flaring; grunting; and suprasternal, intercostal, and subcostal retractions demonstrate increased respiratory effort.
Nasal suctioning and repositioning may allow a more accurate assessment of lower respiratory tract involvement.
Crackles, wheezes, and referred upper airway noise are commonly auscultated sounds.
Apnea may be prominent than wheezing early in very young infants < 2 months or former premature infants.
Bronchiolitis can range from mild tachypnea to impending respiratory failure.
Patients can be expected to have worsening clinical symptoms, with peak symptomatology around day 3–4 of illness “Day of illness” .
“Day of illness” is an important variable in providing anticipatory guidance for outpatient management and in making decisions regarding admission and discharge of patients.
Diagnosis
Clinical features lead to diagnosis; subsequent evaluation important to determine treatment.
Initial step is an evaluation of respiratory rate and oxygen saturation.
CXR is warranted for any infants with respiratory distress.
Common radiological findings include hyperinflation, areas of atelectasis, and infiltrates.
Because of the risk of serious bacterial infection (SBI) among infants 30 days of age or younger, they should receive conservative management for fever, including full evaluation for SBI and administration of empiric antibiotics.
Recognition that infants older than 30 days who have clinical bronchiolitis are at a lower risk for SBIs may allow for decreased invasive testing and observation without administering antibiotics to patients who have classic presentations.
Hyperinflation and atelectasis are common in acute bronchiolitis.
Management
Respiratory rate, work of breathing, and hypoxia are the most clinically significant parameters in determining illness severity and should be assessed routinely in all patients who have bronchiolitis.
Mainstay of treatment is supportive, oxygen if hypoxia, hydration, frequent nasal suctioning, position to elevate chest 30°.
Oxygen should be discontinued once pulse oximetry saturations rise to between 90 and 92 % for most of the time and the patient is demonstrating overall clinical improvement, as evidenced by adequate feeding and improved work of breathing.
Infants with respiratory distress and desaturation or dehydration should be hospitalized.
The American Academy of Pediatrics (AAP) does not recommend the use of bronchodilators or systemic steroids in the routine treatment of bronchiolitis.
Those with recurrent wheezing may respond to bronchodilator therapy.
Corticosteroid medications, inhaled or administered systemically, should not be used in the treatment of bronchiolitis.
If bronchodilator makes the wheezing worse discontinue and consider pulmonary consultation for tracheo or bronchomalacia.
Sweat chloride test for patient with recurrent wheezing and resistant to treatment.
Ribavirin should not be used routinely in the treatment of bronchiolitis .
Prevention
Synagis 15 mg/kg IM for prematures and high-risk infants as monthly IM monoclonal antibody injection.
Hand washing is the best measure to prevent nosocomial infection .
Asthma
Background
Once asthma has been diagnosed, the physician should determine the degree of severity in the individual patient .
Severity is determined best at the time of diagnosis, before initiation of therapy.
Four categories of asthma severity
Intermittent
Mild persistent
Moderate persistent
Severe persistent
Major risk factors
Parental history of asthma
Atopic dermatitis
Sensitization to aeroallergens
Minor risk factors
Sensitization to foods
More than 4 % eosinophilia
Wheezing apart from colds
Triggers
Respiratory infections (most common trigger).
Allergens, airway irritants (e.g., environmental tobacco smoke and air pollution), exercise.
Medications (e.g., nonsteroidal anti-inflammatory medications and beta blockers).
Exposure to environmental tobacco smoke.
Common indoor allergens include house dust mite, cockroach allergen, animal dander, and molds.
Prick skin testing or blood testing (allergen-specific immunoglobulin E [IgE] concentrations) to detect sensitization to common indoor allergens should be considered for any child experiencing persistent asthma.
Clinical presentation
-
Wheezing
- A musical, high-pitched whistling sound produced by airflow turbulence.
- It is one of the most common symptoms of asthma.
-
Cough
- Usually nonproductive and nonparoxysmal.
- Coughing may be present with or without wheezing.
-
Cough at night or with exercise
- Coughing may be the only symptom of asthma, especially in cases of exercise-induced or nocturnal asthma.
- Children with nocturnal asthma tend to cough after midnight, during the early hours of morning .
-
Chest tightness
- Chest tightness or pain in the chest may be present with or without other symptoms of asthma, especially in exercise-induced or nocturnal asthma.
Shortness of breath
Sputum production
-
Infants and young children suffering a severe episode of asthma may present with:
- Breathless during rest
- Not interested in feeding
- Sit upright
- If able to talk using words (not sentences)
- Usually agitated
-
Physical finding:
- Respiratory rate is often greater than 30 breaths/min.
- Accessory muscles of respiration are usually used.
- Suprasternal retractions are commonly present.
- The heart rate is greater than 120 beats/min.
- Loud biphasic (expiratory and inspiratory) wheezing can be heard.
- Pulsus paradoxus is often present (20–40 mmHg).
- Oxyhemoglobin saturation with room air is less than 91 %.
-
Findings in status asthmaticus with imminent respiratory arrest include the following:
- Paradoxical thoracoabdominal movement occurs.
- Wheezing may be absent (in patients with the most severe airway obstruction).
- Severe hypoxemia may manifest as bradycardia.
- Pulsus Paradoxus may disappear: This finding suggests respiratory muscle fatigue.
- Child may become worse, drowsy, and confused.
- Adolescents may not have these symptoms until they are in frank respiratory failure.
Diagnosis
-
Pulmonary function tests:
- Spirometry: obstructive pattern with response to bronchodilators.Plethysmography: may have air trapping with increased RV/TLC ratio
-
Exercise challenge
- Involves baseline spirometry followed by exercise on a treadmill
- Bicycle to a heart rate greater than 60 % of the predicted maximum, with monitoring of the electrocardiogram and oxyhemoglobin saturation
- Repeat spirometry documenting drop in airflow rates
-
Radiography
- May reveal hyperinflation and increased bronchial markings; radiography may also show evidence of parenchymal disease, atelectasis, pneumonia , congenital anomaly, or a foreign body
-
Allergy testing:
- Can identify allergic factors that may significantly contribute to asthma
Exercise-induced asthma
Shortness of breath along with coughing or wheezing during physical exertion can be a symptom of poorly controlled asthma.
Some patients experience symptoms associated with bronchoconstriction only with exercise and otherwise have no history consistent with asthma .
Symptoms typically start within few minutes of initiation of vigorous exercise and subside within 20–30 min, although they can last up to 90 min when left untreated.
Usually self-limited but rare cases of severe attacks and even death have been reported.
Depending on the age and cognitive ability of the child it may be difficult to obtain spirometry data and the diagnosis largely based on clinical presentation and response to therapy.
Differential diagnosis of asthma (Table 1)
Table 1.
Asthma—differential diagnosis
| Red flag | Possible diagnosis |
|---|---|
| Sudden onset of symptoms | Foreign body aspiration |
| Coughing and choking when eating or drinking | Oropharyngeal dysphagia with aspiration |
| Poor growth and low BMI | Cystic fibrosis, immunodeficiency |
| Family history of males infertility | Cystic fibrosis, immotile cilia syndrome |
| Chronic rhinorrhea, recurrent sinusitis | Cystic fibrosis, immotile cilia syndrome |
| Acute onset without history of asthma in teenagers | Vocal cord dysfunction |
| Chronic wet productive cough | Bronchiectasis |
| Recurrent pneumonia | Immunodeficiency |
Management of exercise-induced asthma
Warm-up exercise before vigorous exercise.
Premedication 15 min before exercise with a SABA is typical the first line.
Addition of controller medication (ICSs or leukotriene) if premedication is not sufficient to alleviate asthma symptoms or if the patients needs it more than once per day.
Mast cell-stabilizing agents could be considered before exercise in poorly controlled cases.
LABAs are not recommended.
Management of Asthma (Tables 2–4)
Table 2.
Severity and initiating treatment: children 0–4 years
| Severity category | Days and night with symptoms | Interference with normal activity | Preferred treatment |
|---|---|---|---|
| Intermittent |
≤ 2 days/week (days) 0 night/month (nights) |
None | Step1: SABA as needed (PRN) |
| Mild persistent |
3–6 days/week (days) 1–2 nights/month (nights) |
Minor limitation | Step 2: Low-dose ICS |
| Moderate persistent |
Daily (days) 3–4 nights/month (nights) |
Some limitation | Step 3: Medium-dose ICS and consider short-course OCS |
| Severe persistent |
Throughout (days) > 1 night/week (nights) |
Extremely limited | Step 3: Medium-dose ICS and consider short-course OCS |
OCS oral corticosteroids, LABA long-acting beta2 agonist, SABA short-acting beta2 agonist, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity, ICS inhaled corticosteroid Tables 2–4 are adapted from the National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma, 2007.
Table 4.
Severity and initiating treatment: children 12 years of age and older
| Severity category | Days and night with symptoms | Pulmonary function | Preferred treatment |
|---|---|---|---|
| Intermittent |
≤ 2 days/week (days) ≤ 2 night/month (nights) |
FEV1: > 80 % FEV1/FVC: Normal |
Step1: SABA PRN |
| Mild persistent |
3–6 days/week (days) 3–4 nights/month (nights) |
FEV1: > 80 % FEV1/FVC: Normal |
Step 2: Low-dose ICS |
| Moderate persistent |
Daily (days) 2–6 nights/week (nights) |
FEV1: 60–80 % FEV1/FVC: Reduced 5 % |
Step 3: Medium-dose ICS + LABA or Medium-dose ICS and consider short-course OCS |
| Severe persistent |
Throughout (days) Often, 7 times/week (nights) |
FEV1: < 60 % FEV1/FVC: Reduced > 5 % |
Step 5: High-dose ICS + LABA and consider short-course OCS Step 4: Medium-dose ICS + LABA and consider short-course OCS |
OCS oral corticosteroids, LABA long-acting beta2 agonist, SABA short-acting beta2 agonist, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity, ICS inhaled corticosteroid
Assessment and monitoring: in order to assess asthma control and adjust therapy, impairment and risk must be assessed; because asthma varies over time, follow-up every 2–6 weeks is initially necessary (when gaining control of the disease), and then every 1–6 months thereafter .
Education: self-management education should focus on teaching patients the importance of recognizing their own level of control and signs of progressively worsening asthma symptoms.
Educational strategies should also focus on environmental control and avoidance strategies, as well as on medication use and adherence (e.g., correct inhaler techniques and use of other devices) (Fig. 2).
Control of environmental factors and comorbid conditions.
Long-term control medications depend on severity of asthma.
Fig. 2.
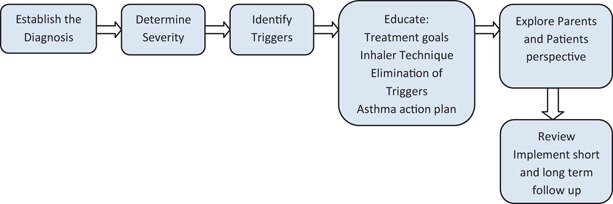
Initial evaluation of asthma. (Adapted with modification from the National Asthma Education and Prevention Program Asthma care)
Asthma Medications
β2-Agonists
Relieve the constriction by binding to specific receptors on airway smooth muscles cells.
SABAs such as albuterol have rapid onset of action: within 15 min and relatively short duration of action approximately 3–4 h.
LABAs effect can last up to 12 h.
Use of LABAs alone is not recommended and put the patient at risk for sudden and life threatening asthma exacerbation .
Frequent use of β2-agonists indicates poor asthma control.
-
Potential adverse effects
- Agitation, irritability, tremors.
- Insomnia, tachycardia, arrhythmia, and agitation.
- Hypokalemia.
- Patients with diabetes mellitus are at risk of hypoglycemia.
Inhaled Corticosteroids
Inhaled corticosteroids are the most commonly prescribed maintenance therapy for asthma.
They effectively decrease airway inflammation, decrease bronchial hypersensitiveness, relieve asthma symptoms, and improve lung function.
Slowing growth and adrenal suppression is a risk in the patients who require high-dose ICSs.
To minimize the risk of adverse effects, eliminate triggers that contribute to airway inflammation.
-
Adverse effects
- Oral thrush
-
Oral deposition and absorption of drug
- ◦ Rinse the mouth after taking the medication.
- ◦ Use metered dose inhaler.
Leukotriene Antagonists
They block inflammatory pathways that are active in the disease.
Most commonly used in children younger than 12 years is montelukast.
It is usually well tolerated.
Montelukast frequently used as add-on therapy in addition to ICSs.
Can be beneficial in patients with comorbid allergic rhinitis , recurrent viral-induced asthma exacerbation , and children with exercise-induced asthma.
Table 3.
Severity and initiating treatment: children 5–11 years
| Severity category | Days and night with symptoms | Pulmonary function | Preferred treatment |
|---|---|---|---|
| Intermittent |
≤ 2 days/week (days) ≤ 2 nights/month (nights) |
FEV1: > 80 % FEV1/FVC: > 85 % |
Step1: SABA PRN |
| Mild persistent |
3–6 days/week (days) 3–4 nights/month (nights) |
FEV1: > 80 % FEV1/FVC: > 80 % |
Step 2: Low-dose ICS |
| Moderate persistent | Daily (days)>1 night/week (nights) |
FEV1: 60–80 % FEV1/FVC: 75–80 % |
Step 3: Medium-dose ICS and consider short-course OCS |
| Severe persistent | Throughout (days) Often (nights) |
FEV1: < 60 % FEV1/FVC: < 75 % |
Step 4: Medium-dose ICS + LABA and consider short-course OCS |
OCS oral corticosteroids, LABA long-acting beta2 agonist, SABA short-acting beta2 agonist, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity, ICS inhaled corticosteroid
Prognosis of Asthma
-
Children at significant risk of having asthma symptoms later in life
-
Children with early onset asthma < 3 years of age:
- ◦ Who had three or more episode of wheezing per year and at least one major criterion (Eczema or parental eczema).
- ◦ Or at least two minor criteria (allergic rhinitis, wheezing unrelated to colds, or blood eosinophil count > 4 %).
-
Pneumonia
Definition
Infection of lung parenchyma
Causes of Pneumonia in Typical Age Groupings:
Three Weeks to Three Months
-
Chlamydia trachomatis
- Interstitial infiltrate on chest radiograph
-
Respiratory syncytial virus
- Bronchiolitis or pneumonia
-
Parainfluenza
- Bronchiolitis or pneumonia
-
Streptococcus pneumoniae
- Major cause of pneumonia throughout childhood
-
Bordetella pertussis
- Tracheobronchitis with severe paroxysm, usually no fever
- Pneumonia may occur secondary to aspiration
Three Months to Four Years
-
RSV, parainfluenza, human metapneumovirus, influenza, and rhinovirus
- Most toddler pneumonia is viral
-
Streptococcus pneumonia
- Major treatable pathogen in this age group
-
Mycoplasma pneumonia
- Increased incidence in children approaching school age
Five Years Through Adolescence
M. pneumonia
-
Chlamydophila pneumoniae
- Similar clinical presentation to mycoplasma
S. pneumoniae
Mycobacterium tuberculosis
Pneumonia Pathogens by Geographic Tropism
-
Histoplasmosis
- Ohio and Mississippi River Valleys and Caribbean
-
Coccidioidomycosis
- California, Arizona, and New Mexico
-
Blastomycosis
- Ohio, Mississippi River Valleys; Great salt lakes states
-
Legionella
- Infected water worldwide
-
Severe acute respiratory syndrome
- Asia
-
Avian influenza
- Southeast Asia
Pneumonia via Animal Vectors
-
Tularemia
- Rabbits and ticks
-
Psittacosis
- Birds specially parakeets
-
Q fever
- Sheep, cow, and goats
Pneumonia with Associated Exanthems
-
Varicella
- Human-to-human spread via airborne droplets nuclei
-
Measles
- Human-to-human spread via droplet
Clinical presentation
The hallmark symptoms of pneumonia are fever and cough.
Most of the children with fever and cough do not have pneumonia.
Tachypnea, retractions (intercostal, subcostal, suprasternal), wheezing, nasal flaring, and grunting, apnea and abdominal pain should be noted.
Grunting, in particular, may be a sign of pneumonia as well as of impending respiratory failure in younger patients/infants.
-
Tachypnea is the most sensitive and specific sign of pneumonia. Know the World Health Organization (WHO) Criteria as follows.
- > 50 breaths/min at 2–12 months of age.
- > 40 breaths/min at 1–5 years
- > 20 breaths/min for those older than 5 years
- Subtracting 10 if the child is febrile
Dullness to percussion, crackles, decreased breath sounds, and bronchial breath.
Absence of fever, tachypnea, increased work of breathing, and auscultatory abnormalities, bacterial pneumonia is unlikely.
Diagnosis
Typically clinical due to above.
Rapid influenza test may help to identify the cause of fever and to reduce the subsequent use of antibacterial agents.
CBC, chemistries, or serology will not help to identify the cause or aid in management.
Blood culture rarely helpful (10 % of the time organism are recovered).
Erythrocyte sedimentation rate and C-reactive protein determinations may be elevated.
-
Chest X-ray (Fig. 3)
- A chest radiograph will not change clinical management for most children who are being treated as outpatients.
- Afebrile children normally do not require chest radiography.
- Image if complicated pneumonia is considered, fever is prolonged and no obvious source of infection.
- Abdominal pain with normal appendix.
- CXR always lag the clinical response, no need to repeat CXR to confirm the response to antibiotics, only if deterioration.
A tuberculin skin test, if there is a risk factor or TB is considered.
Fig. 3.
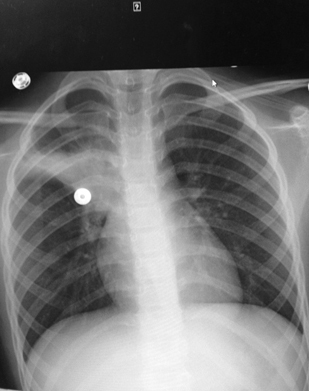
Nine-year-old female presents with cough and fever. Chest X-ray shows right upper lobe infiltrate
Treatment
Community acquired pneumonia (CAP) and national guideline for antibiotic indication
High dose of Amoxicillin, 80–90 mg/kg/day, for uncomplicated cases as outpatient
Augmentin if resistance or oral cefuroxime as outpatient
School age or older > 5 year Azithromycin to cover for mycoplasma
-
Indication for hospitalization: suspected sepsis, severe dehydration, toxic appearing, hypoxemia (under 90 %), unresponsive to outpatient therapy, inability to drink
- Administer IV fluids, oxygen, and antibiotics.
- Consider blood cultures, chemistry profiles, CBC, and chest radiography.
- If inpatient cefuroxime, ceftriaxone or cefotaxime are the drug of choice.
- In adolescent levofloxacin, gatifloxacin, moxifloxacin, may be used in atypical pneumonia.
- If Staphylococcus infection is considered add clindamycin or vancomycin.
- Uncomplicated pneumonia responds to antibiotics within 48–96 h.
- Plan if no response or persistent pneumonia; repeat CXR, consider the following; empyema, bacterial resistance, tuberculosis, non bacterial etiology, foreign body, bronchial obstruction, preexisting disease, CF, pulmonary sequestration, bronchiolitis obliterans, aspiration , and hypersensitivity pneumonitis.
Pleural Effusion
Background
-
Normal fluid balance
- 0.1–0.2 ml/kg of sterile colorless fluid
- Ninety percent filters from arterial capillaries, reabsorbed at venous capillaries
- About 10 % returned via lymphatic channels
-
Effusions
- > 10 ml of fluid in thoracic cavity
- Due to excessive filtration or defective absorption
- Transudates: low protein, lactate dehydrogenase (LDH),
-
Exudates:
- ◦ Pleural fluid-to-serum protein ratio is 0.5 or greater,
- ◦ Pleural fluid-to-serum LDH ratio is more than 0.6,
- ◦ Pleural fluid LDH concentration is more than 66 % of the upper limit of normal for serum
Clinical presentation
Should be suspected in any child with worsening pneumonia
Respiratory distress, tachypnea, pain with pleural inflammation, cough
Decreased to absent breath sounds, pleural rub if smaller collection of fluid
Egophony
Dullness to percussion
Midline shift
Diagnosis and management
CXR: opacification of the thorax, blunted costophrenic angle.
Decubitus views helpful if fluid is free flowing.
Ultrasound is helpful to determine the presence or absence of loculations.
CT scan is helpful to define pulmonary and fluid characteristics for complicated effusions/empyemas
Thoracentesis is helpful to relieve dyspnea for large effusions and determine characteristics of the fluid for treatment of underlying cause.
Oxygen for hypoxemia.
Consultation with experts as needed.
Possible causes: infection, chyle, blood, malignancy, and drug exposures.
In the neonatal period, chylothorax is the most frequent type of pleural effusion.
Pneumothorax
Causes
-
Primary spontaneous pneumothorax
- Occurs without trauma or underlying cause
- More frequently in tall, thin male, thought to have subpleural bleb
- Family history is positive in many patients
-
Secondary pneumothorax
- Underlying lung disease
- Trauma
- Loud music (air pressure)
- Catamenial pneumothorax (unusual condition associated with menses due to passage of intra abdominal air through a diaphragmatic defect)
Clinical presentation
The onset is abrupt, and the severity depends on lung collapse.
In simple pneumothorax, the lung collapses up to 30 %.
In tension pneumothorax, the patient will be hypoxemic dyspneic, and cyanotic.
PMI shifts due to displacement of intrathoracic organs to opposite side.
Diagnosis
CXR.
Expiratory film accentuates the contrast between lung marking and the clear area of pneumothorax.
Treatment
A small pneumothorax < 5 % may resolve spontaneously.
If > 5 % of pneumothorax or collapse, or if pneumothorax is recurrent or under tension, chest tube drainage is necessary.
Pneumothoraces complicating CF frequently recur and definitive treatment may be justified with the first episode.
Sclerosing with doxycycline (chemical pleurodesis).
Video assisted thoracic surgery is preferred therapy for blebectomy, pleural stripping, pleural brushing, and instillation of sclerosing agents over open thoracotomy.
Extensive pleural adhesion and aggressive pleural stripping may interfere with lung transplant in the future; these options must be discussed with the family.
Aspiration Syndrome
General issues
Small volume > 0.8 ml/kg and/or PH < 2.5 can cause hemorrhagic pneumonitis and atelectasis; large volume can cause pulmonary edema .
Most clinical changes appear within minutes to 1–2 h after aspiration event, radiographic change/infiltrate within 1–2 days unless large volume.
Management
Immediate suctioning of airway (do not attempt to neutralize acid).
Image chest.
Intubation and mechanical ventilation in severe cases.
Antibiotics may be used to cover anaerobes if definitive aspiration and usually only if admitted.
If the CXR is clear and patient is asymptomatic can be observed in the hospital or the office for few hours then home observation.
Most dangerous is hydrocarbon: patient may deteriorate impressively though may be minimally or asymptomatic initially. Prolonged observation (minimum 8 h) in setting able to manage respiratory failure is optimal.
Gastric emptying is contraindicated in hydrocarbon aspiration.
Foreign Body Aspiration
Background
Nuts especially peanuts are one 1/3 of cases .
Round globular FB, e.g., hotdog, grape, nuts, and candies are the most frequent offender to cause complete obstruction. Hotdogs are rarely seen as airway FB, because most of victims asphyxiate on the scene unless treated immediately.
Age < 3 years of age.
Clinical presentation
Initial event: violent paroxysms of coughing, choking, gagging, possible airway obstruction if the FB aspirated.
Asymptomatic interval: FB become lodged, reflexes fatigue, the immediate irritation subsides; this stage is the most dangerous, and account for most of delayed diagnosis, during the second stage (asymptomatic interval) that the physician may minimize the possibility of an FB accident, being reassured by absence of symptoms that no FB is present.
Positive history must never be ignored.
Negative history may be misleading.
Choking or coughing episode accompanied by wheezing are highly suggestive FB in airway
Physician should question parents about nuts, small toys, or anything similar.
58% lodge in the right bronchus.
Diagnosis
CXR is negative in 10–30 % of cases.
Patients suspected of having airway foreign bodies should undergo chest radiography.
The lack of radiological findings can never be used to exclude an airway foreign body; most objects are organic and likely to be radiolucent.
Positive findings on radiography can include hyperinflation, atelectasis, or infiltrate.
Inspiratory/expiratory or decubitus films may be helpful, although reports of sensitivity and specificity vary .
Soft-tissue films of the neck can be beneficial for detecting objects in the upper airway.
Patients with tracheostomy are at a higher risk.
Management
Treatment of choice prompt removal with rigid bronchoscopy.
Bronchoscopy can be deferred until proper hydration, emptying the stomach.
Complications
Retained foreign body is associated with bronchiectasis , hemoptysis and lung abscess .
Pulmonary Abscess
Background
Cystic area due to necrotic lung tissue at least 2 cm in diameter.
Primarily due to aspiration or infection.
Secondarily related to predisposing condition cavitary lesion, dysphagia, developmental delays and poor airway protective reflexes and/or poor airway clearance from neuromuscular weakness .
Both aerobic and anaerobic are common causes.
Anaerobic, e.g., bacteroides, fusobacterium, and aerobic Staphylococcus aureus.
Clinical presentation
Fever
Cough
Sputum production
Hemoptysis
Vomiting
Tachypnea
Chest pain
Weight loss
Diagnosis
CXR; air fluid level and CT scan can provide a better anatomic definition
Management
Conservative treatment with antimicrobial is recommended in hospital.
Clindamycin is a good choice until culture and sensitivity is available for immunocompetent hosts, broad spectrum coverage for immunodeficient patients.
2–3 weeks IV antibiotics.
Followed by oral course for 4–6 weeks.
Prognosis is excellent.
Congenital Pulmonary Malformations
Sequestration
Extralobar: more common in males; 65 % in the left lung, covered by pleura, fed by systemic artery and drained via systemic vein, may be associated with diaphragmatic hernia and colonic duplication.
Intralobar: typical in the lower lobe, systemic arterial supply, variable venous drainage, and airway connections.
Dullness on percussion, decreased breath sounds over the lesion, continuous murmur may be heard on the back, crackles if infected.
Imaging may detect pulmonary mass effect on fetal ultrasound or following birth.
CT scan with contrast will confirm the diagnosis.
Treatment is often surgical removal.
Retained sequestrations may become malignant.
Consultations: pulmonology and surgery.
Bronchogenic cyst
Arise from abnormal budding of the tracheal diverticulum.
Patient may become symptomatic if the cyst enlarges or becomes infected.
May be asymptomatic and found accidentally.
Fever, chest pain, and productive cough are the most common presenting symptoms, dysphagia if causing pressure on the surrounding structures.
CXR can show the cyst, and CT or MRI to demonstrate the anatomy.
Treatment is surgical removal.
Vascular ring/sling
May involve airway and or esophagus
Variable severity and timing of presentation
May cause stridor, cough, apnea, and dysphagia
Imaging chest is helpful, more common with right aortic arch
Congenital pulmonary adenomatoid malformation, lobar emphysema, and diaphragmatic hernia
Least common
May be seen on fetal imaging (U/S) and then resolve spontaneously
May cause severe respiratory distress and require surgery
Consult pulmonology
Primary Ciliary Dyskinesia (PCD)
Background
PCD is an autosomal recessive disease with extensive genetic heterogeneity .
Sixty percent of patients have identifiable mutations documented.
Abnormal ciliary motion and impaired mucociliary clearance.
Ultrastructural and functional defects of cilia result in the lack of effective ciliary motility.
In 50 % of the patients, PCD is associated with partial or complete Situs inversus.
Male infertility.
Some patients have asplenia or polysplenia with immune dysfunction .
Clinical presentation
Hundred percent of children have productive cough, sinusitis, and otitis media.
Chronic or recurring upper and lower respiratory infection.
Recurrent otitis media, otorrhea, may begin in neonates.
Lower lobe bronchiectasis , and frequent wheezing and diagnosed as asthma.
Diagnosis
The gold standard test is documentation of abnormal cilia ultrastructure (absent, abnormal dynein arms, radial spokes, doublet arrangements) on nasal and bronchial biopsies or scraping viewed on electron microscope.
Specimen should not be obtained during acute respiratory infection.
-
CT scan:
- Involvement of paranasal sinuses.
- Bronchiectasis.
Children should be examined several times per year.
Survival much longer than CF.
Treatment
ACT, antibiotics for infection documented on culture with sensitivities
ENT or surgery consult if needed
Bronchiectasis
Background
Destruction of the airway wall (bronchi and bronchioles) .
Loss of integrity of the muscular and elastic layers of the bronchial wall results in a dilated and an easily collapsible airway.
Obstructed sections of the bronchial tree.
Causes
CF is the most common cause of bronchiectasis in the children of the USA.
Impaired mucociliary clearance (CF and ciliary dyskinesia).
Infections (especially M Tb, Pseudomonas, adenovirus).
Immunodeficiency syndromes (humoral and cellular).
Immune mediated (connective tissues diseases, ABPA, IBD).
Airway injury (aspiration, inhalation of toxic fumes, hot gases).
Congenital or connective tissues abnormalities (yellow nail, Marfan, alpha 1 antitrypsin deficiency, airway cartilage deficiency, tracheobronchomegaly, young syndrome).
Obstructed airways (retained foreign body, intraluminal masses, and extraluminal compression).
Clinical presentation
Productive cough is the most common symptom of bronchiectasis.
Dyspnea, rhinosinusitis, and hemoptysis are less common.
Crackles, wheezing, and rhonchi; digital clubbing may also be present.
Diagnosis
Pulmonary function testing may show obstruction, restriction, and combinations depending on etiology.
Chest radiograph may reveal airway dilation, increased pulmonary markings with tram tracking (thickening of the bronchial walls), and areas of atelectasis .
(High resolution) HRCT scan is the gold standard for diagnosis and reveals detailed anatomy of the bronchial tree.
Lack of airway tapering with luminal dilation, bronchial wall thickening, honeycombing, and mucus plugging.
Treatment and prognosis
Establishing the primary cause is of critical importance and is best undertaken with direction from a pediatric pulmonologist .
Mucus clearance may be enhanced with hypertonic saline nebulization, inhaled mucolytics, and chest physiotherapy.
Inhaled corticosteroids can reduce airway obstruction.
Chronic macrolide therapy has also been found to be beneficial as anti-inflammatory.
Aggressive treatment of pseudomonal and Staphylococcal infections is indicated, but antimicrobial therapy should be targeted to specific pathogens.
Lobectomy is a last resort in refractory cases without systemic etiology .
Bronchopulmonary Dysplasia
Background
Recognized since 1960 following invention of positive pressure ventilation for premature infants and their survival .
“Old BPD” in late preterm infants with aggressive ventilation causing significant cystic disease.
“New BPD” is a chronic lung disease of extreme prematurity; lung immaturity typically associated with prolonged ventilation.
Pathophysiology
Volutrauma and barotrauma from positive pressure ventilation
Premature or immature lung
-
Inflammatory response to lung injury
- Chorioamnionitis and ureaplasma associated with increased incidence of BPD
Postnatal infection and poor nutrition increase risk
-
Severity determined by two factors:
- Oxygen requirement at 36 weeks postnatal age or home discharge if under 32 weeks at birth
- Oxygen requirement by 56 days postnatal age or home discharge if over 32 weeks at birth
Clinical presentation
Increased lung fluid, often need diuretics
Diffuse inflammation
Areas of atelectasis and hyperexpansion, retractions, respiratory distress evident on exam
Simplified lung and pulmonary vessel architecture
Often require prolonged supplemental oxygen
Management
-
Prevent premature deliveries
- Good prenatal care
- No smoking
-
Manage newborns wisely
- Give surfactant
- Ventilate gently, permit hypercapnia
- Avoid fluid retention and treat if occurs
- Nourish appropriately
- Manage oxygenation to preserve function but prevent retinopathy
- Monitor for complications, PDA, pulmonary hypertension, GERD, etc .
Pulmonary Hemosiderosis
Background
Repeated episodes of intra-alveolar bleeding that lead to abnormal accumulation of iron as hemosiderin in alveolar macrophages.
Subsequent development of pulmonary fibrosis and severe anemia.
Causes and associated conditions
Idiopathic pulmonary alveolar hemosiderosis (IPH)
-
Secondary pulmonary hemosiderosis
-
Cardiovascular:
- Congestive heart failure
- Pulmonary hypertension
- Mitral valve stenosis
-
Inflammatory/autoimmune
- Goodpasture syndrome
- Rheumatoid arthritis
- Wegener granulomatosis
- HSP
-
Allergic
- Heiner syndrome (cow’s milk hypersensitivity)
-
Clinical presentation
Iron deficiency.
Hemoptysis (helpful if occurs).
Alveolar infiltrate.
Presence of hemosiderin, it takes 48–72 h for macrophages to convert erythrocyte to hemosiderin
Widely variable from asymptomatic to shock and sudden death.
After episode of hemorrhage, the patient will present with wheezing, cough, dyspnea, bronchospasm, and alteration of blood gases.
Diagnosis
Best guided by consulting pulmonologist
Recurrent “pneumonia” fever, cough, abnormal chest radiograph
Hypochromic microcytic anemia
Elevation of plasma bilirubin
Infiltrate typically bilateral, and may spare the apices, often with hyperaeration
Ig E, cow’s milk antibody levels, stool specimen for heme
Urinalysis for nephritis
ANCA, ANA, Anti-GBM
Lung biopsy if diffuse alveolar hemorrhage (DAH)
Supportive treatment
Corticosteroid is the treatment of choice for IPH.
Highly dependent on the underlying cause.
Sarcoidosis
Background
Sarcoidosis is a noncaseating granuloma multisystem disease.
More common in African Americans.
Clinical presentation
Approximately 5 % of cases are asymptomatic and incidentally detected by chest radiography.
Systemic complaints (fever, anorexia): 45 % of cases.
Dyspnea on exertion, cough, chest pain, and hemoptysis (rare)—occur in 50 % of cases.
Crackles may be audible.
Anterior or posterior granulomatous uveitis (most frequent).
Erythema nodosum.
Diagnosis
-
Chest radiography is bilateral hilar or mediastinal adenopathy
- Stage 0: normal chest radiographic findings
- Stage I: bilateral hilar lymphadenopathy
- Stage II: bilateral hilar lymphadenopathy and infil- trates
- Stage III: infiltrates alone
- Stage IV: fibrosis
PFTs may either be normal or show restrictive +/− obstructive mechanics.
Hypercalcemia (about 10–13 % of patients)
Hypercalciuria (about one third of patients)
Elevated alkaline phosphatase level
Elevated angiotensin-converting enzyme (ACE) levels
Management
Asymptomatic patients may not require treatment.
In patients with minimal symptoms, serial reevaluation is prudent.
Treatment is indicated for patients with significant respiratory symptoms.
Corticosteroids can produce small improvements in the functional vital capacity and in the radiographic appearance in patients with more severe stage II and III disease.
Cystic Fibrosis
Genetics
The most common life shortening autosomal recessive disease due to mutation on the long arm of chromosome 7 .
Highest incidence in Caucasians, highly prevalent in Latinos, African Americans and seen rarely in African, Asian, and Native Americans races.
> 1500 CF transmembrane regulator (CFTR protein) polymorphisms are associated with CF.
The most prevalent mutation is F508 deletion (85 % of US population have at least one copy) associated with both pulmonary disease and pancreatic insufficiency.
Different classes of gene mutation are identified each with different level of CFTR production and function.
CFTR dysfunction/absence is associated with excessive reabsorption of sodium and deficient chloride secretion. The passive movement of water is decreased and airway secretions are dehydrated with very low surface liquid layer. Cilia become compressed inhibiting ciliary clearance and cough clearance, bacteria thrive; immune function is also abnormal at the airway surface. Repeated and chronic infection leads to airway damage and bronchiectasis in the lung and dysfunction of other organs.
Four organ systems prominently involved, respiratory, GI, GU, and integumentary (sweat glands).
Clinical presentation
-
Pulmonary:
- Cough is the most constant symptom dry at times, frequently productive.
- Increased anteroposterior diameter of the chest.
- Hyperresonance, scattered, and localized crackles.
- Clubbing, cyanosis, acute sinusitis, and nasal obstruction.
- Rhinorrhea and nasal polyps.
- As the lung disease progresses; exercise intolerance, shortness of breath, growth failure, cor-pulmonale (rarely), respiratory failure, and death
- Common pathogens include Staphylococcus aureus, and Pseudomonas aeruginosa though multidrug resistant organisms are increasingly common (MRSA, MDR, Stenotrophomonas maltophilia, and Burkholderia cepacia complex).
-
Gastrointestinal:
- Meconium ileus
- Fifteen to twenty percent of newborn with CF, the ileum are completely obstructed .
- Abdominal distension, emesis, failure to pass meconium in the first 24 and 48 h.
- KUB will show air-fluid level with ground glass material in the central abdomen.
- Gastrografin enema diagnostic and therapeutic.
- Hypertonic solution (electrolyte problem).
- Surgery if medical management fails (to prevent rupture and peritonitis).
- Pancreatic insufficient patients progress to complete or almost complete disruption of pancreatic acini and replacement with fibrous tissue. Lack of endogenous digestive enzymes causes fat malabsorption.
- Frequent foul bulky greasy stools, flatus, FTT < 10 %.
-
Vitamin ADEK deficiency
- ◦ Night blindness, decreased bone density, neurologic dysfunction (dementia, peripheral neuropathy), hypoprothrombinemia. and hemolytic anemia
-
Genitourinary:
- Sexual development is typically delayed 2–3 years
- Females have thicker cervical mucus and minimally delayed time to conception.
- Many females with CF have born healthy children.
- > 95 % of males the vas deferens and the seminal vesicles are obliterated or atretic with associated azoospermia.
- Sexual function is unimpaired.
-
Integumentary:
- Excessive loss of salt in sweat predisposes young children to salt depletion episodes.
- Hypochloremic alkalosis and dehydration, especially in hot environments, can be deadly in infants
Complications
-
Distal intestinal obstruction syndrome (DIOS)
- Typical in teens and those with poor enzyme replacement adherence.
- Fecal material accumulates in the terminal portion of the ileum and the cecum.
- Routine polyethylene glycol = (Miralax) helpful.
- Treatment also includes enteral stool softeners, osmotic laxatives, and osmotic enemas.
-
Rectal prolapse
- Previously common in infants with untreated CF.
- Due to a combination of intestinal disease and poor supporting musculature resulting from poor nutrition.
- Recurrence may be prevented by promoting easy stooling as well as by addressing underlying malnutrition.
- Evidence of rectal prolapse in otherwise healthy children is an indication for sweat chloride analysis to assess for undiagnosed CF.
-
Nasal polyps
- Are most prevalent in the second decade of life
- Local steroids and nasal decongestant occasionally provide some relief
- When completely obstruct the airway, rhinorrhea become constant, or widening of the nasal bridge is noticed, and surgical removal is indicated
-
Depression
- Common in adults with CF
Biliary cirrhosis 2–3 % of cases
IDDM: CFR DM (CF related diabetes mellitus), 8 % by 11–17 years, 18 % by 18–24 years, and 30 % over 30 years
Pan cirrhosis rare
Diagnosis
Newborn screening: most newborn identifies the immunoreactive trypsinogen and limited DNA testing on blood spot coupled with confirmatory sweat chloride test .
-
Sweat chloride abnormal if > 40 under 6 months of age, > 60 meq/L over 6 months old
- Pilocarpine iontophoresis to stimulate sweating, collection and chemical analysis of chloride content is the standard approach to diagnosis
- Positive results should be confirmed and negative results should be repeated if suspicion of diagnosis remain
- False-positive test can occur when testing performed on skin affected by eczema, or contaminated with cream or lotion
-
Non-CF conditions associated with positive sweat chloride test
- Untreated adrenal insufficiency
- Ectodermal dysplasia
- Hereditary nephrogenic diabetes insipidus
- G6PD
- Hypothyroidism
- Hypoparathyroidism
- Mucopolysaccharidoses
- Fucosidosis
- Malnutrition with hypoalbuminemia and edema
It is now known that patients with severe CF exist with normal sweat tests, uncommonly.
DNA testing: this test identifies > 90 % of cases with two CF mutations.
Pancreatic function testing: fecal elastase preferred method. Three days stool fat measurement.
Nasal potential difference testing: research tool.
*Newborn screening is not perfect and small numbers of patients are missed annually. Never stop thinking about this diagnosis even in older children and young adults.
Management per national guidelines
Center care: physician, nursing, social services, nutritional services, psychology, genetic counseling
Visits: monthly during first year, alternate months during second year, quarterly minimum thereafter with annual labs
Imaging: alternate year CXR, expect nodular densities, patchy atelectasis, especially upper lobe bronchiectasis, chest CT for complications, KUB and abdominal ultrasound as needed (PRN)
Pulmonary function: quarterly after 5–6 years, expect obstructive process often with modest response to a bronchodilator.
Microbiology: biannual and PRN sputum cultures, expect S. aureus or Pseudomonas aeruginosa most commonly; MRSA, MDR Pseudomonas and Stenotrophomonas maltophilia increasing nationally, Burkholderia cepacia are rare but stable prevalence.
Management—primary goals
Maintaining lung function as near to normal as possible by hydrating airway surface layer, liquefying mucus and using one of multiple methods to clear airways of mucus airway clearance techniques (ACTs).
Preventing infection by strict avoidance of other CF patients and careful isolation measures within clinics and hospitals.
Treating infection when present with directed antimicrobials.
Administering nutritional therapy (i.e., enzyme supplements, multivitamin and mineral supplements) to maintain adequate growth.
Managing complications
-
Mild acute pulmonary exacerbations of CF can be treated successfully at home with the following measures:
- Inhaled bronchodilator treatment
- Increasing the frequency of aerosols (hydration and mucolytics)
- ACTs, see below
- Antimicrobials (oral, inhaled)
- Moderate and severe pulmonary exacerbations are treated with hospital admission and aggressive respiratory treatment, IV antibiotics and anti-inflammatory medications, nutritional supplementation, tube feeding if needed
Treatments for CF may include the following
Pancreatic enzyme supplements
Multivitamins (including fat-soluble vitamins)
Bronchodilators
Hydrating agents (7 % hypertonic saline)
Mucolytics (DNase)
Nebulized, inhaled, oral, or intravenous antibiotics
ACT (chest physical therapy (CPT), oscillating chest compressive vests, positive expiratory pressure (PEP) devices, oscillating PEP, autogenic drainage (AD), active cycle breathing techniques (ACBTs), directed coughing)
Anti-inflammatory agents (Azithromycin MWF)
Antacids (to improve pancreatic enzyme function)
Agents to treat associated conditions or complications (e.g., insulin)
Agents devised to reverse abnormalities in chloride transport (e.g., ivacaftor)
-
Surgical therapy may be required for the treatment of the following respiratory complications:
- Respiratory—pneumothorax, massive recurrent or persistent hemoptysis, nasal polyps, persistent and chronic sinusitis.
- Lung transplantation is indicated for the treatment of end-stage lung disease.
- GI—meconium ileus, intussusception, gastrostomy tube placement for supplemental feeding, rectal prolapse.
Prognosis
-
Transition to adult caregivers required at all US nationally accredited centers
- Programs often formal to educate families and patients for transition.
- Typical transition over 18 years old, often at 21 years old.
Median cumulative survival is exceeding 35 years, male survival is somewhat better than females without apparent reason
Infants born now with CF center care likely to survive beyond 50 years
Known survivors in their eighties.
Obstructive Sleep Apnea (OSA)
Background
-
OSA must be distinguished from primary snoring
- Primary snoring = no associated obstructive events or gas exchange abnormalities, incidence 12–20 %.
- OSA = obstructive apnea and hypopneas often with arousal and gas exchange abnormalities.
The prevalence of OSA is 2–4 % in healthy children.
The disorder can occur at any age but is most common in the preschool age group (2–6 years) and adolescents.
A higher prevalence has been reported in African–American children.
Risk factors and associated conditions
Adenotonsillar hypertrophy
Obesity
Craniofacial abnormalities, specifically midface hypoplasia and micrognathia
Hypotonia, e.g., Down syndrome
Neuromuscular disease
Cerebral palsy .
Clinical presentation
Loud nightly snoring with observed apnea spells
Parents may note that the child is a restless sleeper
Sweats while sleeping
Sleeps in an abnormal position with the neck extended
Chronic mouth breathing with chronic nasal congestion
Morning headaches
Excessive daytime sleepiness is more common among older children.
Mood changes
ADHD-like symptoms involving inattention and easy distractibility, or academic problems due to difficulty concentrating
Adenoidal facies as well as signs of atopy or nasal congestion such as “allergic shiners,”
Nasal septal deviation
Enlarged turbinates
Redundant soft palate with a long uvula
Cor pulmonale or systemic hypertension (rare in children)
Nocturnal enuresis
Management
All children should be screened for snoring.
Complex, high-risk patients should be referred to a specialist, e.g., craniofacial disorders, genetic syndromes, and neuromuscular disorders.
History and physical examination cannot distinguish between primary snoring and OSA.
Polysomnography is the diagnostic test of choice.
Adenotonsillectomy is the first line of therapy and curative for about 80 % of children with OSA.
Noninvasive positive airway pressure is an option for those who are not surgical candidates or who respond poorly to surgery.
High-risk patients (those with complicated diseases and severe OSA) should be monitored as inpatients postoperatively.
Patients should be reevaluated postoperatively to determine if additional treatment is required.
Patients with neuromuscular disease may desaturate in sleep but appear well when awake. Overnight saturation monitoring can be very helpful to recognize issues that require additional support.
ALTE/Sudden Infant Death Syndrome
Background
-
ALTE a subjective report of a death like event.
- GERD most common association for awake ALTE
- Neurologic from seizure second most common association
- Respiratory from pertussis and RSV third most common association
- High index of suspicion of child abuse important
- Observation, testing, and treatment as supported by history and exam
SIDS age 2–4 months with most deaths having occurred by 6 months
-
National recommendation on SIDS prevention
- “Back to Sleep” supine position except few conditions
- Marked decline in SIDS rate following this public policy education
- Tummy time while awake
- No smoking pre- or postnatally
-
Recognized risk factors:
- Next born siblings of first born infants dying of any noninfectious natural causes are at significant increased risk of infant death from the same cause
- ALTE very rarely associated
- Infant factors: prematurity, low birth weight, co-sleeping, prone sleeping, and overheating
- Maternal factors: young maternal age, smoking during pregnancy, and late or absent prenatal care
More than 95 % of SIDS cases are associated with one or more risk factors.
-
National recommendation on pacifiers:
- Use pacifier once breast feeding has been established
- Offer pacifier at bedtime or nap time
- No correlation between pacifier use and length of breast feeding
Chest Deformities
Pectus Excavatum (Funnel Chest; Fig. 4)
Fig. 4.

Pectus Excavatum 12-year-old healthy boy with funnel shaped chest “pectus excavatum”
-
Incidence
- > 90 % of congenital wall anomalies
- 1/400 birth with 9:1 in males
- Can be isolated or associated with connective tissue diseases like Marfan or Ehlers–Danlos syndrome, neuromuscular disease like SMA.
Clinical presentation
At birth may be not associated with any symptoms
-
In severe cases, patient may become symptomatic
- Decrease exercise tolerance
- Fatigue
- Chest pain
- Palpitations
- Recurrent chest infections
- Wheezing
- Stridor
- Cough
Children may experience a significant psychological stress because of cosmetic appearance
Investigation
CXR; increase AP diameter
-
CT for Haller index, if significant, justifies repair
- HI = lateral internal rib cage dimension/AP internal sternum to vertebrae dimension.
- Normal value 2.5
- Repair if over 3.25
EKG; may show WPW, lateral axis deviations
Treatment
Based on severity of deformity and physiologic compromise
If neuromuscular disease worsens due to excessive efforts and retractions, responds to ventilation such as noninvasive positive pressure ventilation (NIPPV)
Mild: observation and physical therapy to maintain posture
Corrective surgery if significant physiologic compromise (Nuss procedure)
Pectus Carinatum (pigeon chest)
-
Background
- Anterior displacement of midsternum and adjacent costal cartilage
- It is rare 1/1500 of chest wall deformities
- Associated with mild to moderate scoliosis, mitral valve prolapse, and coarctation of aorta
-
Clinical presentation
- Rarely causes limitations
- Physical appearance most common complaint
- Haller index less than two is significant
-
Treatment
- Surgery for cosmetic and psychological stress
Contributor Information
Osama Naga, Email: osamanaga@yahoo.com.
Karen Hardy, Phone: 510-428-3305, Email: khardy@mail.cho.org.
Osama Naga, Email: osama.naga@ttuhsc.edu.
Suggested Readings
- 1.AAP Subcommittee on Diagnosis and Management of Bronchiolitis. Pediatrics. 2006;118(4):1774–93. doi: 10.1542/peds.2006-2223. [DOI] [PubMed] [Google Scholar]
- 2.AAP Committee on Fetus and Newborn. Apnea, sudden infant death syndrome, and home monitoring. Pediatrics. 2003;111(4):914–7. doi: 10.1542/peds.111.4.914. [DOI] [PubMed] [Google Scholar]
- 3.Alario AJ, McCarthy PL, Markowitz R. Usefulness of chest radiographs in children with acute lower respiratory tract disease. J Pediatr. 1987;111:187–93. doi: 10.1016/S0022-3476(87)80065-3. [DOI] [PubMed] [Google Scholar]
- 4.Cherry JD. Clinical practice: croup. N Engl Med. 2008;258:384–91. doi: 10.1056/NEJMcp072022. [DOI] [PubMed] [Google Scholar]
- 5.Cotton RT, Reilly JS. Stridor and airway obstruction. In: Bluestone C, Stool S, Kenna M, editors. Pediatric otolaryngology. 3. Philadelphia: WB Saunders; 1995. pp. 1275–86. [Google Scholar]
- 6.Dodge JA, Lewis PA. Cystic Fibrosis mortality and survival in the UK: 1947–2003. Eur Respir J. 2007;29(3):522–6. doi: 10.1183/09031936.00099506. [DOI] [PubMed] [Google Scholar]
- 7.Haddad GG, Green TP. Diagnosis approach to respiratory disorders. In: Kliegman RM, Behrman RE, Jenson HB, Stanson BF, editors. Nelson textbook of pediatrics. 18. Philadelphia: Saunders Elsevier; 2007. pp. 1731–2. [Google Scholar]
- 8.Haller JA, Kramer SS, Lietman A. Use of CT scans in selection of patients for pectusexcavatum surgery: a preliminary report. J Pediatr Surg. 1987;22:904–6. doi: 10.1016/S0022-3468(87)80585-7. [DOI] [PubMed] [Google Scholar]
- 9.Hardy KA. Airway Clearance Techniques. AAP section on pediatric pulmonology executive committee. 1st ed. “Blue Book” AAP; 2011. p. 894–912.
- 10.Holinger LD. Evaluation of stridor and wheezing. In: Holinger LD, editor. Pediatric laryngology & bronchoesophogology. New York: Lipppincott-Raven; 1997. [Google Scholar]
- 11.Jobe A, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9. doi: 10.1164/ajrccm.163.7.2011060. [DOI] [PubMed] [Google Scholar]
- 12.Koves T, Rubin S. Long-term complication of congenital esophageal atresia and/or tracheaoesophageal fistula. Chest. 2004;126:915–25. [DOI] [PubMed]
- 13.LeGrys VA, Yankaskas JR, Quittell LM, Marshall BC, Mogayzel PJ., Jr Diagnostic sweat testing: the Cystic Fibrosis Foundation guidelines. J Pediatr. 2007;151:85–9. doi: 10.1016/j.jpeds.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Mayer OH, Allen J. Chest wall and spinal deformities pediatric pulmonology: AAP section on pediatric pulmonology executive committee. 1st ed. “Blue Book” AAP; 2011. p. 310–45.
- 15.Mettler FA, Huda W, Yoshizumi T. Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology. 2008;248:254–63. doi: 10.1148/radiol.2481071451. [DOI] [PubMed] [Google Scholar]
- 16.Mindell JA, Owens JA. A clinical guide to pediatric sleep: diagnosis and management of sleep problems. Philadelphia: Lippincott Williams & Wilkins; 2003. [Google Scholar]
- 17.National Heart, Lung, and blood Institute. National Asthma Education Program Expert Panel Report 3 (EPR-3). Guidelines for the Diagnosis and Management of Asthma. Bethesda: National Institutes of Health; 2007. (NIH Publication No. 08–5846).
- 18.Nevin MA. Pulmonary hemosiderosis. In: Kliegman RM, Stanton BF, St. Geme JW III, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 19. Philadelphia: Saunders Elsevier; 2011. pp. 1498–500. [Google Scholar]
- 19.Northway WH, Rosen RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med. 1967;276:357–68. doi: 10.1056/NEJM196702162760701. [DOI] [PubMed] [Google Scholar]
- 20.Penugonda M, Simon D, Light M. Primary ciliary dyskinesia and other genetic lung diseases pediatric pulmonology: AAP section on pediatric pulmonology executive committee. 1st ed. “Blue Book” AAP; 2011. p. 745–75.
- 21.Schechter M, O’Sullivan B. Cystic fibrosis. Pediatric pulmonology: AAP section on pediatric pulmonology executive committee. 1st ed. “Blue Book” AAP; 2011. p. 717–43.
- 22.Sharma G, Conrad C. Croup, epiglottitis and bacterial tracheitis pediatric pulmonology: AAP section on pediatric pulmonology executive committee. 1st ed. “Blue Book” AAP; 2011. p. 348–63.
- 23.Sidhu M, Goske MJ, Connolly B. Image gently, step lightly: promoting radiation safety in pediatric interventional radiology. Am J Roentgenol. 2010;195:W299–W301. doi: 10.2214/AJR.09.3938. [DOI] [PubMed] [Google Scholar]
- 24.Stillwell P. Bronchiectasis pediatric Pulmonology: AAP section on pediatric pulmonology executive committee. 1st ed. “Blue Book” AAP; 2011. p. 346–375.
- 25.Weinberger M. Bronchiolitis. Pediatric pulmonology: AAP section on pediatric pulmonology executive committee. 1st ed. “Blue Book” AAP; 2011. p. 377–90.


