Abstract
Local and systemic infections are a significant cause of morbidity and mortality among immunocompromised children, including but not limited to patients with hematologic and solid malignancies, congenital or acquired immunodeficiencies, or hematopoietic cell or solid organ transplantation patients. Progression to septic shock can be rapid and profound and thus requires specific diagnostic and treatment approaches. This chapter will discuss the diagnosis and the initial hemodynamic management strategies of septic shock in immunocompromised children, including strategies to improve oxygen delivery, reduce metabolic demand, and monitor hemodynamic response to resuscitation. This chapter also discusses strategies to reverse septic shock pathobiology, including the use of both empiric and targeted anti-infective strategies and pharmacologic and cell therapy-based immunomodulation. Specific consideration is also paid to the management of high-risk subpopulations and the care of septic shock patients with resolving injury.
Keywords: Pediatric; Sepsis; Shock, septic; Immunocompromised host; Hematopoietic stem cell transplantation; Cardiopulmonary resuscitation
Introduction
Children with malignancies, primary immunodeficiencies, prior solid organ or hematopoietic cell transplantation, and other immunocompromising conditions are at increased risk of becoming septic and dying from sepsis. Therefore, there are unique considerations for the management of sepsis in the immunocompromised child. First and foremost, fluid resuscitation and empiric broad-spectrum antibiotics covering opportunistic infections within the first 30 min of presentation are critical for reducing morbidity and mortality. This chapter will discuss available data that can be used to tailor the management of sepsis in this population.
Diagnostic Criteria
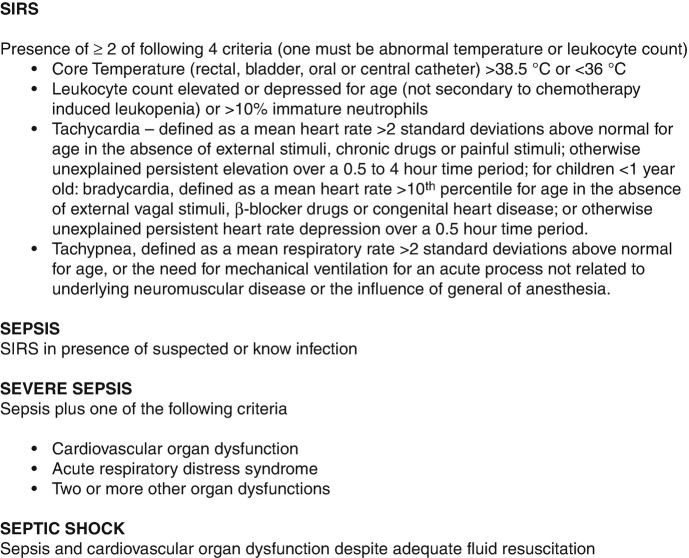
Initial management of presumed sepsis follows standard pediatric sepsis guidelines. According to the International Pediatric Sepsis Consensus Conference (IPSCC) of 2005, the spectrum of sepsis can be divided into systemic inflammatory response syndrome (SIRS), sepsis, severe sepsis, and septic shock [1]. Systemic inflammatory response syndrome describes an inflammatory state with immune activation that may have a variety of underlying etiologies. It is defined by two of the following four criteria (Fig. 14.1). Sepsis is defined by SIRS with a suspected or proven underlying infection. The diagnosis can be escalated to severe sepsis if the patient has developed cardiovascular organ dysfunction or acute respiratory distress syndrome or two other organ system involvements. In cases where cardiovascular dysfunction is refractory to adequate fluid resuscitation, the diagnosis can be further escalated to septic shock.
Fig. 14.1.
Sepsis definitions. (Legend: Ref. [1])
In immunocompromised children, SIRS criteria alone may be present for a variety of infectious and noninfectious reasons (discussed in section “Considerations in High-Risk Patients”). Therefore, a high index of suspicion for infectious causes of SIRS physiology is mandatory. Importantly, the diagnosis of sepsis does not require a proven infection, but rather can be made with clinical suspicion for infection alone. Therefore, we and others advocate that the diagnosis of sepsis be made early, before progression from sepsis to severe sepsis and/or septic shock. [2, 3]
Initial Hemodynamic Management Strategies
The majority of data support that patients meeting the diagnostic criteria for sepsis should receive early empiric hemodynamic management. Interventions should aim to stabilize cardiovascular and respiratory systems, achieve adequate oxygen delivery by normalizing blood pressure and end-organ perfusion with initial fluid resuscitation, and maintain oxygenation and ventilation with supplementation oxygen support and possible advanced airway.
Early goal-directed therapy includes rapid intravascular volume re-expansion guided by hemodynamic monitoring and markers of organ dysfunction. Although initial reports demonstrated reduce mortality in adult emergency department populations by up to 15%, recent re-examination of these bundled interventions has not demonstrated reduction in mortality in adult populations [4–6]. Reports in pediatrics are not specific to immunocompromised patients, but demonstrate that early reversal of shock is associated with improved survival [7–10]. Therefore, the American College of Critical Care Medicine published the updated 2014 “Clinical Guidelines for Hemodynamic Support of Neonates and Children with Septic Shock” (Fig. 14.2), which advocates that recognition of fluid refractory shock should occur within the first 15 min [11, 12].
Fig. 14.2.
Clinical guidelines for hemodynamic support of neonates and children with septic shock. (Legend: Ref. [11, 12])
Strategies to Improve Oxygen Delivery
Early fluid resuscitation is critical to improving cardiac output and oxygen delivery during sepsis. Although some retrospective analyses have analyzed potential benefits for different types of resuscitation fluids, strong prospective data do not exist to favor the use of crystalloid over colloid or balanced over unbalanced fluids in this population [13–15]. The use of hydroxyethyl starches (HESs) is not recommended [16]. Rapid fluid resuscitation typically requires two large-bore peripheral intravenous catheters and should not rely solely on surgically implanted central venous catheters; in cases where difficult peripheral venous access delays fluid resuscitation, physicians should establish intraosseous access [17].
Although the ACCM guidelines advocate for early and aggressive fluid resuscitation of 20–60 mL/kg, the ideal volume of resuscitation fluids likely varies per patient and should be guided first and foremost by clinical exam. Resolution of hypotension, tachycardia, and impaired perfusion can be used to guide volume of resuscitation fluids [17]. Low central venous pressure (CVP) may be used to titrate volume resuscitation, but absolute measurements vary from child to child and thus require frequent or continuous measurement to establish patient-specific trends. Care should be taken when interpreting central venous pressure, as central venous pressure is related to both intravascular volume and right and left ventricular compliance. Further, children in septic shock with elevated central venous pressure frequently have diastolic dysfunction and left heart strain, which are associated with increased mortality [18–20]. Prediction of fluid responsiveness using other hemodynamic variables is an area of active interest, with some data supporting the use of aortic flow velocity and arterial pulse pressure variability with respiration [21, 22].
Oxygen-Carrying Capacity
As arterial oxygen content = 1.36 (Hb g/dL) (% saturation) + 0.003 (PaO2), maintaining an adequate hemoglobin level is crucial for maximizing the oxygen content in blood in sepsis physiology. In the general pediatric ICU population, thresholds of >7 g/dL and > 10 g/dL have been shown to be equally safe, with the advantage that a threshold of >7 g/dL resulted in fewer blood transfusions and potentially fewer nosocomial infections [23]. These results have been repeated in children with sepsis who have completed the resuscitation and stabilization period although sample size limitations precluded an appropriate analysis of mortality differences [24, 25]. However, the optimal transfusion threshold for patients with active septic shock has not been determined, and as of 2014, the majority of English- and French-speaking pediatric intensivists appear to use a transfusion threshold of >10 g/dL for children in active septic shock [26]. In a retrospective propensity score-adjusted study, more frequent RBC transfusions were associated with mortality in septic adults with hematologic malignancies, although whether this may be due to transfusion effects or underlying coagulopathy or hematologic failure is unknown [27]. As immunocompromised patients may have ineffective erythropoiesis and/or increased immune and nonimmune erythrocyte destruction, close attention to hemoglobin levels is warranted in sepsis [28].
Maintenance of hemoglobin saturation is critical for adequate arterial oxygen content and therefore is a principal component of managing sepsis physiology. Hence, early use of noninvasive supplemental oxygen, including nasal cannula, face mask, and non-rebreather masks, is warranted for pediatric immunocompromised patients with sepsis. Although pediatric data are lacking, among immunocompromised adults with infection-related acute respiratory failure, early application of noninvasive oxygen support can reduce progression to invasive mechanical ventilation [29, 30]. Data supporting the optimal timing of transition to noninvasive positive-pressure ventilation, and/or invasive mechanical ventilation, are limited in pediatrics. However, adult data suggest that patients who fail noninvasive ventilation should transition rapidly to endotracheal intubation, as prolonged failure of noninvasive ventilation is strongly associated with mortality [31]. A recent international sepsis point prevalence study identified that more than two-thirds of pediatric HCT patients with sepsis require endotracheal intubation during their course of sepsis [32]. Therefore we advocate that aggressive oxygenation support be offered to all critically ill immunocompromised children with sepsis.
Vasoactive Infusions
Immunocompromised children with septic shock may require vasoactive infusions to improve their ability to meet the elevated metabolic demand of sepsis. Some patients may also have myocardial depression in the face of sepsis-induced hypercytokinemia [33, 34]. The choice of vasoactive infusions depends largely on clinical assessment of warm (vasodilatory) vs. cold (vasoconstricted) shock. Two separate double-blind, randomized controlled trial of dopamine vs. epinephrine for pediatric cold septic shock demonstrated clinical superiority of epinephrine over dopamine for multiple endpoints [35, 36]. Several other larger studies of adult and pediatric septic shock have demonstrated superiority of norepinephrine over dopamine for warm shock as well [37, 38]. Pediatric oncology patients with anthracycline exposure of any amount, particularly >300 mg/m2 but even as low as 50 mg/m2, are at increased risk for cardiotoxicity and may require significant attention to cardiopulmonary dynamics [39]. Additional vasoactive infusions including milrinone, terlipressin, levosimendan, and other agents may be required for refractory shock, although data are insufficient to recommend specific use in the pediatric immunocompromised population.
Extracorporeal Support (ECLS)
Patients who are unable to meet systemic oxygen demand despite maximal medical management may benefit from venoarterial extracorporeal life support (VA-ECLS) to partially or completely augment cardiac output. The use of VA-ECLS is associated with approximately 50% mortality in pediatric septic shock [40]. Reports of ECLS use in immunocompromised children suggest approximately one third survive to hospital discharge [41]. The decision to initiate VA-ECLS for septic shock in immunocompromised children requires rapid but careful multidisciplinary discussion with informed parental consent where possible.
Strategies to Reduce Metabolic Demand
In addition to improving oxygen delivery, efforts to reduce metabolic demand may help balance tissue oxygen consumption and improve end-organ function. By reducing work of breathing and off-loading the left ventricle, invasive mechanical ventilation can reduce metabolic expenditure by up to 30% [42, 43]. Studies of timing of mechanical ventilation in adult sepsis suggest that delayed intubation may be associated with adverse outcomes and some patients may experience cardiopulmonary arrest due to decreased preload associated with vasodilation from sedation required for the procedure [44]. Of note, some data suggest that the use of etomidate during endotracheal intubation, particularly in patients receiving exogenous hydrocortisone, is associated with worse outcomes, potentially due to medication-induced adrenal suppression [45, 46].
Other strategies to reduce metabolic demand include control of fever with antipyretics, although data supporting the use of nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen are limited at this time [47–50]. Although sedation may play a role in reducing metabolic demand, current studies are inadequate to recommend an ideal sedation medication regimen at this time.
Hemodynamic Monitoring
In addition to measurement of central venous pressure and pulse pressure variability as described above, a variety of tools can be used to trend organ dysfunction over time. General biochemical markers of shock include lactate, base deficit, and anion gap, which show moderate-to-strong correlation with each other [51]. Several studies support the use of mixed venous oxygenation saturation measurements in the management of shock, wherein abnormally large arterial-venous saturation differential can suggest inadequate oxygenation and/or mitochondrial dysfunction prior to the rise of traditional markers such as serum lactate [52–56]. Data supporting the routine use of transpulmonary thermodilution are insufficient at this time [57]. Continuous blood pressure transducing with arterial lines allows monitoring of arterial blood pressure and may be useful for rapid changes in hemodynamics. Although ideal blood pressure for each patient varies, the International Pediatric Sepsis Consensus Conference definitions of tachycardia, bradycardia, tachypnea, and hypotension in pediatric sepsis are listed in Table 14.1 (PMID 15636651) [1].
Table 14.1.
Vital sign abnormalities in pediatric sepsis
| Age | Tachycardia | Bradycardia | Respiratory rate | Systolic blood pressure |
|---|---|---|---|---|
| 0 days–1 week | >180 | <100 | >50 | < 65 |
| 1 week–1 month | >180 | <100 | >40 | <75 |
| 1 month–1 year | >180 | <90 | >34 | <100 |
| 2–5 years | >140 | N/A | >22 | <94 |
| 6–12 years | >130 | N/A | >18 | <105 |
| 13–<18 years | >110 | N/A | >14 | <117 |
Legend: Adapted from Ref. [1]
Anti-infective Strategies
Diagnostics
In patients with central catheters, it is recommended to obtain blood cultures both from peripheral venipuncture and from indwelling central catheters. A meta-analysis assessing the utility of paired central and peripheral blood cultures in both pediatric and adult cancer patients with suspected bloodstream infections demonstrated positive paired blood cultures in 17% of cases; 13% were only identified by peripheral blood and 28% only by central venous line samples [58]. Furthermore, a single center study of pediatric cancer patients demonstrated cases in which peripheral blood cultures were positive though central cultures were not. In this study of the 228 episodes of bacteremia, the peripheral blood culture was the only positive culture in 28 cases (12%). Therefore, obtaining both peripheral blood and central cultures could improve the sensitivity of bacteremia detection [59]. Additionally, obtaining both peripheral blood and central cultures and assessing the difference in time to detection in situations when both result in positive may assist with determination of catheter-related sepsis. A positive central line culture two or more hours prior to a positive peripheral culture has been associated with three times increased odds of catheter-related sepsis [60]. There was no direct evidence about the influence of peripheral blood cultures on clinical management decisions. Diagnostic yield can be increased by collecting two sets of blood cultures, and anaerobic cultures should be obtained as well. Blood cultures should be drawn prior to antibiotic administration if possible, but should not delay antibiotic administration [16].
Empiric Therapy
Careful attention to opportunistic organisms including bacteria, viruses, and fungi must be taken into consideration as well as individual patients’ prior infectious history, specifically resistant organisms. Antibiotic administration should occur as early as possible and has been associated with reduced mortality in general pediatric septic shock [61, 62]. In the immunocompromised host, a third- or fourth-generation cephalosporin or carbapenem is frequently indicated for empiric gram-negative coverage, with the addition of vancomycin or other anti-methicillin-resistant Staphylococcus aureus (MRSA) therapy depending on patient and geographic risk factors. Furthermore, for patients presenting with shock, additional gram-negative bacterial coverage with a monobactam, fluoroquinolone, or aminoglycoside is frequently warranted for synergistic effect. Antimicrobial coverage for patients with suspected enteric sepsis or aspiration should include anaerobic coverage. Infectious disease subspecialty consultation is recommended to tailor coverage, review prior infectious history and patient-specific risk factors, recommend alternative therapies in the setting of medication allergy or intolerance, and guide dose adjustment in renal and hepatic injury. Removal of central lines should be strongly considered for refractory septic shock or recurrent positive blood cultures with differential timeto positivity with consultation from infectious disease specialists [63].
Specific Pathogens
Bacterial
Common gram-positive organisms include skin and mucosa-colonizing bacteria such as Staphylococcus aureus and epidermidis and Streptococcus pyogenes and the viridans group streptococci [64, 65]. Streptococcus pneumoniae and enterococci can cause disseminated disease from the upper/lower respiratory and gastrointestinal tracts and may present with antibiotic resistance requiring vancomycin, linezolid, ceftaroline, daptomycin, or other broad antibiotics. Common gram-negative organisms include respiratory colonizers (Haemophilus, Moraxella) as well as enteric and urologic organisms such as Escherichia and Klebsiella. These and other organisms such as Pseudomonas may present with multidrug resistance requiring carbapenem, fluoroquinolone, monobactam, and other extended spectrum therapies. Patients with severe Clostridium difficile enterocolitis may present with sepsis physiology as well.
Viral
Community respiratory viruses including influenza, adenovirus, and enteroviruses can produce SIRS in immunocompromised children. Primary HSV-1 and 2 can cause liver failure, leading to a sepsis/shock overlap. Other herpesviruses such as CMV and EBV can also cause disseminated viremia with viral sepsis [66, 67].
Locally aggressive fungal infections or disseminated fungemia due to Candida, Aspergillus, zygomycoses of the Mucorales order, Pneumocystis, and endemic mycoses due to Histoplasma or Blastomyces can also cause sepsis physiology in immunocompromised children and require a high index of suspicion due to the frequent challenge in obtaining a microbiologic diagnosis [68, 69]. Due to the broad number of common and uncommon organisms that can cause sepsis in immunocompromised children, we strongly advocate close collaboration with infectious disease specialists to guide the diagnostic evaluation and treatment strategy.
Pharmacokinetic/Dynamic Considerations
Pharmacokinetic monitoring of drug levels is recommended where possible [16]. Vancomycin, gentamicin, tobramycin, and voriconazole levels should be followed when used for extended courses of therapy to ensure both therapeutic levels and avoidance of toxicity. Prudent attention to additional medications that may interact with anti-infectives in this high-risk population, specifically, the use of tacrolimus/cyclosporine for immunosuppression in the HSCT patient, is essential. Care should be paid to avoid drug-drug interactions, and hepatic and renal function should be assessed frequently, with dose adjustments as needed. Specialized clinical pharmacologists may assist in this role and reduce the frequency of deleterious drug-drug interactions [70, 71].
Immunomodulation
Patients with vasoplegia, refractory shock, adrenal insufficiency, long-term corticosteroid therapy, or short-term high-dose corticosteroid therapy may require stress-dose hydrocortisone; although steroids are used in nearly 50% of all children with septic shock, they have not been associated with improved outcomes, and some adult data suggest an association with mortality [72–79]. Although corticosteroids can modulate beta-adrenergic receptors, a growing body of evidence suggests they also may affect sepsis physiology through immunomodulation of innate immunity [78, 80]. The optimal patient selection, if any, for the use of corticosteroids in immunocompromised children with septic shock is unclear at this time. Minimal or absent cortisol increase in response to cosyntropin stimulation likely suggests adrenal insufficiency.
Granulocyte colony-stimulating factor (G-CSF) should be used in most neutropenic patients with nonmyeloid malignancies whose neutropenia is expected to respond to colony-stimulating factors [81]. Some centers perform granulocyte infusions to augment antimicrobial immunity, although studies do not support routine use in neutropenic sepsis and other immunocompromised states with infection [82]. Some centers have reported success in augmenting immunity with donor lymphocyte infusions (DLI), particularly with a cell source selected for anti-pathogen T cells [81, 83] or with engineered anti-pathogen cytotoxic T lymphocytes [84, 85]. Each of these therapies bear the risk of triggering inflammation, and clinicians should note that some patient may get worse due to intensified systemic inflammation prior to seeing clinical improvement in hemodynamics and metrics of end-organ function.
Standard use of IVIG in adult and pediatric sepsis has not demonstrated mortality benefit, although select patients with severe hypogammaglobulinemia may benefit [86]. Selective removal of inflammatory cytokines and bacterial endotoxin using customized pheresis membranes has been shown to affect cytokine levels in patients with septic shock, but data supporting a mortality benefit are lacking [87, 88]. Adult sepsis trials of activated protein C, immunomodulation in sepsis, and ARDS have not shown an overall survival benefit, but some subgroups may benefit [89–91]. Strong data supporting the use of antithrombin or thrombomodulin to control sepsis-related coagulopathy are not available at this time [16].
Management After the Acute Resuscitation
Systemic organ toxicities are common during and after the acute resuscitation of septic shock. For example, ARDS co-occurs with sepsis frequently. Pediatric allogeneic HCT patients with ARDS have <40% survival, and mechanical ventilation strategies differ widely by center and include high-frequency oscillatory ventilation (HFOV), inhaled nitric oxide, and veno-venous extracorporeal life support (VV-ECLS) [32, 92]. Secondary AKI is also strongly associated with mortality, and typical indications for continuous veno-venous hemodialfiltration (CVVHDF), including refractory fluid overload and uncontrollable electrolyte abnormalities, should be applied in immunocompromised patients [93]. Risk for secondary infections remains high due to a combination of indwelling invasive devices, altered intestinal and respiratory microbiomes, and sepsis-induced immunoparalysis, and thus care should be maintained to surveil for potential new infections [94]. As pediatric immunocompromised patients are at risk for prolonged PICU stay, they are also at high risk for immobilization-related weakness, and thus physical, occupational, speech, and rehabilitation therapies should be offered to maximize return of daily functional status [95, 96].
Considerations in High-Risk Patients
Immunocompromised patients, especially those with neutropenia, are at increased risk of infection and sepsis. The combination of fever and neutropenia warrants immediate medical attention. Several adult and pediatric studies have evaluated the risk of severe infection and sepsis in patients presenting with fever and neutropenia. An increase odds [OR = 1.80 (95% C.I. 1.43 to 2.26)] of severe infection was associated with severe neutropenia (defined as absolute neutrophil count <100/mm3) in patients presenting with both neutropenia and fever [97–100]. Furthermore, a single center analysis of temperature as a continuous variable in pediatric cancer patients with neutropenia and fever and the associated need for critical care support demonstrated that children presenting with a one degree increase in temperature had a relative increase of the odds of receiving critical care within the first 24 h [1.74 (95% 1.25 to 2.43)] [101].
Predicting Patients at High Risk of Sepsis
Few studies have been published that offer predictive models of immunocompromised patients presenting with fever, neutropenia, and risk for mortality. Some data exist supporting the ability of laboratory markers, including CRP, lactate, and liver and kidney function tests to predict length of hospital stay in patients with fever and neutropenia; however, data are absent on the ability of these parameters to predict the need for critical care. In general, single center studies that have shown lactate, albumin, and creatinine levels have decent specificity though low sensitivity in predicting mortality [102, 103]. A multicenter study of adverse events in children with fever and neutropenia secondary to cancer therapy identified four predictive characteristics of adverse events. Adverse events were defined by either a serious medical complication as a result of infection, including death, complications necessitating critical care, an identified microbiological infection, and radiological confirmation of pneumonia. These four characteristics were an elevated hemoglobin level (>9 g/DL), WBC < 0.3 G/L, platelet count <50 G/L, and preceding chemotherapy with greater intensity than acute lymphoblastic leukemia maintenance therapy. Although a defined weighted score was able to predict an adverse event (as defined above) with an overall sensitivity of > 92%, a specificity of 45% and negative predictive value of 93%, the specific adverse event of intensive care admission or mortality was not predictive [104]. As a result, critical care physicians need to have a high index of suspicion for immunocompromised patients presenting with fever, neutropenia with any laboratory derangements, abnormal radiological findings suggestive of infections, and abnormal vital signs or toxic appearance as a definitive predictive model has not been well elucidated.
Leukemia Induction Therapy
Remission induction therapy for acute leukemia induces a profound immunosuppressive state with severe neutropenia and suppression of the innate immune system. Patients are extremely vulnerable to invasive bacterial and fungal infections. Treatment-related deaths have decreased dramatically with improved supportive care over the past several decades. In the United Kingdom, treatment-related deaths (TRDs) in ALL patients dropped from 9% in 1980 to 2% in 1997 mostly attributable to decrease in measles and Pneumocystis jirovecii infections [105]. Similar results have been demonstrated worldwide with the Berlin-Frankfurt-Munster (BFM) group reporting approximately 1% TRDs in the ALL-BRM-95 trial. The St. Jude Total Therapy XIIIB trial showed grade 4 infections developing in 5% of patients during remission induction therapy, and disseminated fungal (grade 3 or 4) occurred in 4% of patients [106].
All patients receive sulfamethoxazole-trimethoprim (SMX-TMP) prophylaxis which offers coverage for Pneumocystis jiroveci as well as bacterial infections including gram-positive organisms such as Streptococcus pyogenes, S. pneumoniae, Staphylococcus aureus, and S. epidermidis as well as gram-negative organisms like Escherichia coli, Klebsiella, and Salmonella. SMX-TMP inhibits the formation of folinic acid in bacteria and blocks formation of purine, DNA, and RNA [107]. Additional bacterial and fungal prophylaxis during times of prolonged neutropenia with induction therapy may differ by institution, and it is prudent to know current institutional prophylaxis guidelines and understand what infections patient are more susceptible to, as well as appropriate expansion of antibiotic and antifungal coverage for patients undergoing induction who present with sepsis.
Post Hematopoietic Cell Transplant
HCT patients are at particularly high risk for sepsis and sepsis-related mortality [108, 109]. A clear understanding of the timing of immune reconstitution after allogeneic HSCT helps guide the clinician in anticipating which infectious pathogens patients are most at risk of developing during various time points after transplant. Initially, after conditioning therapy, patients develop an aplastic phase which involves severe neutropenia. This may also be termed a pre-engraftment phase. The innate immune system, consisting of neutrophils and NK cells, returns first over a time period of weeks, followed by adaptive immunity, T cells and B cells, over months to years. Specifically, neutrophils are the first cells to appear, followed by NK cells, then T cells and CD19+ B cells. The precise timing differs according to cell source, dose, and conditioning regimen. It is worth noting that even with return of cell counts, full function may be further delayed [110, 111].
With a clear understanding of immune reconstitution, the clinician may predict which infections patients are most vulnerable to in each phase. During the pre-engraftment phase, patients are most at risk of bacterial and fungal infections. Often prophylactic antibiotics and antifungal agents are given during this time with escalation to broader treatment dosing when acute infection is suspected. Following engraftment of neutrophils, the first 100 days, known as engraftment phase, is a time of cellular immunodeficiency as both NK cells from the innate immune system and T cells of the adaptive immune system are attenuated. Viral infections and/or reactivations predominate, including Epstein-Barr virus (EBV) and cytomegalovirus (CMV). Post-engraftment, after day 100, patients may still be vulnerable to viral infections. As B cells are the last to reconstitute, patients often have low levels of circulating immunoglobulins and as such are susceptible to infections with encapsulated bacteria including Streptococcus pneumoniae and Haemophilus influenza [110].
Sickle Cell Disease
Fever and Sepsis
Patients with SCD are at increased risk for bacterial infections, primarily due to impaired or absent splenic function. This often begins as early as 2 to 3 months of age as fetal hemoglobin levels begin to fall. As a result, children with SCD are at extremely high risk for disseminated bacterial infections causing septicemia or meningitis, predominantly with Streptococcus pneumoniae. Young children with HbSS are most at risk for pneumococcal infection and require prophylactic antibiotic coverage in the first 5 years of life with twice daily beta lactams as well as pneumococcal vaccination. Prophylactic antibiotics are discontinued at age 5 unless the child has undergone a splenectomy or has a history of pneumococcal infection [112]. Fever in a child with SCD warrants prompt assessment, blood cultures, and empiric antibiotics. Newborn screening for sickle cell disease is now universal in the United States, and all children with HbSS should be identified early with early initiation of pneumococcal prophylaxis; however, this does not entirely eliminate the risk, and invasive pneumococcal infection must be considered in pediatric patients with HbSS presenting with fever. Specific antibiotic regimens for patients with SCD presenting with fever may vary by institutional and hematology division guidelines; however, these often include ampicillin or third-generation cephalosporin with expansion to vancomycin for children who are toxic appearing, fever >39.5 degrees Celsius, leukopenia with WBC <5, or leukocytosis (WBC > 30).
Acute Chest Syndrome
Acute chest syndrome ( ACS) is another common complication of SCD. It is defined by acute onset of respiratory symptoms (cough, hypoxia, rales) with a new infiltrate on chest X-ray, most commonly right upper or middle lobe in children. The etiology may vary but ACS often arises secondary to infection, usually associated with atypical bacteria, or to pulmonary fat embolism [113, 114]. The Management of Sickle Cell Disease Summary of the 2014 Evidence-Based Report by Expert Panel Members published in JAMA identifies strong recommendations for the following: treatment with an intravenous cephalosporin, an oral macrolide antibiotic, supplemental oxygen to maintain oxygen saturation of >95%, and close monitoring for bronchospasm, acute anemia, and hypoxemia. Children developing critical illness with respiratory insufficiency or failure, worsening hypoxia with oxygen saturations <90% despite supplemental oxygen, progressive infiltrates, or acute anemia should receive urgent exchange transfusion in collaboration with the intensivist, hematologist, and apheresis teams. There is weak evidence for simple transfusion of 10 ml/kg of packed red blood cells to improve oxygen-carrying capacity for symptomatic children with ACS when hemoglobin concentration is >1 g/dL below baseline, with the exception of a baseline hemoglobin of ≥9 g/dL in which case transfusion may not be required. Lastly, the use of incentive spirometry while awake is strongly encouraged [115].
Conditions that May Mimic Sepsis
Several noninfectious conditions may mimic sepsis and warrant astute understanding and prompt recognition in an effort to offer appropriate targeted therapy. These conditions, often resulting in uncontrolled inflammation, have likely been present in pediatric critical care for years; however, they were previously diagnosed as “culture negative sepsis.” Advancements in immunology, understanding of the inflammatory cascade, and genetics have improved the diagnosis of these diseases including hemophagocytic lymphohistiocytosis (HLH) and macrophage activation syndrome (MAS) and, subsequently, improved survival with the development of targeted therapies.
HLH and MAS fall on a spectrum of severe inflammatory disorders characterized by uncontrolled immune activation resulting from impaired cytotoxic T lymphocyte (CTLs) or natural killer (NK) cells. The dysfunctional CTLs and NK cells continually secrete cytokines with loss of normal negative feedback, resulting in further activation of macrophages, NK cells, and CTLs; an uncontrolled cytokine storm ensues [116, 117]. Diagnosis of HLH is clinical and often blurred with similar symptoms of severe sepsis. Signs of uncontrolled inflammation may include fever, distributive shock, and coagulopathy. Additionally, laboratory abnormalities may be present, including elevated liver enzymes, cytopenias, and renal failure. Patients may progress to acute respiratory distress syndrome, neurological impairment with encephalopathy, and seizures. HLH biology and treatment are discussed in detail in Chap. 10.1007/978-3-030-01322-6_9.
Additionally, other therapeutics used in the treatment of hematology/oncology and HSCT patients may cause immunosuppression and may elicit sepsis like clinical pictures. Notably, anti-thymoglobulin (ATG) is used as a therapy for severe aplastic anemia as well as for graft-versus-host disease prophylaxis and treatment in HSCT patients. Studies demonstrate elevations in circulating cytokines after the initiation of anti-T cell therapy with ATG, specifically IL-6, IL-8, IL-10 and granulocyte colony-stimulating factor (GCSF), IL4, IL13, TNFa, IFNg, interferon gamma-inducible protein-10 (IP-10), chemokine (C-C motif) ligand (CCL-2), and CCL-4 [118, 119]. Clinically, patients exposed to ATG (either rabbit or horse source) may develop acute hypersensitivity infusion reaction with fever, hypotension, as well as a delayed (approximately 10 days) serum sickness with fever, myalgias, arthralgias, and rash. Serum sickness results from host antibody responses to foreign proteins followed by formation and then deposition of immune complexes in tissues (skin, joints, and other organs) [118]. Careful attention to recent therapeutics may allow for quick and accurate diagnosis of underlying etiology of hematology/oncology patients presenting with signs and symptoms of sepsis.
Conclusion
In summary, immunocompromised children, including those with primary or acquired immunodeficiencies, malignancies, or hemoglobinopathies and those who have undergone solid organ or hematopoietic cell transplantation, are at particularly high risk for sepsis and sepsis-related mortality. Significant attention should be given to rapid initial hemodynamic resuscitation with empiric broad-spectrum antimicrobial coverage. Subsequent tailoring of care based on unique patient susceptibilities to infections and organ toxicity remains crucial to maximizing outcomes.
Contributor Information
Christine N. Duncan, Email: christine_duncan@dfci.harvard.edu
Julie-An M. Talano, Email: jtalano@mcw.edu
Jennifer A. McArthur, Email: Jennifer.McArthur@STJUDE.ORG
Matt Zinter, Email: matt.zinter@ucsf.edu.
References
- 1.Goldstein B, Giroir B, Randolph A, et al. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6:2–8. doi: 10.1097/01.PCC.0000149131.72248.E6. [DOI] [PubMed] [Google Scholar]
- 2.Agulnik A, Mendez Aceituno A, Mora Robles LN, et al. Validation of a pediatric early warning system for hospitalized pediatric oncology patients in a resource-limited setting. Cancer. 2017;123:4903–4913. doi: 10.1002/cncr.30951. [DOI] [PubMed] [Google Scholar]
- 3.Sano H, Kobayashi R, Iguchi A, et al. Risk factors for sepsis-related death in children and adolescents with hematologic and malignant diseases. J Microbiol Immunol Infect = Wei mian yu gan ran za zhi. 2017;50:232–238. doi: 10.1016/j.jmii.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 5.Kalil AC, Johnson DW, Lisco SJ, et al. Early goal-directed therapy for sepsis: a novel solution for discordant survival outcomes in clinical trials. Crit Care Med. 2017;45:607–614. doi: 10.1097/CCM.0000000000002235. [DOI] [PubMed] [Google Scholar]
- 6.Investigators P. Rowan KM, Angus DC, et al. Early, goal-directed therapy for septic shock – a patient-level meta-analysis. N Engl J Med. 2017;376:2223–2234. doi: 10.1056/NEJMoa1701380. [DOI] [PubMed] [Google Scholar]
- 7.Han YY, Carcillo JA, Dragotta MA, et al. Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics. 2003;112:793–799. doi: 10.1542/peds.112.4.793. [DOI] [PubMed] [Google Scholar]
- 8.Inwald DP, Tasker RC, Peters MJ, et al. Emergency management of children with severe sepsis in the United Kingdom: the results of the Paediatric Intensive Care Society sepsis audit. Arch Dis Child. 2009;94:348–353. doi: 10.1136/adc.2008.153064. [DOI] [PubMed] [Google Scholar]
- 9.Oliveira CF, Nogueira de Sa FR, Oliveira DS, et al. Time- and fluid-sensitive resuscitation for hemodynamic support of children in septic shock: barriers to the implementation of the American College of Critical Care Medicine/Pediatric advanced life support guidelines in a pediatric intensive care unit in a developing world. Pediatr Emerg Care. 2008;24:810–815. doi: 10.1097/PEC.0b013e31818e9f3a. [DOI] [PubMed] [Google Scholar]
- 10.Gelbart B, Glassford NJ, Bellomo R. Fluid bolus therapy-based resuscitation for severe sepsis in hospitalized children: a systematic review. Pediatr Crit Care Med. 2015;16:e297–e307. doi: 10.1097/PCC.0000000000000507. [DOI] [PubMed] [Google Scholar]
- 11.Brierley J, Carcillo JA, Choong K, et al. Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med. 2009;37:666–688. doi: 10.1097/CCM.0b013e31819323c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis AL, Carcillo JA, Aneja RK, et al. American College of Critical Care Medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit Care Med. 2017;45:1061–1093. doi: 10.1097/CCM.0000000000002425. [DOI] [PubMed] [Google Scholar]
- 13.Akech S, Ledermann H, Maitland K. Choice of fluids for resuscitation in children with severe infection and shock: systematic review. Br Med J. 2010;341:c4416. doi: 10.1136/bmj.c4416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emrath ET, Fortenberry JD, Travers C, et al. Resuscitation with balanced fluids is associated with improved survival in pediatric severe sepsis. Crit Care Med. 2017;45:1177–1183. doi: 10.1097/CCM.0000000000002365. [DOI] [PubMed] [Google Scholar]
- 15.Weiss SL, Keele L, Balamuth F, et al. Crystalloid fluid choice and clinical outcomes in pediatric sepsis: a matched retrospective cohort study. J Pediatr. 2017;182:304–310. doi: 10.1016/j.jpeds.2016.11.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med. 2017;45:486–552. doi: 10.1097/CCM.0000000000002255. [DOI] [PubMed] [Google Scholar]
- 17.de Caen AR, Berg MD, Chameides L, et al. Part 12: pediatric advanced life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S526–S542. doi: 10.1161/CIR.0000000000000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choi SJ, Ha EJ, Jhang WK, et al. Elevated central venous pressure is associated with increased mortality in pediatric septic shock patients. BMC Pediatr. 2018;18:58. doi: 10.1186/s12887-018-1059-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sankar J, Das RR, Jain A, et al. Prevalence and outcome of diastolic dysfunction in children with fluid refractory septic shock—a prospective observational study. Pediatr Crit Care Med. 2014;15:e370–e378. doi: 10.1097/PCC.0000000000000249. [DOI] [PubMed] [Google Scholar]
- 20.Lanspa MJ, Pittman JE, Hirshberg EL, et al. Association of left ventricular longitudinal strain with central venous oxygen saturation and serum lactate in patients with early severe sepsis and septic shock. Crit Care. 2015;19:304. doi: 10.1186/s13054-015-1014-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gan H, Cannesson M, Chandler JR, et al. Predicting fluid responsiveness in children: a systematic review. Anesth Analg. 2013;117:1380–1392. doi: 10.1213/ANE.0b013e3182a9557e. [DOI] [PubMed] [Google Scholar]
- 22.Michard F, Boussat S, Chemla D, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med. 2000;162:134–138. doi: 10.1164/ajrccm.162.1.9903035. [DOI] [PubMed] [Google Scholar]
- 23.Lacroix J, Hebert PC, Hutchison JS, et al. Transfusion strategies for patients in pediatric intensive care units. N Engl J Med. 2007;356:1609–1619. doi: 10.1056/NEJMoa066240. [DOI] [PubMed] [Google Scholar]
- 24.Karam O, Tucci M, Ducruet T, et al. Red blood cell transfusion thresholds in pediatric patients with sepsis. Pediatr Crit Care Med. 2011;12:512–518. doi: 10.1097/PCC.0b013e3181fe344b. [DOI] [PubMed] [Google Scholar]
- 25.Shieh Huei Hsin, Barreira Eliane Roseli, Goes Patricia Freitas, Souza Daniela Carla, Ventura Andrea Maria Cordeiro, Bousso Albert. Mortality associated with restrictive threshold for red blood cell transfusion in pediatric patients with sepsis. Pediatric Critical Care Medicine. 2012;13(4):494–495. doi: 10.1097/PCC.0b013e31824fbb29. [DOI] [PubMed] [Google Scholar]
- 26.Du Pont-Thibodeau G, Tucci M, Ducruet T, et al. Survey on stated transfusion practices in PICUs*. Pediatr Crit Care Med. 2014;15:409–416. doi: 10.1097/PCC.0000000000000121. [DOI] [PubMed] [Google Scholar]
- 27.Mirouse A, Resche-Rigon M, Lemiale V, et al. Red blood cell transfusion in the resuscitation of septic patients with hematological malignancies. Ann Intensive Care. 2017;7:62. doi: 10.1186/s13613-017-0292-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shah N, Andrews J, Goodnough LT. Transfusions for anemia in adult and pediatric patients with malignancies. Blood Rev. 2015;29:291–299. doi: 10.1016/j.blre.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Azoulay E, Pickkers P, Soares M, et al. Acute hypoxemic respiratory failure in immunocompromised patients: the Efraim multinational prospective cohort study. Intensive Care Med. 2017;43:1808–1819. doi: 10.1007/s00134-017-4947-1. [DOI] [PubMed] [Google Scholar]
- 30.Lemiale V, Resche-Rigon M, Mokart D, et al. High-flow nasal cannula oxygenation in immunocompromised patients with acute hypoxemic respiratory failure: a groupe de recherche respiratoire en reanimation onco-hematologique study. Crit Care Med. 2017;45:e274–e280. doi: 10.1097/CCM.0000000000002085. [DOI] [PubMed] [Google Scholar]
- 31.Neuschwander A, Lemiale V, Darmon M, et al. Noninvasive ventilation during acute respiratory distress syndrome in patients with cancer: trends in use and outcome. J Crit Care. 2017;38:295–299. doi: 10.1016/j.jcrc.2016.11.042. [DOI] [PubMed] [Google Scholar]
- 32.Rowan CM, Smith LS, Loomis A, et al. Pediatric acute respiratory distress syndrome in pediatric allogeneic hematopoietic stem cell transplants: a multicenter study. Pediatr Crit Care Med. 2017;18:304–309. doi: 10.1097/PCC.0000000000001061. [DOI] [PubMed] [Google Scholar]
- 33.Antonucci E, Fiaccadori E, Donadello K, et al. Myocardial depression in sepsis: from pathogenesis to clinical manifestations and treatment. J Crit Care. 2014;29:500–511. doi: 10.1016/j.jcrc.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 34.Fernandes CJ, Jr, Akamine N, Knobel E. Myocardial depression in sepsis. Shock. 2008;30(Suppl 1):14–17. doi: 10.1097/SHK.0b013e3181818617. [DOI] [PubMed] [Google Scholar]
- 35.Ramaswamy KN, Singhi S, Jayashree M, et al. Double-blind randomized clinical trial comparing dopamine and epinephrine in pediatric fluid-refractory hypotensive septic shock. Pediatr Crit Care Med. 2016;17:e502–e512. doi: 10.1097/PCC.0000000000000954. [DOI] [PubMed] [Google Scholar]
- 36.Ventura AM, Shieh HH, Bousso A, et al. Double-blind prospective randomized controlled trial of dopamine versus epinephrine as first-line vasoactive drugs in pediatric septic shock. Crit Care Med. 2015;43:2292–2302. doi: 10.1097/CCM.0000000000001260. [DOI] [PubMed] [Google Scholar]
- 37.Vasu TS, Cavallazzi R, Hirani A, et al. Norepinephrine or dopamine for septic shock: systematic review of randomized clinical trials. J Intensive Care Med. 2012;27:172–178. doi: 10.1177/0885066610396312. [DOI] [PubMed] [Google Scholar]
- 38.Ranjit S, Natraj R, Kandath SK, et al. Early norepinephrine decreases fluid and ventilatory requirements in pediatric vasodilatory septic shock. Indian J Crit Care Med. 2016;20:561–569. doi: 10.4103/0972-5229.192036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Loar RW, Noel CV, Tunuguntla H, et al. State of the art review: chemotherapy-induced cardiotoxicity in children. Congenit Heart Dis. 2018;13:5–15. doi: 10.1111/chd.12564. [DOI] [PubMed] [Google Scholar]
- 40.Barbaro RP, Paden ML, Guner YS, et al. Pediatric extracorporeal life support organization registry international report 2016. ASAIO J. 2017;63:456–463. doi: 10.1097/MAT.0000000000000603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gow KW, Heiss KF, Wulkan ML, et al. Extracorporeal life support for support of children with malignancy and respiratory or cardiac failure: the extracorporeal life support experience. Crit Care Med. 2009;37:1308–1316. doi: 10.1097/CCM.0b013e31819cf01a. [DOI] [PubMed] [Google Scholar]
- 42.Roussos C, Macklem PT. The respiratory muscles. N Engl J Med. 1982;307:786–797. doi: 10.1056/NEJM198209233071304. [DOI] [PubMed] [Google Scholar]
- 43.Stock MC, Davis DW, Manning JW, et al. Lung mechanics and oxygen consumption during spontaneous ventilation and severe heart failure. Chest. 1992;102:279–283. doi: 10.1378/chest.102.1.279. [DOI] [PubMed] [Google Scholar]
- 44.Delbove A, Darreau C, Hamel JF, et al. Impact of endotracheal intubation on septic shock outcome: a post hoc analysis of the SEPSISPAM trial. J Crit Care. 2015;30:1174–1178. doi: 10.1016/j.jcrc.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 45.Jung B, Clavieras N, Nougaret S, et al. Effects of etomidate on complications related to intubation and on mortality in septic shock patients treated with hydrocortisone: a propensity score analysis. Crit Care. 2012;16:R224. doi: 10.1186/cc11871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dmello D, Taylor S, O’Brien J, et al. Outcomes of etomidate in severe sepsis and septic shock. Chest. 2010;138:1327–1332. doi: 10.1378/chest.10-0790. [DOI] [PubMed] [Google Scholar]
- 47.Eisen DP. Manifold beneficial effects of acetyl salicylic acid and nonsteroidal anti-inflammatory drugs on sepsis. Intensive Care Med. 2012;38:1249–1257. doi: 10.1007/s00134-012-2570-8. [DOI] [PubMed] [Google Scholar]
- 48.Aronoff DM. Cyclooxygenase inhibition in sepsis: is there life after death? Mediat Inflamm. 2012;2012:696897. doi: 10.1155/2012/696897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Janz DR, Bastarache JA, Rice TW, et al. Randomized, placebo-controlled trial of acetaminophen for the reduction of oxidative injury in severe sepsis: the Acetaminophen for the Reduction of Oxidative Injury in Severe Sepsis trial. Crit Care Med. 2015;43:534–541. doi: 10.1097/CCM.0000000000000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee BH, Inui D, Suh GY, et al. Association of body temperature and antipyretic treatments with mortality of critically ill patients with and without sepsis: multi-centered prospective observational study. Crit Care. 2012;16:R33. doi: 10.1186/cc11211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mallat J, Michel D, Salaun P, et al. Defining metabolic acidosis in patients with septic shock using Stewart approach. Am J Emerg Med. 2012;30:391–398. doi: 10.1016/j.ajem.2010.11.039. [DOI] [PubMed] [Google Scholar]
- 52.Deep A, Goonasekera CD, Wang Y, et al. Evolution of haemodynamics and outcome of fluid-refractory septic shock in children. Intensive Care Med. 2013;39:1602–1609. doi: 10.1007/s00134-013-3003-z. [DOI] [PubMed] [Google Scholar]
- 53.Brierley J, Peters MJ. Distinct hemodynamic patterns of septic shock at presentation to pediatric intensive care. Pediatrics. 2008;122:752–759. doi: 10.1542/peds.2007-1979. [DOI] [PubMed] [Google Scholar]
- 54.Raimer Patricia L., Han Yong Y., Weber Monica S., Annich Gail M., Custer Joseph R. A Normal Capillary Refill Time of ≤ 2 Seconds is Associated with Superior Vena Cava Oxygen Saturations of ≥ 70% The Journal of Pediatrics. 2011;158(6):968–972. doi: 10.1016/j.jpeds.2010.11.062. [DOI] [PubMed] [Google Scholar]
- 55.Sankar J, Sankar MJ, Suresh CP, et al. Early goal-directed therapy in pediatric septic shock: comparison of outcomes “with” and “without” intermittent superior venacaval oxygen saturation monitoring: a prospective cohort study*. Pediatr Crit Care Med. 2014;15:e157–e167. doi: 10.1097/PCC.0000000000000073. [DOI] [PubMed] [Google Scholar]
- 56.Boulain T, Garot D, Vignon P, et al. Prevalence of low central venous oxygen saturation in the first hours of intensive care unit admission and associated mortality in septic shock patients: a prospective multicentre study. Crit Care. 2014;18:609. doi: 10.1186/s13054-014-0609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Proulx F, Lemson J, Choker G, et al. Hemodynamic monitoring by transpulmonary thermodilution and pulse contour analysis in critically ill children. Pediatr Crit Care Med. 2011;12:459–466. doi: 10.1097/PCC.0b013e3182070959. [DOI] [PubMed] [Google Scholar]
- 58.Handrup MM, Moller JK, Rutkjaer C, et al. Importance of blood cultures from peripheral veins in pediatric patients with cancer and a central venous line. Pediatr Blood Cancer. 2015;62:99–102. doi: 10.1002/pbc.25171. [DOI] [PubMed] [Google Scholar]
- 59.Scheinemann K, Ethier MC, Dupuis LL, et al. Utility of peripheral blood cultures in bacteremic pediatric cancer patients with a central line. Support Care Cancer. 2010;18:913–919. doi: 10.1007/s00520-009-0725-0. [DOI] [PubMed] [Google Scholar]
- 60.Blot F, Schmidt E, Nitenberg G, et al. Earlier positivity of central-venous- versus peripheral-blood cultures is highly predictive of catheter-related sepsis. J Clin Microbiol. 1998;36:105–109. doi: 10.1128/jcm.36.1.105-109.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Weiss SL, Fitzgerald JC, Balamuth F, et al. Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Crit Care Med. 2014;42:2409–2417. doi: 10.1097/CCM.0000000000000509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Han M, Fitzgerald JC, Balamuth F, et al. Association of delayed antimicrobial therapy with one-year mortality in pediatric sepsis. Shock. 2017;48:29–35. doi: 10.1097/SHK.0000000000000833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Celebi S, Sezgin ME, Cakir D, et al. Catheter-associated bloodstream infections in pediatric hematology-oncology patients. Pediatr Hematol Oncol. 2013;30:187–194. doi: 10.3109/08880018.2013.772683. [DOI] [PubMed] [Google Scholar]
- 64.Slade Michael, Goldsmith Scott, Romee Rizwan, DiPersio John F., Dubberke Erik R., Westervelt Peter, Uy Geoffrey L., Lawrence Steven J. Epidemiology of infections following haploidentical peripheral blood hematopoietic cell transplantation. Transplant Infectious Disease. 2016;19(1):e12629. doi: 10.1111/tid.12629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chang AK, Foca MD, Jin Z, et al. Bacterial bloodstream infections in pediatric allogeneic hematopoietic stem cell recipients before and after implementation of a central line-associated bloodstream infection protocol: a single-center experience. Am J Infect Control. 2016;44:1650–1655. doi: 10.1016/j.ajic.2016.04.229. [DOI] [PubMed] [Google Scholar]
- 66.Sim Starling A., Leung Vivian K.Y., Ritchie David, Slavin Monica A., Sullivan Sheena G., Teh Benjamin W. Viral Respiratory Tract Infections in Allogeneic Hematopoietic Stem Cell Transplantation Recipients in the Era of Molecular Testing. Biology of Blood and Marrow Transplantation. 2018;24(7):1490–1496. doi: 10.1016/j.bbmt.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hiwarkar P, Gaspar HB, Gilmour K, et al. Impact of viral reactivations in the era of pre-emptive antiviral drug therapy following allogeneic haematopoietic SCT in paediatric recipients. Bone Marrow Transplant. 2013;48:803–808. doi: 10.1038/bmt.2012.221. [DOI] [PubMed] [Google Scholar]
- 68.Steinbach WJ, Roilides E, Berman D, et al. Results from a prospective, international, epidemiologic study of invasive candidiasis in children and neonates. Pediatr Infect Dis J. 2012;31:1252–1257. doi: 10.1097/INF.0b013e3182737427. [DOI] [PubMed] [Google Scholar]
- 69.Wattier RL, Dvorak CC, Hoffman JA, et al. A prospective, international cohort study of invasive mold infections in children. J Pediatr Infect Dis Soc. 2015;4:313–322. doi: 10.1093/jpids/piu074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Alexander Maurice D., Rao Kamakshi V., Khan Tippu S., Deal Allison M., Alexander Maurice D., Rao Kamakshi V., Khan Tippu S., Deal Allison M. ReCAP: Pharmacists’ Impact in Hematopoietic Stem-Cell Transplantation: Economic and Humanistic Outcomes. Journal of Oncology Practice. 2016;12(2):147–148. doi: 10.1200/JOP.2015.008797. [DOI] [PubMed] [Google Scholar]
- 71.Lucena M, Bondarenka C, Luehrs-Hayes G, et al. Evaluation of a medication intensity screening tool used in malignant hematology and bone marrow transplant services to identify patients at risk for medication-related problems. J Oncol Pharm Pract. 2018;24:243–252. doi: 10.1177/1078155217690923. [DOI] [PubMed] [Google Scholar]
- 72.El-Nawawy A, Khater D, Omar H, et al. Evaluation of early corticosteroid therapy in management of pediatric septic shock in pediatric intensive care patients: a randomized clinical study. Pediatr Infect Dis J. 2017;36:155–159. doi: 10.1097/INF.0000000000001380. [DOI] [PubMed] [Google Scholar]
- 73.Markovitz BP, Goodman DM, Watson RS, et al. A retrospective cohort study of prognostic factors associated with outcome in pediatric severe sepsis: what is the role of steroids? Pediatr Crit Care Med. 2005;6:270–274. doi: 10.1097/01.PCC.0000160596.31238.72. [DOI] [PubMed] [Google Scholar]
- 74.Zimmerman JJ, Williams MD. Adjunctive corticosteroid therapy in pediatric severe sepsis: observations from the RESOLVE study. Pediatr Crit Care Med. 2011;12:2–8. doi: 10.1097/PCC.0b013e3181d903f6. [DOI] [PubMed] [Google Scholar]
- 75.Atkinson SJ, Cvijanovich NZ, Thomas NJ, et al. Corticosteroids and pediatric septic shock outcomes: a risk stratified analysis. PLoS One. 2014;9:e112702. doi: 10.1371/journal.pone.0112702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Weiss SL, Fitzgerald JC, Pappachan J, et al. Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med. 2015;191:1147–1157. doi: 10.1164/rccm.201412-2323OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Menon K, McNally JD, Choong K, et al. A cohort study of pediatric shock: frequency of corticosteriod use and association with clinical outcomes. Shock. 2015;44:402–409. doi: 10.1097/SHK.0000000000000355. [DOI] [PubMed] [Google Scholar]
- 78.Wong HR, Cvijanovich NZ, Allen GL, et al. Corticosteroids are associated with repression of adaptive immunity gene programs in pediatric septic shock. Am J Respir Crit Care Med. 2014;189:940–946. doi: 10.1164/rccm.201401-0171OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Keh D, Trips E, Marx G, et al. Effect of hydrocortisone on development of shock among patients with severe sepsis: the HYPRESS randomized clinical trial. JAMA. 2016;316:1775–1785. doi: 10.1001/jama.2016.14799. [DOI] [PubMed] [Google Scholar]
- 80.Zimmerman JJ. Adjunctive steroid therapy for treatment of pediatric septic shock. Pediatr Clin N Am. 2017;64:1133–1146. doi: 10.1016/j.pcl.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 81.Phillips R, Hancock B, Graham J, et al. Prevention and management of neutropenic sepsis in patients with cancer: summary of NICE guidance. Br Med J. 2012;345:e5368. doi: 10.1136/bmj.e5368. [DOI] [PubMed] [Google Scholar]
- 82.Price TH, Boeckh M, Harrison RW, et al. Efficacy of transfusion with granulocytes from G-CSF/dexamethasone-treated donors in neutropenic patients with infection. Blood. 2015;126:2153–2161. doi: 10.1182/blood-2015-05-645986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yoshihara S, Kato R, Inoue T, et al. Successful treatment of life-threatening human herpesvirus-6 encephalitis with donor lymphocyte infusion in a patient who had undergone human leukocyte antigen-haploidentical nonmyeloablative stem cell transplantation. Transplantation. 2004;77:835–838. doi: 10.1097/01.TP.0000119603.59880.47. [DOI] [PubMed] [Google Scholar]
- 84.Bao L, Cowan MJ, Dunham K, et al. Adoptive immunotherapy with CMV-specific cytotoxic T lymphocytes for stem cell transplant patients with refractory CMV infections. J Immunother. 2012;35:293–298. doi: 10.1097/CJI.0b013e31824300a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Roddie C, Peggs KS. Immunotherapy for transplantation-associated viral infections. J Clin Invest. 2017;127:2513–2522. doi: 10.1172/JCI90599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Group IC. Brocklehurst P, Farrell B, et al. Treatment of neonatal sepsis with intravenous immune globulin. N Engl J Med. 2011;365:1201–1211. doi: 10.1056/NEJMoa1100441. [DOI] [PubMed] [Google Scholar]
- 87.Kumagai T, Takeyama N, Yabuki T, et al. Apheresis of activated leukocytes with an immobilized polymyxin B filter in patients with septic shock. Shock. 2010;34:461–466. doi: 10.1097/SHK.0b013e3181e14ca0. [DOI] [PubMed] [Google Scholar]
- 88.Bengsch S, Boos KS, Nagel D, et al. Extracorporeal plasma treatment for the removal of endotoxin in patients with sepsis: clinical results of a pilot study. Shock. 2005;23:494–500. [PubMed] [Google Scholar]
- 89.Goldstein B, Nadel S, Peters M, et al. ENHANCE: results of a global open-label trial of drotrecogin alfa (activated) in children with severe sepsis. Pediatr Crit Care Med. 2006;7:200–211. doi: 10.1097/01.PCC.0000217470.68764.36. [DOI] [PubMed] [Google Scholar]
- 90.Dalton HJ, Carcillo JA, Woodward DB, et al. Biomarker response to drotrecogin alfa (activated) in children with severe sepsis: results from the RESOLVE clinical trial*. Pediatr Crit Care Med. 2012;13:639–645. doi: 10.1097/PCC.0b013e318250ad48. [DOI] [PubMed] [Google Scholar]
- 91.Ranieri VM, Thompson BT, Barie PS, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366:2055–2064. doi: 10.1056/NEJMoa1202290. [DOI] [PubMed] [Google Scholar]
- 92.Rowan CM, Gertz SJ, McArthur J, et al. Invasive mechanical ventilation and mortality in pediatric hematopoietic stem cell transplantation: a multicenter study. Pediatr Crit Care Med. 2016;17:294–302. doi: 10.1097/PCC.0000000000000673. [DOI] [PubMed] [Google Scholar]
- 93.Santiago MJ, Lopez-Herce J, Urbano J, et al. Clinical course and mortality risk factors in critically ill children requiring continuous renal replacement therapy. Intensive Care Med. 2010;36:843–849. doi: 10.1007/s00134-010-1858-9. [DOI] [PubMed] [Google Scholar]
- 94.Hall MW, Knatz NL, Vetterly C, et al. Immunoparalysis and nosocomial infection in children with multiple organ dysfunction syndrome. Intensive Care Med. 2011;37:525–532. doi: 10.1007/s00134-010-2088-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mehrholz J, Thomas S, Burridge JH, et al. Fitness and mobility training in patients with Intensive Care Unit-acquired muscle weakness (FITonICU): study protocol for a randomised controlled trial. Trials. 2016;17:559. doi: 10.1186/s13063-016-1687-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zinter MS, Holubkov R, Steurer MA, et al. Pediatric hematopoietic cell transplant patients who survive critical illness frequently have significant but recoverable decline in functional status. Biol Blood Marrow Transplant. 2018;24:330–336. doi: 10.1016/j.bbmt.2017.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ammann RA, Hirt A, Luthy AR, et al. Identification of children presenting with fever in chemotherapy-induced neutropenia at low risk for severe bacterial infection. Med Pediatr Oncol. 2003;41:436–443. doi: 10.1002/mpo.10320. [DOI] [PubMed] [Google Scholar]
- 98.Hakim H, Flynn PM, Srivastava DK, et al. Risk prediction in pediatric cancer patients with fever and neutropenia. Pediatr Infect Dis J. 2010;29:53–59. doi: 10.1097/INF.0b013e3181c3f6f0. [DOI] [PubMed] [Google Scholar]
- 99.Santolaya ME, Alvarez AM, Becker A, et al. Prospective, multicenter evaluation of risk factors associated with invasive bacterial infection in children with cancer, neutropenia, and fever. J Clin Oncol. 2001;19:3415–3421. doi: 10.1200/JCO.2001.19.14.3415. [DOI] [PubMed] [Google Scholar]
- 100.Tezcan G, Kupesiz A, Ozturk F, et al. Episodes of fever and neutropenia in children with cancer in a tertiary care medical center in Turkey. Pediatr Hematol Oncol. 2006;23:217–229. doi: 10.1080/08880010500506719. [DOI] [PubMed] [Google Scholar]
- 101.West DC, Marcin JP, Mawis R, et al. Children with cancer, fever, and treatment-induced neutropenia: risk factors associated with illness requiring the administration of critical care therapies. Pediatr Emerg Care. 2004;20:79–84. doi: 10.1097/01.pec.0000113875.10140.40. [DOI] [PubMed] [Google Scholar]
- 102.Ramzi J, Mohamed Z, Yosr B, et al. Predictive factors of septic shock and mortality in neutropenic patients. Hematology. 2007;12:543–548. doi: 10.1080/10245330701384237. [DOI] [PubMed] [Google Scholar]
- 103.Neutropenic sepsis: prevention and management of neutropenic sepsis in cancer patients. London; 2012. https://www.ncbi.nlm.nih.gov/pubmed/26065059 [PubMed]
- 104.Ammann RA, Bodmer N, Hirt A, et al. Predicting adverse events in children with fever and chemotherapy-induced neutropenia: the prospective multicenter SPOG 2003 FN study. J Clin Oncol. 2010;28:2008–2014. doi: 10.1200/JCO.2009.25.8988. [DOI] [PubMed] [Google Scholar]
- 105.Hargrave DR, Hann II, Richards SM, et al. Progressive reduction in treatment-related deaths in Medical Research Council childhood lymphoblastic leukaemia trials from 1980 to 1997 (UKALL VIII, X and XI) Br J Haematol. 2001;112:293–299. doi: 10.1046/j.1365-2141.2001.02543.x. [DOI] [PubMed] [Google Scholar]
- 106.Pui CH, Sandlund JT, Pei D, et al. Improved outcome for children with acute lymphoblastic leukemia: results of Total Therapy Study XIIIB at St Jude Children’s Research Hospital. Blood. 2004;104:2690–2696. doi: 10.1182/blood-2004-04-1616. [DOI] [PubMed] [Google Scholar]
- 107.Rungoe C, Malchau EL, Larsen LN, et al. Infections during induction therapy for children with acute lymphoblastic leukemia. The role of sulfamethoxazole-trimethoprim (SMX-TMP) prophylaxis. Pediatr Blood Cancer. 2010;55:304–308. doi: 10.1002/pbc.22423. [DOI] [PubMed] [Google Scholar]
- 108.Lindell RB, Gertz SJ, Rowan CM, et al. High levels of morbidity and mortality among pediatric hematopoietic cell transplant recipients with severe sepsis: insights from the sepsis PRevalence, OUtcomes, and therapies international point prevalence study. Pediatr Crit Care Med. 2017;18:1114–1125. doi: 10.1097/PCC.0000000000001338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tamburro R. Pediatric cancer patients in clinical trials of sepsis: factors that predispose to sepsis and stratify outcome. Pediatr Crit Care Med. 2005;6:S87–S91. doi: 10.1097/01.PCC.0000161288.00396.49. [DOI] [PubMed] [Google Scholar]
- 110.Ogonek J, Kralj Juric M, Ghimire S, et al. Immune reconstitution after allogeneic hematopoietic stem cell transplantation. Front Immunol. 2016;7:507. doi: 10.3389/fimmu.2016.00507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bosch M, Khan FM, Storek J. Immune reconstitution after hematopoietic cell transplantation. Curr Opin Hematol. 2012;19:324–335. doi: 10.1097/MOH.0b013e328353bc7d. [DOI] [PubMed] [Google Scholar]
- 112.Gaston MH, Verter JI, Woods G, et al. Prophylaxis with oral penicillin in children with sickle cell anemia. A randomized trial. N Engl J Med. 1986;314:1593–1599. doi: 10.1056/NEJM198606193142501. [DOI] [PubMed] [Google Scholar]
- 113.Miller ST. How I treat acute chest syndrome in children with sickle cell disease. Blood. 2011;117:5297–5305. doi: 10.1182/blood-2010-11-261834. [DOI] [PubMed] [Google Scholar]
- 114.Vichinsky EP, Neumayr LD, Earles AN, et al. Causes and outcomes of the acute chest syndrome in sickle cell disease. National Acute Chest Syndrome Study Group. N Engl J Med. 2000;342:1855–1865. doi: 10.1056/NEJM200006223422502. [DOI] [PubMed] [Google Scholar]
- 115.Yawn BP, Buchanan GR, Afenyi-Annan AN, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA. 2014;312:1033–1048. doi: 10.1001/jama.2014.10517. [DOI] [PubMed] [Google Scholar]
- 116.Morimoto A, Nakazawa Y, Ishii E. Hemophagocytic lymphohistiocytosis: pathogenesis, diagnosis, and management. Pediatr Int. 2016;58:817–825. doi: 10.1111/ped.13064. [DOI] [PubMed] [Google Scholar]
- 117.Weitzman S. Approach to hemophagocytic syndromes. Hematol Am Soc Hematol Educ Program. 2011;2011:178–183. doi: 10.1182/asheducation-2011.1.178. [DOI] [PubMed] [Google Scholar]
- 118.Pihusch R, Holler E, Muhlbayer D, et al. The impact of antithymocyte globulin on short-term toxicity after allogeneic stem cell transplantation. Bone Marrow Transplant. 2002;30:347–354. doi: 10.1038/sj.bmt.1703640. [DOI] [PubMed] [Google Scholar]
- 119.Feng X, Scheinberg P, Biancotto A, et al. In vivo effects of horse and rabbit antithymocyte globulin in patients with severe aplastic anemia. Haematologica. 2014;99:1433–1440. doi: 10.3324/haematol.2014.106542. [DOI] [PMC free article] [PubMed] [Google Scholar]