Abstract
Severe acute respiratory syndrome (SARS) is an emerging infectious disease. After the appearance of an index patient in Hong Kong in February 2003, SARS outbreaks occurred rapidly in hospitals and spread to the community. The aim of this retrospective study is to evaluate the effectiveness of a triage policy and risk-stratified infection control measures in preventing nosocomial SARS infection among paediatric healthcare workers (HCWs) at the Prince of Wales Hospital, a general hospital to which children with SARS are referred in Hong Kong. The acute paediatric wards were stratified into three areas: (1) ultra high-risk area, (2) high-risk area and (3) moderate-risk area according to different risk levels of nosocomial SARS transmission. The implementation of different levels of infection control precautions was guided by this risk stratification strategy. Between 13 March and 23 June, 38 patients with probable and suspected SARS, 90 patients with non-SARS pneumonia, and 510 patients without pneumonia were admitted into our unit. All probable SARS cases were isolated in negative-pressure rooms. Twenty-six HCWs worked in the ultra high-risk area caring for SARS patients and 88 HCWs managed non-SARS patients in other ward areas. None of the HCWs developed clinical features suggestive of SARS. In addition, there was no nosocomial spread of SARS-associated coronavirus to other patients or visitors during this period. In conclusion, stringent infection control precautions, appropriate triage and prompt isolation of potential SARS patients may have contributed to a lack of nosocomial spread and HCW acquisition of SARS in our unit.
Keywords: Children, Infection control, SARS, Triage
1. Introduction
Severe acute respiratory syndrome (SARS) is a serious respiratory infection that has been recently reported in Asia, North America, and Europe. Hong Kong is one of the most severely affected cities. At the time of writing, 1755 people have been reported to have SARS and 298 of them died from the disease within a three-month period. In a review of the first 1425 cases, the estimated case fatality rate was 13% for patients younger than 60 and 43% for patients aged 60 or older.1 Droplet and contact spread through close personal contact is believed to be the main route of transmission.2 Healthcare workers (HCWs) are particularly at risk of being infected. In SARS hospital outbreaks encountered so far, a significant number of HCWs were affected. All had looked after patients with SARS or had direct contact with their body fluids such as respiratory secretions, urine and stool. Stringent infection control measures and a sophisticated triage policy were required to minimize the nosocomial spread of infection between patients and HCWs. The general guidelines issued by the Hospital Authority of Hong Kong on the management of patients who require hospitalization (‘SARS precaution in hospitals—infection control and risk management approach’; available at: http://www.ha.org.hk/hesd/nsapi) may not be applicable for the paediatric population.3 The Department of Paediatrics at the Prince of Wales Hospital (PWH) is the tertiary referral centre for probable or suspected SARS patients in the New Territories East region of Hong Kong. This article summarizes the details of the infection control measures and triage policy in preventing cross-infection of SARS among HCWs of the paediatrics department during the recent major outbreak of SARS in Hong Kong. The information may be useful for other paediatric units in formulating their own infection control plans to prevent the spread of SARS-associated coronavirus in the hospital setting.
2. Subjects and methods
2.1. Floor plan of paediatric wards
The PWH is a regional referral centre serving a population of 1.1 million. It is not an infectious disease hospital and isolation facilities are limited. In total, 86 paediatric beds are distributed among three acute admission wards. Since the SARS outbreak, all emergency paediatric admissions were classified according to different levels of risk stratification (see below).
2.2. Risk stratification for paediatric wards
SARS was diagnosed according to the World Health Organization (WHO) surveillance case definitions (Table I).4 Our hospital has defined three levels of risk stratification for acute admission wards: (1) ultra high-risk (UHR), (2) high-risk (HR) and (3) moderate-risk (MR) areas. The UHR areas include the SARS isolation ward (UHR-S) for admitting probable or suspected SARS patients, and the infection triage ward (UHR-I) for admitting all other febrile patients. The floor plans of these UHR wards are illustrated in Figure 1 . The acute paediatric admission ward for non-febrile patients was classified as a HR area. The paediatric outpatient clinic was designated as an MR area.
Table I.
World Health Organization surveillance case definitions for SARS
| Suspect case |
| 1.A person presenting after 1 November 2002 with history of: high fever (>38 °C) AND cough or breathing difficulty AND one or more of the following exposures during the 10 days prior to onset of symptoms: |
| • close contacta with a person who is a suspect or probable case of SARS |
| • history of travel to an area with recent local transmission of SARS |
| • residing in an area with recent local transmission of SARS |
| 2.A person with an unexplained acute respiratory illness resulting in death after 1 November 2002, but on whom no autopsy has been performed AND one or more of the following exposures during to 10 days prior to onset of symptoms: |
| • close contacta with a person who is a suspect or probable case of SARS |
| • history of travel to an area with recent local transmission of SARS |
| • residing in an area with recent local transmission of SARS |
| Probable case |
| 1.A suspect case with radiographic evidence of infiltrates consistent with pneumonia or respiratory distress syndrome on chest X-ray |
| 2.A suspect case of SARS that is positive for SARS-associated coronavirus by one or more assays (polymerase chain reaction; seroconversion; virus isolation) |
| 3.A suspect case with autopsy findings consistent with the pathology of respiratory distress syndrome without an identifiable cause |
Close contact: having cared for, lived with, or had direct contact with respiratory secretions or body fluids of a suspect or probable case of SARS.
Figure 1.
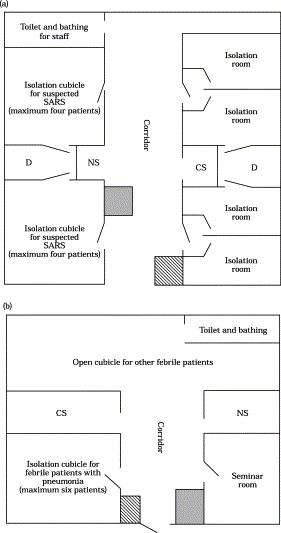
Floor plans of our paediatric wards for admitting (a) patients with probable or suspected SARS (UHR-S) and (b) infection triage patients with fever (UHR-I). The four isolation rooms in (a), operated under negative-pressure ventilation, were designated for patients with probable SARS. Dark areas in (a) and (b) were designated for putting on personal protective equipment whereas shaded areas indicate the place for removing this equipment. Abbreviations: CS, cleaning and storage; D, sewage disposal and urinal and bedpan disinfector; NS, nursing station.
2.3. Departmental triage policy
The attending paediatricians would assess all sick children and adolescents in the accident and emergency department to decide whether they require hospitalization. The triage policy for paediatric patients is summarized in Figure 2 . All patients with pneumonic changes on chest radiographs were admitted either to UHR-S area (with SARS contact) or UHR-I area (without SARS contact). Non-febrile patients were admitted to UHR-S area if they had prior SARS contact. Otherwise, these patients were admitted to the HR area. Before any patient could be admitted to the hospital ward, the relevant history of recent travel and of possible contact with SARS or other forms of acute respiratory illnesses was further checked by the admitting nurse using a specially designed checklist for SARS (Box I).
Figure 2.
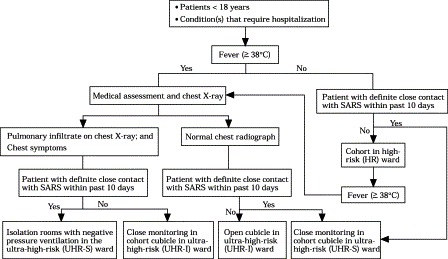
Departmental policy on patient triage for paediatric admission.
Box I.
The checklist for screening contact history of patients before admission into paediatric wards
| Questions | |
|---|---|
| 1. | Source of referral of the child: PWH Accident and Emergency/Specialty outpatient clinic/Other PWH ward/Other hospital/Others (please specify) |
| 2. | Does the child have any recent history of admission to hospitals/wards within recent 3 months? If Yes, which hospital(s)? And which ward(s)? |
| 3. | Is there any possible or definite SARS case in the above ward(s)? |
| 4. | Is there any possible infectious case in the above ward(s)? |
| 5. | Is there any possible contact of the child with the infectious case? If yes, please provide details of contact: Next bed/Same cubicle/Others (specify) |
| 6. | What kind of infection does the infectious case suffer from? |
| 7. | Did the child travel outside Hong Kong in the last 3 months? If yes, where did the child travel to and for how long? |
| 8. | Was any family member of the child getting sick in the last month? If yes, what is the nature of the illness? And, has the sick family member been admitted to hospital? |
| 9. | When was the date of last contact of the child with the sick family member? |
PWH=Prince of Wales Hospital
2.4. General infection control precautions in paediatric wards
The infection control measures were targeted at preventing droplet and close contact transmission.2 The use of N95 respirators was adopted due to the possibility of aerosol transmission. The use of personal protective equipment (PPE) according to different levels of risk stratification is summarized in Table II . Designated places in the paediatric wards were provided for putting on and removing PPE. Two separate stations, one for dressing and the other for removal of PPE, were set up to prevent cross-contamination of protective gear (Figure 1). Routine thorough cleaning and disinfection of the floor, tables, computers and medical equipment in all wards were carried out at least three times per day using sodium hypochlorite solution at 1000 ppm. Each HCW was required to attend an infection control session, organized daily by the hospital infection control team, to remind them of proper infection control precautions to prevent nosocomial transmission of SARS-associated coronavirus.
Table II.
Dress code for staff, patients and visitors in paediatric wards according to different risk categories
| Ultra high-risk area |
High-risk area |
Moderate-risk area |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Measures | Staff | Patients | Visitors | Staff | Patients | Visitors | Staff | Patients | Visitors |
| Handwashing | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Glove | ✓ | X | ✓ | ✓ | X | X | ✓a | X | X |
| Gown | ✓ | X | ✓ | ✓ | X | X | ✓b | X | X |
| Cap | ✓ | X | ✓ | X | X | X | X | X | X |
| Goggle/visor/face shield | ✓ | X | X | ✓b | X | X | ✓b | X | X |
| Face mask | |||||||||
| N95 respirator | ✓ | X | ✓ | ✓ | X | X | ✓b | X | X |
| Surgical mask | X | ✓ | X | X | ✓ | ✓ | ✓ | X | X |
| Paper mask | X | X | X | X | X | X | X | ✓ | ✓ |
| ‘Operating theatre’ type uniform (upper cloth and pant) | ✓ | X | X | ✓ | X | X | X | X | X |
For contact with patients' mucosa, blood, body fluid, secretion and excretion.
Required only for aerosol/splash generating procedures.
2.5. Infection control measures in UHR area
All patients with probable SARS were admitted into isolation rooms operated under negative-pressure ventilation [Figure 1(a)]. In order to minimize the risk of cross-infection, four medical staff (the paediatric SARS team) were assigned to work in the UHR-S area. On entering the UHR area, the following seven steps were required to be followed strictly in sequence: handwashing, putting on N95 respirator, putting on goggles or visor, putting on cap, putting on gown, using an alcoholic handrub and then putting on gloves. HCWs had to follow another seven steps in the given order: removing gloves, handwashing, removing cap, removing goggles or visor, removing gown, removing N95 respirator, and using an alcoholic handrub, before leaving the area. Surgical masks had to be worn outside the UHR area. A ‘police nurse’ was present at the entrance to ensure that the above steps were strictly followed.5 All patients in the UHR area were required to wear surgical masks at all times. Staff members were also requested to leave personal items such as rings, necklaces, watches, as well as stethoscopes, outside the UHR area. Essential items such as hospital pagers were placed in plastic bags and clipped on to the protective clothing to avoid contamination in the ward. All ward equipment, such as computer keyboards and telephones, was protected with plastic wrap that was disinfected every 2 h and the wrap was changed daily.
2.6. Infection control measures for HR procedures
HR procedures include those that can generate large amounts of aerosol (e.g. endotracheal intubation, airway suctioning, nasopharyngeal aspiration and cardiopulmonary resuscitation), as well as others that are likely to generate splashes of blood, body fluids, secretions or excretions [e.g. blood taking, emptying bedpans; see ‘World Health Organization. Hospital infection control guidance for SARS’; available at: http://www.who.int/csr/sars/infectioncontrol/en].6 The treatment room of each ward was designated for carrying out these procedures, and stringent infection control precautions identical to those implemented in the UHR area were adopted. Staff members were requested to discard the N95 respirators, gowns, gloves and caps after these procedures. All used equipment was either discarded (e.g. suction catheters, endotracheal tubes) or disinfected with hypochlorite solution at 1000 ppm for 15 min (e.g. torches, laryngoscopes, stethoscopes). Aerosol-generating treatment procedures including the use of nebulizer or any form of non-invasive positive-pressure ventilation were not allowed to be used in the open ward.6
2.7. Disposal of potentially infected materials and handling of specimens
Patients with probable and suspected SARS were provided with urinals and bedpans. Urine and stools were carefully poured into the hospital sewage disposal system [Figure 1(a)]. Patients or HCWs handling the sewage had to wear visors during the procedure, and the flushers were disinfected immediately with sodium hypochlorite at 1000 ppm. Urinals and bedpans were also either disinfected at 80 °C or by immersing in sodium hypochlorite solution at 1000 ppm for at least 15 min. The designated ‘toilet and bathing’ area for staff in UHR-S ward was disinfected three times daily with sodium hypochlorite at 1000 ppm. The handling of blood and other specimens collected from SARS patients followed the existing policy for universal precautions. Microbiology specimens (e.g. nasopharyngeal aspirates, urine, faeces) collected in primary containers were placed upright and securely sealed in plastic bags within the transport boxes.
2.8. Visitor control in paediatric wards
The Hospital Authority restricted parent visits in all paediatric wards of acute hospitals following the onset of SARS outbreak in order to reduce the risk of cross-infection between family members (‘SARS precaution in hospitals–infection control and risk management approach’; available at http://www.ha.org.hk/hesd/nsapi). However, this policy increases psychological stress on most infants and young children hospitalized for non-SARS illnesses. At PWH, visitors were not allowed to visit paediatric SARS patients in UHR-S area. Instead, doctors-in-charge would phone the parents daily to provide an update on the patients' conditions. However, either the father or the mother was allowed to visit on compassionate grounds for 2 h daily for patients in UHR-I, HR and MR areas. Visitors had to register on arrival at the wards in case future contact tracing was necessary. They were also required to follow the dress codes and put on PPE appropriate for the areas.
2.9. Infection control precautions for HCWs at home
At the end of each shift in the UHR area, HCWs were advised to shower in designated areas in the hospital or immediately when they returned home. They were also advised to follow a guideline for SARS precautions at home such as wearing surgical masks at home, frequent handwashing with liquid soap and avoiding sharing towels, food and utensils with other family members. Staff members were also instructed to disinfect floor, furniture, bathtubs and toilets of their homes at least daily with sodium hypochlorite. Those who developed fever and upper respiratory illnesses were required to report to the departmental infection control officer (PCN) and seek medical consultation to exclude SARS. They were granted sick leave until symptoms subsided.
2.10. Discharge plan for paediatric SARS
All patients with probable or suspected SARS were hospitalized for 21 days. Upon discharge from the hospital, these children and their parents were given an information sheet detailing the precautions that they should take at home. In particular, they were reminded that their body secretions and excretions might still contain the virus at the time of discharge.7 These children were therefore required to limit their social interactions in the public areas (i.e. not to return to school or nursery or go to public places such as cinema or restaurant) for at least 10 days after discharge. This quarantine period, as recommended by the Hospital Authority, was under constant review. These SARS patients would be considered non-infectious at five weeks from the illness onset and after three negative stool samples taken between the third and fourth weeks were negative for SARS-associated coronavirus.
3. Results
The first paediatric SARS patient was admitted on 13 March. From this date until 23 June, nine patients with probable SARS and 29 patients with suspected SARS were admitted into the UHR-S area. The mean and standard deviation (SD) age for these two groups were 8.9 (6.2) years and 7.4 (5.4) years, respectively. The clinical and laboratory characteristics of probable SARS patients are summarized in Table III . Another 88 febrile children and adolescents with pneumonia but no SARS contact, with a mean (SD) age of 8.2 (5.3) years, were admitted into the isolation cubicle of the UHR-I area. Two hundred and twenty-seven patients with febrile illnesses but normal chest radiographs, at a mean (SD) age of 4.9 (5.1) years, were managed in an open cubicle in the UHR-I area. In addition, 274 non-febrile patients aged 7.5 (6.0) years were admitted into the HR area. Eleven non-febrile patients initially admitted to the HR area were subsequently transferred (two for fever and pneumonia and nine for febrile non-respiratory illnesses) to the UHR-I area during their inpatient stay.
Table III.
Summary of clinical and laboratory features of patients with probable SARSa
| Virology for SARS-associated coronavirus |
||||||||
|---|---|---|---|---|---|---|---|---|
| Case no. | Sex | Age (years) | Close SARS contact | Lowest lymphocyte count (×109/L) in PB) (normal range for age) | Highest plasma lactate dehydrogenase (IU/L)b | RT-PCR | Viral isolation | Seroconversion |
| 1 | F | 0.33 | Yes | 2.0 (4.0–13.5) | 606 | Pos | Neg | Pos |
| 2 | M | 2 | Yes | 1.1 (3.0–9.5) | 308 | – | Pos | Pos |
| 3 | F | 5 | Yes | 1.1 (1.5–6.8) | 324 | – | Pos | Pos |
| 4 | F | 6 | Yes | 1.1 (1.5–6.8) | 275 | – | Neg | Neg |
| 5 | M | 7 | Yes | 1.2 (1.5–6.8) | 354 | – | Neg | Pos |
| 6 | M | 13 | Yes | 0.6 (1.2–5.2) | 413 | Neg | Neg | Pos |
| 7 | F | 14 | No | 0.4 (1.2–5.2) | 336 | Pos | Neg | Pos |
| 8 | M | 16 | Yes | 0.6 (1.2–5.2) | 224 | Pos | Neg | Pos |
| 9 | M | 17 | Yes | 0.5 (1.2–5.2) | 339 | Neg | Neg | Pos |
PB, peripheral blood; RT-PCR, reverse transcriptase-polymerase chain reaction; F, female; M, male; Neg, negative; Pos, positive.
All patients had chest radiographic abnormalities compatible with SARS.
Upper limit of normal was 213IU/L.
During this three-month period, four doctors were assigned to manage patients in the UHR-S area, and 19 were responsible for patients in the other areas. Among the other staff, there were 17 nurses, one ward clerk and four healthcare assistants in the UHR-S ward; 16 nurses, one ward clerk and three healthcare assistants in the UHR-I ward and 18 nurses, one ward clerk and six healthcare assistants in the HR area. Also during the SARS outbreak at PWH, the paediatric surgical and orthopaedic wards were closed in order to re-deploy HCWs to the SARS wards of the hospital. As from 9 April, all patients in these wards were moved to the paediatric HR area. With this arrangement, 24 medical staff from various paediatric surgical subspecialties also worked in the paediatric HR area.
A total of 26 HCWs were in close contact4 with patients with probable or suspected SARS in the UHR-S area and 88 medical and para-medical staff had contact with patients in the other areas. None of the medical and para-medical staff in this department developed symptoms or signs suggestive of clinical SARS infection. No patient or visitor acquired SARS during their hospitalization, or during their visit to the paediatric wards.
4. Discussion
SARS-associated coronavirus is highly contagious, and one index patient was responsible for infecting 138 HCWs and their relatives during the hospital outbreak in Hong Kong.8 Being a general hospital not designed for patients with infectious diseases, we tried to implement management guidelines and infection control measures appropriate to the environment in order to minimize cross-infection among HCWs. This article describes the implementation of an effective triage policy and infection control measures in the paediatric department since the outbreak. With prompt and proper control measures, none of the paediatric HCWs was affected over the three months up to the time of writing. We suggest that our strategy can be used as a model for other paediatric units. This information could help to formulate infection control policies against nosocomial SARS infection.
Our results suggest that the combined efforts of proper patient triage, as well as stringent infection control and isolation in a hospital setting, could prevent SARS infection in HCWs. Hong Kong has recently experienced two major SARS outbreaks—one in the adult medical wards of PWH and the other in a community complex, Amoy Gardens.7., 8., 9. The common crucial factor contributing to these outbreaks is that the index cases were not identified and isolated at an early stage. In addition, the workload in the medical wards is heavy and bed occupancy frequently exceeds recommended limits. The wards were overwhelmed by acute admission of over 100 SARS patients in one week. Further, HCWs had limited understanding about the mode of transmission of this new disease in the early stages of the outbreak. The combination of these risk factors perpetuated cross-infection among patients and HCWs in the first week of the outbreak. In contrast, the paediatric wards were relatively less crowded and with fewer SARS admissions. Besides, the paediatric wards have already implemented stringent infection control precautions by the time the first child with SARS was admitted. These infection control measures were adapted from the adult intensive care unit of PWH, which has also prevented nosocomial SARS among HCWs.5 Our results suggest that our preventive strategies are effective against the spread of SARS.
Young children and adults with SARS may have different clinical presentations during the early phase of the disease.8., 10. In Hong Kong, where SARS has spread to the community, a definitive contact history could not be elicited in approximately 10% of adult SARS patients (personal communication, Dr David Hui, Department of Medicine and Therapeutics, PWH). Hence, an effective triage model for hospitalization has to be implemented. The presence of fever (>38 °C) and symptoms of respiratory tract infection including cough and shortness of breath are currently the most important criteria for suspecting SARS in the emergency department.3., 11. Our recent report suggests that fever was present in all 10 children with SARS.10 However, our medical colleagues found that some adult SARS patients developed fever only two weeks after the initial contact exposure, and a small number of them did not even have fever on hospital admission.8 Rainer and colleagues11 also suggested that the absence of chest symptoms could not be reliably used to screen out SARS cases. A number of episodes have occurred where elderly SARS patients were initially admitted to surgical wards (i.e. MR area) for unrelated problems. The diagnosis of SARS was delayed for several days and cross-infection among HCWs had already occurred when the symptoms became more apparent. Thus, the prevailing triage system proposed by the Hospital Authority (‘SARS precaution in hospitals—infection control and risk management approach’; available at: http://www.ha.org.hk/hesd/nsapi) is associated with significant pitfalls.3 One factor for the apparent success of our preventive strategies may be related to the observation that infected children present with more typical SARS symptoms. Thus, febrile children with SARS could be triaged to the UHR area in which a very high level of infection control measures was implemented.
Our experience with children and adolescents with SARS in Hong Kong suggests that younger patients have a milder and shorter clinical course, whereas teenagers present with more severe disease similar to that of adults.7., 8., 9., 10. The milder clinical course in young SARS patients may be due to less pronounced inflammatory responses to SARS-associated coronavirus that result in less severe lung damage. Children with SARS may also shed a lower viral load when compared with adults. The fact that SARS-associated coronavirus could be isolated in only two of our nine children with probable SARS supports this hypothesis. Thus far, there has not been any reports of a school outbreak in the community. Hence, children with SARS may not be as infectious as adults. Our results suggest that personal respirators (disposable hoods with breathing filters) may not be required when caring for children with SARS. Future studies are necessary to delineate the immunological responses to SARS and conduct virological surveillance in children and adults to try to answer these questions.
In summary, an appropriate triage system and prompt isolation of potential SARS patients along with stringent infection control precautions appear to be useful in preventing the cross-infection of SARS-associated coronavirus.
Acknowledgements
This article is dedicated to all healthcare workers who work days and nights to help in fighting against SARS in Hong Kong.
References
- 1.Donnelly C.A., Ghani A.C., Leung G.M. Epidemiological determinants of spread of causal agent of severe acute respiratory syndrome in Hong Kong. Lancet. 2003;361:1761–1766. doi: 10.1016/S0140-6736(03)13410-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seto W.H., Tsang D., Yung R.W.H. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS) Lancet. 2003;361:1519–1520. doi: 10.1016/S0140-6736(03)13168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ho W. Guideline on management of severe acute respiratory syndrome (SARS) Lancet. 2003;361:1313–1315. doi: 10.1016/S0140-6736(03)13085-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hon K.L.E., Li A.M., Cheng F.W.T., Leung T.F., Ng P.C. Personal view of SARS: confusing definition, confusing diagnoses. Lancet. 2003;361:1984–1985. doi: 10.1016/S0140-6736(03)13556-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li T.S.T., Buckley T.A., Yap F.H.Y., Sung J.J.Y., Joynt G.M. Severe acute respiratory syndrome (SARS): infection control. Lancet. 2003;361:1386. doi: 10.1016/S0140-6736(03)13052-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ng P.C., So K.W., Leung T.F. Infection control for SARS in a tertiary neonatal centre. Arch Dis Child Fetal Neonatal Ed. 2003;88:F405–F409. doi: 10.1136/fn.88.5.F405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peiris J.S.M., Chu C.M., Cheng V.C.C. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet. 2003;361:1767–1772. doi: 10.1016/S0140-6736(03)13412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee N., Hui D., Wu A. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348:1986–1994. doi: 10.1056/NEJMoa030685. [DOI] [PubMed] [Google Scholar]
- 9.Peiris J.S.M., Lai S.T., Poon L.L.M. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hon K.L.E., Leung C.W., Cheng W.T.F. Clinical presentations and outcome of severe acute respiratory syndrome in children. Lancet. 2003;361:1701–1703. doi: 10.1016/S0140-6736(03)13364-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rainer T.H., Cameron P.A., Smit D. Evaluation of WHO criteria for identifying patients with severe acute respiratory syndrome out of hospital: prospective observational study. BMJ. 2003;326:1354–1358. doi: 10.1136/bmj.326.7403.1354. [DOI] [PMC free article] [PubMed] [Google Scholar]


