Abstract
Study objective
We describe the implementation of a mobile pediatric emergency response team for mildly ill children with influenza-like illnesses during the H1N1 swine influenza outbreak.
Methods
This was a descriptive quality improvement study conducted in the Texas Children's Hospital (Houston, TX) pediatric emergency department (ED), covered, open-air parking lot from May 1, 2009, to May 7, 2009. Children aged 18 years or younger were screened for viral respiratory symptoms and sent to designated areas of the ED according to level of acuity, possibility of influenza-like illness, and the anticipated need for laboratory evaluation.
Results
The mobile pediatric emergency response team experienced 18% of the total ED volume, or a median of 48 patients daily, peaking at 83 patients treated on May 3, 2009. Although few children had positive rapid influenza assay results and the morbidity of disease in the community appeared to be minimal for the majority of children, anxiety about pandemic influenza drove a large number of ED visits, necessitating an increase in surge capacity. Surge capacity was augmented both through utilization of existing institutional resources and by creating a novel area in which to treat patients with potential airborne pathogens. Infection control procedures and patient safety were also maximized through patient cohorting and adaptation of social distancing measures to the ED setting.
Conclusion
The mobile pediatric emergency response team and screening and triage algorithms were able to safely and effectively identify a group of low-acuity patients who could be rapidly evaluated and discharged, alleviating ED volume and potentially preventing transmission of H1N1 influenza.
Introduction
A Gulf Coast location has ensured that Houston, TX, has been confronted directly or indirectly with many natural disasters.1, 2 These events have led to increased preparedness on the part of the city and its medical services. The emergency department (ED) at Texas Children's Hospital has participated in disaster management in the past, most notably in the aftermath of Hurricane Katrina by creating and implementing a mobile pediatric emergency response team (MPERT). Ultimately, it doubled its capacity and during a 13-day period provided medical care to more than 3,500 pediatric Hurricane Katrina victims housed in the Astrodome.2
Editor's Capsule Summary.
What is already known on this topic
Appropriate response to a natural or manmade disaster requires sufficient regional surge capacity.
What question this study addressed
Can a mobile pediatric emergency response team enhance regional surge capacity during an H1N1 influenza epidemic?
What this study adds to our knowledge
In this single-site observational study during a low-acuity infectious outbreak, the mobile team helped to decrease left without being seen rates and waiting times.
How this might change clinical practice
Disaster mitigation response planners can consider implementation of emergency response teams.
The surge capacity of the ED again was tested in late April of 2009 by H1N1 swine influenza. The unique challenges of dealing with a novel influenza strain with pandemic potential would require triaging and surge potential planning of a very different kind than had previously been used for natural disasters. According to the surge potential of this event and the success of MPERT post–Hurricane Katrina, MPERT was implemented onsite in an open-air parking lot located fewer than 50 feet from the entrance to the Texas Children's Hospital ED.
Background
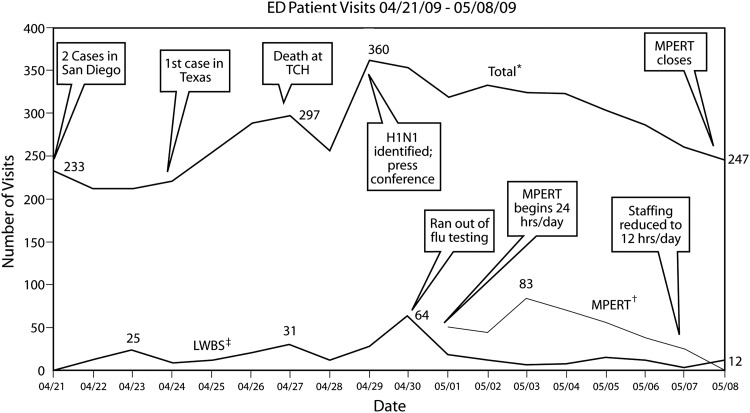
Mexico reported increased cases of pneumonia and death in late April 2009, and cases were seen in Texas shortly thereafter.3, 4, 5 In Houston, the ED noted an increase in patient visits (Figure 1). On the morning of April 27, 2009, a young child died of H1N1 influenza at Texas Children's Hospital. This child, originally from Mexico City, had been transported to Texas Children's Hospital on April 14, 2009. Confirmation of his influenza isolate as H1N1 swine variant was received from the Centers for Disease Control and Prevention (CDC) on April 29, 2009, and was reported in the media on that date. Subsequently, the ED treated 360 patients that day; historically, approximately 230 patients are treated daily in April. On that date, there were 91 confirmed US cases and 16 cases in Texas. Concern for spread of the virus in congregate settings had led to the closure of 3 Houston-area schools.
Figure 1.
Patient volume in the Texas Children's Hospital ED, April 21 to May 8, 2009.
*Total ED visits.
† Children seen daily at MPERT.
‡ Left without being seen.
TCH, Texas Children's Hospital.
Importance
The Texas Children's Hospital ED was already experiencing higher patient volumes even before it was announced that a Texas Children's Hospital patient had died of influenza. Given the widespread media coverage and the anxiety level in the community, these numbers were expected to increase. Consequently, the ED developed plans for patient surge by exploring alternative areas in which children could be evaluated. This is a descriptive study, but one that underscores the pragmatic aspects of implementing flexible responses to disaster situations.
Goals of This Investigation
The hypothesis was that the development and deployment of MPERT will reduce elopements during periods of unexpected emergency department (ED) surge and reduce ED length of stay. The goal was to create a location with good airflow, in which a large volume of low-acuity patients could be treated rapidly, with minimal, if any, laboratory evaluation, with point-of-care testing, and with quick disposition home. A second goal was to describe the implementation of such a unit in a manner that may be reproducible in other settings.
Materials and Methods
Theoretical Model of the Problem
The decision to implement MPERT required monitoring trends of patient volumes and other factors. First, because Texas Children's Hospital treats a large number of medically complicated patients, the need to offer a safer environment in which to care for these and all patients was vital. To this end, early patient cohorting was essential. Second, the high level of community anxiety needed to be addressed. As the largest pediatric hospital in Houston, we were ideally positioned to offer community outreach through educational materials. Third, the need to address patient safety extended beyond infection control, involving efforts to treat children in a timely manner and decreasing the number of elopements. Finally, from an administrative standpoint, the financial ramifications of creating such a unit needed to be considered.
Study Design
This was a descriptive quality improvement project reviewing the creation and implementation of MPERT in response to potential pandemic influenza. The project was exempt from the institutional review board. All children treated in the Texas Children's Hospital ED from May 1 to May 8, 2009, were included in the triage algorithm, except for children actively being resuscitated.
Setting and Selection of Participants
Houston, the fourth largest city in the United States, has a population of approximately 5.7 million persons in the metropolitan area. There are more than 40 hospitals with EDs, including 2 free-standing children's hospitals, in the area. Most area hospitals have limited pediatric resources, resulting in many referrals to the 2 free-standing pediatric facilities in the area. Texas Children's Hospital is a tertiary care pediatric hospital licensed for 715 beds and, at this writing, was applying for Level I trauma designation. The Texas Children's Hospital ED cares for approximately 85,000 children annually, with an average 17% admission rate. The 65-bed ED is divided into several regions: the 24-bed main ED (treating all triage levels), a 19-bed rapid treatment area (treating all triage levels except children being actively resuscitated), a 10-bed urgent care center (treating well-appearing children), and a 12-bed observation unit.
The hospital's pandemic influenza plan included stocking 9,000 N95 respirators and having more than 600 doses of antiviral medications (oseltamivir, zanamivir) in stock. Plans had been made to provide chemoprophylaxis to staff members, as well as to exclude staff members with influenza-like illnesses for 7 days after symptom onset. Had the morbidity of H1N1 influenza been more severe,6 the plan was to utilize a geographically distinct 15-bed unit as the inpatient area for influenza-positive patients, in the hope of limiting nosocomial spread of the virus. A second 14-bed inpatient unit in the same building was designated as an overflow area to be used if necessary. These areas would have been staffed by the hospitalist service, a group that is already a part of the section of emergency medicine at Texas Children's Hospital, facilitating communication and patient care. This group also participated in the physician staffing of MPERT and was prepared to increase their inpatient presence if needed to cover influenza admissions.
Interventions
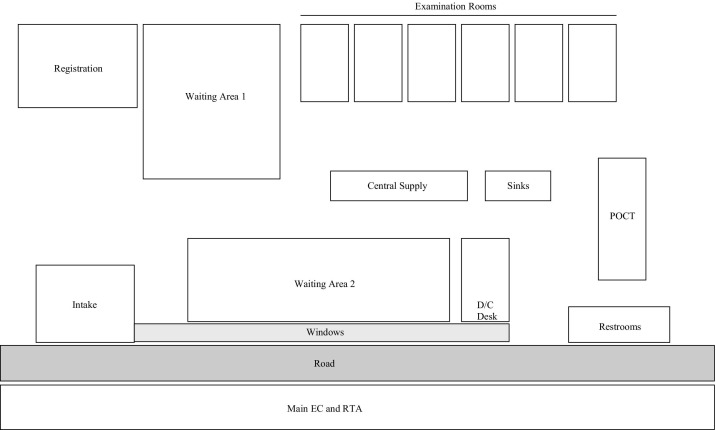
The area that was chosen was a 58-by-150-foot covered, open-air parking lot across from the main ED (Figure 2), offering advantages of proximity and excellent ventilation. Construction of MPERT was accomplished in 8 hours, beginning with improving lighting and cleaning the floors. Mosquito netting was installed around the majority of the unit. An area within MPERT was created for point-of-care testing. Six examination rooms with easily cleanable carpet were constructed, each with a desk, 3 chairs, and supply cart. Chairs in waiting areas were kept 3 feet apart to minimize disease transmission. A video with discharge instructions specific to viral respiratory illnesses was played in English and Spanish in waiting rooms. The video was created by the ED staff in response to family queries. Three portable restrooms, modular sinks, alcohol-based cleaner dispensers, tissue paper, and waste receptacles were readily available. Modular sinks were part of hospital supplies; the restrooms were rented from private vendors. N95 respirators were available for staff, and surgical masks were available for children and their guardians.
Figure 2.
Layout of the MPERT.
There is evidence that heat and humidity may help prevent the spread of droplets.7 However, because the average high temperature in Houston in May is 85°F, with 65% to 91% humidity,8 the importance of cooling was recognized at the outset. Cooling units were placed in each examination room and several were distributed in the waiting areas. The need to balance personal comfort against airborne transmission led to placing the cooling ductwork over the heads of the health care workers, pointed in the direction of patients. A fixed number of air exchanges hourly could not be standardized in this open-air setting.
The MPERT patient care area was open 24 hours per day and staffed by additional personnel working 12-hour shifts: 1 physician, 3 nurses (one of whom was responsible solely for laboratory follow-up and discharge education), 1 respiratory therapist, 1 to 2 patient care assistants, 1 laboratory technician, and 1 housekeeper. A Spanish translator was always available because approximately 30% of the families cared for are Spanish speaking. One senior experienced nurse staffed the intake area. If needed, staff could be diverted to MPERT from other areas of the ED, depending on patient flow patterns. Staffing was accomplished through supplemental pay to physicians and nurses. Many nurses who worked in MPERT ordinarily worked in sections apart from emergency medicine.
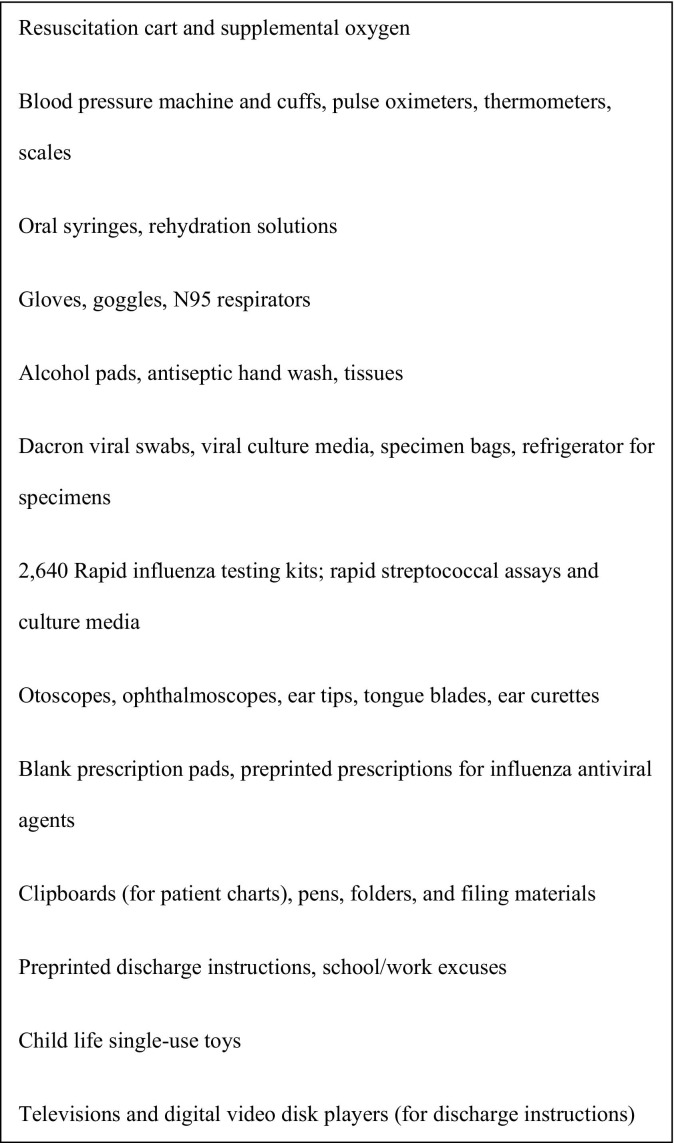
An abbreviated formulary was created for MPERT by the hospital pharmacy with antipyretics and ondansetron. Additional medications were available through the Texas Children's Hospital ED pharmacy through a runner. A pediatric resuscitation cart and supplemental oxygen supply were available. Although the Texas Children's Hospital pharmacy ordinarily does not fill prescriptions for outpatient medications, given the shortage of antivirals in the community, families could purchase these medications before leaving. Children requiring antibiotics or other medications were given prescriptions to be filled at local pharmacies. Supplies stocked in MPERT are listed in Figure 3. Because MPERT was located within the institution, with supplies readily accessible, and inventory space was limited, the decision was made to stock only commonly used supplies.
Figure 3.
Examples of supplies for MPERT.
Trauma patients and children being actively resuscitated were taken directly to a shock room, where health care workers wearing gowns, gloves, and N95 respirators immediately treated patients. A nurse on the ambulance dock evaluated all medically stable children arriving by ambulance for viral respiratory symptoms. The intake area for all patients arriving by private conveyance was located under a tent in front of MPERT. The rationale behind this was to screen all patients before entry into the ED in an environment in which, because of airflow and humidity, transmission risk could be minimized. In addition, identification of children with influenza-like illnesses would facilitate patient cohorting and enable distribution of masks to at-risk children and families. Children were limited to having 1 accompanying adult to decrease nosocomial infections and crowding.
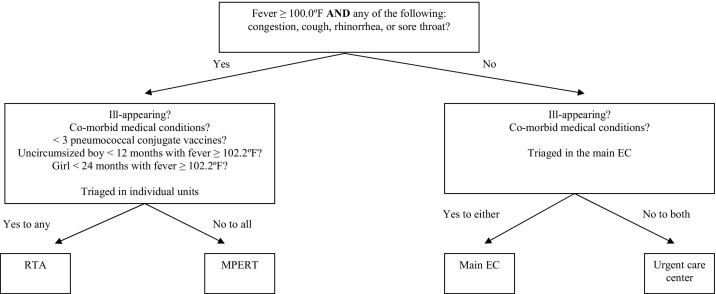
The screening algorithm is shown in Figure 4. The CDC case definition4 was used to stratify patients according to symptoms consistent with viral respiratory disease, ill appearance, and medical comorbidities. The goal of MPERT was social distancing in an open-air environment and the rapid assessment, treatment, and discharge of well-appearing, previously healthy children exhibiting symptoms compatible with H1N1 swine influenza. To this end, the intake screening algorithm attempted to exclude many children who, under commonly used fever protocols,9 may have required laboratory evaluation. A senior nurse experienced with institutional triage guidelines performed the intake screening. The physical layout of the ED facilitated symptom-based cohorting because the different areas in the ED all had separate waiting areas.
Figure 4.
Intake triage algorithm for MPERT.
Once the intake screening identified the proper ED location for the patient, both the patient and guardian were given a colored wristband that allowed them into a specific section of the ED. Patients, guardians, and staff were not granted access to a given area unless they had an appropriately colored wristband; discharged patients had the wristbands removed before exiting the building. To prevent the removal of the wristbands, patients and their families were informed that they could not continue with the registration process or have prescriptions for antivirals filled unless they had the appropriate wristband and remained in their respective assigned locations. Hospital security staff and trained staff volunteers were vital in ensuring compliance with cohorting efforts and also aided in escorting children and their families to their appropriate destinations.
For MPERT patients, registration, medical evaluation, treatment, and discharge were all performed in that area. Patients were in the rooms only for medical evaluation and specimen collection and then were moved back to the waiting area. This enabled rapid room turnover, decreasing wait time and overall patient volumes in MPERT. A hard-copy packet was created for streamlined documentation, including a nursing assessment sheet, preprinted physician order sheets, discharge instructions, and school excuses. A new 1-page history and physical documentation form and modified billing form were used. Charts were entered into the electronic medical record within 24 hours of the patient visit.
Children who had point-of-care testing for influenza or group A streptococcus were sent to the waiting area. The discharge nurse checked the test results. If the test was positive for influenza, the nurse contacted the MPERT physician, who met with the family and prescribed antivirals if the patient had been symptomatic for less than 48 hours. Patients with positive rapid streptococcal assay results were prescribed antibiotics. If the test results were negative, this information was conveyed by the discharge nurse, whose sole job was to follow up results and educate families. The physician was available to answer questions if needed. A detailed set of verbal and written instructions with anticipatory guidance and antipyretic dosing was given to the family in English or Spanish and reemphasized by a bilingual video created by the authors to educate families and address their anxiety. Children were instructed to remain out of school for 7 days (regardless of rapid influenza test result) or until symptom resolution, whichever was later, and given preprinted school or work excuses.
N95 respirators were available for all clinical staff. The hospital inventory of 9,100 respirators was augmented by 4,500 through private vendors. Approximately 700 clinical employees previously were fit-tested for N95 respirators as part of a tuberculosis control program. When possible, these employees were assigned to care for patients suspected of having influenza. For other employees, mass fit-checking of respirators was performed. Because fit-checking would have overwhelmed the resources of employee health, 175 hospital personnel were trained in fit-checking. Subsequently, more than 1,100 staff were fit-checked.
Surgical masks were available for children with respiratory symptoms (and any accompanying guardian with respiratory symptoms), who were to be evaluated in one of the interior portions of the ED, in an attempt to decrease transmission in indoor settings. Children with respiratory symptoms were placed into a private room as quickly as possible; however, immediate placement was not always feasible. Because the ED had only 2 negative-pressure rooms, the emphasis was on conscientious hand hygiene, contact and airborne isolation, and the use of personal protective equipment. Persons caring for a child with viral respiratory symptoms followed CDC guidelines,10 wearing a respirator, disposable gown, and gloves for patient contact. Viral testing was conducted by nasal swab by a respiratory therapist wearing eye protection.
Given increased patient volume, point-of-care testing for influenza A and B was performed with the Binax NOW CLIA-waived test kits (Binax, Inc., Portland, ME)11 in a designated MPERT space by the Diagnostic Virology Laboratory. Samples also were transported on ice to the Diagnostic Virology Laboratory for viral culture and influenza A subtyping, as per existing protocol. As the demand for specimens increased, Diagnostic Virology Laboratory staff trained 6 ED personnel to perform the rapid assays. Another point-of-care test performed was the rapid streptococcal assay because there were many children presenting with pharyngitis; as per existing hospital protocol, all children with negative rapid streptococcal assay results then received a throat culture test. The diagnostic capabilities of MPERT deliberately were limited because of staffing, the need to treat large numbers of children rapidly, and the difficulty in performing certain testing in semiprivate settings. Consequently, the triage algorithm was designed primarily to evaluate children who were unlikely to require extensive laboratory evaluation.
Answers to frequently asked physician questions were posted on the Texas Children's Hospital intranet and Internet sites. E-mail updates were sent daily to inform the Houston medical community on the most recent local epidemiologic data, screening recommendations, and updated CDC recommendations. Effective communication between physicians in the hospital and community, as well as between physicians and families, was essential to decrease anxiety and unnecessary patient visits. Efforts were also made to address health care worker anxiety and involved online modules and videos available on the hospital intranet site to educate staff about H1N1. All clinical staff members and ancillary staff were fit-checked for N95 respirators, which were readily available throughout the hospital.
Methods of Measurement and Primary Data Analysis
Total ED visits and visits to each area of the ED, time in department, numbers of admissions, and patients in whom viral testing was used were captured in a computerized database. Stata (version 10; StataCorp, College Station, TX) was used for data analysis. Statistical significance was set at P≤.05 where appropriate. Mann-Whitney test was used for data that were not normally distributed. To determine confidence intervals (CIs), data were log-transformed, and the 95% CIs of mean differences in time in department between the study intervals were calculated. A 95% CI of a natural logarithm that crosses 0 indicates that the null hypothesis of no difference in time in department cannot be excluded.
Results
MPERT opened at 4 pm on May 1, 2009, and 49 children were cared for by 1 physician in the first 8 hours. In a 7-day period, MPERT experienced 18% of the ED volume (total of 356 patients), a median of 48 patients daily, peaking at 83 patients on May 3, 2009 (Figure 1). This partially compensated for the increased patient volume of 120 (50% excess) children over the baseline flow observed in the springtime. Despite the increase in volume, with MPERT wait time (triage time to room) and time in department (arrival time to discharge from ED) in the ED for all patients and for all triage levels decreased (Table). All MPERT patients were discharged home. The percentage of patients who left without being seen decreased by 44% (from 143 to 81 patients) with the opening of MPERT, and only 3 (<1%) of MPERT patients left without being seen (P<.001). Sixteen children (4.5% of MPERT volume) were mistriaged and had to return to another section of the ED for additional evaluation; reasons included 9 children needing additional laboratory evaluation, 5 requiring intravenous fluids, and 2 requiring breathing treatments. Of these 16, 3 stayed overnight in the observation unit (2 with dehydration; 1 with wheezing) and 1 child with pneumonia and hypoxemia was admitted to the inpatient unit.
Table.
ED time in department preceding and during MPERT.⁎
| Median TID (Hours) |
||||
|---|---|---|---|---|
| Patient Categories | Pre-MPERT (# Patients) | MPERT (# Patients) | Median Difference of TID (Hours) | Ln (Mean Difference of TID)[95% CI]† |
| All patients (MPERT+main ED) | 4.8 (1,417) | 3.5 (1,931) | 1.3 | 0.317 [0.27 to 0.36] |
| MPERT patients | N/A | 1.8 (356) | N/A | — |
| All triage level II: critical | 5.7 (112) | 5 (110) | 0.7 | 0.129 [–0.02 to 0.28] |
| All triage level III: emergency | 5.8 (308) | 5.3 (370) | 0.4 | 0.029 [–0.05 to 0.11] |
| All triage level IV: urgent | 4.9 (563) | 4 (789) | 0.9 | 0.225 [0.16 to 0.29] |
| All triage level V: nonurgent | 4.1 (434) | 2 (662) | 2.1 | 0.627 [0.56 to 0.70] |
TID, Time in department; N/A, not applicable.
MPERT was operational from May 1, 2009, at 4:00 pm until May 7, 2009, at 11:59 pm. Because data are not normally distributed, median times, rather than means, are presented. This period was compared with ED flow from April 27, 2009, at midnight until May 1, 2009, at 3:59 pm. TID: arrival to discharge home or admission to hospital. Differences in numbers between Figure 1 and the Table are due to exclusion of children being actively resuscitated (triage level I) and children who left the ED before triage from the algorithm.
The natural logarithm of TID is presented here. If the 95% CI of the natural logarithm crosses 0, there is no statistically significant difference in TID.
At the onset of the study, patients were being liberally screened for influenza. Three hundred sixty-nine rapid influenza assays were performed in the week preceding MPERT (13 [3.5%] positive for H1N1), and 680 were performed during the MPERT week (11 [1.6%] positive for H1N1). Despite extensive screening, only 18 children (2.8%) had positive rapid influenza assay results from April 21, 2009, to May 4, 2009. This knowledge led to the recommendation on May 4, 2009, that screening be performed only for patients with moderate to severe disease. As of May 5, 2009, the Texas Children's Hospital pharmacy had dispensed only 3 doses of oseltamivir and no doses of zanamivir.
With decreasing patient volumes (Figure 1), the decision was made to change MPERT staffing to 12 hours on May 7, 2009, and ultimately closed on that date, after 7 operational days. Despite MPERT closing, additional physician coverage was provided in the ED for the next 2 days for any unanticipated surge in patient volume; because no such surge was observed, staffing returned to baseline.
Despite Texas Children's Hospital's reporting the first US pediatric death, the overall morbidity of disease in Houston children was minimal, with no hospitalized child having confirmed swine H1N1 as of May 8, 2009. However, 29 children with fever and viral respiratory symptoms were empirically isolated, with airborne and contact precautions, despite negative rapid influenza testing results. The total percentage of patients admitted from the ED was 14%, lower than the 17% admission rate ordinarily observed at Texas Children's Hospital. The lower admission rate was due to the high volume of low-acuity patients. The cost of MPERT was approximately $280,000 above expected ED costs, of which $135,000 was supplemental staff pay and $113,000 was MPERT construction and additional laboratory and medical supplies. However, this does not reflect the overall savings to the hospital from decreased time in department and decreased elopements.
Limitations
The generalizability of MPERT might be limited by the low patient acuity and low positive influenza assays observed in our center. The same effect on patient flow may not have been experienced with higher patient morbidity. However, part of the goal of this intervention was to reduce the number of low-acuity children being treated in the main ED. This decompression of the higher-acuity areas of the ED would have been even more important for influenza with greater morbidity and mortality. Also, the use of an outdoor ED might not be feasible in inclement weather. Although many aspects of MPERT worked well, there remain a few areas for improvement. Work duties must be clearly delineated because personnel often were asked to perform outside their normal roles. One of the advantages of MPERT was the ability to rapidly change processes; however, new algorithms needed to be created and conveyed to the rotating staff. Sustaining the efficient flow of patients through MPERT required reinforcement and continued communication of process changes. A current process manual with delegation of responsibilities would have helped maintain uniformity of procedures. During the outbreak, the screening questionnaire went through revisions as the CDC case definition was modified, and this information also needed to be conveyed. Assessment of ED utilization specifically for influenza was difficult, given the low numbers of positive rapid influenza test results and nonspecific International Classification of Diseases, Ninth Revision coding.
Discussion
Similar to the response to post–Hurricane Katrina, the specialized pediatric resources and response to H1N1 swine influenza were provided and coordinated by a regional tertiary care pediatric facility, drawing on preexisting experience, personnel, and infrastructure. MPERT was developed to provide a readily available specialized regional resource that could be mobilized whenever and wherever needed. Resource utilization and reallocation allowed for a rapid, cohesive institutional response. The ability to quickly respond to a dynamic situation was possible because of experiences dealing with mass casualty situations and a physical infrastructure that could be adapted for a new functionality. The hospital experience with pediatric Hurricane Katrina evacuees identified several areas of improvement: cohorting for infectious diseases, improving communication, and streamlining processes.2 These were addressed before the start of this MPERT. The need to identify venues for obtaining emergency stocks of supplies (eg, rapid influenza testing kits) also was recognized. One possibility would have been contacting the regional hospital preparedness council's Catastrophic Medical Operations Center. The center was used after Hurricane Katrina to coordinate regional resources, avoid duplication of requests, and streamline processes.12
The unique circumstances of the threat of pandemic influenza necessitated a novel strategy in the ED because of increasing patient volumes and infection control concerns. The epicenter of the 1988 to 1989 Houston measles epidemic was the Texas Children's Hospital ED waiting room.13 The threat of another airborne pathogen led to the decisions to perform active surveillance for symptoms, using a screening questionnaire, and to screen patients outdoors. The infection control challenge was to keep care areas safe for staff and patients. Although the community could practice social distancing, we could not; in fact, ill children actively sought out our facility. We performed social distancing through infection control techniques: active screening for symptoms, isolation, contact precautions, and use of N95 respirators.
The first part of this approach was based on the Texas Children's Hospital experience with tuberculosis,14 involving active surveillance of caregivers of children with suspected tuberculosis. Although children with suspected tuberculosis are placed in negative-pressure rooms, the limited number of rooms and high patient volumes made this strategy impossible for H1N1 influenza. As a result, the decision was made to screen patients outdoors. This strategy was based on the Toronto experience with severe acute respiratory syndrome. The Toronto hospitals began screening patients before entry into the hospital to enable appropriate cohorting and to minimize risk to their staff.15, 16 This strategy was particularly attractive at Texas Children's Hospital, where the ED is across a covered breezeway from an open-air parking lot. This setup provided all the advantages of ventilation while retaining proximity to the remainder of the ED. The warmth and humidity of Houston were very useful in this regard because influenza virions do not remain airborne for long periods under these conditions.7
Social distancing measures were also adapted for the realities of an ED waiting room. This involved separation of chairs, cohorting patients by symptoms, and provision of facemasks. Respiratory etiquette stations were created and stocked with antiseptic hand wash, tissues, and waste receptacles. Finally, patients were allowed to have only 1 parent or guardian enter MPERT. Keeping patients in the appropriate areas was facilitated by the use of color-coded wristbands and by creating incentives for parents and children to keep their wristbands in place.
Another lesson learned from Hurricane Katrina was the need to provide current, accurate information to families and physicians. Fears about H1N1 swine influenza created community anxiety and led to a decreasing of the threshold for seeking medical attention. Many pediatricians' offices were overwhelmed with patients, also contributing to increased ED volumes. The role of “epidemic anxiety” has been well documented for infectious and occupational diseases,17 and this was reflected in a number of asymptomatic children brought to the ED to “just make sure they don't have the swine flu.” Future disaster plans will need to incorporate mental health workers accessible to families and staff alike, particularly if morbidity and mortality increase.
A multimedia approach was taken to try to educate parents and community leaders on the realities of influenza. This included a nursing question line and automated telephone line parents could call to obtain answers to frequently asked questions. Patients treated in the ED were all discharged with printed guidance, created by ED physicians, on influenza that described viral symptoms, anticipated symptomatic period, supportive care, and infection control measures that could be implemented within households. These instructions were available in English and Spanish and were reinforced by a specifically created digital video disk and by verbal instructions from the discharge nurse.
Hurricane Katrina also taught the importance of streamlining processes when dealing with a large influx of patients. This was accomplished in several ways. First, a revised single-page documentation sheet for both physicians and nurses was created for MPERT. For hospitals using electronic medical records, disaster circumstances might necessitate temporary use of paper records. Second, redundant evaluations were reduced by combined physician and nursing assessments. Third, to maximize the limited number of rooms, patients were moved to a different waiting area, pending laboratory results; this enabled rapid room turnover. Fourth, the presence of a dedicated discharge nurse for following up laboratory results, counseling, and anticipatory guidance enabled other MPERT providers to continually treat patients. Finally, the ability to perform point-of-care testing decreased turnaround time.
The implementation of the H1N1 MPERT yielded countless benefits to all involved in the collective disaster response. Patients thought to be at risk for having the virus were efficiently triaged, isolated, evaluated, treated, and discharged home directly from the exterior unit. The risk of human-to-human transmission of what was potentially a contagious and deadly airborne virus was minimized by utilizing social distancing, infection control procedures, and an outdoor venue. ED surge capacity was increased. More efficient and flexible practices were developed that will likely become integrated into future ED policy and procedure; these included streamlined documentation, simultaneous physician and nursing evaluation, and use of a designated discharge nurse educator. Strategies and triggers for opening and closing the MPERT were created and successfully implemented by the hospital administration. Perhaps the most unexpected benefit was the serendipitous discovery of the parking lot as a patient care area. This rather inconspicuous, underused piece of real estate will continue to serve as a flexible area to augment ED surge capacity.
Much of the concern about pandemic influenza has focused on critically ill patients overwhelming available resources and the current health care infrastructure. However, from an ED perspective, a rapid influx of minimally ill patients can offer a different set of challenges, taxing a system already overburdened with caring for nonemergency patients lacking access to routine medical care. In this scenario, it does not really matter whether the patients have influenza or not, but the perception that they might triggers anxiety and leads to visits. An unfortunate consequence might be that more seriously ill patients experience a delay in obtaining medical treatment. The lessons learned after Hurricane Katrina and from the current H1N1 swine influenza crisis about resource utilization and reallocation and the creation of multifunctional spaces are applicable in a variety of ED settings requiring increased surge potential. The MPERT model has many possible uses, ranging from pandemic episodes to more common seasonal respiratory illnesses.
Acknowledgments
The authors thank the individuals who volunteered their time and energy to MPERT. Although all of the persons involved cannot be mentioned here, we are especially grateful to the following members of the Texas Children's Hospital family: Robert Adkins; Charles Bradford; Greg Buffone, PhD; Chantal Caviness, MD, PhD; Susan Distefano; Anne Dykes; Erin Endom, MD; Bert Gumeringer; Karen Gurwitch, PharmD; Juan Juarez, MD; Mark Mullarkey; Gail Parazynski, RN; Jeffrey Starke, MD; Ann Stern; Keith Turner; James Versalovic, MD, PhD; Mark Wallace; Randall Wright; and the staff of the Diagnostic Virology and Pathology Laboratories, hospital administration, facilities, supply chain, pharmacy, and security, without whose collaboration MPERT would have been impossible.
Footnotes
Provide feedback on this article at the journal's Web site, www.annemergmed.com.
Supervising editor: Amy H. Kaji, MD, MPH, PhD
Author contributions: ATC, BP, MCD, JES, and PES organized the study. ATC, BP, MCD, CRC, and GJD-H participated in data collection. ATC, BP, and MCD analyzed the data. ATC drafted the article, and all authors contributed substantially to its revision. ATC had had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. ATC takes responsibility for the paper as a whole.
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article that might create any potential conflict of interest. The authors have stated that no such relationships exist. See the Manuscript Submission Agreement in this issue for examples of specific conflicts covered by this statement.
Reprints not available from the authors.
Please see page 24 for the Editor's Capsule Summary of this article.
Publication date: Available online October 17, 2009.
References
- 1.Sirbaugh P.E., Bradley R.N., Macias C.G., et al. The Houston flood of 2001: the Texas Medical Center and lessons learned. Clin Pediatr Emerg Med. 2002;3:275–283. [Google Scholar]
- 2.Sirbaugh P.E., Gurwitch K.D., Macias C.G., et al. Caring for evacuated children housed in the Astrodome: creation and implementation of a mobile pediatric emergency response team: regionalized caring for displaced children after a disaster. Pediatrics. 2006;117:S428–S438. doi: 10.1542/peds.2006-0099Q. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Swine influenza A (H1N1) infection in two children—Southern California, March-April 2009. MMWR Morb Mortal Wkly Rep. 2009;58:1–3. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Update: swine influenza A (H1N1) infections—California and Texas, April 2009. MMWR Morb Mortal Wkly Rep. 2009;58:1–3. [PubMed] [Google Scholar]
- 5.World Health Organization Viral gene sequences to assist diagnostics for swine influenza A(H1N1): GenBank accession numbers: 28 April 2009. http://www.who.int/csr/resources/publications/swineflu/SwinefluViralgenome.pdf Accessed May 3, 2009.
- 6.Morens D.M., Taubenberger J.K., Fauci A.S. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis. 2008;198:962–970. doi: 10.1086/591708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bridges C.B., Kuehnert M.J., Hall C.B. Transmission of influenza: implications for control in healthcare settings. Clin Infect Dis. 2003;37:1094–1101. doi: 10.1086/378292. [DOI] [PubMed] [Google Scholar]
- 8.Texas weather forecasts. http://www.rssweather.com/climate/Texas/Houston Accessed May 4, 2009.
- 9.Baraff L.J. Management of fever without source in infants and children. Ann Emerg Med. 2000;36:602–614. doi: 10.1067/mem.2000.110820. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention Interim guidance for infection control for care of patients with confirmed or suspected swine influenza A (H1N1) virus infection in a healthcare setting (3 May 2009) http://www.cdc.gov/h1n1flu/guidelines_infection_control.htm Accessed May 4, 2009.
- 11.Cruz A.T., Cazacu A.C., McBride L.J., et al. Performance characteristics of a rapid immunochromatographic assay for detection of influenza A virus in children during the 2003-2004 influenza season. Ann Emerg Med. 2006;47:250–254. doi: 10.1016/j.annemergmed.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 12.Hamilton D.R., Gavagan T., Smart K., et al. Houston's medical disaster response to Hurricane Katrina: part 2: transitioning from emergency evacuee care to community health care. Ann Emerg Med. 2009;53:515–527. doi: 10.1016/j.annemergmed.2008.10.024. [DOI] [PubMed] [Google Scholar]
- 13.Farizo K.M., Stehr-Green P.A., Simpson D.M., et al. Pediatric emergency room visits: a risk factor for acquiring measles. Pediatrics. 1991;87:74–79. [PubMed] [Google Scholar]
- 14.Muñoz F.M., Ong L.T., Seavy D., et al. Tuberculosis among adult visitors of children with suspected tuberculosis and employees at a children's hospital. Infect Control Hosp Epidemiol. 2002;23:568–572. doi: 10.1086/501972. [DOI] [PubMed] [Google Scholar]
- 15.Srinivasan A., McDonald L.C., Jernigan D., et al. Foundations of the severe acute respiratory syndrome preparedness and response plan for healthcare facilities. Infect Control Hosp Epidemiol. 2004;25:1020–1025. doi: 10.1086/502338. [DOI] [PubMed] [Google Scholar]
- 16.Tham K.-Y. An emergency department response to severe acute respiratory syndrome: a prototype response to bioterrorism. Ann Emerg Med. 2004;43:6–14. doi: 10.1016/j.annemergmed.2003.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boss L.P. Epidemic hysteria: a review of the published literature. Epidemiol Rev. 1997;19:233–243. doi: 10.1093/oxfordjournals.epirev.a017955. [DOI] [PubMed] [Google Scholar]