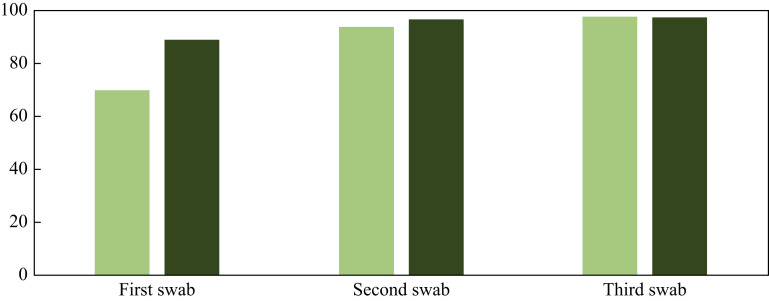
As of 29th February 2020, the World Health Organization had reported a total of 83,652 cases of coronavirus disease 2019 (COVID-19) in 51 countries in addition to China [1]. The diagnosis of respiratory viruses such as Middle East respiratory syndrome coronavirus (MERS-CoV) and severe acute respiratory syndrome coronavirus (SARS-CoV) relies on detection of the virus by real-time reverse transcriptase polymerase chain reaction (rRT-PCR) for in-vitro qualitative detection. The current recommendations are likewise to use rRT-PCR for the detection of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) in respiratory samples. There are many knowledge gaps facing the global health community in dealing with the new emerging SARS-CoV-2. Among the most pertinent is early identification of cases to facilitate application of isolation policies. The currently available RT-PCR kits are variable, offering sensitivities ranging between 45% and 60%; thus, particularly early in the course of an infection, repeat testing may be required to make a diagnosis. This is not easy to apply with the global shortage of testing kits. This mirrors experience with MERS-CoV. In a study of 336 patients with MERS, 89% had a positive result after one swab, 96.5% had a positive result after two swabs, and 97.6% had a positive result after three swabs (Figure 1 ) [2]. China has changed the case definition over the last 2 months to improve the ability to detect new cases. Data have emerged on the value of computed tomography (CT) scanning of the chest in the early diagnosis of cases. Multiple reports published to date have revealed higher sensitivity of chest CT in early detection of cases of SARS-CoV-2 [3]. In a study of 51 patients, the positivity rate for a single respiratory swab was 70%, an additional 24% (94% cumulative) after a second test, and an additional 3.9% (98% cumulative) after a third test (Figure 1) [4]. However, abnormal CT scan findings compatible with viral pneumonia were seen in 98% of patients [4]. This difference resulted in the study authors stating that CT scan is more sensitive than PCR. Reasons for the low sensitivity of PCR may include insensitive nucleic acid detection methods, variations in the accuracies of different tests, low initial viral load or improper clinical sampling [4]. An additional reason may be that lower respiratory samples may be better than upper respiratory samples, as is the case with MERS-CoV [5,6].
Figure 1.
Cumulative positive rate of swabs for the diagnosis of severe acute respiratory syndrome coronavirus-2 (light green bars) and Middle East respiratory syndrome coronavirus (dark green bars) based on reverse transcriptase polymerase chain reaction.
In another study of 167 patients, concordant CT scan and PCR test results were observed in 93% of patients; discordant results were observed in 4% (positive PCR but negative CT scan) and 3% (negative initial PCR and positive CT scan) of cases [7]. In a larger study of 1014 patients with SARS-CoV-2, 59% had positive RT-PCR and 88% had positive CT scan; using RT-PCR as a reference, the sensitivity of chest CT was 97% [8].
Growing evidence of the limitations of rRT-PCR prompts further consideration of the limitations of this diagnostic test. First, there are already more than seven different SARS-CoV-2 nucleic acid PCR tests [9]. When considering the viral load in samples, it has been shown that upper respiratory tract samples have their peak viral loads 3 days after symptom onset, and that nasal (rather than throat) samples have the highest viral loads [10]. As the current SARS-CoV-2 epidemic evolves globally, we need better diagnostic tests that are rapid, reliable, validated and widely available. For hospitalized patients, diagnostic algorithms based on a combination of RT-PCR and chest CT may prove to be necessary in order to ensure accurate detection of cases and to facilitate infection prevention measures. It is also very important to learn from the previous MERS-CoV epidemic and reflect on that experience, especially that a single negative upper respiratory sample is not enough to rule out infection. It may be prudent to keep those patients in isolation while additional swabs are obtained, or until lower respiratory samples can be obtained safely for definite diagnosis.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.World Health Organization . WHO; Geneva: 2020. Situation Report 17. Situation in numbers: total and new cases in last 24 hours.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200206-sitrep-17-ncov.pdf?sfvrsn=17f0dca_2 Available at: [Google Scholar]
- 2.Alfaraj S.H., Al-Tawfiq J.A., Memish Z.A. Middle East respiratory syndrome coronavirus intermittent positive cases: implications for infection control. Am J Infect Control. 2019;47:290–293. doi: 10.1016/j.ajic.2018.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020:200642. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fang Y., Zhang H., Xie J., Lin M., Ying L., Pang P. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020:200432. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Memish Z.A.Z.A., Al-Tawfiq J.A.J.A., Makhdoom H.Q.H.Q., Assiri A., Alhakeem R.F.R.F., Albarrak A. Respiratory tract samples, viral load, and genome fraction yield in patients with Middle East respiratory syndrome. J Infect Dis. 2014;210:1590–1594. doi: 10.1093/infdis/jiu292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corman V.M., Albarrak A.M., Omrani A.S., Albarrak M.M., Farah M.E., Almasri M. Viral shedding and antibody response in 37 patients with Middle East respiratory syndrome coronavirus infection. Clin Infect Dis. 2016;62:477–483. doi: 10.1093/cid/civ951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xie X., Zhong Z., Zhao W., Zheng C., Wang F., Liu J. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology. 2020:200343. doi: 10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wei M., Yuan J., Liu Y., Fu T., Yu X., Zhang Z.-J. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020 doi: 10.1001/jama.2020.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y., Kang H., Liu X., Tong Z. Combination of RT-qPCR testing and clinical features for diagnosis of COVID-19 facilitates management of SARS-CoV-2 outbreak. J Med Virol. 2020 doi: 10.1002/jmv.25721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020:2001737. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]