Abstract
Mesenchymal stem cells (MSCs) are strong immunomodulatory cells investigated in numerous clinical studies on fatal pathologies, such as graft versus host disease and autoimmune diseases; e.g., systemic lupus erythematosus, Crohn's disease, and ulcerative colitis. Macrophages are one of the critical cells linking the innate and adaptive immune system, and it has been shown that MSCs can differentiate between pro-inflammatory M1 phenotype and anti-inflammatory M2 phenotype of macrophages. However, it has not yet been fully clarified whether these differentiated macrophages are functional. In this study, we compared the immunomodulatory effects on the CD4 T cells of M1, M2a and M2c macrophages with the macrophages that directly and indirectly cultured with MSCs. We analyzed the changes in CD14, CD64, CD80, CD163 and CD200R expression to evaluate macrophage phenotypes, and the changes in CD4, IFN-g, IL-4, IL-17a and FoxP3 expression to evaluate T helper subsets using the FACS method. The changes in IL-1b, IL-4, IL-10, IL-12p70, IL-17a and IFN-g in the media supernatants were analyzed using the Luminex method. We also performed WST-1 and Caspase-3 ELISA analyses to observe the proliferation and apoptosis status of the T cells. MSCs were found to differentiate macrophages into a distinctive phenotype, which was close to the M2c phenotype, but was not considered as an M2c cell due to the low expression of CD163, a characteristic marker for M2c. While MEM-D, MEM-ID and MSCs showed similar inhibitory effects on the Th2 and Th17 cells, the most significant increase in Treg cell frequencies was seen in MEM-D cells. Macrophages can alter their phenotypes and functions according to the stimuli from the environment. The fact that macrophages educated with MSCs suppressed the production of all the cytokines we evaluated even after the removal of MSCs suggests that these cells may be differentiated by MSCs into a suppressive macrophage subgroup. However, the Treg cell activation caused by direct interactions between MSCs and macrophage cells may be the most prominent observation of this study compared to previous work. As a result, according to our data, the interactions between MSCs and macrophages may lead to differentiation of macrophage cells into an immunosuppressive phenotype, and these macrophages may suppress the T lymphocyte subgroups at least as effectively as MSCs. However, our data obtained from in vitro experiments should be supported by future in vivo studies.
Keywords: Mesenchymal stem cell, M1 macrophage, M2 macrophage, Th1, Th2, Th17, Treg, Immunomodulation
1. Introduction
Mesenchymal stem cells (MSCs) are adult stem cells that can be isolated from many tissues, and they have different types, such as chondrocyte, adipocyte or osteocyte (El, 2011). MSCs also have strong immunomodulation abilities; e.g., they suppress immune cells through the secretion of cytokines, such as prostaglandin E2 (PGE2), indoleamine 2,3 dioxygenase (IDO), hepatocyte growth factor (HGF), and soluble human leukocyte antigen G (sHLA-G) and transform growth factor beta (TGF-b) and interleukin 10 (IL-10) (Budoni et al., 2013; Özdemir et al., 2016). Due to these unique properties, MSCs are clinically used in the treatment of graft versus host disease (GVHD) caused by uncontrolled activation of immune cells (Sangiorgi and Panepucci, 2016) and certain autoimmune diseases, including rheumatoid arthritis (RA), Crohn’s disease, and systemic lupus erythematosus (SLE) (Dazzi and Krampera, 2011). However, the clinical responses of patients to MSC treatment are variable, ranging from good responses to only temporary or no effect (Mastri et al., 2014; Silva et al., 2018). The immunomodulatory effects of MSCs occur in a non-specific and non-selective manner. When MSCs are activated, they produce certain cytokines, such as PGE2, IDO, HGF, TGF-b and IL-10, which suppress almost all immune cells (El, 2011; Özdemir et al., 2016; Cho et al., 2014). However, this suppressive effect only lasts for the lifespan of MSCs. In both pathogen-related infections and autoimmune pathologies, antigen presentation is a crucial step for T cell activation and lineage specific differentiation. During T cell activation, antigen-specific memory cells are formed, resulting in a life-long response (Berard and Tough, 2002; Gray et al., 1991). To gain a sustainable immune response, T cells should be activated or inhibited by antigen-presenting cells. MSCs are not antigen-presenting cells, and under normal conditions, their major histocompatibility antigen expressions (MHC) are either weak or absent (Dominici et al., 2006; Shi et al., 2018).
Macrophages are a part of innate immunity, and they play important roles in the antigen presentation and the regulation of immune response. According to the exposed type of cytokine and antigen, macrophages can alter their phenotype and function. It has been shown that IFN-g, LPS and TNF-a stimulation leads to the upregulation of MHC-II, CD80 and CD64 expressions of the cell surface and an increase in iNOS, IL-1b, IL-12 and IL-6 production of macrophages. This type of macrophages is called M1, which activate Th1 immune cells important to the immune response of intracellular pathogens and tumor resistance (Ambarus et al., 2012; Martinez and Gordon, 2014). Another macrophage group, called M2 macrophages, antagonize the effects of M1 macrophages. M2 macrophages are further divided into the subgroups of M2a, M2b and M2c according to cytokine and antigen stimulation. IL-4 stimulation is specific to the development of the M2a macrophage phenotype. Through IL-4 stimulation, the cell surface expressions of CD200R and CD206 increase but CD14 decreases. Furthermore, the production of Arginase and IL-10 increases (Ambarus et al., 2012; Van Dyken and Locksley, 2013). M2a macrophages are important for the activation of Th2 cells responsible for immune responses, including encapsulation of parasites and allergy (Martinez and Gordon, 2014; Martinez et al., 2009). For the emergence of the M2b phenotype, immune complexes and TLR stimulation are required. An appropriate stimulation would increase the IL-10 production of M2b cells but decrease IL-12 production (Anderson and Mosser, 2002; Sironi et al., 2006). M2c is another subset of M2 macrophages, which are activated by IL-10 stimulation. An increase in the CD163 and CD16 expressions and upregulation of IL-10 and TGF-b production caused by IL-10 stimuli, are specific to the M2c phenotype (Ambarus et al., 2012; Schwarz et al., 2013).
In the current literature, there are several studies showing that MSCs could inhibit pro-inflammatory M1 macrophages and stimulate anti-inflammatory M2 macrophages (Cho et al., 2014; Vasandan et al., 2016). However, it has not been yet fully clarified whether these differentiated macrophages are functional. As a professional antigen-presenting cell, te macrophages can help to transfer the immunomodulation effects of MSCs to the adaptive immune cells. In this study, we aimed to investigate the interactions of macrophage and MSCs, and the resulting effects of these interactions on CD4 T cells. For this purpose, we differentiated the macrophage cells into M1, M2a and M2c phenotypes to observe the effects on CD4 T cells with known macrophage phenotypes. In addition, we generated MSC-educated macrophage (MEM) cells by direct and indirect co-culture and compared their effects on CD4 T cells with known macrophage phenotypes.
2. Material and methods
The protocol, sample collection procedures and informed consent form of this study were approved by Ethical committee of Ege University (16-5.2/1). To perform cell culture experiments, after informed consent blood samples collected from three female (23, 36 and 37 age) and three male (24, 27 and 39 age) healthy volunteers. Peripheral blood mononuclear cells (PBMCs) were isolated by using density centrifugation (Ficoll-Paque) method.
2.1. Cell culture
Human adipose tissue derived MSCs (PCS-500-011™) were purchased from American Type Culture Collection (ATCC). Frozen cells were thawed in 37 °C and cultured by using DMEM-F12 (Biosera, USA) medium that including 10% fetal bovine serum (FBS) (Biosera, USA), 100 U/ml penicillin, 100 μg/ml streptomycin (Biosera, USA) and 1% 2 mM L-glutamate (Biosera, USA) at 37 °C and %5 CO2 incubator. Cells were controlled daily, and sub cultured when they reached 70–80 % confluence. 3th passage MSCs were used to perform co-culture experiments.
To obtain macrophage cells from PBMCs, the cells of each subjects were cultured by using RPMI 1640 (Biosera, USA) medium that including 10% fetal bovine serum (FBS) (Biosera, USA), 100 U/ml penicillin, 100 μg/ml streptomycin (Biosera, USA) and 1% 2 mM L-glutamate (Biosera, USA) at 37 °C and %5 CO2 incubator for 4 h. After the culture period, non-adherent cells were washed with phosphate-buffered saline (PBS) and cultured in different culture plate by using RPMI 1640 complete medium and 10 ng/ml human IL-2 (Reprokine Ltd, Israel) till to co-culture experiments. Adherent cells were detached by Trypsin-EDTA (Biosera, USA) and divided as 3 × 105 cells per well in two 6 well plates. Cells were cultured by using RPMI 1640 complete medium and human 25 ng/ml macrophage colony-stimulating factor (M-CSF) (Reprokine Ltd, Israel) at 37 °C and %5 CO2 incubator for 4 days.
After the culture period, to stimulation of M1 macrophage phenotype different wells of each plates were cultured with RPMI 1640 complete medium and 50 ng/ml IFN-g (Reprokine Ltd, Israel), 50 ng/ml TNF-a (Reprokine Ltd, Israel) and 50 ng/ml GM-CSF (Reprokine Ltd, Israel), to M2a phenotype 50 ng/ml IL-4 (Reprokine Ltd, Israel) and to M2c 50 ng/ml IL-10 (Reprokine Ltd, Israel) and 50 ng/ml TGF-b1 (Reprokine Ltd, Israel). To generate the MSC educated macrophages (MEM), cells were direct co-cultured with 1 × 105 (Dazzi and Krampera, 2011) MSCs (MEM-D) and indirect by using 0.4 μm pore sized inserts (MEM-ID) and added 25 ng/ml M-CSF and 25 ng/ml GM-CSF. One well of each plate were remained as unstimulated control cells. All cells cultured at 37 °C and %5 CO2 incubator for 3 days. Then, the cells of first plate were used to evaluation of phenotype changes of macrophages by FACS analyses. The other plate was used to co-culture experiments.
To compare of immunomodulatory effects of MEM-D and MEM-ID cells on CD4 T cells with known macrophage phenotypes, co-culture experiments were performed by using PBMCs. Before adding the PBMC, transwell cultured MSCs in the MEM-ID group were removed. PBMCs of each donor were activated by 50 ng/ml IL-2 and 37.5 μL Dynabeads Human T-Activator CD3/CD28 (Thermo Scientific, USA). Than 1× 105 (Mastri et al., 2014) activated PBMCs were added in all different macrophage phenotypes. In different 6 well plate, same amount of activated PBMCs were co-cultured with AD-MSCs only and cultured only as activated control. To evaluation unstimulated control group, 1× 105 (Mastri et al., 2014) unstimulated PBMCs were cultured in different well. All cells cultured at 37 °C and %5 CO2 incubator for 3 days.
2.2. FACS analyses
Ambarus et al. have systematically validated the specific markers that change in response to macrophage polarization (Ambarus et al., 2012). They have showed that CD80 and CD64 expressions of macrophages increased with IFN-g stimulation. They have demonstrated that CD14 expression of IL-4-stimulated macrophages decreased, but that CD200R expressions were specifically increased. Finally, they have reported a specific increase in CD163 in IL-10-stimulated macrophages. In our study, we performed FACS analyses by using CD14 FITC, CD64 PE, CD80 PE-Cy5, CD163 PerCP.Cy5.5 and CD200R PE (Biolegend, USA) antibody staining to evaluation of phenotypic changes of macrophage cells. To evaluation of changes of CD4 T cells CD4 FITC, IFN-g PE, IL-4 PE, IL-17a PE (Diaclone, France) and FoxP3 (Biolegend, USA) antibody staining were performed. All measurements were performed with BD Accuri C5 flow cytometry device (BD Biosicience, USA) and all analyses were performed by using FlowJo v10 software (Becton, Dickinson & Company, USA).
2.3. Luminex analyses
To evaluation of effects of different macrophage phenotypes on inflammatory cytokines IL-1b, IL-4, IL-10, IL-12p70, IL-17a and IFN-g levels were measured by using Luminex Kit (Thermo Fisher Scientific, USA). All measurements were performed with LUMINEX 200™ device (Merck Millipore, USA) that calibrated xPonent 3.1 compatible Calibration Kit (EMD Millipore Cat. # 40–275) and Verification Kit (EMD Millipore Cat. # 40–276). Obtained signal densities were evaluated with xPotent 3.1 software (Merck Millipore, USA). Median Fluorescence Intensity (MFI) data of each sample were calculated by 5-parameter logistic spline curve-fitting method and cytokine concentrations were determined.
2.4. Cell proliferation and apoptosis assays
To observe the effect of different macrophage phenotypes on proliferation, we performed WST-1 (Roche, Germany) analysis. 1 × 104 cells of each macrophage phenotype and AD-MSCs were seeded a 96 well plate and cultured for 4 h to adhesion of plate surface. Than 4 × 105 (Dazzi and Krampera, 2011) activated PBMCs were added on these cells. As control, 4 × 105 (Dazzi and Krampera, 2011) activated and unstimulated PBMCs only were seeded different wells. All cells cultured at 37 °C and %5 CO2 incubator for 24 h. After the culture period, 20 μL WST-1 solution was added to each well and cultured for 2 h. Absorbance changes were measured at a wavelength of 480 nm with the multi-plate reader Versamax (Sunnyvale, CA, USA). The CD69 surface expressions, which is activation marker of lymphocytes, were analyzed by flow-cytometry to observe activation status of pre-co-culture T cells. For this, pre-activated and activated T cells were stained with CD4 FITC and CD69 PE labeled antibodies and analyzed on BD Accuri C5 device. To assess the apoptosis status of the cells, Caspase-3 levels from the media supernatants which collected after co-culture were analyzed using the ELISA kit (MyBioSource, USA).
2.5. Statistic
Data obtained from all experiments were evaluated as mean ± SD and were analyzed by using SPSS v23 (IBM, USA). To finding statistical differences of all groups, the One-Way ANOVA test was used, and according to Levene statistic results the Tukey HSD or Dunnett T3 post-hoc test results were used. The difference between the groups was considered statistically significant when p < 0.05. To performing graphical charts of statistical results, the Prism v.7 software (GraphPad, USA) were used.
3. Results
3.1. Macrophage culture and phenotype analyses
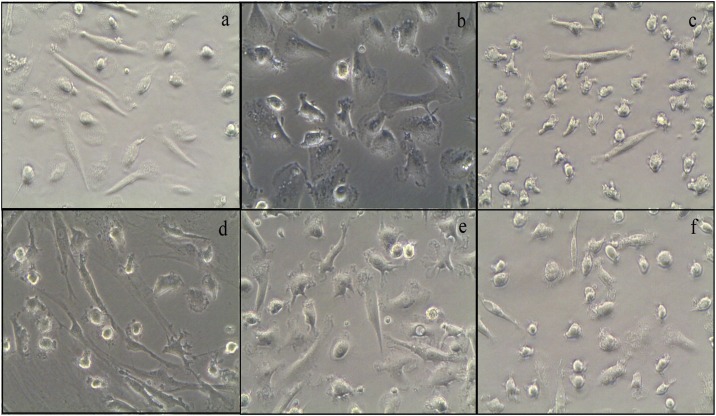
To observe the effects of macrophage and MSC interactions on phenotype, we generated unstimulated (US), M1, M2a and M2c macrophages cells via specific cytokine stimulations, and then compared the phenotypes of each cell type. In microscopic examinations, we observed that M1 and M2c macrophages were predominantly spindle-shaped, whereas M2a, MEM-D and MEM-ID macrophages were round cells with dendritic extensions. The microscopic images of each macrophage phenotype are shown in Fig. 1 .
Fig. 1.
The microscopic images of M1 (a), M2a (b), M2c (c), MEM-D (d), MEM-ID (e) and unstimulated macrophages (US-M). The cells in spindle morphology were observed more intensely in macrophages stimulated with IFN-g (a) and IL-10 (c). The morphology of the macrophages that stimulated with IL-4 (b) and direct (d) or indirect (e) cultured with MSCs was in the form of a round and dendritic extension.
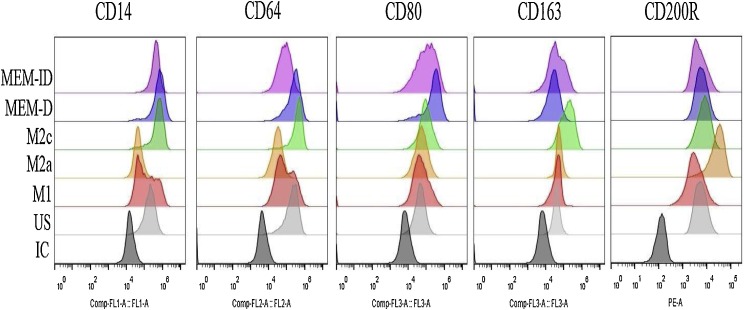
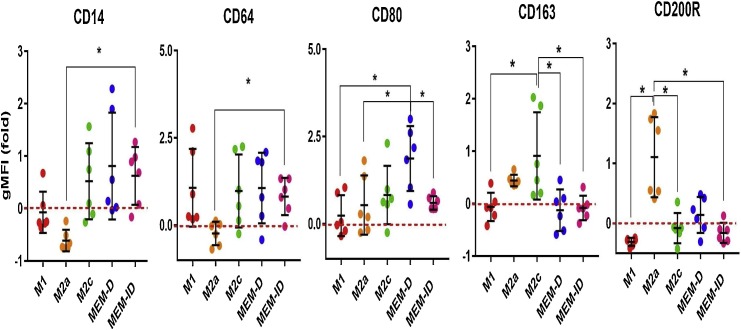
We then analyzed the changes in CD14, CD64, CD80, CD163 and CD200R molecules to evaluate the macrophage phenotypes. To minimize the differences due to biological variations and inter-assay biases, we used the fold of geometric median fluorescence intensity (gMFIfold) values obtained from the gMFI values of stimulated (S) and unstimulated (US) macrophages [gMFIfold=(S-gMFI/US-gMFI)-1]. The histogram plots obtained from FACS analyses are presented in Fig. 2 , and the comparison of the gMFIfold values of the groups is given in Fig. 3 .
Fig. 2.
The histogram plots of FACS analyses of CD14, CD64, CD80, CD163 and CD200R markers. IC: isotype control, US: unstimulated macrophage, MEM: MSC educated macrophage, D: direct cultured, ID: indirect cultured.
Fig. 3.
The comparative chats of CD14, CD64, CD80, CD163 and CD200R expressions (gMFI fold) of macrophages. The red dashed line represents US macrophage gMFI values. Data are presented as mean ± SD (standard deviation). (*= statistically significant p < 0.05). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
In our experiments, the CD14 expression of the M1 and M2a cells was lower than that of the US—M cells, but this was not statistically significant. Even if the CD14 expressions of the M2c, MEM-D and MEM-ID groups were higher compared to the M1 and M2a groups, the difference was only significant between the M2a and MEM-ID groups. The CD64 expression was increased in all groups except M2a cells, and we found that the MEM-ID group had a significantly higher CD64 expression than the M2a group (Fig. 3). The highest and statistically significant CD80 expression was observed in the MEM-D group, and the CD80 levels of the M1 cells were almost similar to those of the US-M cells. The CD163 expressions of the M1, MEM-D and MEM-ID cells were significantly lower compared to the M2c cells. The CD200R expressions of M2a cells were significantly higher than those of the remaining groups, except the MEM-D group.
3.2. PBMC co-culture
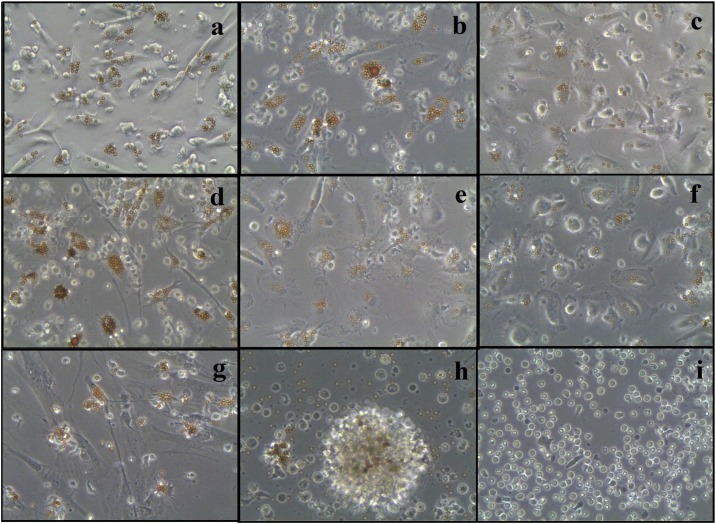
To observe the effects of the MEM cells on CD4 T cells, we performed co-culture experiments. Before the co-culture of PBMCs, we validated the activation status of lymphocytes. For this purpose, we labeled unstimulated and activated PBMCs by CD4 FITC and CD69PE antibodies and analyzed them using FACS. For all donors, we detected a significant increase in CD69 expression in activated PBMCs compared to the unstimulated PBMCs (Supplementary Fig-1). During the co-culture experiments, we observed differences in the interactions between cells. The T cells marked with CD3/CD28 beads were orange under a light microscope due to the deposition of iron on their surface. In the microscopic examinations, we found that T lymphocytes generated clusters similar to antigen presentation, and these clusters were more prominent in M2a and MEM-D cells (Fig. 4 ).
Fig. 4.
The microscopic images of co-cultured activated T cells with the M1 (a), M2a (b), M2c (c), MEM-D (d), MEM-ID (e), US-M (f) and MSCs (g). The microscopic images of activated PBMCs (h) and unstimulated PBMCs (i). The activated T cells (orange colored) have accumulated on the surface of macrophage cells, however these accumulations were detected as more dense at M2a and MEM-D co-culture groups compared with the US-M, M1 and M2c co-culture groups.
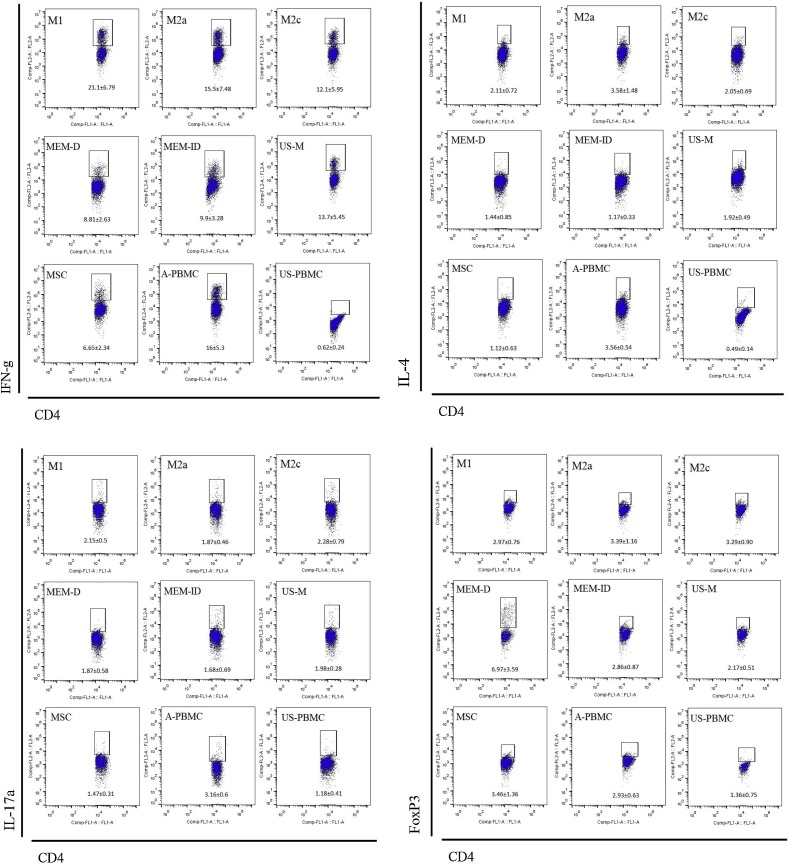
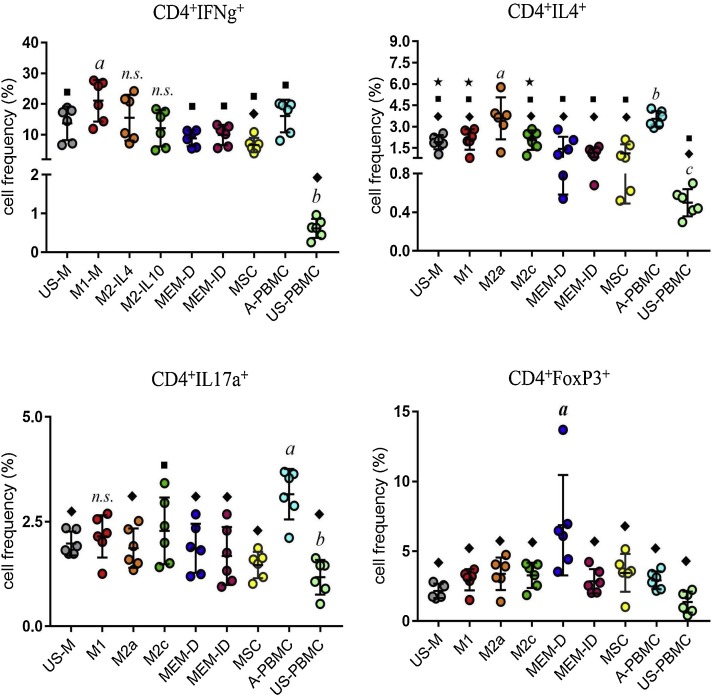
The changes in CD4 T cell subsets were evaluated by a FACS analysis and the dot-plot charts of each T cell subsets are given in Fig. 5 . The cell frequencies (%) are summarized in supplementary Table-1, and the comparison charts between the groups in Fig. 6 . The Th1 (CD4+IFNg+) cell frequencies of all groups, except the M2a and M2c groups, were significantly higher compared to the US-PBMC group. In addition, the Th1 frequencies of the M1 group was significantly higher than that of the MSC group. The Th2 (CD4+IL4+) cell frequencies of the M2a and A-PBMC groups were significantly higher compared to the remaining groups. This finding confirmed that M2a macrophages were more effective in inducing the Th2 subset, but it also showed that the MEM-D and MEM-ID cells might be as effective as MSCs in suppressing the Th2 cells. The frequencies of the Th17 (CD4+IL17a+) cells of all groups, except the M1 group, were significantly lower compared with the A-PBMC group. Unlike the other groups, the M2c group had a significantly higher Th17 frequency than the US-PBMC group. Lastly, we detected that the Treg (CD4+FoxP3+) cell frequencies of the MEM-D cells were significantly higher than the other groups. This finding suggested that the direct interaction of macrophages and MSCs might have led to a more effective increase in Treg cell levels.
Fig. 5.
The dot plot charts of CD4+IFNg+, CD4+IL4+, CD4+IL17a+ and CD4+FoxP3+ T cells of cultured with M1, M2a, M2c, MEM-D, MEM-ID US-M and MSCs.
Fig. 6.
The comparison charts of CD4+IFNg+, CD4+IL4+, CD4+IL17a+ and CD4+FoxP3+ T cell frequencies according to experiment groups. Data are presented as mean ± SD (standard deviation). There are significant differences (p < 0.05) between the “a” and the rhombus symbols, “b” and the square symbols, “c” and the star symbols.
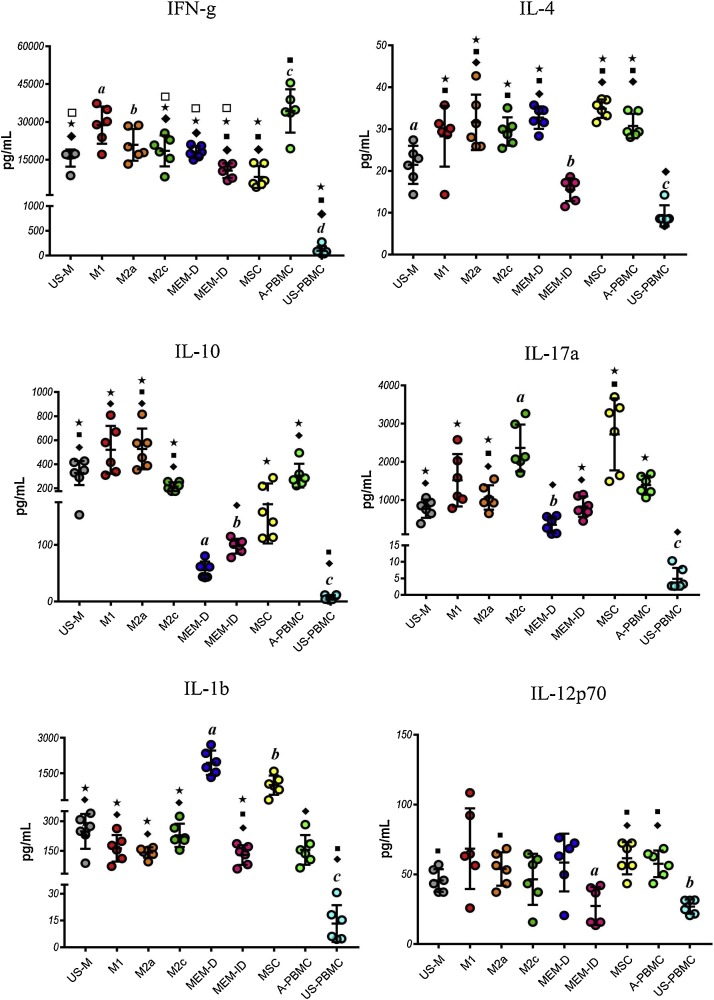
After the evaluation of phenotypic alterations of CD4 T cells, we evaluated the changes in inflammatory cytokines. The comparative charts of all cytokines are provided in Fig. 7 , and the results of all cytokines are shown in supplementary Table-2. The IFN-g levels of the M1 groups were significantly higher compared to all co-culture groups, except the M2a and A-PBMC groups. The IL-4 levels of the US-M and MEM-ID groups were significantly lower than those of the other groups (p < 0.05), except the US-PBMC group. The IL-10 levels of all groups were significantly higher compared to the US-PBMC group. In addition, the IL-10 levels of the MEM-D group were significantly lower than all groups, except the MSC group. Similarly, the MEM-ID group had significantly lower IL-10 levels than the US-M, M2a and M2c groups. The IL-17a levels of the US-PBMS group were significantly lower than those of the other groups, except the MEM-D group (p < 0.05), and the M2c group had significantly higher IL-17a levels than the US-M, M2a, MEM-D and MEM-ID groups. The IL-12p70 levels were similar in all groups, but they were significantly lower in the MEM-ID groups compared to the MSC and A-PBMC groups (p < 0.05). For IL-1b, surprisingly, the MEM-D and MSC groups had significantly higher levels compared with the remaining co-culture groups (p < 0.05).
Fig. 7.
The comparison charts of IFN-g, IL-1b, IL-4, IL-10, IL-12p70 and IL-17a cytokine levels according to experiment groups. Data are presented as mean ± SD (standard deviation). There are significant differences (p < 0.05) between the “a” and the rhombus symbols, “b” and the square symbols, “c” and the star symbols, “d” and empty square symbols.
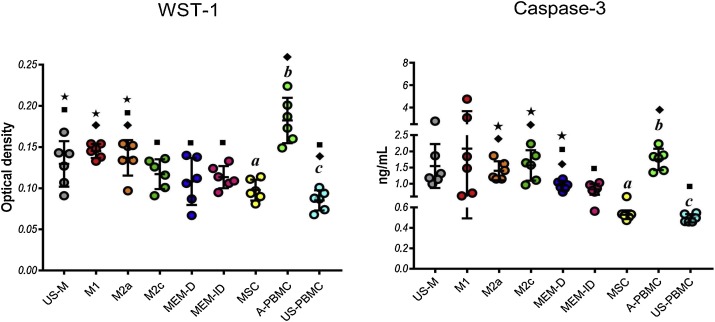
To compare the effects of all macrophage phenotypes on lymphocyte proliferation and apoptosis, we performed WST-1 analyses. The comparative charts of all WST-1 and Caspase-3 results are summarized in Fig. 8 and all results are given in supplementary Table-3. The optical densities (ODs) of the activated PBMC groups were significantly higher than those of the co-culture groups, except the M1 group. In the other hand, the ODs of the unstimulated PBMC groups were significantly lower compared to the US-M, M1 and M2a groups. In addition, the ODs of the MSC group were significantly lower than those of the US-M, M1 and M2a groups. To evaluate apoptosis, we performed Caspase-3 ELISA analyses. The Caspase-3 levels of the MSC and US-PBMSC groups were significantly lower than those of the M2a, M2c, MEM-D and A-PBMC groups.
Fig. 8.
The comparison chart of WST-1 optical densities, and Caspase-3 levels of medium supernatants of each group. Data are presented as mean ± SD (standard deviation). There are significant differences (p < 0.05) between the “a” and the rhombus symbols, “b” and the square symbols, “c” and the star symbols.
4. Conclusions
In this study, we evaluated macrophage polarizations by identifying several distinctive markers for M1, M2a and M2c macrophage phenotypes (Fig. 3). One of the markers evaluated was CD14, which is a specific marker of monocytes with reduced expression during macrophage maturation (Ambarus et al., 2012). It is well known that MSCs are IL-10-producing cells (Ma et al., 2016; Qu et al., 2012), and it has been shown that their maturation can be prevented by IL-10 (Schwarz et al., 2013; Allavena et al., 1998). We observed that the CD14 expressions of the MEM-D and MEM-ID groups showed a similar pattern to the M2c group, suggesting that MSCs can differentiate macrophage cells into the M2c-like phenotype through direct or indirect effects. CD64 is a member of the Fcγ family and plays a role in antibody-mediated phagocytosis. It has been reported that CD64 expression in monocytes and macrophages increases in response to IFN-g and LPS stimulation but decreases with IL-4 stimulation (Hristodorov et al., 2015). In another study, Ji et al. showed that the CD64 expression of macrophages increased by M-CSF and IL-10 stimulation (Ji et al., 2004). For CD64, our findings were similar to the literature in that the CD64 expression of macrophages increased in the M1 and M2c group but decreased in the M2a group. Additionally, the CD64 expressions of the MEM-D and MEM-ID macrophages were similar to those of the M1 and M2c macrophages. As in the case of CD14 expressions, this finding supports the idea MSCs may alter macrophages into the M2c-like phenotype. CD80 is a molecule involved in the full activation of T cells by interacting with the CD28 co-stimulatory molecule of T cells during antigen presentation (Freeman et al., 1992). Jiang et al. reported that the CD80 expressions of LPS-stimulated macrophages were suppressed by MSCs; however, Spaggiari et al. reported no change (Jiang et al., 2005; Spaggiari et al., 2009). In our experiments, we observed that the CD80 expressions of the MEM-D group were significantly higher compared to the other groups, except M2c. As shown in Fig. 4, clusters where T cells interacted, indicating antigen presentation were more common in the MEM-D group than in the other groups. These observations suggest that the co-stimulatory properties of macrophages could be increased by the presence of MSCs.
CD163 is a scavenger receptor, the expression of which is increased by macrophages in response to IL-10 and TGF-b stimulation, but it is antagonized by IFN-g and IL-4 stimulation (Fabriek et al., 2005). In this respect, CD163 is a sensitive marker for M2c macrophages, and we found that the CD163 expressions of the M2c macrophages significantly increased compared to the other groups. Based on CD14 and CD64 expressions observed, we assumed that IL-10 produced by MSCs might differentiate macrophages into the M2c-like phenotype. However, the absence of a CD163 increase in the MEM-D and MEM-ID groups did not support this assumption. Finally, we found that CD200R, a specific marker for M2a cells, decreased in M1 macrophages and increased in M2a macrophages, which is consistent with the literature. We also observed that similar to CD163, the CD200R expressions of the MEM-D and MEM-ID macrophages were not altered compared to US-M. Not only IL-10, IL-4 and TGF-b, but also various immunosuppressive molecules, such as IDO, HGF, and PGE2 are known to be involved in the formation of immunomodulation effects of MSCs (Chen et al., 2011). Therefore, macrophages cultured with MSCs are likely to be of a different phenotype than known phenotypes, which is also partially supported by our findings. We used limited and specific markers to evaluate the macrophage phenotypes; therefore, based on limited data, we were not able to make a definitive conclusion concerning the phenotype to which the macrophages cultured with MSCs were closest.
In this study, we focused on the functional comparison of the immunomodulatory effects of MEM-D and MEM-ID cells on CD4 T cells. Th1 cells, with the main cytokines of IFN-g and IL-2, orchestrate the elimination of intracellular pathogens (Boehm et al., 1997), and they are related to certain organ-specific autoimmune pathologies, such as Type I diabetes (Luckheeram et al., 2012). In terms of macrophages, M1 macrophages stimulate the differentiation of naive T cells into the Th1 phenotype. In contrast, M2 macrophages stimulate Th2 and/or Treg cell differentiation and suppress Th1 differentiation (Martinez and Gordon, 2014; Charles A Janeway et al., 2001; Mills et al., 2000). Previous research also reported that MSCs suppressed the Th1 response and stimulated Treg cells (Chen et al., 2011; Luz-Crawford et al., 2013). According to our findings, the CD4+ IFNg+ (Th1) frequencies of all groups were similar, except the US-PBMC group. However, there were dramatic and significant decreases in the IFN-g levels of the M2c, MEM-D, MEM-ID and MSC groups. This finding suggests that the CD4+ IFNg+ cell frequencies may not be affected by different macrophage phenotypes, but their functions can be suppressed by M2c, MEM and MSC cells.
Th2 cells orchestrate the immune response to extracellular parasites, and they are associated with asthma and allergic disorders. The main cytokines of Th2 cells are IL-4, IL-5, IL-13, and IL-10 (Deo et al., 2010; Steinke and Borish, 2001). The presence of a synergistic interaction between the Th2 cells and M2 macrophages has previously been reported (Muraille et al., 2014). Our data confirmed that IL-4 stimulated macrophages (M2a) could significantly stimulate Th2 frequencies and IL-4 production. However, although the Th2 frequencies of the groups except M2a were close to each other, the IL-4 levels of the US-M and MEM-ID groups were significantly lower than those of the other groups. In the current literature, different results have been reported about MSC and Th2 interactions. Mareschi et al. found that amniotic fluid MSCs and placenta MSCs could stimulate the IL-4 expressions of activated PBMCs, but not in bone marrow MSCs (Mareschi et al., 2015). Özdemir et al. and Genç et al. showed that dental tissue MSCs could suppress the IL-4 expressions of T cells (Özdemir et al., 2016; Genç et al., 2018). In our experiments, we used adipose tissue MSCs and observed that the IL-4 levels significantly increased in the MSC and MEM-D groups compared with the MEM-ID and US-PBMC groups. The similarity we observed in US-M and MEM-ID for IL-4 levels may indicate that MSCs may have forced the macrophages to remain in an unstimulated form when there was no direct interaction.
Th17 cells have been reported to play a role in the pathogenesis of many autoimmune diseases; e.g., RA, SLE and Crohn's disease (Tabarkiewicz et al., 2015). As opposed to Th1 and Th2 cells that are terminally differentiated, Th17 cells can alter their phenotype in response to signals from the environment. For example, Bofeng et al. reported that IL-10 induced macrophages contributed to the pathogenesis of colitis by increasing Th17 activity (Li et al., 2015a). Haribhai et al. showed that TGF-b-producing M2a macrophages differentiated Th17 cells into anti-inflammatory iTreg cells (Haribhai et al., 2016). For MSCs and Th17 interactions, Qu et al. reported that Th17 cells were suppressed by IL-10 secreted by MSCs (Qu et al., 2012), Rozenberg et al. showed that PGE2 secreted from MSCs increased the Th17 response but suppressed the Th1 response (Rozenberg et al., 2016), and Ghannam et al. noted that MSCs increased Treg cells by suppressing Th17 cells (Ghannam et al., 2010). Our findings revealed that the Th17 frequencies of the A-PBMC group was significantly higher than those of the remaining groups, except M1 and M2c. The IL-17a levels and Th17 frequencies of the M1 and M2c groups were consistent, but IL-17a remained high in the MSC group (Fig. 7). According to our data, IL-10 induced macrophages may be important for stimulating both Th17 cell frequency and IL-17a production. However, even if there is no effect on Th17 frequencies, direct or indirect interaction of macrophages with MSCs may have a negative effect on IL-17a production.
Treg cells are important since they are responsible for the suppression of the immune system and tolerance to self-antigens. Activation of FoxP3, a specific transcription factor of these cells, leads to the secretion of suppressive cytokines, such as IL-10 and TGF-b (Li et al., 2015b). A co-inhibitor molecule CTLA-4 is highly expressed on Treg cells and interacts with CD80/CD86 molecules, leading to the secretion of IDO from antigen-presenting cells (Oderup et al., 2006). Schmidt et al. reported that M2 macrophages stabilized the FoxP3 expression of CD4 T cells, and in this way, led to a decrease in IFN-g and IL-17 production (Schmidt et al., 2016). Similar to M2 macrophages, MSCs have a positive effect on the activation of Treg cells. Gazdic et al. showed that the interaction between MSCs and Treg cells played an important role in improving acute liver injury in mouse models (Gazdic et al., 2018). Ozdemir et al. suggested that dental pulp MSCs increased the Treg cell ratio, probably due to the phenotypic shift of Th17 cells to Treg cells (Özdemir et al., 2016). In our study, the Treg cell frequencies were significantly higher in the MEM-D group than in the other groups. However, the IL-10 levels of the MEM-D group were significantly lower compared to the other groups, except the MSC group. We reviewed the literature to interpret this finding and found studies showing that over-activated Th1, Th2 and even Th17 cells could produce IL-10 to manage this activation (Maynard and Weaver, 2008; O’Garra and Vieira, 2007; Ye et al., 2007). It has been reported that the Borrelia burgdorferi and Toxoplasma gondii infections lead to an increase in IFNg+IL-10+ cells (O’Garra and Vieira, 2007). Another interesting study reported that over-activated virus-specific CD8+ T cells could produce IL-10 in coronavirus infection, and these cells were shown to produce higher levels of pro-inflammatory cytokines and cytotoxic proteins than other cells (Maynard and Weaver, 2008). If we try to interpret our data according to the information in the literature, the direct interaction of MSCs and macrophage cells may increase the frequency of Treg cells even more than the other macrophage phenotypes, and even MSCs themselves. Furthermore, overactivation of T cells may be the cause of elevated IL-10 in the US-M, M1, M2a and A-PBMC groups. As a result, MEM-D, MEM-ID and MSCs may have led to a decrease in IL-10 production due to their potent inhibitory effects on T cell activation.
Netea et al. and Quintin et al. reported that macrophages could develop a memory by being educated against a situation they had previously encountered (Netea, 2013; Quintin et al., 2014). Interestingly, we observed that the MEM-ID cells had similar effects on the Th1, Th2, Th17, and Treg cell frequencies as MEM-D cells. Besides, these effects were similar for the IFN-g, IL-10 and IL-17a levels. This suggests that macrophage and MSC interactions may cause a kind of memory formation in macrophage cells. In addition, this memory appears to develop in a suppressive direction for all T cell cytokine responses.
We performed a WST-1 analysis to observe the changes in proliferation of T cells as a result of activation. It is known that M2 macrophages can suppress T cell proliferation via secretion of NO and IDO or surface molecule PD-L2 (Bingisser et al., 1998; Huber et al., 2010; Munn et al., 1999). MSCs can also effectively suppress T cell proliferation via cytokines, such as IDO, PGE2, IL-10, and TGF-b (Chen et al., 2011). According to our findings, consistent with the literature, the proliferation rates of all co-culture groups, except M1 macrophages, were significantly lower than those of the A-PBMC group, and the proliferation rates of the M1 and M2a group were significantly higher compared to the MSC group. These data suggest that macrophages may not be as effective as MSCs in suppressing T cell proliferation. It is also known that macrophages can lead to over-activated T cell apoptosis by secretion of NO and by Fas/FasL mechanism in acute bacterial infections or IFN-g and LPS stimulation (Daigneault et al., 2012; Hortelano et al., 2000). However, MSCs do not cause lymphocyte apoptosis while suppressing proliferation (Haddad and Saldanha-Araujo, 2014; Xu et al., 2007). We observed that the Caspase-3 levels were significantly higher in M1 macrophages than in the MEM-ID, MSC and US-PBMC groups, confirming that MSCs can successfully suppress T cell proliferation, but does not lead to apoptosis.
Overall, our data revealed that MSC and macrophage interactions may lead to the formation of a different phenotype than the known macrophage phenotypes. Although this phenotype was closer to the M2c phenotype, it cannot be considered a M2c cell due to the low expression of CD163, which is the characteristic marker of M2c. While MEM-D, MEM-ID, and MSCs had similar inhibitory effects on Th2 and Th17 cells, the most significant increase in Treg cell frequencies was seen in MEM-D cells. Macrophages can alter their phenotypes and functions according to the stimuli from the environment. The fact that macrophages educated with MSCs suppressed the production of all the cytokines evaluated even after the removal of MSCs suggests that these cells may be differentiated by MSCs into a suppressive macrophage subgroup. However, Treg cell activation caused by direct interactions between MSC and macrophage cells may be the most prominent observation of this study. In conclusion, according to our data, interactions of MSCs and macrophages may lead to differentiate macrophage cells into an immunosuppressive phenotype, and these macrophages may suppress T lymphocyte subgroups at least as effectively as MSCs. However, considering that we obtained our data from in vitro experiments, our findings should be supported by future in vivo studies.
Declaration of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The Scientific and Technological Research Council of Turkey (TUBITAK) supported the project for this study, whose reference number is 216 S 761.
Acknowledgement
The Scientific and Technological Research Council of Turkey (TUBITAK)2 supported the project for this study, whose reference number is 216 S 761.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.imbio.2019.04.002.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- Allavena P., Piemonti L., Longoni D., Bernasconi S., Stoppacciaro A., Ruco L., et al. IL-10 prevents the differentiation of monocytes to dendritic cells but promotes their maturation to macrophages. Eur. J. Immunol. 1998;28(January (1)):359–369. doi: 10.1002/(SICI)1521-4141(199801)28:01<359::AID-IMMU359>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- Ambarus C.A., Krausz S., van Eijk M., Hamann J., TRDJ Radstake, Reedquist K.A., et al. Systematic validation of specific phenotypic markers for in vitro polarized human macrophages. J. Immunol. Methods. 2012;375(January (1–2)):196–206. doi: 10.1016/j.jim.2011.10.013. [DOI] [PubMed] [Google Scholar]
- Anderson C.F., Mosser D.M. A novel phenotype for an activated macrophage: the type 2 activated macrophage. J. Leukoc. Biol. 2002;72(July (1)):101–106. [PubMed] [Google Scholar]
- Berard M., Tough D.F. Qualitative differences between naïve and memory T cells. Immunology. 2002;106(June (2)):127–138. doi: 10.1046/j.1365-2567.2002.01447.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingisser R.M., Tilbrook P.A., Holt P.G., Kees U.R. Macrophage-derived nitric oxide regulates t cell activation via reversible disruption of the Jak3/STAT5 signaling pathway. J. Immunol. 1998;160(June (12)):5729–5734. [PubMed] [Google Scholar]
- Boehm U., Klamp T., Groot M., Howard J.C. Cellular responses to interferon-gamma. Annu. Rev. Immunol. 1997;15:749–795. doi: 10.1146/annurev.immunol.15.1.749. [DOI] [PubMed] [Google Scholar]
- Budoni M., Fierabracci A., Luciano R., Petrini S., Di Ciommo V., Muraca M. The immunosuppressive effect of mesenchymal stromal cells on B lymphocytes is mediated by membrane vesicles. Cell Transplant. 2013;22(2):369–379. doi: 10.3727/096368911X582769. [DOI] [PubMed] [Google Scholar]
- Charles A Janeway J., Travers P., Walport M., Shlomchik M.J. Macrophage activation by armed CD4 TH1 cells. Immunobiol. Immune Syst. Health Dis. 2001 https://www.ncbi.nlm.nih.gov/books/NBK27153/ 5th edition [Internet]. [cited 2018 Oct 22]; Available from: [Google Scholar]
- Chen P.-M., Yen M.-L., Liu K.-J., Sytwu H.-K., Yen B.-L. Immunomodulatory properties of human adult and fetal multipotent mesenchymal stem cells. J. Biomed. Sci. 2011;18(July (1)):49. doi: 10.1186/1423-0127-18-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho D.-I., Kim M.R., Jeong H., Jeong H.C., Jeong M.H., Yoon S.H., et al. Mesenchymal stem cells reciprocally regulate the M1/M2 balance in mouse bone marrow-derived macrophages. Exp. Mol. Med. 2014;46(January (1)):e70. doi: 10.1038/emm.2013.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daigneault M., Silva T.I.D., Bewley M.A., Preston J.A., Marriott H.M., Mitchell A.M., et al. Monocytes regulate the mechanism of T-cell death by inducing fas-mediated apoptosis during bacterial infection. PLoS Pathog. 2012;8(July (7)) doi: 10.1371/journal.ppat.1002814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dazzi F., Krampera M. Mesenchymal stem cells and autoimmune diseases. Best Pract. Res. Clin. Haematol. 2011;24(March (1)):49–57. doi: 10.1016/j.beha.2011.01.002. [DOI] [PubMed] [Google Scholar]
- Deo S.S., Mistry K.J., Kakade A.M., Niphadkar P.V. Role played by Th2 type cytokines in IgE mediated allergy and asthma. Lung India. 2010;27(2):66–71. doi: 10.4103/0970-2113.63609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominici M., Le Blanc K., Mueller I., Slaper-Cortenbach I., Marini F., Krause D., et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315–317. doi: 10.1080/14653240600855905. [DOI] [PubMed] [Google Scholar]
- El N. In: Stem Cells in Clinic and Research. Gholamrezanezhad A., editor. 2011. Mesenchymal stem cells: immunology and therapeutic benefits.http://www.intechopen.com/books/stem-cells-in-clinic-and-research/mesenchymal-stem-cells-immunology-and-therapeutic-benefits [Internet]. InTech; [cited 2013 Dec 3]. Available from: [Google Scholar]
- Fabriek B.O., Dijkstra C.D., van den Berg T.K. The macrophage scavenger receptor CD163. Immunobiology. 2005;210(August (2)):153–160. doi: 10.1016/j.imbio.2005.05.010. [DOI] [PubMed] [Google Scholar]
- Freeman G.J., Disteche C.M., Gribben J.G., Adler D.A., Freedman A.S., Dougery J., et al. The gene for B7, a costimulatory signal for T-cell activation, maps to chromosomal region 3q13.3-3q21. Blood. 1992;79(January (2)):489–494. [PubMed] [Google Scholar]
- Gazdic M., Markovic B.S., Arsenijevic A., Jovicic N., Acovic A., Harrell C.R., et al. Crosstalk between mesenchymal stem cells and T regulatory cells is crucially important for the attenuation of acute liver injury. Liver Transpl. 2018;24(5):687–702. doi: 10.1002/lt.25049. [DOI] [PubMed] [Google Scholar]
- Genç D., Zibandeh N., Nain E., Gökalp M., Özen A.O., Göker M.K., et al. Dental follicle mesenchymal stem cells down-regulate Th2-mediated immune response in asthmatic patients mononuclear cells. Clin. Exp. Allergy. 2018;48(June (6)):663–678. doi: 10.1111/cea.13126. [DOI] [PubMed] [Google Scholar]
- Ghannam S., Pène J., Torcy-Moquet G., Jorgensen C., Yssel H. Mesenchymal stem cells inhibit human Th17 cell differentiation and function and induce a T regulatory cell phenotype. J. Immunol. 2010;185(July (1)):302–312. doi: 10.4049/jimmunol.0902007. [DOI] [PubMed] [Google Scholar]
- Gray D., Kosco M., Stockinger B. Novel pathways of antigen presentation for the maintenance of memory. Int. Immunol. 1991;3(February (2)):141–148. doi: 10.1093/intimm/3.2.141. [DOI] [PubMed] [Google Scholar]
- Haddad R., Saldanha-Araujo F. Mechanisms of T-Cell immunosuppression by mesenchymal stromal cells: what do we know so far? Biomed Res. Int. 2014 doi: 10.1155/2014/216806. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4082893/ [cited 2018 Oct 23];2014. [Internet]Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haribhai D., Ziegelbauer J., Williams C.B. TGF-β1 produced by alternatively activated macrophages synchronizes a tolerogenic iTreg-Th17 cell axis. J. Immunol. 2016;196(May (1 Supplement)) doi: 10.4049/jimmunol.1501956. 56.7-56.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hortelano S., Castrillo A., Alvarez A.M., Boscá L. Contribution of cyclopentenone prostaglandins to the resolution of inflammation through the potentiation of apoptosis in activated macrophages. J. Immunol. 2000;165(December (11)):6525–6531. doi: 10.4049/jimmunol.165.11.6525. [DOI] [PubMed] [Google Scholar]
- Hristodorov D., Mladenov R., von Felbert V., Huhn M., Fischer R., Barth S., et al. Targeting CD64 mediates elimination of M1 but not M2 macrophages in vitro and in cutaneous inflammation in mice and patient biopsies. MAbs. 2015;7(5):853–862. doi: 10.1080/19420862.2015.1066950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber S., Hoffmann R., Muskens F., Voehringer D. Alternatively activated macrophages inhibit T-cell proliferation by Stat6-dependent expression of PD-L2. Blood. 2010;116(October (17)):3311–3320. doi: 10.1182/blood-2010-02-271981. [DOI] [PubMed] [Google Scholar]
- Ji X.-H., Yao T., Qin J.-C., Wang S.-K., Wang H.-J., Yao K. Interaction between M-CSF and IL-10 on productions of IL-12 and IL-18 and expressions of CD14, CD23, and CD64 by human monocytes. Acta Pharmacol. Sin. 2004;25(October (10)):1361–1365. [PubMed] [Google Scholar]
- Jiang X.-X., Zhang Y., Liu B., Zhang S.-X., Wu Y., Yu X.-D., et al. Human mesenchymal stem cells inhibit differentiation and function of monocyte-derived dendritic cells. Blood. 2005;105(May (10)):4120–4126. doi: 10.1182/blood-2004-02-0586. [DOI] [PubMed] [Google Scholar]
- Li B., Gurung P., Malireddi R.K.S., Vogel P., Kanneganti T.-D., Geiger T.L. IL-10 engages macrophages to shift Th17 cytokine dependency and pathogenicity during T-cell-mediated colitis. Nat. Commun. 2015;21(January 6):6131. doi: 10.1038/ncomms7131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Li D., Tsun A., Li B. FOXP3+ regulatory T cells and their functional regulation. Cell. Mol. Immunol. 2015;12(September (5)):558–565. doi: 10.1038/cmi.2015.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luckheeram R.V., Zhou R., Verma A.D., Xia B. CD4+T cells: differentiation and functions. Clin. Dev. Immunol. 2012;2012 doi: 10.1155/2012/925135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luz-Crawford P., Kurte M., Bravo-Alegría J., Contreras R., Nova-Lamperti E., Tejedor G., et al. Mesenchymal stem cells generate a CD4+CD25+Foxp3+ regulatory T cell population during the differentiation process of Th1 and Th17 cells. Stem Cell Res. Ther. 2013;4(June (3)):65. doi: 10.1186/scrt216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma H.-C., Wang X., Wu M.-N., Zhao X., Yuan X.-W., Shi X.-L. Interleukin-10 contributes to therapeutic effect of mesenchymal stem cells for acute liver failure via signal transducer and activator of transcription 3 signaling pathway. Chin. Med. J. 2016;129(April (8)):967–975. doi: 10.4103/0366-6999.179794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mareschi K., Castiglia S., Sanavio F., Rustichelli D., Muraro M., Defedele D., et al. Immunoregulatory effects on T lymphocytes by human mesenchymal stromal cells isolated from bone marrow, amniotic fluid, and placenta. Exp. Hematol. 2015;(November 11) doi: 10.1016/j.exphem.2015.10.009. [DOI] [PubMed] [Google Scholar]
- Martinez F.O., Gordon S. 2014. The M1 and M2 Paradigm of Macrophage Activation: Time for Reassessment. F1000Prime Rep [Internet]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3944738/ Mar 3 [cited 2018 Oct 11];6. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez F.O., Helming L., Gordon S. Alternative activation of macrophages: an immunologic functional perspective. Annu. Rev. Immunol. 2009;27:451–483. doi: 10.1146/annurev.immunol.021908.132532. [DOI] [PubMed] [Google Scholar]
- Mastri M., Lin H., Lee T. Enhancing the efficacy of mesenchymal stem cell therapy. World J. Stem Cells. 2014;6(April (2)):82–93. doi: 10.4252/wjsc.v6.i2.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maynard C.L., Weaver C.T. Diversity in the contribution of IL-10 to T-cell-mediated immune regulation. Immunol. Rev. 2008;226(December):219–233. doi: 10.1111/j.1600-065X.2008.00711.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills C.D., Kincaid K., Alt J.M., Heilman M.J., Hill A.M. M-1/M-2 macrophages and the Th1/Th2 paradigm. J. Immunol. 2000;164(June (12)):6166–6173. doi: 10.4049/jimmunol.164.12.6166. [DOI] [PubMed] [Google Scholar]
- Munn D.H., Shafizadeh E., Attwood J.T., Bondarev I., Pashine A., Mellor A.L. Inhibition of t cell proliferation by macrophage tryptophan catabolism. J. Exp. Med. 1999;189(May (9)):1363–1372. doi: 10.1084/jem.189.9.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muraille E., Leo O., Moser M. Th1/Th2 paradigm extended: macrophage polarization as an unappreciated pathogen-driven escape mechanism? Front. Immunol. 2014;(November 26) doi: 10.3389/fimmu.2014.00603. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4244692/ [cited 2018 Dec 20];5. Available from: [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netea M.G. Training innate immunity: the changing concept of immunological memory in innate host defence. Eur. J. Clin. Invest. 2013;43(August (8)):881–884. doi: 10.1111/eci.12132. [DOI] [PubMed] [Google Scholar]
- O’Garra A., Vieira P. TH1 cells control themselves by producing interleukin-10. Nat. Rev. Immunol. 2007;7(June (6)):425–428. doi: 10.1038/nri2097. [DOI] [PubMed] [Google Scholar]
- Oderup C., Cederbom L., Makowska A., Cilio C.M., Ivars F. Cytotoxic T lymphocyte antigen-4-dependent down-modulation of costimulatory molecules on dendritic cells in CD4+ CD25+ regulatory T-cell-mediated suppression. Immunology. 2006;118(June (2)):240–249. doi: 10.1111/j.1365-2567.2006.02362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özdemir A.T., Özgül Özdemir R.B., Kırmaz C., Sarıboyacı A.E., Ünal Halbutoğlları Z.S., Özel C., et al. The paracrine immunomodulatory interactions between the human dental pulp derived mesenchymal stem cells and CD4 T cell subsets. Cell. Immunol. 2016;310:108–115. doi: 10.1016/j.cellimm.2016.08.008. [DOI] [PubMed] [Google Scholar]
- Qu X., Liu X., Cheng K., Yang R., Zhao R.C.H. Mesenchymal stem cells inhibit Th17 cell differentiation by IL-10 secretion. Exp. Hematol. 2012;40(September (9)):761–770. doi: 10.1016/j.exphem.2012.05.006. [DOI] [PubMed] [Google Scholar]
- Quintin J., Cheng S.-C., van der Meer J.W., Netea M.G. Innate immune memory: towards a better understanding of host defense mechanisms. Curr. Opin. Immunol. 2014;29(August):1–7. doi: 10.1016/j.coi.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Rozenberg A., Rezk A., Boivin M.-N., Darlington P.J., Nyirenda M., Li R., et al. Human mesenchymal stem cells impact Th17 and Th1 responses through a prostaglandin E2 and myeloid-dependent mechanism. Stem Cells Transl. Med. 2016;5(November (11)):1506–1514. doi: 10.5966/sctm.2015-0243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sangiorgi B., Panepucci R.A. Modulation of immunoregulatory properties of mesenchymal stromal cells by toll-like receptors: potential applications on GVHD. Stem Cells Int. 2016;21(September 2016) doi: 10.1155/2016/9434250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt C.S., Aranda Lopez P., Dopheide J.F., Schmidt F., Theobald M., Schild H., et al. Phenotypic and functional characterization of neutrophils and monocytes from patients with myelodysplastic syndrome by flow cytometry. Cell. Immunol. 2016;308(October):19–26. doi: 10.1016/j.cellimm.2016.07.005. [DOI] [PubMed] [Google Scholar]
- Schwarz A.M., Banning-Eichenseer U., Seidel K., Mauz-Körholz C., Körholz D., Staege M.S. Impact of Interleukin-10 on phenotype and gene expression during early monocyte differentiation into dendritic cells. Anticancer Res. 2013;33(January (11)):4791–4798. [PubMed] [Google Scholar]
- Shi Y., Wang Y., Li Q., Liu K., Hou J., Shao C., et al. Immunoregulatory mechanisms of mesenchymal stem and stromal cells in inflammatory diseases. Nat. Rev. Nephrol. 2018;14(August (8)):493–507. doi: 10.1038/s41581-018-0023-5. [DOI] [PubMed] [Google Scholar]
- Silva L.H.A., Antunes M.A., Dos Santos C.C., Weiss D.J., Cruz F.F., Rocco P.R.M. Strategies to improve the therapeutic effects of mesenchymal stromal cells in respiratory diseases. Stem Cell Res. Ther. 2018;9(February (1)):45. doi: 10.1186/s13287-018-0802-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sironi M., Martinez F.O., D’Ambrosio D., Gattorno M., Polentarutti N., Locati M., et al. Differential regulation of chemokine production by Fcgamma receptor engagement in human monocytes: association of CCL1 with a distinct form of M2 monocyte activation (M2b, Type 2) J. Leukoc. Biol. 2006;80(August (2)):342–349. doi: 10.1189/jlb.1005586. [DOI] [PubMed] [Google Scholar]
- Spaggiari G.M., Abdelrazik H., Becchetti F., Moretta L. MSCs inhibit monocyte-derived DC maturation and function by selectively interfering with the generation of immature DCs: central role of MSC-derived prostaglandin E2. Blood. 2009;113(June (26)):6576–6583. doi: 10.1182/blood-2009-02-203943. [DOI] [PubMed] [Google Scholar]
- Steinke J.W., Borish L. Th2 cytokines and asthma — Interleukin-4: its role in the pathogenesis of asthma, and targeting it for asthma treatment with interleukin-4 receptor antagonists. Respir. Res. 2001;2(February (2)):66. doi: 10.1186/rr40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabarkiewicz J., Pogoda K., Karczmarczyk A., Pozarowski P., Giannopoulos K. The role of IL-17 and Th17 lymphocytes in autoimmune diseases. Arch. Immunol. Ther. Exp. (Warsz). 2015;63:435–449. doi: 10.1007/s00005-015-0344-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Dyken S.J., Locksley R.M. Interleukin-4- and interleukin-13-mediated alternatively activated macrophages: roles in homeostasis and disease. Annu. Rev. Immunol. 2013;31:317–343. doi: 10.1146/annurev-immunol-032712-095906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasandan A.B., Jahnavi S., Shashank C., Prasad P., Kumar A., Prasanna S.J. Human Mesenchymal stem cells program macrophage plasticity by altering their metabolic status via a PGE2-dependent mechanism. Sci. Rep. 2016;(December 2) doi: 10.1038/srep38308. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5133610/ [cited 2018 Oct 16];6. Available from ([Internet].) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu G., Zhang Y., Zhang L., Ren G., Shi Y. The role of IL-6 in inhibition of lymphocyte apoptosis by mesenchymal stem cells. Biochem. Biophys. Res. Commun. 2007;361(September (3)):745–750. doi: 10.1016/j.bbrc.2007.07.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Z., Huang H., Hao S., Xu S., Yu H., Van Den Hurk S., et al. IL-10 has a distinct immunoregulatory effect on naive and active t cell subsets. J. Interferon Cytokine Res. 2007;27(December (12)):1031–1038. doi: 10.1089/jir.2006.0144. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.