A 29-year-old, otherwise healthy woman presented to the emergency eye clinic with a 1-day history of right eye conjunctivitis, photophobia, and clear watery discharge from the right eye. She returned from a 1-month vacation in the Philippines 3 days before presentation; she spent 1 day in San Francisco en route to her return to Canada. During her time in the Philippines, she swam in the ocean and hotel swimming pools. She was feeling well on her date of return on February 29 (Fig. 1 ). In Canada, she visited a public swimming pool the day after return. On March 1, 18 hours after returning from her trip, she developed rhinorrhea, cough, nasal congestion, and right eye conjunctivitis; she denied any fever though took over-the-counter antipyretic medication which may have masked a mild fever. Her travel partner developed a cough and rhinorrhea soon after she did (although he has tested negative for coronavirus disease 2019 [COVID-19]).
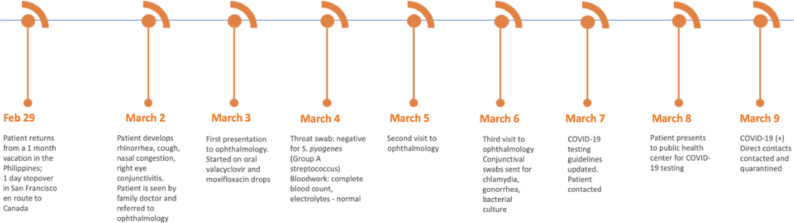
Fig. 1.
Timeline depicting the patient's clinical course.
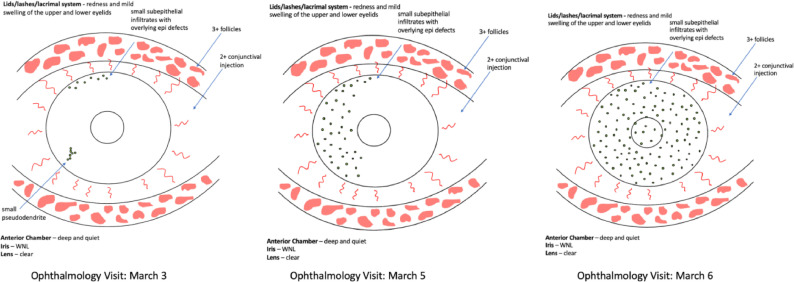
The patient was initially seen by her family doctor on the day of symptom onset and referred to ophthalmology (Fig. 2 ). Upon the first presentation to our service on March 3, she had worsening eye-related symptoms of photophobia, a sore and swollen eyelid, and mucous discharge of the right eye. On examination, she had 20/20 visual acuity OU. Anterior segment examination of the affected eye was remarkable for 1–2+ conjunctival injection, 3+ follicles, 1 small pseudodendrite in the inferior temporal cornea, and 8 small (0.2 mm) subepithelial infiltrates with overlying epithelial defects at the superior temporal limbus. Fundus examinations were unremarkable without any evidence of inflammation (Table 1 and Fig. 3 ). The patient was started on oral valacyclovir 500 mg PO TID and moxifloxacin 1 drop QID to the right eye based on a presumed diagnosis of herpetic keratoconjunctivitis.
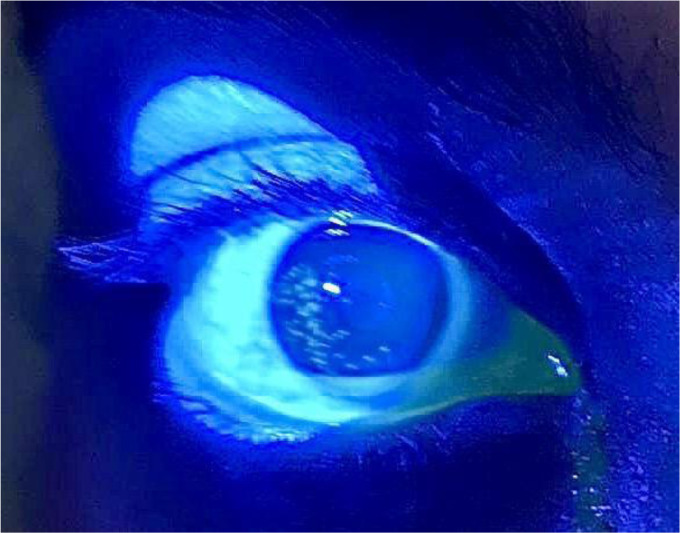
Fig. 2.
External photograph of the right eye after instillation of fluorescein taken under cobalt blue light demonstrating areas of fluorescein uptake consistent with the epithelial changes. Photograph was taken by the patient at her family doctor's office (March 2nd) before her first visit to the eye clinic; photograph provided by the patient (used with permission).
Table 1.
Summary of clinical findings over progressive visits to ophthalmology
| Ophthalmology Visit | March 3 | March 5 | March 6 |
|---|---|---|---|
| Vision | |||
| OD | 20/20 | 20/20 | 20/40 → pinhole to 20/30 |
| OS | 20/20 | 20/20 | 20/20 |
|
Intraocular pressure (mmHg), measured by tonopen | |||
| OD | 16 | 21 | 22 |
| OS | 13 | 18 | 18 |
| Pupils | |||
| No RAPD | No RAPD | No RAPD | |
| Left eye examination | |||
| Within normal limits | Within normal limits | Within normal limits | |
RAPD; relative afferent pupillary defect.
Fig. 3.
Schematic representation of the slit-lamp examination findings over progressive clinic visits; note the increase in the cornea lesions over time.
The following day, the patient's family physician coordinated a throat swab to screen for acute pharyngitis, which was negative for group A Streptococcus. Blood work was done, including a complete blood count and electrolytes, which were all within normal limits.
The patient returned to the eye clinic on March 5 due to worsening redness, pain, and irritation. A tender right pre-auricular node was noted. Visual acuity was measured to be 20/20 OU. On slit-lamp examination, 2+ conjunctival injection was noted along with a change in the appearance of the cornea, showing the development of numerous subepithelial infiltrates with overlying epithelial defects. Right after instillation of fluorescein, there was only pin-point staining with associated overlying epithelial defects on the temporal cornea (Table 1 and Fig. 4 ). The patient was continued on oral valacyclovir and moxifloxacin drops, but a presumed diagnosis of epidemic keratoconjunctivitis was given and contact precautions were suggested.
Fig. 4.
External photograph of the right eye taken by the patient before the second visit (March 5th) to the eye clinic demonstrating marked conjunctival injection and watery discharge. Photograph provided by the patient (used with permission).
The patient was seen by ophthalmology the next day on March 6th owing to persistently worsening symptoms and vision decline. At this visit, vision in the right eye vision was 20/40 pinhole to 20/30. A tender right preauricular lymph node was again noted, as well as cervical lymphadenopathy. Slit-lamp examination of the eye revealed follicular conjunctivitis with 2+ conjunctival injection and over 50 discrete areas of subepithelial infiltrates with overlying epithelial defects spread diffusely through the entire cornea (Table 1; Fig. 3). The patient was continued on valacyclovir, counselled regarding this being very contagious given the presumed viral etiology. Conjunctival swabs to test for chlamydia, gonorrhea, and bacterial culture were sent and were negative.
At the time of the visits to our clinic (March 3rd and 5th), the patient did not meet provincial health authority recommendations for testing of coronavirus infectious disease 2019 (COVID-19) based on country of travel. By March 6, however, testing recommendations in terms of geographic locations visited had expanded to any person with symptoms who had travelled outside of Canada. Thus, the Medical Officer of Health and institutional Infection Prevention and Control were contacted and facilitated testing. A nasopharyngeal (NP) swab collected on March 8th was positive for detection of the SARS-CoV-2 virus (the causative agent of COVID-19) by an in-house real-time reverse transcriptase polymerase chain reaction (rRT-PCR), using the E and the RNA-dependent RNA polymerase (RdRp) genes as targets, respectively.
Retrospective testing of the eye swab originally submitted for gonorrhea/chlamydia PCR on March 6th was found to be weakly positive for the SARS-CoV-2 virus (COVID-19) as well. Although the viral loads were not directly quantified, cycle thresholds of rRT-PCR assays from the NP swab produced stronger signal than those from the eye swab (23–25 cycles in NP vs 37 in eye; negative considered undetectable or >40 cycles).
Workplace Health and Safety, Public Health, and Infection Prevention and Control collaborated on follow-up of health care workers and clinic patients who may have been in contact with the case patient.
Discussion
To the best of our knowledge, this is the first reported case of COVID-19 (caused by the SARS-CoV-2 virus) presenting with keratoconjunctivitis as the main symptom.
On January 5, 2020, the World Health Organization (WHO) published a report on a pneumonia of unknown cause detected in Wuhan City, Hubei Province of China.1 Analysis of lower respiratory tract samples isolated from affected cases implicated a novel coronavirus as the causative agent in this illness.2 This illness is being compared with other global coronavirus-related outbreaks such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome, which affected approximately 8000 and 2400 people worldwide, respectively. Signs and symptoms of COVID-19 have thus far been described as fever, cough, myalgia, fatigue, sputum production, headache, hemoptysis, and diarrhea.3 Interestingly, a recent update provided by the American Academy of Ophthalmology discussed conjunctivitis as a presenting symptom of COVID-19 in affected patients.4
Initial reports of COVID-19 did not report ocular transmission as a possibility. Xia and colleagues at the First Affiliated Hospital of Zhejiang University evaluated the conjunctival secretions of 30 confirmed cases of COVID-19.5 In one of these patients, both tear and conjunctival secretions tested positive for the virus by rRT-PCR.5 Additionally, data from 1099 patients were published in the New England Journal of Medicine, in which “conjunctival congestion” was found in 0.8% of the patients.6 Despite these uncommonly reported statistics, there are numerous anecdotal reports of a red eye being the initial symptom before the onset of pneumonia, including that of Guangfa Wang, a national expert on the panel for pneumonia during the early investigations in Wuhan, China.7 Mr. Wang wore an N95 mask during his initial investigations of patients in Wuhan but did not have any protective eye equipment. Several days before his respiratory symptoms, he reported having a red eye, suggesting possible ocular transmission.8 Given this, eye care professionals, most notably ophthalmologists, may be the first point of contact in the health care field for patients with possible COVID-19, before the onset of characteristic respiratory symptoms.
In this case report, it can be seen that the clinical presentation can vary and fluctuate. The patient did not present with conjunctivitis as previously reported for COVID-19 cases, but as keratoconjunctivitis. It was also apparent from the clinical examinations that the epithelial defects varied from one examination to the next and appeared as a pseudodendrite perhaps from a healing epithelial defect or possibly as a progressing subepithelial infiltrate.
Therefore, front-line health care and eye care providers, including family physicians, emergency physicians, ophthalmologists, and optometrists, seeing patients presenting with a red eye should ensure that a thorough review of infectious contacts and travel history is undertaken. Patients who have a red eye; respiratory symptoms such as cough and shortness of breath; and recently travelled to areas with known outbreaks are at higher risk of having COVID-19. Clinical interactions with any patients presenting with similar upper respiratory tract symptoms should be done with mouth and eye protection routinely, if exposure to the patient's secretions is possible. This would be expected during the proximity of an eye examination.9 Our case highlights the necessity of using these additional precautions as the patient's conjunctival swab was positive for SARS-CoV-2, indicating the presence of potentially infectious virus.
There was a delay in testing our patient for COVID-19 because the initial guidelines from the Government of Canada (February 25, 2020) suggested testing for COVID-19 in any patient who presented with fever and/or new onset of (or exacerbation of chronic) cough and had travelled to an affected area within the past 14 days. Affected areas at that time included mainland China, Hong Kong, Iran, Italy, Japan, Singapore, and South Korea. Other exposure criteria included close contact with a confirmed or probable case of COVID-19 or laboratory exposure to biological material known to contain COVID-19.10 , 11 Our patient did not meet the initial testing guidelines and was only tested once the guidelines were updated to include all travel outside of Canada, emphasizing the importance of adapting quickly to rapidly evolving epidemiology in the context of an evolving pandemic. Unfortunately, this case resulted in 5 physicians and 3 health care workers being placed in 14 days of self-isolation.
As we learn more about the virus and its pathogenesis, we recommend that all practitioners caring for patients suspected of COVID-19 wear appropriate personal protective equipment (PPE) to mitigate mouth, eyes, and nose exposure.10 , 11 Because COVID-19 is a respiratory illness, the WHO recommends that health care workers examining and treating patients with suspected and/or confirmed COVID-19 infection use contact and droplet precautions.12, 13, 14 This includes wearing a gown, gloves, face mask covering the mouth and nose, and eye shield/goggles. Regardless of travel history or known or suspected infectious pathogen, every patient interaction should include an assessment of the risk of exposure to bodily fluids (including respiratory or eye secretions) to the health care worker and the appropriate PPE should be selected.9 , 15 The WHO also notes that a number of aerosol-generating medical procedures, including tracheal intubation and manual ventilation, have been associated with an increased risk of coronavirus transmission.12, 13, 14 As a result, health care workers engaging in such aerosol-generating medical procedures should additionally use a certified N95 mask.12, 13, 14 As always, for patients suspected of having an infectious red eye, it is imperative to follow disinfection practices that have already been outlined to prevent the spread of viral infection before and after each patient visit. Given that COVID-19 is due to an enveloped virus, it is susceptible to the alcohol and bleach disinfectants that are typically used in current ophthalmic practice.16
A formalized protocol for all hospital-based and private eye clinics should be developed to minimize the risk of exposure for patients and health care providers. A report from the Hong Kong experience suggests that protocols should include prescreening at the administrative level to call and reschedule nonurgent patients with symptoms or travel history in the last 14 days, avoiding micro-aerosol generating procedures such as noncontact tonometry, environment, and infection control protocols to reduce droplet transmission and availability of proper PPE.17 Patients can also be screened or managed through tele-ophthalmology if patients are able to send photographs of their eye to their eye care professional. Importantly, it should be noted that asymptomatic individuals can still pass on viral infection up to 48 hours before the onset of symptoms.18 , 19
Conclusions
We present a case of COVID-19 that presented initially to ophthalmology with keratoconjunctivitis and mild respiratory symptoms, without fever. The patient's primary symptom and reason for repeatedly seeking care was a red eye with watery discharge. The case emphasizes the importance for eye care professionals to remain vigilant and consider SARS-CoV-2 as the causative agent in patients presenting with viral conjunctivitis, particularly in high-risk patients with travel to areas of active transmission of the virus. These cases could represent an early presentation of COVID-19. Protocols should be put in place to minimize exposure risk to other patients and health care providers.
Acknowledgments
Footnotes and Disclosure
The authors have no relevant financial interests or disclosures.
Acknowledgements
The authors would like to acknowledge Dr. Yi (Fay) Zhai for relaying the experiences of ophthalmologists in China in response to the COVID-19 outbreak, and Dr. Errol Prasad at DynaLife Medical Labs (Edmonton, Alberta, Canada) for coordinating the viral testing of the conjunctival swab.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jcjo.2020.03.003.
Appendix. Supplementary materials
References
- 1.World Health Organization. Pneumonia of unknown cause – China. www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/. Accessed March 10, 2020.
- 2.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report – 51. www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf. Accessed March 12, 2020.
- 3.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Academy of Ophthalmology. Alert: important coronavirus updates for ophthalmologists. www.aao.org/headline/alert-important-coronavirus-context. Accessed March 10, 2020.
- 5.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection [E-pub ahead of print]. J Med Virol. doi: 10.1002/jmv.25725, Accessed [DOI] [PMC free article] [PubMed]
- 6.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China [E-pub ahead of print]. N Engl J Med. [DOI] [PMC free article] [PubMed]
- 7.Lu C.W., Liu X.F., Jia Z.F. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li J.P., Lam D.S., Chen Y., Ting D.S. Novel Coronavirus disease 2019 (COVID-19): the importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020;104:297–298. doi: 10.1136/bjophthalmol-2020-315994. [DOI] [PubMed] [Google Scholar]
- 9.Government of Canada. Infection prevention and control for coronavirus disease (COVID-19): interim guidance for acute healthcare settings. www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/interim-guidance-acute-healthcare-settings.html. Accessed March 14, 2020.
- 10.Government of Canada. COVID-19 affected areas list. www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/covid-19-affected-areas-list.html. Accessed March 10, 2020.
- 11.Government of Canada. Interim national case definition: Coronavirus Disease (COVID-19). www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/national-case-definition.html. Accessed March 10, 2020.
- 12.World Health Organization. Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected - Interim guidance. www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125. Accessed March 10, 2020.
- 13.World Health Organization. Advice on the use of masks in the community, during home care and in health care settings in the context of the novel coronavirus (2019-nCoV) outbreak - Interim guidance. www.who.int/publications-detail/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak. Accessed March 10, 2020.
- 14.World Health Organization. Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19). apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf. Accessed March 10, 2020.
- 15.Centers for Disease Control and Prevention. Isolation precautions. Cdc.gov. www.cdc.gov/infectioncontrol/guidelines/isolation/index.html. Accessed March 14, 2020.
- 16.Government of Canada. Infection prevention and control for coronavirus disease (COVID-19): interim guidance for acute healthcare settings. www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/interim-guidance-acute-healthcare-settings.html. Accessed March 10, 2020.
- 17.Lai THT, Tang EWH, Chau SKY, Fung KSC, Li KKW. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong [E-pub ahead of print]. Graefes Arch Clin Exp Ophthalmol. doi: 10.1007/s00417-020-04641-8. Accessed [DOI] [PMC free article] [PubMed]
- 18.Macintyre C.R. On a knife's edge of a COVID-19 pandemic: is containment still possible? Public Health Res Pract. 2020;30 doi: 10.17061/phrp3012000. [DOI] [PubMed] [Google Scholar]
- 19.Luo SH, Liu W, Liu ZJ, et al. A confirmed asymptomatic carrier of 2019 novel coronavirus (SARS-CoV-2) [Epub ahead of print]. Chin Med J (Engl). doi: 10.1097/CM9.0000000000000798, Accessed [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.