Abstract
Study objective
On March 13, 2003, Singapore physicians were alerted about an outbreak of atypical pneumonia that became known as severe acute respiratory syndrome (SARS). I describe the application of an emergency department (ED) disaster response plan to manage the SARS outbreak.
Methods
The ED implemented protection for staff, patients, and facility; infection control measures; and disaster-response workflow changes. The Ministry of Health, Singapore, centralized SARS cases in the hospital, and the ED became the national screening center. A screening questionnaire and a set of admission criteria were applied after assessment of clinical features and chest radiograph findings.
Results
For the duration of the outbreak that ended on May 31, 2003, the ED screened 11,461 persons for SARS, of whom 1,386 (12.9%) were admitted to rule out SARS and 235 (17%) were confirmed to have SARS. Among 10,075 persons discharged from the ED, there were 28 reattending patients who were admitted and diagnosed with SARS, giving an undertriage rate of 0.3% (95% confidence interval [CI] 0.1% to 0.4%). The sensitivity of an ED admission for SARS was 89.4% (95% CI 85.6% to 93.1%), and specificity was 89.7% (95% CI 89.2% to 90.3%). The positive predictive value was 17% (95% CI 15.7% to 18.4%), and the negative predictive value was 99.7% (95% CI 99.6% to 99.8%). No patient contracted SARS as a result of an ED visit. After full implementation of protective measures, 1 ED nurse with undiagnosed diabetes mellitus was treated for suspected SARS.
Conclusion
Although the SARS outbreak was not a bioterrorism event, the ED disaster response was applicable in the outbreak's management. The use of a screening questionnaire and admission criteria enabled the ED to screen, treat, and safely discharge the majority of the patients.
Capsule Summary.
What is already known on this topic
The Asian severe acute respiratory syndrome (SARS) outbreak strained the capacity of many hospitals and emergency departments (EDs) and caused illness and death among health care workers.
What question this study addressed
The evolving disaster response plan of an ED affected by the SARS outbreak is described.
What this study adds to our knowledge
This article describes the development of a SARS screening unit, with designated areas and roles for health care workers. A tool based on clinical features allowed screening of a large number of patients. Infection control measures minimized the risk of SARS to health care workers.
How this might change clinical practice
Experience gained in this hospital's response to SARS may provide helpful guidelines for implementing a disaster response plan to screen large numbers of patients while protecting health care workers in the event of a large communicable disease outbreak.
Introduction
Singapore is a small nation-state with a total population of 4.1 million.1 It has 6 public hospitals providing 6,228 acute care beds and 7 private hospitals providing 1,925 acute care beds.1
On March 13, 2003, at 3:36 pm, the Ministry of Health, Singapore, sent an alert2 via e-mail to physicians about an outbreak of atypical pneumonia in Hong Kong, Vietnam, and Guangdong Province in China. It stated that 3 Singaporeans were admitted to the hospital for pneumonia after returning from Hong Kong at the end of February 2003, but no hospital staff had reported sick. The e-mail was circulated to alert emergency department (ED) physicians and nurses.
On March 14, 4 nurses who worked in the same ward in the study hospital presented to the ED with fever, cough, and infective changes on chest radiograph. They were admitted for pneumonia. Because they presented at different times on the same day, the cluster effect was not apparent to ED staff, and they were not linked to the atypical pneumonia outbreak. A nursing officer from the same ward had been admitted for evaluation of prolonged fever 2 days earlier. The nursing supervisors of the hospital noted the cluster effect and a hospital-wide alert went out.
This report describes the interventions adopted by the ED and hospital as part of the nation's effort to contain the outbreak that was subsequently named severe acute respiratory syndrome (SARS).
Materials and methods
The ED of the study hospital is the busiest in Singapore, providing care to persons aged 15 years or older and had an annual attendance of 131,127 in 2002.3 The ED has a public entrance that is separate from 3 other hospital entrances. Over this ED entrance is a wide shelter that extends toward an open-air car park. The Communicable Disease Center, Singapore, is an annex to the main hospital and is Singapore's tertiary referral center for infectious diseases. The hospital is an urban acute general hospital and has a total of 1,100 beds.
Adjacent to the ED is a decontamination chamber completed in 2002 as part of the hospital's preparation for a hazardous material or biologic terrorist event. The decontamination chamber is hexagonal and has the capacity to hold 96 walking patients and 12 trolleys. The middle section has 5 lanes of showerheads suspended from the ceiling, whereas the 2 ends of the chamber are empty spaces with walls that have electrical outlets, telephone and intranet sockets, and washbasins. Ventilation was through an exhaust fan system. Staff of the hospital had regular drills in the use of the decontamination chamber and in disaster response, the last drill having ended on March 11, 2003.
Protection of patients, visitors, and environment
From March 13 onward, all at-risk patients were given surgical masks. Because airborne transmission of an infectious agent was not excluded, the decontamination chamber was opened, with 1 end set up with a computer system, tables, chairs, stationery, and medical equipment and supplies to function as an isolation and consultation area for at-risk patients. After normal triage, at-risk patients were directed to the decontamination chamber, thereby bypassing the rest of the ED. On March 17, in response to the surge in number of SARS patients during the weekend, a satellite radiology service was set up within the decontamination chamber, catering to at-risk patients. On March 18, a screening station and a separate registration service were set up in front of the glass-door entrance to the ED. At the outdoor screening station and registration service, all at-risk patients were given masks, identified, registered, and treated in the decontamination chamber so that none passed into the air-conditioned interior of the ED.
Although the evidence in Singapore was against airborne transmission, reports from international experts4 stated that airborne transmission was possible; hence, the decision was made to replicate a physical ED in a well-ventilated outdoor environment to screen patients and provide outpatient treatment. On March 23, an inverted U-shaped tent was erected outside the ED entrance, extending out toward the car park. Seven cubicles that could be used for triage or consultation were set up under the tent, with facilities for a second satellite radiology service. Other essential utilities (eg, lighting, air coolers, computers, hand-washing facilities, portable toilets) were set up. The waiting area in front of the tent under the ED shelter could seat 50 persons, each with a clear radius of 0.5 m. All documentation by our electronic system was replicated in the outdoor ED. Although high-risk patients were treated in the decontamination chamber, the outdoor ED had separate sections for no-risk and low-risk patients and for moderate-risk patients. After screening, all patients were directed to the different risk areas to be triaged by nurses and assessed by physicians in their respective areas, thus minimizing mingling of patients from different risk categories. Each risk area had its separate team of physicians, nurses, and ancillary staff, and staff movement into another risk area was not allowed without a complete change in personal protection equipment. Medical and nursing manpower was reconfigured to match these changes in ED workflow and volume.
No family member was allowed into the high-risk area, and 1 family member was allowed to stay with the other patients. However, all accompanying persons were strongly advised to stay in a waiting area designated for them, and many chose to use this area and did not enter the patient areas. If resuscitation were to be required, it would be carried out in the indoor resuscitation room. All entrances and exits from the main ED were sealed, except for the entrance into the resuscitation room and 2 other entrances for staff traffic. Security personnel were deployed to the ED to direct vehicle, patient, and visitor traffic and to prevent unauthorized access into the treatment areas.
Staff protection and welfare
Protection with an N95 mask, a disposable gown, and gloves for ED staff began on day 2 and was adopted by all staff by days 5 to 6. For airway procedures that would expose staff to oral and respiratory secretions, all staff wore the personal air-powered respirator for better protection. Everyone was reminded to observe personal hygiene, to wash hands between treating patients, and to clean instruments (eg, stethoscopes) with alcohol swabs between treating patients.
The daytime outdoor temperature ranged from 27°C (80.6°F) to 32°C (89.6°F), with humidity more than 90%, making the outdoor ED an uncomfortable place to work in the late morning and afternoon. Uniforms were discarded in favor of T-shirts and pants for comfort. Frequent breaks were mandated to prevent dehydration and heat stress. Everyone was reminded regularly to drink plenty of fluids, to have sufficient rest, and to keep a balanced diet. Food caterers were engaged when the food and beverage outlets in the hospital discontinued their services, probably as a result of declining patient and visitor traffic and fear of SARS.
Because fever was reported to be present in 100% of SARS patients and was often the first symptom, everyone was given a personal thermometer to measure their temperature 3 times daily. Any staff recording a temperature of 37.5°C (99.4°F) or higher was required to stop work immediately and seek treatment. Senior members encouraged all ED staff to approach them freely to talk. The hospital psychiatric team offered counseling to any member of the staff who needed to speak to them.
Screening process
In response to the Ministry of Health alert on March 13, 2003, ED triage nurses started to ask febrile patients about recent travel to affected areas. On March 15, according to Ministry of Health information,5 triage nurses started to ask about close contact with atypical pneumonia patients. On March 16, the term “SARS” was adopted in line with the World Health Organization (WHO) and Ministry of Health recommendation.6 When the outdoor screening station was set up, the screening questionnaire was expanded to include documentation of tympanic temperature in addition to travel and contact history. When the ED took over the screening function from the Communicable Disease Center, Singapore, on March 26, the screening questionnaire was revised to become a flow chart to enable rapid screening of a large number of patients. Screening categories based on patient's temperature, symptoms of cough,7 breathing difficulty,7 sore throat, running nose, myalgia, headache, malaise, vomiting or diarrhea, and exposure to SARS were refined: (1) no risk or low risk: no or tenuous history of exposure without symptoms or with mild symptoms; (2) moderate risk: positive exposure with mild symptoms or temperature less than 38°C (<100.3°F); and (3) high risk: positive exposure with temperature 38°C or greater (≥100.3°F).
Disposal and admission criteria
During the first 10 days of the outbreak, all at-risk patients identified by the ED were referred to the Communicable Disease Center, Singapore, infectious diseases physician for review. The infectious diseases physician would decide which patient needed admission. The admission decision was transferred from the infectious diseases physician to the emergency physicians on March 24. The admission criteria evolved from a simple version consisting of travel to a SARS-affected area or close contact with SARS patient, temperature of 38°C or greater (≥100.3°F), and cough with or without shortness of breath to the following: (1) travel to an affected area; (2) contact with a SARS patient; (3) health care worker; (4) cluster fever (eg, persons in the same household or workplace all becoming sick within a short interval); (5) person on home quarantine order; (6) cough with or without shortness of breath; (7) chest radiograph changes of pneumonia; (8) clinical features of atypical pneumonia; and (9) clinical features of pneumonia or infective process in an immunocompromised person recently discharged from the hospital. The admission criteria and screening questionnaire expanded in response to a new understanding and information about SARS.
On completion of the consultation, the prevailing admission criteria were applied to decide which patients needed admission. Patients requiring admission were admitted to isolation rooms. Patients who were discharged from the ED proceeded to the pharmacy, where the waiting area was also an open-air area. All patients who were discharged were instructed to measure their temperature 3 times daily, isolate themselves during their illness, observe personal hygiene, keep in touch with the hospital, and return if symptoms persisted or their temperature was 38°C or greater (≥100.3°F). Staff from the hospital were mobilized to set up home surveillance to telephone all patients discharged from the ED on days 1, 2, 3, and 14.
National strategy of SARS containment
On March 19, day 7, the ED was feeling the strain of caring for the normal load of patients and persons seeking consultation for SARS. Therefore, on March 20, public ambulances were diverted away from the ED until further notice. On day 10, March 22, the Ministry of Health decided to centralize all SARS cases at the study hospital and to free hospital resources to care for SARS patients.8 The measures included diversion of all ambulances away from the ED, mass media announcements advising the public not to come to this ED for non-SARS problems, and cancellation of elective surgery and outpatient clinic sessions. The ED started preparations to cater to pediatric SARS patients and to take over SARS screening from the Communicable Disease Center, Singapore. On day 14, March 26, this ED became the sole screening and referral center for all SARS cases in Singapore. Members of the public worried about SARS could also walk in for screening and consultation.
Communications
The chief of the ED and 3 senior nurses were taken off clinical duties to deal with liaison, operational, and communications issues. All senior members had regular meetings and briefings at the start of each shift, supplemented by e-mail reminders.
E-mails and briefings by the attending emergency physician or nursing officer at the start of each shift became the main source of communication with front-line staff (ie, residents, nurses, clerks). On certain days, changes were happening so fast that a debriefing was needed at the end of an 8-hour shift to update all staff. Fixed-line phones and mobile phones replaced the indoor paging system.
The Internet sites of the WHO, the Centers for Disease Control and Prevention, and the Ministry of Health were checked for regular updates. Dedicated hotlines to handle inquiries from general practitioners, health care workers, and members of the public were manned by staff deemed unsuitable for clinical work for this period (eg, pregnant staff).
Data and measurements
Total ED attendance and the number of persons who came for screening, were admitted, and were confirmed to have suspected or probable SARS7 were captured in the computerized log. The diagnosis of SARS was extracted from the electronic inpatient case records, and they were based on WHO case definitions before May 1, 2003. The number of persons with no risk and those at risk who came for screening, contact or travel history, and repeated ED attendances resulting in admission were also captured. The proportion of admitted patients confirmed to have suspected or probable SARS was calculated. The undertriage rate (whereby undertriage equaled the number of discharged patients diagnosed to have SARS subsequently divided by the number of at-risk persons discharged from ED), the sensitivity, and the specificity of ED screening and disposal were calculated. The number of ED staff who were sick and their diagnoses were reflected in a separate log. The attending emergency physician's clinical hours were calculated, and the nature of work was described.
SPSS for Windows (version 11; SPSS, Inc., Chicago, IL) was used for data analysis. The χ2 test was used for categorical data, and statistical significance was set at a P value less than or equal to .05 where appropriate. This study was approved by the hospital review board.
Results
The outbreak lasted 80 days until Singapore was removed from the WHO's list of SARS-affected areas on May 31, 2003.9 For this period, total ED attendance was 16,606, of whom 11,461 (69%) patients were screened for SARS (Figure 1). Between days 2 and 13, 9.9% of ED attendances were for SARS screening. From day 14 onward, when the ED took over from the Communicable Disease Center, Singapore, 88.4% of patients attended the ED for SARS screening. Among those 11,461 patients screened, the median age was 33 years. Fifty-three percent were men, with a mean age of 35.8 years (95% confidence interval [CI] 35.4 to 36.2 years), and 47% were women, with a mean age of 35 years (95% CI 34.6 to 35.4 years).
Figure 1.
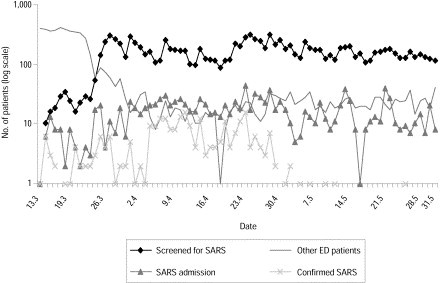
ED workload from March 13 to May 31, 2003.
Of the 11,461 screened, after the first ED visit, 1,386 (12.1%) patients were admitted to rule out SARS. Out of 1,386 patients admitted, 235 (17%) patients were confirmed to have suspected or probable SARS (Figure 1). Table 1 summarizes the features of the probable and suspected SARS cases and the other patients. No SARS patient required resuscitation. Admitted patients without SARS had the following diagnoses: upper respiratory tract infection (15.5%), fever for observation or viral fever (11.9%), dengue fever (9%), pneumonia or lower respiratory tract infection (8.3%), and other (eg, gastroenteritis, tonsillitis, pulmonary tuberculosis, HIV-related infections) (35.7%).
Table 1.
Features of patients screened by the ED.
| Features | Probable SARS (n=117) | Suspected SARS (n=146) | Admitted Non-SARS (n=1,151) | Discharged From ED (n=10,047) |
|---|---|---|---|---|
| Men, % (95% CI) | 40.2 (31.3–49.1) | 51.4 (43.3–59.5) | 55 (52.1–58) | 52.8 (51.8–53.8) |
| Mean age, y (95% CI) | 38 (35–41) | 35.6 (33.1–38.2) | 42.7 (41.4–44) | 34.5 (34.2–34.8) |
| Median age, y | 37 | 33 | 38 | 32 |
| Travel to affected areas, % (95% CI) | 2.6 (0.5–7.3) | 24 (17–30.9) | 20 (17.6–22.4) | 15 (14.4–15.9) |
| Risk categorization, no/low, % (95% CI); | 26.5 (18.5–34.5); | 22 (15.2–28.6); | 33.2 (30.4–36); | 58.9 (57.9–59.9); |
| moderate/high, % (95% CI) | 73.5 (65.5–81.5) | 78 (71.4–84.8) | 66.8 (63.9–69.5) | 41.1 (40.1–42.1) |
| Undertriage at first ED consultation, % (95% CI) | 11.1 (5.4–16.8) | 10.3 (5.4–15.2) | Not applicable | Not applicable |
Figure 2 shows the outcome of all persons who came to the ED for screening. Among 10,075 (87.9%) persons discharged from the ED, 28 reattended, of whom 13 patients were diagnosed as having probable SARS and 15 as having suspected SARS later, giving an overall undertriage rate of 0.3% (95% CI 0.1% to 0.4%). There were 15 women and 13 men, with a mean age of 35 years (95% CI 29.5 to 40.5 years) and median age of 32 years. The mean temperature of these 28 persons during their first ED consultation was 37.6°C (99.6°F; 95% CI 37.3 to 37.9°C), which increased to 38°C (100.3°F; 95% CI 37.7 to 38.3°C) during their repeated visit. Twenty-two (78.6%) of these 28 patients had a temperature lower than 38°C (<100.3°F), and 9 (32.1%) did not have a cough during their first ED consultation. Three patients did not have a chest radiograph examination because they presented early and their symptoms were mild, whereas 21 (84%) of 25 chest radiographs were normal during the initial ED visit. Four patients with infective changes on chest radiograph were presumed to have bacterial pneumonia and were discharged from the ED with outpatient treatment. The mean interval between the first and second ED visits was 55.4 hours (95% CI 41.6 to 69.2 hours), the median was 47.3 hours, and the range was 10.5 to 137.7 hours. None of these 28 patients caused secondary transmission during the interval between their first and second ED consultations. Eighteen of these patients returned to the ED voluntarily when their symptoms persisted, and 10 patients were tracked and recalled by the home surveillance or ED hotline team.
Figure 2.
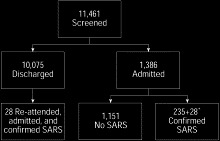
Outcome of SARS screening. ∗Reattendance cases confirmed to have SARS after admission.
The performance of ED admission to rule out SARS achieved an overall sensitivity of 89.4% (95% CI 85.6% to 93.1%) and specificity of 89.7% (95% CI 89.2% to 90.3%). The positive predictive value was 17% (95% CI 15.7% to 18.4%), and the negative predictive value was 99.7% (95% CI 99.6% to 99.8%). One thousand seven hundred seventy-six (15.5%) persons traveled to affected areas,10 with Hong Kong being the most common. None of the SARS patients contracted the disease because of their ED visits. Table 2 shows the outcome of risk categorization from April 9 to May 31. There were significant trends for higher risk categories to result in admission (P<.0001) and confirmation of SARS (P=.003). Risk categorizations changed twice before April 9 and hence were inappropriate for analysis of outcome.
Table 2.
Outcome of risk categorization from April 9 to May 31, 2003.
| Patients, No. | No Risk or Low Risk | Moderate Risk | High Risk | Total |
|---|---|---|---|---|
| Admitted (% total) | 356 (6.9) | 407 (14.4) | 255 (67.8) | 1018 (12.2) |
| [95% CI] | [6.2–7.6] | [13.1–15.7] | [63.1–72.5] | [11.5–12.9] |
| Total | 5,180 | 2,822 | 376 | 8,378 |
| Diagnosis of admitted patients | ||||
| SARS (% total) | 42 (11.8) | 63 (15.5) | 56 (22) | 161 (15.8) |
| [95% CI] | [8.5–15.1] | [12–19] | [16.9–27] | [13.6–18.1] |
| No SARS | 314 | 344 | 199 | 857 |
| Total | 356 | 407 | 255 | 1,018 |
One ED nurse was treated for a suspected case of SARS when she became ill after nursing a SARS patient before the hospital alert went out. After full implementation of protective measures, 1 ED nurse who had undiagnosed diabetes was treated for suspected SARS. With 170 staff members, the number of sick ED staff did not show any significant increase from baseline. Each attending emergency physician worked an average of 39.2 clinical hours per week during the outbreak compared with 38.1 hours before the outbreak. From March 13 to April 30, 15.3% of morning shifts had coverage by 2 emergency physicians, whereas all afternoon and night shifts had single emergency physician coverage. In May, a junior attending physician joined the team of 6 emergency physicians, and we were able to provide coverage by 2 emergency physicians for 100% of morning and 40.3% of afternoon shifts. Before SARS, 33.8% of morning shifts had double emergency physician coverage. There was no increase in the resident and nursing manpower.
The spectrum of clinical practice was confined mainly to evaluation of patients with fever, respiratory tract complaints, chest radiographs, and occasionally CBC count results. Besides clinical work, the role of the attending emergency physician expanded to become a screening or triage officer at times, a repository of the latest changes affecting clinical work, a counselor to front-line staff, and a SARS consultant providing telephone advice to general practitioners and physicians from other EDs. The senior nursing staff had oversight of the hospital beds, workflow, and working conditions in the outdoor ED and the physical well-being of the frontline staff.
Limitations
During the outbreak, the first version of the screening questionnaire underwent 3 revisions, and the admission criteria underwent 2 revisions. The revisions of these 2 tools did not coincide temporally. As such, it was difficult to assess the performance (ie, sensitivity and specificity) of any single version of either tool. In practice, both tools worked in tandem; therefore, it was the overall performance of the combination of the tools that was reported. Neither the questionnaire nor the admission criteria had been validated in any other population.
At writing, the diagnosis of SARS was based on WHO case definitions before May 1, 2003, which did not depend on laboratory testing. Since then, the WHO case definition for probable SARS was revised to include laboratory diagnosis, and the Ministry of Health had tested and reviewed the status of all patients with suspected SARS, reclassifying 32 patients as probable SARS.11
The Ministry of Health e-mail alert system is targeted at individual physicians. When an e-mail alert is received, it is up to the recipient to take appropriate action and inform the health care institution. Therefore, a review of the ED surveillance system would be needed to enable more efficient detection and communication of suspicious clusters of cases. The decision to let the study hospital concentrate on SARS cases and for the ED to take over SARS screening from the Communicable Disease Center, Singapore, created unique circumstances that might not be easily replicated elsewhere. The resources and support of the Ministry of Health made available to the ED and the hospital underlie strong political will and availability of resources, which again may not be reproducible elsewhere. Finally, the psychologic effect on ED staff has yet to be fully assessed, which may affect the resumption of normal ED services.
Discussion
Unlike an earthquake12 or a terrorist event13, 14, 15 in which a sentinel event heralds the arrival of a large number of casualties immediately afterward, the first 3 imported cases of SARS presented in early March 2003 and had already unobtrusively spawned secondary and tertiary cases by the time the cluster effect became apparent 2 weeks later. The SARS outbreak can serve as a natural model for a covert release of a communicable biologic weapon. It has characteristics common to some biologic agents, such as being invisible; odorless; tasteless; able to cause secondary person-to-person transmission, with its clinical manifestation occurring days later; and being indistinguishable from common illnesses such as dengue fever, influenza, and community-acquired pneumonia.
The ED, study hospital, and Ministry of Health recognized on days 2 to 3 that an incident had occurred, and the disaster response plan was put into action. Protection for staff, patients, and visitors; strict infection control; and facility protection for the ED were top priorities, as pointed out by Macintyre et al.16 The decision to replicate an outdoor ED was based on 3 factors: (1) the anticipated surge in number of persons coming for screening in response to reports in the mass media; (2) the expected increase in the number of tertiary SARS cases before infection control measures could break transmission; and (3) the remote but real possibility of airborne transmission. After protective measures were implemented, no SARS cases were traced to a visit to this ED. One ED nurse whose diabetes mellitus was undiagnosed previously was treated as having a suspected case of SARS, despite protection with gloves, a gown, and an N95 mask. It remained unclear whether there was a lapse in her personal protection and infection control practice or whether her undiagnosed diabetes mellitus might have compromised her immunity and rendered her more susceptible to SARS. Otherwise, the personal protective equipment and infection control measures were adequate, and no other ED staff contracted SARS.
Because SARS was so new, there was no vaccine or specific therapy, which worked to the advantage of the ED because staff were able to concentrate on screening and discharge or admission without the extra work associated with acquisition, stockpiling, and administration of vaccine and medications. The clinical course of SARS was such that, when they presented to the ED, the majority of the patients were stable and did not require complicated care processes or extensive investigations. Therefore, the time and manpower needed to assess and then care for each patient was kept to a minimum, allowing a rapid turnover of patients, which helped to minimize the physical stress borne by ED staff wearing protective gear and working in a hot and humid outdoor environment.
The ED disposal decision of SARS patients gave an undertriage rate of 0.3%, a sensitivity of 89.4%, and specificity of 89.7%. The article by Rainer et al17 reported a sensitivity of 26% and specificity of 96% when WHO guidelines were used to identify patients with suspected SARS before admission to the hospital. Comparison with this study is difficult because this ED used a lower threshold for fever, chose a more liberal interpretation of contact history than that in the WHO guidelines, and added other symptoms to the screening questionnaire and admission criteria. For the small group of SARS patients undertriaged by the ED and inadvertently discharged after their first visit, the combination of discharge instructions and telephone contact enabled the hospital to track and recall every one of them. This process highlighted a hitherto unrecognized aspect of ED disaster management and planning: the need and resources required to maintain telephone contact with a large number of patients discharged from the ED. For the group of no-risk or low-risk persons, the majority were either asymptomatic or had minor ailments such as upper respiratory tract infection that could have been treated by general practitioners. Instead of medical treatment, education about SARS, counseling, and reassurance became the major component of the ED consultation for these persons.
Once the doors were closed to non-SARS patients, the ED functioned in a disaster-response mode by screening and risk-categorizing large numbers of persons rapidly, isolating and admitting the small number of high-risk patients and rendering outpatient treatment to the majority expediently. Resuscitation, extensive investigations, and extended care in observation rooms, routine daily activities for this ED previously, were not needed for the SARS patients. To function in disaster mode entails changes to duty rosters and work assignments, adjustment to wearing protective gear and working in an outdoor environment, use of a skill set different from that of routine ED work, and acceptance of the risks involved in working with SARS patients, all to be done within a short period of 3 to 4 days. It was therefore encouraging that there was no unexpected resignation and there was no increase in the proportion of sick ED staff, despite no increase in ED manpower to cope with the outbreak. Disaster response drills in the past had established lines of communication and command in the hospital and within the ED, allowing timely flow of information to front-line staff. During the outbreak, senior ED staff often performed “communications triage” (ie, selecting information that affected patient care for immediate release to front-line staff) leaving the other information for staff to access in their own time. Without communications triage, front-line staff might have been unnecessarily burdened with too much information.
To enable the infectious diseases team to concentrate on inpatient care, the ED took over the screening function and admission decision. Although evaluation of fever, respiratory complaints, and chest radiographs was not difficult, the emergency physician found it stressful to make disposal decisions for some patients because of the unknown behavior of SARS, the fear of an inadvertent discharge leading to community spread, and the concern about inappropriate admissions straining hospital resources, thus compromising patient and staff safety. In the majority of cases, the admission decisions were straightforward. However, for patients for whom the exposure history was tenuous or the clinical features were atypical, the availability of the infectious diseases physician or a second emergency physician for discussion was helpful. The stressful aspects of the expanded role of the emergency physician included (1) providing telephone consultation to other physicians without the opportunity to evaluate the patient personally; (2) keeping up with large amount of new information daily and performing communications triage; (3) trying to care for front-line staff while learning to cope with fears and uncertainties; and (4) concern about attrition of non-SARS skills and knowledge, should the outbreak be prolonged.
The hospital worked closely with the Ministry of Health and the Quarantine and Epidemiological Department of the Ministry of Environment, and ED work was able to proceed smoothly partly because of the resources and support made available to this ED by these agencies. With hospital support, the mass media became an ally and did not cause any disruption to ED work.
Although the Ministry of Health quarterly report has not been released, anecdotal accounts reported an initial increase in the ED workload and ambulance cases in all the other public hospitals, resulting in long waiting times for consultation and admission and also resulting in bed shortage. There were also reports of increased ambulance transit and turnaround time. However, in week 4 when some of the public hospitals reported the presence of a few SARS cases, there was a sudden sharp decline in their ED attendance that increased again within 2 weeks. The protection and infection control measures of the study hospital became the benchmark for the other public hospitals, and various teams visited this ED to understand its practices and protocols better.
In summary, although the SARS outbreak was not a bioterrorism event, the ED disaster response to bioterrorism was applied with satisfactory results. Infection control measures and protection for patients and visitors worked, and no SARS case was traced to a visit to the study ED. Except for 1 nurse with undiagnosed diabetes mellitus, protection for ED staff worked well, and none of them contracted SARS. Replication of an outdoor ED reduced the risk of airborne infection to a minimum, but it was unclear whether this reduction would be applicable in places with fewer resources.
The role of the attending emergency physician expanded considerably beyond clinical duties and was associated with additional stress. Comprehensive discharge advice and telephone contact with the large number of patients discharged from ED were important safety nets and needed significant resources. By using a simple screening questionnaire and a set of admission criteria that were diligently updated according to new information, the ED was able to screen, treat, and safely discharge the majority of patients.
Acknowledgements
This report is a tribute to all health care workers in Singapore and other countries as they work to prevent SARS from doing more damage, to my colleagues and their families who have contracted SARS, and most of all, to 3 of my colleagues whose untimely demise was due to SARS.
I thank Dr. H-P Chia for his statistical advice; Dr. S-C Quah, S-H Sim, and R Yeo for their help with the data; Dr. S-Y Tay for his comments; Dr. E Seow, my chief, who has been a tower of strength for our ED; and Dr. S-W Lim and his team for their tremendous support.
Footnotes
The author reports this study did not receive any outside funding or support.
Editor's note:This article was first published on Annals' Web site (www.mosby.com/AnnEmergMed) on October 9, 2003. Articles of particular interest are published on the Web site in advance of their appearance in the print journal. In the future, an increasing percentage of our content will be published first on the Web, predating the print publication as a service to our readers.
References
References
- 1.Ministry of Health, Singapore. Health Facts Singapore 2002. Available at: http://app.moh.gov.sg/sta/sta0101.asp and http://app.moh.gov.sg/sta/sta0105.asp. Accessed April 4, 2003.
- 2.Ministry of Health, Singapore. Ministry of Health Medical Alert: Outbreak of Atypical Pneumonia in Hong Kong, Vietnam and Guangdong Province in China. Ministry of Health publication No. MH 34:03, Vol. 14.
- 3.Office of Quality Management. Trends of Tan Tock Seng Hospital Emergency Department Attendances. Office of Quality Management, Tan Tock Seng Hospital, Singapore.
- 4.Centers for Disease Control and Prevention. Severe acute respiratory syndrome (SARS): updated interim domestic infection control guidance in the health care and community setting for patients with suspected SARS. Available at: http://www.cdc.gov/ncidod/sars/infectioncontrol.htm. Accessed April 26, 2003.
- 5.Ministry of Health, Singapore. Update (II) on atypical pneumonia cases in Singapore, March 15, 2003, press release. Available at: http://app.moh.gov.sg/new/new02.asp. Accessed April 4, 2003.
- 6.Ministry of Health, Singapore. Update (III) on atypical pneumonia cases in Singapore, March 16, 2003 [press release]. Available at: http://app.moh.gov.sg/new/new02.asp. Accessed April 4, 2003.
- 7.World Health Organization. Case definitions for surveillance of severe acute respiratory syndrome (SARS). Available at: http://www.who.int/csr/sars/casedefinition/en/. Accessed April 24, 2003.
- 8.Ministry of Health, Singapore. Enhanced precautionary measures to break SARS transmission, March 22, 2003 [press release]. Available at: http://app.moh.gov.sg/new/new02.asp. Accessed April 4, 2003.
- 9.World Health Organization. Update 70: Singapore removed from list of areas with local SARS transmission. Available at: http://www.who.int/csr/don/2003_05_30a/en/. Accessed on June 28, 2003.
- 10.World Health Organization. Affected areas: severe acute respiratory syndrome (SARS). Available at: http://www.who.int/csr/sarsareas/2003_04_02/en/. Accessed April 26, 2003.
- 11.Ministry of Health, Singapore. Singapore SARS-free for 66 days and clear of any smoldering cases. July 16, 2003, press release. Available at: http://app.moh.gov.sg/new/new02.asp. Accessed July 24, 2003.
- 12.Chen WK, Cheng YC, Ng KC. Were there enough physicians in an emergency department in the affected area after a major earthquake? An analysis of the Taiwan Chi-Chi earthquake in 1999. Ann Emerg Med. 2001;38:556–561. doi: 10.1067/mem.2001.119054. [DOI] [PubMed] [Google Scholar]
- 13.Okumura T, Suzuki K, Fukuda A. The Tokyo subway sarin attack: disaster management, part 2: hospital response. Acad Emerg Med. 1998;5:618–624. doi: 10.1111/j.1553-2712.1998.tb02471.x. [DOI] [PubMed] [Google Scholar]
- 14.Rapid assessment of injuries among survivors of the terrorist attack on the World Trade Center, New York City, September 2001MMWR Morb Mortal Wkly Rep. 2002;51:1–5. [PubMed] [Google Scholar]
- 15.Cushman JG, Pachter HL, Beaton HL. Two New York City hospitals' surgical response to the September 11, 2001, terrorist attack in New York City. J Trauma. 2003;54:147–154. doi: 10.1097/00005373-200301000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Macintyre AG, Christopher GW, Eitzen E. Weapons of mass destruction events with contaminated casualties: effective planning for health care facilities. JAMA. 2000;283:242–249. doi: 10.1001/jama.283.2.242. [DOI] [PubMed] [Google Scholar]
- 17.Rainer TH, Cameron PA, Smit DV. Evaluation of WHO criteria for identifying patients with severe acute respiratory syndrome out of hospital: prospective observational study. BMJ. 2003;326:1354–1358. doi: 10.1136/bmj.326.7403.1354. [DOI] [PMC free article] [PubMed] [Google Scholar]


