Sir,
As of February 19th, the Chinese government has converted 13 large-scale public places in Wuhan City, Hubei Province into makeshift hospitals for patients in the coronavirus disease 2019 (COVID-19) with mild symptoms and such conversion will continue to contain the spread of the COVID-19 (Table I ). However, insufficient ventilation in these makeshift hospitals may increase infection risk of opportunistic airborne transmission. This was seen in the spread of Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) [1], similar to the current novel coronavirus (SARS-CoV-2). According to the regulations in Hubei Province, the exhaust air volume in ventilation systems for makeshift hospitals is approximately 150 m3 per hour per person now [2], much lower than the guideline of 288 m3 per hour per person advised by World Health Organization (WHO) for infection control in health care for natural or mechanical ventilation system [1].
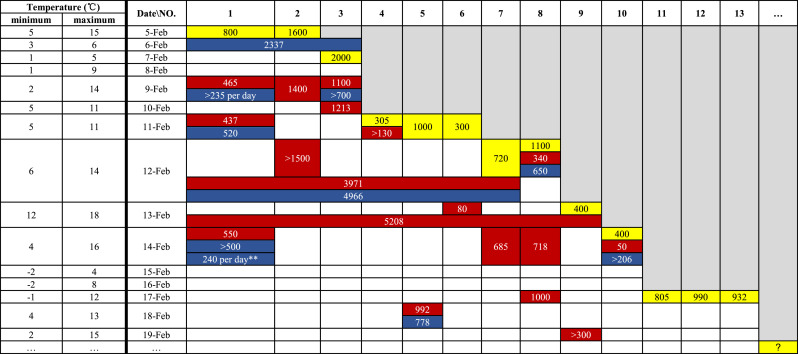
Table I.
Information about makeshift hospitals in Wuhan from 236 news articles collected by Health Knowledge Graph for COVID-19∗ and Health Commission of Hubei Province until February 19th [5]. Values in yellow represent numbers of beds provided by makeshift hospitals on the first day of patient admission, values in red represent numbers of patients, and values in blue represent numbers of health-care workers
∗ An information collection and evaluation system developed by the group of Prof. Bin Xu from Tsinghua University (website address: edukg.cn/fy).
∗∗ The number includes hospital cleaners.
Opportunistic airborne transmission usually occurs during aerosol-generating medical procedures, but a nurse wearing protection equipment was infected with SARS-CoV by the airborne virus generated from patient's coughing during treatment [3]. Although the transmission potential of SARS-CoV-2 by coughing is still unclear, 1716 health-care workers have been infected with SARS-CoV-2 and the protection for health-care workers in these makeshift hospitals is urgent [4]. Personal protective equipment and sufficient resting time may be the basic procedure.
On the other hand, the patients may also contract other diseases in the hospitals when they are being treated for COVID-19. This cross-contamination of patients should also be prevented and is also closely related to ventilation conditions inside the hospitals.
Therefore, the ventilation rates in makeshift hospitals should be increased to as high as the system can support. With more ventilation, current low outdoor temperature will increase the need for heating inside the hospitals. Air conditionings and electric blankets are necessary to keep the patients warm. There remain challenges in energy consumption to exhaust such high-volume air for hundreds of people, and risks in potential unventilated zones in the large space buildings. An alternative to increasing dilution of contaminated air is to use air purifiers to reduce the possible virus-laden aerosols. And all the filters should be collected and disposed as medical waste or disinfected thoroughly to prevent secondary contamination.
Acknowledgements
CC and BZ are grateful for Prof. Bin Xu's help on the collection of news articles, and Dr. Bin Zhou's comments and edits.
Authorship
All authors have made substantial contributions to all of the following:
(1) Chen Chen drafted the manuscript.
(2) Bin Zhao designed the conception, and revised the manuscript for the important intellectual content.
Conflict of interest statement
None.
Funding sources
CC and BZ have received funding from the Innovative Research Groups of the National Natural Science Foundation of China (51521005).
References
- 1.WHO . 2009. Natural ventilation for infection control in health-care settings.https://www.who.int/water_sanitation_health/publications/natural_ventilation/en/ [last accessed 20 February 2020] [PubMed] [Google Scholar]
- 2.Department of Housing and Urban-Rural Development of Hubei Province . 2020. Technical requirements for the design and conversion of makeshift hospitals.http://www.hubei.gov.cn/hbfb/bmdt/202002/P020200206474193410088.pdf [last accessed 20 February 2020] [Google Scholar]
- 3.Christian M.D., Loutfy M., McDonald C., Martinez K.F., Ofner M., Wong T. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerg Infect Dis. 2004;10(2):287–293. doi: 10.3201/eid1002.030700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chin J Epidemiol. 2020;41(2):145–151. [PMC free article] [PubMed] [Google Scholar]
- 5.Health Commission of Hubei Province. 2020. http://wjw.hubei.gov.cn/ [last accessed 20 February 2020]