Abstract
Background
Lifetime use of bituminous (‘smoky’) coal is associated with nearly a 100-fold higher risk of lung cancer mortality compared with anthracite (‘smokeless’) coal use in rural Xuanwei, China, among women. Risk of mortality from ischaemic heart disease (IHD) and stroke for these coal types has not been evaluated.
Methods
A cohort of 16 323 non-smoking women in Xuanwei, who were lifetime users of either smoky or smokeless coal, were followed up from 1976 to 2011. We estimated hazard ratios (HRs) and 95% confidence intervals (CI) to evaluate lifetime use of coal types and stoves in the home in relation to risk of IHD and stroke mortality.
Results
Among lifetime users of smokeless coal, higher average exposure intensity (≥4 tons/year vs <2.5 tons/year, HR = 7.9, 95% CI = 3.5–17.8; Ptrend =<0.0001) and cumulative exposure (>64 ton-years vs ≤28 ton-years, HR = 6.5, 95% CI = 1.5–28.3; Ptrend =0.003) during follow-up and over their lifetime was associated with increased IHD mortality, and ventilated stove use dramatically reduced this risk (HR = 0.2, 95% CI 0.1–0.5). Higher cumulative exposure to smoky coal during follow-up showed positive associations with IHD mortality, but the evidence for other metrics was less consistent compared with associations with smokeless coal use.
Conclusions
Higher use of smokeless coal, which is burned throughout China and is generally regarded to be a cleaner fuel type, is associated with IHD mortality. Use of cleaner fuels or stove interventions may be effective in reducing the increasing burden of IHD in developing regions that currently rely on smokeless coal for cooking and heating.
Keywords: Solid fuels, coal, cardiovascular disease, indoor air pollution, Chinese cohort, stove improvement
Key Messages
Smokeless coal use was associated with increased risk of ischaemic heart disease (IHD) mortality, and improving household ventilation strongly decreased this risk.
The associations with IHD mortality were stronger for use of smokeless than for smoky coal.
Our findings suggest that smokeless coal should not be considered a safer alternative to smoky coal.
Introduction
Emissions from burning solid fuels for cooking and heating substantially contribute to the global disease burden, accounting for over four million annual deaths worldwide, particularly in low- and middle-income countries.1 Emerging epidemiological evidence suggests that burning solid fuels may increase the risk of ischaemic heart disease (IHD) and/or stroke, the burden of which is rapidly increasing in developing countries.1–5 Cardiovascular disease (CVD) is the leading cause of death worldwide, with over 75% of these deaths occurring in low- and middle-income countries. IHD and stroke account for nearly 85% of CVD deaths.6 In China, mortality rates from IHD and stroke are increased in both men and women, particularly in rural areas.4,7 Whereas China has one of the highest smoking rates among men in the world, only ∼2% of women smoke tobacco, suggesting that other factors contribute to the increased mortality rates among women.4
Risk of IHD and stroke mortality in relation to coal use has been evaluated in two large population-based cohort studies. Among ∼73 000 predominantly never-smoking Chinese women in the Shanghai Women’s Health Study (SWHS),2 an exposure-response relationship between longer duration of domestic coal use and risk of mortality from IHD, but not from stroke, was observed.2 This risk of mortality from IHD decreased monotonically with increasing number of years since last use.2 In the Kadoorie Biobank cohort, which included ∼271 000 adults enrolled from five rural areas in China, an increased risk of stroke and to a lesser extent IHD mortality was found for self-reported use of solid fuels, with stronger associations observed for use of wood than for coal.3
To follow up on these findings for coal use and IHD and stroke mortality, we identified a unique population in rural Xuanwei, China, who continue to use coal for indoor cooking and heating. In Xuanwei, residents primarily use either of two distinct types of coal that differ with respect to composition and combustion characteristics.8 These include bituminous (‘smoky’) coal, which contains a tarlike substance called bitumen, and anthracite (‘smokeless’) coal, which has a comparatively higher carbon content and generates less smoke when burned. The lifetime use of smoky relative to smokeless coal was associated with nearly a 100-fold higher risk of lung cancer mortality among women enrolled in a large cohort in Xuanwei.9 Further, changing from using an unvented firepit to a portable stove or stove with chimney reduced the risk of lung cancer by nearly 50% in this cohort.10 The risk of IHD and stroke mortality in relation to coal use and improving ventilation has not previously been evaluated in this population. Further, previous epidemiological studies have not evaluated whether the risk of these outcomes may differ based on coal type. Substantial aetiological heterogeneity based on the type of coal being used in Xuanwei has been reported for risk of lung cancer mortality, thus raising the plausibility of differential effects by coal type for other disease outcomes as well.9,11 We evaluated the risk of mortality from IHD and stroke stratified by lifetime and exclusive use of smoky or smokeless coal among non-smoking women in the Xuanwei cohort, with 35 years of follow-up (1976–2011).
Methods
Study population and outcome ascertainment
The design and population of the Xuanwei cohort have been described previously.9,10 Briefly, the study area comprised three communes in which smoky coal was the main fuel source, and one commune in which smokeless coal was the main fuel source. A review of administrative records was conducted in 1992 to identify all people born between 1917 and 1951, who lived in the study area. The overall cohort included 42 420 participants (age range 25 to 59 years at cohort entry) who were alive as of 1 January 1976, including a subcohort of 20 719 women nearly all of whom were non-smokers at baseline (n = 20 658; 99.7%) and who are the focus of the current study.
The date and cause of death for participants in the cohort over the follow-up period (1 January 1976 to 31 December 2011) were obtained from hospital records and death certificates. In Xuanwei, each commune or ‘administrative village’ typically has one or a small number of doctors who oversee the medical care of residents in their jurisdiction, and these doctors are generally very familiar with the medical histories of the residents. When a death is reported in a certain commune, the cause of death is reviewed by the local doctor in collaboration with the Xuanwei Center for Disease Control, and is assigned an ICD-9 code that is based on the official hospital-determined cause of death or on a review of the medical history and reported symptoms of the subject as determined from interviews with next of kin (for deaths occurring outside hospital). Causes of death were coded by the Xuanwei Center for Disease Control according to the International Classification of Diseases, 9th Revision (ICD-9), including for IHD (ICD-9: 410–414) and stroke (ICD-9: 430–438). The study was approved by the Institutional Review Board of the Chinese Academy of Preventive Medicine. Informed consent was obtained from all participants or their proxies if they could not understand the written consent form.
Exposure measures
In 1992, trained interviewers administered a standardized questionnaire directly to the non-smoking women (n = 12 487, 60%) or to her surrogate respondent (n = 8171, 40%). The questionnaire assessed lifetime residential history, household stove and fuel use, cooking practices, average time spent inside the home, average number of rooms and people in each residence, education and active smoking history. Participants or their proxies were asked to report the primary fuel source, the amount/tons of coal used and the type of stove that was used in the main living area (none, unvented fire pit, portable stove, stove with chimney or stove without chimney) for each residence over their entire lifetime. Participants were assigned the same exposure information for each year corresponding to the total number of years in a particular residence. Between 2009 and 2011, follow-up questionnaire information was collected for the non-smoking women who were still alive after 1992 (n = 16 292), except for 1395 participants who were lost to follow-up after 1992 and had no additional exposure information. The questionnaire information for the follow-up was collected either from self-report (26%) or surrogate respondents (74%), and included the same variables as the baseline questionnaire for the period 1992–2011. Based on these questionnaire responses, participants were classified as lifetime and exclusive smoky or smokeless coal users if they only reported primary use of these coal types, respectively, throughout their lifetime. Participants who used a combination of smoky and smokeless coal during their life, but no other fuel types, were classified as mixed coal users. Of the original 20 658 non-smoking women, 16 323 participants who were lifetime users of either smoky or smokeless coal were included in the analyses. Among these women, 11 188 and 1954 participants exclusively used smoky and smokeless coal, respectively, and the remaining women used a mix of both smoky and smokeless coal through the end of their follow-up (see supplementary material, available as Supplementary data at IJE).
The reported information on amount of coal use per year from the questionnaire was used to construct time-dependent average and cumulative coal use variables for each participant for two different time periods: during the cohort follow-up period (1976–2011) and for their entire lifetime starting at birth. The approach of using exposure information during follow-up only was used to minimize exposure misclassification that may result from having to recall specific amounts of coal use in early life and to account for a hypothesized shorter latency between air pollution exposure and mortality from IHD and stroke.12,13 In our previous study in Shanghai, an attenuation in risk of IHD mortality with increasing number of years since last use of coal was observed, indicating that more recent exposure may be important for this outcome.2
Statistical analysis
Mortality rates for IHD and stroke among non-smoking women in Xuanwei were calculated in lifetime and exclusive users of smoky and smokeless coal separately, and were age-adjusted to the World Standard population. For comparison, age-adjusted rates were also calculated for non-smoking women from the SWHS (see supplementary material, available as Supplementary data at IJE online).2 Cumulative incidence functions of IHD and stroke mortality which accounted for competing causes of death14 were also calculated in Xuanwei to evaluate the absolute risks of mortality from IHD and stroke in lifetime and exclusive users of smoky and smokeless coal across the full cohort follow-up period.
We estimated cause-specific hazard ratios (HRs) and 95% confidence intervals (CIs) for risk of IHD and stroke mortality in relation to time-dependent cumulative and average tons of coal use, as well as for stove use (see supplementary material, available as Supplementary data at IJE online). In estimating these cause-specific HRs, all subjects were included in each model, and deaths due to any cause other than the specific outcome variables (i.e. IHD or stroke) were treated as censored observations. Cumulative tons of coal use during follow-up only and for the entire lifetime were analysed based on tertiles of exposure in lifetime and exclusive users of smoky and smokeless coal combined, with the lowest tertile used as the reference. The highest tertiles were further subdivided based on the intracategory medians to evaluate associations across a greater range of exposure levels. For analyses of average intensity of coal use, this variable was categorized as follows: <2.5 tons (reference; 25th percentile in lifetime and exclusive users of smoky and smokeless coal users combined), 2.5–<4 average tons used per year (25th–75th percentiles) and ≥4 average tons used per year (≥75th percentile). Tests for trend were conducted by modelling a continuous ordinal variable corresponding to each of the exposure categories.
Stove improvement was analysed as a time-dependent variable to evaluate the risk of IHD and stroke mortality in relation to use of ventilated stoves in the home. For these analyses, the study population was restricted to participants who had a permanent change to a stove with a chimney or portable stove, or those who did not use either of these ventilated stoves at any time in their life (reference group). Those who changed to using either a stove with chimney or a portable stove, but subsequently went back to using an unvented stove (‘non-permanent’ users), were excluded from this primary analysis (n = 2395). We also conducted analyses for stove use that included all lifetime smoky or smokeless coal users, regardless of whether they were non-permanent ventilated stove users.
Analyses for the coal and stove use metrics were initially conducted for smoky and smokeless coal users combined, which included lifetime and exclusive smoky or smokeless coal users, respectively, as well as mixed coal users who used both of these coal types in their lifetime. Tests for multiplicative interaction between the main exposures and coal type (i.e. smoky or smokeless) were conducted by including cross-product terms in the models. Separate models were then fitted for lifetime and exclusive users of smoky and smokeless coal which excluded mixed coal users. We also conducted several additional secondary analyses. Analyses for cumulative and average coal use which combined lifetime smoky and smokeless coal users in one model (excluding mixed coal users) were conducted using the previously described cut-points, with the lowest category of smoky coal use as the reference group. We conducted stratified analyses restricting the models evaluating coal metrics to the two communes that used smoky coal from Laibin, a prefecture-level city in Xuanwei. Smoky coal from this area is particularly toxic and has previously been reported to be associated with the highest risk of lung cancer relative to smoky coal from other geographical areas in Xuanwei.15 In addition, sensitivity analyses for average coal use were conducted during the prospective follow-up period separately (1992–2011).
Coal use and stove improvement variables were mutually adjusted for each other in the respective models. Additional covariates in the models were categorized as follows: education (no formal vs formal education); study period (retrospective follow-up: 1976–92, prospective follow-up: 1992–2011); birth cohort [1917–21 (ref.), 1922–26, 1927–31, 1932–36, 1937–41, 1942–46, 1946–51]; average number of hours spent indoors doing activities other than sleeping (time-dependent continuous); average number of rooms and people living in the same home as the subject (time-dependent continuous); a time-dependent categorical variable for cumulative years of cooking [<20 years (ref.), 20–40 years, >40 years] and continuous baseline age to account for potential residual confounding within the stratified age groups (see supplementary material, available as Supplementary data at IJE online). Education was used as the main proxy for socioeconomic status (SES) since the variability of other indices such as income is limited in this population. A four-level variable for educational attainment was originally assessed on the questionnaire (no education, primary school only, middle school only and attended university or higher). Among the individuals included in our analysis, 98% reported either not having any formal education (76%) or attending primary school only (22%). A small percentage of subjects attended middle school or higher, and the primary differences between lifetime smoky and smokeless coal users were for not having any formal education vs attending primary school (i.e. the proportion attending middle school or university are comparable between the groups). Given these proportions, we collapsed education into the binary variable (formal education vs no formal education). Models for cumulative and average coal use, which combined lifetime smoky and smokeless coal users in one model with a common referent, were also adjusted for commune of residence to control for potential community-level differences. Analyses were conducted using SAS version 9.4.
Results
Subject characteristics
The mean (± standard deviation) ages in years at entry into the cohort were 39.4 (10.6) for lifetime smoky coal users and 44.3 (11.2) for lifetime smokeless coal users, and mean ages in years at the end of follow-up were 63.8 (10.8) and 66.3 (11.4), respectively (Table 1). The mean age at death from IHD and stroke was 68.2 (11.4) and 64.5 (11.2) years in lifetime smoky coal users and 69.0 (11.4) and 69.8 (11.1) years in lifetime smokeless coal users, respectively. Smoky and smokeless coal users had generally similar fuel use and home characteristics (Table 1). About 90% of non-smoking women in the analysis ever used a portable stove or stove with chimney in their lifetime, and nearly all women cooked in the home, for an average of about 47 years. A minority of women in the study population had a formal education (23.2% in smoky coal users and 14.6% in smokeless coal users). Surrogate measures for SES, such as average number of rooms and people in the home, were very similar across coal exposure tertiles for smoky and smokeless coal users (Supplementary Table 1, available as Supplementary data at IJE online). There was a tendency for subjects in the highest tertiles to have more formal education than those in the lowest exposure tertiles (Supplementary Table 1, available as Supplementary data at IJE online).
Table 1.
Characteristics of lifetime smoky and smokeless coal users among non-smoking women in Xuanwei, China, 1976–2011
| Lifetime smoky or smokeless coal usea | Lifetime and exclusive smoky coal use | Lifetime and exclusive smokeless coal use | |
|---|---|---|---|
| Follow-up characteristics | |||
| Number of lifetime coal users, retrospective + prospective follow-up (1976–2011), n | 16 323 | 11 188 | 1954 |
| Person-years of follow-up, 1976–2011, n | 439 003 | 283 638 | 45 051 |
| Mean age at entry into follow-up ± SD | 39.4 (10.6) | 39.4 (10.6) | 44.3 (11.2) |
| Mean age at end of follow-up ± SD | 65.3 (10.8) | 63.8 (10.8) | 66.3 (11.4) |
| Mortality characteristics | |||
| Mean age at death from ischaemic heart disease ± SD | 69.2 (11.6) | 68.2 (11.4) | 69.0 (11.4) |
| Mean age at death from stroke ± SD | 66.7 (11.5) | 64.5 (11.2) | 69.8 (11.1) |
| Ischaemic heart disease (ICD 410–414), n/age-adjusted mortality rate per 100 000 | 105/20.9 | 59/20.4 | 34/53.3 |
| Cerebrovascular disease (ICD 430–438), n/age-adjusted mortality rate per 100 000 | 363/68.1 | 243/73.2 | 89/138.2 |
| Stove use characteristics | |||
| Never stove improvement, n (%) | 1596 (10) | 1316 (12) | 241 (12) |
| Improvement to portable stove or stove with chimney, n (%) | 14 728 (90) | 9872 (88) | 1713 (88) |
| Other lifestyle and demographic characteristics | |||
| Mean no. of rooms in home during lifetime ± SD | 2 (1) | 2 (1) | 2 (1) |
| Mean no. of people in home during lifetime ± SD | 5 (1) | 5 (1) | 4 (2) |
| Mean no. of hours spent inside the home doing activities while awake ± SD | 7.3 (2.0) | 7.7 (1.9) | 7.7 (1.9) |
| Mean tons of coal used per year during follow-up ± SD | 3.2 (1.1) | 3.4 (1.0) | 2.8 (1.6) |
| Mean cumulative tons of coal used during follow-up ± SD | 42.5 (22.1) | 43.0 (22.0) | 32.0 (23.4) |
| Had any formal education (primary school or higher), n (%) | 3898 (23.9) | 2600 (23.2) | 286 (14.6) |
| Ever cooked food during lifetime, n (%) | 16 002 (98.0) | 10 940 (97.8) | 1933 (98.9) |
| Cumulative years of cooking during lifetime among ever cookers ± SD | 47.8 (11.0) | 46.7 (11.1) | 47.9 (11.5) |
Includes participants who used exclusively smoky or smokeless coal through to the end of their follow-up, as well as those who used a mix of smoky and smokeless coal through to the end of their follow-up.
Absolute risk and mortality rates of IHD and stroke
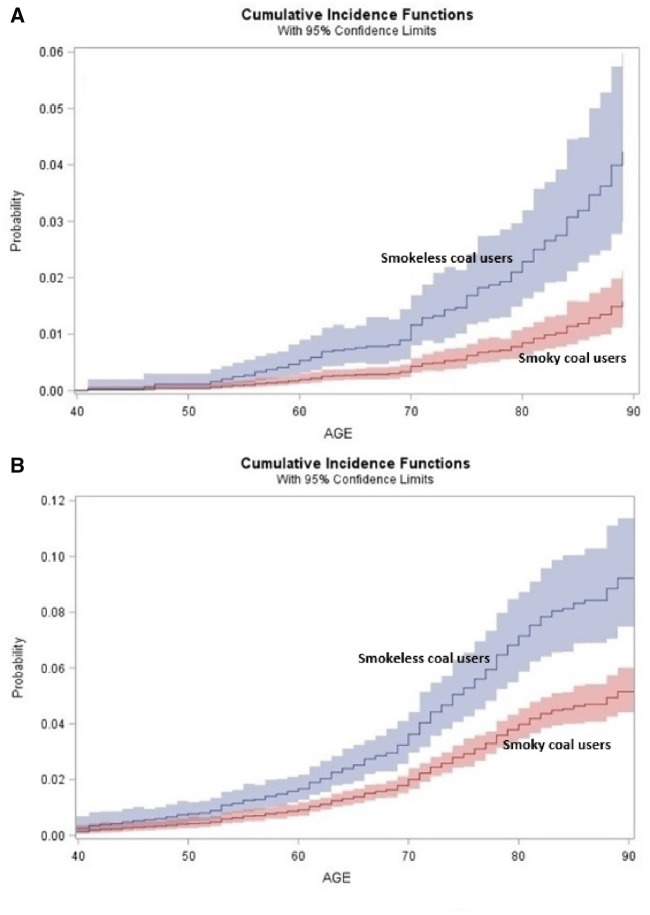
The absolute risks of mortality from IHD and stroke in Xuanwei were higher in lifetime and exclusive smokeless coal users compared with lifetime and exclusive smoky coal users, particularly after 70 years of age (Figure 1). In lifetime smoky coal users, overall age-adjusted mortality rates of IHD and stroke were 20.4 deaths/100 000 person-years and 73.2 deaths/100 000 person-years, respectively, and in lifetime smokeless coal users were 53.3 deaths/100 000 person-years and 138.2 deaths/100 000 person-years, respectively (Table 1). Mortality rates of IHD and stroke among those ≥50 years of age were similar among non-smoking women in Shanghai and Xuanwei smoky coal users and were about three times higher in smokeless coal users compared with each of these groups (Figure 2). The mortality rate ratios comparing lifetime smokeless coal users with women in Shanghai were 2.9 (95% CI = 1.6–5.0) for IHD and 3.1 (95% CI = 2.2–4.3) for stroke (Figure 2).
Figure 1.
A, B Absolute risk of mortality from ischaemic heart disease (A) and stroke (B) in the Xuanwei cohort (1976–2011) stratified by coal type. Lines and shaded boxes depict the cumulative probability and 95% confidence intervals for mortality from ischaemic heart disease and stroke among lifetime and exclusive smoky and smokeless coal users in Xuanwei.
Figure 2.
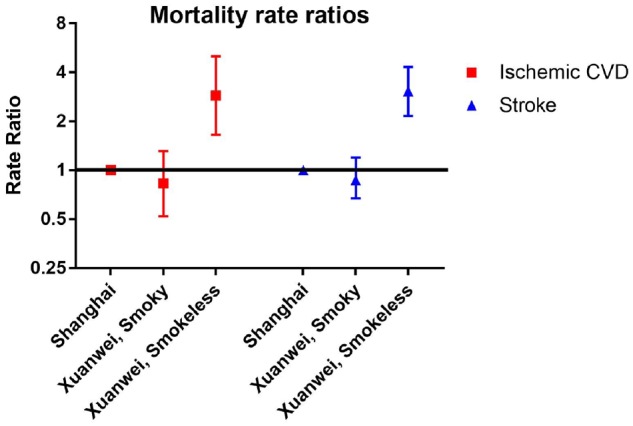
Mortality rate ratios and 95% confidence intervals for ischaemic heart disease and stroke comparing lifetime and exclusive users of smoky and smokeless coal in Xuanwei and Shanghai women. Overall rates for subjects aged ≥50 years were calculated and age-adjusted to the World Standard population using four age categories (50–59, 60–69, 70–79, 80+ years).
Cumulative exposure to coal and risk of IHD and stroke mortality
Analyses of cumulative ton-years of coal use during the follow-up period among lifetime users of smoky or smokeless coal combined suggested an exposure-response association for IHD mortality (tertile 3 vs 1, HR = 5.3, 95% CI = 1.9–15.1; Ptrend = 0.0008), but not for stroke (tertile 3 vs 1, HR = 1.2, 95% CI = 0.8–1.9; Ptrend=0.39) (Table 2). Higher cumulative ton-years of coal use during follow-up were associated with IHD mortality among both lifetime smoky (HR = 3.6, 95% CI = 1.1–11.8; Ptrend = 0.13) and smokeless (HR = 6.5, 95% CI = 1.5–28.3; Ptrend = 0.003) coal users individually (P-heterogeneity = 0.16) (Table 2; and Supplementary Table 2, available as Supplementary data at IJE online).
Table 2.
Cumulative coal use during follow-up and risk of ischemic heart disease and stroke mortality among non-smoking women in the Xuanwei cohort, 1976–2011
| Ischaemic heart disease cases | HR (95% CI)a | P-value | Stroke cases | HR (95% CI)a | P-value | |
|---|---|---|---|---|---|---|
| Lifetime smoky or smokeless coal users | ||||||
| Tertile 1 (≤28 ton-years) | 10 | 1.0 (ref) | 76 | 1.0 (ref) | ||
| Tertile 2 (29–64 ton-years) | 30 | 2.6 (1.1–6.4) | 0.04 | 144 | 1.2 (0.9–1.7) | 0.30 |
| Tertile 3 (>64 ton-years) | 65 | 5.3 (1.9–15.1) | 0.002 | 143 | 1.2 (0.8–1.9) | 0.34 |
| >64–85 ton-years | 28 | 4.9 (1.7–14.2) | 0.004 | 77 | 1.2 (0.8–1.7) | 0.34 |
| >85 ton-years | 37 | 6.8 (2.2–21.3) | 0.001 | 66 | 1.1 (0.7–1.8) | 0.64 |
| P-trend | 0.0008 | 0.39 | ||||
| P-heterogeneity (coal type)b | 0.16 | <0.0001 | ||||
| Lifetime and exclusive smoky coal users | ||||||
| ≤28 ton-years | 5 | 1.0 (ref) | 56 | 1.0 (ref) | ||
| 29–64 ton-years | 19 | 3.0 (1.1–8.0) | 0.03 | 97 | 1.1 (0.8–1.7) | 0.52 |
| >64 ton-years | 35 | 3.6 (1.1–11.8) | 0.03 | 90 | 0.9 (0.5–1.5) | 0.65 |
| >64–85 ton-years | 20 | 3.8 (1.2–12.1) | 0.02 | 47 | 0.9 (0.5–1.6) | 0.75 |
| >85 ton-years | 15 | 2.7 (0.7–10.4) | 0.16 | 43 | 0.8 (0.4–1.4) | 0.44 |
| P-trend | 0.13 | 0.54 | ||||
| Lifetime and exclusive smokeless coal users | ||||||
| ≤28 ton-years | 5 | 1.0 (ref) | 18 | 1.0 (ref) | ||
| 29–64 ton-years | 8 | 2.1 (0.5–9.3) | 0.32 | 33 | 1.4 (0.7–2.8) | 0.37 |
| >64 ton-years | 21 | 6.5 (1.5–28.3) | 0.01 | 38 | 1.8 (0.8–3.9) | 0.13 |
| >64–85 ton-years | 6 | 4.3 (0.8–22.7) | 0.08 | 19 | 1.9 (0.8–4.2) | 0.14 |
| >85 ton-years | 15 | 9.8 (2.1–45.8) | 0.004 | 19 | 1.7 (0.8–4.0) | 0.19 |
| P-trend | 0.003 | 0.11 |
Adjusted for education (categorical variable no formal school vs any formal school), birth cohort [categorical six-level variable: 1917–21 (ref.), 1922–26, 1927–31, 1932–36, 1937–41, 1942–46, 1947–51], use of a portable stove or stove with chimney (time-dependent variable categorized as ‘1’ for ages when either stove type was used), cumulative years of cooking (<20, 20–40, >40 years), average number of hours spent indoors doing activities other than sleeping (continuous time-dependent variable), average number of rooms in home during lifetime (continuous time-dependent), average number of people in home during lifetime (continuous time-dependent), follow-up period (retrospective or prospective follow-up) and age.
P-heterogeneity calculated including cross-product terms (cumulative coal use x coal type) in models that only included lifetime and exclusive users of smoky and smokeless coal users.
Among smokeless coal users, the strongest risk of IHD mortality was seen among women with the highest cumulative exposure during follow-up (>85 ton-years, HR = 9.8, 95% CI = 2.1–45.8), whereas a clear monotonic exposure-response relationship with increasing cumulative levels was not observed among smoky coal users (Table 2). The association between cumulative exposure to smokeless coal during follow-up and IHD mortality became even stronger when using ≤28 ton-years/smoky coal as the reference group (HR for >64 ton-years/smokeless coal =17.2, 95% CI = 5.4–54.9; Supplementary Table 3, available as Supplementary data at IJE online). Consistent associations with IHD mortality were also observed for higher cumulative levels of smokeless coal use over the entire lifetime (>196 ton-years, HR = 4.9, 95% CI = 1.9–12.9) and when comparing the highest lifetime cumulative levels of smokeless coal use with the lowest lifetime cumulative levels of smoky coal use (HR = 3.4, 95% CI = 1.5–7.9), but risk of IHD mortality was not increased in relation to cumulative lifetime coal use among smoky coal users (Supplementary Tables 2–4, available as Supplementary data at IJE online).
An increased risk of stroke mortality was observed for lifetime users of smokeless coal with higher cumulative exposures during follow-up (>85 ton-years, HR = 1.7, 95% CI = 0.8–4.0; Ptrend =0.11) and across the lifetime (>196 ton-years, HR = 1.9, 95% CI = 1.1–3.3; Ptrend = 0.03; Table 2 and Supplementary Table 4, available as Supplementary data at IJE online). Among lifetime smokeless coal users, positive associations with stroke mortality were also observed for higher average and cumulative use of coal when the lowest categories of smoky coal were the referent, particularly after adjusting for commune of residence (Supplementary Table 3, available as Supplementary data at IJE online). No association with stroke mortality was observed in relation to cumulative exposure either during follow-up or across the lifetime among smoky coal users (Table 2; and Supplementary Tables 2–4, available as Supplementary data at IJE online).
Average intensity of coal use and risk of IHD and stroke mortality
Among lifetime smoky or smokeless coal users combined, women with the highest average intensity of coal use during follow-up had an increased risk of IHD mortality (HR = 3.7, 95% CI = 2.1–6.5 for ≥4 tons vs <2.5 tons per year; Ptrend =<0.0001), but not for stroke mortality (Table 3). There was evidence of heterogeneity in the IHD association by coal type (P-heterogeneity = 0.005). An exposure-response association between increasing average intensity of coal use during follow-up and risk of IHD mortality was evident (HR = 7.9, 95% CI = 3.5–17.8 for ≥ 4 tons/year vs <2.5 tons/year; Ptrend <0.0001) among lifetime users of smokeless coal, but not for lifetime smoky coal users (Table 3; Supplementary Table 2, available as Supplementary data at IJE online). For stroke mortality, no exposure-response relationship was evident for average intensity of coal use during follow-up among smoky (Ptrend = 0.85) or smokeless (Ptrend = 0.33) coal users, although a positive association was observed among smokeless coal users comparing 2.5-<4 tons/year vs <2.5 tons/year on average (Table 3). Compared with participants who used <2.5 tons of smoky coal per year either during follow-up or across the lifetime, smokeless coal users who used >4 tons/year had a higher risk of IHD mortality (Supplementary Table 3, available as Supplementary data at IJE online). Similar results for average coal use were also observed among lifetime smokeless coal users in analyses that considered lifetime exposure (Supplementary Table 4, available as Supplementary data at IJE online) and in those restricted to the prospective follow-up period (Supplementary Table 5, available as Supplementary data at IJE online).
Table 3.
Average intensity of coal use during follow-up and risk of ischaemic heart disease and stroke mortality among non-smoking women in the Xuanwei cohort, 1976–2011
| Ischaemic heart disease cases | HR (95% CI)a | P-value | Stroke cases | HR (95% CI)a | P-value | |
|---|---|---|---|---|---|---|
| Lifetime smoky or smokeless coal users | ||||||
| <2.5 tons/year | 28 | 1.0 (ref) | 132 | 1.0 (ref) | ||
| 2.5–<4 tons/year | 47 | 1.7 (1.1–2.8) | 0.03 | 156 | 1.1 (0.9–1.5) | 0.29 |
| ≥4 tons/year | 30 | 3.7 (2.1–6.5) | <0.0001 | 75 | 1.2 (0.9–1.7) | 0.27 |
| P-trend | <0.0001 | 0.22 | ||||
| P-heterogeneity (coal type)b | 0.005 | 0.84 | ||||
| Lifetime and exclusive smoky coal users | ||||||
| <2.5 tons/year | 14 | 1.0 (ref) | 72 | 1.0 (ref) | ||
| 2.5–<4 tons/year | 35 | 1.5 (0.8–2.9) | 0.23 | 109 | 0.9 (0.7–1.2) | 0.44 |
| ≥4 tons/year | 10 | 1.5 (0.6–3.5) | 0.40 | 62 | 1.0 (0.7–1.4) | 0.92 |
| P-trend | 0.29 | 0.85 | ||||
| Lifetime and exclusive smokeless coal users | ||||||
| <2.5 tons/year | 8 | 1.0 (ref) | 41 | 1.0 (ref) | ||
| 2.5–<4 tons/year | 9 | 2.1 (0.8–5.6) | 0.12 | 35 | 1.6 (1.0–2.6) | 0.04 |
| ≥4 tons/year | 17 | 7.9 (3.5–17.8) | <0.0001 | 13 | 1.1 (0.6–2.2) | 0.78 |
| P-trend | <0.0001 | 0.33 |
Adjusted for education (categorical variable no formal school vs any formal school), birth cohort [categorical six-level variable: 1917–21 (ref.), 1922–26, 1927–31, 1932–36, 1937–41, 1942–46, 1947–51], use of a portable stove or stove with chimney (time-dependent variable categorized as ‘1’ for ages when either stove type was used), cumulative years of cooking (<20, 20–40, >40 years), average number of hours spent indoors doing activities other than sleeping (continuous time-dependent variable), average number of rooms in home during lifetime (continuous time-dependent), average number of people in home during lifetime (continuous time-dependent), follow-up period (retrospective or prospective follow-up) and age.
P-heterogeneity calculated including cross-product terms (average intensity of coal use x coal type) in models that only included lifetime and exclusive users of smoky and smokeless coal users.
Stove use and risk of IHD and stroke mortality
Among lifetime users of smoky or smokeless coal combined, changing permanently to the use of a portable stove or stove with chimney in the primary living area was associated with a substantially reduced risk of IHD mortality (HR = 0.4, 95% CI = 0.2–0.7). In contrast, no reduction in risk for stroke mortality was observed when changing to a portable stove or stove with chimney (Table 4). There was no statistical evidence of heterogeneity in these associations according to coal type (P-heterogeneity = 0.15 for IHD and stroke). Among exclusive smoky coal users, changing permanently to a portable or vented stove was associated with a reduction in IHD mortality (HR = 0.6, 95% CI = 0.2–1.4), but not for stroke mortality. Among smokeless coal users, changing permanently to the use of a portable or vented stove was strongly associated with reduced risk of IHD mortality (HR = 0.2, 95% CI = 0.1–0.5), but not for stroke mortality (Table 4). In analyses that did not exclude non-permanent ventilated stove users, the magnitudes of the HRs for associations between IHD mortality and ventilated stove use were slightly weaker but remained strongly protective among lifetime smokeless coal users (HR = 0.3, 95% CI = 0.1–0.6; Supplementary Table 6, available as Supplementary data at IJE online).
Table 4.
Changing to the use of a portable stove or stove with chimney among lifetime smoky and smokeless coal users and risk of ischaemic heart disease and stroke mortality among women in the Xuanwei cohort, 1976–2011
| No stove intervention/change |
Any stove change/intervention HR(95% CI)a,b |
P-value | P-heterogeneity (coal type)c | |||
|---|---|---|---|---|---|---|
| # cases | HR (95% CI) | # cases | HR (95% CI) | |||
| Lifetime smoky or smokeless coal users | ||||||
| Ischaemic heart disease | 14 | 1.0 (ref) | 76 | 0.4 (0.2–0.7) | 0.002 | 0.15 |
| Stroke | 34 | 1.0 (ref) | 286 | 1.2 (0.8–1.7) | 0.48 | 0.15 |
| Lifetime and exclusive smoky coal users | ||||||
| Ischaemic heart disease | 7 | 1.0 (ref) | 41 | 0.6 (0.2–1.4) | 0.23 | |
| Stroke | 30 | 1.0 (ref) | 192 | 1.2 (0.8–1.8) | 0.43 | |
| Lifetime and exclusive smokeless coal users | ||||||
| Ischaemic heart disease | 7 | 1.0 (ref) | 24 | 0.2 (0.1–0.5) | 0.001 | |
| Stroke | 4 | 1.0 (ref) | 72 | 1.3 (0.4–4.1) | 0.62 | |
Analyses for any stove improvement include subjects who changed to using either a portable stove or stove with chimney (including subjects who used both of these stove types at some point in their life). Models exclude subjects who did not permanently use these stoves after the intervention.
Adjusted for education (categorical variable no formal school vs any formal school), birth cohort [categorical six-level variable: 1917–21 (ref.), 1922–26, 1927–31, 1932–36, 1937–41, 1942–46, 1947–51), average tonnage of smoky or smokeless coal use for given year (time-dependent variable), cumulative years of cooking (<20, 20–40, >40 years), average number of hours spent indoors doing activities other than sleeping (continuous time-dependent variable), average number of rooms in home during lifetime, average number of people in home during lifetime, follow-up period (retrospective or prospective follow-up) and age.
P-heterogeneity calculated including cross-product terms (stove improvement x coal type) in models that only included lifetime and exclusive users of smoky and smokeless coal users.
Discussion
This is the first study to our knowledge to evaluate whether distinct types of coal are associated with risk of IHD and stroke mortality. We observed that age-adjusted mortality rates of IHD and stroke were higher among lifetime smokeless coal users compared with lifetime smoky coal users in Xuanwei as well as in non-smoking women in Shanghai. For both higher average intensity and cumulative ton-years of smokeless coal use during follow-up and across the lifetime, we found exposure-response associations with IHD mortality, with suggestive but less consistent evidence for stroke. Improved ventilation when cooking or heating with smokeless coal strongly reduced the risk of IHD, but not of stroke. Collectively, these findings suggest that the use of smokeless coal, which is generally regarded to be a ‘cleaner’ fuel source relative to smoky coal, may be associated with increased mortality from IHD and possibly stroke. Associations between lifetime smoky coal use and IHD mortality were suggestive but were less consistent compared with lifetime smokeless coal use.
Among lifetime and exclusive smokeless coal users, there were consistent exposure-response associations with IHD mortality for cumulative exposure and higher intensity of coal use, along with a reduction in IHD risk following use of ventilated stoves. These findings suggest that the elevated IHD mortality rates in these women compared with smoky coal users in Xuanwei and non-smoking women in Shanghai are likely due to their use of this coal type. Although suggestive associations with stroke mortality were apparent for higher cumulative tons of smokeless coal use, the associations were weaker than for IHD mortality, and ventilated stove use was not found to reduce this risk. This finding could potentially indicate that some combustion components of smokeless coal are more strongly associated with IHD than stroke, or that levels of certain coal components specifically associated with stroke (but not IHD) are not adequately reduced following ventilation. Alternatively, a potential explanation for the null or weaker findings for stroke mortality in our analysis could relate to different aetiological factors associated with specific stroke subtypes (i.e. ischaemic and haemorrhagic stroke).16 We were unable to evaluate associations by stroke subtype, given the relatively small number of cases and the limited confirmation of subtype diagnoses in rural Xuanwei.
Among lifetime and exclusive smoky coal users, improving ventilation through the use of a portable stove or stove with a chimney has been reported to substantially reduce the risk of lung cancer,10 as well as of pneumonia17 and chronic obstructive pulmonary disease.18 In the current study, women who had higher cumulative levels and intensity of smoky coal use during follow-up had an increased risk of IHD mortality, and improved ventilation reduced this risk, but this higher risk was not apparent for coal metrics that integrated exposure information from across the entire lifetime. Stronger associations with IHD mortality for smokeless coal users in Xuanwei could reflect the specific constituents that are emitted when burning smokeless vs smoky coal. For example, levels of NO2 and SO2 are higher in homes burning smokeless coal relative to smoky coal,19 and ambient levels of these gaseous pollutants have each been associated with risk of IHD in studies conducted in China.20–22
A previous exposure assessment study in Xuanwei found that improving ventilation in homes burning smokeless coal reduced indoor levels of SO2.19 Mechanistically, data from rat models have suggested that SO2 exposure contributes to increased reactive oxygen species in cardiac muscle, leading to mitochondrial dysfunction and abnormal left ventricular function.23 Homes burning smokeless coal also contain comparatively higher levels of certain metals such as aluminum, titanium and barium, which were associated with incident coronary heart disease in a large Chinese cohort.24 Other ambient pollutants that may be associated with IHD, such as PM2.5 and polycyclic aromatic hydrocarbons (PAHs),20,21 have also been demonstrated to be significantly lower in homes following improvement in ventilation.25,26 Alternatively, the stronger associations for IHD mortality in smokeless coal users could be due to some other pollutant (that is higher in homes burning smokeless coal) that we have not yet directly measured in homes in Xuanwei.
Second, the mortality burden among smoky coal users in Xuanwei is very unique and is driven by lung cancer, given the nearly 100-fold higher risk of lung cancer mortality among women who use this type of coal9 (i.e. 40% of deaths among smoky coal users are due to cancer, and 90% of these are lung cancers). The mean age of lung cancer death among smoky coal users in Xuanwei is also nearly a decade earlier compared with Western countries (59 years in Xuanwei) and is also earlier compared with the average age of CVD deaths in Xuanwei. Consequently, this unique mortality spectrum among smoky coal users could potentially have resulted in an underestimation of the number of CVD deaths that would have developed if lung cancer was not such a profound contributor to the mortality burden. However, analyses of the absolute risk of IHD and stroke mortality that accounted for competing causes of death suggested higher risks in smokeless compared with smoky coal users, and stronger associations with the coal and stove metrics were observed for IHD mortality among smokeless coal users in the cause-specific hazard models, which is the suggested modelling approach for aetiological research questions.27 To follow up on our findings, further studies in Xuanwei and other regions will be needed to comprehensively characterize levels of specific indoor pollutants that are emitted in the home when burning smokeless and smoky coal, and to directly evaluate these indoor levels in relation to risk of IHD and stroke.
A primary strength of this study is the large cohort for which we had detailed questionnaire data on lifetime fuel and stove use for all residences of the study participants across their life course, including quantitative assessments of the amount of coal used per year and the type of coal used. This provided a unique opportunity to conduct analyses among lifetime and exclusive users of either smoky or smokeless coal and enabled exposure-response analyses by coal type. Our study population of non-smoking women also mitigated confounding by active smoking.
Some degree of misclassification for the primary exposure metrics may be expected, particularly for participants who had questionnaire data from proxy respondents, who accounted for the majority of the follow-up interviews. Nevertheless, these proxies were primarily living family members of the subject, who would likely be aware of whether their household had a stove and the type of coal being used. Whereas the amount of coal used per year may be comparatively more difficult to reliably recall, we note that the strongest associations for IHD mortality were observed for the highest vs lowest amount of coal use, which may be a more reliable metric given the greater contrast in exposure. These associations were also consistent in sensitivity analyses that restricted to exposure information obtained from self-report or first-degree relatives of the participants, and that excluded data from non-relatives. Causes of death were derived from death certificates, which may also result in some misclassification. However, all participants lived within the confined geographical area of Xuanwei and would have been subject to the same diagnostic criteria for IHD and stroke. It is possible that IHD and stroke may have been under- or over-diagnosed if participants died outside the hospital, but this would likely be non-differential with respect to type of coal use or stove use habits. Finally, we note that the case numbers within the subcohorts of lifetime smoky and smokeless coal users were relatively small, particularly for analyses of ventilated stove use. Therefore, some degree of caution is warranted when interpreting our findings, including observed differences in associations by coal type.
Because the questionnaire used in the Xuanwei cohort was designed primarily to evaluate associations between coal use and improving ventilation on risk of lung cancer, additional information that may be relevant for aetiological studies of IHD and stroke was not collected. For example, documented lifestyle risk factors for IHD and/or stroke other than smoking include higher body mass index (BMI), hypertension and physical inactivity.28 We analysed data from a separate cross-sectional exposure assessment study in Xuanwei from the same catchment area as our cohort population, and observed that factors such as BMI, diet and prevalence of hypertension were similar when comparing users of smoky and smokeless coal, as well as users of higher vs lower coal tonnage (unpublished data). This observation is consistent with the fact that Xuanwei has a relatively homogeneous population, most of whom are physically active farmers and have similar dietary habits. Potential confounding by SES is also a consideration in studies of household air pollution. We did not have adequate case numbers to conduct detailed stratified analyses by education, but we note that there is limited variability in this variable and other proxy measures of SES among Xuanwei residents, as 76% of participants in our analysis did not have a formal education. Thus, our overall findings are driven by results among women without a formal education. Further, our analyses suggested that smokeless coal users had a consistently higher risk of IHD mortality for each tertile when compared with users of <28 ton-years of smoky coal, despite similar distributions of education and household characteristics. Although these observations provide evidence to suggest that confounding by SES is not primarily driving the larger associations observed for smokeless coal use, future studies of indoor air pollution in settings with more diverse study populations should consider this possibility.
These data may have substantial public health implications, given that as many as 800 million people worldwide are still estimated to use coal as their primary fuel source.29 The local government in Xuanwei has encouraged the use of smokeless coal for cooking and heating, and consequently this coal type has been regarded by many residents as a ‘cleaner’ fuel source. Although smoky coal is currently the predominant coal type used in China,30 the prioritization of smokeless coal has also been emphasized based on findings of its substantially lower PAH emissions compared with combustion of smoky coal. One study even suggested that 93% of PAHs would be reduced by 2020 if only smokeless coal was used in China.31 Our findings suggest that smokeless coal should not be considered a safer alternative to smoky coal. Additional studies conducted in other geographical regions are urgently needed to replicate our findings and evaluate associations between smokeless coal use and mortality from IHD and stroke.
In conclusion, our findings showed a consistent association between smokeless coal use and IHD mortality among non-smoking women in Xuanwei and indicate the importance of evaluating the specific type of coal being used when analysing these associations. With the intention to reduce PAHs and other emissions in an effort to lower the risk of lung cancer in China by switching to the use of smokeless coal, the potential resulting adverse effect of higher IHD and potentially stroke risk should be considered. These data suggest the need for alternative fuel sources such as electricity or gas in regions that still rely on coal for indoor cooking and heating. If implementation of these alternative fuel sources is not feasible, public health interventions designed to mitigate exposure to smokeless coal may also be effective in reducing the burden of IHD in rural Chinese populations.
Funding
This work was supported by: the Chinese Academy of Preventive Medicine, Beijing, China; Yunnan Province Antiepidemic Station, Kunming, China; the U.S. Environmental Protection Agency [contract 5D2290NFFX]; and by the Intramural Research Program of the National Cancer Institute, National Institutes of Health.
Supplementary Material
Acknowledgements
We are grateful to the Xuanwei residents who participated in this research and to the late Drs Robert Chapman and Xingzhou He for their extensive contributions to the study design, field implementation and data collection for this study. This study also would not have been possible without the cooperation of many Chinese administrative and public health officials, physicians and survey workers.
Conflict of interest: None declared.
References
- 1.World Health Organization. Burden of Disease From Household Air Pollution for 2012. Geneva: WHO, 2014. [Google Scholar]
- 2. Kim C, Seow WJ, Shu XO. et al. Cooking coal use and all-cause and cause-specific mortality in a prospective cohort study of women in Shanghai, China. Environ Health Perspect 2016;124:1384–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yu K, Qiu G, Chan KH. et al. Association of solid fuel use with risk of cardiovascular and all-cause mortality in rural China. JAMA 2018;319:1351–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen WW, Gao RL, Liu LS. et al. China cardiovascular diseases report 2015: a summary. J Geriatr Cardiol 2017;14:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Celermajer DS, Chow CK, Marijon E, Anstey NM, Woo KS.. Cardiovascular disease in the developing world: prevalences, patterns, and the potential of early disease detection. J Am Coll Cardiol 2012;60:1207–16. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Cardiovascular Diseases (CVDs), 2017. http://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)) (30 October 2018, date last accessed).
- 7. Zhang X, Khan AA, Haq EU. et al. Increasing mortality from ischaemic heart disease in China from 2004 to 2010: disproportionate rise in rural areas and elderly subjects. 438 million person-years follow-up. Eur Heart J Qual Care Clin Outcomes 2017;3:47–52. [DOI] [PubMed] [Google Scholar]
- 8. Downward GS, Hu W, Large D. et al. Heterogeneity in coal composition and implications for lung cancer risk in Xuanwei and Fuyuan counties, China. Environ Int 2014;68:94–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Barone-Adesi F, Chapman RS, Silverman DT. et al. Risk of lung cancer associated with domestic use of coal in Xuanwei, China: retrospective cohort study. BMJ 2012;345:e5414.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lan Q, Chapman RS, Schreinemachers DM, Tian L, He X.. Household stove improvement and risk of lung cancer in Xuanwei, China. J Natl Cancer Inst 2002;94:826–35. [DOI] [PubMed] [Google Scholar]
- 11. Hosgood HD III, Wei H, Sapkota A. et al. Household coal use and lung cancer: systematic review and meta-analysis of case-control studies, with an emphasis on geographic variation. Int J Epidemiol 2011;40:719–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shah AS, Lee KK, McAllister DA. et al. Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ 2015;350:h1295.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Franchini M, Mannucci PM.. Short-term effects of air pollution on cardiovascular diseases: outcomes and mechanisms. J Thromb Haemost 2007;5:2169–74. [DOI] [PubMed] [Google Scholar]
- 14. Lin G, So Y, Johnston G.. Analyzing Survival Data With Competing Risks Using SAS Software, 2012. https://support.sas.com/resources/papers/proceedings12/344–2012.pdf (30 October 2018, date last accessed).
- 15. Lan Q, He X, Shen M. et al. Variation in lung cancer risk by smoky coal subtype in Xuanwei, China. Int J Cancer 2008;123:2164–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Leening MJG, Cook NR, Franco OH. et al. Comparison of cardiovascular risk factors for coronary heart disease and stroke type in women. J Am Heart Assoc 2018;7:e007514.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shen M, Chapman RS, Vermeulen R. et al. Coal use, stove improvement, and adult pneumonia mortality in Xuanwei, China: a retrospective cohort study. Environ Health Perspect 2009;117:261–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chapman RS, He X, Blair AE, Lan Q.. Improvement in household stoves and risk of chronic obstructive pulmonary disease in Xuanwei, China: retrospective cohort study. BMJ 2005;331:1050.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Seow WJ, Downward GS, Wei H. et al. Indoor concentrations of nitrogen dioxide and sulfur dioxide from burning solid fuels for cooking and heating in Yunnan Province, China. Indoor Air 2016;26:776–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Uzoigwe JC, Prum T, Bresnahan E, Garelnabi M.. The emerging role of outdoor and indoor air pollution in cardiovascular disease. N Am J Med Sci 2013;5:445–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhao L, Liang HR, Chen FY, Chen Z, Guan WJ, Li JH.. Association between air pollution and cardiovascular mortality in China: a systematic review and meta-analysis. Oncotarget 2017;8:66438–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Huang J, Li G, Qian X. et al. The burden of ischemic heart disease related to ambient air pollution exposure in a coastal city in South China. Environ Res 2018;164:255–61. [DOI] [PubMed] [Google Scholar]
- 23. Qin G, Wu M, Wang J, Xu Z, Xia J, Sang N.. Sulfur dioxide contributes to the cardiac and mitochondrial dysfunction in rats. Toxicol Sci 2016;151:334–46. [DOI] [PubMed] [Google Scholar]
- 24. Yuan Y, Xiao Y, Feng W. et al. Plasma metal concentrations and incident coronary heart disease in Chinese adults: the Dongfeng-Tongji cohort. Environ Health Perspect 2017;125:107007.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Downward GS, Hu W, Rothman N. et al. Polycyclic aromatic hydrocarbon exposure in household air pollution from solid fuel combustion among the female population of Xuanwei and Fuyuan counties, China. Environ Sci Technol 2014;48:14632–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hu W, Downward GS, Reiss B. et al. Personal and indoor PM2.5 exposure from burning solid fuels in vented and unvented stoves in a rural region of China with a high incidence of lung cancer. Environ Sci Technol 2014;48:8456–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Austin PC, Lee DS, Fine JP.. Introduction to the analysis of survival data in the presence of competing risks. Circulation 2016;133:601–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stewart J, Manmathan G, Wilkinson P.. Primary prevention of cardiovascular disease: a review of contemporary guidance and literature. JRSM Cardiovasc Dis 2017;6:2048004016687211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, Vol: 95: Household Use of Solid Fuels and High-temperature Frying, 2010. https://monographs.iarc.fr/wp-content/uploads/2018/06/mono95.pdf (30 October 2018, date last accessed). [PMC free article] [PubMed]
- 30. Aden N, Fridley D, Zheng N.. Ernest Orlando Berkeley National Laboratory: China’s Coal: Demand, Constraints, and Externalities, 2009. https://www.circleofblue.org/wp-content/uploads/2011/02/coal_bohai_report.pdf (30 October 2018, date last accessed).
- 31. Huang W, Huang B, Bi X. et al. Emission of PAHs, NPAHs and OPAHs from residential honeycomb coal briquette combustion. Energy Fuels 2014;28:636–42. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.