Abstract
Background
This study examined the incidence of a person’s first diagnosis of a selected chronic disease, and the relationships between modifiable lifestyle risk factors and age to first of six chronic diseases.
Methods
Ontario respondents from 2001 to 2010 of the Canadian Community Health Survey were followed up with administrative data until 2014 for congestive heart failure, chronic obstructive respiratory disease, diabetes, lung cancer, myocardial infarction and stroke. By sex, the cumulative incidence function of age to first chronic disease was calculated for the six chronic diseases individually and compositely. The associations between modifiable lifestyle risk factors (alcohol, body mass index, smoking, diet, physical inactivity) and age to first chronic disease were estimated using cause-specific Cox proportional hazards models and Fine-Gray competing risk models.
Results
Diabetes was the most common disease. By age 70.5 years (2015 world life expectancy), 50.9% of females and 58.1% of males had at least one disease and few had a death free of the selected diseases (3.4% females; 5.4% males). Of the lifestyle factors, heavy smoking had the strongest association with the risk of experiencing at least one chronic disease (cause-specific hazard ratio = 3.86; 95% confidence interval = 3.46, 4.31). The lifestyle factors were modelled for each disease separately, and the associations varied by chronic disease and sex.
Conclusions
We found that most individuals will have at least one of the six chronic diseases before dying. This study provides a novel approach using competing risk methods to examine the incidence of chronic diseases relative to the life course and how their incidences are associated with lifestyle behaviours.
Keywords: Alcohol, body mass index, chronic disease, competing risks, diet, life course, multimorbidity, physical activity, smoking
Key Messages
Time-to-event data under the presence of competing risks with age as a time scale can be used to examine age to first chronic disease.
The majority of individuals have at least one major chronic disease before death (cardiovascular disease, COPD, diabetes, lung cancer).
Modifiable lifestyle risk factors have different magnitudes of associations with age to first chronic disease, by sex.
Introduction
In 2014, the World Health Organization attributed more than two-thirds of deaths worldwide (38 million) to chronic diseases.1 Most chronic disease deaths were attributable to cancer, cardiovascular disease, chronic respiratory disease or diabetes. Although the combined impacts of chronic diseases on health and survival are substantial,1–4 epidemiology has traditionally studied chronic diseases in ‘silos’.5–7 Clinically, researching chronic diseases separately is beneficial for understanding the epidemiology of individual diseases. However, considering multiple chronic diseases simultaneously is advantageous because it better reflects the experience of patients, who accumulate multiple conditions, as well as more accurately reflects overall health.8 Well-established evidence shows that the incidence of cancer, cardiovascular disease, chronic respiratory disease and diabetes share modifiable risk factors such as alcohol consumption, body mass index (BMI), cigarette smoking, unhealthy diet and physical inactivity, which account for more than two-thirds of these diseases.1,9,10
Despite the importance of studying chronic diseases compositely, this area of research has been studied less extensively relative to disease-specific research.6,7 In addition, there is a gap in understanding the sequence of chronic disease over the life course. From a population health perspective, understanding the relationship between age and modifiable lifestyle risk factors with the first occurrence of chronic disease is critical to inform age-appropriate disease prevention strategies for multiple chronic diseases.9,11–13
This study examined the relationship between age, five modifiable lifestyle risk factors (alcohol consumption, body mass index (BMI), cigarette smoking, unhealthy diet and physical inactivity) and the incidence of an individual’s first chronic disease [congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), diabetes, lung cancer, myocardial infarction (MI) and stroke including transient ischaemic attacks (TIA)] over the adult life course (age to first chronic disease). Whereas many chronic conditions could have been selected, we focused on these six diseases based on: their known associations with the modifiable lifestyle risk factors; high prevalence; and impact on health status, morbidity and mortality.
Methods
A cohort study was conducted in Ontario using survey data from the Canadian Community Health Survey (CCHS) linked to administrative data held by the Institute for Clinical Evaluative Sciences. The study period was 1 January 2000 to 31 December 2014.
Data sources
The CCHS is a cross-sectional survey, originating in 2000, which collects self-reported information on personal health status and determinants of health, and represents 98% of the Canadian population over 12 years.14 The administrative databases were: the Discharge Abstract Database, which contains hospital discharge data including diagnoses based on the International Classification of Diseases (ICD) 9th (ICD-9) and 10th revisions (ICD-10); the Ontario Health Insurance Plan Claims Database, which contains physician billing claims that include the visit reason (ICD-9); the Ontario Cancer Registry, which contains all cancer diagnoses in Ontario except non-melanoma skin cancers (ICD for Oncology 3rd edition); the Registered Persons Database, which contains demographic information; and vital statistics, which contain cause of death (ICD-9). These datasets were linked using unique encoded identifiers and analysed at the Institute for Clinical Evaluative Sciences (ICES).
Cohort
Individuals who completed any of the six cycles from the Ontario CCHS—Cycles 1.1 (2000), 2.1 (2003), 3.1 (2005), 4.1 (2007), 2009/10 and 2011/12—and consented to linkage via their provincial health card to administrative data were included. Individuals were excluded if they were under 20 years at interview; had existing CHF, COPD, diabetes, lung cancer, MI or stroke based on administrative data algorithms or self-reported disease; or had missing data on the five modifiable lifestyle risk factors, sociodemographic factors or other health-related risk factors. Less than 2% were missing for each variable individually, and 5% overall. BMI and household income were missing more frequently, so individuals with missing values for either variable were categorized as unknown.
Chronic disease outcomes
The outcome was chronic disease, consisting of incident CHF, COPD, diabetes, lung cancer, MI and stroke including TIA. Lung cancer was identified from the Cancer Registry.15 The other diseases were identified using validated algorithms from hospital and physician data (Supplementary Appendix 1, available as Supplementary data at IJE online).16–20 Using cause of death from vital statistics, deaths were reclassified to chronic diseases when possible to reduce under-reporting of chronic diseases from the health services data. For example, some individuals die due to MI outside the health care system, so MI would be under reported without vital statistics. All diseases were eligible as outcomes starting at age 20 years except for COPD, which was eligible at age 35 years as this is when COPD onset typically begins. If an individual had more than one incident chronic disease, the first-occurring chronic disease incidence date was used.
Modifiable lifestyle risk factors
The modifiable lifestyle risk factors were: alcohol consumption, BMI adjusted with correction equations for self-report,21 cigarette smoking, daily fruit and vegetable consumption and physical activity (Table 1). All factors were defined using the CCHS and were only collected once upon study entry.
Table 1.
Modifiable lifestyle risk factors and their definitions
| Modifiable lifestyle risk factor | Definition |
|---|---|
| Alcohol consumption | |
| Non-drinker | Did not drink in the past 12 months or drinking frequency is less than weekly |
| Light drinker | Drinks at least once per week, and up to 2 drinks in the past week (females), or had up to 3 drinks in the past week (males) |
| Moderate drinker | Drinks at least once per week, and had between 3 and 14 drinks in the past week (females), or between 4 and 21 drinks in the paast week (males) |
| Heavy drinker | Drinks at least once per week, and had more than 14 drinks (females), or more than 21 drinks (males) |
| Body mass index (BMI) | |
| Healthy weight | 18.5 to 25 kg/m2 |
| Underweight | <18.5 kg/m2 |
| Overweight | 25 to 30 kg/m2 |
| Obese, class 1 | 30 to 35 kg/m2 |
| Obese, class 2 | 35 to 40 kg/m2 |
| Obese, class 3 | >40 kg/m2 |
| Cigarette smoking | |
| Never smoked | Less than 100 cigarettes smoked ever |
| Heavy smoker | Currently smokes 1 or more packs per day |
| Light smoker | Currently smokes less than 1 pack per day |
| Former heavy smoker | Formerly smoked 1 or more packs per day |
| Former light smoker | Formerly smoked less than 1 pack per day |
| Former smoker, unknown amount | Formerly smoked, but packs per day was not reported |
| Daily fruit and vegetable consumption | |
| 0 to 3 times | Consumed fruits and vegetables between 0 and 3 times a day |
| 3 to 6 times | Consumed fruits and vegetables between 3 and 6 times a day |
| 6 or more times | Consumed fruits and vegetables 6 or more times a day |
| Leisure physical activity | |
| No physical activity | 0 metabolic equivalents per day |
| Slightly active | 0 to 1.5 metabolic equivalents per day |
| Moderately active | 1.5 to 3 metabolic equivalents per day |
| Active | 3 or more metabolic equivalents per day |
For daily fruit and vegetable consumption, starchy vegetables (e.g. potatoes) were not considered and fruit juice was counted maximum once per day.
Statistical analysis
To examine age to first chronic disease, methods for examining time-to-event data under the presence of competing risks were used. Age was the time scale because age is biologically meaningful for chronic disease incidence.22 Individuals were eligible for follow-up starting at age 20 years. Left truncation (delayed entry) accounted for the fact that an individual is at risk for chronic diseases right from birth and that all individuals were free of the selected chronic diseases before study entry.23,24 Left truncation accounts for this immortal time by only using the time after the interview to calculate the survival-analysis based estimates; all time before the interview is truncated. Individuals were followed up from their age at interview for up to 15 years until their age of first chronic disease, age of chronic disease-free death or age at study end. Death free of chronic disease was a competing risk. Individual chronic diseases were also competing risks for each other; for example, if an individual developed diabetes as their first chronic disease, diabetes was a competing risk for the other five diseases. All analyses were stratified by sex because biological causes for chronic disease vary by sex and the potential for risk factors to be modified by sex.25–28
The cumulative incidence of first chronic disease using an age-time scale describes the percentage of individuals at a specific age with at least one incident chronic disease. The cumulative incidence was estimated using the cumulative incidence function (CIF) with chronic disease-free death as a competing risk with the etm package in R. The cumulative incidence was also calculated for each chronic disease separately. At a given age, the sum of the individual chronic disease probabilities equals the total cumulative probability of having at least one chronic disease by that age.
The cause-specific Cox proportional hazards (PH) model estimated the associations between the modifiable lifestyle risk factors and age to first chronic disease. Cause-specific hazards ratios (csHRs) were generated to describe the relative change in the rate of chronic disease occurrence at a specific age. Univariable and multivariable models were constructed and adjusted for modifiable lifestyle risk factors, sociodemographic factors and other health-related factors. Confounder selection was guided by the Canadian Chronic Disease Indicators.8,29 The sociodemographic factors were: ethnicity, Canadian immigrant status, rural residence, highest level of education, household income quintile and marital status. The health-related factors were: second-hand smoke exposure at home, asthma, high blood pressure, self-rated health and life stress. As the rate of an event and the corresponding event risk do not have a direct relationship under the presence of competing events, the Fine-Gray competing risk model was also used to examine the associations while accounting for death (without experiencing chronic disease) as a competing risk. The Fine-Gray model computes the subdistribution hazards ratio (sdHR) where the direction of the sdHR describes the direction of the covariate effect on the incidence of chronic disease.30 Cause-specific Cox PH models and Fine-Gray models were also used to examine the association of the modifiable lifestyle risk factors with each chronic disease separately.
We performed six additional analyses that considered other chronic diseases as endpoints. For the first additional analysis, we included all other cancers, dementia and osteo- and other arthritis (arthritis) as outcomes, and repeated the analysis among individuals who were free of the six chronic diseases plus other cancers, dementia and arthritis. The additional analysis was repeated five more times where the other cancers outcome was modified to only include those cancers with known associations with a specific lifestyle factor31–35 (summarized in Supplementary Appendix 2, available as Supplementary data at IJE online). For example, the second additional analysis was limited to those cancers with known associations with alcohol consumption. The analysis was repeated five times, once for each lifestyle factor. The purpose of the additional analyses was to assess how the estimates (e.g. CIF, HRs) would change when other chronic diseases were added.
A sensitivity analysis was also performed on individuals that self-reported being free of fourteen common chronic conditions (Supplementary Appendix 1, available as Supplementary data at IJE online), including conditions that were not outcomes (e.g. asthma). This purpose of the sensitivity analysis was to evaluate the robustness of the associations between the modifiable lifestyle risk factors and the six chronic diseases among individuals who were free of a larger set of chronic conditions in addition to the six chronic diseases at baseline.
All regression analyses were conducted using SAS Enterprise Guide 7.1. To ensure the estimates were representative of the Ontario population, survey weights from Statistics Canada were normalized. This project has been approved by the Research Ethics Boards at the University of Toronto, Toronto Canada; and Sunnybrook Health Sciences Center, Toronto Canada.
Results
Baseline characteristics
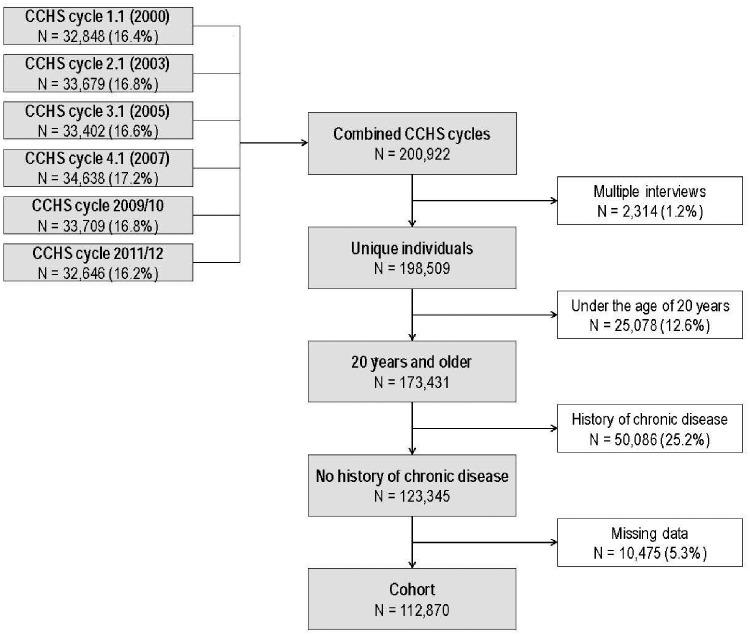
There were 200 922 CCHS respondents eligible, 2413 of which appeared in more than one cycle. After exclusions (Figure 1), there were 112 870 individuals (56.2% female). The cohort characteristics are in Table 2. On average, females were older than males. There were more heavy drinkers and fewer non-drinkers in males than females. Men also tended to be classified as being overweight or with obesity, be current or former smokers, eat fewer fruits and vegetables daily, and be more physically active compared with women.
Figure 1.
Eligubilty criteria for the CCHS Cohort, ON, Canada, 2000–14.
Table 2.
Characteristics of the Ontario CCHS cohort as of their interview date, by sex, 2000–14
| Baseline characteristic | Both sexes | Females | Males |
|---|---|---|---|
| n = 112 870 | n = 63 401 | n = 49 469 | |
| (56.2%) | (43.8%) | ||
| Sociodemographic factors | |||
| Age, mean ± SD | |||
| Mean ± SD | 45.86 ± 16.05 | 46.82 ± 16.71 | 44.64 ± 15.06 |
| 20 to 34 years | 33 211 (29.4%) | 18 385 (29.0%) | 14 826 (30.0%) |
| 35 to 44 years | 26 144 (23.2%) | 13 661 (21.5%) | 12 483 (25.2%) |
| 45 to 54 years | 20 404 (18.1%) | 10 978 (17.3%) | 9426 (19.1%) |
| 55 to 64 years | 17 446 (15.5%) | 10 095 (15.9%) | 7351 (14.9%) |
| 65 to 74 years | 10 012 (8.9%) | 6185 (9.8%) | 3827 (7.7%) |
| 75 to 84 years | 4653 (4.1%) | 3317 (5.2%) | 1336 (2.7%) |
| 85+ years | 1000 (0.9%) | 780 (1.2%) | 220 (0.4%) |
| Visible minority, n (%) | 13 958 (12.4%) | 7 664 (12.1%) | 6294 (12.7%) |
| Immigrant, n (%) | 22 696 (20.1%) | 12 816 (20.2%) | 9880 (20.0%) |
| Rural residence, n (%) | 22 813 (20.2%) | 12 684 (20.0%) | 10 129 (20.5%) |
| Highest level of education, n (%) | |||
| Less than secondary school graduation | 14 692 (13.0%) | 8265 (13.0%) | 6427 (13.0%) |
| Secondary school graduation | 21 801 (19.3%) | 12 420 (19.6%) | 9381 (19.0%) |
| Post-secondary education (include partial) | 76 377 (67.7%) | 42 716 (67.4%) | 33 661 (68.0%) |
| Household income quintile, n (%) | |||
| 1 (Lowest) | 11 513 (10.2%) | 7448 (11.7%) | 4065 (8.2%) |
| 2 | 13 794 (12.2%) | 8603 (13.6%) | 5191 (10.5%) |
| 3 | 20 501 (18.2%) | 12 156 (19.2%) | 8345 (16.9%) |
| 4 | 28 777 (25.5%) | 15 401 (24.3%) | 13 376 (27.0%) |
| 5 (Highest) | 31 762 (28.1%) | 15 518 (24.5%) | 16 244 (32.8%) |
| Unknown income | 6523 (5.8%) | 4275 (6.7%) | 2248 (4.5%) |
| Marital status, n (%) | |||
| Single, never married | 25 147 (22.3%) | 12 243 (19.3%) | 12 904 (26.1%) |
| Domestic partner (married/common-law) | 68 987 (61.1%) | 38 092 (60.1%) | 30 895 (62.5%) |
| Widowed/separated/divorced | 18 736 (16.6%) | 13 066 (20.6%) | 5670 (11.5%) |
| Modifiable lifestyle risk factors | |||
| Alcohol consumption status, n (%) | |||
| Non-drinker | 60 296 (53.4%) | 40 131 (63.3%) | 20 165 (40.8%) |
| Light drinker | 16 553 (14.7%) | 8274 (13.1%) | 8279 (16.7%) |
| Moderate drinker | 26 363 (23.4%) | 12 479 (19.7%) | 13 884 (28.1%) |
| Heavy drinker | 9658 (8.6%) | 2517 (4.0%) | 7141 (14.4%) |
| Body mass index (BMI) | |||
| Mean ± SD | 26.89 ± 5.13 | 26.46 ± 5.50 | 27.42 ± 4.58 |
| Healthy weight (18.5 to 25 kg/m2) | 41 433 (36.7%) | 26 427 (41.7%) | 15 006 (30.3%) |
| Underweight (<18.5 kg/m2) | 1231 (1.1%) | 915 (1.4%) | 316 (0.6%) |
| Overweight (25 to 30 kg/m2) | 40 616 (36.0%) | 18 841 (29.7%) | 21 775 (44.0%) |
| Obese, class 1 (30 to 35 kg/m2) | 16 799 (14.9%) | 8234 (13.0%) | 8565 (17.3%) |
| Obese, class 2 (35 to 40 kg/m2) | 4763 (4.2%) | 2792 (4.4%) | 1971 (4.0%) |
| Obese, class 3 (>40 kg/m2) | 2130 (1.9%) | 1410 (2.2%) | 720 (1.5%) |
| Unknown BMI | 5898 (5.2%) | 4782 (7.5%) | 1116 (2.3%) |
| Cigarette smoking status, n (%) | |||
| Never smoked | 56 641 (50.2%) | 34 788 (54.9%) | 21 853 (44.2%) |
| Heavy smoker | 4802 (4.3%) | 1767 (2.8%) | 3035 (6.1%) |
| Light smoker | 21 640 (19.2%) | 11 329 (17.9%) | 10 311 (20.8%) |
| Former heavy smoker | 7014 (6.2%) | 2855 (4.5%) | 4159 (8.4%) |
| Former light smoker | 19 354 (17.1%) | 10 851 (17.1%) | 8503 (17.2%) |
| Former smoker, unknown amount | 3419 (3.0%) | 1811 (2.9%) | 1608 (3.3%) |
| Daily fruit and vegetable consumption, n (%) | |||
| 0 to 3 times | 35 519 (31.5%) | 15 627 (24.6%) | 19 892 (40.2%) |
| 3 to 6 times | 52 389 (46.4%) | 30 067 (47.4%) | 22 322 (45.1%) |
| 6 or more times | 24 962 (22.1%) | 17 707 (27.9%) | 7255 (14.7%) |
| Leisure physical activity, n (%) | |||
| No physical activity | 8761 (7.8%) | 5281 (8.3%) | 3480 (7.0%) |
| Slightly active | 43 623 (38.6%) | 25 292 (39.9%) | 18 331 (37.1%) |
| Moderately active | 30 222 (26.8%) | 17 349 (27.4%) | 12 873 (26.0%) |
| Active | 30 264 (26.8%) | 15 479 (24.4%) | 14 785 (29.9%) |
| Other health-related risk factors | |||
| Household second-hand smoke exposure, n (%) | 4795 (9.7%) | 5486 (8.7%) | 10 281 (9.1%) |
| Asthma, n (%) | 13 439 (11.9%) | 8682 (13.7%) | 4757 (9.6%) |
| High blood pressure, n (%) | 23 439 (20.8%) | 13 769 (21.7%) | 9670 (19.5%) |
| Self-rated health, n (%) | |||
| Poor | 1798 (1.6%) | 1118 (1.8%) | 680 (1.4%) |
| Fair | 6936 (6.1%) | 4099 (6.5%) | 2837 (5.7%) |
| Good | 28 877 (25.6%) | 15 932 (25.1%) | 12 945 (26.2%) |
| Very good | 46 777 (41.4%) | 26 204 (41.3%) | 20 573 (41.6%) |
| Excellent | 28 482 (25.2%) | 16 048 (25.3%) | 12 434 (25.1%) |
| Life stress, n (%) | |||
| Not at all stressful | 11 663 (10.3%) | 5934 (9.4%) | 5729 (11.6%) |
| Not very stressful | 26 949 (23.9%) | 14 999 (23.7%) | 11 950 (24.2%) |
| A bit stressful | 48 651 (43.1%) | 27 494 (43.4%) | 2157 (42.8%) |
| Quite a bit/extremely stressful | 25 607 (22.7%) | 14 974 (23.6%) | 10 633 (21.5%) |
Any chronic disease
Incidence
Approximately 15.1% (n = 17 043) of the cohort developed at least one of the six chronic diseases over the study period (Supplementary Figure 1, available as Supplementary data at IJE online). Overall, the cohort had 1.98 chronic diseases per 100 person-years with males having a higher incidence than females (2.09 vs 1.90 per 100 person-years). Of the selected diseases, the most frequently-occurring one was diabetes (40.9%) followed by COPD (32.8%), stroke including TIA (9.6%), CHF (8.2%), MI (5.9%) and lung cancer (2.6%). Overall, 2099 persons (1.9%) died before having one of the six chronic diseases (1167 females). Of these deaths, 192 were reclassified as a chronic disease with MI’s reclassified the most (n = 127).
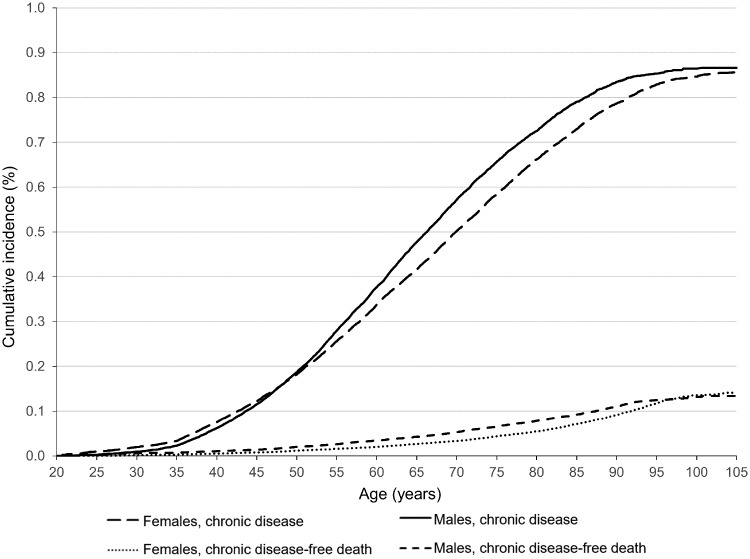
The cumulative incidence of first chronic disease is shown in Figure 2. The cumulative incidence of any of the six chronic diseases was greater in females until age 48 years, after which the incidence was greater in males. By sex, 50% of males and females had at least one of the six chronic diseases by age 66.3 and 70.5 years, respectively. By age 70.5 years (2015 world life expectancy),36 50.9% (95% CI: 50.0, 51.9) of females and 58.1% (95% CI: 57.2, 59.1) of males had at least one chronic disease. Over the life course, the risk of a chronic disease-free death was low.
Figure 2.
Cumulative incidence function of age to first chronic disease with death as a competing risk, by sex.
Modifiable lifestyle risk factors
The associations between the lifestyle factors and any of the six chronic diseases calculated using cause-specific Cox PH models are shown in Tables 3a and 3b. Non-drinkers were associated with an increased hazard of any of the six chronic diseases compared with light drinkers. A dose-response relationship for BMI was observed for both sexes where increasing levels of overweightness and obesity was associated with increasing hazard of first chronic disease. In females, current heavy smokers had a greater hazard of first chronic disease than current light smokers, and former heavy smokers had a greater hazard than former light smokers. Similar associations were observed in males, but the magnitudes of the associations were lower. In both sexes, the relative hazard of any first chronic disease increased as the daily consumption of fruits and vegetables decreased. For both sexes, less physical activity increased the hazard of any of the six chronic diseases. As expected based on the low risk of a chronic disease-free death, the subdistribution HR’s were similar to the cause-specific HR’s (Supplementary Table 1, available as Supplementary data at IJE online).
Table 3a.
Associations of the modifiable lifestyle risk factors with age to first chronic disease among females (cause-specific Cox PH models)
| Characteristic | Comparison group | Reference group | Univariable model |
Multivariable models |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Risk factors |
Risk factors & sociodemographic factors |
Risk factors, sociodemographic factors & health factors |
||||||||
| csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | |||||||
| Alcohol consumption | Non-drinker | Light drinker | 1.57 | 1.45, 1.70 | 1.40 | 1.29, 1.52 | 1.31 | 1.21, 1.42 | 1.28 | 1.18, 1.38 |
| Moderate drinker | 0.95 | 0.86, 1.04 | 0.96 | 0.87, 1.05 | 0.97 | 0.88, 1.07 | 0.98 | 0.89, 1.08 | ||
| Heavy drinker | 1.72 | 1.49, 2.00 | 1.28 | 1.10, 1.49 | 1.27 | 1.09, 1.47 | 1.22 | 1.05, 1.42 | ||
| BMI | Underweight | Healthy weight | 0.97 | 0.74, 1.27 | 0.86 | 0.65, 1.13 | 0.83 | 0.63, 1.09 | 0.80 | 0.61, 1.05 |
| Overweight | 1.50 | 1.41, 1.59 | 1.48 | 1.39, 1.57 | 1.50 | 1.41, 1.59 | 1.43 | 1.34, 1.52 | ||
| Obese, class 1 | 2.12 | 1.97, 2.28 | 1.96 | 1.82, 2.11 | 2.01 | 1.87, 2.17 | 1.80 | 1.67, 1.94 | ||
| Obese, class 2 | 3.35 | 3.04, 3.69 | 3.11 | 2.82, 3.43 | 3.19 | 2.89, 3.52 | 2.70 | 2.44, 2.98 | ||
| Obese, class 3 | 3.99 | 3.52, 4.53 | 3.54 | 3.12, 4.03 | 3.68 | 3.23, 4.19 | 3.04 | 2.67, 3.47 | ||
| Unknown BMI | 1.69 | 1.55, 1.85 | 1.59 | 1.45, 1.73 | 1.64 | 1.50, 1.79 | 1.58 | 1.45, 1.72 | ||
| Cigarette smoking | Heavy smoker | Never smoked | 4.22 | 3.82, 4.66 | 3.76 | 3.40, 4.17 | 3.92 | 3.52, 4.38 | 3.86 | 3.46, 4.31 |
| Light smoker | 2.21 | 2.08, 2.35 | 2.26 | 2.13, 2.41 | 2.37 | 2.22, 2.54 | 2.39 | 2.23, 2.56 | ||
| Former heavy smoker | 1.43 | 1.28, 1.59 | 1.35 | 1.21, 1.50 | 1.48 | 1.33, 1.65 | 1.47 | 1.32, 1.64 | ||
| Former light smoker | 1.05 | 0.98, 1.12 | 1.12 | 1.05, 1.20 | 1.21 | 1.13, 1.30 | 1.20 | 1.12, 1.29 | ||
| Former smoker, amount unknown | 0.71 | 0.59, 0.84 | 0.77 | 0.65, 0.92 | 0.83 | 0.69, 0.98 | 0.84 | 0.71, 1.00 | ||
| Daily fruit and vegetable consumption | 0 to 3 times | 6 or more times | 1.66 | 1.56, 1.78 | 1.18 | 1.10, 1.27 | 1.16 | 1.08, 1.24 | 1.15 | 1.07, 1.24 |
| 3 to 6 times | 1.17 | 1.11, 1.25 | 1.08 | 1.02, 1.15 | 1.07 | 1.01, 1.14 | 1.08 | 1.01, 1.15 | ||
| Leisure physical activity | Moderately active | Active | 1.12 | 1.03, 1.20 | 1.03 | 0.96, 1.11 | 1.02 | 0.95, 1.10 | 0.99 | 0.92, 1.07 |
| Slightly active | 1.35 | 1.26, 1.44 | 1.10 | 1.03, 1.18 | 1.07 | 1.00, 1.15 | 1.02 | 0.95, 1.09 | ||
| No physical activity | 1.79 | 1.65, 1.95 | 1.30 | 1.19, 1.41 | 1.19 | 1.09, 1.30 | 1.08 | 0.98, 1.18 | ||
| Visible minority | White | 1.20 | 1.13, 1.28 | 1.33 | 1.24, 1.43 | 1.33 | 1.24, 1.43 | |||
| Immigrant | Canadian-born | 1.06 | 1.01, 1.12 | 1.09 | 1.03, 1.16 | 1.08 | 1.02, 1.14 | |||
| Rural residence | 0.96 | 0.89, 1.04 | 0.93 | 0.86, 1.00 | 0.94 | 0.87, 1.02 | ||||
| Education | Less than secondary school graduation | Secondary school graduation | 1.27 | 1.19, 1.37 | 1.06 | 0.99, 1.14 | 1.00 | 0.93, 1.08 | ||
| Post-secondary education (include partial) | 0.81 | 0.76, 0.86 | 0.95 | 0.89, 1.00 | 0.94 | 0.89, 1.00 | ||||
| Household income quintile | 1 (Lowest) | 5 (highest) | 1.74 | 1.60, 1.90 | 1.22 | 1.11, 1.34 | 1.12 | 1.02, 1.23 | ||
| 2 | 1.59 | 1.46, 1.73 | 1.21 | 1.11, 1.32 | 1.15 | 1.05, 1.25 | ||||
| 3 | 1.52 | 1.41, 1.64 | 1.18 | 1.09, 1.28 | 1.15 | 1.07, 1.25 | ||||
| 4 | 1.31 | 1.22, 1.41 | 1.10 | 1.02, 1.18 | 1.07 | 1.00, 1.15 | ||||
| Unknown income | 1.47 | 1.35, 1.60 | 1.20 | 1.10, 1.31 | 1.15 | 1.06, 1.26 | ||||
| Marital status | Domestic partner (married/common-law) | Single never married | 0.83 | 0.76, 0.90 | 0.94 | 0.86, 1.02 | 0.94 | 0.86, 1.02 | ||
| Widowed / separated / divorced | 1.07 | 0.97, 1.17 | 0.99 | 0.90, 1.09 | 0.99 | 0.90, 1.09 | ||||
| Household second-hand smoke | No household second hand smoke | 1.66 | 1.54, 1.78 | 1.11 | 1.03, 1.20 | 1.11 | 1.03, 1.19 | |||
| Asthma | No asthma | 1.55 | 1.46, 1.66 | 1.35 | 1.26, 1.44 | |||||
| High blood pressure | No high blood pressure | 1.75 | 1.66, 1.85 | 1.44 | 1.36, 1.52 | |||||
| Self-rated health | Poor | Good | 1.72 | 1.52, 1.94 | 1.31 | 1.16, 1.49 | ||||
| Fair | 1.38 | 1.27, 1.49 | 1.13 | 1.04, 1.23 | ||||||
| Very good | 0.72 | 0.68, 0.76 | 0.86 | 0.81, 0.91 | ||||||
| Excellent | 0.54 | 0.50, 0.58 | 0.78 | 0.72, 0.84 | ||||||
| Life stress | Quite a bit/extremely stressful | Not at all stressful | 1.17 | 1.07, 1.28 | 0.98 | 0.90, 1.08 | ||||
| Not very stressful | 0.87 | 0.79, 0.95 | 0.88 | 0.80, 0.96 | ||||||
| A bit stressful | 1.04 | 0.96, 1.13 | 0.99 | 0.91, 1.08 | ||||||
Table 3b.
Associations of the modifiable lifestyle risk factors with age to first chronic disease among males (cause-specific Cox PH models)
| Characteristic | Comparison group | Reference group | Univariable model |
Multivariable models |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Risk factors |
Risk factors & sociodemographic factors |
Risk factors, sociodemographic factors & health factors |
||||||||
| csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | |||||||
| Alcohol consumption | Non-drinker | Light drinker | 1.36 | 1.27, 1.46 | 1.24 | 1.15, 1.32 | 1.17 | 1.09, 1.25 | 1.16 | 1.08, 1.24 |
| Moderate drinker | 0.99 | 0.92, 1.06 | 0.96 | 0.89, 1.04 | 0.98 | 0.91, 1.06 | 0.97 | 0.90, 1.05 | ||
| Heavy drinker | 1.17 | 1.06, 1.28 | 0.89 | 0.81, 0.98 | 0.88 | 0.80, 0.98 | 0.85 | 0.77, 0.94 | ||
| BMI | Underweight | Healthy weight | 1.90 | 1.45, 2.50 | 1.65 | 1.26, 2.17 | 1.58 | 1.20, 2.08 | 1.52 | 1.16, 2.00 |
| Overweight | 1.11 | 1.05, 1.18 | 1.20 | 1.12, 1.27 | 1.24 | 1.16, 1.32 | 1.19 | 1.12, 1.27 | ||
| Obese, class 1 | 1.75 | 1.63, 1.88 | 1.86 | 1.73, 2.00 | 1.97 | 1.83, 2.12 | 1.77 | 1.65, 1.91 | ||
| Obese, class 2 | 2.87 | 2.59, 3.18 | 2.86 | 2.58, 3.17 | 3.01 | 2.71, 3.34 | 2.50 | 2.25, 2.77 | ||
| Obese, class 3 | 4.13 | 3.55, 4.81 | 4.00 | 3.43, 4.67 | 4.26 | 3.65, 4.97 | 3.40 | 2.91, 3.98 | ||
| Unknown BMI | 1.40 | 1.23, 1.59 | 1.39 | 1.22, 1.58 | 1.46 | 1.28, 1.67 | 1.49 | 1.31, 1.69 | ||
| Cigarette smoking | Heavy smoker | Never smoked | 2.84 | 2.60, 3.09 | 2.76 | 2.52, 3.01 | 2.70 | 2.46, 2.97 | 2.61 | 2.37, 2.87 |
| Light smoker | 1.96 | 1.84, 2.09 | 1.99 | 1.87, 2.13 | 1.89 | 1.77, 2.02 | 1.87 | 1.74, 1.99 | ||
| Former heavy smoker | 1.35 | 1.25, 1.47 | 1.29 | 1.18, 1.40 | 1.31 | 1.21, 1.43 | 1.24 | 1.14, 1.35 | ||
| Former light smoker | 1.09 | 1.01, 1.16 | 1.10 | 1.03, 1.18 | 1.11 | 1.04, 1.19 | 1.07 | 1.00, 1.15 | ||
| Former smoker, amount unknown | 0.94 | 0.81, 1.08 | 0.97 | 0.84, 1.12 | 0.95 | 0.82, 1.10 | 0.92 | 0.80, 1.06 | ||
| Daily fruit and vegetable consumption | 0 to 3 times | 6 or more times | 1.37 | 1.27, 1.48 | 1.12 | 1.03, 1.21 | 1.12 | 1.03, 1.21 | 1.09 | 1.01, 1.18 |
| 3 to 6 times | 1.09 | 1.01, 1.18 | 1.05 | 0.97, 1.13 | 1.05 | 0.97, 1.13 | 1.03 | 0.96, 1.12 | ||
| Leisure physical activity | Moderately active | Active | 1.09 | 1.01, 1.17 | 1.05 | 0.97, 1.12 | 1.04 | 0.97, 1.12 | 1.01 | 0.94, 1.08 |
| Slightly active | 1.41 | 1.32, 1.50 | 1.21 | 1.14, 1.29 | 1.18 | 1.11, 1.26 | 1.12 | 1.05, 1.20 | ||
| No physical activity | 1.73 | 1.59, 1.88 | 1.41 | 1.29, 1.53 | 1.29 | 1.18, 1.41 | 1.22 | 1.12, 1.33 | ||
| Visible minority | White | 1.21 | 1.14, 1.28 | 1.30 | 1.21, 1.39 | 1.25 | 1.16, 1.35 | |||
| Immigrant | Canadian-born | 1.07 | 1.02, 1.12 | 1.04 | 0.98, 1.11 | 1.04 | 0.97, 1.10 | |||
| Rural residence | 0.97 | 0.90, 1.05 | 0.93 | 0.87, 1.01 | 0.94 | 0.87, 1.01 | ||||
| Education | Less than secondary school graduation | Secondary school graduation | 1.22 | 1.13, 1.32 | 1.03 | 0.95, 1.11 | 1.01 | 0.94, 1.10 | ||
| Post-secondary education (include partial) | 0.82 | 0.77, 0.87 | 0.94 | 0.88, 1.00 | 0.95 | 0.89, 1.01 | ||||
| Household income quintile | 1 (lowest) | 5 (highest) | 1.66 | 1.52, 1.82 | 1.22 | 1.11, 1.35 | 1.16 | 1.05, 1.28 | ||
| 2 | 1.33 | 1.22, 1.46 | 1.09 | 1.00, 1.19 | 1.03 | 0.94, 1.13 | ||||
| 3 | 1.34 | 1.25, 1.44 | 1.13 | 1.05, 1.22 | 1.10 | 1.02, 1.19 | ||||
| 4 | 1.20 | 1.12, 1.28 | 1.04 | 0.97, 1.10 | 1.03 | 0.96, 1.09 | ||||
| Unknown income | 1.34 | 1.22, 1.48 | 1.15 | 1.04, 1.27 | 1.12 | 1.02, 1.24 | ||||
| Marital status | Domestic partner (married/ common-law) | Single never married | 0.87 | 0.80, 0.94 | 0.94 | 0.87, 1.02 | 0.96 | 0.89, 1.04 | ||
| Widowed/separated/divorced | 1.17 | 1.06, 1.30 | 1.13 | 1.02, 1.25 | 1.14 | 1.02, 1.26 | ||||
| Household secondhand smoke | No household second-hand smoke | 1.57 | 1.46, 1.69 | 1.18 | 1.10, 1.28 | 1.17 | 1.09, 1.27 | |||
| Asthma | No asthma | 1.37 | 1.26, 1.49 | 1.35 | 1.24, 1.46 | |||||
| High blood pressure | No high blood pressure | 1.68 | 1.60, 1.78 | 1.46 | 1.38, 1.54 | |||||
| Self-rated health | Poor | Good | 1.43 | 1.22, 1.68 | 1.11 | 0.94, 1.31 | ||||
| Fair | 1.33 | 1.22, 1.46 | 1.11 | 1.02, 1.22 | ||||||
| Very good | 0.69 | 0.65, 0.73 | 0.83 | 0.78, 0.87 | ||||||
| Excellent | 0.49 | 0.45, 0.52 | 0.66 | 0.61, 0.71 | ||||||
| Life stress | Quite a bit/extremely stressful | Not at all stressful | 0.91 | 0.83, 0.99 | 0.88 | 0.80, 0.96 | ||||
| Not very stressful | 0.90 | 0.83, 0.97 | 0.92 | 0.85, 1.00 | ||||||
| A bit stressful | 0.95 | 0.88, 1.03 | 0.96 | 0.89, 1.04 | ||||||
Specific chronic diseases
Incidence
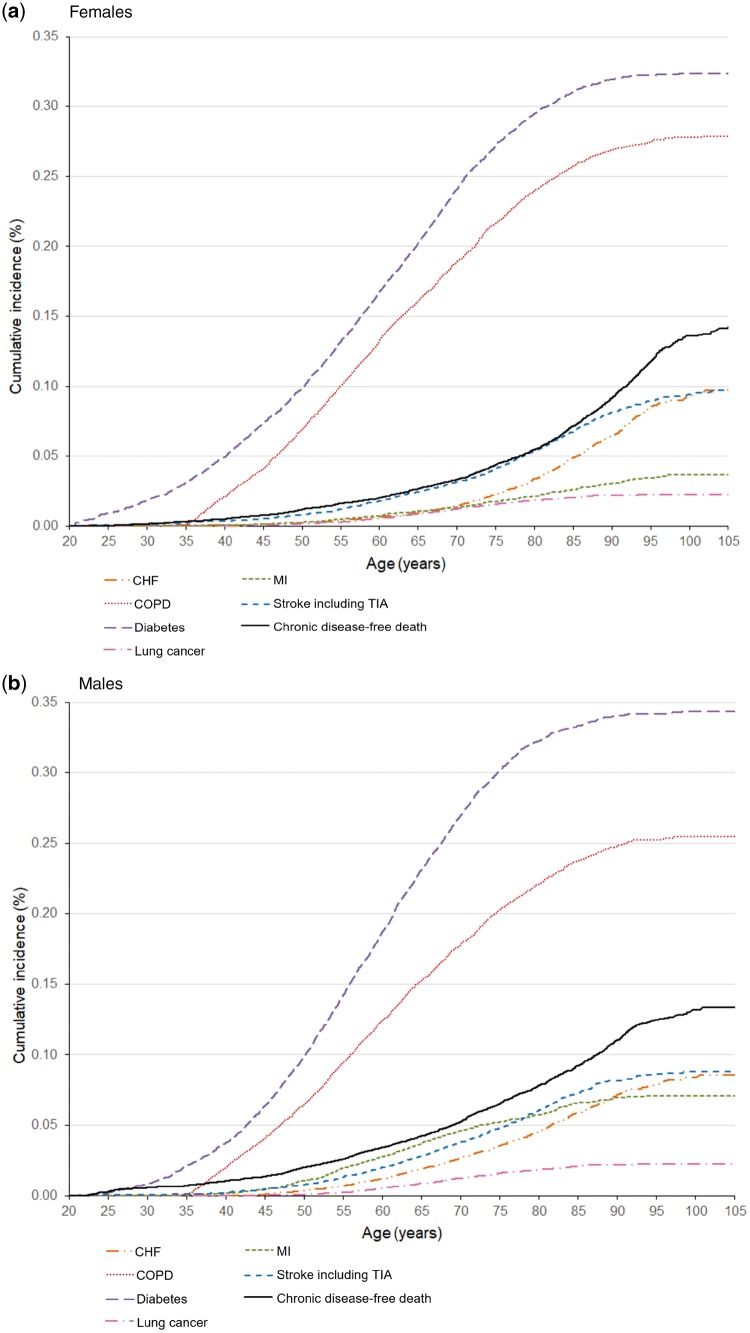
The cumulative incidence was examined for each chronic disease specifically (Figure 3a and b). Among females, by the end of the life course, the order of chronic diseases in terms of descending cumulative incidence was: diabetes, COPD, CHF, stroke, MI and lung cancer. The ordering was similar for males except CHF and stroke were reversed.
Figure 3.
Cumulative incidence function for age-to-first chronic disease among females (top) and males (bottom), by chronic disease. The individual chronic diseases are competing risks of one another, so the cumulative incidence shows the risk of a specific chronic disease without the presence of any other event (chronic disease or death). For example, ‘diabetes’ implies ‘diabetes without the presence of another chronic disease or death’.
Modifiable lifestyle risk factors
The associations between the risk factors and each of the six specific chronic disease were examined, and the associations varied by specific chronic disease (Tables 4a and 4b;Supplementary Tables 2a and 2 b, available as Supplementary data at IJE online contain the full models). For both sexes, not consuming alcohol was associated with a higher hazard of diabetes and MI’s in both sexes. Unhealthy BMI was associated with increased hazards of diabetes in both sexes. Current cigarette smoking (light smoker and heavy smoker) was associated with all chronic diseases in females, except for CHF; and COPD, lung cancer and MI in males. Decreased daily fruit and vegetable consumption was associated with a higher hazard of diabetes in both sexes. The associations with physical activity were mixed. Among females, decreased physical activity was associated with increased hazards of CHF and stroke, but decreased hazard of MI’s. Among males, decreased physical activity was associated with increased hazards of lung cancer, COPD, diabetes. The sdHR’s varied depending on the risk factor and chronic disease (Supplementary Tables 3a and 3b, available as Supplementary data at IJE online). The values of the sdHR’s were different than the csHR’s, which suggests that the rate of each chronic disease occurrence was different than their probability of occurrence over the life course.30
Table 4a.
Associations of the modifiable lifestyle risk factors with age to first chronic disease among females, by chronic disease type (cause-specific cox PH models)
| Characteristic | Comparison group | Reference group | CHF |
COPD |
Diabetes |
Lung cancer |
MI |
Stroke including TIA |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | |||||||||
| Alcohol consumption | Non-drinker | Light drinker | 1.12 | 0.84, 1.49 | 1.20 | 1.04, 1.38 | 1.40 | 1.24, 1.58 | 0.93 | 0.58, 1.50 | 1.92 | 1.14, 3.25 | 1.16 | 0.90, 1.50 |
| Moderate drinker | 1.00 | 0.70, 1.42 | 1.08 | 0.92, 1.27 | 0.87 | 0.74, 1.02 | 0.90 | 0.53, 1.53 | 1.30 | 0.71, 2.36 | 0.98 | 0.73, 1.32 | ||
| Heavy drinker | 0.91 | 0.39, 2.16 | 1.53 | 1.24, 1.90 | 0.82 | 0.62, 1.10 | 1.40 | 0.65, 3.02 | 2.08 | 0.85, 5.11 | 0.95 | 0.52, 1.74 | ||
| BMI | Underweight | Healthy weight | 0.38 | 0.08, 1.76 | 1.32 | 0.96, 1.80 | 0.15 | 0.05, 0.45 | 0.77 | 0.14, 4.07 | 0.23 | 0.02, 3.62 | 0.71 | 0.28, 1.77 |
| Overweight | 1.28 | 1.00, 1.66 | 1.04 | 0.94, 1.15 | 2.44 | 2.20, 2.70 | 0.95 | 0.65, 1.39 | 0.97 | 0.69, 1.37 | 0.87 | 0.70, 1.07 | ||
| Obese, class 1 | 1.52 | 1.12, 2.06 | 0.80 | 0.69, 0.92 | 4.05 | 3.62, 4.53 | 0.97 | 0.59, 1.60 | 1.07 | 0.68, 1.66 | 1.06 | 0.81, 1.37 | ||
| Obese, class 2 | 0.84 | 0.43, 1.64 | 0.98 | 0.78, 1.22 | 7.04 | 6.16, 8.06 | 0.74 | 0.27, 2.09 | 1.48 | 0.75, 2.93 | 0.96 | 0.60, 1.53 | ||
| Obese, class 3 | 6.16 | 3.92, 9.69 | 1.36 | 1.04, 1.76 | 7.00 | 5.87, 8.34 | 0.92 | 0.23, 3.61 | 0.52 | 0.10, 2.83 | 0.77 | 0.36, 1.65 | ||
| Unknown BMI | 1.42 | 1.08, 1.86 | 0.96 | 0.82, 1.14 | 3.00 | 2.61, 3.46 | 0.71 | 0.40, 1.29 | 0.98 | 0.63, 1.51 | 1.09 | 0.85, 1.41 | ||
| Cigarette smoking | Heavy smoker | Never smoked | 1.39 | 0.70, 2.76 | 10.24 | 8.69, 12.1 | 1.73 | 1.41, 2.13 | 27.19 | 14.0, 52.9 | 6.80 | 3.73, 12.4 | 1.75 | 1.03, 2.97 |
| Light smoker | 0.90 | 0.62, 1.32 | 6.36 | 5.67, 7.14 | 1.14 | 1.02, 1.28 | 13.92 | 8.42, 23.0 | 3.15 | 2.11, 4.71 | 1.51 | 1.15, 1.97 | ||
| Former heavy smoker | 1.08 | 0.72, 1.63 | 2.63 | 2.18, 3.18 | 1.06 | 0.9, 1.26 | 8.43 | 4.50, 15.8 | 1.65 | 0.89, 3.06 | 1.38 | 0.96, 1.98 | ||
| Former light smoker | 0.61 | 0.46, 0.82 | 1.67 | 1.45, 1.92 | 1.08 | 0.98, 1.20 | 4.62 | 2.74, 7.80 | 1.13 | 0.75, 1.71 | 1.44 | 1.17, 1.78 | ||
| Former smoker, amount unknown | 0.76 | 0.44, 1.30 | 0.82 | 0.56, 1.21 | 0.85 | 0.66, 1.08 | 1.04 | 0.19, 5.56 | 1.28 | 0.60, 2.75 | 0.95 | 0.58, 1.55 | ||
| Daily fruit and vegetable consumption | 0 to 3 times | 6 or more times | 0.87 | 0.66, 1.15 | 1.27 | 1.12, 1.44 | 1.12 | 1.01, 1.24 | 1.03 | 0.65, 1.64 | 1.40 | 0.93, 2.10 | 1.01 | 0.79, 1.29 |
| 3 to 6 times | 0.85 | 0.69, 1.06 | 1.06 | 0.95, 1.19 | 1.13 | 1.04, 1.23 | 0.93 | 0.62, 1.39 | 1.06 | 0.74, 1.50 | 1.01 | 0.83, 1.22 | ||
| Leisure physical activity | Moderately active | Active | 1.13 | 0.82, 1.55 | 1.06 | 0.93, 1.20 | 0.88 | 0.78, 0.99 | 1.37 | 0.82, 2.29 | 0.54 | 0.36, 0.81 | 1.44 | 1.11, 1.88 |
| Slightly active | 1.07 | 0.79, 1.44 | 0.99 | 0.88, 1.12 | 0.98 | 0.89, 1.09 | 1.40 | 0.86, 2.27 | 0.61 | 0.42, 0.87 | 1.38 | 1.07, 1.78 | ||
| No physical activity | 1.57 | 1.12, 2.19 | 1.07 | 0.91, 1.25 | 1.07 | 0.94, 1.22 | 1.17 | 0.62, 2.22 | 0.46 | 0.28, 0.75 | 0.96 | 0.68, 1.35 | ||
Models have also been adjusted for: ethnicity, immigrant status, rural residence, education level, income, marital status, self-rated health, life stress, asthma and high blood pressure.
Table 4b.
Associations of the modifiable lifestyle risk factors with age to first chronic disease among males, by chronic disease type (cause-specific cox PH models)
| Characteristic | Comparison group | Reference group | CHF |
COPD |
Diabetes |
Lung cancer |
MI |
Stroke including TIA |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | csHR (95% CI) | |||||||||
| Alcohol consumption | Non-drinker | Light drinker | 1.39 | 1.05, 1.84 | 1.10 | 0.96, 1.27 | 1.17 | 1.06, 1.29 | 1.10 | 0.67, 1.80 | 1.51 | 1.16, 1.95 | 0.84 | 0.66, 1.07 |
| Moderate drinker | 0.85 | 0.62, 1.16 | 1.01 | 0.88, 1.17 | 0.97 | 0.87, 1.08 | 1.00 | 0.59, 1.68 | 1.11 | 0.84, 1.46 | 0.80 | 0.62, 1.02 | ||
| Heavy drinker | 1.27 | 0.84, 1.92 | 0.89 | 0.74, 1.06 | 0.72 | 0.62, 0.84 | 1.10 | 0.59, 2.02 | 0.95 | 0.67, 1.36 | 1.01 | 0.72, 1.41 | ||
| BMI | Underweight | Healthy weight | 1.43 | 0.42, 4.82 | 1.71 | 1.15, 2.54 | 1.55 | 0.98, 2.46 | 1.96 | 0.59, 6.52 | 0.00 | 0.00, 99.99 | 1.32 | 0.43, 40.00 |
| Overweight | 1.01 | 0.79, 1.29 | 0.88 | 0.79, 0.97 | 1.83 | 1.64, 2.03 | 0.63 | 0.44, 0.91 | 1.08 | 0.87, 1.33 | 0.92 | 0.75, 1.14 | ||
| Obese, class 1 | 1.46 | 1.08, 1.98 | 0.85 | 0.73, 0.98 | 3.68 | 3.28, 4.12 | 0.55 | 0.32, 0.96 | 1.40 | 1.08, 1.81 | 0.77 | 0.57, 1.03 | ||
| Obese, class 2 | 2.08 | 1.31, 3.31 | 0.81 | 0.62, 1.05 | 6.03 | 5.22, 6.97 | 0.54 | 0.18, 1.62 | 1.18 | 0.75, 1.86 | 1.44 | 0.94, 2.20 | ||
| Obese, class 3 | 1.78 | 0.73, 4.33 | 0.76 | 0.47, 1.25 | 8.95 | 7.4, 10.82 | 0.49 | 0.05, 5.05 | 1.30 | 0.57, 2.97 | 1.24 | 0.54, 2.87 | ||
| Unknown BMI | 1.39 | 0.99, 1.96 | 1.08 | 0.84, 1.38 | 2.16 | 1.71, 2.73 | 0.73 | 0.34, 1.54 | 1.17 | 0.75, 1.81 | 1.12 | 0.78, 1.60 | ||
| Cigarette smoking | Heavy smoker | Never smoked | 0.99 | 0.57, 1.72 | 7.99 | 6.75, 9.46 | 1.09 | 0.92, 1.30 | 38.60 | 18.7, 79.7 | 5.29 | 3.84, 7.28 | 1.27 | 0.84, 1.93 |
| Light smoker | 1.16 | 0.84, 1.59 | 5.52 | 4.81, 6.33 | 1.01 | 0.91, 1.12 | 15.40 | 7.88, 29.9 | 3.37 | 2.63, 4.31 | 1.03 | 0.79, 1.35 | ||
| Former heavy smoker | 1.12 | 0.83, 1.50 | 1.91 | 1.58, 2.31 | 1.09 | 0.97, 1.23 | 7.41 | 3.57, 15.4 | 1.44 | 1.06, 1.96 | 1.02 | 0.78, 1.33 | ||
| Former light smoker | 0.96 | 0.75, 1.23 | 1.62 | 1.38, 1.91 | 0.95 | 0.86, 1.04 | 4.01 | 1.96, 8.22 | 1.75 | 1.37, 2.23 | 0.69 | 0.54, 0.88 | ||
| Former smoker, amount unknown | 1.04 | 0.65, 1.65 | 0.90 | 0.61, 1.32 | 1.01 | 0.84, 1.21 | 2.59 | 0.73, 9.15 | 0.80 | 0.43, 1.49 | 0.74 | 0.46, 1.20 | ||
| Daily fruit and vegetable consumption | 0 to 3 times | 6 or more times | 1.02 | 0.75, 1.39 | 1.12 | 0.95, 1.32 | 1.13 | 1.01, 1.27 | 1.16 | 0.64, 2.09 | 1.03 | 0.78, 1.36 | 0.87 | 0.66, 1.14 |
| 3 to 6 times | 0.98 | 0.74, 1.30 | 1.09 | 0.93, 1.28 | 1.04 | 0.93, 1.15 | 1.16 | 0.65, 2.06 | 1.00 | 0.77, 1.30 | 1.00 | 0.78, 1.28 | ||
| Leisure physical activity | Moderately active | Active | 0.75 | 0.57, 0.99 | 0.89 | 0.77, 1.03 | 1.06 | 0.95, 1.17 | 1.81 | 1.06, 3.08 | 1.28 | 1/00, 1.62 | 0.88 | 0.69, 1.11 |
| Slightly active | 0.91 | 0.71, 1.16 | 1.20 | 1.06, 1.36 | 1.16 | 1.05, 1.27 | 1.70 | 1.03, 2.83 | 0.98 | 0.77, 1.24 | 0.90 | 0.72, 1.12 | ||
| No physical activity | 1.11 | 0.79, 1.58 | 1.31 | 1.11, 1.54 | 1.18 | 1.03, 1.35 | 1.81 | 0.96, 3.41 | 1.32 | 0.96, 1.80 | 1.02 | 0.73, 1.43 | ||
Models have also been adjusted for: ethnicity, immigrant status, rural residence, education level, income, marital status, self-rated health, life stress, asthma and high blood pressure.
For the analyses of additional chronic disease outcomes (n = 68 943), the added outcomes shifted the CIF for any chronic disease towards a lower age in both sexes compared with the main results (Supplementary Figure 2, available as Supplementary data at IJE online shows the composite chronic disease CIF using all other cancers). In general, the cause-specific associations between the modifiable lifestyle risk factors and any of the nine chronic diseases were attenuated (Supplementary Tables 4a and 4b, available as Supplementary data at IJE online). For the other five additional analyses that limited the other cancers outcome to lifestyle-associated cancers, the same amount of attenuation was observed in the composite chronic disease outcome, even for the lifestyle factor that was associated with the other cancers (Supplementary Table 4a and 4b, available as Supplementary data at IJE online). With the expanded definition, arthritis became the most frequent-occurring first chronic disease (Supplementary Figure 3a and b, available as Supplementary data at IJE online shows the CIF of all other cancers).
For the sensitivity analysis of 55 461 individuals who self-reported being free of common chronic conditions, the CIF for any chronic disease was shifted towards an older age in both sexes versus the main results (Supplementary Figure 4, available as Supplementary data at IJE online). Diabetes and COPD were less likely to occur in this subgroup, and CHF and stroke were more common (Supplementary Figure 5a and 5b, available as Supplementary data at IJE online). In both sexes, the csHRs were generally similar except that the associations between BMI and any of the six chronic diseases were greater than the main results (Supplementary Table 5, available as Supplementary data at IJE online).
Discussion
Any chronic disease
This study found that most individuals accumulated at least one of the six selected chronic diseases over their life. These findings are consistent with a recent study in the Ontario population, which found that two-thirds of individuals had four or more chronic conditions at the time of death.37 These findings also contribute to understanding multimorbidity,38 by characterizing when individuals develop their first chronic disease. Multimorbidity is a pressing strain on health systems, as individuals with multimorbidity have complex care needs and greater health expenditures.39–41
This study also examined the sex-specific associations between modifiable lifestyle risk factors and age to six chronic diseases. The sdHRs and csHRs estimated were similar because the competing event risk of death was low. From a relative hazard perspective, the magnitude of the associations between the lifestyle factors and age to first chronic diseases were generally higher in females than males. However, from a cumulative incidence perspective, males had a higher cumulative incidence of these diseases. The discrepancy can be attributed to the high burden of unhealthy lifestyle factors in males compared with females. Whereas relative hazards are important for understanding aetiology, these findings highlight the importance of understanding the distribution of lifestyle factors in the population, and that strategies to increase healthy lifestyle choices can have a greater absolute impact if segments of the population with unhealthy lifestyle choices are targeted, even if they are at lower hazard on a relative scale.
Specific chronic diseases
The cumulative incidences of each of the six chronic diseases separately by age provide insights into multimorbidity by showing which diseases are expected to occur first. This study shows that diabetes and COPD tend to occur first, reinforcing that prevention efforts that target the lifestyle risk factors of COPD (e.g. cigarette smoking) and diabetes (e.g. physical inactivity, BMI) should be directed at younger people. This will have subsequent effects later in the life course by improving quality of life and reducing health care utilization.
The associations of the lifestyle risk factors by specific chronic disease re-emphasizes that lifestyle factors are associated differently depending on the chronic disease. As expected, current cigarette smoking was found to increase the hazards of many of the selected chronic diseases, and it was found that the associations for type of smoker (e.g. current smoker) were stronger for certain diseases. Being a non-drinker was associated with an increased hazard for several of the chosen chronic diseases in both sexes. These findings agree with several existing studies showing that moderate consumption of alcohol is associated with reduced incidence of chronic diseases like coronary heart disease and diabetes.42,43 There may also be residual confounding with non-drinkers, as this may be a heterogeneous group that includes lifetime abstainers of alcohol and individuals who have stopped drinking, potentially for health reasons. Although no protective association of physical activity was observed in females, this is not entirely unexpected as physical activity as measured in the CCHS has limitations. Only leisure physical activity was measured historically; other forms of physical activity (e.g. transportation, work) were not collected. Nevertheless, these results underscore the importance of using age- and sex-specific health prevention strategies that focus on modifying lifestyle behaviours to prevent multiple diseases simultaneously, instead of disease-specific strategies.
Strengths and limitations
One strength of the study was that we were able to improve chronic disease outcome identification by attributing certain deaths to a chronic disease using vital statistics data in addition to diagnosis from the health care use data. This reduced the misclassification of MI and, to a lesser extent, stroke. Another strength of the study is that the individuals were drawn from a representative, population-based sample. It should be noted that the results are only generalizable to adults over the age of 20 years living without the six chronic diseases of interest at baseline, and may not represent the general risk profile in the population (Supplementary Table 6, available as Supplementary data at IJE online). However, the sensitivity analysis among individuals free of common chronic diseases at baseline show that the associations between lifestyle factors and any of the six chronic diseases were similar in direction and magnitude compared with the main results. These results suggest that previous chronic disease (which can be considered as competing risk for our diseases of interest) does not seem to affect the relationship between lifestyle factors and future chronic disease. However, future work into how individuals transition to multimorbidity as they age would help elucidate the role of previous chronic diseases on the association between the modifiable lifestyle risk factors and ensuing chronic disease.
A limitation of the study is that lifestyle information was only measured once. Longitudinal data would help elucidate the temporal relationships between lifestyle factors and chronic disease incidence, and how changes in lifestyle behaviours during the life course relate to chronic disease incidence. They would also help explain how the risks of different chronic diseases vary by lifestyle behaviour, and how the contributions of the lifestyle behaviours to chronic disease incidence may change. Another limitation is that diet was only measured using the daily consumption frequency of fruits and vegetables. The serving size was not measured, and the consumption patterns of other food groups (e.g. carbohydrates) or specific dietary risk factors (e.g. sodium) were not collected. Also, whereas strong associations were observed with cigarette smoking, there may still be residual confounding as aspects of smoking history were not adequately captured, such as time since quitting among former smokers.
We intentionally sought to include diseases with known associations with: the modifiable lifestyle risk factors; high prevalence; and impact on health status, morbidity and mortality. However, other chronic diseases could have been included in the composite endpoint. The additional analysis also showed that the choice of chronic diseases can affect the associations of interest. When more chronic diseases were added as outcomes, the results were maintained in terms of direction, but the magnitude of the associations were attenuated because of the predominance of arthritis as the most commonly occurring chronic disease. Whereas arthritis is associated with some of the lifestyle factors, such as BMI,44 it is less clearly related to the others. Surprisingly, the cause-specific hazard ratios did not change much when all other cancers were modelled versus only cancers with known associations with the lifestyle factors. We attribute this null finding to the fact that the overall effect of other cancers on the cumulative incidence and hazard ratios is weighted by the overall magnitudes of their effect sizes and their incidence in our cohort. In this case, the incidence of all other cancers was low overall (12.8%), and further limiting the cancers to ones associated with lifestyle behaviours decreased the incidence further (3.8% to 7.6%, depending on the lifestyle factor).
Conclusions
In summary, we found that most people will have at least one chronic disease by the end of their life. This study provides a novel approach using methods for competing risks to examine the incidence of several chronic diseases relative to the life course and how their incidences are associated with lifestyle factors. Further studies that consider how multiple diseases relate to shared risk factors will support more impactful chronic disease prevention strategies and the management and treatment of multimorbidity.
Funding
This work was supported by the Canadian Institutes of Health Research Partnerships for Health System Improvement (grant number FRN 141803); and the Ontario Ministry of Health and Long-Term Care (grant number 6717). This study was also assisted by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Conflict of interest: None declared.
Supplementary Material
References
- 1.World Health Organization. Global Status Report on Noncommunicable Diseases 2014. Geneva: WHO, 2014. [DOI] [PubMed] [Google Scholar]
- 2.Public Health Agency of Canada. How Healthy Are Canadians: A Trend Analysis of Canadians From a Healthy Living and Chronic Disease Perspective. Ottawa: PHAC, 2016. [Google Scholar]
- 3. Busse R, Blumel M, Scheller-Kreinsen D, Zentner A.. Tackling Chronic Disease in Europe: Strategies, Interventions, and Challenges. Geneva: WHO, 2010. [Google Scholar]
- 4. Bauer UE, Briss PA, Goodman RA, Bowman BA.. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014;384:45–52. [DOI] [PubMed] [Google Scholar]
- 5. Fortin M, Pinho G, Gignac J, Almirall J, Lapointe L, Dionne J.. Randomized controlled trials: do they have external validity for patients with multiple comorbidities? Ann Fam Med 2006;4:104–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Parekh AK, Barton MB.. The challenge of multiple comorbidity for the US Health Care System. JAMA 2010;303:1303–4. [DOI] [PubMed] [Google Scholar]
- 7. Fortin M, Soubhi H, Hudon C, Bayliss EA, van den Akker M.. Multimorbidity’s many challenges. BMJ 2007;334:1016–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Betancourt MT, Roberts KC, Bennett T-L, Driscoll ER, Jayaraman G, Monitoring PL.. Chronic diseases in Canada: the Chronic Disease Indicator Framework. Chronic Dis Inj Can 2014;34(Suppl 1):1–30. [PubMed] [Google Scholar]
- 9. Beaglehole R, Bonita R, Horton R. et al. Priority actions for the non-communicable disease crisis. Lancet 2011;377:1438–47. [DOI] [PubMed] [Google Scholar]
- 10. Kearns K, Dee A, Fitzgerald AP, Doherty E, Perry IJ.. Chronic disease burden associated with overweight and obesity in Ireland: the effects of a small BMI reduction at population level. BMC Public Health 2014;14:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gaziano TA, Galea G, Reddy KS.. Scaling up interventions for chronic disease prevention: the evidence. Lancet 2007;370:1939–46. [DOI] [PubMed] [Google Scholar]
- 12. Brownson RC, Haire-Joshu D, Luke DA.. Shaping the context of health: a review of environmental and policy approaches in the prevention of chronic diseases. Annu Rev Public Health 2006;27:341–70. [DOI] [PubMed] [Google Scholar]
- 13. Bunnell R, O’Neil D, Soler R. et al. Fifty communities putting prevention to work: accelerating chronic disease prevention through policy, systems and environmental change. J Community Health 2012;37:1081–90. [DOI] [PubMed] [Google Scholar]
- 14. Béland YC. Canadian community health survey - methodological overview. Health Rep 2002;13:9–14. [PubMed] [Google Scholar]
- 15. McLaughlin JR, Kreiger N, Marrett LD, Holowaty EJ.. Cancer incidence registration and trends in Ontario. Eur J Cancer 1991;27:1520–4. [DOI] [PubMed] [Google Scholar]
- 16. Schultz SE, Rothwell DM, Chen Z, Tu K.. Identifying cases of congestive heart failure from administrative data: a validation study using primary care patient records. Chronic Dis Inj Can 2013;33:160–6. [PubMed] [Google Scholar]
- 17. Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T.. Identifying individuals with physician diagnosed COPD in health administrative databases. COPD 2009;6:388–94. [DOI] [PubMed] [Google Scholar]
- 18. Hux JE, Ivis F, Flintoft V, Bica A.. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care 2002;25:512–6. [DOI] [PubMed] [Google Scholar]
- 19. Austin PC, Daly PA, Tu JV.. A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. Am Heart J 2002;144:290–6. [DOI] [PubMed] [Google Scholar]
- 20. Tu K, Wang M, Young J. et al. Validity of administrative data for identifying patients who have had a stroke or transient ischemic attack using EMRALD as a reference standard. Can J Cardiol 2013;29:1388–94. [DOI] [PubMed] [Google Scholar]
- 21. Shields M, Gorber SC, Janssen I, Tremblay MS.. Bias in self-reported estimates of obesity in Canadian health surveys: an update on correction equations for adults. Health Rep 2011;22:35–45. [PubMed] [Google Scholar]
- 22. Korn EL, Graubard BI, Midthune D.. Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol 1997;145:72–80. [DOI] [PubMed] [Google Scholar]
- 23. Hosmer DW, Lemeshow S, May S.. Applied Survival Analysis. 2nd edn Hoboken, NJ: Wiley, 2008. [Google Scholar]
- 24. Therneau TM, Grambsch PM.. Modeling Survival Data: Extending the Cox Model. 1st edn New York, NY: Springer; 2000. [Google Scholar]
- 25. Hu FB. Globalization of diabetes: The role of diet, lifestyle, and genes. Diabetes Care 2011;34:1249–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mosca L, Barrett-Connor E, Kass Wenger N.. Sex/gender differences in cardiovascular disease prevention: What a difference a decade makes. Circulation 2011;124:2145–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Postma DS, Bush A, Van Den Berge M.. Risk factors and early origins of chronic obstructive pulmonary disease. Lancet 2015;385:899–909. [DOI] [PubMed] [Google Scholar]
- 28. Irigaray P, Newby JA, Clapp R. et al. Lifestyle-related factors and environmental agents causing cancer: An overview. Biomed Pharmacother 2007;61:640–58. [DOI] [PubMed] [Google Scholar]
- 29. Marisol B, Brenda B, Geneviève G. et al. At-a-glance - The 2017 Canadian Chronic Disease Indicators. Health Promot Chronic Dis Prev Canada 2017;37:248–51. [Google Scholar]
- 30. Austin PC, Fine JP.. Practical recommendations for reporting Fine-Gray model analyses for competing risk data. Stat Med 2017;36:4391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.International Agency for Research on Cancer. Personal Habits and Indoor Combustions. Volume 100 E. A Review of Human Carcinogens. IARC Monogr Eval Carcinog Risks to Humans [Internet] 2012. http://www.ncbi.nlm.nih.gov/pubmed/23193840 (11 February 2019, date last accessed). [PMC free article] [PubMed]
- 32.International Agency for Research on Cancer. IARC Handbooks of Cancer Prevention: Weight Control and Physical Activity Vol. 6. Lyon, France: IARC Press, 2002.
- 33.International Agency for Research on Cancer. IARC Handbooks of Cancer Prevention: Fruits and Vegetables Vol. 8. Lyon, France: IARC Press, 2003.
- 34.International Agency for Research on Cancer. Personal Habits and Indoor Combustions Volume 100 E. Consumption of Alcoholic Beverages 2011. http://monographs.iarc.fr/ENG/Monographs/vol100E/mono100E-11.pdf (11 February 2019, date last accessed).
- 35.International Agency for Research on Cancer. IARC Handbooks of Cancer Prevention: Absensce of Excess Body Fatness Vol. 16. Lyon, France: IARC Press, 2018.
- 36.United Nations, Department of Economic and Social Affairs. World Population Prospects: The 2015 Revision New York, NY; UNO, 2015.
- 37. Rosella L, Kornas K, Huang A, Bornbaum C, Henry D, Wodchis WP.. Accumulation of chronic conditions at the time of death increased in Ontario from 1994 to 2013. Health Aff 2018;37:1–9. [DOI] [PubMed] [Google Scholar]
- 38. Pefoyo AJK, Bronskill SE, Gruneir A. et al. The increasing burden and complexity of multimorbidity. BMC Public Health 2015;15:415.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wodchis W. Performance measurement for people with multimorbidity and complex health needs. Healthc Q 2016;19:44–8. [DOI] [PubMed] [Google Scholar]
- 40. Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, van den Bos GA.. Causes and consequences of comorbidity: a review. J Clin Epidemiol 2001;54:661–74. [DOI] [PubMed] [Google Scholar]
- 41. Thavorn K, Maxwell CJ, Gruneir A. et al. Effect of socio-demographic factors on the association between multimorbidity and healthcare costs: a population-based, retrospective cohort study. BMJ Open 2017;7:e017264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Corrao G, Rubbiati L, Bagnardi V, Zambon A, Poikolainen K.. Alcohol and coronary heart disease: A meta-analysis. Addiction 2000;95:1505–23. [DOI] [PubMed] [Google Scholar]
- 43. Baliunas DO, Taylor BJ, Irving H. et al. Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2009;32:2123–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Litwic A, Edwards MH, Dennison EM, Cooper C.. Epidemiology and burden of osteoarthritis. Br Med Bull 2013;105:185–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.