Abstract
Black women and Latinas have more symptoms of depression and anxiety during pregnancy than do their non-Latina White counterparts. While effective interventions targeting internalizing disorders in pregnancy are available, they are primarily tested with White women. This article reviews randomized controlled trials and non-randomized studies to better understand the effectiveness of psychological interventions for anxiety and depression during pregnancy in Latinas and Black women. Additionally, this review summarizes important characteristics of interventions such as intervention format, treatment modality, and the use of cultural adaptations. Literature searches of relevant research citation databases produced 68 studies, 13 of which were included in the final review. Most studies were excluded because their samples were not majority Latina or Black women, or because they did not test an intervention. Of the included studies, three interventions outperformed a control group condition and showed statistically significant reductions in depressive symptoms. An additional two studies showed reductions in depressive symptoms from pre to post-treatment using non-controlled designs. The remaining eight studies (seven randomized and one non-randomized) did not show significant intervention effects. Cognitive behavioral therapy was the modality with most evidence for reducing depressive symptoms in pregnant Black and Latina women. No intervention was found to reduce anxiety symptoms, although only two of the 13 measured anxiety as an outcome. Five studies made cultural adaptations to their treatment protocols. Future studies should strive to better understand the importance of cultural modifications to improve engagement and clinical outcomes with pregnant women receiving treatment for anxiety and depression.
Keywords: pregnancy, Latinos/Latinas, Blacks/African Americans, depression, anxiety, treatment
Prevalence rates of depression during pregnancy range from 12% to 27%. Rates of anxiety during pregnancy are similar, affecting 9% to 22% of women (Mahaffey & Lobel, 2018). Variability in these rates often depends on whether the data are taken from epidemiological or high-risk samples. A diagnosis of depression (Grote et al., 2010) or anxiety (Ding et al., 2014) during the prenatal period increases risk for complications during delivery such as preterm birth and low birthweight, and is a robust predictor of postpartum depression (Coelho, Murray, Royal-Lawson, & Cooper, 2011; Robertson, Grace, Wallington, & Stewart, 2004). Black women and Latinas in the U. S. have higher rates of depression (e.g., Rich-Edwards et al., 2006) and anxiety (Collins & David, 2005) during pregnancy than do their non-Latina White counterparts. Immigrant Black and Latina women are at especially high-risk for internalizing distress during pregnancy due to a host of social stressors such as separation from extended families and lack of familiarity with medical systems of the countries they have immigrated to (Edge, Baker, & Rogers, 2004; Fung & Dennis, 2010). Black women and Latinas are also disproportionately exposed to financial and cultural stressors (e.g. poverty, discrimination), which invoke additional risk for clinical distress (Rosenthal & Lobel, 2011).
Data indicate disparities in mental health service utilization during the perinatal period; rates of services use in Latinas and Black women, are 5% and 4% respectively, and the rate of service use in White women, is 10%, a statistically significant difference (Kozhimannil, Trinacty, Busch, Huskamp, & Adams, 2011). Black women and Latinas are at a greater disadvantage than White women when it comes to treating their depression and anxiety during pregnancy because they are less likely to attend perinatal medical appointments than White women, where symptoms are often first detected (Kozhimannil et al., 2011; Lucero, Beckstrand, Callister, & Sanchez Birkhead, 2012). Even when Latinas and Black women initiate mental health treatment, they are less likely to receive follow up or continued care treatment (Kozhimannil et al., 2011). System level barriers include infrequent screening for anxiety and depression by obstetrics providers during pregnancy (Goodman & Tyer-Viola, 2010), which is even more pronounced in under-resourced clinics which are often attended by Black women and Latinas. Other barriers that disproportionately affect ethno-racial women include difficulties accessing transportation and child care, unmet or unrealistic expectations about treatment outcome, stigma, and healthcare mistrust (Levy & O’Hara, 2010). A challenge unique to pregnant women with depression and anxiety more broadly is that psychiatric care is often declined or delayed due to the potential adverse effects of psychotropic medications for mother and fetus (Schofield & Kapoor, 2019). Psychological interventions fare better in terms of safety and acceptability during pregnancy (Goodman, 2009), yet it is relatively uncommon for women with internalizing distress to receive psychological interventions during this time (Ko, Farr, Dietz, & Robbins, 2012).
Most existing interventions for internalizing distress have been examined during the postpartum period (Mahaffey & Lobel, 2018). However, a growing body of literature shows that psychological interventions can successfully reduce depressive symptoms during pregnancy for women considered high-risk (i.e. elevated symptoms, below clinical levels) (Bledsoe & Grote, 2006; Dennis & Hodnett, 2007; Werner, Miller, Osborne, Kuzava, & Monk, 2015) and clinically impacted (van Ravesteyn, Lambregtse - van den Berg, Hoogendijk, & Kamperman, 2017). The evidence for treating anxiety during pregnancy is much more sparse, and existing interventions to treat prenatal anxiety require more rigorous evaluation (Loughnan et al., 2018). Importantly, the vast majority of intervention trials for prenatal depression and anxiety have been tested with non-Latina White women (Nillni, Mehralizade, Mayer, & Milanovic, 2018). The lack of representation of ethno-racial minority women in clinical trials during pregnancy makes it difficult to ascertain whether these interventions are effective for Black and Latina women.
Evidence for Psychological Interventions for Depression and Anxiety in Pregnancy
Meta-analytic findings show that the most effective psychological intervention modalities for depression during pregnancy are Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT) (Curry et al., 2019; Dennis & Hodnett, 2009; van Ravesteyn et al., 2017). There is less of an evidence base for prenatal anxiety, and CBT delivered in a group setting is the only modality with any research support (Nillni et al., 2018). CBT conceptualizes depression and anxiety as caused and maintained by maladaptive patterns of thinking, emotional responses and behavior, and targets thoughts and activities in order to improve mood. IPT, on the other hand, conceptualizes depression as caused and maintained in large part by interpersonal dysfunction; thus, it targets interpersonal functioning and social support. Both CBT and IPT are time-limited interventions and are most often delivered in-person by a therapist (Sockol, Epperson, & Barber, 2011). However, despite the success of these evidence-based interventions at reducing depression, and the emerging support for anxiety reduction during the perinatal period (e.g. Goodman et al., 2014), their efficacy with ethno-racial minority women is mixed (Nillni et al., 2018). Nillni and colleagues (2018) report that while several pilot studies for pregnant ethno-racial minority women have shown that psychotherapies such as CBT and IPT successfully reduce depressive symptoms, larger scale RCTs often report null findings. Findings that have indicated no intervention effect are often attributed to worse treatment engagement of minority women when compared to White women (Grote, Zuckoff, Swartz, Bledsoe, & Geibel, 2007) but it is possible that other factors are at play.
Taken together, findings suggest that pregnant Latinas and Black women appear to utilize and benefit from interventions to treat internalizing distress less often than pregnant White women, indicating a potential mental health care disparity. The present study systematically reviewed the treatment outcome literature with Latina and Black pregnant women in order to better understand mental health care and treatment disparities in this group. This systematic review examined 1) outcomes of psychological interventions for anxiety and depression during the prenatal period in Latina and Black women; 2) treatment characteristics (i.e., treatment modality, format, context of delivery, provider type) of effective interventions with pregnant Latina and Black women and 3) types of cultural adaptations used to tailor interventions to meet the needs of ethnic/racial minority women. Given that treatment during pregnancy is uniquely positioned to create positive intergenerational change at a particularly sensitive developmental period (Stewart, 2011), a better understanding of the evidence for treating ethno-racial minority women prenatally is critical to addressing service gaps for pregnant Black and Latina women and their infants.
Methods
Protocol and registration
The review was preregistered with PROSPERO, the International Prospective Register of Ongoing Systematic Reviews (ID: CRD42018106228), and can be found at: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=106228
Eligibility Criteria (Inclusion/Exclusion Criteria)
The following criteria had to be met for inclusion in the review: Studies were published in peer reviewed journals or as a doctoral thesis and tested the effect of a psychological intervention on depressive or anxious symptoms during pregnancy. Psychological interventions were inclusive of manualized psychoeducational strategies, cognitive behavioral therapy, interpersonal psychotherapy, psychodynamic therapy, acceptance and commitment therapy, and mindfulness training delivered during the prenatal period via telephone, home or clinic visits, or individual or group sessions by a health professional or lay person (Dennis & Hodnett, 2009). Unstructured interventions (e.g. providing social support) were excluded from the review because of the difficulties replicating their delivery and ascertaining fidelity of delivery—of concern when assessing the evidence for a particular intervention modality (Chambless & Ollendick, 2001). Studies also had to measure depression and anxiety symptoms as an outcome using standardized depression and anxiety instruments (e.g. Edinburgh Postnatal Depression Scale; EPDS; Cox, Holden, & Sagovsky, 1987).
Additionally, in order for a study to eligible for inclusion, study participants had to be: a) pregnant women, b) 18 years or older, and c) residing in the United States. Further, a majority of the sample (75% or more) had to identify as Latina/Hispanic or Black/African American. This threshold was chosen based on previous reviews and meta-analyses (Huey & Polo, 2008; Pina, Polo, & Huey, 2019) where a 3:1 ratio of ethnic minority participants to White participants was identified as providing sufficient representation to suggest that observed treatment effects are in fact applicable to minorities. However, studies were also included if they had fewer than 75% of Latina or Black women but provided a separate analysis with a subset of ethnic/racial minority participants. Inclusion was constrained to women living in the United States in order to more easily interpret results based on common system level factors (e.g., perinatal health care policies), and specific sociocultural experiences related to being Latina or Black in the United States that may impact anxiety and depression in this population.
Search Strategy
The following databases were searched: Cumulative Index to Nursing and Allied Health Literature (CINAHL®), PubMed®, PsycINFO®, Web of Science® and ProQuest Dissertation and Theses AI® using the following search terms: (prenatal OR antenatal OR pregnancy) AND (intervention OR treatment OR therapy) AND (postpartum depression OR depression OR anxiety), AND (African-American OR Black OR Latino(a) OR Hispanic OR minority); see Figure A.1 in the Appendix for exact search syntax. Reference sections of the articles that met inclusion criteria were also examined. No date restrictions were placed on database searches, and unpublished studies were not considered due to the increased likelihood that identified studies would introduce greater methodological weakness (Copeland, Gallo, & Alolabi, 2019) in a review that was already inclusive of non-randomized trials. Database searches were conducted from 6/2018–9/2018, by authors CP and HZ, with consultation as needed from NM and DC. In total, searches produced 503 studies, with 363 remaining once duplicates were removed. Duplicates were identified using Mendeley’s duplication feature, and manually checked by the authors. Abstracts and titles were subsequently screened using inclusion criteria, eliminating 296 articles, most often because the studies did not test an intervention (n=243) (of note, search terms did not include design specifications such as “RCT”). Of the 67 articles remaining, methods sections were examined to further assess inclusion criteria (e.g., intervention was delivered during pregnancy). An additional 56 articles were excluded (see Figure 1, below, for detailed information about exclusion), leaving 13 studies that met all inclusion criteria and were included in the final review.
Figure 1.
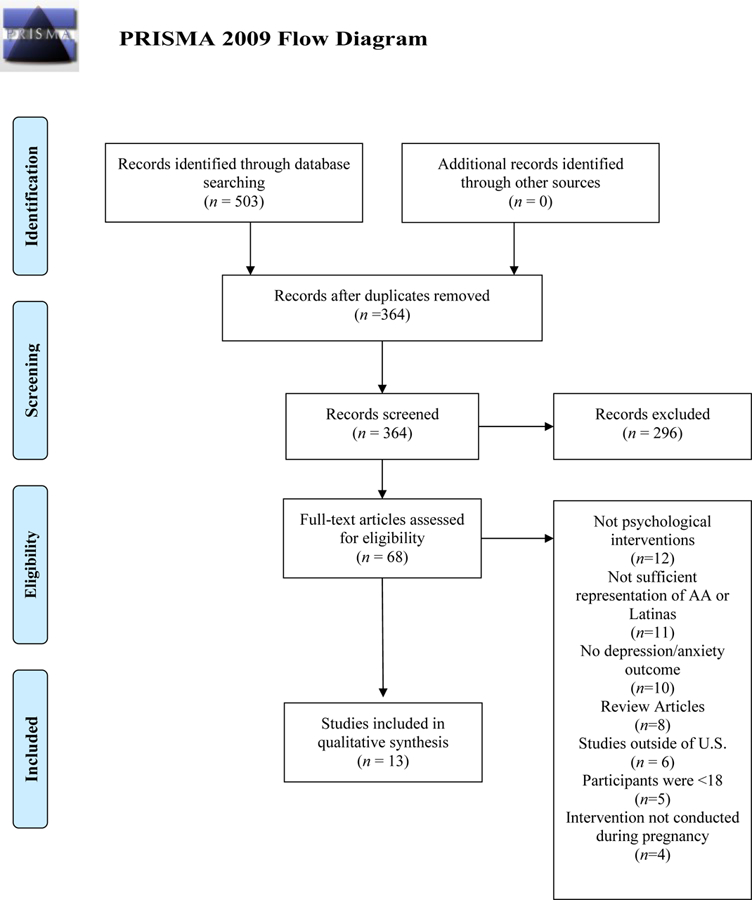
Prisma Flow Diagram of Study Inclusion
Data Extraction
Data were extracted from the 13 articles independently by two members of the research team, who conferred to check for accuracy. Variables extracted from each study were: intervention characteristics (i.e., intervention format, treatment modality, provider type, number of sessions, setting and fidelity indices), participant demographics (i.e., race/ethnicity, language spoken, US vs. foreign born, indicators of income), the perinatal period during intervention delivery, type of study design (e.g., RCT, pre-post design, study sample), the use of a control group and what kind, if applicable, attrition rates, outcomes pertaining to depression or anxiety, and the use of intervention cultural adaptations.
Data Quality Assessment
The methodological biases of the studies in this review were assessed using the Cochrane Risk of Bias Assessment. The risk of bias tool is recommended over the use of other quality scales (e.g., Outcome Reporting Bias in Trials, ORBIT-II; GRADE rating of quality evidence; see Page, McKenzie & Higgins, 2018 for extensive list) due to the assessment of different aspects of biases in trial conduct. Specifically, six categories of bias are assessed: a) selection bias, (b) performance bias, (c) detection bias, (d) attrition bias, (e) reporting bias, and (f) baseline imbalance. In addition, the tool requires that researchers provide evidence (e.g. direct quotes from the article) that support each judgment of bias, increasing transparency (Higgins et al., 2011). Studies were coded as having a high risk of bias, low risk of bias, or an unclear risk of bias by the first author, who was not blind to study authors, place of publication, or results. Studies rated as “low risk of bias” on four of the six categories were considered to have an overall low risk of bias; studies with two or three categories rated as “low risk of bias” were considered to have an overall medium risk of bias; and studies with one or fewer categories rated as “low risk of bias” were considered to have an overall high risk of bias. Documentation supporting bias ratings is available upon request.
Results
Of the 13 studies that met the inclusion criteria, 10 were randomized controlled trials (RCT) and three of these studies were self-described as pilot studies. Only one RCT used an active control group, which consisted of a social support intervention in addition to regular prenatal care (Field, Diego, Delgado, & Medina, 2013). Three other studies were non-randomized pre-post designs (one did not use a comparison group, one used a comparison group similar in demographic characteristics, and one study used a TAU comparison group).
Sample sizes in the studies ranged from 13 to 913, and the combined sample size of included studies totaled 1,971 women whose outcomes are included in this review. Among the 13 studies, four tested interventions in Black-only samples, three in Latina-only samples, three with a combination of Latina and Black women, and three with a combination of Black and White women. Women across all studies were considered low-income, and most Latinas were of Mexican origin. Most studies required women to have elevated symptoms of depression (Crockett, Zlotnick, Davis, Payne, & Washington, 2008; Grote et al., 2009; Jesse et al., 2015.; Le, Perry, & Stuart, 2011; Muñoz et al., 2007; Sampson, Villarreal, & Rubin, 2016), or meet a clinically significant cutoff for depression (Field et al., 2013; Jesse et al., 2010; Lenze & Potts, 2017; McKee, Zayas, Fletcher, Boyd, & Nam, 2006). None of the 13 eligible studies required women to meet any anxiety symptom cutoff. In addition, only two studies measured anxiety as a secondary outcome (Field et al., 2013; Lenze & Potts, 2017). For detailed sociodemographic information about included participants see Table 1.
Table 1.
Sociodemographic Characteristics of Study Samples
| Publication | Study Sample | Nativity | Age M (SD) | Language | Weeks Gestation | Socioeconomic status |
|---|---|---|---|---|---|---|
| Crockett et al, 2008 | n= 36 AA/B | 100% U.S. born | 23.4 (4.98) | English | 24–31 | All participants received public assistance |
| El-Mohandes, et al., 2008 | n= 913 AA/B | 100% U.S. born | 24.6* | English | ≤ 28 | 75% of sample was on Medicaid |
| Field et al., 2013 |
n= 38
AA/B n= 5 L/H n= 1 W |
Not Reported | 24.90 (5.40) | English | 20–24 | State low income, no additional data provided |
| Grote et al., 2009 |
n= 33
AA/B n= 2 L/H n=15 W n= 3 Biracial |
Not Reported | 24.6 (5.46) | English | 10–32 | Annual income: 58.5% < $10,000, 26.4% $10,000-$20,000, 15.1% >$20,000 |
| Jesse et al., 2010 |
n=21
AA/B n= 5 W |
100% US born | 24.69 (5.33) | English | 6–30 | State low income, no additional data provided |
| Jesse et al., 2015 |
n=99 AA/B
n=47 W |
Not Reported | 25.05 (5.49) | English, Spanish | 6–30 | 38.4% Employed, 61.6% Unemployed, 82.2% Medicaid recipient, 4.8% Medicare recipient |
| Kieffer et al., 2013 | n= 275 L/H | 97% foreign born | 34% over 30 years | Spanish | <20 | State low income, no additional data provided |
| Le et al., 2011 | n= 217 L/H | 100% foreign born | 25.41 (4.59) | Spanish | ≤ 24 | 90% of the households had an annual income under $30,000 |
| Lenze & Potts, 2017 |
n= 33
AA/B n=7 W n= 2 Other |
Not Reported | 26.64 (5.89) | English | 12–30 | Annual income: 40% <$10,000; 20% $10,001–$20,000; 5% $20,001–$30,000; 12.5% $30,001–$60,000; 2.5% >$60,001 |
| McKee et al., 2006 |
n= 43
AA/B n= 57 L/H |
23% foreign born | 24.7 (5.6) | English, Spanish | <32 weeks | State low income, no additional data provided |
| Muñoz et al., 2007 | n= 41 L/H | 76% foreign born | 24.9 (4.54) | English, Spanish | 12–32 | Mean annual income $19,773.2 |
| Sampson et al., 2016 | n= 13 AA/B | Not Reported | 24.0 (5.0) | English | ≥ 12 | 100% unemployed, mean monthly income $1,153 |
| Zhang & Emory, 2015 | n= 65 AA/B | 100% U.S. born | 25.3 (4.6) | English | 6–30 | Monthly income: 32.3% <$249, 30.8% $250–499, 29.2% $500-$999, 7.7%>$999 |
Note. AA/B=African American/Black, L/H= Latina /Hispanic, W= Non-Hispanic/Latina white. NR=not reported.
Indicates that the standard error, and not the SD was reported
Intervention Characteristics
A variety of psychological interventions to reduce perinatal depressive symptoms among Black women and Latinas emerged as part of this review. The most common treatment modality was CBT (El-Mohandes et al., 2008; Jesse et al., 2010; Jesse et al., 2015; Le et al., 2011; Muñoz et al., 2007; Sampson et al., 2016), followed by IPT (Crockett et al., 2008; Field et al., 2013; Grote et al., 2009; Lenze & Potts, 2017). CBT+ social support (McKee et al., 2006), behavioral activation (Kieffer et al., 2013) and mindfulness (Zhang and Emory, 2015) were also examined. Of the six interventions that included Latina participants, four of them gave the option for the delivery of the intervention to be in Spanish (Le et al., 2011; Kieffer et al., 2013; McKee et al., 2006; Muñoz et al., 2007).
Interventionists were primarily master’s or PhD level therapists (Crockett et al., 2008; El-Mohades et al., 2008; Field et al., 2013; Grote et al., 2009; Jesse et al., 2010; Jesse et al., 2015; Lenze & Potts, 2018; McKee et al., 2006; Muñoz et al., 2007; Zhang and Emory, 2015), followed by community health workers (Kieffer et al., 2013) or community case workers (Sampson et al., 2016). Only one study relied on trained bachelor’s level study staff (Le et al., 2011). Most often, interventions were delivered in group format (Crockett et al., 2008; El-Mohandes et al., 2008; Field et al., 2013; Jesse et al., 2015; Le et al., 2011; Zhang and Emory, 2015) although some studies provided a combination of group and individual sessions (Kieffer et al., 2013; Muñoz et al., 2007) or individual sessions only (Grote et al., 2009; Lenze & Potts, 2017; McKee et al., 2006; Sampson et al., 2016). Jesse and colleagues (2010) allowed women to choose whether they wanted to complete the intervention individually or in a group.
Treatment Response
Treatment response was determined by evaluating clinical outcomes for depression or anxiety (which was a secondary outcome in two studies). Outcomes are reported first for randomized controlled trials and then for non-randomized intervention studies. For additional intervention characteristics as well as their clinical outcomes, see Table 2.
Table 2.
Design, Measurement and Results of Reviewed Studies
| Publication | Intervention a) format, b) treatment modality, c) # sessions, M session attendance, d) provider (and provider education), e) setting |
Control Group | Results Main Effects | Cultural Factors |
|---|---|---|---|---|
| Randomized Controlled Trials
(RCT) | ||||
| Crockett, et al., 2008 | a) group, + 1 in home one-on-one booster
session postpartum b) IPT c) 4 90-minute sessions + 1 50-min booster, (M=4.58) session d) community therapists (Ph.D. or M.Ed. in counseling) e) not reported, not at participant home |
prenatal TAU | Women in the intervention and control groups showed no significant differences in depression scores (EPDS) 4 weeks post-intake (during pregnancy), 2 weeks after delivery, or 3 months postpartum. | No |
| El-Mohandes, et al., 2008 | a) group, (2 optional individual booster
sessions) b) CBT c) 8 sessions, (M=4) d) master’s level counselors e) clinic-based |
prenatal TAU | Women in the intervention group were more likely to resolve their depression (e.g. no longer show clinical elevations; Hopkins Symptom Checklist) in the postpartum period as compared to women in control group | Not reported |
| Field, et al., 2013 | a) group b) IPT c) 12 60-minute sessions, (M=11.7) d) therapist (education not known) e) not reported |
Peer Support: 20-minute group session 1/week for 12 weeks | Women in both the intervention and active control group showed significant reductions in depression (CES-D) and anxiety symptoms (STAI) from first to last session of treatment (during pregnancy). IPT did not outperform the active control condition. | Not reported |
| Grote, et al., 2009 | a) individual b) IPT c) 8 sessions d) master’s and doctoral level therapists e) OBGYN office |
Enhanced Prenatal Care (with referrals for mental health services) | Women in the intervention group showed significantly greater reductions in depressive symptoms (EPDS) between baseline and post-intervention, and between baseline and 6-months postpartum, as compared to women in the control group. | Yes: Use of therapists trained in cultural competence with experience working with poor racial-ethnic minority groups, culturally relevant pictures, stories from the participants’ cultural background to reinforce treatment goals, culturally sensitive psychoeducation about depression and use of cultural resources (e.g., spirituality, familism). |
| Kieffer et al., 2013 | a) individual and group (2 individual home
visits, 9 meetings during pregnancy; 2 individual home visits 1 group
meeting postpartum) b) “healthy lifestyle intervention”- pre and postnatal care, behavioral activation, psychoeducation c) 14 sessions, (M=10.5) d) community health workers/”women’s health advocates”, education not reported e) community partner settings (e.g., Community Health and Social Services) |
Healthy Pregnancy Education--four group meetings; 3 during pregnancy and 1 postpartum. | Women in the intervention group, but not in the control group showed significant reductions in depressive symptoms (CES-D) between baseline and follow-up (during pregnancy). The significant intervention effect did not extend into the early postpartum period. | No |
| Le et al., 2011 | a) group b) CBT c) 8 weeks 2-hour sessions, 3 individual booster sessions postpartum, (M=4) d) Bachelor’s level study staff e) clinic |
prenatal TAU | Women in both the intervention and control groups showed significant decreases in depressive symptoms (BDI-II) from pre to post-treatment. The cumulative incidence of major depressive episodes was not significantly different between the intervention (7.8%) and control (9.6%) groups. | Yes: incorporation of healthy management of reality and developmental/parenting issues for the unique needs of the predominantly Central American families such as immigration stressors. |
| Lenz & Potts, 2017 | a) individual b) IPT c) 9 sessions (1 ethnographic introductory session + 8 IPT sessions); plus maintenance treatment session if participant finish all 9 sessions d) Clinical Psychologists, master’s level clinicians e) research clinic, participant homes, or other community locations |
Enhanced Prenatal Care (with referrals for mental health services and brief case management) | Women in both the intervention and enhanced prenatal care group showed significant decreases in depressive symptoms (EDS) from baseline to 37–39 weeks gestation. 58% of women assigned to brief-IPT and 67% of the women in enhanced prenatal care reported clinically significant improvement in depressive symptoms. There were no differences in improvement between groups. Additionally, women in both the intervention and enhanced prenatal care groups did not show significant reductions in anxiety symptoms (STAI-Brief). | Not reported |
| McKee et al., 2006 | a) individual b) multicomponent psychosocial intervention (CBT/psychoeducation/social support building) c) Total possible of 8 CBT sessions, 3 psychoeducation sessions and 14 social support sessions (M=5) d) therapists (education not reported) e) home or health centers |
prenatal TAU | Women in both the intervention and control group showed significant reductions in depressive symptoms (BDI-II) from third trimester to three months postpartum. There was no significant difference depressive symptom reduction for women in the control compared with the intervention group. | Not reported |
| Muñoz et al., 2007 | a) group, 4 individual postpartum b) mood management course (CBT, attachment, psychoeducation, relaxation) c) 12 sessions, 4 booster, (M=6.7) d) group facilitators (faculty, postdoctoral fellows, and advanced doctoral graduate students in clinical psychology) e) medical (prenatal care) setting |
prenatal TAU | Women in the intervention and controls groups showed no significant differences in major depressive episode incidence (Maternal Mood Screener) from pre to post intervention. | Yes: reinforced values (e.g., collectivism, familism), fostered new outlets of support in a foreign context, validated cultural values and beliefs regarding pregnancy and motherhood, validated the role of religion and spirituality healing, discussions of discrimination and racism. |
| Zhang & Emory, 2015 | a) group b) mindfulness (components of mindfulness, ACT, DBT) c) 8 sessions over 4 weeks, (M=1.6) d) advanced PhD student in clinical psychology e) not reported |
prenatal TAU | Women receiving the intervention did not show significant reductions in depressive symptoms (BDI-II) from pre to immediate post intervention. 4 weeks post intervention, participating in more intervention sessions was associated with fewer depressive symptoms. | Not reported |
| Non-Randomized Trials | ||||
| Jesse et al., 2010 | a) individual OR group b) CBT c) 6 2-hour sessions, (M=6) d) Principal Investigator (PI), a nurse-midwife, and facilitators with master’s training in mental health and rehabilitation e) not reported |
Not applicable | Women who received intervention showed a 65% rate of “recovery” in the sixth intervention week and an 81% rate of “recovery” at one-month post-intervention (13/16 EPDS < 10). Women had significantly lower depressive symptoms post-treatment, and maintained their improvement over time | Yes: Use of colorful and attractive graphics, real-world examples. Culturally relevant guided visualization and inspirational literature/affirmations |
|
Jesse et al.,
2015 |
a) group b) CBT c) 6 weeks 2-hour session, (M=6) d) master’s and doctoral trained mental health professionals, resource mom (co-facilitated the group, offered weekly booster session telephone calls and provided case management services) e) prenatal clinic |
TAU | African-American women at high-risk for depression in the intervention group showed significantly greater decreases in their mean depressive symptom scores at post-intervention and follow-up compared to TAU. African American women at low-moderate risk for depression in the intervention showed mean reductions in depressive symptom scores at post-intervention and follow-up equivalent to those in to TAU. | Yes: First chapter of manual addressed depression in women of color, translated into Spanish for Spanish speaking participants. Inclusion of non-denominational spiritual related resources, use of personal check-ins, and emphasis on confidentiality |
| Sampson, et al., 2016 | a) individual b) CBT (problem solving therapy + 1 session motivational interviewing) c) 5 sessions, 1–2 hours d) community caseworkers, 1 with an associate’s degree and 1 who was a licensed professional counselor e) home based |
Not applicable | Women receiving the intervention showed significant reduction in depressive symptoms pre to post intervention (EPDS and PHQ-9). | No |
Note. CBT= Cognitive Behavioral Therapy, IPT= Interpersonal Therapy, TAU =Treatment as Usual, RCT= Randomized Control Trail, EPDS= Edinburgh Postnatal Depression Scale, CES-D= Center for Epidemiologic Studies Depression Scale, STAI= State-Trait Anxiety Inventory, BDI-II= Beck Depression Inventory, II, EDS= Edinburgh Depression Scale, PHQ-9= Patient Health Questionnaire-9 item.
Randomized Controlled Trials
Depression.
Of the 10 RCTs, two studies reported statistically significant reductions in depressive symptoms when compared to a control group receiving prenatal care as usual. The first study used a CBT group intervention lead by master’s level therapists (El-Mohades et al., 2008); and the second study used a combined (i.e., group and individual sessions) behavioral activation intervention delivered by community health workers (Kieffer et al., 2013). One study using IPT lead by master’s and doctoral level therapists outperformed enhanced usual prenatal care (Grote et al., 2009). Four studies found that the tested intervention reduced depressive symptoms from baseline to post-treatment, however, these interventions did not outperform prenatal care as usual (Le et al., 2011; McKee et al., 2006; Field et al., 2013; Lenze & Potts, 2017). Three studies found no effect of the intervention on depressive symptoms (Crocket et al., 2008; Muñoz et al., 2007; Zhang et al., 2015). While randomized trials demonstrated that CBT and IPT approaches were effective, it is notable that there were more CBT and IPT interventions that did not outperform standard care than those that did.
Of the three efficacious interventions, only two examined long term benefits. Grote and colleagues (2009) reported significant reductions in depressive symptoms that were maintained from immediate post-intervention to six-months postpartum. However, Kieffer et al. (2013) reported that the intervention effect did not extend into the early postpartum period (6 weeks postpartum), and thus was only significant immediately post-treatment (in late pregnancy).
Anxiety.
Of the 10 RCTs, only two measured anxiety symptoms as an outcome. Of those, one study showed a significant reduction in anxiety symptoms from pre- to post-treatment (Field et al., 2013); however this was not different from the active control condition.
Non-Randomized Trials.
Depression.
Of the three non-randomized trials included in this review, two studies reported statistically significant reductions in depressive symptoms from pre- to post-treatment. Both studies tested a CBT intervention, though the method of delivery differed by study. The first was led by mental health and perinatal professionals (e.g., marriage and family therapists, licensed clinical social workers, midwife) (Jesse et al., 2010), while the second study was led by community caseworkers (Sampson et al., 2016). Jesse and colleagues (2015) found significant reductions in depressive symptoms in Black women, only when they were considered high-risk for depression (as opposed to low or moderate risk), demonstrating a moderating effect of depressive symptom severity. Jesse and colleagues (2010; 2015) reported significant reductions in depressive symptoms that continued from immediate post-intervention to six-month post-treatment. Importantly, the lack of randomization in the aforementioned studies limits our ability to confidently attribute symptom change to the intervention.
Anxiety.
There were no non-randomized trials that examined anxiety as an outcome.
Attrition and Attendance
Attrition ranged from 8% to 45% but was low overall (mean attrition=17%). Most studies kept attrition rates below 10% (Crockett et al., 2008; Field et al., 2008; Jesse et al., 2010; Le et al., 2011; Lenze & Potts, 2017; Muñoz et al., 2007 & Sampson et al., 2016), and only two studies had attrition rates larger than 30% (McKee et al., 2006; Zhang & Emory, 2015). Intervention duration ranged from four to 14 sessions, with a modal intervention length of eight sessions. Across studies, pregnant women attended about 6 sessions on average (M=6.21). For additional information about average session length by study (when reported), see Table 1.
Cultural Adaptations
Only a minority of studies (five of 13) included cultural adaptations to their treatment protocols (Grote et al., 2009; Jesse et al., 2010; Jesse et al., 2015; Le et al., 2011; Muñoz et al. 2007). Those interventions that did include adaptations were CBT protocols, and used focus groups with stakeholders (both clients and providers) to inform the adaptation process. As an example, in a sample of Latinas of primarily Mexican origin, Muñoz and colleagues (2007) attempted to improve cultural fit of the intervention by reinforcing values such as collectivism and familism, fostering new outlets of support in a foreign context, validating cultural values regarding pregnancy, motherhood, religion and spirituality, and providing women with an opportunity to discuss their frustrations with discrimination and racism. In another study, Le and colleagues (2011) incorporated parenting issues of particular salience to Central American families (e.g. immigration stressors), and linguistic changes relevant for the population. Finally, in a sample of rural Black women, adaptations included adjustments to the reading level of intervention materials, adding colorful and attractive graphics, assigning brief homework assignments using real-world examples, and using guided visualization and inspirational literature and affirmations (Jesse et al., 2010; 2015). The RCTs that used cultural adaptations (Grote et al., 2009; Le et al., 2011 Muñoz et al., 2007) were not more likely to be effective than the RCTs without adaptations; of the three RCTs that outperformed a control condition and significantly reduced depressive symptoms, only one had been culturally adapted (Grote et al., 2009).
Data Quality
Included studies were of mixed methodological bias. Though most studies used random sequence generation (n=8) to avoid selection bias, fewer studies described allocation concealment in detail (n=4). Further, most studies did not blind study personnel to intervention condition. Finally, it was not possible for the authors to assess selective reporting with certainty, as only five studies had pre-registered their trials, and thus had pre-defined variables of interest. For a summary of bias estimates by study see Table A.1 in the appendix1.
Discussion
This review is the first to assess the efficacy of interventions for anxiety and depression during pregnancy among the two largest minority groups in the United States (U.S. Census, 2018). Overall, findings suggest that most treatment outcome studies with pregnant Latina and Black women are limited and often do not result in favorable outcomes for depression. Although CBT is the treatment modality most often tested for depression with pregnant ethno-racial minority women, methodological limitations and a preponderance of nonsignificant findings (i.e., lack of favorable support for interventions) preclude us from naming CBT an efficacious intervention in this group of women. Indeed, for Black and Latina women, only behavioral activation had unanimously favorable research support but this was based on just one randomized trial. All other modalities (i.e. IPT, mindfulness) had more limited support.
These findings are particularly concerning in the context of recent data from the U.S. Preventive Services Taskforce which reviewed data from 17 randomized controlled trials of pregnant women primarily identifying as White from the U.S. and Europe, and found that both CBT and IPT had a small yet favorable effect on perinatal depression symptoms (O’Connor et al., 2019). In another study, the pooled relative risk score for depression remission, usually defined as the “proportion below a specified cut point on a depression symptom scale” across 11,869 women receiving CBT and living in North America, Europe and Australia was calculated at 1.34 (O’Connor, Rossom, Henninger, Groom, & Burda, 2016), indicating a clear benefit of treatment. CBT also has been established as the intervention with the most evidence for treating prenatal anxiety in the U.S. and European population, inclusive primarily of non-Latina White women (Austin et al., 2008; Lilliecreutz, Josefsson, & Sydsjö, 2010; Thomas, Komiti, & Judd, 2014). In light of these findings, this review identifies an important treatment gap and suggests an urgent need to investigate why these interventions fall short when being used with pregnant women of color with internalizing distress.
Strikingly, in the current review with Black women and Latinas, only two interventions measured anxiety as an outcome and neither of these studies found that the intervention outperformed a control condition in reducing anxiety symptoms. Anxiety during pregnancy has garnered increased attention due to its associations with adverse birth outcomes (Dunkel Schetter & Tanner, 2012) and subsequent postpartum depression (Heron, O’Connor, Evans, Golding, & Glover, 2004). Yet, detection and management of clinically significant anxiety is restricted due to a lack of valid screeners during pregnancy (Misri, Abizadeh, Sanders & Swift, 2015) and physicians’ uncertainty about appropriate treatment (Leddy, Lawrence, & Schulkin, 2011), which is understandable given the state of the evidence. This is of particular concern for Latinas and Black women who not only experience higher rates of anxiety during pregnancy than their non-Latina White counterparts (Collins & David, 2005), but also have access to poorer quality obstetric and gynecologic care (McKenney, Martinez, & Yee, 2018). Interestingly, mind-body therapies (e.g. yoga, tai-chi), which were not part of this review, have received more attention as treatments for anxiety than psychological interventions and show favorable effects on symptomatology in pregnancy (Davis, Goodman, Leiferman, Taylor, & Dimidjian, 2015; Field, Diego, Delgado, & Medina, 2013b; Satyapriya, Nagarathna, Padmalatha, & Nagendra, 2013), including among primarily Black women (Jallo, Ruiz, Elswick, & French, 2014). However, systematic reviews of mind-body interventions and other complementary and alternative therapies have cautioned against drawing conclusions about these therapies given concerns about adequate power, randomization, and the measurement of anxiety (Beddoe & Lee, 2008; Hall, Beattie, Lau, East, & Anne Biro, 2016; Marc et al., 2011). Thus, well designed studies examining psychological and mind-body interventions (i.e., non-pharmacological interventions) to reduce prenatal anxiety are critically needed.
It is possible that the lack of significant findings supporting psychological interventions for Black women and Latinas with anxiety and depressive symptoms relates to the level of clinical risk of participants included in the intervention trials. In general, effects of preventive interventions for depression tend to be modified by risk level, such that stronger effects are seen for participants with higher baseline symptomology (Barrera, Torres, & Muñoz, 2007). Consistent with this pattern, Jesse and colleagues (2015) reported greater improvement for pregnant Black women with higher baseline depressive symptoms, and other authors have suggested that better treatment effects would have emerged with more severely depressed women (Le et al., 2011; McKee et al., 2008). Interestingly, findings are mixed regarding severity as a moderator of depression treatment outcome in samples of primarily non-Latina White women. While some researchers report that women with higher baseline depressive symptoms improve less (Sockol et al., 2011), others report that women “at risk” for depression show greater symptom improvement post-treatment (Bittner et al., 2014; Dennis & Hodnett, 2007). There is a need to test psychological interventions with clinically depressed women to better elucidate whether available intervention modalities are unable to resolve depression for pregnant ethno-racial minorities, or whether effects are simply difficult to detect in a prevention context.
Despite findings suggesting that cultural adaptations can improve clinical outcomes in ethnic minority adults with depression and anxiety (van Loon, van Schaik, Dekker, & Beekman, 2013), it is of interest that only five (of 13) of the interventions included in this review incorporated such adaptations. Adaptations varied from surface-level modifications of intervention materials (e.g., language, photos), to reinforcement of traditional values, or incorporation of culturally-salient topics (e.g., coping with discrimination). In our review, two of the five effective interventions used cultural adaptations to improve fit for the respective racial and ethnic minority women. Importantly, RCTs with cultural adaptations reported less attrition on average compared to RCT’s without adaptations (10% vs. 19.9%). Future studies should strive to better understand the importance of cultural modifications to improve engagement and clinical outcomes with pregnant women receiving treatment for anxiety and depression.
Findings from this systematic review should be considered in light of several limitations. First, the selection criteria, which required a minimum of 75% ethnic minority participants, limited the number of studies eligible for our systematic review. This decision was based on previous studies which have argued that a 3:1 ratio of ethnic minority participants to White participants provides strongest evidence of treatment effectiveness for the participating minority groups (Huey & Polo, 2008). A less conservative inclusion criteria of 50%, would have added an additional six RCTs—four IPT (Spinelli & Endicott, 2003; Spinelli et al., 2013; Zlotnick, Miller, Pearlstein, Howard, & Sweeney, 2006; Zlotnick, Tzilos, Miller, Seifer, & Stout, 2016), one CBT (O’Mahen, Himle, Fedock, Henshaw, & Flynn, 2013) and one family systems therapy (Heinicke et al., 1999) —of which one CBT (O’Mahen et al., 2013) and two IPT interventions significantly reduced depressive symptoms and outperformed control conditions (Spinelli & Endicott, 2003; Zlotnick, Tzilos, Miller, Seifer, & Stout, 2016). Had these studies been included our conclusions would have remained largely the same—that there are few efficacious trials that include Latinas and Black women, and that though CBT and IPT are the intervention modalities that have garnered most support, neither have sufficient support to be considered well-established or in other words, “gold standard” treatments for pregnant ethnic minority women.
This review was restricted to studies conducted in the United States in order to more confidently make comparisons across studies and are not generalizable to ethno-racial minority women living in other countries. Ethnic/racial minority status is differentially associated with depressive symptoms across countries, in part because of the variance in risk factors such as ethnic discrimination encountered in these countries (Missinne & Bracke, 2012). Further, given that heterogeneity in prenatal health systems across countries would change the level of care afforded to women randomized to the prenatal care ‘as-usual’ control conditions, our focus on one national context, though regionally diverse, allows us to draw conclusions and make suggestions under a more homogenous social and structural backdrop.
Finally, our results regarding the evidence base for interventions in the prenatal period for Latinas and Black women are confounded by socioeconomic status. Because all women enrolled in included studies were considered to be low income, we were not able to test the relative impact of race/ethnicity versus socioeconomic status on intervention response. It is notable that by including studies of low-income pregnant women with a greater proportion of White women (i.e., 26–50%), the number of effective RCTs would have doubled (i.e. from three to six), suggesting that interventions tested with greater numbers of White women showed better treatment response. Greater representation of Latinas and Black women from diverse SES backgrounds in clinical trials is necessary to elucidate the role of SES as a potential moderator of treatment outcomes. Until recently, few NIMH funded trials of psychological interventions have included meaningful numbers of ethnic-minorities (Mak, Law, Alvidrez, & Pérez-Stable, 2007). As a result, the field is at a disadvantage when it comes to creating an evidence base for ethno-racial minority women during an already understudied time in the life course—pregnancy (Mendle, Eisenlohr-Moul, & Kiesner, 2016).
Depression and anxiety often persist from pregnancy to the postpartum period when left untreated (Heron, O’Connor, Evans, Golding, & Glover, 2004). Treating anxiety and depression during pregnancy is optimal as it can reduce adverse intergenerational outcomes via multiple pathways including improving parenting behaviors (Feldman et al., 2009) and reducing physiological stress responses in mothers and their infants (Urizar & Muñoz, 2011). This review finds that for pregnant Latinas and Black women, CBT, behavioral activation and IPT are promising interventions for depression though they require additional research support. Addressing this gap in the field may help to improve physical and psychological health outcomes for ethno-racial minority pregnant women who are known to experience significant mental health disparities.
Appendix
Figure A.1.
Review Search Syntax
Table A.1.
Assessment of Study Bias
| Random sequence generation (selection bias) | Allocation concealment (selection bias) | Blinding of participants and personnel (performance bias) | Blinding of outcome assessment (detection bias) | Incomplete outcome data (attrition bias) | Selective reporting (reporting bias) | Other (Baseline Imbalance) | Overall Bias | |
|---|---|---|---|---|---|---|---|---|
| Crocket et al., 2008 | ⴲ | ⵁ | ⭙ | ⭙ | ⴲ | ⵁ | ⴲ | Medium |
| El-Mohandes et al., 2008 | ⴲ | ⴲ | ⭙ | ⴲ | ⵁ | ⴲ | ⴲ | Low |
| Field et al., 2013 | ⴲ | ⵁ | ⴲ | ⴲ | ⴲ | ⵁ | ⭙ | Low |
| Grote et al., 2009 | ⭙ | ⭙ | ⭙ | ⭙ | ⵁ | ⵁ | ⵁ | High |
| Jesse et al., 2010 | ⭙ | ⭙ | ⭙ | ⵁ | ⵁ | ⴲ | ⴲ | Medium |
| Jesse et al., 2015 | ⴲ | ⵁ | ⭙ | ⭙ | ⭙ | ⴲ | ⴲ | Medium |
| Keiffer et al., 2013 | ⴲ | ⴲ | ⭙ | ⴲ | ⴲ | ⵁ | ⴲ | Low |
| Le et al., 2011 | ⴲ | ⴲ | ⴲ | ⭙ | ⵁ | ⵁ | ⴲ | Low |
| Lenze & Potts, 2017 | ⴲ | ⴲ | ⴲ | ⵁ | ⴲ | ⴲ | ⴲ | Low |
| McKee et al., 2006 | ⴲ | ⵁ | ⵁ | ⴲ | ⭙ | ⵁ | ⵁ | Medium |
| Muñoz et al., 2007 | ⴲ | ⴲ | ⭙ | ⵁ | ⴲ | ⵁ | ⴲ | Low |
| Sampson et al, 2016 | ⭙ | ⭙ | ⭙ | ⵁ | ⴲ | ⴲ | ⴲ | Medium |
| Zhang & Emory, 2015 | ⴲ | ⵁ | ⭙ | ⵁ | ⭙ | ⵁ | ⭙ | High |
Note. ⊕ indicates low risk of bias, ⊘ indicates unclear risk of bias, and ⊗ indicates high risk of bias.
Footnotes
Support for bias judgments will be provided upon request.
References
- Austin M-P, Frilingos M, Lumley J, Hadzi-Pavlovic D, Roncolato W, Acland S, … Parker G (2008). Brief antenatal cognitive behaviour therapy group intervention for the prevention of postnatal depression and anxiety: A randomised controlled trial. Journal of Affective Disorders, 105(1–3), 35–44. 10.1016/j.jad.2007.04.001 [DOI] [PubMed] [Google Scholar]
- Barrera AZ, Torres LD, & Muñoz RF (2007). Prevention of depression: The state of the science at the beginning of the 21st Century. International Review of Psychiatry, 19(6), 655–670. 10.1080/09540260701797894 [DOI] [PubMed] [Google Scholar]
- Beddoe AE, & Lee KA (2008). Mind-body interventions during pregnancy. JOGNN, 37, 165–175. 10.1111/j.1552-6909.2008.00218. [DOI] [PubMed] [Google Scholar]
- Bittner A, Peukert J, Zimmermann C, Junge-Hoffmeister J, Parker LS, Stöbel-Richter Y, & Weidner K (2014). Early Intervention in Pregnant Women With Elevated Anxiety and Depressive Symptoms. The Journal of Perinatal & Neonatal Nursing, 28(3), 185–195. 10.1097/JPN.0000000000000027 [DOI] [PubMed] [Google Scholar]
- Bledsoe SE, & Grote NK (2006). Treating depression during pregnancy and the postpartum: A preliminary meta-analysis. 10.1177/1049731505282202 [DOI]
- Chambless DL, & Ollendick TH (2001). Empirically supported psychological interventions: Controversies and evidence. Annual Review of Psychology, 52(1), 685–716. 10.1146/annurev.psych.52.1.685 [DOI] [PubMed] [Google Scholar]
- Coelho HF, Murray L, Royal-Lawson M, & Cooper PJ (2011). Antenatal anxiety disorder as a predictor of postnatal depression: A longitudinal study. Journal of Affective Disorders, 129(1–3), 348–353. 10.1016/J.JAD.2010.08.002 [DOI] [PubMed] [Google Scholar]
- Collins JW, & David RJ (2005). Pregnancy Outcome of Mexican-American Women: The Effect of Generational Residence in the United States. Obstetrical & Gynecological Survey, 60(3), 147–148. 10.1097/01.ogx.0000154429.92315.3c [DOI] [PubMed] [Google Scholar]
- Copeland A, Gallo L, & Alolabi N (2019). The surgeon’s guide to systematic review and meta-analysis In Evidence-Based Surgery (pp. 145–157). Cham: Springer International Publishing; 10.1007/978-3-030-05120-4_15 [DOI] [Google Scholar]
- Cox JL, Holden JM, & Sagovsky R (1987). Edinburgh Postnatal Depression Scale (EPDS). British Journal of Psychiatry. [DOI] [PubMed]
- Crockett K, Zlotnick C, Davis M, Payne N, & Washington R (2008). A depression preventive intervention for rural low-income African-American pregnant women at risk for postpartum depression. Archives of Women’s Mental Health, 11(5–6), 319–325. [DOI] [PubMed] [Google Scholar]
- Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, … Wong JB (2019). Interventions to prevent perinatal depression. JAMA, 321(6), 580 10.1001/jama.2019.0007 [DOI] [PubMed] [Google Scholar]
- Davis K, Goodman SH, Leiferman J, Taylor M, & Dimidjian S (2015). A randomized controlled trial of yoga for pregnant women with symptoms of depression and anxiety. Complementary Therapies in Clinical Practice, 21(3), 166–172. 10.1016/J.CTCP.2015.06.005 [DOI] [PubMed] [Google Scholar]
- Dennis CL, & Hodnett ED (2007). Psychosocial and psychological interventions for treating postpartum depression. Cochrane Database of Systematic Reviews, (4), CD006116 10.1002/14651858.CD006116.pub2 [DOI] [PubMed] [Google Scholar]
- Dennis CL, & Hodnett ED (2009). Psychosocial and psychological interventions for treating postpartum depression (Review). 10.1002/14651858.CD006116.pub2 [DOI] [PubMed]
- Ding XX, Wu Y. Le, Xu SJ, Zhu RP, Jia XM, Zhang SF, … Tao FB (2014). Maternal anxiety during pregnancy and adverse birth outcomes: A systematic review and meta-analysis of prospective cohort studies. Journal of Affective Disorders. 10.1016/j.jad.2014.02.027 [DOI] [PubMed]
- Dunkel Schetter C, & Tanner L (2012). Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Current Opinion in Psychiatry. 10.1097/YCO.0b013e3283503680 [DOI] [PMC free article] [PubMed]
- Edge D, Baker D, & Rogers A (2004). Perinatal depression among black Caribbean women. Health & Social Care in the Community, 12(5), 430–438. 10.1111/j.1365-2524.2004.00513.x [DOI] [PubMed] [Google Scholar]
- El-Mohandes AA, Kiely M, Joseph JG, Subramanian S, Johnson AA, Blake SM, … & El-Khorazaty MN (2008). An intervention to improve postpartum outcomes in African-American mothers: a randomized controlled trial. Obstetrics and gynecology, 112(3), 611–620. 10.1097/AOG.0b013e3181834b10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman R, Granat A, Pariente C, Kanety H, Kuint J, & Gilboa-Schechtman E (2009). Maternal Depression and Anxiety Across the Postpartum Year and Infant Social Engagement, Fear Regulation, and Stress Reactivity. Journal of the American Academy of Child & Adolescent Psychiatry, 48(9), 919–927. 10.1097/CHI.0b013e3181b21651 [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Delgado J, & Medina L (2013a). Peer support and interpersonal psychotherapy groups experienced decreased prenatal depression, anxiety and cortisol. Early Human Development, 89(9), 621–624. 10.1016/j.earlhumdev.2013.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Diego M, Delgado J, & Medina L (2013b). Tai chi/yoga reduces prenatal depression, anxiety and sleep disturbances. Complementary Therapies in Clinical Practice, 19(1), 6–10. 10.1016/j.ctcp.2012.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung K, & Dennis CL (2010). Postpartum depression among immigrant women. Current Opinion in Psychiatry, 23(4), 342–348. 10.1097/YCO.0b013e32833ad721 [DOI] [PubMed] [Google Scholar]
- Goodman JH (2009). Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth, 36(1), 60–69. 10.1111/j.1523-536X.2008.00296. [DOI] [PubMed] [Google Scholar]
- Goodman JH, Guarino A, Chenausky K, Klein L, Prager J, Petersen R, … Freeman M (2014). CALM Pregnancy: Results of a pilot study of mindfulness-based cognitive therapy for perinatal anxiety. Archives of Women’s Mental Health, 17(5), 373–387. 10.1007/s00737-013-0402-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman JH, & Tyer-Viola L (2010). Detection, treatment, and referral of perinatal depression and anxiety by obstetricalpProviders. Journal of Women’s Health, 19(3), 477–490. 10.1089/jwh.2008.1352 [DOI] [PubMed] [Google Scholar]
- Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, & Katon WJ (2010). A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Archives of General Psychiatry, 67(10), 1012 10.1001/archgenpsychiatry.2010.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote NK, Swartz HA, Geibel SL, Zuckoff A, Houck PR, & Frank E (2009). A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiatric Services, 60(3), 313–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote NK, Zuckoff A, Swartz H, Bledsoe SE, & Geibel S (2007). Engaging women who are depressed and economically disadvantaged in mental health treatment. Retrieved from https://academic.oup.com/sw/article-abstract/52/4/295/1911779 [DOI] [PMC free article] [PubMed]
- Hall HG, Beattie J, Lau R, East C, & Anne Biro M (2016). Mindfulness and perinatal mental health: A systematic review. Women and Birth, 29(1), 62–71. 10.1016/J.WOMBI.2015.08.006 [DOI] [PubMed] [Google Scholar]
- Heinicke CM, Fineman NR, Ruth G, Recchia SL, Guthrie D, & Rodning C (1999). Relationship-based intervention with at-risk mothers: Outcome in the first year of life. Infant Mental Health Journal, 20(4), 349–374. [DOI] [Google Scholar]
- Heron J, O’Connor TG, Evans J, Golding J, & Glover V (2004). The course of anxiety and depression through pregnancy and the postpartum in a community sample. Journal of Affective Disorders, 80(1), 65–73. 10.1016/j.jad.2003.08.004 [DOI] [PubMed] [Google Scholar]
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, … & Sterne JA (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj, 343, d5928 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huey SJ, & Polo AJ (2008). Evidence-based psychosocial treatments for ethnic minority youth. Journal of Clinical Child and Adolescent Psychology. 10.1080/15374410701820174 [DOI] [PMC free article] [PubMed]
- Jallo N, Ruiz RJ, Elswick RK, & French E (2014). Guided imagery for stress and symptom management in pregnant african american women. Evidence-Based Complementary and Alternative Medicine : ECAM, 2014, 840923 10.1155/2014/840923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jesse DE, Blanchard A, Bunch S, Dolbier C, Hodgson J, & Swanson MS (2010). A pilot study to reduce risk for antepartum depression among women in a public health prenatal clinic. Issues in Mental Health Nursing, 31(5), 355–364. [DOI] [PubMed] [Google Scholar]
- Jesse DE, Gaynes BN, Feldhousen EB, Newton ER, Bunch S, & Hollon SD (2015). Performance of a culturally tailored cognitive-behavioral intervention integrated in a public health setting to reduce risk of antepartum depression: A randomized controlled trial. Journal of Midwifery & Women’s Health, 60(5), 578–592. 10.1111/jmwh.12308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kieffer EC, Caldwell CH, Welmerink DB, Welch KB, Sinco BR, & Guzmán JR (2013). Effect of the healthy MOMs lifestyle intervention on reducing depressive symptoms among pregnant Latinas. American journal of community psychology, 51(1–2), 76–89. 10.1007/s10464-012-9523-9 [DOI] [PubMed] [Google Scholar]
- Ko JY, Farr SL, Dietz PM, & Robbins CL (2012). Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005–2009. Journal of Womens Health., 21(8), 830–836. 10.1089/jwh.2011.3466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozhimannil KB, Trinacty CM, Busch AB, Huskamp HA, & Adams AS (2011). Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatric Services, 62(6), 619–625. 10.1176/ps.62.6.pss6206_0619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le HN, Perry DF, & Stuart EA (2011). Randomized controlled trial of a preventive intervention for perinatal depression in high-risk Latinas. Journal of Consulting and Clinical Psychology, 79(2), 135–141. [DOI] [PubMed] [Google Scholar]
- Leddy MA, Lawrence H, & Schulkin J (2011). Obstetrician-gynecologists and womenʼs mental health: Findings of the collaborative ambulatory research network 2005–2009. Obstetrical & Gynecological Survey, 66(5), 316–323. 10.1097/OGX.0b013e31822785ee [DOI] [PubMed] [Google Scholar]
- Lenze SN, & Potts MA (2017). Brief interpersonal psychotherapy for depression during pregnancy in a low-income population: A randomized controlled trial. Journal of Affective Disorders. 10.1016/j.jad.2016.12.029 [DOI] [PMC free article] [PubMed]
- Levy LB, & O’Hara MW (2010). Psychotherapeutic interventions for depressed, low-income women: A review of the literature. Clinical Psychology Review, 30(8), 934–950. 10.1016/j.cpr.2010.06.006 [DOI] [PubMed] [Google Scholar]
- Lilliecreutz C, Josefsson A, & Sydsjö G (2010). An open trial with cognitive behavioral therapy for blood- and injection phobia in pregnant women—a group intervention program. Archives of Women’s Mental Health, 13(3), 259–265. 10.1007/s00737-009-0126- [DOI] [PubMed] [Google Scholar]
- Loughnan SA, Wallace M, Joubert AE, Haskelberg H, Andrews G, & Newby JM (2018). A systematic review of psychological treatments for clinical anxiety during the perinatal period. Archives of Women’s Mental Health, 21(5), 481–490. 10.1007/s00737-018-0812-7 [DOI] [PubMed] [Google Scholar]
- Lucero NB, Beckstrand RL, Callister LC, & Sanchez Birkhead AC (2012). Prevalence of postpartum depression among Hispanic immigrant women. Journal of the American Academy of Nurse Practitioners, 24(12), 726–734. 10.1111/j.1745-7599.2012.00744.x [DOI] [PubMed] [Google Scholar]
- Mahaffey BL, Lobel M (2018). Mental Health and Emotional Distress during Pregnancy in Revenson TA & Gurung RAR (Eds.),The New Handbook of Health Psychology. NY: Taylor & Francis/Routledge. [Google Scholar]
- Mak WWS, Law RW, Alvidrez J, & Pérez-Stable EJ (2007). Gender and ethnic diversity in NIMH-funded clinical trials: Review of a decade of published research. Administration and Policy in Mental Health and Mental Health Services Research, 34(6), 497–503. 10.1007/s10488-007-0133-z [DOI] [PubMed] [Google Scholar]
- Marc I, Toureche N, Ernst E, Ed, H., Blanchet C, Dodin S, & Mm, N. (2011). Mind-body interventions during pregnancy for preventing or treating women’s anxiety. Retrieved from http://www.thecochranelibrary.com [DOI] [PMC free article] [PubMed]
- McKee MD, Zayas LH, Fletcher J, Boyd RC, & Nam SH (2006). Results of an intervention to reduce perinatal depression among low-income minority women in community primary care. Journal of Social Service Research, 32(4), 63–81. 10.1300/J079v32n04_04 [DOI] [Google Scholar]
- McKenney KM, Martinez NG, & Yee LM (2018). Patient navigation across the spectrum of women’s health care in the United States. American Journal of Obstetrics and Gynecology, 218(3), 280–286. 10.1016/j.ajog.2017.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendle J, Eisenlohr-Moul T, & Kiesner J (2016). From menarche to menopause. Clinical Psychological Science, 4(5), 859–866. 10.1177/2167702616650424 [DOI] [Google Scholar]
- Misri S, Abizadeh J, Sanders S, & Swift E (2015). Perinatal generalized anxiety disorder: Assessment and treatment. Journal of Women’s Health, 24(9), 762–779. 10.1089/jwh.2014.5150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Missinne S, & Bracke P (2012). Depressive symptoms among immigrants and ethnic minorities: A population based study in 23 European countries. Social Psychiatry and Psychiatric Epidemiology, 47(1), 97–109. 10.1007/s00127-010-0321-0 [DOI] [PubMed] [Google Scholar]
- Muñoz RF, Le HN, Ippen CG, Diaz MA, Urizar GG, Soto J, … Lieberman AF (2007). Prevention of oostpartum depression in low-income women: Development of the mamás y bebés/mothers and babies course. Cognitive and Behavioral Practice. 10.1016/j.cbpra.2006.04.021 [DOI]
- Nillni YI, Mehralizade A, Mayer L, & Milanovic S (2018). Treatment of depression, anxiety, and trauma-related disorders during the perinatal period: A systematic review. Clinical Psychology Review, 66, 136–148. 10.1016/j.cpr.2018.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor E, Rossom RC, Henninger M, Groom HC, & Burda BU (2016). Primary care screening for and treatment of depression in pregnant and postpartumwomen evidence report and systematic review for the US preventive services task force. JAMA - Journal of the American Medical Association. 10.1001/jama.2015.18948 [DOI] [PubMed]
- O’Connor E, Senger CA, Henninger M, Gaynes BN, Coppola E, & Weyrich MS (2019). Interventions to Prevent Perinatal Depression: A Systematic Evidence Review for the U.S. Preventive Services Task Force. Interventions to Prevent Perinatal Depression: A Systematic Evidence Review for the U.S. Preventive Services Task Force. Agency for Healthcare Research and Quality (US). Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/30807060 [PubMed] [Google Scholar]
- O’Mahen H, Himle JA, Fedock G, Henshaw E, & Flynn H (2013). A pilot randomized controlled trial of cognitive behavioral therapy for perinatal depression adapted for women with low incomes. Depression and Anxiety, 30(7), 679–687. 10.1002/da.22050 [DOI] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, & Higgins JP (2018). Tools for assessing risk of reporting biases in studies and syntheses of studies: a systematic review. BMJ open, 8(3), e019703 10.1136/bmjopen-2017-019703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pina AA, Polo AJ, & Huey SJ (2019). Evidence-based psychosocial interventions for ethnic minority youth: The 10-year update. Journal of Clinical Child & Adolescent Psychology, 48(2), 179–202. 10.1080/15374416.2019.1567350 [DOI] [PubMed] [Google Scholar]
- Rich-Edwards JW, Kleinman K, Abrams A, Harlow BL, McLaughlin TJ, Joffe H, & Gillman MW (2006). Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. Journal of Epidemiology and Community Health. 10.1136/jech.2005.039370 [DOI] [PMC free article] [PubMed]
- Robertson E, Grace S, Wallington T, & Stewart DE (n.d.). Antenatal risk factors for postpartum depression: a synthesis of recent literature. Retrieved from https://yorkspace.library.yorku.ca/xmlui/bitstream/handle/10315/2553/Antenatal+risk+factors+for+postpartum+depression.pdf?sequence=1 [DOI] [PubMed]
- Rosenthal L, & Lobel M (2011). Explaining racial disparities in adverse birth outcomes: Unique sources of stress for Black American women. Social Science & Medicine, 72(6), 977–983. 10.1016/j.socscimed.2011.01.013 [DOI] [PubMed] [Google Scholar]
- Sampson M, Villarreal Y, & Rubin A (2016). A problem-solving therapy intervention for low-income, pregnant women at risk for postpartum depression. Research on Social Work Practice, 26(3), 236–242. 10.1177/1049731514551143 [DOI] [Google Scholar]
- Satyapriya M, Nagarathna R, Padmalatha V, & Nagendra HR (2013). Effect of integrated yoga on anxiety, depression & well being in normal pregnancy. Complementary Therapies in Clinical Practice, 19(4), 230–236. 10.1016/J.CTCP.2013.06.003 [DOI] [PubMed] [Google Scholar]
- Schofield Z, & Kapoor D (2019). Pre-existing mental health disorders and pregnancy. Obstetrics, Gynaecology & Reproductive Medicine, 29(3), 74–79. 10.1016/J.OGRM.2019.01.005 [DOI] [Google Scholar]
- Sockol LE, Epperson CN, & Barber JP (2011). A meta-analysis of treatments for perinatal depression. Clinical Psychology Review, 31(5), 839–849. 10.1016/j.cpr.2011.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinelli MG, & Endicott J (2003). Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. American Journal of Psychiatry, 160(3), 555–562. 10.1176/appi.ajp.160.3.555 [DOI] [PubMed] [Google Scholar]
- Spinelli MG, Endicott J, Leon AC, Goetz RR, Kalish RB, Brustman LE, … Schulick JL (2013). A controlled clinical treatment trial of interpersonal psychotherapy for depressed pregnant women at 3 New York City sites. The Journal of Clinical Psychiatry, 74(4), 393–399. 10.4088/JCP.12m07909 [DOI] [PubMed] [Google Scholar]
- Stewart DE (2012). Clinical Practice: Depression during pregnancy. Obstetric Anesthesia Digest 32(4), 208–209. 10.1097/01.aoa.0000422687.34124.5c [DOI] [Google Scholar]
- Thomas N, Komiti A, & Judd F (2014). Pilot early intervention antenatal group program for pregnant women with anxiety and depression. Archives of Women’s Mental Health, 17(6), 503–509. 10.1007/s00737-014-0447-2 [DOI] [PubMed] [Google Scholar]
- Urizar GG, & Muñoz RF (2011). Impact of a prenatal cognitive-behavioral stress management intervention on salivary cortisol levels in low-income mothers and their infants. Psychoneuroendocrinology, 36(10), 1480–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2018). Population Estimates: Race and Hispanic Origin. Washington, DC: U.S. Government Printing Office. [Google Scholar]
- van Loon A, van Schaik A, Dekker J, & Beekman A (2013). Bridging the gap for ethnic minority adult outpatients with depression and anxiety disorders by culturally adapted treatments. Journal of Affective Disorders, 147(1–3), 9–16. 10.1016/J.JAD.2012.12.014 [DOI] [PubMed] [Google Scholar]
- van Ravesteyn LM, Lambregtse - van den Berg MP, Hoogendijk WJG, & Kamperman AM (2017). Interventions to treat mental disorders during pregnancy: A systematic review and multiple treatment meta-analysis. PLOS ONE, 12(3), e0173397 10.1371/journal.pone.0173397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner E, Miller M, Osborne LM, Kuzava S, & Monk C (2015). Preventing postpartum depression: Review and recommendations. Archives of Women’s Mental Health, 18(1), 41–60. 10.1007/s00737-014-0475-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H, & Emory EK (2015). A mindfulness-based intervention for pregnant African-American women. Mindfulness, 6(3), 663–674. 10.1007/s12671-014-0304-4 [DOI] [Google Scholar]
- Zlotnick C, Miller IW, Pearlstein T, Howard M, & Sweeney P (2006). A preventive intervention for pregnant women on public assistance at risk for postpartum depression. American Journal of Psychiatry, 163(8), 1443–1445. 10.1176/ajp.2006.163.8.1443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlotnick C, Tzilos G, Miller I, Seifer R, & Stout R (2016). Randomized controlled trial to prevent postpartum depression in mothers on public assistance. Journal of Affective Disorders, 189, 263–268. 10.1016/j.jad.2015.09 [DOI] [PMC free article] [PubMed] [Google Scholar]