Abstract
The reason of the biological stability loss of mini-implants is still a matter of discussion between dentistry professionals. The main objective of this systematic literature review and meta-analysis was to analyze the risk factors that prejudice this loss. A search was made in the electronic databases Pubmed, Scopus, Embase and Cochrane, in addition a manual search was made too in Grey Literature (Opengrey). No limits were set on the year of publication or language. The inclusion criteria were: studies in humans treated with fixed appliances with mini-implants, where the risk factors for secondary stability were evaluated for a minimum of 8 weeks. After eliminating duplicate studies and assessing which ones achieve the inclusion criteria, a total of 26 studies were selected for the qualitative synthesis, 18 of them were included in the quantitative synthesis. Common risk variables were compared in all of them. Analyzing the forest and funnel plots, statistically significant differences were obtained only for location, the upper maxilla having lower risk than the mandible with an odds ratio of 0.56 and confidence interval of 0.39 to 0.80. Prospective studies under controlled conditions should be required in order to obtain a correct assessment of the variables analyzed.
Subject terms: Health care, Dental treatments, Dental treatment planning
Introduction
The use of mini-implants to provide anchorage for force application has simplified and improved the efficacy of many orthodontic treatments, reducing unwanted movements of other teeth, especially in adult patients. For this reason, anchorage in bone is becoming a much more widely used technique1.
Mini-implants are made of titanium or stainless steel, their structure has three different parts: the top one (supra-gingival, which allows the anchor), the medium area or neck, and the thread, which is inserted inside the bone and provides mechanic anchor. Moreover, the most common types of mini-implants are: Mini Implant System (dbOrthodontics), Vector Temporary Anchorage System (Omco) and the Abso Anchor System (Dentos). All of them are available in different lengths (6–12 mm) and diameters (1–2 mm)2.
Mini-implants or TADs (Temporary Anchorage Devices)2 have been used mainly as an auxiliary fixing method but more recently have been adopted for additional functions such as: mid-line or inclined plane alignment, space opening, or molar intrusion or extrusion3. The increasing use of mini-implants is justified by its multiple advantages, the simplicity of the surgical technique, and low cost. Moreover, it is well accepted by patients and achieves success rates of 80–90%4. While failure may be avoided by establishing the right therapeutic protocols, the fact that a percentage of mini-implants fail should not be overlooked.
Stability refers to the resistance to reactive forces, offered by teeth or other oral or extraoral structures, that would lead to unwanted movements5. In the case of mini-implants, two types of stability can be distinguished: primary and secondary. Primary stability is mechanical and is achieved by the mini-implant compressing the bone during insertion, while secondary, or biological stability, begins at the moment of placement and increases during the bone remodeling or healing process6.
The transition from primary to secondary stability takes at least 8 weeks. In this period of time, the failure of mini-implants can occur. A mini-implant failure is regarded as the appearance of mobility (eventual loss), inflammation or infection. Although biological stability is reached by orthodontic mini-implants when these are successful, osseointegration does not occur in this type of implants since they are temporary devices6.
Some controversy exists as to which risk factors affect mini-implant secondary stability7. The aim of this systematic literature review and meta-analysis was to analyze the variables affecting biological stability of mini-implants use for orthodontic anchorage.
The primary hypothesis of the present meta-analysis was that multiple factors can affect secondary or biological stability: patient-dependent (age, sex, hygiene), mini-implants-dependent (length and diameter) or technique-dependent (clinical experience, location, time, predrilling or not). The null hypothesis was that there are not any variables that significantly affect biological stability of mini-implants.
Materials and Methods
Review question
Meta-analysis was performed following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines8. The review protocol was registered in the PROSPERO database (reg. no. CRD42018083900). The review question of the present study was the following: in patients treated with fixed appliances (brackets) and mini-implants, what are the risk factors for secondary stability?
PICO(S) elements9 included in our review can be defined as follows: Patients treated with orthodontic fixed appliances (P) where mini-implants were placed as auxiliary devices (I) in different locations (anterior/posterior upper maxilla, anterior/posterior mandible), different ages and genders and different lengths and diameters of the mini-implants (C) and where the secondary stability of this temporary devices had been analyzed (O). Randomized clinical trials, longitudinal studies, cohort and case/control studies were eligible to be included (S).
Eligibility criteria
“Articles” and “Articles in press” were included: randomized clinical trials (RCT), longitudinal studies, cohort or case/control studies both retrospective and prospective. No restrictions were applied regarding the year of publication or language. Inclusion criteria were: human studies that evaluated risk factors for secondary stability of mini-implants used in orthodontic treatment for a period of at least 8 weeks.
Outcome
Secondary, or biological stability, begins at the moment of placement and increases during the bone remodeling or healing process. Biological stability is lost when mobility, severe inflammation or infection appear.
Information sources, search strategy, and study selection
To identify relevant articles, an electronic search was conducted in four databases: Pubmed, Embase, Scopus and Cochrane. A manual search was conducted in Opengrey literature. In some cases, the authors were contacted by e-mail to request additional information. The key search terms used to identify articles were: (Humans/human OR patients OR adults OR male OR female) AND (mini-screws OR micro-screws OR mini-implants OR temporary anchorage devices OR TAD* OR stability OR long-term stability OR skeletal-anchorage OR orthodontic treatment) AND (orthodontic failure-rates OR orthodontic success-rates). Two reviewers (MDC-R and CB-A), assessed the titles and abstracts of the articles identified in the electronic search; whenever disagreement occurred a third reviewer was consulted (JMM-C). If the abstract did not provide sufficient information to reach a decision to include it in analysis, the reviewers read the full text. Then, the full texts of the articles selected were read, and if they failed to meet inclusion criteria, the reasons for rejection were recorded. (Table 1).
Table 1.
Records excluded and reasons for exclusion.
| RECORDS EXCLUDED | ARTICLES EXCLUDED, WITH REASONS |
|---|---|
| Männchen et al., 2008 | No answer research question. |
| Ji et al., 2008 | No answer research question. |
| Tsoudis et al., 2008 | Study design not considered expedient (literary review). |
| Reynders et al., 2009 | Study design not considered expedient (literary review). |
| Antoszewska et al., 2009 | No answer research question. |
| Schätzle et al., 2009 | Study design not considered expedient (literary review). |
| Schätzle et al., 2010 | Study design not considered expedient (literary review). |
| Kim et al., 2010 | No answer research question. |
| Papadopoulus et al., 2011 | Study design not considered expedient (literary review). |
| Min et al., 2012 | No answer research question. |
| Consolaro et al., 2014 | Study design not considered expedient (literary review). |
| Kuroda et al., 2014 | Study design not considered expedient (literary review). |
| Rodriguez et al., 2014 | Study design not considered expedient (meta-analysis). |
| Dalesandri et al., 2014 | Study design not considered expedient (meta-analysis). |
| Romano et al., 2015 | Study design not considered expedient (literary review). |
| Uribe et al., 2015 | Study design not considered expedient (literary review). |
| Cornelis et al., 2015 | Study design not considered expedient (book chapter). |
| Papadopoulus et al., 2015 | Study design not considered expedient (book chapter). |
| Sarul et al., 2015 | Study design not considered expedient (literary review). |
| Lin et al., 2015 | Study design not considered expedient (literary review). |
| Liu et al., 2016 | Study design not considered expedient (literary review). |
| Kim et al., 2016 | Study design not considered expedient (literary review). |
| Leo et al., 2016 | Study design not considered expedient (literary review). |
| Hong et al., 2016 | Study design not considered expedient (literary review). |
| Yi et al., 2016 | Study design not considered expedient (literary review). |
| Afrashtehfer et al., 2016 | Study design not considered expedient (meta-analysis). |
| Yi et al., 2017 | Study design not considered expedient (meta-analysis). |
| Alharbi et al., 2018 | Study design not considered expedient (meta-analysis). |
| Mohammed et al., 2018 | Study design not considered expedient (meta-analysis). |
| Lyczek et al., 2019 | Study design not considered expedient (literary review). |
| Azeem et al., 2019 | Primary stability |
| Azeem et al., 2019 | Primary stability |
| Kakali et al., 2019 | Study design not considered expedient (literary review). |
| Ichsnoke et al., 2019 | No answer research question. |
Data items and collection
The review and meta-analysis was updated for the last time on January 4th 2020. The following variables were extracted from the works selected: author; year of publication; study type; sample size; demographic variables (patient age and sex); type of mini-implant (length and diameter); mini-implant location (maxillary or mandibular); position (left or right, vestibular, lingual/palatine, or crestal); and the number of mini-implants per patient. (Table 2)
Table 2.
Study data. Analyzed variables: study design, diameter, length, patient, age, total number of TADs, position, number of success TADs, definition of success and definition of failure.
| AUTHOR YEAR | STUDY DESIGN | DIAMETER (MM) | LENGTH (MM) | PATIENT (N) | AGE | N° of TAD | POSITION | N° of SUCCESS | DEFINITION OF SUCCESS | DEFINITION OF FAILURE |
|---|---|---|---|---|---|---|---|---|---|---|
| Miyawaki et al., 2003 | Retrospective | 1.0 /1.5/2.3 | 6 / 11/ 14 | 51 | 21.8+_ 7.8 | 134 |
Upper jaw. 63 Lower jaw. 61 |
103 | NA | Diameter 1 mm or less, inflammation periimplant tissue, high mandibular plane. |
| Chen et al., 2004 | Prospective | 2.0 | 5/7/9/11/13/15 | 44 | 29 _+ 8.9 | 140 |
Upper jaw. 105 Lower jaw. 35 |
125 | Absence of inflammation and clinical movement. | NA |
| Park et al., 2006 | Retrospective | 1.2/ 1.2/ 1.2/ 2 | 5/ 6,8,10/ 4,6,8,10/ 10,12,14,15 | 87 | 15.5 _+ 8.3 | 227 |
Upper jaw. 124 Lower jaw. 103 |
208 | Keep until the final of the treatment. Try to remove. | Lost during the treatment. |
| Chen et al., 2007 | Retrospective | 2/ 2/ 1.2 | 5–9/ 5–21/ 4–10 | 129 | 24.5 | 359 |
Upper jaw x. 263 Lower jaw. 96 |
306 | Enough stability during the treatment. | Lost during the treatment. |
| Wiechmann et al., 2007 | Prospective | 1.1 /1.6 | 5/ 6/ 7/ 8/ 10 | 49 | 26.9 _+ 8.9 | 133 |
Upper jaw. 88 Lower jaw. 45 |
102 | Absence of inflammation and clinical movement. | NA |
| Kuroda et al., 2007 | Retrospective | 1.3/ 2.0/ 2.3 | 6 /7/ 8/ 10/ 11/ 12 | 75 | 21.8 _+ 8.2 | 79 |
Upper jaw. 156 Lower jaw. 60 |
70 | Steady during one year. | NA |
| Chen et al., 2008 | Retrospective | 2.0 | 5–9/ 8–14 | 194 | 25.1 | 489 |
Upper jaw. 399 Lower jaw. 90 |
445 | NA | Lost during the treatment. |
| Moon et al., 2008 | Retrospective | 1.6 | 8 | 209 | 20.3 | 480 |
Upper jaw. 279 Lower jaw 0.201 |
402 | Absence of mobility after 8 month. | NA |
| Wu et al., 2009 | Retrospective | 1.1–1.5/ 1.7/ 2.0 | 7/ 8/ 10/ 11/ 12/ 13/ 14/ 15 | 166 | 26.5_+ 8.9 | 414 |
Upper jaw. 268 Lower jaw. 135 |
372 | NA | Lost after 8 month, or fractured after the insertion. |
| Viwattanatipa et al., 2009 | Prospective | 1.2 | 8/ 10/ 12 | 49 | 23.2 | 97 |
Upper jaw. 97 Lower jaw. 0 |
65 | NA | Mobility, displacement or infection. |
| Motoyoshi et al., 2009 | Retrospective | 1.6 | 8 | 52 | 26.1_+ 8.4 | 109 |
Upper jaw. 42 Lower jaw. 67 |
103 | No mobility, no lost during the treatment. | NA |
| Lee et al., 2010 | Prospective | 1.8 | 8.5 | 141 | 27 | 260 |
Upper jaw. 260 Lower jaw. 0 |
238 | NA | NA |
| Moon et al., 2010 | Retrospective | 1.6 | 8 | 306 |
14.45_+ 2.64 23.73_+ 2.70 37.04_+ 7.26 |
778 | NA | 614 | Steady during one year. | NA |
| Manni et al., 2010 | Retrospective | 1.5/ 1.3 | 9/ 11 | 132 | 25.9 | 300 |
Upper jaw. 427 Lower jaw. 351 |
243 | Absence of inflammation or loss. | Inflammation and instability. |
| Takaki et al., 2010 | Retrospective | NA | NA | 455 | 25.7 _+ 9.8 | 904 |
Upper jaw. 265 Lower jaw. 639 |
842 | NA | Mobility or loss of the implant. |
| Sharma et al., 2011 | Retrospective | 1.3 | 8 | 73 | 22.45 | 139 |
Upper jaw. 97 Lower jaw. 42 |
122 | Absence of inflammation and clinical movement. Keep until the final of the treatment | Spontaneous loss, severe mobility, replacement, infection, pain, pathology of soft tissue. |
| Topouzelis et al., 2012 | Retrospective | 1.2/ 1.4 | 8/ 10 | 34 | 27.2_+ 7.3 | 82 |
Upper jaw. 62 Lower jaw. 20 |
74 | Absence of inflammation, pain or mobility. | Infección or mobility. Instability with orthodontics forces. |
| Kim et al., 2012 | Retrospective | 1.6 | 6/ 8 | 286 | 10–30 | 429 |
Upper jaw. 357 Lower jaw. 72 |
332 | NA | Mobility or loss after 6 months. |
| Dobranski et al., 2014 | Prospective | 1.6/ 1.8 | 6/8/10 | 166 | 25.8 | 293 |
Upper jaw. 259 Lower jaw. 34 |
256 | NA | Loss of stability. |
| Yao et al. 2015 | Retrospective | NA | NA | 220 | 29.3 | 727 |
Upper jaw. 412 Lower jaw.231 |
643 | NA | Mobility or loss during the treatment. |
| Melo et al., 2016 | Retrospective | 1.3/ 1.4/ 1.6 | 5/ 7/ 9/ 11 | 570 | 42.7 | 1356 |
Upper jaw. 816 Lower jaw. 539 |
1208 | NA | Clinical mobility or o fracture during the insertion. |
| Jing et al., 2016 | Retrospective | 1.4/ 2.0 | 6/ 8/ 10 | 114 | 19.26_+ 9.19 | 253 |
Upper jaw. 170 Lower jaw. 83 |
224 | Keep until the success. | NA |
| Lee et al., 2016 | Retrospective | 1.2/ 1.3 | 8 | 71 | 19.2_+ 6.63 | 127 | NA | 108 | Keep the insertion in the bone with success during one year. | NA |
| Tsai et al., 2016 | Prospective | 1.5/2 | 8/9/10/11/12 | 139 | 25,7 + − 7,5 | 254 |
Upper jaw. 213 Lower jaw. 41 |
218 | NA | NA |
| Aly et al. 2018 | Prospective | 1.5/1.6/1.8 | 6/8710 | 82 | 21.41 | 180 |
Upper jaw. 52 Lower jaw. 128 |
148 | Being functionally stable until the end of the treatment with no signs of inflammation or any pathological condition around the TAD site, and anchorage function sustained until the end of the purpose | Sudden spontaneous loss or the presence of mobility or looseness during routine visits that required replacing the TAD used, or infected painful pathological condition that could be seen as normal inflammation. |
| Park et al., 2018 | Retrospective | 1.2/ 1.3 | 8 | 80 | 17.95_+ 6.13 | 160 | NA | 136 | Keep the insertion in the bone with success during one year. |
MM: millimeters; N: number of total patients; TAD: temporary anchorage device; NA: not applicable.
Risk of bias/quality assessment in individual studies
The quality of the studies was assessed by the same reviewers independently, using the Newcastle-Ottawa scale10. In case of any discrepancies in quality assessment, consensus was reached between the reviewers and if this was not possible a third reviewer was consulted. (Table 3)
Table 3.
Quality assessment. Newcastle-Ottawa scale10.
| Author. Year | Selection | Comparability | Outcome | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5a | 5b | 6 | 7 | 8 | ||
| Miyawaki et al., 2003 | * | NA | * | * | * | * | * | * | 7/9 | |
| Chen et al., 2004 | * | NA | * | * | * | * | * | * | 7/9 | |
| Park et al., 2006 | * | NA | * | * | * | * | * | * | 7/9 | |
| Chen et al., 2007 | * | NA | * | * | * | * | * | * | 7/9 | |
| Wiechmann et al., 2007 | * | NA | * | * | * | * | * | * | 7/9 | |
| Kuroda et al., 2007 | * | NA | * | * | * | * | * | * | 7/9 | |
| Chen et al., 2008 | * | NA | * | * | * | * | * | * | 7/9 | |
| Moon et al., 2008 | * | NA | * | * | * | * | * | * | 7/9 | |
| Wu et al., 2009 | * | NA | * | * | * | * | * | 6/9 | ||
| Motoyoshi et al., 2009 | * | NA | * | * | * | * | * | * | 7/9 | |
| Viwattanatipa et al., 2009 | * | NA | * | * | * | * | * | * | 7/9 | |
| Lee et al., 2010 | * | NA | * | * | * | * | * | * | 7/9 | |
| Takaki et al., 2010 | * | NA | * | * | * | * | * | 6/9 | ||
| Moon et al., 2010 | * | NA | * | * | * | * | * | * | 7/9 | |
| Manni et al., 2010 | * | NA | * | * | * | * | * | * | 7/9 | |
| Sharma et al., 2011 | * | NA | * | * | * | * | * | 6/9 | ||
| Topouzelis et al., 2012 | * | NA | * | * | * | * | * | * | 7/9 | |
| Kim et al., 2012 | * | NA | * | * | * | * | * | * | 7/9 | |
| Dobranski et al., 2014 | * | NA | * | * | * | * | * | * | 7/9 | |
| Yao et al., 2015 | * | NA | * | * | * | * | * | * | 7/9 | |
| Melo et al., 2016 | * | NA | * | * | * | * | * | * | 7/9 | |
| Jing et al., 2016 | * | NA | * | * | * | * | * | * | 7/9 | |
| Lee et al., 2016 | * | NA | * | * | * | * | * | * | 7/9 | |
| Tsai et al., 2016 | * | NA | * | * | * | * | * | * | 7/9 | |
| Aly et al. 2018 | * | NA | * | * | * | * | * | * | 7/9 | |
| Park et al., 2018 | * | NA | * | * | * | * | * | * | 7/9 | |
Summary measures and approach to synthesis
Means and confidence intervals were calculated for patient age, mini-implant length and diameter. Adverse events (loss of mini-implant stability) were recorded in relation to possible risk factors: mandibular or maxillary placement; vestibular, palatine/lingual, or crestal placement; placement on the left or right sides, in anterior or posterior regions; patient age and sex; mini-implant length and diameter.
Statistical analysis
For the quantitative synthesis odds ratios and 95% confidence intervals of risk factors were calculated, together with their confidence intervals. Heterogeneity was assessed by the Q test and the I2 statistic. A Q test p-value <0.1 was considered heterogeneous. The random effects method was used to calculate the odds ratios. Publication bias was analyzed using funnel plots and Egger’s regression intercept method. The software employed was comprehensive meta-analysis V 3.0 Biostat.
Results
Study selection and characteristics
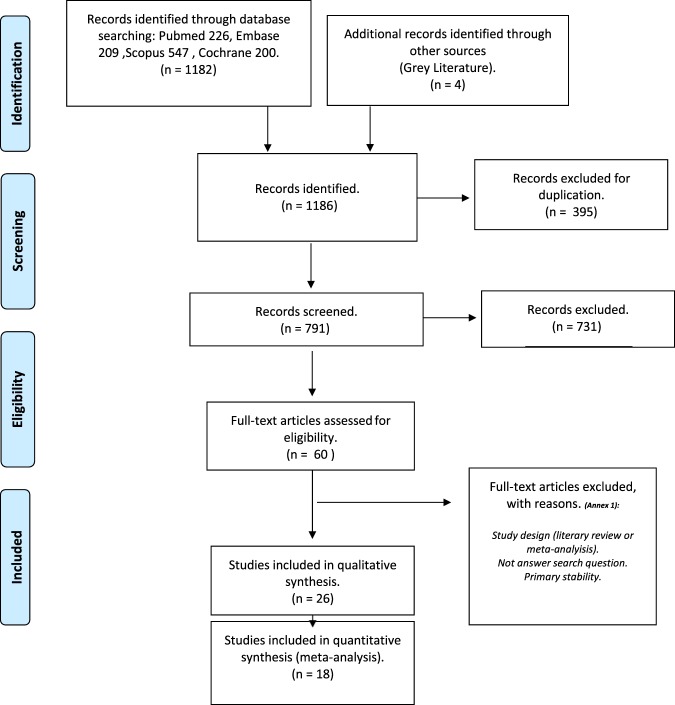
The electronic search in four databases identified 1182 articles: 226 in Pubmed, 547 in Scopus, 209 in Embase, and 200 in Cochrane; the grey literature manual search located four further works. Duplicates were eliminated leaving a total of 791 studies for analysis. After reading the titles and abstracts of the selected papers, 731 articles were discarded leaving 60 studies for thorough assessment. Full texts of these 60 studies were revised and 34 articles were eliminated as these were literature reviews or meta-analyses or because they failed to answer the research question or did not meet inclusion criteria (Table 1). A total of 26 articles fulfilled all inclusion criteria (qualitative synthesis), 18 of which were used for quantitative synthesis (meta-analysis). The PRISMA flow diagram (Fig. 1. Study selection and characteristics) illustrates the entire selection process.
Figure 1.
The PRISMA flow diagram8.
Results of individual studies, meta-analysis and additional analyses
Patient sample sizes in the articles selected ranged from a minimum of 3411 to a maximum of 57012, although most had sample sizes averaging around 150 patients. As for distribution by sex, there were more women than men. For example, one study13 included 295 women and 64 men, while another study14 included 39 women and 5 men. In most of the studies mean patient age was around 25 years, samples generally consisting of predominantly young adults. Of the 26 articles, 7 were prospective studies15–21 and 19 retrospective11–14,22–36. Follow-up periods ranged from approximately 18 months to 2 years. The shortest follow-up period was 4 months30 and the longest 10 years26.
Analyzing quality with the Newcastle-Ottawa scale, scores of 6/9 or 7/9 were obtained, which indicated moderate or moderate-high quality respectively. (Table 2)
Qualitative synthesis
With regard to the number of mini-implants, high variability was found, one of the study using a total of 1,356 mini-implants12 (study with the greatest number of mini-implants within this review) contrarily to another study that used 79 mini-implants, being the study with the lowest number of mini-implants28. Most works used an average of around 350 mini-implants. The analysis of mini-implant location found more common placement in the maxilla than in the mandible, excepting 3 studies21,25,26. Length and diameter were also evaluated, finding that the most widely used mini-implants were of 8 mm in length and 1.4 mm diameter. Mini-implants of different diameters were used ranging from 1.0 mm27 to a maximum of 2.3 mm27. As for length, the minimum length used was 5 mm12 and the maximum 21 mm13. Among studies that provided information about the side on which mini-implants were placed (left or right), only one study placed the same number of mini-implants on both sides18; in the other studies, the right side received higher number of mini-implants17,22,31,34,35. When mini-implant positions (vestibular, lingual/palatine, or crestal) were compared, the most usual position for mini-implant placement was the vestibular area33, with the exception of one article where a higher number of mini-implants were placed in lingual areas11.
Quantitative synthesis
The failure rate calculated from the total of mini-implants placed was analyzed for the risk factors studied. The highest values were observed for ages under 30 years with 19.7%, the mandibular location 18.8% and length higher than 8 mm 18.6% (Table 4).
Table 4.
Risk factors and event rate.
| Risk Factor | EVENT RATE (%) | IC 95%LOWER LIMIT | UPPER LIMIT | Q-VALUE | P-VALUE | I2 (%) | N TOTAL | NUMBER OF STUDIES INCLUDIED |
|---|---|---|---|---|---|---|---|---|
| <30 yr-old | 19.7 | 12.9 | 28.8 | 219.5 | <0.001 | 96.4 | 2934 | 8 |
| Lower jaw | 18.8 | 14.2 | 24.5 | 105,7 | <0.001 | 87.7 | 2433 | 14 |
| Length > 8 mm | 18.6 | 8.4 | 36.4 | 36.2 | <0.001 | 88.9 | 729 | 5 |
| Right side | 17.3 | 12.7 | 23.0 | 23.2 | 0.001 | 74.1 | 930 | 7 |
| Anterior | 15.7 | 9.4 | 25.1 | 24.6 | <0.001 | 87.8 | 653 | 3 |
| Women | 15.5 | 12.6 | 18.9 | 123.9 | <0.001 | 87.1 | 4541 | 16 |
| Diameter > 1.4 mm | 15.3 | 10.1 | 22.5 | 26.1 | <0.001 | 84.7 | 1591 | 5 |
| Ridge | 15.1 | 10 | 22.3 | 6.655 | 0.248 | 24.87 | 258 | 6 |
| Men | 15.0 | 12.0 | 18.5 | 63.9 | <0.001 | 74.9 | 1715 | 16 |
| Length < 8 mm | 13.6 | 9.6 | 18.9 | 13.5 | 0.009 | 70.3 | 1239 | 5 |
| Left side | 13.4 | 9.5 | 18.7 | 22.4 | 0.001 | 73.2 | 920 | 7 |
| Palate | 13.4 | 9.8 | 18 | 13.2 | 0.068 | 46.8 | 600 | 7 |
| Vestibular | 12.5 | 10.3 | 15.0 | 24.1 | 0.001 | 70.9 | 2544 | 7 |
| Posterior | 12.1 | 7.8 | 18.3 | 6.7 | 0.080 | 55.6 | 618 | 3 |
| Upper jaw | 11.4 | 9.1 | 14.4 | 65.4 | 0.000 | 80.1 | 3550 | 14 |
| Diameter < 1.4 mm | 10.8 | 8.9 | 12.9 | 0.111 | 0.991 | 0.000 | 912 | 4 |
| >30 yr-old | 9.5 | 7.4 | 12.3 | 10.4 | 0.234 | 23.5 | 755 | 8 |
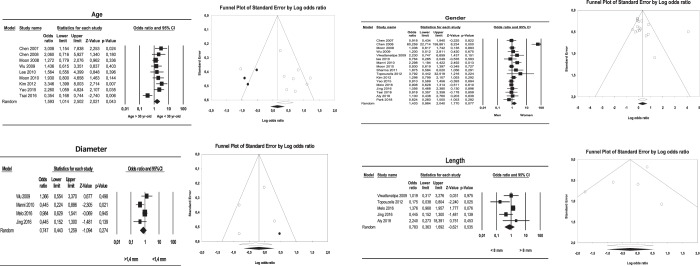
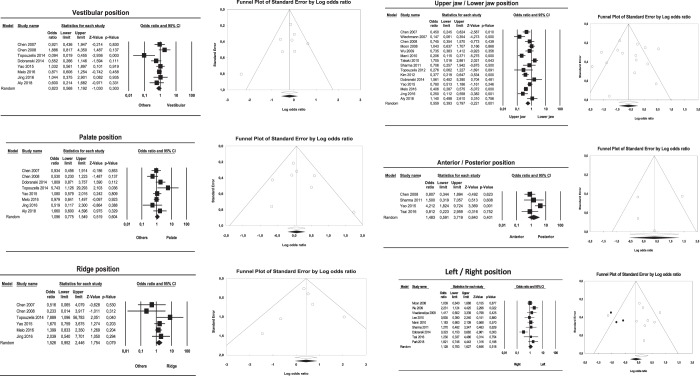
Mini-implant location in the maxilla or mandible showed a significant relation with secondary stability; the odds ratio obtained in the forest plot of this meta-analysis was 0.56 (95% confidence interval (CI) between 0.39 and 0.80), which indicates that mandibular mini-implant placement is a protective factor. Moreover, the I2 value (I2 = 78%) indicated heterogeneity (Q = 63.72; p < 0.001). Analysis of the age variable found that ages of 30 or lower were also a protective factor for mini-implant secondary stability although this did not reach statistical significance, with an odds ratio of 1.59 and 95% CI of 1.01 to 2.50. The I2 value in this case was 63.67%, indicating moderate heterogeneity (Q = 22.02; p = 0.005).
Gender did not show a statistically significant relation with secondary stability, obtaining an odds ratio of 1.40 and 95% CI of 0.96 to 2.04; the I2 value indicated heterogeneity 79.4 (Q = 77.8; p < 0.001). The same occurred with the mini-implant position variable, where vestibular placement showed an I2 value of 47.55% (Q = 13.35; p = 0.06). Palatine/lingual placement obtained a lower value, I2 = 34.62% (Q = 10.71; p = 0.15). Lastly, ridge placement obtained I2 = 13.16 (Q = 5.75; p = 0.33), indicating that vestibular placement showed moderate heterogeneity, while lingual and crestal placement showed low heterogeneity. Odds ratios and confidence intervals showed that none of these variables reached statistical significance (vestibular odds ratio 0.82; CI = 0.56 to 1.19; lingual odds ratio 1.10; 95% CI = 0.78 to 1.55; ridge odds ratio 1.53; 95% CI = 0.95 to 2.45).
With regard to placement on the left side or right side, or in anterior or posterior regions, statistically significant relations were found for both variables (left/right side: odds ratio 1.128, with a 95% CI = 0.783 to 0.627; anterior/posterior location: odds ratio 1.48, with a 95% CI = 0.59 to 3.72). The I2 value showed an absence of heterogeneity; I2 values were 50.9 (Q = 16.30; p = 0.03), and I2 = 53.94 (Q = 8.68; p = 0.06), respectively.
Lastly, mini-implant dimension variables, length and diameter, did not obtain statistically significant relations (diameter: odds ratio 0.74, with a 95% CI = 0.44 to 1.25; length: odds ratio 0.78, with a 95% CI = 0.36 to 1.69). In both cases the I2 value indicated heterogeneity: I2 = 61.11 (Q = 10.28; p = 0.03) and I2 = 69.6 (Q = 9.87; p = 0.02).
Publication bias
Funnel plots presented symmetrical images without differences in estimations when imputed values were added, with the exception of crestal placement. The plot for this variable did show some asymmetry, indicating the existence of publication bias (Figs. 2 and 3).
Figure 2.
Forest and funnel plots for meta-analyses for: gender, age, mini-implant length and mini-implant diameter.
Figure 3.
Forest and funnel plots for meta-analyses for different mini-implant locations.
None of the Egger’s regression intercepts calculated for the different Odds ratio estimations, have shown significance. For upper and lower jaw, the results were −0.37 between −3.87 and 3.21, p = 0.84; for gender 2.06 between −0.73 and 4.86, p = 0.13; for age 2.26 between −3.05 and 7.59, p = 0.34, vestibular position −1.1, p = 0.36; palatine/lingual 0.82 between −2.09 and 3.75, p = 0.51; ridge position −0.14 between −2.69 and 2.40, p = 0.88; age 2.26, p = 0.34; diameter −1.38, p = 0.631; length −1.45 between −4.95 and 2.04, p = 0.27; anterior and posterior position −1.10 between −19.1 and 15.3, p = 0.70; and right and left location 0.35, p = 0.85.
Discussion
Summary of evidence
The null hypothesis of the present study was rejected. When analyzing failure rates, significant differences were found when comparing different mini-implant locations. The maxillary location showed significantly lower failure rates than the mandibular, while the rest of the analyzed variables did not show significant effects.
Bone anchorage in orthodontic treatments is becoming ever more widespread. As the literature states repeatedly, the advantages offered by mini-implants are numerous, and the technique shows a success rate of over 80%37. But when mini-implants fail they do so during the first 8 weeks after placement, the period when implant stability changes from mechanical to biological stability6. The reasons for failure (mobility, displacement or infection of the surrounding soft tissues) were not assessed in the present literature review, as its objective was to determine which variables predispose mini-implants to failure.
Longitudinal studies, cohort and case/control studies both prospective and retrospective were included in the present review. Although RCTs were eligible to be included, none met the inclusion criteria. Cohort, case/control and RCT studies are the ones that better evaluate the risk factors associated with mini-implants stability. Including different study designs could lead to broad variations in outcome and quality terms. However, when analysing the quality of all of them we found that most of them present values between 6 and 7 in the Newcastle-Ottawa scale indicating that they have moderate quality (Table 3).
Since weaker studies can influence the outcome of the present study, the sensitivity of the estimation of the 19 conducted meta-analyzes was analyzed and none of the studies was found to significantly influence the results, except one (Figs. 2 and 3).
The variables analyzed can be divided into three groups: variables deriving from the patient, others related to the mini-implant used (length and diameter), and a third set related to location and technique. Among the variables deriving from the patient, the present study identified some controversy surrounding the possible association between mini-implant failure and age. Some studies found no association between age and failure14,15,32, while others found that the patient’s age could influence mini-implant failure because younger patients present finer cortical bone and lower bone density19,30–34. (Fig. 2)
The variable sex was also subject to controversy. While some studies12–14,30,31 claim that the patients’ gender does not influence the success or failure of treatment with mini-implants, other works33,35 found a higher mini-implant success rate among men, which they attributed due to their higher bone density. However, the present review did not generally find a significant association between sex and loss of secondary stability.
Several other factors may influence failure/success rates but the present review was unable to analyze them due to the lack of published articles. These include poor hygiene, inflammation of surround tissues and the individual patient’s bone density36, all thought to play a role in treatment failure13.
When mini-implant characteristics were analyzed, those articles that analyzed different implant sizes16,27,28, agreed that diameters smaller than 1 mm show a tendency to failure. These findings make sense since smaller diameters provide less attachment surface and also, they are weaker so prone to fracture. But other studies14,31 found that length and diameter were not variables with any significant influence on success/failure rates. Meanwhile, two studies11,24 found that length was a factor that influences stability. The present meta-analysis did not show that mini-implants longer than 8 mm or with diameters over 1.4 mm undergo fewer failures than those with smaller dimensions.
Regarding mini-implant location, two studies14,16 stated that mini-implants presented a worse prognosis in posterior regions and in the alveolar mucosa. Between vestibular, lingual/palatine and crestal placement, two studies16,26 agreed that there is a higher risk of loss of mini-implant stability in lingual/palatine areas. But another study24 found that placement in crestal areas shows greater risk of failure. Meanwhile, two studies31,34 affirmed that the right side presents a higher risk of failure than the left. This could be due to patient’s oral hygiene maintenance capability or the dexterity of the clinician. The present review did not find significant relations between mini-implant failure and vestibular, lingual, or crestal placement or between placement on the left or right side. Only two articles14,26 differentiate jaw and maxilla together with the anterior and posterior position obtaining higher success rates in the anterior maxillary area (including the palate), with no statistically significant differences.
However, in agreement with some studies33,35 placement of mini-implants in the mandible could be a protective factor due to the mandible’s higher bone density. (Fig. 3)
Among the technical characteristics of mini-implant placement, there is also some controversy surrounding the intensity and duration of the force applied. One study16 claimed that the correct force is between 100 and 200 grams, and concluded that lower forces produced higher success rates, as did applying force for the shortest possible time. As for surgical technique, one work28 concluded that mini-implant placement without flap raising produces less damage and so higher success rates. Mini-implant placement using a motor also favored a successful outcome, moreover the surgical protocol with or without predrilling has only been assessed in a study that showed no significant differences. One study33 obtained a success rate of 88.38% for no-predrilling mini-implant insertion and 89.09% for predrilling, with an odds ratio of 0.93 (95% CI 0.36 to 2.42). For some authors, surgical technique is one of the most influential variables affecting stability18.
Knowledge of the factors involved in the failure of mini-implants can help the clinicians to improve their clinical practice. Within the analyzed factors there are some that could be adapted for a higher success. Only location seems to have a significant effect, having the upper jaw lower failure rate than the lower. However, this cannot be clinically modified since it depends on the biomechanics required in each case. The other analyzed factors did not show differences and their failure rates are very similar. (Table 4)
Limitations
The limited number of studies that have investigated the variables analyzed in the present review could lead to estimation bias or even failure to identify their significance. Further prospective studies under controlled conditions could produce better information and improve the outcomes of orthodontic treatment involving the use of mini-implants.
Conclusions
Based on the results of the present study, some variables both mini-implant and patient-dependent are related to the success rates of mini-implants (age, location and mini-implant length). The only significant factor was location, being upper maxilla placement of mini-implants more successful than mandible. The conclusions drawn from the present analysis regarding correlations between success/failure and the analyzed factors should be treated with caution due to the different methodologies employed in the different studies reviewed.
Acknowledgements
The authors wish to thank William James Packer for translating the manuscript into English.
Author contributions
All authors contributed to the study: M.D.C.-R. and C.B.-A. participated in data collection, analysis and interpretation, and in drafting and revising the manuscript. J.M.M.-C. and V.P.-G. participated in designing and interpreting the statistical analysis and in critical revision. J.M.A.-S. and V.G.-S. participated in interpretation, drafting and revision.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zawawi K. Acceptance of orthodontic miniscrews as temporary anchorage devices. Patient Prefer Adherence. 2014;8:933–937. doi: 10.2147/PPA.S66133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharif MO, Waring DT. Contemporary orthodontics: the micro-screw. Br Dent J. 2013;214:403–408. doi: 10.1038/sj.bdj.2013.376. [DOI] [PubMed] [Google Scholar]
- 3.Liu H, Wu X, Yang L, Ding Y. Safe zones for miniscrews in maxillary dentition distalization assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2017;151:500–506. doi: 10.1016/j.ajodo.2016.07.021. [DOI] [PubMed] [Google Scholar]
- 4.Dalessandri D, et al. Determinants for success rates of temporary anchorage devices in orthodontics: a meta-analysis (n > 50) Eur J Orthod. 2014;36(3):303–313. doi: 10.1093/ejo/cjt049. [DOI] [PubMed] [Google Scholar]
- 5.Bravo, L.A. Manual de Ortodoncia. Ed. Síntesis. Madrid. (2003).
- 6.Cadavid D, Duque L, Correa S, Buschang P, Roldán S. Miniimplant stability in Orthodontics. “Bone Biology and Biomechanics”. CES J Odont. 2014;27(2):93–103. [Google Scholar]
- 7.Watanabe H, et al. Orthodontic miniscrew failure rate and root proximity, insertion angle, bone contact length, and bone density. Orthod Craniofac Res. 2013;16(1):44–55. doi: 10.1111/ocr.12003. [DOI] [PubMed] [Google Scholar]
- 8.Liberati A, et al. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Systematic Review, CRD guidance for Undertaking Reviews in Health Care (UK). University of York, Centre for Review and Dissemination. (2009).
- 10.Wells, G.A. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses (2014).
- 11.Topouzelis N, Tsaousoglou P. Clinical factors correlated with the success rate of miniscrews in orthodontic treatment. Int J Oral Science. 2012;4:38–44. doi: 10.1038/ijos.2012.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Melo A, et al. Risk factors associated with the failure of miniscrews – a ten-year cross sectional study. Braz Oral Res. 2016;30(1):e124. doi: 10.1590/1807-3107BOR-2016.vol30.0124. [DOI] [PubMed] [Google Scholar]
- 13.Chen YJ, et al. A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems. Clin Oral Implants Res. 2007;18:768–775. doi: 10.1111/j.1600-0501.2007.01405.x. [DOI] [PubMed] [Google Scholar]
- 14.Chen YJ, et al. Stability of miniplates and miniscrews used for orthodontic anchorage: experience with 492 temporary anchorage devices. Clin Oral Implants Res. 2008;19:1188–1196. doi: 10.1111/j.1600-0501.2008.01571.x. [DOI] [PubMed] [Google Scholar]
- 15.Cheng SJ, Tseng IY, Lee JJ, Kok SH. A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage. Int J Oral Max Impl. 2004;19:100–106. [PubMed] [Google Scholar]
- 16.Wiechmann D, Meyer U, Bücher A. Success rate of mini-and micro-implants used for orthodontic anchorage: a prospective clinical study. Clin Oral Implants Res. 2007;18:263–267. doi: 10.1111/j.1600-0501.2006.01325.x. [DOI] [PubMed] [Google Scholar]
- 17.Viwattanatipa N, Thanakitcharu S, Uttraravichien A, Pitiphat W. Survival analyses of surgical miniscrews as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2009;136:29–36. doi: 10.1016/j.ajodo.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 18.Lee SJ, Ahn SJ, Lee J, Kim SH, Kim TW. Survival analysis of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010;137:194–199. doi: 10.1016/j.ajodo.2008.03.031. [DOI] [PubMed] [Google Scholar]
- 19.Dobranszki D, Faber J, Scatolino I, Dobranszki N, Ayrton O. Analysis of Factors Associated with Orthodontic Microscrew Failure. Braz Oral Res. 2014;25(4):346–351. doi: 10.1590/0103-6440201300125. [DOI] [PubMed] [Google Scholar]
- 20.Tsai C, Chang H, Pan C, Chou S, Tseng Y. A prospective study of factors associated with orthodontic mini-implant survival. J Oral Science. 2016;58:515–521. doi: 10.2334/josnusd.16-0145. [DOI] [PubMed] [Google Scholar]
- 21.Aly SA, Alyan D, Fayed MS, Alhammadi MS, Mostafa YA. Success rates and factor associated with failure of temporary anchorage devices: a prospective clinical trial. J Invest Clin Dent. 2018;9(3):e12331. doi: 10.1111/jicd.12331. [DOI] [PubMed] [Google Scholar]
- 22.Sharma P, Valiathan A, Sivakumar A. Success Rate of Microimplants in a University Orthodontic Clinic. ISRN Surg. 2011;2011:982671. doi: 10.5402/2011/982671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim J, et al. Comparison of success rates of orthodontic mini-screws by the insertion method. Korean J Orthod. 2012;42(5):242–248. doi: 10.4041/kjod.2012.42.5.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yao CC, et al. Revisiting the stability of mini-implants used for orthodontic anchorage. J Formos Med Assoc. 2015;114(11):1122–1128. doi: 10.1016/j.jfma.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 25.Motoyoshi M, Inaba M, Ono A, Ueno S, Shimizu N. The effect of cortical bone thickness on the stability of orthodontic mini-implants and on the stress distribution in surrounding bone. Int J Oral Max Surg. 2009;38:13–18. doi: 10.1016/j.ijom.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 26.Takaki T, et al. Clinical Study of Temporary Anchorage Devices for Orthodontic Treatment Stability of Micro/Mini-screws and Mini-plates: Experience with 455 Cases. Bull Tokyo Dent Coll. 2010;51(3):151–163. doi: 10.2209/tdcpublication.51.151. [DOI] [PubMed] [Google Scholar]
- 27.Miyawaki S, et al. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2003;124:373–378. doi: 10.1016/S0889-5406(03)00565-1. [DOI] [PubMed] [Google Scholar]
- 28.Kuroda S, Sugawara Y, Deguchi T, Kyung H, Takano-Yamamoto T. Clinical use of miniscrew implants as orthodontic anchorage: Success rates and postoperative discomfort. Am J Orthod Dentofacial Orthop. 2007;131:9–15. doi: 10.1016/j.ajodo.2005.02.032. [DOI] [PubMed] [Google Scholar]
- 29.Park HS, Jeong SW, Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006;130:18–25. doi: 10.1016/j.ajodo.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 30.Moon CH, Lee DG, Lee HS, Im JS, Baek HS. Factors Associated with the Success Rate of Orthodontic Miniscrews Placed in the Upper and Lower Posterior Buccal Region. Angle Orthod. 2008;78(1):101–106. doi: 10.2319/121706-515.1. [DOI] [PubMed] [Google Scholar]
- 31.Wu TY, Kuang SH, Wu CH. Factors Associated With the Stability of Mini-Implants for Orthodontic Anchorage: A Study of 414 Samples in Taiwan. J Oral Max Surg. 2009;67:1595–1599. doi: 10.1016/j.joms.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 32.Moon CH, Park HK, Nam JS, Im JS, Baek SH. Relationship between vertical skeletal pattern and success rate of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010;138:51–57. doi: 10.1016/j.ajodo.2008.08.032. [DOI] [PubMed] [Google Scholar]
- 33.Jing MS, et al. Factors affecting the clinical success rate of miniscrew implants for orthodontic treatment. Int J Oral Max Impl. 2016;31:835–841. doi: 10.11607/jomi.4197. [DOI] [PubMed] [Google Scholar]
- 34.Park H, et al. Evaluation of factors influencing the success rate of orthodontic microimplants using panoramic radiographs. Korean J Orthod. 2018;48(1):30–38. doi: 10.4041/kjod.2018.48.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Manni A, Cozzani M, Tamborrino F, Rinaldis S, Menini A. Factors influencing the stability of miniscrews. A retrospective study on 300 miniscrews. Eu J Orthod. 2010;33:388–395. doi: 10.1093/ejo/cjq090. [DOI] [PubMed] [Google Scholar]
- 36.Lee MY, et al. Bone density effects on the success rate of orthodontic microimplants evaluated with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2016;149:217–224. doi: 10.1016/j.ajodo.2015.07.037. [DOI] [PubMed] [Google Scholar]
- 37.Reynders R, Ronchi L, Bipat S. Mini-implants in orthodontics: a systematic review of the literature. Am J Orthod Dentofacial Orthop. 2009;135:564.e1–564.e19. doi: 10.1016/j.ajodo.2008.09.026. [DOI] [PubMed] [Google Scholar]