Abstract
Persistent Thebesian veins with the appearance of multiple coronary artery microfistulas are a rare finding and little is known about their physiologic and clinical features. In addition, few reports have demonstrated the perfusion status of patients with Thebesian veins. We report a 75-year-old woman referred for non-ST-elevation myocardial infarction due to prominent Thebesian veins who displayed a perfusion defect in cardiac magnetic resonance imaging.
<Learning objective: This case emphasizes that non-obstructive coronary arterial anomaly can lead to myocardial ischemia with angina symptoms and cardiac enzyme rise. Moreover, it provided the typical angiographic appearance of Thebesian vein network and image of myocardial perfusion defect induced by coronary steal.>
Keywords: Thebesian veins, Acute myocardial infarction, Cardiac magnetic resonance imaging
Introduction
Visualization of Thebesian vein drainage of the coronary circulation is a rare finding during coronary angiography [1]. Although most patients with coronary fistulae remain asymptomatic, some develop congestive heart failure, infective endocarditis, or myocardial ischemia induced by a coronary steal syndrome [2]. Here, we describe a rare case of prominent Thebesian veins with subsequent subendocardial ischemia, confirmed by cardiac magnetic resonance imaging (MRI), in an old patient presenting as acute myocardial infarction.
Case report
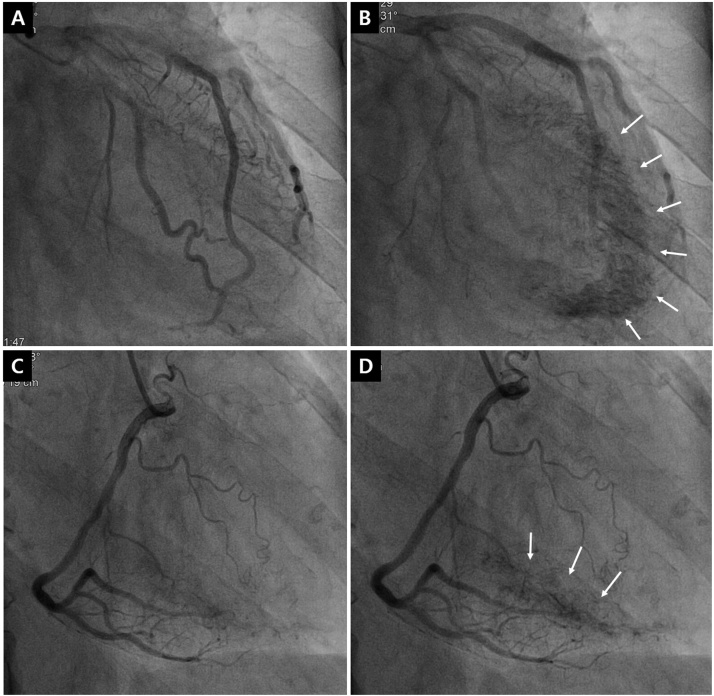
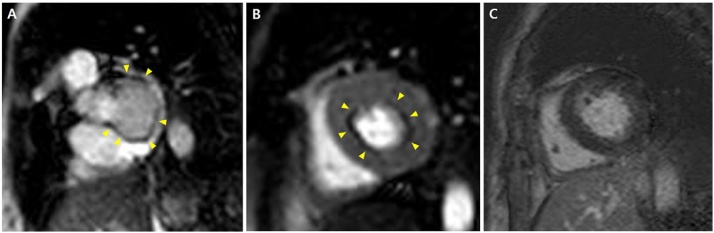
A 75-year-old woman was brought to the emergency room with anterior chest pain that had developed one day previously. The patient had a medical history of diabetes treated with insulin injection. Her vital signs were stable. However, the electrocardiography showed a T wave inversion on lead V3–6 (Fig. 1) and serum cardiac enzymes were elevated (creatine kinase-MB 8.56 ng/ml and troponin T 0.225 ng/ml, respectively). Transthoracic echocardiography demonstrated a concentric left ventricular (LV) hypertrophy and normal LV systolic function without regional wall motion abnormality. Since it was suspected as myocardial infarction, coronary angiography was performed. Left coronary angiography revealed no significant obstructive lesions, but a marked contrast blush at endocardial surface, nearly producing ventriculogram, via extensive multiple microfistulae arising from the diagonal branch of left anterior descending artery, and draining into the LV cavity (Fig. 2A and B, Supplementary movie 1). The left coronary artery was not filled enough with contrast due to the large amount of leakage into the LV chamber. Right coronary angiography also showed capillary blush draining into the LV cavity from posterolateral branch and posterior descending artery (Fig. 2C and D, Supplementary movie 2). These appearances suggested arterioluminal type of Thebesian venous network draining blood from the coronary arteries into the ventricle. LV angiogram using pigtail catheter showed no other fistulae or defects (Supplementary movie 3). We performed cardiac MRI and it showed a definite subendocardial perfusion defect at the level of base to mid-LV during rest perfusion sequence (Fig. 3A and B, Supplementary movie 4). From these findings, we could notice that prominent Thebesian veins can be a cause of subendocardial ischemia even in the resting state and clinically present as acute coronary syndrome. However, late gadolinium enhancement suggesting subendocardial myocardial infarction was not observed at delayed phase (Fig. 3C). With administration of bisoprolol and valsartan for reducing cardiac afterload, the patient was discharged with improved symptoms and was stable for 3 months of follow-up in the outpatient clinic.
Fig. 1.
Twelve-lead electrocardiography showing left ventricular hypertrophy with a T-wave inversion on lead V3-6.
Fig. 2.
Coronary angiography showing no significant stenosis. Abnormal contrast blush with drainage into the left ventricular chamber can be observed on both coronary arteries, left (A and B) and right (C and D). Arrows point to the contrast blush through the Thebesian venous network, allowing the visualization of the endocardial border (B and D).
Fig. 3.
Cardiac magnetic resonance imaging of perfusion sequence (A and B) and late gadolinium enhancement imaging sequence (C). The yellow arrows point to a subendocardial ring of low signal enhancement, showing the perfusion defect in the subendocardium from the base (A) to mid-left ventricle (B). No late gadolinium enhancement was seen at a delayed phase (C).
Discussion
Thebesian veins, small valveless venous channels were initially described by Vieussens in 1706 [3]. This primitive network supplies the subendocardial myocardium during embryogenesis and interference in the fetal regression of this structure might produce a prominent Thebesian vein system with the appearance of multiple coronary microfistulae [4]. Thebesian vessels have three distinct forms: (1) veins drain blood from the capillary bed into the ventricular cavity; (2) arterioluminal vessels directly drain from the arteries into the ventricles; and (3) venoluminal vessels that connect the coronary veins into the ventricular cavities [3]. Our case is the arterioluminal type, which communicates between the coronary arteries and LV cavity bypassing a myocardial capillary bed, and thus acting as a coronary-cameral shunt and potentially leading to myocardial ischemia due to coronary steal. In addition, a profound drop in perfusion pressure because of rapid run-off and impaired subendocardial perfusion of the hypertrophied myocardium could also induce myocardial ischemia [5]. Some cases of prominent Thebesian veins present as ischemic heart disease [2], [6] and even, acute coronary syndrome [7], but reports demonstrating the imaging evidence of inducible ischemia in these patients are sparse [8]. In this report, we described the subendocardial nature of definite perfusion defect using cardiac MRI in a patient with significant coronary microfistulae through Thebesian veins. The area of hypoperfusion is believed to correspond to the myocardium region that is bypassed via the Thebesian venous network.
The management of patients with multiple coronary fistulae remains controversial. Nitrate can exacerbate ischemic symptoms by increasing coronary steal and decreasing total coronary flow to the myocardium. A few cases have proven the effect of beta-blockers and renin-angiotensin-aldosterone system agents in these patients [2], [8]. Similarly, in this case, the patient’s symptoms were relieved by beta-blocker and angiotensin II receptor blocker which might reduce cardiac afterload.
We presented a rare case of prominent Thebesian veins presenting as acute myocardial infarction accompanied by subendocardial perfusion defect which was detected by cardiac MRI. Further studies are needed to elucidate the long-term physiologic and clinical impact of this anomaly.
Conflict of interest
The authors declare that there is no conflict of interest.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jccase.2019.11.007.
Contributor Information
Sung Woo Cho, Email: drswcho@hanmail.net.
Byung Gyu Kim, Email: bong9abc@naver.com.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Yamanaka O., Hobbs R.E. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990;21:28–40. doi: 10.1002/ccd.1810210110. [DOI] [PubMed] [Google Scholar]
- 2.Jung Y., Kim H.J., Yoon C.H. Severe form of persistent thebesian veins presenting as ischemic heart disease. Korean Circ J. 2012;42:714–717. doi: 10.4070/kcj.2012.42.10.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ansari A. Anatomy and clinical significance of ventricular Thebesian veins. Clin Anat. 2001;14:102–110. doi: 10.1002/1098-2353(200103)14:2<102::AID-CA1018>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 4.Hong G.R., Choi S.H., Kang S.M., Lee M.H., Rim S.J., Jang Y.S. Multiple coronary artery-left ventricular microfistulae in a patient with apical hypertrophic cardiomyopathy: a demonstration by thoracic colar Doppler echocardiography. Yonsei Med J. 2003;44:710–714. doi: 10.3349/ymj.2003.44.4.710. [DOI] [PubMed] [Google Scholar]
- 5.Jacob M.A., Goyal S.B., Pacifico L., Spodick D.H. Multiple coronary artery-left ventricular fistulas associated with hereditary hemorrhagic telangiectasia. Chest. 2001;120:1415–1417. doi: 10.1378/chest.120.4.1415. [DOI] [PubMed] [Google Scholar]
- 6.Krishnan U., Schmitt M. Images in cardiovascular medicine. Persistent thebesian sinusoids presenting as ischemic heart disease. Circulation. 2008;117 doi: 10.1161/CIRCULATIONAHA.107.748863. e315–6. [DOI] [PubMed] [Google Scholar]
- 7.Alam R., Skehan J., Gunarathne A. A significant’ coronary steal’ by thebesian veins, a rare congenital coronary defect masquerading as acute coronary syndrome. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2014-208880. pii:bcr2014208880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strange J.W., Bucciarelli-Ducci C., Mathur A., Pennell D.J. Images in cardiovascular medicine. Multiple coronary fistulae: a cause of subendocardial ischemia. Circulation. 2008;117:853–856. doi: 10.1161/CIRCULATIONAHA.107.725515. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.