Abstract
Pacemaker implantations are minimally invasive procedures commonly used for patients with bradycardic arrhythmias. Takotsubo cardiomyopathy, which is usually induced by life-threatening stress hardly ever occurs after this minimally invasive procedure. Here, we experienced a patient who developed takotsubo cardiomyopathy leading to ventricular fibrillation the day after a pacemaker implantation. At that time, a cardiac echocardiogram and left ventriculogram revealed hypercontraction of the base of the heart and a decreased contraction of the apex. A coronary angiogram revealed no significant coronary stenosis. Ten days later, the electrocardiogram findings normalized, and an echocardiogram revealed that the left ventricular function had fully recovered. Therefore, we diagnosed this patient with takotsubo cardiomyopathy. In general, pacemaker implantations are routine procedures and fatal complications are low. We report a case that developed potentially fatal complications after a pacemaker implantation.
<Learning objective: This patient developed in-hospital cardiac arrest due to ventricular fibrillation from takotsubo cardiomyopathy after a pacemaker implantation, which is of special interest because complications leading to in-hospital cardiac arrest just after a pacemaker implantation are rare. We consider this case report as an educational case that caused potentially fatal complications even after pacemaker implantation.>
Keywords: Takotsubo cardiomyopathy, Ventricular fibrillation, Pacemaker implantation, Dialysis
Introduction
Patients with sick sinus syndrome complicated with paroxysmal atrial fibrillation (AF) usually require pacemaker therapy. Pacemaker implantation procedures are well established and the risk of this procedure is not high. It is rare for fatal complications to occur soon after surgery [1].
On the other hand, takotsubo cardiomyopathy, which is caused by emotional and physical stress, is generally known as a disease with a good prognosis. However, these cases often lead to cardiogenic shock or lethal arrhythmias [2]. Several cases of takotsubo cardiomyopathy after pacemaker implantations have been reported, but most of those cases have had a good clinical course [3], [4]. This present case developed an in-hospital cardiac arrest due to ventricular fibrillation (VF) from takotsubo cardiomyopathy after a pacemaker implantation. We should consider the possibility of a rare fatal complication even after a pacemaker implantation.
Case report
The patient was an 81-year-old male and for 11 years he had been maintained on dialysis due to end-stage renal disease. The frequency of his paroxysmal AF had increased from one year previously. Then sinus arrest was observed, accompanied by a feeling of presyncope at the end of the dialysis. He was hospitalized for a pacemaker implantation for sick sinus syndrome type III.
At the time of the hospitalization his height was 143.0 cm, weight 36.7 kg, blood pressure 104/73 mmHg, and pulse rate 86/min regular. The blood tests 4 h before the procedure revealed severe renal dysfunction (blood urea nitrogen 44.0 mg/dl and creatinine 9.07 mg/dl) and electrolyte values within normal range (sodium 134 mEq/l, potassium 5.6 mEq/l, and chlorine 96 mEq/l). The other data were within normal limits. A preoperative echocardiographic examination revealed an ejection fraction of 53% and no wall motion abnormalities or valvular disease.
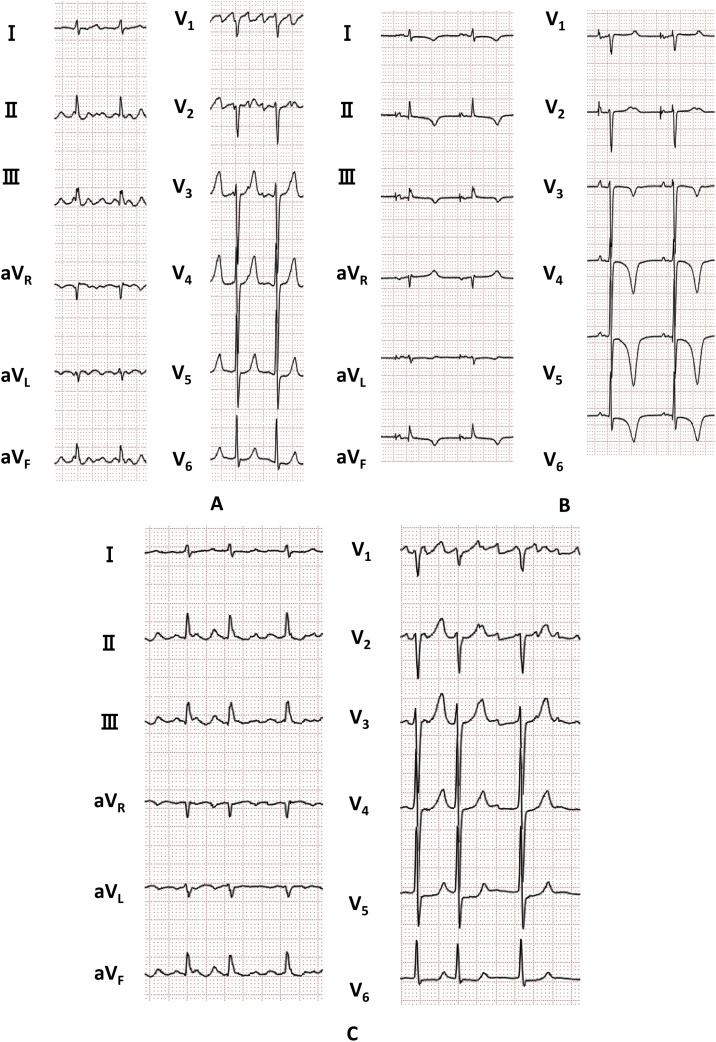
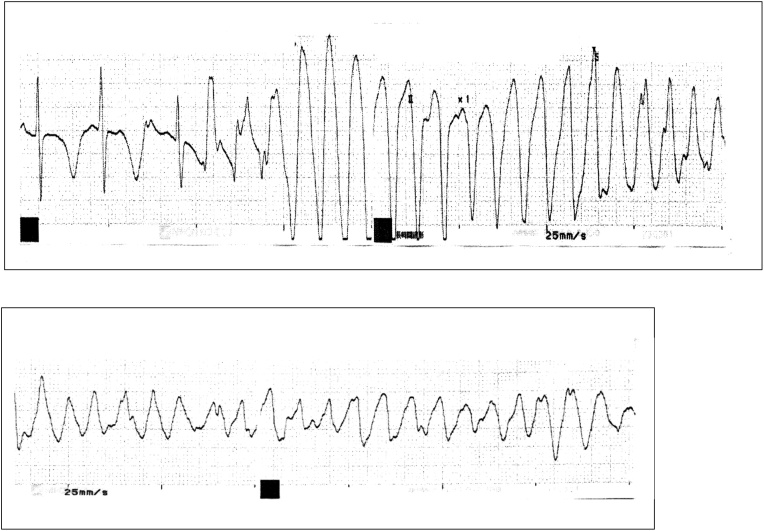
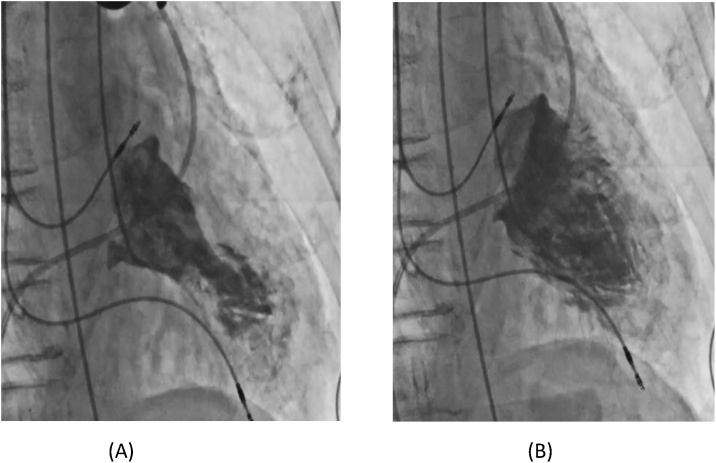
A DDD pacemaker implantation was performed under local anesthesia (1% xylocaine) on the 2nd hospital day. The operation time was 1 h and 13 min without any complications. The recorded data at the time of the implantation were an amplitude of 2.6 mV, threshold value of 0.75 V/0.4 ms, and impedance of 440 Ω in the atrium, and an amplitude of 6.9 mV, threshold of 1.25 V/0.4 ms, and impedance of 490 Ω in the right ventricle. At this time, the electrocardiography (ECG) findings revealed AF, a normal QT interval (corrected QT interval, 403 ms), and no ST-T abnormalities. The patient took aprindine only once after the pacemaker implantation because AF developed. Since the AF terminated within about 3 h, he did not take any aprindine thereafter. There were no symptoms 18 h after the implantation, but the ECG changed to sinus rhythm with giant negative T waves and a prolonged QT interval (corrected QT interval, 501 ms) as compared to that on admission (Fig. 1A, B). During the dialysis 26 h after the implantation, polymorphic ventricular tachycardia appeared just after a further QT prolongation (corrected QT interval, 539 ms) and short coupled premature ventricular beats. The polymorphic ventricular tachycardia immediately degenerated into VF (Fig. 2). Three electrical shocks were immediately delivered and terminated the VF. The blood test electrolytes just after the termination of the VF did not change compared to that at admission (sodium 141 mEq/l, potassium 4.7 mEq/l, chlorine 106 mEq/l, calcium 7.5 mg/dl, phosphorus 3.8 mg/dl) but the cardiac enzymes increased (creatine phosphokinase 239 U/L and cardiac troponin-I 0.143 ng/ml). Echocardiography revealed akinesis of the apical wall and a hyper-construction on the basal wall without any evidence of a pericardial effusion. We confirmed that no bleeding or traumatic changes had occurred on the brain computed tomography (CT). Emergency coronary angiography found no significant stenosis. A left ventriculogram revealed a hypercontraction at the base of the heart and decreased contraction at the apex (Fig. 3). Therefore, the patient was diagnosed with takotsubo cardiomyopathy. On the 10th hospital day, the electrocardiogram findings normalized (Fig. 1C) and an echocardiogram revealed that the left ventricular function had fully recovered.
Fig. 1.
(A) Electrocardiographic findings on admission, (B) 18 h after the pacemaker implantation, and (C) 10 days after the pacemaker implantation.
Fig. 2.
Monitored electrocardiogram findings at the time of the occurrence of ventricular fibrillation during dialysis.
Fig. 3.
Left ventriculography after the ventricular fibrillation. (A) Systolic phase and (B) diastolic phase.
Discussion
We experienced a case in which VF developed due to takotsubo cardiomyopathy. In particular, the characteristics observed in this case were that he was a male whose initial symptom was an in-hospital cardiac arrest due to VF just after a pacemaker implantation.
According to the diagnostic criteria of the Mayo clinic [5], in this case, the transient left ventricular wall motion abnormality did not match the reflux area of the ischemia, acute ischemic heart disease was denied by coronary angiography, new negative T waves were recognized, and no bleeding or traumatic changes were recognized on the brain CT at the onset. Myocarditis was denied because the ECG and cardiac function recovered after 2 weeks. Coronary spastic angina was denied because this patient had no typical symptoms such as resting chest pain, and the negative T waves on the ECG persisted for several days instead of hours, including while there was no evidence of coronary spasms confirmed by coronary angiography. No pheochromocytoma was suspected because he had no paroxysmal or resistant hypertension, no typical symptoms (perspiration, headache, tremors, pallor, or palpitations during sinus rhythm) and contrast-enhanced CT revealed no tumorous lesions of the adrenal and extraadrenal glands. Therefore, this case completely matched the diagnostic criteria.
Although takotsubo cardiomyopathy generally has a good prognosis, the acute phase mortality rate during hospitalization is described to be 4–5% [6]. In the results of the registry of 1750 patients with takotsubo cardiomyopathy, most endpoints, including in-hospital death, occur more frequently among men than women, which is similar to this case report. Ventricular tachycardia was recognized in 3% during the course of the takotsubo cardiomyopathy and no lethal ventricular arrhythmias were recognized in the ECG findings at the time of admission [7]. In a report of 136 patients with takotsubo cardiomyopathy, there were three deaths during the course, but there were no deaths due to ventricular arrhythmias [8]. The occurrence of VF as a course of takotsubo cardiomyopathy such as in this case is less frequent. However, previous reports have described the association between lethal arrhythmias and QT prolongation in takotsubo cardiomyopathy [9]. In this case, the corrected QT interval prolonged and a short coupled premature ventricular contraction were confirmed at the onset of the VF. We speculated that takotsubo cardiomyopathy was the main cause of the VF rather than the adverse effects of the aprindine taken only once.
The cause of takotsubo cardiomyopathy is emotional or physical stress, and stress from surgery is one such cause [10]. In previous reports, several cases who developed takotsubo cardiomyopathy after pacemaker implantations have been reported [3], [4]. Most of the patients were elderly females, with a procedure to onset time from 10 min to 3 days, and they finally recovered. Those cases did not develop VF at the onset of takotsubo cardiomyopathy. To the best of our knowledge, this is the first description of a clinically diagnosed takotsubo cardiomyopathy case associated with VF after a pacemaker implantation.
Patients who receive cardiovascular implantable electronic devices (CIEDs) including pacemakers are increasing year by year. According to the registry data of 5918 cases, a total of 5.5% of patients died within 6 months and the in-hospital mortality was 0.1%. There was only one death related to surgery [1]. Therefore, complications leading to in-hospital cardiac arrest just after a pacemaker implantation are rare.
In conclusion, we report a case that developed takotsubo cardiomyopathy with an in-hospital cardiac arrest due to VF the day after a pacemaker implantation. The clinicians need to consider that a direct fatal complication can occur even after a general pacemaker implantation.
Conflict of interest
The authors have no conflicts of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgment
None.
References
- 1.Kirkfeldt R.E., Johansen J.B., Nohr E.A., Jørgensen O.D., Nielsen J.C. Complications after cardiac implantable electronic device implantations: an analysis of a complete, nationwide cohort in Denmark. Eur Heart J. 2014;35:1186–1194. doi: 10.1093/eurheartj/eht511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stiermaier T., Moeller C., Oehler K., Desch S., Graf T., Eitel C. Long-term excess mortality in takotsubo cardiomyopathy: predictors, causes and clinical consequences. Eur J Heart Fail. 2016;18:650–656. doi: 10.1002/ejhf.494. [DOI] [PubMed] [Google Scholar]
- 3.Kurisu S., Inoue I., Kawagoe T., Ishihara M., Shimatani Y., Hata T. Persistent left ventricular dysfunction in takotsubo cardiomyopathy after pacemaker implantation. Circ J. 2006;70:641–644. doi: 10.1253/circj.70.641. [DOI] [PubMed] [Google Scholar]
- 4.Postema P.G., Wiersma J.J., van der Bilt I.A., Dekkers P., van Bergen P.F. Takotsubo cardiomyopathy shortly following pacemaker implantation-case report and review of the literature. Neth Heart J. 2014;22:456–459. doi: 10.1007/s12471-012-0320-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bybee K.A., Kara T., Prasad A., Lerman A., Barsness G.W., Wright R.S. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med. 2004;141:858–865. doi: 10.7326/0003-4819-141-11-200412070-00010. [DOI] [PubMed] [Google Scholar]
- 6.Singh K., Carson K., Shah R., Sawhney G., Singh B., Parsaik A. Meta-analysis of clinical correlates of acute mortality in takotsubo cardiomyopathy. Am J Cardiol. 2014;113:1420–1428. doi: 10.1016/j.amjcard.2014.01.419. [DOI] [PubMed] [Google Scholar]
- 7.Templin C., Ghadri J.R., Diekmann J., Napp L.C., Bataiosu D.R., Jaguszewski M. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373:929–938. doi: 10.1056/NEJMoa1406761. [DOI] [PubMed] [Google Scholar]
- 8.Sharkey S.W., Windenburg D.C., Lesser J.R., Maron M.S., Hauser R.G., Lesser J.N. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol. 2010;55:333–341. doi: 10.1016/j.jacc.2009.08.057. [DOI] [PubMed] [Google Scholar]
- 9.Madias C., Fitzgibbons T.P., Alsheikh-Ali A.A., Bouchard J.L., Kalsmith B., Garlitski A.C. Acquired long QT syndrome from stress cardiomyopathy is associated with ventricular arrhythmias and torsades de pointes. Heart Rhythm. 2011;8:555–561. doi: 10.1016/j.hrthm.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 10.Pelliccia F., Parodi G., Greco C., Antoniucci D., Brenner R., Bossone E. Comorbidities frequency in takotsubo syndrome: an international collaborative systematic review including 1109 patients. Am J Med. 2015;128 doi: 10.1016/j.amjmed.2015.01.016. 654.e11–9. [DOI] [PubMed] [Google Scholar]