Abstract
Health care–acquired viral respiratory infections are common and cause increased patient morbidity and mortality. Respiratory syncytial virus and influenza virus are frequently transmitted in the hospital setting. Studies report decreased nosocomial transmission when aggressive infection control measures are implemented with more success using a multicomponent approach. Influenza vaccination of health care personnel has been shown to further decrease rates of transmission, thus mandatory vaccination is becoming more common. This article focuses on the epidemiology, transmission, and control of health care–associated respiratory viral infections.
Keywords: Influenza, Respiratory syncytial virus, Middle East respiratory syndrome, Nosocomial infection, Health care–acquired infection
Key points
-
•
Health care–acquired viral respiratory infections are common with increased patient morbidity and mortality.
-
•
Multicomponent infection-control measures consisting of education, hand washing, isolation, consistent use of personal protective equipment, cohorting patients, and cohort nursing reduces transmission of respiratory infections.
-
•
Health care worker influenza vaccination is recommended with mandatory vaccination policies becoming more common.
Introduction
Health care–associated viral respiratory infections result in increased patient morbidity, mortality and health care costs. Approximately 20% of patients with health care–associated pneumonia have viral respiratory infections, with an incidence that typically reflects the level of virus activity within the community.1, 2 This article focuses on the epidemiology, transmission, and control of health care–associated respiratory viral infections.
Respiratory syncytial virus
Epidemiology
Respiratory syncytial virus (RSV) is the most common cause of pneumonia and bronchiolitis in infants3 and is a common pathogen in older and high-risk adults.4 Rates of respiratory hospitalizations secondary to RSV infection are highest among infants, although patients 75 years and older have similar rates to children aged 1 to 4 years.5 Outbreaks of RSV have occurred in a variety of health care settings,6, 7, 8, 9 with the risk for nosocomial RSV infection varying by setting.10 Secondary attack rates of 19% to 45% have been reported among patients when limited or no infection control measures are implemented.6, 11, 12 Similarly, 34% to 56% of health care personnel (HCP) on infant wards may become infected.6, 11, 12 Most infected HCP are symptomatic, but asymptomatic shedding of RSV occurs in 15% to 20%.13 Although some symptomatic HCP may not come to work,13 symptomatic HCP working while ill (presenteeism) is a concern and is reported to be high (51%–75%) in some populations.14, 15
Transmission
Transmission of RSV occurs via inoculation of the eye and nose16 and by indirect inoculation of large droplets after touching contaminated fomites.17 RSV has been recovered on countertops for up to 6 hours, rubber gloves up to 2 hours, and on cloth gowns and hands for 15 to 60 minutes after contamination with infected nasal secretions.18 The duration of viral shedding among hospitalized infants averages 6.7 days but can be 21 days.19 Infants with lower respiratory disease and a compromised immune status have more prolonged shedding and shed greater quantities of virus.19
Prevention and Control
Currently, there is no specific treatment or licensed vaccine readily available for RSV; therefore, effective infection control measures are paramount for minimizing transmission. Studies evaluating the use of gowns and masks to prevent RSV transmission have shown mixed results. In a before-after design, the rate of health care–associated RSV infection among infants during the period that gowns and masks were routinely worn by HCP was not statistically different from the rate during the period when gowns and masks were not used (32% vs 41%).20 A second prospective, randomized study failed to show that the use of gowns and masks prevented respiratory illness among HCP.21 One factor in the ineffectiveness of gowns and masks in these studies may have been poor personal protective equipment adherence among HCP. In another study, as compliance with use of gowns and gloves increased from 39% to 95%, the incidence of health care–associated RSV decreased from 6.4 to 3.1 per 1000 patient-days.22 Some have expressed concerns that the use of gowns and gloves may facilitate transmission by serving as fomites, particularly given the prolonged survival of RSV on rubber gloves compared with skin.18 One study of seven Canadian pediatric hospitals actually noted an increased risk of transmission with the use of gowns, believed to be caused by decreased adherence of other infection control measures related to the overuse of gowns.23
Another explanation for the lack of benefit from gowns and masks in RSV transmission may be from failure to protect the eye as a portal of entry. Two studies suggested that wearing eye protection is beneficial.24, 25 Other studies have evaluated the effectiveness of a variety of measures in combination to prevent health care–associated RSV infection. A combination of cohort nursing and routine use of gowns and gloves significantly reduced RSV transmission compared with either intervention alone.26 An intervention consisting of education, hand washing, consistent use of gowns and gloves, isolation or cohorting patients, restriction of visitors, and cohort nursing was associated with a 39% reduction in health care–associated RSV.27 Transmission of RSV in a special care nursery ended after instituting cohort nursing; active surveillance; patient cohorting; a strict policy limiting visitation in the winter; construction of segregate areas; and the use of gown, gloves, and masks with all patient contact.28 A similar intervention that included isolation or cohorting infected infants, hand washing, use of gowns, cohort nursing, isolation of asymptomatic high-risk infants, and limitation of visitors seemed to be effective in reducing transmission among infants from 45% in the previous year to 19%.11 In general, multicomponent infection control measures have shown significantly lower rates of nosocomial RSV infections, although effectiveness of specific components remains unclear.10
In addition to standard precautions, the Centers for Disease Control and Prevention (CDC) recommends contact precautions for infected children and immunocompromised adults to prevent health care–associated RSV (Tables 1 and 2 ).29 Some institutions use contact precautions for all RSV-infected patients. Contact precautions should continue for the duration of illness but may be extended for immunocompromised patients because of prolonged viral shedding. Additional interventions to prevent health care–associated RSV include cohort nursing and the exclusion from the hospital of ill HCP and visitors. Rapid RSV antigen screening has also been proposed to prevent health care–associated RSV. Rapid screening of symptomatic children on admission resulted in a greater than 50% decrease in the proportion of RSV infections that were health care–associated.30 Screening of all pediatric admissions, regardless of the presence of symptoms, with cohorting of infected patients reduced the incidence of health care–associated RSV from 7.2 to less than 1 per 1000 patient-days.31 However, rapid antigen detection is an insensitive method for diagnosing RSV infection in adults.32
Table 1.
Precautions for preventing transmission of respiratory infections
| Precautions | Component | Recommendation |
|---|---|---|
| Standard | Hand hygiene |
|
| Respiratory hygiene |
|
|
| Gloves | Wear when contact with respiratory secretions could occur | |
| Gowns | Wear during procedures and activities when contact of clothing or exposed skin with respiratory secretions is anticipated | |
| Masks and eye protection | Wear during procedures and activities likely to generate splashes or sprays of respiratory secretions | |
| Contacta | Patient placement | Place patient in a single-patient room, if possible, or cohort with other patients infected with the same organism Limit patient movement to medically necessary purposes |
| Gloves and gowns | Wear on room entry whenever contact is likely with the patient, patient’s respiratory secretions, or potentially contaminated items in the patient’s vicinity, including equipment and environmental surfaces | |
| Masks and eye protection | As per Standard Precautions | |
| Dropleta | Patient placement | Place patient in a single-patient room, if possible, or cohort with other patients infected with the same organism Limit patient movement to medically necessary purposes, and patients should wear a mask and follow respiratory hygiene during transport |
| Gloves, gowns, and eye protection | As per Standard Precautions | |
| Masks | Wear a surgical mask on room entry if close contact (eg, <3 ft) with the patient is anticipated | |
| Airbornea | Patient placement | Place infected patients in a single-patient airborne infection isolation roomb Limit patient movement to medically necessary purposes, and patients should wear a mask and follow respiratory hygiene during transport |
| Gloves, gowns, and eye protection | As per Standard Precautions | |
| Masks | Wear a fit-tested N95 respirator before room entry |
Contact, droplet, and airborne precautions include hand hygiene and respiratory hygiene as per Standard Precautions.
Airborne infection isolation room consists of negative pressure relative to the surrounding area, 6 to 12 air changes per hour, and air is exhausted directly to the outside or recirculated through high-efficiency particulate air filtration before return.
From Siegel JD, Rhinehart E, Jackson M, et al; Health Care Infection Control Practices Advisory C. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control 2007;35:S65–164.
Table 2.
Infection prevention recommendations for viral respiratory pathogens
| Common Measures for Reducing Transmission in the Health Care Setting |
|---|
| Hand hygiene |
| Respiratory hygiene/cough etiquette |
| Standard precautions |
| Restrict ill visitorsa |
| Restrict ill personnel (prevent “presenteeism”) |
| Cohort nursing |
| Prompt diagnosis of respiratory infections among patients by rapid diagnostic testsb |
| Restrict elective admissions of patients during outbreaks in the community and/or facility |
| Surveillance for an increase in activity of viral infections within the community |
| Measures for Reducing Transmission of Specific Pathogens in the Health Care Setting | ||||||
|---|---|---|---|---|---|---|
| Intervention | RSV | Adenovirus | Parainfluenza Virus | Influenza |
Novel Coronavirus | |
| Seasonal | Novel | |||||
| Precautions | ||||||
| Contact | ● | ● | ● | ● | ● | |
| Droplet | ● | ● | ||||
| Airborne | ●c | ● | ● | |||
| Eye protection | ● | ● | ||||
| Vaccination of personnel | ● | |||||
| Chemoprophylaxis | ○d | ○e | ○ | |||
Closed circles denote recommended measures. Open circles denote measures recommended in certain circumstances.
Institutions may restrict only young children and/or screen all visitors for illness by using a trained health care worker to assess for signs and symptoms or by using an educational patient information list to advise ill visitors.
To control outbreaks, institutions may perform preadmission screening of patients for infection.
The Centers for Disease Control and Prevention recommends an N95 respirator for HCP performing aerosol-generating procedures.
In addition to other infection control measures, palivizumab prophylaxis of high-risk infants has been used to control outbreaks in the neonatal intensive care unit.
During a facility outbreak of influenza, administer antiviral chemoprophylaxis to all patients in the involved unit, regardless of vaccination status, and to unvaccinated HCP working in the involved unit. If feasible, administer facility-wide chemoprophylaxis for all residents in long-term care facilities. Chemoprophylaxis may also be administered to personnel when the outbreak strain is not well-matched by the vaccine.
Palivizumab is a humanized mouse IgG monoclonal antibody that is effective in preventing hospitalizations caused by RSV infections,33 and the use of palivizumab as prophylaxis for susceptible infants to control outbreaks in neonatal intensive care units has been described.7, 34 The American Academy of Pediatrics recommends that palivizumab be administered to the following groups of patients: infants younger than 12 months of age and born before 29 weeks gestation at the beginning of RSV season, preterm infants with chronic lung disease of prematurity who are born before 32 weeks gestation during their first year of life, and infants younger than 12 months of age with hemodynamically significant congestive heart disease.35 There are currently no guidelines for more generalized use in controlling outbreaks of health care–associated RSV infections.
Seasonal influenza
Epidemiology
Influenza infects approximately 5% to 20% of the United States population annually, resulting in 226,000 hospitalizations and 36,000 deaths.36 Transmission of influenza has been reported in a variety of health care settings, and HCP are often implicated as index cases for nosocomial outbreaks.36 HCP are at increased risk of acquiring influenza because of exposure to infection in the health care and community settings,37 and they often fail to recognize they are infected.38 Asymptomatic and mildly symptomatic HCP may also shed influenza virus, potentially transmitting infection to patients or other personnel, and ill HCP often work while ill.15, 39
Secondary attack rates of 50% have been reported among HCP and patients,37 resulting in HCP absenteeism and subsequent disruption of patient care. A 2003 to 2004 survey of 221 US hospital epidemiologists indicated that a substantial portion of hospitals experienced staffing shortages (34%), bed shortages (28%), intensive care unit bed shortages (43%), and diversion of patients (9%) during peak influenza activity.40
Transmission
The typical incubation period for influenza in healthy volunteers is 1 to 3 days.41 Viral shedding begins before the appearance of symptoms and within the first 24 hours following inoculation, peaks on the second day following inoculation, and usually declines rapidly thereafter.42, 43, 44 Virus is typically no longer detectable after 6 to 10 days after inoculation. Prolonged viral shedding has been documented in children45 and immunocompromised adults.46 Transmission via contact with fomites has been suggested by the recovery of influenza on porous surfaces (eg, cloth, paper, tissues) for 8 to 12 hours and nonporous surfaces (eg, steel, plastic) for 24 to 48 hours following inoculation47 and by the recovery from 23% to 53% of inanimate objects present in day-care centers during influenza season.48
Several studies have suggested that influenza may be transmitted by droplet nuclei (<5 μm) or small particle aerosols between infected and noninfected animals. Transmission of influenza occurred among ferrets in wire-mesh cages separated by at least 5 ft despite susceptible ferrets being placed at a higher elevation.49 To control for air currents in the laboratory, additional experiments were conducted using cages connected by an S- or U-shaped duct. Infection occurred at low air speeds using both types of ducts, which prevented transmission of coarse droplets. Mouse experiments provided similar results on the effect of ventilation and physical separation. Twenty-four hours after their exposure to an aerosol spray of influenza, infected mice were placed in the same cage as noninfected mice in a closed chamber for 24 hours.50 Transmission was not affected by physical separation with a wire screen; however, transmission was inversely correlated with airflow. Because air currents rather than separation affected transmission, the authors concluded that droplet nuclei are the principal means of influenza transmission. Recovery of infectious particles less than 10 μm from air surrounding the infected mice provided additional support for droplet nuclei transmission.51
Studies have also examined the ability to infect humans with influenza via experimental aerosol. Twenty-three healthy adult men were exposed to various doses of influenza via aerosolized particles of 1 to 3 μm.52 Half of the men with absent titers before inoculation became infected with a dose that was 40- to 500-fold lower than that required to cause disease when administered by nasal drops.41 To a lesser extent, another study similarly demonstrated that smaller doses were required to cause illness among normal volunteers when administered as an aerosol rather than nasal drops.53 Although the lower respiratory tract seems to be a more efficient route of infection than the upper respiratory tract, the proportion of natural influenza infections acquired by aerosols remains unknown. Several studies have demonstrated that the size of particles produced during various activities is within the range where deposition in the lower respiratory tract can occur.54, 55, 56
Two commonly cited epidemiologic studies have suggested influenza may be spread by droplet nuclei. During the 1957 to 1958 influenza outbreak, 150 patients with tuberculosis were housed in a building at a Veterans Administration Hospital with upper air ultraviolet radiation.57 An additional 250 patients with tuberculosis were housed in a separate building with nonradiated air. Serologic evidence of influenza infection was found in only 2% of patients in the radiated building compared with 19% of patients in the nonradiated building and 18% of personnel. Radiated and nonradiated patients were equally exposed to personnel, and all persons were assumed susceptible because the influenza strain was new and antigenically distinct from previous strains. Because upper air radiation would not disinfect large respiratory droplets, transmission of influenza via droplet nuclei was proposed. However, the possibility that influenza was not introduced into the radiated building cannot be excluded. The second observation occurred in 1977 when 54 persons aboard a commercial airliner were grounded for 3 hours during which time the ventilation system was inoperative.58 A single index case became ill within 15 minutes after boarding. Within 72 hours, 72% of the remaining passengers developed influenza-like illness. The high illness rates and epidemic curve suggest airborne transmission from a single point source. However, passengers were allowed to move about the plane freely and the index patient sat immediately adjacent to the lavatory and galley areas, so droplet and contact transmission cannot be excluded.
Conversely, other observations have suggested large respiratory droplets (>10 μm) play a more significant role in transmission than droplet nuclei. During the 1958 to 1959 pandemic, a single patient with influenza was hospitalized in a general medical ward before the appearance of influenza in the community.59 Sixteen patients and staff became ill over the next 3 days. The epidemic curve suggested an initial source with subsequent person-to-person spread. Furthermore, no patients in single rooms became infected as would have been expected of airborne transmission. Similarly, most health care–associated influenza cases at the University of Rochester Medical Center occurred in patients housed in the same room adjacent to case patients.60 Patients across the hall from infected patients were less likely to acquire influenza despite open doors and nonuse of airborne infection isolation rooms. Salgado and colleagues37 reported health care–associated influenza was rare, although most cases were placed in private, positive-pressure rooms. Finally, the lack of reports of explosive clusters of health care–associated influenza during annual influenza seasons supports the lack of widespread airborne transmission in health care settings. Although transmission by droplet nuclei may play a role in certain conditions, large respiratory droplets are likely the primary mode of transmission within a health care setting, an environment where frequent air changes and exhaust ventilation occurs.
Prevention and Control
In addition to standard precautions, the CDC recommends implementation of droplet precautions to prevent health care–associated influenza (see Tables 1 and 2).2, 29 Droplet precautions should continue for 7 days after illness onset or until 24 hours after the resolution of fever and respiratory symptoms, whichever is longer, but may be extended for immunocompromised patients because of prolonged viral shedding. A randomized controlled trial demonstrated that masks were noninferior to respirators in protecting HCP from influenza.61 Although a second randomized controlled trial initially reported a difference between respirators and surgical masks, adjustment for the clustered randomization and multiple outcomes yielded no statistical significance between the two types of respiratory protection.62 If patients with influenza must undergo aerosol-generating procedures, such as bronchoscopy, sputum induction, intubation/extubation, cardiopulmonary resuscitation, or autopsy, HCP should wear respiratory protection equivalent to a fitted N95 filtering respirator mask and perform these procedures in a negative pressure room, if feasible.63
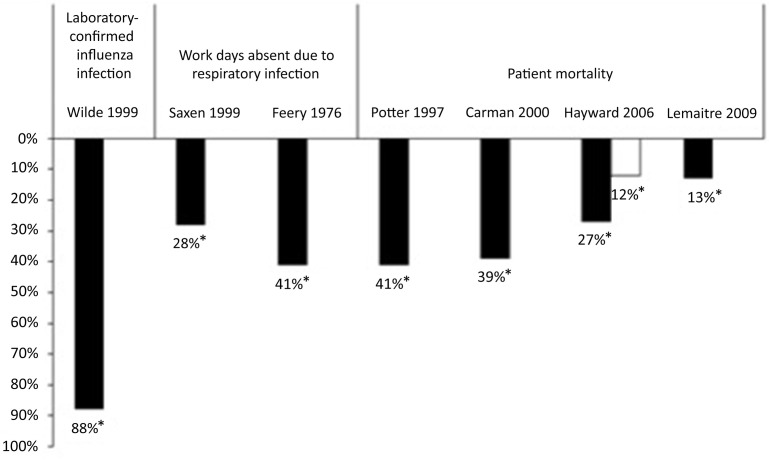
In a susceptible-exposed-infected-recovered model, vaccination of HCP was the second most effective strategy in preventing influenza transmission in the hospital by reducing number of cases 6% to 19% only behind hand washing with an 11% to 27% case reduction.64 Vaccination is recommended for HCP for several reasons.65 First, vaccination has been shown to be 88% effective in preventing laboratory-confirmed influenza in HCP (Fig. 1 ).66 Second, HCP absenteeism can stress the health system during influenza epidemics, and influenza vaccination resulted in a statistically significant 28% to 41% decrease in work-days lost because of respiratory illness (see Fig. 1).67, 68 Third, HCP have frequent contact with patients at high risk for complications from influenza and may transmit influenza to susceptible patients, resulting in increased patient morbidity and mortality.69 Improved HCP vaccination rates have been linked with decreased health care–associated influenza among patients and personnel.70, 71 Three cluster-randomized trials demonstrated that HCP vaccination was associated with a statistically significant decrease in mortality among nursing home patients (see Fig. 1).72, 73, 74 Similarly, HCP vaccination led to a nonsignificant 13% decrease in patient mortality during a mild influenza season in a fourth cluster-randomized trial.75 However, the study was likely underpowered, and a multivariate analysis showed that HCP vaccination was a significant independent predictor of patient mortality (odds ratio, 0.80; 95% confidence interval, 0.67–0.97). Despite recommendations for vaccination and evidence supporting its use, HCP vaccination rates have been traditionally low (45% during the 2007–2008 season).76 Barriers to vaccination include fear of needles and vaccine side effects, inconvenience, failure of the employer to pay for the vaccine, doubt about the risk of influenza, perceived lack of vaccine effectiveness, and failure to recognize the role of HCP in transmission of influenza to patients.36, 77 Strategies for improving acceptance of vaccine by HCP have been published, and fortunately vaccination rates among HCP have increased in recent years.36, 77 Many health care organizations have now adopted a policy requiring annual influenza vaccination of all HCP as a condition of employment because of the patient safety ramifications of an unvaccinated workforce.77 In 2013, multiple professional societies and safety advocacy organizations endorsed policies for mandatory influenza vaccination for HCP (Box 1 ). In 2015, the National Patient Safety Foundation Board advocated for two “must do’s” for HCP to ensure patient safety: hand washing and HCP influenza vaccination.78 During the 2014 to 2015 influenza season, HCP vaccination rate was 44% in clinical settings where influenza vaccines were not required, promoted, or offered on site, whereas HCP vaccination rate was 96% in clinical settings where vaccination was required.79
Fig. 1.
Percent reduction in noted outcomes in HCP receiving influenza vaccination. Values marked by an asterisk were statistically significant (P<.05) compared with an unvaccinated control group. Patient mortality data from Hayward and colleagues74 are from two different seasons. A multivariate analysis of the study by Lemaitre and coworkers75 showed that HCP vaccination was a significant independent predictor of patient mortality.
(Adapted from Talbot TR, Bradley SE, Cosgrove SE, et al. Influenza vaccination of healthcare workers and vaccine allocation for healthcare workers during vaccine shortages. Infect Control Hosp Epidemiol 2005;26:882–90.)
Box 1. Professional societies and safety advocacy organisms that recommend mandatory HCP influenza immunization.
American Academy of Family Physicians (AAFP)
American Academy of Pediatrics (AAP)
American College of Physicians (ACP)
American Hospital Association (AHA)
American Medical Directors Association (AMDA)
American Nurses Association (ANA)
American Pharmacists Association
American Public Health Association (APHA)
Association for Professionals in Infection Control and Epidemiology (APIC)
Infectious Diseases Society of America (IDSA)
National Association of County & City Health Officials (NACCHO)
National Business Group on Health
National Foundation for Infectious Diseases (NFID)
National Patient Safety Foundation (NPSF)
Society for Healthcare Epidemiology of America (SHEA)
United States Department of Defense
Data from observational studies and controlled trials support recommendations to provide antiviral chemoprophylaxis to residents in long-term care facilities, regardless of vaccination status, during an institutional influenza outbreak.80 In this setting, chemoprophylaxis should be continued for 14 days or for 7 to 10 days after the onset of symptoms in the last person infected, whichever is longer.80, 81 Effectiveness of employee chemoprophylaxis in the acute care setting is unclear. Chemoprophylaxis may also be considered for unvaccinated HCP or when the vaccine is likely to be ineffective because of strain mismatch.81 Chemoprophylaxis for hospitalized patients who were close contacts of hospitalized influenza-infected patients showed benefit in reducing transmission.82
In addition to vaccination and antiviral chemoprophylaxis, interventions to prevent health care–associated influenza include early identification of suspected patients with source control (ie, wearing a mask), cohort nursing, exclusion of ill HCP and visitors, and rapid diagnostic testing of symptomatic children. Similar to RSV, rapid antigen detection is an insensitive method for diagnosing influenza infection in most adults.83
Novel pandemic influenza
Novel pandemic influenza results when an emerging strain to which the population has little or no immunity achieves the ability to spread easily between humans, resulting in rapid spread across several continents. A novel virus emerges as a result of reassortment of human influenza genes with those of avian or swine strains. Over the past century there have been four major pandemics: (1) 1918 to 1919 “Spanish” influenza (H1N1), (2) 1957 to 1958 “Asian” influenza (H2N2), (3) 1968 to 1969 “Hong Kong” influenza (H3N2), and (4) 2009 H1N1 influenza A.
A highly pathogenic avian influenza A (H5N1) virus was first reported to cause human infections in 1997 in China.84 However, no other human infections were reported until the virus reemerged in Hong Kong in 2003. Since that time, it has caused several hundred infections worldwide with a case-fatality ratio of 60%.85 Several family clusters of disease suggest probable human-to-human transmission.86, 87 A study of the 1997 cluster indicated that 3.7% of exposed HCP had serologic evidence of infection88; however, more recent serologic surveys have not identified any cases among exposed personnel despite lack of appropriate infection control precautions.89, 90 The inefficient spread among humans may be explained by recent evidence showing a preferential binding of the H5N1 virus in the lower respiratory tract of humans.91 The United States government maintains a stockpile of H5N1 vaccine. Human infection with avian influenza (H7N9) was first reported 2013 in China and has caused severe respiratory illness with 307 deaths from a total of 786 cases (39.1% fatality rate) as of May 2016.92 Although most of these 786 infections are from zoonotic exposure (typically to poultry), human-to-human transmission rarely occurs. These reports are health care–associated infecting HCP and nearby hospitalized patients.93, 94 Sustained human-to-human spread has not been reported.
The CDC has issued interim guidelines for infection control for patients with suspected novel influenza A infection associated with severe disease, which would include patients with either H5N1 or H7N9. Although there may be some differences between seasonal and pandemic influenza strains, many of the basic infection control recommendations for prevention of health care–associated seasonal influenza also apply for pandemic strains. Avian influenza should be suspected in patients presenting with a severe respiratory illness within 10 days of travel to a country with avian influenza activity.95 Contact and airborne precautions should be used for patients with suspected avian influenza (see Tables 1 and 2). Additionally, all HCP should wear eye protection when entering the patient’s room. Transmission-based precautions for avian influenza should be continued for 14 days after onset of illness. Antiviral chemoprophylaxis for 7 to 10 days should also be considered for HCP with unprotected exposures.96 For novel respiratory viruses causing severe illness, aggressive infection control measures are implemented until mechanism and risk of transmission is better understood, at which time guidelines may be altered if needed.
Novel human coronaviruses
Epidemiology
Human coronaviruses (CoV) are enveloped positive sense single-stranded RNA viruses historically known to cause mild respiratory infections. In 2002 a novel CoV, severe acute respiratory syndrome (SARS)–CoV, was identified from patients with severe respiratory illness resulting in 8096 cases globally and 774 deaths (9.6% mortality rate). There have been no additional cases reported since 2003.97 Middle East respiratory syndrome (MERS), another novel CoV, was identified in the Arabian Peninsula in 2012 from a man with severe pneumonia resulting in death.98 Since that time, 1733 cases in 27 countries have been reported with 628 deaths (36.2% mortality rate) as of May 2016.99 Early in the epidemiologic description of MERS, it was noted that 91.3% of infections in Eastern Saudi Arabia were acquired from person-to-person spread in health care facilities.100 There have been multiple MERS nosocomial outbreaks reported in the literature100, 101, 102 and 13% to 70% of nosocomial MERS cases are infected HCP.102, 103
Transmission
MERS-CoV has a low human-to-human transmission potential. However, most infections occur in the hospital setting where severely ill patients with high viral loads and increased virus shedding, who typically undergo aerosol-generating procedures, come into close contact with HCP, other patients, and visitors. Inadequate or inconsistent infection control measures have been cited as factors in MERS-CoV transmission during nosocomial outbreaks.100, 101, 102, 104, 105 Transmission of MERS-CoV occurs through environmental contamination by large droplets, contact, and aerosols. A study of MERS-CoV environmental contamination from four hospitalized patients in South Korea identified MERS-CoV RNA on sheets, bedrails, intravenous poles, devices, air ventilation equipment, and in anterooms 5 days after the last patient specimen was found to be positive, suggesting wide contamination of many surfaces.106
Prevention and Control
Hospitalized patients with MERS-CoV should be placed in contact and airborne precautions with the use of eye protection.107 The duration of infection control precautions is not overtly stated, although factors to consider include presence of symptoms, laboratory information, and other conditions that require further precaution.107 Of note, identification of viable MERS-CoV from viral culture of a respiratory specimen has been reported up to 25 days following symptom onset.106 When exceptional infection control practices are implemented, nosocomial transmission of MERS-CoV can be prevented.108
Adenovirus
Health care–associated outbreaks of respiratory tract infections caused by adenovirus have been reported from various settings.109, 110, 111 Attack rates among patients have ranged from 15% to 56%.109, 110 HCP are often infected, and many continued to provide patient care while ill.112 Similar to influenza, adenovirus is transmitted through large respiratory droplets. Transmission also occurs via self-inoculation after contact with contaminated fomites because adenovirus can survive on nonporous environmental surfaces for up to 49 days.113 In addition to standard precautions, the CDC recommends contact and droplet precautions to prevent health care–associated adenovirus infection (see Tables 1 and 2).2, 29
Parainfluenza virus
Transmission of parainfluenza has been documented in pediatric wards,114 neonatal nurseries,115 and adult transplant units.116 Transmission of parainfluenza is similar to RSV and primarily occurs by direct person-to-person contact. Parainfluenza can survive up to 4 hours on porous surfaces and up to 10 hours on nonporous surfaces.117 However, viral recovery from hands falls rapidly, with only 5% detected after 10 minutes.118 The CDC recommends contact precautions for the prevention of health care–associated parainfluenza infection (see Tables 1 and 2).2, 29
Summary
Transmission of viral respiratory infections occurs in a variety of health care settings, resulting in increased patient morbidity and health care costs. Transmission may occur via aerosol, large respiratory droplets, or self-inoculation after touching contaminated fomites. Different viruses have different modes of transmission, and prevention of transmission requires early recognition of symptomatic patients and prompt institution of appropriate transmission-based precautions, in addition to adherence to basic infection control practices, such as hand hygiene. In addition to administrative and environmental controls, influenza vaccination of HCP is an effective means of prevention of health care–associated influenza infection.
Footnotes
Disclosure Statement: R.K. Dare has no disclosures; T.R. Talbot reports that his spouse received research support from Sanofi Pasteur, MedImmune, and Gilead and has served as a consultant for Novartis.
References
- 1.Hall C.B. Nosocomial viral respiratory infections: perennial weeds on pediatric wards. Am J Med. 1981;70:670–676. doi: 10.1016/0002-9343(81)90594-5. [DOI] [PubMed] [Google Scholar]
- 2.Tablan O.C., Anderson L.J., Besser R. Guidelines for preventing health-care-associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep. 2004;53:1–36. [PubMed] [Google Scholar]
- 3.Shay D.K., Holman R.C., Newman R.D. Bronchiolitis-associated hospitalizations among US children, 1980-1996. JAMA. 1999;282:1440–1446. doi: 10.1001/jama.282.15.1440. [DOI] [PubMed] [Google Scholar]
- 4.Falsey A.R., Hennessey P.A., Formica M.A. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med. 2005;352:1749–1759. doi: 10.1056/NEJMoa043951. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein E., Greene S.K., Olson D.R. Estimating the hospitalization burden associated with influenza and respiratory syncytial virus in New York City, 2003-2011. Influenza Other Respir Viruses. 2015;9:225–233. doi: 10.1111/irv.12325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall C.B., Douglas R.G., Jr., Geiman J.M. Nosocomial respiratory syncytial virus infections. N Engl J Med. 1975;293:1343–1346. doi: 10.1056/NEJM197512252932604. [DOI] [PubMed] [Google Scholar]
- 7.Halasa N.B., Williams J.V., Wilson G.J. Medical and economic impact of a respiratory syncytial virus outbreak in a neonatal intensive care unit. Pediatr Infect Dis J. 2005;24:1040–1044. doi: 10.1097/01.inf.0000190027.59795.ac. [DOI] [PubMed] [Google Scholar]
- 8.Englund J.A., Anderson L.J., Rhame F.S. Nosocomial transmission of respiratory syncytial virus in immunocompromised adults. J Clin Microbiol. 1991;29:115–119. doi: 10.1128/jcm.29.1.115-119.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mathur U., Bentley D.W., Hall C.B. Concurrent respiratory syncytial virus and influenza A infections in the institutionalized elderly and chronically ill. Ann Intern Med. 1980;93:49–52. doi: 10.7326/0003-4819-93-1-49. [DOI] [PubMed] [Google Scholar]
- 10.French C.E., McKenzie B.C., Coope C. Risk of nosocomial respiratory syncytial virus infection and effectiveness of control measures to prevent transmission events: a systematic review. Influenza Other Respir Viruses. 2016;10(4):268–290. doi: 10.1111/irv.12379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall C.B., Geiman J.M., Douglas R.G., Jr. Control of nosocomial respiratory syncytial viral infections. Pediatrics. 1978;62:728–732. [PubMed] [Google Scholar]
- 12.Hall C.B., Kopelman A.E., Douglas R.G., Jr. Neonatal respiratory syncytial virus infection. N Engl J Med. 1979;300:393–396. doi: 10.1056/NEJM197902223000803. [DOI] [PubMed] [Google Scholar]
- 13.Hall C.B. Nosocomial respiratory syncytial virus infections: the “Cold War” has not ended. Clin Infect Dis. 2000;31:590–596. doi: 10.1086/313960. [DOI] [PubMed] [Google Scholar]
- 14.Jena A.B., Baldwin D.C., Jr., Daugherty S.R. Presenteeism among resident physicians. JAMA. 2010;304:1166–1168. doi: 10.1001/jama.2010.1315. [DOI] [PubMed] [Google Scholar]
- 15.Jena A.B., Meltzer D.O., Press V.G. Why physicians work when sick. Arch Intern Med. 2012;172:1107–1108. doi: 10.1001/archinternmed.2012.1998. [DOI] [PubMed] [Google Scholar]
- 16.Hall C.B., Douglas R.G., Jr., Schnabel K.C. Infectivity of respiratory syncytial virus by various routes of inoculation. Infect Immun. 1981;33:779–783. doi: 10.1128/iai.33.3.779-783.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hall C.B., Douglas R.G., Jr. Modes of transmission of respiratory syncytial virus. J Pediatr. 1981;99:100–103. doi: 10.1016/s0022-3476(81)80969-9. [DOI] [PubMed] [Google Scholar]
- 18.Hall C.B., Douglas R.G., Jr., Geiman J.M. Possible transmission by fomites of respiratory syncytial virus. J Infect Dis. 1980;141:98–102. doi: 10.1093/infdis/141.1.98. [DOI] [PubMed] [Google Scholar]
- 19.Hall C.B., Douglas R.G., Jr., Geiman J.M. Respiratory syncytial virus infections in infants: quantitation and duration of shedding. J Pediatr. 1976;89:11–15. doi: 10.1016/s0022-3476(76)80918-3. [DOI] [PubMed] [Google Scholar]
- 20.Hall C.B., Douglas R.G., Jr. Nosocomial respiratory syncytial viral infections. Should gowns and masks be used? Am J Dis Child. 1981;135:512–515. doi: 10.1001/archpedi.1981.02130300012006. [DOI] [PubMed] [Google Scholar]
- 21.Murphy D., Todd J.K., Chao R.K. The use of gowns and masks to control respiratory illness in pediatric hospital personnel. J Pediatr. 1981;99:746–750. doi: 10.1016/S0022-3476(81)80401-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leclair J.M., Freeman J., Sullivan B.F. Prevention of nosocomial respiratory syncytial virus infections through compliance with glove and gown isolation precautions. N Engl J Med. 1987;317:329–334. doi: 10.1056/NEJM198708063170601. [DOI] [PubMed] [Google Scholar]
- 23.Langley J.M., LeBlanc J.C., Wang E.E. Nosocomial respiratory syncytial virus infection in Canadian pediatric hospitals: a pediatric investigators collaborative network on infections in Canada Study. Pediatrics. 1997;100:943–946. doi: 10.1542/peds.100.6.943. [DOI] [PubMed] [Google Scholar]
- 24.Gala C.L., Hall C.B., Schnabel K.C. The use of eye-nose goggles to control nosocomial respiratory syncytial virus infection. JAMA. 1986;256:2706–2708. [PubMed] [Google Scholar]
- 25.Agah R., Cherry J.D., Garakian A.J. Respiratory syncytial virus (RSV) infection rate in personnel caring for children with RSV infections. Routine isolation procedure vs routine procedure supplemented by use of masks and goggles. Am J Dis Child. 1987;141:695–697. doi: 10.1001/archpedi.1987.04460060111049. [DOI] [PubMed] [Google Scholar]
- 26.Madge P., Paton J.Y., McColl J.H. Prospective controlled study of four infection-control procedures to prevent nosocomial infection with respiratory syncytial virus. Lancet. 1992;340:1079–1083. doi: 10.1016/0140-6736(92)93088-5. [DOI] [PubMed] [Google Scholar]
- 27.Macartney K.K., Gorelick M.H., Manning M.L. Nosocomial respiratory syncytial virus infections: the cost-effectiveness and cost-benefit of infection control. Pediatrics. 2000;106:520–526. doi: 10.1542/peds.106.3.520. [DOI] [PubMed] [Google Scholar]
- 28.Snydman D.R., Greer C., Meissner H.C. Prevention of nosocomial transmission of respiratory syncytial virus in a newborn nursery. Infect Control Hosp Epidemiol. 1988;9:105–108. doi: 10.1086/645804. [DOI] [PubMed] [Google Scholar]
- 29.Siegel J.D., Rhinehart E., Jackson M., Health care infection control practices advisory C 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35:S65–S164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karanfil L.V., Conlon M., Lykens K. Reducing the rate of nosocomially transmitted respiratory syncytial virus. Am J Infect Control. 1999;27:91–96. doi: 10.1016/s0196-6553(99)70087-8. [DOI] [PubMed] [Google Scholar]
- 31.Krasinski K., LaCouture R., Holzman R.S. Screening for respiratory syncytial virus and assignment to a cohort at admission to reduce nosocomial transmission. J Pediatr. 1990;116:894–898. doi: 10.1016/s0022-3476(05)80646-8. [DOI] [PubMed] [Google Scholar]
- 32.Chartrand C., Tremblay N., Renaud C. Diagnostic accuracy of rapid antigen detection tests for respiratory syncytial virus infection: systematic review and meta-analysis. J Clin Microbiol. 2015;53:3738–3749. doi: 10.1128/JCM.01816-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Feltes T.F., Cabalka A.K., Meissner H.C. Palivizumab prophylaxis reduces hospitalization due to respiratory syncytial virus in young children with hemodynamically significant congenital heart disease. J Pediatr. 2003;143:532–540. doi: 10.1067/s0022-3476(03)00454-2. [DOI] [PubMed] [Google Scholar]
- 34.Kurz H., Herbich K., Janata O. Experience with the use of palivizumab together with infection control measures to prevent respiratory syncytial virus outbreaks in neonatal intensive care units. J Hosp Infect. 2008;70:246–252. doi: 10.1016/j.jhin.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 35.American Academy of Pediatrics Committee on Infectious D, American Academy of Pediatrics Bronchiolitis Guidelines C Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics. 2014;134:415–420. doi: 10.1542/peds.2014-1665. [DOI] [PubMed] [Google Scholar]
- 36.Talbot T.R., Bradley S.E., Cosgrove S.E. Influenza vaccination of healthcare workers and vaccine allocation for healthcare workers during vaccine shortages. Infect Control Hosp Epidemiol. 2005;26:882–890. doi: 10.1086/502512. [DOI] [PubMed] [Google Scholar]
- 37.Salgado C.D., Farr B.M., Hall K.K. Influenza in the acute hospital setting. Lancet Infect Dis. 2002;2:145–155. doi: 10.1016/s1473-3099(02)00221-9. [DOI] [PubMed] [Google Scholar]
- 38.Elder A.G., O'Donnell B., McCruden E.A. Incidence and recall of influenza in a cohort of Glasgow healthcare workers during the 1993-4 epidemic: results of serum testing and questionnaire. BMJ. 1996;313:1241–1242. doi: 10.1136/bmj.313.7067.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Widera E., Chang A., Chen H.L. Presenteeism: a public health hazard. J Gen Intern Med. 2010;25:1244–1247. doi: 10.1007/s11606-010-1422-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Poland G.A., Tosh P., Jacobson R.M. Requiring influenza vaccination for health care workers: seven truths we must accept. Vaccine. 2005;23:2251–2255. doi: 10.1016/j.vaccine.2005.01.043. [DOI] [PubMed] [Google Scholar]
- 41.Douglas R.G., Jr. Influenza in man. In: Kilbourne E.D., editor. The influenza viruses and influenza. Academic Press; New York: 1975. pp. 395–447. [Google Scholar]
- 42.Murphy B.R., Chalhub E.G., Nusinoff S.R. Temperature-sensitive mutants of influenza virus. III. Further characterization of the ts-1[E] influenza A recombinant (H3N2) virus in man. J Infect Dis. 1973;128:479–487. doi: 10.1093/infdis/128.4.479. [DOI] [PubMed] [Google Scholar]
- 43.Hayden F.G., Fritz R., Lobo M.C. Local and systemic cytokine responses during experimental human influenza A virus infection. Relation to symptom formation and host defense. J Clin Invest. 1998;101:643–649. doi: 10.1172/JCI1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ip D.K., Lau L.L., Chan K.H. The dynamic relationship between clinical symptomatology and viral shedding in naturally acquired seasonal and pandemic influenza virus infections. Clin Infect Dis. 2016;62:431–437. doi: 10.1093/cid/civ909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hall C.B., Douglas R.G., Jr. Nosocomial influenza infection as a cause of intercurrent fevers in infants. Pediatrics. 1975;55:673–677. [PubMed] [Google Scholar]
- 46.Englund J.A., Champlin R.E., Wyde P.R. Common emergence of amantadine- and rimantadine-resistant influenza A viruses in symptomatic immunocompromised adults. Clin Infect Dis. 1998;26:1418–1424. doi: 10.1086/516358. [DOI] [PubMed] [Google Scholar]
- 47.Bean B., Moore B.M., Sterner B. Survival of influenza viruses on environmental surfaces. J Infect Dis. 1982;146:47–51. doi: 10.1093/infdis/146.1.47. [DOI] [PubMed] [Google Scholar]
- 48.Boone S.A., Gerba C.P. The occurrence of influenza A virus on household and day care center fomites. J Infect. 2005;51:103–109. doi: 10.1016/j.jinf.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 49.Andrewes C.H., Glover R.E. Spread of infection from the respiratory tract of the ferret. I. Transmission of influenza A virus. Br J Exp Pathol. 1941;22:91–97. [Google Scholar]
- 50.Schulman J.L., Kilbourne E.D. Airborne transmission of influenza virus infection in mice. Nature. 1962;195:1129–1130. doi: 10.1038/1951129a0. [DOI] [PubMed] [Google Scholar]
- 51.Schulman J.L. Experimental transmission of influenza virus infection in mice. IV. Relationship of transmissibility of different strains of virus and recovery of airborne virus in the environment of infector mice. J Exp Med. 1967;125:479–488. doi: 10.1084/jem.125.3.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Alford R.H., Kasel J.A., Gerone P.J. Human influenza resulting from aerosol inhalation. Proc Soc Exp Biol Med. 1966;122:800–804. doi: 10.3181/00379727-122-31255. [DOI] [PubMed] [Google Scholar]
- 53.Knight V. Viruses as agents of airborne contagion. Ann N Y Acad Sci. 1980;353:147–156. doi: 10.1111/j.1749-6632.1980.tb18917.x. [DOI] [PubMed] [Google Scholar]
- 54.Loudon R.G., Roberts R.M. Droplet expulsion from the respiratory tract. Am Rev Respir Dis. 1967;95:435–442. doi: 10.1164/arrd.1967.95.3.435. [DOI] [PubMed] [Google Scholar]
- 55.Papineni R.S., Rosenthal F.S. The size distribution of droplets in the exhaled breath of healthy human subjects. J Aerosol Med. 1997;10:105–116. doi: 10.1089/jam.1997.10.105. [DOI] [PubMed] [Google Scholar]
- 56.Blachere F.M., Lindsley W.G., Pearce T.A. Measurement of airborne influenza virus in a hospital emergency department. Clin Infect Dis. 2009;48(4):438–440. doi: 10.1086/596478. [DOI] [PubMed] [Google Scholar]
- 57.McLean R.L. The American Review of Respiratory Diseases; Bethesda (MD): 1960. International conference on Asian influenza; 1960 February 17-19; pp. 36–38. [Google Scholar]
- 58.Moser M.R., Bender T.R., Margolis H.S. An outbreak of influenza aboard a commercial airliner. Am J Epidemiol. 1979;110:1–6. doi: 10.1093/oxfordjournals.aje.a112781. [DOI] [PubMed] [Google Scholar]
- 59.Blumenfeld H.L., Kilbourne E.D., Louria D.B. Studies on influenza in the pandemic of 1957-1958. I. An epidemiologic, clinical and serologic investigation of an intrahospital epidemic, with a note on vaccination efficacy. J Clin Invest. 1959;38:199–212. doi: 10.1172/JCI103789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bridges C.B., Kuehnert M.J., Hall C.B. Transmission of influenza: implications for control in health care settings. Clin Infect Dis. 2003;37:1094–1101. doi: 10.1086/378292. [DOI] [PubMed] [Google Scholar]
- 61.Loeb M., Dafoe N., Mahony J. Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA. 2009;302(17):1865–1871. doi: 10.1001/jama.2009.1466. [DOI] [PubMed] [Google Scholar]
- 62.Macintyre CR, Wang Q, Cauchemez S, et al. The first randomised, controlled clinical trial of surgical masks compared to fit-tested and non-fit tested N95 masks in the prevention of respiratory virus infection in hospital health care workers in Beijing, China. Presented at the 47th Annual Meeting of the Infectious Diseases Society of America; 2009. Philadelphia. October 31, 2009. p. 40.
- 63.Centers for Disease Control and Prevention. Prevention Strategies for Seasonal Influenza in Healthcare Settings. Available at: http://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm. Accessed May 30, 2016.
- 64.Blanco N., Eisenberg M.C., Stillwell T. What transmission precautions best control influenza spread in a hospital? Am J Epidemiol. 2016;183(11):1045–1054. doi: 10.1093/aje/kwv293. [DOI] [PubMed] [Google Scholar]
- 65.Fiore A.E., Shay D.K., Broder K. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009. MMWR Recomm Rep. 2009;58:1–52. [PubMed] [Google Scholar]
- 66.Wilde J.A., McMillan J.A., Serwint J. Effectiveness of influenza vaccine in health care professionals: a randomized trial. JAMA. 1999;281:908–913. doi: 10.1001/jama.281.10.908. [DOI] [PubMed] [Google Scholar]
- 67.Saxen H., Virtanen M. Randomized, placebo-controlled double blind study on the efficacy of influenza immunization on absenteeism of health care workers. Pediatr Infect Dis J. 1999;18:779–783. doi: 10.1097/00006454-199909000-00007. [DOI] [PubMed] [Google Scholar]
- 68.Feery B.J., Evered M.G., Morrison E.I. Different protection rates in various groups of volunteers given subunit influenza virus vaccine in 1976. J Infect Dis. 1979;139:237–241. doi: 10.1093/infdis/139.2.237. [DOI] [PubMed] [Google Scholar]
- 69.Vanhems P., Voirin N., Roche S. Risk of influenza-like illness in an acute health care setting during community influenza epidemics in 2004-2005, 2005-2006, and 2006-2007: a prospective study. Arch Intern Med. 2011;171:151–157. doi: 10.1001/archinternmed.2010.500. [DOI] [PubMed] [Google Scholar]
- 70.Salgado C.D., Giannetta E.T., Hayden F.G. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Infect Control Hosp Epidemiol. 2004;25:923–928. doi: 10.1086/502321. [DOI] [PubMed] [Google Scholar]
- 71.Frenzel E., Chemaly R.F., Ariza-Heredia E. Association of increased influenza vaccination in health care workers with a reduction in nosocomial influenza infections in cancer patients. Am J Infect Control. 2016 doi: 10.1016/j.ajic.2016.03.024. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 72.Potter J., Stott D.J., Roberts M.A. Influenza vaccination of health care workers in long-term-care hospitals reduces the mortality of elderly patients. J Infect Dis. 1997;175:1–6. doi: 10.1093/infdis/175.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Carman W.F., Elder A.G., Wallace L.A. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: a randomised controlled trial. Lancet. 2000;355:93–97. doi: 10.1016/S0140-6736(99)05190-9. [DOI] [PubMed] [Google Scholar]
- 74.Hayward A.C., Harling R., Wetten S. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006;333:1241. doi: 10.1136/bmj.39010.581354.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lemaitre M., Meret T., Rothan-Tondeur M. Effect of influenza vaccination of nursing home staff on mortality of residents: a cluster-randomized trial. J Am Geriatr Soc. 2009;57(9):1580–1586. doi: 10.1111/j.1532-5415.2009.02402.x. [DOI] [PubMed] [Google Scholar]
- 76.Vaccination coverage estimates from the National Health Interview Survey: United States, 2008. Centers for Disease Control and Prevention. 2009. Available at: http://www.cdc.gov/nchs/data/hestat/vaccine_coverage.htm. Accessed October 8, 2009.
- 77.Honor roll for patient safety. Mandatory influenza vaccination policies for healthcare workers. Immunization Action Coalition. Available at: http://www.immunize.org/laws/influenzahcw.asp. Accessed November 19, 2009.
- 78.Health Affairs Blog. The ‘Must Do’ List: Certain patient safety rules should not be elective. Available at: http://healthaffairs.org/blog/2015/08/20/the-must-do-list-certain-patient-safety-rules-should-not-be-elective/. Accessed May 30, 2016.
- 79.Black C.L., Yue X., Ball S.W. Influenza vaccination coverage among health care personnel—United States, 2014-15 influenza season. MMWR Morb Mortal Wkly Rep. 2015;64:993–999. doi: 10.15585/mmwr.mm6436a1. [DOI] [PubMed] [Google Scholar]
- 80.Fiore A.E., Shay D.K., Broder K. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2008. MMWR Recomm Rep. 2008;57:1–60. [PubMed] [Google Scholar]
- 81.Harper S.A., Bradley J.S., Englund J.A. Seasonal influenza in adults and children–diagnosis, treatment, chemoprophylaxis, and institutional outbreak management: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:1003–1032. doi: 10.1086/604670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Higa F., Tateyama M., Tomishima M. Role of neuraminidase inhibitor chemoprophylaxis in controlling nosocomial influenza: an observational study. Influenza Other Respir Viruses. 2012;6:299–303. doi: 10.1111/j.1750-2659.2011.00311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Steininger C., Kundi M., Aberle S.W. Effectiveness of reverse transcription-PCR, virus isolation, and enzyme-linked immunosorbent assay for diagnosis of influenza A virus infection in different age groups. J Clin Microbiol. 2002;40:2051–2056. doi: 10.1128/JCM.40.6.2051-2056.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.H5N1 avian influenza: timeline of major events, March 23, 2009. World Health Organization. 2009. Available at: http://www.who.int/csr/disease/avian_influenza/Timeline_09_03_23.pdf. Accessed July 27, 2009.
- 85.Cumulative number of confirmed human cases of avian influenza A/(H5N1) reported to WHO, September 24, 2009. World Health Organization. 2009. Available at: http://www.who.int/csr/disease/avian_influenza/country/cases_table_2009_09_24/en/index.html. Accessed October 8, 2009.
- 86.Ungchusak K., Auewarakul P., Dowell S.F. Probable person-to-person transmission of avian influenza A (H5N1) N Engl J Med. 2005;352:333–340. doi: 10.1056/NEJMoa044021. [DOI] [PubMed] [Google Scholar]
- 87.Wang H., Feng Z., Shu Y. Probable limited person-to-person transmission of highly pathogenic avian influenza A (H5N1) virus in China. Lancet. 2008;371:1427–1434. doi: 10.1016/S0140-6736(08)60493-6. [DOI] [PubMed] [Google Scholar]
- 88.Buxton Bridges C., Katz J.M., Seto W.H. Risk of influenza A (H5N1) infection among health care workers exposed to patients with influenza A (H5N1), Hong Kong. J Infect Dis. 2000;181:344–348. doi: 10.1086/315213. [DOI] [PubMed] [Google Scholar]
- 89.Liem N.T., Lim W. Lack of H5N1 avian influenza transmission to hospital employees, Hanoi, 2004. Emerg Infect Dis. 2005;11:210–215. doi: 10.3201/eid1102.041075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Schultsz C., Dong V.C., Chau N.V. Avian influenza H5N1 and healthcare workers. Emerg Infect Dis. 2005;11:1158–1159. doi: 10.3201/eid1107.050070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Shinya K., Ebina M., Yamada S. Avian flu: influenza virus receptors in the human airway. Nature. 2006;440:435–436. doi: 10.1038/440435a. [DOI] [PubMed] [Google Scholar]
- 92.World Health Organization. Human infection with avian influenza A(H7N9) virus – China. Available at: http://www.who.int/csr/don/17-may-2016-ah7n9-china/en/. Accessed May 30, 2016.
- 93.Fang C.F., Ma M.J., Zhan B.D. Nosocomial transmission of avian influenza A (H7N9) virus in China: epidemiological investigation. BMJ. 2015;351:h5765. doi: 10.1136/bmj.h5765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Farooqui A., Liu W., Kelvin D.J. Probable hospital cluster of H7N9 influenza infection. N Engl J Med. 2016;374:596–598. doi: 10.1056/NEJMc1505359. [DOI] [PubMed] [Google Scholar]
- 95.Centers for Disease Control and Prevention. Interim guidance for infection control within healthcare settings when caring for confirmed cases, probable cases, and cases under investigation for infection with novel influenza A viruses associated with severe disease. Available at: http://www.cdc.gov/flu/avianflu/novel-flu-infection-control.htm. Accessed May 30, 2016.
- 96.Beigel J.H., Farrar J., Han A.M. Avian influenza A (H5N1) infection in humans. N Engl J Med. 2005;353:1374–1385. doi: 10.1056/NEJMra052211. [DOI] [PubMed] [Google Scholar]
- 97.World Health Organization. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. Available at: http://www.who.int/csr/sars/country/table2004_04_21/en/. Accessed May 30, 2016.
- 98.Zaki A.M., van Boheemen S., Bestebroer T.M. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 99.World Health Organization. Middle East respiratory syndrome coronavirus (MERS-CoV). Available at: http://www.who.int/emergencies/mers-cov/en/. Accessed May 30, 2016.
- 100.Assiri A., McGeer A., Perl T.M. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013;369:407–416. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Balkhy H.H., Alenazi T.H., Alshamrani M.M. Notes from the field: nosocomial outbreak of middle east respiratory syndrome in a large tertiary care Hospital - Riyadh, Saudi Arabia, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:163–164. doi: 10.15585/mmwr.mm6506a5. [DOI] [PubMed] [Google Scholar]
- 102.Hunter J.C., Nguyen D., Aden B. Transmission of middle east respiratory syndrome coronavirus infections in healthcare settings, Abu Dhabi. Emerg Infect Dis. 2016;22:647–656. doi: 10.3201/eid2204.151615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chowell G., Abdirizak F., Lee S. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. 2015;13:210. doi: 10.1186/s12916-015-0450-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hastings D.L., Tokars J.I., Abdel Aziz I.Z. Outbreak of middle east respiratory syndrome at tertiary care hospital, Jeddah, Saudi Arabia, 2014. Emerg Infect Dis. 2016;22:794–801. doi: 10.3201/eid2205.151797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hsieh Y.H. 2015 middle east respiratory syndrome coronavirus (MERS-CoV) nosocomial outbreak in South Korea: insights from modeling. PeerJ. 2015;3:e1505. doi: 10.7717/peerj.1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bin S.Y., Heo J.Y., Song M.S. Environmental contamination and viral shedding in MERS patients during MERS-CoV outbreak in South Korea. Clin Infect Dis. 2016;62:755–760. doi: 10.1093/cid/civ1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Centers for Disease Control and Prevention. Interim infection prevention and control recommendations for hospitalized patients with middle east respiratory syndrome coronavirus (MERS-CoV). Available at: https://www.cdc.gov/coronavirus/mers/infection-prevention-control.html. Accessed May 30, 2016.
- 108.Fu C., Wang S. Nosocomial infection control in healthcare settings: protection against emerging infectious diseases. Infect Dis Poverty. 2016;5:30. doi: 10.1186/s40249-016-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Brummitt C.F., Cherrington J.M., Katzenstein D.A. Nosocomial adenovirus infections: molecular epidemiology of an outbreak due to adenovirus 3a. J Infect Dis. 1988;158:423–432. doi: 10.1093/infdis/158.2.423. [DOI] [PubMed] [Google Scholar]
- 110.James L., Vernon M.O., Jones R.C. Outbreak of human adenovirus type 3 infection in a pediatric long-term care facility—Illinois, 2005. Clin Infect Dis. 2007;45:416–420. doi: 10.1086/519938. [DOI] [PubMed] [Google Scholar]
- 111.Lessa F.C., Gould P.L., Pascoe N. Health care transmission of a newly emergent adenovirus serotype in health care personnel at a military hospital in Texas, 2007. J Infect Dis. 2009;200:1759–1765. doi: 10.1086/647987. [DOI] [PubMed] [Google Scholar]
- 112.Gerber S.I., Erdman D.D., Pur S.L. Outbreak of adenovirus genome type 7d2 infection in a pediatric chronic-care facility and tertiary-care hospital. Clin Infect Dis. 2001;32:694–700. doi: 10.1086/319210. [DOI] [PubMed] [Google Scholar]
- 113.Gordon Y.J., Gordon R.Y., Romanowski E. Prolonged recovery of desiccated adenoviral serotypes 5, 8, and 19 from plastic and metal surfaces in vitro. Ophthalmology. 1993;100:1835–1839. doi: 10.1016/s0161-6420(93)31389-8. [discussion: 9–40] [DOI] [PubMed] [Google Scholar]
- 114.Gardner P.S., Court S.D., Brocklebank J.T. Virus cross-infection in paediatric wards. Br Med J. 1973;2:571–575. doi: 10.1136/bmj.2.5866.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Meissner H.C., Murray S.A., Kiernan M.A. A simultaneous outbreak of respiratory syncytial virus and parainfluenza virus type 3 in a newborn nursery. J Pediatr. 1984;104:680–684. doi: 10.1016/s0022-3476(84)80943-9. [DOI] [PubMed] [Google Scholar]
- 116.Zambon M., Bull T., Sadler C.J. Molecular epidemiology of two consecutive outbreaks of parainfluenza 3 in a bone marrow transplant unit. J Clin Microbiol. 1998;36:2289–2293. doi: 10.1128/jcm.36.8.2289-2293.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Brady M.T., Evans J., Cuartas J. Survival and disinfection of parainfluenza viruses on environmental surfaces. Am J Infect Control. 1990;18:18–23. doi: 10.1016/0196-6553(90)90206-8. [DOI] [PubMed] [Google Scholar]
- 118.Ansari S.A., Springthorpe V.S., Sattar S.A. Potential role of hands in the spread of respiratory viral infections: studies with human parainfluenza virus 3 and rhinovirus 14. J Clin Microbiol. 1991;29:2115–2119. doi: 10.1128/jcm.29.10.2115-2119.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]