Abstract
Purpose
The aims of this study were to assess the feasibility of cardiopulmonary exercise testing (CPET) for the early assessment of cardiorespiratory fitness in general adult intensive care unit (ICU) survivors and to characterize the pathophysiology of exercise limitation in this population.
Methods
Fifty general ICU survivors (ventilated for ≥5 days) performed a maximal cycle ergometer CPET within 6 weeks of hospital discharge. Health-related quality of life was measured by the Medical Outcome Study Short Form 36 version 2.0 questionnaire.
Results
Fifty patients (median age, 57 years; median Acute Physiology And Chronic Health Evaluation II score, 16) completed a CPET 24 ± 14 days after hospital discharge with no adverse events. Significant exercise limitation was present with peak Vo2 56% ± 16% predicted and anaerobic threshold (AT) 41% ± 13% of peak predicted Vo2. Prospectively stratified subgroup comparison showed that patients ventilated for 14 days or more had a significantly lower AT and peak Vo2 than those ventilated for 5 to 14 days (AT: 9.6 vs 11.7 mL/kg per minute O2, P = .009; peak Vo2: 12.9 vs 15.3 mL/kg per minute O2, P = .022). At peak exercise, heart rate reserve was 25% ± 14%, breathing reserve was 47% ± 19%, and the respiratory exchange ratio was 0.96 ± 0.11. Ventilatory equivalents for CO2 (Eqco2) were 39 ± 9.
Conclusions
Significant exercise limitation is evident in patients who have had critical illness. Etiology of exercise limitation appears multifactorial, with general deconditioning and muscle weakness as major contributory factors. Early CPET appears a practical method of assessing exercise capacity in ICU survivors. Cardiopulmonary exercise testing could be used to select patients who may benefit most from a targeted physical rehabilitation program, aid in exercise prescription, and help assess the response to intervention.
Keywords: Cardiopulmonary exercise test, Critical care, Rehabilitation, Health-related quality of life
1. Purpose
The deleterious effect of critical illness on physical function is well described, with exercise limitation and neuromuscular abnormalities persisting for long periods after hospital discharge [1], [2]. The rehabilitation of patients after critical illness has gained increased prominence in the United Kingdom recently after the publication of a national guideline. This provides a broad framework for patient assessment but falls short of providing details of how best to improve physical function [3].
In contrast to conditions such as chronic obstructive airways disease and congestive cardiac failure, there is little published evidence regarding the optimal physical rehabilitation strategy for survivors of critical illness after hospital discharge. In these patients, the relative contribution of cardiac, respiratory, and musculoskeletal impairment to exercise limitation is also not well characterized. Commonly used assessment tools such as the 6-minute walk test (6MWT) are well validated and simple measures of exercise capacity but are subject to a learning effect and do not differentiate between the many potential causes of exercise limitation in intensive care unit (ICU) survivors [4], [5].
Cardiopulmonary exercise testing (CPET) provides an objective, noninvasive global assessment of the integrated physiologic response to exercise. A major advantage over other objective measures of exercise capacity (eg, 6MWT) is that it provides information that may identify cardiac, respiratory, or musculoskeletal contributions to any exercise limitation present. The anaerobic threshold (AT) is an objective measure of functional or aerobic capacity that normally occurs at 50% to 60% of peak exercise capacity. Importantly and unlike peak oxygen consumption (peak Vo 2), it is less influenced by either learning effect or patient effort. Cardiopulmonary exercise testing is advocated as a tool to guide exercise prescription in chronic obstructive pulmonary disease and heart failure [6], [7]. To date, its use after critical illness has been restricted to the study of specific patient populations including survivors of the severe acute respiratory syndrome and the acute respiratory distress syndrome (ARDS) [8], [9]. To our knowledge, CPET has never been used in the assessment of general adult ICU survivors in the immediate post–hospital discharge period. The purpose of our study was therefore 2-fold:
-
1.
To determine the feasibility and safety of CPET as a tool for the objective assessment of exercise capacity in unselected adult general ICU survivors.
-
2.
To help to further characterize the pathophysiology of any exercise limitation present in this patient population.
2. Materials and methods
2.1. Patient selection
Fifty survivors of critical illness were recruited into the study and underwent a CPET within 6 weeks of hospital discharge. No changes were made to patients' medications in preparation for the test (eg, withholding of β-blockade). All patients ventilated for at least 5 days during their general ICU admission were eligible for inclusion; patients were prospectively stratified into 2 groups based on the duration of ventilation (5-14 days and >14 days). Exclusion criteria were age younger than 18 years, duration of mechanical ventilation less than 5 days, inability to perform CPET because of physical or mental impairment, pregnancy, terminal illness, and acute coronary syndrome within the preceding 30 days. Approval for the study was obtained from the local research ethics committee. Written informed consent was obtained from all participants.
2.2. Cardiopulmonary exercise testing
A maximal, symptom-limited incremental CPET using a cycle ergometer was conducted according to a standard ramped protocol [10]. Patients were seated on a bicycle ergometer with 12-lead electrocardiogram and gas exchange monitoring using a Jaeger Oxycon Pro ergospirometry system (Jaeger, Wurzburg, Germany). Peripheral oxygen saturations (Spo 2) and noninvasive blood pressure were monitored throughout the test. After a period of observation at rest to allow the respiratory exchange ratio (RER) to plateau (typically 1-3 minutes), subjects completed 3 minutes of unloaded cycling at 60 revolutions per minute. Load was then applied to the pedals in a ramp-like fashion increasing by 10 to 15 W/min until maximum exercise capacity was reached. For safety reasons, the study protocol required immediate termination of the test if the subject experienced any of the following adverse events: chest pain, altered sensorium, ST depression greater than 2 mm on the exercise electrocardiogram, and emotional distress. Two intensive care physicians with advanced life support skills were present throughout all tests. After termination of the test, subjects were monitored until cardiorespiratory parameters returned to baseline levels.
Anaerobic threshold was determined using a combination of the V-slope and ventilatory equivalents methods as described by Wasserman et al [10].
Data for the following parameters were collected: AT, peak Vo 2, ventilatory equivalents for CO2 (Eqco 2), oxygen pulse (Vo 2/HR), heart rate reserve (HRR), breathing reserve (BR) at peak exercise and static spirometry. Values of Eqco 2 were taken at AT or recorded as the lowest value achieved during incremental exercise when AT was not able to be determined. Maximum voluntary ventilation (MVV) was determined indirectly: MVV (L/min) = Forced expiratory volume in 1 second (FEV1) × 40. Heart rate reserve at peak exercise was expressed as an absolute value or as a percentage: HRR (beats per minute) = peak predicted HR − HR at peak exercise or %HRR = (1 − [HR at peak exercise/peak predicted HR]) × 100. Breathing reserve at peak exercise was expressed as both an absolute value and as a percentage: BR (L/min) = MVV − VE at peak exercise or %BR = (1 − [VE at peak exercise/MVV]) × 100.
2.3. Health-related quality of life assessment
Exercise capacity has been shown to correlate with various measures of quality of life [11]. Patients' health-related quality of life (HRQL) was assessed using the Medical Outcome Study Short Form 36 version 2.0 (SF-36v2) questionnaire (Quality Metric, Lincoln, RI) [12]. This was performed immediately before their CPET. Physical component summary (PCS) and mental component summary (MCS) scores were generated as a measure of patients' self-reported physical and mental well-being.
2.4. Data analysis
Peak Vo 2 and AT values were expressed as both milliliter per kilogram per minute O2 and as a percentage of peak predicted Vo 2 achieved by a reference (Wasserman) population of normal sedentary healthy volunteers. Descriptive statistics were prepared using Microsoft Excel 2007 (Microsoft, Redmond, Wash). Data were characterized as normally distributed after calculation of skewness and kurtosis. Subgroups were compared with an unpaired t test using SPSS for Windows (Rel. 10.0.0. 1999; SPSS Inc, Chicago, Ill).
3. Results
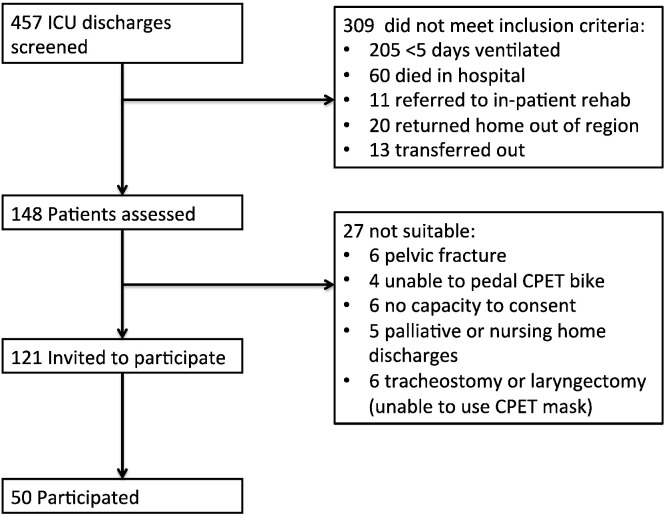
Fifty patients were recruited from a pool of 457 ICU discharges screened for participation over a 2-year period (Fig. 1 ). Of the 121 eligible patients who were approached, 59% declined to participate. The commonest reason for declining to participate was a reluctance to undergo further clinical investigations unless absolutely necessary.
Fig. 1.
Recruitment flowchart.
Characteristics of the enrolled patients and comparison with nonenrolled patients are shown in Table 1 , and premorbid comorbidities of participating patients are presented in Table E1. All 50 enrolled patients completed a CPET. No patient had any adverse event during testing. The mean time from hospital discharge to CPET was 24 ± 14 days (all data presented as mean ± SD unless otherwise stated). In 70% of cases, the reason given for cessation of pedaling was leg fatigue; shortness of breath accounted for most of the remainder (26%). One patient had to stop because of back pain, and one, because of anxiety.
Table 1.
Patient demographics
| Study patients | Invited patients who declined to participate | |
|---|---|---|
| No. | 50 | 71 |
| Age (y) | 57 (31-82) | 56 (19-80) |
| Male/female | 64% | 63% |
| APACHE II | 16 (5-30) | 16 (5-34) |
| Days ventilated | 18 (5-60) | 14 (6-53) |
| Days on critical care | 31 (8-120) | 16 (6-57) |
| Days in hospital | 38 (15-168) | 52 (10-189) |
Data are presented as median (range). Data on patients declining to participate were extracted from the Intensive Care National Audit and Research Centre audit database maintained on all intensive care unit patients in our institution. No additional data were collected on these patients. APACHE indicates Acute Physiology And Chronic Health Evaluation.
Baseline spirometry showed an FEV1 of 2.2 ± 0.9 L/min (mean predicted FEV1, 2.9 L/min) and an forced vital capacity (FVC) of 3.0 ± 0.8 L/min (mean predicted FVC, 3.6 L/min); the mean FEV1/FVC ratio was 74%. Individual patient CPET data are shown in Table E1. Peak Vo 2 was 56% ± 16% predicted (13.8 ± 4.0 mL/kg per minute Vo 2), and AT was 41% ± 13% of peak predicted Vo 2 (10.4 ± 2.7 mL/kg per minute O2). It was not possible to determine the AT for 7 patients. At peak exercise, HRR was 25% ± 14%; BR at peak exercise was 47 ± 19%; and the RER was 0.96 ± 0.11. The Eqco 2 was 39 ± 9. Mean hemoglobin concentration at the time of hospital discharge was 10.3 ± 1.2 g/dL. Of 50 patients, 18 (36%) were taking rate-limiting medication at the time of the test. The mean oxygen pulse at peak exercise was 8.6 ± 2.5 mL per beat (74% predicted).
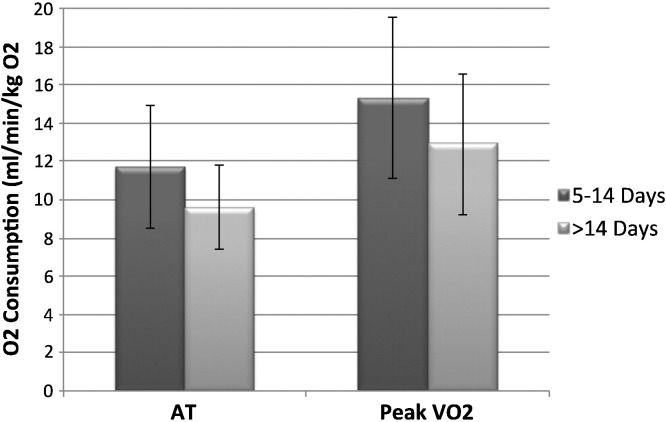
The difference in oxygen consumption between patients who stopped because of shortness of breath and those stopping because of leg fatigue did not reach statistical significance (AT: 9.4 ± 1.9 vs 10.7 ± 3.0 mL/kg per minute O2, P = .23; peak Vo 2: 12.9 ± 3.0 vs 14.1 ± 4.4 mL/kg per minute O2, P = .36). Comparison of the prospectively stratified subgroups (Fig. 2 ) showed that patients ventilated for 14 days or more had a significantly lower AT than those ventilated for 5 to 14 days (9.6 ± 3.2 vs 11.7 ± 2.2 mL/kg per minute O2, P = .009) and a significantly lower peak Vo 2 (12.9 ± 3.7 vs 15.3 ± 4.2 mL/kg per minute O2, P = .023).
Fig. 2.
Anaerobic threshold and peak Vo2 stratified by length of ventilation.
Ventilatory limitation to exercise was defined as present if either of the 2 following criteria were met:
-
1.
VE at peak exercise was greater than 80% of indirectly measured MVV (or BR <20%),
-
2.
Indirectly measured MVV minus VE at peak exercise was less than 12 L/min.
Five patients demonstrated evidence of ventilatory limitation to exercise based on these criteria. One patient demonstrated significant desaturation during exercise from baseline levels (>4%).
All patients completed an SF-36v2 questionnaire; mean PCS and MCS scores were 32 ± 8 and 37 ± 11, respectively. Only 1 patient had an MCS score greater than 50 (the population norm), and only 4 patients had a PCS score greater than 50. There was no significant correlation between exercise capacity, measured by either peak Vo 2 or AT, and either PCS or MCS.
4. Conclusions
Cardiopulmonary exercise testing appears to be a practical method of assessing exercise capacity in ICU survivors when performed within 6 weeks of hospital discharge. To our knowledge, only 1 previously published study has used CPET to assess patients in a similar setting, testing 44 severe acute respiratory syndrome survivors 3 months after hospital discharge [8]. In comparison with this study, our patient cohort was older (57 vs 37 ± 11 years), spent longer in hospital (47 ± 30 vs 20 ± 17 days), and was more likely to have received mechanical ventilation (100% vs 16%). Our patient cohort performed worse in terms of peak Vo 2 (52% ± 16% vs 79% ± 17%), AT (41% ± 13% vs 70% ± 13%), and ability to reach HRR (40 ± 22 beats per minute vs 7 ± 22 beats per minute). Breathing reserve values were similar between the 2 studies (49 ± 15 vs 46 ± 26 L/min).
Importantly, no adverse events occurred during any of the exercise tests performed during this study. Although the safety of CPET in this patient population has not previously been examined, it has been performed safely in other debilitated patient groups including those with advanced cancer and chronic heart failure [13], [14]. In the latter study, no deaths were reported in over 4400 tests, with a rate of major cardiovascular events of 0.45 per 1000 tests. Although not powered to detect morbidity and mortality, our study adds to the general body of evidence supporting the safety of CPET in debilitated patients.
Patients demonstrated reduced exercise capacity both in terms of AT (41% ± 13% peak predicted Vo 2) and peak Vo 2 (56% ± 16% predicted). This is in keeping with several follow-up studies of ICU survivors where exercise capacity, measured at 3 months using the 6MWT, ranged from 49% to 80% of predicted values [1], [15], [16]. Patients displayed raised Eqco 2 (39 ± 9), suggesting inefficient gas exchange and ventilation/perfusion (V/Q) mismatching. This finding has been previously documented in ICU survivors, especially those with prior ARDS [9], [17]. A raised Eqco 2 found in the presence of a reduced AT is suggestive of pulmonary vascular disease contributing to exercise limitation. This can be secondary to cardiac disease or intrinsic lung pathology. Interestingly, only 1 of our patient cohort demonstrated significant desaturation during exercise.
Oxygen pulse at peak exercise was reduced compared with population norms (mean O2 pulse 8.6 ± 2.5 mL per beat, 74% predicted). Contributing factors in this cohort might include cardiac dysfunction, pulmonary vascular changes, anemia, and impaired peripheral oxygen extraction. A number of our patients were known to have premorbid cardiac failure as documented in Table E1; because routine echocardiography was not performed as part of this study, it is not possible to further define the contribution of impaired stroke volume to the reduced oxygen pulse values seen. Patients were also anemic, with a mean hemoglobin concentration of 10.3 ± 1.2 g/dL at the time of hospital discharge. The interpretation of oxygen pulse data is further confounded by the number of patients β-blocked at the time of their CPET. Rate-limiting medication can affect the results of a CPET by increasing diastolic filling time and therefore stroke volume and oxygen pulse. This effect is countered by a reduction in peak heart rate achieved and consequently the peak cardiac output and oxygen consumption achievable. Patients taking rate-limiting drugs (36%) had a significantly greater oxygen pulse than those who were not (9.8 vs 8.1 mL per beat, P = .009), although no significant difference in exercise capacity was seen.
Patients demonstrated reduced values for FEV1 (76% predicted) and FVC (83% predicted) compared with population normal values with 5 patients demonstrating ventilatory limitation to exercise based on classically defined criteria. Premorbid spirometry was not available for most of our cohort, and therefore, the contribution of preexisting ventilatory pathology to this picture cannot be determined.
Critically ill patients lose muscle and lean body mass at up to 2% per day, with weight loss of 18% noted at the time of ICU discharge in 1 follow-up study [9]. The commonest reason for test termination in our cohort was leg fatigue. This is in keeping with previous studies of CPET after critical illness where more than 75% of patients described leg fatigue as the main symptom limiting exercise [8]. The RER at peak exercise was 0.96 ± 0.11 with both BR and HRR evident in most of the patients, indicating the presence of cardiorespiratory reserve at the peak exercise level achieved by the patient. These findings support muscle weakness and deconditioning as major contributory factors in the reduced exercise capacity seen in our patient cohort. The reduced exercise capacity evident in those patients ventilated for more than 14 days can also be explained in part by the expected increased loss of muscle mass and further deconditioning as a result of more prolonged critical illness. An objective measure of muscle strength was not an outcome measure in this study.
Intensive care unit survivors have a risk of death of nearly 3 times that of the general population at 1 year postdischarge with reduced quality of life; these effects diminish with time but may persist for many years [18], [19]. The SF-36 results show our patients to be well below population norms in this respect. Our patients had a mean PCS score of 32, agreeing closely with the results of a recent study of survivors of acute necrotising pancreatitis, where the mean PCS score was 33 at 3 months [16]. The reason for such low scores is likely to be multifactorial, influenced by factors such as premorbid personality, employment status, and posttraumatic stress disorder [20].
Although it might be expected that patients performing best in terms of exercise capacity would also score highest on measurement of HRQL, we were unable to demonstrate any correlation between SF-36 scores and CPET performance. One possible explanation is that SF-36 scores might bear more relation to the decline in exercise capacity (compared with the premorbid state) than to the absolute value. For example, a previously fit patient who has now lost the ability to climb 2 flights of stairs might feel worse about his situation than a previously housebound patient who is now chair bound, despite the former performing better on CPET testing.
Our study was designed primarily to describe the causes of exercise limitation in ICU survivors and to assess the practicality of routine CPET testing in this patient population. One limitation of our study is that we tested only 41% of eligible discharged patients during the study period. Although patients declining to take part had similar Acute Physiology And Chronic Health Evaluation II scores, length of ventilation, and age profile to participants (Table 1), we cannot exclude the possibility that those patients making themselves available for CPET testing were not representative of the whole. A “healthy volunteer” effect has been demonstrated in many studies whereby the healthiest and most active patients participate, who have better health than the general population from which they are sampled [21], [22]. This may have skewed our results, underestimating the degree of debility experienced by this population as a whole. Equally, an “unhealthy volunteer” effect is also a possibility, where the patients presenting are the worst affected, having failed to resume daily activities (including employment) and therefore have the time to attend. This latter possibility seems less likely, given the early proximity to hospital discharge.
Another limitation of our study is the lack of accurate premorbid functional capacity and HRQL data. Although we have included patients' major cardiorespiratory comorbidities in our data table, we have not presented information regarding patients' premorbid exercise capacity because this was documented inconsistently in the medical notes at the time of critical care admission. It is therefore difficult to assign the relative contributions of critical illness and poor preexisting functional status to the low AT and Vo 2 peak scores seen in most of our patients. One possible area for future research would be to look at a population of patients who have premorbid CPET data available and then have critical illness, for example, patients undergoing CPET as part of preoperative assessment before major elective surgery who subsequently become critically ill.
Rehabilitation programs have been shown to enhance quality of life and reduce mortality in other areas of medicine and are beginning to be developed after critical illness [23], [24]. Our results suggest that these programs should specifically target improvements in muscle mass and strength as well as general cardiorespiratory fitness. The early use of CPET in ICU survivors has the potential to objectively identify those patients most in need of such programs and allows individually tailored exercise prescription, making best use of limited resources in an era of financial restraint. Cardiopulmonary exercise testing might also provide an objective assessment of the impact of such interventions in addition to other objective measures, for example, muscle strength.
In summary, the results of this study suggest that the cause of exercise limitation in survivors of critical illness is multifactorial. Premorbid pathology, anemia, V/Q mismatching, and pulmonary vascular changes and ventilatory abnormalities all appear to contribute in varying amounts between individuals. However, our findings are supportive of muscle deconditioning and weakness as major limiting factors affecting exercise capacity in these patients. By providing further information on the cause of an individual's exercise limitation after critical illness, CPET offers the potential to guide further investigation and treatment of a cohort of patients with known high morbidity and mortality after hospital discharge with the aim of improving long-term outcomes.
Such hypotheses require testing in appropriate clinical trials.
Supplementary materials related to this article can be found online at doi:10.1016/j.jcrc.2011.07.080.
The following are the supplementary materials related to this article.
Patient demographics and CPET data presented in ascending order of length of mechanical ventilation. Abbreviations: AAA, abdominal aortic aneurysm; ARDS, acute respiratory distress syndrome; BR, breathing reserve; CCF, congestive cardiac failure; CMV, cytomegalovirus; CRF, chronic renal failure; CVD, cerebrovascular disease; Eqco2, ventilatory equivalents for CO2 at AT; HRR, heart rate reserve; IBD, inflammatory bowel disease; IHD, ischemic heart disease; LOS, hospital length of stay; MI, myocardial infarction; MOF, multiorgan failure; PVD, peripheral vascular disease; SOB, shortness of breath; STEMI, ST-elevation myocardial infarction; tx, transplant; ARS, advanced respiratory support.
References
- 1.Herridge M.S., Cheung A.M., Tansey C.M. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348:683–693. doi: 10.1056/NEJMoa022450. [DOI] [PubMed] [Google Scholar]
- 2.Fletcher S.N., Kennedy D.D., Ghosh I.R. Persistent neuromuscular and neurophysiologic abnormalities in long-term survivors of prolonged critical illness. Crit Care Med. 2003;31:1012–1016. doi: 10.1097/01.CCM.0000053651.38421.D9. [DOI] [PubMed] [Google Scholar]
- 3.Tan T., Brett S.J., Stokes T. Rehabilitation after critical illness: summary of NICE guidance. BMJ. 2009;b822:338. doi: 10.1136/bmj.b822. [DOI] [PubMed] [Google Scholar]
- 4.Wu G., Sanderson B., Bittner V. The 6-minute walk test: how important is the learning effect? Am Heart J. 2003;146:129–133. doi: 10.1016/S0002-8703(03)00119-4. [DOI] [PubMed] [Google Scholar]
- 5.Crapo R.O., Casaburi R., Coates A.L. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 6.Nici L., Donner C., Wouters E. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173:1390–1413. doi: 10.1164/rccm.200508-1211ST. [DOI] [PubMed] [Google Scholar]
- 7.Hunt S.A., Abraham W.T., Chin M.H. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112:e154–235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 8.Ong K.C., Ng A.W.K., Lee L.S.U. Pulmonary function and exercise capacity in survivors of severe acute respiratory syndrome. Eur Respir J. 2004;24:436–442. doi: 10.1183/09031936.04.00007104. [DOI] [PubMed] [Google Scholar]
- 9.Neff T.A., Stocker R., Frey H.R. Long-term assessment of lung function in survivors of severe ARDS. Chest. 2003;123:845. doi: 10.1378/chest.123.3.845. [DOI] [PubMed] [Google Scholar]
- 10.Wasserman K.H.J.E., Sue D.Y., Stringer W.W., Whipp B.J. Lippincott Williams & Wilkins; Philadelphia: 2005. Principles of exercise testing and interpretation. [Google Scholar]
- 11.Myers J., Zaheer N., Quaglietti S. Association of functional and health status measures in heart failure. J Card Fail. 2006;12:439–445. doi: 10.1016/j.cardfail.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 12.Ware J.E.J. SF-36 health survey update. Spine (Phila Pa 1976) 2000;25:3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 13.Jones L.W., Eves N.D., Mackey J.R. Safety and feasibility of cardiopulmonary exercise testing in patients with advanced cancer. Lung Cancer. 2007;55:225–232. doi: 10.1016/j.lungcan.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 14.Keteyian S.J., Isaac D., Thadani U. Safety of symptom-limited cardiopulmonary exercise testing in patients with chronic heart failure due to severe left ventricular systolic dysfunction. Am Heart J. 2009;158:S72–7. doi: 10.1016/j.ahj.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hui D.S., Joynt G.M., Wong K.T. Impact of severe acute respiratory syndrome (SARS) on pulmonary function, functional capacity and quality of life in a cohort of survivors. Thorax. 2005;60:401–409. doi: 10.1136/thx.2004.030205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wright S.E., Lochan R., Imrie K. Quality of life and functional outcome at 3, 6 and 12 months after acute necrotising pancreatitis. Intensive Care Med. 2009;35:1974–1978. doi: 10.1007/s00134-009-1616-z. [DOI] [PubMed] [Google Scholar]
- 17.Schelling G., Stoll C., Vogelmeier C. Pulmonary function and health-related quality of life in a sample of long-term survivors of the acute respiratory distress syndrome. Intensive Care Med. 2000;26:1304–1311. doi: 10.1007/s001340051342. [DOI] [PubMed] [Google Scholar]
- 18.Williams T.A., Dobb G.J., Finn J.C. Determinants of long-term survival after intensive care. Crit Care Med. 2008;36:1523–1530. doi: 10.1097/CCM.0b013e318170a405. [DOI] [PubMed] [Google Scholar]
- 19.Cuthbertson BH, Roughton S, Jenkinson D et al.: Quality of life in the five years after intensive care: a cohort study. Crit Care. 14; R6, Jan 20. [DOI] [PMC free article] [PubMed]
- 20.Myhren H., Ekeberg O., Stokland O. Health-related quality of life and return to work after critical illness in general intensive care unit patients: a 1-year follow-up study. Crit Care Med. 2010;38:1554–1561. doi: 10.1097/CCM.0b013e3181e2c8b1. [DOI] [PubMed] [Google Scholar]
- 21.Thomson C.A., Harris R.B., Craft N.E. A cross-sectional analysis demonstrated the healthy volunteer effect in smokers. J Clin Epidemiol. 2005;58:378–382. doi: 10.1016/j.jclinepi.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 22.Pinsky P.F., Miller A., Kramer B.S. Evidence of a healthy volunteer effect in the prostate, lung, colorectal, and ovarian cancer screening trial. Am J Epidemiol. 2007;165:874–881. doi: 10.1093/aje/kwk075. [DOI] [PubMed] [Google Scholar]
- 23.McWilliams D.J., Atkinson D., Carter A. Feasibility and impact of a structured, exercise-based rehabilitation programme for intensive care survivors. Physiother Theory Pract. 2009;25:566–571. doi: 10.3109/09593980802668076. [DOI] [PubMed] [Google Scholar]
- 24.Jones C., Skirrow P., Griffiths R.D. Rehabilitation after critical illness: a randomized, controlled trial. Crit Care Med. 2003;31:2456–2461. doi: 10.1097/01.CCM.0000089938.56725.33. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Patient demographics and CPET data presented in ascending order of length of mechanical ventilation. Abbreviations: AAA, abdominal aortic aneurysm; ARDS, acute respiratory distress syndrome; BR, breathing reserve; CCF, congestive cardiac failure; CMV, cytomegalovirus; CRF, chronic renal failure; CVD, cerebrovascular disease; Eqco2, ventilatory equivalents for CO2 at AT; HRR, heart rate reserve; IBD, inflammatory bowel disease; IHD, ischemic heart disease; LOS, hospital length of stay; MI, myocardial infarction; MOF, multiorgan failure; PVD, peripheral vascular disease; SOB, shortness of breath; STEMI, ST-elevation myocardial infarction; tx, transplant; ARS, advanced respiratory support.