Abstract
Ethnopharmacological relevance
The African continent is home to a large number of higher plant species used over centuries for many applications, which include treating and managing diseases such as HIV. Due to the overwhelming prevalence and incidence rates of HIV, especially in sub-Saharan Africa, it is necessary to develop new and affordable treatments.
Aim of the study
The article provides an extensive overview of the status on investigation of plants from the southern African region with ethnobotanical use for treating HIV or HIV-related symptoms, or the management of HIV. The review also provide an account of the in vitro assays, anti-viral activity and phytochemistry of these plants.
Materials and methods
Peer-reviewed articles investigating plants with ethnobotanical information for the treatment or management of HIV or HIV-related symptoms from the southern African region were acquired from Science Direct, PubMed central and Google Scholar. The selection criteria was that (1) plants should have a record of traditional/popular use for infectious or viral diseases, HIV treatment or symptoms similar to HIV infection, (2) if not traditionally/popularly used, plants should be closely related to plants with popular use and HIV activity identified by means of in vitro assays, (3) plants should have been identified scientifically, (4) should be native to southern African region and (5) anti-HIV activity should be within acceptable ranges.
Results
Many plants in Africa and specifically the southern African region have been used for the treatment of HIV or HIV related symptoms and have been investigated suing various in vitro techniques. In vitro assays using HIV enzymes such as reverse transcriptase (RT), integrase (IN) and protease (PR), proteins or cell-based assays have been employed to validate the use of these plants with occasional indication of the selectivity index (SI) or therapeutic index (TI), with only one study, that progressed to in vivo testing. The compounds identified from plants from southern Africa is similar to compounds identified from other regions of the world, and the compounds have been divided into three groups namely (1) flavonoids and flavonoid glycosides, (2) terpenoids and terpenoid glycosides and (3) phenolic acids and their conjugated forms.
Conclusions
An investigation of the plants from southern Africa with ethnobotanical use for the treatment of HIV, management of HIV or HIV-related symptoms, therefore provide a very good analysis of the major assays employed and the anti-viral compounds and compound groups identified. The similarity in identified anti-viral compounds worldwide should support the progression from in vitro studies to in vivo testing in development of affordable and effective anti-HIV agents for countries with high infection and mortality rates due to HIV/AIDS.
Chemical compounds studied in this article: Chloroquine (PubChem CID: 2719); genistein (PubChem CID: 5280961); EGCG (PubChem CID: 65064) and strictinin (PubChem CID: 73330); fulvoplumierin (PubChem CID: 5281541); catechin (CID 73160); epicatechin (PubChem CID: 72276); meliacine and 28-deacetylsendanin; lycorine (PubChem CID: 72378); narciclasine (PubChem CID: 72376); pretazettine (PubChem CID: 73360); crinine (PubChem CID: CID 398937); galanthamine (PubChem CID: 9651); rosmarinic acid (PubChem CID: 5281792); caffeic acid (PubChem CID: 689043); friedelin (PubChem CID: 91472); B-sitosterol (PubChem CID: 222284); asiatic acid (PubChem CID: 119034); madecassic acid (PubChem CID: 73412); ellagitannin (PubChem CID: 101601927); punicalagin (PubChem CID: 16129869); arjunglucoside I (PubChem CID: 14658050); sericoside (PubChem CID: 76972524); digitoxigenin-3-O-glucoside (PubChem CID: 25202015); 4’-O-methylepigallocatechin (ourateacatechin) (PubChem CID: 176920); 4’-O-methylgallocatechin (PubChem CID: 10087345); 4’,4’’-di-O-methyl-prodelphinidin B4 or 4’-O- methylgallocatechin-(4α→8)-4’-O-methylepigallocatechin; 3,4 dicaffeoylquinic acid (PubChem CID: 5281780); 3,5 dicaffeoylquinic aicd (isochlorogenic acid A) (PubChem CID: 6474310); 4,5 dicaffeoylquinic acid (PubChem CID: 6474309); galangin (PubChem CID: 5281616); 3,4,5 tri-O-galloylquinic acid (PubChem CID: 452237); bergenin (PubChem CID: 66065); betulinic acid (PubChem CID: 64971); pinitol (PubChem CID: 164619); 2-hydroxyisobutyrate (PubChem CID: 4277439); asparagine (PubChem CID: 6267); trigonelline (PubChem CID: 5570); sutherlandioside B (PubChem CID: 25137458); sutherlandioside D (PubChem CID: 25137459); synapoic (sinapic) acid (PubChem CID: 637775); anolignan B (PubChem CID: 72388); gallic acid (PubChem CID: 370); chlorogenic acid (5-O-caffeoylquinic acid) (PubChem CID: 179442); quercetin (PubChem CID: 5280343); 1-methoxyoxalyl-3,5-DCQA (1-MO-3,5-DCQA); 1,5- dicaffeoylquinic acid (PubChem CID: 6474640); L-chicoric acid (PubChem CID: 5281764); 3-caffeoylquinic acid (PubChem CID: 12310830); ferulic acid (PubChem CID: 445858); isoferulic acid (PubChem CID: 736186); p-coumaric acid (PubChem CID: 637542); hyperin (PubChem CID: 90657624); isoquercitrin (PubChem CID: 5280804); thiarubrine A (PubChem CID: 72386); procyanidin (PubChem CID: 107876); isorhamnetin (PubChem CID: 5281654); euphol (PubChem CID: 441678); euphorbin B (PubChem CID: 16197485); hoslunddiol (PubChem CID: 44257619); euscaphic acid (PubChem CID: 471426); kigelin (PubChem CID: 22295076); anacardic acid (PubChem CID: 167551); forksolin (PubChem CID: 47936); docosanol (PubChem CID: 12620); lauric acid (PubChem CID: 3893); myristic acid (PubChem CID: 11005); emodin (PubChem CID: 3220); chrysophanol (PubChem CID: 10208); physcion (PubChem CID: 10639); aloesin (PubChem CID: 160190); rumexoside (PubChem CID: 637097); torachrysone (PubChem CID: 5321977); boeravinone A (PubChem CID: 14018346); boeravinone B (PubChem CID: 14018348); boeravinone C (PubChem CID: 13940642); coccineone B (PubChem CID: 44420939); pinocembrin (PubChem CID: 68071); cardamonin (PubChem CID: 641785); pheophorbide a (PubChem CID: 5323510); aesculetin glucoside (PubChem ID: 5359437); santin (PubChem ID: 5281695); scoparone (PubChem CID: 8417); muzigadial (PubChem CID: 442346); drimenin (PubChem CID: 442202); warburganal (PubChem CID: 72502); polygodial (PubChem CID: 72503); celerythrine (PubChem CID: 2703); nepodin (PubChem CID: 100780)
Keywords: Anti-viral, HIV, Southern Africa, In vitro, Medicinal plants, Flavonoids, Phenolic acids, Terpenoids
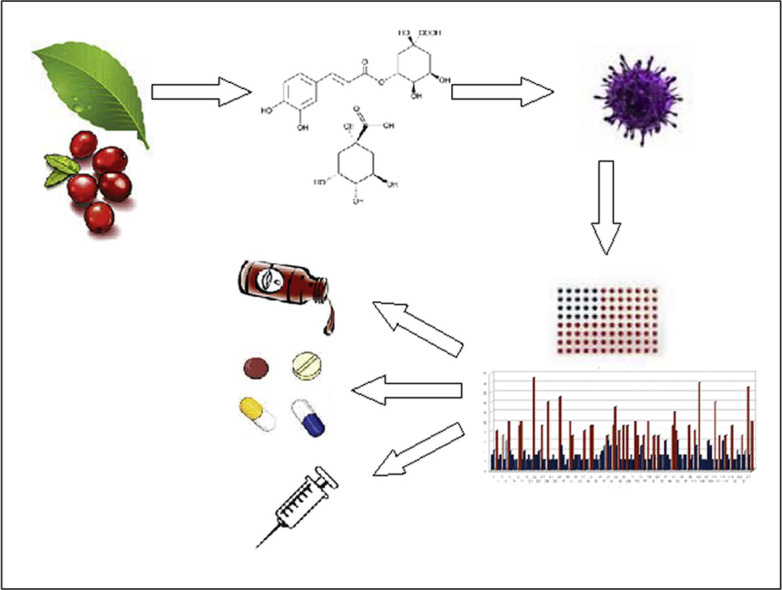
Graphical abstract
1. Introduction
Southern Africa is remarkably rich in plant diversity with approximately 30 000 flowering plant species which equates to nearly 10% of the higher plants globally (van Wyk, 2001). Plants have been used medicinally for centuries and the medicinal plant trade is still prominent today. According to the World Health Organization (WHO), up to 80% of people living on the African continent, equating to more than a half billion people, use traditional medicines to meet their primary health care needs. Nonetheless, the industry is not yet exploited to its full capacity. In South Africa, for example, around 3 000 medicinal plant species are frequently used in plant-based medicines, however less than 40 indigenous species have been commercialized to some degree (van Wyk, 2008).
The statistics on HIV in the southern African region emphasizes its devastating effects. In 2015, there were 36.7 million people living with HIV. Worldwide, 2.1 million people became newly infected with HIV (UNAIDS, 2016). In 2012, sub-Saharan Africa accounted for 70% of all people newly infected with HIV and 71% of all people living with HIV (UNAIDS, 2013). Collectively eastern and southern Africa are home to 6% of the global population, but accounted for 52% of all people living with HIV and nearly half the approximated 2.3 million people who became infected with HIV in 2012 (UNAIDS, 2013).
Anti-retroviral therapy (ART) is an effective treatment for people living with HIV. The standard treatment seeks to suppress the HIV replication cycle and halt disease progression. Antiretroviral therapy is significant in improving the life of people living with HIV, however the drugs have many disadvantages, including resistance, toxicity, limited availability, and lack of curative effect (Chinsembu and Hedimbi, 2010a). The potential of HIV becoming resistant to anti-retroviral (ARV) treatment has become an increasing concern since it was first reported decades ago (De Clercq, 1995). As pathogens become drug resistant, the need for development of new medicines is being realized all over the world. These shortcomings open avenues for the use of natural products in the management of HIV/AIDS.
2. Methodology
Electronic searches of Science Direct, PubMed central and Google Scholar were undertaken with search terms “HIV”, “medicinal plants”, “Africa”, “anti-viral” and “southern Africa”. Initially publication titles were screened for suitability and plant species, active compounds and their mode of action were documented from primary literature sources. Ethnobotanical surveys in other African countries such as Ethiopia (Asres et al., 2001), Uganda (Lamorde et al., 2010), Cameroon (Mbaveng et al., 2011), Zimbabwe (Viol et al., 2016), Namibia (Chinsembu and Hedimbi, 2010) and Zambia (Chinsembu, 2016) also assisted in identifying plants traditionally used for management of HIV or HIV symptoms. The inclusion criteria were: (1) plants should have a record of traditional/popular use for infectious or viral diseases, HIV treatment or symptoms similar to HIV infection, (2) if not traditionally/popularly used, plants should be closely related to plants with popular use and HIV activity identified by means of in vitro assays, (3) plants should have been identified scientifically, (4) should be native to the southern African region and (5) anti-HIV activity should be within acceptable ranges. Clinical relevant concentrations have been defined as IC50 of<50 or<100 µg/ml for extracts and at<5 or<25 µM for individual compounds and have been applied as a selection criterion in this study (Agarwal et al., 2014; Butterweck and Nahrstedt, 2012; Cos et al., 2006; Gertsch, 2009). Since traditional refers to plants with a long history of use, and HIV being a relatively new disease, the use of these plants are referred to as “popular” or “popularly used” against HIV.
3. Screening methods for anti-HIV activity in medicinal plants
Many plants have been traditionally used to treat viral infections and other ailments. Investigation of these claims led to the discovery of numerous plant derived anti-HIV compounds which are widely distributed in nature (Singh et al., 2011). Therefore, screening medicinal plants provides an opportunity for the discovery of HIV inhibitors with lower or no toxicity and/or side effects (Narayan et al., 2013). Biologically active substances harvested from plants, can be found in any organ of the plant, although leaf material is most traditionally used (Narayan et al., 2013).
Various laboratory based investigations have been conducted using plant extracts and isolated compounds employing a variety of assays. Most of the tests are performed on the enzymes reverse transcriptase (RT), integrase (IN) and protease (PR), proteins involved in activation of viral genes or cells that are infected with viruses or pseudoviruses, and the activity determined by an indicator such as MTT or luciferase activity. The MTT assays are based on the reduction of the yellow coloured 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) by mitochondrial dehydrogenases of metabolically active cells. In metabolically active cells, blue formazan is produced which is measured spectrophotometrically to indicate cell viability in assays of cell proliferation and cytotoxicity (Cos et al., 2002; Shoemaker et al., 2004). These targets aim to determine the inhibition or reduction of viral infection on various levels, and present various advantages and disadvantages to be considered in evaluating anti-viral activity ( Table 1).
Table 1.
A summary of the most popular anti-HIV assays presenting the advantages and disadvantages of each assay.
| Assay | Target | Advantages | Disadvantages | Reference |
|---|---|---|---|---|
| HIV-1 Reverse Transcriptase (RT) assay | Reverse Transcriptase is an enzyme that converts the viral RNA genome to viral DNA. | The assay kits can be acquired from various companies. | False positives due to unspecific binding of plant compounds such as tannins to proteins and inhibit RT. RT uses magnesium or manganese divalent ions as co-factors. The presence of palladium and iron is known to induce irreversible inhibition of RT. Sulfated polysaccharides show anti-HIV activity with aqueous extracts by destabilizing the glycoprotein complex and/or inhibiting reverse transcriptase. | (Bessong and Obi, 2006, Bolton et al., 2002, Chukwujekwu et al., 2014, Collins et al., 1998, Eldeen et al., 2011, Filler and Lever, 1997, Kapewangolo et al., 2013, Klos et al., 2009, Tshikalange et al., 2008a, Wang et al., 2014). |
| HIV-1 Integrase (IN) assay | Integrase enzyme is required for the integration of the synthesized viral double stranded DNA into the chromosome in the nucleus. | The Xpress HIV-1 IN Assay Kit can be acquired from various companies. | False positives obtained due to unspecific binding of plant compounds to proteins. | (Bessong and Obi, 2006, Jiang et al., 2010, Klos et al., 2009, Wang et al., 2014) |
| HIV-1 Protease (PR) assay | Protease enzyme cleaves viral polyproteins into structural and functional components which are assembled to form progeny virions. | Assay kits such as the HIV-II PR HIV-FRET (fluorescence resonance energy transfer) and the recombinant HIV-1 protease solution can be acquired from various companies. | False positives can be obtained due to unspecific binding of plant compounds to proteins. | (Bessong and Obi, 2006, Harnett et al., 2005, Jiang et al., 2010, Kapewangolo et al., 2013, Klos et al., 2009, Wang et al., 2014). |
| HIV-1 p24 assay | It is an enzyme-linked immunosorbent assay used to detect and quantify HIV-1 p24 core protein. HIV-1 inhibition is determined by a decrease in viral p24 antigen levels measuring absorbance at 450 nm. | The antigen assay kit can be acquired from various companies. | False positives can be obtained due to unspecific binding of plant compounds to proteins. | (Klos et al., 2009). |
| Cell based assays infected with isolated HIV strains or pseudovirions | HIV cell cultures are maintained and added to cells containing plant extracts and compounds. The activity is measured using the MTT assay. Cells infected with a recombinant virus is obtained by the transfection of a plasmid containing the luciferase gene and luciferase activity is measured. | The assay does not rely on inhibition of a single enzyme, and more targets can be tested using a virus or pseudovirion transfection. | Constituents with antioxidant activity result in too high MTT activity as it is a redox-based assay. Free thiols lead to the reduction of MTT to the formazon product and therefore inaccurate results are obtained. Plant compounds such as (iso) flavonoids, stabilize the firefly luciferase reporter enzyme increasing the bioluminescent signal, probably due to the direct interaction of the compounds with the firefly luciferase reporter enzyme thereby increasing its half-life and stabilizing the enzyme activity. Compounds stabilizing the firefly luciferase reporter protein give false positives. | (Auld et al., 2008, Cos et al., 2002, Ngwira et al., 2015, Prinsloo et al., 2010, Shoemaker et al., 2004, Sotoca et al., 2010, Wang et al., 2014) |
| NF-κB activation assay | Cells are stably transfected with a plasmid containing the firefly luciferase gene driven by the HIV-LTRpromoter, highly dependent on NF-κB activation induced by TNFα. High expression of luciferase activity reflects NF-κB activation through the canonical pathway. | Plant-derived antiviral compounds interfering with HIV-1 LTR promoter regulatory proteins are unlikely to generate drug-resistant HIV strains. | Plant compounds such as (iso) flavonoids, stabilize the firefly luciferase reporter enzyme increasing the bioluminescent signal, probably due to the direct interaction of the compounds with the firefly luciferase reporter enzyme thereby increasing its half-life and stabilizing the enzyme activity. Compounds stabilizing the firefly luciferase reporter protein give false positives. | (Auld et al., 2008, Sotoca et al., 2010, Tshikalange et al., 2008b) |
| Hela-Tat-Luc assay | The Hela-Tat-Luc cells are stably transfected with the plasmid pcDNA3-TAT together with a reporter plasmid LTR-Luc. HIV-1 LTR is highly activated in this cell line as a consequence of high levels of intracellular Tat protein. | Plant-derived antiviral compounds interfering with HIV-1 LTR promoter regulatory proteins are unlikely to generate drug-resistant HIV strains. | Plant compounds such as (iso) flavonoids, stabilize the firefly luciferase reporter enzyme increasing the bioluminescent signal, probably due to the direct interaction of the compounds with the firefly luciferase reporter enzyme thereby increasing its half-life and stabilizing the enzyme activity. | (Auld et al., 2008, Sotoca et al., 2010, Tshikalange et al., 2008b) |
| Hela-Tet-ON-Luc assay | Extracts active in both NF-κB (>50% inhibition) and Tat (>30% inhibition) assays, evaluated by Hela-Tet-ON assay to discard nonspecific luciferase inhibitory activity. | Plant-derived antiviral compounds interfering with HIV-1 LTR promoter regulatory proteins are unlikely to generate drug-resistant HIV strains. Eliminate the nonspecific luciferase activity. | (Auld et al., 2008, Sotoca et al., 2010, Tshikalange et al., 2008b) |
RT converts the viral RNA genome to viral DNA using its polymerase domain (RNA dependent DNA polymerase activity), while the ribonuclease H (RNase H) domain degrades the RNA component from the intermediary RNA/DNA complex. The enzyme also has a DNA-dependent DNA polymerase function and most clinically available RT drugs, therefore target this enzyme. Numerous studies focused on the HIV-1 RT enzyme and various protocols have been employed measuring ethyl-3H thymidine triphosphate (3H TTP) by RT using polyadenylic acid-oligodeoxythymidilic acid (polyA-oligodT) as template primer in the presence and absence of a test substance such as isolated compounds or plant extracts (Ali et al., 2002, Bessong et al., 2005). Various kits are used for determining the inhibition of enzymes and viral components such as the Capture ELISA kit (GenxBio Health Science, India) (Chinnaiyan et al., 2013) and HIV-RT colourimetric enzyme-linked-immunosorbent serologic assay (ELISA) kit obtained from Roche Diagnostics, Mannheim, Germany (Chukwujekwu et al., 2014, Eldeen et al., 2011, Kapewangolo et al., 2013, Klos et al., 2009, Tshikalange et al., 2008a, Wang et al., 2014) or a purified recombinant HIV-1 RT enzyme (Merck, Darmstadt, Germany) (Kapewangolo et al., 2013). Several interactions and measures have been identified to optimise the assay conditions. It has been found that HIV-1 RT uses magnesium or manganese divalent ions as a co-factor (Bolton et al., 2002) and that palladium and iron might also affect the assay as they are responsible for irreversible inhibition of RT and subsequent reduction in virus proliferation (Filler and Lever, 1997). Since ions of various metals are accumulated by plants and therefore present in plant extracts, these ions may be present in and might affect the outcomes. Most methodologies describing the inhibition of HIV-1 RT by crude plant extracts do not take into consideration the effect of metal ions in regulating the activity of HIV-1 RT (Bessong and Obi, 2006). Consequently, it would be important to determine metal ions in plant extracts prior to screening in order to avoid false inhibitory observations at the screening stage.
IN, in conjunction with accessory viral proteins, is required for the integration of the synthesized viral double stranded DNA into the chromosome in the nucleus of the host cell. The HIV-1 integrase (HIV-1 IN) enzyme has also been employed on extracts and compounds such as catechins in various studies using the Xpress HIV-1 IN Assay Kit (Express Biotech International, USA) or in an in vitro model (Jiang et al., 2010). A recombinant HIV-1 IN of E. coli origin (Wang et al., 2014) and the evaluation against the 3’ processing activity of HIV-1 IN have been performed on extracts and compounds (Bessong et al., 2005). The unspecific binding of plant compounds to proteins is, however, mostly not considered.
PR cleaves viral polyproteins into structural and functional components which are assembled to form progeny virions (Bessong and Obi, 2006). The protease enzyme has also been investigated in various assays such as the fluorometric detection of HIV-PR activity using HIV-II PR HIV-FRET (fluorescence resonance energy transfer) (AnaSpec Inc., USA) and a recombinant HIV-1 protease solution (Bachem, Switzerland). The glycohydrolase enzymes are found in the eukaryotic host cell's Golgi apparatus and are responsible for glycosylation of proteins. Inhibition of the glycohydrolase enzymes decreases the infectivity of the HIV virion, as the HIV envelope proteins are highly glycosylated during the life cycle of the virus. Glucosidase was found to be partly responsible for the glycosylation of HIV gp120 (Harnett et al., 2005, Kapewangolo et al., 2013, Klos et al., 2009). Escherichia coli expressing recombinant HIV-1 PR has also been used to detect the inhibitory effects of samples on HIV-1 PR by observing the bacterial growth curve (Jiang et al., 2010, Wang et al., 2014).
An ELISA kit (another enzyme-linked immunosorbent assay) is also available to detect and quantify HIV-1 p24 core protein using the HIV-1 p24 Antigen Assay kit (Beckman Coulter, Miami, FL, USA) (Klos et al., 2009) and can be distinguished from the cell based assays. Cell based assays are commonly used with various different cell types and viruses. The CXCR4-tropic (NL4-3) or CCR5-tropic (NL-AD87) wild-type reference viruses (Louvel et al., 2013) and HIV-1c binding and entry assay on PBMCs have been described (Leteane et al., 2012). The utilised format “iFIGS” (Infection format of “Fusion-induced gene stimulation”) represents an in vitro infection system in human HeLa cells. Thereby, upon infection with HIV, the reporter gene will be induced in a quantifiable fashion as beta galactosidase allows quantification of inhibitory effects of compounds or extracts (Lubbe et al., 2012). HIV-1 pseudovirions and viruses has been used (Ngwira et al., 2015, Prinsloo et al., 2010, Wang et al., 2014) and Hela-Tat-Luc cells that are stably transfected with for instance a plasmid pcDNA3-TAT together with a reporter plasmid LTR-Luc indicates protein activation. Therefore the HIV-1 LTR is highly activated in this cell line as a consequence of high levels of intracellular Tat protein (Tshikalange et al., 2008b). Isolated HIV strains (strain HTLV-IIIB/LAI) obtained from the culture supernatant of a HIV-infected HUT-78 cell line have been tested and cell viability was evaluated using the MTT assay (Cos et al., 2002). African green monkey kidney cells (Vero) have also been used (Dang et al., 2011) and linked to cytotoxicity assays on MT-4 cells (Maregesi et al., 2010a, Maregesi et al., 2010b).
Even though the MTT assay is generally applied to determine cell viability in in vitro assays, very little or no consideration is given to the possibility of constituents with antioxidant potential that result in extremely high MTT readings, and might provide false positive results. The stabilization of the luciferase gene is also often not considered, even though many plant components might provide false positive results (Auld et al., 2008, Sotoca et al., 2010). The cytotoxicity of extracts and compounds are often also neglected and therefore the Selectivity Index (SI) which is achieved by dividing the cytotoxic concentration (CC50) by the effective inhibitory concentration (EC50) or Therapeutic Index (TI) which is achieved by dividing the cytotoxic concentration (CC50) by the non-cytotoxic concentration that inhibits/protects 50% uninfected cells (ID50), are not reported. A value of more than 1 is indicative of an extract that is selective in inhibition and not only toxic to both the virus and the cells (Cos et al., 2002).
In vitro assays have an important role in determining anti-HIV activity, mindful of the pitfalls and false positives that might arise from compounds in plant crude extracts. The lack of absorption, distribution, metabolism and excretion (ADME) characteristics and the lack of direct correlation with in vivo/clinical doses, limit the scope of application of in vitro bioassays and add to the challenges faced by in vitro screening (Agarwal et al., 2014). It is often inaccurate to relate in vitro results from enzyme or protein inhibition assays to the in vivo situation, and these should be considered in screening of botanicals and botanical preparations. The hydrolysis and phase-II transformation of compounds within the in vivo system contribute to the incompatibility of in vitro results to the in vivo situation. Hydrolysis of flavonoids may result in formation of non-conjugated analogues able to induce a specific biological response to an even larger extent than the non-hydrolysed extract. Hydrolysis will also provide a site for conjugation which will result in excretion of the conjugate in the urine and the bile (Day et al., 1998). The type of flavonoid, the position and nature of the sugar may also affect the metabolism in the intestine and passing to the large intestine for absorption there (Barrington et al., 2009, Hollman, 2004). Once the aglycone is absorbed it is quickly metabolised to form phase-II conjugates, mostly sulphates and glucuronides or O-methylation, which have a major impact on their activity as well as the ability of the body to excrete compounds (Barrington et al., 2009, Hollman, 2004). These phase-II conjugates, obviously are not representative of the compounds in the original plant extract or botanical preparation anymore, and challenge the results obtained from in vitro assays. Well-known flavonoids such as kaempferol, apigenin and galangin are only present in low concentrations in plasma as they are nearly exclusively present as conjugated glucuronides in the systemic circulation after phase-II biotransformation (Barrington et al., 2009, Chen et al., 2003, Hollman, 2004). Quercetin is often reported in anti-viral assays and is known for its specific absorption and hydrolysis patterns. Quercetin glucoside is absorbed in the small intestine, whereas quercetin rutinoside is absorbed from the colon after deglycosylation (Hollman, 2004). Caffeic acid and ferulic acid, also well-known anti-viral compounds are examples of compounds subjected to transformation, both metabolised to glucuronides although not very effectively (Spencer et al., 1999). No glucuronides have, however, been observed for chlorogenic acid and anthocyanidin glycosides which are rapidly absorbed and able to withstand deglycosylation reactions in humans (Hollman, 2004).
It is therefore important to consider the factors of transformation and conjugation of compounds in the intestines. Transformation of these compounds during absorption, or transformation by the liver in the human body affect the extrapolation of in vitro results to the in vivo situation. ADME characteristics for many compounds are not available, and therefore in vitro assays based on enzymes and cell based assays with protein targets are useful in screening and aims to link the traditional use of plants to activity. In vitro to in vivo extrapolation is however very complex, with more information needed to determine the in vivo situation for compounds from a botanical preparation with numerous compounds possibly being active components.
4. Anti-HIV activity of medicinal plant compounds
A number of medicinal plants have been reported to have anti-HIV properties (Chinsembu and Hedimbi, 2010a, Cos et al., 2002, Singh et al., 2005). The structural diversity and adaptation ability to various environmental conditions have resulted in development of a range of defense compounds with various biological activities, therefore plant secondary metabolites represent a huge source for novel anti-HIV drugs that may be functional against HIV. Guided fractionation of these crude extracts has provided a platform for the discovery of novel and known anti-HIV compounds. With the emergence of drug resistant HIV variants in patients receiving ARV treatment, the search for novel effective inhibitors of HIV has accelerated. A condensed summary of some of the most active and most studied classes of plants compounds are provided in Table 2.
Table 2.
A summary of important compound groups with examples with strong anti-HIV activity.
| Compound group | Example | Mode of action | Species/ Family | Reference |
|---|---|---|---|---|
| Alkaloids | Papavarine | Inhibits HIV replication in vitro and reduces HIV protein production | Papaver somniferum L. (Papaveraceae) | (Vlietinck et al., 1998) |
| Coumarins | Suksdorfin | Inhibits HIV replication | Lomatium suksdorfii (S. Watson) J.M. Coult.&Rose (Apiaceae) | (Lee et al., 1994, Vlietinck et al., 1998) |
| Flavonoids | Quercetin 3–0-(2-galloyl) α-L arabinopyranose | Anti-HIV-1 integrase activity | Acer mono Maxim (Sapindaceae) | (Kim et al., 1998) |
| Saponins | Escin | Moderate anti-HIV-1 protease activity | Aesculus chinensis Bunge (Sapindaceae) | (Kim et al., 1998) |
| Phenolics | Gallic acid | Exhibits HIV integrase and reverse transcriptase activity | Terminalia chebula Retz. (Combretaceae) | (Yadav et al., 2009) |
| Quinones | Conocurvone | Showed potent anti-HIV activity | Conospermum incurvum Lindl. (Proteaceae) | (Decosterd et al., 1993) |
| Lignans | Demethoxyepiexceisin | Good anti-HIV activity in vitro | Litsea verticillata Hance (Lauraceae) | (Hoang et al., 2002) |
Known compounds with anti-HIV activity include chloroquine, genistein and strictinin. Chloroquine, a 9-aminoquinoline, has a range of antiviral effects varying from the endocytosis to the exocytosis of viral particles, and, in addition, down regulates IFN-g and TNF-a production and TNF-receptors. It has shown activity against HIV-1, SARS coronavirus, human coronavirus OC43 and EBOV infection in vivo in newborn mice (De Clercq, 2014). Strictinin and green tea catechins are active against the Influenza virus, Herpes simplex and HIV-RT (Saha et al., 2010) and genistein inhibits arenaviral hemorrhagic fever infection in vitro (Vela et al., 2010). Citrus limon (lemon) (Lackman-Smith et al., 2010), Psidium guajava (guava) (Mao et al., 2010), Ricinus communis (castor oil) (Bessong et al., 2005), Zingiber officinalis (ginger) (Feng et al., 2011), Mangifera indica (mango) and Cocos nucifera (coconut) are all examples of commonly used food plants with proven anti-viral activity.
Often a specific genus is identified with activity against a microorganism. The Amaryllidaceae is known for their alkaloid compounds, of which many have been identified with anti-viral activity. The major group of secondary metabolites occurring in the Amaryllidaceae is isoquinoline alkaloids with various structural variations (Nair and Van Staden, 2014). Lycorine, narciclasine and pretazettine are well known compounds isolated from this family. Narciclasine inhibits protein synthesis at the step of peptide bond formation whereas pretazettine strongly inhibits the activity of RNA-dependent DNA polymerase (RT), from various oncogenic viruses by binding to the enzyme (Fennell and van Staden, 2001). Other important compounds known to treat other ailments from this family include crinine and galanthamine with central nervous system activity due to their resemblance to morphine and codeine skeletons (Fennell and van Staden, 2001). Studies on a specific family such as the Amaryllidaceae might also yield novel mechanisms and compounds for the treatment of HIV and can be a directed research focus in the search for anti-viral agents.
5. Inventory of medicinal plant species
Medicinal plants with proven anti-HIV properties usually have other medicinal values, which may be an indication for these to be used as new drugs against the virus and its commonly associated infections (Asres et al., 2001). Table 3 provides a summary of plants investigated from southern Africa and where present, the compounds that have been isolated, the activity and the possible mode of action of the compounds indicates the specific uses of the medicinal plants to treat HIV.
Table 3.
An inventory of plants from the southern African region with anti-HIV activity, presenting their distribution, traditional uses, assays and results of the assays obtained.
| Plant species | Distribution | Traditional use | Model/Control | Active constituents | Mode of action | Pharmacological activity/Concentration ranges | Reference |
|---|---|---|---|---|---|---|---|
| Acacia brevispica Harms (Leguminosae) | Widespread in Africa, found in Sudan, Ethiopia, Somalia, Kenya, Zaire, Angola and South Africa | Traditionally used to treat infectious diseases | Tetrazolium based colometric assay using HIV-1 (strain III b) and HIV-2 (strain ROD). Azidothymidine (AZT) as positive control. | None tested, coumaric and ferulic acid, quercetin, kaempferol isoquercitrin and hyperin present. | HIV-1, 80% methanol leaves extract IC50 = 64.8 µg/ml and water extract IC50= 60.4 µg/ml. | (Maregesi et al., 2010a, Maregesi et al., 2010b, Mueller-Harvey et al., 1987) | |
| HIV-2 Water extract of shoots IC50 = 88.7 µg/ml. | |||||||
| Acacia tortilis (Forssk.) Hayne (Leguminosae) | Senegal, Nigeria, Sudan, Kenya, Tanzania, Israel, Jordan, Arabian Peninsula, Southern Africa and Namibia. | Traditionally used to treat infectious diseases, vermifuge, skin infections, edema and allergic dermatoses. | Tetrazolium based colorimetric assay using HIV-1 (strain III b) and HIV-2 (strain ROD). AZT as positive control. | HIV-1 80% methanol stem bark extract IC50 = 8.5 µg/ml and water extract IC50 = 4.2 µg/ml. | (Maregesi et al., 2010a, Maregesi et al., 2010b) | ||
| HIV-2 80% methanol stem bark extract IC50 = 23.6 µg/ml. | |||||||
| Adansonia digitata L (Bombaceae) | Endemic to Africa. | Antimicrobial, anti-malarial, diarrhea, anemia, asthma, antiviral, anti-oxidant and anti-inflammatory. | HIV-RT colorimetric ELISA assay, HIV-1 PR | Various flavonoid glycosides and proanthocyanidin compounds in the leaves and the epicatechin compounds in fruit pulp. | HIV-1 RT | (Rahul et al., 2015, Sharma and Rangari, 2016) | |
| HIV-FRET and a recombinant HIV-1 protease solution. Nevirapine as positive control. | Root bark extract 26.5% and 12.2% leaf extract inhibition at 50 μg/ml. Fruit pulp extract (100 μg/ml) 5.9% inhibition. Nevirapine (100 nM) 27.5% inhibition. | ||||||
| HIV-PR | |||||||
| Leaf extract and fruit pulp extract (50 μg/ml) 75% and 74% inhibition respectively. | |||||||
| Root bark extract 35% inhibition. | |||||||
| Alepidea amatymbica Eckl.&Zeyh. (Apiaceae) | Widely distributed in southern Africa from the eastern Cape northwards to eastern Zimbabwe | Colds, coughs, rheumatism, HIV, wounds and to wash divining bones. | A cell-based assay targeting the replication of prototypic CXCR4-tropic (NL4–3) or CCR5-tropic (NL-AD87) HIV-1 strains. Positive and negative controls included in the assay. | Rosmarinic acid and caffeic acid. | Compounds bind to the catalytic core of purified HIV-1 integrase and blocks both activities of this enzyme. | EC50 of aqueous extract at 22 μg/ml against the HIV-1 strain NL4–3 and 85 μg/ml against NL-AD87. | (Castro and Wyk, 1994; Louvel et al., 2013) |
| Artemisia afra Jacq. ex Willd. (Asteraceae) | Kenya, Tanzania, Uganda, north to Ethiopia and south to South Africa and Namibia. | Perfume, treat smallpox, infectious diseases and stomach ache. Anti-HIV for A. annua, but not A. afra. | HIV-1 (IIIB) and HIV-2 (ROD) tested. Efavirenz (EFV) as control and Aspalathus linearis as negative drug. | Many volatile and non-volatile compounds. | Tea infusion IC50 = 2.0 µg/ml. | (Asres et al., 2001, Liu et al., 2009, Lubbe et al., 2012) | |
| A validated cellular system by testing each sample at various dilutions in triplicates. | Extract against HIV- 1 and HIV-2 EC50 of>123.5 µg/ml. | ||||||
| Aspilia pluriseta Schweinf. (Compositae) | DRC, Burundi, Rwanda, Uganda, Kenya, Tanzania, Malawi, Mozambique, Zambia, Zimbabwe and South Africa | Traditionally used for infection and rheumatic diseases, fevers and malaria. | HIV (strain HTLV-IIIB/LAI) evaluating cytotoxicity and viral cytopathic effect. | Thiarubrine-A, a dithiacyclohexadiene polyacetylen from the leaves | Target the interaction between the viral envelope glycoprotein gp120 and the CD4 receptor. The virus adsorp to the cells, but also virus-induced syncytium (giant cell) formation is inhibited. In addition, sulfated polysaccharides may also directly interfere with the binding of HIV particles to the heparin sulfate proteoglycan of the cell surface. | Ethanolic extract EC50 = 16.3, SI>12 with complete protection. | (Cos et al., 2002) |
| Bersama abyssinica Fresen. (Melianthaceae) | From Guinea Bissau through the coastal countries of West Africa except Benin, east to Eritrea and Ethiopia and south to Angola, Zambia, Zimbabwe and Mozambique | A purgative to treat abdominal pain, colic, diarrhea, cholera, intestinal worms, amoebiasis, dysentery, rabies, syphilis, gonorrhea and malaria, cancer, rheumatism, as an aphrodisiac, diabetes mellitus, feverish pains, loss of appetite, debility, jaundice, leprosy, burns, ulcers, wounds, convulsions, snakebites, migraine, headache, colds, hemorrhoids and epilepsy. | HIV-RT colorimetric ELISA kit with Doxorubicin as positive control and the cytotoxicity and antiviral activity assays based on evaluating cell death caused by plant extract toxicity and inhibition of viral cytopathic effect with HIV-I (IIIB) and HIV-2 (ROD). | The stem bark contain 2 bufadienolides, which are cardiac glycosides, sterols and mangiferin. | Methanol extracts of leaves, bark and root inhibition of 89.17%, 85.11% and 95.21% respectively at 200 µg/ml with IC50 of 11.95, 18.75 and 9.38 µg/ml. Methanol root bark SI of 3.8 against HIV-1. | (Asres et al., 2001, Mbaveng et al., 2011) | |
| Boerhavia coccinea Mill. (Nyctaginaceae) | South-eastern United States, Africa including Namibia and South Africa, Asia, Australia, and South America. | Traditionally used to treat infectious diseases | Tetrazolium based colometric assay using HIV-1 (strain III b) and HIV-2 (strain ROD). AZT as positive control. | Boeravinone A, Boeravinone B, Boeravinone C, Coccineon B, Coccineon C, Coccineon D, Coccineon A | HIV-1, 80% methanol shoot extract IC50 = 54.8 µg/ml and water extract IC50= 37.1 µg/ml. | (Maregesi et al., 2010a, Maregesi et al., 2010b, Patil and Bhalsing, 2016) | |
| Boerhavia erecta L. (Nyctaginaceae) | Native to the United States, Mexico, Central America and western South America, but now cosmopolitan in tropical and subtropical regions. In Africa its distribution extends from West Africa, eastwards to Somalia and down to South Africa. In Asia, it occurs in India, Java, Malaysia, the Philippines, China and the Ryukyu Islands. | Traditionally used to treat infectious diseases | HIV-1 IN assay | Procyacanidin, catechin, epicatechin, quercetin, kaempferol and isorhamnetin glucosides present. | HIV-IN | (Patil and Bhalsing, 2016, Stintzing et al., 2004) | |
| Quercetin-3-O-rutinoside IC50 = 10 µg/ml and isorhamnetin-3-O-rutinoside IC50 = 22 µg/ml isolated from stem bark. | |||||||
| Bridelia micrantha (Hochst.) Baill. (Euphorbiaceae) | Native to most of sub-Saharan Africa except South Africa and Namibia. | HIV, diarrhea, sore eyes, stomach aches and abortifacient. | HIV-1 RT. Isolated compounds also evaluated on HIV-1 IN. | ß-sistosterol and friedelin isolated from roots. | Ethyl acetate fraction of roots IC50 = 7.3 μg/ml. No effect on HIV-1 IN. | (Bessong and Obi, 2006) | |
| Bulbine alooides (L.) Willd. (Asphodeliaceae) | Distribution not well documented, occurs in South Africa. | Burns, cracked lips, diarrhea, herpes simplex, itching, skin rash, ringworm, vomiting, HIV and wounds. | HIV-1 p24 antigen assay. | HIV-1 PR Tannin- dereplicated ethanol extract IC50 = 94.3 µg/ml. Ritonavir IC50 = 5.3 ng/ml | (Gail et al., 2015, Klos et al., 2009, Maroyi, 2014) | ||
| HIV-1 RT, positive control nevirapine. The HIV-1 PR assay, HIV-FRET and a recombinant HIV-1 protease solution. Positive control pepstatin and ritonavir. | |||||||
| Cassia abbreviata Oliv. (Caesalpiniaceae) | Widespread in Africa, from Somalia to South Africa. | Backache, abdominal pains, diarrhea, constipation, tooth ache, fever, ulcers, STI's such as syphilis and gonorrhea. Root and bark used as a general blood cleanser, appetite enhancer and reducing HIV levels. | HIV-1c (MJ4) p24 antigen assay with AZT as positive control. Therapeutic index determined by neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells using the Spearman-Karber formula and by the End point titration technique with acyclor as positive control. | Cassia roots contains anthocyanin, anthra- noids, anthraquinones, polyphenols and tannins. | Ethanolic root extract EC50 = 102.8 μg/ml. | (Leteane et al., 2012, Viol et al., 2016) | |
| P24% inhibition | |||||||
| Tannin-containing = 55.1% and tannin-free = 38.5%. | |||||||
| Methanol leaf and root extracts therapeutic index of 7.5 and 15 respectively and EPTT of 103 for the root. | |||||||
| Centella asiatica (L.) Urb. (Apiaceae) | It is native to wetlands in Asia, but due to its invasive nature now found world-wide including southern Africa. | Used to treat various diseases, such as gonorrhea, syphilis, diabetes, fever, leprosy, wound healing, gastro-intestinal ailments, HIV, asthma and neurosis. | Contains various essential oils, asiatic acid, asiaticoside, madecassic acid, terminolic acid, quercetin, kaempferol and luteolin. Also phenylpropane and acetate metabolites. | Immunomodulatory effect of aqueous or alcoholic extract. | Asiatic acid and an anti-HIV agent with IC50 of 36 and 8 μg/ml. | (Brinkhaus et al., 2000, Lamorde et al., 2010, Yasurin et al., 2015) | |
| Combretum adenogonium Steud. ex A.Rich (Combretaceae) | Widespread in Africa to the south in Botswana and Zimbabwe. | Traditionally used to treat infectious diseases. | Tetrazolium based colorimetric VSV T2 inhibition assay. AZT as positive control. | Flavonoids, tannins, saponins, phytosterols, sitosterol and stigmasterol. | HIV – 1 | (Jordaan et al., 2011, Maregesi et al., 2008) | |
| 80% methanol leaf extract IC50 = 2.7 μg/ml and water = 4.8 μg/ml. | |||||||
| 80% methanol stem bark extract IC50 = 4.4 μg/ml and water = 5.6 μg/ml. | |||||||
| HIV-2 | |||||||
| 80% methanol stem bark extract IC50 = 23.9 µg/ml and water =>67.5 μg/ml. | |||||||
| Combretum molle R.Br. ex G.Don (Combretaceae) | Wide distribution, from Saudi Arabia, Yemen and Ethiopia, to South Africa in the south and westwards to West Africa, DRC and Angola. | HIV, abdominal pains, snake bites, leprosy, fever, convulsions and Hookworm infection. | HIV-1 RT. Isolated compounds were additionally evaluated on HIV-1 IN. | Tannin, ellagitannin, pentacyclic triterpene glucosides namely punicalagin, arjunglucoside and sericoside. | Inhibit RNA-dependent-DNA polymerase activity of HIV-1 RT | IC50 = 37.5 µg/ml (water) and 9.5 µg/ml (methanol) against RDDP and IC50 of 13.7 µg/ml (water) and 9.7 µg/ml (methanol) against RNase H. | (Bessong et al., 2005, Jordaan et al., 2011) |
| Combretum paniculatum Vent. (Combretaceae) | West Africa, east to Ethiopia, south to Angola, Mozambique and South Africa. | Eye diseases, infectious diseases and leprosy. | Cytotoxicity and antiviral activity assays based on evaluating cell death caused by plant extract toxicity and inhibition of viral cytopathic effect with HIV-I (IIIB) and HIV-2 (ROD). | Pheophorbide a, pheophorbide, cardamonin, pinocembrin, quercetrin and kaempferol. | Acetone leaf extract SI of 6.4 and 32.0 for HIV-1 and HIV-2 and the methanol extract with SI of 4.7 for HIV-1. | (Asres et al., 2001) | |
| Dichrostachys cinerea (L.) Wight&Arn. (Leguminosae) | Native to Africa, Indian subcontinent and North Australia and introduced to the Caribbean and parts of Southeast Asia. | Headache, toothache, dysentery, elephantiasis, leprosy, syphilis, coughs, as an anthelmintic, purgative epilepsy, diuretic and laxative. | Neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells with acyclor as positive control. Determined the reduction factor (RF). | Friedelin, friedlan-3-ol, sitosterol and amyrin, octacosanol, hentricontanol, coumarins imperatorin, marmesin and aesculetin | Therapeutic index of 7.5 for leaf and 3.7 for root methanol extract. | (Viol et al., 2016) | |
| Dodonaea angustifolia L.f. (Sapindaceae) | Southern Africa to Arabia, as well as in Australia and New Zealand | Colds, influenza, measles, sore throat, oral thrush, stomach ailments, fever, itchy skin, rheumatism, hemorrhoids, pneumonia, tuberculosis and skin rashes. | HIV-1 (IIIB) and HIV-2 (ROD) infected MT-4 cell lines. MTT colorimetric assay used for evaluation. | Pinocembrin, santin, 2-hydroxy-15,16-epoxyceloda-3,13(16),14-trien-18-oic acid, 5,7,4'-trihydroxy-3,6-dimethoxyflavone, ent-16-hydroxy-labdan-3α,8β-dihydroxy,13(14)-en-15,16-olide and 5,6,7-trihydroxy-3,4'-dimethoxyflavone. | HIV-1 | (Asres et al., 2001) | |
| Leaf acetone and methanol extract EC50 of 27.7 and 21.3 µg/ml and SI of 3.9 and 4.9 respectively. | |||||||
| Elaeodendron croceum (Thunb.) DC. (Celastraceae) | South Africa and eastern escarpment of Zimbabwe. | Similar species E. transvaalensis used for HIV. | Recombinant HIV strain in an MT-2 VSV-pseudotyped recombinant virus assay. | Digitoxigenin-3-O-glucoside, 4’-O-methyl epigallocatechin dimethyl-1, 3, 8, 10-tetra-hydroxy-9-methoxy-peltogynan, canophyllol, 30-hydroxylup-20(29)-en-3-one, 30-Hydroxylupeol, tingenin B, tingenone, galacticol, ouratea proanthocyanidin, ouratea proanthocyanidin-nona-O-acetate. | VSV-pseudotype HI virus inhibition. Extract active at 100 ng/ml. Pure compound 90% inhibition at 0.2 µM. | (Archer and Wyk, 1998; Prinsloo et al., 2010) | |
| Elaeodendron schlechterianum (Loes.) Loes. (Celastraceae) | Widespread in the southern and tropical east African countries of Kenya, Tanzania, Mozambique, Malawi, Zambia and Zimbabwe. | Traditionally used to treat infectious diseases. | HIV-1 RT. Isolated compounds were additionally evaluated on HIV-1 IN and viral proteins (NF-κB and Tat). Tetrazolium based colorimetric assay using HIV-1 (strain III b) and HIV-2 (strain | Cardiac glycosides and tannins namely 4’-O-methylepigallocatechin, 4’-O-methylgallocatechin, 4’,4’’-di-O-methyl-prodelphinidin B4 or 4’-O- methylgallocatechin-(4α→8)-4’-O-methylepigallocatechin. ROD). AZT as positive control. | HIV-1, 80% methanol stem bark extract IC50 = 7.1 µg/ml and water extract IC50= 28.7 µg/ml. | (Archer and Wyk, 1998; S. M. Maregesi et al., 2010) | |
| 80% methanol root bark extract IC50 = 5.4 µg/ml and water extract IC50= 66.3 µg/ml. | |||||||
| HIV-2 | |||||||
| 80% methanol leaves extract IC50 = 16 µg/ml. | |||||||
| 80% methanol stem bark extract IC50 = 11.1 µg/ml and water extract IC50= 46.8 µg/ml. | |||||||
| 80% methanol root bark extract IC50 =8.7 µg/ml. | |||||||
| Potent inhibitory activity in both the NF-κB and Tat assays with inhibitory activity of 76% and 75%. No activity of pure compounds. | |||||||
| Elaeodendron transvaalense (Burtt Davy) R.H.Archer (Celastraceae) | Widespread in southern Africa, including Namibia. | HIV, colds, skin rashes, fever, candidiasis, dysmenorrhea and stomach ache. | HIV-1 RT. Isolated compounds were additionally evaluated on HIV-1 IN and viral proteins (NF-κB and Tat). Mesuol as positive control. | 3-Oxo-28-hydroxylbetuli-20(29)-ene and 3,28-dihydroxylbetuli-20(29)-ene | IC50 of 80 µg/ml (water) and 131 µg/ml (methanol) against RDDP and IC50 of 31.2 µg/ml (water) and 30 µg/ml (methanol) against RNase H. | (Archer and Wyk, 1998; Bessong et al., 2005; Mthethwa et al., 2014; Tshikalange et al., 2008a) | |
| Chloroform and ethyl acetate extracts 64% and 76% inhibition respectively (1 µg/ml) in the NF-κB assay. Chloroform and ethyl acetate extracts>70% inhibition at 15 µg/ml. | |||||||
| Elephantorrhiza goetzei (Harms) Harms (Leguminosea) | Wide distribution in south central Africa. | Pain, sores, sexually transmitted infections (STIs), gastro-intestinal disorders, microbial infections and genito-urinary system disorders. | Neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells with acyclor as positive control. Determined the reduction factor (RF). | Phenolic compounds, coumarins, flavonoids, saponins, stilbenoids, tannins and triterpenoids from bark, leaves and roots. | Methanol root extract therapeutic index of 1.9. | (Viol et al., 2016) | |
| Emilia coccinea (Sims) G.Don (Compositae) | Native to DR Congo, Burundi, Sudan, Kenya, Uganda, Tanzania, Malawi, Zambia, Angola, Zimbabwe and Mozambique. | Traditionally used to treat infectious diseases, ulcers, craw-craw, ringworm, fever and convulsions in children. | Tetrazolium based colometric assay using HIV-1 (strain III b) and HIV-2 (strain ROD). AZT as positive control. | Alkaloids, phenolics, flavonoids terpenoids and cardiac glycosides. | HIV-1 | (Edeoga et al., 2005, Maregesi et al., 2010a, Maregesi et al., 2010b) | |
| 80% methanol shoot extract IC50 = 73.7 µg/ml and water = 27.9 µg/ml. | |||||||
| Euphorbia hirta L. (Euphorbiaceae) | Worldwide distribution. Very common in pan-tropic and partly subtropic areas including China, India, Philippines, Australia, Africa and Malaysia. | Traditionally used to treat infectious diseases, female disorders, respiratory ailments, cough, coryza, bronchitis, asthma, worm infestations in children, dysentery, jaundice, pimples, gonorrhea, digestive problems and tumors. | HIV-1 RT. The cytotoxic effect was measured by means of the colorimetric MTT assay. | Alkanes, triterpenes, phytosterols, tannins, polyphenols and flavonoids. | Inhibits HIV-1, 2 reverse transcriptase. | (Gyuris et al., 2009) | |
| Dose-dependent inhibition of | |||||||
| RT on HIV-1, HIV-2 and SIVmac251 IC50 = 38, 22 and 177 μg/ml respectively. | |||||||
| Aqueous and 50% methanolic extracts HIV-1,2 activity with IC50 = 9 μg/ml and 5 μg/ml. | |||||||
| Euphorbia tirucalli L. (Euphorbiaceae) | Wide distribution in Africa, in northeastern, central and southern Africa. | Traditionally used to treat infectious diseases, cancer, tumors, warts asthma, cough, earache, neuralgia, rheumatism, toothache, | Tetrazolium based colorimetric assay using HIV-1 (strain III b) and HIV-2 (strain | Many compounds such as euphol, euphorbin and tirucallin | HIV-1 | (Maregesi et al., 2010a, Maregesi et al., 2010b) | |
| ROD). AZT as positive control. | Water extract (root) IC50 = 23.9 μg/ml. | ||||||
| HIV-2 | |||||||
| Water extract (root) IC50 = 56.2 μg/ml. | |||||||
| Ficus sycomorus L. (Moraceae) | Native to Africa also grows naturally in Lebanon, Cyprus, Madagascar and naturalized in Israel and Egypt. | Traditionally used to treat infectious diseases. | Tetrazolium based colorimetric assay using HIV-1 (strain III b) and HIV-2 (strain ROD). AZT as positive control. | Various volatile compounds | HIV-1 | (Maregesi et al., 2010a, Maregesi et al., 2010b, Maregesi et al., 2008) | |
| 80% methanol stem extract IC50 = 8.3 µg/ml and water extract IC50= 37.6 µg/ml. | |||||||
| HIV-2 | |||||||
| 80% methanol stem bark extract IC50 = 16.1 µg/ml and water extract IC50= 107 µg/ml. | |||||||
| Flacourtia indica (Burm. f.) Merr. (Salicaceae) | Tropical Africa south to northern South Africa, Swaziland, Madagascar, India, Sri Lanka, Indonesia and China | Snakebite, arthritis, STI, cough, pneumonia, and bacterial throat infection. | Neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells with acyclor as positive control. Determined the reduction factor (RF). | Phenolic glycosides, lignin, β-sitosterol, polysaccharides, flavonoids, condensed tannins, alkaloids, terpenoids, sugars, coumarin such as scoparone and aesculetin, also flacourtin, pyrocatechol, homaloside D, poliothrysoside, β- sitosterol, β-D-glucopyranoside, ramantoside&butyrolactone lignan disaccharides. | Methanol leaf and root extract therapeutic index of 0.9 and 1.3 respectively. Root RF of 103. | (Patro et al., 2013, Viol et al., 2016) | |
| Gymnosporia senegalensis (Lam.) Loes. (Celastraceae) | Sub-Saharan Africa from Senegal to Eritrea and south to northern Namibia, Botswana and South Africa. Also found in southern Spain, North Africa, Afghanistan to India, Aldabra and Madagascar. | Gastro-intestinal troubles, schistosomiasis mouthwash for toothache, tooth-abscesses and mouth-infections, sores, eye-trouble, gastric ulcers, tertiary syphilis, female complaints, leprosy, dysentery and Blennorrhea. | Neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells with acyclor as positive control. Determined the reduction factor (RF). | The leaves and branches contain dulcite and tannins. The leaves contain sterol, flavonol, slavonic glycoside, saponosides, flavone derivatives and tannins. | Methanol extracts of leaf, root and twigs therapeutic index of 3.8, 3.8 and 1.2 respectively and RF of 103 for all extracts. | (Viol et al., 2016) | |
| Helichrysum spp. (30) investigated with the highest activity in Helichrysum populifolium | Most species occur in Africa, including Madagascar, South Africa and Namibia, also Southern Europe, south-west Asia, southern India, Sri Lanka and Australia. | Coughs, colds, fever, infection, headaches, menstrual pain, HIV and wound dressing. | The reporter cell line HeLa-SXR5, stably expresses the CD4 receptor and the CXCR4/CCR5 chemokine receptors DeCIPhR method on a full virus model. | Di- and tricaffeoylquinic acids; 3, 4 dicaffeoylquinic acid; 3, 5 dicaffeoylquinic acid and 4,5 dicaffeoylquinic acid. | Extracts tested at 25 and 2.5 μg/ml. | (Gail et al., 2015, Heyman et al., 2015) | |
| Helichrysum populifolium DC (Asteraceae). | Efavirenz positive control and negative control PBS/5% DMSO. | Anti-HIV IC50 = 12–21 µg/ml. | |||||
| Hoslundia opposita Vahl (Lamiaceae) | Widespread in tropical Africa and south to South Africa. | Traditionally used to treat infectious diseases, gonorrhea, cystitis, coughs, fever, wounds, convulsions, sores, mental disturbances, abdominal pains, snake bites and for the relief of swellings. | Tetrazolium based colorimetric assay using HIV-1 (strain III b) and HIV-2 (strain ROD). AZT as positive control. | 5,7-dimethoxy-6-methylflavone, hoslunddiol and euscaphic acid with 5,7-dimethoxy-6-methylflavone HIV- 1 RT activity of 52%, at 100 µg/ml. | HIV-1 | (Maregesi et al., 2010a, Maregesi et al., 2010b, Mujovo et al., 2008; Prakash and Staden, 2007) | |
| Leaves extract (water) IC50 = 14.8 µg/ml. | |||||||
| HIV-2 | |||||||
| Leaves extract (water) IC50 = 17.4 µg/ml. | |||||||
| Hypoxis hemerocallidea Fisch., C.A.Mey.&Avé-Lall. (Hypoxidaceae) | Native to southern Africa from South Africa as far north as Mozambique and Zimbabwe. | Headaches, stomach ailments, dysentery, dizziness, burns, cancer, HIV, symptoms of benign prostrate hypertrophy, diabetes, high blood pressure, pimples, wounds, skin rush, dermatitis, mental disorders and general tonic for good health. | HIV-1 RT assay and the therapeutic index determined by neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells using the Spearman-Karber formula and by the End point titration technique with acyclor as positive control. Determined the reduction factor (RF). | Phytosterolglucosides (β-sitosterol), diglucoside hypoxoside, aglycone rooperol, sterols and sterolins. | Remarkably stable CD lymphocyte counts concurrently with the decrease in serum p24 HIV antigen and expression of the HLA-DR CD8 lymphocyte activation marker on HIV patients. Show interference with the efflux of nevirapine across intestinal epithelial cells and potentially increase the bioavailability of this anti-retroviral drug when taken concomitantly. | Inhibit HIV-1 RT. Methanol extract of tuber therapeutic index of 15 and RF of 103. | (Gail et al., 2015, Ncube et al., 2013, Viol et al., 2016) |
| Hypoxis sobolifera Jacq.(Hypoxidaceae) | Endemic to South Africa | Traditionally used directly in HIV/AIDS or symptoms/conditions closely associated with this disease. | HIV-1 RT and PR assay. | ≥50% inhibition of HIV-1 RT and HIV-1 PR. Aqueous and ethanolic extracts inhibition at 0.2 µg/ml against HIV-1 RT. | (Klos et al., 2009) | ||
| Kigelia africana (Lam.) Benth. (Bignoniaceae) | Throughout tropical Africa and to the south in South Africa, Namibia and Swaziland. Introduced as an ornamental to Cape Verde, Madagascar, Iraq, Pakistan, India, China, South-East Asia, Australia, Hawaii and Central and South America. | Traditionally used to treat infectious diseases, HIV, fainting, anemia, sickle-cell anemia, epilepsy, respiratory ailments, hepatic and cardiac disorders, and nutritional illnesses such as kwashiorkor, rickets, wasting, leprosy, impetigo, and worm infestations in the blood. | Tetrazolium based colorimetric assay using HIV-1 (strain III b) and HIV-2 (strain ROD). AZT as positive control. Neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells with acyclor as positive control. Determined the reduction factor (RF). | Various naphthoquinones, iridoids, sterols, coumarins, flavonoids and alkaloids kigelin, β-sitosterol, 1,3-dimethylkigelin and ferulic acid have been isolated from the bark, quercetin | HIV-1 | (Atawodi and Olowoniyi, 2015, Maregesi et al., 2010a, Maregesi et al., 2010b, Rukunga et al., 2002, Saha et al., 2010, Viol et al., 2016)(Lamorde et al., 2010) | |
| Stem bark water extract IC50 = 83.2 µg/ml | |||||||
| Fruit | |||||||
| 6.93% RT inhibition at 100 µg/ml and 5.21 at 50 µg/ml. | |||||||
| Leaves | |||||||
| 33% RT inhibition at 100 µg/ml and 11.3 at 50 µg/ml. | |||||||
| Therapeutic index of methanol extract of bark and fruit of 1.2 for both and 103 and 104 RF values respectively. | |||||||
| Lannea schweinfurthii Engl. (Anacardiaceae) | Kenya, Uganda, Tanzania, Zanzibar, Malawi, Mozambique, Zambia, Zimbabwe, Swaziland and South Africa. | Treatment of infectious diseases. | Tetrazolium based colorimetric assay using HIV-1 (strain III b) and HIV-2 (strain ROD). AZT as positive control. | HIV-1 | (Maregesi et al., 2010a, Maregesi et al., 2010b) | ||
| 80% methanol stem bark extract IC50 = 7.1 µg/ml and water extract IC50= 53.2 µg/ml. | |||||||
| HIV-2 | |||||||
| 80% methanol stem bark extract IC50 = 9.9 µg/ml and water extract IC50= 89.4 µg/ml. | |||||||
| Leonotis leonurus (L.) R.Br. (Lamiaceae) | Native to southern Africa. | Fevers, headaches, coughs, dysentery, remedy for snake bite and charm to keep snakes away. | HIV-1 p24 antigen assay. | No anti-HIV compounds, contains sterols, diterpenes, triterpenoids, tannins, flavonoids, alkaloids, quinines and saponins. | Tannin-dereplicated ethanol extracts HIV-1 PR inhibition IC50 = 120.6 µg/ml. Ritonavir control IC50 = 5.3 ng/ml | (Gail et al., 2015, Klos et al., 2009) | |
| HIV-1 RT. Positive control nevirapine. HIV-1 PR assay, HIV-FRET and a recombinant HIV-1 protease solution used. | |||||||
| Positive control for HIV-1 PR acetyl pepstatin and ritonavir. | |||||||
| Leonotis nepetifolia (L.) R.Br. (Lamiaceae) | It is native to tropical Africa and southern India, Latin America and the West Indies. | Traditionally used to treat infectious diseases and HIV | Tetrazolium based colorimetric assay using HIV-1 (strain III b) and HIV-2 (strain ROD). AZT as positive control. | Ethanolic extract cytotoxic with SI<1 against HIV-1. | HIV-1 | (Cos et al., 2002, Lamorde et al., 2010, Maregesi et al., 2010a, Maregesi et al., 2010b) | |
| HIV (strain HTLV-IIIB/LAI) evaluating cytotoxicity and viral cytopathic effect. | 80% methanol leaves extract IC50 = 32.8 µg/ml and water extract IC50= 34.9 µg/ml. | ||||||
| HIV-2 | |||||||
| 80% methanol leaves extract IC50 = 119 µg/ml. | |||||||
| Lobostemon trigonus (Thunb.) H.Buek (Boraginaceae) | Endemic to South Africa | Decoction for wound healing, ulcers and ringworm or as an infusion for blood purification. | HIV-1 RT assay and HIV-II PR assay. | The genus is known to contain naphthoquinone derivatives, pyrrolizidine alkaloids, cyclitols, phenolic acids, tannins and the ureide allantoin | Aqueous extract of leaves HIV-1 RT activity at IC50 = 49 µg/ml. No HIV-II PR activity. | (Harnett et al., 2005) | |
| Myrothamnus flabellifolia Welw. (Myrothamnaceae) | South Africa, Angola, Botswana, Madagascar, Zimbabwe, Mozambique, Malawi, Tanzania, Namibia, Zambia and Kenya. | Treatment of chest complaints (smoke of burning leaves), wounds (in ointments for topical application), and to treat cough, influenza, mastitis, backaches, kidney disorders, hemorrhoids, abdominal pains, scurvy, halitosis and gingivitis. | HIV-1 RT assay. | Polyphenolic compounds and 3, 4, 5 tri-O-galloylquinic acid. Pinocarveol, pinocarvone, and β-selinene are the most abundant volatiles, along with α-pinene, limonene, and a few other terpenoids. | Abolished virus entry into the host cell by blocking viral attachment to the cell surface. Directly interacted with viral particles, leading to the oligomerisation of envelope proteins as demonstrated for the essential viral glycoprotein D (gD). | Inhibition non-competitive, with IC50 for 3, 4, 5, tri-O-galloylquinic acid of 5 μM for M-MLV and 34 μM for HIV-1. | (Gechev et al., 2014, Gescher et al., 2011, Moore et al., 2007) |
| Ozoroa reticulata (Baker f.) R. Fern.&A. Fern (Anacardiaceae) | Widely distributed from southern Ethiopia, Zaire to southern Africa. | Traditionally used to treat infectious diseases, kidney and liver complaints, chest pain, diarrhea, schistosomiasis, ulcers and hernias, otitis, colic, dysentery, muscle pains, fever, hypertension and throat infections. | Tetrazolium based colorimetric assay using HIV-1 (strain III b) and HIV-2 (strain ROD). AZT as positive control. | 6-pentadecylsalicylic acid, toxic to brine shrimp and anacardic acid and ginkgoic acid as cytotoxic components. | HIV-1 | (Maregesi et al., 2010a, Maregesi et al., 2010b) | |
| Leaves 80% methanol = 16.2 µg/ml and water = 81.4 µg/ml. | |||||||
| Stem bark 80% methanol = 11.6 µg/ml and water = 15.8 µg/ml. | |||||||
| Root bark 80% methanol = 20.6 µg/ml | |||||||
| Pelargonium sidoides DC. (Geraniaceae) | Native to South Africa and Lesotho. | Gonorrhea, diarrhea, dysentery, a prolapsed rectum and intisila, colic, wounds, acute bronchitis, cold, acute rhino sinusitis, influenza and herpes virus. | Transfection with the proviral HIV- 1 plasmid. HIV-1 particles pseudotyped with the VSV protein. Positive controls AZT and Efavirenz. | Gallic acid, umckalin, catechin, oleic acid, linoleic acid and coumarins. | Interferes directly with viral infectivity and blocks the attachment of HIV-1 particles to target cells, protecting them from virus entry. | HIV-1 attachment inhibitor with EC50 = 8.13 µg/ml. EC50 for gallocatechin-(4β-8)- gallocatechin 7.3 µg/ml, epigallocatechin-(4β-8)-gallocatechin 6.3 µg/ml, epigallocatechin 42.5 µg/ml and gallocatechin 28.4 µg/ml. | (Helfer et al., 2014, Moyo and Van Staden, 2014) |
| Peltophorum africanum Sond.(Ceasalpiniaceae) | Native from southern DR Congo to South Africa and Swaziland. Cultivated in Kenya, Tanzania, Madagascar, Australia and the United States. | HIV, wounds, toothache, sore throat, cough, tuberculosis, abdominal disorders, diarrhea, dysentery, menorrhagia, infertility. | HIV-1 RT assay. Isolated compounds were additionally evaluated on HIV-1 IN. | Contains flavonoids and C-galloylglycosides namely (+)-catechin, bergenin and betulinic acid. | Gallotannin inhibited RDDP and RNase H RT IC50 = 6.0 and 5.0 µM, respectively, and abolished the 3’-end processing activity of IN (100 µM). Bergenin no effect on IN (100 µM). | (Bessong et al., 2005) | |
| Catechin no effect on RT, moderate activity on HIV-1 IN. | |||||||
| HIV-NL4–3: Betulinic acid = 0.04 µg/ml, HIV-1JRCSF: Betulinic acid = 0.002 µg/ml. | |||||||
| Plectranthus barbatus Andrews (Lamiaceae) | Worldwide, found in sub-Saharan Africa as an invasive species | Anti-spasmodic, gastric disturbances, malaria, candida, managing HIV/AIDS, and opportunistic infections, herpes simplex, herpes zoster and skin rashes. | HIV-1 PR assay. Acetyl pepstatin (AP) was used as a positive control. | Various compounds isolated including betulinic acid, caffeic acid, diterpenes and forskolin. | PR activity could be attributed to diterpenoids. | HIV-1 PR | (Alasbahi and Melzig, 2010, Chinsembu and Hedimbi, 2010b, Kapewangolo et al., 2013, Kim et al., 2013) |
| HIV-1 RT assay, doxorubicin as positive control. | Ethyl acetate extract 70% inhibition at 100 µg/ml (IC50 = 62.07 µg/ml) | ||||||
| Acetyl-pepstatin 97% at10 µg/ml and its IC50 was 0.3 µg/ml. | |||||||
| HIV-1 RT | |||||||
| 50% inhibition. | |||||||
| Doxorubicin, IC50 = 25 µg/ml. | |||||||
| Prunus africana (Hook. f.) Kalkman (Rosaceae) | Wide distribution in Africa, from central to South Africa and on the islands of Bioko, São-Tomé, and Grande Comore. | Fevers, malaria, wound dressing, arrow poison, stomach pain, purgative, HIV, kidney disease, appetite stimulant and gonorrhea. | HIV-1 RT assay | Ferulic acid, n-docosanol, lauric acid myristic acid, β-sitostenone and β-sitosterol | Stem bark ethanol extract % RT at 100 µg/ml = 99.2 and 50 µg/ml = 71.2 | (Gail et al., 2015, Kadu et al., 2012, Rukunga et al., 2002) | |
| Rhus chirindensis Baker f. (Anacardiaceae) | Widespread in African from Tanzania in the north to the Cape in the south. | Treating heart complaints, strengthen the body, stimulate circulation and treatment of rheumatism and mental disorders and sexually transmitted diseases. | Neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells with acyclor as positive control. Determined the reduction factor (RF) | Flavonoids and triterpenoids. | Methanol root extract therapeutic index of 3.8. | (Viol et al., 2016) | |
| Rumex bequaertii De Wild. (Polygonaceae) | Europe through Asia to China, Vietnam and Indonesia, Africa, mainly in the east from Eritrea and Somalia to South Africa. | Traditionally used for infection and rheumatic diseases, purgative, rheumatism, colic, stomach-ache and abdominal pains, abscesses, schistosomiasis and headaches | HIV (strain HTLV-IIIB/LAI) evaluating cytotoxicity and viral cytopathic effect, examined spectrophotometrically by the MTT-method. | Emodin, chrysophanol, physcion, anthraquinones aloesin, rumexoside, orientaloside, torachrysone, nepodin, nepodin-8-O-β-D-glucopyranoside, torachrysone and torachrysone-8-O-β-D-glucopyranoside. | Target the interaction between the viral envelope glycoprotein gp120 and the CD4 receptor. The virus adsorp to the cells, but also virus-induced syncytium (giant cell) formation is inhibited. Sulfated polysaccharides may also directly interfere with the binding of HIV particles to the heparin sulfate proteoglycan of the cell surface. | Ethanolic extract EC50 = 17.69 with SI>11% and 89% cell protection. | (Cos et al., 2002, Vasas et al., 2015) |
| Sclerocarya birrea (A. Rich.) Hochst. (Anacardiaceae) | Widespread throughout the semi-arid deciduous savannas of much of sub-Saharan Africa. | Hypertension, dysentery, stomachache, gastro-enteritis, anti-cough remedy, hypertension, antihyperglaecemic, diarrhea, dysentery, malaria, general tonic and sexually transmitted diseases. | Neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells with acyclor as positive control. Determined the reduction factor (RF). | Phenolic compounds, proanthocyanidins, gallotannins and flavonoids such as quercetin 3-O-alpha-l-(5' '-galloyl)-arabinofuranoside. | Methanol extract of bark therapeutic index of 1.9 and RF of 103. | (Viol et al., 2016) | |
| Securidaca longipedunculata Fresen. (Polygalaceae) | Tropical and subtropical areas of Africa with protected status in South Africa. | Stomach complaints, tuberculosis, | The anti-HIV and anti-SIV activities and toxicities of compounds | Caffeoylquinic acids: 3,4,5-tri -O-caffeoylquinic | Binds irreversibly to gp120 and inactivates virus. | EC50 for 3,4,5-tri-O-caffeoylquinic | (Asres et al., 2001, Mahmood et al., 1993, Muazu and Kaita, 2008, Viol et al., 2016) |
| wound dressing, rheumatism, syphilis, cough, diarrhea, syphilis and typhus. | assessed in C8166 cells infected with HIV-1 III-B, | acid and 4,5-di-O-caffeoylquinic acid as well as Caffeic acid, rosmarinic acid and synapoic acid. | acid HIV 1 and HIV 2 = 0.32 µg/ml and no activity, 4,5-di-O-caffeoylquinc acid at 0.6 and 8 µg/ml, caffeic acid at 0.16 µg/ml and no activity and synapoic acid at 200 and>200 µg/ml. Rosmarininc acid 40 and 100 µg/ml. | ||||
| HIV-2 Rod or SIV MacCell viability of virus-infected and uninfected control. | Methanol extract of root therapeutic index of 3.8 and RF of 103. | ||||||
| Evaluated by the MTI-Formazan method. AZT as control. Neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells with acyclor as positive control. Determined the reduction factor (RF). | |||||||
| Sutherlandia frutescens (L.) R.Br. (Fabaceae) | Endemic to southern Africa | HIV, relieving cold, influenza, chicken pox, diabetes, varicose veins, piles, backache, rheumatism, physical and mental stress. | Non-radioactive HIV-RT colorimetric | High levels of free amino acids, non-protein amino acids such as canavanine and GABA, cyclitol pinitol, flavonols and triterpenes including SU1. | Canavanine is an inhibitor of nitric oxide synthase and has potential for the treatment of septic shock, a condition associated with advanced stages of AIDS. | Leaves and flowers>50% inhibition against HIV-1 RT. No HIV-II PR activity (≥50%) when assayed at 0.2 mg/ml. | (Gail et al., 2015, Harnett et al., 2005, van Wyk and Albrecht, 2008) |
| ELISA kit with fluorometric detection of HIV-II PR. | |||||||
| Terminalia mollis M.A.Lawson (Combretaceae) | Widespread in Africa occurring in West Africa, Angola, DR Congo, Uganda, Kenya, Tanzania, Zambia and Zimbabwe. | Treatment of infectious diseases. | Tetrazolium based colorimetric VSV T2 inhibition assay. AZT as positive control. | Tannins and saponins. | HIV-1 | (Maregesi et al., 2010a, Maregesi et al., 2010b, Maregesi et al., 2008) | |
| 80% methanol stem bark extract IC50 = 5.9 µg/ml and water extract IC50= 9.8 µg/ml. | |||||||
| 80% methanol root bark extract IC50 = 2.06 µg/ml and water extract IC50= 4.4 µg/ml. | |||||||
| HIV-2 | |||||||
| 80% methanol stem bark extract IC50 = 13.6 µg/ml and water root bark extract IC50 = 16.4 µg/ml. | |||||||
| Terminalia sericea Burch. ex DC. (Combretaceae) | Endemic to Africa from Tanzania and the DR of Congo southwards to South Africa. | Diabetes, diarrhea and STI. | HIV-1 RT and viral proteins (NF-κB and Tat) assays. Reference drug Adriamycin. Mesuol as a reference inhibitor of NF-κB. Neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells with acyclor as positive control. Determined the reduction factor (RF). | Triterpenoids, saponins, tannins and Anolignan B | Extracts tested at 50 µg/ml and the active extracts were further tested at 25, 15, 5 and 1 µg/ml. | HIV-1 RT | (Eldeen et al., 2011, Tshikalange et al., 2008a, Viol et al., 2016) |
| IC50 = 43 µg/ml | |||||||
| Adriamycin (IC50 = 100 µg/ml. | |||||||
| No activity on NF-κB and Tat. | |||||||
| Methanol extract of leave and roots with therapeutic index of 1.2 and 1.9 respectively. | |||||||
| Tithonia diversifolia (Hemsl.) A.Gray (Asteraceae) | Native to Mexico, Central America and Cuba, naturalized in tropical parts of Asia, Africa and Pacific islands. | Traditionally used for infections, rheumatic diseases, ascariasis and diarrhea. | HIV (strain HTLV-IIIB/LAI) evaluating cytotoxicity and viral cytopathic effect, examined spectrophotometrically by the MTT-method. | Sulfated polysaccharides, polyphenolic compounds such as hydrolysable tannins, diversifolin, diversifolin methyl ether and tirotundin. | Target the interaction between the viral envelope glycoprotein gp120 and the CD4 receptor. The virus adsorp to the cells, but also virus-induced syncytium (giant cell) formation is inhibited. In addition, sulfated polysaccharides may also directly interfere with the binding of HIV particles to the heparin sulfate proteoglycan of the cell surface. diversifolin, diversifolin methyl ether, tirotundin | HIV-1 | (Cos et al., 2002) |
| They inhibited the DNA binding activity of the transcription factor NF-κB, resulting in a decreased production of inflammatory mediators, such as cytokines and chemokines. | EC50 =>1.60 µg/ml with SI<1. Water sub-fraction EC50 = 0.04 µg/ml with SI>461 with complete cell protection. | ||||||
| Vernonia amygdalina Delile (Asteraceae) | Wild in most countries of tropical Africa, from Guinea east to Somalia and south to north-eastern South Africa, and in Yemen. | Traditionally used for infections, rheumatic diseases, ascariasis, hepatitis, malaria, diabetes, worms, tonsillitis, fever, STI, HIV, measles, skin problems and chicken pox. | HIV (strain HTLV-IIIB/LAI) evaluating cytotoxicity and viral cytopathic effect, examined spectrophotometrically by the MTT-method. | Gallic acid, chlorogenic acid, dicaffeoyl acids, quercetin, vernolide, octahydrovernodalin, vernonioside A3, vernodalol, vernomenin, vernolide, vernolepin, vernodalin and vernodalinol. | HIV-1 inhibition EC50 =>19.66 µg/ml. | (Cos et al., 2006, Lamorde et al., 2010, Toyang and Verpoorte, 2013) | |
| SI<1. | |||||||
| Vernonia stipulacea Klatt (Asteraceae) | Zambia, Tanzania, Malawi, Mozambique, Zimbabwe; widespread in tropical Africa, extending to South Africa. | HIV, diarrhea, fever, flu and contraceptive. | HIV-1 RT assay and HIV-II PR assay. | Weak HIV-1 RT activity at>100 µg/ml. | (Bessong et al., 2005) | ||
| Warburgia salutaris (G.Bertol.) Chiov. (Canellaceae) | Botswana, Namibia, Tanzania, Zambia, Mozambique, South Africa, Swaziland, Malawi and Zimbabwe. | Malaria, respiratory complaints such as cold and cough and sexually transmitted diseases and HIV. | Neutralization test to determine non-cytotoxic concentration (ID50) that inhibits/protects 50% of the monolayer cells against destruction by the virus compared to uninfected cells with acyclor as positive control. Determined the reduction factor. | Muzigadial, 9B-Octahydro-6, 6, 9Atrimethylnaphtho[1, 2c] furan-1-(3H)-one (drimenin), 5, 10-Dihydro-6, 7-dimethyl-4H-benzo [5, 6] cyclohepta [1, 2-b]-furan, warburganal and polygodial. | Methanol root extract therapeutic index of 1.2 and RF of 103. | (Lamorde et al., 2010, Viol et al., 2016) | |
| Zanthoxylum davyi Waterm. (Rutaceae) | Native to South Africa, western Swaziland and eastern Zimbabwe. | Traditionally used in treatment of sexually transmitted diseases, chest pains, wounds, toothache, coughs, pleurisy, toothache, snakebites, heal sores, sore throat and aphrodisiac. | HIV-1 RT and viral proteins (NF-κB and Tat). | Benzo[c]phenanthridine alkaloids, chelerythrine, dihydrochelerythrine, bocconoline, 6-hydroxydihydrochelerythrine and 6-methoxy-7-demethyldihydrochelerythrine, together with 4-methoxy-1-methyl-2(1H)-quinolinone and the uncommon lignan meso-sesamin. | 70% acetone extract | (Tarus et al., 2006, Tshikalange et al., 2008b) | |
| Mesuol as positive control. | Nf-κB 54% inhibition at 15 µg/ml, Tat 50% inhibition at 15 µg/ml. | ||||||
| Ximenia americana L. (Olacaceae) | Tropical and temperate regions. | Contagious diseases, stomach complaints, placenta expulsion, internal parasitism and worm infestations. | HIV-1 (IIIB) and HIV-2 (ROD) infected MT-4 cell lines. MTT colorimetric assay used for evaluation. | Proanthocyanidins and a triterpenoid saponin. | Inhibits HIV-1 replication | HIV-1 | (Asres et al., 2001) |
| Senegal to Ethiopia and south to South Africa. | Stem bark extract | ||||||
| EC50 = 8.3–27.7 µg/ml and selectivity | |||||||
| indices 3.9–4.9. Hydroalcohol extract | |||||||
| EC50 = 8.3 µg/ml (HIV-1) and 27.1 µg/ml | |||||||
| (HIV-2) with SI of 4.5 and 1.4 respectively. | |||||||
| Ziziphus mucronata Willd. (Rhamnaceae) | Botswana, Namibia-Caprivi, DR Congo, southern Tanzania, Mozambique, Zambia, South Africa and Zimbabwe | HIV, diarrhea, dysentery, stomach ulcers, fever, anti-peristalsis, skin diseases, anti-inflammatory, menorrhagia, infertility | HIV-1 RT assay and HIV-II PR assay. | RDDP | (Bessong et al., 2005) | ||
| IC50 = 77.5 µg/ml (water) and 81.5 µg/ml (methanol) HIV-1 RT IC50>100 µg/ml (water) and 75 µg/ml (methanol) |
The distribution of each species is presented and the traditional use of the species therefore reflect the distribution of the species as it is strongly linked to the availability of a species in a region. Of the 56 plant species (excluding the group of Helichrysum species) documented in this study; 20 have reported popular use to treat HIV or HIV symptoms, 20 have been reported for treatment of infectious diseases and another 13 other anti-viral activity such as influenza and chicken pox, whereas the mode of action was scientifically reported in only 13 plants. The other 3 plants have been tested for anti-HIV activity based on similarity of plants with popular or tested anti-HIV or anti-viral activity such as Elaeodendron croceum (E. transvaalensis and E. schlechterianum with popular use for HIV and infectious diseases) and Leonotis leonurus (L. nepetifolia with popular use for HIV). The species that are similar to those commonly used for HIV have been included, as ethnobotanical documentation are often incomplete and species are often misidentified. The activity of “related” species might therefore be species that have also been commonly used to treat HIV or other viral infections, but not correctly identified or documented.
6. Phytochemistry of anti-viral components
By analyzing and comparing the information on plants from the southern African region popularly used for HIV treatment, or tested anti-HIV activity, several compounds and compound groups have been repeatedly reported, and by evaluation of these compounds and compound groups, been classified into three distinct groups. The three groups identified are:
-
-
Flavonoids such as quercetin in Vernonia amygdilana and flavonoid glycosides in Sutherlandia frutescens.
-
-
Terpenoid and terpenoid glycosides such as sericoside in Combretum molle, betulinic acid in Peltophorum africanum including the cardiac glycosides found in the two Elaeodendrom species E. croceum and E. schlechteranum
-
-
The phenolic acids such as gallic acid, rosmarinic acid and caffeic acid from Alepidea amatymbica and their conjugated acids such as dicaffeoylquinic acids (DQCA) from Vernonia amygdilana, di- and tricaffeoylquinic acids (TCQA) from various Helichrysum species and trigalloylquinic acids (TGQA) from Myrothamnus flabellifolius and Securidaca longipedunculata.
Sufficient evidence for the antiviral activity of the phenolic acids has accumulated over the years and is still explored in many medicinal plant species (Heyman et al., 2015). Some of the dicaffeoylquinic acids (DCQAs) and the dicaffeoyltartaric acids (DCTAs) are selective inhibitors of HIV-1 IN at concentrations between 150 and 840 nM. The compounds that have been reported to date include 3,5-DCQA, 1-methoxyoxalyl-3,5-DCQA (1-MO-3,5-DCQA), 1,5-DCQA, 3,4-DCQA and 4,5-DCQA, as well as a related dicaffeoyltartaric acid (L-chicoric acid) (McDougall et al., 1998). Some of the caffeoyl- and galloylquinic acids is nonspecific in its anti-HIV activity and binds to the gp120 protein to inhibit virus replication, preventing binding to the CD4 receptor. They are also not specific to the HI virus as similar anti-viral activity was also observed with HSV type 1. The galloyl derivatives were previously shown to inhibit the in vitro activities of both HIV-RT and cellular DNA polymerases, in particular DNA polymerase a (Mahmood et al., 1993). McDougall et al. (1998), however, strongly argue that the activity of these compounds is not linked to HIV-RT, but that they are several times more active on the HIV IN enzyme. Some caffeoylquinic acids showed activity against HIV-1 IN, but caffeic acid and chlorogenic acid were not active, and show the selective nature of this wide variety of related compounds. Chlorogenic acid and quinic acid, which was not active on HIV-1 IN reduced the amount of HBV-DNA more effectively than that of the viral antigens (Wang et al., 2009) also showing the potential use of the CQA's to treat other viral infection. The CQA's have been reported in numerous studies to have potent activity against HSV as well (Khan et al., 2005, Lall et al., 2005, Meyer et al., 1997, Thompson, 2006). Furthermore, it was shown that very active and abundant anti-HIV compounds such as 5-O-chlorogenic acid (5-CGA) is highly bioavailable as it is absorbed in the stomach and jejunum followed by absorption along the small intestine and also the large intestine (Farah et al., 2008). Other compounds such as 3-CQA, 5-CQA, 3,4-DCQA, 3,5-DCQA, and 4,5-DCQA are all present in the plasma with low concentrations of caffeic, ferulic, isoferulic, and p-coumaric acids (Farah et al., 2008) and might not be realistically recorded in in vitro assays which are often reported at much higher concentrations.
Chlorogenic acids and other dihydroxycinammic acids such as caffeic acid have been described previously as anti-oxidants and therefore beneficial compounds. A more possible explanation is however their pro-oxidant activity as they can be oxidized to form quinones when oxidized by peroxidase/H2O2 or tyrosinase/O2. These quinones can be very toxic in cells due to creating oxidative stress, but are kept in their unoxidised state by antioxidants such as glutathione or ascorbic acid (Moridani et al., 2011). Flavonoids act as pro-oxidants in producing a quinone which produce reactive oxygen species (ROS) which are very effective in the defense of herbivores and pathogenic attack. Addition of 0.2% caffeic acid or 0.2% 5-CQA to mice, resulted in a significantly increased level of Glutathione S-transferase (GST), probably due to their pro-oxidant activity and electrophile-responsive element (EpRE) activation. Similarly many cinnamic acids have been shown to be potent inducers of NAD(P)H:(quinone-acceptor) oxidoreductase (Clifford, 1999). The DCQA's and DCTA's are bis-catechols and do not appear to inhibit HIV-1 RT within the cell, but acting directly through inhibition of IN (McDougall et al., 1998).
The mechanism of how the phenolic acids act on viruses to inhibit their replication or infection is however not well researched. Compounds such as 5-CQA and related chlorogenic acids have been tested numerously, not only to confirm their anti-HIV activity, but also their activity on HSV-1, HSV-2 and Adenovirus-11 (Chiang et al., 2002; McDougall et al., 1998; Tamura et al., 2006; Thompson, 2006; Wang et al., 2009). This also supports the traditional or popular use of many of these plants for other viral infections, but showing potent anti-HIV activity when tested in vitro.
7. Discussion
Poor nutrition, inaccessibility to health systems and overburdened health budgets and resources contribute to the spread and inadequate control and continued infection of HIV (Coovadia et al., 2009). Many studies have relied on the traditional uses of medicinal plants in treating viral infections and various accounts of very active plants have been documented (Bessong et al., 2005). Where anti-HIV activity could be linked to isolated compounds from southern African plants, it is often compounds previously identified for anti-HIV activity in plants from other regions of the world. It is therefore evident that similar compounds or compound groups have been identified as the active principles in plant preparations from various regions in the world and the repeated identification should be supported by progression into in vivo studies, especially in the southern African region where affordable and safe medicines are needed urgently.
Plants continue to provide drug leads and numerous plants and/or plant compounds have been advanced to clinical trials (Yang et al., 2011). Enough evidence has been accumulated in various studies to warrant further investigation into the active principles and chemical profile of anti-viral plants with specific focus on the three mentioned groups. A systematic review by Liu and Yang (2005) assessed the beneficial effects and risks of herbal medicines in patients with HIV infection and AIDS, and concluded that there is inadequate evidence to support the use of herbal medicines in HIV-infected individuals and AIDS patients. However, potential beneficial effects need to be confirmed in large, rigorous trials (Liu et al., 2005). Few southern African plants or plant compounds are currently in clinical trial studies. For example, S. frutescens, indigenous to Lesotho, South Africa, southern Namibia and southeastern Botswana has a wealth of preclinical data (van Wyk and Albrecht, 2008). A phase I study has shown that S. frutescens is well tolerated and that it showed no significant side effects (Johnson et al., 2007). Recently the results of an adaptive two-stage randomized double-blind placebo controlled study were published. The study evaluated the safety of consuming dried S. frutescens by HIV seropositive adults with CD4 T-lymphocyte count of>350 cells/μL. Sutherlandia frutescens did not change HIV viral load, and CD4 T-lymphocyte count and was similar in the two arms at 24 weeks; however, mean and total burden of infection was greater in the S. frutescens arm attributed to two tuberculosis cases in subjects taking isoniazid preventive therapy (IPT). The study concluded that possible interaction between S. frutescens and IPT needs further evaluation, although no other safety issues relating to consumption of S. frutescens were identified (Wilson et al., 2015). The equally good activity of some of the compounds such as the chlorogenic acids on other viruses such as HSV also support intensified in vivo studies to support developing these plant extracts or compounds into anti-viral treatments. Apart from S. frutescens entering clinical studies, no other plants from this region have advanced to this stage, even though the majority of HIV infected individuals are treated with medicinal plant preparations from this region. The low number of plant extracts and compounds in advanced studies support the need for more focus on developing the research potential identified in the published studies to reach the commercial market. By evaluating and advancing more herbal preparations and compounds for testing in vivo will ensure that more treatments reach the commercial markets.
8. Conclusion
Throughout the paper, evidence is presented which shows that although southern Africa possesses a wealth of medicinal plants, most of the research on the screening and isolation of active compounds was carried out only in vitro on enzymes and viral proteins, with no follow-up research to validate the results in vivo. This could be attributed to the lack of long term funding and infrastructure and is supported by many plants tested in facilities not within the southern African region. From screening literature, it would therefore seem as if common compounds or compound groups from southern African plants, of which many are well-known and previously confirmed for their anti-viral activity from plants from other areas of the world, are repeatedly identified as anti-HIV agents. It is therefore argued that the presence of well-known and well-researched plant compounds with anti-HIV activity from southern Africa should direct future focus in development of anti-viral agents for rapid development of affordable anti-HIV treatments. This should also be followed-up in in vivo studies as this information is lacking and anti-HIV activity is only dependent on the in vitro assay results currently available. In this review current information on southern African plants with traditional use against viral infections and specifically HIV treatment or HIV related diseases or symptoms is presented with the aim to develop treatments for people living with HIV/AIDS, as there is an urgent need to fast track in vivo testing and HIV/AIDS clinical trials of candidate drugs developed from compounds isolated from plants for effective and affordable alternatives to current treatment options.
Contribution of authors
Gerhard Prinsloo originated the work and led the discussions on topics, and managed the progress of the manuscript.
Cynthia Marokane is a postgraduate student which contributed significantly in collation of information and discussions on the manuscript.
Renée Street has extensive experience in medicinal plant research and an extensive background on HIV as part of the HIV unit at the MRC and contributed significantly to the content of the paper. She was also responsible for final editing and proof reading of the paper.
Conflict of interest
The authors declare no conflict of interests.
Funding source
No specific financial support was received for this project.
Contributor Information
Gerhard Prinsloo, Email: prinsg@unisa.ac.za.
Cynthia K. Marokane, Email: marokck@unisa.ac.za.
Renée A. Street, Email: Renee.Street@mrc.ac.za.
References
- Agarwal A., D’Souza P., Johnson T.S., Dethe S.M., Chandrasekaran C. Use of in vitro bioassays for assessing botanicals. Curr. Opin. Biotechnol. 2014;25:39–44. doi: 10.1016/j.copbio.2013.08.010. [DOI] [PubMed] [Google Scholar]
- Alasbahi R.H., Melzig M.F. Plectranthus barbatus: a review of Phytochemistry. Ethnobot. Uses Pharmacol. – Part 1. Planta Med. 2010;76:653–661. doi: 10.1055/s-0029-1240898. [DOI] [PubMed] [Google Scholar]
- Ali H., König G., Khalid S., Wright A., Kaminsky R. Evaluation of selected Sudanese medicinal plants for their in vitro activity against hemoflagellates, selected bacteria, HIV-1-RT and tyrosine kinase inhibitory, and for cytotoxicity. J. Ethnopharmacol. 2002;83:219–228. doi: 10.1016/s0378-8741(02)00245-3. [DOI] [PubMed] [Google Scholar]
- Archer R.H., Wyk A.E., Van A taxonomic revision of Elaeodendron Jacq . ( Cassinoideae : Celastraceae ) in Africa. South Afr. J. Bot. 1998;64:93–109. [Google Scholar]
- Asres K., Bucar F., Kartnig T., Witvrouw M., Pannecouque C., De Clercq E. Antiviral activity against human immunodeficiency virus type 1 (HIV-1) and type 2 (HIV-2) of ethnobotanically selected ethiopian medicinal plants. Phytother. Res. 2001;15:62–69. doi: 10.1002/1099-1573(200102)15:1<62::aid-ptr956>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Atawodi S.E., Olowoniyi O.D. Pharmacological and therapeutic activities of Kigelia africana ( Lam.) Benth. Annu. Res. Rev. Biol. 2015;5:1–17. [Google Scholar]
- Auld D.S., Thorne N., Nguyen D.-T., Inglese J. A specific mechanism for nonspecific activation in reporter-gene assays. ACS Chem. Biol. 2008;3:463–470. doi: 10.1021/cb8000793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington R., Williamson G., Bennett R., Davis B., Brodbelt J., Kroon P. Absorption, conjugation and efflux of the flavonoids, kaempferol and galangin, using the intestinal CaCo-2/TC7 cell model. J. Funct. Foods. 2009;1(1):74–87. doi: 10.1016/j.jff.2008.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bessong P., Obi C.L. Review: ethno-pharmacology of human immundeficiency virus in South Africa. Afr. J. Biotechnol. 2006;5(19):1693–1699. (5, 1693–1699) [Google Scholar]
- Bessong P.O., Obi C.L., Andréola M.-L., Rojas L.B., Pouységu L., Igumbor E., Meyer J.J.M., Quideau S., Litvak S. Evaluation of selected South African medicinal plants for inhibitory properties against human immunodeficiency virus type 1 reverse transcriptase and integrase. J. Ethnopharmacol. 2005;99:83–91. doi: 10.1016/j.jep.2005.01.056. [DOI] [PubMed] [Google Scholar]
- Bolton E.C., Mildvan A.S., Boeke J.D. Inhibition of reverse transcription in vivo by elevated manganese ion concentration. Mol. Cell. 2002;9:879–889. doi: 10.1016/s1097-2765(02)00495-1. [DOI] [PubMed] [Google Scholar]
- Brinkhaus B., Lindner M., Schuppan D., Hahn E.G. Chemical, pharmacological and clinical profile of the East Asian medical plant Centella aslatica. Phytomedicine. 2000;7:427–448. doi: 10.1016/s0944-7113(00)80065-3. [DOI] [PubMed] [Google Scholar]
- Castro A. De, Wyk B. Van, Van B. Diagnostic characters and geographic distribution of A lep idea species used in traditional medicine. South Afr. J. Bot. 1994;60:345–350. [Google Scholar]
- Chen J., Lin H., Hu M. Metabolism of flavonoids via enteric recycling: role of intestinal disposition. J. Pharmacol. Exp. Ther. 2003;304:1228–1235. doi: 10.1124/jpet.102.046409. [DOI] [PubMed] [Google Scholar]
- Chiang L.C., Chiang W., Chang M.Y., Ng L.T., Lin C.C. Antiviral activity of Plantago major extracts and related compounds in vitro. Antivir. Res. 2002;55:53–62. doi: 10.1016/s0166-3542(02)00007-4. [DOI] [PubMed] [Google Scholar]
- Chinnaiyan S.K., Subramanian M.R., Vinoth Kumar S., Chandu A.N., Deivasigamani K. Antimicrobial and anti-HIV activity of extracts of Canthium coromandelicum (Burm.f.) Alston leaves. J. Pharm. Res. 2013;7:588–594. [Google Scholar]
- Chinsembu K.C., Hedimbi M. An ethnobotanical survey of plants used to manage HIV/AIDS opportunistic infections in Katima Mulilo, Caprivi region, Namibia. J. Ethnobiol. Ethnomed. 2010;6:1–9. doi: 10.1186/1746-4269-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinsembu K.C., Hedimbi M. Ethnomedicinal plants and other natural products with anti-HIV active compounds and their putative modes of action. Int. J. Biotechnol. Mol. Biol. Res. 2010;1:74–91. [Google Scholar]
- Chukwujekwu J.C., Ndhlala A.R., de Kock C.A., Smith P.J., Van Staden J. Antiplasmodial, HIV-1 reverse transcriptase inhibitory and cytotoxicity properties of Centratherum punctatum Cass. and its fractions. South Afr. J. Bot. 2014;90:17–19. [Google Scholar]
- Clifford M.N. 5-O-caffeoylquinic acid (5-CQA).s and other cinnamates—nature, occurrence and dietary burden. J. Sci. Food Agric. 1999;79:362–372. [Google Scholar]
- Collins R.A., Ng T.B., Fong W.P., Wan C.C., Yeung H.W. Removal of polyphenolic compounds from aqueous plant extracts using polyamide minicolumns. IUBMB Life. 1998;45:791–796. doi: 10.1080/15216549800203212. [DOI] [PubMed] [Google Scholar]
- Coovadia H., Jewkes R., Barron P., Sanders D., McIntyre D. Health in South Africa 1. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009:347. doi: 10.1016/S0140-6736(09)60951-X. [DOI] [PubMed] [Google Scholar]
- Cos P., Hermans N., De Bruyne T., Apers S., Sindambiwe J.B., Witvrouw M., De Clercq E., Vanden Berghe D., Pieters L., Vlietinck A.J. Antiviral activity of Rwandan medicinal plants against human immunodeficiency virus type-1 (HIV-1) Phytomedicine. 2002;9:62–68. doi: 10.1078/0944-7113-00083. [DOI] [PubMed] [Google Scholar]
- Cos P., Vlietinck A.J., Berghe D., Vanden, Maes L. Anti-infective potential of natural products: how to develop a stronger in vitro “proof-of-concept”. J. Ethnopharmacol. 2006;106:290–302. doi: 10.1016/j.jep.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Day A., DuPont M., Ridley S., Rhodes M., Rhodes M., Morgan M., Williamson G. Deglycosylation of £avonoid and iso£avonoid glycosides by human small intestine and liver L-glucosidase activity. Fed. Eur. Biochem. Soc. Lett. 1998;436:71–75. doi: 10.1016/s0014-5793(98)01101-6. [DOI] [PubMed] [Google Scholar]
- De Clercq E. Ebola virus (EBOV) infection: therapeutic strategies. Biochem. Pharmacol. 2014;93:1–10. doi: 10.1016/j.bcp.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decosterd L.A., Parsons I.C., Custafson K.R., Ii J.H.C., Mcmahon J.B., Cragg G.M., Murata Y., Pannell L.K., Steiner J.R., Clardy J., Boyd M.R. Structure, absolute stereochemistry, and synthesis of Conocurvone. J. Am. Chem. Soc. 1993;115:6673–6679. [Google Scholar]
- Edeoga H.O., Okwu D.E., Mbaebie B.O. Phytochemical constituents of some Nigerian medicinal plants. Afr. J. Biotechnol. 2005;4:685–688. [Google Scholar]
- Eldeen I.M.S., Seow E.-M., Abdullah R., Sulaiman S.F. In vitro antibacterial, antioxidant, total phenolic contents and anti-HIV-1 reverse transcriptase activities of extracts of seven Phyllanthus sp. South Afr. J. Bot. 2011;77:75–79. [Google Scholar]
- Farah A., Monteiro M., Donangelo C., Lafay S. 5-O-caffeoylquinic acid (5-CQA) from green coffee extract are highly bioavailable in humans. J. Nutr. 2008:2309–2315. doi: 10.3945/jn.108.095554. [DOI] [PubMed] [Google Scholar]
- Feng T., Su J., Ding Z., Zheng Y., Li Y., Leng Y., Liu J. Chemical constituents and their bioactivities of “tongling white ginger”(zingiber officinale) J. Agric. Food Chem. 2011;59:11690–11695. doi: 10.1021/jf202544w. [DOI] [PubMed] [Google Scholar]
- Fennell C., van Staden J. Crinum species in traditional and modern medicine. J. Ethnopharmacol. 2001;78:15–26. doi: 10.1016/s0378-8741(01)00305-1. [DOI] [PubMed] [Google Scholar]
- Filler A., Lever A.M. Effects of cation substitutions on reverse transcriptase and on human immunodeficiency virus production. AIDS Res. Hum. Retrovir. 1997;13:291–299. doi: 10.1089/aid.1997.13.291. [DOI] [PubMed] [Google Scholar]
- Gail H., Tarryn B., Oluwaseyi A., Denver D., Oluchi M., Charlotte V.K., Joop D.J., Diana G. An ethnobotanical survey of medicinal plants used by traditional health practitioners to manage HIV and its related opportunistic infections in Mpoza, Eastern Cape Province, South Africa. J. Ethnopharmacol. 2015;171:109–115. doi: 10.1016/j.jep.2015.05.029. [DOI] [PubMed] [Google Scholar]
- Gechev T.S., Hille J., Woerdenbag H.J., Benina M., Mehterov N., Toneva V., Fernie A.R., Mueller-Roeber B. Natural products from resurrection plants: potential for medical applications. Biotechnol. Adv. 2014;32:1091–1101. doi: 10.1016/j.biotechadv.2014.03.005. [DOI] [PubMed] [Google Scholar]
- Gescher K., Kühn J., Lorentzen E., Hafezi W., Derksen A., Deters A., Hensel A. Proanthocyanidin-enriched extract from Myrothamnus flabellifolia Welw. exerts antiviral activity against herpes simplex virus type 1 by inhibition of viral adsorption and penetration. J. Ethnopharmacol. 2011;134:468–474. doi: 10.1016/j.jep.2010.12.038. [DOI] [PubMed] [Google Scholar]
- Gyuris A., Szlavik L., Minarovits J., Vasas A., Molnar J., Hohmann J. Antiviral activities of extracts of euphorbia hirta L. against HIV-1, HIV-2 and SIVmac251. In Vivo. 2009;23:429–432. doi:doi:23/3/429. [PubMed] [Google Scholar]
- Harnett S.M., Oosthuizen V., van de Venter M. Anti-HIV activities of organic and aqueous extracts of Sutherlandia frutescens and Lobostemon trigonus. J. Ethnopharmacol. 2005;96:113–119. doi: 10.1016/j.jep.2004.08.038. [DOI] [PubMed] [Google Scholar]
- Helfer M., Koppensteiner H., Schneider M., Rebensburg S., Forcisi S., Müller C., Schmitt-Kopplin P., Schindler M., Brack-Werner R. The root extract of the medicinal plant Pelargonium sidoides is a potent HIV-1 attachment inhibitor. PLoS One. 2014:9. doi: 10.1371/journal.pone.0087487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyman H.M., Senejoux F., Seibert I., Klimkait T., Maharaj V.J., Meyer J.J.M. Identification of anti-HIV active dicaffeoylquinic- and tricaffeoylquinic acids in Helichrysum populifolium by NMR-based metabolomic guided fractionation. Fitoterapia. 2015;103:155–164. doi: 10.1016/j.fitote.2015.03.024. [DOI] [PubMed] [Google Scholar]
- Hoang V.D., Tan G.T., Dinh V., Teng G., Zhang H., Tamez P.A. Natural anti-HIV agents. Part I. (+) - demethoxyepiexcelsin and verticillatol from Litsea verticillata. Phytochemistry. 2002;59:325–329. doi: 10.1016/s0031-9422(01)00454-x. [DOI] [PubMed] [Google Scholar]
- Hollman P. Absorption, bioavailability, and metabolism of flavonoids. Pharm. Biol. 2004;42(Suppl):74–83. [Google Scholar]
- Jiang F., Chen W., Yi K., Wu Z., Si Y., Han W., Zhao Y. The evaluation of catechins that contain a galloyl moiety as potential HIV-1 integrase inhibitors. Clin. Immunol. 2010;137:347–356. doi: 10.1016/j.clim.2010.08.007. [DOI] [PubMed] [Google Scholar]
- Jordaan M., Wyk A.E.V.A.N., Maurin O. A conspectus of Combretum (Combretaceae) in southern Africa, with taxonomic and nomenclatural notes on species and sections. Bothalia. 2011;41:135–160. [Google Scholar]
- Kadu C.A.C., Parich A., Schueler S., Konrad H., Muluvi G.M., Eyog-Matig O., Muchugi A., Williams V.L., Ramamonjisoa L., Kapinga C., Foahom B., Katsvanga C., Hafashimana D., Obama C., Vinceti B., Schumacher R., Geburek T. Bioactive constituents in Prunus africana: geographical variation throughout Africa and associations with environmental and genetic parameters. Phytochemistry. 2012;83:70–78. doi: 10.1016/j.phytochem.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Kapewangolo P., Hussein A.A., Meyer D. Inhibition of HIV-1 enzymes, antioxidant and anti-inflammatory activities of Plectranthus barbatus. J. Ethnopharmacol. 2013;149:184–190. doi: 10.1016/j.jep.2013.06.019. [DOI] [PubMed] [Google Scholar]
- Khan M.T.H., Ather A., Thompson K.D., Gambari R. Extracts and molecules from medicinal plants against herpes simplex viruses. Antivir. Res. 2005;67:107–119. doi: 10.1016/j.antiviral.2005.05.002. [DOI] [PubMed] [Google Scholar]
- Kim H.J., Woo E., Shin C., Park H. A new flavonol glycoside Gallate Ester from Acer okamotoanum and its inhibitory activity against Human Immunodeficiency Virus-1 ( HIV-1) integrase. J. Nat. Prod. 1998;61:145–148. doi: 10.1021/np970171q. [DOI] [PubMed] [Google Scholar]
- Kim S.B., Chang B.Y., Jo Y.H., Lee S.H., Han S.-B., Hwang B.Y., Kim S.Y., Lee M.K. Macrophage activating activity of pyrrole alkaloids from Morus alba fruits. J. Ethnopharmacol. 2013;145:393–396. doi: 10.1016/j.jep.2012.11.007. [DOI] [PubMed] [Google Scholar]
- Klos M., van de Venter M., Milne P.J., Traore H.N., Meyer D., Oosthuizen V. In vitro anti-HIV activity of five selected South African medicinal plant extracts. J. Ethnopharmacol. 2009;124:182–188. doi: 10.1016/j.jep.2009.04.043. [DOI] [PubMed] [Google Scholar]
- Lackman-Smith C.S., Snyder B.A., Marotte K.M., Osterling M.C., Mankowski M.K., Jones M., Sanders-Beer B.E. Safety and anti-HIV assessments of natural vaginal cleansing products in an established topical microbicides in vitro testing algorithm. AIDS Res. Ther. 2010;7(1):1. doi: 10.1186/1742-6405-7-22. (7, 1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lall N., Meyer J.J.M., Taylor M.B., van Staden J. Anti-HSV-1 activity of Euclea natalensis. South Afr. J. Bot. 2005;71:444–446. [Google Scholar]
- Lamorde M., Tabuti J.R.S., Obua C., Kukunda-Byobona C., Lanyero H., Byakika-Kibwika P., Bbosa G.S., Lubega A., Ogwal-Okeng J., Ryan M., Waako P.J., Merry C. Medicinal plants used by traditional medicine practitioners for the treatment of HIV/AIDS and related conditions in Uganda. J. Ethnopharmacol. 2010;130:43–53. doi: 10.1016/j.jep.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Lee T.T., Kashiwada Y., Huang L., Snider J., Cosentinob M., Lee K. Suksdorfin: an anti-HIV principle from Lomutium suksdor ~ i, its structure-activity correlation with related coumarins, and synergistic effects with anti-AIDS nucleosides” f. Bioorg. Med. Chem. 1994;2:1051–1056. doi: 10.1016/s0968-0896(00)82054-4. [DOI] [PubMed] [Google Scholar]
- Leteane M.M., Ngwenya B.N., Muzila M., Namushe A., Mwinga J., Musonda R., Moyo S., Mengestu Y.B., Abegaz B.M., Andrae-Marobela K. Old plants newly discovered: cassia sieberiana D.C. and Cassia abbreviata Oliv. Oliv. root extracts inhibit in vitro HIV-1c replication in peripheral blood mononuclear cells (PBMCs) by different modes of action. J. Ethnopharmacol. 2012;141:48–56. doi: 10.1016/j.jep.2012.01.044. [DOI] [PubMed] [Google Scholar]
- Liu N.Q., Kooy F. Van, Der, Verpoorte R. Artemisia afra: a potential flagship for African medicinal plants? South Afr. J. Bot. 2009;75:185–195. [Google Scholar]
- Louvel S., Moodley N., Seibert I., Steenkamp P., Nthambeleni R., Vidal V., Maharaj V., Klimkait T. Identification of compounds from the plant species Alepidea amatymbica active against HIV. South Afr. J. Bot. 2013;86:9–14. [Google Scholar]
- Lubbe A., Seibert I., Klimkait T., van der Kooy F. Ethnopharmacology in overdrive: the remarkable anti-HIV activity of Artemisia annua. J. Ethnopharmacol. 2012;141:854–859. doi: 10.1016/j.jep.2012.03.024. [DOI] [PubMed] [Google Scholar]
- Mahmood N., Moore P.S., De Tommasi N., De Simone F., Colman S., Hay A.J., Pizza C. Inhibition of HIV infection by caffeoylquinic acid derivatives. Antivir. Chem. Chemother. 1993;4:235–240. [Google Scholar]
- Mao Q.C., Zhou Y.C., Li R.M., Hu Y.P., Liu S.W., Li X.J. Inhibition of HIV-1 mediated cell-cell fusion by saponin fraction from psidium guajava leaf. J. Chin. Med. Mater. 2010;33:1751–1754. [PubMed] [Google Scholar]
- Maregesi Van, Miert S., Pannecouque C., Haddad Feis, Hermans M.H., Wright N., Vlietinck C.W., Aspers A.J., Pieters, L S. Screening of Tanzanian medicinal plants against Plasmodium falciparum and human immunodeficiency virus. Planta Med. 2010;76:195–201. doi: 10.1055/s-0029-1186024. [DOI] [PubMed] [Google Scholar]
- Maregesi S.M., Hermans N., Dhooghe L., Cimanga K., Ferreira D., Pannecouque C., Vanden Berghe D.A., Cos P., Maes L., Vlietinck A.J., Apers S., Pieters L. Phytochemical and biological investigations of Elaeodendron schlechteranum. J. Ethnopharmacol. 2010;129:319–326. doi: 10.1016/j.jep.2010.03.034. [DOI] [PubMed] [Google Scholar]
- Maregesi S.M., Pieters L., Ngassapa O.D., Apers S., Vingerhoets R., Cos P., Berghe D.A., Vanden, Vlietinck A.J. Screening of some Tanzanian medicinal plants from Bunda district for antibacterial, antifungal and antiviral activities. J. Ethnopharmacol. 2008;119:58–66. doi: 10.1016/j.jep.2008.05.033. [DOI] [PubMed] [Google Scholar]
- Maroyi A. Alternative medicines for HIV / AIDS in resource-poor settings: insight from traditional medicines use in Sub-Saharan Africa. Trop. J. Pharm. Res. 2014;13:1527–1536. [Google Scholar]
- Mbaveng A.T., Kuete V., Mapunya B.M., Beng V.P., Nkengfack A.E., Meyer J.J.M., Lall N. Evaluation of four Cameroonian medicinal plants for anticancer, antigonorrheal and antireverse transcriptase activities. Environ. Toxicol. Pharmacol. 2011;32:162–167. doi: 10.1016/j.etap.2011.04.006. (doi:10.1016/j.etap.2011.04.006) [DOI] [PubMed] [Google Scholar]
- McDougall B., King P.J., Wu B.W., Hostomsky Z., Reinecke M.G., Robinson W.E., Jr. Dicaffeoylquinic and dicaffeoyltartaric acids are selective inhibitors of human immunodeficiency virus type 1 integrase. Antimicrob. Agents Chemother. 1998;42:140–146. doi: 10.1128/aac.42.1.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J.J.M., Afolayan A.J., Taylor M.B., Erasmus D. Antiviral activity of galangin isolated from the aerial parts of Helichrysum aureonitens. J. Ethnopharmacol. 1997;56:165–169. doi: 10.1016/s0378-8741(97)01514-6. [DOI] [PubMed] [Google Scholar]
- Moore J.P., Lindsey G.G., Farrant J.M., Brandt W.F. An overview of the biology of the desiccation-tolerant resurrection plant Myrothamnus flabellifolia. Ann. Bota. 2007;99:211–217. doi: 10.1093/aob/mcl269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moridani M.A., Scobie H., Jamshidzadeh A., Salehi P., O’Brien P.J. Caffeic acid, chlorogenic acid, and dihydrocaffeic acid metabolism: glutathione conjugate formation. Drug Metab. Dispos. 2011;29:1432–1439. [PubMed] [Google Scholar]
- Moyo M., Van Staden J. Medicinal properties and conservation of Pelargonium sidoides DC. J. Ethnopharmacol. 2014;152:243–255. doi: 10.1016/j.jep.2014.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mthethwa N.S., Oyedeji B.A.O., Obi L.C., Aiyegoro A. Studies of four South African medicinal plants and isolation of bioactive compounds from Cassine transvaalensis ( Burtt. Davy) codd. BMC Complement. Altern. Med. 2014;14:1–9. doi: 10.1186/1472-6882-14-512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muazu J., Kaita M. A review of traditional plants used in the treatment of epilepsy amongst the Hausa/Fulani tribes of northern nigeria. Afr. J. Tradit. Complement. Altern. Med. 2008;5:387–390. doi: 10.4314/ajtcam.v5i4.31294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller-Harvey, I., Reedb, J.D., Hartley, R.D., 1987. Characterisation of phenolic compounds, including flavonoids and tannins , of ten Ethiopian Browse Species by High Performance Liquid Chromatography, 1–14.
- Mujovo S.F., Hussein A.A., Meyer J.J.M., Fourie B., Muthivhi T., Lall N. Bioactive compounds from Lippia javanica and Hoslundia opposita. Nat. Prod. Res. 2008;22:1047–1054. doi: 10.1080/14786410802250037. [DOI] [PubMed] [Google Scholar]
- Nair J.J., Van Staden J. Traditional usage, phytochemistry and pharmacology of the South African medicinal plant Boophone disticha (L.f.) Herb. (Amaryllidaceae) J. Ethnopharmacol. 2014;151:12–26. doi: 10.1016/j.jep.2013.10.053. [DOI] [PubMed] [Google Scholar]
- Narayan L.C., Rai V.R., Tewtrakul S. Emerging need to use phytopharmaceuticals in the treatment of HIV. J. Pharm. Res. 2013;6:218–223. [Google Scholar]
- Ncube B., Ndhlala A.R., Okem A., Van Staden J. Hypoxis (Hypoxidaceae) in African traditional medicine. J. Ethnopharmacol. 2013;150:818–827. doi: 10.1016/j.jep.2013.10.032. [DOI] [PubMed] [Google Scholar]
- Ngwira K.J., Maharaj V.J., Mgani Q.A. In vitro antiplasmodial and HIV-1 neutralization activities of root and leaf extracts from Berberis holstii. J. Herb. Med. 2015 [Google Scholar]
- Patil K.S., Bhalsing S.R. Ethnomedicinal uses, phytochemistry and pharmacological properties of the genus Boerhavia. J. Ethnopharmacol. 2016;182:200–220. doi: 10.1016/j.jep.2016.01.042. [DOI] [PubMed] [Google Scholar]
- Patro S.K., Behera P., Kumar P.M., Sasmal D., Padhy R.K. Pharmacological review of Flacourtia sepiaria ( Ruxb.) Sch. Acad. J. Pharm. 2013;2:89–93. [Google Scholar]
- Prakash S., Staden J., Van Micropropagation of Hoslundia opposita Vahl — a valuable medicinal plant. South Afr. J. Bot. 2007;73:60–63. [Google Scholar]
- Prinsloo G., Meyer J.J.M., Hussein A.A., Munoz E., Sanchez R. A cardiac glucoside with in vitro anti-HIV activity isolated from Elaeodendron croceum. Nat. Prod. Res. 2010;24:1743–1746. doi: 10.1080/14786410903211912. [DOI] [PubMed] [Google Scholar]
- Rahul J., Jain M.K., Singh S.P., Kamal R.K., Naz A., Gupta A.K., Kumar S. Adansonia digitata L. (baobab): a review of traditional information and taxonomic description Jitin. Asian Pac. J. Trop. Biomed. 2015;5:79–84. [Google Scholar]
- Rukunga G.M., Kofi-Tsekpo M.W., Kurokawa M., Kageyama S., Mungai G.M., Muli J.M., Tolo F.M., Kibaya R.M., Muthaura C.N., Kanyara J.N., Tukai P.M., Shiraki K. Evaluation of the HIV-1 reverse transcriptase inhibitory properties of extracts from some medicinal plant in Kenya. Afr. J. Health Sci. 2002;9:81–90. doi: 10.4314/ajhs.v9i1.30758. [DOI] [PubMed] [Google Scholar]
- Saha R.K., Takahashi T., Kurebayashi Y., Fukushima K., Minami A., Kinbara N., Ichitani M., Sagesaka Y.M., Suzuki T. Antiviral effect of strictinin on influenza virus replication. Antivir. Res. 2010;88:10–18. doi: 10.1016/j.antiviral.2010.06.008. [DOI] [PubMed] [Google Scholar]
- Sharma A., Rangari V. HIV-1 reverse transcriptase AND protease assay OF methanolic extracts OF. Int. J. Pharm. Pharm. Sci. 2016;8:124–127. [Google Scholar]
- Shoemaker M., Cohen I., Campbell M. Reduction of MTT by aqueous herbal extracts in the absence of cells. J. Ethnopharmacol. 2004;93:381–384. doi: 10.1016/j.jep.2004.04.011. [DOI] [PubMed] [Google Scholar]
- Singh D., Singh B., Goel R.K. Traditional uses, phytochemistry and pharmacology of Ficus religiosa: a review. J. Ethnopharmacol. 2011;134:565–583. doi: 10.1016/j.jep.2011.01.046. [DOI] [PubMed] [Google Scholar]
- Singh I., Bharate S.B., Bhutani K.K. Anti-HIV naturalproducts. Curr. Sci. 2005;89:269–289. [Google Scholar]
- Sotoca A.M., Bovee T.F.H., Brand W., Velikova N., Boeren S., Murk A.J., Vervoort J., Rietjens I.M.C.M. Superinduction of estrogen receptor mediated gene expression in luciferase based reporter gene assays is mediated by a post-transcriptional mechanism. J. Steroid Biochem. Mol. Biol. 2010;122:204–211. doi: 10.1016/j.jsbmb.2010.06.010. [DOI] [PubMed] [Google Scholar]
- Spencer J., Chowrimootoo G., Choudhurya R., Debnam E., Srai S., Rice-Evans C. The small intestine can both absorb and glucuronidate luminal £avonoids. FEBS Lett. 1999;458:224–230. doi: 10.1016/s0014-5793(99)01160-6. [DOI] [PubMed] [Google Scholar]
- Stintzing F.C., Kammerer D., Schieber A., Adama H. Betacyanins and phenolic compounds from Amaranthus spinosus L. and Boerhavia erecta L. Z. Nat. 2004;2004:1–8. doi: 10.1515/znc-2004-1-201. [DOI] [PubMed] [Google Scholar]
- Tamura H., Akioka T., Ueno K., Chujyo T., Okazaki K., King P.J., Robinson W.E., Jr. Anti-human immunodeficiency virus activity of 3,4,5-tricaffeoylquinic acid in cultured cells of lettuce leaves. Mol. Nutr. Food Res. 2006;50:396–400. doi: 10.1002/mnfr.200500216. [DOI] [PubMed] [Google Scholar]
- Tarus P.K., Coombes P.H., Crouch N.R., Mulholland D.A. Benzo [ c] phenanthridine alkaloids from stem bark of the Forest Knobwood, Zanthoxylum davyi ( Rutaceae) South Afr. J. Bot. 2006;72:555–558. [Google Scholar]
- Thompson K.D. Elsevier; 2006. Lead Molecules from Natural Products - Discovery and New Trends, Advances in Phytomedicine, Advances in Phytomedicine. [Google Scholar]
- Toyang N.J., Verpoorte R. A review of the medicinal potentials of plants of the genus Vernonia (Asteraceae) J. Ethnopharmacol. 2013;146:681–723. doi: 10.1016/j.jep.2013.01.040. [DOI] [PubMed] [Google Scholar]
- Tshikalange T.E., Meyer J.J.M., Hattori T., Suzuki Y. Anti-HIV screening of ethnobotanical selected SA plants. South Afr. J. Bot. 2008;74:391. [Google Scholar]
- Tshikalange T.E., Meyer M.J.J., Lall N., Muñoz E., Sancho R., Van de Venter M., Oosthuizen V. In vitro anti-HIV-1 properties of ethnobotanically selected South African plants used in the treatment of sexually transmitted diseases. J. Ethnopharmacol. 2008;119:478–481. doi: 10.1016/j.jep.2008.08.027. [DOI] [PubMed] [Google Scholar]
- van Wyk B.-E. A broad review of commercially important southern African medicinal plants. J. Ethnopharmacol. 2008;119:342–355. doi: 10.1016/j.jep.2008.05.029. [DOI] [PubMed] [Google Scholar]
- van Wyk, B.-.E., 2001. People’s Plants, by Ben-Erik van Wyk and Nigel Gericke, Briza Publ., Arcadia, Pretoria, South Africa, 2000. Colour photographs, bibliographies, index, 1st edition, 1351 pp. ISBN 1875093-19-2; Zar 170, US$50, Journal of Ethnopharmacology. doi: 10.1016/S0378-8741(00)00308-1. [DOI]
- van Wyk B.-E., Albrecht C. A review of the taxonomy, ethnobotany, chemistry and pharmacology of Sutherlandia frutescens (Fabaceae) J. Ethnopharmacol. 2008;119:620–629. doi: 10.1016/j.jep.2008.08.003. [DOI] [PubMed] [Google Scholar]
- Vasas A., Orban-Gyapai O., Hohmann J. The Genus Rumex: review of traditional uses, phytochemistry and pharmacology. J. Ethnopharmacol. 2015;175:198–228. doi: 10.1016/j.jep.2015.09.001. [DOI] [PubMed] [Google Scholar]
- Vela E.M., Knostman K.A., Mott J.M., Warren R.L., Garver J.N., Vela L.J., Stammen R.L. Genistein, a general kinase inhibitor, as a potential antiviral for arenaviral hemorrhagic fever as described in the Pirital virus-Syrian golden hamster model. Antivir. Res. 2010;87:318–328. doi: 10.1016/j.antiviral.2010.06.007. [DOI] [PubMed] [Google Scholar]
- Viol, D.I., Chagonda, L.S., Moyo, S.R., 2016. Toxicity and antiviral activities of some medicinal plants used by traditional medical practitioners in Zimbabwe, pp. 1538–1544.
- Vlietinck A.J., Bruyne T., De, Apers S., Pieters L.A. Plant-derived leading compounds for chemotherapy of Human Immunodeficiency Virus ( HIV) infection. Planta Med. 1998;64:97–109. doi: 10.1055/s-2006-957384. [DOI] [PubMed] [Google Scholar]
- Wang C.R., Zhou R., Ng T.B., Wong J.H., Qiao W.T., Liu F. First report on isolation of methyl gallate with antioxidant, anti-HIV-1 and HIV-1 enzyme inhibitory activities from a mushroom (Pholiota adiposa) Environ. Toxicol. Pharmacol. 2014;37:626–637. doi: 10.1016/j.etap.2014.01.023. [DOI] [PubMed] [Google Scholar]
- Wang G.-F., Shi L.-P., Ren Y.-D., Liu Q.-F., Liu H.-F., Zhang R.-J., Li Z., Zhu F.-H., He P.-L., Tang W., Tao P.-Z., Li C., Zhao W.-M., Zuo J.-P. Anti-hepatitis B virus activity of chlorogenic acid, quinic acid and caffeic acid in vivo and in vitro. Antivir. Res. 2009;83:186–190. doi: 10.1016/j.antiviral.2009.05.002. [DOI] [PubMed] [Google Scholar]
- Yadav I.K., Jaiswal D., Singh H.P., Mishra A., Jain D.A. Anti-HIV drugs from natural sources. Pharm. Res. 2009;1:93–109. [Google Scholar]
- Yasurin P., Sriariyanun M., Phusantisampan T. Review: the bioavailability activity of Centella asiatica. KMUTNB Int. J. Appl. Sci. Technol. 2015;9:1–9. [Google Scholar]


