Abstract
Up-converting phosphor technology (UPT)-based lateral-flow immunoassay has been developed for quantitative detection of Yersinia pestis rapidly and specifically. In this assay, 400 nm up-converting phosphor particles were used as the reporter. A sandwich immumoassay was employed by using a polyclonal antibody against F1 antigen of Y. pestis immobilized on the nitrocellulose membrane and the same antibody conjugated to the UPT particles. The signal detection of the strips was performed by the UPT-based biosensor that could provide a 980 nm IR laser to excite the phosphor particles, then collect the visible luminescence emitted by the UPT particles and finally convert it to the voltage as a signal. VT and VC stand for the multiplied voltage units for the test and the control line, respectively, and the ratio VT/VC is directly proportional to the number of Y. pestis in a sample. We observed a good linearity between the ratio and log CFU/ml of Y. pestis above the detection limit, which was approximately 104 CFU/ml. The precision of the intra- and inter-assay was below 15% (coefficient of variation, CV). Cross-reactivity with related Gram-negative enteric bacteria was not found. The UPT-LF immunoassay system presented here takes less than 30 min to perform from the sample treatment to the data analysis. The current paper includes only preliminary data concerning the biomedical aspects of the assay, but is more concentrated on the technical details of establishing a rapid manual assay using a state-of-the-art label chemistry.
Keywords: Up-converting phosphor technology, Lateral-flow immunoassay, Sandwich immunoassay, Yersinia pestis
1. Introduction
Yersinia pestis, a small Gram-negative rod belonging to the family Enterobacteriaceae, is the etiological agent of plague. This organism is one of the three human pathogenic species, including Y. pestis, Yersinia pseudotuberculosis, and Yersinia enterocolitica, in the genus Yersinia [1]. Plague occurs predominantly in three different forms, that is, bubonic, pneumonic, and septicaemic, depending on the route of exposure to the pathogen. Bubonic plague usually involves one group of lymph nodes, contracted following the bite by a flea that has previously fed on an infected rodent and developed a blocked proventriculus, and the infection can spread to the lungs (pneumonic plague) when the suitable treatment is not administered in time. Septicaemic plague is the result of haematogenous dissemination of the bacteria from a bubo. Pneumonic plague can also be transmitted by airborne droplets. The infection takes place within a few hours and causes bronchopneumonia. What is more, the Y. pestis is the most dangerous bacterial agent that could potentially be used for biological warfare or bioterrorism [2].
Plague is a typical zoonosis distributed in Asia, Africa and America and it was redefined by the World Health Organization (WHO) as a reemerging infectious disease due to the increased outbreak of plague around the world [3]. The rapid detection of Y. pestis is critical for controlling the spread of plague. The laboratory detection of Y. pestis is based on bacteriological, serological and nucleic acid-based methods [1]. The bacterial culture is not well suitable for rapid detection of Y. pestis due to the time delay. The passive haemagglutination assay (PHA), which is used to detect Y. pestis-specific antibodies, has repeatedly shown to lack sensitivity and specificity [4]. Therefore, rapid and sensitive assays are desirable for the detection of Y. pestis, its specific antigens or nucleic acid sequences. At present, sensitive PCR (polymerase chain reaction)-based detection methods have been described to identify Y. pestis [5], [6], [7]. Especially, real-time PCR is highly specific and less prone to cross-contamination [8]. Although offering reasonable sensitivity, these assays are time consuming (include both DNA/RNA preparation and the longer detection procedure), and not readily available for on-site detection. Detection of F1 capsular antigen (F1 CA) of Y. pestis by immunoassay methods such as immunogold chromatographic dipstick assay and ELISA (enzyme-linked immunosorbent assay) has been developed [9], [10].
Immunochromatographic assay, also called lateral-flow (LF) immunoassay, with benefits of low-cost, easy-to-use, rapid and sensitive detection of various analytes, has been developed for many years and mainly been used to detect drugs of abuse and for pregnancy testing at the early stage [11]. Now, it has been surging in infectious disease diagnostics [12], [13]. Jung et al. developed a colloidal gold particles-based LF strip for detecting Escherichia coli O157 at a minimum of 1.8 × 105 CFU/ml [22]. LF procedure utilizes the specific interaction between antigens and antibodies and provides rapid detection of various analytes. In the field of biomedical diagnostics, the search for the increased detection sensitivity and the possibility of quantitative detection using simple inexpensive assays is an ongoing challenge. In this respect, LF assays have become the popular diagnostic tools in a variety of settings because they are sensitive, simple to perform, inexpensive to manufacture, and perhaps most important, well suitable for rapid on-site detection and can be carried out nearly anywhere by non-technical personnel [14].
UPT particles are submicrometer-sized, lanthanide-doped ceramic particles that possess anti-Stokes shift emission by up-converting infrared excitation light (980 nm) to emit visible light. Up-converting phosphors have also been used to realize quantitative assays and increase sensitivity. UPT reporters are 10- to 100-fold more sensitive than assays using conventional reporter systems such as colloidal gold or colored latex beads [15]. They have attracted considerable attention as the relatively novel luminescent labels, especially in LF assays. UPT has already been demonstrated for the sensitive detection of nucleic acids in microarray [16], single-stranded nucleic acids in a sandwich-hybridization assay [17] and Streptococcus pneumonia in an amplification-free hybridization-based DNA [18]; cell and tissue surface antigens by immunocytochemistry [19]; human chorionic gonadotropin [15], drugs of abuse, pathogenic E. coli by lateral-flow immunoassay [20]. In this study, up-converting phosphor is used as a reporter in rapid LF immunoassay for quantitative detection of Y. pestis.
2. Experimental
2.1. Materials
Affinity-purified polyclonal antibody from rabbit against F1 antigen of Y. pestis and affinity-purified antibody from goat against rabbit IgG were prepared in our laboratory. Materials used in preparation of reagents, including HNO3 (concentrated), tetraethylorthosilicate (TEOS), NH4·OH, isopropanol, triethoxyaminopropylsilane (APES), CHCl3, ninhydrin, glycine, glutaraldehyde, sodium cyanoborohydride (NaCNBH3), polyoxyethylene bis-amino (NH2-PEG-NH2, with an average molecule weight of 3350), Na2CO3, NaHCO3, NaCl, Na2HPO4, NaH2PO4, NaN3, albumin bovine V from bovine serum (BSA), p-nitrophenyl phosphate (pNPP), Tween-20, NP-40, sucrose, etc., were all obtained from Sigma Chemical Co. (St. Louis, MO). UPT particles (NaYF4:Yb3+, Er3+) with 400 nm in diameter, which emit visible green light of 541 nm when excited by infrared light of 980 nm, were obtained from Kerune Phosphor Technology Co. (KPT, Shanghai).
Strains of Y. pestis EV76, Y. enterocolitica (LAM 00980, LAM 1310 and LAM 1311), Y. pseudotuberculosis (LAM00942, LAM00943 and LAM00644) and other Gram-negative enteric bacteria [E. coli (LAM00001 and LAM00003) and Salmonella choleraesuis (LAM00993)] were collected by our laboratory [Laboratory of Analytical Microbiology (LAM)]. All bacteria were cultured in Luria–Bertani (LB) broth at 37 °C with shaking at 200 rpm.
2.2. Preparation of UPT-labelled antibody conjugates
UPT particles (400 nm in diameter) were used to conjugate with the antibody against F1 antigen of Y. pestis. The biological molecules cannot be directly coupled to the untreated UPT particles. Therefore, a series of surface modifications and activations of UPT particles were required to realize covalent coupling of antibodies to them [14]. Firstly, UPT particles were coated with a thin layer of silica by using TEOS. Then the silica-coated surface of UPT particles can be functionalized with amino-, aldehyde-functional groups using APES, polyoxyethylene bis-amino and glutaraldehyde, respectively. Eventually these aldehyde-functionalized UPT particles can be conjugated to the antibody directly in a 4 °C-prechilled Na2CO3–NaHCO3 buffer (50 mM, pH 9.5) under stirring. Uncoupled antibodies to the UPT particles were separated from the conjugated ones by a series of washing steps involving centrifugation and resuspension of pelleted UPT particles in a phosphate buffer of 30 mM pH 7.2. After several washes, UPT conjugates (1 mg/ml) were stored at 4 °C in 30 mM phosphate buffer [pH 7.2, containing 0.1% (w/v) BSA, 0.05% (v/v) Tween-20, 0.02% (w/v) NaN3].
2.3. Preparation of UPT-based lateral-flow test strips
The shape of the test strip is rectangle with dimension of 74 mm × 4 mm. The components of the strip were the same as those used in immunogold chromatographic dipstick assay (Fig. 1 ). To prepare LF strips, the sample pad (15 mm, glass-fiber GFCP20300, Millipore), the conjugate release pad (10 mm, GFCP20300, Millipore), the nitrocellulose membrane (25 mm, Hi-Flow nitrocellulose, SRHF09002, Millipore) and the absorbent pad (30 mm, paper no. 470, Scheicher and Schuell) were mounted on the laminating card with proper overlaps. That is, the sample pad overlaps the conjugate release pad with 3 mm, the latter overlaps the nitrocellulose membrane with 1 mm, and the absorbent pad overlaps the nitrocellulose membrane with 2 mm.
Fig. 1.
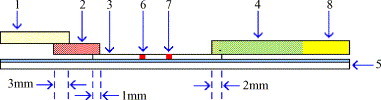
Schematic description of the UPT-based lateral-flow test strip. The components of the strip include a sample pad (1), a conjugate pad (2), a nitrocellulose membrane (3), an absorbent pad (4), and a laminating card (5). During the manufacture, a test line (6), a control line (7), and an ending index line (8) are disposed on the strip and other components are pasted on the laminating card with proper overlapping.
In this study, UPT-antibody conjugates (1.0 mg/ml) were dispersed into the glass-fiber in a conjugate diluting phosphate buffer [pH 7.2, containing 1% (w/v) BSA, 10% (w/v) sucrose, 1% (v/v) Tween-20]. The conjugate release pad was incubated at 37 °C for 3 h. Using the dispenser (XYZ3050, Bio-Dot), the nitrocellulose was provided simultaneously with a capture line of rabbit polyclonal antibody IgG against F1 antigen of Y. pestis (1 mg/ml) and a control line of goat against rabbit IgG (1 mg/ml) at a dispensing rate of 0.1 μl/cm. The nitrocellulose membrane was allowed to dry at 37 °C for 2 h. After the nitrocellulose membrane, the conjugate release, the sample and the absorbent pads were adhered on laminating card with special overlapping seriation, an automatic cutter (CM4000, Bio-Dot) was used to cut the assembled strips into 4 mm in width. The strips were used immediately or stored dry at room temperature until used. Finally, the strip was put into a disposable plastic cartridge, which was designed to fit to the stage of the UPT-based biosensor.
2.4. Instrumentation
The portable biosensor (UPT-based biosensor) was co-developed by Shanghai Institute of Optics and Fine Mechanics, Chinese Academy of Sciences and our institute (Fig. 2 ). Fig. 3 illustrates a design of the UPT-based biosensor, which is similar, at least partly, to what was presented by Zijlmans et al. and Niedbala et al. [19], [20]. The mainboard PC104 installed inside the biosensor was used instead of the accessory computer to control the whole system and the convenient Windows 98 system was employed as the platform to support the running of biosensor software programmed by us. Therefore, just equipped with the keyboard and mouse, the UPT-based biosensor can work independently, and the user can accomplish the scanning process just by pressing the icons displayed on the LCD of biosensor. During detection, firstly the strip was inserted in the biosensor and put on the stage, and then PC104 through multifunction DAS (Data Acquisition Station) card made the laser diode emit the infrared light with wavelength about 980 nm. This light irradiated on the dichroic mirror A, and a part of this light passed through it to the photodiode and gave an electric signal to collimate the instability of the system. The rest light was refracted and irradiated on the dichroic mirror B. This dichroic mirror made the infrared light refracted totally on the focusing lens A and through it focused on the strip. UPT particles on the strip were excited by this infrared light and then emitted visible light with wavelength about 541 nm. This visible light through focusing lens A irradiated on the dichroic mirror B and was transmitted completely. After filtrated away the light with other wavelength by a filter, the visible light emitted by UPT particles was focused on the PMT and gave multiplied voltage (relative fluorescence unit) as a signal. At the ending of data collection on this point, the stage held the strip to slide along X-axis to the next point of the nitrocellulose membrane and then another data-collecting process began. In the whole process of strip-scanning, the biosensor set 50 data-collecting points per millimeter of the nitrocellulose membrane, that is, 2000 points per strip. Therefore, the integrated scanning curve representing the diffusion of UCP particles on the nitrocellulose membrane was obtained. Voltage unit was plotted against the strip length increment to identify the height of peaks.
Fig. 2.

Photograph of the portable prototype UPT-based biosensor.
Fig. 3.
Schematic representation of the design of UPT-based biosensor.
In conclusion, this UPT-based biosensor with an infrared laser (980 nm) was used to scan the resulting test strips. Upon IR excitation, the green light with the wavelength of 541 nm emitted by UPT particles was collected and detected by the UPT-based biosensor. Luminescence was measured, compiled and displayed as voltage units in a 2D plot as a function of the position of the strip. The software used for analysis included algorithms for background subtraction and peak-height determination.
2.5. Sensitivity and specificity of the UPT-LF immunoassay
Sensitivity testing was conducted to determine the detection limit of the UPT-LF immunoassay for Y. pestis by using pure cultures of Y. pestis EV76 as a model. For preparation of a bacterial suspension, pure cultures of Y. pestis EV76 in LB broth were centrifuged at 8000 rpm for 10 min, then the cell pellet was washed once, resuspended and serially diluted in PBS (137 mM NaCl, 2.7 mM KCl, 4.3 mM Na2HPO4, 1.4 mM KH2PO4, pH 8.0). In order to determine the viable cell number (CFU/ml) in the diluted samples, aliquots of 100 μl from 10−4, 10−5, 10−6 and 10−7 dilution tubes were plated in duplicate onto LB agar plates. For detection by the UPT-LF strip, 100 μl of each sample containing different concentrations of Y. pestis ranging from 102 to 109 CFU/ml was mixed with 900 μl of a dilution buffer [2% (w/v) BSA, 0.5% (v/v) Tween-20, 0.5% (v/v) NP-40, in PBS] by gently stirring for 15 min in 1.5-ml microcentrifuge tubes. One hundred microlitres of each sample was applied to the sample window of the test strip and the same amount of the dilution buffer was added as blank control in triplicate. The LF immunoassay lasted for approximately 15 min at room temperature, and then the strip was scanned by the UPT-based biosensor for the results. The cut-off value of this assay was calculated as the mean ratio V T/V C of the blank controls plus three standard deviations.
The bacterial strains of Y. enterocolitica, Y. pseudotuberculosis and other Gram-negative enteric bacteria (E. coli and S. choleraesuis) were used to test the specificity of the UPT-LF assay. Overnight cultures of these bacteria were centrifuged and diluted either in PBS to determine CFU/ml by plate counting or in the dilution buffer for the UPT-LF assay. Cultures diluted in the dilution buffer from 100 to 107 CFU/ml were tested as described above. 108 CFU/ml of Y. pseudotuberculosis spiked with 104 to 108 CFU/ml of Y. pestis EV76 in the dilution buffer was used for evaluating the interference of other bacteria on the sensitivity and specificity of the assay.
2.6. Quantitative detection of Y. pestis by UPT-LF immunoassay
2.6.1. Construction of standard curve
To quantify the cell number in an unknown sample, serial 10-fold dilutions of pure cultures of Y. pestis EV76 ranging from 108 to 104 CFU/ml in the dilution buffer were assayed. Each cell concentration was detected in six repeats, and then the mean V T/V C ratio was plotted against the logarithmic cell number for constructing the standard curve.
2.6.2. Quantitative analysis by blind experiment
Blind experiment was applied to examine the accuracy of the UPT-LF further. Ten different dilutions of pure cultures of Y. pestis EV76 in PBS were prepared and coded randomly for an assay operator by another person. The UPT-LF was performed by the same batch of the strips that were used to construct the standard curve and each dilution was detected in six repeats.
2.6.3. Quantitative detection of Y. pestis from lung specimens of the experimentally infected mouse
Balb/c mice were infected through intranasal inoculation of 10 μl of a phosphate buffer 30 mM pH 7.2 containing 107 CFU/ml of Y. pestis strain 201. Y. pestis 201 was isolated from Microtus brandti in Inner Mongolia, China. It has major phenotypes, such as F1+ (able to produce fraction 1 antigen), VW+ (presence of V antigen), Pst+ (able to produce pesticin) and Pgm+ (pigmentation on Congo-red media). Strain 201 has an LD50 of less than 100 cells for mice by subcutaneous challenge. It belongs to a newly established Y. pestis biovar, microtus [21]. Bacterial CFU were enumerated by plating serial dilutions of lung tissue homogenates from experimentally infected Balb/c mice on LB agar at 28 °C for 36 h. Fifty-one lung tissue homogenates from experimentally infected Balb/c mice were tested in triplicate by the UPT-LF immunoassay.
3. Results and discussion
3.1. Performance of the UPT-LF lateral-flow immunoassay
In this study, our aim was to develop and optimize a rapid, specific and sensitive UPT-LF immunoassay to quantitatively detect the whole cells of Y. pestis using pure cultures of Y. pestis EV76 as a model. Optimal results were obtained with the purified rabbit polyclonal antibody IgG against F1 antigen of Y. pestis immobilized on the nitrocellulose membrane as a capture antibody and the same UPT-antibody conjugate as a detector antibody in a sandwich immunoassay.
We set up experiments for the dose-response curve with serial dilutions of pure cultures of Y. pestis EV76 from 101 to 108 CFU/ml in the dilution buffer. The raw data (data not shown) and background subtraction data (Fig. 4 ) could be obtained by the UPT-based biosensor. The first peak (C) and the second peak (T) in Fig. 4 displayed the multiplied voltage units for the control and the test line, respectively, as plotted in Y-axis. The distance from the scanning window of cartridge was plotted in X-axis. It should note that absolute values of these signals depend on the physical properties of test strips and the photomultiplier tube used for detection and cannot necessarily be used to compare data from different experiments [15]. The variability observed from strip to strip at the same cell concentration attributes to variations in membrane properties, humidity effects, batch to batch variability of the phosphor conjugates, storage conditions, and many other factors. So the data were treated by using the formula (V t − V B)/(V c − V B), where V t represented the multiplied voltage units for the test line signal, V B for the background signal, and V c for the control line signal. The UPT-based biosensor can give the background subtraction values of V T = V t − V B, V C = V c − V B, and the ratio of V T/V C for each scanning, and then a mean value ± S.D. was calculated for repeated tests. In order to get the quantitative result, the ratio V T/V C was treated as the final result for each assay. The mean ratio of the V T/V C values corresponding to serial dilutions of bacterial samples ranging from 101 to 108 CFU/ml was plotted against the logarithmic cell number (CFU/ml). The cut-off value of the current assay was calculated as the mean ratio (V T/V C) of the blank controls plus three standard deviations, which corresponded to 99% confidence. The dose-response curve was obtained by plotting the ratio V T/V C as the Y-axis against logarithmic cell count at the X-axis (Fig. 5 ).
Fig. 4.
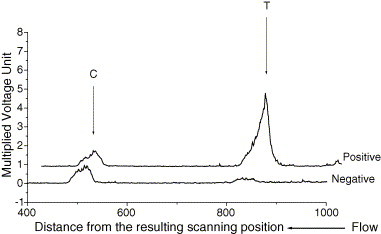
The illustrations of UPT-based lateral-flow immunoassay test results.
Fig. 5.
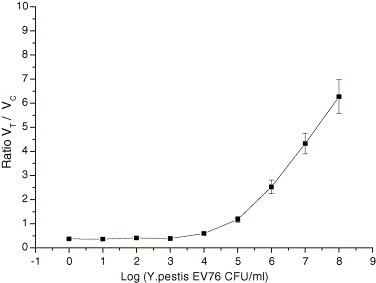
The dose-response curve obtained from the mean ratio VT/VC against log (Y. pestis EV76 CFU/ml) in the dilution buffer. Six repeated tests of each concentration were performed.
The key feature of UPT is a high signal-to-noise ratio due to the elimination of autofluorescence interference. UPT particles, in conjunction with the portable UPT-based biosensor, offer increased sensitivity when used in a rapid LF format. The UPT-based biosensor provides a simple instrument to read assays by avoiding the possibility of subjective errors compared to interpreting a visual strip.
3.2. Sensitivity, specificity and precision of the UPT-LF immunoassay
In order to test the sensitivity of the UPT-LF, serial dilutions of Y. pestis EV76 in the dilution buffer were tested with UPT-LF (Fig. 5). The detection limit of the current assay was 104 CFU/ml, which was below the levels of Y. pestis that may be found in the blood of mice or human infected with Y. pestis. In mice, bacterial levels in blood may reach >104 CFU/ml and in humans it may reach 107 CFU/ml. The ratio V T/V C for 104 CFU/ml was easily distinguished from the mean ratio of V T/V C of the blank controls plus three standard deviations (cut-off value). The UPT-LF immunoassay is 10-fold more sensitive than the colloidal gold particles-based immunochromatography [22].
Our data showed that the high level of other bacteria (108 CFU/ml of Y. pseudotuberculosis) in the dilution buffer did not interfere with the detection of low levels of Y. pestis EV76. Y. pseudotuberculosis did not cross react with antibodies specific for F1 antigen of Y. pestis at the cell concentrations tested. The specificity of the UPT-LF immunoassay was 100%, which was further demonstrated by showing no cross-reactivity to three strains of Y. pseudotuberculosis, three strains of Y. enterocolitica, two strains of E. coli and one strain of S. choleraesuis.
To demonstrate the intra-assay variance, a series of cell concentrations from 104 to 108 CFU/ml was repeatedly tested by using the same batch of test strips. The coefficient of variation ranged from 6.43% to 11.74% (n = 20). The inter-assay variance was determined by repeating the assay at six different days by the same investigator. These experiments were performed in parallel at our laboratory and at the National Academy of Inspection and Quarantine, China. The coefficient of variation for the cell concentrations above the cut-off value (104 CFU/ml) varied between 9% and approximately 12% (Table 1 ). To evaluate the scanning process by the UPT-based biosensor, the test strip was scanned repeatedly (n = 10), resulting in an average CVs of less than 5% in peak height for test and control line reads at any time.
Table 1.
Inter-assay variation of the UPT-LF immunoassay system
| Sample | Mean ratio (VT/VC) ± S.D. |
|
|---|---|---|
| Institute of Microbiology and Epidemiology | National Academy of Inspection and Quarantine | |
| Negative control | 0.203 ± 0.015 | 0.237 ± 0.017 |
| S5 (104 CFU/ml) | 0.592 ± 0.053 | 0.614 ± 0.065 |
| S4 (105 CFU/ml) | 1.180 ± 0.135 | 1.173 ± 0.116 |
| S3 (106 CFU/ml) | 2.528 ± 0.267 | 2.537 ± 0.285 |
| S2 (107 CFU/ml) | 5.129 ± 0.568 | 5.068 ± 0.518 |
| S1 (108 CFU/ml) | 6.272 ± 0.635 | 6.285 ± 0.701 |
S.D.: standard deviation, (n = 10, same investigator, different batches of test strips used).
3.3. Quantitative detection of Y. pestis by the UPT-LF from lung specimens of the experimentally infected mice
A 10-fold serial dilution of pure cultures of Y. pestis EV76 ranging from 108 to 104 CFU/ml in the dilution buffer was assayed and the ratio V T/V C was plotted against the logarithmic cell number for the standard curve. A reliable correlation of coefficient (r) was observed between them (r = 0.97857), and a good linearity was displayed throughout the entire measuring range (Fig. 6 ). By applying the corresponding standard curve, the ratio V T/V C of each unknown sample could be converted into the cell number in the sample. To examine the accuracy further, we tested ten different samples by blind experiment. The results of quantitative analysis showed a good correlation (r = 0.96842, p < 0.001). We also tested 51 lung tissue homogenates from the experimentally infected Balb/c mice by the UPT-LF and calculated bacterial CFUs by converting the ratio into the cell count. The correlation between the UPT-LF assay and the plate counting was evaluated with these 51 lung tissue homogenates. There was a significant correlation (r = 0.92406, p < 0.001) between the two assays (Fig. 7 ).
Fig. 6.

Correlation between the ratio VT/VC and the log (Y. pestis EV76 CFU/ml) in the dilution buffer. Six repeated tests of each concentration were performed.
Fig. 7.
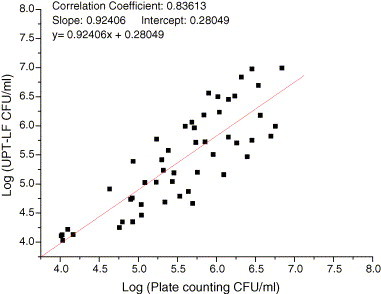
Correlation between the UPT-LF and the plate counting for Y. pestis strain 201 in lung samples of the experimentally infected Balb/c mice.
4. Conclusions
This study demonstrates the feasibility of combining a UPT-based biosensor with an LF immunoassay to create a rapid, on-site testing method for quantitative detection of the whole cells of Y. pestis. We developed and evaluated this assay by using pure cultures of Y. pestis EV76 as a model. By using a sandwich format, we observed a good linearity between the signal ratio (V T/V C) and log CFU/ml of Y. pestis above the detection limit, which was approximately 104 CFU/ml. So the quantitative detection of Y. pestis could be easily achieved by the UPT-LF and it was confirmed by applying it to testing the lung tissue homogenates from the experimentally infected Balb/c mice by Y. pestis. The precision of the intra- and inter-assay was below 15% (coefficient of variation, CV). The specificity of this assay was also satisfactory because no cross-reactivity with related Gram-negative enteric bacteria was found. Furthermore, 104 to 108 CFU/ml of Y. pestis could be specifically and sensitively detected when 108 CFU/ml of Y. pseudotuberculosis were mixed together in the sample. The assay, which does not need washing and incubation steps, can be completed within 30 min.
To our knowledge, this is the first report of the combined use of a UPT-based biosensor and an LF immunoassay for quantitative detection of the whole cells of Y. pestis. The method described here is rapid, specific and sensitive; and it has the potential to be optimized for greater sensitivity for on-site detection. Therefore, the described method can be used for detection and monitoring of plague in combination of an LF immunoassay and a UPT-based biosensor. Moreover, the UPT-LF assay strips can be easily adapted for detecting other microorganisms, as we have applied this assay to detection of E. coli O157:H7, Bacillus anthracis spores and SARS-CoV etc.
Acknowledgements
We highly appreciate Ms. Jin Wang, Hongxia Wang and Xiangxiu Qin for their assistant in antibody preparation. This work was financially supported by the National High Technology Research and Development Program of China (Program 863, No. 2002AA215011) and the National Natural Science Foundation of China (No. 60378024).
Biographies
Zhongqiang Yan received his Bachelor degree of Science in Medicine from Tianjin Medical University in 1999. Since September 2003, he has been working toward the Master degree of Medical Science at the Laboratory of Analytical Microbiology, Institute of Microbiology and Epidemiology, Academy of Military Medical Science, Beijing. His research interest is the development of on-site detection techniques for medically important pathogens.
Lei Zhou received her Bachelor degree of Science from Hebei Normal University in 2001 and her Master degree of Science in the Institute of Microbiology and Epidemiology, Academy of Military Medical Science, Beijing in 2004. Since September 2004, she has been working toward the PhD degree of Science in the same institute. Her research interests include the surface modification and activation of up-converting phosphor and the design of UPT-based biosensor.
Yongkai Zhao is an assistant researcher in Shanghai Institute of Optics and Fine Mechanics (SIOM), Chinese Academy of Sciences. He received his Bachelor degree in Mechanical Engineering from Huazhong University of Science and Technology, and his Master degree in Optical Engineering from SIOM in 2004. His interests focus on optical biosensors, mechanical design of optical instrument.
Jing Wang is an associate professor in Institute of Health Quarantine, Chinese Academy of Inspection and Quarantine. She received a Master degree of Science in Medicine in 1995 from Chinese Academy of Preventive Medicine. Since September 2004, she has been working toward the PhD degree of Medical Science at the Institute of Microbiology and Epidemiology, Academy of Military Medical Science, Beijing. Her research interests focus on development of rapid assay for infectious disease pathogens.
Lihua Huang received her Master degree of Engineering in Huazhong University of Science and Technology in 2003. Now she is an assistant researcher in Shanghai Institute of Optics and Fine Mechanics, Chinese Academy of Sciences. Her interest is optoelectronic measure and control.
Kongxin Hu is an assistant researcher in the Department of External Infectious Diseases, Chinese Academy of Inspection and Quarantine. In July of 2004, he received his PhD from the Chinese Center for Disease Control and Prevention. His research interests focus on development of rapid assay for infectious disease pathogens.
Haihong Liu received her Bachelor degree of Science from Shandong medical University in 1999 and her Master degree of Science in 2004 from the Institute of Microbiology and Epidemiology, Academy of Military Medical Science, Beijing. Since September 2004, she has been working toward the PhD degree of Science in the same institute. Her research interests include chemical taxonomy of bacteria and rapid detection of pathogen by nucleic acid-based assays.
Hong Wang received her Bachelor degree of Science in Medicine from Jilin Medical College in 1986 and her Master degree of Medical Science from the same University in 2003. Since then, she has been working toward the PhD degree of Medical Science at the Institute of Microbiology and Epidemiology, Academy of Military Medical Science, Beijing. Her research interests include histopathology and molecular pathology of infectious diseases.
ZhaoBiao Guo is a senior technician in the Institute of Microbiology and Epidemiology, Academy of Military Medical Science, Beijing. His interest is the development of rapid detection methods for pathogen.
Yajun Song is an associate professor in the Institute of Microbiology and Epidemiology, Academy of Military Medical Science, Beijing. He received his Bachelor degree of Science from Nankai university and his Master degree in 1999 and his PhD degree in 2003 from the institute he is working now. His interests include researches on bacterial genomics and microevolution of pathogen.
Huijie Huang is a professor in Shanghai Institute of Optics and Fine Mechanics (SIOM), Chinese Academy of Sciences. He received his Bachelor degree in Optical Instrument from Zhejiang University in 1989, and his Master degree in Optical Instrument in 1992 and Doctor degree in Optical Engineering in 2005 from SIOM. He joined SIOM in 1992. His interests include laser lithography, optical/laser particle counters, optical biosensors, optical measurement and test, and optical and mechanical design.
Ruifu Yang is a professor in the Institute of Microbiology and Epidemiology, Academy of Military Medical Science, Beijing. He received his Bachelor degree of Science in 1985 from Hebei University of Medicine and his Master degree in 1998 and his PhD degree in 2002 from the institute he is working now. His interests include development of rapid methods for detection of medically important pathogens, bacterial genomics and pathogenesis, and microbial forensics.
References
- 1.Perry R.D., Fetherston J.D. Yersinia pestis-etiologic agent of plague. Clin. Microbiol. Rev. 1997;10:35–66. doi: 10.1128/cmr.10.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kortepeter M., Parker G. Potential biological weapons threats. Emerg. Infect. Dis. 1999;5:523–527. doi: 10.3201/eid0504.990411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Human plague in 2002 and 2003. Wkly. Epidemiol. Rec. 2004;79(33):301–306. [PubMed] [Google Scholar]
- 4.Williams J.E., Arntzen L., Robinson D.M., Cavanaugh D.C., Isaacson M. Comparison of passive haemagglutination and enzyme-linked immunosorbent assay for serodiagnosis of plague. Bull. WHO. 1982;60:777–781. [PMC free article] [PubMed] [Google Scholar]
- 5.Hinnebusch J., Schwan T.G. A new method for plague surveillance using the polymerase chain reaction to detect Yersinia pestis in fleas. J. Clin. Microbiol. 1998;31:1511–1514. doi: 10.1128/jcm.31.6.1511-1514.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Higgins J.A., Ezzell J., Hinnebusch B.J., Shipley M., Henchal E.A., Ibrahim M.S. 5′ Nuclease PCR assay to detect Yersinia pestis. J. Clin. Microbiol. 1998;38:2284–2288. doi: 10.1128/jcm.36.8.2284-2288.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neubauer H., Meyer H., Prior J., Aleksic S., Hensel A., Splettstoesser W. A combination of different polymerase chain reaction (PCR) assays for the presumptative identification of Yersinia pestis. J. Vet. Med. B. 2000;47:573–580. doi: 10.1046/j.1439-0450.2000.00384.x. [DOI] [PubMed] [Google Scholar]
- 8.Herbert T., Emil C.R., Sascha A.D., Dimitrios F., Alexander R., Olfert L., Heinrich N. Rapid detection of Yersinia pestis with multiplex real-time PCR assays using fluorescent hybridization probes. FEMS Immunol. Med. Microbiol. 2003;38:117–126. doi: 10.1016/S0928-8244(03)00184-6. [DOI] [PubMed] [Google Scholar]
- 9.Chanteau S., Rahalison L., Ratsitorahina M., Mahalfaly M., Rasolomaharo M., Boisier P., O’Brien T., Aldrich J., Keleher A., Morgan C., Burans J. Early diagnosis of bubonic plague using F1 antigen capture ELISA assay and rapid immunogold dipstick. Int. J. Med. Microbiol. 2000;290:279–283. doi: 10.1016/S1438-4221(00)80126-5. [DOI] [PubMed] [Google Scholar]
- 10.Wolf D.S., Lila R., Roland G., Heinrich N., Suzanne C. Evaluation of a standardized F1 capsular antigen capture ELISA test kit for the rapid diagnosis of plague. FEMS Immunol. Med. Microbiol. 2004;41:149–155. doi: 10.1016/j.femsim.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Zuk R.F., Ginsberg V.K., Gouts T., Rabbie J., Merrick H., Ullman E.F., Fischer M.M., Sizto C.C., Stiso S.N., Litman D.J. Enzyme immunochromatography—a quantitative immunoassay requiring no instrumentation. Clin. Chem. 1985;31:1144–1150. [PubMed] [Google Scholar]
- 12.Reddy J.R., Kwang J., Lechtenberg K.F., Kham N.C., Prasad Reddy B., Changappa M.M. An immunochromatogarphic serological assay for the diagnosis of Mycobacterium tuberculosis. Comp. Immun. Microbiol. Infect. Dis. 2002;25:21–27. doi: 10.1016/s0147-9571(01)00016-9. [DOI] [PubMed] [Google Scholar]
- 13.Hasegawa W., Yamada T., Azumi J., Honda T., Yanagiya T. The establishment of highly sensitive monoclonal antibodies for influenza viruses and development of the new lateral-flow test strip device. Int. Congr. Ser. 2004;1263:259–262. [Google Scholar]
- 14.R.S. Niedbala, T.L. Vail, H. Feindt, S. Li, J.L. Burton, Multiphoton up-converting phosphors for use in rapid immunoassays, in: Gerald E. Cohn (Ed.), In-Vitro Diagnostic Instrumentation, Proc. SPIE, 3913 (2000) 193–203.
- 15.Hampl J., Hall M., Mufti N.A., Yao Y.M., MacQueen D.B., Wright W.H., Cooper D.E. Up-converting phosphor reporters in immunochromatographic assays. Anal. Biochem. 2001;288:176–187. doi: 10.1006/abio.2000.4902. [DOI] [PubMed] [Google Scholar]
- 16.Van De Rijke F., Zijlmans H., Li S., Vail T., Raap A.K., Niedbala R.S., Tanke H.J. Up-converting phosphor reporters for nucleic acid microarrays. Nat. Biotechnol. 2001;19:273–276. doi: 10.1038/85734. [DOI] [PubMed] [Google Scholar]
- 17.Corstjens P.L.A.M., Zuiderwijk M., Nillsson M., Feindt H., Niedbala R.S., Tanke H.J. Lateral-flow and up-converting phosphor reporters to detect single-stranded nucleic acids in a sandwich-hybridization assay. Anal. Biochem. 2003;312:191–200. doi: 10.1016/s0003-2697(02)00505-5. [DOI] [PubMed] [Google Scholar]
- 18.Zuiderwijk M., Tanke H.J., Niedbala R.S., Corstjens P.L.A.M. An amplification-free hybridization-based DNA assay to detect Streptococcus pneumoniae utilizing the up-converting phosphor technology. Clin. Chem. 2003;36:401–403. doi: 10.1016/s0009-9120(03)00057-2. [DOI] [PubMed] [Google Scholar]
- 19.Zijlmans H., Bonnet J., Burton J., Kardos K., Vail T., Niedbala R.S., Tanke H.J. Detection of cell and tissue surface antigens using up-converting phosphors: a new reporter technology. Anal. Biochem. 1999;267:30–36. doi: 10.1006/abio.1998.2965. [DOI] [PubMed] [Google Scholar]
- 20.Niedbala R.S., Feindt H., Kardos K., Vail T., Burton J., Bielska B., Li S., Milunic D., Bourdelle P., Vallejo R. Detection of analytes by immunoassay using up-converting phosphor technology. Anal. Biochem. 2001;293:22–30. doi: 10.1006/abio.2001.5105. [DOI] [PubMed] [Google Scholar]
- 21.Zhou D., Tong Z., Song Y., Han Y., Pei D., Pang X., Zhai J., Li M., Cui B., Qi Z., Jin L., Dai R., Du Z., Wang J., Guo Z., Huang P., Yang R. Genetics of metabolic variations between Yersinia pestis biovars and the proposal of a new biovar, microtus. J. Bacteriol. 2004;186:5147–5152. doi: 10.1128/JB.186.15.5147-5152.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jung B.Y., Jung S.C., Kweon C.H. Development of a rapid immunochromatographic strip for detection of Escherichia coli O157. J. Food Prot. 2005;68:2140–2143. doi: 10.4315/0362-028x-68.10.2140. [DOI] [PubMed] [Google Scholar]


