Abstract
Vaccination is a critical component of cattle health management. Effective cattle vaccine programs should consider the timing of vaccination in relation to expected disease challenge, risk for wild-type exposure of various bovine pathogens, and host factors during vaccination. Nearly all consulting veterinarians recommend vaccination of stressed, high-risk calves on feedlot arrival. However, this recommendation fails to consider several factors associated with vaccine efficiency. Further research evaluating vaccine interactions in stressed cattle and potential additive effects of endotoxin from multiple bacterin administration may reveal new evidence-based vaccination guidelines for cattle in the various segments of beef and dairy production systems.
Keywords: Bovine respiratory disease, Cattle, Endotoxin, Vaccination management
Key points
-
•
When administered under appropriate conditions, vaccines provide safe, effective, and economically important immunologic prevention of respiratory and other infectious bovine diseases.
-
•
Modified-live virus (MLV) vaccination against respiratory pathogens in cattle on feedlot arrival has been unanimously recommended by consulting veterinarians.
-
•
There is surprisingly limited, but emerging literature, describing the efficiency and safety of vaccination in different cattle production environments, including delayed administration of MLV vaccines in stressed, high-risk cattle.
-
•
Stress-induced immunosuppression in cattle is likely during weaning, marketing, and relocation to a stocker or feedlot facility and should be considered when designing efficient vaccination protocols.
-
•
Endotoxin concentration and handling of gram-negative bacterins should be considered when designing vaccination protocols for cattle to reduce the potential for adverse reactions.
Introduction
Prevention of infectious diseases in beef cattle is critically important, yet difficult because of the segmented infrastructure of the beef industry. Cattle progress through different stages of production and may experience exposure to novel pathogens, transportation and relocation stress, different management, and commingling with other animals.1, 2 Although there are many potential infectious disease challenges that beef cattle may encounter, bovine respiratory disease (BRD) remains the most prevalent and costly disease affecting cattle production in North America, and the impact is greatest in the stocker and feedlot sectors of the beef industry.3 Stress-induced immune dysfunction, viral infection, and bronchopneumonia caused by bacteria are interwoven within the complicated etiology of BRD. Therefore, vaccination against viral and bacterial agents involved in BRD is a vital instrument in the “animal health tool box” for cow-calf, stocker, and feedlot operators.
Some important considerations regarding vaccination of beef cattle at the cow-calf, preconditioning, stocker, and feedlot phases of beef production include the following:
-
•
Cow-calf phase: at birth, branding, and weaning, beef calves could experience acute (short-term) rather than chronic (long-term) stress, which may result in priming of the immune system and contribute to an enhanced vaccine response in calves.4 In general, the timing of vaccination during the cow-calf phase is most favorable because it allows sufficient time for vaccinates to develop immunologic protection before natural challenge with BRD-causative agents during and after transition to a stocker or feedlot facility.
-
•
Preconditioning phase: calves that are vaccinated and retained on their ranch of origin after weaning for other preparatory management exhibit less morbidity and health costs at the feedlot and generate greater net return to the cow-calf producer because calf value is increased.5, 6, 7, 8 Despite clear health improvements for preconditioned cattle, the industry-wide adoption of this management practice is low, as only 39% of all beef operations vaccinated calves against respiratory disease before sale.9
-
•
Stocker phase: most beef calves placed in stocker programs are lightweight, immunologically naïve, and stressed. Veterinary practitioners and stocker producers should consider vaccine safety and the potential for inadvertent antigenic enhancement of modified-live virus (MLV) vaccines administered to newly received stocker calves. Because subsequent disease challenge in the feedlot phase is probable, stocker calves should be administered vaccines with adequate time for immunization to occur before feedlot shipment. However, stocker producers should consider delaying MLV vaccination for 14 to 30 days after arrival, as improved health and performance outcomes have been reported in high-risk stocker calves using this strategy.10, 11
-
•
Feedlot phase: the adoption rate of respiratory vaccination in the feedlot is nearly 100% due to tradition, practical design, and labor structure of feedlot facilities, and the relatively low cost of vaccines.12 However, further research is needed to understand the efficiency of vaccination against the numerous disease-causing agents that exist in the feedlot. As suggested for the stocker phase, delayed MLV vaccination may improve health outcomes in auction-derived feedlot cattle.13
Current vaccination recommendations
Beef cow-calf operations and feedlots across North America are frequently provided vaccine recommendations from veterinary practitioners or other sources; however, a scarcity of literature exists that summarizes and reports these recommendations at the cow-calf level.14 In contrast, several publications exist that describe recommendations and practices for vaccination and health management at the feedlot level.12, 15, 16
Results from a US Department of Agriculture (USDA)-Animal and Plant Health Inspection Service survey17 indicated that although vaccinating cattle is a relatively common practice in the cow-calf sector, it is not universally adopted, which leaves a significant portion of the US beef cattle population susceptible to numerous preventable diseases. Only 68.9% of cow-calf operations vaccinated cattle for any disease in 2007,17 which is in sharp contrast to a 2016 survey of veterinary practitioners indicating that 93% of cow-calf operations in the United State have a vaccination plan in place for cattle.14 It is possible that recommendations and/or adoption of vaccination protocols changed over the 9-year lapse between surveys; however, it is more likely that a discrepancy between veterinarian recommendations of vaccination and implementation by beef cow-calf operations exists. This is further supported by a survey indicating that only 39% of all beef operations vaccinated calves against respiratory disease before sale,9 despite the overwhelming recommendation of veterinarians to vaccinate calves against BRD pathogens during the cow-calf production phase.
There are 3 distinct times in the cow-calf sector when veterinarians recommend initial vaccinations: at branding, before weaning, and after weaning. According to a survey,14 the most common vaccine antigens recommended for calves vaccinated at branding were clostridial (96%), infectious bovine rhinotracheitis virus (IBRV; 94%), bovine respiratory syncytial virus (BRSV; 91%), parainfluenza-3 virus (PI-3V; 90%), and bovine viral diarrhea virus (BVDV) Type 1 and 2 (78% and 77%, respectively). Eighty percent of veterinarians recommended MLV vaccines at this time, with 12% of veterinarians recommending killed virus vaccines at branding.
When vaccinating calves for the first time before weaning, the most frequently recommended vaccine antigens were IBRV (99%), BRSV (98%), BVDV Types 1 and 2 (96%), PI-3 (93%), clostridial (77%), and Mannheimia haemolytica (77%).14 Before weaning, most veterinarians recommended using MLV over killed virus vaccines (90% and 10%, respectively). First-time vaccination recommendations for cattle after weaning were for BVDV Type 2 (97%), IBRV (97%), BVDV Type 1 (96%), BRSV (96%), and PI-3V (91%).14 As calf age increased (ie, preweaning vs postweaning), there was a slight increase in the percentage of veterinarians who recommended MLV vaccines versus killed virus vaccines (93% and 7%, respectively).14
Although the preceding information is consistent with other vaccine recommendations18 and reports,19, 20, 21 where most veterinarians recommended routine administration of respiratory vaccines to beef calves, the USDA reported9 that 60.6% of beef cow-calf operations (accounting for 30% of the US cattle population) did not vaccinate calves for respiratory disease from birth until the time they were sold. This discrepancy between veterinarian recommendation and producer implementation is concerning, given that 99% of veterinarians in the United States and Canada recommend some type of vaccination protocol at the cow-calf level of production.14
For the feedlot sector, however, there is a stark contrast in respiratory vaccine use, as administration of a multivalent respiratory vaccine during initial feedlot processing is nearly 100%.12 Furthermore, consulting feedlot veterinarians revealed that they unanimously recommend respiratory vaccination during initial processing of cattle considered high risk.12 Despite a limited amount of research-based evidence to support on-arrival vaccination of high-risk cattle, it has been a routine practice in feedlots for decades. Several previous reviews have examined respiratory vaccination outcomes in the production setting and convey a general lack of evidence for vaccine efficiency in high-risk, newly received beef cattle.22, 23, 24 Therefore, a need exists to critically examine current vaccination paradigms in the beef industry and consider the safety of vaccination under various conditions (eg, acute vs chronic stress, production phase, commingling), the types of vaccines selected (MLV vs killed virus), and timing of vaccine administration in relation to expected natural pathogen challenge.
Vaccine efficacy versus efficiency
The distinction between vaccine efficacy and efficiency is critical for understanding vaccination management. Commercial vaccines that are deemed efficacious via USDA approval standards for biologics may not be efficient under all circumstances or in all vaccinates in the production setting.25 Vaccine efficacy is defined as the percent reduction in disease incidence and pathology in a vaccinated group compared with an unvaccinated group. Typically, this is determined from a controlled BRD challenge model with previously vaccinated and nonvaccinated calves that have been inoculated with a respiratory virus and bacteria. A vaccine may also be considered efficacious if it has biological activity and stimulates an active immune response against the agents in the vaccine.
Vaccine efficiency may be defined as the ability of a vaccine to improve health outcomes in the production setting.26 In commercial cattle production, vaccine efficiency translates to a significant reduction in clinical illness and/or death loss, improvement in weight gain, and a clear economic advantage.27 Although bovine vaccines must demonstrate efficacy to receive USDA approval, the primary concern for producers is the efficiency, or effectiveness, of the vaccine under field conditions. It is important to note that vaccine efficiency is always associated with vaccine efficacy; however, vaccine efficacy does not always result in vaccine efficiency.
Vaccine safety
Vaccine safety is vital to ensuring the efficiency of a vaccine. The safety of a vaccine may be compromised by several factors including the following:
-
•
Improper time of administration of vaccine, such as during acute infection with wild-type virus and concurrent administration of MLV vaccine or in otherwise unhealthy animals
-
•
Improper storage and/or handling of vaccine (ie, temperature, UV light, excessive shaking, expiration)
-
•
Disrupted physiologic and immunologic status of cattle being vaccinated
-
•
Manufacturing errors that may compromise safety of a particular lot group of vaccine28
Based on the segmented structure of the beef industry, millions of cattle annually enter the feedlot considered high-risk; however, the USDA approval process does not require examining the safety of vaccination in highly stressed, immunosuppressed cattle.28 In fact, the USDA CVM Web site states, “Products are shown to be effective in healthy animals. A protective immune response may not be elicited if animals are incubating an infectious disease, are malnourished or parasitized, are stressed due to shipment or environmental conditions, are otherwise immunocompromised, or the vaccine is not administered in accordance with label directions.”29 The new single claim vaccine label amended by USDA in 2019 states, “This product has been shown to be effective for the vaccination of healthy cattle against (antigen).” For a vaccine to “work,” it must stimulate the immune system; therefore, mild local and systemic reactions to vaccines are not uncommon.30 It is widely accepted that physiologic stress has an impact on the bovine immune system and newly arrived feedlot cattle are often highly stressed; therefore, it is prudent to consider the interaction of stress and vaccination when providing vaccine recommendations to cattle producers.
Stress and vaccine efficiency
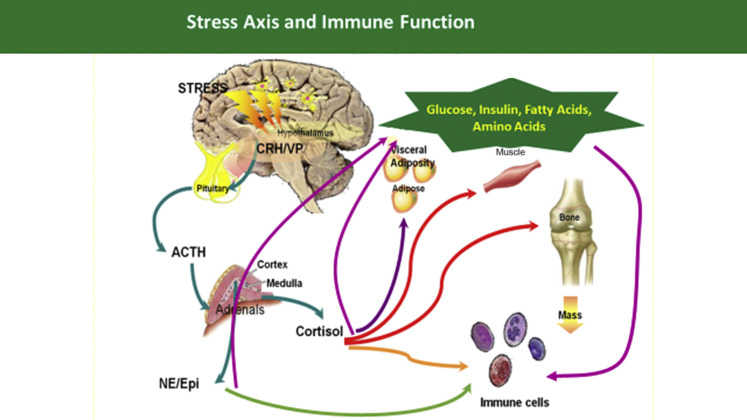
Stress stimulates the hypothalamic-pituitary-adrenal axis (Fig. 1 ) and may be differentiated into 2 types: (1) acute stress, that is, short-term (<24 hours), and (2) chronic stress that occurs when a stressor(s) is imposed on an animal for days or even weeks. The importance of this distinction is due to the differential impact that acute or chronic stress may have on vaccine response. It is postulated that acute stress has the ability to prime the immune system, and possibly potentiate the vaccine response4; whereas, chronic stress is known to inhibit the humoral immune response to vaccination.31 However, these phenomena are difficult to evaluate in research and are rarely explored in the bovine model.
Fig. 1.
The hypothalamic-pituitary-adrenal axis and some of the biological components affected by cortisol and epinephrine. ACTH, adrenocorticotropic hormone; CRH/VP, corticotropin-releasing hormone/vasopressin.
Stress and vaccine interactions in cattle are also poorly understood. Nevertheless, a different humoral response to killed versus MLV respiratory antigens in immunosuppressed cattle may exist. An inhibited antibody response against killed Salmonella dublin vaccination was observed when calves were concurrently administered cortisol.32 An opposing antibody response was noted when replicating MLV vaccine antigens (bovine herpesvirus-1 [BHV-1] and BVDV) were administered concurrent with increased stress-induced cortisol concentrations; the antibody response to these viruses was enhanced in stress-challenged cattle.32 These findings are likely due to increased cortisol causing immunosuppression that allowed increased antigenicity of MLV vaccine antigens and a subsequently enhanced antibody titer response. Cattle treated with an “acute,” “chronic,” or “control” stress model, induced by dexamethasone treatment and vaccinated with a multivalent combination respiratory vaccine-bacterin, generated different antibody titer responses depending on the antigen-specific antibody evaluated.33 The leukotoxin-specific antibody response from a M haemolytica toxoid was least in the chronic dexamethasone-challenged steers, intermediate for acute, and greatest for control steers.33 Conversely, both the BHV-1- and BVDV-specific antibody response from the MLV fraction of the combination vaccine was greatest for chronic dexamethasone-challenged steers, intermediate for acute, and least for control steers.33 The greater antibody titer for dexamethasone-treated cattle administered MLV is probably a result of much greater replication of the live-attenuated vaccine agents in the immunosuppressed host. Therefore, MLV vaccination in high-risk cattle that are immunosuppressed may not be safe, which is a primary rationale for delayed vaccination recommendations.
Delayed vaccination
Almost all stocker and feedlot facilities administer a parenteral multivalent MLV respiratory vaccine during initial processing with the goal of stimulating a systemic immune response against viral agents involved in BRD. However, because there is limited research to support vaccine efficiency in high-risk, newly received cattle, the practice of delaying the MLV vaccine for a time has been considered to allow the immune system to return to a homeostatic state and postpone replicating antigen exposure during the time of arrival when stress-induced immunosuppression is greatest. A previous review34 summarized important considerations for vaccinating high-risk calves and indicated that existing literature for vaccine efficiency in newly received feedlot cattle is inconsistent. The multitude of vaccine products and regimens, random variation of population dynamics between studies or pens within a study, difficulties with clinical BRD diagnosis, and sample size limitations of research were noted as possible reasons for inconsistent findings.34
In a study with 528 high-risk stocker calves,10 a delayed (14 days) MLV administration procedure was evaluated against the traditional on-arrival (day 0) MLV administration; calves receiving the delayed procedure had improved performance and numerically less BRD-associated morbidity, relapse, and mortality. A large pen study13 with 5179 auction-derived heifers observed a decrease in the number of heifers treated twice for BRD and numerically less morbidity, mortality, and case fatality rate for those receiving their initial MLV at 30 days after feedlot arrival compared with on-arrival. However, other small studies suggest no difference in health or performance for either the on-arrival or delayed procedure35, 36, 37 or vaccine versus control38 in high-risk cattle. It is valuable to mention that in smaller studies it can be problematic to analyze proportional data means while avoiding a statistical type II error; therefore, when interpreting these small pen studies, the practitioner should consider evidence of biological relevance that may exist in the absence of statistical significance. In another study comparing MLV respiratory vaccination or control (no MLV vaccine) during the stocker receiving period, the vaccinated calves had significantly greater odds of BRD morbidity and mortality.11 Ultimately, difficulty arises when assessing the current literature with regard to the benefits, or lack thereof, of vaccinating cattle immediately on feedlot arrival, due to the variation of cattle conditions (eg, immune status, marketing channels used, age, breed) and the complex nature of BRD. Therefore, it is also important to consider the biological implications of vaccine components, such as endotoxins, on the immune system.
Immunity against endotoxin
In general, bacteria produce 2 primary types of toxins that are classified as either endotoxins or exotoxins. Endotoxin was first defined in 1892 as a heat-stable toxic substance released when the cell membrane of a microorganism is disrupted.39 Endotoxins are a major component of the outer cell wall of the gram-negative bacteria40 and are not secreted by live bacteria but released from bacterial cells when the cell is killed or lysed. The term endotoxin is most commonly associated with the lipopolysaccharide (LPS) cell membrane fractions of bacteria; however, endotoxins include peptidoglycans, lipoproteins, and other bacterial components.39 In general, endotoxins are considered to be moderate in their toxicity and antigenicity,40 but bovines are particularly sensitive to endotoxin41 and differences in endotoxin reactivity, or endotoxigenicity, between bacterial antigens exist (Table 1 ).
Table 1.
Endotoxigenicity of common bacterial antigens used in cattle production
| Antigen (Primary Bovine Disease) | Endotoxigenicity of Antigen |
|---|---|
| Escherichia coli (mastitis) | High |
| Moraxella bovis (pinkeye) | High |
| Histophilus somni (bronchopneumonia) | High |
| Salmonella spp. (salmonellosis) | Moderate |
| E coli (scours) | Moderate |
| Mannheimia haemolytica (bronchopneumonia) | Moderate |
| Pasteurella multocida (bronchopneumonia) | Moderate |
| Leptospira spp. (leptospirosis) | Low |
Exotoxins, such as leukotoxins, are diffusible proteins that are primarily produced and actively released from bacteria during log-phase growth. Unlike endotoxins, exotoxins are heat-liable, highly antigenic proteins that are also considered highly toxic. However, similar to endotoxins, exotoxins may be released when bacterial cells are lysed. In 1959, Sambhu Nath De42 discovered the first exotoxin by isolating the toxin that causes cholera. This seminal work led to subsequent research on immunologic responses to toxins and the development of vaccines, or toxoids containing attenuated toxin, and antitoxins.43 Exotoxins are often used for vaccine development via chemical or heat inactivation of the exotoxin to create a toxoid. Although the resulting toxoid antigen maintains immunogenicity, the biological properties associated with exotoxin-related toxicity are disabled. The bacterial exotoxins can be classified threefold according to their mode of action: Type I are membrane-acting toxins that bind surface receptors and stimulate transmembrane signals; type II are membrane-damaging toxins that directly affect cell membranes by forming pores or disrupting the lipid bilayers of the cell membranes; type III toxins modify an intracellular target molecule by translocating an active enzymatic component into the cell.44
The innate immune system does not distinguish every possible antigen within the host, rather a few highly conserved structures present in many different microorganisms. These conserved structures are known as pathogen-associated molecular patterns45 (PAMPs) and interact with receptors on the surface of the immune cells.46 For example, the lipid A domain in LPS represents a specific PAMP associated with infection of gram-negative bacteria47, 48 and PAMP recognition by the innate immune system is mediated through a diverse group of receptors known as pattern-recognition receptors49 (PRRs). The PRRs are divided into 3 functional groups: (1) circulating humoral proteins, such as the endotoxin receptor CD14 and complement proteins, (2) endocytic receptors that are expressed on the cell surface and mediate endocytosis, and (3) signaling receptors, such as toll-like receptors, that are expressed on the surface of the cell.50
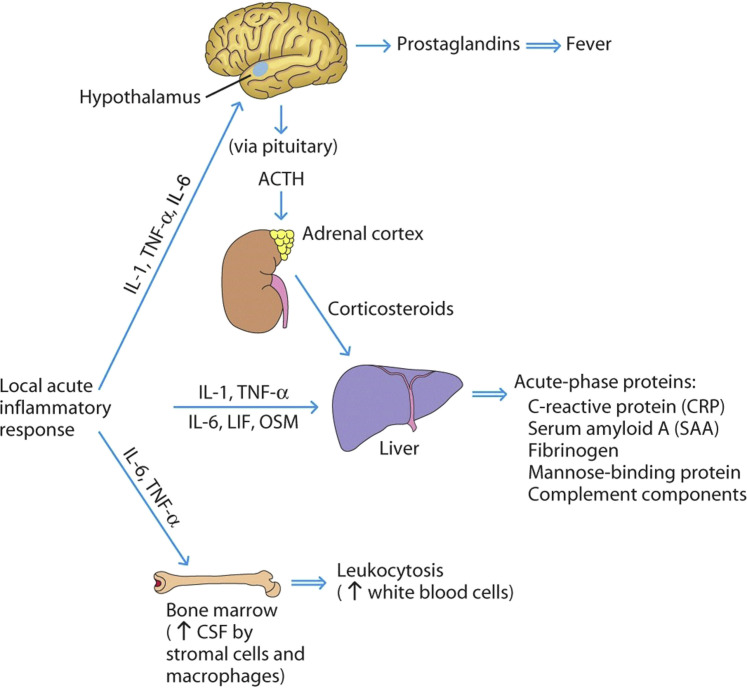
Endotoxin exposure in cattle results in a rather predictable and conserved set of physiologic and immunologic responses known as the acute-phase response, primarily mediated by the innate immune system.51, 52 Some of the more commonly recognized inflammatory reactions include increased production of proinflammatory cytokines, fever, increases in circulating white blood cells, increased production of acute-phase proteins (APPs) by hepatocytes, and behavioral changes (Fig. 2 ). Behavioral changes can be unambiguous and varied, including lethargy, anorexia, decreased social and sexual behavior, decreased aggressive behavior, and hyperalgesia. The mechanisms by which proinflammatory cytokines, such as tumor necrosis factor-α, interleukin (IL)-1, and IL-6 induce sickness behaviors such as anorexia and depression remain to be fully elucidated; however, it has been suggested that cytokines directly act on the organum vasculosum laminae terminalis region of the brain, perhaps via intermediate messengers such as prostaglandins. Stimulation of prostaglandins could have a direct effect on the central nervous system and/or stimulate local production of cytokines in the brain.53
Fig. 2.
Diagram of the inflammatory response. ACTH, adrenocorticotropic hormone; CSF, cerebrospinal fluid; LIF, leukemia inhibitory factor; OSM, outer surface membrane; TNF, tumor necrosis factor.
(From R. Goldsby, T. Kindt, B. Osborne, J. Kuby. Immunology, 5th Edition. W. H. Freeman; 2002; with permission.)
A group of APPs are also released during endotoxin exposure, inflammation, bacterial infection, or physical injury. These APPs become an integral component of proper immunologic function and restoration of homeostasis. In addition, APPs are associated with alterations in plasma iron, zinc, and copper which may play an important role in overall immune function and modulation of bacterial growth in the animal. In cattle, some primary APPs include haptoglobin, serum amyloid A, fibrinogen, α1-acid glycoprotein, ceruloplasmin, α1-antitrypsin, α1-antichymotrypsin, α2-macroglobulin, and fetuin.54 As an indicator of inflammation and/or disease, haptoglobin, α1-acid glycoprotein, fibrinogen, and serum amyloid A are the most commonly evaluated APPs in bovines.51, 55, 56, 57
Endotoxin in vaccines
Vaccines against gram-negative bacteria may contain endotoxins such as peptidoglycans, lipoproteins, and LPS. Commonly used vaccines against gram-negative bacteria and the associated diseases in cattle production are indicated in Table 2 . Use of bacterins began when a physician named William Coley began treating patients with both live- and heat-killed Serratia marcescens and streptococci to treat sarcomas. This practice, known as Coley toxins, was used for more than 30 years with much success, despite occasionally inducing severe adverse effects, such as extreme fever and toxic shock.58 Today, most gram-negative vaccines contain whole cell modified and/or killed bacteria, with relatively small amounts of free endotoxin, thus resulting in less risk for severe adverse effects after use. Endotoxins in each of these vaccines have different antigenicity based on the bacterium used to produce the vaccine and the structure of the endotoxin molecule present. For example, the LPS molecule can vary structurally between Escherichia coli vaccines depending on the strain used to develop the vaccine, and thus the antigenicity of the LPS present in a vaccine can vary. Although free endotoxin concentrations are generally low, mishandling of vaccines can increase free endotoxin released from the cell wall membrane due to killing or lysis of the bacteria, thereby increasing the antigenicity of the vaccine. Therefore, it is critical that vaccines are handled appropriately to reduce the risk of endotoxicity in vaccinated cattle. Factors that may constitute mishandling of gram-negative bacterins include the following:
-
•
Improper temperature during storage or use leading to increased endotoxin concentration (for example, exposing bacterins to high heat or freezing temperatures can rupture bacterial cells, thus causing the release of endotoxin from the outer cell wall membrane)
-
•
Excessive shaking of bacterins before use, resulting in lysis of the bacterial whole cells or fragments leading to the release of LPS and other endotoxins or exotoxins
-
•
Exposure to UV light (direct sunlight) that may result in cellular degradation and release of free endotoxin
Table 2.
Licensed veterinary biological products containing bacterins, bacterial extracts, and/or toxoids approved for use in cattle
| Product and Form | Licensed Producers |
|---|---|
| Autogenous vaccine, killed virus, autogenous bacterin | SolidTech Animal Health |
| Autogenous vaccine-autogenous bacterin | Biomune Company, Cambridge Technologies, Colorado Serum Company, Elanco US, Hennessy Research Associates, Huvepharma, Kennebec River Biosciences, Newport Laboratories, Phibro Animal Health, Texas Vet Lab |
| Bovine rhinotracheitis vaccine-Haemophilus somnus-Mannheimia haemolytica-Pasteurella multocida-Salmonella typhimurium bacterin-toxoid | Texas Vet Lab |
| Bovine rhinotracheitis vaccine-Leptospira hardjo-pomona bacterin | Boehringer Ingelheim Vetmedica |
| Bovine rhinotracheitis vaccine-Leptospira pomona bacterin | Diamond Animal Health |
| Bovine rhinotracheitis-virus diarrhea vaccine-Campylobacter fetus-Leptospira canicola-grippotyphosa-hardjo-icterohaemorrhagiae-pomona bacterin | Zoetis |
| Bovine rhinotracheitis-virus diarrhea-parainfluenza 3 vaccine-Leptospira canicola-grippotyphosa-hardjo-icterohaemorrhagiae-pomona bacterin | Colorado Serum Company, Diamond Animal Health |
| Bovine rhinotracheitis-virus diarrhea-parainfluenza 3-respiratory syncytial virus vaccine-Campylobacter fetus-Haemophilus somnus-Leptospira canicola-grippotyphosa-hardjo-icterohaemorrhagiae-pomona bacterin | Elanco US |
| Bovine rhinotracheitis-virus diarrhea-parainfluenza 3-respiratory syncytial virus vaccine-Campylobacter fetus-Leptospira canicola-grippotyphosa-hardjo-icterohaemorrhagiae-pomona bacterin | Boehringer Ingelheim Vetmedica, Elanco US, Intervet, Zoetis |
| Bovine rhinotracheitis-virus diarrhea-parainfluenza 3-respiratory syncytial virus vaccine-Haemophilus somnus bacterin | Boehringer Ingelheim Vetmedica |
| Bovine rhinotracheitis-virus diarrhea-parainfluenza 3-respiratory syncytial virus vaccine-Haemophilus somnus-Leptospira canicola-grippotyphosa-hardjo-icterohaemorrhagiae-pomona bacterin | Boehringer Ingelheim Vetmedica, Elanco US |
| Bovine rhinotracheitis-virus diarrhea-parainfluenza 3-respiratory syncytial virus vaccine-Leptospira canicola-grippotyphosa-hardjo-icterohaemorrhagiae-pomona bacterin | Boehringer Ingelheim Vetmedica, Diamond Animal Health, Elanco US, Intervet, Zoetis |
| Bovine rhinotracheitis-virus diarrhea-parainfluenza 3-respiratory syncytial virus vaccine-Leptospira canicola-grippotyphosa-hardjo-icterohaemorrhagiae-pomona-Mannheimia haemolytica bacterin | Boehringer Ingelheim Vetmedica, Elanco US |
| Bovine rhinotracheitis-virus diarrhea-parainfluenza 3-respiratory syncytial virus vaccine-Leptospira hardjo bacterin | Zoetis |
| Bovine rhinotracheitis-virus diarrhea-parainfluenza 3-respiratory syncytial virus vaccine-Mannheimia haemolytica bacterin | Boehringer Ingelheim Vetmedica, Elanco US |
| Bovine rhinotracheitis-virus diarrhea-parainfluenza 3-respiratory syncytial virus vaccine-Mannheimia haemolytica toxoid | Boehringer Ingelheim Vetmedica, Zoetis |
| Bovine rhinotracheitis-virus diarrhea-parainfluenza 3-respiratory syncytial virus vaccine-Mannheimia haemolytica-Pasteurella multocida bacterin-toxoid | Diamond Animal Health |
| Bovine rhinotracheitis-virus diarrhea-respiratory syncytial virus vaccine-Leptospira pomona bacterin | Diamond Animal Health |
| Bovine rotavirus-coronavirus vaccine-Clostridium perfringens type C-Escherichia coli bacterin-toxoid | Elanco US, Zoetis |
| Bovine rotavirus-coronavirus vaccine-Clostridium perfringens types C and D-Escherichia coli bacterin-toxoid | Intervet |
| Bovine rotavirus-coronavirus vaccine-Escherichia coli bacterin | Zoetis |
| Bovine virus diarrhea vaccine-Campylobacter fetus-Leptospira canicola-grippotyphosa-hardjo-icterohaemorrhagiae-pomona bacterin | Zoetis |
| Bovine virus diarrhea vaccine-Leptospira canicola-grippotyphosa-hardjo-icterohaemorrhagiae-pomona bacterin | Zoetis |
| Bovine virus diarrhea vaccine-Mannheimia haemolytica toxoid | Zoetis |
| Trichomonas foetus vaccine, killed protozoa-Campylobacter fetus-Leptospira canicola-grippotyphosa-hardjo-icterohaemorrhagiae-pomona bacterin | Boehringer Ingelheim Vetmedica, Elanco US |
| Clostridium botulinum type C bacterin-toxoid | United Vaccines |
| Clostridium chauvoei-septicum-haemolyticum-novyi-sordellii-perfringens types C and D bacterin-toxoid | Boehringer Ingelheim Vetmedica, Intervet, Zoetis |
| Clostridium chauvoei-septicum-haemolyticum-novyi-sordellii-perfringens types C and D-Haemophilus somnus bacterin-toxoid | Intervet |
| Clostridium chauvoei-septicum-haemolyticum-novyi-sordellii-perfringens types C and D-Mannheimia haemolytica bacterin-toxoid | Zoetis |
| Clostridium chauvoei-septicum-haemolyticum-novyi-sordellii-tetani-perfringens types C and D bacterin-toxoid | Intervet |
| Clostridium chauvoei-septicum-haemolyticum-novyi-tetani-perfringens types C and D bacterin-toxoid | Intervet |
| Clostridium chauvoei-septicum-novyi bacterin-toxoid | Colorado Serum Company |
| Clostridium chauvoei-septicum-novyi-sordellii bacterin-toxoid | Colorado Serum Company |
| Clostridium chauvoei-septicum-novyi-sordellii-perfringens types C and D bacterin-toxoid | Boehringer Ingelheim Vetmedica, Elanco US, Intervet, Zoetis |
| Clostridium chauvoei-septicum-novyi-sordellii-perfringens types C and D-Haemophilus somnus bacterin-toxoid | Boehringer Ingelheim Vetmedica, Intervet, Zoetis |
| Clostridium chauvoei-septicum-novyi-sordellii-perfringens types C and D-Mannheimia haemolytica bacterin-toxoid | Zoetis |
| Clostridium chauvoei-septicum-novyi-sordellii-perfringens types C and D-Moraxella bovis bacterin-toxoid | Boehringer Ingelheim Vetmedica, Intervet |
| Clostridium perfringens type C-Escherichia coli bacterin-toxoid | Elanco US, Intervet, Zoetis |
| Clostridium perfringens types C and D bacterin-toxoid | Elanco US, Intervet, Zoetis |
| Clostridium perfringens types C and D-tetani bacterin-toxoid | Intervet |
| Clostridium tetani-perfringens type D-Corynebacterium pseudotuberculosis bacterin-toxoid | Colorado Serum Company |
| Corynebacterium pseudotuberculosis bacterin-toxoid | Boehringer Ingelheim Vetmedica, Colorado Serum Company |
| Escherichia coli bacterin-toxoid | Merial |
| Haemophilus somnus-Mannheimia haemolytica-Pasteurella multocida bacterin-toxoid | Texas Vet Lab |
| Haemophilus somnus-Mannheimia haemolytica-Pasteurella multocida-Salmonella typhimurium bacterin-toxoid | Texas Vet Lab |
| Mannheimia haemolytica bacterial extract-toxoid | Elanco US |
| Mannheimia haemolytica bacterin-toxoid | Zoetis |
| Mannheimia haemolytica-Pasteurella multocida bacterin-toxoid | American Animal Health, Merial |
| Pasteurella multocida bacterial extract-Mannheimia haemolytica toxoid | Boehringer Ingelheim Vetmedica |
| Salmonella typhimurium bacterin-toxoid | Immvac |
| Staphylococcus aureus bacterin-toxoid | Hygieia Biological Laboratories |
| Clostridium botulinum type B toxoid | Neogen |
| Clostridium perfringens type A toxoid | Elanco US, Intervet |
| Clostridium perfringens type C toxoid | Colorado Serum Company |
| Clostridium perfringens type D toxoid | Colorado Serum Company |
| Clostridium perfringens type D-tetanus toxoid | Colorado Serum Company |
| Clostridium perfringens types C and D toxoid | Boehringer Ingelheim Vetmedica, Colorado Serum Company |
| Clostridium perfringens types C and D-tetanus toxoid | Boehringer Ingelheim Vetmedica, Colorado Serum Company |
| Crotalus atrox toxoid | Hygieia Biological Laboratories |
| Mannheimia haemolytica toxoid | Boehringer Ingelheim Vetmedica, Elanco US, Zoetis |
| Tetanus toxoid | Boehringer Ingelheim Vetmedica, Colorado Serum Company, Intervet, Zoetis |
Data from United States Department of Agriculture, Animal and Plant Health Inspection Service, Veterinary Services, Center for Veterinary Biologics, Veterinary Biological Products; 2019.
Endotoxin stacking
Adverse events associated with endotoxin-containing bacterins occur due to a phenomenon known as endotoxin stacking (ie, giving multiple gram-negative endotoxin-containing vaccines at one time). Due to the potential for endotoxins in bacterins to produce a synergistic or additive response, endotoxin stacking can lead to toxicity that could be fatal.59 As previously mentioned, the mechanism by which endotoxins such as LPS create an immunologic response is via a cytokine cascade. This cascade is influenced by the amount of endotoxin present, whether the endotoxin is bound or free, and host factors that can make an animal more vulnerable to endotoxin. A report noted that endotoxin from multiple bacterial sources resulted in more drastic physiologic and immunologic responses than that of the same endotoxin concentration from a single source. Estimating the frequency with which endotoxin stacking occurs in beef production and the impact on cattle health and performance is difficult, as cattle vaccination protocols differ depending on the producer, veterinarian, and geographic location. However, 2 or more gram-negative vaccines are often administered simultaneously in production settings, and often these bacterins or toxoids are administered concurrent with MLV vaccines and other biological or pharmaceutical products (ie, antimicrobials, anthelmintics) and negative interactions could occur in some cattle, but the interaction of the various animal health products used in cattle is poorly understood.
The physiologic and immunologic status of cattle also should be considered before vaccination with endotoxin-containing products. Sick cattle or cattle exposed to stressful conditions for an extended period should not be vaccinated with endotoxin-containing vaccines, as these cattle may have an altered immune system and be more susceptible to the negative effects of endotoxin. Endotoxins are well known for their pyrogenic properties; therefore, endotoxin vaccination during times of heat stress also should be avoided, as this could potentially increase the overall heat load in the animal. It is again noteworthy to mention that vaccine labels stipulate use in healthy animals. In addition, the hydration and nutritional status of the animal may influence the effectiveness of a vaccine. Generating an adequate immune response to a vaccine requires a significant amount of energy and nutrients and undernourished and/or dehydrated cattle may not be physiologically capable of mounting an appropriate response to the vaccine. The conundrum of these scenarios is that most producers and veterinarians vaccinate juxtaposed to other processes, such as weaning, branding, or arrival at a new location. To further complicate vaccination protocols and cattle-processing procedures, with respect to endotoxin overloading, producers often administer metaphylactic antimicrobials at processing in conjunction with vaccination. Many antimicrobials target gram-negative pathogens, resulting in endotoxin release after the targeted action of the antimicrobial results in killing or lysis of bacteria. Different antimicrobial classes, and different antimicrobials within classification, vary with respect to their impact on cell wall morphology and the subsequent amount of endotoxin released.60
Potential benefits and consequences
The amount, type, and structure of the endotoxin, and whether or not endotoxins are introduced from multiple sources (endotoxin stacking) combined with the physiologic and immunologic status of the host animal, affect the magnitude of the endotoxin response that may have positive or negative outcome. Exposure to structurally altered or lesser amounts of endotoxin may initiate a small immunologic response that could enhance the effectiveness of bacterins and result in immunologic memory against gram-negative bacteria. In fact, the low concentrations of endotoxins in a bacterin may indeed exert beneficial actions similar to the proposed immune-priming effects of acute stress and some commercial MLV vaccines contain very small quantities of endotoxin for this very reason. Furthermore, low concentrations of LPS will lead to a mild to moderate febrile response that can aid in controlling bacterial proliferation in the host.40 Endotoxin exposure also stimulates B-cell differentiation and enhances phagocytic activity, thus helping the host animal immune system to recognize and eliminate invading pathogens more rapidly and effectively. For example, genetically altered mice that do not respond to LPS have been reported to be more susceptible to bacterial infections.61 Therefore, exposure to small quantities of LPS typically aids immune function and may be beneficial in eliminating pathogens by increasing effector capacities of macrophages and other leukocytes.
Conversely, when greater endotoxin exposure occurs because of, for example, mishandling of vaccines or endotoxin stacking, the effect can be detrimental due to varying degrees of sepsis related to bacteremia and endotoxemia.59, 62, 63 Exposure to high concentration of endotoxin can elicit a severe febrile and hypotensive response that rapidly leads to multiorgan failure, septic shock, and death. Interestingly, it has been reported that gram-negative bacterial endotoxins are responsible for almost half of septic cases in humans.64 In addition to the potential for inducing lethal septic shock, endotoxin exposure stimulates the release of the proinflammatory cytokines as previously discussed. Increased cytokine production leads to vasodilation that can inadvertently increase bacterial translocation and dissemination throughout the body65 and may lead to increased proliferation of virulent strains of bacteria, such as Escherichia coli.66 Compounding this problem is the inhibited bacterial clearance invoked by endotoxicity and the impaired function of immune cells, such as monocytes.67 Thus, although the release of proinflammatory cytokines is essential for maintaining homeostasis within the animal, there exists a “catch-22” scenario in that the permissive effects of these cytokines on bacterial proliferation leads to a perpetuating cycle of increased cytokine production and subsequent increased risk of sepsis.
Summary
Vaccines provide immunologic protection against economically important cattle diseases. However, vaccine efficiency may not be realized if the timing of vaccination is inappropriate, vaccinates are immunosuppressed, and/or if the infectious challenge is greater than the immunologic protection afforded by vaccination. Vaccine recommendations in cattle often rely on anecdotal evidence and tradition, rather than scientific evidence, because there is a dearth of randomized, controlled field studies that evaluate vaccine efficiency, and some vaccination practices disregard vaccine label instructions. Veterinary practitioners should consider emerging research on the efficiency of on-arrival versus delayed vaccination in newly received stocker and feedlot cattle monitored under field conditions. Furthermore, endotoxicity risk is increased when 2 or more gram-negative bacterins are administered concurrently; therefore, veterinarians and producers should avoid endotoxin stacking when designing cattle vaccination protocols.
Acknowledgments
The article cited was prepared by a USDA employee as part of his or her official duties. Copyright protection under US copyright law is not available for such works. Accordingly, there is no copyright to transfer. The fact that the private publication in which the article appears is itself copyrighted does not affect the material of the US government, which can be freely reproduced by the public.
Mention of trade names or commercial products in this article is solely for the purpose of providing specific information and does not imply recommendation or endorsement by the USDA.
The USDA prohibits discrimination in all its programs and activities on the basis of race, color, national origin, age, disability, and, where applicable, sex, marital status, familial status, parental status, religion, sexual orientation, genetic information, political beliefs, reprisal, or because all or part of an individual's income is derived from any public assistance program. (Not all prohibited bases apply to all programs.) Persons with disabilities who require alternative means for communication of program information (eg, Braille, large print, audiotape) should contact USDA's TARGET Center at (202) 720-2600 (voice and TDD). To file a complaint of discrimination, write to USDA, Director, Office of Civil Rights, 1400 Independence Avenue, SW, Washington, DC 20250-9410, or call (800) 795-3272 (voice) or (202) 720-6382 (TDD). USDA is an equal opportunity provider and employer.
Footnotes
Disclosure Statement: None.
References
- 1.Taylor J.D., Fulton R.W., Lehenbauer T.W. The epidemiology of bovine respiratory disease: what is the evidence for predisposing factors? Can Vet J. 2010;51:1095–1102. [PMC free article] [PubMed] [Google Scholar]
- 2.Ives S.E., Richeson J.T. Use of antimicrobial metaphylaxis for the control of bovine respiratory disease in high-risk cattle. Vet Clin North Am Food Anim Pract. 2015;31:341–350. doi: 10.1016/j.cvfa.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Griffin D. Economic impact associated with respiratory disease in beef cattle. Vet Clin North Am Food Anim Pract. 1997;13:367–377. doi: 10.1016/s0749-0720(15)30302-9. [DOI] [PubMed] [Google Scholar]
- 4.Hughes H.D., Carroll J.A., Burdick Sanchez N.C. Natural variations in the stress and acute phase response of cattle. Innate Immun. 2013;20:888–896. doi: 10.1177/1753425913508993. [DOI] [PubMed] [Google Scholar]
- 5.Dhuyvetter K.C., Bryan A.M., Blasi D.A. Case study: preconditioning beef calves: are expected premiums sufficient to justify the practice? Prof Anim Sci. 2005;21:502–514. [Google Scholar]
- 6.King M.E., Salman M.D., Wittum T.E. Effect of certified health programs on the sale price of beef calves marketed through a livestock videotape auction service from 1995 through 2005. J Am Vet Med Assoc. 2006;229(9):1389–1400. doi: 10.2460/javma.229.9.1389. [DOI] [PubMed] [Google Scholar]
- 7.Step D.L., Krehbiel C.R., DePra H.A. Effects of commingling beef calves from different sources and weaning protocols during a forty-two-day receiving period on performance and bovine respiratory disease. J Anim Sci. 2008;11:3146–3158. doi: 10.2527/jas.2008-0883. [DOI] [PubMed] [Google Scholar]
- 8.Hilton W.M., Olynk N.J. Profitability of preconditioning: lessons learned from an 11-year case study of an Indiana beef herd. Bov Pract (Stillwater) 2011;45:40–50. [Google Scholar]
- 9.USDA . USDA – Anim Plant Health Insect Serv-Vet Serv, Ctr Epidemiol Anim Health; Fort Collins (CO): 2009. Vaccination of calves for respiratory disease on U. S. beef cow-calf operations. Info Sheet.https://www.aphis.usda.gov/animal_health/nahms/beefcowcalf/downloads/beef0708/Beef0708_is_CalfVacc.pdf Available at: Accessed April 01, 2019. [Google Scholar]
- 10.Richeson J.T., Beck P.A., Gadberry M.S. Effects of on-arrival versus delayed modified live virus vaccination on health, performance, and serum infectious bovine rhinotracheitis titers of newly received beef calves. J Anim Sci. 2008;86:999–1005. doi: 10.2527/jas.2007-0593. [DOI] [PubMed] [Google Scholar]
- 11.Griffin C.M., Scott J.A., Karisch B.B. A randomized controlled trial to test the effect of on-arrival vaccination and deworming on stocker cattle health and growth performance. Bov Pract (Stillwater) 2018;52:26–33. [PMC free article] [PubMed] [Google Scholar]
- 12.Terrell S.P., Thomson D.U., Wileman B.W. A survey to describe current feeder cattle health and well-being program recommendations made by feedlot veterinary consultants in the United States and Canada. Bov Pract (Stillwater) 2011;45:140–148. [Google Scholar]
- 13.Rogers K.C., Miles D.G., Renter D.G. Effects of delayed respiratory viral vaccine and/or inclusion of an immunostimulant on feedlot health, performance, and carcass merits of auction-market derived feeder heifers. Bov Pract (Stillwater) 2016;50:154–162. [Google Scholar]
- 14.Fike G.D., Simroth J.C., Thomson D.U. A survey of recommended practices made by veterinary practitioners to cow-calf operations in the United States and Canada. Prof Anim Sci. 2017;33:716–728. doi: 10.15232/pas.2017-01642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Terrell S.P., Thomson D.U., Reinhardt C.D. Perception of lameness management, education, and effects on animal welfare of feedlot cattle by consulting nutritionists, veterinarians, and feedlot managers. Bov Pract (Stillwater) 2014;48:53–60. [Google Scholar]
- 16.Lee T.L., Terrell S.P., Bartle S.J. Current feedlot cattle health and well-being program recommendations in the United States and Canada: the 2014 feedlot veterinary consultant survey. Bov Pract (Stillwater) 2015;49:124–131. [Google Scholar]
- 17.USDA . USDA – Anim Plant Health Insect Serv-Vet Serv, Ctr Epidemiol Anim Health; Fort Collins (CO): 2010. Beef 2007-08. Part IV: reference of beef cow-calf management practices in the United States, 2007-08. #523.0210. [Google Scholar]
- 18.Comerford J.W., Greaser G.L., Moore H.L. Penn State Coop Ext, The Pennsylvania State Univ, University Park (PA); 2013. Beef cow-calf production. Agricultural alternatives. [Google Scholar]
- 19.Waldner C.M., Jelinski D., McIntyre-Zimmer K. Survey of western Canadian beef producers regarding calf-hood diseases, management practices, and veterinary service usage. Can Vet J. 2013;54:559–564. [PMC free article] [PubMed] [Google Scholar]
- 20.Woolums A.R., Berghaus R.D., Smith D.R. A survey of veterinarians in 6 US states regarding their experience with nursing beef calf respiratory disease. Bov Pract (Stillwater) 2014;48:26–35. [Google Scholar]
- 21.USDA. Vaccine usage in U.S. feedlots. No. 672.0513. Fort Collins (CO): USDA, Animal and Plant Health Inspection Service, Veterinary Services, Centers for Epidemiology and Animal Health; 2013.
- 22.Martin S.W. Vaccination: is it effective in preventing respiratory disease of influencing weight gains in feedlot calves? Can Vet J. 1983;24:10–19. [PMC free article] [PubMed] [Google Scholar]
- 23.Perino L.J., Hunsaker B.D. A review of bovine respiratory disease vaccine field efficacy. Bov Pract (Stillwater) 1997;31:59–66. [Google Scholar]
- 24.Tripp H.M., Step D.L., Krehbiel C.R. Evaluation of outcomes in beef cattle comparing preventive health protocols utilizing viral respiratory vaccines. Bov Pract (Stillwater) 2013;47:54–64. [Google Scholar]
- 25.Larson B.L. A new look at reducing infectious disease in feedlot cattle. Proc Plains Nutr Coun. 2005;AREC05-20:9–17. [Google Scholar]
- 26.Weinberg G.A., Szilagyi P.G. Vaccine epidemiology: efficacy, effectiveness, and translational research roadmap. J Infect Dis. 2010;201:1607–1610. doi: 10.1086/652404. [DOI] [PubMed] [Google Scholar]
- 27.Richeson J.T., Beck P.A., Poe K.D. Effects of administration of a modified-live virus respiratory vaccine and timing of vaccination on health and performance of high-risk beef stocker calves. Bov Pract (Stillwater) 2015;49:37–42. [Google Scholar]
- 28.Rashid A., Rasheed K., Asim M. Risks of vaccination: a review. J Venom Anim Toxins Incl Trop Dis. 2009;15:19–27. [Google Scholar]
- 29.USDA, APHIS Licensed veterinary biological product information. https://www.aphis.usda.gov/aphis/ourfocus/animalhealth/veterinary-biologics/CT_Vb_licensed_products Available at: Accessed March 29, 2019.
- 30.Roth J.A. Mechanistic bases for adverse vaccine reactions and vaccine failures. Adv Vet Med. 1999;41:681–700. doi: 10.1016/S0065-3519(99)80053-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen S., Miller G.E., Ravin B.S. Psychological stress and antibody response to immunization: a critical review of the human literature. Psychosom Med. 2001;63:7–18. doi: 10.1097/00006842-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Roth J.A. Animal stress. Springer; New York: 1985. Cortisol as mediator of stress-associated immunosuppression in cattle; pp. 225–243. [Google Scholar]
- 33.Richeson J.T., Carroll J.A., Burdick Sanchez N.C. Dexamethasone treatment differentially alters viral shedding and the antibody and acute phase protein response after multivalent respiratory vaccination in beef steers. J Anim Sci. 2016;94:3501–3509. doi: 10.2527/jas.2016-0572. [DOI] [PubMed] [Google Scholar]
- 34.Richeson J.T. Vaccinating high-risk calves against BRD. Proc Am Assoc Bov Pract. 2015;48:169–172. [Google Scholar]
- 35.Richeson J.T., Kegley E.B., Gadberry M.S. Effects of on-arrival versus delayed clostridial or modified live respiratory vaccinations on health, performance, bovine viral diarrhea virus type I titers, and stress and immune measures of newly received beef calves. J Anim Sci. 2009;87:2409–2418. doi: 10.2527/jas.2008-1484. [DOI] [PubMed] [Google Scholar]
- 36.Poe K.D., Beck P.A., Richeson J.T. Effects of respiratory vaccination timing and growth-promoting implant on health, performance, and immunity of high-risk, newly received stocker cattle. Prof Anim Sci. 2013;29:413–419. [Google Scholar]
- 37.Hagenmaier J.A., Terhaar B.L., Blue K. A comparison of three vaccine programs on the health, growth performance, and carcass characteristics of high-risk feedlot heifers procured from auction markets. Bov Pract (Stillwater) 2018;52:120–130. [Google Scholar]
- 38.Duff G.C., Malcolm-Callis K.J., Walker D.A. Effect of intranasal versus intramuscular modified live vaccines and vaccine timing on health and performance by newly received beef cattle. Bov Pract (Stillwater) 2000;34:66–71. [Google Scholar]
- 39.Pfeiffer R. Untersuchungen über das Choleragift. Med Microbiol Immunol. 1892;11(1):393–412. [Google Scholar]
- 40.Woltmann A., Hamann L., Ulmer A.J. Molecular mechanisms of sepsis. Langenbecks Arch Surg. 1998;383:2–10. doi: 10.1007/s004230050085. [DOI] [PubMed] [Google Scholar]
- 41.Carroll J.A., Reuter R.R., Chase C.C. Profiling of the bovine acute phase response following an intravenous lipopolysaccharide challenge. Innate Immun. 2009;15:81–89. doi: 10.1177/1753425908099170. [DOI] [PubMed] [Google Scholar]
- 42.De S.N. Enterotoxicity of bacteria-free culture filtrate of Vibrio cholerae. Nature. 1959;183:1533–1534. doi: 10.1038/1831533a0. [DOI] [PubMed] [Google Scholar]
- 43.Nairv G.B., Narainv J.P. From endotoxin to exotoxin: De’s rich legacy to cholera. Bull World Health Organ. 2010;88(3):161–240. doi: 10.2471/BLT.09.072504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ala’Aldeen D.A.A., Wooldridge K.G. 18th edition. 2012. Medical microbiology. [Google Scholar]
- 45.Janeway C.A., Jr., Travers M., Walport M. Garland Science Publishing; New York: 2005. Immunobiology, the immune system in health and disease. [Google Scholar]
- 46.Takeda K., Kaisho T., Akira S. Toll-like receptors. Annu Rev Immunol. 2003;21:335–376. doi: 10.1146/annurev.immunol.21.120601.141126. [DOI] [PubMed] [Google Scholar]
- 47.Mackay I.R., Janeway C., Jr. Innate immunity. N Engl J Med. 2000;343:338–344. doi: 10.1056/NEJM200008033430506. [DOI] [PubMed] [Google Scholar]
- 48.Janeway C.A., Jr., Medzhitov R. Innate immune recognition. Annu Rev Immunol. 2002;20:197–216. doi: 10.1146/annurev.immunol.20.083001.084359. [DOI] [PubMed] [Google Scholar]
- 49.Medzhitov R., Janeway J. Innate immunity: the virtues of a nonclonal system of recognition. Cell. 1997;91:295–298. doi: 10.1016/s0092-8674(00)80412-2. [DOI] [PubMed] [Google Scholar]
- 50.Mann D.L. Tumor necrosis factor and viral myocarditis: the fine line between innate and inappropriate immune responses in the heart. Circulation. 2001;103:626–629. doi: 10.1161/01.cir.103.5.626. [DOI] [PubMed] [Google Scholar]
- 51.Bishop R.E. Fundamentals of endotoxin structure and function. Contrib Microbiol. 2005;12:1–27. doi: 10.1159/000081687. [DOI] [PubMed] [Google Scholar]
- 52.Peterson J.W. Bacterial pathogenesis. In: Baron S., editor. Medical microbiology. 4th edition. University of Texas Medical Branch at Galveston; Galveston (TX): 1996. [Chapter: 7] [Google Scholar]
- 53.Exton M.S. Infection-induced anorexia: active host defense strategy. Appetite. 1997;29:369–383. doi: 10.1006/appe.1997.0116. [DOI] [PubMed] [Google Scholar]
- 54.Godson D.L., Baca-Estrada M.E., Van Kessel A.G. Regulation of bovine acute phase responses by recombinant interleukin-1β. Can J Vet Res. 1995;59(4):249–255. [PMC free article] [PubMed] [Google Scholar]
- 55.Kahl S., Elsasser T.H. Exogenous testosterone modulates tumor necrosis factor- and acute phase protein responses to repeated endotoxin challenge in steers. Domest Anim Endocrinol. 2006;31:301–311. doi: 10.1016/j.domaniend.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 56.McSherry B.J., Horney F.D., deGroot J.J. Plasma fibrinogen levels in normal and sick cows. Can J Comp Med. 1970;34:191–197. [PMC free article] [PubMed] [Google Scholar]
- 57.Eckersall P.D., Conner J.G. Bovine and canine acute phase proteins. Vet Res Commun. 1988;12:169–178. doi: 10.1007/BF00362798. [DOI] [PubMed] [Google Scholar]
- 58.Alexander C., Rietschel E.T. Bacterial lipopolysaccharides and innate immunity. J Endotoxin Res. 2001;7:167–202. [PubMed] [Google Scholar]
- 59.Ellis J.A., Yong C. Systemic adverse reactions in young Simmental calves following administration of a combination vaccine. Can Vet J. 1997;38:45–47. [PMC free article] [PubMed] [Google Scholar]
- 60.Crosby H.A., Bion J.F., Penn C.W. Antibiotic induced release of endotoxin from bacteria in vitro. J Med Microbiol. 1994;40:23–30. doi: 10.1099/00222615-40-1-23. [DOI] [PubMed] [Google Scholar]
- 61.von Jeney N., Günther E., Jann K. Mitogenic stimulation of murine spleen cells: relation to susceptibility to Salmonella infection. Infect Immun. 1977;15:26–33. doi: 10.1128/iai.15.1.26-33.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang F.X., Kirschning C.J., Mancinelli R. Bacterial lipopolysaccharide activates nuclear factor-κB through interleukin-1 signaling mediators in cultured human dermal endothelial cells and mononuclear phagocytes. J Biol Chem. 1999;274:7611–7614. doi: 10.1074/jbc.274.12.7611. [DOI] [PubMed] [Google Scholar]
- 63.Muzio M., Bosisio D., Polentarutti N. Differential expression and regulation of toll-like receptors (TLR) in human leukocytes: selective expression of TLR3 in dendritic cells. J Immunol. 2000;164:5998–6004. doi: 10.4049/jimmunol.164.11.5998. [DOI] [PubMed] [Google Scholar]
- 64.Jones G., Lowes J. The systemic inflammatory response syndrome as a predictor of bacteraemia and outcome from sepsis. QJM. 1996;89:515–522. doi: 10.1093/qjmed/89.7.515. [DOI] [PubMed] [Google Scholar]
- 65.Haziot A., Ferrero E., Köntgen F. Resistance to endotoxin shock and reduced dissemination of gram-negative bacteria in CD14-deficient mice. Immun. 1996;4:407–414. doi: 10.1016/s1074-7613(00)80254-x. [DOI] [PubMed] [Google Scholar]
- 66.Porat R., Clark B.D., Wolff S.M. Enhancement of growth of virulent strains of Escherichia coli by interleukin-1. Science. 1991;254:430–432. doi: 10.1126/science.1833820. [DOI] [PubMed] [Google Scholar]
- 67.Koch T., Duncker H.P., Axt R. Alterations of bacterial clearance induced by endotoxin and tumor necrosis factor. Infect Immun. 1993;61:3143–3148. doi: 10.1128/iai.61.8.3143-3148.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]