Highlights
-
•
Passive immunisation studies were conducted in IFNAR −/− mice using splenocytes and antiserum from donors.
-
•
Donors were immunised with modified vaccinia Ankara (MVA) expressing African horse sickness virus (AHSV) VP2.
-
•
After AHSV challenge, splenocyte recipients were poorly protected against clinical signs and not protected against viraemia.
-
•
After AHSV challenge, antiserum recipients were highly protected against viraemia and clinical signs.
-
•
MVA-VP2 vaccination immunity is strongly associated with neutralising antibodies, indicating potential for sero-therapy.
Keywords: African horse sickness, AHSV, MVA-VP2, Protection, Humoral immunity, Passive immunisation
Abstract
Previous studies show that a recombinant modified vaccinia Ankara (MVA) virus expressing VP2 of AHSV serotype 4 (MVA-VP2) induced virus neutralising antibodies in horses and protected interferon alpha receptor gene knock-out mice (IFNAR −/−) against challenge. Follow up experiments indicated that passive transfer of antiserum, from MVA-VP2 immune donors to recipient mice 1 h before challenge, conferred complete clinical protection and significantly reduced viraemia.
These studies have been extended to determine the protective effect of MVA-VP2 vaccine-induced antiserum, when administered 48 h before, or 48 h after challenge. In addition, passive transfer of splenocytes was undertaken to assess if they confer any degree of immunity to immunologically naïve recipient mice. Thus, antisera and splenocytes were collected from groups of mice that had been vaccinated with MVA-VP2, or wild type MVA (MVA-wt), for passive immunisation of recipient mice. The latter were subsequently challenged with AHSV-4 (together with appropriate vaccinated or unvaccinated control animals) and protection was assessed by comparing clinical signs, lethality and viraemia between treated and control groups. All antiserum recipients showed high protection against disease (100% survival rates even in mice that were immunised 48 h after challenge) and statistically significant reduction or viraemia in comparison with the control groups. The mouse group receiving splenocytes from MVA-VP2 vaccinates, showed only a 40% survival rate, with a small reduction in viraemia, compared to those mice that had received splenocytes from MVA-wt vaccinates. These results confirm the primarily humoral nature of protective immunity conferred by MVA-VP2 vaccination and show the potential of administering MVA-VP2 specific antiserum as an emergency treatment for AHSV.
1. Introduction
African horse sickness (AHS) is an arthropod-borne viral disease of solipeds transmitted by haematophagous insects of the genus Culicoides, the horse being the most severely affected species. Mortality rates of AHSV outbreaks in immunologically naïve populations may exceed 90% (Mellor and Hamblin, 2004).
All of the different isolates, strains and serotypes of African horse sickness virus (AHSV) are classified within the species African horse sickness virus, genus Orbivirus, family Reoviridae. AHSV is closely related to bluetongue virus, which causes bluetongue disease in ruminants. The orbiviruses are characterised by a genome composed of ten linear segments of dsRNA, with one copy of each of the ten segments packaged within each virus particle. The spherical, non-enveloped capsid of AHSV is approximately 70 nm in diameter, is composed of three concentric protein layers (Roy et al., 1994). The outer-capsid layer is formed by two major structural proteins, VP2 and VP5 (encoded by genome-segments 2 and 6 respectively), and is primarily involved in cell attachment and cell entry. VP2 is the most variable antigen of AHSV and is responsible for serotype definition (Burrage et al., 1993).
AHSV infection in horses most often results in severe clinical disease and death, although animals that do survive, exhibit a solid, life-long but serotype-specific immunity. The humoral nature of AHS immunity has been associated with virus neutralising antibodies (VNAb) in both horses and mice using colostrum and monoclonal antibodies respectively (Blackburn and Swanepoel, 1988, Burrage et al., 1993, Crafford et al., 2013). The main target of VNAb is AHSV VP2 (Burrage et al., 1993) and several studies have mapped neutralising epitopes to the amino terminal half of the VP2 protein (Bentley et al., 2000, Martinez-Torrecuadrada and Casal, 1995, Martinez-Torrecuadrada et al., 2001).
Although less important in this respect than VP2, AHSV-VP5 appears to be both directly involved in the formation of virus neutralising epitopes and indirectly involved by influencing the conformation of VP2 (Martinez-Torrecuadrada and Casal, 1995, Martinez-Torrecuadrada et al., 1996). Unsurprisingly, experimental vaccines based on the outer-capsid proteins VP2 and/or VP5, were successful (Castillo-Olivares et al., 2011, Chiam et al., 2009, Romito et al., 1999, Roy and Sutton, 1998, Scanlen et al., 2002, Stone-Marschat et al., 1996).
Recently, cell-mediated immune responses have been detected in horses following inoculation with live attenuated AHSV vaccines (Pretorius et al., 2012), or recombinant Canarypox virus expressing AHSV VP2 and VP5 (El Garch et al., 2012). More recently, cell-mediated immune responses have also been observed in interferon alpha receptor gene knock-out mice (IFNAR −/−) after vaccination with single MVA recombinant viruses expressing AHSV VP2 or NS1 (de la Poza et al., 2013). Since cellular immunity has been associated with protection against BTV, it is generally assumed that the same applies to AHSV.
After showing that MVA expressing AHSV VP2 (MVA-VP2) was protective against AHSV infection in mice (Castillo-Olivares et al., 2011) and horses (Alberca et al., 2014), the mechanisms of immunity underlying the protective effect of MVA-VP2 vaccination were investigated. Passive transfer of AHSV neutralising antiserum, from MVA-VP2 vaccinated mice to immunologically naïve recipients, was shown to be highly protective against a lethal AHSV challenge (Calvo-Pinilla et al., 2014).
In this paper, follow-up studies investigating the relative contribution of humoral and cell-mediated immunity to the protection conferred by MVA-VP2 vaccination, using passive immunisation of naïve recipient IFNAR −/− mice with splenocytes or antiserum from MVA-VP2 vaccinated mice, are described.
2. Materials and methods
2.1. Viruses and cells
Chicken embryo fibroblast (DF-1) (ATCC, Cat. No. CRL-12203) and Vero cells (ATCC, Cat. No. CCL-81) were grown in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 2 mM glutamine, penicillin (100 units/ml), streptomycin (100 μg/ml) and 10% foetal calf serum (FCS). AHSV-4 (Madrid/87) (AHSV-4) was grown in Vero cells and MVA viruses grown in DF-1 cells. Virus stocks were generated by infection of confluent cells using a multiplicity of infection (MOI) of 0.1. At 48 h post-infection, or when a total cytopathic effect (CPE) was visible, the cells and supernatants were harvested and centrifuged. The virus was released from the cells by three freeze and thaw cycles and then titrated by plaque assay. The MVA-VP2 virus used in this study has been previously described (Chiam et al., 2009).
2.2. Mice
IFN α/β Ro/o IFNAR −/− mice on an A129 background were purchased from B&K Universal Ltd (UK). Eight-week old mice were used throughout. Mice were maintained under pathogen-free conditions and allowed to acclimatise to the biosafety level 3 (BSL3) animal facilities at the Centro de Investigacion en Sanidad Animal, INIA, Madrid (INIA-CISA), for 1 week before use. All experiments with live animals were performed under the guidelines of the European Community (86/609) and were approved by the ethical review committee of INIA-CISA (CEEA 2010-034).
2.3. Murine immunisations with MVA-VP2 and MVA-wt and preparation of donor antisera and splenocytes
Groups of mice were vaccinated (107 pfu/mouse) with either MVA-VP2 (Group 1a and Group 1b) or MVA-wt (Group 2) and used as donors of serum and splenocytes as shown in Table 1 . A third dose was given on day 35 to 5 mice from Group 1a (mouse 1.6–mouse 1.10). Mice from Group 1b and Group 2 were euthanised on day 35. Mice from Group 1a were euthanized on day 50. Splenocytes and blood samples were collected at termination and subsequently used for passive immunisation. The blood was used to prepare donor antisera.
Table 1.
Vaccination and preparation of splenocytes and antiserum donors.
| Groups | Day 0 | Day 21 | Day 35 | Day 50 |
|---|---|---|---|---|
| 1a (5 mice) | MVA-VP2 107 pfu/mouse | MVA-VP2 107 pfu/mouse | MVA-VP2 107 pfu/mouse | Collection of serum (S1a) |
| 1b (5 mice) | MVA-VP2 107 pfu/mouse | MVA-VP2 107 pfu/mouse | Collection of serum (S1b) and spleen (L1) | |
| 2 (5 mice) | MVA-wt 107 pfu/mouse | MVA-wt 107 pfu/mouse | Collection of serum (S2) and spleen (L2) |
2.4. Adoptive transfer of splenocytes
Pools of spleen cells, obtained from mice from Group 1b (MVA-VP2) and Group 2 (MVA-wt), were transferred via intravenous injection (2 × 107 cells/mouse) to immunologically naïve recipients Groups 3 and 4 (Table 2 a). Transfers were performed 24 h before infection with AHSV-4 (106 pfu/mouse).
Table 2.
Passive immunisation and AHSV challenge.
| Groups | Treatment | Volume and VNAb titre of Serum | Challenge AHSV-4 |
|---|---|---|---|
| (a) Splenocyte transfer and challenge | |||
| Group 3 | Transferred with splenocytes from Group 1b (MVA-VP2 vaccinates) 24 h before challenge | 2 × 107 cells/mouse | 106 pfu/mouse |
| Group 4 | Transferred with splenocytes from Group 2 (MVA-wt vaccinates) 24 h before challenge | 2 × 107 cells/mouse | 106 pfu/mouse |
| (b) Serum transfer and challenge | |||
| Group 5 | Transferred with serum from MVA-VP2 vaccinates (day 0) 1 h before challenge | 400 μl S1a 2.25 |
106 pfu/mouse |
| Group 6 | Transferred with serum from MVA-VP2 vaccinates (day 0) 1 h before challenge | 100 μl S1b 1.95 |
106 pfu/mouse |
| Group 7 | Transferred with serum from MVA-VP2 vaccinates (day −2) 48 h before challenge | 100 μl S1b 1.95 |
106 pfu/mouse |
| Group 8 | Transferred with serum from MVA-VP2 vaccinates (day +2) 48 h after challenge | 100 μl S1b 1.95 |
106 pfu/mouse |
| Group 9 | Vaccinated twice with MVA-wt 107 pfu per mouse 21 and 14 days before challenge | N/A∗ | 106 pfu/mouse |
| Group 10 | Vaccinated twice with MVA-VP2 107 pfu per mouse 21 and 14 days before challenge | N/A | 106 pfu/mouse |
N/A: not applicable.
2.5. Passive immunisation with donor antiserum
Donor antisera S1a, S1b and S2 were prepared by pooling individual serum samples from Groups 1a, 1b and 2 respectively (Table 2b). The donor antisera were inactivated (30 min at 56 °C) and used for intra-peritoneal injection of 4 Groups of 10-week-old recipient IFNAR −/− mice: (a) Group 5, received 400 μl of undiluted S1a antiserum administered 1 h before challenge; (b) Group 6 received 100 μl of diluted S1b antiserum, administered 1 h before challenge; (c) Group 7 received 100 μl of S1b 48 h before challenge and (d) Group 8 received 100 μl of S1b antiserum 48 after challenge.
Passively immunised mice were challenged with 106 pfu of AHSV-4 administered subcutaneously. MVA-wt (Group 9) and MVA-VP2 (Group 10) vaccinated control mice were infected at the same time as the recipients. Clinical signs and viraemia were evaluated in all the animals following challenge.
2.6. Evaluation of clinical signs after challenge with AHSV-4
Following challenge, animals were monitored twice daily and more regularly (at least three times per day) at the onset of any signs of morbidity, including: changes in behaviour and activity, changes in water or food intake, alterations in the hair coat appearance, body weight loss, presence of ocular signs (conjunctivitis, ocular discharge, swelling), changes in hydration and presence of neurological signs (i.e. paresis, paralysis, ataxia). The humane end-points for euthanasia included: persistent hunching, severe conjunctivitis, signs of dehydration, loss of more than 20% of body weight, presence of any neurological signs, or any other condition that prevented food or water intake. Animals that displayed any of these clinical signs were humanely euthanised by cervical dislocation following anaesthesia with 5% isoflurane.
A clinical scoring system was used (Table 3 ) whereby each animal received a clinical score value per day. The value used for analysis was the individual mean clinical score for the study period (sum of daily scores of each animal/number of days).
Table 3.
Daily clinical score.
| Possible clinical signs of AHS infection in mice | Possible score values per clinical sign |
||
|---|---|---|---|
| 0 | 1 | 2 | |
| Ruffled hair/pilo-erection | Absent | Present | – |
| Separation from the Group | Absent | Present | – |
| Reduced activity | Absent | Present | Frequent |
| Ocular watery discharge | Absent | Present | – |
| Nasal watery discharge | Absent | Present | – |
| Abnormal respiratory rate | Absent | Present | – |
| Weight loss | Absent | Present | >10% body weight |
| Dehydration | Absent | Present | – |
| Periorbital swelling | Absent | Present | Compromising vision |
| Tremors | Absent | Present | – |
| Ataxia | Absent | Present | – |
| Paralysis or paresis | Absent | Present | – |
| Circling gate | Absent | Present | – |
| Hunching | Absent | Present | – |
| Daily score (sum) | |||
2.7. Virus neutralisation test and VP2-specific ELISA
Determination of VNAb titres of serum samples was carried out as described previously (Calvo-Pinilla et al., 2014). Briefly, twofold serial dilutions of serum samples were incubated with 100 TCID50 of AHSV-4 for 1 h and then overnight at 4 °C. The following day, 2 × 104 Vero cells were added to each well and incubated for 3 days at 37 °C, 5% CO2. The end-point of the assay was the highest dilution that prevented AHSV cytopathic effect in 50% of the wells. Antibody titres were then calculated according to Karber (1931). Antibody levels of VP2-specific antibodies in serum were determined as previously described (Calvo-Pinilla et al., 2014).
2.8. Detection of AHSV-4 in blood
Whole blood from animals was collected in EDTA at regular intervals after challenge. Volumes of 50 μl of blood were washed in PBS, mixed with 400 μl of water to lyse the cells and then 50 μl of 10× PBS was added to the sample. Infectious virus was measured by standard plaque assay on Vero cells.
2.9. ELISpot assay for the detection of IFN-γ producing cells
Spleens were homogenised and then filtered through 70 μm cell strainers. Erythrocytes were lysed with NH4Cl and the remaining cells were re-suspended in RPMI media. AHSV-specific IFN-γ producing cells were measured by ELISpot assay as described previously (Calvo-Pinilla et al., 2009). Splenocytes were stimulated for 24 h with either AHSV-4 cell extract that had been inactivated by 30 min exposure to ultraviolet light (400 J/cm2) or with affinity purified AHSV-4 VP2 expressed from recombinant baculovirus (Chiam et al., 2009). PHA (Phytohemagglutinin, 5 μg/ml) stimulated control cells used as positive control and uninfected cell extract stimulated cells were used as the negative control. The spot count of antigen-specific cells was calculated as the spot count difference between AHSV4-stimulated cells and non-stimulated cells.
2.10. Statistical methods
Unless otherwise stated, the methods used were the same for the splenocyte and serum transfer experiments.
Virus neutralising titre (VNT) in donor mice: titres in MVA VP2-vaccinated and MVA-wt vaccinated mice (splenocyte transfer) and in mice vaccinated twice or three times with MVA-VP2 (serum transfer) were compared using Wilcoxon rank-sum tests.
Elispot data for donor mice: the numbers of cells excreting IFNγ were compared using a Kruskal–Wallis test, with mice grouped according to vaccination status (MVA-VP2 or MVA-wt) and stimulus (AHSV or VP2) (i.e. there are four groups in total). Differences between groups were then explored using post hoc Wilcoxon rank-sum tests.
Clinical scores in recipient mice: clinical scores in different groups of mice were compared using a Wilcoxon rank-sum test (splenocyte transfer) or a Kruskal–Wallis test (serum transfer). In the latter case, differences between groups were then explored using post hoc Wilcoxon rank-sum tests.
Viraemia in recipient mice: differences in viraemia amongst groups of mice were assessed using linear mixed models with log10 pfu as the response variable, days post infection (as a factor) and group as fixed effects and mouse as a random effect. Model selection proceeded by stepwise deletion of non-significant terms (as judged by the Akaike information criterion) starting from a model including days post infection and group as main effects.
Survival in recipient mice: survival in different groups of mice were compared using log-rank tests.
VNT in recipient mice: titres at experiment end point (either death or 14 days post infection) were analysed using a one-way analysis of variance, followed by post hoc Tukey tests to identify differences between groups.
A significance level of P = 0.05 was used in all analyses. All methods were implemented in R version 3.1.0 (R Core Team 2014).
3. Results
It has recently been demonstrated that immunologically naïve mice can be protected against challenge with a virulent strain of AHSV-4, by administering serum from mice previously vaccinated with MVA-VP2). This suggests that the protection afforded by MVA-VP2 vaccination is mediated mainly by antibodies (Calvo-Pinilla et al., 2014). However, it was shown in that study that MVA-VP2 vaccination also induced a CD8+ T-cell response. These studies have been extended to determine: (a) whether adoptive transfer of splenocytes from MVA-VP2 vaccinates could protect against AHSV-4 infection; and (b) whether protection by passive immunisation with antibodies from MVA-VP2 vaccinated mice could be observed when administered 48 h before, or 48 h after the challenge.
3.1. Immune responses in antiserum and splenocytes donors following MVA-VP2 and MVA-wt vaccination
Serum and splenocytes were obtained from mice that had been vaccinated with MVA-VP2 or MVA-wt, as indicated in Section 2. Consistent with previous findings (Calvo-Pinilla et al., 2013; Castillo-Olivares et al., 2011), the mice did not show any signs of infection following MVA-VP2 vaccination and developed an AHSV-VP2-specific VNAb response. Titres at day 35 (following two vaccinations) ranged between 1.95 and 2.15 (average 2.02) and these were subsequently boosted on day 45 (average titre 2.25). AHSV-VP2-specific antibodies in MVA-VP2 vaccinates were also detected by ELISA on days 35 (mean OD value 3.17; SD 0.28) and 45 (mean OD value 3.48; SD 0.15). Antisera collected on days 35 and 50 were used for passive immunisation.
Adoptive transfer of splenocytes was carried out using spleens harvested from MVA-VP2 and MVA-wt vaccinates collected on day 35. Results of IFN-γ ELISpot assays (Fig. 1 ) confirmed that the splenocytes from MVA-VP2 vaccinated donors (mice 1.1–1.5) were functional and secreted IFN-γ, with the frequency of responder cells being significantly higher than in the MVA-wt vaccinates (mice 2.1–2.3) regardless of whether they were stimulated with AHSV or VP2. Samples from mice 2.4 and 2.5 could not be used in this assay.
Fig. 1.
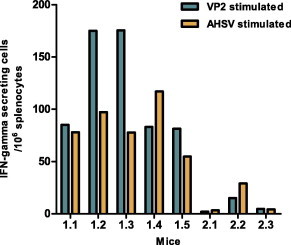
AHSV specific IFN-γ secreting cells measured by ELISpot assay. At 35 days post vaccination splenocytes from MVA-VP2 and MVA-wt immunized mice were stimulated with UV inactivated AHSV-4, baculovirus expressed AHSV-4 VP2 protein or negative cell extracts for 24 h. Bars represent the number of IFNA-g producing cells in samples stimulated with AHSV or VP2 after subtraction of values from cell extract stimulated samples.
3.2. Adoptive transfer of splenocytes and protection against AHSV
Once donor splenocytes were confirmed as viable and functional in the IFN-γ ELIspot assay, they were transferred to groups of 5 recipient mice, which were subsequently challenged with AHSV-4 to assess the protective capacity of the cell-mediated immunity.
All mice from Group 4 (receiving splenocytes from MVA-wt vaccinates) and three from Group 3 (receiving MVA-VP2 splenocytes) succumbed to the infection (Table 3), and AHSV was detected in the blood of all mice in these groups (Fig. 2 ). The survival rates (40%) and viraemia levels of Group 3 did not differ significantly (P > 0.05) from those of Group 4. However, a reduction of clinical score values in Group 3 relative to Group 4 was statistically significant (P = 0.008). Altogether, these data indicate that cell mediated immunity does not play a critical role in the high level of protection that was afforded against the homologous serotype by MVA-VP2 vaccination (see Table 4 ).
Fig. 2.
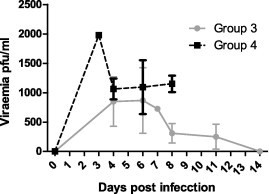
Viraemia of splenocyte recipients following AHSV challenge. Virus titres, expressed as pfu/ml of blood, were measured in mice from Group 3 (recipients of splenocytes from MVA-VP2 vaccinates) and Group 4 (recipients of splenocytes from MVA-wt vaccinates). Blood samples were collected on days 4, 6, 8, 11 and 14 after challenge except for mice that died on days 3 and 7. Data are shown as mean ± STD.
Table 4.
Adoptive transfer of splenocytes and AHSV-4 challenge: survival and clinical score.
| Groups | Splenocyte transfer | Animal ID number | Survival | Clinical score |
|---|---|---|---|---|
| 3 (5 mice) | Splenocytes from MVA-VP2 vaccinates | 3.1 | No | 2.50 |
| 3.2 | No | 3.00 | ||
| 3.3 | Yes | 0.71 | ||
| 3.4 | Yes | 0.75 | ||
| 3.5 | No | 2.50 | ||
| 4 (5 mice) | Splenocytes from MVA-wt vaccinates | 4.1 | No | 3.69 |
| 4.2 | No | 3.75 | ||
| 4.3 | No | 3.67 | ||
| 4.4 | No | 3.33 | ||
| 4.5 | No | 3.57 |
3.3. Passive immunisation with MVA-VP2 antiserum
In this study, the influence of the time of administration and dose of MVA-VP2-specific antiserum in protection against AHSV was evaluated. Thus, two groups of mice were passively immunised, as indicated in Section 2, and were subsequently infected with AHSV-4, together with two vaccinated groups. As expected, the mice that were vaccinated with MVA-wt (Group 9) developed clinical signs typical of AHS in the IFNAR −/− mouse model (Table 5 ). These started on day 3 post-infection and reached the humane end-point between days 5 and 10 post-challenge. All mice from this group were euthanised. In contrast, mice from all other groups survived the challenge and developed, at most, very mild clinical signs. Survival was significantly (P < 0.001) lower for mice in Group 9 compared with all other Groups. The clinical scores were also significantly higher (P < 0.001) in Group 9 compared with all of the other Groups, and in Group 8 compared with Groups 5, 7 and 10.
Table 5.
Clinical scores and survival rates of mice following immunisation (passive or active) and AHSV-4 challenge.
| Groups | Treatment | Animal ID number | Survival | Clinical score |
|---|---|---|---|---|
| Group 5 | Transferred with serum from MVA-VP2 vaccinates 400 μl 1 h before challenge | 5.1 | Yes | 0.00 |
| 5.2 | Yes | 0.00 | ||
| 5.3 | Yes | 0.00 | ||
| 5.4 | Yes | 0.00 | ||
| 5.5 | Yes | 0.00 | ||
| Group 6 | Transferred with serum from MVA-VP2 vaccinates 100 μl 1 h before challenge | 6.1 | Yes | 0.20 |
| 6.2 | Yes | 0.40 | ||
| 6.3 | Yes | 0.00 | ||
| 6.4 | Yes | 0.00 | ||
| 6.5 | Yes | 0.00 | ||
| Group 7 | Transferred with serum from MVA-VP2 vaccinates 100 μl 48 h before challenge | 7.1 | Yes | 0.00 |
| 7.2 | Yes | 0.10 | ||
| 7.3 | Yes | 0.00 | ||
| 7.4 | Yes | 0.00 | ||
| 7.5 | Yes | 0.10 | ||
| Group 8 | Transferred with serum from MVA-VP2 vaccinates 100 μl 48 h after challenge | 8.1 | Yes | 0.20 |
| 8.2 | Yes | 0.60 | ||
| 8.3 | Yes | 0.10 | ||
| 8.4 | Yes | 0.10 | ||
| 8.5 | Yes | 0.30 | ||
| Group 9 | Vaccinated twice with MVA-wt 107 pfu per mouse 21 and 14 days before challenge | 9.1 | No | 3.33 |
| 9.2 | No | 3.50 | ||
| 9.3 | No | 3.86 | ||
| 9.4 | No | 3.20 | ||
| 9.5 | No | 3.86 | ||
| Group 10 | Vaccinated twice with MVA-VP2 107 pfu per mouse 21 and 14 days before challenge | 10.1 | Yes | 0.00 |
| 10.2 | Yes | 0.00 | ||
| 10.3 | Yes | 0.00 | ||
| 10.4 | Yes | 0.00 | ||
| 10.5 | Yes | 0.00 |
Differences in viraemia levels were also significant (P < 0.05), being highest in Group 9 relative to all other Groups, but also evident in Group 8 relative to Groups 5 and 10 (Fig. 3 ). Thus, the levels of protection from the serum transfer experiment can be ranked in the following order: Group 10 > Group 5 > Group 6 = Group 7 > Group 8 > Group 9. These data collectively indicate that transfer of antiserum was protective when given in a time window of plus or minus 48 h around the time of challenge. This protection is defined by a complete prevention of lethality of AHSV infection, a significant reduction of clinical signs and a significant reduction of viraemia for every sampling point. Protection was maximum when the dose was increased (Group 5, 400 μl/mouse) and when the administration was performed prior to virus challenge (Group 7, serum transferred 48 h before challenge). As expected the administration of the antiserum 48 h after challenge (Group 8) was less protective than in Groups 5, 6 and 7, but even in these conditions the affected mice recovered and clinical signs had completely disappeared by day 10 post-infection.
Fig. 3.
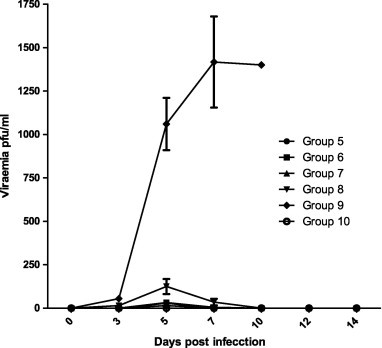
Viraemia of antiserum recipients following AHSV challenge. Mean virus titres, expressed as pfu/ml of blood, were measured on days 3, 5, 7 and 10 from mice from Groups 5–10. Data are shown as mean ± STD.
4. Discussion
Despite the inability of MVA to replicate in most mammalian cells in vitro and in vivo, even in immunocompromised individuals (Gilbert, 2013, Gomez et al., 2008) recombinant MVA vaccines can express foreign antigens in host cells upon inoculation and induce immune responses specific for the foreign antigen. MVA vector vaccines for viral infections have proven to be effective against a wide range of viral diseases (Gilbert, 2013), such as Chikungunya (Garcia-Arriaza et al., 2014) or severe acute respiratory syndrome (Chen et al., 2005). Humoral and cellular immune responses elicited against a foreign MVA-encoded antigen are higher than those triggered with the vaccinia Western Reverse strain, in part due to the higher levels of expression of the foreign antigen by MVA (Ramirez et al., 2000). Moreover, MVA is able to elicit strong, specific responses under conditions of pre-existing immunity to the vector (Ramirez et al., 2000), as seen in previous studies using MVA in both prime and boost immunisations.
The use of MVA based vaccines, in heterologous prime-boost vaccination regimes, is most often pursued for diseases where cell-mediated immunity definitely plays an important role in protection, as in the case of Plasmodium falciparum (Ogwang et al., 2013), HIV (Gomez et al. 2012; Cosma et al., 2003), or influenza (Berthoud et al., 2011). However, MVA based vaccines are also able to elicit strong antibody responses (Draper et al., 2013). MVA has been used to develop a promising antibody-inducing vaccine against viral surface proteins, such as the haemagglutinin (HA) of influenza virus (Kreijtz et al., 2009), or the spike glycoprotein of SARS (Chen et al., 2005). In vaccination studies for BTV, MVA has been very effective as a vaccine, inducing a robust VNAb response against the expressed VP2 protein (Calvo-Pinilla et al., 2009, Jabbar et al., 2013). Similarly, MVA expressing AHSV-VP2 has been shown to elicit high levels of neutralizing antibodies (Castillo-Olivares et al., 2011, Chiam et al., 2009).
A previous passive immunisation study showed that MVA-VP2 vaccination induces a highly protective humoral immune response against AHSV (Calvo-Pinilla et al., 2014). In that study, AHSV-specific interferon-γ secreting CD8+ T cells were also induced by vaccination with MVA-VP2, but their role in protection could not be evaluated at that time. Previously, Pretorius et al. (2012) demonstrated an increase of virus specific CD8+ T-cells in horses, in response to vaccination with live attenuated AHSV. Vaccination studies in mice using recombinant MVA expressing AHSV-4 NS1, administered in combination with MVA-VP2, also showed specific T-cell responses and a reduction in viraemia following heterologous challenge (de la Poza et al., 2013). In addition, a recombinant Canarypox expressing AHSV-VP2 and VP5 was able to induce VP2-specific CD8+ T-cell responses, alongside VNAb. This suggests cell-mediated immunity could play a significant role in the overall level of protection against AHSV (El Garch et al., 2012). However, a clear demonstration of the protective effect of this effector mechanism of immunity, through adoptive transfer of CD8+ T-cells has not yet been reported.
In the present study, adoptive transfer of splenocytes from MVA-VP2 vaccinated mice, significantly reduced the clinical score of AHSV challenged recipient mice, and resulted in a 40% survival, although changes in the survival rate and the reduction in viraemia were not considered to be mathematically significant. This suggests that the role of cell-mediated immune responses is less important than the antibody responses in the protection generated by MVA-VP2 vaccination. In addition, it can be argued that the marginal protection against AHSV shown by the recipients of splenocytes could be due to AHSV-VP2-specific B cells contained in the transferred cells. Additional adoptive transfer experiments using cell-sorted CD8+ lymphocytes from donors before challenge could help to elucidate the precise contribution of cell-mediated immunity following MVA-VP2 vaccination.
In studies with the related orbivirus BTV, adoptive transfer of CD8+ cytotoxic cells from a BTV infected sheep, partially protected recipient sheep against infection with either homologous or heterologous BTV serotypes (Jeggo et al., 1984a). In contrast, when passive transfer of antibodies from infected animals was performed, the protection was complete against virulent virus (Jeggo et al., 1984b). In the case of AHSV, the humoral nature of protection against the virus has been demonstrated by the passive transfer of a monoclonal neutralising antibody against VP2 protein in the neonatal mouse model (Burrage et al., 1993). Passive transfer of neutralising antibodies has also been described from AHSV vaccinated mares to foals via colostrum (Blackburn and Swanepoel, 1988, Crafford et al., 2013).
In the present study, consistent with previous observations, the highly protective effect of antiserum derived from MVA-VP2 vaccinated mice was also demonstrated even when transferred 48 h post-infection. When the antiserum dose was increased (Group 5), the protective effect was very close to that shown by the actively immunized MVA-VP2 vaccinated mice. The limited clinical signs that were still evident in mice infected 48 h before transfer, eventually disappeared and the animals recovered completely (Group 8). This suggests that passive immunisation with MVA-VP2 antiserum could be used for therapeutic applications, in particular for emergency treatment of AHS in horses during the initial stages of an outbreak, before containment measures or widespread vaccination campaigns are initiated.
In this and previous studies it has been shown that MVA-VP2 vaccination induces high VNAb responses both in mice and horses and is highly protective against AHSV in both experimental systems. It can be concluded that protection is mainly associated with antibodies, since passive transfer of immune serum from MVA-VP2 vaccinated mice is sufficient to provide clinical protection.
Acknowledgements
This work was funded by Department for Food, Environment and Rural Affairs, UK (DEFRA Project number: SE4109). Javier Ortego is recipient supported by grant AGL-2011-23506 from the Spanish Ministerio de Economia y Competitividad. We would like to thank Prof Malcolm McCrae for critically reading the manuscript.
References
- Alberca B., Bachanek-Bankowska K., Cabana M., Calvo-Pinilla E., Viaplana E., Frost L., Gubbins S., Urniza A., Mertens P., Castillo-Olivares J. Vaccination of horses with a recombinant modified vaccinia Ankara virus (MVA) expressing African horse sickness (AHS) virus major capsid protein VP2 provides complete clinical protection against challenge. Vaccine. 2014;32(29):3670–3674. doi: 10.1016/j.vaccine.2014.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley L., Fehrsen J., Jordaan F., Huismans H., du Plessis D.H. Identification of antigenic regions on VP2 of African horse sickness virus serotype 3 by using phage-displayed epitope libraries. J. Gen. Virol. 2000;81(Pt 4):993–1000. doi: 10.1099/0022-1317-81-4-993. [DOI] [PubMed] [Google Scholar]
- Berthoud T.K., Hamill M., Lillie P.J., Hwenda L., Collins K.A., Ewer K.J., Milicic A., Poyntz H.C., Lambe T., Fletcher H.A., Hill A.V., Gilbert S.C. Potent CD8+ T-cell immunogenicity in humans of a novel heterosubtypic influenza A vaccine, MVA-NP+M1. Clin. Infect. Dis. 2011;52(1):1–7. doi: 10.1093/cid/ciq015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackburn N.K., Swanepoel R. Observations on antibody levels associated with active and passive immunity to African horse sickness. Trop. Anim. Health Prod. 1988;20(4):203–210. doi: 10.1007/BF02239981. [DOI] [PubMed] [Google Scholar]
- Burrage T.G., Trevejo R., Stone-Marschat M., Laegreid W.W. Neutralizing epitopes of African horse sickness virus serotype 4 are located on VP2. Virology. 1993;196(2):799–803. doi: 10.1006/viro.1993.1537. [DOI] [PubMed] [Google Scholar]
- Calvo-Pinilla E., de la Poza F., Gubbins S., Mertens P.P., Ortego J., Castillo-Olivares J. Vaccination of mice with a modified Vaccinia Ankara (MVA) virus expressing the African horse sickness virus (AHSV) capsid protein VP2 induces virus neutralising antibodies that confer protection against AHSV upon passive immunisation. Virus Res. 2014;180:23–30. doi: 10.1016/j.virusres.2013.12.002. [DOI] [PubMed] [Google Scholar]
- Calvo-Pinilla E., Rodriguez-Calvo T., Sevilla N., Ortego J. Heterologous prime boost vaccination with DNA and recombinant modified vaccinia virus Ankara protects IFNAR(−/−) mice against lethal bluetongue infection. Vaccine. 2009;28(2):437–445. doi: 10.1016/j.vaccine.2009.10.027. [DOI] [PubMed] [Google Scholar]
- Castillo-Olivares J., Calvo-Pinilla E., Casanova I., Bachanek-Bankowska K., Chiam R., Maan S., Nieto J.M., Ortego J., Mertens P.P. A modified vaccinia Ankara virus (MVA) vaccine expressing African horse sickness virus (AHSV) VP2 protects against AHSV challenge in an IFNAR −/− mouse model. PLoS One. 2011;6(1):e16503. doi: 10.1371/journal.pone.0016503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosma A., Nagaraj R., Buhler S., Hinkula J., Busch D.H., Sutter G., Goebel F.D., Erfle V. Therapeutic vaccination with MVA-HIV-1 nef elicits Nef-specific T-helper cell responses in chronically HIV-1 infected individuals. Vaccine. 2003;22(1):21–29. doi: 10.1016/s0264-410x(03)00538-3. [DOI] [PubMed] [Google Scholar]
- Crafford J.E., Lourens C.W., Gardner I.A., Maclachlan N.J., Guthrie A.J. Passive transfer and rate of decay of maternal antibody against African horse sickness virus in South African thoroughbred foals. Equine Vet. J. 2013;45(5):604–607. doi: 10.1111/evj.12015. [DOI] [PubMed] [Google Scholar]
- Chen H., Hou J., Jiang X., Ma S., Meng M., Wang B., Zhang M., Tang X., Zhang F., Wan T., Li N., Yu Y., Hu H., Yang R., He W., Wang X., Cao X. Response of memory CD8+ T cells to severe acute respiratory syndrome (SARS) coronavirus in recovered SARS patients and healthy individuals. J. Immunol. 2005;175(1):591–598. doi: 10.4049/jimmunol.175.1.591. [DOI] [PubMed] [Google Scholar]
- Chiam R., Sharp E., Maan S., Rao S., Mertens P., Blacklaws B., Davis-Poynter N., Wood J., Castillo-Olivares J. Induction of antibody responses to African horse sickness virus (AHSV) in ponies after vaccination with recombinant modified vaccinia Ankara (MVA) PLoS One. 2009;4(6):e5997. doi: 10.1371/journal.pone.0005997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de la Poza F., Calvo-Pinilla E., Lopez-Gil E., Marin-Lopez A., Mateos F., Castillo-Olivares J., Lorenzo G., Ortego J. Ns1 is a key protein in the vaccine composition to protect Ifnar(-/-) mice against infection with multiple serotypes of African horse sickness virus. PloS one. 2013;8:e70197. doi: 10.1371/journal.pone.0070197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Draper S.J., Cottingham M.G., Gilbert S.C. Utilizing poxviral vectored vaccines for antibody induction-progress and prospects. Vaccine. 2013;31(39):4223–4230. doi: 10.1016/j.vaccine.2013.05.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Garch H., Crafford J.E., Amouyal P., Durand P.Y., Edlund Toulemonde C., Lemaitre L., Cozette V., Guthrie A., Minke J.M. An African horse sickness virus serotype 4 recombinant canarypox virus vaccine elicits specific cell-mediated immune responses in horses. Vet. Immunol. Immunopathol. 2012;149(1–2):76–85. doi: 10.1016/j.vetimm.2012.06.009. [DOI] [PubMed] [Google Scholar]
- Garcia-Arriaza J., Cepeda V., Hallengard D., Sorzano C.O., Kummerer B.M., Liljestrom P., Esteban M. A novel poxvirus-based vaccine, MVA-CHIKV, is highly immunogenic and protects mice against chikungunya infection. J. Virol. 2014;88(6):3527–3547. doi: 10.1128/JVI.03418-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert S.C. Clinical development of modified vaccinia virus Ankara vaccines. Vaccine. 2013;31(39):4241–4246. doi: 10.1016/j.vaccine.2013.03.020. [DOI] [PubMed] [Google Scholar]
- Gomez C.E., Najera J.L., Krupa M., Esteban M. The poxvirus vectors MVA and NYVAC as gene delivery systems for vaccination against infectious diseases and cancer. Curr. Gene Ther. 2008;8:97–120. doi: 10.2174/156652308784049363. [DOI] [PubMed] [Google Scholar]
- Jabbar T.K., Calvo-Pinilla E., Mateos F., Gubbins S., Bin-Tarif A., Bachanek-Bankowska K., Alpar O., Ortego J., Takamatsu H.H., Mertens P.P., Castillo-Olivares J. Protection of IFNAR (−/−) mice against bluetongue virus serotype 8, by heterologous (DNA/rMVA) and homologous (rMVA/rMVA) vaccination, expressing outer-capsid protein VP2. PLoS One. 2013;8(4):e60574. doi: 10.1371/journal.pone.0060574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeggo M.H., Wardley R.C., Brownlie J. A study of the role of cell-mediated immunity in bluetongue virus infection in sheep, using cellular adoptive transfer techniques. Immunology. 1984;52(3):403–410. [PMC free article] [PubMed] [Google Scholar]
- Jeggo M.H., Wardley R.C., Taylor W.P. Role of neutralising antibody in passive immunity to bluetongue infection. Res. Vet. Sci. 1984;36(1):81–86. [PubMed] [Google Scholar]
- Karber G. 50% end-point calculation. Arch. Exp. Pathol. Pharmak. 1931;162:480–483. [Google Scholar]
- Kreijtz J.H., Suezer Y., de Mutsert G., van Amerongen G., Schwantes A., van den Brand J.M., Fouchier R.A., Lower J., Osterhaus A.D., Sutter G., Rimmelzwaan G.F. MVA-based H5N1 vaccine affords cross-clade protection in mice against influenza A/H5N1 viruses at low doses and after single immunization. PLoS One. 2009;4(11):e7790. doi: 10.1371/journal.pone.0007790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Torrecuadrada J.L., Casal J.I. Identification of a linear neutralization domain in the protein VP2 of African horse sickness virus. Virology. 1995;210(2):391–399. doi: 10.1006/viro.1995.1355. [DOI] [PubMed] [Google Scholar]
- Martinez-Torrecuadrada J.L., Diaz-Laviada M., Roy P., Sanchez C., Vela C., Sanchez-Vizcaino J.M., Casal J.I. Full protection against African horse sickness (AHS) in horses induced by baculovirus-derived AHS virus serotype 4 VP2, VP5 and VP7. J. Gen. Virol. 1996;77(Pt 6):1211–1221. doi: 10.1099/0022-1317-77-6-1211. [DOI] [PubMed] [Google Scholar]
- Martinez-Torrecuadrada J.L., Langeveld J.P., Meloen R.H., Casal J.I. Definition of neutralizing sites on African horse sickness virus serotype 4 VP2 at the level of peptides. J. Gen. Virol. 2001;82(Pt 10):2415–2424. doi: 10.1099/0022-1317-82-10-2415. [DOI] [PubMed] [Google Scholar]
- Mellor P.S., Hamblin C. African horse sickness. Vet. Res. 2004;35(4):445–466. doi: 10.1051/vetres:2004021. [DOI] [PubMed] [Google Scholar]
- Ogwang C., Afolabi M., Kimani D., Jagne Y.J., Sheehy S.H., Bliss C.M., Duncan C.J., Collins K.A., Garcia Knight M.A., Kimani E., Anagnostou N.A., Berrie E., Moyle S., Gilbert S.C., Spencer A.J., Soipei P., Mueller J., Okebe J., Colloca S., Cortese R., Viebig N.K., Roberts R., Gantlett K., Lawrie A.M., Nicosia A., Imoukhuede E.B., Bejon P., Urban B.C., Flanagan K.L., Ewer K.J., Chilengi R., Hill A.V., Bojang K. Safety and immunogenicity of heterologous prime-boost immunisation with Plasmodium falciparum malaria candidate vaccines, ChAd63 ME-TRAP and MVA ME-TRAP, in healthy Gambian and Kenyan adults. PLoS One. 2013;8(3):e57726. doi: 10.1371/journal.pone.0057726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pretorius A., Van Kleef M., Van Wyngaardt W., Heath J. Virus-specific CD8(+) T-cells detected in PBMC from horses vaccinated against African horse sickness virus. Vet. Immunol. Immunopathol. 2012;146(1):81–86. doi: 10.1016/j.vetimm.2012.01.016. [DOI] [PubMed] [Google Scholar]
- Ramirez J.C., Gherardi M.M., Rodriguez D., Esteban M. Attenuated modified vaccinia virus Ankara can be used as an immunizing agent under conditions of preexisting immunity to the vector. J. Virol. 2000;74(16):7651–7655. doi: 10.1128/jvi.74.16.7651-7655.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romito M., Du Plessis D.H., Viljoen G.J. Immune responses in a horse inoculated with the VP2 gene of African horse sickness virus. Onderstepoort J. Vet. Res. 1999;66(2):139–144. [PubMed] [Google Scholar]
- Roy P., Mertens P.P., Casal I. African horse sickness virus structure. Comp. Immunol. Microbiol. Infect. Dis. 1994;17(3–4):243–273. doi: 10.1016/0147-9571(94)90046-9. [DOI] [PubMed] [Google Scholar]
- Roy P., Sutton G. New generation of African horse sickness virus vaccines based on structural and molecular studies of the virus particles. Arch. Virol. Suppl. 1998;14:177–202. doi: 10.1007/978-3-7091-6823-3_17. [DOI] [PubMed] [Google Scholar]
- Scanlen M., Paweska J.T., Verschoor J.A., van Dijk A.A. The protective efficacy of a recombinant VP2-based African horse sickness subunit vaccine candidate is determined by adjuvant. Vaccine. 2002;20(7–8):1079–1088. doi: 10.1016/s0264-410x(01)00445-5. [DOI] [PubMed] [Google Scholar]
- Stone-Marschat M.A., Moss S.R., Burrage T.G., Barber M.L., Roy P., Laegreid W.W. Immunization with VP2 is sufficient for protection against lethal challenge with African horse sickness virus Type 4. Virology. 1996;220(1):219–222. doi: 10.1006/viro.1996.0304. [DOI] [PubMed] [Google Scholar]


