Abstract
2017 marked the 30th anniversary of the approval of zidovudine (AZT) as the first HIV/AIDS therapy. Since then, more than eighty antiviral drugs have received FDA approval, half of which treat HIV infection. Here, we provide a retrospective analysis of approved antiviral drugs, including therapeutics against other major chronic infections such as hepatitis B and C, and herpes viruses, over the last thirty years. During this time, only a few drugs were approved to treat acute viral infections, mainly influenza. Analysis of these approved antiviral drugs based on molecular class and mode of action shows that a large majority are small molecules and direct-acting agents as opposed to proteins, peptides, or oligonucleotides and host-targeting therapies. In addition, approvals of combination therapies accelerated over the last five years. We also provide a prospective study of future potential antiviral therapies, based on current clinical research pipelines across the pharmaceutical industry. Comparing past drug approvals with current clinical candidates hints at the future evolution in antiviral therapies and reveals how antiviral medicines are often discovered. Overall, this work helps forecast future trends and innovation in the field of antiviral research and development.
Keywords: Antiviral, Small molecule, Direct acting agent, Chronic viral infection, Respiratory virus
Highlights
-
•
This review summarizes all approved antiviral drugs over the last thirty years.
-
•
Most are small molecules and direct-acting agents over biologics, oligonucleotides, and host-targeting therapies.
-
•
We provide a prospective study and trend analysis of future potential antivirals based on current clinical research.
1. Introduction
1.1. Scope of the study
The field of antiviral research has taken on a new dimension since the global spread of human immunodeficiency virus (HIV) caused the acquired immune deficiency syndrome (AIDS) epidemic in the 1980s, with unprecedented efforts in academic and pharmaceutical laboratories to develop new effective antiviral therapies. These efforts have led to advances in basic science and many therapeutic breakthroughs including development of inhibitors targeting HIV and other viruses. In this review, we analyze all antiviral therapeutics on the market since the approval of zidovudine (Retrovir®) on the basis of clinical indication, molecular size (small versus large), mode of action (or molecular target), and use in combination with other therapeutic agents. We also report all antiviral therapeutics currently in clinical-stage evaluation with the goal of comparing current research with past approvals to predict potential trends and changes in antiviral medicine. This work also helps to understand the driving forces behind innovation and success in antiviral research.
1.2. Definitions and method of analysis
1.2.1. FDA-approved drugs
The information about antiviral drugs for this evaluation was gathered directly from the Food and Drug Administration (FDA) Drug Database (https://www.accessdata.fda.gov/scripts/cder/daf/). Monthly approval reports from January 1987 through December 2017 were scanned to create an exhaustive list of 179 antiviral medications approved in the United States over the 30-year period. To narrow the focus to novel therapeutic agents, generic drugs were excluded from the list by identifying agents with “tentative approval.” When a generic drug product is ready for approval before patents or exclusivity protections on the reference listed drug product expire, the FDA issues a tentative approval letter and delays final approval of the generic drug product until all patent or exclusivity issues are resolved. Tentative approval letters, therefore, provided a means for screening out generic equivalents from this evaluation. Next, drugs not considered explicitly antivirals, such as pharmacokinetic enhancers like cobicistat, were excluded resulting in a subset of 108 drugs. This list was condensed further by restricting it to drugs submitted as either Class 1 (new molecular entity [NME]) or Class 4 (new combination) to eliminate approvals related to formulation changes, such as extended-release versions of previously approved drugs (https://www.fda.gov/downloads/aboutfda/centersoffices/officeofmedicalproductsandtobacco/cder/manualofpoliciesprocedures/ucm470773.pdf). We define NME as a drug that contains an active moiety that has never been approved by the FDA or marketed in the US. When drugs such as Epivir® received approval for a novel indication, first for HIV and later for hepatitis B virus (HBV), each approval was included as a separate entry. The final list consisted of 88 unique antiviral drug approvals, which were cataloged using the following characteristics:
| Trade Name | Direct-acting or Host-acting agent | Submission classification |
| Generic Name(s) | Molecular mechanism of action | Dosage |
| Year/Month of approval | Size: small or large molecule | Route |
| Indication | Mono- or Combination therapy | Company (when approved/listed in Drugs@FDA) |
Out of 88 approved antiviral drugs, ten were discontinued or withdrawn (marked as a in Table 1 ).
Table 1.
List of FDA-Approved Antiviral Drugs 1987–2017.
| Year | Trade Name | Generic Name (Abbreviation) | Indication (Virus) | Target (MOA) | Type | Mono/Combo |
|---|---|---|---|---|---|---|
| 1987 | Retrovir | Zidovudine (AZT) | HIV-1 | Pol | Small Molecule | Mono |
| 1988 | Intron A | Interferon Alfa-2B (INT2B) | HPV | Host | Protein | Mono |
| 1989 | Cytovene | Ganciclovir Sodium (GAN) | CMV | Pol | Small Molecule | Mono |
| 1989 | Alferon N Injection | Interferon Alfa-N3 (INTN3) | HPV | Host | Protein | Mono |
| 1991 | Intron A | Interferon Alfa-2B (INT2B) | HCV | Host | Protein | Mono |
| 1991 | Foscavir | Foscarnet Sodium (FOS) | CMV | Pol | Small Molecule | Mono |
| 1991 | Videxa | Didanosine (ddI) | HIV-1 | Pol | Small Molecule | Mono |
| 1992 | Hivida | Zalcitabine (ddC) | HIV-1 | Pol | Small Molecule | Mono |
| 1992 | Intron A | Interferon Alfa-2B (INT2B) | HBV | Host | Protein | Mono |
| 1993 | Flumadine | Rimantadine (RIM) | Influenza | O | Small Molecule | Mono |
| 1994 | Zerit | Stavudine (d4T) | HIV-1 | Pol | Small Molecule | Mono |
| 1994 | Famvira | Famciclovir (FAM) | HSV | Pol | Small Molecule | Mono |
| 1995 | Valtrex | Valacyclovir Hydrochloride (VAL) | HSV | Pol | Small Molecule | Mono |
| 1995 | Epivir | Lamivudine (3TC) | HIV-1 | Pol | Small Molecule | Mono |
| 1995 | Invirase | Saquinavir Mesylate (SQV) | HIV-1 | Pr | Small Molecule | Mono |
| 1996 | Norvir | Ritonavir (RTV) | HIV-1 | Pr | Small Molecule | Mono |
| 1996 | Crixivan | Indinavir Sulfate (IDV) | HIV-1 | Pr | Small Molecule | Mono |
| 1996 | Viramune | Nevirapine (NVP) | HIV-1 | Pol | Small Molecule | Mono |
| 1996 | Vistidea | Cidofovir (CID) | CMV | Pol | Small Molecule | Mono |
| 1996 | Denavir | Penciclovir (PEN) | HSV | Pol | Small Molecule | Mono |
| 1997 | Aldara | Imiquimod (IMI) | HPV | Host | Small Molecule | Mono |
| 1997 | Viracepta | Nelfinavir Mesylate (NFV) | HIV-1 | Pr | Small Molecule | Mono |
| 1997 | Rescriptor | Delavirdine Mesylate (DLV) | HIV-1 | Pol | Small Molecule | Mono |
| 1997 | Combivir | Lamivudine (3TC)/Zidovudine (AZT) | HIV-1 | Pol/Pol | Small Molecule | Combo |
| 1997 | Infergen | Interferon Alfacon-1 (INTA1) | HCV | Host | Protein | Mono |
| 1998 | Synagis | Palivizumab (PAV) | RSV | O | Protein | Mono |
| 1998 | Rebetol | Ribavirin (RIB) | HCV | Host | Small Molecule | Mono |
| 1998 | Vitravenea | Fomivirsen Sodium (FOM) | CMV | O | Oligo-nucleotide | Mono |
| 1998 | Sustiva | Efavirenz (EFV) | HIV-1 | Pol | Small Molecule | Mono |
| 1998 | Epivir-HBV | Lamivudine (3TC) | HBV | Pol | Small Molecule | Mono |
| 1998 | Ziagen | Abacavir Sulfate (ABC) | HIV-1 | Pol | Small Molecule | Mono |
| 1999 | Agenerasea | Amprenavir (APV) | HIV-1 | Pr | Small Molecule | Mono |
| 1999 | Relenza | Zanamivir (ZAN) | Influenza | O | Small Molecule | Mono |
| 1999 | Tamiflu | Oseltamivir (OSE) | Influenza | O | Small Molecule | Mono |
| 2000 | Abreva | Docosanol (DOC) | HSV | O | Small Molecule | Mono |
| 2000 | Kaletra | Lopinavir (LPV)/Ritonavir (RTV) | HIV-1 | Pr/Pr | Small Molecule | Combo |
| 2000 | Trizivir | Abacavir Sulfate (ABC)/Lamivudine (3TC)/Zidovudine (AZT) | HIV-1 | Pol/Pol/Pol | Small Molecule | Combo |
| 2001 | Pegintron/Sylatron | Peginterferon Alfa-2B (PEG2B) | HCV | Host | Protein | Mono |
| 2001 | Valcyte | Valganciclovir Hydrochloride (VALG) | CMV | Pol | Small Molecule | Mono |
| 2001 | Viread | Tenofovir Disoproxil Fumarate (TDF) | HIV-1 | Pol | Small Molecule | Mono |
| 2002 | Hepsera | Adefovir Dipivoxil (ADE) | HBV | Pol | Small Molecule | Mono |
| 2002 | Pegasys | Peginterferon Alfa-2A (PEG2A) | HCV | Host | Protein | Mono |
| 2003 | Fuzeon | Enfuvirtide (T20) | HIV-1 | O | Peptide | Mono |
| 2003 | Reyataz | Atazanavir Sulfate (ATV) | HIV-1 | Pr | Small Molecule | Mono |
| 2003 | Emtriva | Emtricitabine (FTC) | HIV-1 | Pol | Small Molecule | Mono |
| 2003 | Lexiva | Fosamprenavir Calcium (FPV) | HIV-1 | Pr | Small Molecule | Mono |
| 2004 | Epzicom | Abacavir Sulfate (ABC)/Lamivudine (3TC) | HIV-1 | Pol/Pol | Small Molecule | Combo |
| 2004 | Truvada | Emtricitabine (FTC)/Tenofovir Disoproxil Fumarate (TDF) | HIV-1 | Pol/Pol | Small Molecule | Combo |
| 2005 | Baraclude | Entecavir (ENT) | HBV | Pol | Small Molecule | Mono |
| 2005 | Pegasys | Peginterferon Alfa-2A (PEG2A) | HBV | Host | Protein | Mono |
| 2005 | Aptivus | Tipranavir (TPV) | HIV-1 | Pr | Small Molecule | Mono |
| 2006 | Prezista | Darunavir Ethanolate (DRV) | HIV-1 | Pr | Small Molecule | Mono |
| 2006 | Atripla | Efavirenz (EFV)/Emtricitabine (FTC)/Tenofovir Disoproxil Fumarate (TDF) | HIV-1 | Pol/Pol/Pol | Small Molecule | Combo |
| 2006 | Tyzekaa | Telbivudine (TEL) | HBV | Pol | Small Molecule | Mono |
| 2006 | Veregen | Sinecatechins (SIN) | HPV | Host | Small Molecule | Mono |
| 2007 | Selzentry | Maraviroc (MVC) | HIV-1 | Host | Small Molecule | Mono |
| 2007 | Isentress | Raltegravir Potassium (RAL) | HIV-1 | Int | Small Molecule | Mono |
| 2008 | Intelence | Etravirine (ETR) | HIV-1 | Pol | Small Molecule | Mono |
| 2008 | Viread | Tenofovir Disoproxil Fumarate (TDF) | HBV | Pol | Small Molecule | Mono |
| 2009 | Xerese | Acyclovir/Hydrocortisone (ACY) | HSV | Pol | Small Molecule | Combo |
| 2011 | Victrelis | Boceprevir (BOC) | HCV | Pr | Small Molecule | Mono |
| 2011 | Edurant | Rilpivirine Hydrochloride (RPV) | HIV-1 | Pol | Small Molecule | Mono |
| 2011 | Inciveka | Telaprevir (TELA) | HCV | Pr | Small Molecule | Mono |
| 2011 | Complera | Emtricitabine (FTC)/Rilpivirine Hydrochloride (RPV)/Tenofovir Disoproxil Fumarate (TDF) | HIV-1 | Pol/Pol/Pol | Small Molecule | Combo |
| 2012 | Stribild | Cobicstat (COBI)/Elvitegravir (EVG)/Emtricitabine (FTC)/Tenofovir Disoproxil Fumarate (TDF) | HIV-1 | O/Int/Pol/Pol | Small Molecule | Combo |
| 2013 | Tivicay | Dolutegravir Sodium (DTG) | HIV-1 | Int | Small Molecule | Mono |
| 2013 | Olysio | Simeprevir Sodium (SIM) | HCV | Pr | Small Molecule | Mono |
| 2013 | Sovaldi | Sofosbuvir (SOF) | HCV | Pol | Small Molecule | Mono |
| 2014 | Triumeq | Abacavir Sulfate (ABC)/Dolutegravir Sodium (DTG)/Lamivudine (3TC) | HIV-1 | Pol/Int/Pol | Small Molecule | Combo |
| 2014 | Vitekta | Elvitegravir (EVG) | HIV-1 | Int | Small Molecule | Mono |
| 2014 | Harvoni | Ledipasvir (LED)/Sofosbuvir (SOF) | HCV | NS5A/Pol | Small Molecule | Combo |
| 2014 | Rapivab | Peramivir (PER) | Influenza | O | Small Molecule | Mono |
| 2014 | Viekira Pak | Dasabuvir Sodium (DAS)/Ombitasvir (OMB)/Paritaprevir (PAR)/Ritonavir (RTV) | HCV | Pr/Pr/NS5A/Pol | Small Molecule | Combo |
| 2015 | Prezcobix | Cobicstat (COBI)/Darunavir Ethanolate (DRV) | HIV-1 | Pr | Small Molecule | Combo |
| 2015 | Evotaz | Atazanavir Sulfate (ATV)/Cobicstat (COBI) | HIV-1 | Pr | Small Molecule | Combo |
| 2015 | Dutrebisa | Lamivudine (3TC)/Raltegravir (RAL) | HIV-1 | Pol/Int | Small Molecule | Combo |
| 2015 | Daklinza | Daclatasvir Dihydrochloride (DAC) | HCV | NS5A | Small Molecule | Mono |
| 2015 | Technivie | Ombitasvir (OMB)/Paritaprevir (PAR)/Ritonavir (RTV) | HCV | Pr/Pr/NS5A | Small Molecule | Combo |
| 2015 | Genvoya | Cobicstat (COBI)/Elvitegravir (EVG)/Emtricitabine (FTC)/Tenofovir Alafenamide Fumarate (TAF) | HIV-1 | O/Int/Pol/Pol | Small Molecule | Combo |
| 2016 | Zepatier | Elbasvir (ELB)/Grazoprevir (GRA) | HCV | Pr/NS5A | Small Molecule | Combo |
| 2016 | Odefsey | Emtricitabine (FTC)/Rilpivirine Hydrochloride (RPV)/Tenofovir Alafenamide Fumarate (TAF) | HIV-1 | Pol/Pol/Pol | Small Molecule | Combo |
| 2016 | Descovy | Emtricitabine (FTC)/Tenofovir Alafenamide Fumarate (TAF) | HIV-1 | Pol | Small Molecule | Combo |
| 2016 | Epclusa | Sofosbuvir (SOF)/Velpatasvir (VEL) | HCV | Pol/NS5A | Small Molecule | Combo |
| 2016 | Vemlidy | Tenofovir Alafenamide Fumarate (TAF) | HBV | Pol | Small Molecule | Mono |
| 2017 | Vosevi | Sofosbuvir (SOF)/Velpatasvir (VEL)/Voxilaprevir (VOX) | HCV | Pr/Pol/NS5A | Small Molecule | Combo |
| 2017 | Mavyret | Glecaprevir (GLE)/Pibrentasvir (PIB) | HCV | Pr/NS5A | Small Molecule | Combo |
| 2017 | Prevymis | Letermovir (LET) | CMV | O | Small Molecule | Mono |
| 2017 | Juluca | Dolutegravir (DTG)/Rilpivirine (RPV) | HIV-1 | Pol/Int | Small Molecule | Combo |
Viruses.
HIV-1= Human immunodeficiency virus-1.
HCV= Hepatitis C virus.
HBV= Hepatitis B virus.
CMV= Cytamegalovirus.
HSV= Herpes simplex virus.
HPV= Human papillomavirus.
Targets.
Pol = Polymerase.
Pr= Protease.
Int = Integrase.
NS5A= Nonstructural protein 5A.
O= Other.
Other abbreviations.
Mono = Monotherapy.
Combo = Combination therapy.
Discontinued or Withdrawn.
1.2.2. Drugs in development
Four criteria were established to include drug candidates on the list of antivirals in development for this evaluation. Each drug candidate was required to be: (1) in human trials, Phase 1–3, (2) a therapeutic agent (i.e., not a vaccine), (3) submitted to the US FDA or listed in ClinicalTrials.gov, and (4) in “active” development, meaning a clinical or company update was evident in the past 2 years. The initial list of drug candidates in clinical development was gleaned from research pipeline information available on company websites (both large and small companies active in the antiviral drug development space). Next, recent published reviews covering drug development for different viruses or drug classes were screened, e.g. (Salazar et al., 2017). Finally, the list was supplemented by records generated through Informa's PharmaProjects database.
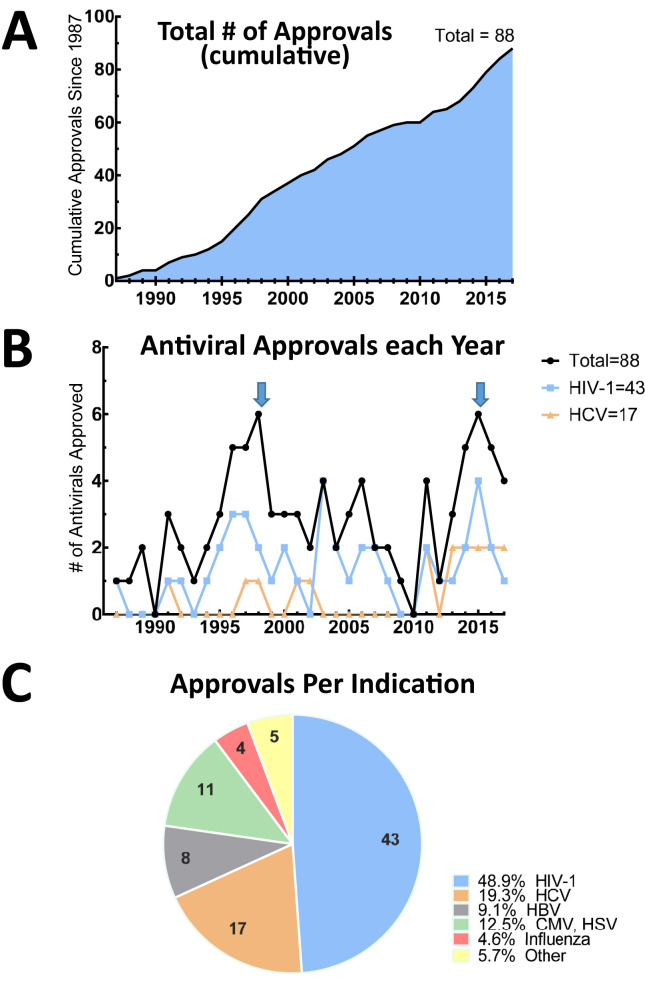
1.3. Trends for 1987–2017
The chronological order of market approvals for antiviral drugs over the last thirty years is represented in Fig. 1 . The cumulative analysis of FDA-approved antivirals during this time interval shows an almost linear progression of about 2.8 approvals per year (Fig. 2 A). This represents roughly one-tenth of the yearly FDA approvals across all indications (https://www.fda.gov/downloads/aboutfda/transparency/basics/ucm247465.pdf). A more detailed inspection of the number of antiviral agent approvals per year reveals two discrete waves, the first corresponding to the emergence of HIV therapeutics, which peaked in 1996–1997 and the second corresponding to anti-hepatitis C virus (HCV) drugs in 2011–2017 (Fig. 2B).
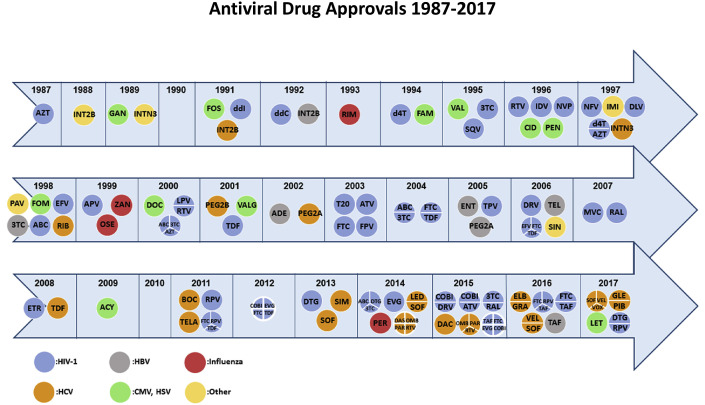
Fig. 1.
Timeline of US FDA Antiviral Drug Approvals: 1987–2017. Chronology of US FDA approvals of all antiviral drugs (see Table 1 for drug name abbreviations) using the criteria described in Section 1.2.1. HIV-1 drug approvals are shown in blue, influenza drug approvals in red, HBV drug approvals in grey, CMV and HSV drug approvals in green, and approvals of drugs for other indications in yellow. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Time and indication of US FDA antiviral drug approvals. (A) Total cumulative number of antiviral drug approvals from 1987 to 2017. (B) Number of approval per year, indicating total (black), HIV-1 (blue), HCV (orange). Blue arrows indicate the peaks of two distinct waves of antiviral approvals, the first for HIV-1 therapies (1996–1998), the second for anti-HCV drugs (2011–2017) (C) Proportion and number of US FDA antiviral drug approvals per indication from 1987 to 2017. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
1.4. General attributes of approved antiviral drugs
1.4.1. Indications
With 43 approvals during the 1987–2017 period, HIV-1 is the indication with the single largest share of antiviral agent approvals (Fig. 2C). The indication with the next largest share of approvals is HCV, with 17 during the same interval. When combined, HIV-1 and HCV therapeutics account for more than two-thirds of all antiviral drug approvals from 1987 to 2017 (Fig. 2B and C). Eleven and eight drugs have been approved to treat Herpesviridae (cytomegalovirus [CMV] and herpes simplex virus [HSV]) and HBV infection, respectively. Finally, four drugs were approved to treat external genital warts associated with human papilloma virus (HPV) infection. Taken together, drugs approved to treat chronic viral infections represent over 90% of all antivirals approved during the last 30 years. With respect to acute infections, five drugs were approved to treat respiratory viruses: four for the treatment of influenza infection, and one for respiratory syncytial virus (RSV).
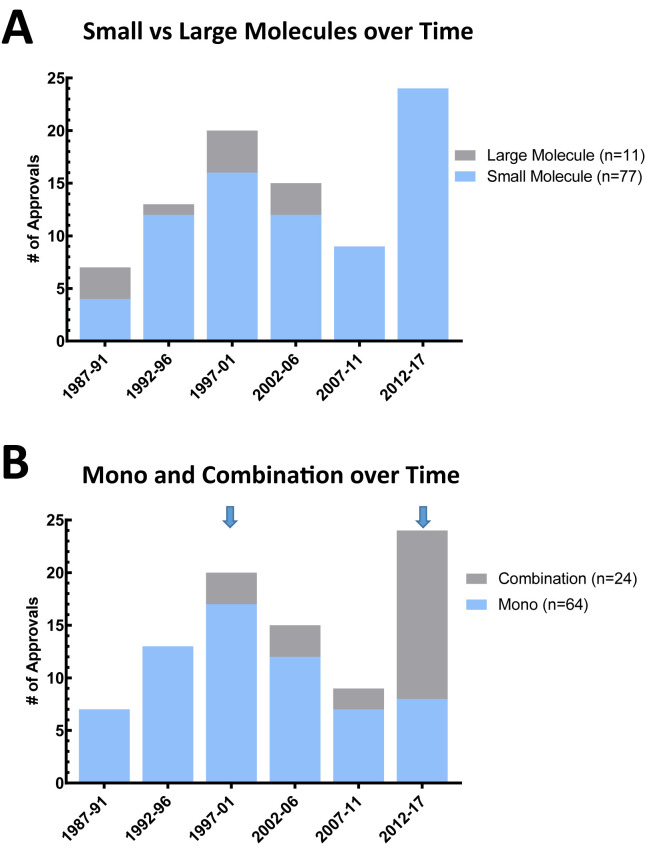
1.4.2. Small versus large molecules
Small molecules represent the dominant class of antivirals, with 77 approvals out of the total of 88. Most antiviral large molecules were approved during the 1997–2006 period (Fig. 3 A) and include five unique interferons, one monoclonal antibody, one peptide, and one oligonucleotide. The first large molecule approved for antiviral therapy was interferon alpha-2b (Intron A®), a mixture of human interferon alpha proteins used to treat external genital warts associated with HPV since 1988 (Suppl 1). Different forms of recombinant interferons were subsequently approved, such as interferon alpha n3 (Alferon N®) in 1989 also treating HPV-associated infection, with interferon alfacon-1 (Infergen®) being the first HCV therapeutic in 1997.Pegylated interferons were then introduced soon with the approvals of peginterferon Alfa-2B (Pegintron/Sylatron®) in 2001, and peginterferon Alfa-2A (Pegasys®) in 2002. The only antiviral monoclonal antibody, palivizumab (Synagis®), was approved in 1998 for the prophylactic treatment of infants at risk of contracting severe RSV infection. In 2003, the 36 amino acid peptide enfuvirtide (Fuzeon®) received FDA approval for the treatment of HIV-1 infection in salvage therapy. The only approved antiviral oligonucleotide, fomivirsen (Vitravene®), is an antisense antiviral drug used to treat cytomegalovirus (CMV)-induced retinitis in immunocompromised patients.
Fig. 3.
Attributes of approved antiviral drugs. (A) Number of small (blue) versus large (grey) molecules over time in 5-year intervals. (B) Number of monotherapies (blue) versus combination therapies (grey) over time in 5- to 6-year intervals. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
1.4.2.1. Mono- and combination therapies
Although combination therapies are now widely used for antimicrobial and anticancer treatments, the concept of combination therapy was originally pioneered for antiretroviral treatments. The main purpose of combination therapies is to prevent or delay the emergence of drug resistance by inhibiting viral replication at multiple points in the viral life cycle. During the 1987–2017 period, antiviral monotherapy approvals totaled 64 and combination therapy approvals totaled 24 (Fig. 3B). Approval of the initial combination therapies against HIV-1 infection followed the approvals of the individual components as monotherapies, which helps explain their later emergence as combination drug therapy approvals (Fig. 3B). Lamivudine/zidovudine (Combivir®) was the first fixed-dose combination therapy approved for HIV-infected patients in 1997, soon after the approval of lamivudine in 1995 (Fig. 1). For HCV combination therapies, most NMEs were approved as part of a combination therapy without any prior individual drug approval. One notable exception is sofosbuvir (Sovaldi®), which was approved first in 2013 as a monotherapy against HCV and was approved soon after in combination therapies: Harvoni® in 2015, Epclusa® in 2016, and Vosevi® in 2017 (Fig. 1 and Table 1).
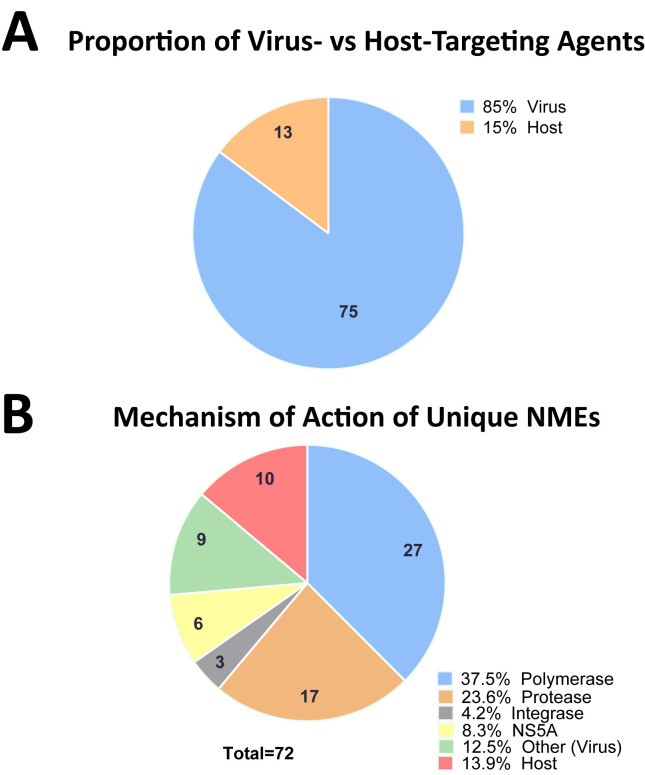
1.4.3. Virus- versus host-targeting agents
Over the last thirty years, only thirteen antiviral drug approvals (ten NMEs) target host mechanisms; most approved antivirals work as virus-targeting (or direct-acting) agents interacting with viral targets (Fig. 4 A). Approved host-targeting molecules include interferons as immunomodulating agents (interferon alpha-2b, interferon alpha-n3, interferon alfacon-1, peginterferon Alfa-2B, and peginterferon Alfa-2A). Five host-targeting small molecules have been approved. Imiquimod (Aldara®) is a toll-like receptor (TLR)7 agonist approved in 1997 for the topical treatment of genital and perianal warts, superficial basal cell carcinoma, and actinic keratosis. Docosanol (Abreva®) was approved as a topical cream in 2000 to treat herpes labialis caused by HSV-1 infections. Although the mechanism of action of docosanol is not entirely understood, its very broad antiviral spectrum and interaction with plasma membranes suggests that it does not act directly on viral particles (Leung and Sacks, 2004). In 1998, ribavirin (Rebetol®), a guanosine analog, was approved for the treatment of HCV infection. Ribavirin is believed to have multiple mechanisms of action, including immunomodulation and inhibition of human inosine-5′-monophosphate dehydrogenase (IMPDH) (Paeshuyse et al., 2011). In 2007, maraviroc (Selzentry®) was approved to treat HIV-1 infection by targeting C-C chemokine receptor type 5 (CCR5), one of the main host chemokine receptors for virus entry into T-cells. Topical Sinecatechins (Veregen®) is a water extract of green tea leaves that was approved in 2006 for treatment of genital warts caused by the HPV, without a well-defined mechanism of action.
Fig. 4.
Mechanism of action of FDA-approved antiviral drugs: 1987–2017. (A) Proportion and number of virus-targeting agents (blue) and host-targeting agents (orange). (B) Mechanism of action of FDA-approved unique NMEs designated as polymerases (blue); proteases (orange); integrases (grey); non-structural protein 5A [NS5A] (yellow); other mechanism (green); and host-targeting agents (red). We define NME as a drug that contains an active moiety that has never been approved by the FDA or marketed in the US. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
1.5. Mechanisms of action of direct acting agents
Out of the 88 therapies approved between 1987 and 2017, 72 were unique NMEs. Each NME was classified as targeting either the viral polymerase, protease, integrase, nonstructural protein 5A (NS5A), “other”, or acting on the host. Examples of antiviral drugs falling in the other classification include fomivirsen (Vitravene®), which is an antisense oligonucleotide and oseltamivir (Tamiflu®), an influenza virus neuraminidase inhibitor.
1.5.1. Polymerase inhibitors
Viral enzymes (polymerase + protease + integrase) represent the main protein targets of antiviral agents. Inhibitors of viral enzymes account for more than two-thirds of all antivirals including virus- and host-targeting agents approved between 1987 and 2017 (Fig. 4B). With 27 approved NMEs, polymerase inhibitors represent the largest class of virus-targeting agents (Fig. 4B). Polymerase inhibitors fall into two categories: nucleoside analogs and non-nucleoside inhibitors. Although zidovudine (Retrovir®) was the first nucleoside analog approved for HIV-1 treatment, other nucleoside analogs used as virus-targeting antimetabolites such as acyclovir (Zovirax®) for HSV had already been approved. Nucleoside analogs are prodrugs that mimic natural nucleosides and are used, in their triphosphate forms, as substrates for the synthesis of viral nucleic acid. This means that nucleoside analogs must not only be substrates for viral polymerases, they also need to be recognized and phosphorylated by host nucleo(s/t)ide kinases. Long-term use of first-generation anti-HIV nucleoside analogs zalcitabine (Hivid®) and didanosine (Videx®) has been limited by acute toxicity due to insufficient selectivity between viral and human DNA polymerases (Johnson et al., 2001). Second-generation HIV-nucleosides such as lamivudine (Epivir®), emtricitabine (Emtriva®), and tenofovir disoproxil fumarate (Viread®) displayed greater selectivity and tolerability. Non-nucleoside polymerase inhibitors typically bind to allosteric pockets distinct from the enzyme active site. In 1996, the anti-HIV compound nevirapine (Viramune®) became the first non-nucleoside polymerase inhibitor to receive FDA approval. Since then, four more non-nucleoside polymerase inhibitors have been approved for HIV-1 treatment: delavirdine mesylate (Rescriptor®), efavirenz (Sustiva®), etravirine (Intelence®) and rilpivirine hydrochloride (Edurant®) (Sluis-Cremer, 2014). Dasabuvir (Exviera®) is currently the only non-nucleoside polymerase inhibitor approved for the treatment of HCV infection.
1.5.2. Protease inhibitors
With 17 approved NMEs, protease inhibitors represent the second most prevalent class of antivirals after polymerase inhibitors. Protease inhibitors block an essential maturation step in polyprotein processing that is common to many viruses and involve viral proteases. Ten HIV-1 protease inhibitors have been commercialized: saquinavir mesylate (Invirase®), indinavir sulfate (Crixivan®), ritonavir (Norvir®), nelfinavir mesylate (Viracept®), amprenavir (Agenerase®), fosamprenavir calcium (Lexiva®), lopinavir (Kaletra®), atazanavir (Reyataz®), tipranavir (Aptivus®), and darunavir (Prezista®) (Lv et al., 2015). The first HIV-1 protease inhibitor, saquinavir (Invirase®), resulting from peptidomimetic design, was approved in 1995. In combination with ritonavir boosting, more recently approved protease inhibitors such as atazanavir and darunavir aim to increase potency and bioavailability and reduce the potential side effects experienced with first-generation drugs of this class. Seven inhibitors targeting HCV protease have been approved and include boceprevir (Victrelis®), grazoprevir (Zepatier®), paritaprevir (Viekira Pak®), simeprevir (Olysio®), telaprevir (Incivek®), voxilaprevir (Vosevi®), and glecaprevir (Mavyret®) (Fig. 1). The first-generation inhibitors such as boceprevir and telaprevir, both approved in 2011, had to be prescribed alongside the pegylated interferons and ribavirin. More potent and better-tolerated protease inhibitors were later approved in combination with an all-oral interferon-free regimen, with those acting on all genotypes becoming best-in-class and most widely used (McCauley and Rudd, 2016).
1.5.3. Integrase inhibitors
Integrase inhibitors represent the third major class of HIV-1 therapeutics. Integrase inhibitors block the integration of HIV genome by the viral integrase into human chromosomal DNA. Three HIV-1 integrase inhibitors are currently approved: raltegravir (Isentress®), elvitegravir (Vitekta®), and dolutegravir sodium (Tivicay®). Raltegravir and elvitegravir were approved in 2007 and 2012, respectively, and are first-generation integrase inhibitors with partially overlapping resistance mutation profiles (Fig. 1). Dolutegravir is a second-generation integrase inhibitor that displays a higher genetic barrier to resistance and retains antiviral potency against some but not all raltegravir/elvitegarvir-dominant escape mutations (Anstett et al., 2017).
1.5.4. NS5A inhibitors
Unlike the previously described viral drug targets for direct acting agents, the HCV non-structural protein NS5A has no enzymatic activity. NS5A is a dimeric membrane protein that interacts with viral RNA and other non-structural proteins, making it essential for HCV replication. Ledipasvir (Harvoni®) and daclatasvir dihydrochloride (Daklinza) were the first NS5A inhibitors to receive FDA approval in 2014/2015 (Fig. 1). They were soon followed by approvals of ombitasvir (Viekira Pak®), velpatasvir (Epclusa®), pibrentasvir (Mavyret®), and elbasvir (Zepatier®) in 2016 and 2017. All NS5A inhibitors share a similar NS5A binding site and exquisite in vitro antiviral potencies in the picomolar range, translating to impressive viral load reduction and cure rate in patients (Gao et al., 2016).
2. Forecast for 2018 and beyond
2.1. Changes in trends compared with approved drugs
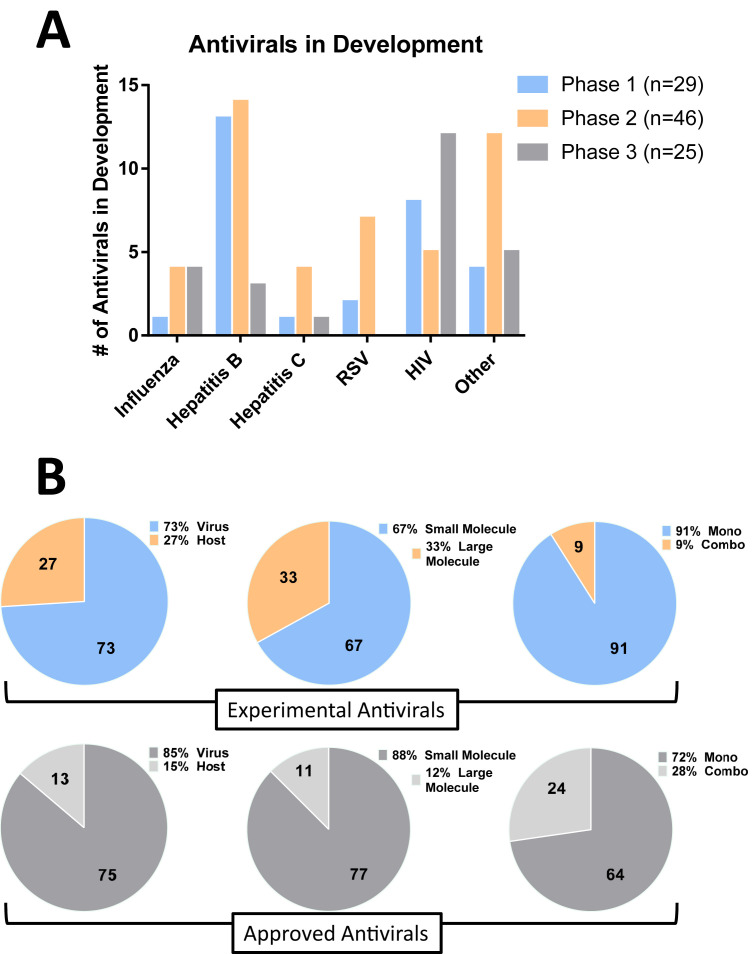
As of January 2018, a total of 100 active drug candidates are in active development spanning 29 Phase 1, 46 Phase 2, and 25 Phase 3 human clinical trials (Fig. 5 A). Of these clinical-stage drug candidates, 25 programs target HIV, 30 are for HBV, and 6 are for HCV (Table 2 ). An increase in focus toward respiratory infections is supported by 9 and 9 compounds under evaluation to treat influenza and RSV infections, respectively. Although virus-targeting agents continue to dominate the clinical landscape, the number of candidates with host-targeting mechanisms has increased significantly from 14% of approved antivirals to 27% of all antiviral clinical candidates (Fig. 5B). Similarly, small molecules continue to represent the major class of antiviral candidates, although a net increase in the number of biologics and oligonucleotide candidates has occurred relative to approved antiviral drugs. Finally, a large majority (∼91%) of antiviral clinical candidates are developed as monotherapeutic agents rather than combination therapies, which could be simply the result of the surge in new indications under evaluation (such as RSV, dengue, smallpox), new mechanisms of actions being exploited for intervention, and first-in-class molecules in development. In most of these cases, first-in-class therapies will have to be approved first as monotherapies before being combined with other agents.
Fig. 5.
Antivirals in clinical development. (A) Number drug candidates in Phase 1 (blue), 2 (orange), and 3 (grey) clinical trials per indication. (B) Number and proportion of virus-versus host-targeting agents, monotherapy versus combination therapy antiviral agents, and small versus large molecules. Experimental drugs are represented with colors, whereas approved antivirals are in grey. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Table 2.
Antiviral Drugs in Active Clinical Stage Development.
| Name | Indication | Phase | Type | Mono/Combo | Company | NCT or other references |
|---|---|---|---|---|---|---|
| ABI-H0731(CpAM) | HBV | 2 | Small Molecule | Mono | Assembly Biosciences | NCT03109730 |
| ARB-1467 | HBV | 2 | Oligonucleotide | Mono | Arbutus Biopharma | NCT02631096 |
| AB-423 | HBV | 1 | Small Molecule | Mono | Arbutus Biopharma | http://bit.ly/2GShPvO |
| ALN-HBV | HBV | 2 | Oligonucleotide | Mono | Alnylam Pharmaceuticals | NCT02826018 |
| Morphothiadine | HBV | 2 | Small Molecule | Mono | HEC Pharm | ChiCTR-IIR-16008284 |
| AL-034 | HBV | 1 | Small Molecule | Mono | Janssen Pharmaceuticals | NCT03285620 |
| RO6870868 | HBV | 2 | Small Molecule | Combo | Roche | NCT02391805 |
| Tenofovir Exalidex | HBV | 2 | Small Molecule | Mono | Contravir | NCT02710604 |
| Inarigavir (SB 9200) | HBV | 2 | Small Molecule | Combo | Spring Bank Pharmaceuticals | NCT02751996 |
| REP 2139 | HBV | 2 | Oligonucleotide | Mono | Replicor Inc. | NCT02233075 |
| REP 2165 | HBV | 2 | Oligonucleotide | Mono | Replicor Inc. | NCT02565719 |
| GSK-3389404 | HBV | 2 | Oligonucleotide | Mono | GlaxoSmithKline | NCT03020745 |
| GSK-3228836 | HBV | 2 | Oligonucleotide | Mono | GlaxoSmithKline | NCT02981602 |
| JNJ-379 | HBV | 1 | Small Molecule | Mono | Janssen Pharmaceuticals | NCT03361956 |
| RG-7907 | HBV | 1 | Small Molecule | Mono | Roche | NCT02952924 |
| GS-9688 | HBV | 1 | Small Molecule | Mono | Gilead Sciences | ACTRN12617000235303 |
| RG-6004 | HBV | 1 | Oligonucleotide | Mono | Roche | NCT03038113 |
| RG-7854 | HBV | 1 | Small Molecule | Mono | Roche | NCT02956850 |
| INO-9112 | HBV | 1 | Small Molecule | Mono | Roche/Inovio | NCT02431312 |
| GS-5801 | HBV | 1 | Small Molecule | Mono | Gilead Sciences | ACTRN12616001260415 |
| Myrcludex B | HBV | 2 | Peptide | Mono | MYR Pharma | NCT02637999 |
| EYP-001 | HBV | 1 | Small Molecule | Mono | Enyo Pharma | NCT03272009 |
| GC1102 | HBV | 2 | Protein | Mono | Green Cross | NCT02304315 |
| Hepalatide (L47) | HBV | 1 | Peptide | Mono | Shanghai HEP Pharmaceuticals | NCT02612506 |
| Besifovir | HBV | 3 | Small Molecule | Mono | Il-Dong | NCT02792088 |
| Tenofovir disoproxil orotate | HBV | 3 | Small Molecule | 816. Mono | 817. Dong-A ST | 818. NCT02967939 |
| Tenofovir disoproxil aspartate | HBV | 3 | Small Molecule | Mono | Chong Kun Dang Pharmaceutical Corp. | NCT02805738 |
| QL-007 | HBV | 1 | Small Molecule | Mono | Qliu Pharmaceuticals | NCT03244085 |
| APG-1387 | HBV | 1 | Small Molecule | Mono | Ascentage Pharma | NCT03386526 |
| AT-527 | HCV | 1 | Small Molecule | Mono | Atea Pharmaceuticals | NCT03219957 |
| Faldaprevir | HCV | 3 | Small Molecule | Mono | Trek Therapeutics/Boehringer Ingelheim | NCT02716428 |
| VX-222 | HCV | 2 | Small Molecule | Mono | Trek Therapeutics/Vertex | NCT01516918 |
| VX-497 | HCV | 2 | Small Molecule | Mono | Trek Therapeutics/Vertex | NCT00088504 |
| Ravidasvir | HCV | 2 | Small Molecule | Mono | Presidio | NCT02961426 |
| TD-6450 | HCV | 2 | Small Molecule | Mono | Trek Therapeutics/Theravance | NCT02716428 |
| ABX464 | HIV | 2 | Small Molecule | Mono | Abivax | NCT02990325 |
| Bictegravir/F/TAF (non-boosted integrase inhibitor/emtricitabine/tenofovir alafenamide) (Biktarvy®) | HIV | 3 | Small Molecule | Combo | Gilead Sciences | NCT02603107 |
| LA cabotegravir | HIV | 3 | Small Molecule | Mono | ViiV Healthcare | NCT02478463 |
| LA cabotegravir + LA rilpivirine | HIV | 3 | Small Molecule | Combo | Janssen/ViiV Healthcare | NCT02951052 |
| Darunavir STR darunavir/cobicistat/emtricitabine/tenofovir alafenamide (Symtuza®) | HIV | 3 | Small Molecule | Combo | Janssen Pharmaceuticals | NCT02578550 |
| dolutegravir + lamivudine | HIV | 3 | Small Molecule | Combo | ViiV Healthcare | NCT02211482 |
| Doravirine | HIV | 3 | Small Molecule | Mono | Merck | NCT02275780 |
| Doravirine/lamivudine/tenofovir disoproxil fumarate | HIV | 3 | Small Molecule | Combo | Merck | NCT03332095 |
| Elsulfavirine | HIV | 3 | Small Molecule | Mono | Viriom | NCT02489461 |
| Fostemsavir | HIV | 3 | Small Molecule | Mono | ViiV Healthcare | NCT01384734 |
| Ibalizumab | HIV | 3 | Protein | Mono | US TaliMed Biologics | NCT02707861 |
| PRO 140 | HIV | 3 | Protein | Mono | CytoDyn | NCT02483078 |
| BIT-225 | HIV | 2 | Small Molecule | Mono | Biotron | ACTRN12613001296729 |
| SB-728-T | HIV | 2 | Gene Therapy | Mono | Sangamo Therapeutics | NCT01543152 |
| UB-421 | HIV | 3 | Protein | Mono | United Biopharma | NCT03045861 |
| MK8591 | HIV | 1 | Small Molecule | Mono | Merck | NCT02369146 |
| ALT-803 | HIV | 1 | Protein | Mono | Altor BioScience | NCT03272347 |
| Vesatolimod (GS-9620) | HIV | 1 | Small Molecule | Mono | Gilead Sciences | NCT02191098 |
| TMB-607 | HIV | 1 | Small Molecule | Mono | TaiMed Biologics | NCT02858401 |
| VRC01LS | HIV | 1 | Protein | Mono | Xencor/NIH | NCT03110549 |
| CAL-1 | HIV | 2 | Gene Therapy | Mono | CalImmune | NCT02797171 |
| GS-9722 | HIV | 1 | Protein | Mono | Gilead Sciences | NCT02390297 |
| MK-4250 | HIV | 1 | Small Molecule | Mono | Merck | |
| PGT-121 | HIV | 1 | Protein | Mono | Theraclone Sciences | NCT03351699 |
| Baloxavir marboxil (Xofluza®) | Influenza | 3 | Small Molecule | Mono | Roche (Shionogi) | NCT02954354 |
| VIS-410 | Influenza | 3 | Protein | Mono | Visterra | NCT03040141 |
| MEDI-8852 | Influenza | 2 | Protein | Mono | AstraZeneca | NCT02603952 |
| Pimodivir (JNJ-872) | Influenza | 3 | Small Molecule | Mono | Janssen Pharmaceuticals | NCT03376321 |
| JNJ-5806 | Influenza | 2 | Small Molecule | Mono | Janssen Pharmaceuticals | NCT03411421 |
| NT-300 | Influenza | 3 | Small Molecule | Mono | Romark Laboratories | NCT03336619 |
| FluDase | Influenza | 2 | Protein | Mono | Ansun Biopharma | NCT01113034 |
| Laninamivir Octanoate | Influenza | 2 | Small Molecule | Mono | Aviragen | NCT02014649 |
| Radavirsen | Influenza | 1 | Oligonucleotide | Mono | Sarepta Therapeutics | NCT01747148 |
| RV-521 | RSV | 2 | Small Molecule | Mono | ReViral | NCT03258502 |
| Presatovir (GS-5806) | RSV | 2 | Small Molecule | Mono | Gilead Sciences | NCT02534350 |
| Lumicitabine (ALS-8176) | RSV | 2 | Small Molecule | Mono | Janssen Pharmaceuticals | NCT02935673 |
| ALX-0171 | RSV | 2 | Protein | Mono | Ablynx | NCT02979431 |
| AK0529 | RSV | 2 | Small Molecule | Mono | Ark Biosciences | NCT03400995 |
| JNJ-678 | RSV | 2 | Small Molecule | Mono | Janssen Pharmaceuticals | NCT02593851 |
| MEDI8897 | RSV | 2 | Protein | Mono | AstraZeneca | NCT02878330 |
| PC-786 | RSV | 1 | Small Molecule | Mono | Pulmocide | NCT03382431 |
| EDP-938 | RSV | 1 | Small Molecule | Mono | Enanta Pharmaceuticals | NCT03384823 |
| GS-5734 | Ebola Virus | 2 | Small Molecule | Mono | Gilead Sciences | NCT02818582 |
| BTA074 | HPV | 2 | Small Molecule | Mono | Aviragen Therapeutics | NCT01532102 |
| Pritelivir | HSV | 2 | Small Molecule | Mono | AiCuris | NCT03073967 |
| Ranpirnase | HPV | 2 | Small Molecule | Mono | Tamir Biotechnology | NCT02535104 |
| DAS181 | Para-influenza/Influenza Virus | 3 | Protein | Mono | Ansun Biopharma | NCT01644877 |
| ATA 129 | Epstein-Barr Virus | 2 | Cell Therapy | Mono | Atara Biotherapeutics | NCT03392142 |
| Tecovirimat | Smallpox (Variola Virus) | 3 | Small Molecule | Mono | SIGA | NCT02080767 |
| Modipafant | Dengue Virus | 2 | Small Molecule | Mono | 60 Degrees Pharmaceuticals | NCT02569827 |
| Celgosivir | Dengue Virus | 2 | Small Molecule | Mono | 60 Degrees Pharmaceuticals | NCT02569827 |
| Maribavir (SHP-620) | CMV | 3 | Small Molecule | Mono | Shire Pharmaceuticals | NCT02931539 |
| Cyclopropavir (MBX-400) | CMV | 1 | Small Molecule | Mono | Microbiotix Inc. | NCT02454699 |
| SHP-640 | Adenoviral Conjunctivi-tis | 3 | Small Molecule | Combo | Shire Pharmaceuticals | NCT02998554 |
| Brincidofovir | Adenovirus/Smallpox (Variola Virus)/CMV | 2/3 | Small Molecule | Mono | Chimerix | NCT02596997 |
| Viralym M | CMV, AdV, BKV, EBV HHV-6 | 2 | Cell Therapy | Mono | ViraCyte | NCT02765802 |
| Viralym C | CMV | 1 | Cell Therapy | Mono | ViraCyte | NCT02313857 |
| Lonafarnib | HDV | 2 | Small Molecule | Mono | Eiger Biopharma | NCT02527707 |
| Pegylated-interferon-lambda (PEG-IFN-λ) | HDV | 2 | Protein | Mono | Eiger Biopharma | NCT02765802 |
| SB206 | HPV | 2 | Small Molecule | Mono | Novan Therapeutics | NCT03436615 |
| VP-102 | HPV | 2 | Small Molecule | Mono | Verrica Pharmaceuticals | NCT03377803 |
| SAB-301 | Corona-virus | 1 | Protein | Mono | SAb Biotherapeutics | NCT02788188 |
| ZMapp | Ebola Virus | 1 | Protein | Mono | Mapp Biopharma | NCT02389192 |
Viruses.
HIV-1= Human immunodeficiency virus-1.
HCV= Hepatitis C virus.
HBV= Hepatitis B virus.
HDV= Hepatitis D virus.
CMV= Cytamegalovirus.
HSV= Herpes simplex virus.
HPV= Human papillomavirus.
AdV = Adenovirus.
BKV= BK virus.
EBV = Epstein-Barr virus.
HHV-6= Human herpesvirus-6.
Other abbreviations.
Mono = Monotherapy.
Combo = Combination therapy.
2.2. The radical evolution of future HIV therapeutics
Adherence remains a problem for combination antiretroviral therapies requiring life-long daily oral medications. Lack of adherence can result in suboptimal drug exposure and development of viral mutations associated with drug resistance. To address these limitations, there are now three injectable long-acting antiretrovirals under clinical development as alternatives to daily oral regimens (Jacobson and Flexner, 2017; Margolis and Boffito, 2015). In addition, MK8591 (EfdA) is a clinical-stage nucleoside reverse transcriptase inhibitor (NRTI) with extremely long half-life compatible with weekly oral or even monthly parenteral dosing. Reformulation of Rilpivirine and Cabotegravir to intramuscular nanoparticle delivery also provides pharmacokinetic coverage allowing long-acting weekly injections (Table 2).
Another significant evolution in HIV therapeutics is the intense effort towards evaluation of entry inhibitors. Fostemsavir is a small molecule that blocks gp120 attachment to CD4 T-cells. Broadly neutralizing monoclonal antibodies are also currently being considered as entry inhibitors (Caskey et al., 2016). These experimental drugs include ibalizumab, PRO 140, UB-421, PGT-121, GS-9722, and VRC01LS, which share a similar mechanism consisting in preventing virus attachment to CD4 receptor. Although the utility of these novel antivirals remains to be fully defined, broadly neutralizing antibody could provide an alternative to current oral treatments and also may open the door to long-acting regimen because of their extended half-lives.
Gene therapies are also being evaluated in the clinic as new generations of HIV therapeutics. CAL-1 is a dual therapeutic lentiviral vector that downregulates CCR5 expression of transduced cells via RNA interference (RNAi) and also targets X4-tropic HIV-1, with the goal to control HIV infection after a single treatment (Burke et al., 2015). SB-728-T uses a zinc-finger based nuclease approach to edit the CCR5 gene and alter the corresponding receptor, making corresponding autologous CD4 T-cells resistant to HIV infection (Tebas et al., 2014) (Table 2).
2.3. Second-generation HBV therapeutics
Multiple novel therapeutic approaches are being evaluated in an effort to find more effective therapies for the management or cure of chronic hepatitis B. These include, for example, hepatitis B surface antigen (HBsAg) blockers such as the neutralizing HBV human immunoglobulin GC1102, and the peptide Hepalatide. In addition, REP 2139 is a phosphorothioated oligonucleotide targeting HBsAg release (Table 2) (Fung et al., 2016). Silencing oligonucleotides that target HBV mRNA such as ARB-1467, GSK3389404, GSK-3228836, and RG6004 are also progressing into Phase 2 proof-of-concept studies. One clinical program focuses on targeting the host-based protein bile acids regulating farnesoid X receptor (FXR) with EYP001, a synthetic FXR agonist.
Capsid assembly modulators (CAMs) represent a major class of novel HBV inhibitors. CAMs currently in clinical trial evaluation are JNJ379, RG7907, AB-423, and ABI-H0731 (Table 2). The viral capsid is formed by the core protein that has multiple functions in HBV replication. CAMs accelerate the kinetics of core oligomerization and prevent encapsidation of the polymerase-pregenomic RNA, resulting in a genome-free capsid and reduction of covalently closed circular DNA (cccDNA) (Berke et al., 2017). This dual mode of action is believed to differentiate from previously approved nucleoside analogs and may be key to achieving higher functional cure rates when given alone or in combination with current standard of care.
Chronic HBV infection often results in weak or absent virus-specific T-cell reactivity, a phenomenon now better understood and referred to as T-cell exhaustion (Ye et al., 2015). Immunotherapies provide a novel approach to counteract T-cell exhaustion and enhance clearance of HBV-infected cells. Iniragivir (SB 9200) is a dinucleotide in Phase 2 clinical trials that is claimed to induce interferon signaling pathways by binding to the cellular proteins retinoic acid-inducible gene 1 (RIG-I) and nucleotide-binding oligomerization domain-containing protein 2 (NOD2) (Table 2). Since TLR 7 stimulation also mediates type I interferon signaling, TLR7 agonists AL-034, GS-9688, RG7854, and RO6870868 (RG 7863) are currently being evaluated for the treatment of chronic HBV infection.
2.4. Emergence of drugs against respiratory infections
The need for new therapeutic options against influenza virus remains high despite existing vaccines and antivirals. Novel polymerase inhibitors are currently in late-stage clinical development. The nucleoside analog Favipiravir (T-705, AVIGAN®) has been approved in Japan for the treatment of influenza infection limited to cases in which other anti-flu drug are ineffective. There is to our knowledge no indication that favipiravir is currently being developed in the United States or elsewhere. Baloxavir marboxil and pimodivir, both in Phase 3 studies in the United States as of January 2018, target the polymerase acidic (PA) and polymerase basic 2 (PB2) subunit of influenza virus polymerase, respectively (Table 2). Both compounds prevent the virus from hijacking the host capped mRNA and block transcription of viral genes.
The emergence of RSV inhibitors in the clinical pipeline is justified by years of unsuccessful vaccine attempts, combined with a high medical need unaddressed by palivizumab prophylactic treatment in high-risk infants. Currently, three classes of RSV inhibitors are in clinical development. Second-generation monoclonal antibodies represent the first class of RSV inhibitors. MEDI8897, a recombinant monoclonal antibody with a modified Fc region that extends its half-life, is being developed for RSV prophylaxis for all infants (Griffin et al., 2017). ALX-0171 is a trivalent nanobody that targets the RSV Fusion (F) protein for delivery via inhalation (Detalle et al., 2015). Fusion inhibitors, the second class of novel RSV inhibitors, block an essential conformational change of the RSV F protein, thereby inhibiting cell entry by preventing fusion between the virus envelope and the host-cell membrane (Roymans et al., 2017). Current fusion inhibitors include JNJ-678, presatovir (GS-5806), AK0529, and RV521 (Table 2). Replication inhibitors represent the third class of RSV drug candidates. Lumicitabine and PC-786 bind to the polymerase L subunit (Deval et al., 2015; Coates et al., 2017), whereas EDP-938 interferes with the nucleoprotein N. Lumicitabine is currently the only RSV replication inhibitor with demonstrated clinical proof-of-concept efficacy (DeVincenzo et al., 2015).
2.5. Experimental treatments for other acute viral infections
2.5.1. Ebola
The recent Ebola virus outbreak in West Africa during 2013–2016 triggered intense efforts to identify novel inhibitors for filoviruses. BCX4430 and favipiravir, two nucleoside analog with very broad spectrum activity once considered for treatment of Ebola virus disease, are no longer under clinical development (Sissoko et al., 2016). ZMapp is a combination of 3 humanized antibodies produced in genetically-modified tobacco plants and target 3 Ebola glycoprotein epitopes. ZMapp was tested in the clinic during the West Africa Ebola outbreak. Although ZMapp seemed to be beneficial, the results did not meet statistical significance for efficacy (Group et al., 2016). The new research and development efforts also resulted in the identification of GS-5734, a nucleotide analog polymerase inhibitor with broad antiviral spectrum activity (Warren et al., 2016). Following Phase 1 safety studies, GS-5734 was first given to two patients, one in the United Kingdom in October 2015 and one in Guinea the following month, through a compassionate use request (Jacobs et al., 2016; Dornemann et al., 2017). The current Phase 2 study aims to evaluate the antiviral efficacy of 5 days of GS-5734 given intravenously to male Ebola virus disease survivors shedding Ebola virus in their semen (Table 2).
2.5.2. Dengue
Currently no drugs are approved for the treatment of dengue virus infection. Modipafant and celgosivir are currently in Phase 2 clinical trials for the treatment of adults with dengue infection presenting within 48 h of fever onset. Modipavant is an antagonist of activation the of platelet-activating factor receptor (PAFR), a host protein believed to be implicated in the pathogenesis of severe dengue infection through inflammation. Celgosivir is derived from a natural product and is also a host-targeting agent that inhibits alpha-glucosidase I, which is needed for the folding of viral glycoproteins. These two compounds were selected for clinical development because their safety has previously been demonstrated in humans and because they inhibit dengue virus replication in vitro and improve survival in a lethal mouse efficacy model (Souza et al., 2009; Rathore et al., 2011).
2.5.3. Smallpox (variola virus)
The development of smallpox inhibitors has been rationalized by the need to stockpile agents aimed to contain potential future biothreats. Brincidofovir is a lipid-conjugated prodrug of cidofovir, an acyclic nucleoside analog with broad antiviral spectrum against DNA and RNA viruses. Brincidofovir is currently in clinical evaluation for the treatment of smallpox infection for biodefense applications, and in Phase 2 for the treatment of adenovirus in pediatric stem cell transplant recipients. Brincidofovir is being developed for smallpox under the FDA's Animal Rule, which allows for testing of investigational drugs in animal models to support effectiveness in diseases that are not ethical or feasible to study in humans. Tecovirimat is also being developed for smallpox under the Animal Rule for smallpox biodefense applications. Tecovirimat was identified via a high-throughput screen of a small molecule chemical library and has been shown to protect nonhuman primates from smallpox infection (Mucker et al., 2013). Tecovirimat inhibits p37, a viral protein involved as virulence factor in the formation of enveloped virions.
3. Driving forces for innovation in antiviral research
Although the discovery of each antiviral drug has a unique story and distinct circumstances that may not apply to other programs, this section aims to identify guidelines or examples of attributes that drive success in identifying and developing antiviral drugs.
3.1. Biological breakthroughs: first-in-class
Breakthroughs in basic biological and biochemical science can lead to the acceleration of antiviral research and provide a springboard to drug discovery applications. A striking example is the establishment of a robust cell culture surrogate system for HCV replication. Although HCV was first isolated and identified in 1989, attempts to grow the virus in cell culture were unsuccessful and greatly limited the ability to evaluate novel antiviral therapies. Ten years of research were needed to develop a subgenomic replicon system that captured the functionality of the non-structural proteins and recapitulated the intracellular steps of viral genomic replication (for review: (Kaul et al., 2009)). Because the HCV replicon was used extensively as a primary screen for antiviral testing, establishing this cell culture system was key to the discovery of all current HCV direct acting agents. This is particularly true in cases where biochemical or structural biology tools were not available to assist medicinal chemistry efforts. The discovery of daclatasvir, the first approved HCV NS5A inhibitor, resulted from a high-throughput screen using the HCV replicon assay (Belema and Meanwell, 2014).
Targeted phenotypic screens have become major contributors to the understanding of novel mechanisms of inhibition leading to differentiated antiviral programs. The flu inhibitor pimodivir was identified using a phenotypic screen under conditions of high multiplicity of infection (MOI) in which oseltamivir is not active. This targeted screen approach was key to differentiating novel PB2 inhibitors, largely MOI independent, from other classes of anti-flu agents that prevent virus replication only at the early stage of infection (Byrn et al., 2015). Fluorescence microscopy has also been used in conjunction with high-throughput screening to identify phenotypic changes associated with antiviral effects. Nucleozin, a preclinical first-in-class influenza inhibitor, was first characterized by its ability to block the nuclear accumulation of nucleoprotein in infected cells (Kao et al., 2010). Considering the growing use of high-content imaging for antiviral testing (Mudhasani et al., 2015; Watterson et al., 2016), it is likely that targeted phenotypic screens with early access to mechanism of action information will have an increasingly important role in antiviral drug discovery. These examples also show that, in many cases, the discovery of first-in-class antiviral drugs has its roots in biological innovations and ingenious use of novel in vitro assays.
3.2. Chemical innovation: best-in-class
The analysis of all antiviral drug approvals over the last 30 years reveals many examples of best-in-class programs that follow approved drugs or more advanced clinical candidates. As we detailed earlier in this review (e.g., polymerase and protease inhibitors), second- or third-generation HIV and HCV small molecule therapeutics have led to best-in-class drug approvals, providing the foundations for current standards of care. In these cases, research programs tend to leverage the biological advances made with first-in-class prototype molecules, and focus on chemical innovation through follow-on or back-up approaches (Schulze and Ringel, 2013). Different strategies have been used to foster best-in-class innovation for small molecules, sometimes relying on competitive intelligence (i.e., “patent busting”). In all cases, best-in-class “fast-follower” antiviral programs result from intensified medicinal chemistry efforts aimed at addressing the shortcomings of the first-generation drugs: intrinsic binding or inhibition potency, strain/genotype/resistance mutation potency coverage, safety, or convenience. For example, the anti-HCV drug sofosbuvir is a monophosphate nucleoside prodrug as a follow-on to the first-generation molecule mericitabine. Sofosbuvir was designed to improve metabolic activation leading to the higher liver triphosphate formation by evading the first and limiting kinase phosphorylation step (Murakami et al., 2008). Similarly, the HIV-1 drug etravirine was designed to overcome suboptimal potency and drug resistance mutations associated with first-generation non-nucleoside reverse transcriptase inhibitors (Das et al., 2004). In the latter case, X-ray crystallography of the reverse transcriptase target provided valuable information for a structure-based drug design approach. Fragment screening and expansion campaigns have also contributed to the discovery of novel chemical starting points aimed at identifying next-generation antivirals. For example, crystallographic fragment screening of HIV integrase binders recently led to the discovery of novel allosteric inhibitors for the protein target (Patel et al., 2016). More generally, structural biology has proven to be a valuable tool in antiviral research to optimize ligand efficiency and therefore improve potency of inhibitors interacting with well-defined molecular targets.
3.3. Clinical innovation
One of the main challenges in the development of antiviral medicines targeting acute viral infections is the limited time window for therapeutic intervention, which may greatly fluctuate depending on the virus, patient population, and mode of action of the drug candidate. This is particularly problematic for first-in-class drug candidates targeting novel and therefore clinically unproven targets or pathways. This enormous obstacle to antiviral development has been partly addressed with the introduction of human challenge studies, now commonly used in early RSV and influenza clinical programs to obtain first proof-of-concept efficacy in healthy volunteers and to help design subsequent clinical trials in naturally infected patients (Bagga et al., 2013). Healthy adult volunteers are typically infected with low quantities of virus inoculum under controlled conditions resulting in mild symptoms. Human challenge studies were critical to the clinical development of first-in-class RSV fusion and polymerase inhibitors presatovir and lumicitabine, respectively (DeVincenzo et al., 2014; DeVincenzo et al., 2015).
Another clinical innovation in antiviral research is the increasing use of combination therapies for HIV-1 and HCV therapeutics (Fig. 3B). This was made possible by the availability of single agents with non-overlapping mechanisms of actions and additive or synergistic potential, with a gradual evolution toward best-in-class combinations. Single-tablet regimens using combination therapies represent another major clinical innovation aiming to increase efficacy and adherence to long-term HIV-1 treatment regimens. In comparison with therapies requiring two or more pills per day, once-daily single-tablet regimens were associated with greater adherence, fewer hospitalizations, and lower overall health care costs (Cohen et al., 2013). Considering the recent surge in first-in-class HBV drug candidates with novel mechanisms of action, evaluation of these drug candidates as potential combination treatments should be expected. Likewise, it will be exciting to consider novel combination treatments for respiratory viruses given the recent advances in novel monotherapies targeting influenza and RSV. In a Phase 2b study, pimodivir combined with oseltamivir demonstrated a significant reduction in viral load in adults with influenza A (https://www.jnj.com/media-center/press-releases/pimodivir-alone-or-in-combination-with-oseltamivir-demonstrated-a-significant-reduction-in-viral-load-in-adults-with-influenza-a).
Finally, the establishment of national programs or organizations such as the National Institute of Allergy and Infectious Diseases (NIAID) have been instrumental to systematically and more efficiently recruit eligible patients for new experimental treatments.
4. Conclusions and perspective
In summary, the analysis of the last 30 years of 88 antiviral drug approvals in the United States demonstrates that a majority of them target chronic infections caused by HIV-1, HBV, HCV, and herpesviruses (HSV and CMV). Only a few drugs were approved to treat acute infections, mainly influenza. A large majority of the approvals were for small molecules and virus-targeting agents over large molecules and host-targeting therapies. The high rate of combination therapy approvals during the last five years is attributed to the rich HIV-1 and HCV drug pipelines that are now reaching maturation with multiple therapeutic options and competing best-in-class molecules. In contrast, 91% of molecules currently in clinical development are under evaluation as monotherapies because they are first-in-class experimental therapies for indications lacking other therapeutic options (Fig. 5B). The current experimental antiviral clinical pipeline also reflects, at least partially, a departure from classical targets (polymerase, protease…) with oligonucleotide-based therapeutics, cell fusion inhibitors, capsid-assembly modulators, and an array of novel host-based mechanisms. In addition, we observe a surge in anti-HIV broadly neutralizing monoclonal antibodies reaching clinical stage evaluation.
The current antiviral clinical pipeline is constantly evolving with new candidates entering development and other clinical programs being terminated. During preparation of this manuscript, the US FDA approved Biktarvy® (bictegravir, emtricitabine, tenofovir alafenamide) on 7 February 2018 for the treatment of HIV-1 infection; on 23 February 2018, Xofluza® (baloxavir marboxil) received Japanese regulatory approval for use against influenza infection. On 6 March 2018, the FDA approved the anti-CD4 monoclonal antibody Trogarzo® (ibalizumab) for heavily treatment-experienced adult HIV patients at risk of failing other antiretroviral therapies.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
Janssen Research & Development provided support in the form of salaries for all authors but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
We thank Amy Fung, John Fry, Francisco Talamas, and Peggy Korn for their insightful comments and editorial input.
References
- Anstett K., Brenner B., Mesplede T., Wainberg M.A. HIV drug resistance against strand transfer integrase inhibitors. Retrovirology. 2017;14:36. doi: 10.1186/s12977-017-0360-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagga B., Woods C.W., Veldman T.H., Gilbert A., Mann A., Balaratnam G., Lambkin-Williams R., Oxford J.S., McClain M.T., Wilkinson T., Nicholson B.P., Ginsburg G.S., Devincenzo J.P. Comparing influenza and RSV viral and disease dynamics in experimentally infected adults predicts clinical effectiveness of RSV antivirals. Antivir. Ther. 2013;18:785–791. doi: 10.3851/IMP2629. [DOI] [PubMed] [Google Scholar]
- Belema M., Meanwell N.A. Discovery of daclatasvir, a pan-genotypic hepatitis C virus NS5A replication complex inhibitor with potent clinical effect. J. Med. Chem. 2014;57:5057–5071. doi: 10.1021/jm500335h. [DOI] [PubMed] [Google Scholar]
- Berke J.M., Dehertogh P., Vergauwen K., Van Damme E., Mostmans W., Vandyck K., Pauwels F. Capsid assembly modulators have a dual mechanism of action in primary human hepatocytes infected with hepatitis B virus. Antimicrob. Agents Chemother. 2017;61(8) doi: 10.1128/AAC.00560-17. e00560–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke B.P., Levin B.R., Zhang J., Sahakyan A., Boyer J., Carroll M.V., Colon J.C., Keech N., Rezek V., Bristol G., Eggers E., Cortado R., Boyd M.P., Impey H., Shimizu S., Lowe E.L., Ringpis G.E., Kim S.G., Vatakis D.N., Breton L.R., Bartlett J.S., Chen I.S., Kitchen S.G., An D.S., Symonds G.P. Engineering cellular resistance to HIV-1 infection in vivo using a dual therapeutic lentiviral vector. Molecular therapy. Nucleic Acids. 2015;4:e236. doi: 10.1038/mtna.2015.10. [DOI] [PubMed] [Google Scholar]
- Byrn R.A., Jones S.M., Bennett H.B., Bral C., Clark M.P., Jacobs M.D., Kwong A.D., Ledeboer M.W., Leeman J.R., McNeil C.F., Murcko M.A., Nezami A., Perola E., Rijnbrand R., Saxena K., Tsai A.W., Zhou Y., Charifson P.S. Preclinical activity of VX-787, a first-in-class, orally bioavailable inhibitor of the influenza virus polymerase PB2 subunit. Antimicrob. Agents Chemother. 2015;59:1569–1582. doi: 10.1128/AAC.04623-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caskey M., Klein F., Nussenzweig M.C. Broadly neutralizing antibodies for HIV-1 prevention or immunotherapy. N. Engl. J. Med. 2016;375:2019–2021. doi: 10.1056/NEJMp1613362. [DOI] [PubMed] [Google Scholar]
- Coates M., Brookes D., Kim Y.I., Allen H., Fordyce E.A.F., Meals E.A., Colley T., Ciana C.L., Parra G.F., Sherbukhin V., Stockwell J.A., Thomas J.C., Hunt S.F., Anderson-Dring L., Onions S.T., Cass L., Murray P.J., Ito K., Strong P., DeVincenzo J.P., Rapeport G. Preclinical characterization of PC786, an inhaled small-molecule respiratory syncytial virus L protein polymerase inhibitor. Antimicrob. Agents Chemother. 2017;61 doi: 10.1128/AAC.00737-17. e00737–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen C.J., Meyers J.L., Davis K.L. Association between daily antiretroviral pill burden and treatment adherence, hospitalisation risk, and other healthcare utilisation and costs in a US medicaid population with HIV. BMJ Open. 2013;3(8) doi: 10.1136/bmjopen-2013-003028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das K., Clark A.D., Jr., Lewi P.J., Heeres J., De Jonge M.R., Koymans L.M., Vinkers H.M., Daeyaert F., Ludovici D.W., Kukla M.J., De Corte B., Kavash R.W., Ho C.Y., Ye H., Lichtenstein M.A., Andries K., Pauwels R., De Bethune M.P., Boyer P.L., Clark P., Hughes S.H., Janssen P.A., Arnold E. Roles of conformational and positional adaptability in structure-based design of TMC125-R165335 (etravirine) and related non-nucleoside reverse transcriptase inhibitors that are highly potent and effective against wild-type and drug-resistant HIV-1 variants. J. Med. Chem. 2004;47:2550–2560. doi: 10.1021/jm030558s. [DOI] [PubMed] [Google Scholar]
- Detalle L., Stohr T., Palomo C., Piedra P.A., Gilbert B.E., Mas V., Millar A., Power U.F., Stortelers C., Allosery K., Melero J.A., Depla E. Generation and characterization of ALX-0171, a potent novel therapeutic nanobody for the treatment of respiratory syncytial virus infection. Antimicrob. Agents Chemother. 2015;60:6–13. doi: 10.1128/AAC.01802-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deval J., Hong J., Wang G., Taylor J., Smith L.K., Fung A., Stevens S.K., Liu H., Jin Z., Dyatkina N., Prhavc M., Stoycheva A.D., Serebryany V., Liu J., Smith D.B., Tam Y., Zhang Q., Moore M.L., Fearns R., Chanda S.M., Blatt L.M., Symons J.A., Beigelman L. Molecular basis for the selective inhibition of respiratory syncytial virus RNA polymerase by 2'-fluoro-4'-chloromethyl-cytidine triphosphate. PLoS Pathog. 2015;11 doi: 10.1371/journal.ppat.1004995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVincenzo J.P., McClure M.W., Symons J.A., Fathi H., Westland C., Chanda S., Lambkin-Williams R., Smith P., Zhang Q., Beigelman L., Blatt L.M., Fry J. Activity of oral ALS-008176 in a respiratory syncytial virus challenge study. N. Engl. J. Med. 2015;373:2048–2058. doi: 10.1056/NEJMoa1413275. [DOI] [PubMed] [Google Scholar]
- DeVincenzo J.P., Whitley R.J., Mackman R.L., Scaglioni-Weinlich C., Harrison L., Farrell E., McBride S., Lambkin-Williams R., Jordan R., Xin Y., Ramanathan S., O'Riordan T., Lewis S.A., Li X., Toback S.L., Lin S.L., Chien J.W. Oral GS-5806 activity in a respiratory syncytial virus challenge study. N. Engl. J. Med. 2014;371:711–722. doi: 10.1056/NEJMoa1401184. [DOI] [PubMed] [Google Scholar]
- Dornemann J., Burzio C., Ronsse A., Sprecher A., De Clerck H., Van Herp M., Kolie M.C., Yosifiva V., Caluwaerts S., McElroy A.K., Antierens A. First newborn baby to receive experimental therapies survives Ebola virus disease. J. Infect. Dis. 2017;215:171–174. doi: 10.1093/infdis/jiw493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung J., Lai C.L., Seto W.K., Yuen M.F. Emerging drugs for the treatment of hepatitis B. Expert Opin. Emerg. drugs. 2016;21:183–193. doi: 10.1517/14728214.2016.1162155. [DOI] [PubMed] [Google Scholar]
- Gao M., O'Boyle D.R., 2nd, Roberts S. HCV NS5A replication complex inhibitors. Curr. Opin. Pharmacol. 2016;30:151–157. doi: 10.1016/j.coph.2016.07.014. [DOI] [PubMed] [Google Scholar]
- Griffin M.P., Khan A.A., Esser M.T., Jensen K., Takas T., Kankam M.K., Villafana T., Dubovsky F. Safety, tolerability, and pharmacokinetics of MEDI8897, the respiratory syncytial virus prefusion F-Targeting monoclonal antibody with an extended half-life, in healthy adults. Antimicrob. Agents Chemother. 2017;61 doi: 10.1128/AAC.01714-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group P.I.W., Multi-National P.I.I.S.T., Davey R.T., Jr., Dodd L., Proschan M.A., Neaton J., Neuhaus Nordwall J., Koopmeiners J.S., Beigel J., Tierney J., Lane H.C., Fauci A.S., Massaquoi M.B.F., Sahr F., Malvy D. A randomized, controlled trial of ZMapp for Ebola virus infection. N. Engl. J. Med. 2016;375:1448–1456. doi: 10.1056/NEJMoa1604330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs M., Rodger A., Bell D.J., Bhagani S., Cropley I., Filipe A., Gifford R.J., Hopkins S., Hughes J., Jabeen F., Johannessen I., Karageorgopoulos D., Lackenby A., Lester R., Liu R.S., MacConnachie A., Mahungu T., Martin D., Marshall N., Mepham S., Orton R., Palmarini M., Patel M., Perry C., Peters S.E., Porter D., Ritchie D., Ritchie N.D., Seaton R.A., Sreenu V.B., Templeton K., Warren S., Wilkie G.S., Zambon M., Gopal R., Thomson E.C. Late Ebola virus relapse causing meningoencephalitis: a case report. Lancet. 2016;388:498–503. doi: 10.1016/S0140-6736(16)30386-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson J.M., Flexner C.W. Universal antiretroviral regimens: thinking beyond one-pill-once-a-day. Curr. Opin. HIV AIDS. 2017;12:343–350. doi: 10.1097/COH.0000000000000374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson A.A., Ray A.S., Hanes J., Suo Z., Colacino J.M., Anderson K.S., Johnson K.A. Toxicity of antiviral nucleoside analogs and the human mitochondrial DNA polymerase. J. Biol. Chem. 2001;276:40847–40857. doi: 10.1074/jbc.M106743200. [DOI] [PubMed] [Google Scholar]
- Kao R.Y., Yang D., Lau L.S., Tsui W.H., Hu L., Dai J., Chan M.P., Chan C.M., Wang P., Zheng B.J., Sun J., Huang J.D., Madar J., Chen G., Chen H., Guan Y., Yuen K.Y. Identification of influenza A nucleoprotein as an antiviral target. Nat. Biotechnol. 2010;28:600–605. doi: 10.1038/nbt.1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaul A., Worz I., Bartenschlager R. Adaptation of the hepatitis C virus to cell culture. Methods Mol. Biol. 2009;510:361–372. doi: 10.1007/978-1-59745-394-3_27. [DOI] [PubMed] [Google Scholar]
- Leung D.T., Sacks S.L. Docosanol: a topical antiviral for herpes labialis. Expert Opin. Pharmacother. 2004;5:2567–2571. doi: 10.1517/14656566.5.12.2567. [DOI] [PubMed] [Google Scholar]
- Lv Z., Chu Y., Wang Y. HIV protease inhibitors: a review of molecular selectivity and toxicity. Hiv/Aids. 2015;7:95–104. doi: 10.2147/HIV.S79956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis D.A., Boffito M. Long-acting antiviral agents for HIV treatment. Curr. Opin. HIV AIDS. 2015;10:246–252. doi: 10.1097/COH.0000000000000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley J.A., Rudd M.T. Hepatitis C virus NS3/4a protease inhibitors. Curr. Opin. Pharmacol. 2016;30:84–92. doi: 10.1016/j.coph.2016.07.015. [DOI] [PubMed] [Google Scholar]
- Mucker E.M., Goff A.J., Shamblin J.D., Grosenbach D.W., Damon I.K., Mehal J.M., Holman R.C., Carroll D., Gallardo N., Olson V.A., Clemmons C.J., Hudson P., Hruby D.E. Efficacy of tecovirimat (ST-246) in nonhuman primates infected with variola virus (Smallpox) Antimicrob. Agents Chemother. 2013;57:6246–6253. doi: 10.1128/AAC.00977-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mudhasani R., Kota K.P., Retterer C., Tran J.P., Tritsch S.R., Zamani R., Whitehouse C.A., Bavari S. High-content image-based screening of a signal transduction pathway inhibitor small-molecule library against highly pathogenic RNA viruses. J. Biomol. Screen. 2015;20:141–152. doi: 10.1177/1087057114556253. [DOI] [PubMed] [Google Scholar]
- Murakami E., Niu C., Bao H., Micolochick Steuer H.M., Whitaker T., Nachman T., Sofia M.A., Wang P., Otto M.J., Furman P.A. The mechanism of action of beta-D-2'-deoxy-2'-fluoro-2'-C-methylcytidine involves a second metabolic pathway leading to beta-D-2'-deoxy-2'-fluoro-2'-C-methyluridine 5'-triphosphate, a potent inhibitor of the hepatitis C virus RNA-dependent RNA polymerase. Antimicrob. Agents Chemother. 2008;52:458–464. doi: 10.1128/AAC.01184-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paeshuyse J., Dallmeier K., Neyts J. Ribavirin for the treatment of chronic hepatitis C virus infection: a review of the proposed mechanisms of action. Curr. Opin. Virol. 2011;1:590–598. doi: 10.1016/j.coviro.2011.10.030. [DOI] [PubMed] [Google Scholar]
- Patel D., Antwi J., Koneru P.C., Serrao E., Forli S., Kessl J.J., Feng L., Deng N., Levy R.M., Fuchs J.R., Olson A.J., Engelman A.N., Bauman J.D., Kvaratskhelia M., Arnold E. A new class of allosteric HIV-1 integrase inhibitors identified by crystallographic fragment screening of the catalytic core domain. J. Biol. Chem. 2016;291:23569–23577. doi: 10.1074/jbc.M116.753384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathore A.P., Paradkar P.N., Watanabe S., Tan K.H., Sung C., Connolly J.E., Low J., Ooi E.E., Vasudevan S.G. Celgosivir treatment misfolds dengue virus NS1 protein, induces cellular pro-survival genes and protects against lethal challenge mouse model. Antivir. Res. 2011;92:453–460. doi: 10.1016/j.antiviral.2011.10.002. [DOI] [PubMed] [Google Scholar]
- Roymans D., Alnajjar S.S., Battles M.B., Sitthicharoenchai P., Furmanova-Hollenstein P., Rigaux P., Berg J.V.D., Kwanten L., Ginderen M.V., Verheyen N., Vranckx L., Jaensch S., Arnoult E., Voorzaat R., Gallup J.M., Larios-Mora A., Crabbe M., Huntjens D., Raboisson P., Langedijk J.P., Ackermann M.R., McLellan J.S., Vendeville S., Koul A. Therapeutic efficacy of a respiratory syncytial virus fusion inhibitor. Nat. Commun. 2017;8:167. doi: 10.1038/s41467-017-00170-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar G., Zhang N., Fu T.M., An Z. Antibody therapies for the prevention and treatment of viral infections. NPJ Vaccines. 2017;2:19. doi: 10.1038/s41541-017-0019-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulze U., Ringel M. What matters most in commercial success: first-in-class or best-in-class? Nature reviews. Drug Discov. 2013;12:419–420. doi: 10.1038/nrd4035. [DOI] [PubMed] [Google Scholar]
- Sissoko D., Laouenan C., Folkesson E., M'Lebing A.B., Beavogui A.H., Baize S., Camara A.M., Maes P., Shepherd S., Danel C., Carazo S., Conde M.N., Gala J.L., Colin G., Savini H., Bore J.A., Le Marcis F., Koundouno F.R., Petitjean F., Lamah M.C., Diederich S., Tounkara A., Poelart G., Berbain E., Dindart J.M., Duraffour S., Lefevre A., Leno T., Peyrouset O., Irenge L., Bangoura N., Palich R., Hinzmann J., Kraus A., Barry T.S., Berette S., Bongono A., Camara M.S., Chanfreau Munoz V., Doumbouya L., Souley H., Kighoma P.M., Koundouno F.R., Rene L., Loua C.M., Massala V., Moumouni K., Provost C., Samake N., Sekou C., Soumah A., Arnould I., Komano M.S., Gustin L., Berutto C., Camara D., Camara F.S., Colpaert J., Delamou L., Jansson L., Kourouma E., Loua M., Malme K., Manfrin E., Maomou A., Milinouno A., Ombelet S., Sidiboun A.Y., Verreckt I., Yombouno P., Bocquin A., Carbonnelle C., Carmoi T., Frange P., Mely S., Nguyen V.K., Pannetier D., Taburet A.M., Treluyer J.M., Kolie J., Moh R., Gonzalez M.C., Kuisma E., Liedigk B., Ngabo D., Rudolf M., Thom R., Kerber R., Gabriel M., Di Caro A., Wolfel R., Badir J., Bentahir M., Deccache Y., Dumont C., Durant J.F., El Bakkouri K., Gasasira Uwamahoro M., Smits B., Toufik N., Van Cauwenberghe S., Ezzedine K., D'Ortenzio E., Pizarro L., Etienne A., Guedj J., Fizet A., Barte de Sainte Fare E., Murgue B., Tran-Minh T., Rapp C., Piguet P., Poncin M., Draguez B., Allaford Duverger T., Barbe S., Baret G., Defourny I., Carroll M., Raoul H., Augier A., Eholie S.P., Yazdanpanah Y., Levy-Marchal C., Antierrens A., Van Herp M., Gunther S., de Lamballerie X., Keita S., Mentre F., Anglaret X., Malvy D., Group J.S. Experimental treatment with favipiravir for Ebola virus disease (the JIKI trial): a historically controlled, single-arm proof-of-concept trial in Guinea. PLoS Med. 2016;13 doi: 10.1371/journal.pmed.1001967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sluis-Cremer N. The emerging profile of cross-resistance among the nonnucleoside HIV-1 reverse transcriptase inhibitors. Viruses. 2014;6:2960–2973. doi: 10.3390/v6082960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza D.G., Fagundes C.T., Sousa L.P., Amaral F.A., Souza R.S., Souza A.L., Kroon E.G., Sachs D., Cunha F.Q., Bukin E., Atrasheuskaya A., Ignatyev G., Teixeira M.M. Essential role of platelet-activating factor receptor in the pathogenesis of Dengue virus infection. Proc. Natl. Acad. Sci. U. S. A. 2009;106:14138–14143. doi: 10.1073/pnas.0906467106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tebas P., Stein D., Tang W.W., Frank I., Wang S.Q., Lee G., Spratt S.K., Surosky R.T., Giedlin M.A., Nichol G., Holmes M.C., Gregory P.D., Ando D.G., Kalos M., Collman R.G., Binder-Scholl G., Plesa G., Hwang W.T., Levine B.L., June C.H. Gene editing of CCR5 in autologous CD4 T cells of persons infected with HIV. N. Engl. J. Med. 2014;370:901–910. doi: 10.1056/NEJMoa1300662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren T.K., Jordan R., Lo M.K., Ray A.S., Mackman R.L., Soloveva V., Siegel D., Perron M., Bannister R., Hui H.C., Larson N., Strickley R., Wells J., Stuthman K.S., Van Tongeren S.A., Garza N.L., Donnelly G., Shurtleff A.C., Retterer C.J., Gharaibeh D., Zamani R., Kenny T., Eaton B.P., Grimes E., Welch L.S., Gomba L., Wilhelmsen C.L., Nichols D.K., Nuss J.E., Nagle E.R., Kugelman J.R., Palacios G., Doerffler E., Neville S., Carra E., Clarke M.O., Zhang L., Lew W., Ross B., Wang Q., Chun K., Wolfe L., Babusis D., Park Y., Stray K.M., Trancheva I., Feng J.Y., Barauskas O., Xu Y., Wong P., Braun M.R., Flint M., McMullan L.K., Chen S.S., Fearns R., Swaminathan S., Mayers D.L., Spiropoulou C.F., Lee W.A., Nichol S.T., Cihlar T., Bavari S. Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature. 2016;531:381–385. doi: 10.1038/nature17180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watterson D., Robinson J., Chappell K.J., Butler M.S., Edwards D.J., Fry S.R., Bermingham I.M., Cooper M.A., Young P.R. A generic screening platform for inhibitors of virus induced cell fusion using cellular electrical impedance. Sci. Rep. 2016;6:22791. doi: 10.1038/srep22791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye B., Liu X., Li X., Kong H., Tian L., Chen Y. T-cell exhaustion in chronic hepatitis B infection: current knowledge and clinical significance. Cell Death Dis. 2015;6:e1694. doi: 10.1038/cddis.2015.42. [DOI] [PMC free article] [PubMed] [Google Scholar]