Abstract
Background
A critical adaptation strategy for reducing heat-related health risk under climate change is to establish a heat warning system with a proper threshold that requires evaluation of heat-health relationships using empirical data.
Objectives
This work presents a new approach to selecting proper health-based thresholds for a heat warning system which are different from thresholds of heat-health relationship.
Methods
The proposed approach examined heat-health relationships through analyzing 15 years of health records with a modified generalized additive model (GAM), compared risk ratio increments (RRIs) of threshold candidates against a reference, assessed frequency of days above these candidates, and presented results graphically for easy communication. The candidate with the maximum RRI and proper occurring frequency is potentially the best threshold. Three heat indicators, including wet-bulb globe temperature (WBGT), temperature (T), and apparent temperature (AT), as well as three health outcomes, including all-cause mortality, heat-related hospital admissions, and heat-related emergency visits were evaluated.
Results
Risk ratios for all three health outcomes showed a consistent rising trend with increasing threshold candidates for all three heat indicators among different age and gender groups. WBGT had the most obvious increasing trend of RRIs with the three health outcomes. The maximum RRI was observed in heat-related emergency visits (242%), followed by heat-related hospital admissions (73%), and all-cause mortality (9%). The RRIs assessed for the three health outcomes pointed to the same thresholds, 33.0 °C, 34.0 °C, and 37.5 °C for WBGT, T, and AT, respectively. The number of days above these thresholds and for warning to be issued ranged between 0 and 7 days during 2000–2014.
Discussion
This study demonstrated a new approach to determining heat-warning thresholds with different heat indicators and health outcomes. The proposed approach provides a straightforward, feasible, and flexible scientific tool that assists the authorities around the world in selecting a proper threshold for a heat warning system.
Keywords: Health adaptation strategy, Heat-health relationship, Heat-stress threshold, Wet-bulb globe temperature
Highlights
-
•
This work shows a new approach to select proper thresholds for heat warning systems.
-
•
Modified generalized additive model and risk ratio increments (RRIs) were applied.
-
•
Threshold of wet-bulb globe temperature (WBGT) at 33.0 °C were identified for Taiwan.
-
•
WBGT had the most obvious increasing trend of RRIs among three heat indicators.
-
•
The maximum RRI of WBGT was observed in emergency visits (242%).
1. Introduction
Record-breaking temperatures have occurred more frequently worldwide under the trend of climate change (IPCC Intergovernmental Panel on Climate Change, 2014). Since the dreadful heat waves that occurred in Chicago in 1995, a heat warning system has been recognized as the most effective way to reduce heat-related health risks (Changnon et al., 1996, Kaiser et al., 2007, Semenza et al., 1996). The disastrous heat waves in Europe in 2003 further demonstrated the necessity of establishing a heat warning system to prevent significant causality, even in developed countries previously considered to have adequate health care systems for coping with heat-related health impacts (Le Tertre et al., 2006, Pascal et al., 2006). In developing countries where health care systems lagged behind those in developed countries, an effective heat warning system that advises people for self-protection and activates heat-health intervention measures is even more critical to preventing high causality, as in the case of extreme heat waves that hit India and Pakistan in 2015, causing tens of thousands of deaths (Ghumman and Horney, 2016, Sarath Chandran et al., 2017). Governmental agencies are in need of a systematical approach to establishing a heat warning system with sound scientific evidences. An effective heat warning system with a carefully chosen threshold should be able to arouse the attention of the public for proper self-protection and trigger adequate responsive actions from the authorities.
One of the critical elements of a heat warning system is the determination of a proper threshold for issuing a heat warning which ideally should be supported with historical records of significant heat-health impacts. Most of the studies focusing on heat-related mortality or morbidity during high heat-stress periods were in fact assessing the thresholds of heat-related health impacts rather than the thresholds of issuing a heat warning. It should be emphasized that these two types of thresholds are distinctly different. Prior research found that both mortality and morbidity increase at temperatures beyond the optimum ranges that local residents are accustomed to (Astrom et al., 2011, Gasparrini et al., 2015, Honda et al., 2013, Li et al., 2015, Tong et al., 2014, Xu et al., 2012). For example, increase in mortality in Taipei was observed at temperature above apparent temperature (AT), 31.5 °C, between 1994 and 2003 and above the upper bound of optimum temperature (OT), 33.4 °C, between 1994 and 2007 (Chung et al., 2009, Honda et al., 2013). In fact, according to the above definition of AT and OT, Taipei had 134 and 93 days above 31.5 °C and 33.4 °C, respectively in 2017. Therefore, in practice, the thresholds of the heat-related mortality or morbidity increase are not appropriate thresholds for issuing a heat warning. Too frequent issue of warnings may cause the general public to ignore them, thus rendering them ineffective. In particular, for resource-scarce developing countries, the required manpower and resources associated with governmental heat-health intervention programs is also a limiting factor for a prolonged heat-health warning. In Taiwan, periods of high temperature were found to be associated with different health outcomes (Chung et al., 2009, Chung et al., 2015, Gasparrini et al., 2015, Guo et al., 2014, Honda et al., 2013, Lin et al., 2011, Lin et al., 2012, Sung et al., 2013). Some studies used percentiles of heat indicators as the thresholds to avoid frequent announcement of heat advisory (Gasparrini et al., 2015, Ye et al., 2012); other works further evaluated excess health risks at these percentiles (Gasparrini et al., 2015). However, there is yet a systematic approach to comparing and evaluating excess risks of these percentiles and selecting the most suitable threshold. Up to now, only a few studies focused on providing a systematic approach to assisting governmental agencies to establish a proper threshold for issuing a heat warning. Petitti et al. (2016) attempted to identify, with data from USA, multiple trigger points at which heat-health intervention measures might be activated. Minimal risk temperature, increasing risk temperature, and excess risk temperature were defined according to heat-health relationships, using 95% confidence interval as a criterion for selecting increasing risk temperature and excess risk temperature above the minimum risk temperature (Petitti et al., 2016). The present research proposes a more straightforward approach to evaluating simultaneously proper thresholds and damage coefficients of heat-health relationships above several threshold candidates in order to provide a systematic way of selecting proper health-based thresholds for different countries located in different climate zones. It is a useful scientific tool for assisting the authorities to establish a heat warning system with solid scientific evidences. An appropriate warning system is urgently needed especially in developing countries with high population density, such as those in Asia, where medical resource is limited and self-protection is critical for adaptation.
Moreover, a proper indicator is also essential for establishing a heat warning system. Different heat indicators such as daily maximum temperature, AT, and wet-bulb globe temperature (WBGT) have been widely discussed (Astrom et al., 2011, Li et al., 2015, Petitti et al., 2016, Tong et al., 2014, Xu et al., 2012, Ye et al., 2012). Though the present approach can be applied to any heat indicator, WBGT is selected in this study as the target indicator for the following reasons. First, WBGT comprises four essential meteorological parameters, namely, temperature (T), relative humidity (RH%), wind speed, and solar radiation, all of which have significant association with heat stress. It goes without saying that direct exposure to solar radiation enhances heat stress human being experiences while high wind speed reduces heat stress. Heat indicators with only T and RH% taken into account, as in most studies, may have high false-negative rates, thus causing some high heat-stress days to be missed. Current heat indicators considering only T and RH% have their basis on human comfort (Coccolo et al., 2016), which is subjective and different from “heat stress”. A proper heat-stress indicator in a heat warning system should be related to human physiological changes with negative health impacts; and WBGT as a heat-stress indicator has extensive physiological-based evidences (Bernard, 2012). Secondly, WBGT has been used in occupational health as an indicator to prevent heat-stress-related health impacts in workplaces for the past 60 years with a lot of studies demonstrating the relationships between WBGT and heat-related health outcomes (Bernard, 2012, Błażejczyk et al., 2014, Brode et al., 2018, ISO (International Standards Organization), 2017, Spector and Sheffield, 2014, Yaglou and Minard, 1956). Thirdly, in recent years, increasing research has found that WBGT can be an indicator not only in workplaces (Hyatt et al., 2010, Kakamu et al., 2017, Lin et al., 2012, Sung et al., 2013, Yamamoto et al., 2007). However, the warning thresholds for occupational health cannot be directly applied to the general public with vulnerable populations, such as the elderly and children, involved. Hence, there is a need for proper WBGT thresholds for heat warning systems for different countries in different climate zones. Fourthly, the Hong Kong government has recently begun using a modified WBGT as one of their heat indices (Lee et al., 2016). Japan and Australia also present WBGT as one of the heat indicators for the general public (Australian Government-Bureau of Meteorology, 2018; Japanese Ministry of the Environment 2018). In view of the above and in line with the global trend, the new approach presented in this work focus on assessing WBGT thresholds for reducing heat-stress health risks.
For comparison purpose, the proposed approach is also applied to assessing T and AT thresholds. Temperature is the most commonly used heat indicator and AT is also used by the Central Weather Bureau (CWB) in Taiwan and in other countries such as Italy and Australia (Australian Government - Bureau of Meteorology, 2018, Michelozzi et al., 2010) for routine forecast. In the literature, AT has different formulas comprising T, RH%, wind speed, and/or radiation absorbed by the human body (Coccolo et al., 2016, Steadman, 1984). However, radiation absorbed by the human body is closely related to the clothing condition of individuals and it is difficult to measure. On the other hand, solar radiation in the environment as used in WBGT does not vary with clothing. Thus, in practice, solar radiation is easier to measure compared with radiation absorbed by the human body.
When assessing heat-related health outcomes, most studies used daily all-cause or cardiovascular mortality, hospital admissions of cardiovascular or respiratory diseases, and/or emergency visits of heat-related diseases (Astrom et al., 2011, Bai et al., 2014, Knowlton et al., 2009, Li et al., 2015, Mastrangelo et al., 2007, Semenza et al., 1999, Sheridan and Lin, 2014). In this work, all-cause mortality, hospital admissions and emergency visits of heat-related illness (such as heat stroke and heat exhaustion) are used in view of their different considerations in evaluating proper thresholds of the heat warning system. A warning system with the threshold identified using all-cause mortality aims at reducing overall mortality, while those with thresholds determined using hospital admissions and emergency visits target at reducing morbidity related to work productivity and/or human wellbeing (Xia et al., 2018). In reality, some countries may only have complete datasets for one of the health records presented here. There were also studies evaluating heat-health relationships for multiple health outcomes (Petitti et al., 2016, Williams et al., 2012). Petitti et al. emphasized the advantage of adaptation strategies formulated with comprehensive information spanning a range of health outcomes associated with heat (Petitti et al., 2016). Thus, using these three types of health records to evaluate the consistency and differences in threshold identification can shed light on the selection of threshold according to availability of health records.
In summary, to fill the scientific gap of a method, useful to meteorological and/or public health authorities, for selecting proper thresholds of a heat warning system on the basis of health evidences, the objectives of this work are (1) to demonstrate an approach to evaluating proper thresholds of a heat warning system and the damage coefficients (the slope) of heat-health relationships above the thresholds simultaneously, with data from Taiwan for illustration; (2) to apply this approach with WBGT, T, and AT for comparison; and (3) to evaluate thresholds identified using different health records (all-cause mortality, heat-related hospital admissions, and heat-related emergency visits) to assess the consistency and differences in identifying thresholds of issuing a heat warning.
2. Materials and methods
2.1. Health records
All-cause mortality counts (excluding accidents and suicide) between 2008 and 2014 were obtained from the Taiwan National Mortality Registry. Data before 2008 cannot be used in this work since the location of death was not specified. Daily hospital admissions and emergency visits of heat-related illness between 2000 and 2014 were obtained from the database of the Health and Welfare Data Science Center of the Ministry of Health and Welfare. This database contains hospital visit information of almost the entire population of Taiwan (23.71 million) on a daily basis, including hospital admissions, emergency visits, and hospital locations. Cases of heat-related illness (ICD9: 992 according to the 9th Revision of the International Classification of diseases (ICD9), including heat stroke and heat exhaustion) and statistics on age and gender were analyzed in this work. This study was reviewed and approved by the Internal Review Board of Academia Sinica.
2.2. Heat indicators and air pollutant data
Hourly meteorological data from 2000 to 2014 were obtained from the CWB, Taiwan. There are 32 weather monitoring stations throughout Taiwan; among which, mountain stations were excluded because of the sparse population in those areas. Daily maximum temperatures of the 22 non-mountain stations were obtained and averaged for analysis. This study also assessed AT, which comprises T, RH% and wind speed, as used by the CWB, Taiwan (Steadman, 1984). The equation is listed in the Appendices (see Eq. (A) of Appendix A). The daily maximum ATs of these stations were averaged for analysis.
WBGT is a weighed combination of dry-bulb temperature, globe temperature and natural wet-bulb temperature (Bernard, 2012) (see Eq. (B) of Appendix A); it considers T, RH%, wind speed, and solar radiation. However, natural wet-bulb temperature and globe temperature were not provided by routine meteorological measurements. Nevertheless, equations for calculating WBGT according to fundamental principles of heat and mass transfer with standard meteorological data have been derived and validated (Liljegren et al., 2008). Thus, these equations with inputs of routine meteorological measurements of hourly temperature, RH%, wind speed, and solar radiation were used for calculating WBGT (see Eq. (C) and Eq. (D) of Appendix A). The daily maximum WBGTs of these stations were also averaged for analysis.
In the heat-health model, confounders such as air pollutants (Ye et al., 2012) were adjusted using hourly measurements of air pollutant levels from 2000 to 2014. These measurements were obtained from the Environmental Protection Administration (EPA), Taiwan, which has 76 air-quality monitoring stations throughout Taiwan. PM2.5 was used as a confounder instead of other air pollutants because it is currently the most concerned pollutant in Taiwan and has high correlation with other pollutants. Measurements of PM2.5 from 55 ambient stations between 2000 and 2014 were used while data from other types of stations (such as industrial, traffic and background) were excluded.
2.3. Analysis
This study focused on health outcomes of heat-related illness; hence, only data of May to October (warm season) were used for modeling. Data of health outcomes were fitted to generalized additive models (GAMs) with Poisson distribution to examine relationships between heat indicators and health outcomes. Non-parametric smoothers are considered in the GAMs to explore the respective association patterns between one of the daily maximum heat indicators, denoted by , (WBGT, T, and AT) and one of the health outcomes, denoted by , (all-cause mortality counts, heat-related hospital admissions and heat-related emergency visits). The model is specified as
| (1) |
where α is a constant, is a thin plate spline function of the heat indicator with a number of knots over days in each warm season, and is another thin plate spline function of time with some number of knots for examining daily change pattern during warm seasons. Potential covariates on day t, denoted by , such as daily PM2.5 concentration, day of week, holiday and periods prevalent with the severe acute respiratory syndrome (SARS) are considered for adjustment. Model selection was conducted to obtain influential covariates and to choose the number of knots according to the Akaike information criterion (AIC). The model with a lower AIC value is a better-fitted model. By using the above evaluation, the number of knots was adopted for fitting the thin plate spline function . The AIC values for models with k ranging from 3 to 10 did not reduce significantly and the fitted patterns of the health outcomes showed almost the same linear relationship for heat indicators above 30. The fitted curve of is presented in Fig. 1 of Appendix B for comparison. The spline function models the same health outcome pattern during each warm season of 184 days; choices of k = 1, 2, 3 and 4 for a warm season were evaluated. According to the AIC values of the fitted models, k = 3 for a warm season is the best choice. Hence, were adopted for modeling in health outcomes of heat-related hospital admissions and emergency visits (15 years) and all-cause mortality (7 years), respectively. After obtaining the best model, the estimated smooth function was plotted to examine the heat-health relationships. As shown in the Results section, the plots did reveal a linear heat-health relationship for heat indicator beyond certain cut-points, and that the model can be modified for determining proper thresholds. Specifically, the daily maximum heat indicator on day t in the model is replaced by which is defined as,
where is a specified threshold candidate of the heat indicator. The model is then modified as
| (2) |
where is a damage coefficient associated with an increased value of heat indicator from the chosen threshold . For assessing changes in health risk in relation to a heat indicator threshold, this study evaluated the risk ratio (RR), , which is the expected health outcome for 1 °C increment over the threshold candidate divided by the expected health outcome for that heat indicator below the threshold. With this damage coefficient in the modified model, different threshold candidates could be compared to shed light on the potential reduced health risks. The threshold candidates were assessed starting from 30 °C at 0.5 °C increments sequentially for the three heat indicators. Increments of 0.5 °C were used because a threshold defined by the authority is typically a round number or with 0.5 °C increments for easy communication with the general public. This work set 30 °C as the lowest threshold candidate of the three heat indicators because the median values of WBGT, T, and AT from 2000 to 2014 in Taiwan are 30.1 °C, 30.8 °C, and 33.6 °C, respectively. Previous studies also showed that Taiwan had higher mortality of various diseases at temperature above 30 °C (Pan et al., 1995). The models were repeatedly fitted with the threshold candidates till either the number of days above the threshold candidate or the number of cases was too small, a limitation of small sample size.
Risk ratios of different threshold candidates were compared to determine the best threshold candidate with the maximum increments of risk ratio (RR) in comparison with a reference, which, in this work, is the chosen lowest threshold candidate denoted by 30 °C. The risk ratio increment (RRI) is calculated using
| (3) |
Such increment in association with a threshold candidate was adjusted by the RR of the reference level of a heat indicator; hence, the sensitivity of the threshold candidate to the RR could be examined and comparisons among different health outcomes associated with the heat indicator could be conducted. The patterns of RRI associated with different threshold candidates were graphically illustrated to determine the proper threshold value. The threshold candidate of the heat indicator with the maximum RRI, the largest increase in RR from the reference, was potentially the proper threshold value. Thresholds selected on the basis of different health outcomes for different purposes were evaluated for their consistency and differences. Finally, the numbers of days exceeding different threshold candidates in previous years were also assessed and provided as a complementary consideration for threshold selection.
Previous studies showed that heat-health thresholds determined by spline functions (the change point of the segmented regressions) were usually too low for a heat warning system as discussed in the Introduction. A spline function (k = 3) for was adopted to explore the patterns of health outcomes above certain cut-points in this work; rather than determining the thresholds. After confirming that the patterns of health outcome are linear above certain cut-points with Eq. (1), threshold candidates can be evaluated through comparing their associated RRI values with Eqs. (2), (3). Moreover, thresholds determined according to the change point of the segmented regressions are typically shown in graphic presentations without quantification. Instead, the proposed approach presents quantitative RRI values to facilitate the authorities in their choice of thresholds. The quantitative graphical presentation is the major advantage of the proposed approach.
Data processing and statistical analyses were carried out using SAS 9.3 (SAS Institute Inc., Cary, NC, USA) and R 3.3.3 with mgcv package (Wood, 2006). Regarding the lag effect, recent studies have found much smaller effect of heat waves in “extended periods” than the acute effects (Barnett et al., 2012, Gasparrini and Armstrong, 2011, Gosling et al., 2009), and the focus of an effective heat warning system should minimize health risks of the acute effects on the event days (WMO and WHO, 2015). For demonstration purpose, lagged effect was assessed for all-cause mortality and the results are shown in Table 1 of Appendix C. As can be seen, lagged effect was found to be relatively weak, and hence not evaluated further in this work.
3. Results
Table 1 shows the summary of data in the warm season of 2000–2014 in Taiwan as used in the models. The daily maximum of all-cause mortality was 463 with more males than females; and the elderly had the highest counts among all age groups, as expected. Daily maximum of heat-related hospital admissions and emergency visits reached 1533 and 73, respectively. The mean heat-related emergency visit was almost 0.5% of the mean heat-related hospital admission. Among different age groups, people aged 15–64 years accounted for the majority of heat-related hospital admissions. In terms of gender, the number of females was higher than that of males. In contrast, females have fewer hospital emergency visits than males. The average daily maximum WBGT, T, and AT in the warm season of these 15 years were 29.5 °C, 30.4 °C, and 32.9 °C, respectively.
Table 1.
Summary of data used in GAM, May to October in years 2000–2014.
| Variables | N | Mean | S.D. | Min. | Max. |
|---|---|---|---|---|---|
| Daily all-cause mortalitya | 1288 | 360 | 30 | 278 | 463 |
| Female | 1288 | 144 | 16 | 105 | 195 |
| Male | 1288 | 215 | 19 | 156 | 283 |
| Age 0–14 | 1288 | 3 | 2 | 0 | 9 |
| Age 15–64 | 1288 | 97 | 11 | 64 | 134 |
| Age > 65 | 1288 | 260 | 24 | 197 | 340 |
| Heat-related hospital admissions | 2760 | 178 | 220 | 1 | 1533 |
| Female | 2760 | 101 | 128 | 0 | 856 |
| Male | 2760 | 75 | 90 | 0 | 674 |
| Age 0–14 | 2760 | 8 | 8 | 0 | 63 |
| Age 15–64 | 2760 | 151 | 191 | 0 | 1351 |
| Age > 65 | 2760 | 18 | 22 | 0 | 147 |
| Heat-related emergency visits | 2760 | 7 | 7 | 0 | 73 |
| Female | 2760 | 2 | 2 | 0 | 26 |
| Male | 2760 | 5 | 6 | 0 | 45 |
| Age 0–14 | 2760 | 1 | 1 | 0 | 7 |
| Age 15–64 | 2760 | 5 | 6 | 0 | 51 |
| Age > 65 | 2760 | 1 | 2 | 0 | 19 |
| Heat indicator | |||||
| Daily max. WBGT (°C) | 2760 | 29.5 | 2.35 | 19.5 | 33.6 |
| Daily max. T (°C) | 2760 | 30.4 | 2.18 | 20.9 | 34.5 |
| Daily max. AT (°C) | 2760 | 32.9 | 2.82 | 20.8 | 38.0 |
| Air pollutant | |||||
| PM2.5 (μg/m3) | 2760 | 28.4 | 13.3 | 8.55 | 149 |
Dataset of daily all-cause mortality covers years 2008–2014.
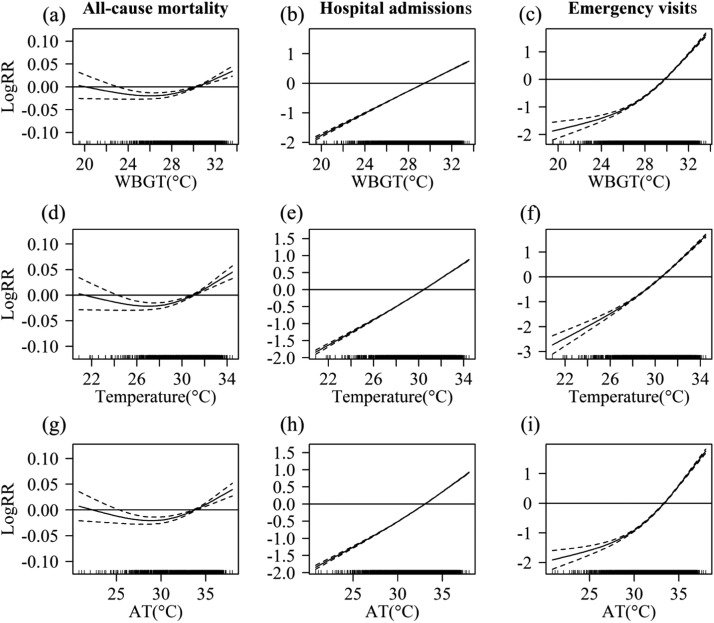
The associations of WBGT, T, and AT with different health outcomes during warm season of the studied periods are shown in Fig. 2 of Appendix B. As can be seen, the health impacts increased linearly with the heat indicator after certain values in the right tails of these graphs. Fig. 1(a)-(i) displays the associations of WBGT, T, and AT with different health outcomes in GAMs after confounder adjustments. Similarly, the right tails seen in Fig. 1(a)-(i) also show linear exposure-response relationships of maximum WBGT, T, and AT with different health impacts above certain values. Such agreement in results obtained indicates the suitability of the GAMs for this analysis.
Fig. 1.
Heat-health relationship of daily maximum WBGT, T and AT with all-cause mortality, heat-related hospital admissions and heat-related emergency visits obtained from smooth functions of heat indicator in GAMs after confounder adjustment.
Table 2(a)-(c) shows RRs estimated by the modified GAMs with different threshold candidates for WBGT, T, and AT, respectively. Whether stratified or not, RRs for all-cause mortality, heat-related hospital admissions, and heat-related emergency visits showed a rising trend with increase in threshold values for WBGT, T, and AT. The RRs for WBGT were statistically significant up to the cut-point of 32.5 °C (RR = 1.06), 33.0 °C (RR = 2.03), and 33.0 °C (RR = 4.19) for all-cause mortality, heat-related hospital admissions, and heat-related emergency visits, respectively. The RRs for T were statistically significant up to the cut-point of 33.5 °C (RR = 1.11), 34.0 °C (RR = 1.69), and 34.0 °C (RR = 4.13) for the three health outcomes, respectively. The RRs for AT were statistically significant up to the cut-point of 36.0 °C (RR = 1.05), 37.5 °C (RR = 1.52), and 37.5 °C (RR = 4.67) for the three health outcomes, respectively. The highest RRs for all three heat indicators occurred in heat-related emergency visits (RR = 4.13–4.67), followed by heat-related hospital admissions (RR = 1.52–2.03) and all-cause mortality (RR = 1.05–1.11).
Table 2.
Risk ratios at different threshold candidates of (a) WBGT, (b) T, and (c) AT.
| (a) WBGT | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Threshold | > 30 °C | > 31.0 °C | > 32.0 °C | > 32.5 °C | > 33.0 °C | |||||
| RR | (95% CI)a | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | |
| All-cause mortality | 1.02* | (1.01, 1.02) | 1.03* | (1.02, 1.03) | 1.05* | (1.03, 1.07) | 1.06† | (1.01, 1.11) | 1.10 | (0.96, 1.26) |
| Female | 1.01* | (1.00, 1.02) | 1.02* | (1.01, 1.03) | 1.04† | (1.00, 1.07) | 1.03 | (0.96, 1.11) | 1.09 | (0.88, 1.34) |
| Male | 1.02* | (1.01, 1.03) | 1.03* | (1.02, 1.04) | 1.05* | (1.03, 1.08) | 1.08† | (1.01, 1.14) | 1.10 | (0.93, 1.31) |
| Age 0–14 | 1.02 | (0.97, 1.08) | 1.02 | (0.94, 1.12) | 1.08 | (0.84, 1.37) | 1.44 | (0.86, 2.42) | 2.23 | (0.47, 10.53) |
| Age 15–64 | 1.01* | (1.01, 1.02) | 1.02* | (1.01, 1.04) | 1.03 | (0.99, 1.07) | 1.04 | (0.96, 1.14) | 1.15 | (0.88, 1.49) |
| Age > 65 | 1.02* | (1.01, 1.02) | 1.03* | (1.02, 1.04) | 1.05* | (1.03, 1.08) | 1.06† | (1.01, 1.12) | 1.07 | (0.92, 1.26) |
| Heat-related hospital admissions | 1.3* | (1.30, 1.31) | 1.36* | (1.35, 1.37) | 1.47* | (1.45, 1.49) | 1.68* | (1.62, 1.73) | 2.03* | (1.82, 2.28) |
| Female | 1.29* | (1.28, 1.29) | 1.33* | (1.32, 1.35) | 1.43* | (1.40, 1.46) | 1.61* | (1.54, 1.68) | 1.83* | (1.57, 2.13) |
| Male | 1.33* | (1.32, 1.34) | 1.39* | (1.38, 1.41) | 1.52* | (1.48, 1.55) | 1.76* | (1.67, 1.85) | 2.28* | (1.92, 2.71) |
| Age 0–14 | 1.31* | (1.29, 1.34) | 1.40* | (1.35, 1.44) | 1.54* | (1.42, 1.66) | 1.72* | (1.45, 2.04) | 2.61* | (1.49, 4.56) |
| Age 15–64 | 1.31* | (1.31, 1.32) | 1.37* | (1.36, 1.38) | 1.48* | (1.46, 1.51) | 1.69* | (1.63, 1.75) | 2.01* | (1.78, 2.28) |
| Age > 65 | 1.24* | (1.23, 1.26) | 1.27* | (1.24, 1.29) | 1.33* | (1.27, 1.39) | 1.58* | (1.43, 1.76) | 2.05* | (1.45, 2.91) |
| Heat-related emergency visits | 1.77* | (1.73, 1.81) | 1.96* | (1.89, 2.02) | 2.26* | (2.10, 2.42) | 2.77* | (2.41, 3.17) | 4.19* | (2.92, 6.03) |
| Female | 1.67* | (1.59, 1.75) | 1.87* | (1.75, 2.00) | 2.31* | (2.01, 2.66) | 3.29* | (2.55, 4.25) | 3.81* | (1.92, 7.57) |
| Male | 1.80* | (1.75, 1.85) | 1.98* | (1.91, 2.06) | 2.23* | (2.05, 2.42) | 2.55* | (2.16, 3.01) | 4.29* | (2.76, 6.65) |
| Age 0–14 | 1.29* | (1.19, 1.40) | 1.52* | (1.33, 1.74) | 2.38* | (1.76, 3.23) | 3.45* | (1.90, 6.28) | 6.86† | (1.49, 31.65) |
| Age 15–64 | 1.82* | (1.77, 1.87) | 1.99* | (1.92, 2.07) | 2.24* | (2.07, 2.43) | 2.66* | (2.27, 3.11) | 3.86* | (2.52, 5.91) |
| Age > 65 | 1.84* | (1.73, 1.95) | 1.99* | (1.83, 2.16) | 2.25* | (1.89, 2.66) | 3.15* | (2.30, 4.31) | 5.50* | (2.50, 12.13) |
| (b) T | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Threshold | > 30 °C | > 31.0 °C | > 32.0 °C | > 33.0 °C | > 33.5 °C | > 34.0 °C | ||||||
| RR | (95% CI)a | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | |
| All-cause mortality | 1.01* | (1.01, 1.02) | 1.02* | (1.02, 1.03) | 1.04* | (1.03, 1.05) | 1.08* | (1.05, 1.11) | 1.11* | (1.04–1.17) | 1.16 | (0.97, 1.39) |
| Female | 1.01* | (1.01, 1.02) | 1.02* | (1.01, 1.03) | 1.03* | (1.02, 1.05) | 1.07* | (1.02, 1.12) | 1.06 | (0.96–1.16) | 1.11 | (0.83, 1.48) |
| Male | 1.02* | (1.01, 1.02) | 1.02* | (1.02, 1.03) | 1.04* | (1.03, 1.05) | 1.08* | (1.05, 1.12) | 1.14* | (1.06–1.23) | 1.20 | (0.94, 1.51) |
| Age 0–14 | 1.01 | (0.97, 1.06) | 1.01 | (0.95, 1.07) | 0.99 | (0.89, 1.10) | 0.88 | (0.62, 1.26) | 0.68 | (0.29–1.62) | 0.37 | (0.02, 7.13) |
| Age 15–64 | 1.01* | (1.00, 1.02) | 1.01* | (1.00, 1.03) | 1.02† | (1.00, 1.04) | 1.05 | (0.99, 1.11) | 1.09 | (0.97–1.23) | 1.22 | (0.86, 1.74) |
| Age > 65 | 1.02* | (1.01, 1.02) | 1.02* | (1.02, 1.03) | 1.04* | (1.03, 1.05) | 1.09* | (1.06, 1.13) | 1.11* | (1.04–1.20) | 1.15 | (0.93, 1.42) |
| Heat-related hospital admissions | 1.31* | (1.30, 1.31) | 1.36* | (1.35, 1.36) | 1.44* | (1.43, 1.45) | 1.59* | (1.56, 1.62) | 1.68* | (1.61–1.74) | 1.69* | (1.50, 1.90) |
| Female | 1.30* | (1.29, 1.30) | 1.35* | (1.34, 1.35) | 1.43* | (1.42, 1.44) | 1.56* | (1.53, 1.60) | 1.60* | (1.52–1.69) | 1.56* | (1.33, 1.82) |
| Male | 1.32* | (1.32, 1.33) | 1.37* | (1.36, 1.38) | 1.45* | (1.43, 1.46) | 1.63* | (1.58, 1.67) | 1.77* | (1.67–1.88) | 1.84* | (1.54, 2.20) |
| Age 0–14 | 1.31* | (1.29, 1.33) | 1.37* | (1.34, 1.40) | 1.49* | (1.44, 1.54) | 1.76* | (1.61, 1.93) | 2.01* | (1.66–2.44) | 2.20* | (1.21, 4.00) |
| Age 15–64 | 1.31* | (1.31, 1.32) | 1.36* | (1.36, 1.37) | 1.44* | (1.43, 1.45) | 1.59* | (1.56, 1.62) | 1.66* | (1.59–1.73) | 1.66* | (1.47, 1.89) |
| Age > 65 | 1.26* | (1.24, 1.27) | 1.30* | (1.28, 1.31) | 1.36* | (1.33, 1.39) | 1.53* | (1.44, 1.62) | 1.72* | (1.52–1.94) | 1.69* | (1.17, 2.45) |
| Heat-related emergency visits | 1.65* | (1.62, 1.68) | 1.74* | (1.70, 1.78) | 1.88* | (1.82, 1.95) | 2.36* | (2.18, 2.57) | 3.06* | (2.59–3.62) | 4.13* | (2.40, 7.12) |
| Female | 1.61* | (1.55, 1.67) | 1.74* | (1.66, 1.82) | 1.99* | (1.86, 2.13) | 2.76* | (2.35, 3.24) | 4.19* | (3.05–5.76) | 7.45* | (2.65, 20.98) |
| Male | 1.66* | (1.62, 1.69) | 1.74* | (1.69, 1.79) | 1.85* | (1.77, 1.92) | 2.25* | (2.04, 2.48) | 2.81* | (2.30–3.43) | 3.58* | (1.88, 6.82) |
| Age 0–14 | 1.24* | (1.17, 1.32) | 1.29* | (1.19, 1.40) | 1.49* | (1.30, 1.70) | 2.20* | (1.54, 3.13) | 3.69* | (1.78–7.66) | 2.17 | (0.11, 44.82) |
| Age 15–64 | 1.68* | (1.65, 1.72) | 1.76* | (1.71, 1.80) | 1.86* | (1.79, 1.94) | 2.21* | (2.01, 2.43) | 2.60* | (2.13–3.17) | 4.05* | (2.19, 7.48) |
| Age > 65 | 1.83* | (1.74, 1.92) | 1.96* | (1.85, 2.08) | 2.16* | (1.99, 2.35) | 3.13* | (2.60, 3.77) | 5.29* | (3.73–7.51) | 5.25† | (1.47, 18.73) |
| (c) AT | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Threshold | > 30 °C | > 32.0 °C | > 34.0 °C | > 36.0 °C | > 37.0 °C | > 37.5 °C | ||||||
| RR | (95% CI)a | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | RR | (95%CI) | |
| All-cause mortality | 1.01* | (1.00, 1.01) | 1.01* | (1.01, 1.01) | 1.02* | (1.01, 1.02) | 1.05* | (1.03, 1.07) | 1.04 | (0.97–1.12) | 1.11 | (0.93, 1.32) |
| Female | 1.00† | (1.00, 1.01) | 1.01* | (1.00, 1.01) | 1.01* | (1.01, 1.02) | 1.04* | (1.01, 1.08) | 1.01 | (0.90–1.14) | 1.02 | (0.77, 1.35) |
| Male | 1.01* | (1.00, 1.01) | 1.01* | (1.01, 1.02) | 1.02* | (1.01, 1.03) | 1.06* | (1.03, 1.09) | 1.06 | (0.96–1.17) | 1.17 | (0.93, 1.47) |
| Age 0–14 | 0.99 | (0.97, 1.01) | 1.00 | (0.97, 1.03) | 1.00 | (0.94, 1.05) | 1.03 | (0.82, 1.31) | 1.22 | (0.47–3.17) | 0.99 | (0.09, 11.13) |
| Age 15–64 | 1.01* | (1.00, 1.01) | 1.01* | (1.00, 1.01) | 1.01* | (1.00, 1.02) | 1.03 | (0.99, 1.07) | 1.05 | (0.90–1.22) | 1.28 | (0.92, 1.79) |
| Age > 65 | 1.01* | (1.00, 1.01) | 1.01* | (1.01, 1.01) | 1.02* | (1.01, 1.03) | 1.06* | (1.04, 1.09) | 1.04 | (0.95–1.14) | 1.05 | (0.85, 1.29) |
| Heat-related hospital admissions | 1.21* | (1.21, 1.22) | 1.24* | (1.24, 1.25) | 1.30* | (1.29, 1.30) | 1.45* | (1.43, 1.47) | 1.37* | (1.30–1.44) | 1.52* | (1.35, 1.71) |
| Female | 1.21* | (1.20, 1.21) | 1.23* | (1.23, 1.24) | 1.29* | (1.28, 1.29) | 1.43* | (1.40, 1.46) | 1.28* | (1.20–1.38) | 1.38* | (1.18, 1.62) |
| Male | 1.23* | (1.22, 1.23) | 1.26* | (1.25, 1.26) | 1.32* | (1.31, 1.32) | 1.48* | (1.45, 1.51) | 1.47* | (1.35–1.59) | 1.68* | (1.40, 2.01) |
| Age 0–14 | 1.19* | (1.18, 1.21) | 1.24* | (1.22, 1.25) | 1.31* | (1.28, 1.33) | 1.53* | (1.43, 1.64) | 1.58* | (1.21–2.06) | 1.97† | (1.07, 3.62) |
| Age 15–64 | 1.22* | (1.22, 1.22) | 1.25* | (1.25, 1.25) | 1.30* | (1.30, 1.31) | 1.46* | (1.44, 1.48) | 1.35* | (1.28–1.43) | 1.50* | (1.32, 1.70) |
| Age > 65 | 1.18* | (1.17, 1.19) | 1.21* | (1.19, 1.22) | 1.24* | (1.23, 1.26) | 1.36* | (1.30, 1.42) | 1.45* | (1.23–1.70) | 1.58† | (1.08, 2.29) |
| Heat-related emergency visits | 1.42* | (1.40, 1.44) | 1.51* | (1.49, 1.54) | 1.64* | (1.61, 1.68) | 2.02* | (1.90, 2.14) | 2.60* | (2.13–3.18) | 4.67* | (2.82, 7.75) |
| Female | 1.38* | (1.34, 1.41) | 1.47* | (1.43, 1.52) | 1.61* | (1.54, 1.68) | 2.16* | (1.92, 2.44) | 2.91* | (1.97–4.30) | 6.08* | (2.22, 16.68) |
| Male | 1.44* | (1.42, 1.46) | 1.53* | (1.50, 1.55) | 1.65* | (1.61, 1.69) | 1.96* | (1.82, 2.10) | 2.52* | (1.98–3.19) | 4.38* | (2.41, 7.95) |
| Age 0–14 | 1.14* | (1.10, 1.18) | 1.18* | (1.12, 1.23) | 1.23* | (1.14, 1.33) | 1.85* | (1.43, 2.39) | 3.46* | (1.46–8.21) | 5.93 | (0.52, 67.74) |
| Age 15–64 | 1.46* | (1.44, 1.49) | 1.55* | (1.53, 1.58) | 1.67* | (1.63, 1.71) | 1.97* | (1.84, 2.11) | 2.43* | (1.93–3.07) | 4.59* | (2.59, 8.15) |
| Age > 65 | 1.52* | (1.47, 1.58) | 1.63* | (1.56, 1.69) | 1.77* | (1.67, 1.87) | 2.29* | (1.98, 2.64) | 3.30* | (2.11–5.15) | 5.12* | (1.53, 17.10) |
p < 0.01.
p < 0.05.
Risk Ratio (RR) and 95% confidence interval (95% CI) of each outcome with a 1 °C increase above the threshold.
In general, males have higher RRs for these three health outcomes with all three heat indicators than females, with the few exceptions observed for emergency visits with the WBGT threshold set at 32.0 °C, T thresholds at 32.0, 33.0, and 34.0 °C, and AT thresholds at 36.0, 37.0, and 37.5 °C. The differences in RRs between males and females became greater with increasing threshold values. In heat-related emergency visits, the highest RR for males was 4.29 for WBGT with threshold of 33.0 °C, while that for females reached 7.45 for T with threshold of 34.0 °C and 6.08 for AT with threshold of 37.5 °C. The above estimates were all statistically significant.
Differences in RR for health outcomes among the three age groups also widened with increasing threshold values of heat indicators. The following description focuses on results with statistical significance. For WBGT, the highest RR for all-cause mortality (1.06) occurred in the population aged above 65 years at threshold of 32.5 °C; while that for both heat-related hospital admissions (2.61) and heat-related emergency visits (6.86) occurred among the age group of 0–14 years at threshold of 33.0 °C and 33.0 °C, respectively. For T, the population aged above 65 years had the highest RR for all-cause mortality (1.11) and heat-related emergency visits (5.29) at threshold of 33.5 °C; while the age group of 0–14 had the highest RR for heat-related hospital admissions (2.20) at threshold of 34.0 °C. Similarly, for AT, the population aged above 65 years had the highest RR for all-cause mortality (1.06) and heat-related emergency visits (5.12) at threshold of 36.0 °C and 37.5 °C, respectively; while the age group of 0–14 had the highest RR for heat-related hospital admissions (1.97) at threshold of 37.5 °C. In short, the age group of either 0–14 or > 65 had the highest RRs for these three different heat indicators, with those for all-cause mortality consistently in the population aged above 65 and those for heat-related hospital admissions consistently in age group of 0–14. Moreover, for the age group of 0–14, the RRs for heat-related hospital admissions (1.97–2.61) and emergency visits (3.46–6.86) showed statistically significant increase with most of the threshold candidates for the different heat indicators; while those for all-cause mortality did not.
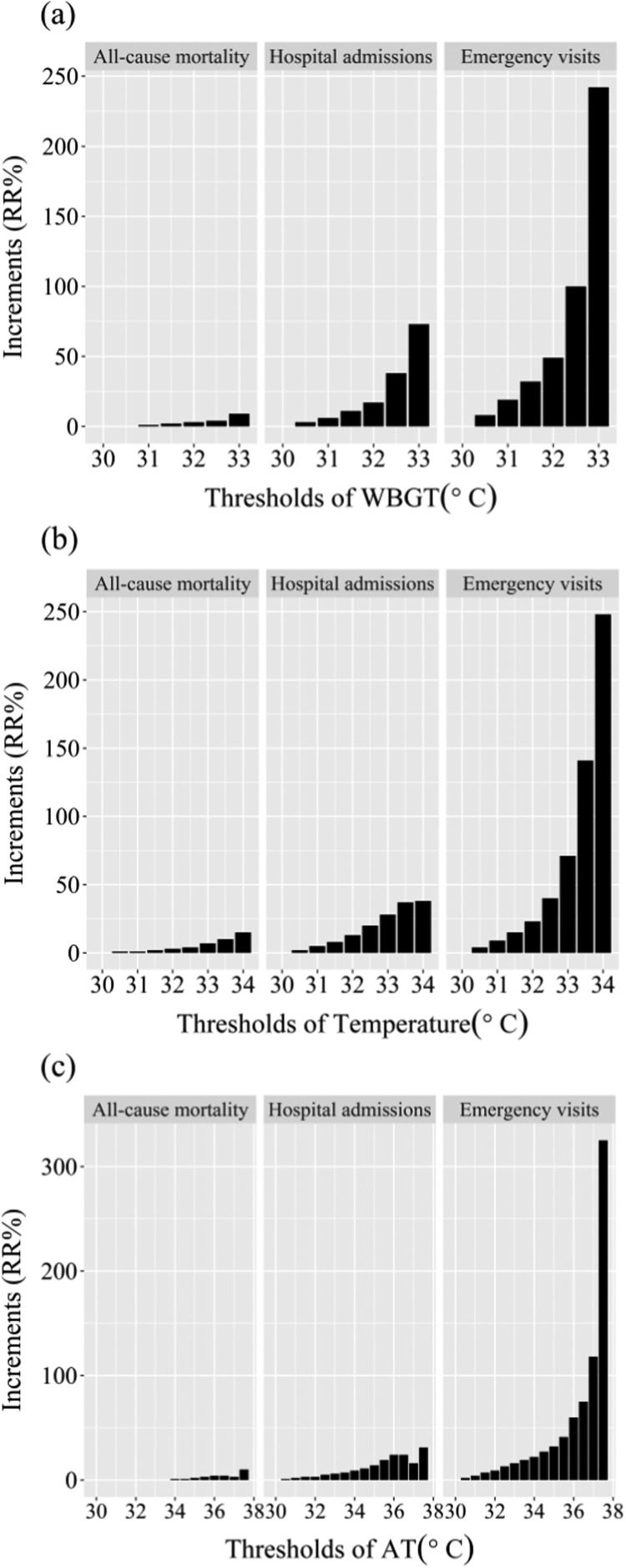
The incremental changes in RRs of different threshold candidates compared with RRs of the reference, as shown in Fig. 2(a)-(c), show a rapid rising trend with increase in threshold values. For WBGT (Fig. 2(a)) with threshold of 33.0 °C, the RRI of heat-related hospital admissions (73%) and heat-related emergency visits (242%) are numerically much higher than that of all-cause mortality (9%). The same pattern is observed for T (Fig. 2(b)) with threshold of 34.0 °C and AT (Fig. 2(c)) with threshold of 37.5 °C. In addition, the rapid increase in RRIs for these three different health outcomes occurred between WBGT threshold at 32.0 °C and 33.0 °C. During the period of 2000–2014, WBGT of 32.0 °C and 33.0 °C correspond to 89.8 percentile and 99.6 percentile, respectively. For T, the rapid increase in RRIs occurred between thresholds of 33.0 °C and 34.0 °C for all-cause mortality and heat-related emergency visits only. Temperature of 33.0 °C and 34.0 °C correspond to 94.1 percentile and 99.8 percentile, respectively during 2000–2014. For AT, the rapid increase in RRIs occurred between thresholds of 36.0 °C and 37.5 °C for all-cause mortality and heat-related emergency visits only, which correspond to 90.6 percentile and 99.9 percentile, respectively for 2000–2014.
Fig. 2.
Risk ratio increments (%) of different threshold candidates for (a) WBGT, (b) T, and (c) AT, compared with those of the reference threshold (WBGT, 30 °C; T, 30 °C; and AT, 30 °C) for all-cause mortality, heat-related hospital admissions and heat-related emergency visits.
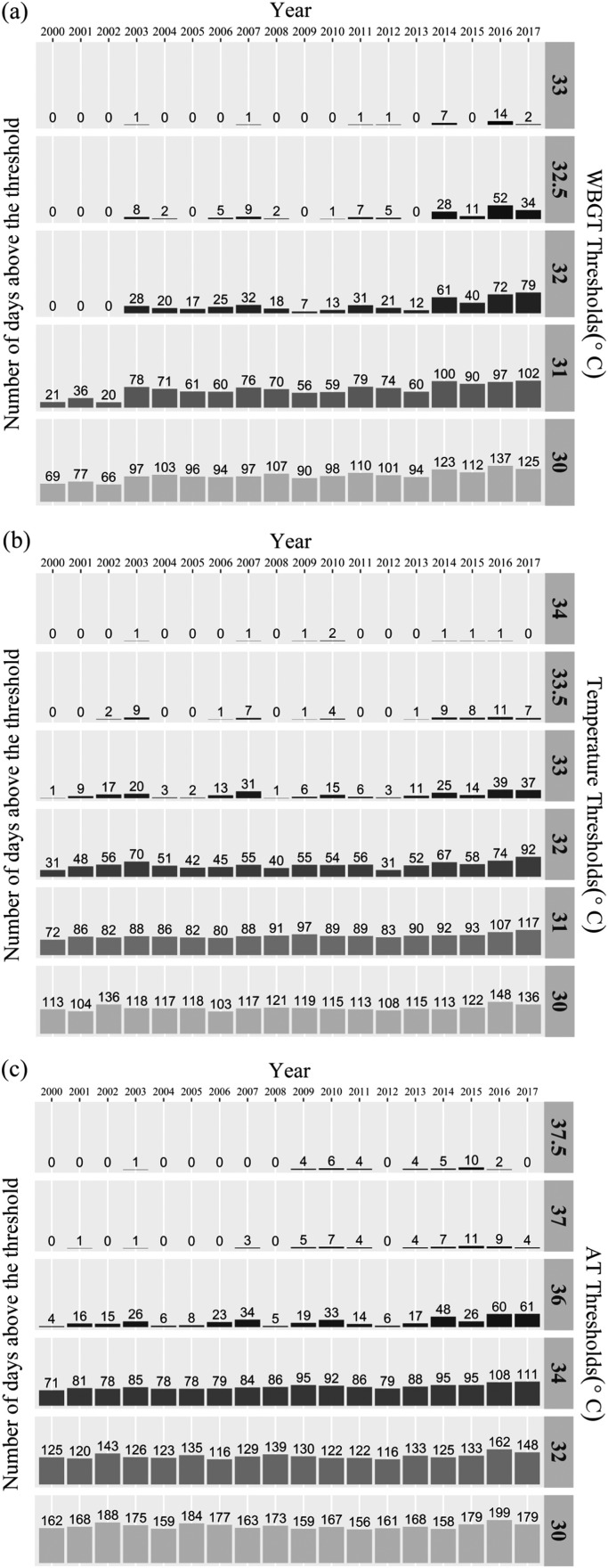
To further evaluate whether the identified thresholds are proper for a heat warning system, the number of days above different threshold values for WBGT, T, and AT between 2000 and 2017 are plotted in Fig. 3(a)-(c), respectively. For better clarity in illustration, only the plots of several selected threshold values are presented. The threshold for a heat warning system can be chosen according to the RRIs and these historical health outcomes with different policy considerations in mind. If preventing increase in all-cause mortality is the policy target and the selected threshold needed to be supported by statistically significant evidence, the choice of threshold for WBGT, T and AT could be 32.5 °C, 33.5 °C and 36.0 °C, respectively. However, it may result in frequent warnings issued. In the cases of WBGT at 32.5 °C and AT at 36.0 °C; there were 52 days in 2016 and 61 in 2017 above these thresholds, respectively. The warm season in Taiwan is usually hot and humid. Too frequent issue of heat warnings may cause the general public to pay no heed to them and pose burden on manpower and resources for supporting heat-health responsive actions associated with warnings. The aforementioned thresholds may be good for heat advisory but not for a heat warning, which should be accompanied with governmental emergency response actions. Thus, an effective heat warning system aiming to prevent increase in heat-related hospital admissions and emergency visits may pick a threshold for an extreme high heat-stress situation; for example, the choice of threshold for WBGT, T and AT could be 33.0 °C, 34.0 °C and 37.5 °C, respectively. The numbers of days exceeding these thresholds in years of 2000–2017 were mostly 0–2 days, with two exceptions for WBGT and six for AT. The highest number of days, 14, occurred in the case of WBGT in 2016 (an El Niño year). For the whole period of 2000–2017, the average days above the thresholds for WBGT, T and AT at 33.0 °C, 34.0 °C and 37.5 °C were 1.5, 0.4, and 2.0 days, respectively (see Table 2 of Appendix C). Thus, the heat-warning system with such thresholds can arouse the attention of the public for proper self-protection and trigger adequate responsive actions from the authorities to reduce causalities under extreme heat-stress events.
Fig. 3.
Number of days with (a) WBGT, (b) T, and (c) AT above the respective threshold candidate in the period of 2000–2017.
4. Discussion
Under the impacts of climate change, high heat-related causality highlights the urgency and importance of establishing a heat warning system with a proper heat indicator and an appropriate threshold. Sustainable Development Goals set by the United Nations call for collaborative actions to face the challenge of changing environments UN (United Nations), 2018. The International Council for Science (ICSU) also strongly encourages scientists collaborating with stakeholders to conduct solution-oriented science, especially to work together with policy-makers in providing sound scientific evidences to support effective mitigation and adaptation policies for the sustainable development of our society (ICSU International Council for Science, 2014). Particularly, in tropical and subtropical zones where the population deem themselves already adapted to hot climate, which is not true as shown in various studies (Ghumman and Horney, 2016, Sarath Chandran et al., 2017, Sung et al., 2013), people may ignore heat-related health risks. A heat warning system with proper heat indicator and threshold is essential for reducing the negative impact of heat on their health. In the quantitative risk assessment of the climate change effects conducted by the World Health Organization (WHO (World Health Organization), 2014), it was projected that there would be higher excess mortality due to heat-related events in various areas around the world including Europe, North American, Australia, East Asia, and high-income Asia Pacific countries, compared with casualties due to undernutrition and infectious diseases in the 2030 s and 2050 s. An effective heat warning system accompanied with responsive actions is viewed as the critical health adaptation strategy which should be implemented in all countries (Smith et al., 2014). The lack of a systematic methodology for selecting a proper threshold for heat warnings hinders the authorities worldwide in setting up a heat warning system. This study presents a straightforward systematic approach to selecting the appropriate threshold for warning the public so as to reduce health risks of heat stress under climate change.
The proposed approach examines historical heat-health relationships using a modified GAM, evaluates increments in RR, assesses frequency of days above certain threshold candidates, and presents analysis results graphically for easy understanding by stakeholders (policy-makers and the general public). The candidate with the maximum RRI and proper occurring frequency is potentially the best threshold. It can be adopted by the authority in any country in establishing a heat warning system for different heat indicators with any health outcome records available. The modified form of GAM successfully obtained the slope of heat-health relationship above any specified threshold, which could be chosen according to a given percentile or any set value, giving the regulatory authority a flexibility to test any threshold candidate in mind. This model provides a way to compare RRs of different threshold candidates. After comparing with the RR of the reference, RRI of any threshold candidate can be presented graphically to facilitate threshold selection. The emphasis on “increments” in RR rather than RR itself is a critical concept different from previous heat-health evaluations. The rising trend of increments confirmed the significant health impacts of heat-stress represented by the selected heat indicator. The point at which the heat indicator had the maximum RRI could be taken as the proper threshold of a heat warning system. The health risk above this threshold could be reduced if the heat warning system is accompanied with an effective intervention action plan. The graphic presentation of the RRI trends will guide policy-makers in selecting the proper threshold for different policy considerations. With the frequency of occurrence above the specified threshold assessed, a proper threshold of a heat warning system can be selected according to the discretion of the authority. Policy considerations may involve reducing heat-related mortality or morbidity, establishing tiered advisory/warning system or not, frequency of warnings issued, and the corresponding intervention plans, which are beyond the scope of this manuscript. Nevertheless, the proposed approach provides policy-makers a systematic scientific tool for considering those factors in the light of sound scientific evidences. This analysis used 15 years of meteorological and health data of Taiwan for demonstration. Only data of warm seasons were included; hence, no seasonal effect needed to be considered. The results clearly show the feasibility and flexibility of the proposed approach. In view of climate changes, periodical evaluations should be conducted to update the chosen threshold.
Compared with traditional graphic presentation of the change point of spline functions of health outcomes, the proposed approach using quantitative RRIs to select thresholds have two advantages. First, thresholds obtained from spline functions are usually too low, resulting in too frequent warnings, which can be avoided by the proposed approach. Secondly, it is easier to communicate to the general public with a quantitative value of RRI of the chosen threshold, rather than a mere graphic presentation of a spline curve, for demonstrating increase in heat-related health risks. Lagged effect which used to be adopted for evaluating excess deaths or cases after extreme heat events was found to be weak, and hence not considered in the final selection criteria. For issuing a heat warning system in advance, the most important consideration is to minimize heat exposure and health impacts occurring on the event days. If heat warnings can be accompanied with effective heat-health intervention programs, heat exposure on the event days could be reduced and there would be no (or very minor) lagged effects that have to be taken into account.
Three types of health data were used, representing two extremes of heat-related health outcomes. All-cause mortality was the most general and the most commonly used health outcome for evaluating heat-health relationship; while heat-related hospital admissions and emergency visits were the morbidity specific to heat-stress. Heat-related mortality was not included due to limited number of cases possibly because the deceased had other types of complication and may not be classified as heat-related deaths. A heat warning system developed on the basis of mortality or morbidity represents different policy considerations. If only statistically significant RRI was considered, the choice of threshold according to mortality and morbidity (heat-related hospital admissions and emergency visits) would not be the same. The threshold for WBGT, T and AT would respectively be 32.5 °C, 33.5 °C and 36.0 °C chosen on the basis of mortality, but 33.0 °C, 34.0 °C, and 37.5 °C selected in terms of morbidity. Moreover, the RRI trends of heat-related emergency visits were similar among WBGT, T, and AT; all showing dramatic increase at 33 °C, 34 °C, and 37.5 °C, respectively, much higher than those of all-cause mortality and heat-related hospital admissions. Thus, heat-related emergency visits, if available, could be the initial choice of health outcome in evaluating proper thresholds. These results demonstrate the wide applicability of this approach, covering health records of mortality and morbidity.
As shown in Fig. 2(a), the increments of all three health outcomes almost doubled from WBGT at 32.5 °C to WBGT at 33 °C; and the patterns were consistent among all three health outcomes. Thus, regardless of the health outcome considered, the same threshold of 33 °C would be chosen. Note that the RRs of WBGT at 33 °C were not statistically significant, which may be due to the limitation of sample size or certain adaptation behaviors (e.g., turning on air-conditioning) under such high heat-stress condition. It should be emphasized that “statistical significance” is an important criterion in academic publications, while it serves merely as a reference in policy-making. In this work, the rising trend of RRI (30–33 °C) was so obvious that it together with number of days above the threshold supported the adoption of WBGT at 33.0 °C as the threshold of the warning system. For this reason, the recommended threshold for different heat indicators would be WBGT at 33.0 °C, T at 34.0 °C, and AT at 37.5 °C, regardless whether the results are statistically significant. By choosing these thresholds, mortality and heat-related morbidity could be both reduced by corresponding emergency response actions.
Thresholds for heat-health impacts in Taiwan have been assessed with different heat indicators. Honda et al. considered a daily maximum temperature between 80 and 85 percentiles of daily maximum temperatures as the best climate index for estimation of optimal temperature. From 1994–2007, the optimal temperature for the three biggest cities in Taiwan ranged from 31.2 °C to 33.4 °C (Honda et al., 2007, Honda et al., 2013). In agreement with these findings, the present results also revealed increases in RR above 30 °C, but the temperature threshold of a warning system chosen in this work is even higher, 34 °C. In addition, Chung et al. (2009) took daily maximum AT of 31.5 °C as the threshold of heat-health relationship in summer Taipei (the biggest city in Taiwan) with the daily mortality risk of 5.1% (3.1–7.2%) per 1 °C increment. This work also found an increased risk of 5% (3–7%) per 1 °C increment above AT of 36 °C for the whole Taiwan region. Furthermore, studies have shown that the impacts of heat indicators on all-cause mortality and all-cause outpatient visits started emerging in the temperature range of 25–30 °C in Taiwan (Lin et al., 2011, Lin et al., 2012). Again, these previously determined lower thresholds further demonstrated that prior research focused only on identifying thresholds of heat-health impacts rather than thresholds of a heat warning system.
Related literature (Honda et al., 2007, Li et al., 2015, Petitti et al., 2016, Tong et al., 2014) either identified thresholds for increase in health outcomes with heat indicator rather than thresholds of a heat warning system or selected them on the basis of percentiles of occurrence frequency with health outcome evidences but without comparison among different percentiles. In contrast, the present approach systematically evaluated RRIs of a series of threshold candidates with a complement assessment of occurrence frequency of days exceeding these threshold candidates in previous years. Quantitative RRIs of different threshold candidates were presented graphically; thus, even by visual examination, a threshold suitable for regulatory purposes can be identified. It has the advantages of providing health outcome evidences and frequency of occurrence for this specified threshold of a heat warning system.
Besides studies focusing on the threshold of heat outcomes, there have also been attempts made to identify thresholds for heat-health intervention measures. For example, with data from USA, Petitti et al. (2016) evaluated comprehensively 10 different types of health outcomes using six heat indicators (minimum/mean/maximum of temperature and heat index which considers temperature and relative humidity), and tried to identify multiple trigger points at which heat-health intervention measures might be activated. They defined minimal risk temperature as the temperature of minimum mortality, and used 95% confidence interval as a criterion for selecting increasing risk temperature and excess risk temperature according to the RR of a given health outcome (Petitti et al., 2016). They obtained different increasing risk temperatures and excess risk temperatures from different health outcomes. While only three health outcomes were assessed in this work, the proposed approach emphasized RRI and selected the proper threshold with a more straightforward way using visual inspection of the rising trend of RRI without requiring statistical significance which conceptually is difficult to communicate to stakeholders. With the proposed approach, the same threshold for heat warning was selected regardless of health outcomes considered for the chosen heat indicator, demonstrating the robustness of the approach in determining the same threshold from different health records for the specified heat indicator.
Additionally, Tong et al. (2014) also assessed RR of daily mortality and emergency hospital admissions of previous heatwave events in Brisbane, Australia and proposed a tiered heat warning system according to health risks under a heatwave. Their method required first the identification of heatwave events, where are defined as two or more consecutive days with the mean temperature above a certain percentile. This study evaluated thresholds of the heat indicator in one day only; our future work will aim to evaluate thresholds of the heat indicator for two or more consecutive days. The present results showed that the proposed approach can be applied to a tiered warning system mentioned by Tong et al. (2014). For example, thresholds identified by statistically significant RRs selected on the basis of mortality and morbidity can be adopted to define a tiered heat warning system with separate thresholds ideal for heat advisory and heat warning, respectively.
Furthermore, most previous studies on heat-health relationships or heat warning system used temperature as the heat indicator (Ye et al., 2012, Gasparrini et al., 2015, Petitti et al., 2016). However, temperature alone is not a good indicator for heat stress. This work compared heat-health evaluations using WBGT, T and AT; and found that RRIs of WBGT were more consistent than those of T and AT. For AT, there was even a dip at 37 °C for all-cause mortality and hospital admissions. WBGT showed a clearer increasing trend for the three health outcomes than T and AT, revealing that WBGT is a more suitable heat indicator. As mentioned above, WBGT comprises four essential meteorological parameters associated with heat stress. Prior research has also demonstrated that WBGT is a good indicator of heat stress for the general public (Lin et al., 2012, Lee et al., 2016). In view of the above, WBGT is recommended as the apt heat indicator for a heat warning system.
Most heat-health relationships focusing on mortality found the elderly population most vulnerable (Astrom et al., 2011, Changnon et al., 1996, Le Tertre et al., 2006). Some previous works also indicated children as one of the vulnerable populations for heat stress (Xu et al., 2012). Our findings echo both. The results of all-cause mortality with WBGT, T, and AT all showed the highest RRs in the age group above 65, while heat-related hospital admissions and emergency visits had the highest RRs in the group aged 0–14 for all three heat indicators. These findings emphasized that not only the elderly but also the young need a better heat adaptation strategy to reduce their health risks. A proper heat warning system is an essential heat adaptation strategy to alert them to take actions for self-protection and for healthcare workers to pay special attention to those vulnerable groups. Moreover, although the RRs of the heat-health relationships for those aged 15–64 were usually the lowest among the three age groups, the total numbers of heat-related hospital admissions and emergency visits for those aged 15–64 were the highest, accounting for almost 90% of the cases (Table 1). Therefore, heat adaptation strategy to reduce the health risks for this age group is also important.
In summary, the aforementioned results demonstrated the following. First, a proper threshold for a heat warning system can be identified through evaluating both RRI of different threshold candidates in heat-health relationships and the occurrence frequency of days exceeding these threshold candidates in previous years. Threshold for a heat warning system can be selected on the basis of these sound scientific evidences and policy considerations. Secondly, the threshold candidates of the specified heat indicator with the maximum RRIs were consistent among different health outcomes (Fig. 3), namely, all-cause mortality, hospital admissions, and emergency visits, even though the numerical incremental change varied among different health outcomes. In this work, WBGT at 33.0 °C, T at 34.0 °C, and AT at 37.5 °C were the points with the maximum RRI in Taiwan. In other words, for countries with only one of the three health outcome records, applying the proposed methodology can still help identify the cut-point of the specified heat indicator with the maximum RRI for threshold selection. Thirdly, the proposed approach can be applied to different heat indicators, in this case, WBGT, T, and AT. More consistent results and a more obvious rising trend of RRI with increasing threshold were found for WBGT than for T and AT. In addition, WBGT fundamentally considers four important meteorological parameters related to heat stress. Using an inappropriate heat indicator in a warning system may result in high false-negative rate and days with heat-stress being missed, thus rendering the warning ineffective. In view of this, WBGT is recommended as a better heat-stress indicator than the other two for an effective warning system. Fourthly, the proposed approach combined sound scientific facts and easy-to-communicate graphs. That is, heat-health relationships are established using sound scientific methods and the results are presented with straightforward illustrations on RRI. Thresholds can be identified with visual inspection on RRI, which makes easier the communication to the general public and policy-makers. With the heat warning system established, the authorities should formulate effective intervention plans in response to different levels of heat advisory/warning to reduce health risks due to heat stress.
There are two limitations in this study. First, although Taiwan does not have an official heat warning system, the government did send out alert in the daily weather report if the forecasted temperature is high, particularly above 37 °C in the past 4–5 years. The dataset analyzed covers 15 years; and the alert issued in recent years may change people's behaviors and reduce the number of recent cases in the health database. Secondly, adaptation measures taken on hot days in Taiwan were not taken into account. Taiwan has 93% prevalence of air-conditioning (Taiwan National Development Council, 2018). Almost all office buildings during daytime and most households in the evening turn on air-conditioning in summer time. These adaptation measures may affect the analysis, giving statistically insignificant results even in high heat-stress condition.
5. Conclusions
In response to the call from UN and ICSU for solution-oriented research, this study presents a new approach to identifying a proper health-based threshold for a heat warning system. The proposed approach examines heat-health relationships using a modified GAM, compares RRI, assesses occurrence frequency, and presents analysis results graphically. Results showed that RRI of three different health outcomes (all-cause mortality, heat-related hospital admissions, heat-related emergency visits) all consistently identified the same candidate as the appropriate threshold for a specified heat indicator. Heat-related emergency visits gave the most distinctive RRI among the three health records. The recommended thresholds for Taiwan are WBGT at 33.0 °C, T at 34.0 °C, and AT at 37.5 °C. Emergency response actions corresponding to these chosen thresholds could reduce both mortality and heat-related morbidity risks. Among these three heat indicators, WBGT gave more consistent results in RRIs of health outcomes and showed a more obvious rising trend. Although the proposed approach can be applied to any heat indicator, WBGT is recommended as the best for a heat warning system because it considers four essential meteorological parameters for heat stress, namely, T, RH%, wind speed, and solar radiation. Under the trend of climate change, the selection of a proper heat indicator with a proper threshold is crucial for an effective heat warning system to reduce health risks. This work presents a straightforward scientific tool for selecting a proper threshold as the basis of an effective warning system for better heat-stress adaptation of our society.
Acknowledgement
We would like to acknowledge the in-house funding support from the Research Center for Environmental Changes of Academia Sinica in Taiwan and the Academia Sinica thematic project “Integrated Multi-source and High-resolution Heat Wave Vulnerability Assessment of Taiwan (AS-104-SS-A02)”. We also thank the Health and Welfare Data Science Center of the Ministry of Health and Welfare in Taiwan, Taiwan Environmental Protection Administration, and Taiwan Central Weather Bureau for providing data. The contents of this paper are solely the responsibility of the authors and do not represent the official views of the aforementioned institutes and funding agencies.
Acknowledgments
Declaration of competing financial interests
The authors declare no competing financial interests on funding, employment, or personal financial interests. The funding agencies had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Funding
This work was supported by the Research Center for Environmental Changes of Academia Sinica and the Academia Sinica thematic project “Integrated Multi-source and High-resolution Heat Wave Vulnerability Assessment of Taiwan (AS-104-SS-A02)”.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.envres.2018.12.059
Contributor Information
Shih-Chun Candice Lung, Email: sclung@rcec.sinica.edu.tw.
Jing-Shiang Hwang, Email: jshwang@stat.sinica.edu.tw.
Appendix A. Supplementary material
Supplementary material
References
- Astrom D.O., Forsberg B., Rocklov J. Heat wave impact on morbidity and mortality in the elderly population: a review of recent studies. Maturitas. 2011 doi: 10.1016/j.maturitas.2011.03.008. [DOI] [PubMed] [Google Scholar]
- Australian Government - Bureau of Meteorology, 2018. Homepage: Heatwave Service for Australia. Available: 〈http://www.bom.gov.au/australia/heatwave/index.shtml〉 (Accessed 11 May 2018).
- Bai L., Ding G., Gu S., Bi P., Su B., Qin D. The effects of summer temperature and heat waves on heat-related illness in a coastal city of China, 2011–2013. Environ. Res. 2014 doi: 10.1016/j.envres.2014.04.002. [DOI] [PubMed] [Google Scholar]
- Barnett A.G., Hajat S., Gasparrini A., Rocklov J. Cold and heat waves in the United States. Environ. Res. 2012 doi: 10.1016/j.envres.2011.12.010. [DOI] [PubMed] [Google Scholar]
- Bernard T.E. Thermal stress. In: Plog B.A., Quinlan P., editors. Fundamentals of Industrial Hygene. 6th edition. Ill. National Safety Council; Itasca: 2012. pp. 335–361. [Google Scholar]
- Błażejczyk K., Baranowski J., Błażejczyk A. Heat stress and occupational health and safety – spatial and temporal differentiation. Misc. Geogr. - Reg. Stud. Dev. 2014 [Google Scholar]
- Brode P., Fiala D., Lemke B., Kjellstrom T. Estimated work ability in warm outdoor environments depends on the chosen heat stress assessment metric. Int. J. Biometeorol. 2018 doi: 10.1007/s00484-017-1346-9. [DOI] [PubMed] [Google Scholar]
- Changnon S.A., Kunkel K.E., Reinke B.C. Impacts and responses to the 1995 heat wave: a call to action. B Am. Meteorol. Soc. 1996;77:1497–1506. [Google Scholar]
- Chung J.Y., Honda Y., Hong Y.C., Pan X.C., Guo Y.L., Kim H. Ambient temperature and mortality: an international study in four capital cities of East Asia. Sci. Total Environ. 2009 doi: 10.1016/j.scitotenv.2009.09.009. [DOI] [PubMed] [Google Scholar]
- Chung Y., Lim Y.H., Honda Y., Guo Y.L., Hashizume M., Bell M.L. Mortality related to extreme temperature for 15 cities in Northeast Asia. Epidemiology. 2015 doi: 10.1097/EDE.0000000000000229. [DOI] [PubMed] [Google Scholar]
- Coccolo S., Kämpf J., Scartezzini J.-L., Pearlmutter D. Outdoor human comfort and thermal stress: a comprehensive review on models and standards. Urban Clim. 2016 [Google Scholar]
- Gasparrini A., Armstrong B. The impact of heat waves on mortality. Epidemiology. 2011 doi: 10.1097/EDE.0b013e3181fdcd99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A., Guo Y., Hashizume M., Lavigne E., Zanobetti A., Schwartz J. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015 doi: 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghumman U., Horney J. Characterizing the impact of extreme heat on mortality, Karachi, Pakistan, June 2015. Prehosp. Disaster Med. 2016 doi: 10.1017/S1049023X16000273. [DOI] [PubMed] [Google Scholar]
- Gosling S.N., Lowe J.A., McGregor G.R., Pelling M., Malamud B.D. Associations between elevated atmospheric temperature and human mortality: a critical review of the literature. Clim. Change. 2009 [Google Scholar]
- Guo Y., Gasparrini A., Armstrong B., Li S., Tawatsupa B., Tobias A. Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology. 2014 doi: 10.1097/EDE.0000000000000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honda Y., Kabuto M., Ono M., Uchiyama I. Determination of optimum daily maximum temperature using climate data. Environ. Health Prev. Med. 2007 doi: 10.1265/ehpm.12.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honda Y., Kondo M., McGregor G., Kim H., Guo Y.L., Hijioka Y. Heat-related mortality risk model for climate change impact projection. Environ. Health Prev. Med. 2013 doi: 10.1007/s12199-013-0354-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyatt O.M., Lemke B., Kjellstrom T. Regional maps of occupational heat exposure: past, present, and potential future. Glob. Health Action. 2010 doi: 10.3402/gha.v3i0.5715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICSU (International Council for Science), 2014. Future earth 2025 vision. Available: 〈www.futureearth.org/〉 (Accessed 11 May 2018).
- IPCC (Intergovernmental Panel on Climate Change) In: Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Field C.B., Barros V.R., Dokken D.J., Mach K.J., Mastrandrea M.D., Bilir T.E., Chatterjee M., Ebi K.L., Estrada Y.O., Genova R.C., Girma B., Kissel E.S., Levy A.N., MacCracken S., Mastrandrea P.R., White L.L., editors. Cambridge University Press; Cambridge, United Kingdom and New York, NY, USA: 2014. p. 1132. [Google Scholar]
- ISO (International Standards Organization), 2017. Ergonomics of the thermal environment – assessment of heat stress using the WBGT (wet bulb globe temperature) index. Available: 〈https://www.iso.org/standard/67188.html〉 (Accessed 11 May 2018).
- Japanese Ministry of the Environment, 2018. Homepage: Heat illness prevention information. Available: 〈http://www.wbgt.env.go.jp/en/〉 (Accessed 11 May 2018).
- Kaiser R., Le Tertre A., Schwartz J., Gotway C.A., Daley W.R., Rubin C.H. The effect of the 1995 heat wave in Chicago on all-cause and cause-specific mortality. Am. J. Public Health 97. 2007;Suppl 1:S158–S162. doi: 10.2105/AJPH.2006.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakamu T., Wada K., Smith D.R., Endo S., Fukushima T. Preventing heat illness in the anticipated hot climate of the Tokyo 2020 summer Olympic Games. Environ. Health Prev. Med. 2017;22:68. doi: 10.1186/s12199-017-0675-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowlton K., Rotkin-Ellman M., King G., Margolis H.G., Smith D., Solomon G. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ. Health Perspect. 2009;117:61–67. doi: 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Tertre A., Lefranc A., Eilstein D., Declercq C., Medina S., Blanchard M. Impact of the 2003 heatwave on all-cause mortality in 9 French cities. Epidemiology. 2006 doi: 10.1097/01.ede.0000187650.36636.1f. [DOI] [PubMed] [Google Scholar]
- Lee K.L., Chan Y.H., Lee T.C., Goggins W.B., Chan E.Y. The development of the Hong Kong Heat Index for enhancing the heat stress information service of the Hong Kong Observatory. Int. J. Biometeorol. 2016;60:1029–1039. doi: 10.1007/s00484-015-1094-7. [DOI] [PubMed] [Google Scholar]
- Li M., Gu S., Bi P., Yang J., Liu Q. Heat waves and morbidity: current knowledge and further direction - a comprehensive literature review. Int. J. Environ. Res. Public Health. 2015;12:5256–5283. doi: 10.3390/ijerph120505256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liljegren J.C., Carhart R.A., Lawday P., Tschopp S., Sharp R. Modeling the wet bulb globe temperature using standard meteorological measurements. J. Occup. Environ. Hyg. 2008;5:645–655. doi: 10.1080/15459620802310770. [DOI] [PubMed] [Google Scholar]
- Lin Y.K., Ho T.J., Wang Y.C. Mortality risk associated with temperature and prolonged temperature extremes in elderly populations in Taiwan. Environ. Res. 2011 doi: 10.1016/j.envres.2011.06.008. [DOI] [PubMed] [Google Scholar]
- Lin Y.K., Chang C.K., Li M.H., Wu Y.C., Wang Y.C. High-temperature indices associated with mortality and outpatient visits: characterizing the association with elevated temperature. Sci. Total Environ. 2012 doi: 10.1016/j.scitotenv.2012.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mastrangelo G., Fedeli U., Visentin C., Milan G., Fadda E., Spolaore P. Pattern and determinants of hospitalization during heat waves: an ecologic study. BMC Public Health. 2007 doi: 10.1186/1471-2458-7-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michelozzi P., de' Donato F.K., Bargagli A.M., D'Ippoliti D., De Sario M., Marino C. Surveillance of summer mortality and preparedness to reduce the health impact of heat waves in Italy. Int. J. Environ. Res. Public Health. 2010 doi: 10.3390/ijerph7052256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan W.-H., Li L.-A., Tsai M.-J. Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet. 1995 doi: 10.1016/s0140-6736(95)90341-0. [DOI] [PubMed] [Google Scholar]
- Pascal M., Laaidi K., Ledrans M., Baffert E., Caserio-Schonemann C., Le Tertre A. France's heat health watch warning system. Int. J. Biometeorol. 2006 doi: 10.1007/s00484-005-0003-x. [DOI] [PubMed] [Google Scholar]
- Petitti D.B., Hondula D.M., Yang S., Harlan S.L., Chowell G. Multiple trigger points for quantifying heat-health impacts: new evidence from a hot climate. Environ. Health Perspect. 2016 doi: 10.1289/ehp.1409119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarath Chandran M.A., Subba Rao A.V.M., Sandeep V.M., Pramod V.P., Pani P., Rao V.U.M. Indian summer heat wave of 2015: a biometeorological analysis using half hourly automatic weather station data with special reference to Andhra Pradesh. Int. J. Biometeorol. 2017 doi: 10.1007/s00484-016-1286-9. [DOI] [PubMed] [Google Scholar]
- Semenza J.C., Rubin C.H., Falter K.H., Selanikio J.D., Flanders W.D., Howe H.L. Heat-related deaths during the July 1995 heat wave in Chicago. N. Engl. J. Med. 1996 doi: 10.1056/NEJM199607113350203. [DOI] [PubMed] [Google Scholar]
- Semenza J.C., McCullough J.E., Flanders W.D., McGeehin M.A., Lumpkin J.R. Excess hospital admissions during the July 1995 heat wave in Chicago. J. Prev. Med. 1999 doi: 10.1016/s0749-3797(99)00025-2. [DOI] [PubMed] [Google Scholar]
- Sheridan S.C., Lin S. Assessing variability in the impacts of heat on health outcomes in New York City over time, season, and heat-wave duration. Ecohealth. 2014 doi: 10.1007/s10393-014-0970-7. [DOI] [PubMed] [Google Scholar]
- Smith K.R., Woodward A., Campbell-Lendrum D., Chadee D.D., Honda Y., Liu Q. Human health: impacts, adaptation, and co-benefits. In: Field C.B., Barros V.R., Dokken D.J., Mach K.J., Mastrandrea M.D., Bilir T.E., Chatterjee M., Ebi K.L., Estrada Y.O., Genova R.C., Girma B., Kissel E.S., Levy A.N., MacCracken S., Mastrandrea P.R., White L.L., editors. Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press; Cambridge, United Kingdom and New York, NY, USA: 2014. pp. 709–754. [Google Scholar]
- Spector J.T., Sheffield P.E. Re-evaluating occupational heat stress in a changing climate. Ann. Occup. Hyg. 2014 doi: 10.1093/annhyg/meu073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steadman R.G. A universal scale of apparent temperature. J. Clim. Appl. Meteorol. 1984 [Google Scholar]
- Sung T.I., Wu P.C., Lung S.C., Lin C.Y., Chen M.J., Su H.J. Relationship between heat index and mortality of 6 major cities in Taiwan. Sci. Total Environ. 2013 doi: 10.1016/j.scitotenv.2012.09.068. [DOI] [PubMed] [Google Scholar]
- Taiwan National Development Council, 2018. Government website open information announcement. Available: 〈https://data.gov.tw/en〉 (Accessed 11 May 2018).
- Tong S.L., Wang X.Y., FitzGerald G., McRae D., Neville G., Tippett V. Development of health risk-based metrics for defining a heatwave: a time series study in Brisbane, Australia. BMC Public Health. 2014 doi: 10.1186/1471-2458-14-435. (Online May) [DOI] [PMC free article] [PubMed] [Google Scholar]
- UN (United Nations), 2018. Sustainable Development Goals (SDGs). Available: 〈https://www.un.org/sustainabledevelopment/〉 (Accessed 11May 2018).
- WHO (World Health Organization) Quantitative risk assessment of the effects of climate change on selected causes of death. In: Hales S., Kovats S., Lloyd S., Campbell-Lendrum D., editors. 2030s and 2050s. World Health Organization (WHO); 2014. [Google Scholar]
- Williams S., Nitschke M., Sullivan T., Tucker G.R., Weinstein P., Pisaniello D.L. Heat and health in Adelaide, South Australia: assessment of heat thresholds and temperature relationships. Sci. Total Environ. 2012 doi: 10.1016/j.scitotenv.2011.11.038. [DOI] [PubMed] [Google Scholar]
- WMO and WHO (World Meteorological Organization and World Health Organization) In: Heatwaves and Health: Guidance on Warning-System Development. McGregor G.R., Bessemoulin P.E., K., Menne B., editors. World Meteorological Organization(WMO); 2015. [Google Scholar]
- Wood S.N. Chapman and Hall/CRC; 2006. Generalized Additive Models: An Introduction with R. [Google Scholar]
- Xia Y., Li Y., Guan D., Tinoco D.M., Xia J., Yan Z. Assessment of the economic impacts of heat waves: a case study of Nanjing, China. J. Clean. Prod. 2018 [Google Scholar]
- Xu Z., Etzel R.A., Su H., Huang C., Guo Y., Tong S. Impact of ambient temperature on children's health: a systematic review. Environ. Res. 2012;117:120–131. doi: 10.1016/j.envres.2012.07.002. [DOI] [PubMed] [Google Scholar]
- Yaglou C.P., Minard D., 1956. Prevention of heat casualties at marine corps training centers. Armed Services Technical Information Agency Document Service Center AD099920.
- Yamamoto S., Iwamoto M., Inoue M., Harada N. Evaluation of the effect of heat exposure on the autonomic nervous system by heart rate variability and urinary catecholamines. J. Occup. Health. 2007 doi: 10.1539/joh.49.199. [DOI] [PubMed] [Google Scholar]
- Ye X., Wolff R., Yu W., Vaneckova P., Pan X., Tong S. Ambient temperature and morbidity: a review of epidemiological evidence. Environ. Health Perspect. 2012 doi: 10.1289/ehp.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material