Abstract
BACKGROUND
PrEP-001 Nasal Powder, a proprietary formulation of polyriboinosinic and polyribocytidylic acid effectively elicits a cellular innate immune response in nasal epithelium. The aim of these 2 studies was to investigate the safety and efficacy of PrEP-001 prophylaxis against rhinovirus (HRV-A16) and influenza-A (H3N2-IAV).
METHODS
Healthy subjects randomly received 2 doses of PrEP-001 or placebo, 48 and 24 h pre-challenge with 10 TCID50 of HRV-A16 (Study 1) or H3N2-IAV (Study 2).
RESULTS
In Study 1, PrEP-001 reduced median total symptom score from 38.5 to 4.5 (p = 0.004), median symptom duration from 6.0 to 1.7 days and median mucus production from 15 g to 3 g. The percentage of subjects classified as ill was reduced 3-fold (placebo 73%, PrEP-001 23%, p = 0.002). In Study 2, PrEP-001 reduced median total symptom score from 8.0 to 4.1 (p = 0.021), median symptom duration from 4.6 to 3.7 days and median mucus production from 3.6 g to 1.5 g. The percentage of subjects classified as ill was reduced 2-fold (placebo 48%, PrEP-001 24%, p = 0.064). PrEP-001 reduced peak viral shedding in both studies, as assessed by qRT-PCR of nasal lavage. Seroconversion rates were comparable between placebo and PrEP-001 (Study 1: 77% [both arms]; Study 2: placebo 73%, PrEP-001 80%). PrEP-001 was well-tolerated, with no clinically significant adverse events.
CONCLUSIONS
PrEP-001 reduced the number of individuals with clinical illness and attenuated severity and duration of HRV-A16 and H3N2-IAV infections without compromising seroconversion, and was well-tolerated. This supports further evaluation of PrEP-001 as a potential pan-viral prophylaxis for upper respiratory tract infections.
CLINICAL TRIAL REGISTRATION
Study 1, HRV-A16 study: EudraCT Number 2012-005579-14 (study conducted before ClinicalTrials.gov registration required). Study 2, H3N2-IAV study: EudraCT Number 2015-002895-26 and ClinicalTrials.gov: NCT03220048.
Keywords: Upper respiratory viral infections, Nasal, Innate immune response, Poly I:C, Prophylaxis, Viral disease
1. Background
Hundreds of millions of people worldwide suffer upper respiratory viral infections (URVIs) annually. They are caused by a wide range of viruses that are generally divided into influenza and non-influenza illnesses, the latter usually being referred to simply as the ‘common cold’, the most common human viral affliction (Eccles, 2005). Common colds and ‘flus share common symptoms including sore throat, cough, nasal congestion, and rhinorrhea. Generally, viral transmission is via contaminated surfaces or aerosols of viral particles (Fiore et al., 2011; Turner, 2007; Turner et al., 2007; Eccles, 2007) and, although variable in terms of pathogenesis, epidemiology and temporal appearance, their manifestations are similar. Most cases of URVIs are self-limiting, causing minor illness before the patient fully recovers.
However, serious illness can develop, especially among certain high-risk groups, such as the very young, elderly, adults with underlying respiratory conditions, and immunosuppressed patients (Chidekel et al., 1997; Ghosh et al., 1999; Kim and Hodinka, 1998), resulting in an annual estimated total economic burden of $40 billion in the USA for non-influenza infections (Fendrick et al., 2003) and $87.1 billion attributable to annual influenza epidemics (Molinari et al., 2007).
Viral pathogens primarily responsible for the common cold are Picornaviridae (mostly rhinoviruses), Coronaviridae, and Adenoviridae. During the peak season, up to 80% of URVIs may be the result of rhinoviruses (Turner, 2007; Turner et al., 2007). Human rhinovirus (HRV) infection accounts for around 50% of asthma and chronic obstructive pulmonary disease (COPD) exacerbations, occasionally leading to serious complications, such as pneumonia (Tan et al., 2003). Currently, no approved vaccines or direct-acting antivirals exist for the prevention or treatment of rhinovirus, coronavirus, adenovirus or the other etiologic agents of the common cold, and available medications can only provide symptomatic relief (National Institute of Allergy and Infectious Diseases). Regarding influenza, in addition to the seasonal influenza vaccine, there are approved antiviral treatments (e.g. oseltamivir), although each has notable limitations.
During a typical URVI, the virus enters the nasal epithelium and replicates rapidly, spreading throughout the upper respiratory system within 24–72 h. As the viral proteins and virus particles appear on the surface of the epithelial cells, the adaptive immune system begins the process of selecting and expanding the T- and B-cells necessary to eliminate the infected epithelial cells and block re-infection by free virus (via neutralizing antibodies), respectively. The innate immune response acts rapidly as a first-line defence to prevent viral invasion or replication before protection by the adaptive immune system occurs. In the cellular innate immune response, pattern recognition receptors (PRRs) are engaged to detect specific viral components, such as viral RNA or DNA, or viral replication intermediates. In the case of URVIs, caused mostly by RNA viruses or involving double-stranded RNA intermediates, the key PRRs are Toll-like Receptor 3 (TLR3) and two Rig-like helicases, retinoic acid-inducible gene I (RIG-I) and Melanoma Differentiation-Associated protein 5 (MDA-5) (Pichlmair et al., 2009). Once activated, the PRRs precipitate a cascade of signalling events leading to a pleiotropic response that inhibits viral replication within the cell (Thompson et al., 2011), signals neighbouring cells rendering them refractory to viral invasion (Takeuchi and Akira, 2010), and enhances migration of immune system cells into the area (Koyama et al., 2008; Mogensen, 2009; Slater et al., 2010). Once the infection has been cleared, T- and B-cells provide a ‘memory’ of the infection, which confers immunity to the specific virus lasting years.
PrEP-001 (previously JNJ-43260295) Nasal Powder, is a dry powder proprietary formulation of polyinosinic and polycytidylic acid, sodium salt (poly I and poly C). Applied nasally, PrEP-001 or Poly I:C, is an effective immunomodulator currently in development for pan-viral prophylaxis against the common cold and influenza illness. Poly I:C is a well-established synthetic double-stranded RNA that acts as a viral genome surrogate and activates the antiviral response of the cellular innate immune system by stimulating the PRRs Rig-1, MDA-5, and TLR3 (Caskey et al., 2011; Mian et al., 2013).
Pre-clinical (in-house mouse influenza H1N1 lethal challenge studies, unpublished) and early clinical studies (Single ascending dose, unpublished) suggested PrEP-001 would be a safe and effective prophylaxis for URVIs. Thus, 2 placebo-controlled studies were conducted to further evaluate the effects of PrEP-001 in healthy volunteers challenged with either HRV-A16 (Study 1) or H3N2-IAV (Study 2).
2. Methods
These studies were phase Ib/II, double-blind, placebo-controlled trials to examine the efficacy, safety, and tolerability of repeated prophylactic nasal dosing of PrEP-001 in healthy adult subjects who were subsequently inoculated with HRV-A16 (Study 1) or H3N2-IAV (Study 2). These two viral strains were selected as models since HRV-A16 is known to effectively elicit symptomatic colds and H3N2-IAV viruses are circulating in most flu seasons, so they represent frequently occurring strains that are suitable for use in healthy volunteers challenge studies. The HRV-A16 was obtained as a Wild-Type HRV-16 Challenge Virus from Retroscreen Virology Ltd and H3N2-IAV was obtained as a Wild-Type Influenza A/Perth/16/2009 Challenge Virus from Meridian Life Sciences. Both challenge viruses were manufactured under current Good Manufacturing Practice (GMP) and had undergone quality testing by the manufacturer regarding appearance, sterility, infectivity and contaminants according to pre-determined specifications. Before study initiation, independent ethics committee approval was obtained (Study 1 - NRES Committee London - City & East; Study 2 - North East - Newcastle & North Tyneside 2 Research Ethics Committee) and all subjects provided written informed consent prior to their participation. Both studies were conducted at specialised quarantine units in the UK; Study 1 between July 2013 and September 2014, and Study 2 between September 2015 and March 2016.
In Study 1, eligible subjects comprised healthy males or females aged 18–45 years (inclusive), with a body mass index (BMI) between 18 and 28 kg/m2 (inclusive) and body weight ≥50 kg. Study inclusion criteria were similar in Study 2, although subjects up to 55 years were eligible to participate. All subjects were screened for the absence of antibodies to the relevant challenge virus. Subjects were excluded if they had any significant acute or chronic uncontrolled medical illness or had any condition, including a history of abnormal pulmonary function, associated with increased risk of complications of respiratory viral illness or that would make the subject unsuitable for a quarantine challenge study. All subjects were non-smokers and non-atopic. The use of any medication other than the study drug was prohibited, except for hormone replacement therapy (HRT) and contraceptive therapy during the entire quarantine phase of the study.
Both studies followed the same format: screening, prophylaxis/inoculation (within a quarantine environment), and follow-up. Eligible subjects were randomized 1:1, with randomization numbers generated by the sponsor and corresponding to blinded treatment kits that were assigned sequentially in ascending order. The assigned randomization number determined whether a subject was given either 2 doses of PrEP-001 or matching placebo, one dose at 48 h and one dose at 24 h prior to nasal inoculation with 10 TCID50 of either HRV-A16 (Study 1) or H3N2-IAV (Study 2). The 2-dose regimen was chosen based on results from an initial rhinovirus challenge study where a single dose was administered 24 h pre-inoculation (see Additional File 1 for study results, including Additional Fig. 1 and Additional Table 1, Table 2, Table 3 ).
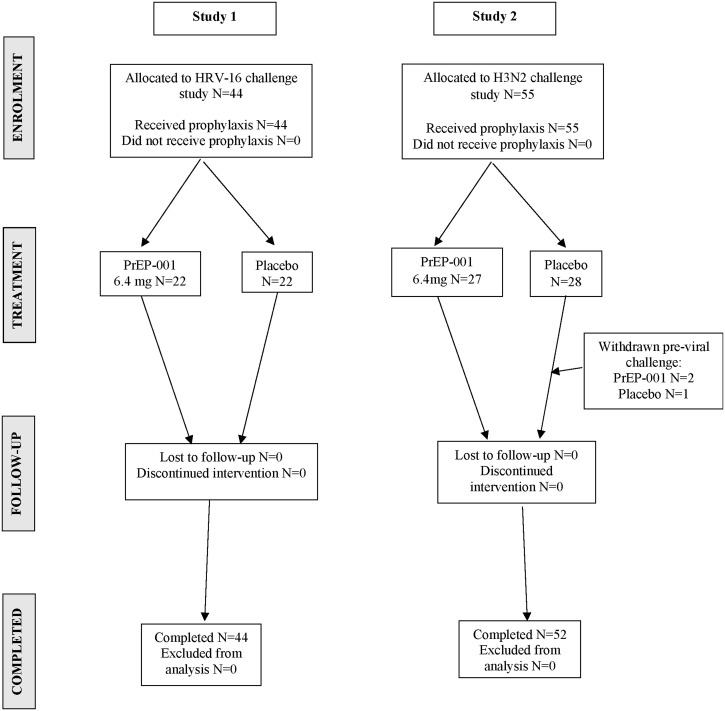
Fig. 1.
CONSORT diagram.
Table 1.
Baseline demographic characteristics.
| Study 1 |
Study 2 |
|||
|---|---|---|---|---|
| PrEP-001 N = 22 | Placebo N = 22 | PrEP-001 N = 27 | Placebo N = 28 | |
| Gender, n (%) | ||||
| Male | 15 (68.2) | 16 (72.7) | 19 (70.4) | 17 (60.7) |
| Female | 7 (31.8) | 6 (27.3) | 8 (29.6) | 11 (39.3) |
| Age | ||||
| Mean (SD) | 24.7 (6.53) | 25.1 (5.76) | 26.4 (5.52) | 26.0 (5.74) |
| Median (range) | 22.5 (20, 44) | 24.0 (18, 44) | 25.0 (19, 41) | 24.0 (19, 41) |
| BMI | ||||
| Mean (SD) | 23.74 (2.492) | 22.92 (2.553) | 23.74 (2.992) | 23.31 (2.976) |
| Median (range) | 23.30 (18.5, 27.8) | 22.90 (19.3, 27.9) | 23.40 (18.0, 30.2) | 23.30 (18.7, 29.2) |
| Race, n (%) | ||||
| White | 20 (90.9) | 21 (95.5) | 25 (92.6) | 21 (75.0) |
| Black | 1 (4.5) | 0 | 0 | 1 (3.6) |
| Other | 1 (4.5) | 1 (4.5) | 2 (7.4) | 6 (21.4) |
| Smoker | ||||
| Yes | 8 (36.4) | 9 (40.9) | 12 (44.4) | 6 (21.4) |
| No | 14 (63.6) | 13 (59.1) | 15 (55.6) | 22 (78.6) |
Table 2.
Summary of total symptom scores (Days 1–8).
| PrEP-001 | Placebo | |
|---|---|---|
| Study 1 | ||
| N | 22 | 22 |
| Median (range) | 4.5 (0–71) | 38.5 (0–106) |
| Mean (SE) | 10.2 (3.89) | 40.6 (7.18) |
| 95% CI | 2.1, 18.3 | 25.7, 55.5 |
| Difference PrEP-001/placebo | −30.4 | |
| 95% CI | −46.9, −13.9 | |
| Study 2 | ||
| N | 25 | 27 |
| Median (range) | 4 (0–39) | 8 (0–92) |
| Mean (SE) | 9.1 (1.83) | 20.6 (3.97) |
| 95% CI | 5.3, 12.9 | 12.3, 28.9 |
| Difference PrEP-001/placebo | −11.5 | |
| 95% CI | −20.1, −2.9 | |
Table 3.
Common treatment-emergent adverse events (reported in >2 subjects in any group).
| n (%) | Study 1 |
Study 2 |
||
|---|---|---|---|---|
| PrEP-001 N = 22 | Placebo N = 22 | PrEP-001 N = 27 | Placebo N = 28 | |
| Any AE | 14 (63.6) | 14 (63.6) | 17 (63.0) | 21 (75.0) |
| ALT increased | 2 (9.1) | 4 (18.4) | 2 (7.4) | 6 (21.4) |
| AST increased | 1 (3.7) | 2 (9.1) | 3 (11.1) | 4 (14.3) |
| CRP increased | 4 (18.2) | 0 | 1 (3.7) | 1 (3.6) |
| Blood cholesterol increased | 0 | 0 | 2 (7.4) | 4 (14.3) |
| aPTT prolonged | 0 | 0 | 2 (7.4) | 4 (14.3) |
| Low density lipoprotein increased | 0 | 0 | 0 | 3 (10.7) |
| Epistaxisa | 8 (36.4) | 8 (36.4) | 0 | 0 |
| Procedural haemorrhage | 0 | 0 | 6 (22.2) | 9 (32.1) |
All AEs shown above were treatment-emergent AEs, i.e. they had an onset on or after the start of PrEP-001 or placebo dosing.
Epistaxis is defined as abrasions caused by the delivery device itself. This and Procedural haemorrhage (as it was labeled in Study 2) were immediate, minor, transient and self-resolving.
In both studies, each nasally administered dose of PrEP-001 was 6.4 mg (4 × 800 μg administrations per nostril using a dry powder applicator). Following inoculation (10 TCID50 in 100 μl administered as two 25 μl instillations per nostril, alternating nostrils between instillations), subjects were observed specifically for potential allergic reactions within 30 min, and for the following 24 h; subjects were then monitored throughout the quarantine period. Subjects completed a modified Jackson questionnaire which assessed 10 symptoms on a 4 point scale, 3 times daily for 8 days. Daily nasal discharge was collected and regular nose and throat lavage samples were taken. Patients returned for follow up 28 days after the study.
The approach in both studies was to assess total symptom score, duration of symptoms, mucus production, viral shedding, seroconversion, and the percentage of subjects with study-defined clinical illness over an 8-day quarantine period. Viral shedding was monitored in nasal lavage by quantitative real-time polymerase chain reaction (qRT-PCR) (Mackay et al., 2002). Safety was assessed throughout the study by the incidence of treatment emergent adverse events (TEAEs) and changes from baseline in routine clinical laboratory parameters, vital signs, physical examination, and 12-lead electrocardiogram (ECG).
2.1. Statistical analysis
With respect to Study 1, since this was an early development, exploratory study, no formal statistical calculations of sample size were conducted and the number of subjects to be included per cohort was deemed sufficient to evaluate the objectives. Similarly, with respect to Study 2, no formal sample size calculation was performed; however the sample size was consistent with a previous HRV-A16 challenge study, with a similar design, conducted at the same unit and the sample size was supported by historical placebo data from previously conducted influenza virus studies. The historical data showed that the within-group coefficient of variation of total symptom score AUC ranged from a minimum of 102% to an average of 120%. Assuming a two-sided t-test with a 5% significance level and 80% power, in order to detect 90% reduction in total symptom score AUC between placebo and PrEP-001, then between 22 and 29 evaluable subjects per treatment group, respectively, were required. Thus, the number of subjects included was deemed sufficient to evaluate the objectives for both studies.
All endpoints were summarized using descriptive statistics. Comparison between groups were made for total symptom scores using Wilcoxon Rank Sum Test, with statistical significance based on the 5% alpha level. Changes in viral load were reported as 95% CIs, and clinical illness was evaluated as relative risks and compared between groups using Fishers Exact Test.
3. Results
3.1. Disposition
Forty-four subjects were enrolled into Study 1 (HRV-A16 challenge virus) and 55 were enrolled into Study 2 (H3N2-IAV challenge virus). All subjects in Study 1 received the viral challenge and completed the study (Fig. 1). In Study 2, three subjects were withdrawn prior to receiving viral challenge (2 subjects had elevated laboratory results and 1 subject was withdrawn due to nasal bleeding) so only 52 subjects received the viral challenge, all of whom completed the study (Fig. 1).
3.2. Demography
In Study 1, 70% of subjects were male, age ranged from 18 to 44 years, BMI ranged 18.5–27.9 kg/m2, and most subjects were white (93%). In Study 2, 65% of subjects were male, age ranged from 19 to 41 years, BMI ranged 18.0–30.2 kg/m2, and most subjects were white (83%). Full demographic details are provided in Table 1. Nasopharyngeal swabs taken from all subjects on admission to the quarantine unit tested negative for the respiratory virus screen and all female subjects had a negative pregnancy test.
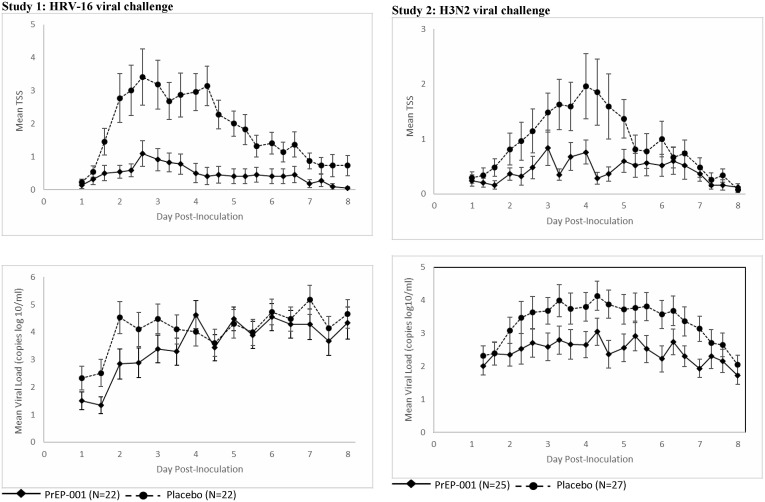
3.3. Total symptom scores
In Study 1, 16 (73%) and 18 (82%) subjects reported any clinical symptoms in the PrEP-001 and placebo arms, respectively. Lower mean overall total symptom scores were observed in the PrEP-001 group compared with placebo (10.2 and 40.6 in PrEP-001 and placebo, respectively), with this difference being statistically significant at the 5% alpha level (Table 2). PrEP-001 also reduced median total symptom score from 38.5 to 4.5 (Wilcoxon Rank Sum Test, p = 0.004). The median duration of symptoms was also reduced to 1.7 days in the PrEP-001 arm compared to 6.0 days in the placebo group.
In Study 2, 18 (72%) and 23 (85%) subjects reported any clinical symptoms in the PrEP-001 and placebo arms, respectively. PrEP-001 prophylaxis resulted in a significantly lower median total symptom score of 4.0 compared to 8.0 for placebo (p = 0.021, Wilcoxon Rank Sum Test).
Furthermore, comparing the upper quartiles of subjects with the most severe symptom scores (median symptom scores of 27.5 and 52.5 for PrEP-001 and placebo, respectively), PrEP-001 prophylaxis demonstrated a comparable 2-fold lower total symptom score (p = 0.03). The median duration of symptoms was 3.7 days in the PrEP-001 arm compared to 4.6 days in the placebo group.
Mean total symptom scores over time for both studies are shown in Fig. 2 .
Fig. 2.
Mean (SE) total symptom scores over time.
3.4. Mucus production
In Study 1, mean mucus production was 5.8 g in the PrEP-001 group compared with 17.3 g in the placebo group. In Study 2, mean mucus production was 4.0 g in the PrEP-001 group compared to 13.4 g in the placebo group.
3.5. Viral load and viral shedding
In Study 1, the mean area under the viral load-time curve was lower in the PrEP-001 group (1970.8) compared to placebo (9031.2), with a difference between the groups of −7060.3 (95% CI: [−13152.5, 968.1]). Time to peak viral shedding was also delayed in the PrEP-001 arm (6.0 days) compared to placebo (4.3 days). In Study 2, the mean area under the viral load-time curve was lower in the PrEP-001 group (23781.6) compared to placebo (32944.4). The time to peak viral shedding was also delayed in the PrEP-001 arm (6.0 days) compared to placebo (3.3 days). In both studies PrEP-001 reduced peak viral shedding.
3.6. Clinical illness rate
A subject was considered to be clinically ill if they had a laboratory-confirmed presence of HRV-A16 (i.e. positive cell culture assay at least once or at least 2 positive detections by PCR assay between Day 1 and day of discharge; or seroconversion) and clinical symptoms, i.e. reporting ≥1 of 4 cold symptoms (runny nose, stuffy nose, sneezing, sore throat) and scoring ≥2 points on a diary card on at least 2 consecutive days. Based on these criteria, in Study 1, 5/22 (22.7%) and 16/22 (72.7%) of subjects were considered clinically ill in the PrEP-001 and placebo arms, respectively. This resulted in an observed relative risk of clinical illness of 31.2% (95% CI [5.2%, 57.3%]). The difference between PrEP-001 and placebo was statistically significant (p = 0.002, Fisher Exact Test). In Study 2, the same criteria were applied for clinical illness, regardless of whether the subject was deemed febrile as many subjects experienced no significant temperature elevation, consistent with literature reports on naturally occurring influenza (Chughtai et al., 2017). Application of this definition yielded 6/25 (24%) and 13/27 (48%) subjects who were considered clinically ill in the PrEP-001 and placebo arms, respectively (p = 0.064, Fisher Exact Test, one-tailed).
3.7. Seroconversion rates
In Study 1, seroconversion was observed in 17 (77.3%) subjects in both the PrEP-001 and placebo groups. Seroconversion rates between the PrEP-001 and placebo arms were also comparable in Study 2 (PrEP-001 12 patients [48%]; placebo 16 patients [59%]).
3.8. Safety
No deaths, serious adverse events (SAEs), or adverse events (AEs) considered to be of severe intensity were reported in either study. No subjects withdrew from Study 1. In Study 2, three subjects were withdrawn prior to receiving the viral challenge: in the PrEP-001 group, 1 subject reported nasal bleeding and another subject had increased CRP; in the placebo group, 1 subject had increased ALT. All AEs leading to withdrawal were considered mild in intensity.
In Study 1, 63.6% of subjects in both treatment groups reported at least one AE and in Study 2, 75.0% of subjects in the placebo group and 63.0% of subjects in the PrEP-001 group reported AEs. The majority of AEs were considered mild in intensity and no AEs were considered severe. The most frequently observed AEs (>2 subjects in any treatment group) in both studies are shown in Table 3. The cases of procedural haemorrhage seen in this study were thought to be as a result of scraping the nasal lining with the delivery device and not the result of the active pharmaceutical ingredient. No reports of nasal irritation or taste sensation were associated with the administration of either the placebo or the active in either study.
In both studies, there was no consistent pattern of clinical concern for any safety laboratory or urinalysis tests. In most cases where abnormalities were noted, these were judged not to be clinically significant. There was no pattern of findings on physical examination, vital signs, or ECG that suggested an adverse effect of PrEP-001 at the end of the quarantine period or at the 28 day follow up. Overall, PrEP-001 was well-tolerated in both viral challenge studies.
4. Discussion
PrEP-001, or Poly I:C, is a well-established synthetic double-stranded RNA that acts as a viral genome surrogate and activates the antiviral response of the cellular innate immune system by stimulating the PRRs Rig-1, MDA-5, and TLR3 (Caskey et al., 2011; Mian et al., 2013). It is a potent immunomodulating agent whose mechanism of action is well characterized (Wong et al., 1995). Upon entering the cell, Poly I:C activates the expression of a number of gene products that renders the host cell refractory to viral replication (Kumar et al., 2006), releases cytokines and chemokines which act in a paracrine fashion to activate the antiviral response in adjacent cells and recruits cells of the adaptive immune system into the area (Kawai and Akira, 2010; Savan, 2014). The prophylactic potential of Poly I:C has been demonstrated using multiple viruses in cell culture (Pan et al., 2012), animal models (Wong et al., 1995), and clinical trials (Lee et al., 2014), however, pharmaceutically useful formulations for nasal application were unavailable.
PrEP-001 Nasal Powder is a proprietary formulation of poly I and poly C that protects the RNA from degradation by ubiquitous RNAses and enhances its retention in the nose and uptake by nasal epithelial cells, as demonstrated by early in-house animal studies. Applied to the nasal cavity, PrEP-001 Nasal Powder adheres to the mucosa allowing the particles to be pynocytosed into nasal epithelial cells where PrEP-001 activates the innate immune response. As a high molecular weight polymer, PrEP-001 remains in the cell and does not enter systemic circulation (DeVincenzo et al., 2008). Within the cell, like all RNAs, it is rapidly degraded into mononucleosides and immediately recycled via cellular nucleoside pools into new cellular RNA molecules (de Clercq, 1979; Nordlund et al., 1970). Consequently, there is no liver burden or potential for hepatic drug-drug interactions, and primary pharmacological effects are localized to the area of application. Finally, as a synthetic, non-coding, non-replicating RNA polymer, there is no risk of unintended amplification (as with an attenuated virus), nor the possibility of protein production that potentially could lead to sensitization upon repeated administration. Taken together, this gives PrEP-001 the appropriate profile for use as a topical prophylactic agent against URVIs. As anticipated by the nature of PrEP-001 itself, and supported by toxicology and initial first-in-human safety studies, PrEP-001 has the exceptionally safe profile suitable for prophylaxis of the common cold.
Based on pre-clinical results, an initial rhinovirus challenge study was conducted. This study was identical to the studies outlined in this paper, however only a single dose was administered 24 h pre-inoculation. Total symptom scores were marginally reduced compared with placebo.
Full details of this single dose study are provided in the Additional File 1, including Additional Fig. 1 and Additional Table 1, Table 2, Table 3. Based on reports in the literature (Stowell et al., 2009), a ‘booster dose’ was proposed, leading to the study design used for the studies reported in this manuscript.
These two randomized, placebo-controlled studies aimed to assess the prophylactic effect of repeated nasal doses of PrEP-001 in healthy volunteers challenged with either HRV-A16 (Study 1) or H3N2-IAV (Study 2). Results from both studies demonstrated a strong prophylactic effect after repeated dosing of PrEP-001 in healthy subjects challenged with either HRV-A16 or H3N2-IAV, with symptom scores, duration of symptoms, mucus production, and viral shedding all being reduced. These findings are significant because PrEP-001 demonstrated effectiveness against two strains of respiratory viruses with different structures, i.e. enveloped and non-enveloped viruses, with different types of RNA genomes and replication schemes, and therefore supports its potential as a pan-viral prophylaxis agent. Furthermore, the percentage of volunteers with study-defined laboratory confirmed illness was reduced by 3-fold in Study 1 and 2-fold in Study 2. It is noteworthy that even those subjects with the most severe symptom scores showed a significant comparative improvement after PrEP-001 treatment (p = 0.03). Seroconversion rates were comparable, suggesting use of PrEP-001 would not prevent the generation of protective long-term memory responses to specific viruses. Finally, PrEP-001 was well-tolerated with no clinically significant AEs observed in either study. However, it is important to acknowledge limitations to the studies since both were small (sample size of approximately 50 subjects per study) and were also conducted under highly controlled conditions (i.e. inoculation timed 24 h after prophylaxis), so further larger scale studies are needed to confirm efficacy and safety in ‘real world’ settings.
Prophylaxis with PrEP-001 (2 doses, 48 and 24 h pre-challenge) proved efficacious for two entirely different viral classes, rhinovirus and influenza-A virus. This suggests that the pleiotropic effects of triggering the innate immune response will be beneficial against many viral pathogens and that PrEP-001 has the potential to be an effective prophylactic agent against upper respiratory viral pathogens.
Although the study size was small and the rhinovirus and influenza challenge models are each sui generis, it would appear that the prophylaxis was more effective against rhinovirus than influenza. Whether this is simply the nature of the innate immune response or a function of the fact that rhinovirus is a temperature-restricted virus (i.e. <34 °C) limited to the upper airways (unlike influenza) is unclear and requires further investigation. Nevertheless, it appears that topical PrEP-001 prophylaxis has the potential to provide broad coverage and impact any viral infection that initiates in the upper respiratory system. Specifically regarding influenza, where a seasonal vaccine is available, PrEP-001 has the potential to augment vaccine protection.
PrEP-001 Nasal Powder as an innate immune system stimulant, should provide protection against all variants of influenza viruses that may not be included in the seasonal vaccine. PrEP-001 also has a rapid onset of efficacy compared with a vaccine (within 24–48 h of dosing). Additionally, it is expected that the cellular innate immune response remains robust with age (Zhao et al., 2012), suggesting that the use of PrEP-001 in the elderly could augment the diminished efficacy of the seasonal influenza vaccine in this population (Weinberger et al., 2008).
In comparison with chemoprophylaxis with neuraminidase inhibitors, PrEP-001 appears, based on the initial challenge study above, to be less effective, however, both oseltamivir and zanamivir, are: 1) limited to influenza (unlike PrEP-001), 2) carry toxicity issues that preclude their extended (seasonal) use, and 3) being direct antivirals, have the potential to select resistant variants. (Gubareva et al., 2000). Although larger, long-term studies have yet to be conducted with PrEP-001, its mechanism of action (i.e. activation of the pleotropic innate immune response), make it unlikely to select for simple resistant variants of influenza or any other upper respiratory virus. Likewise, without longer-term trials it is impossible to predict if there will be toxicity issues with extended administration, however these potential side-effects would undoubtedly be local due to the lack of systemic exposure. Finally, there remains the possibility that long-term exposure may result in tachyphylaxis due to a local down-regulation of the innate response in the nasal lining but this will only become apparent in long-term studies.
5. Conclusion
In conclusion, PrEP-001 attenuated the severity and duration of both HRV-A16 and H3N2-IAV infections and reduced the number of individuals with study-defined laboratory confirmed illness (both common cold and influenza illness) without compromising seroconversion, and was safe and well-tolerated. This supports further evaluation of PrEP-001 as a potential pan-viral prophylaxis for upper respiratory viral infections and may be a novel strategy to improve HRV and influenza control, especially for high-risk populations, such as the elderly and those with underlying respiratory conditions (e.g. asthma and COPD), for whom URVIs present a serious concern.
Ethics approval and consent to participate
Before study initiation, independent ethics committee approval was obtained (Study 1 - NRES Committee London - City & East; Study 2 - North East - Newcastle & North Tyneside 2 Research Ethics Committee) and all subjects provided written informed consent prior to their participation.
Consent for publication
Not applicable.
Availability of data and material
The datasets generated and/or analysed during the current study are not publicly available since the information is confidential and a proprietary part of patent filings. However, the authors are willing to release appropriate information if the request is legitimate and the appropriate confidentiality agreements are in place.
Conflicts of interest
PrEP-001 was developed by Janssen Research & Development and is now being developed by PrEP Biopharm Ltd. All authors are either past or present salaried employees of either Janssen Research & Development or PrEP Biopharm Ltd. BM is also the Chief Scientific Officer for PrEP Biopharm Ltd.
Funding
These studies were funded by PrEP Biopharm Ltd, and Janssen Research & Development, who also designed the study protocols, collected the data and conducted the analyses.
Medical writing support was provide by Debbie Jordan, with funding from PrEP Biopharm, Ltd.
Authors' contributions
Malcolm, B: Conception, design, analysis, and interpretation; drafting and revising; final approval; accountable.
Aerts, C: Acquisition and interpretation; drafting and revising; final approval; accountable.
Dubois, K: Design, analysis and interpretation; drafting and revising; final approval; accountable.
Geurts, F: Interpretation; drafting and revising; final approval; accountable.
Marien, K: Design and acquisition; drafting and revising; final approval; accountable.
Rusch, S: Design, analysis and interpretation; drafting and revising; final approval; accountable.
Van Dijk, A: Acquisition; drafting and revising; final approval; accountable.
Verloes, R: Acquisition and interpretation; drafting and revising; final approval; accountable Vingerhoets, J: Interpretation; drafting and revising; final approval; accountable.
Acknowledgements
The authors would like to sincerely thank the numerous colleagues at Janssen Research & Development who contributed to the preliminary efforts and studies that made these clinical proof of concept studies possible. In addition, many thanks to the staff of hVivo for their careful and meticulous work to bring these studies to fruition. Medical writing support was provide by Debbie Jordan, with funding from PrEP Biopharm, Ltd.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.antiviral.2018.03.005.
List of Abbreviations
- AEs
Adverse events
- AIDS
Acquired immune deficiency syndrome
- ALT
Alanine aminotransferase
- AST
Aspartate aminotransferase
- BMI
Body mass index
- COPD
Chronic obstructive pulmonary disease
- CRP
C-reactive protein
- DNA
Deoxyribonucleic acid
- ECG
Electrocardiogram
- HIV
Human immunodeficiency virus
- HRT
Hormone replacement therapy
- HRV
Human rhinovirus
- MDA-5
Melanoma Differentiation-Associated protein 5
- PrEP-001
Polyinosinic and polycytidylic acid sodium salt (poly I and poly C)
- PRRs
Pattern recognition receptors
- qRT-PCR
Quantitative real-time polymerase chain reaction RIG-I Retinoic acid-inducible gene I
- RNA
Ribonucleic acid
- SAEs
Serious adverse events
- TEAEs
Treatment emergent adverse events
- TLR3
Toll-like Receptor 3
- URVIs
Upper respiratory viral infections
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Caskey M., Lefebvre F., Filali-Mouhim A., Cameron M.J., Goulet J.P., Haddad E.K. Synthetic double-stranded RNA induces innate immune responses similar to a live viral vaccine in humans. J. Exp. Med. 2011;208(12):2357–2366. doi: 10.1084/jem.20111171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chidekel A.S., Rosen C.L., Bazzy A.R. Rhinovirus infection associated with serious lower respiratory illness in patients with bronchopulmonary dysplasia. Pediatr. Infect. Dis. J. 1997;16(1):43–47. doi: 10.1097/00006454-199701000-00010. [DOI] [PubMed] [Google Scholar]
- Chughtai A.A., Wang Q., Dung T.C., Macintyre C.R. The presence of fever in adults with influenza and other viral respiratory infections. Epidemiol. Infect. 2017;145(1):148–155. doi: 10.1017/S0950268816002181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Clercq E. Degradation of poly(inosinic acid) - poly(cytidylic acid) [(I)n - (C)n] by human plasma. Eur. J. Biochem. 1979;93(1):165–172. doi: 10.1111/j.1432-1033.1979.tb12807.x. [DOI] [PubMed] [Google Scholar]
- DeVincenzo J., Cehelsky J.E., Alvarez R., Elbashir S., Harborth J., Toudjarska I. Evaluation of the safety, tolerability and pharmacokinetics of ALN-RSV01, a novel RNAi antiviral therapeutic directed against respiratory syncytial virus (RSV) Antivir. Res. 2008;77(3):225–231. doi: 10.1016/j.antiviral.2007.11.009. [DOI] [PubMed] [Google Scholar]
- Eccles R. Understanding the symptoms of the common cold and influenza. Lancet Infect. Dis. 2005;5(11):718–725. doi: 10.1016/S1473-3099(05)70270-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccles R. Mechanisms of symptoms of the common cold and influenza. Br. J. Hosp. Med. (Lond) 2007;68(2):71–75. doi: 10.12968/hmed.2007.68.2.22824. [DOI] [PubMed] [Google Scholar]
- Fendrick A.M., Monto A.S., Nightengale B., Sarnes M. The economic burden of non- influenza-related viral respiratory tract infection in the United States. Arch. Intern Med. 2003;163(4):487–494. doi: 10.1001/archinte.163.4.487. [DOI] [PubMed] [Google Scholar]
- Fiore A.E., Fry A., Shay D., Gubareva L., Bresee J.S., Uyeki T.M. Antiviral agents for the treatment and chemoprophylaxis of influenza –- recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm. Rep. 2011;60(1):1–24. [PubMed] [Google Scholar]
- Ghosh S., Champlin R., Couch R., Englund J., Raad I., Malik S. Rhinovirus infections in myelosuppressed adult blood and marrow transplant recipients. Clin. Infect. Dis. 1999;29(3):528–532. doi: 10.1086/598627. [see comment] [DOI] [PubMed] [Google Scholar]
- Gubareva L.V., Kaiser L., Hayden F.G. Infuenza virus nuriminidase inhibitors. Lancet. 2000;355:827–835. doi: 10.1016/S0140-6736(99)11433-8. [DOI] [PubMed] [Google Scholar]
- Kawai T., Akira S. The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Nat. Immunol. 2010;11(5):373–384. doi: 10.1038/ni.1863. [DOI] [PubMed] [Google Scholar]
- Kim J.O., Hodinka R.L. Serious respiratory illness associated with rhinovirus infection in a pediatric population. Clin. Diagn Virol. 1998;10(1):57–65. doi: 10.1016/s0928-0197(98)00004-x. [DOI] [PubMed] [Google Scholar]
- Koyama S., Ishii K.J., Coban C., Akira S. Innate immune response to viral infection. Cytokine. 2008;43(3):336–341. doi: 10.1016/j.cyto.2008.07.009. [DOI] [PubMed] [Google Scholar]
- Kumar A., Zhang J., Yu F.S. Toll-like receptor 3 agonist poly(I: C)-induced antiviral response in human corneal epithelial cells. Immunology. 2006;117(1):11–21. doi: 10.1111/j.1365-2567.2005.02258.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee N.L., Wong C.K., Hui D.S., Chan P.K. Role of toll-like receptors in naturally occurring influenza virus infection. Hong Kong Med. J. 2014;20(Suppl. 6):11–15. [PubMed] [Google Scholar]
- Mackay I.M., Arden K.E., Nitsche A. Real-time PCR in virology. Nucleic Acids Res. 2002;30(6):1292–1305. doi: 10.1093/nar/30.6.1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mian M.F., Ahmed A.N., Rad M., Babaian A., Bowdish D., Ashkar A.A. Length of dsRNA (poly I: C) drives distinct innate immune responses, depending on the cell type. J. Leukoc. Biol. 2013;94(5):1025–1036. doi: 10.1189/jlb.0312125. [DOI] [PubMed] [Google Scholar]
- Mogensen T.H. Pathogen recognition and inflammatory signaling in innate immune defenses. Clin. Microbiol. Rev. 2009;22(2):240–273. doi: 10.1128/CMR.00046-08. Table of Contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molinari N.A., Ortega-Sanchez I.R., Messonnier M.L., Thompson W.W., Wortley P.M., Weintraub E. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086–5096. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- National Institute of Allergy and Infectious Diseases. Common Cold Facts [Available from: http://www.niaid.nih.gov/topics/commoncold/pages/treatment.aspx.
- Nordlund J.J., Wolff S.M., Levy H.B. Inhibition of biologic activity of poly I: poly C by human plasma. Proc. Soc. Exp. Biol. Med. 1970;133(2):439–444. doi: 10.3181/00379727-133-34492. [DOI] [PubMed] [Google Scholar]
- Pan L.N., Zhu W., Li C., Xu X.L., Guo L.J., Lu Q. Toll-like receptor 3 agonist Poly I: C protects against simulated cerebral ischemia in vitro and in vivo. Acta Pharmacol. Sin. 2012;33(10):1246–1253. doi: 10.1038/aps.2012.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pichlmair A., Schulz O., Tan C.P., Rehwinkel J., Kato H., Takeuchi O. Activation of MDA5 requires higher-order RNA structures generated during virus infection. J. Virol. 2009;83(20):10761–10769. doi: 10.1128/JVI.00770-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savan R. Post-transcriptional regulation of interferons and their signaling pathways. J. Interferon Cytokine Res. 2014;34(5):318–329. doi: 10.1089/jir.2013.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slater L., Bartlett N.W., Haas J.J., Zhu J., Message S.D., Walton R.P. Co-ordinated role of TLR3, RIG-I and MDA5 in the innate response to rhinovirus in bronchial epithelium. PLoS Pathog. 2010;6(11) doi: 10.1371/journal.ppat.1001178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stowell N.C., Seideman J., Raymond H.A., Smalley K.A., Lamb R.J., Egenolf D.D. Long- term activation of TLR3 by poly(I: C) induces inflammation and impairs lung function in mice. Respir. Res. 2009;10:43. doi: 10.1186/1465-9921-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi O., Akira S. Pattern recognition receptors and inflammation. Cell. 2010;140(6):805–820. doi: 10.1016/j.cell.2010.01.022. [DOI] [PubMed] [Google Scholar]
- Tan W.C., Xiang X., Qiu D., Ng T.P., Lam S.F., Hegele R.G. Epidemiology of respiratory viruses in patients hospitalized with near-fatal asthma, acute exacerbations of asthma, or chronic obstructive pulmonary disease. Am. J. Med. 2003;115(4):272–277. doi: 10.1016/s0002-9343(03)00353-x. [DOI] [PubMed] [Google Scholar]
- Thompson M.R., Kaminski J.J., Kurt-Jones E.A., Fitzgerald K.A. Pattern recognition receptors and the innate immune response to viral infection. Viruses. 2011;3(6):920–940. doi: 10.3390/v3060920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner R.B. Rhinovirus: more than just a common cold virus. J. Infect. Dis. 2007;195(6):765–766. doi: 10.1086/511829. [DOI] [PubMed] [Google Scholar]
- Turner R.B., Couch R.B. Rhinoviruses. In: Knipe D.M., Howley P.M., editors. Fields Virology. fifth ed. Lippincott Williams & Williams; Philadelphia: 2007. pp. 895–909. [Google Scholar]
- Weinberger B., Herndler-Brandstetter D., Schwanninger A., Weiskopf D., Grubeck- Loebenstein B. Biology of immune responses to vaccines in elderly persons. Clin. Infect. Dis. 2008;46(7):1078–1084. doi: 10.1086/529197. [DOI] [PubMed] [Google Scholar]
- Wong J.P., Saravolac E.G., Sabuda D., Levy H.B., Kende M. Prophylactic and therapeutic efficacies of poly(IC.LC) against respiratory influenza A virus infection in mice. Antimicrob. Agents Chemother. 1995;39(11):2574–2576. doi: 10.1128/aac.39.11.2574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Wohlford-Lenane C., Zhao J., Fleming E., Lane T.E., McCray P.B., Jr. Intranasal treatment with poly(I*C) protects aged mice from lethal respiratory virus infections. J. Virol. 2012;86(21):11416–11424. doi: 10.1128/JVI.01410-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available since the information is confidential and a proprietary part of patent filings. However, the authors are willing to release appropriate information if the request is legitimate and the appropriate confidentiality agreements are in place.