Highlights
-
•
We first present a HRV-C and HBoV1 co-infection in an adult woman with severe acute respiratory distress syndrome.
-
•
Our study suggests that HBoV1 co-infection might worsen the disease caused by HRV-C infection, and raises a question whether HRV-C-related severe pneumonia is often associated with co-infection of other respiratory viruses such as bocavirus.
Dear Editor,
Human rhinovirus (HRV) and bocavirus (HBoV) are two of the most common respiratory viruses associated with acute respiratory tract infections among children.1, 2 Recent articles in this journal have highlighted the role of bocavirus and rhinovirus in potentially severe pneumonia in adults and younger children.3, 4 However co-infection with both viruses was very rare among adults. A previous study reported a 16-month child who was infected by HBoV1 and also showed presence of HRV, developed severe pneumonia.5 Here we reported co-infection with HBoV1 and HRV-C in an adult woman with acute respiratory distress syndrome (ARDS).
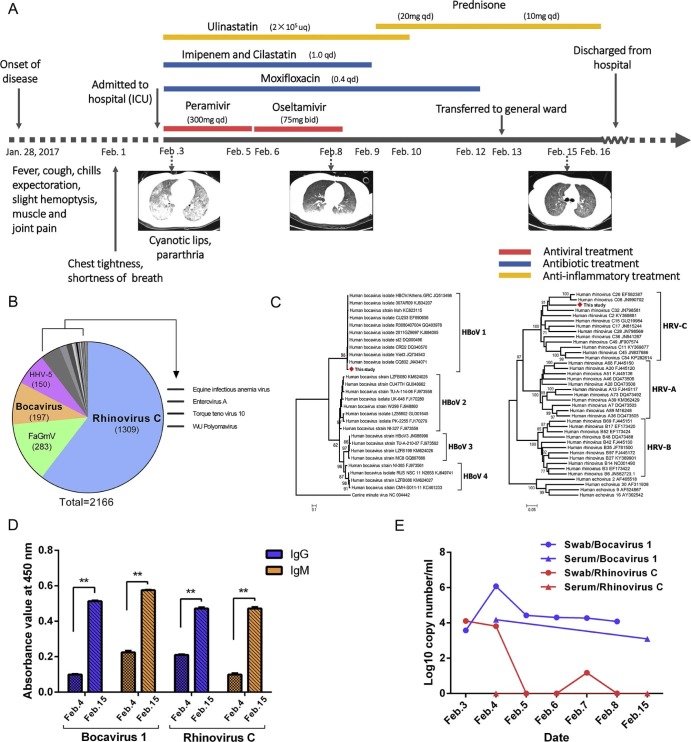
A 26-year-old woman caught a cold on Jan. 28, 2017, and developed symptoms of recurrent fever, cough, chills, expectoration, slight hemoptysis, muscle and joint pain in the following days (Fig. 1A ). She felt chest tightness and shortness of breath on February 1, and visited Guangzhou Eighth People's Hospital for further examination and treatment on February 3 since her condition continuously worsened with cyanotic lips and pararthria.
Figure 1.
Timeline of the patient's clinical course and evidence supporting the co-infection with HRV-C and HBoV1. A, Timeline of the patient's clinical course and outcome. B, Viral reads distribution. Viral reads were classified by aligning again the NCBI viral sequence database with blast-n and blast-x. C, Maximum-likelihood phylogenetic trees were generated by MEGA6 based on partial VP1/VP2 sequences (~550 bp) of Bocavirus (left) and partial VP4/VP2 sequences (~530 bp) of Rhinovirus (right). D, Antibody responses to HBoV1 and HRV-C at two time-points. Results are shown as absorbance values at 450 nm, cutoff 0.15. Difference between different groups was determined by the Student's t-test. ** P < 0.01. E, Viral load dynamic of HBoV1 and HRV-C in swabs and serums collected in different time-points.
A high-resolution version of this slide for use with the Virtual Microscope is available as eSlide: VM04609.
The patient had fever of 39.3 °C, heart rate of 144 beats/min, respiratory rate of 38 breaths/min, blood pressure of 112/66 mmHg, and pulse oxygen saturation (SpO2) of 85%. Laboratory evaluation showed white blood cell count 2.2–3.77 × 109/L(normal, 3.5–9.5 × 109/L), lymphocyte 0.61 × 109/L (normal, 1.1–3.2 × 109/L), platelet count (PLT) 72 × 109/L (normal, 100–350 × 109/L), C-reactive protein 89.5 mg/L (normal, <8.0 mg/L), hemoglobin (HB) 108 g/L (normal, 110–150 g/L), oxygenation index (OI) 105 mmHg (normal, 400–500 mmHg), CD3 T cell 197/mm3 (normal, 500–1500/mm3), CD4 T cell 197/mm3 (normal, 300–1200/mm3), and CD8 T cell 121/mm3 (normal, 238–874/mm3) (Supplementary Table S1). Auscultation of the lungs revealed extensive moist rales and computed tomographic (CT) scan showed bilateral diffuse infiltration (Fig. 1A). She was diagnosed with severe pneumonia with ARDS, and admitted immediately to the ICU with high flow oxygen to maintain the SPO2 at approximately 90% on February 3. During this period, she showed polypnea, dysphoria, frequent cough and slight hemoptysis. Abundant hemorrhagic secretions were observed through bronchofiberscope. She was treated with antiviral and antibiotic therapies in combination with ulinastatin (Fig. 1A).
Antiviral drug peramivir was used in the first three days, followed by oseltamivir in another three days. Antibiotics (imipenem, cilastatin and moxifloxacin) were given for 10 days. Her body temperature returned normal on the fourth day and CT showed significant improvement in the patient's condition. She was switched to sequential non-invasive ventilation from February 10 to 12, and then transferred to general ward and treated with low-flow oxygen and prednisone. The patient was discharged from the hospital on February 17 and showed a sustained recovery in two subsequent visits on February 28 and March 15.
Throat swabs and sera were collected during her hospitalization. Blood and respiratory secretions were negative for bacteria, and fungi in cultures, and G-test and GM-test, respectively. HIV, HBV, influenza viruses, SARS-CoV, MERS-CoV and other coronaviruses were negative by ELISA and/or (RT-)PCR assays. Pulmonary secretions from the first day of hospitalization were further analyzed using metagenomic sequencing as described previously.6 Of 64,024,857 total reads, 2166 (0.0034%) were of viral origin. Two respiratory viruses, HRV (1309 reads, 60.4%) and HBoV (197 reads, 9.1%) were found with high percentages (Fig. 1B). The presence of HRV and HBoV were confirmed by specific (RT-)qPCR assays, and HBoV1 RNA was also detected at all sample points. HRV-C and HBoV1 were determined by phylogenetic analyses of HRV VP4/VP2 and HBoV VP1/VP2 fragments, respectively (Fig. 1C). Specific IgM and IgG responses against HBoV1 and HRV-C were further investigated by ELISA (Feiya BioTech, China). The serum IgG and IgM levels of the patient showed 2.2 to 4.7 fold increases for HRV-C and 5.1 to 2.6 fold increases for HBoV1 from February 4 to February 15, respectively (Fig. 1D). Above results indicated an acute co-infection with HBoV1 and HRV-C in the patient. We further characterized the dynamics of both viruses using (RT-)qPCR assays (Fig. 1E). After 2 days of treatment, the viral load of HRV-C and HBoV1 among swabs showed a rapid decrease from 1.3 × 104 copy/ml to below the detection limit, and from 1.2 × 106 copy/ml to 2.7 × 104 copy/ml, respectively. Then, HRV-C viral load remained undetectable among swabs and sera, while HBoV1 viral load started a slowdown from 2.7 × 104 copy/ml to 1.2 × 103 copy/ml during whole treatment, indicating a persistent infection of HBoV1.5 Accompanied by the antiviral treatment, the patient progressively recovered and bilateral lung opacity improved rapidly, indicating that the treatment was effective. It was difficult to determine which virus was mainly responsible for the case. But the recovery of the patient from the rapid elimination of HRV-C and a persistent presence of HBoV1 among swabs and sera suggested that HRV-C may be the principal causative agent for the severe pneumonia. HRV was often associated as severe respiratory illness in children and adults.7, 8, 9 As there are still questions about the role of HBoV as a single causative agent, it is possible that the simultaneous HBoV1 infections worsen the illness caused by preceding HRV-C infection.
In this case, metagenomic sequencing showed a robust power to detect the causative agents of severe illness when the routine and traditional methods (e.g. culture, ELISA, PCR, etc.) failed. After excluding bacterica, fungi, and major pneumonia-causing viruses (i.e. SARS-CoV, MERS-CoV, and H7N9), we applied metagenomic sequencing to obtain the DNA and RNA sequences present in the sample, and determined the potential pathogens by similarity search with the sequence database covering all known viruses. The candidate viruses were further confirmed by specific (RT-)qPCR assays, phylogentic analysis, as well as seroconversion of IgM and IgG responses. Using this pipeline, HRV-C and HBoV1 were identified as the causative agents of this index patient with ARDS.
In conclusion, our study reports a life-threatening pneumonia case caused by co-infection with HRV-C and HBoV1, and raises a question whether HRV-C-related severe pneumonia is often associated with co-infection of other respiratory viruses such as bocavirus.
Potential conflicts of interest
No reported conflicts.
Acknowledgement
We thank Profs. Yongzhen Zhang at Chinese Center for Disease Control and Prevention, Marc Eloit at Institut Pasteur (Paris) and Qibin Leng at Institut Pasteur of Shanghai, CAS, for their valuable suggestions.
This work was supported by grants from the China National Mega-projects for Infectious Diseases (2017ZX10101001-005-001 and 2017ZX10103009-002), and the Bureau of Science and Information Technology of Guangzhou Municipality (2014Y2-00550 and 201400000002).
Footnotes
Supplementary data related to this article can be found online at https://doi.org/10.1016/j.jinf.2017.10.012.
Contributor Information
Fuchun Zhang, Email: gz8hzfc@126.com.
Chiyu Zhang, Email: zhangcy1999@ips.ac.cn.
Appendix. Supplementary data
The following is the supplementary data to this article:
Clinical parameters of the index patient during hospitalization.
References
- 1.Guido M., Tumolo M.R., Verri T., Romano A., Serio F., De Giorgi M. Human bocavirus: current knowledge and future challenges. World J Gastroenterol. 2016;22(39):8684–8697. doi: 10.3748/wjg.v22.i39.8684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacobs S.E., Lamson D.M., St George K., Walsh T.J. Human rhinoviruses. Clin Microbiol Rev. 2013;26(1):135–162. doi: 10.1128/CMR.00077-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taylor S., Lopez P., Weckx L., Borja-Tabora C., Ulloa-Gutierrez R., Lazcano-Ponce E. Respiratory viruses and influenza-like illness: epidemiology and outcomes in children aged 6 months to 10 years in a multi-country population sample. J Infect. 2017;74(1):29–41. doi: 10.1016/j.jinf.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y., Li Y., Liu J., Zhao Y., Xie Z., Shen J. Genetic characterization of human bocavirus among children with severe acute respiratory infection in China. J Infect. 2016;73(2):155–163. doi: 10.1016/j.jinf.2016.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jula A., Waris M., Kantola K., Peltola V., Soderlund-Venermo M., Hedman K. Primary and secondary human bocavirus 1 infections in a family, Finland. Emerg Infect Dis. 2013;19(8):1328–1331. doi: 10.3201/eid.1908.130074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Legoff J., Resche-Rigon M., Bouquet J., Robin M., Naccache S.N., Mercier-Delarue S. The eukaryotic gut virome in hematopoietic stem cell transplantation: new clues in enteric graft-versus-host disease. Nat Med. 2017;23(9):1080–1085. doi: 10.1038/nm.4380. [DOI] [PubMed] [Google Scholar]
- 7.Hai le T., Bich V.T., Ngai le K., Diep N.T., Phuc P.H., Hung V.P. Fatal respiratory infections associated with rhinovirus outbreak, Vietnam. Emerg Infect Dis. 2012;18(11):1886–1888. doi: 10.3201/eid1811.120607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lau S.K., Yip C.C., Lin A.W., Lee R.A., So L.Y., Lau Y.L. Clinical and molecular epidemiology of human rhinovirus C in children and adults in Hong Kong reveals a possible distinct human rhinovirus C subgroup. J Infect Dis. 2009;200(7):1096–1103. doi: 10.1086/605697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi S.H., Hong S.B., Kim T., Kim S.H., Huh J.W., Do K.H. Clinical and molecular characterization of rhinoviruses A, B, and C in adult patients with pneumonia. J Clin Virol. 2015;63:70–75. doi: 10.1016/j.jcv.2014.12.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Clinical parameters of the index patient during hospitalization.