Abstract
The delivery of optimal palliative care requires an integrated and coordinated approach of many health care providers across the continuum of care. In response to identified gaps in the region, the Palliative Care Integration Project (PCIP) was developed to improve continuity and decrease variability of care to palliative patients with cancer. The infrastructure for the project included multi-institutional and multisectoral representation on the Steering Committee and on the Development, Implementation and Evaluation Working Groups. After review of the literature, five Collaborative Care Plans and Symptom Management Guidelines were developed and integrated with validated assessment tools (Edmonton Symptom Assessment System and Palliative Performance Scale). These project resources were implemented in the community, the palliative care unit, and the cancer center. Surveys were completed by frontline health professionals (defined as health professionals providing direct care), and two independent focus groups were conducted to capture information regarding: 1) the development of the project and 2) the processes of implementation and usefulness of the different components of the project. Over 90 individuals from more than 30 organizations were involved in the development, implementation, and evaluation of the PCIP. Approximately 600 regulated health professionals and allied health professionals who provided direct care, and over 200 family physicians and medical residents, received education/training on the use of the PCIP resources. Despite unanticipated challenges, frontline health professionals reported that the PCIP added value to their practice, particularly in the community sector. The PCIP showed that a network in which each organization had ownership and where no organization lost its autonomy, was an effective way to improve integration and coordination of care delivery.
Key Words: Palliative care, cancer, symptom management, evidence-based, collaborative care plans (CCPs), symptom management guidelines (SMGs), health services, health system integration, formative evaluation
Introduction
Surveys, focus groups, and accreditation processes conducted in Southeastern Ontario in 1998–2000 identified gaps in the provision of optimal palliative care. Findings indicated minimal use of assessment tools; lack of evidence-based practice(s); discomfort of family physicians in managing symptoms of advanced illness; inconsistent symptom management practices; discontinuity of care at critical transition points; need for coordination and communication among health care providers/services; lack of awareness and/or underutilization of available resources; and unmet patient and family needs.1, 2, 3, 4, 5 Other Canadian studies found similar limited integration between care providers and facilities3, 4 that had resulted in late referrals, unnecessary delays for treatment or transfer to an appropriate setting of care, and unnecessary suffering and cost.2, 3, 4
In response, a group of administrative and clinical leaders within palliative medicine, the regional cancer center, and local health organizations from Kingston, Frontenac, Lennox & Addington (KFL&A) counties came together to investigate the possibility of establishing a Palliative Care Program. A decision was made at the onset that the immediate focus would not be on program governance, (infra)structure, or developing an entirely “new palliative program,” but rather, on optimizing existing clinical services, resources, and funding through the development and implementation of a quality improvement project, the Palliative Care Integration Project (PCIP). The PCIP would serve as the basis for the development of more integrated clinical relationships, and thus efficient and effective client care. The intention was that the PCIP “project” format would eventually transition to a “program” and expand into surrounding regions in Southeastern Ontario.
It was posited that the development of the appropriate project infrastructure, processes, and operational plan would ensure timely decision making, unquestionable implementation, maximized shared ownership, and evolve into expanded and sustainable palliative care best practices at a regional level. A formative evaluation framework was chosen to: 1) enhance program development and improvement, and 2) help others set up similar services or networks. This article details this framework and describes the infrastructure, development and implementation processes, and evaluation of the KFL&A PCIP. A previous published article delineates the PCIP outcome evaluation.6
Methods
Target Population and Geographic Region
The target population included all cancer patients in the noncurative phase of illness and the health professionals who provided their care, regardless of the site of care. This included 1347 cancer patients followed by community care (KFL&A Community Care Access Centre [CCAC]), Queen's Palliative Care Medicine and the complex continuing care palliative care unit (St. Mary's of the Lake Hospital), an acute care hospital (Kingston General Hospital), and a regional cancer center (Cancer Centre of Southeastern Ontario) during the calendar years of 2001–2003. A detailed description of this target population is provided in the PCIP outcome evaluation article.6
The KFL&A counties, located in Southeastern Ontario, Canada, cover approximately 6660 km2. These counties are a mixture of relatively small urban areas, small rural towns, and hamlets. At the time of the development and implementation of the PCIP, there were approximately 190,000 people living in the region (114,200 in the largest city, Kingston);7 over 500 practicing physicians (approximately 200 general practitioners); two tertiary acute care hospitals (with one palliative care consult service but no acute care designated palliative care units); one community hospital; a regional cancer center (3000 new patients per year, one palliative care clinic); and a complex continuing care hospital (housing a six-bed palliative care unit). Community-based nursing care was delivered primarily by two agencies contracted for service by one CCAC. Within all of these health care sectors, care for palliative patients was provided by a mix of regulated nurses and unregulated health care providers. Many members of this frontline staff were not designated within a “palliative care staff or team,” but rather, were among a staff roster that changed from shift to shift and day to day.
The challenges to develop and provide optimal and integrated palliative care delivery in this region included:
-
•
Number of organizations providing palliative care;
-
•
Desire of organizations to maintain autonomy;
-
•
No new funding;
-
•
Large geographic region—travel to deliver and/or access services and varied access to services;
-
•
Staff fluctuations and turnovers;
-
•
Competing demands;
-
•
Expectations that primary care physicians and community-regulated and unregulated staff would provide most of the palliative and end-of-life care;
-
•
No formal process for interacting or sharing of clinical information, best practices, documentation between and across sites.
Goals and Objectives
The goal of the KFL&A PCIP was to ensure the integration of efficient, high-quality palliative care for patients with incurable cancer and their families across all sites of care delivery.
The project's objectives were: 1) improved access to palliative care services; 2) improved symptom management; 3) increased home and long-term care (LTC) facility deaths; 4) decreased unnecessary emergency visits and hospital admissions; 5) use of common evaluation methods; and 6) use of evidence-based practice across the continuum of care.
The PCIP used the World Health Organization (1992) definition of palliative care: active total care of persons for whom curative therapies are no longer possible. The target population for this project was adults (older than 18 years) with noncurative cancer, who resided in the KFL&A region.
Infrastructure
The PCIP project structure objectives were:
-
1.
To create a governing body of key stakeholders who were committed to change and integration of services, with the understanding that no organization would forfeit any organizational autonomy.
-
2.
To develop Expert Working Groups by pooling clinical and nonclinical representation from across the entire palliative care service delivery continuum.
Palliative Care Integration Project Steering Committee
The 13-member KFL&A Steering Committee included chief executive officers, vice presidents, chief nursing officers, executive directors, and managers of health care organizations who provided palliative care in different settings. Decisions were made by consensus. The Steering Committee developed the project vision, goal, and objectives. A clinical champion who also served as the chair of this committee provided positive leadership, linkage, and influence to all of the project components. The Steering Committee met bimonthly throughout the duration of the project and was responsible for overseeing all aspects of this project. Until 2004, the Steering Committee provided approximately 1000 “in-kind” hours per year. A Project Coordinator, funded through donated dollars from two of the participating organizations, was hired and supervised by the Steering Committee.
Expert Working Groups
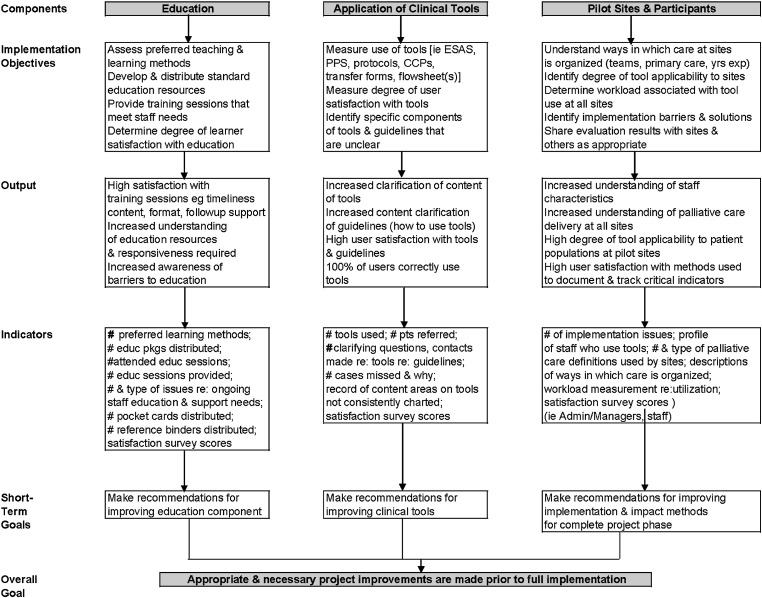
Three Expert Working Groups were established by the Steering Committee: 1) Development, 2) Implementation, and 3) Evaluation. The Project Coordinator formally recruited working group members from all levels of care/across the continuum of care, cofacilitated the development and implementation of working groups, provided management support to the groups, and participated as a member of each working group. A pilot logic model (Fig. 1 ) was developed by the members of the PCIP as a means of guiding and communicating the various activities of the Expert Working Groups during the project's pilot phase. The logic model detailed the processes involved in determining the best educational strategies and provided clarity regarding the content, format, and processes for the most efficient incorporation of the new clinical resources into daily practice.
Fig. 1.
KFL&A PCIP Pilot Logic Model, 2002.
Development Working Groups—Composition and Responsibilities
The Development Working Groups included family physicians, physician specialists (palliative care, oncologists), advanced practice nurses/clinical nurse specialists, registered nurses, clinical educators, community case managers, a respiratory therapist, dietitians, social workers, bereavement counselors, physiotherapists, spiritual care providers, and pharmacists. In total, there were 55 members from over 30 different organizations.
The Development Working Groups were responsible for: 1) confirming the evidence-based and validated assessment tools, and 2) the development of evidence-based collaborative care plans (CCPs) and symptom management guidelines (SMGs), and integrating them with the selected assessment tools.
Implementation Working Group—Composition and Responsibilities
The 15-member Implementation Working Group comprised the project coordinator, administrators/managers, educators, and frontline health care professionals. These individuals were identified as champions of clinical practices by their peers and organizations, for example, long-term-care facilities, public and private community-care organizations, acute and complex continuing care facilities, and a regional cancer center, and further described as motivators and enablers in their day-to-day roles and activities. Because the responsibilities and associated tasks of the Implementation Working Group were extensive, two implementation subgroups, Documentation and Education, were established.
The Documentation subgroup developed policies and procedures on documentation and use of the assessment tools, CCPs and SMGs. The development of documentation procedures and accompanying policies was complicated given the number and variation of participating sites.
The Education subgroup was responsible for: 1) standardizing the approach to CCP education across the continuum; 2) identifying educational needs and the available resources to meet these needs; 3) ensuring that timely provisions were made to educate and support frontline staff involved in the pilot of the CCPs and during full implementation; and 4) developing a plan for the training of facilitators in each participating site.
The core Implementation Working Group developed the overall timelines and action plans for education for the pilot phase and for full implementation in the participating organizations (LTC, community nursing agencies, acute care inpatient, continuing complex care [palliative care unit], and the regional cancer center). In addition, this committee developed a strategy to increase the awareness of the project and the use of CCPs and SMGs throughout the KFL&A region.
Evaluation Working Group—Composition and Responsibilities
The 10-member Evaluation Working Group was comprised of people with expertise in research-evaluation methodology, biostatistics, epidemiology, and clinical nursing and medical palliative care. This working group developed the evaluation framework and submitted a proposal to secure funding to measure the effectiveness of implementing the PCIP in and across all participating sites of care in the KFL&A region.
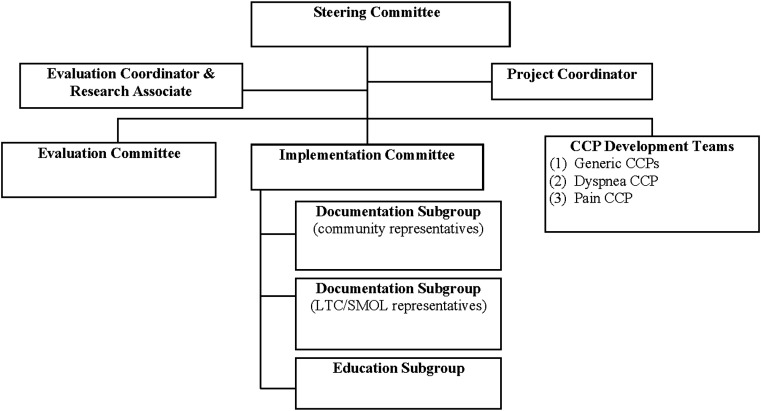
The project's evaluation was supported by a two-year (2002–2004) grant from the Canadian Health Services Research Foundation. The Evaluation Coordinator was funded through this grant. Figure 2 illustrates the KFL&A PCIP organizational structure and reporting matrix.
Fig. 2.
KFL&A Palliative Care Integration Project Organizational Structure. KFL&A Steering Committee and related subcommittees. Steering Committee Representatives: Kingston General Hospital, St. Mary's of the Lake Hospital, Southeastern Ontario Cancer Centre (KGH) (formerly Kingston Regional Cancer Centre), Hospice Kingston, Queen's Palliative Care Medicine Program, Rideaucrest Home, Fairmount Home, Community Care Access Centre for KFL&A.
Development Phase
The development phase objective was to develop an evidence-based integrated model of palliative care delivery for the KFL&A region.
Developmental Phase—Processes
Team membership on each Expert Working Group was interdisciplinary and represented all levels of care. System users and clinical champions played a pivotal role. Ownership of this project was shared and all contributions were acknowledged and valued. Virtual and face-to-face meetings were organized every four to six weeks. Meeting sites were rotated between sites of care to optimize engagement of participants. Communication and cooperation were key attributes to success. Agendas and detailed meeting minutes for each expert working group were provided to all members.
Developmental Phase—Activities
Assessment Tools
The Edmonton Symptom Assessment System (ESAS) and the Palliative Performance Scale (PPS) were identified by the Steering Committee and confirmed by the Development Working Group as the two primary assessment tools for inclusion in the PCIP. The ESAS8 is a validated instrument that uses a Likert scale (0–10) to assess the intensity of the following symptoms: pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, well-being, and shortness of breath; 0 represents no symptoms, whereas 10 represents the worst possible symptom intensity. The PPS9 is a succinct method of assessing and reporting a patient's functional status. It communicates changes in the person's condition (stable, transitional, end of life) so that appropriate care can be allocated.
Collaborative Care Plans and Symptom Management Guidelines
The Development Working Group created five CCPs. CCPs are interdisciplinary guides to practice that are designed to: 1) place the patient at the focal point of care; 2) promote continuity and coordination of care; and 3) promote communication among all disciplines.
In creating the CCPs, the Development Working Group undertook an extensive literature search that focused on optimal management practices (Appendix). These were examined against current practice in the KFL&A region. Where the literature did not give clear direction, this expert panel came to a consensus before adding a recommendation.
Three CCPs were developed to define the activities, interventions, and expected patient outcomes that should occur based on that patient's functional performance as determined by the PPS. The three stages of palliative care based on the PPS include: 1) stable CCP (PPS: 70–100); 2) transitional CCP (PPS: 40–60); and 3) end-of-life CCP (PPS 0–30).
The SMGs developed by the Development Working Group are evidence-based guidelines for the management of cancer-related symptoms. The SMGs for pain and dyspnea are based on the ESAS scores. This working group also developed SMGs for nausea and vomiting, agitation, mouth care, and bowel care.
Implementation Phase
The implementation phase objective was to disseminate the evidence-based integrated model of palliative care delivery throughout KFL&A.
Implementation Phase—Processes
Planning for implementation began a year before full implementation of the PCIP. The preliminary work included an organizational impact analysis. The Project Coordinator held face-to-face meetings with managers and senior leaders of key stakeholder agencies. At these sessions, the coordinator introduced the project and outlined a proposed infrastructure and operational processes. The number of regulated and nonregulated staff employed by each organization, the availability of in-service training, and potential challenges to participation were assessed. Agencies were invited to participate in the project with the expectation that they would identify internal champions who could participate in development teams and assist with training in their own organization. Estimates and expectations regarding human resources and time commitments also were discussed.
“Champions” were recruited from each of the participating sites to help with education, implementation, and documentation. A customized education format was developed by the educator/clinical leads for their organization that used the standardized materials from the PCIP Development and Education Working Groups. An inventory of resources was developed and maintained.
Once the CCPs and SMGs were developed, a one-month pilot study was conducted to test the format of the assessment tools, CCPs and the SMGs, the documentation processes, and the education processes in each participating organization.
To optimize and simplify education and uptake, the implementation process used a phased-in approach. The ESAS was first introduced in August 2002, followed by the introduction of the PPS in November–December 2002. On January 15, 2003, the CCPs were introduced during a Train-the-Trainer day. This event marked the beginning of full implementation.
The various strategies used to continue the education and disseminate the integrated palliative care model within the KFL&A region included:
-
•
Community (monthly) and palliative care medicine (weekly) (multidisciplinary) rounds;
-
•
Workshops/“train-the-trainer” and networking of champions and educators (half or full day);
-
•
Continuing professional development—accredited (half day);
-
•
Presentations to small local groups; train-the-trainer presentations on the project website;
-
•
Discussion/follow-up meetings/mentorship;
-
•
Case-study format community nursing rounds with the PCIP Project Coordinator and a palliative care physician.
Implementation Phase—Activities
A Resource Manual included the ESAS and PPS, CCPs, and SMGs. The project web site and a CD that contained the contents of the Resource Manual and training presentations were available to participating organizations.
Evaluation Phase
The evaluation phase objective was to measure the processes, structure, and outcomes of developing and implementing the PCIP.
The following outcome question was addressed: Does the implementation and use of standardized assessment tools, CCPs and SMGs improve and facilitate continuity of care for palliative cancer patients in and across all points of care? Specifically, does the use of common assessment tools, evidence-based CCPs and SMGs, by regulated and unregulated health care providers:
-
(a)
Decrease variability of palliative care practice?
-
(b)
Improve efficiencies in patient care?
-
(c)
Improve access to palliative care services?
-
(d)
Improve responsiveness of the system to meet the needs of the patients undergoing palliative care and their families?
As stated earlier, these findings were recently published.6
A formative evaluation framework was used to evaluate the structure and processes for the development and implementation of the PCIP in the KFL&A region over the two-year period (2002–2004). This evaluation framework provided ongoing feedback about the various aspects of the implementation process to the participating organizations. The key findings are discussed here.
Evaluation Phase—Processes
The Evaluation Working Group met a minimum of twice a month throughout the evaluation timeline. The Evaluation Working Group worked collaboratively with the Implementation Working Group to closely synchronize the timing of the implementation with the evaluation process. In addition, a representative of the Evaluation Working Group attended the Documentation and Education subgroup meetings to inform and coordinate progress in these areas with proposed evaluation measures. The evaluation framework used both previously developed validated tools, and custom-developed data collection tools.
Evaluation Phase—Activities
Research Ethics
Approval to conduct the pilot study and formative evaluation was received from each of the primary participating sites and the Queen's University Research Ethics Board. Consenting health professionals completed the self-administered questionnaires and participated in the process focus groups. All data were kept strictly confidential and secure.
Methods and Analysis
Pilot Study (Preimplementation of Full Palliative Care Integration Project)
Four organizations participated in the pilot study that tested the format of the assessment tools, CCPs and SMGs and the documentation and education processes. The obtained written feedback was used to revise the resource materials, documentation, and educational processes before full implementation.
Self-Administered Surveys
In the spring of 2004, frontline health professionals who actively participated in the full implementation of the PCIP were invited to complete a self-administered survey. By this stage, frontline users had been engaged with the PCIP for up to 18 months. Respondent demographics, career history, and clinical experience were collected. This survey measured user impressions of the PCIP, clinical application, relevance and changes to their practice, and any barriers experienced at the time of implementation or afterward. The responses also were used to guide the focus group sessions that followed.
The survey results were analyzed using descriptive statistics (frequency calculations for categorical variables, and mean and standard deviation for continuous variables).
Focus Groups
Two independent focus groups were conducted to: 1) capture information regarding the development of the project; and 2) capture information regarding the processes of implementation and usefulness of the different components of the project.
Members of the Development Working Groups participated in the focus group sessions held in September 2002. Frontline registered health professionals involved in implementing the PCIP participated in the focus groups held in the spring of 2004.
To ensure objective analyses, an independent facilitator was hired to conduct and analyze all of the focus groups. Focus group discussions were tape-recorded and notes taken. These records were then transcribed verbatim. The facilitator confirmed any questionable comments and/or gaps with the focus group attendees.
Results
Infrastructure
A network for integration of care delivery was created and included organizations providing care in the community, acute care hospitals, outpatient cancer clinic, long-term and complex continuing care facilities. This was accomplished without a change in governance or any service foregoing autonomy.
Development and Implementation Phases
The multidisciplinary Development Expert Working Groups integrated the ESAS and PPS with the five CCPs and SMGs that they developed. These evidence-based resources provided a common language and guidelines to help plan, manage, monitor, and provide palliative care delivery across the continuum of care. Between the summer of 2002 and 2004, approximately 600 frontline regulated health care professionals and allied health professionals, and over 200 family physicians and medical residents, received education/training on the use of the assessment tools CCPs and SMGs. These learners represented a minimum of 30 organizations.
Evaluation Phase
Pilot Study (Preimplementation of Full Palliative Care Integration Project)
Based on the feedback of the pilot study, the assessment tools CCPs and SMGs were changed for easier access and integration. The feedback led to the development of a pocket version of the SMGs (September 2003), a laminated ESAS/PPS pocket-sized assessment card (2004), and a pocket or “Lite” version of the CCPs (2005).
Self-Administered Surveys
A total of 30 of 122 (24.6%) frontline health care professionals consented and responded to a self-administered questionnaire during the postimplementation phase. Four of these participants (13.3%) also participated in the 2002 Development Working Group focus group session. Most of the participants were experienced registered nurses (RNs) (93.3% of the RNs had that designation for more than one year), with most of them having more than one year of work experience in the palliative care field (80.0%). Most of them (93.1%) worked two to four shifts per week and cared for one or more palliative patients per week (89.3%). The community setting represented the location of work for most of the participating health care professionals (53.3%). Because the numbers for the survey were low, the respondents were not identified by organizational site.
Forty percent of the participants reported being very familiar with the PCIP and the assessment tools. In the month before the survey, the PPS was the most frequently used tool (76.7%), followed by the ESAS (63.3%), SMGs (56.6%), and the CCPs (53.4%). Most (93.3%) of the participants reported that they received training on how to use the ESAS and PPS, followed by 80% and 76.7% for SMG and CCP training, respectively. The participants reported that their organization supported both the training (90%) and the time needed to apply the training (80%).
Responses to questions regarding the influence of the PCIP in general, and to the specific assessment tools and CCPs on the care delivered to palliative patients, were evenly distributed between “having no influence” to “having a strong influence.” However, most (63.3%) of the participants did report that each project tool added value to their practice. The greatest level of influence on practice and associated with the use of all the tools was reported by the community agencies (53.3%), with the lowest level of influence reported by health care professionals in the regional cancer center (10%) setting.
Focus Groups
2002 Focus Group—Development Working Groups (Decision Makers and Clinical Educators)
Nine (16.4%) of 55 invited health care professionals (frontline workers) who were involved in the development of the PCIP CCPs participated in focus group sessions held in 2002. Participants reported that they were very positive about their involvement in the process: the amount of work accomplished, the collaborative attitude, the number and diversity of organizations involved, the client focus, and the opportunity to look at the “big picture” of the palliative care in the community.
Participating members of the Development Working Groups stated that the personal benefits experienced from their involvement in the PCIP included increase in personal growth and development, networking, and a sense of personal satisfaction from their contribution. The professional benefits participants experienced included increased knowledge of “best practices” and community resources. Organizational benefits included increased profile of palliative care both within the organization and within community and better collaboration and communication between agencies.
Concerns were expressed regarding the workload demands of the project. Suggestions were made that development and implementation would have been facilitated if the time commitments were known before entry into the project; if back-fill positions for developers, educators, and learners were available; and if the Project Coordinator had secretarial support. Participants thought that the role of the Project Coordinator was essential and that the drive, leadership, consistency, and enthusiasm of key people were also crucial.
2004 Focus Groups—FrontLine Health Care Professionals
Participants agreed that the Resource Manual was very informative and comprehensive, and was an excellent resource. The PPS was used by organizations to assess when a patient needed to be moved to a different level of care; when the family could have access to extended visiting hours; and to monitor and communicate changing care needs, often indicating the need for more service. Participants generally found the ESAS less useful than the PPS; the reasons included: the patients were often too ill to complete the nine symptom-related questions, and therefore, a proxy or nurse completed the form; there was no consistent system of collection and documenting the symptom intensity; there was a lack of time to explain the form; and the tools were perceived as an “add-on” to existing nursing-assessment protocols.
Implementation challenges expressed during the focus group included the following: assessment tool forms were not readily available; there was a need for standardized documentation; and “one size fits all” does not apply to all patients. It was suggested that the resources and conceptualized use for the PCIP needed to be tailored for a health care organization's patient population. Limited time and human resources were also reported. Participants did report that the Resource Manual and CCPs were particularly useful for new staff and medical residents who were not familiar with care of palliative patients.
The term “palliative” posed a challenge. Despite the fact that the project had a definition of “palliative,” how each site interpreted and applied the definition varied, for example, palliative meant end of life, or palliative meant a person with incurable disease.
Challenges
Developmental Phase
Members of the Development Expert Working Group were specialists in their own fields of practice but had limited insight into the regional “system” perspective of palliative care provision. In addition, the palliative care knowledge base, work experience, and practice varied within and between sites of care. Over the period of development, there was significant staff turnover in every health care organization.
Implementation Phase
The participation of multiple health care organizations meant that the organizational cultures, patient populations, and staff compositions and skill sets varied. In addition, each participating organization had different practice protocols and expectations, educational time allotments, and requirements. Targeting the PCIP to regulated nursing and unregulated health professional staff, for example, personal support workers (community) and health care aides (LTC), also required sensitivity to the varying levels of education, knowledge, and experience in palliative care.
As planning for implementation began before the completion of development of the CCPs and SMGs, frontline users who were members of the Implementation Working Group were, at times, hesitant to buy-in or completely endorse the process. Limited relief staff, competing demands and priorities in each participating health care organization influenced the amount and quality of education provided and received.
Evaluation Phase
This was a huge project with an objective to influence and evaluate a system's delivery of palliative care between 2002 and 2004. The evaluation timelines were predicated on the implementation timelines but also limited by the duration of the grant funding. Numerous systems' related factors that were beyond the control of the PCIP had an impact on the implementation of the project. This in turn meant that the planned evaluation measures occurred before the full uptake of the implementation and before some processes, for example, documentation, were in place at certain sites.
Unanticipated System Changes
Unanticipated system changes also impacted the PCIP. In the spring of 2003, one of the project's participating community health agencies stopped providing palliative care nursing services. This resulted in staff turnover, disruption in community palliative care delivery, and adjustments to PCIP-implementation timeline.
In March 2003, the severe acute respiratory syndrome (SARS) outbreak struck patients in Toronto, Ontario. This had a huge impact on all health care providers in Ontario. Hospital and clinic processes were changed, which required considerable effort from health care providers at all levels of the health care system. This event essentially stopped further development of a common PCIP documentation form and restricted the time people could devote to education and implementation regarding PCIP. Delays in implementation were also influenced by staff shortages and heavy caseloads of frontline health professionals across the continuum of care.
Further Developments
Despite the expected and unexpected challenges, the PCIP moved forward. During the summer of 2003, the Steering Committee began work with the District Health Council to prepare for the rollout of the PCIP to the neighboring counties of Southeastern Ontario. In 2004, with funding support from the Ministry of Health and Long-Term Care of Ontario, expansion into the neighboring counties began.
In early 2005, in response to limited ESAS and PPS documentation across the continuum of care, an electronic solution was developed. The Cancer Centre of Southeastern Ontario and the KFL&A CCAC, with funding from Cancer Care Ontario's (CCO) Innovation Fund, developed touch-screen kiosk computer technology to capture ESAS scores of patients attending clinics in the cancer center and secure Internet technology and touch-tone telephone technology to capture symptom and functional assessments from patients at home. If scores were more than a designated threshold, as determined by the professional caregivers, then appropriate health care professionals were automatically notified.10
A Fatigue CCP was developed by a 23-person interdisciplinary team from across the South East region of Ontario. Fatigue is the most common symptom of oncology patients and others living with palliative needs. A literature review was completed in December 2004. Development of the Fatigue CCP was completed by September 2005.
To address the complex needs of residents in LTC facilities, educators from the PCIP, the Stroke Strategy, Best Practice Guidelines, and Dementia Networks came together to plan and deliver educational events that were interactive, informative, and of practical use to the registered and nonregistered LTC practitioners who attended. These sessions were offered every three months and are being offered to date. In addition, work is on to develop a toolkit for the assessment, management, and documentation of pain for people living with dementia in LTC settings.
In 2006, with financial support from the Ministry of Health and Long-Term Care of Ontario and administrative and financial support from CCO, the PCIP intervention was adopted and implemented by the regional End-of-Life Networks, CCACs, and Regional Cancer Programs across Ontario. To maximize uptake, the Provincial Palliative Care Integration Project (PPCIP) included a continuous quality improvement methodology.11 Conceptualizing the PPCIP within this context followed a primary recommendation that came from the PCIP final outcome evaluation report written by the KFL&A PCIP Evaluation Working Group.
Discussion
The KFL&A PCIP was a highly successful, but very complex, endeavor. It involved the endorsement and implementation of common assessment tools, the development and implementation of CCPs and SMGs, and the evaluation of the processes and outcomes related to the project. There were nearly 100 individuals from over 30 different organizations who actively participated in bringing it to fruition. Although we cannot say that all outcomes are attributable to the project alone, the evaluation of administrative data showed that across the three-year study period, there was evidence of improvement in efficiencies in patient care, for example, a consistent decrease in the length of stay, reduced visits to the Emergency Department, and an increase in home or non-acute care facility deaths. In addition, there were improvements in patient symptom intensity, although these were not statistically significant.6
Our findings showed that a multi-institutional and multisectoral network, in which each organization had ownership and where no organization lost its autonomy, was an effective and successful way to build relationships among organizations and to improve integration of care delivery. Our keys to success included strong, upper-level administrative leadership from the key organizations providing palliative care in the region; strong clinical leadership; a dedicated Project Coordinator who was a member of all expert working groups, and therefore, provided continuity; and broad membership of all working groups in both the development and implementation planning to establish “buy-in/ownership” early in the process. A project of this magnitude, involving multiple sites, disciplines, and geography, required open communication, objectives (short, interim, and long term), and a strong commitment to continuous collaboration and quality improvement. The PCIP was successful as well, because it addressed identified gaps in the provision of optimal palliative care for the patient.
Unanticipated challenges, such as SARS, changes in agencies providing care in the community, as well as staff load limitations and resistance, and challenges with the definition of the “palliative” patient, led to barriers and delays in full implementation. Projects that involve multiple sites and people should probably anticipate significant delays when determining evaluation timelines. When the project was evaluated, the processes regarding documentation within and between sites of care had not been addressed. This meant that some of the outcomes were not captured. The relatively low participation in focus group discussions and completion of surveys might reflect fatigue with the project or the priorities of frontline health care professionals. With this in mind, the results might reflect some bias.
Change takes time. Implementation and education regarding the components of the PCIP have continued, and the processes are more embedded into “usual” care throughout the region. There is sustained commitment from the participating organizations, and the data are now used to monitor care and quality improvement activities. The KFL&A PCIP also formed the basis of a provincial initiative with the implementation of ESAS, PPS, CCPs, and SMGs for cancer patients in all the regional cancer centers and the communities throughout the province of Ontario, Canada. The PCIP model has been integrated into other regional and provincial strategies, that is, Stroke, Geriatric Psychiatry's P.I.E.C.E.S., CCO, all of which provide evidence that the PCIP goal continues to be achieved.
Acknowledgments
Innumerable additional persons have contributed to this project, its development, implementation, evaluation, funding, and document preparation. It is also of importance to thank the residents and health care community for their participation and contribution.
Footnotes
Funding support from the following agencies is acknowledged: Canadian Health Services Research Foundation; Ministry of Health and Long-Term Care through the Ontario Health Services Research Co-sponsorship Fund; Cancer Centre of Southeastern Ontario; Kingston, Frontenac and Lennox & Addington Community Care Access Centre; Kingston General Hospital; St. Mary's of the Lake Complex Continuing Care Hospice, Kingston, Ontario, Canada. Other support was provided by Health Care Network of Southeastern Ontario.
Appendix. Development of Collaborative Care Plans and Symptom Management Guidelines: Search Strategies
To facilitate the development of the Pain CCP and SMG, in January 2001, a search in MEDLINE (1997–2000) and CINAHL (Cumulative Index to Nursing and Allied Health Literature [1982–2000]) was conducted using Medical Subject Headings (MeSH) and text words, including neuropathic pain, algorithm, bibliography, care plan, clinical innovation, controlled clinical trial, critical path, guideline, standards, review article, systematic review, clinical conference, congresses, consensus literature, and multi-case. The full text of the article was retrieved and reviewed if it met the inclusion criteria.
The Dyspnea CCP and SMG development was aided by a literature search in MEDLINE, AIDSLine, HealthSTAR, Cancerlit, and the Clinics of North America series for the period 1966 to December 4, 2000. Initially, all articles found under the MeSH heading “dyspnea” and “palliative care” were reviewed. This permitted an overview of common management strategies for dyspnea. Further searches using “dyspnea” and the MeSH heading most appropriate to the management strategy were then done. Articles that addressed management were assessed. Bibliographies were reviewed to find articles not identified in searches. Where appropriate, each article was critically appraised using the JAMA Critical Appraisal series as a guide.
References
- 1.Hospice Kingston. Needs assessment: Kingston, Frontenac, Lennox and Addington Counties, 2000. Kingston, Ontario: Hospice Kingston, 2000.
- 2.Johnston G.M., Gibbons L., Burge F.I. Identifying potential need for cancer palliation in Nova Scotia. CMAJ. 1998;158:1691–1698. [PMC free article] [PubMed] [Google Scholar]
- 3.Chapman C. Southeastern Ontario Palliative Pain and Symptom Management Program; Brockville, Ontario: 1998. Perceived barriers to delivery of palliative care: Guide to program planning. [Google Scholar]
- 4.Ostic H. Survey of family physicians—impediments to dying at home (unpublished). Kingston, Ontario, 1999.
- 5.Rosenbaum C. Health Care Network of Southeastern Ontario; Kingston, Ontario: 2000. Integrating health services in Southeastern Ontario: Moving forward 2000. [Google Scholar]
- 6.Dudgeon D., Knott T.C., Eichholz M. Palliative care integration project (PCIP) quality improvement strategy evaluation. J Pain Symptom Manage. 2008;35:573–582. doi: 10.1016/j.jpainsymman.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Health Care Network of Southeastern Ontario Population Estimates (unpublished). Southeastern Ontario District Health Council Health Systems Monitoring Report, 2003.
- 8.Bruera E., Kuehn N., Miller M.J., Selmser P., Macmillan K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care. 1991;7:6–9. [PubMed] [Google Scholar]
- 9.Downing GM, Wainwright W, Victoria Hospice Society. Palliative Performance Scale (PPSv2) version 2. Medical care of the dying, 4th ed. Victoria, BC: Victona Hospice Society, Learning Centre for Palliative Care, 2006:120.
- 10.Dudgeon D., Smith A., Van Dijk J.P. Symptom identification and management: a rapid notification system. Oncol Exchange. 2007;6:56–58. [Google Scholar]
- 11.Dudgeon D., Vaitonis V., Seow H. Ontario, Canada: using networks to integrate palliative care province-wide. J Pain Symptom Manage. 2007;33:640–644. doi: 10.1016/j.jpainsymman.2007.02.001. [DOI] [PubMed] [Google Scholar]