Coronavirus disease 2019 (COVID-19)1 , 2 is currently a major medical issue, and several studies have reported the typical lung features of the disease on chest computed tomography (CT). We present manifestations of COVID-19 in a patient with lung adenocarcinoma.
In February 2020, a 46-year-old female patient presented with a growing palpable mass on the right parietal region with no any other symptoms or history. She initially visited the Second Hospital of Luohe City on February 4 2020, and was examined by one physician who was diagnosed with COVID-10 on 5 February 2020 (day 1, was in contact with the infected patient). The diagnosis of lung adenocarcinoma was confirmed by bronchoscopic biopsy, and the mass on the right parietal region was considered metastatic. The patient was transferred to Henan Chest Hospital for further treatment on 9 February 2020 (day 5). Henan Chest Hospital was informed that this patient had been in contact with the diagnosed infected physician on 14 February 2020, and she immediately had chest CT and RT-PCR tests for COVID-19 nucleic acid using nasopharyngeal swabs. Results of RT-PCR testing for COVID-19 nucleic acid were positive on 14 February 2020 (day 10), however, chest CT did not demonstrate typical reported signs of COVID-19. The patient subsequently developed intermittent fever to 38°C on the morning of 15 February 2020, and was transferred to the Sixth People Hospital of Zhengzhou, which is a designated hospital for COVID-19. The patient experienced intermittent chest tightness, nausea, and vomiting, and she received treatment with traditional Chinese medicine. Chest CT scanning was carried out again on 18 February 2020 (day 14), and no typical CT features for COVID-19 were found. RT-PCR tests for COVID-19 were repeated on 18 February (day 14) and 20 February (day 16) 2020, and both were negative. She had increased C-reactive protein levels and reduced lymphocyte ratios (Table 1 ). Her symptoms started to improve, and she was transferred to a general ward.
Table 1.
Summary of laboratory results of a patient with adenocarcinoma of the lung, who is infected with the novel coronavirus that causes coronavirus disease 2019
| 14 Feb | 15 Feb | 18 Feb | 20 Feb | Reference range | |
|---|---|---|---|---|---|
| Eosinophils, ×109/l | 2.58 | 3.13 | 3.46 | 3.92 | 0.05–0.5 |
| Eosinophil ratios, % | 11.6 | 11.70 | 10.50 | 10.90 | 0.5–5 |
| Lymphocytes, ×109/l | 2.68 | 3.02 | 2.15 | 1.99 | 0.8–4 |
| Lymphocyte ratios, % | 12.10 | 3.02 | 6.50 | 5.5. | 20–40 |
| Neutrophils, ×109/l | 15.23 | 18.94 | 25.63 | 27.91 | 2–7 |
| Neutrophil ratios, % | 68.80 | 70.50 | 77.90 | 77.40 | 50–70 |
| White blood cell count, ×109/l | 22.16 | 26.82 | 32.89 | 36.07 | 4–10 |
| C-reactive protein, mg/l | 2.0 | 25.79 | 60.08 | 67.62 | 0–0.3 |
Feb, February.
Chest CT images showed diffuse, irregular, small, ground-glass nodular opacities with partial consolidation in bilateral lungs on day 10 (Figure 1 A–D), in addition to the mass in the left lung. The nodules increased in size and number on day 14 (Figure 1E–H).
Figure 1.
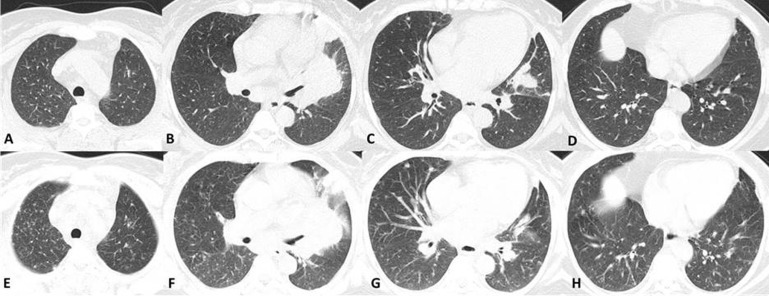
Axial chest computed tomography findings in a 46-year-old female with adenocarcinoma of the left lung also infected with COVID-19.
Diffuse, irregular, small, ground-glass opacity nodules with partial consolidation in bilateral lungs on day 10 (A–D), increasing in size and number on day 14 (E–H).
These diffuse, irregular, small, ground-glass opacities with partial consolidation rapidly increased in 4 days in this patient with left lung cancer, which was consistent with inflammation, rather than metastasis. Repeat positive RT-PCR tests for nucleic acid confirmed the diagnosis of COVID-19. White blood cell counts remained elevated, even after the patient’s symptoms improved, likely due to obstructive pneumonia caused by the tumor.
Chest CT images showed diffuse, irregular, small, ground-glass opacities with partial consolidation in bilateral lungs on day 10, in addition to the mass in the left lung. The nodular opacities increased in size and number on day 14, which was not a typically reported COVID-19 feature including ground glass opacity, crazy-paving pattern, and consolidation.3 , 4 The typical distribution of lung abnormalities in COVID-19 was reported as predominantly subpleural; however, this case showed predominantly diffuse involvement.5
Acknowledgements
This study was approved by the local institutional review board, and written informed consent was obtained from the patient.
Disclosure
The authors have declared no conflicts of interest.
References
- 1.Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of Covid-19 - studies needed. N Engl J Med. 2020;382(13):1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 2.Paules C.I., Marston H.D., Fauci A.S. Coronavirus infections-more than just the common cold. JAMA. 2020 doi: 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- 3.Bernheim A., Mei X., Huang M. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020 doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fang Y., Zhang H., Xie J. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020 doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan F., Ye T., Sun P. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]


