Abstract
Background
Previous in-hospital studies suggest that there are significant circadian rhythms associated with the incidence of acute coronary syndromes (ACSs). No study to date has examined the presentation of ACS in the prehospital setting. Our goal was to examine circadian, day-of-week, and age patterns of occurrence in ACS in a large, urban emergency medical services (EMS) system.
Methods
We retrospectively reviewed the electronic prehospital medical records from the Beijing's EMS system spanning August 1, 2005, to July 31, 2007. Data were analyzed by hour of the day and day of the week. χ2 tests were performed to compare the difference.
Results
Seven thousand thirty-two cases of ACS were identified by the EMS system physicians during the 2-year study period, including 536 cases of acute myocardial infarction. A significant variation of circadian distribution of ACS was observed in both 24-hour (P < .001) and 2-hour (P < .001) interval time course. Two peaks were observed in the morning from 0800 to 1000 and approaching midnight from 2200 to 2400. Increases of 50% and 60.8% in the morning and evening peaks were found, respectively, when compared with the early morning baseline (nadir). No significant difference was found among the accumulated cases in 2 years on each day in a week (P = .203).
Conclusions
Our study shows that, in the Beijing metropolitan area, the presentation of ACS has significant circadian rhythm characterized by 2 peaks within 24 hours, the morning peak is 0800 to 1000, and the late evening peak is 2200 to 2400. No significant weekly rhythm was observed in the present study.
1. Introduction
Acute coronary syndrome (ACS) usually presents in the late stages of coronary heart disease and is one of the leading causes of death in the world. For the past 50 years, in-hospital studies on the circadian rhythm of ACS have been performed, suggesting there are significant circadian rhythms of the incidence of ACS [1], [2], [3], [4], [5]. No study to date, however, has examined the presentation of ACS in the prehospital setting. We examined data from the emergency medical services (EMS) system in Beijing, China. Our goal was to examine circadian, day-of-week, and age patterns of occurrence in ACS in an EMS system. Understanding of the rhythm can aid in the preventive strategy as well as the preparation and planning for ACS in EMS systems.
2. Methods
Emergency medical services system ambulances in Beijing are staffed by physicians with training in emergency medicine diagnosis and procedures appropriate for the prehospital evaluation and treatment of ACS in the prehospital setting. Emergency medical services system physicians enter clinical data on standardized forms, including the patients' general information, chief complaint, medical history, bedside physical examination, and a preliminary diagnosis. In this study, the electronic prehospital medical records from the Beijing's EMS system spanning August 1, 2005, to July 31, 2007, were reviewed by 2 emergency attending physicians. Acute coronary syndrome was diagnosed by EMS system physicians in the prehospital setting, based on symptoms, medical history, physical examination, and the patient's prehospital 12-lead electrocardiogram. Physicians reviewing the charts for purposes of this study did not seek to agree or disagree with the diagnosis so long as all the required data were present on the EMS system run sheets.
According to the defined population in the reports of the World Health Organization Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA) project and the high incidence of ACS in the aged population in Beijing, ACS events in individuals older than 20 years were studied. The MONICA project monitors the prevalence of acute cardiac events in 21 countries, including China [6], [7]. Data from the case records including age, sex, date, time of onset of ACS, and the diagnosis were extracted for the present study. Cases were grouped in intervals by decade from the age of 20 to 89 years, with one group including all patients older than 89 years. Demographic data (in the year of 2006) of population ratio of age groups and sex groups were obtained from the Web site of Beijing Statistical Information Net (http://www.bjstats.gov.cn/tjnj/2006-tjnj/).
Data were analyzed by hour of the day and day of the week. χ 2 test was performed to evaluate the distribution variation during the day or the week, and P < .05 was taken as the statistically significant level. All analyses were carried out with the software Statistical Package for Social Sciences 11.5 (SPSS Inc, Chicago, Ill). Adjusted frequency, corresponding to relative ACS frequency in unit population of the age group, was calculated by the following equation: adjusted frequency = cases of the age group/population ratio of the age group (%)/100.
3. Results
3.1. Age distribution
There were a total of 355 418 electronic medical records in Beijing's EMS system during the study period. Among them, 61 169 medical records with “heart” or “chest pain” as the chief complaint or the diagnosis were reviewed. From these, 7032 cases of ACS were identified by the EMS system physicians during the 2-year study period. Of these cases meeting ACS criteria, there were 536 cases of acute myocardial infarction (AMI). Of the 7032 ACS cases, there were 4134 female patients (58.8%) and 2898 male patients (41.2%). The mean age was 64.5 ± 14.4 years old. More than two thirds (69.8%) of cases occurred in patients older than 55 years. There was a small but statistically significant difference in age for males (63.0 ± 14.7 years) vs females (66.0 ± 13.7 years) (P < .001).
Peak incidence was observed at the seventh decade (Fig. 1A). When the frequency of ACS was adjusted by the percentage of the decade to the total population, a definite increment of episodes was noticed as age increased. The variation of the frequency of ACS in each decade showed a curve approximating exponential growth (R 2 = 0.999, P < .001), with a sharp takeoff after the sixth decade. People in the eighth decade had a higher risk ratio of about 50-fold compared with individuals in their 30s. In males, the increase of ACS frequency was even more prominent after the seventh decade (Fig. 1B).
Fig. 1.
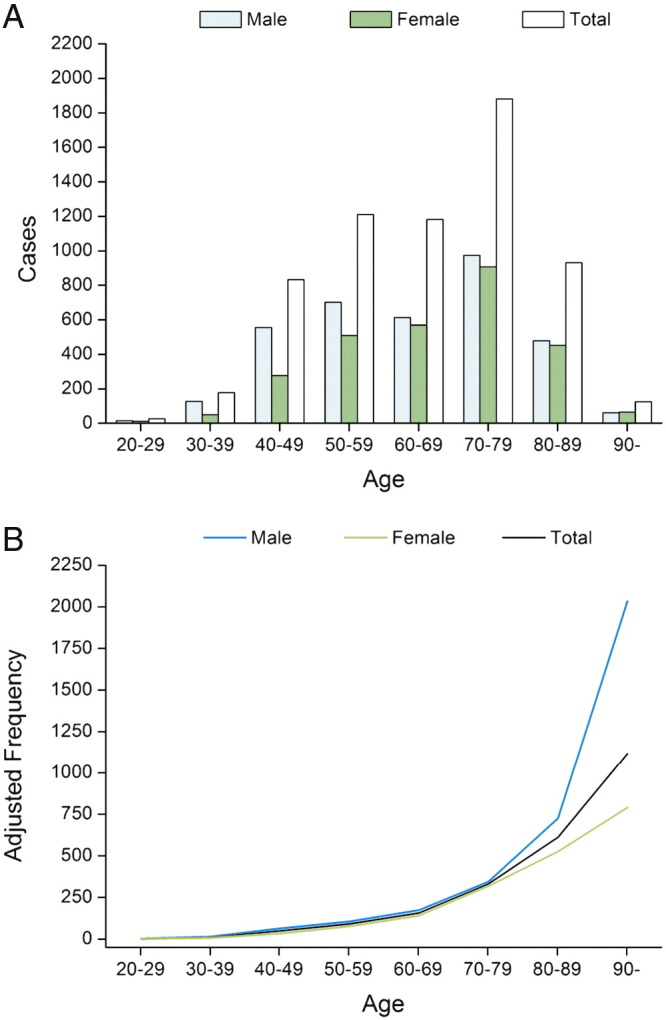
A, The age distribution of the total 7006 cases of ACS, grouped by sex. B, The increasing tendency of adjusted frequency of ACS in each decade.
3.2. The circadian and weekly patterns of ACS
A significant variation of circadian distribution of ACS was observed in both 24-hour (χ 2 = 144.157, P < .001) and 2-hour interval time course (χ 2 = 123.870, P < .001). Two peaks were observed in the morning from 0800 to 1000 and approaching midnight from 2200 to 2400 (Fig. 2A). Compared with the trough hours during 0400 to 0600, an increase of 50.0% from 0800 to 1000 and 60.8% from 2200 to 2400 hours was observed.
Fig. 2.
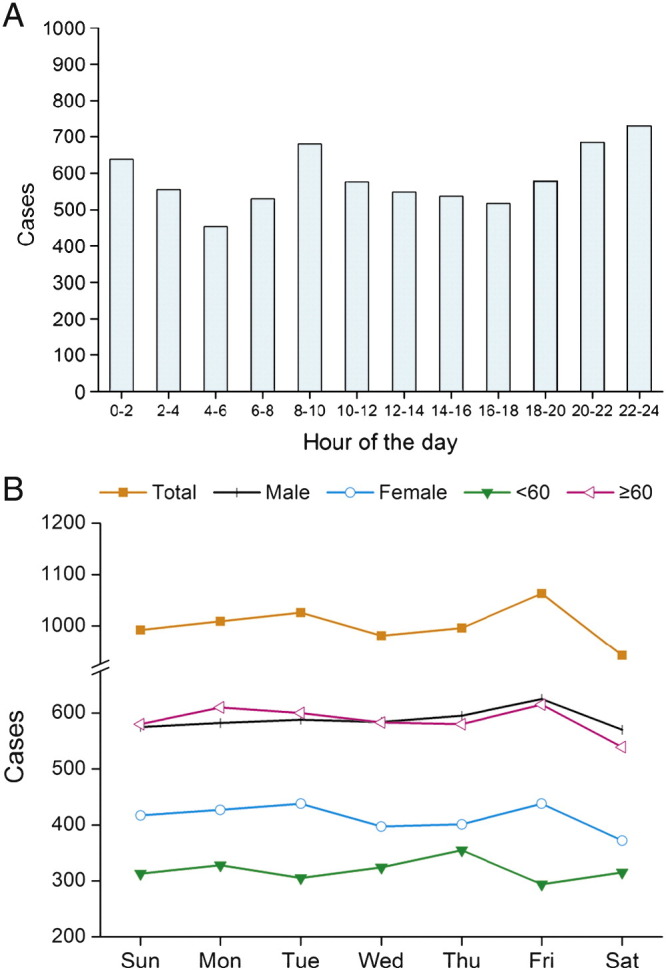
A, Diurnal variation of ACS occurrence with the 2-hour intervals. B, Variation of the accumulated cases of the day in a week in 2 years.
When cases were analyzed by day of the week, no significant difference was found among the accumulated cases in 2 years on each day in a week (χ 2 = 8.508, P = .203), nor among the accumulated cases of younger than 60 years (χ 2 = 7.128, P = .309) or older than 60 years (χ 2 = 6.646, P = .355). Although there were no significant differences in the variations during a week of 2 years in different groups, ACS most frequently occurred on Friday and occurred least on Saturday (Fig. 2B). A similar result was noticed regarding the occurrence of ACS in male (χ 2 = 3.334, P = .766) or female (χ 2 = 8.581, P = .199) patients.
4. Discussion
This is the first study examining the circadian rhythm of ACS cases derived from the prehospital data. All other studies to date have examined inpatient populations. The composition of inpatient populations may differ greatly from that in the prehospital setting. Data from EMS system can reflect the exact time of disease onset and the incidence more accurately than data from the hospital admission, especially because of the extraordinarily variable travel times, the triage times, and the wide disparity in access to medical care [8]. Although retrospective, our study minimizes reliance on recall and optimizes objective measures based on EMS system medical records data.
Beijing is a city with a population holding steady at about 16 million people during the investigative period. Most residents are the Han ethnic population accounting for about 95% of the population. During the study period, there were no significant social events (such as severe acute respiratory syndrome, the Olympic Games) that could lead migration or other significant changes in the composition of the population in Beijing. In previous Sino-MONICA census on the population aged 25 to 74 years old (471 462 people in 7 districts of Beijing were surveyed in 1997), acute coronary events have an incidence of about 178 per 100 000 people per year in Beijing [9]. Our identified ACS cases have a similar age distribution as the acute coronary events identified in the Beijing Sino-MONICA project.
4.1. The circadian rhythm of ACS
Our data showed the presence of circadian variation in patients with ACS. The peak of ACS was noted in early morning and late evening hours. In the past, the morning peak circadian variation has been tracked using pain estimation and creatine kinase-MB to estimate timing [3]. Fries et al [4] confirmed the finding that there was a circadian variation in the onset of AMI with a morning (0600-1200) peak.
The reason for a morning peak has been elucidated in various studies. First, there is a morning increase in plasma catecholamine, and serum cortisol levels can increase the direct sympathetic overactivity in the morning hours, which may also enhance myocardial demand [10], [11]. Second, an increase in sympathetic tone occurring on awaking causes increases in blood pressure, heart rate, coronary tone, and myocardial contractility, which singly or together may result in a substantial augmentation of myocardial oxygen consumption [12], [13]. Finally, the increased tendency of ACS in the morning can be explained by several mechanisms including increase in platelet aggregation and activation of the clotting system due to a decrease in fibrinolytic and anti–thrombin Ш activity [14]. A combination of all these factors may possibly explain the cardiac events occurring more frequently in the morning hours. Atherosclerotic plaques may rupture from rapid and large changes of mechanical stresses on awakening in the morning.
In most studies on the incidence of cardiovascular events, single morning peak was noted, whereas our data showed a clear double-peak rhythm, which is similar to the study of Kinjo et al [5]. The reasons for the late evening peak incidence are less clear, although mental stress and overtime work have been suspected [15], [16]. Kinjo et al [5] suggested that smoking and drinking may also play important role in triggering the onset of AMI at night.
4.2. The weekly distribution of ACS
Previous studies on the weekly distribution of AMI have had conflicting results. Some authors have suggested an increased risk on Monday [17], [18], whereas others indicate no significant weekly variation at all [19]. Some authors suggested that the sudden change in physical activity pattern from weekend to workday might increase the risk of myocardial infarction. A more recent study by Ku also suggests that the incidence of AMI was significantly lower on Sundays (9%) than on the other weekdays (Monday through Saturday) [20].
Behar et al reported that exceptionally heavy physical exertion, a violent quarrel at work, and mental stress are the most frequent external factors precipitating the AMI [15]. Although not significant, our study shows that the incidence is higher on Friday and not on Monday in Beijing. This may be explained as follows: (1) When Friday comes, people have been exhausted by their work for 5 days. The accumulated work load during a week could be an important factor for ACS. (2) The home gathering of the Chinese people, especially city dwellers, usually occurs on the weekend. The aged people may experience more excitement than on other days in a week. These explanations need to be confirmed in future studies.
A limitation of this study is the assignment of patients to ACS by the EMS system physicians. Some diagnoses of ACS may have been missed by the 2 emergency attending reviewing the EMS system medical records because of recording errors or missed or wrong diagnosis by the EMS system physicians. No stress tests or coronary angiography can be obtained to confirm the diagnosis. This can be argued that most unstable angina cases can be diagnosed based on the patients' medical history, physical examination, and electrocardiograms.
In conclusion, our study shows that, in the Beijing metropolitan area, the presentation of ACS has significant circadian rhythm characterized by 2 peaks within 24 hours: the morning peak is from 0800 to 1000, and the late evening peak is from 2200 to 2400. No significant weekly rhythm was observed in the present study.
References
- 1.Spielberg C., Falkenhahn D., Willich S.N., Wegscheider K., Völler H. Circadian, day-of-week, and seasonal variability in myocardial infarction: comparison between working and retired patients. Am Heart J. 1996;132:579–585. doi: 10.1016/s0002-8703(96)90241-0. [DOI] [PubMed] [Google Scholar]
- 2.Marchant B., Ranjadayalan K., Stevenson R., Wilkinson P., Timmis A.D. Circadian and seasonal factors in the pathogenesis of acute myocardial infarction: the influence of environment temperature. Br Heart J. 1993;69:385–387. doi: 10.1136/hrt.69.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muller J.E., Stone P.H., Turi Z.G., Rutherford J.D., Czeisler C.A., Parker C. Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med. 1985;313(21):1315–1322. doi: 10.1056/NEJM198511213132103. [DOI] [PubMed] [Google Scholar]
- 4.Fries R., Jung J., Ozbek C., Bay W., Schieffer H., Heisel A. Influence of thermal stress on the incidence of acute myocardial infarction in a temperate climate. Cardiology. 1998;90(1):67–71. doi: 10.1159/000006820. [DOI] [PubMed] [Google Scholar]
- 5.Kinjo K., Sato H., Sato H., Shiotani I., Kurotobi T., Ohnishi Y. Circadian variation of the onset of acute myocardial infarction in the Osaka area, 1998-1999: characterization of morning and nighttime peaks. Jpn Circ J. 2001;65(7):617–620. doi: 10.1253/jcj.65.617. [DOI] [PubMed] [Google Scholar]
- 6.WHO MONICA Project Principal Investigators The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. J Clin Epidemiol. 1988;41(2):105–114. doi: 10.1016/0895-4356(88)90084-4. [DOI] [PubMed] [Google Scholar]
- 7.Tunstall-Pedoe H., Kuulasmaa K., Mahonen M., Tolonen H., Ruokokoski E., Amouyel P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA Project populations. Lancet. 1999;353(9164):1547–1557. doi: 10.1016/s0140-6736(99)04021-0. [DOI] [PubMed] [Google Scholar]
- 8.Wang H.L., Xu T., Xu J. Factors contributing to high costs and inequality in China's health care system. JAMA. 2007;298(16):1928–1930. doi: 10.1001/jama.298.16.1928. [DOI] [PubMed] [Google Scholar]
- 9.Zhao D., Wu Z., Wang W., Yao L., Zhou M.R. The trend of incidence rate of acute coronary events from 1984 to 1997 in Beijing area: Sino-MONICA Project. Chin J Cardiol. 2000;28(1):41–44. [in Chinese] [Google Scholar]
- 10.Turton M.B., Deegan T. Circadian variations of plasma catecholamine, cortisol and immunoreactive insulin concentrations in supine subjects. Clin Chim Acta. 1974;55(3):389–397. doi: 10.1016/0009-8981(74)90014-x. [DOI] [PubMed] [Google Scholar]
- 11.Middlekauff H.R., Sontz E.M. Morning sympathetic nerve activity is not increased in humans. Implications for mechanisms underlying the circadian pattern of cardiac risk. Circulation. 1995;91(10):2549–2555. doi: 10.1161/01.cir.91.10.2549. [DOI] [PubMed] [Google Scholar]
- 12.Millar-Craig M.W., Bishop C.N., Raftery E.B. Circadian variation of blood-pressure. Lancet. 1978;1(8068):795–797. doi: 10.1016/s0140-6736(78)92998-7. [DOI] [PubMed] [Google Scholar]
- 13.Rocco B., Nadel E.G., Selwyn A.P. Circadian rhythms and coronary artery disease. Am J Cardiol. 1987;59(Suppl I):13C–17C. doi: 10.1016/0002-9149(87)90190-1. [DOI] [PubMed] [Google Scholar]
- 14.Tofler G.H., Brezinski D., Schafer A.I., Czeisler C.A., Rutherford J.D., Willich S.N. Concurrent morning increase in platelet aggregability and the risk of myocardial infarction and sudden cardiac death. N Engl J Med. 1987;316(24):1514–1518. doi: 10.1056/NEJM198706113162405. [DOI] [PubMed] [Google Scholar]
- 15.Behar S., Tanne D., Abinader E., Agmon J., Barzilai J., Friedman Y. Cerebrovascular accident complicating acute myocardial infarction: incidence, clinical significance and short- and long-term mortality rates. The SPRINT Study Group. Am J Med. 1991;91(1):45–50. doi: 10.1016/0002-9343(91)90072-6. [DOI] [PubMed] [Google Scholar]
- 16.Krantz D.S., Kop W.J., Santiago H.T., Gottdiener J.S. Mental stress as a trigger of myocardial ischemia and infarction. Cardiol Clin. 1996 May;14(2):271–287. [PubMed] [Google Scholar]
- 17.Ganelina I.E., Borisova I.Y.. Circadian rhythm of working capacity, sympathicoadrenal activity, and myocardial infarction. Hum Physiol. 1983;9(2):113–120. [PubMed] [Google Scholar]
- 18.Gnecchi-Ruscone T., Piccaluga E., Guzzetti S., Contini M., Montano N. Morning and Monday: critical periods for the onset of acute myocardial infarction. The GISSI 2 Study experience. Eur Heart J. 1994;15(7):882–887. doi: 10.1093/oxfordjournals.eurheartj.a060605. [DOI] [PubMed] [Google Scholar]
- 19.Willich S.N., Löwel H., Lewis M., Hörmann A., Arntz H.R., Keil U. Weekly variation of acute myocardial infarction. Increased Monday risk in the working population. Circulation. 1994;90(1):87–93. doi: 10.1161/01.cir.90.1.87. [DOI] [PubMed] [Google Scholar]
- 20.Ku C.S., Yang C.Y., Lee W.J., Chiang H.T., Liu C.P., Lin S.L. Absence of a seasonal variation in myocardial infarction onset in a region without temperature extremes. Cardiology. 1998;89(4):277–282. doi: 10.1159/000006800. [DOI] [PubMed] [Google Scholar]


