Abstract
This article reviews the noninfectious pulmonary syndromes that cause morbidity and mortality early after hematopoietic cell transplantation with an emphasis on risk factors, clinical manifestations, treatment, and outcomes. The first section covers idiopathic pneumonia syndrome and its subtypes: peri-engraftment respiratory distress syndrome, diffuse alveolar hemorrhage, delayed pulmonary toxicity syndrome, and cryptogenic organizing pneumonia. The second section covers pulmonary toxicities of chemotherapies and immunosuppressive agents used in this setting. The final section covers less common syndromes, including pulmonary alveolar proteinosis, venous thromboembolism, pulmonary cytolytic thrombi, pulmonary venoocclusive disease, and transfusion-related acute lung injury.
Keywords: Idiopathic pneumonia syndrome, Cryptogenic organizing pneumonia, Hematopoietic cell transplantation
Key points
-
•
Idiopathic pneumonia syndrome (IPS) is an uncommon but deadly complication of transplantation with many clinical phenotypes.
-
•
A better understanding of IPS pathobiology and the role of occult infection is needed to develop effective therapies.
-
•
Some drugs given for conditioning or graft-versus-host disease prevention and treatment have known potential pulmonary toxicities.
-
•
Venous thromboembolism and pulmonary hypertension can cause pulmonary symptoms with normal chest imaging after a hematopoietic cell transplant.
Introduction
More than a million hematopoietic cell transplants (HCTs) have been performed worldwide to treat a spectrum of benign and malignant diseases.1, 2 Survival rates after HCT are increasing over time because of advances in donor and recipient selection, pretransplant conditioning, infection and graft-versus-host disease (GVHD) prevention and treatment, blood transfusion management, and critical care.3, 4, 5, 6 Nonrelapse mortality within 200 days of allogeneic HCT decreased from 30% to 16% comparing years 1993–1997 to 2003–2007, respectively, at one high-volume US transplant center.4 Despite improved overall survival, noninfectious lung injuries remain an important cause of morbidity and mortality after HCT. A recent “call to arms” urges concerted efforts toward identifying effective preventive and therapeutic strategies.7
This article focuses on noninfectious pulmonary complications that manifest within the first few months after HCT. The first section reviews epidemiology, pathogenesis, treatment, and outcomes of the diffuse lung injuries collectively referred to as idiopathic pneumonia syndrome (IPS) and its clinically relevant subtypes, including diffuse alveolar hemorrhage (DAH) and cryptogenic organizing pneumonia. The second section reviews pulmonary toxicities of drugs commonly used for conditioning or GVHD prophylaxis and treatment. The final section summarizes the limited knowledge of less common pulmonary syndromes that occur after HCT, including pulmonary alveolar proteinosis, venous thromboembolism, and pulmonary hypertension.
Idiopathic pneumonia syndrome
Definition
The National Institutes of Health sponsored a workshop in 1991 with the goal of unifying research on lung complications of transplantation.8 The standard IPS definition proposed by this group required evidence of widespread alveolar injury and absence of active lower respiratory tract infection (LRTI). LRTI could be excluded by either nonresponse to broad-spectrum antibiotics or at least one bronchoscopy with bronchoalveolar lavage (BAL) testing negative for an extensive panel of known pulmonary pathogens. Transbronchial biopsy was recommended when clinically permissible. Many clinical syndromes were included in this IPS definition, including acute respiratory distress syndrome (ARDS), acute interstitial pneumonitis, delayed pulmonary toxicity syndrome, peri-engraftment respiratory distress syndrome, DAH, cryptogenic organizing pneumonia, and bronchiolitis obliterans syndrome. The working group acknowledged the clinical heterogeneity within this definition and recommended multidisciplinary investigation to improve our understanding of IPS pathobiology and motivate novel treatments.
The emergence of new diagnostic technologies and newly recognized pulmonary pathogens resulted in updates to the original IPS definition.9, 10 The most recent published revision requires the exclusion of heart failure, acute kidney injury, and iatrogenic fluid overload as cause for the widespread alveolar injury.11 The modified definition in Box 1 incorporates an evolved understanding of pulmonary pathogens12, 13, 14, 15, 16 and an appreciation that inflammatory lung injury and hydrostatic pulmonary edema can coexist.17
Box 1. Modified definition of idiopathic pneumonia syndrome.
-
1.Widespread alveolar injury, as evidenced by
-
a.Multilobar opacities on chest imaging
-
b.Symptoms and signs of pneumonia
-
c.Abnormal pulmonary physiology
-
i.Increased alveolar to arterial oxygen difference
-
ii.New or increased restrictive pulmonary physiology
-
i.
-
a.
-
2.Absence of active LRTI
-
a.Negative tests for
-
i.Bacteria: stains and cultures for bacteria, acid-fast bacilli, Nocardia, Legionella, Mycoplasma
-
ii.Viruses: culture, DFA, and PCR for respiratory viruses (adenovirus, influenza, parainfluenza, metapneumovirus); shell vial culture (CMV, RSV); DFA for CMV, VZV, HSV; cytopathology for viral inclusions
-
iii.Fungi: stain and culture; serum and BALF galactomannan ELISA for Aspergillus species; PCR for Zygomycetes and other non-Aspergillus invasive molds in some clinical settings
-
i.
-
b.Consider tests for possible pulmonary pathogens: HHV6, rhinovirus, coronavirus
-
c.Consider lung biopsy if clinical condition permits and less invasive diagnostics are insufficient
-
a.
-
3.
No alternate explanatory cause for pulmonary dysfunction, such as heart failure, acute kidney injury, or iatrogenic fluid overload
Abbreviations: BALF, BAL fluid; CMV, cytomegalovirus; DFA, direct fluorescent antibody staining; ELISA, enzyme-linked immunosorbent assay; HHV6, human herpesvirus 6; HSV, herpes simplex virus; PCR, polymerase chain reaction; RSV, respiratory syncytial virus; VZV, varicella zoster virus.
Adapted with permission of the American Thoracic Society. Copyright (c) 2016 American Thoracic Society. Panoskaltsis-Mortari A, Griese M, Madtes DK, et al. An official American Thoracic Society research statement: noninfectious lung injury after hematopoietic stem cell transplantation: idiopathic pneumonia syndrome. Am J Respir Crit Care Med 2011;183(9):1263. The Am J Respir Crit Care Med is an official journal of the American Thoracic Society.
Epidemiology
Our knowledge of IPS epidemiology in the contemporary era is limited by the age of the currently available evidence and heterogeneous definitions used (Table 1 ). Two large retrospective cohort studies applied the standard IPS definition and found results similar to earlier studies of noninfectious interstitial pneumonitis and idiopathic interstitial pneumonitis. Incidence of IPS in these populations that included children and adults was 5.7% after autologous HCT18 and 8% after allogeneic HCT.18, 19 Median time to IPS onset was 21 days, ranging from 7 to 34 days. Risk factors included high-grade GVHD, age, total-body-irradiation (TBI) dose, and transplant indication. Mechanical ventilation was used in 62% to 69% of IPS cases, and mortality rates were approximately 75% in the hospital or within 30 days of discharge. Recent studies added prior HCT and receipt of blood component transfusions to the list of IPS risk factors.20, 21, 22
Table 1.
Idiopathic pneumonia syndrome risk factor studies
| First Author, Year | Years | Population | N | IPS Incidence (%) | IPS Risk Factors | Fatality/Mortality (%) |
|---|---|---|---|---|---|---|
| Meyers et al,146 1982 | 1969–1979 | Allo, syn BMT | 625 | 11–12a | HM/AA, age, TBI in AA | 61 |
| Weiner et al,147 1989 | 1978–1983 | Allo BMT | 1183 | 11a | Methotrexate, age, severe GVHD, BMT >6 mo after diagnosis, reduced performance status, TBI dose >4 cGy/min | 78 |
| Wingard et al,148 1988 | 1976–1985 | BMT | 382 | 15a | HM | 73 |
| Kantrow et al,18 1997 | 1989–1991 | First BMT | 1165 | 5.7–7.6 | Nonleukemia malignancy, grade IV acute GVHD | 74 |
| Bilgrami et al,149 2001 | 1993–1997 | Auto PBSCT | 271 | 3.4 | — | 80 |
| Wong et al,150 2003 | 1992–2000 | Auto HCT | 164 | 12 | — | 15 |
| Fukuda et al,19 2003 | 1997–2001 | Allo HCT | 1100 | 2.2–8.4 | Age, grade II–IV acute GVHD, acute leukemia or MDS, TBI dose | 75 |
| Keates-Baleeiro et al,23 2006 | 1999–2005 | Allo HCTb | 93 | 11.8 | Acute GVHDc | 64 |
| Zhu et al,151 2008 | 1997–2007 | Allo HCT | 192 | 12 | HLA matched unrelated donor, grade III–IV acute gut GVHD | 87–100 |
| Sakaguchi et al,24 2012 | 1990–2009 | Auto, allo HCTb | 251 | 8 | High-risk disease, busulfan conditioning | 15 |
| Sano et al,20 2014 | 1988–2007 | Allo HCTb | 210 | 6.7 | Grade II–IV acute GVHD, prior HCT | 79 |
Abbreviations: AA, aplastic anemia; allo, allogeneic; auto, autologous; BMT, bone marrow transplantation; HM, hematologic malignancy; MDS, myelodysplastic syndrome; PBSCT, peripheral blood stem cell transplantation; syn, syngeneic; TBI, total body irradiation.
Idiopathic interstitial pneumonia considered equivalent to IPS.
Study population included children only.
Univariate analysis.
Although IPS definitions, study populations, conditioning regimens, and observation times varied across these studies, there was a consistently high rate of respiratory failure and death. Reported outcomes were better in children than adults.23, 24 Updated studies are needed to better understand potential targets for intervention and inform bedside conversations about prognosis.
Pathogenesis
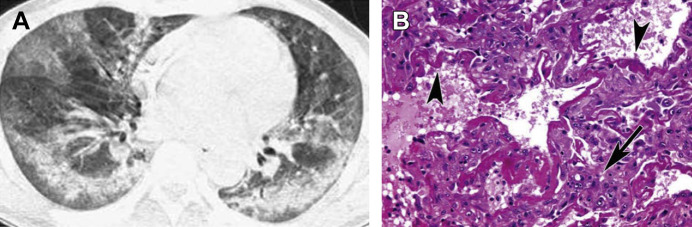
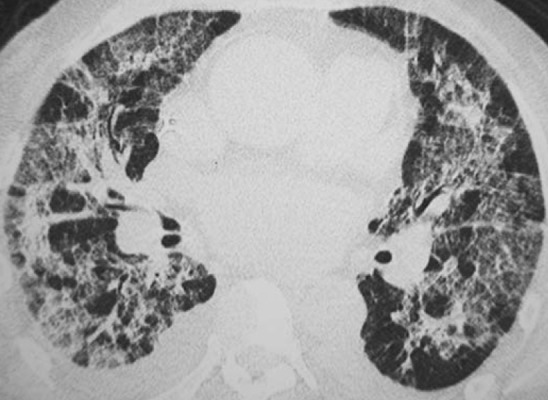
The histopathology of IPS spans a spectrum that includes diffuse alveolar damage, lymphocytic bronchiolitis, organizing pneumonia, and interstitial pneumonitis (Fig. 1 ).25 Efforts to elucidate the pathogenesis of IPS are challenged by the heterogeneity of the syndrome and the concurrence of processes that modify biology, such as extrapulmonary GVHD and use of mechanical ventilation. Our current knowledge of IPS pathobiology derives largely from studies using murine models that recapitulate many of the biological features and physiologic changes observed in clinical settings.
Fig. 1.
IPS in 40-year-old man with acute myelogenous leukemia 4 weeks after allogeneic hematopoietic stem cell transplantation. (A) High-resolution computed tomography scan obtained at level of lower lung zones shows bilateral patchy areas of consolidation and ground-glass attenuation. (B) Photomicrograph of histopathologic specimen shows that alveolar septa are thickened by edema and round cell infiltration (arrow). Hyperplasia and desquamation of alveolar lining cells, fibrinous exudation, and hyaline membranes (arrowheads) are seen within alveolar spaces (hematoxylin-eosin, original magnification ×250).
(From Franquet T, Müller NL, Lee KS, et al. Pictorial essay. High-resolution CT and pathologic findings of noninfectious pulmonary complications after hematopoietic stem cell transplantation. Am J Roentgenol 2005;184:629–37. Reprinted with permission from the American Journal of Roentgenology.)
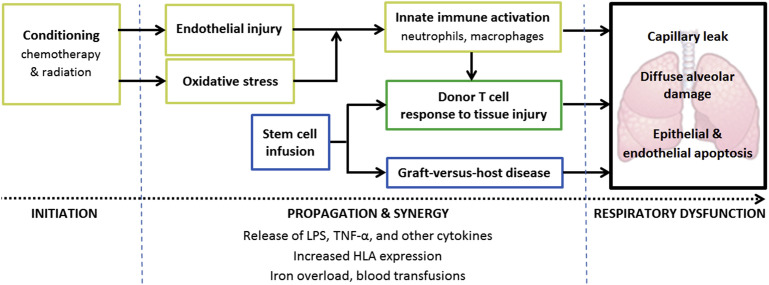
In experimental IPS models, cytokine/chemokine-mediated signal transduction cascades orchestrate noninfectious lung inflammation and injury (Fig. 2 ). Tumor necrosis factor (TNF)-α,26, 27 interferon (IFN)-γ,28, 29 and lipopolysaccharide (LPS)27 are proposed to mediate key pathways that converge in the lung.30 Early in IPS development, TNF-α released from injured tissues may enhance costimulatory communication between the donor T cells migrating into the lung and radioresistant host monocytes/antigen-presenting cells.31, 32, 33, 34, 35 Through dysregulation of interleukin (IL)-6, low IFN-γ levels promote expansion of alloreactive donor CD4+ cells, including T helper 17 (Th17) cells.30, 31, 35, 36 Neutrophilic alveolitis is noted in the later stages of experimental IPS.26, 37 It is hypothesized that LPS translocates from intestines that were damaged by conditioning or acute GVHD and circulates to the lung where it activates neutrophils and macrophages.30 The exact mechanisms of this proposed composite biology and how it ultimately injures host cells are not fully elucidated. In the end, severe pulmonary dysfunction results from capillary leak, pulmonary edema, disruption of pulmonary surfactant, and injury to and in some cases apoptosis of the bronchial epithelium, alveolar epithelium, and/or vascular endothelium.33, 38
Fig. 2.
IPS pathobiology. IPS can result from damage caused by pretransplant conditioning (yellow boxes) or from GVHD (blue boxes). These two pathways may act simultaneously and synergistically (green box) and may be amplified by inflammatory stimuli, such as iron overload and blood transfusions. LPS, lipopolysaccharide; TNF-α, tumor necrosis factor-α.
The few clinical studies examining cytokine levels in patients with IPS support some of these experimental findings. Blood and BAL fluid levels of TNF-α signaling and LPS-binding protein are elevated before and during IPS,39, 40, 41, 42, 43, 44 a finding that could be consistent with a “complex interaction of donor cells and recipient macrophages.”41 These studies support the hypothesized model of the dual roles played by TNF-α and LPS in IPS pathogenesis and suggest there is overlapping biology occurring in the systemic and lung compartments. The cytokines IL-2,42 IL-6,43 and monocyte chemoattractant protein (MCP)-1 are also elevated in clinical IPS.
Although these studies are important progress toward understanding IPS pathobiology, there remains work to be done. For example, it is not known how biology varies between IPS subtypes. A recent study by Seo and colleagues45 highlights another important limitation to our understanding of IPS. Using modern molecular diagnostic technologies, the investigators detected occult potential pathogens in 57% of BAL fluid samples taken from clinically diagnosed IPS cases. Patients with occult microorganisms experienced worse outcomes. This study suggests that infection may play unrecognized roles in IPS development, phenotype, or severity. Alternatively, it is possible that clinical research from which the basic understanding of IPS arose was biased because of misclassification of true infectious pneumonia as IPS. Additional research is needed to progress our ability to develop new preventive and therapeutic strategies for IPS.
Predicting the Development and Outcome of Idiopathic Pneumonia Syndrome
Effective methods to identify patients at highest risk for IPS and predict responsiveness to specific immunomodulatory therapies could focus preventive efforts and treatment on those most likely to benefit. Using an unbiased proteomic approach, Schlatzer and colleagues44 compared profiles of peptides found in blood collected the day of HCT between individuals who subsequently developed IPS and controls. The investigators generated and internally validated high-performing models that used varied combinations of peptides to predict the development of IPS and its response to treatment with etanercept, a soluble TNF-α-binding protein. Several proteins in the acute phase response signaling pathway were selected for inclusion in the prediction models and changed throughout the course of IPS, consistent with dysregulated innate immunity. Although this single study requires validation in an independent population with special attention to the potential role of occult infection, it highlights that biomarkers may be useful to advance our understanding of IPS.
Several other lines of inquiry examined associations between genetic polymorphisms or other biomarkers and the development of end points that overlap with IPS, such as acute lung injury and GVHD.46, 47, 48, 49, 50, 51 Whether the results of these studies are generalizable to IPS and their potential to identify new therapeutic targets is unknown.
Treatments and Outcomes
High-dose systemic corticosteroids and supportive care are the current standard treatments for IPS. Metcalf and colleagues first reported their observations treating 63 people with DAH following autologous or allogeneic HCT.52 Survival to hospital discharge was higher in those treated with more than 30 mg of methylprednisolone daily for 4 to 5 days followed by a taper (67% survival vs 10% on lower doses and 0% with supportive therapy alone). The 3 treatment groups experienced similar infection rates. A subsequent cohort study that included 81 IPS cases confirmed better survival with corticosteroids and showed similar outcomes when comparing 2 mg/kg/d prednisolone with 4 mg/kg/d.19 In these observational studies, corticosteroids may have been withheld from the sickest patients who subsequently died, resulting in an inflated estimate of their benefit. Regardless, survival was unacceptably low at 30% to 33% despite treatment.
In an effort to improve outcomes, a series of studies motivated by preclinical data examined the clinical impact of modulating TNF-α in IPS. In observational studies, coadministration of methylprednisolone 1 to 2 mg/kg/d with etanercept 0.4 mg/kg given twice weekly for a maximum of 8 doses resulted in low toxicity, improved pulmonary physiology,43, 53 and increased short-term survival for IPS.54 In contrast, a randomized placebo-controlled trial of etanercept/glucocorticoid combination therapy showed no survival benefit.55 Importantly, enrollment was terminated early resulting in an increased chance of a false-negative result. In another trial, children receiving etanercept experienced higher rates of survival without supplemental oxygen 28 days after enrollment compared with historical controls.40 Although long-term survival was not studied, 63% of etanercept-treated children remained alive 1 year later, a higher survival rate than seen in prior studies of corticosteroid therapy. The limitations of this trial include the lack of a contemporary control group and potential that participants have different characteristics than the broader population at risk for IPS. Whether etanercept improves survival or not and who is most likely to benefit remains unanswered.
A few other agents may meaningfully modify the biology of IPS; however, currently available evidence does not support their routine use. Keratinocyte growth factor (KGF) protects against chemoradiation-induced epithelial cell injury and enhances tissue repair, limiting IPS severity in mice and GVHD severity in clinical settings.56, 57 The limited data regarding the potential impact of antioxidants on IPS are conflicting.58 Antifibrinolytic therapy may improve outcomes by directly reducing hemorrhage or indirectly by reducing the number of blood component transfusions, though the results of small observational studies are mixed.59, 60 Defibrotide is a profibrinolytic therapy that prevents and improves survival from sinusoidal obstruction syndrome,61, 62 a complication of HCT that also arises from endothelial injury.63 Its use for IPS, however, may be limited by increased risk of hemorrhage. Macrolides suppress production of macrophage-derived cytokines implicated in IPS pathogenesis64 and improve cryptogenic organizing pneumonia in small studies outside HCT settings.65, 66 Macrolides may similarly benefit patients with IPS when administered at doses higher than are commonly used for infection prophylaxis. The recent discovery of Th17 CD4+ T cells67 and their important role in IPS and GVHD28, 36, 68 may lead to new directions using halofuginone 69 or other Th17-suppressing therapies for IPS.
Clinical subtypes of idiopathic pneumonia syndrome
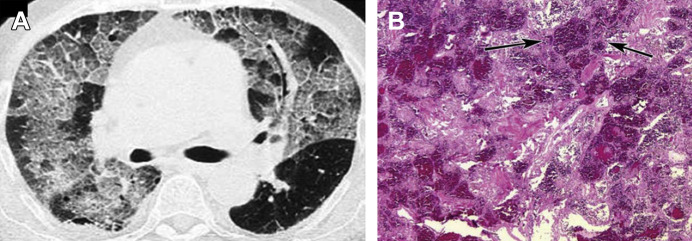
Peri-Engraftment Respiratory Distress Syndrome
Engraftment syndrome (ES) is defined as fever or rash occurring within 5 days of neutrophil engraftment.70 Risk factors for ES include male sex, myeloablative conditioning, high-dose TBI, and non–matched-related stem cell donor.71 A subset of patients with ES develops the noninfectious pulmonary infiltrates and hypoxemia characteristic of peri-engraftment respiratory distress syndrome (PERDS), also known as capillary leak syndrome (Fig. 3 ).72, 73 The capillary leak of PERDS results from activation of engrafting neutrophils, possibly in response to conditioning toxicity or T-cell autoreactivity.72, 74 PERDS occurs after 2.5% of autologous HCT. Its reported incidence varies widely after allogeneic HCT, whereby neutrophil activation may be a component of acute GVHD.75 In the original description of PERDS after autologous HCT, 32% of 19 patients were mechanically ventilated and 26% died.70 Most severe PERDS cases treated with systemic corticosteroids improved. Whereas ES is associated with transplant-related mortality,71, 75 the better response to corticosteroids and higher survival of PERDS relative to other IPS subtypes highlights the fact that IPS subtypes may have importantly different biology.
Fig. 3.
ES in 46-year-old woman with non-Hodgkin lymphoma 3 weeks after allogeneic hematopoietic stem cell transplantation. High-resolution computed tomography scan shows bilateral areas of consolidation having peribronchovascular and subpleural distribution. Note right pleural effusion.
(From Franquet T, Müller NL, Lee KS, et al. Pictorial essay. High-resolution CT and pathologic findings of noninfectious pulmonary complications after hematopoietic stem cell transplantation. Am J Roentgenol 2005;184:629–37. Reprinted with permission from the American Journal of Roentgenology.)
Diffuse Alveolar Hemorrhage
DAH is a subtype of IPS defined as BAL showing any of the following76, 77, 78:
-
•
At least 20% hemosiderin-laden macrophages
-
•
Blood in at least 30% of alveolar surfaces
-
•
Progressively bloodier return on serial lavages
DAH manifests as dyspnea, nonproductive cough or hemoptysis, and hypoxemia with or without fever and may be progressive. Radiographically, diffuse alveolar and interstitial infiltrates in a predominantly central and basilar distribution are particularly suggestive of DAH; however, other patterns of diffuse opacities may be seen (Fig. 4 ).79 Although proposed to be a biologically distinct subtype of IPS,80, 81 DAH epidemiology and its poor outcomes are similar to those of IPS as a whole. In studies specifically examining DAH in transplant settings, incidence ranges from 1% to 21% with similar rates between autologous and allogeneic HCT.80 Median onset ranges from 11 to 19 days after HCT.77, 80, 82, 83 Risk factors for DAH include myeloablative conditioning, TBI, and increased age.79, 80, 81, 84 Respiratory failure requiring mechanical ventilation occurs in most cases, and overall mortality ranges from 64% to 100%.52, 82, 85, 86 High-dose systemic corticosteroids and supportive care that may include platelet transfusions are standard; procoagulant therapies had variable success in small studies and are not routinely used.59, 60, 87, 88
Fig. 4.
DAH in 46-year-old woman with non-Hodgkin lymphoma 3 weeks after allogeneic hematopoietic stem cell transplantation. (A) High-resolution computed tomography scan obtained at level of carina shows diffuse ground-glass opacity in addition to septal thickening (crazy paving). (B) Photomicrograph of histopathologic specimen shows that macrophages containing hemosiderin are present within alveolar spaces (arrows) (hematoxylin-eosin, original magnification ×100).
(From Franquet T, Müller NL, Lee KS, et al. Pictorial essay. High-resolution CT and pathologic findings of noninfectious pulmonary complications after hematopoietic stem cell transplantation. Am J Roentgenol 2005;184:629–37. Reprinted with permission from the American Journal of Roentgenology.)
Delayed Pulmonary Toxicity Syndrome
Delayed pulmonary toxicity syndrome is a subtype of IPS that only occurs after autologous HCT. It presents with exertional dyspnea, nonproductive cough, often fever, reduced diffusing capacity, and radiographic findings of bilateral ground-glass, linear-nodular, consolidative, or mixed opacities. The incidence is 29% to 64% after receiving pre-HCT conditioning regimens containing carmustine (BCNU), cyclophosphamide, and cisplatin in combination. The median time of onset is 45 days (range, 21–149 days), and treatment with corticosteroids (1 mg/kg/d) results in resolution in up to 92% of cases.89
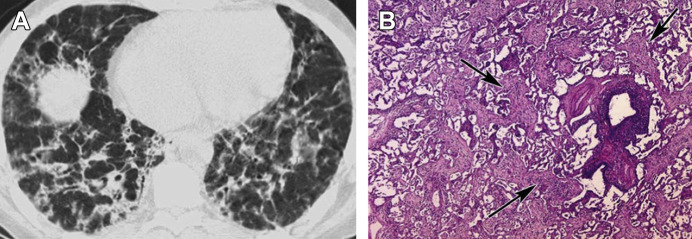
Cryptogenic Organizing Pneumonia/Acute Fibrinous Organizing Pneumonia
Cryptogenic organizing pneumonia (COP), previously called bronchiolitis obliterans-organizing pneumonia, is an idiopathic interstitial pneumonia that occurs after HCT. COP typically manifests as a subacute illness characterized by fever, dyspnea, and nonproductive cough. However, the timing and pace of onset of COP varies; its severity ranges from mild to severe respiratory failure.90 The median onset is 108 days after HCT.91 Risk factors include acute and chronic GVHD, female donors for male recipients, and conditioning with combination cyclophosphamide and TBI.91, 92 Radiographs commonly show unilateral or bilateral patchy foci of consolidation and ground-glass opacities with a subpleural, peribronchial, or bandlike pattern (Fig. 5 ).93 Pulmonary function tests show ventilatory restriction and reduced diffusing capacity with or without obstruction. The definitive diagnosis of COP requires surgical lung biopsy; however, a case presenting with typical clinical features and bronchoscopy excluding infectious pneumonia may justify a treatment trial.94 Histologic samples are characterized by patchy proliferation of immature fibroblasts called Masson bodies in a matrix of loose connective tissue involving the terminal airways, alveolar ducts, and alveoli with or without bronchiolar intraluminal polyps.95 COP most often resolves with several months of corticosteroid therapy and frequently relapses with discontinuation of steroids. In one study of 51 COP cases treated with 1 mg/kg/d prednisolone following HCT, 78% resolved or remained stable and 22% progressed resulting in 16% case fatality.91
Fig. 5.
Organizing pneumonia after hematopoietic stem cell transplantation in 38-year-old man. (A) High-resolution computed tomography scan obtained at level of lower lung zones shows bilateral patchy areas of consolidation in predominantly peribronchial distribution. (B) Photomicrograph of histopathologic specimen shows presence of fibroblastic tissue in lumina of peribronchial alveoli (arrows) (hematoxylin-eosin, original magnification ×100).
(From Franquet T, Müller NL, Lee KS, et al. Pictorial essay. High-resolution CT and pathologic findings of noninfectious pulmonary complications after hematopoietic stem cell transplantation. Am J Roentgenol 2005;184:629–37. Reprinted with permission from the American Journal of Roentgenology.)
Acute fibrinous organizing pneumonia (AFOP) is a recently recognized, rare, and poorly understood complication of HCT.96, 97 AFOP may be part of the spectrum of nonspecific dysregulated response to lung injury along with diffuse alveolar damage and COP.96 AFOP coexistent with COP marks a worse prognosis.98 The original series of 17 AFOP cases described an acute to subacute respiratory illness with bibasilar reticular or nodular infiltrates.99 Histologically, AFOP is characterized by patchy aggregates of intra-alveolar fibrin deposition (fibrin balls) with associated organizing pneumonia and in some cases neutrophilic inflammation of the alveolar walls. The clinical course of AFOP follows one of 2 trajectories: fulminant respiratory failure or subacute disease with recovery after treatment with corticosteroids. Corticosteroids and mycophenolate mofetil dual therapy may be effective for severe cases.100
Toxicities of conditioning and graft-versus-host disease prophylaxis regimens
The patterns of pulmonary toxicity caused by drugs used for pre-HCT conditioning or GVHD are listed in Table 2 . The drugs are categorized as those with established toxicity in HCT and drugs with toxicities observed outside HCT settings.
Table 2.
Pulmonary toxicity of chemotherapeutic and immunosuppressive agents
| Agent | Pulmonary Toxicity |
|---|---|
| Known pulmonary toxicity in HCT | |
| Carmustine | Acute pneumonitis |
| Cyclosporine | Capillary leak (noncardiogenic pulmonary edema), ARDS |
| Sirolimus | Organizing pneumonia, DAH, ARDS, pulmonary alveolar proteinosis |
| Known pulmonary toxicity in other clinical settings | |
| Cyclophosphamide | Interstitial pneumonia, organizing pneumonia |
| Fludarabine | Interstitial pneumonitis, acute eosinophilic pneumonia |
| Azathioprine | Organizing pneumonia, DAH, interstitial pneumonitis, laryngeal edema, vasculitis |
| Tacrolimus | Organizing pneumonia |
| Mycophenolate mofetil | Pulmonary edema, ARDS, pulmonary fibrosis, bronchiectasis |
| Rituximab anti-CD-20 antibody | ARDS, DAH, interstitial pneumonitis, organizing pneumonia, pulmonary fibrosis, hypersensitivity pneumonitis |
| Alemtuzumab anti-CD52 antibody | DAH |
Drugs with Known Toxicities in Hematopoietic Cell Transplant
Carmustine, or BCNU, sometimes used alone or in combination before autologous HCT, is associated with acute-onset pneumonitis with an incidence of 4% to 59%. Prior mediastinal radiation therapy, BCNU dose greater than 1000 mg, and age younger than 54 years are risk factors for developing pneumonitis after autologous HCT for lymphoma.101
Noncardiogenic pulmonary edema and ARDS have been reported in association with cyclosporine after bone marrow transplantation that resolves when the medication is discontinued and is postulated to be an idiosyncratic reaction.102
Sirolimus, used for acute GVHD prophylaxis103 and for primary immunosuppression in active chronic GVHD, causes rare pulmonary toxicities that may be severe and fatal.104, 105 The predominant histologic patterns are organizing pneumonia, pulmonary hemorrhage, diffuse alveolar damage, and in a minority of cases pulmonary alveolar proteinosis.104, 106 The mainstay of treatment is discontinuation of the drug with or without corticosteroids (1 mg/kg/d), which typically results in complete resolution of symptoms within 2 to 4 months.
Drugs with Potential Toxicities in Hematopoietic Cell Transplant
Some chemotherapeutic or immunosuppressive agents used in HCT have known pulmonary toxicities in other clinical settings and should be considered during the evaluation of lung disease following HCT. Cyclophosphamide, used in combination with TBI or other chemotherapy agents in preparative regimens for HCT, is associated with interstitial pneumonia.107 Fludarabine, a purine analogue used in nonmyeloablative conditioning regimens before allogeneic HCT, is infrequently associated with pulmonary toxicity in the forms of interstitial pneumonitis or, less commonly, acute eosinophilic pneumonia usually 3 to 14 days after the last dose.108, 109 Most cases respond to systemic corticosteroid therapy (1 mg/kg/d), suggesting an immunologic mechanism in the pathogenesis. Fludarabine-associated pulmonary toxicity can recur during steroid taper with improvement after reinstitution of steroid therapy.108, 110, 111
Monoclonal antibodies used for prophylaxis or treatment of acute GVHD are infrequently associated with pulmonary toxicity. Rituximab, a chimeric antibody against CD20, can result in ARDS and DAH developing within hours of administration or interstitial pneumonitis and COP developing within weeks.112 Most cases resolve completely after discontinuation of therapy with or without corticosteroids.113 A case series of renal transplant recipients reported DAH after treatment with Alemtuzumab, a cytolytic anti-CD52 monoclonal antibody used in reduced-intensity conditioning regimens to decrease the incidence and severity of acute and chronic GVHD and reduce graft rejection.114
Other noninfectious pulmonary syndromes
Pulmonary Alveolar Proteinosis
In pulmonary alveolar proteinosis (PAP), terminal bronchioles and alveoli accumulate pulmonary surfactant and other amorphous periodic acid Schiff (PAS)–positive lipoproteins consequent to macrophage dysfunction.115, 116 PAP presents with cough, dyspnea, hypoxemia, and diffuse alveolar opacities with central mid and lower lung predominance.117 There are congenital, autoimmune, and secondary forms of PAP. The congenital and autoimmune types arise from malformation of the granulocyte-macrophage colony-stimulating factor (GM-CSF) receptor118, 119 and formation of anti–GM-CSF autoantibody,120 respectively. Secondary PAP occurs rarely after HCT, possibly from macrophage depletion or anti–GM-CSF alloantibody.121 The diagnosis is suggested by bronchoscopy yielding opaque/milky BAL fluid and PAS-positive material present within macrophages after exclusion of infectious pneumonia. However, lung biopsy is required for definitive diagnosis. PAP after HCT may be self-limited but can also progress to fatal respiratory failure. Optimal treatment of this rare entity, including the role of GM-CSF therapy, is unknown. As is done in other settings, whole lung lavage should be considered in severe cases to restore alveolar ventilation with repeat lavage considered for recurrences.122
Venous Thromboembolism
Venous thromboembolism (VTE) is an underrecognized complication of HCT. In a retrospective study of 1,514 HCT recipients, the incidence of symptomatic VTE within the first 180 days after transplantation was 4.6%, including 0.7% incidence of non–catheter-associated lower extremity deep venous thrombosis (DVT) and 0.6% incidence of pulmonary embolism.123 The median time after HCT admission to the development of non–catheter-associated lower extremity DVT and pulmonary embolism was 63 and 66 days, respectively. Prior VTE and GVHD were risk factors for the development of VTE after HCT. Thrombocytopenia was only partially protective against the development of VTE. The safety and efficacy of thromboprophylaxis in patients with HCT remains uncertain. In patients with thrombocytopenia, anticoagulant therapy for documented VTE should be accompanied by platelet transfusions to maintain a platelet count of 5 × 104/L or greater to reduce the risk of bleeding complications.
Pulmonary Cytolytic Thrombus
Pulmonary cytolytic thrombus (PCT) is seen exclusively in allogeneic HCT recipients and almost always in children.124 The incidence of PCT has been reported to range from 1.2% to 4.0% with a median onset at 3 months (range 1.3–11.3 months) after transplant. Clinical manifestations include fever, cough, and respiratory distress. Radiographic findings range from small, peripheral nodules to diffuse opacities. Diagnosis requires lung biopsy with histology characterized by vascular occlusions in distal pulmonary vessels, entrapment of leukocytes, endothelial disruption, and infarction of adjacent tissue. In a single-center, retrospective study, grades II to IV acute and chronic GVHD were independent risk factors for developing PCT. Treatment of PCT consists of systemic corticosteroids (prednisone 1–2 mg/kg/d) until pulmonary symptoms resolve (typically within 2 weeks) followed by a steroid taper over 2 to 4 weeks. The strong association with acute and chronic GVHD, as well as the response to corticosteroid therapy, suggests that PCT is a manifestation of alloreactive lung injury. The prognosis with PCT is favorable, and there have been no reported deaths attributable to this entity.
Pulmonary Hypertension
Pulmonary hypertension can occur after HCT secondary to a variety of causes that are managed by treating the underlying problem, including VTE, left heart failure, and hypoxemia-inducing diseases of the pulmonary parenchyma and airways.125 Pulmonary arterial hypertension (PAH) is rarely reported after HCT and is best described in other clinical contexts.126 This section focuses on pulmonary venoocclusive disease (PVOD), a syndrome of increased vascular resistance that is a rare cause of fatigue, dizziness, weakness, and dyspnea after HCT. Because of the overlapping clinical features, PVOD is easily misdiagnosed as PAH and may represent a spectrum of the same process125; however, it is important to distinguish from PAH because of the therapeutic implications discussed later.
The true incidence, risk factors, and outcomes of PVOD after HCT are unknown given the lack of prospective studies, nonspecific early manifestations, and heterogeneity of clinical phenotype.126, 127 Reported mortalities are close to 100% 2 years from diagnosis.128 PVOD is hypothesized to arise from HCT-related vascular endothelial damage129 and is characterized by pulmonary interstitial edema and capillary congestion due to fibrous occlusion of the postcapillary venules and sometimes larger veins.130 As a result of elevated capillary pressures, PVOD may be accompanied by radiographic evidence of pulmonary edema and pleural effusions.131 Elevated pulmonary artery pressures may be detected on echocardiogram; however, cardiac catheterization is recommended to confirm elevated pulmonary vascular resistance.132 The triad of increased pulmonary vascular resistance with normal left heart filling pressures and radiographic edema is variably present in PVOD133; therefore, surgical lung biopsy should be considered if important for prognostication and referral for lung transplantation.128
Many therapies used in other clinical settings have been tried for PVOD that develops after HCT. Supplemental oxygen should be prescribed for all patients with hypoxemia.134 Although there are case reports describing benefits from systemic anticoagulation or immunosuppression, especially in the presence of autoimmune features, the role of these therapies in the contemporary era of pulmonary vasodilator therapies is unknown.135, 136 In some cases, a trial of systemic immunosuppression may be reasonable.128 Additional potential therapies include diuretics, inotropes, and pulmonary vasodilators (eg, calcium channel blockers, phosphodiesterase-5 inhibitors, endothelin receptor antagonists, prostanoids).126, 128 In contrast to PAH, historical experience with pulmonary vasodilators in PVOD demonstrates mixed results.137, 138, 139 Vasodilators may cause harm and even death in patients with predominantly postcapillary vascular constriction. Alveolar flooding may result from increased perfusion in regions of fixed high postcapillary resistance.140 Consultation with a pulmonary hypertension specialist is advised before giving vasodilators or inotropes to this population. Therapy may be most safely initialized in closely monitored settings.
Transfusion-Related Acute Lung Injury
Transfusion-related acute lung injury (TRALI) is defined as noncardiogenic pulmonary edema and respiratory failure occurring during or within 6 hours of a blood component transfusion.141, 142 TRALI is likely underrecognized in the highly transfused HCT population.143 TRALI is caused by activation of pulmonary-sequestered neutrophils in response to passive transfusion of antibodies or other activating substances.144 TRALI may be mild or result in mechanical ventilation and death.145 Treatment is supportive care.
Summary
A broad spectrum of noninfectious pulmonary syndromes contributes to morbidity and mortality after HCT. By being aware of the syndromes described in this article, practitioners can diagnose important causes of pulmonary dysfunction and institute appropriate therapies. Research is needed to identify individuals at risk for these syndromes and better elucidate their biology in effort to find more effective therapies.
Footnotes
Disclosures: The authors have no disclosures to report.
References
- 1.Gratwohl A., Baldomero H., Aljurf M. Hematopoietic stem cell transplantation: a global perspective. JAMA. 2010;303(16):1617–1624. doi: 10.1001/jama.2010.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gratwohl A., Pasquini M.C., Aljurf M. One million haematopoietic stem-cell transplants: a retrospective observational study. Lancet Haematol. 2015;2(3):e91–e100. doi: 10.1016/S2352-3026(15)00028-9. [DOI] [PubMed] [Google Scholar]
- 3.Horan J.T., Logan B.R., Agovi-Johnson M.A. Reducing the risk for transplantation-related mortality after allogeneic hematopoietic cell transplantation: how much progress has been made? J Clin Oncol. 2011;29(7):805–813. doi: 10.1200/JCO.2010.32.5001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gooley T.A., Chien J.W., Pergan S.A. Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med. 2010;363(22):2091–2101. doi: 10.1056/NEJMoa1004383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giebel S., Labopin M., Holowiecki J. Outcome of HLA-matched related allogeneic hematopoietic stem cell transplantation for patients with acute leukemia in first complete remission treated in Eastern European centers. Better results in recent years. Ann Hematol. 2009;88(10):1005–1013. doi: 10.1007/s00277-009-0719-5. [DOI] [PubMed] [Google Scholar]
- 6.Gratwohl A., Brand R., Frassoni F. Cause of death after allogeneic haematopoietic stem cell transplantation (HSCT) in early leukaemias: an EBMT analysis of lethal infectious complications and changes over calendar time. Bone Marrow Transplant. 2005;36(9):757–769. doi: 10.1038/sj.bmt.1705140. [DOI] [PubMed] [Google Scholar]
- 7.Radhakrishnan S.V., Hildebrandt G.C. A call to arms: a critical need for interventions to limit pulmonary toxicity in the stem cell transplantation patient population. Stem Cell Transplant. 2015;10(1):8–17. doi: 10.1007/s11899-014-0244-z. [DOI] [PubMed] [Google Scholar]
- 8.Clark J.G., Hansen J.A., Hertz M.I. NHLBI workshop summary. Idiopathic pneumonia syndrome after bone marrow transplantation. Am Rev Respir Dis. 1993;147(6 Pt 1):1601–1606. doi: 10.1164/ajrccm/147.6_Pt_1.1601. [DOI] [PubMed] [Google Scholar]
- 9.Englund J.A., Boeckh M., Kuypers J. Brief communications: fatal human metapneumovirus infection in stem-cell transplant recipients. Ann Intern Med. 2006;144:344–349. doi: 10.7326/0003-4819-144-5-200603070-00010. [DOI] [PubMed] [Google Scholar]
- 10.Boeckh M., Erard V., Zerr D. Emerging viral infections after hematopoietic cell transplantation. Pediatr Transplant. 2005;9(Suppl 7):48–54. doi: 10.1111/j.1399-3046.2005.00442.x. [DOI] [PubMed] [Google Scholar]
- 11.Panoskaltsis-Mortari A., Griese M., Madtes D.K. An official American Thoracic Society research statement: noninfectious lung injury after hematopoietic stem cell transplantation: idiopathic pneumonia syndrome. Am J Respir Crit Care Med. 2011;183(9):1262–1279. doi: 10.1164/rccm.2007-413ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams J.V., Martino R., Rabella N. A prospective study comparing human metapneumovirus with other respiratory viruses in adults with hematologic malignancies and respiratory tract infections. J Infect Dis. 2005;192:1061–1065. doi: 10.1086/432732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Renaud C., Xie H., Seo S. Mortality rates of human metapneumovirus and respiratory syncytial virus lower respiratory tract infections in hematopoietic cell transplantation recipients. Biol Blood Marrow Transplant. 2013;19(8):1220–1226. doi: 10.1016/j.bbmt.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Pauw B., Walsh T.J., Donnelly J.P. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813–1821. doi: 10.1086/588660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fisher C.E., Stevens A.M., Leisenring W. Independent contribution of bronchoalveolar lavage and serum galactomannan in the diagnosis of invasive pulmonary aspergillosis. Transpl Infect Dis. 2014;16(3):505–510. doi: 10.1111/tid.12211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neofytos D., Horn D., Anaissie E. Epidemiology and outcome of invasive fungal infection in adult hematopoietic stem cell transplant recipients: analysis of Multicenter Prospective Antifungal Therapy (PATH) Alliance registry. Clin Infect Dis. 2009;48(3):265–273. doi: 10.1086/595846. [DOI] [PubMed] [Google Scholar]
- 17.Ranieri V.M., Rubenfeld G.D., Thompson B.T. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 18.Kantrow S.P., Hackman R.C., Boeckh M. Idiopathic pneumonia syndrome: changing spectrum of lung injury after marrow transplantation. Transplantation. 1997;63(8):1079–1086. doi: 10.1097/00007890-199704270-00006. [DOI] [PubMed] [Google Scholar]
- 19.Fukuda T., Hackman R.C., Guthrie K.A. Risks and outcomes of idiopathic pneumonia syndrome after nonmyeloablative and conventional conditioning regimens for allogeneic hematopoietic stem cell transplantation. Blood. 2003;102(8):2777–2785. doi: 10.1182/blood-2003-05-1597. [DOI] [PubMed] [Google Scholar]
- 20.Sano H., Kobayashi R., Iguchi A. Risk factor analysis of idiopathic pneumonia syndrome after allogeneic hematopoietic SCT in children. Bone Marrow Transplant. 2014;49(1):38–41. doi: 10.1038/bmt.2013.123. [DOI] [PubMed] [Google Scholar]
- 21.Vande Vusse L.K., Madtes D.K., Guthrie K.A. The association between red blood cell and platelet transfusion and subsequently developing idiopathic pneumonia syndrome after hematopoietic stem cell transplantation. Transfusion. 2014;54(4):1071–1080. doi: 10.1111/trf.12396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Solh M., Morgan S., McCullough J. Blood transfusions and pulmonary complications after hematopoietic cell transplantation. Transfusion. 2016;56(3):653–661. doi: 10.1111/trf.13415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keates-Baleeiro J., Moore P., Koyama T. Incidence and outcome of idiopathic pneumonia syndrome in pediatric stem cell transplant recipients. Bone Marrow Transplant. 2006;38(4):285–289. doi: 10.1038/sj.bmt.1705436. [DOI] [PubMed] [Google Scholar]
- 24.Sakaguchi H., Takahashi Y., Watanabe N. Incidence, clinical features, and risk factors of idiopathic pneumonia syndrome following hematopoietic stem cell transplantation in children. Pediatr Blood Cancer. 2012;58(5):780–784. doi: 10.1002/pbc.23298. [DOI] [PubMed] [Google Scholar]
- 25.Yousem S.A. The histological spectrum of pulmonary graft-versus-host disease in bone marrow transplant recipients. Hum Pathol. 1995;26(6):668–675. doi: 10.1016/0046-8177(95)90174-4. [DOI] [PubMed] [Google Scholar]
- 26.Hildebrandt G.C., Olkiewicz K.M., Corrion L.A. Donor-derived TNF-alpha regulates pulmonary chemokine expression and the development of idiopathic pneumonia syndrome after allogeneic bone marrow transplantation. Blood. 2004;104(2):586–593. doi: 10.1182/blood-2003-12-4259. [DOI] [PubMed] [Google Scholar]
- 27.Cooke K.R., Hill G.R., Gerbitz A. Tumor necrosis factor-alpha neutralization reduces lung injury after experimental allogeneic bone marrow transplantation. Transplantation. 2000;70(2):272–279. doi: 10.1097/00007890-200007270-00006. [DOI] [PubMed] [Google Scholar]
- 28.Mauermann N., Burian J., von Garnier C. Interferon-gamma regulates idiopathic pneumonia syndrome, a Th17+CD4+ T-cell-mediated graft-versus-host disease. Am J Respir Crit Care Med. 2008;178(4):379–388. doi: 10.1164/rccm.200711-1648OC. [DOI] [PubMed] [Google Scholar]
- 29.Burman A.C., Banovic T., Kuns R.D. IFN-gamma differentially controls the development of idiopathic pneumonia syndrome and GVHD of the gastrointestinal tract. Blood. 2007;110(3):1064–1072. doi: 10.1182/blood-2006-12-063982. [DOI] [PubMed] [Google Scholar]
- 30.Cooke K.R., Yanik G. Acute lung injury after allogeneic stem cell transplantation: is the lung a target of acute graft-versus-host disease? Bone Marrow Transplant. 2004;34(9):753–765. doi: 10.1038/sj.bmt.1704629. [DOI] [PubMed] [Google Scholar]
- 31.Clark J.G., Madtes D.K., Hackman R.C. Lung injury induced by alloreactive Th1 cells is characterized by host-derived mononuclear cell inflammation and activation of alveolar macrohpages. J Immunol. 1998;161:1913–1920. [PubMed] [Google Scholar]
- 32.Panoskaltsis-Mortari A., Taylor P.A., Yaeger T.M. The critical early proinflammatory events associated with idiopathic pneumonia syndrome in irradiated murine allogeneic recipients are due to donor T cell infusion and potentiated by cyclophosphamide. J Clin Invest. 1997;100(5):1015–1027. doi: 10.1172/JCI119612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cooke K.R., Krenger W., Hill G. Host reactive donor T cells are associated with lung injury after experimental allogeneic bone marrow transplantation. Blood. 1998;92(7):2571–2580. [PubMed] [Google Scholar]
- 34.Shankar G., Bryson J.S., Jennings C.D. Idiopathic pneumonia syndrome in mice after allogeneic bone marrow transplantation. Am J Respir Cell Mol Biol. 1998;18:235–242. doi: 10.1165/ajrcmb.18.2.2988. [DOI] [PubMed] [Google Scholar]
- 35.Holt P.G., Haining S., Nelson D.J. Origin and steady-state turnover of class II MHC-bearing dendritic cells in the epithelium of the conducting airways. J Immunol. 1994;153:256–261. [PubMed] [Google Scholar]
- 36.Varelias A., Gartlan K.H., Kreijveld E. Lung parenchyma-derived IL-6 promotes IL-17A-dependent acute lung injury after allogeneic stem cell transplantation. Blood. 2015;125(15):2435–2444. doi: 10.1182/blood-2014-07-590232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bhalla K.S., Folz R.J. Idiopathic pneumonia syndrome after syngeneic bone marrow transplant in mice. Am J Respir Crit Care Med. 2002;166(12 Pt 1):1579–1589. doi: 10.1164/rccm.200201-044OC. [DOI] [PubMed] [Google Scholar]
- 38.Gerbitz A., Nickoloff B.J., Olkiewicz K. A role for tumor necrosis factor-α-mediated endothelial apoptosis in the development of experimental idiopathic pneumonia syndrome. Transplantation. 2004;78(4):494–502. doi: 10.1097/01.tp.0000128839.13674.02. [DOI] [PubMed] [Google Scholar]
- 39.Holler E., Kolb H.J., Kempeni J. Increased serum levels of tumor necrosis factor alpha precede major complications of bone marrow transplantation. Blood. 1990;4:1011–1016. [PubMed] [Google Scholar]
- 40.Yanik G.A., Grupp S.A., Pulsipher M.A. TNF-receptor inhibitor therapy for the treatment of children with idiopathic pneumonia syndrome. A joint Pediatric Blood and Marrow Transplant Consortium and Children's Oncology Group Study (ASCT0521) Biol Blood Marrow Transplant. 2015;21(1):67–73. doi: 10.1016/j.bbmt.2014.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hauber H.P., Mikkila A., Erich J.M. TNF-alpha, interleukin-10 and interleukin-18 expression in cells of the bronchoalveolar lavage in patients with pulmonary complications following bone marrow or peripheral stem cell transplantation: a preliminary study. Bone Marrow Transplant. 2002;30(8):485–490. doi: 10.1038/sj.bmt.1703722. [DOI] [PubMed] [Google Scholar]
- 42.Clark J.G., Madtes D.K., Marin T.R. Idiopathic pneumonia after bone marrow transplantation: cytokine activation and lipopolysaccharide amplification in the bronchoalveolar compartment. Crit Care Med. 1999;27(9):1800–1806. doi: 10.1097/00003246-199909000-00016. [DOI] [PubMed] [Google Scholar]
- 43.Yanik G.A., Ho V.T., Levine J.E. The impact of soluble tumor necrosis factor receptor etanercept on the treatment of idiopathic pneumonia syndrome after allogeneic hematopoietic stem cell transplantation. Blood. 2008;112(8):3073–3081. doi: 10.1182/blood-2008-03-143412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schlatzer D.M., Dazard J.-E., Ewing R.M. Human biomarker discovery and predictive models for disease progression for idiopathic pneumonia syndrome following allogeneic stem cell transplantation. Mol Cell Proteomics. 2012;11(6) doi: 10.1074/mcp.M111.015479. M111.015479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Seo S., Renaud C., Kuypers J.M. Idiopathic pneumonia syndrome after hematopoietic cell transplantation: evidence of occult infectious etiologies. Blood. 2015;125(24):3789–3797. doi: 10.1182/blood-2014-12-617035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kallianpur A.R. Genomic screening and complications of hematopoietic stem cell transplantation: has the time come? Bone Marrow Transplant. 2005;35(1):1–16. doi: 10.1038/sj.bmt.1704716. [DOI] [PubMed] [Google Scholar]
- 47.Paczesny S., Raiker N., Brooks S. Graft-versus-host disease biomarkers: omics and personalized medicine. Int J Hematol. 2013;98(3):275–292. doi: 10.1007/s12185-013-1406-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dickinson A.M., Harrold J.L., Cullup H. Haematopoietic stem cell transplantation: can our genes predict clinical outcome? Expert Rev Mol Med. 2007;9(29):1–19. doi: 10.1017/S1462399407000488. [DOI] [PubMed] [Google Scholar]
- 49.Miyamoto M., Onizuka M., Machida S. ACE deletion polymorphism is associated with a high risk of non-infectious pulmonary complications after stem cell transplantation. Int J Hematol. 2014;99(2):175–183. doi: 10.1007/s12185-013-1494-6. [DOI] [PubMed] [Google Scholar]
- 50.Ueda N., Chihara D., Kohno A. Predictive value of circulating angiopoietin-2 for endothelial damage-related complications in allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2014;20(9):1335–1340. doi: 10.1016/j.bbmt.2014.04.030. [DOI] [PubMed] [Google Scholar]
- 51.Ponce D.M., Hilden P., Mumaw C. High day 28 ST2 levels predict for acute graft-versus-host disease and transplant-related mortality after cord blood transplantation. Blood. 2015;125(1):199–205. doi: 10.1182/blood-2014-06-584789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Metcalf J.P., Rennard S.I., Reed E.C. Corticosteroids as adjunctive therapy for diffuse alveolar hemorrhage associated with bone marrow transplantation. Am J Med. 1994;96(4):327–334. doi: 10.1016/0002-9343(94)90062-0. [DOI] [PubMed] [Google Scholar]
- 53.Yanik G., Hellerstedt B., Custer J. Etanercept (Enbrel) administration for idiopathic pneumonia syndrome after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2002;8:395–400. doi: 10.1053/bbmt.2002.v8.pm12171486. [DOI] [PubMed] [Google Scholar]
- 54.Tizon R., Frey N., Heitjan D.F. High-dose corticosteroids with or without etanercept for the treatment of idiopathic pneumonia syndrome after allo-SCT. Bone Marrow Transplant. 2012;47(10):1332–1337. doi: 10.1038/bmt.2011.260. [DOI] [PubMed] [Google Scholar]
- 55.Yanik G.A., Horowitz M.M., Weisdorf D.J. Randomized, double-blind, placebo-controlled trial of soluble tumor necrosis factor receptor: Enbrel (etanercept) for the treatment of idiopathic pneumonia syndrome after allogeneic stem cell transplantation: blood and marrow transplant clinical trials network protocol. Biol Blood Marrow Transplant. 2014;20(6):858–864. doi: 10.1016/j.bbmt.2014.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Clouthier S.G., Cooke K.R., Teshima T. Repifermin (keratinocyte growth factor-2) reduces the severity of graft-versus-host disease while preserving a graft-versus-leukemia effect. Biol Blood Marrow Transplant. 2003;9:592–603. doi: 10.1016/s1083-8791(03)00230-1. [DOI] [PubMed] [Google Scholar]
- 57.Panoskaltsis-Mortari A., Taylor P.A., Rubin J.S. Keratinocyte growth factor facilitates alloengraftment and ameliorates graft-versus-host disease in mice by a mechanism independent of repair of conditioning-induced tissue injury. Blood. 2000;96:4350–4356. [PubMed] [Google Scholar]
- 58.Haddad I.Y. Idiopathic pneumonia after marrow transplantation: when are antioxidants effective? Am J Respir Crit Care Med. 2002;166(12 Pt 1):1532–1534. doi: 10.1164/rccm.2209010. [DOI] [PubMed] [Google Scholar]
- 59.Rathi N.K., Tanner A.R., Dinh A. Low-, medium- and high-dose steroids with or without aminocaproic acid in adult hematopoietic SCT patients with diffuse alveolar hemorrhage. Bone Marrow Transplant. 2015;50(3):420–426. doi: 10.1038/bmt.2014.287. [DOI] [PubMed] [Google Scholar]
- 60.Wanko S.O., Broadwater G., Folz R.J. Diffuse alveolar hemorrhage: retrospective review of clinical outcome in allogeneic transplant recipients treated with aminocaproic acid. Biol Blood Marrow Transplant. 2006;12:949–953. doi: 10.1016/j.bbmt.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 61.Corbacioglu S., Cesaro S., Faraci M. Defibrotide for prophylaxis of hepatic veno-occlusive disease in paediatric haemopoietic stem-cell transplantation: an open-label, phase 3, randomised controlled trial. Lancet. 2012;379(9823):1301–1309. doi: 10.1016/S0140-6736(11)61938-7. [DOI] [PubMed] [Google Scholar]
- 62.Richardson P.G., Riches M.L., Kernan N.A. Phase 3 trial of defibrotide for the treatment of severe veno-occlusive disease and multi-organ failure. Blood. 2016;127(13):1656–1665. doi: 10.1182/blood-2015-10-676924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cooke K.R., Jannin A., Ho V. The contribution of endothelial activation and injury to end-organ toxicity following allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2008;14(1 Suppl 1):23–32. doi: 10.1016/j.bbmt.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 64.Cai M., Bonella F., Dai H. Macrolides inhibit cytokine production by alveolar macrophages in bronchiolitis obliterans organizing pneumonia. Immunobiology. 2013;218(6):930–937. doi: 10.1016/j.imbio.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 65.Pathak V., Kuhn J.M., Durham C. Macrolide use leads to clinical and radiological improvement in patients with cryptogenic organizing pneumonia. Ann Am Thorac Soc. 2014;11(1):87–91. doi: 10.1513/AnnalsATS.201308-261CR. [DOI] [PubMed] [Google Scholar]
- 66.Stover D.E., Mangino D. Macrolides: a treatment alternative for bronchiolitis obliterans organizing pneumonia? Chest. 2005;128(5):3611–3617. doi: 10.1378/chest.128.5.3611. [DOI] [PubMed] [Google Scholar]
- 67.Weaver C.T., Elson C.O., Fouser L.A. The Th17 pathway and inflammatory diseases of the intestines, lungs, and skin. Annu Rev Pathol. 2013;8:477–512. doi: 10.1146/annurev-pathol-011110-130318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Carlson M.J., West M.L., Coghill J.M. In vitro-differentiated Th17 cells mediate lethal acute graft-versus-host disease with severe cutaneous and pulmonary pathologic manifestations. Blood. 2009;113(6):1365–1374. doi: 10.1182/blood-2008-06-162420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sundrud M.S., Koralov S.B., Feuerer M. Halofuginone inhibits Th17 cell differentiation by activating the amino acid starvation response. Science. 2009;324(5932):1334–1338. doi: 10.1126/science.1172638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Capizzi S.A., Kumar S., Huneke N.E. Peri-engraftment respiratory distress syndrome during autologous hematopoietic stem cell transplantation. Bone Marrow Transplant. 2001;27:1299–1303. doi: 10.1038/sj.bmt.1703075. [DOI] [PubMed] [Google Scholar]
- 71.Schmid I., Stachel D., Pagel P. Incidence, predisposing factors, and outcome of engraftment syndrome in pediatric allogeneic stem cell transplant recipients. Biol Blood Marrow Transplant. 2008;14(4):438–444. doi: 10.1016/j.bbmt.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 72.Spitzer T.R. Engraftment syndrome following hematopoietic stem cell transplantation. Bone Marrow Transplant. 2001;27:893–898. doi: 10.1038/sj.bmt.1703015. [DOI] [PubMed] [Google Scholar]
- 73.Cahill R.A., Spitzer T.R., Mazumder A. Marrow engraftment and clinical manifestations of capillary leak syndrome. Bone Marrow Transplant. 1996;18(1):177–184. [PubMed] [Google Scholar]
- 74.Afessa B., Abdulai R.M., Kremers W.K. Risk factors and outcome of pulmonary complications after autologous hematopoietic stem cell transplant. Chest. 2012;141(2):442–450. doi: 10.1378/chest.10-2889. [DOI] [PubMed] [Google Scholar]
- 75.Chang L., Frame D., Braun T. Engraftment syndrome after allogeneic hematopoietic cell transplantation predicts poor outcomes. Biol Blood Marrow Transplant. 2014;20(9):1407–1417. doi: 10.1016/j.bbmt.2014.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.De Lassence A., Fleury-Feith J., Escudier E. Alveolar hemorrhage. Diagnostic criteria and results in 194 immuncompromised hosts. Am J Respir Crit Care Med. 1995;131:157–163. doi: 10.1164/ajrccm.151.1.7812547. [DOI] [PubMed] [Google Scholar]
- 77.Robbins R.A., Linder J., Stahl M.G. Diffuse alveolar hemorrhage in autologous bone marrow transplant recipients. Am J Med. 1989;87(5):511–518. doi: 10.1016/s0002-9343(89)80606-0. [DOI] [PubMed] [Google Scholar]
- 78.Agusti C., Ramirez J., Picado A. Diffuse alveolar hemorrhage in allogeneic bone marrow transplantation: a postmortem study. Am J Respir Crit Care Med. 1995;151:1006–1010. doi: 10.1164/ajrccm/151.4.1006. [DOI] [PubMed] [Google Scholar]
- 79.Witte R.J., Gurney J.W., Robbins R.A. Diffuse pulmonary alveolar hemorrhage after bone marrow transplantation: radiographic findings in 39 patients. AJR Am J Roentgenol. 1991;157(3):461–464. doi: 10.2214/ajr.157.3.1872226. [DOI] [PubMed] [Google Scholar]
- 80.Afessa B., Tefferi A., Litzow M.R. Diffuse alveolar hemorrhage in hematopoietic stem cell transplant recipients. Am J Respir Crit Care Med. 2002;166(5):641–645. doi: 10.1164/rccm.200112-141cc. [DOI] [PubMed] [Google Scholar]
- 81.Majhail N.S., Parks K., Defor T.E. Diffuse alveolar hemorrhage and infection-associated alveolar hemorrhage following hematopoietic stem cell transplantation: related and high-risk clinical syndromes. Biol Blood Marrow Transplant. 2006;12(10):1038–1046. doi: 10.1016/j.bbmt.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 82.Lewis I.D., DeFor T., Weisdorf D.J. Increasing incidence of diffuse alveolar hemorrhage following allogeneic bone marrow transplantation: cryptic etiology and uncertain therapy. Bone Marrow Transpl. 2000;26:539–543. doi: 10.1038/sj.bmt.1702546. [DOI] [PubMed] [Google Scholar]
- 83.Raptis A., Marvroudis D., Suffredini A.F. High-dose corticosteroid therapy for diffuse alveolar hemorrhage in allogeneic bone marrow stem cell transplant recipients. Bone Marrow Transplant. 1999;24:879–883. doi: 10.1038/sj.bmt.1701995. [DOI] [PubMed] [Google Scholar]
- 84.Sisson J.H., Thompson A.B., Anderson J.R. Airway inflammation predicts diffuse alveolar hemorrhage during bone marrow transplantation in patients with Hodgkin disease. Am Rev Respir Dis. 1992;146:439–443. doi: 10.1164/ajrccm/146.2.439. [DOI] [PubMed] [Google Scholar]
- 85.Nevo S., Swan V., Enger C. Acute bleeding after bone marrow transplantation (BMT) - incidence and effect on survival. A quantitative analysis in 1,402 patients. Blood. 1998;91(4):1469–1477. [PubMed] [Google Scholar]
- 86.Wojno K.J., Vogelsang G.B., Beschorner W.E. Pulmonary hemorrhage as a cause of death in allogeneic bone marrow recipients with severe acute graft-versus-host disease. Transplantation. 1994;57(1):88–92. doi: 10.1097/00007890-199401000-00016. [DOI] [PubMed] [Google Scholar]
- 87.Baker M.S., Diab K.J., Carlos W.G. Intrapulmonary recombinant factor VII as effective treatment for diffuse alveolar hemorrhage. J Bronchology Interv Pulmonol. 2016;23(3):255–258. doi: 10.1097/LBR.0000000000000286. [DOI] [PubMed] [Google Scholar]
- 88.Elinoff J.M., Bagci U., Moriyama B. Recombinant human factor VIIa for alveolar hemorrhage following allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2014;20(7):969–978. doi: 10.1016/j.bbmt.2014.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wilczynski S.W., Erasmus J.J., Petros W.P. Delayed pulmonary toxicity syndrome following high-dose chemotherapy and bone marrow transplantation for breast cancer. Am J Respir Crit Care Med. 1998;157(2):565–573. doi: 10.1164/ajrccm.157.2.9705072. [DOI] [PubMed] [Google Scholar]
- 90.American Thoracic Society, European Respiratory Society American Thoracic Society/European Respiratory Society international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2002;165(2):277–304. doi: 10.1164/ajrccm.165.2.ats01. [DOI] [PubMed] [Google Scholar]
- 91.Freudenberger T.D., Madtes D.K., Curtis J.R. Association between acute and chronic graft-versus-host disease and bronchiolitis obliterans organizing pneumonia in recipients of hematopoietic stem cell transplants. Blood. 2003;102(10):3822–3828. doi: 10.1182/blood-2002-06-1813. [DOI] [PubMed] [Google Scholar]
- 92.Nakasone H., Onizuka M., Suzuki N. Pre-transplant risk factors for cryptogenic organizing pneumonia/bronchiolitis obliterans organizing pneumonia after hematopoietic cell transplantation. Bone Marrow Transplant. 2013;48(10):1317–1323. doi: 10.1038/bmt.2013.116. [DOI] [PubMed] [Google Scholar]
- 93.Pipavath S.N.J., Chung J.H., Chien J.W. Organizing pneumonia in recipients of hematopoietic stem cell transplantation: CT features in 16 patients. J Comput Assist Tomogr. 2012;36:431–436. doi: 10.1097/RCT.0b013e31825ba274. [DOI] [PubMed] [Google Scholar]
- 94.Cottin V., Cordier J.F. Cryptogenic organizing pneumonia. Semin Respir Crit Care Med. 2012;33(5):462–475. doi: 10.1055/s-0032-1325157. [DOI] [PubMed] [Google Scholar]
- 95.Tabaj G.C., Fernandez C.F., Sabbagh E. Histopathology of the idiopathic interstitial pneumonias (IIP): a review. Respirology. 2015;20(6):873–883. doi: 10.1111/resp.12551. [DOI] [PubMed] [Google Scholar]
- 96.Travis W.D., Costabel U., Hansell D.M. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188(6):733–748. doi: 10.1164/rccm.201308-1483ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lee S.M., Park J.J., Sung S.H. Acute fibrinous and organizing pneumonia following hematopoietic stem cell transplantation. Korean J Intern Med. 2009;24(2):156–159. doi: 10.3904/kjim.2009.24.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nishino M., Mathai S.K., Schoenfeld D. Clinicopathologic features associated with relapse in cryptogenic organizing pneumonia. Hum Pathol. 2014;45(2):342–351. doi: 10.1016/j.humpath.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 99.Beasley M.B., Franks T.J., Galvin J.R. Acute fibrinous and organizing pneumonia: a histological pattern of lung injury and possible variant of diffuse alveolar damage. Arch Pathol Lab Med. 2002;126(9):1064–1070. doi: 10.5858/2002-126-1064-AFAOP. [DOI] [PubMed] [Google Scholar]
- 100.Bhatti S., Hakeem A., Torrealba J. Severe acute fibrinous and organizing pneumonia (AFOP) causing ventilatory failure: successful treatment with mycophenolate mofetil and corticosteroids. Respir Med. 2009;103(11):1764–1767. doi: 10.1016/j.rmed.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 101.Lane A.A., Armand P., Feng Y. Risk factors for development of pneumonitis after high-dose chemotherapy with cyclophosphamide, BCNU and etoposide followed by autologous stem cell transplant. Leuk Lymphoma. 2012;53(6):1130–1136. doi: 10.3109/10428194.2011.645208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Madtes D.K. Pulmonary complications of stem cell and solid organ transplantation. In: Broaddus V.C., editor. Murray and Nadel's textbook of respiratory medicine. 6th edition. vol. 2. Saunders; Philadelphia: 2016. pp. 1612–1623.e8. [Google Scholar]
- 103.Cutler C., Logan B., Nakamura R. Tacrolimus/sirolimus vs tacrolimus/methotrexate as GVHD prophylaxis after matched, related donor allogeneic HCT. Blood. 2014;124(8):1372–1377. doi: 10.1182/blood-2014-04-567164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Garrod A.S., Goyal R.K., Weiner D.J. Sirolimus-induced interstitial lung disease following pediatric stem cell transplantation. Pediatr Transplant. 2015;19(3):E75–E77. doi: 10.1111/petr.12438. [DOI] [PubMed] [Google Scholar]
- 105.Patel A.V., Hahn T., Bogner P.N. Fatal diffuse alveolar hemorrhage associated with sirolimus after allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2010;45(8):1363–1364. doi: 10.1038/bmt.2009.339. [DOI] [PubMed] [Google Scholar]
- 106.Champion L., Stern M., Israel-Biet D. Brief communication: sirolimus-associated pneumonitis: 24 cases in renal transplant recipients. Ann Intern Med. 2006;144(7):505–509. doi: 10.7326/0003-4819-144-7-200604040-00009. [DOI] [PubMed] [Google Scholar]
- 107.Malik S.W., Myers J.L., DeRemee R.A. Lung toxicity associated with cyclophosphamide use. Two distinct patterns. Am J Respir Crit Care Med. 1996;154(6 Pt 1):1851–1856. doi: 10.1164/ajrccm.154.6.8970380. [DOI] [PubMed] [Google Scholar]
- 108.Helman D.L., Jr., Byrd J.C., Ales N.C. Fludarabine-related pulmonary toxicity: a distinct clinical entity in chronic lymphoproliferative syndromes. Chest. 2002;122(3):785–790. doi: 10.1378/chest.122.3.785. [DOI] [PubMed] [Google Scholar]
- 109.Trojan A., Meier R., Licht A. Eosinophilic pneumonia after administration of fludarabine for the treatment of non-Hodgkin's lymphoma. Ann Hematol. 2002;81:535–537. doi: 10.1007/s00277-002-0497-9. [DOI] [PubMed] [Google Scholar]
- 110.Hurst P.G., Habib M.P., Garewal H. Pulmonary toxicity associated with fludarabine monophosphate. Invest New Drugs. 1987;5(2):207–210. doi: 10.1007/BF00203548. [DOI] [PubMed] [Google Scholar]
- 111.Disel U., Paydas S., Yavuz S. Severe pulmonary toxicity associated with fludarabine and possible contribution of rituximab. Chemotherapy. 2010;56(2):89–93. doi: 10.1159/000305255. [DOI] [PubMed] [Google Scholar]
- 112.Liote H., Liote F., Seroussi B. Rituximab-induced lung disease: a systematic literature review. Eur Respir J. 2010;35(3):681–687. doi: 10.1183/09031936.00080209. [DOI] [PubMed] [Google Scholar]
- 113.Hadjinicolaou A.V., Nisar M.K., Parfrey H. Non-infectious pulmonary toxicity of rituximab: a systematic review. Rheumatology (Oxford) 2012;51(4):653–662. doi: 10.1093/rheumatology/ker290. [DOI] [PubMed] [Google Scholar]
- 114.Sachdeva A., Matuschak G.M. Diffuse alveolar hemorrhage following alemtuzumab. Chest. 2008;133(6):1476–1478. doi: 10.1378/chest.07-2354. [DOI] [PubMed] [Google Scholar]
- 115.Rosen S.H., Castleman B., Liebow A.A. Pulmonary alveolar proteinosis. N Engl J Med. 1958;258:1123–1142. doi: 10.1056/NEJM195806052582301. [DOI] [PubMed] [Google Scholar]
- 116.Seymour J.F., Presneill J.J. Pulmonary alveolar proteinosis: progress in the first 44 years. Am J Respir Crit Care Med. 2002;166(2):215–235. doi: 10.1164/rccm.2109105. [DOI] [PubMed] [Google Scholar]
- 117.Trapnell B.C., Whitsett J.A., Nakata K. Pulmonary alveolar proteinosis. N Engl J Med. 2003;349:2527–2539. doi: 10.1056/NEJMra023226. [DOI] [PubMed] [Google Scholar]
- 118.Dirksen U., Nishinakamura R., Groneck P. Human pulmonary alveolar proteinosis associated with a defect in GM-CSF/IL-3/IL-5 receptor common beta chain expression. J Clin Invest. 1997;100(9):2211–2217. doi: 10.1172/JCI119758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Suzuki T., Sakagami T., Rubin B.K. Familial pulmonary alveolar proteinosis caused by mutations in CSF2RA. J Exp Med. 2008;205(12):2703–2710. doi: 10.1084/jem.20080990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sakagumi T., Uchida K., Suzuki T. Human GM-CSF autoantibodies and reproduction of pulmonary alveolar proteinosis. N Engl J Med. 2009;361(27):2679–2681. doi: 10.1056/NEJMc0904077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Pidala J., Khalil F., Fernandez H. Pulmonary alveolar proteinosis following allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2011;46(11):1480–1483. doi: 10.1038/bmt.2010.321. [DOI] [PubMed] [Google Scholar]
- 122.Beccaria M., Luisetti M., Rodi G. Long-term durable benefit after whole lung lavage in pulmonary alveolar proteinosis. Eur Respir J. 2004;23(4):526–531. doi: 10.1183/09031936.04.00102704. [DOI] [PubMed] [Google Scholar]
- 123.Gerber D.E., Segal J.B., Levy M.Y. The incidence of and risk factors for venous thromboembolism (VTE) and bleeding among 1514 patients undergoing hematopoietic stem cell transplantation: implications for VTE prevention. Blood. 2008;112(3):504–510. doi: 10.1182/blood-2007-10-117051. [DOI] [PubMed] [Google Scholar]
- 124.Woodard J.P., Gulbahce E., Shreve M. Pulmonary cytolytic thrombi: a newly recognized complication of stem cell transplantation. Bone Marrow Transplant. 2000;25(3):293–300. doi: 10.1038/sj.bmt.1702137. [DOI] [PubMed] [Google Scholar]
- 125.Simonneau G., Gatzoulis M.A., Adatia I. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D34–D41. doi: 10.1016/j.jacc.2013.10.029. [DOI] [PubMed] [Google Scholar]
- 126.Dandoy C.E., Hirsch R., Chima R. Pulmonary hypertension after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2013;19(11):1546–1556. doi: 10.1016/j.bbmt.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 127.Bunte M.C., Patnaik M.M., Pritzker M.R. Pulmonary veno-occlusive disease following hematopoietic stem cell transplantation: a rare model of endothelial dysfunction. Bone Marrow Transplant. 2008;41(8):677–686. doi: 10.1038/sj.bmt.1705990. [DOI] [PubMed] [Google Scholar]
- 128.Mandel J., Mark E.J., Hales C.A. Pulmonary veno-occlusive disease. Am J Respir Crit Care Med. 2000;162:1964–1973. doi: 10.1164/ajrccm.162.5.9912045. [DOI] [PubMed] [Google Scholar]
- 129.Jodele S., Hirsch R., Laskin B. Pulmonary arterial hypertension in pediatric patients with hematopoietic stem cell transplant-associated thrombotic microangiopathy. Biol Blood Marrow Transplant. 2013;19(2):202–207. doi: 10.1016/j.bbmt.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 130.Troussard X., Bernaudin J.F., Cordonnier C. Pulmonary veno-occlusive disease after bone marrow transplantation. Thorax. 1984;39:956–957. doi: 10.1136/thx.39.12.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Resten A., Maitre S., Humbert M. Pulmonary hypertension: CT of the chest in pulmonary venoocclusive disease. AJR Am J Roentgenol. 2004;183:65–70. doi: 10.2214/ajr.183.1.1830065. [DOI] [PubMed] [Google Scholar]
- 132.Galie N., Humbert M., Vachiery J.L. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2015;46:903–975. doi: 10.1183/13993003.01032-2015. [DOI] [PubMed] [Google Scholar]
- 133.Rambihar V.S., Fallen E.L., Cairns J.A. Pulmonary veno-occlusive disease: antemortem diagnosis from roentgenographic and hemodynamic findings. Can Med Assoc J. 1979;120:1519–1522. [PMC free article] [PubMed] [Google Scholar]
- 134.Roberts D.H., Lepore J.J., Maroo A. Oxygen therapy improves cardiac index and pulmonary vascular resistance in patients with pulmonary hypertension. Chest. 2001;120(5):1547–1555. doi: 10.1378/chest.120.5.1547. [DOI] [PubMed] [Google Scholar]
- 135.Frank H., Ruber K., Mlczoch J. The effect of anticoagulant therapy in primary and anorectic drug-induced pulmonary hypertension. Chest. 1997;112(3):714–721. doi: 10.1378/chest.112.3.714. [DOI] [PubMed] [Google Scholar]
- 136.Sanderson J.E., Spiro S.G., Hendry A.T. A case of pulmonary veno-occlusive disease responding to treatment with azathioprine. Thorax. 1977;32:140–148. doi: 10.1136/thx.32.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kuroda T., Hirota H., Masaki M. Sildenafil as adjunct therapy to high-dose epoprostenol in a patient with pulmonary veno-occlusive disease. Heart Lung Circ. 2006;15(2):139–142. doi: 10.1016/j.hlc.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 138.Okumura H., Nagaya N., Kyotani S. Effects of continuous IV prostacyclin in a patient with pulmonary veno-occlusive disease. Chest. 2002;122(3):1096–1098. doi: 10.1378/chest.122.3.1096. [DOI] [PubMed] [Google Scholar]
- 139.Palevsky H.I., Pietra G.G., Fishman A.P. Pulmonary veno-occlusive disease and its response to vasodilator agents. Am Rev Respir Dis. 1990;142:426–429. doi: 10.1164/ajrccm/142.2.426. [DOI] [PubMed] [Google Scholar]
- 140.Palmer S.M., Robinson L.J., Wang A. Massive pulmonary edema and death after prostacyclin infusion in a patient with pulmonary veno-occlusive disease. Chest. 1998;113(1):237–240. doi: 10.1378/chest.113.1.237. [DOI] [PubMed] [Google Scholar]
- 141.Kleinman S., Caulfield T., Chan P. Toward an understanding of transfusion-related acute lung injury: statement of a consensus panel. Transfusion. 2004;44:1774–1789. doi: 10.1111/j.0041-1132.2004.04347.x. [DOI] [PubMed] [Google Scholar]
- 142.Toy P., Popovsky M.A., Abraham E. Transfusion-related acute lung injury: definition and review. Crit Care Med. 2005;33(4):721–726. doi: 10.1097/01.ccm.0000159849.94750.51. [DOI] [PubMed] [Google Scholar]
- 143.Ganguly S., Carrum G., Nizzi F. Transfusion-related acute lung injury (TRALI) following allogeneic stem cell transplant for acute myeloid leukemia. Am J Hematol. 2004;75:48–51. doi: 10.1002/ajh.10452. [DOI] [PubMed] [Google Scholar]
- 144.Bux J., Sachs U.J. The pathogenesis of transfusion-related acute lung injury (TRALI) Br J Haematol. 2007;136(6):788–799. doi: 10.1111/j.1365-2141.2007.06492.x. [DOI] [PubMed] [Google Scholar]
- 145.Looney M.R., Roubinian N., Gajic O. Prospective study on the clinical course and outcomes in transfusion-related acute lung injury. Crit Care Med. 2014;42(7):1676–1687. doi: 10.1097/CCM.0000000000000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Meyers J.D., Flournoy N., Thomas E.D. Nonbacterial pneumonia after allogeneic marrow transplantation: a review of ten years' experience. Rev Infect Dis. 1982;4(6):1119–1132. doi: 10.1093/clinids/4.6.1119. [DOI] [PubMed] [Google Scholar]
- 147.Weiner R.S., Horowitz M.M., Gale R.P. Risk factors for interstitial pneumonia following bone marrow transplantation for severe aplastic anemia. Br J Haematol. 1989;71:535–543. doi: 10.1111/j.1365-2141.1989.tb06314.x. [DOI] [PubMed] [Google Scholar]
- 148.Wingard J.R., Mellits E.D., Sostrin M.B. Interstitial pneumonitis after allogeneic bone marrow transplantation: nine-year experience at a single institution. Medicine. 1988;67(3):175–186. doi: 10.1097/00005792-198805000-00004. [DOI] [PubMed] [Google Scholar]
- 149.Bilgrami S.F., Metersky M.L., McNally D. Idiopathic pneumonia syndrome following myeloablative chemotherapy and autologous transplantation. Ann Pharmacother. 2001;35:196–201. doi: 10.1345/aph.10071. [DOI] [PubMed] [Google Scholar]
- 150.Wong R., Rondon G., Saliba R.M. Idiopathic pneumonia syndrome after high-dose chemotherapy and autologous hematopoietic stem cell transplantation for high-risk breast cancer. Bone Marrow Transplant. 2003;31:1157–1163. doi: 10.1038/sj.bmt.1704141. [DOI] [PubMed] [Google Scholar]
- 151.Zhu K.E., Hu J.Y., Zhang T. Incidence, risks, and outcome of idiopathic pneumonia syndrome early after allogeneic hematopoietic stem cell transplantation. Eur J Haematol. 2008;81(6):461–466. doi: 10.1111/j.1600-0609.2008.01149.x. [DOI] [PubMed] [Google Scholar]