Abstract
Infectious enteritis in adult ruminants is often a result of 1 or more viral, bacterial, or parasitic pathogens. Diagnosis of etiologic agents causing enteritis is important when considering herd implications and zoonotic potential of some etiologies. Differential diagnoses for enteritis in adult ruminants is not simple based on clinical signs alone. Diagnostic samples include feces, blood, and antemortem and postmortem tissues. Treatment of infectious enteritis is aimed at correcting dehydration and electrolyte imbalances secondary to diarrhea. In cases of some bacterial and parasitic pathogens, additional targeted treatment and control are recommended. Management of enteritis may be instituted while awaiting laboratory test results.
Keywords: Ruminant, Enteritis, Infection, Adult, Diarrhea, Treatment
Key points
-
•
Viral, bacterial, and protozoal pathogens are the most significant causes of infectious enteritis in adult ruminants.
-
•
The most common consistent presenting sign in ruminants with infectious enteritis is diarrhea.
-
•
Diagnosis of etiology of enteritis has important zoonotic and herd implications.
-
•
Severity of clinical signs with similar pathogens may differ between large and small ruminants.
-
•
Treatment of enteritis is symptomatic to correct fluid and electrolyte imbalances and, when relevant, pathogen-specific treatment.
Introduction
Enteritis refers to the inflammation of the intestine. Several bacterial, protozoal, and viral diseases cause infectious enteritis in adult cattle and small ruminants. Diagnosis of specific pathogens is warranted, particularly when herd implications or zoonotic implications are considered. This review summarizes the most important differential diagnoses, diagnosis, and management of infectious enteritis in adult ruminants. Important diagnostic samples, diagnostic tests, supportive therapy, and specific treatments for infectious enteritis are discussed.
Pathophysiology of infectious enteritis in adult ruminants
The pathophysiology of diarrhea secondary to enteritis in adult ruminants is similar to young ruminants. In adult ruminants, diarrhea is more likely to develop due to maldigestion and malabsorption secondary to infectious enteritis, whereas osmotic diarrhea is likely to develop secondary to carbohydrate engorgement. Detailed pathophysiologic mechanism of diarrhea in young ruminants please see Meera C. Heller and Munashe Chigerwe’s article “Diagnosis and treatment of infectious enteritis in neonatal and juvenile ruminants,” in this issue.
Patient history
The most common presenting clinical sign associated with enteritis in ruminants is diarrhea. Patient history should include information regarding the age and use of the animal (eg, dairy, beef, or show), presence of hyporexia or anorexia, duration and progression of diarrhea, number of animals affected or dead in the herd or flock, vaccination history, deworming history, recent dietary or husbandry changes, recent transportation, reproductive status (eg, pregnant), characteristics of the diarrhea (eg, color, odor, and volume of feces and presence of tenesmus, blood, mucus, or gravel), and evidence of abdominal pain (eg, arching of back, treading of hind feet, or lying down).
Physical examination
In clinic settings, ruminant patients should be should be examined in the isolation area according to infectious disease control protocols. In farm settings, a cow may be examined in a sick pen or handling facilities when applicable. In either scenario, the examination room or facility should be cleaned and disinfected after the examination. The examiner should wear personal protective equipment (eg, gloves, boots that can be disinfected, and coveralls).
Although it is necessary to perform a full physical examination in a ruminant patient with enteritis, this review focuses on the specific organ examination for ruminants with enteritis. This includes the following:
-
•
Body condition — enteritis may be associated with weight loss.
-
•
Posture — posture of the patient may indicate evidence of abdominal pain, for instance, abdominal distension, arching of back, treading of hind feet, or lying down.
-
•
Rectal temperature — enteritis is an inflammatory condition, which may cause pyrexia.
-
•
Oral examination — checking for evidence of oral ulceration and hypersalivation (ptyalism). This is important because some viral causes of enteritis also cause oral lesions.
-
•
Assessment of hydration status and mucous membrane color — hydration status and color of mucous membranes (ocular, oral, and or vulva), including capillary refill time should be assessed.
-
•
Abdominal palpation, auscultation, percussion, and succussion — abdominal palpation is practical in adult sheep and goats but unrewarding in adult cattle. Abdominal palpation may help identify evidence of pain or allow palpation of abdominal viscera. Simultaneous auscultation and percussion on the left and right abdominal wall help identify viscera filled with air, including the intestine. Succussion of the abdomen confirms the presence of excessive fluid in abdominal viscera, including the small intestine.
-
•
Rectal examination — rectal examination is practical in cattle but may be delayed in cases of presence of a rectal prolapse (secondary to diarrhea). Rectal examination aids in identifying distended abdominal viscera, including small intestine, rumen, colon, or cecum. If not performed already, characteristics of the diarrhea (eg, color, odor, and volume of feces and presence of tenesmus, blood, mucus, or gravel) should be evaluated during the rectal examination and by evaluating feces on the rectal sleeve.
Differential diagnoses
-
•
Important differential diagnoses for infectious enteritis can be broadly classified into bacterial (salmonellosis, paratuberculosis, and Clostridium perfringens type A), viral (bovine viral diarrhea [BVD]virus, malignant catarrhal fever, and bovine coronavirus [BCoV]), and parasitic (coccidiosis and nematodiasis).
-
•
Differential diagnoses, species affected, recommended samples, and diagnostic tests to be requested for infectious causes of enteritis in adult ruminants are summarized in Table 1 .
-
•
An in-depth discussion of paratuberculosis (see Marie-Eve Fecteau’s article “Paratuberculosis in Cattle,” in this issue), coccidiosis and nematodiasis (see Sarah Tammy Nicole Keeton and Christine B. Navarre’s article “Coccidiosis in Large and Small Ruminants,” in this issue), clostridial enteritis (see Robert Callan’s article “Clostridial Abomasitis and Enteritis in Ruminants,” in this issue), and herd assessment and control of Salmonella are reviewed. This article briefly describes the salient features of the various diseases causing infectious enteritis in adult ruminants.
Table 1.
Important differential diagnoses, species affected, recommended samples, and diagnostic tests to be requested for infectious causes of enteritis in adult ruminants
| Differential Diagnosis | Species Affected | Samples | Tests |
|---|---|---|---|
| Bacterial | |||
| Salmonellosis | Bovine, caprine, ovine | Feces | Culture, PCR |
| Blood | Culture | ||
| Intestinal tissues | Culture | ||
| Paratuberculosis | Bovine, caprine, ovine | Feces | Culture, PCR |
| Serum | ELISA or AGID | ||
| Intestinal tissues | Culture Histopathology |
||
| Milk | ELISA or AGID | ||
| Mesenteric lymph node | Culture Histopathology |
||
| C perfringens | Bovine, caprine, ovine | Feces or intestinal contents | Anaerobic culture Genomic-type testing Immunohistochemistry ELISA—toxin testing for types A, B, C, and D |
| Viral | |||
| BVD virus | Bovine | EDTA blood, milk, serum, tissue | PCR for acute infections |
| Tissue (ear notch) | Antigen capture ELISA, IHC | ||
| Malignant catarrhal fever | Bovine | EDTA blood, lung, spleen | PCR |
| BCoV | Bovine | Feces | PCR |
| Parasitic | |||
| Coccidiosis | Bovine, caprine, and ovine | Feces | Fecal flotation |
| Nematodiasis | Bovine, caprine, and ovine | Feces | Fecal flotation |
Abbreviations: AGID, agar gel immunodiffusion; IHC, immunohistochemistry; PCR, polymerase chain reaction.
Bacterial Enteritis
Salmonellosis
-
•
Salmonella enterica subsp enterica serovars (serotypes) are of clinical importance in adult ruminants. Examples of important serovars include Typhimurium, Dublin, and Newport.1
-
•
Transmission is through the fecal-oral route in all ages. Transmission via milk or colostrum is a possible route of infection for neonates.
-
•
Clinical signs associated with salmonellosis in adult ruminants include pyrexia and diarrhea.2 The diarrheic feces may vary from watery to mucoid and may contain fibrin and blood.3 Due to the presence of significant concentrations of proteins, the diarrheic feces have a putrid, foul odor.3
-
•
Endotoxemia may occur in part due to the damaged intestinal mucosa, leading to pyrexia, depressed attitude, and shock. Bacteremia is also possible secondary to the enteritis. The enteritis causes an acute protein-losing enteropathy.
-
•
Some Salmonella serotypes are potentially zoonotic (eg, Salmonella Typhimurium and Salmonella Newport)4 whereas Salmonella Dublin is host-adapted (serotypes found in the host species and long-term carriers exist) in cattle.3
Paratuberculosis
-
•
Paratuberculosis (Johne disease) is a chronic enteric disease of ruminants caused by the bacterium, Mycobacterium avium subsp paratuberculosis.
-
•
Transmission of the bacterium is through the fecal-oral route in all ages of ruminants. Additionally, transmission through milk orcolostrum or transplacentally is possible in neonates.5
-
•
Infection generally occurs at a young age; however, clinical signs are seen only in adult animals due to the long incubation period.
-
•
Clinical signs include watery diarrhea, submandibular edema due to hypoproteinemia, and weight loss in the face of a good appetite.6 Hypoproteinemia is secondary to chronic protein-losing enteropathy (due to maldigestion and malabsorption).
-
•
Diarrhea is an inconsistent sign in goats and sheep, which may only exhibit chronic weight loss.6
-
•
Fig. 1 depicts a 5-year-old mixed breed bull showing clinical signs of paratuberculosis, including thin body condition and profuse diarrhea.
Fig. 1.
A 5-year-old mixed breed bull showing clinical signs of paratuberculosis, including thin body condition and profuse diarrhea.
Clostridium perfringens type A
-
•
Although Clostridium infections occur more commonly in young ruminants, C perfringens type A has been associated with highly fatal hemolytic hemorrhagic enteritis in adult cattle and sheep and hemolytic enterotoxemia in goats.7
-
•
Clinical signs include acute onset of depression, dyspnea, pyrexia, diarrhea, pale or jaundiced mucous membranes, abdominal pain, and hemoglobinuria.
-
•
The disease is often fatal and animals are likely to die within 12 hours after onset of clinical signs.7
-
•
C perfringens type A has also been associated with jejunal hemorrhagic syndrome in adult dairy cattle.8
Viral Enteritis
Bovine viral diarrhea
-
•
Peracute diarrhea due BVD virus infection can occur in immunocompetent, nonpersistently infected adult ruminants.7
-
•
Morbidity rates of peracute BVD may reach up to 40% with mortality rates reported at 20%.7
-
•
Clinical signs associated with peracute BVD include severe diarrhea, pyrexia, thrombocytopenia, hemorrhagic disease, agalactia, and death.7
-
•
Reproductive disorders associated with peracute disease include decreased conception rates, abortion, stillbirth, congenital defects, and weak calves.7
Malignant catarrhal fever
-
•
In North America, sheep-associated malignant catarrhal fever caused by ovine herpes virus type 2 affects cattle and other wild ruminants. Sheep and goats are asymptomatic carriers.9
-
•
Wildebeest-associated malignant catarrhal fever, caused by alcelaphine herpes virus type 1, may occur outside Africa in zoologic establishments where domestic or wild ruminants are in contact with wildebeest.
-
•
Transmission from sheep to cattle is presumably through direct or indirect contact, aerosols, and nasal or ocular secretions from infected sheep.10
-
•
Clinical signs include diarrhea, oral and nasal erosions, corneal opacity, hyperemic coronary bands with lameness, hematuria, dermatitis, and encephalitis.11
-
•
The disease has a low morbidity but high mortality rates.
Winter dysentery
-
•
The etiologic agent of winter dysentery is BCoV.
-
•
Transmission is through fecal-oral route and outbreaks occur more commonly in adult lactating dairy cows in winter.12 Occurrence of disease in the herd may coincide with a rise in respiratory disease also caused by BCoV.
-
•
Outbreaks are associated with high morbidity (30%–50%) but low mortality (2%).7
-
•
Clinical signs associated with BCoV include acute onset of decreased appetite, decreased milk production, diarrhea, and pyrexia.7
-
•
Clinical signs of diarrhea are associated with virus-induced enterocolitis.7
-
•
A majority of cows recover within 24 hours to 36 hours after the onset of clinical signs.7
Parasitic Gastroenteritis
Nematodiasis
-
•
Nematodes in the genera Haemonchus, Trichostrongylus, Ostertagia, Cooperia, and Nematodirus cause gastroenteritis in ruminants.
-
•
The life cycle of the nematodes is direct and transmission is through ingestion of infective larval stages (third larval stage).
-
•
Although all young ruminants are more susceptible to nematodiasis compared with adult ruminants, adult goats do not build an effective immunity against trichostrongylid-type nematodes and are susceptible throughout their life span.7
-
•
Grazing adult goats are more susceptible to ingestion of high larval loads compared with browsing goats.7
-
•
Risk factors for occurrence of clinical nematodiasis include ingestion of high larval loads, overcrowding on pasture, wet weather, lush pastures, and low plane of nutrition.7
-
•
Clinical signs associated with nematodiasis in adult ruminants include diarrhea, weight loss, decreased production, pale mucous membranes (Haemonchus spp), submandibular edema, and death.
-
•
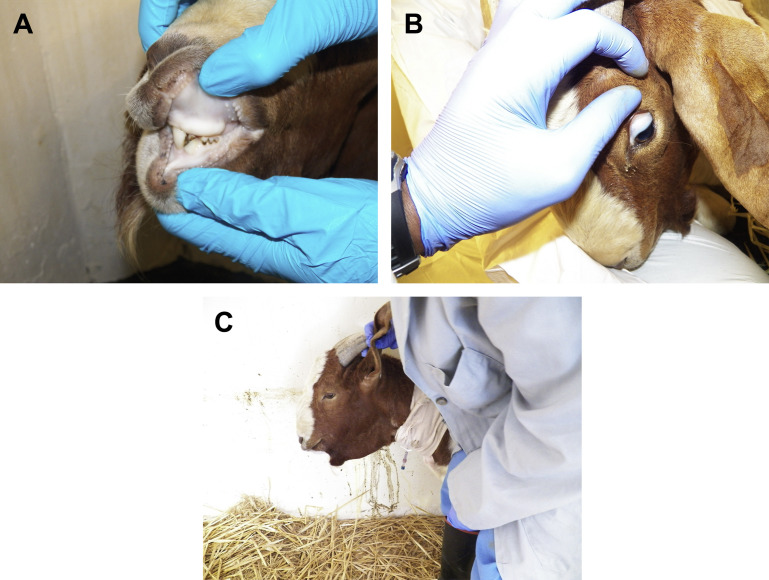
Fig. 2 depicts a Boer buck showing clinical signs of haemonchosis.
Fig. 2.
A Boer buck with haemonchosis. (A) Depicts pale oral mucous membranes. (B) Depicts pale ocular mucous membranes. (C) Depicts submandibular edema. Note the diarrhea stained wall.
Coccidiosis
-
•
Coccidial parasites of the genus Eimeria are important in ruminants. The life cycle of coccidia is direct, and infection occurs via ingestion of the infective oocysts.
-
•
Coccidiosis is commonly a disease of young, nonimmune ruminants.
-
•
Other risk factors for clinical coccidiosis other than young age include nutritional status of the animal, high stocking density, other concurrent diseases such as helminthiasis, and environmental or management stressors.
-
•
Coccidiosis is uncommon in adult sheep and cattle because of acquired immunity after infection13 but an important disease of adult goats.14
-
•
Additionally, outbreaks of coccidiosis have been reported in adult beef cattle.15
-
•
Clinical signs include inappetence and acute diarrhea, with foul-smelling feces containing blood and mucus.
-
•
Pale mucous membranes might be present depending on the degree of blood loss in the feces.
-
•
In cattle, muscle tremors, hyperesthesia, and seizures are associated with nervous coccidiosis.16
Noninfectious differential diagnoses for enteritis in adult ruminants
Differential diagnoses of noninfectious causes of diarrhea in adult ruminants include the following:
-
•
Copper deficiency
-
•
Lactic acidosis/grain overload
-
•
Renal amyloidosis
-
•
Liver and cardiac disease
-
•
Ragwort (Senecio jacobaea) poisoning
-
•
Arsenic poisoning
Diagnostics
Table 1 summarizes the specific samples and diagnostic tests for consideration in diagnosing causes of enteritis in adult ruminants. Ancillary diagnostic test may help differentiate causes of infectious enteritis and help with clinical management of ruminants while waiting for other specific test results. The following tests are performed in clinical practice without the need to send samples to a specialty laboratory.
Fecal Flotation
-
1.
Saturated solutions of sodium chloride, sugar (sucrose), or magnesium sulfate are inexpensive and easy to use.
-
2.
To make a saturated float solution, mix 400 g of sodium chloride, or 400 g of magnesium sulfate, with 1 L of warm tap water. For the sucrose solution, mix 454 g of granulated sugar with 355 mL of warm of tap water.17
-
3.
The saturated solution of sodium chloride, sugar, or magnesium sulfate is sufficient to float common helminths eggs and coccidia oocysts in ruminants.
-
4.
Mix 1 g of feces with 10 mL to 12 mL of the saturated float solution. Mixing of the fecal sample is easy in cases of diarrhea.
-
5.
Pour the mixture through a strainer or gauze into a 15-mL centrifuge tube. Add the float solution into the centrifuge tube so that the liquid is level with the top of the tube (forms a meniscus).
-
6.
Place a coverslip on top of the tube and centrifuge the tube at 1500 rpm for 5 minutes to 10 minutes. If the centrifuge does not have free-swinging buckets, the coverslip must be placed on the tube after centrifugation (otherwise it falls off during centrifugation). If a centrifuge is not available, the sample in step 5 is allowed to sit with coverslip in place for 30 minutes.
-
7.
Remove the coverslip and place on a glass slide and examine under the microscope at ×100 [magnification] (×10 ocular and ×10 objective).
-
8.
For qualitative assessments of microscopy of the coverslip, using routine slides is sufficient. For quantitative assessments, McMaster chambers are required.
-
9.
Other quantitative method techniques without the use of McMaster chambers have been described as follows: in step 4, mix 2 g of feces with 30 mL of the saturated sugar solution and follow through step 5. Follow step 6 but without placing the coverslip on top of the tube. Collect 0.15 mL of the centrifuged solution (solution making the meniscus), drop it on a routine slide, and place a coverslip. Count all the eggs under the coverslip at ×100, then multiply by 200. This represents the approximate number of eggs per gram in the sample.
Packed Cell Volume and Serum Total Protein
-
•
Determination of packed cell volume (PCV) and serum total protein (STP) assesses the levels of anemia and hypoproteinemia, respectively.
-
•
PCV and STP assessment is determined using a hematocrit centrifuge and refractometer, respectively.
-
•
Heamonchosis is consistently associated with severe anemia whereas salmonellosis, Clostridium, and coccidiosis might cause mild anemia due to blood loss in the feces.
-
•
Paratuberculosis may be associated with mild anemia due the chronicity of the disease.
-
•
Paratuberculosis, helminthiasis, and coccidiosis are consistently associated with hypoproteinemia.
Other Ancillary Diagnostics
Complete blood cell count and serum biochemical analysis
-
•
A complete blood cell count further classifies the anemia present (smear evaluation) and assesses inflammation (leukocytes with differential counts and fibrinogen).
-
•
Leukopenia characterized by neutropenia with a left shift and presence of cellular toxic changes might be present in salmonellosis due to endotoxemia and bacteremia.
-
•
Leukopenia and thrombocytopenia might be present with BVD virus infection.
-
•
Serum biochemical analysis assesses concentrations of albumin and globulin and identifies electrolyte derangements and evidence of organ insufficiency secondary to the infectious agent.
-
•
Portable serum biochemical analyzers may be useful in identifying electrolyte imbalances but may not be equipped to assess albumin, globulins, and enzyme activities.
Plasma pepsinogen levels
-
•
Acidic pH in the abomasum is required for conversion of pepsinogen to pepsin.
-
•
When parietal cells (responsible for abomasal acid production) are damaged secondary to abomasal parasites, conversion of pepsinogen to pepsin (active enzyme) is impaired and thus protein digestion is impaired.
-
•
Elevated plasma plasminogen levels are used to aid in diagnosis of ostertagiosis.7 Plasma pepsinogen levels are also elevated in haemonchosis.
-
•
Plasma pepsinogen level reference ranges differ among laboratories.
Treatment
Principles of Treatment of Infectious Enteritis in Adult Ruminants
Infectious enteritis causes diarrhea and associated fluid and electrolyte losses. Thus, fluid therapy is an important part of management of infectious enteritis. Maldigestion and malabsorption are the dominant underlying pathophysiologic mechanisms; hence, intravenous therapy is more effective (at least initially) at correcting the electrolyte imbalances and fluid loss compared with oral administration. Blood and protein loss should also be considered and treated accordingly. The following type of fluids should considered as part of the fluid therapy.
Crystalloids
-
•
Crystalloids include 0.9% sodium chloride, lactated Ringer solution, and other balanced crystalloid fluids, such as Plasma-Lyte.
-
•
The choice of the crystalloids may depend on the test results of serum biochemical analysis.
-
•
When serum biochemical analysis test results are not available, balanced electrolytes, such as Plasma-Lyte (Baxter Healthcare Corporation, Deerfield, IL), should be considered.
-
•
The level of dehydration at presentation and ongoing losses due to diarrhea must be considered when calculating fluid administration rates. Administration rates above maintenance must be considered. The patient’s STP status must also be considered; intravenous fluids should be administered with caution in patients with albumin levels less than 2 g/dL.
Colloids
-
•
Plasma transfusion or hetastarch should be considered in ruminants with submandibular edema on clinical examination or those that have severe hypoproteinemia (albumin levels <1.5 g/dL) on serum biochemical analysis.
-
•
Dosage rates for plasma and hetastarch administration range from 15 mL/kg to 20 mL/kg18 and 10 mL/kg to 20 mL/kg (based on equine doses),19 respectively.
-
•
Whole-blood transfusion (particularly in haemonchosis) should be considered when PCV is less than 12%.20
-
•
After plasma, hetastarch, or blood transfusion administration, fluid therapy may be continued with crystalloids.
Antimicrobial and Nonsteroidal Anti-Inflammatory Therapy
-
•
Diarrhea can predispose ruminants to secondary bacterial infections.
-
•
Prophylactic antibiotic therapy is usually considered. Broad-spectrum antibiotics, including tetracyclines, macrolides (nonlactating ruminants), and florfenicol (nonlactating animals), may be considered. Tetracyclines should be avoided in dehydrated patients if normal hydration and renal perfusion cannot be reestablished within several hours due to the risk of nephrotoxicity.
-
•
Use of nonsteroidal anti-inflammatory drugs (NSAIDs) (eg, flunixin meglumine) may be considered to control pyrexia and inflammation. NSAIDs are contraindicated, however, in dehydrated patients if normal hydration and renal perfusion cannot be reestablished within several hours due to the risk of nephrotoxicity.
Specific Treatments
Bacterial Pathogens
Salmonellosis
-
•
Use of antibiotics in salmonellosis is controversial due to concerns of their effectiveness and selection of antimicrobial resistance. This concern, however, is based on human studies where invasive salmonella infections are uncommon and antimicrobial therapy is not recommended.21
-
•
Successful treatment of bacteremia due to salmonellosis may rely on early administration of appropriate antibiotics, fluid and electrolyte therapy, and NSAID.3
-
•
Bacteremia is common in calves with salmonellosis; hence, antibiotics are recommended.21 Likewise, bacteremia might occur in adult ruminants.
-
•
Although the choice of antibiotics should be based on susceptibility of the isolate cultured and antibiotic sensitivity test, broad-spectrum antibiotics should be considered while awaiting test results. Susceptibility of Salmonella to tetracyclines, ampicillin, and amoxicillin is variable whereas resistance to penicillin, erythromycin, and tylosin is highly likely.3 Florfenicol may be considered for treatment of salmonellosis.3 Use of aminoglycosides is discouraged because they have prolonged tissue residues in ruminant animals intended for food. Sulfonamides, cephalosporins, and fluoroquinolones have extralabel restrictions in the United States.
-
•
Flunixin meglumine (1.1–2.2 mg/kg intravenously) was reported to improve outcome in calves with nonspecific diarrhea and should be considered in adult ruminants.22 The use of NSAIDs should be withheld in dehydrated ruminants until the patient is sufficiently hydrated.
-
•
Intravenous fluids, as previously described, are important as part of therapy in adult ruminants with salmonellosis.
Paratuberculosis
-
•
Treatment of paratuberculosis is uncommon in adult ruminants used for production.
-
•
In instances where the animal’s genetic or sentimental value is important to the client, treatment may be considered.
-
•
Most chemotherapeutic agents recommended for treatment of paratuberculosis are not labeled for use in ruminants. Thus, animals treated with these chemotherapeutic agents should not be used for milk or meat production or have greatly extended drug withdrawal times to ensure no detectable residues in meat or milk.
-
•
A majority of ruminants with clinical paratuberculosis maintain a good appetite until the terminal stages. Hence, intravenous fluids (crystalloids or colloids) may not be warranted until submandibular edema develops.
Clostridium perfringens type A
-
•
The disease has an acute onset and swift progression of clinical signs.
-
•
For therapy to be effective, it must be instituted immediately. Supportive intravenous fluid therapy and administration of antibiotics to halt the production of C perfringens toxins and decrease pathogen numbers in the intestinal tract are the cornerstones of successful treatment.
-
•
In cases of hemorrhagic bowel syndrome, laparotomy with manual massage to break down obstructing blood clots or removal by enterotomy may be necessary to clear intraluminal blood clots and restore intestinal function.
Viral Pathogens
-
•
There is no specific treatment of viral pathogens causing enteritis in adult ruminants.
-
•
Supportive treatment, including intravenous fluids, NSAIDs, and prophylactic antibiotics, should be considered, as indicated previously (principles of treatment of infectious enteritis in adult ruminants).
Parasitic pathogens
Helminths and coccidiosis
-
•
Intravenous fluids (at least twice maintenance) is recommended in parasitic gastroenteritis to correct dehydration and ongoing losses.
-
•
In cases of submandibular edema present, plasma (15–20 mL/kg)18 or hetastarch (10–20 mL/kg) is recommended.19
-
•
When severe anemia is present (PCV <12%), whole-blood transfusion is warranted.
-
•
To control pain associated with the diarrhea, NSAIDs may administered (flunixin meglumine at 1.1–2.2 mg/kg) once the patient is hydrated.
-
•
Administration of antibiotics to treat helminthiasis and coccidiosis may not be necessary but should be considered based on other concurrent diseases or evidence of systemic sepsis.
-
•
Specific anthelmintic and anticoccidiosis therapeutic agents are summarized in Tables 2 and 3 , respectively.13, 23
-
•
The choice of the anthelmintic may depend on the withdrawal time for meat and milk, safety of the drug, spectrum of activity, ease of administration, cost, and evidence of anthelmintic resistance.
-
•
A detailed review of helminthiasis can be seen in Thomas M. Craig's article, “Gastrointestinal Nematodes, Diagnosis and Control,” in this issue; and coccidiosis is reviewed in detail in Sarah Tammy Nicole Keeton and Christine B. Navarre’s article “Coccidiosis in Large and Small Ruminants,” in this issue .
Table 2.
Summary of commonly used anthelmintics for management of helminthiasis in cattle, sheep, and goats
| Drug | Species | Dose and Route |
|---|---|---|
| Ivermectin | Cattle | 0.2 mg/kg SC or po 0.5 mg/kg topical |
| Sheep | 0.2 mg/kg SC or po | |
| Goats | 0.2 mg/kg SC or po 0.5 mg/kg topical |
|
| Doramectin | Cattle (beef) | 0.2 mg/kg SC or IM 0.5 mg/kg topical |
| Moxidectin | Cattle | 0.2 mg/kg po or SC 0.5 mg/kg topical |
| Goats | 0.2 mg/kg po or SC 0.5 mg/kg topical |
|
| Sheep | 0.2 mg/kg po or SC | |
| Eprinomectin | Cattle | 0.5 mg/kg topical |
| Albendazole | Cattle and goats | 10 mg/kg po |
| Sheep | 7.5 mg/kg po | |
| Fenbendazole | Cattle, goats, and sheep | 5 mg/kg po |
| Levamisole | Cattle and sheep | 7.5 mg/kg po |
| Goats | 12 mg/kg po |
Abbreviations: IM, intramuscularly; SC, subcutaneously.
Data from Baynes RE, Payne M, Martin-Jimenez T, et al. Extralable use of ivermectin and moxidectin. J Am Vet Med Assoc 2000;217:668–71.
Table 3.
Summary for drugs used to treat coccidiosis in cattle, goats, and sheep
| Drug | Species | Dose and Route |
|---|---|---|
| Amprolium | Cattle | 10 mg/kg po for 5 d |
| Goats and sheep | 20–40 mg/kg po for 5 d or 65 mg/kg po once | |
| Monensin | Sheep | 2 mg/kg po for 20 d |
| Sulfadimethoxine | Cattle, goats, and sheep | 55 mg/kg po on day 1 followed by 27.5 mg/kg on days 2–5 |
| Sulfamethazine | Cattle |
|
Extralabel use of sulfonamides in dairy cattle greater than 20 mo of age is prohibited in the United States.
Data from Ballweber LR. Coccidiosis in food animals. In: Smith BP, editor. Large animal internal medicine. 5th edition. St Louis (MO): Elsevier Mosby; 2015. p. 1516–7.
Summary
Causes of infectious enteritis in adult ruminants are bacterial, viral, and parasitic. The most consistent clinical sign of infectious enteritis is diarrhea. Specific etiologies causing infectious enteritis in adult ruminants cannot be distinguished easily based on clinical examination alone. Laboratory diagnostic tests are required to differentiate the etiologies. A majority of the etiologies have herd implications; thus, identification of the etiology is recommended. Management of infectious enteritis in adult ruminants includes administration of intravenous fluids, such as crystalloids and colloids; NSAID; antibiotics; anthelmintics; and coccidiostats.
Footnotes
Disclosure Statement: The authors have nothing to disclose.
References
- 1.Salmonellosis. The Center For Food Security and Public Health. Institute for International Cooperation in Animal Biologics. Iowa State University. 2005-2013. Available: http://www.cfsph.iastate.edu/Factsheets/pdfs/nontyphoidal_salmonellosis.pdf. Accessed June 23, 2017.
- 2.Gibson E.A. Salmonella infection in cattle. J Dairy Res. 1965;32:97–134. [Google Scholar]
- 3.Smith B.P. Salmonellosis in ruminants. In: Smith B.P., editor. Large animal internal medicine. 5th edition. Elsevier Mosby; St Louis (MO): 2015. pp. 830–834. [Google Scholar]
- 4.Cobbold R.N., Rice D.H., Davis M.A. Long-term persistence of multi-drug-resistant Salmonella enterica serovar Newport in two dairy herds. J Am Vet Med Assoc. 2006;288:588–591. doi: 10.2460/javma.228.4.585. [DOI] [PubMed] [Google Scholar]
- 5.Seitz S.E., Heider L.E., Heuston W.D. Bovine fetal infection with mycobacterium paratuberculosis. J Am Vet Med Assoc. 1989;194:1423–1426. [PubMed] [Google Scholar]
- 6.Sweeney R.W. Paratuberculosis (Johne’s disease) In: Smith B.P., editor. Large animal internal medicine. 5th edition. Elsevier Mosby; St Louis (MO): 2015. pp. 834–837. [Google Scholar]
- 7.Constable P.D., Hinchcliff K.W., Done S.H. Veterinary medicine: a textbook of the diseases of cattle, horses, sheep, pigs, and goats. 11th edition. Elsevier; St Louis (MO): 2017. Diseases of the alimentary tract; pp. 436–621. [Google Scholar]
- 8.Elhanafy M.M., French D.D., Braun U. Understanding jejunal hemorrhage syndrome. J Am Vet Med Assoc. 2013;243:352–358. doi: 10.2460/javma.243.3.352. [DOI] [PubMed] [Google Scholar]
- 9.Metzler A.E. The malignant catarrhal fever complex. Comp Immunol Microbiol Infect Dis. 1991;14:107–124. doi: 10.1016/0147-9571(91)90125-w. [DOI] [PubMed] [Google Scholar]
- 10.Taus N.S., Oaks J.L., Gailbreath K. Experimental aerosol infection of cattle (Bos taurus) with ovine herpesvirus 2 using nasal secretions from infected sheep. Vet Microbiol. 2006;116:29–36. doi: 10.1016/j.vetmic.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 11.Callan R.J. Malignant catarrhal fever. In: Smith B.P., editor. Large animal internal medicine. 5th edition. Elsevier Mosby; St Louis (MO): 2015. pp. 759–762. [Google Scholar]
- 12.Boileau M.J., Kapil S. Bovine coronavirus associated syndromes. Vet Clin North Am Food Anim Pract. 2010;26:123–146. doi: 10.1016/j.cvfa.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ballweber L.R. Coccidiosis in food animals. In: Smith B.P., editor. Large animal internal medicine. 5th edition. Elsevier Mosby; St Louis (MO): 2015. pp. 1516–1517. [Google Scholar]
- 14.Chhabra R.C., Pandy V.S. Coccidia of goats in Zimbabwe. Vet Parasitol. 1991;39:199–205. doi: 10.1016/0304-4017(91)90036-u. [DOI] [PubMed] [Google Scholar]
- 15.Reddy B.S., Sivajothi S., Rayulu V.C. Clinical coccidiosis in adult cattle. J Parasit Dis. 2015;39:557–559. doi: 10.1007/s12639-013-0395-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jolley W.R., Bardsley K.D. Ruminant coccidiois. Vet Clin North Am Food Anim Pract. 2006;22:613–621. doi: 10.1016/j.cvfa.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Foreyt W.J. 5th edition. Iowa State University Press; Ames (IO): 1997. Veterinary parasitology reference manual; pp. 3–10. [Google Scholar]
- 18.Barrington G.M., Parish S.M. Ruminant immunodeficiency diseases. In: Smith B.P., editor. Large animal internal medicine. 3rd edition. Mosby; St Louis (MO): 2002. pp. 1600–1602. [Google Scholar]
- 19.Radostits O.M., Gay C.C., Hinchcliff K.W. Veterinary medicine: a textbook of the diseases of cattle, horses, sheep, pigs, and goats. 10th edition. Elsevier; St Louis (MO): 2007. Drug doses and intervals for horses and ruminants; p. 2057. [Google Scholar]
- 20.Balcomb C.B., Foster D. Update on the use of blood products in ruminants. Vet Clin North Am Food Anim Pract. 2014;30:455–474. doi: 10.1016/j.cvfa.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 21.Mohler V.L., Izzo M.M., House J.K. Salmonella in calves. Vet Clin North Am Food Anim Pract. 2009;25:47–54. doi: 10.1016/j.cvfa.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 22.Barnett S.C., Sischo W.M., Moore D.A. Evaluation of flunixin meglumine as an adjunct treatment for diarrhea in dairy calves. J Am Vet Med Assoc. 2003;223:1329–1333. doi: 10.2460/javma.2003.223.1329. [DOI] [PubMed] [Google Scholar]
- 23.Baynes R.E., Payne M., Martin-Jimenez T. Extralable use of ivermectin and moxidectin. J Am Vet Med Assoc. 2000;217:668–671. doi: 10.2460/javma.2000.217.668. [DOI] [PubMed] [Google Scholar]