Abstract
Background
In Hong Kong Emergency Departments (EDs), the timeliness of providing high-quality services has been compromised by the increasing attendance of non-emergent patients in addition to the unpredictable arrival of emergency patients.
Objectives
We sought to quantify the impact of the presence of emergent patients and other related factors on the delay in service for non-emergent patients.
Methods
We conducted a retrospective study in patients who visited the ED of a large hospital in Hong Kong from July 1, 2009 to June 30, 2010. We estimated waiting and length of stay (LOS) for individual non-emergent patients registered during day and evening shifts. Using multiple linear regression, we estimated waiting time and LOS as a function of the presence of emergent patients and other related factors such as patient demographics and clinical factors. In particular, we evaluated the influence of the arrival or presence of emergent patients on the odds of violating the 120-min waiting time target for semi-urgent patients.
Results
The arrival of a new emergent patient prolonged the waiting time and LOS of a non-emergent patient by 14.9% (95% confidence interval [CI] 14.2–15.5) and 10.8% (95% CI 10.6–11.0), respectively. An additional patient-hour needed for an emergent patient increased the probability of violating the waiting time target for non-emergent patients (odds ratio 2.3, 95% CI 2.2–2.4).
Conclusions
The arrival of an emergent patient significantly prolonged the waiting time and LOS for non-emergent patients. Discouraging non-urgent ED utilization and building a real-time decision-support system are critical methods needed to relieve staff pressure and guide contingent resource reallocation when emergent patients arrive.
Keywords: Emergency Department, overcrowding, length of stay, waiting times, non-emergent patients, emergent patients
Introduction
Waiting time and length of stay (LOS) are two measures commonly used to evaluate the quality of emergency services. A substantial amount of research has been dedicated to identifying factors that contribute to patient LOS in Emergency Departments (EDs) 1, 2, 3, 4, 5, 6, 7, 8, 9, 10. Apart from the patient demographics (e.g., age, sex, race, mode of arrival, insurance status) and clinical factors (e.g., chief complaint, triage category), LOS is highly dependent on factors that are either at the ED or hospital level 1, 2, 3, 4, 5, 6, 7, 8, 9, 10. The former includes disposition status, patient census, and bed occupancy rate, whereas the latter includes hospital census and inpatient bed occupancy rate 3, 4, 6, 7, 8, 9, 10. Similarly, waiting times are another key indicator of ED performance, and prolonged waiting times can increase the risk of health deterioration 1, 6, 11, 12. Although there have been a few studies regarding the effect of non-urgent patients on crowding in the ED, little is known about how emergent patients affect crowding and the consequent service delay to the majority of non-emergent patients in the ED (12).
This is particularly pertinent in the era of increased performance measurement (and potentially reimbursement) of emergency-specific quality metrics globally (such as in the United States (US), the United Kingdom, and parts of Australia, New Zealand, and Canada) and locally in Hong Kong. In Hong Kong, the Hospital Authority has set waiting time targets for patients since 1999, and thus has created intense pressure on health systems to meet these targets (13).
The rise in waiting times and LOS in EDs has become an increasingly serious problem in developed nations (14). Hong Kong, with its aging population, complex case mix, and decreasing ED personnel is no exception, and arguably provides a setting for more intensified crowding than other countries (15). Given the lack of access to primary care within the system, many patients with non-emergent conditions in Hong Kong present to the EDs, known as Accident & Emergency Departments (A&Es) (16). In Hong Kong, at the current time, the A&Es function similarly to a combination of primary and urgent care, to handle the increased number of non-emergent patients.
Similar to the Emergency Severity Index (ESI), the Hong Kong triage system divides patients into five categories (Table 1 ) according to the nature and severity of their medical conditions (15). Category I is considered critical; Category II emergency; Category III urgent; Category IV semi-urgent; and Category V non-urgent. Essentially, Categories I and II are considered emergent and Categories III–V non-emergent. A&Es are mandated to comply with waiting times determined by the Hospital Authority, which are determined separately for different categories. In Hong Kong’s system, most emergent patients are immediately placed in the resuscitation room upon arrival and undergo continuous close monitoring. The emergent patients account for <4% of total ED patients, much less than in the US. In the study A&E, the percentage of critical, emergency, and urgent patients first seen by a medical officer within the recommended time were 100%, 96.8%, and 91.2%, respectively. However, only 67% of semi-urgent patients were seen within 120 min, in contrast to the 75% recommendation (the waiting time target for semi-urgent patients is unofficial and the result is currently for internal assessment only). There is no target set for non-urgent patients, as they are discouraged from attending A&Es.
Table 1.
Triage System in Hong Kong Accident and Emergency Departments
| Triage Category | Patient Conditions | Actions of Staff Target | Response Time |
|---|---|---|---|
| 1 (Critical) | |||
|
|
|
|
| 2 (Emergency) | |||
|
|
|
|
| 3 (Urgent) | |||
|
|
|
|
| 4 (Semi-urgent) | |||
|
|
||
| 5 (Non-urgent) | |||
|
|
A typical A&E in Hong Kong is divided into resuscitation rooms where critical and emergency patients are managed, cubicles for patients on gurneys who are mostly urgent, and walk-in clinics where semi-urgent and non-urgent patients are consulted. Non-urgent patients are normally seen 30 min later than semi-urgent patients. There is a fast-track stream for semi-urgent patients with minor injury between 7:00 a.m. and 5:00 p.m. through which they can jump in front of other semi-urgent patients who have arrived earlier. Emergent patients are managed by a resuscitation team consisting of one to two medical officers and two to three nurses. All non-emergent patients are consulted by one medical officer, including non-urgent patients who only need brief check-ups.
Although emergent patients comprise a small proportion of the total number of ED visits in Hong Kong, they nevertheless are one of the main factors that contribute to increased waiting time and LOS for non-urgent patients. Given the current targets placed upon EDs, there is a vital need to quantitatively evaluate the potential impact of the emergent patients to increase understanding of these processes.
The purpose of this study is to assess the impact of emergent patients’ arrival on the service targets of the non-emergent patients measured by the waiting time and LOS. This study was conducted as part of an attempt to determine the contributing factors to long waiting time and LOS in Hong Kong A&Es, and to build an A&E simulation model that incorporates improvements in the existing operations 17, 18.
Methods
Study Design and Setting
This was a retrospective cross-sectional study based on 12 months of electronic patient data from a general hospital’s A&E in Hong Kong. Our A&E provides 24 h per day/7 days per week emergency care and a wide range of specialist and ambulatory services to the residents of Kowloon West district and New Territory. The daily census ranges from 350 to 420, with an annual census of more than 140,030. Approximately 30% of A&E patients are brought by ambulances, with the remaining patients arriving as walk-ins. The full A&E staff in the day and evening shifts includes five medical officers (who are the equivalent of mds in the US) and 11 nurses at any one time, whereas staffing is reduced to two medical officers and four nurses on overnight shifts. In other words, there are 96 h of md coverage per day. The number of patients per hour (average 4.04) is almost twice that of other developed countries, which reflects the excessive burden of non-emergent patients who seek care in our system.
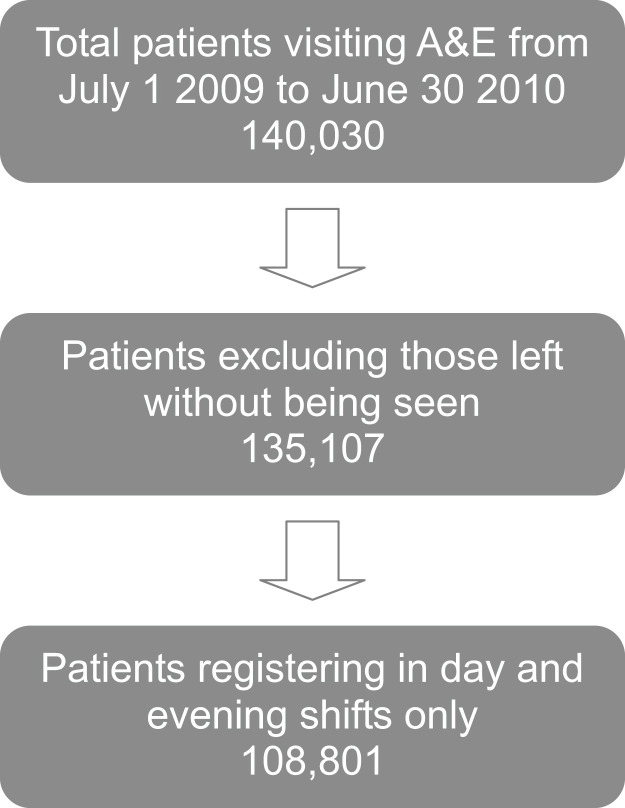
We studied all patients who were registered during day and evening shifts for 12 months, from July 1, 2009 to June 30, 2010. Some patients left the A&E before their first consultation or while waiting for test results, due to the long waiting time. Patients who left prematurely (3.5% of the total patients) were omitted from the study because their times at first consultation or discharge were not recorded. Because the patient flow and staffing levels are different on night shifts (11:00 p.m. to 7:00 a.m.), we omitted patients arriving during those hours to obtain data that would represent the best possible scenario of fully staffed periods. The data selection criteria are summarized in Figure 1 . This study was approved by the A&E management, and verbal informed consent was obtained from providers.
Figure 1.
Study criteria for data selection. A&E = Accident & Emergency Departments.
Data Collection and Processing
Patient information was recorded on an A&E card issued to each patient on arrival at the registration counter, containing a personal barcode. These barcodes are scanned by either medical officers or nurses at four operational points of registration: start of triage, start of first consultation by a medical officer, disposition, and time entering the observation room (for those sent there). We did not record the time of physical departure of admitted patients. For these patients, we addressed the discrepancy between time of disposition and physical departure from the A&E by adding a boarding time (15 min during the 7:00 a.m. to 10:00 a.m. shift and the 7:00 p.m. to 11:00 p.m. shift, and 30 min between the two shifts). For discharged patients, the disposition time was assumed to be the same as the time of physical departure from the A&E.
These time-stamped data were stored in the Hong Kong-wide Accident and Emergency Information System together with other patient information, including patient attributes (e.g., age, sex, mode of arrival) and clinical factors (e.g., triage category, disposition status). The original data were exported to Excel worksheets, screened and manipulated in Excel VBA (Microsoft Corporation, Redmond, WA, 2003).
Outcome Measures
There were three outcome variables identified for the purpose of this study: log-transformed waiting times and LOS for individual non-emergent patients, and the odds of violation of the 120-min waiting time target for semi-urgent patients. We transformed the individual waiting times and LOS to a logarithmic scale due to the positive skew of the data, confirmed by the Shapiro-Wilk test (p < 0.001) 19, 20. We chose to focus on the waiting times of semi-urgent patients because they represent a significant proportion of our visits (n = 63,639, or 49.2% of all A&E visits), and the hospital experienced difficulty in complying with the mandated targets.
Measurements
The waiting time for emergent patients was defined as the interval between registration and first consultation with a medical officer, or start of resuscitation. Those who survived were transferred to the intensive care unit or operating room once stabilized, and their LOS was defined as between registration and physical departure from the A&E. The majority of the deaths were out-of-hospital cardiac arrest, and death was usually declared within a few minutes of arrival. This significantly shortened the LOS for the emergent patients.
For non-emergent patients, the waiting time was similarly defined as the time from registration to first consultation, and the LOS from registration to physical departure from the A&E. For patients in observation, because there were two dedicated nurses in the observation unit who did not manage other patients in the A&E, LOS for these patients was counted only between registration and time of entering the observation room. Other terms and concepts that appear in the Results section are as follows:
-
•
Four time points segmented the entire process of A&E care for a non-emergent patient into three phases, which we referred to in a sequence as “waiting for triage,” “waiting for consultation,” and “in treatment.”
-
•
The crowding level upon arrival of each patient was measured by patient volumes of Category III–V patients in the three phases of A&E care.
-
•
The effect of emergency patients was measured as the total number of emergency patients in resuscitation and arriving during a non-emergent patient’s wait for consultation or LOS, depending on the outcome variables.
Data Analysis
The analysis was started by calculating the median waiting time and LOS of the selected patients stratified by the categorical variables of age, gender, mode of arrival, disposition, and triage level (Figure 1). For each variable, the median values were compared between categories using a non-parametric test (Wilcoxon rank-sum test), knowing that the values of waiting time and LOS were positively skewed. Second, we calculated the median waiting time and LOS, and performed basic descriptive analysis of patient characteristics. Third, we used multiple linear regression to estimate the average waiting time and LOS of individual non-emergency patients to reflect levels of crowding with patient volume upon arrivals. Finally, we assessed the specific associations between the violation of the 120-min waiting time target of semi-urgent patients and the explanatory variables using logistic regression. Odds ratios (ORs) were used to represent the strength of the associations. We adopted the same explanatory variables as in the first analysis. Based on the model, we determined the discriminatory power of forecasting violation cases from the area under the receiver operating characteristic curve (ROC [AUC]), where a value of 1.0 represents perfect discrimination and a value of 0.5 represents no discrimination. We evaluated the goodness-of-fit using the Hosmer-Lemeshow test. All the analyses were conducted in R, version 2.11.0 (available at http://www.r-project.org/).
Results
We analyzed 108,801 patient visits. Table 2 provides the descriptive characteristics of the study sample, as well as a summary of the median waiting time and LOS. The median waiting time and LOS for all patients was 34 min and 112 min, respectively. In general, patients over 65 years old, brought in by ambulance, and admitted, experienced shorter waiting time and LOS than their complementary counterparts. There was no significant variation between genders.
Table 2.
Summary of Median Waiting Time and LOS (Minutes) for Different Patient Groups
| Patient Groups | n = 108,801 | % | Median Waiting Time (IQR) | Wilcoxon Rank-Sum Test | Median LOS (IQR) | Wilcoxon Rank-Sum Test |
|---|---|---|---|---|---|---|
| Age, years | ||||||
| ≤65 | 79,642 | 73.2 | 49 (18–112) | <0.001 | 123 (76–190) | <0.001 |
| >65 | 29,159 | 26.8 | 18 (10–41) | Ref | 104 (74–163) | Ref |
| Sex | ||||||
| Female | 54,074 | 49.7 | 34 (14–100) | <0.522 | 117 (75–182) | <0.301 |
| Male | 54,727 | 50.3 | 33 (14–98) | Ref | 118 (75–185) | Ref |
| Mode of arrival | ||||||
| Walk-in | 76,161 | 70.0 | 53 (21–116) | <0.001 | 124 (78–191) | <0.001 |
| Ambulance | 32,640 | 30.0 | 16 (9–34) | Ref | 104 (71–163) | Ref |
| Disposition | ||||||
| Discharged | 72,244 | 66.4 | 65 (24–125) | <0.001 | 137 (85–204) | <0.001 |
| Admitted | 36,557 | 33.6 | 15 (9–27) | Ref | 91 (66–131) | Ref |
| Triage category | ||||||
| I | 1,632 | 1.5 | 0 (0–0) | <0.001 | 30 (23–41) | <0.001 |
| II | 2,720 | 2.5 | 6 (2–10) | <0.001 | 45 (33–63) | <0.001 |
| III | 42,324 | 38.9 | 15 (10–24) | Ref | 95 (68–139) | Ref |
| IV | 53,639 | 49.3 | 83 (42–138) | <0.001 | 147 (93–215) | <0.001 |
| V | 8,486 | 7.8 | 112 (70–165) | <0.001 | 137 (92–199) | <0.001 |
LOS = length of stay; IQR = interquartile range.
Table 3 displays the contribution of patient demographics, clinical factors, crowding factors, and emergent patients on the waiting times of non-emergent patients. Patients who had lower acuity had higher waiting times, and patients who arrived by ambulance and were admitted had significantly lower waiting times, as most of those patients were triaged to Category I–III. The more important finding shown in this table is that emergent patients prolonged a non-emergent patient’s waiting time by 14.9% (95% confidence interval [CI] 14.2–15.5).
Table 3.
Summary of Multiple Linear Regression Model Estimating Log-transformed Waiting Time for Individual Non-emergency (Category III–V) Patients
| Explanatory Variable | Percent Change in Waiting Time on Non-emergent Patients |
|
|---|---|---|
| Percent Change (95% CI) | p-Value | |
| Age, years | ||
| ≤65 | Reference | |
| >65 | 0.1 (−0.9–1.2) | 0.810 |
| Mode of arrival | ||
| Walk-in | Reference | |
| Ambulance | −13.2 (−13.9 to −12.2) | <0.001 |
| Disposition status | ||
| Discharged | Reference | |
| Admitted | −5.3 (−6.4 to −4.2) | <0.001 |
| Triage category | ||
| III | Ref | |
| IV | 374.5 (369.4–379.7) | <0.001 |
| V | 529.5 (518.4–540.8) | <0.001 |
| Crowding factor | ||
| Number of all non-emergent patients waiting for triage | 4.6 (4.4–4.8) | <0.001 |
| Number of Category III patients waiting for consultation | 8.2 (7.9–8.4) | <0.001 |
| Number of Category IV patients waiting for consultation | 2.7 (2.6–2.7) | <0.001 |
| Number of Category V patients waiting for consultation | 0.9 (0.8–1.1) | <0.001 |
| Number of Category III patients in treatment | 1.0 (0.9–1.1) | <0.001 |
| Number of Category IV patients in treatment | 0.6 (0.6–0.7) | <0.001 |
| Number of Category V patients in treatment | −2.3 (−2.7 to −1.9) | <0.001 |
| Number of emergent patients | 14.9 (14.2–15.5) | <0.001 |
CI = confidence interval.
Table 4 presents the results of the multiple linear regression model estimating LOS. Longer LOS were found among elderly patients because they usually underwent further observation after testing and treatment. Patients brought in by ambulance and those admitted had a shorter LOS. This model also shows that emergent patients prolonged a non-emergency patient’s LOS by 10.8% (95% CI 10.6–11.0). In other words, given that the median LOS for non-emergent patients was 118 min and the average number of emergent patients arriving during their visit was 1.4, this would increase the waiting time to 16.8 min. Overall, the volume of the earlier arrived patients in different phases of care prolonged a newly arrived patient’s LOS except for the negative impact imposed by non-urgent patients in treatment (−0.6, 95% CI −0.9 to −0.2). The patient attributes were significantly associated with the LOS. For example, patients in higher categories stayed longer in the A&E, whereas those brought by ambulance and finally being admitted stayed shorter because most of them suffered from major conditions that require less waiting before the first consultation.
Table 4.
Summary of Multiple Linear Regression Model Estimating Log-transformed LOS of Individual Non-emergency (Category III–V) Patients
| Explanatory Variable | Percent Change in Waiting Time on Non-emergent Patients |
|
|---|---|---|
| Percent Change (95% CI) | p-Value | |
| Age, years | ||
| ≤65 | Reference | |
| >65 | 10.4 (9.5–11.4) | <0.001 |
| Mode of arrival | ||
| Walk-in | Reference | |
| Ambulance | −11.0 (−11.8 to −10.3) | <0.001 |
| Disposition status | ||
| Discharged | Reference | |
| Admitted | −21.8 (−22.6 to −20.9) | <0.001 |
| Triage category | ||
| III | Ref | |
| IV | 50.6 (49.2–52.0) | <0.001 |
| V | 45.3 (43.2–47.7) | <0.001 |
| Crowding factor | ||
| Number of all non-emergent patients waiting for triage | 2.0 (1.8–2.1) | <0.001 |
| Number of Category III patients waiting for consultation | 2.8 (2.6–3.0) | <0.001 |
| Number of Category IV patients waiting for consultation | 1.5 (1.5–1.6) | <0.001 |
| Number of Category V patients waiting for consultation | 0.8 (0.7–1.0) | <0.001 |
| Number of Category III patients in treatment | 0.8 (0.7–0.9) | <0.001 |
| Number of Category IV patients in treatment | 0.2 (0.1–0.3) | 0.001 |
| Number of Category V patients in treatment | −0.6 (−0.9 to −0.2) | <0.001 |
| Number of emergent patients | 10.8 (10.6–11.0) | |
LOS = length of stay; CI = confidence interval.
Table 5 displays the results of the secondary aim of this study, to determine if emergent patients increase the probability of violating the 120-min waiting time target for semi-urgent patients. The logistic regression model shows that the presence of each additional emergent patient predicted a higher likelihood of violation of the mandate (OR 2.31, 95% CI 2.18–2.45). The subsequent ROC curve demonstrated good discriminative power of a 0.889 (95% CI 0.880–0.898) AUC value, and the Hosmer-Lemeshow goodness-of-fit test provided no evidence of rejecting the model (p > 0.05).
Table 5.
Summary of Logistic Regression Model Estimating the Odds of Violation of Waiting Time KPI (Target) of Category IV Patients
| Explanatory Variable | Waiting Time KPI of Category IV Patient (120-Min Maximum) |
||
|---|---|---|---|
| Odds Ratio | 95% CI | p-Value | |
| >65 years | 1.09 | (1.02–1.16) | 0.015 |
| Ambulance | 0.93 | (0.87–1.00) | 0.047 |
| Admitted | 0.90 | (0.84–0.99) | 0.026 |
| Number of all patients waiting for triage | 1.02 | (1.01–1.03) | <0.001 |
| Number of Category III patients waiting for consultation | 1.09 | (1.07–1.10) | <0.001 |
| Number of Category IV patients waiting for consultation | 1.19 | (1.19–1.20) | <0.001 |
| Number of Category V patients waiting for consultation | 1.03 | (1.03–1.04) | <0.001 |
| Number of Category III patients in treatment | 1.05 | (1.05–1.06) | <0.001 |
| Number of Category IV patients in treatment | 0.99 | (0.99–1.00) | 0.001 |
| Number of Category V patients in treatment | 0.97 | (0.94–0.99) | 0.011 |
| Number of emergent patients | 2.31 | (2.18–2.45) | <0.001 |
KPI =key performance indicator; CI = confidence interval.
Discussion
This study provides evidence to substantiate the hypothesis that the arrival or presence of emergent patients significantly prolongs waiting time and LOS of non-emergent patients, both individually and collectively. In addition, the results demonstrate moderate predictive ability of the imminent violation of the 120-min waiting time target for semi-urgent patients. There is high face validity for our results, including the finding that non-urgent patients who could potentially seek primary care in outpatient clinics only underwent brief check-ups in the A&E (most of them only came in the early mornings to collect sick notes). A greater proportion of non-urgent patient visits could therefore expedite the entire A&E process, as reflected by the negative impact in Tables 3 and 4.
The overflow of non-emergent patients engenders the question of how to adequately provide timely care that meets governmental mandates (instituted for the purposes of measuring and improving quality) in A&E service in the context of limited ability to provide adequate service in alternative settings 16, 21, 22. Although the existing triage categories hardly discriminate the true A&E cases from others that could be managed by primary care facilities, two local studies have found that as much as 57% of the total A&E cases could actually be handled by general practitioners 21, 23. In fact, our semi-urgent and non-urgent patients are the group most vulnerable to the arrival of emergency patients when staff are reallocated to secure the service targets of urgent patients first. Although there are many reasons for patient preferences to seek care in the A&E rather than general outpatient clinics (e.g., a perception of more “professional” service in A&Es, insufficient primary care services, long appointment time for specialist services), there is a push to improve quality by the provision of timely care (16). Although many other countries may not yet experience this pressure as intensely as Hong Kong, it is not implausible to consider that, given major shifts in health care reform, similar situations will arise in many other parts of the world where Emergency Medicine has rapidly developed.
This research opens up a wide discussion of health care service improvement in Hong Kong and, potentially, elsewhere. Although non-emergency A&E visits have slightly decreased in recent years due to situational factors such as the deterrent of severe acute respiratory syndrome and policy-related factors such as the implementation of emergency fees, this trend has been offset by dwindling A&E personnel and more complexity of the case-mix 15, 24, 25, 26. Several immediate measures, such as relinquishing treatment of the semi- and non-urgent patients to nurses and opening parallel ambulatory clinics next to A&Es, could be more widely adopted 20, 27. Although there are no laws that forbid turning away patients or diverting ambulances to other A&Es, morality and ethical concerns preclude such measures as policy 12, 28. However, the Hong Kong government is considering an expansion of public and private primary care services, such as 24/7 and Sunday/Holiday clinics, and also extending primary care services in private clinics. At the same time, the government may enhance public health education through mass media and communities to prevent inappropriate A&E visits. Nevertheless, even widespread adoption of these measures would be insufficient to address the level of crowding in Hong Kong A&Es, and if hospitals are required to comply with governmental mandates regarding waiting time and LOS targets for patient care, additional nurses and medical officers in walk-in clinics would be crucial to buffer the burden of resuscitating emergent patients. The optimal staffing level in an A&E relies on the calculation of time-varying patient demands and the A&E capacity. Previous papers have studied the application of the time-series method, queuing theory, and discrete event simulation to determine the optimal staffing level 29, 30, 31. These advances in application of such methods for streamlining A&E processes of care could be applied in many systems and countries.
Limitations
There are several limitations to this study. First, the study was conducted in a single hospital in Hong Kong, which has its own set of demographic and system-level factors related to input, throughput, and output of the A&E. As mentioned previously, in Hong Kong, A&Es in general function similarly to a combination of primary and urgent care centers, along with emergency, due to the need for health care services by an enormous population. Therefore, the results of this study may not be easily generalized to other regions’ A&E settings (32).
Second, although the triage system used in our study is based on a five-point scale similar to many other countries, ours is not precisely the ESI, and therefore does not capture triage patterns for each point of the scale in the same way as when the ESI system was adopted 32, 33, 34, 35. Specifically, in those studies done with ESI, there was a higher proportion of Category II cases (over 28%) and a lower proportion of Category IV cases (below 30%), whereas the corresponding figures are 4.0% and 49.3%, respectively, in this study. The very few Category II cases reflects the fundamental difference in triage systems, that is, that Hong Kong’s system has rigorously defined Category II patients, many of whom would be placed in Category I in many other systems. On the other hand, we suspect the disproportionately large number of Category IV patients was partly due to our A&E staff’s reluctance to triage patients to Category III, in which the recommended waiting time is much shorter. This disparity between the numbers of emergency and non-emergency patients has also been identified in other local studies 16, 24, 31. At the same time, we believe that our main finding, that sicker patients of higher acuity significantly impact our ability to deliver care in a timely fashion to the lower acuity patients, is applicable in many other contexts.
Finally, some factors believed to be associated with waiting time and LOS could not be controlled in this retrospective study. Typically, the hospital census variables were confirmed to have an impact on ED LOS (8).
Conclusion
This study substantiates and quantifies the hypothesis that emergent patients in the A&E prolong waiting times and LOS for non-emergent patients, and that the emergent patients are associated with increased risk of violating waiting time targets for semi-urgent patients. Quality metrics that measure waiting times and LOS may need to include consideration of the relative burden of emergent patients and excessive non-emergent patients with limited resources for medical care who visit A&E Departments and EDs.
Article Summary
1. Why is this topic important?
This study shows that an Accident and Emergency Department (A&E) has frequently failed to meet the waiting time target for non-emergent patients. It is imperative to determine the key factors contributing to the long waiting time and length of stay so that the service quality of the A&E can be maintained.
2. What does the study attempt to show?
Apart from the A&E misuse by a large number of non-emergent patients, this study attempts to investigate the impact of another important factor in the long waiting time and length of stay of non-emergent patients: the arrival of emergent patients.
3. What are the key findings?
This study finds that the emergent patients extend the waiting time and length of stay of the non-emergent patients, who make up the majority of A&E patients. This impact has been demonstrated to be statistically significant for both the individual and the entire group of non-emergent patients. Particularly important is that the emergent patients increase the probability of violating the 120-min waiting time target for Category 4 (non-emergent) patients.
4. How is patient care impacted?
This study provides insights on adjusting nurse staffing levels in response to a variety of A&E crowding situations, especially during a surge of non-emergent patients and sudden arrival of emergent patients. The real-time adjustment of nurse staffing level could improve patient satisfaction and enhance nurse morale.
Acknowledgment
This study was partially supported by the University Grants Committee – CRF projects no. CITYU8/CRF/09 and City University of Hong Kong – SRG Grant no. 7002773, as well as NIH/NCRR/OD UCSF-CTSI grant number KL2 RR024130 (R.Y.H.), and the Robert Wood Johnson Foundation Physician Faculty Scholars (R.Y.H.). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of any of the funding agencies.
References
- 1.Horwitz L.I., Green J., Bradley E.H. US emergency department performance on waiting time and length of visit. Ann Emerg Med. 2010;55:133–141. doi: 10.1016/j.annemergmed.2009.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yoon P., Steiner I., Reinhardt G. Analysis of factors influencing length of stay in the emergency department. Can J Emerg Med. 2003;5:155–161. doi: 10.1017/s1481803500006539. [DOI] [PubMed] [Google Scholar]
- 3.McCarthy M.L., Zeger S.L., Ding R. Crowding delays treatment and lengthens emergency department length of stay, even among high-acuity patients. Ann Emerg Med. 2009;54:492–503. doi: 10.1016/j.annemergmed.2009.03.006. e4. [DOI] [PubMed] [Google Scholar]
- 4.Vermeulen M.J., Ray J.G., Bell C. Disequilibrium between admitted and discharged hospitalized patients affects emergency department length of stay. Ann Emerg Med. 2009;54:794–804. doi: 10.1016/j.annemergmed.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 5.Pines J.M., Localio A.R., Jollander J.E. Racial disparities in emergency department length of stay for admitted patients in the United States. Acad Emerg Med. 2009;16:403–410. doi: 10.1111/j.1553-2712.2009.00381.x. [DOI] [PubMed] [Google Scholar]
- 6.Ding R., McCarthy M.L., Desmond J.S. Characterizing waiting room time, treatment time, and boarding time in the emergency department using quantile regression. Acad Emerg Med. 2010;17:813–823. doi: 10.1111/j.1553-2712.2010.00812.x. [DOI] [PubMed] [Google Scholar]
- 7.Rathlev N.K., Chessare J., Olshaker J. Time series analysis of variables associated with daily mean emergency department length of stay. Ann Emerg Med. 2007;49:265–271. doi: 10.1016/j.annemergmed.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 8.Lucas R., Farley H., Twanmoh J. Emergency department patient flow: the influence of hospital census variables on emergency department length of stay. Acad Emerg Med. 2009;16:597–602. doi: 10.1111/j.1553-2712.2009.00397.x. [DOI] [PubMed] [Google Scholar]
- 9.McCarthy M.L., Aronsky D., Jones I.D. The emergency department occupancy rate: a simple measure of emergency department crowding? Ann Emerg Med. 2008;51:15–24.e2. doi: 10.1016/j.annemergmed.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Forster A.J., Stiell I., Wells G. The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad Emerg Med. 2003;10:127–133. doi: 10.1111/j.1553-2712.2003.tb00029.x. [DOI] [PubMed] [Google Scholar]
- 11.Lambe S., Washington D.L., Fink A. Waiting times in California’s emergency departments. Ann Emerg Med. 2003;41:35–44. doi: 10.1067/mem.2003.2. [DOI] [PubMed] [Google Scholar]
- 12.Schull M.J., Kiss A., Szalai J.P. The effect of low-complexity patients on emergency department waiting times. Ann Emerg Med. 2007;49:257–264. doi: 10.1016/j.annemergmed.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 13.Medicare.gov. National Voluntary Consensus Standards for Emergency Care: A Consensus Report. Washington, DC: National Quality Forum; 2009; and United States Department of Health & Human Services, “Potential Future Measures for Hospital Value-based Purchasing Program.” Available at: http://www.hospitalcompare.hhs.gov/staticpages/for-consumers/value-based-purchasing.aspx. Accessed February 4, 2012.
- 14.Herring A., Wilper A., Himmelstein D.U. Increasing length of stay among adult visits to U. S. emergency departments, 2001–2005. Acad Emerg Med. 2009;16:609–616. doi: 10.1111/j.1553-2712.2009.00428.x. [DOI] [PubMed] [Google Scholar]
- 15.Wai A.K.C., Chor C.M., Lee A.T.C. Analysis of trends in emergency department attendances, hospital admissions and medical staffing in a Hong Kong university hospital: 5-year study. Int J Emerg Med. 2009;2:141–148. doi: 10.1007/s12245-009-0098-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graham G.A., Kwok W.O., Tsang Y.L. Preferences and perceptions of patients attending emergency departments with low acuity problems in Hong Kong. Hong Kong J Emerg Med. 2009;16:148–154. [Google Scholar]
- 17.Hoot N.R., LeBlanc L.J., Jones I. Forecasting emergency department crowding: a discrete event simulation. Ann Emerg Med. 2008;52:116–125. doi: 10.1016/j.annemergmed.2007.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Connelly L.G., Bair A.E. Discrete event simulation of emergency department activity: a platform for system-level operations research. Acad Emerg Med. 2004;11:1177–1185. doi: 10.1197/j.aem.2004.08.021. [DOI] [PubMed] [Google Scholar]
- 19.Qualls M., Pallin D.J., Schuur J.D. Parametric versus nonparametric statistical tests: the length of stay example. Acad Emerg Med. 2010;17:1113–1121. doi: 10.1111/j.1553-2712.2010.00874.x. [DOI] [PubMed] [Google Scholar]
- 20.Ong Y.S., Tsang Y.L., Ho Y.H. Nurses treating patients in the emergency department: a patient survey. Hong Kong J Emerg Med. 2007;14:10–15. [Google Scholar]
- 21.Lee A., Lau F.L., Hazlett C.B. Measuring the inappropriate utilization of accident and emergency services? Int J Health Care Quality Assurance. 1999;12:287–292. doi: 10.1108/09526869910287558. [DOI] [PubMed] [Google Scholar]
- 22.Chung C.H. Emergency department misuse and administrative interventions. Hong Kong J Emerg Med. 2000;7:220–230. [Google Scholar]
- 23.Lee A., Lau F.L., Hazelett C.B. Morbidity patterns of non-urgent patients attending accident and emergency departments in Hong Kong: cross-sectional study. Hong Kong Med J. 2001;7:131–138. [PubMed] [Google Scholar]
- 24.Man C.Y., Yeung R.S.D., Chung J.Y.M. Impact of SARS on an emergency department in Hong Kong. Hong Kong J Emerg Med. 2003;15:418–422. doi: 10.1046/j.1442-2026.2003.00495.x. [DOI] [PubMed] [Google Scholar]
- 25.Joshi A.J., Rys M.J. Study on the effect of different arrival patterns on an emergency department’s capacity using discrete event simulation. Int J Ind Eng. 2011;18:40–50. [Google Scholar]
- 26.Chan J.T.S. What will be the percentage drop in attendance of Accident & Emergency department after implementation of charges? Hong Kong J Emerg Med. 2001;8:241–246. [Google Scholar]
- 27.Leung G.M., Chan S.S.C., Chau P.Y.K. Using conjoint analysis to assess patients’ preferences when visiting emergency departments in Hong Kong. Acad Emerg Med. 2001;8:894–898. doi: 10.1111/j.1553-2712.2001.tb01151.x. [DOI] [PubMed] [Google Scholar]
- 28.Vertesi L. Does the Canadian Triage and Acuity Scale identify non-urgent patients who can be triaged away from the emergency department? Can J Emerg Med. 2004;6:337–342. doi: 10.1017/s1481803500009611. [DOI] [PubMed] [Google Scholar]
- 29.Ong M.E.H., Ho K.K., Tan T.P. Using demand analysis and system status management for predicting ED attendances and rostering. Am J Emerg Med. 2009;27:16–22. doi: 10.1016/j.ajem.2008.01.032. [DOI] [PubMed] [Google Scholar]
- 30.Kırıs Ş., Yüzügüllü N., Ergün N. A knowledge-based scheduling system for emergency departments. Knowledge Based Syst. 2010;23:890–900. [Google Scholar]
- 31.Green L.V., Soares J., Giglio J.F. Using queueing theory to increase the effectiveness of emergency department provider staffing. Acad Emerg Med. 2006;13:61–68. doi: 10.1197/j.aem.2005.07.034. [DOI] [PubMed] [Google Scholar]
- 32.Farrohknia N., Castren M., Ehrenberg A. Emergency department triage scales and their components: a systematic review of the scientific evidence. Scand J Trauma Resusc Emerg Med. 2011;19:42. doi: 10.1186/1757-7241-19-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tanabe P., Gimbel R., Yarnold P.R. Reliability and validity on the Emergency Severity Index version 3. Acad Emerg Med. 2004;11:59–65. doi: 10.1197/j.aem.2003.06.013. [DOI] [PubMed] [Google Scholar]
- 34.Wuerz R.C., Travers D., Gilboy N. Implementation and refinement of the Emergency Severity Index. Acad Emerg Med. 2001;8:170–176. doi: 10.1111/j.1553-2712.2001.tb01283.x. [DOI] [PubMed] [Google Scholar]
- 35.Wuerz R.C., Milne L.W., Eitel D.R. Reliability and validity of a new five-level triage instrument. Acad Emerg Med. 2000;7:236–242. doi: 10.1111/j.1553-2712.2000.tb01066.x. [DOI] [PubMed] [Google Scholar]