Abstract
Chikungunya disease results from an infection with the arbovirus, chikungunya virus (CHIKV). Symptoms of CHIKV include fever and persistent, severe arthritis. In recent years, several antiviral drugs have been evaluated in clinical trials; however, no registered antivirals have been approved for clinical therapy. In this study, we established a high-throughput screening (HTS) system based on CHIKV 26S mediated insect cell fusion inhibition assay. Our screening system was able to search potential anti-CHIKV drugs in vitro. Using this system, four compounds (niclosamide, nitazoxanide, niflumic acid, tolfenamic acid) were identified. These compounds were then further analyzed using a microneutralization assay. We determined that niclosamide and nitazoxanide exhibit ability to against CHIKV-induced CPE. The anti-CHIKV abilities of these compounds were further confirmed by RT-qPCR and IFA. Moreover, niclosamide and nitazoxanide were found to (1) limit virus entry, (2) inhibit both viral release and cell-to-cell transmission, and (3) possess broad anti-alphavius activities, including against two clinical CHIKV isolates and two alphaviruses: Sindbis virus (SINV) and Semliki forest virus (SFV). In conclusion, our findings suggested that niclosamide and nitazoxanide were able to inhibit CHIKV entry and transmission, which might provide a basis for the development of novel human drug therapies against CHIKV and other alphavirus infections.
Keywords: Antiviral screening, Chikungunya virus, Insect cell fusion assay, Niclosamide, Nitazoxanide
Highlights
-
•
Fusion inhibition assay was successfully established an anti-CHIKV drugs HTS system.
-
•
Niclosamide and nitazoxanide were found and verified their ability to against CHIKV entry and transmission.
-
•
Both of niclosamide and nitazoxanide also possessed broad anti-alphavirus abilities.
1. Introduction
Chikungunya disease is caused by an infection with Chikungunya virus (CHIKV), and sporadic outbreaks have occurred in Africa and Asia for decades. In 2005, 2006, an outbreak of chikungunya disease on La Réunion Island in France resulted in one-third of residents becoming infected. During this outbreak, the virus was also transmitted to south India (Parola et al., 2006) and southern Europe, including Italy and France (Gould et al., 2010, Rezza et al., 2007). Furthermore, the Carribean has been affected by an outbreak of chikungunya disease since December 2013, and the virus has become a public health threat in central America (Weaver and Forrester, 2015). Together, the two aforementioned outbreaks has led to hundreds of deaths and caused more than one million people to fall ill (Mavalankar et al., 2007, Weaver and Forrester, 2015). Symptoms of chikungunya disease include high fever, arthritis, arthralgia, headache, nausea, vomiting, and conjunctivitis. Some patients also suffer from severe joint pain for weeks or months (Burt et al., 2012, Weaver and Lecuit, 2015).
CHIKV is an alphavirus belonging to the family Togaviridae and has been classified as a risk group-3 (RG-3) pathogen (Staples et al., 2009) that enters cells through receptor-mediated endocytosis (i.e. the binding phase). Upon entry, the endosome undergoes acidification, which can lead to conformational changes in CHIKV envelope glycoproteins E1 and E2 (Voss et al., 2010). Envelop glycoproteins then form trimers, which cause the viral membrane and the endosome membrane to fuse together, forming a pore (i.e. the fusion phase) (van Duijl-Richter et al., 2015). The viral genome is then released into the cytosol.
The CHIKV RNA includes 49S genomic RNA and 26S subgenomic RNA. The 49S genomic RNA encodes four non-structural proteins which are responsible for viral genome synthesis (i.e. genome synthesis). CHIKV envelope glycoproteins and capsid proteins are translated by 26S subgenomic RNA in the endoplasmic reticulum (ER) and then are delivered into Golgi apparatus for further processing and glycosylation. Those structural proteins form the spike complexes pE2-E1, which are transported to the plasma membrane. Finally, the spike complexes are assembled with the nucleocapsid cores (Schwartz and Albert, 2010, van Duijl-Richter et al., 2015); and the viruses bud out and release to become mature virions (i.e. the release phase). CHIKV can also be spread through cell-to-cell transmission, which allows virions to efficiently avoid attacks from the host immune system (Hahon and Zimmerman, 1970).
Antiviral drugs are developed to disrupt the life cycle of virus. As indicated, the four main steps of viral multiplication include binding, fusion, genome synthesis, and transmission (including release and cell-to-cell transmission) (Abdelnabi et al., 2015, Parashar and Cherian, 2014). Virus fusion is a critical step of CHIKV infection. The fusion process is dependent on low-pH and the presence of cholesterol (Kuo et al., 2011); (Kuo et al., 2012). Similar findings have been reported for the Sindbis virus (SINV) and the Semliki forest virus (SFV) (Boggs et al., 1989, Chanel-Vos and Kielian, 2004, Kempf et al., 1987, Lanzrein et al., 1993). Therefore, fusion inhibitors are potential candidates for anti-CHIKV drugs. In this report, we described the use of an CHIKV 26S mediated insect cell fusion inhibition assay that uses baculovirus-based expression as a high-throughput screening (HTS) system to search for novel anti-CHIKV drugs (Macarron et al., 2011). We also discussed the effects and mechanisms of two potential anti-CHIKV candidates, niclosamide and nitazoxanide. Our results suggested that the antiviral properties of niclosamide, and nitazoxanide made them promising compounds for further development of anti-CHIKV drugs.
2. Materials and methods
2.1. Cell lines and viruses
BHK-21 (ATCC CCL-10, baby hamster kidney cells) cells were grown in Dulbecco's modified Eagle's medium (DMEM, Invitrogen, catalog # 10564–011) containing 5% fetal bovine serum (FBS, Invitrogen, catalog # 10082–147) at 37 °C and 5% CO2. Sf21 cells were grown in Sf-900 II SFM (Invitrogen, catalog # 10902–096) containing 5% FBS at 27 °C. We used BHK-21 cells to propagate CHIKV strains S27 (ATCC-VR-64, African prototype), 0611aTw (Singapore/0611aTw/2006/FJ807896, provided by the centers for disease control, ROC [TCDC]), and 0810bTw (Malaysia/0810bTw/2008/FJ807899, with 226V mutant, provided by TCDC) as well as Sindbis virus (ATCC-VR-68, original strain) and Semliki forest viruses (ATCC-VR-67, original strain). S-WT (i.e. a baculovirus constructed with the CHIKV 26S genome) and vector baculovirus (which was used as a control) were propagated in Sf21 cells (Kuo et al., 2011).
2.2. Compounds
An FDA-approved 788 drug library (Selleckchem, catalog No.L1300, 10 mM in DMSO) was purchased from Selleckchem to facilitate the CHIKV 26S mediated insect cell fusion inhibition assay. Niclosamide (Sigma, N3510), nitazoxanide (Sigma, N0290) and suramin (Sigma, S2671) were purchased from Sigma-Aldrich. T1105 (3-hydroxy-2-pyrazinecarboxamide, Toronto Research Chemicals (TRC), D454150) were purchased from TRC.
2.3. CHIKV 26S mediated insect cell fusion inhibition assay
Sf21 cells were transduced with vAc-CHIKV 26S-Rhir-E (S-WT) (Kuo et al., 2011) at an MOI (multiplicity of infection) of 2 and held at 27 °C overnight. Vector baculoviruses (vAc-Rhir-E) were transduced at the same time and under the same conditions. To delay membrane fusion, on the second day, we replaced the old medium with fresh medium (at a pH of 6.8). On the third day, infected cells were pre-treated with 100 μM of the 788 FDA-approved drugs (pH 6.8) for 1 h. The medium was then replaced with fresh medium (pH 5.8) containing 0.1 mg/ml cholesterol and 100 μM of the 788 FDA-approved drugs, and cells were incubated for 2 h. Images of viral fusion were captured using an inverted fluorescence microscope (Olympus, IX71), and fusion area was analyzed by Image J software. The fusion index was calculated using the formula: 1 – [cell count/(total area of fused cells/average area of single cells)] (Ho et al., 2015). Related fusion indexs of test compounds were normalized with respect to the group of S-WT at pH5.8.
2.4. Microneutralization assay
BHK-21 cells were infected with CHIKV strain S27 at an MOI of 0.001 in the presence of compounds at indicated dosages in Fig. 2B and Fig. S1. After an incubation period of 3 days, infected cells were fixed and stained using 0.1% crystal violet solution.
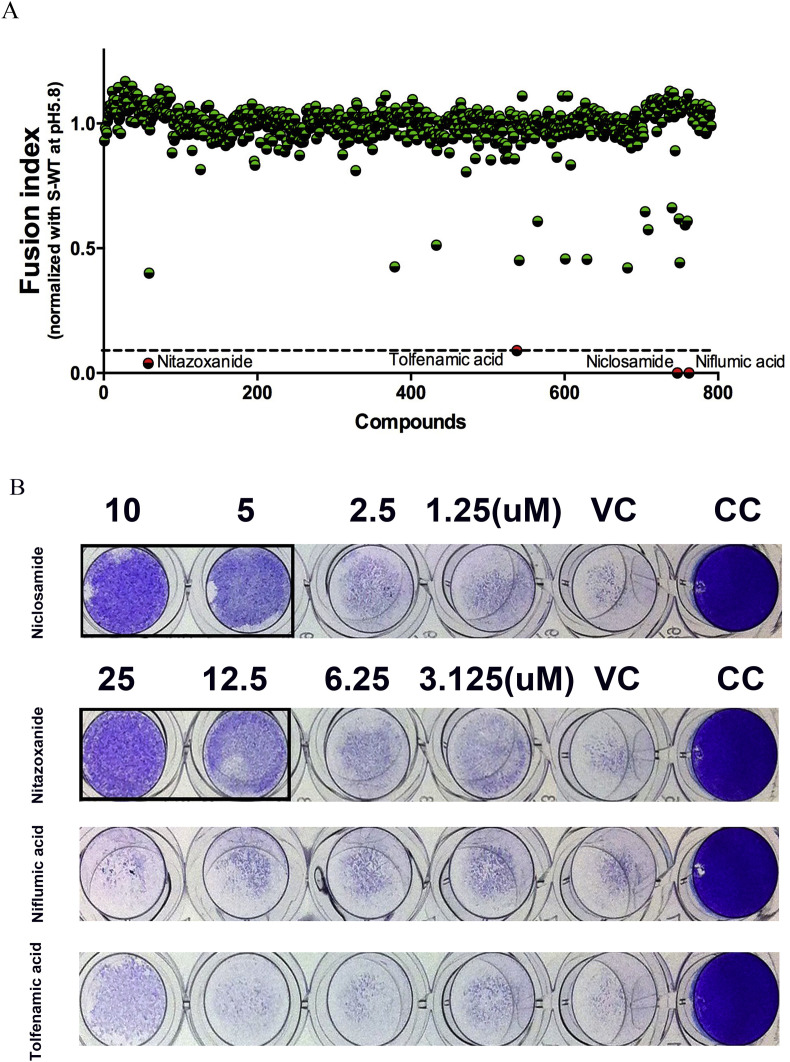
Fig. 2.
Compound screening and confirmation. (A) High-throughput screening of CHIKV 26S mediated insect cell fusion inhibitors obtained from a library of 788 FDA-approved drugs. (B) Microneutralization assay. The square frame represents the protective effects of niclosamide and nitazoxanide against CHIKV-induced CPE. (VC: as CHIKV infection control, CC: as negative control.)
2.5. Immunofluorescence assay (IFA)
Infected cells were fixed and incubated with rabbit anti-CHIKV E2 antibodies (1:200) (Kuo et al., 2011) or J2 anti-dsRNA IgG2a monoclonal antibodies (1:200; Scicons, catalog #J2-1406) for 1 h. These pre-stained cells were subsequently washed three times with PBS and incubated with Alexa Fluor 594-conjugated goat anti-rabbit IgG (1:500; Invitrogen, A11037), Alexa Fluor 594-conjugated goat anti-mouse IgG (1:500; Invitrogen, A11032) or Alexa Fluor 488-conjugated goat anti-mouse IgG (1:500; Invitrogen, A11029) for 1 h. After a final wash with PBS, images of cells were captured using an inverted fluorescence microscope (Olympus, IX71).
2.6. Reverse transcription-quantitative real-time polymerase chain reaction (RT-qPCR)
Total RNA was isolated using Trizol reagent (Invitrogen, catalog # 15596–026). The QuantiTect SYBR Green RT-PCR kit (Qiagen, catalog # 52906) was used to quantify viral RNA and actin RNA. (Primer sequences are listed in Table S1(Fragkoudis et al., 2007, Ho et al., 2015, Sane et al., 2012). Specifically, RT-qPCR was conducted (using the Roche LightCycler 480 System) for 30 min at 50 °C, 15 min at 95 °C, and then for forty-five additional cycles (where 1 cycle consisted of 15 s at 95 °C, 25 s at 57 °C, and 10 s at 72 °C). Relative values were calculated using the ΔΔCt method, and each experiment was performed in triplicate.
2.7. Cell viability
Cell viability was examined using the cell counting kit-8 (CCK-8) assay (Sigma-Aldrich, catalog #96992). For this, cells were seeded in 96-well plates. The cells were then incubated with the candidate drugs at the indicated dosages for 16 h. The CCK-8 reagent was diluted by culture medium at 1/10 (v/v) and replaced into all wells for 1–4 h of incubation. Optical density (OD) was detected using the Tecan Infinite 200 Pro multiplate reader. Cell viability was determined according to the following formula: cell viability = [(OD 450 treated cells – OD 650 reference control)/(OD450 control cells – OD650 reference control)] × 100.
2.8. Entry assay
BHK-21 cells were infected with CHIKV strain S27 at an MOI of 0.001 and incubated with indicated concentrations of niclosamide and nitazoxanide for 1 h at 37 °C. After washing with DMEM, the infected cells were covered with medium containing 4.5 ml 1% agarose and incubated for 2 days. Finally, infected cells were fixed and stained with 1% crystal violet solution. Plaque formations were counted and normalized with respect to the virus control group. All results were obtained from at least three independent experiments.
2.9. Time of addition assay
BHK-21 cells were infected with CHIKV strain S27 at an MOI of 1 and incubated for 2 h. The viruses were removed and the medium was replaced. In addition, 2.5 μM niclosamide or 12.5 μM nitazoxanide were added to cells prior to infection (pre), during infection (co), or during post-infection (post) stages. After an 8 h incubation period, the intracellular production of CHIKV RNA in cells was determined by RT-qPCR, and the percentage of inhibition associated with each compound was normalized with respect to the virus control group (VC). The release of CHIKV progeny was collected from the supernatant and analyzed using a TCID50 assay.
2.10. Cell-to-cell transmission assay
BHK-21 cells were seeded in a 24 well plate, infected with CHIKV strain S27 at an MOI of 0.001, and incubated period of 1 h. The inoculum was subsequently removed and the medium was replaced with fresh medium containing CHIKV neutralization antibodies (Ho et al., 2015, Kuo et al., 2011) and the indicated drugs. Cells were then incubated for 16 h and then fixed and stained with J2 anti-dsRNA IgG2a monoclonal antibodies (1:200; Scicons, catalog #J2-1406) according to standard IFA protocols. Finally, nuclei were stained with DAPI so that the number of cells per focus could be counted (Ho et al., 2015).
2.11. In-vivo zebrafish assays for toxicity testing
We used a dissecting microscope (Hamlet, MSH655-T) to observe morphological anomalies in zebrafish, including chorion with attached debris, delayed development, lack of spontaneous movement, pericardial edema, yolk sac edema, bent trunk, tail malformation, and uninflated swim bladder. We also recorded hatch and survival rates, which are expressed as the number of that have hatched or dead embryos as compared with the control group. We stored 4–5 h post fertilization (hpf) embryos in 48-well plates at a concentration of two embryos/well, and each well contained 1 ml of test solution (i.e. either niclosamide at 2.5 or 10 μM, or nitazoxanide at 50 or 12.5 μM). Specifically, embryos were stored at 28 °C for 7 days (with a 14/10 h light/dark photoperiod) and were updated daily (Ho et al., 2015). Study protocol was approved by the Institutional Animal Care and Use Committee (IACUC) of National Taiwan University and conformed to criteria outlined in the “Guide for the Care and Use of Laboratory Animals” by the National Institutes of Health. After experiments were completed, zebrafish were sacrificed using 0.5% tricaine (Sigma-Aldrich, catalog # MS-222), whereby all efforts were made to minimize suffering.
2.12. Statistical analysis
Experimental results were analyzed using the Student's t-test and the Kaplan-Meier test, performed in GraphPad prism software. All data were obtained from at least three independent experiments, and a p value of <0.05 was considered significant.
3. Results
3.1. Establishment of CHIKV 26S mediated insect cell fusion inhibition assay
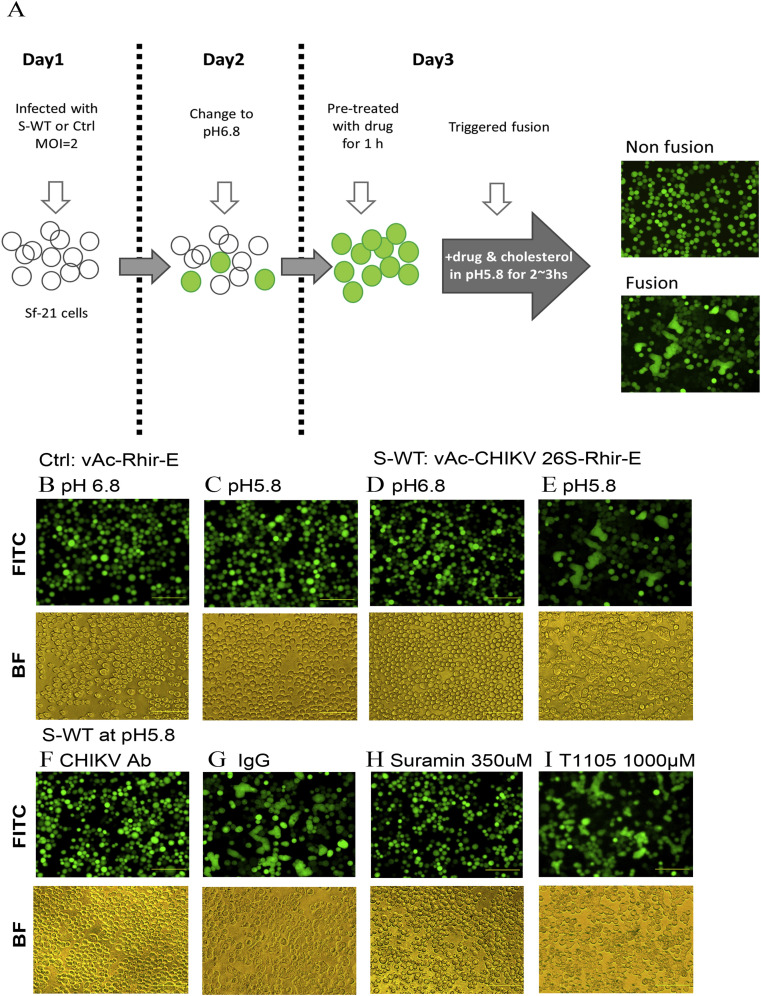
CHIKV 26S subgenomic RNA encoded structural proteins (including Capsid (C) and envelope proteins (E3, E2, 6K, and E1)) which played roles in receptor binding and membrane fusion. Co-expressed CHIKV structural proteins and enhanced green fluorescence protein (EGFP) by bi-cistronic baculovirus expression system was utilized to acquire EGFP-positive Sf21 cells expressing CHIKV structure proteins. The EGFP-positive cells were able to characterize cell fusion (Chen et al., 2005). An illustration of CHIKV 26S mediated insect cell fusion inhibition assay protocol is shown in Fig. 1 A. The fusion phenomenon was not observed when Sf21 cells were transduced with control vector baculovirus (vAc-Rhir-E) whether at pH6.8 (Fig. 1B) or at pH5.8 (Fig. 1C). When Sf21 cell were transduced with S-WT, the fusion phenomenon was retarded at pH6.8 (Fig. 1D) but accelerated in the presence of cholesterol at pH5.8 (Fig. 1E). Therefore, the group of S-WT at pH5.8 (Fig. 1E) was as a fusion control, all compounds were detected under this condition.
Fig. 1.
Construction and analysis of CHIKV 26S mediated insect cell fusion inhibition assay. (A) Schematic representation of the CHIKV 26S mediated insect cell fusion inhibition assay. (B and C) Vector baculovirus (control: vAc-Rhir-E) infection at pH6.8 and pH5.8. (D and E) S-WT (vAc-CHIKV 26S-Rhir-E) infection at pH6.8 and pH5.8. (F and G) S-WT infection at pH5.8 in the presence of CHIKV neutralization antibodies and IgG. (H and I) S-WT infection at pH5.8 in the presence of suramin and T1105.
CHIKV neutralizing antibodies (Kuo et al., 2011) (Fig. 1F) was able to inhibit CHIKV 26S mediated cell fusion but not IgG (Fig. 1G). These findings suggest that the fusion phenomenon was specifically triggered by CHIKV structural proteins. Suramin has been shown to possess anti-CHIKV activities such as fusion inhibition, and was thus used as positive control (Ho et al., 2015). Conversely, T1105 was considered to be a CHIKV replication antagonist and was used as negative control. Suramin was able to disrupt cell fusion of S-WT transduction at pH5.8 (Fig. 1H), but T1105 could not (Fig. 1I). These findings provided evidence to suggest that our novel platform can be used to identify potential fusion inhibitors.
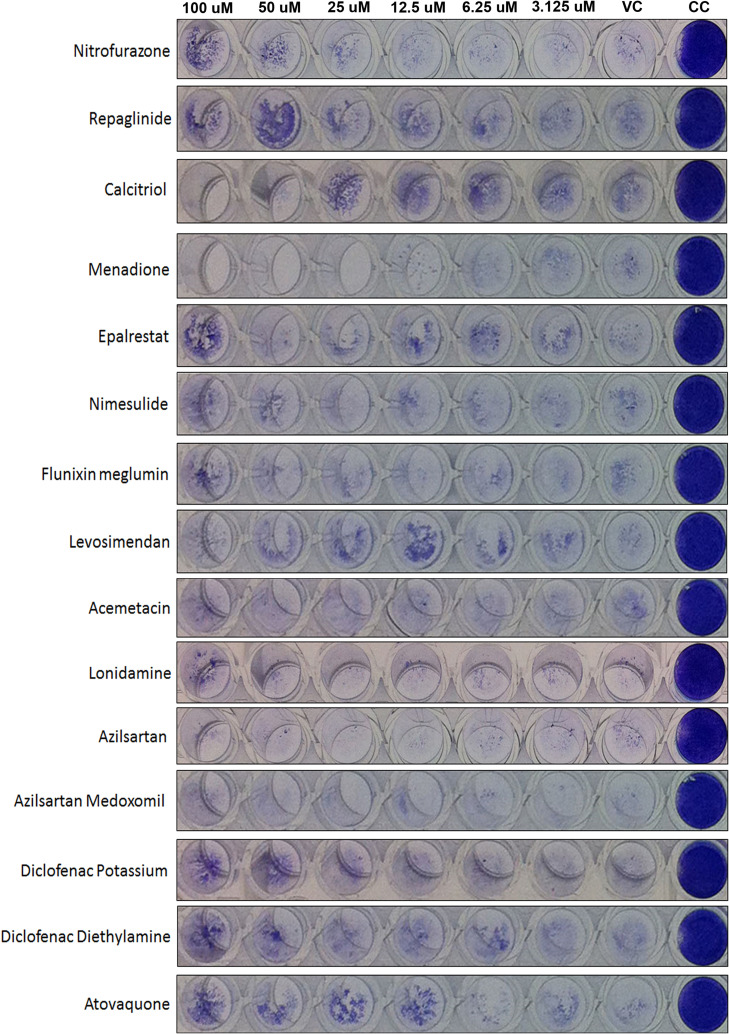
3.2. Compound screening and anti-CHIKV effects of candidate drugs
We used a CHIKV 26S mediated insect cell fusion inhibition assay to perform high-throughput screening of CHIKV fusion inhibitors (obtained from an FDA-approved 788 drug library). Afterwards, the related fusion index was normalized with respect to the group of S-WT at pH5.8 (Fig. 1E), and determined that four compounds, niclosamide, nitazoxanide, niflumic acid, and tolfenamic acid, had fusion index lower than 0.1 (red points in Fig. 2 A) and the Z-scores were −8.812, -8.467, -8.812, and −8.012. Anti-CHIKV abilities were further characterized by a microneutralization assay, both niclosamide and nitazoxanide exhibited activity against CHIKV-induced CPE (Fig. 2B). The compounds with intermediate inhibitory activity (Fusion index 0.5) further tested by microneutralization assay and confirmed they did not inhibit CHIKV infection (Fig. S1). These results indicate that some fusion inhibitors (Fusion index<0.1) are potential candidates for the development of anti-CHIKV drugs.
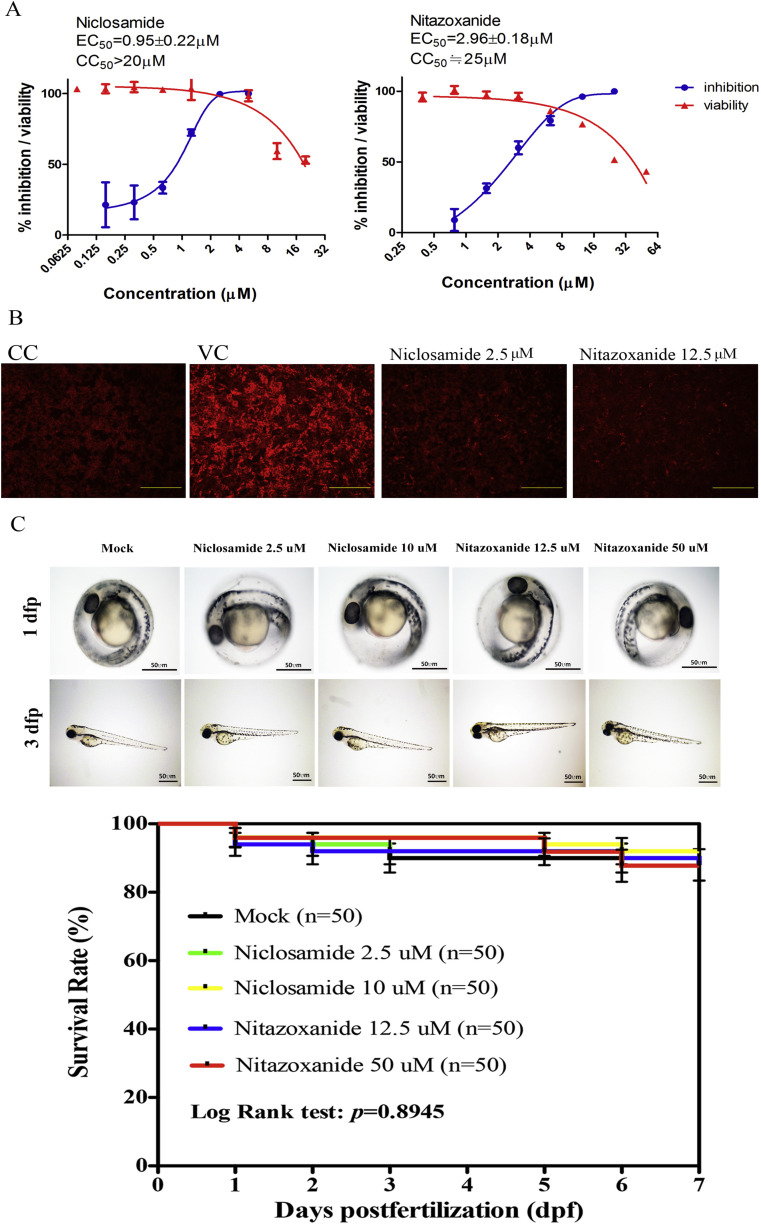
To further confirm the anti-CHIKV effects of niclosamide and nitazoxanide, RT-qPCR and IFA were performed. For these tests, BHK-21 cells were infected with CHIKV at an MOI of 0.01 in the presence of various dosages of niclosamide and nitazoxanide. Intracellular RNA was extracted at 16 h p.i., and the CHIKV RNA level was normalized with actin. Percent inhibition of CHIKV RNA level was normalized with respect to CHIKV infection group to define EC50. The effects of niclosamide and nitazoxanide on BHK-21 cell viability were analyzed with a CCK-8 assay to define CC50. Niclosamide showed an EC50 value of 0.95 ± 0.22 μM and a CC50 value of >20 μM. Conversely, the EC50 and CC50 values of nitazoxanide were determined to be 2.96 ± 0.18 μM and 25 μM (Fig. 3 A, Table 1 ).
Fig. 3.
Evaluation of anti-CHIKV abilities and toxicity of niclosamide and nitazoxanide. (A) Dose-dependent curves showing the anti-CHIKV activities of niclosamide and nitazoxanide (blue) and associated effects on the viability of BHK-21 cells (red). (B) IFA of niclosamide and nitazoxanide. (C) In vivo toxicity assay using zebrafish. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Table 1.
Antiviral activity of Niclosamide and Nitazoxanide against various alphaviruses in vitro.
| Cell line | Virus strains | Niclosamide (μM) |
Nitazoxanide (μM) |
||||
|---|---|---|---|---|---|---|---|
| EC50a | CC50b | SIc | EC50a | CC50b | SIc | ||
| BHK-21 | CHIKV | 0.95 ± 0.22 | >20 | >21.05 | 2.96 ± 0.18 | 25 | 8.45 |
| CHIKV 0611aTw | 0.85 ± 0.12 | >20 | >23.53 | 1.96 ± 0.48 | 25 | 12.76 | |
| CHIKV 0810bTw | 0.90 ± 0.12 | >20 | >22.22 | 4.95 ± 0.23 | 25 | 5.05 | |
| SINV | 1.07 ± 0.40 | >20 | >18.69 | 1.53 ± 1.10 | 25 | 16.34 | |
| SFV | 1.79 ± 0.23 | >20 | >11.17 | 3.56 ± 0.27 | 25 | 7.02 | |
| U2OS | CHIKV | 0.36 ± 0.08 | >20 | >55.55 | 3.01 ± 0.61 | 25 | 8.31 |
The EC50s were determined using RT-qPCR and were presented as means ± SD (n ≥ 3).
The CC50s were determined using a CCK-8 assay and were presented as means ± SD (n ≥ 3).
The SI (selectively index) represented the ratio of CC50 to EC50.
In addition, BHK-21 cells were infected with CHIKV at an MOI of 1 in the presence of 2.5 μM niclosamide or 12.5 μM nitazoxanide and incubated for 8 h. Anti-CHIKV E2 antibodies were used in IFA to determine CHIKV replication, and both niclosamide and nitazoxanide were confirmed possessing anti-CHIKV activities (Fig. 3B). The toxicity of these compounds was also analyzed in vivo using zebrafish embryos, and neither compound was found to negatively affect survival, body length, development, or hatch rate (Fig. 3C). These findings indicated that the dosages of niclosamide and nitazoxanide we applied were safe and could be used to verify their anti-CHIKV effects.
3.3. Anti-CHIKV mechanisms of niclosamide and nitazoxanide
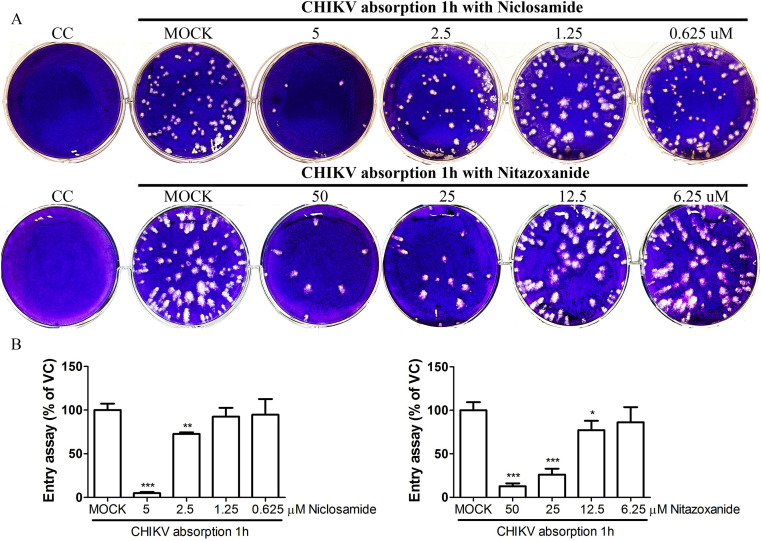
Niclosamide and nitazoxanide can inhibit CHIKV 26S mediated cell fusion; therefore, these compounds might also be able to suppress the early stage of CHIKV infection. To further investigate this possibility, BHK-21 cells were infected with CHIKV at an MOI of 0.01 and co-treated with niclosamide (5, 2.5, 1.25, or 0.625 μM) or nitazoxanide (50, 25, 12.5, or 6.25 μM) at 37 °C for a 1 h incubation period. The inoculum was then removed, and treated cells were washed and covered with 1% agarose without any drugs to determine the effects of niclosamide and nitazoxanide on virus entry. Both compounds were found to significantly inhibit CHIKV entry in a dose-dependent manner (Fig. 4 ).
Fig. 4.
Dose-dependent responses of niclosamide and nitazoxanide on CHIKV entry. (A) An entry assay showing the inhibitory effects of different niclosamide and nitazoxanide doses. (B) Quantification of entry assay. The percentage was calculated by counting the number of plaque formations and normalizing this value with respect to that of the virus control group (MOCK).
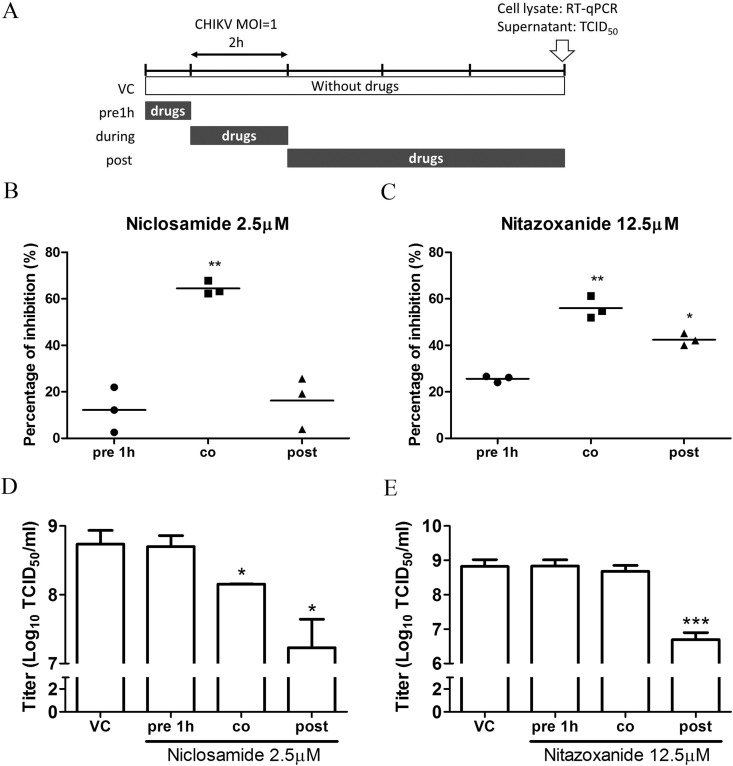
To investigate the stage of CHIKV infection which was affected by niclosamide and nitazoxanide, a time-of-addition assay was used. For this, BHK-21 cells were infected with CHIKV at an MOI of 1 for 2 h incubation. Subsequently, the inoculum was removed and placed into fresh medium. The 2.5 μM niclosamide or 12.5 μM nitazoxanide were added prior to infection (pre), during infection (co), or post-infection (post). At 8 h p.i., cell lysate and supernatant were collected and analyzed by RT-qPCR and a TCID50 assay (Fig. 5 A). Fig. 5B shows the percent inhibition which was observed at the intracellular CHIKV RNA level. Specifically, niclosamide and nitazoxanide presented inhibition of CHIKV attachment during infection stage (co), and these findings confirm results of the entry assay. In addition, nitazoxanide presented minor inhibition during the post-infection stage (post), which implied the inhibition of nitazoxanide in CHIKV genome synthesis. Besides, the production of CHIKV progeny was determined using a TCID50 assay (Fig. 5C) to analyze the release of CHIKV virions. Both compounds were able to suppress the production of CHIKV progeny during the post-infection stage (post), which indicate their inhibition in virus release. Besides, niclosamide showed the ability to inhibit progeny production during infection stage (co), which meant niclosamide possess high efficacy during virus entry. Even though niclosamide treated only during infection, it still affects virus progeny production.
Fig. 5.
Time of addition assay. (A) The illustration of time of addition assay. (B) Anti-CHIKV effects of niclosamide and nitazoxanide on intracellular CHIKV RNA. (C) Anti-CHIKV effects of niclosamide and nitazoxanide on the production of CHIKV progeny.
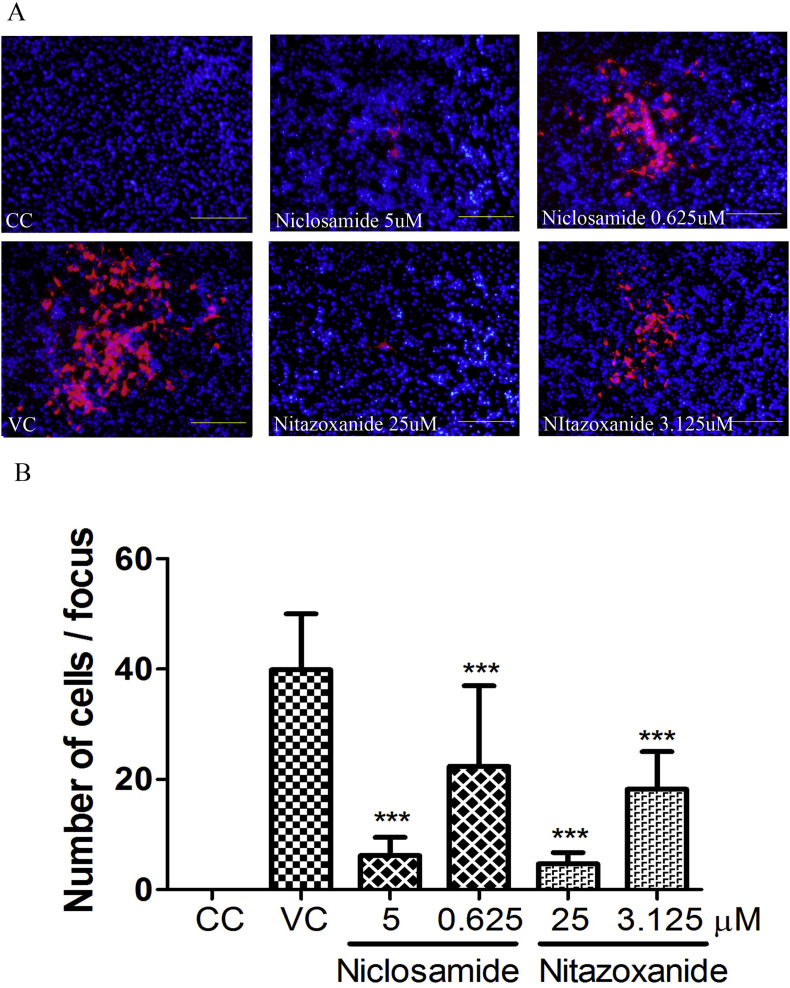
Cell-to-cell transmission is another important pathway for CHIKV transmission (Hahon and Zimmerman, 1970). In the previous finding, suramin possessed the anti-CHIKV ability not only in cell fusion but also transmission (i.e. release and cell-to-cell transmission) (Ho et al., 2015). The above results show that both niclosamide and nitazoxanide were able to inhibit CHIKV entry and disrupt the release of CHIKV virions. Therefore, we analyzed the roles that niclosamide and nitazoxanide played in cell-to-cell transmission. BHK-21 cells were infected with CHIKV at an MOI of 0.001 for 1 h incubation and then the medium was replaced with fresh medium containing CHIKV neutralization antibodies and the indicated drugs. CHIKV neutralizing antibodies were added to neutralize releasing CHIKV progeny, therefore the area of CHIKV infection was considered which was caused by cell-to-cell transmission. The infected area was determined by dsRNA staining. As shown in Fig. 6 A, both niclosamide and nitazoxanide significantly reduced the area of CHIKV infection. These results also indicated that niclosamide and nitazoxanide significantly reduce cell-to-cell transmission with a dose-dependent manner (Fig. 6B).
Fig. 6.
Cell-to-cell transmission. (A) Cell-to-cell transmission of niclosamide and nitazoxanide identified by IFA. The infected cells were stained by dsRNA antibodies (red). DAPI staining (blue) was used to determine the cell nucleus. (B) The quantification of cell-to-cell transmission assay. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.4. Antiviral abilities of niclosamide and nitazoxanide on CHIKV and other alphaviruses in vitro
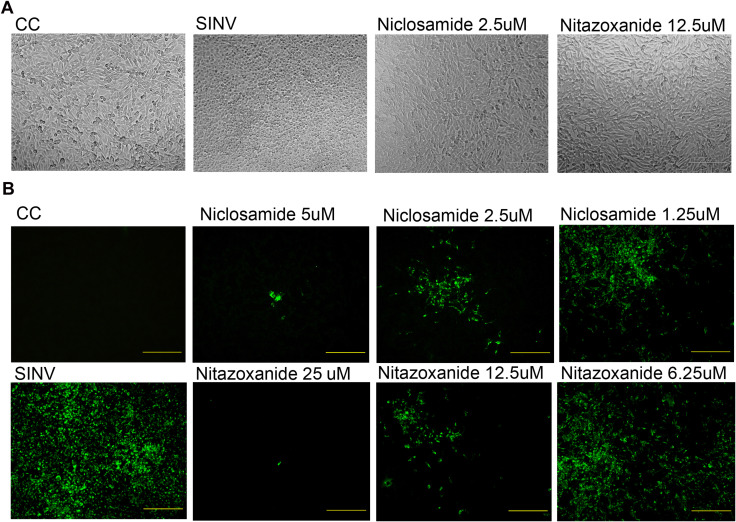
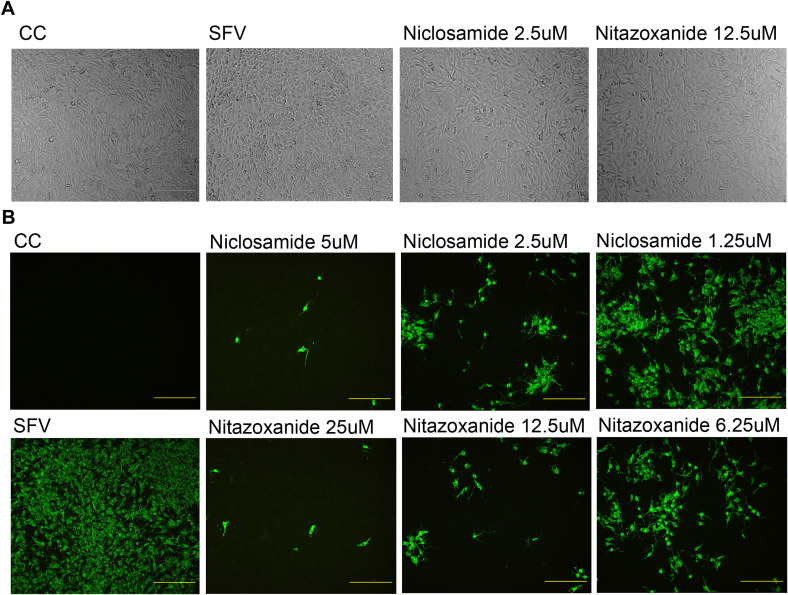
To determine the anti-viral spectrum of niclosamide and nitazoxanide, BHK-21 cells were infected with two different clinical strains of CHIKV (i.e. 0611aTw and 0810bTw, a 226V mutant strain) as well as two other alphaviruses, SINV and SFV. For this, all MOIs were 0.01, and cells were treated with various dosages of niclosamide or nitazoxanide. After 16 h of incubation, the cell lysate was used to extract intracellular RNA, which was analyzed by RT-qPCR to define EC50. For niclosamide, EC50 values were between 0.85 and 0.95 μM in different CHIKV strains, while EC50 values in SINV and SFV were 1.07 and 1.79 μM, respectively. The selectively index (SI) for this drug was between 11.17 and 23.53. Conversely, for nitazoxanide, EC50 values were between 1.96 and 4.95 μM in different CHIKV strains, while EC50 values in SINV and SFV were 1.53 and 3.56 μM, respectively. The selectively index (SI) for this drug was between 5.05 and 16.34. The cytopathic effect of BHK-21 cells infected with SINV (Fig. S2A) and SFV (Fig. S3A) were further observed but not appeared under the treatment of niclosamide or nitazoxanide. The dsRNA staining was further used to detect SINV (Fig. S2B) and SFV (Fig. S3B) infection and also confirmed the ability of anti-SINV and anti-SFV of niclosamide and nitazoxanide.
U2OS cells were a kind of human bone osteosarcoma epithelial cells and were able to be infected with CHIKV. Both niclosamide and nitazoxanide showed their inhibition of CHIKV, when U2OS were infected with CHIKV. The EC50 of niclosamide and nitazoxanide were 0.36 ± 0.08 and 3.01 ± 0.61, the CC50 were >20 and > 25 and the SI were >55.55 and 8.31. Taken together, this evidence indicates that niclosamide and nitazoxanide possessed the potential to become anti-CHIKV drugs.
4. Discussion
CHIKV was classified into risk group-3 pathogens. However, the baculovirus-based expression system is safe and can be operated in a BSL-2 laboratory. Therefore, using a CHIKV 26S mediated insect cell fusion inhibition assay can decrease the risk of HTS to search for anti-CHIKV drugs. In this study, four of the 788 FDA approved drugs showed the ability to block cell fusion; however, only two of them, niclosamide and nitazoxanide, were confirmed to have anti-CHIKV effects (Fig. 2B and Fig. 3). An entry assay was used to verify the inhibition mechanisms of drugs during early infection. Niclosamide and nitazoxanide both showed inhibition abilities during the early stages of CHIKV infection (Fig. 4). Furthermore, these drugs were able to inhibit two CHIKV clinical isolates, and also two other alphaviruses as well (Table 1). Experimental data further indicated that both compounds possess broad anti-alphavirus abilities. The anti-CHIKV activity of niclosamide and nitazoxanide also proved using U2OS cells, which verified their potential use in human cells (Table 1).
A previous study indicates that niclosamide is a proton carrier that targets acidic endosomes and has broad antiviral effects (Jurgeit et al., 2012). Nitazoxanide is also considered to be a broad-spectrum antiviral agent that can be used to treat dengue, yellow fever, JEV, respiratory syncytial virus (RSV), parainfluenza, coronavirus, rotavirus, norovirus, hepatitis B (HBV), hepatitis C (HCV), and human immunodeficiency virus (HIV) (Rossignol, 2014). Furthermore, nitazoxanide has been found to inhibit the early and mid-stages of Japanese encephalitis virus (JEV) infection (Shi et al., 2014). Based on these findings, we suggested that niclosamide and nitazoxanide might possess broad anti-alphavirus abilities in suppressing the early stages of CHIKV infection.
In a time-of-addition assay, cell lysate and supernatant were separately analyzed by RT-qPCR and TCID50 assay. Depending on assay design, intracellular CHIKV RNA was used to determine the effects of test compounds on virus binding (pre-infection, pre), virus entry (during infection, co) and viral genome replication (post-infection, post). Moreover, a TCID50 assay conducted during the post-infection stage was used to quantify extracellular CHIKV progeny (i.e. viral release). Niclosamide treatment during infection (co) significantly reduced the intracellular CHIKV RNA level (Fig. 5B). Moreover, the production of extracellular CHIKV progeny was significantly reduced when cells were treated with niclosamide both during and post-infection stages (Fig. 5C). Above results implied that niclosamide could affect both virus entry and release. Nitazoxanide also decreased the intracellular CHIKV RNA level when it was added during infection (co) and post-infection (post) (Fig. 5B). Besides, nitazoxanide was able to suppress the production of CHIKV progeny during the post-infection stage (Fig. 5C). Previous studies indicated nitazoxanide with the antiviral activity in post infection of influenza A virus and rotavirus (Rossignol, 2014). Nitazoxanide might affected influenza A virus assembly (Rossignol et al., 2009) and rotavirus replication (La Frazia et al., 2013). Our data also suggested that nitazoxanide might possess inhibition abilities against virus entry, genome synthesis and virus release.
Virus transmission was including extracellular transmission (virus release) and intracellular transmission (cell-to-cell transmission). Cell-to-cell transmission is considered an important transmission pathway and allows viruses to avoid attacks by immune system. Previous studies indicated that CHIKV structural proteins might involve not only in virus binding and fusion but also virus release (Masrinoul et al., 2014) and cell-to-cell transmission (Lee et al., 2011). Our previous study indicated that suramin was able to inhibit virus entry, fusion, release and cell-to-cell transmission (Ho et al., 2015). The above data had proved that niclosamide and nitazoxanide were able to inhibit virus entry and release. Furthermore, niclosamide and nitazoxanide were tested and found to significantly suppress cell-to-cell transmission of CHIKV infection. This study is the first to demonstrate that those two compounds can inhibit the cell-to-cell transmission of CHIKV infection.
In conclusion, CHIKV 26S mediated insect cell fusion assays could be used to search for anti-CHIKV drugs. Using this platform, we found and determined that niclosamide and nitazoxanide possessed the anti-CHIKV abilities. Further investigated those two compounds can affect CHIKV entry and transmission and also possess broad anti-alphaviruses abilities. Niclosamide and nitazoxanide could be used for the development of anti-CHIKV or anti-alphavirus drugs in the future. Formulation altering or combining with other anti-CHIKV drugs were able to improve drug efficacy and reduce their dosage. Besides, through structure modification to find some novel derivatives was also another way to develop safe and efficacious anti-CHIKV drugs.
Author contributions
JWL, SCK, and YJH conceived and designed the experiments. YMW, JWL, YFC, and YJH performed the experiments. JWL and YJH analyzed the data. YMW, JWL, CCL, TYW, ZZL, LIL, SCK, and YJH contributed reagents, materials, and analytical tools. JWL and YJH wrote the paper. JWL, YJH, LIL, and SCK helped interpret results.
Conflict of interest
The authors declare that they have no conflicts of interest.
Acknowledgements
This study was supported by grants (104-9-B19, 105-G6-1(3), 105-G6-2(3), 105-G6-3(3), and MAB-105-023) from the Institute of Preventive Medicine, National Defense Medical Center.
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.antiviral.2016.10.003.
Contributor Information
Szu-Cheng Kuo, Email: szucheng1234@gmail.com.
Yi-Jung Ho, Email: ejung330@gmail.com.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
Fig. S1. Microneutralization assay of the drugs with intermediate inhibitory activity (Fusion index 0.5). Those 15 compounds were tested and did not observe the inhibition of CHIKV infection.
Fig. S2. Analysis of the anti-SINV effect of niclosamide and nitazoxanide. BHK-21 cells were infected with SINV at a MOI of 0.01under the treatment of niclosamide and nitazoxanide at the indicated concentrations for 16 h incubation. (A) The SINV-induced CPE was examined under a light microscope. (B) The SINV were determined by dsRNA staining.
Fig. S3. Analysis of the anti-SFV effect of niclosamide and nitazoxanide. BHK-21 cells were infected with SFV at a MOI of 0.01under the treatment of niclosamide and nitazoxanide at the indicated concentrations for 16 h incubation. (A) The SFV-induced CPE was examined under a light microscope. (B) The SFV were determined by dsRNA staining.
References
- Abdelnabi R., Neyts J., Delang L. Towards antivirals against chikungunya virus. Antivir. Res. 2015;121:59–68. doi: 10.1016/j.antiviral.2015.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boggs W.M., Hahn C.S., Strauss E.G., Strauss J.H., Griffin D.E. Low pH-dependent Sindbis virus-induced fusion of BHK cells: differences between strains correlate with amino acid changes in the E1 glycoprotein. Virology. 1989;169:485–488. doi: 10.1016/0042-6822(89)90178-5. [DOI] [PubMed] [Google Scholar]
- Burt F.J., Rolph M.S., Rulli N.E., Mahalingam S., Heise M.T. Chikungunya: a re-emerging virus. Lancet. 2012;379:662–671. doi: 10.1016/S0140-6736(11)60281-X. [DOI] [PubMed] [Google Scholar]
- Chanel-Vos C., Kielian M. A conserved histidine in the ij loop of the Semliki Forest virus E1 protein plays an important role in membrane fusion. J. Virol. 2004;78:13543–13552. doi: 10.1128/JVI.78.24.13543-13552.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y.J., Chen W.S., Wu T.Y. Development of a bi-cistronic baculovirus expression vector by the Rhopalosiphum padi virus 5' internal ribosome entry site. Biochem. Biophys. Res. Commun. 2005;335:616–623. doi: 10.1016/j.bbrc.2005.07.116. [DOI] [PubMed] [Google Scholar]
- Fragkoudis R., Breakwell L., McKimmie C., Boyd A., Barry G., Kohl A., Merits A., Fazakerley J.K. The type I interferon system protects mice from Semliki Forest virus by preventing widespread virus dissemination in extraneural tissues, but does not mediate the restricted replication of avirulent virus in central nervous system neurons. J. Gen. Virol. 2007;88:3373–3384. doi: 10.1099/vir.0.83191-0. [DOI] [PubMed] [Google Scholar]
- Gould E.A., Gallian P., De Lamballerie X., Charrel R.N. First cases of autochthonous dengue fever and chikungunya fever in France: from bad dream to reality! Clin. Microbiol. Infect. 2010;16:1702–1704. doi: 10.1111/j.1469-0691.2010.03386.x. [DOI] [PubMed] [Google Scholar]
- Hahon N., Zimmerman W.D. Chikungunya virus infection of cell monolayers by cell-to-cell and extracellular transmission. Appl. Microbiol. 1970;19:389–391. doi: 10.1128/am.19.2.389-391.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho Y.J., Wang Y.M., Lu J.W., Wu T.Y., Lin L.I., Kuo S.C., Lin C.C. Suramin inhibits chikungunya virus entry and transmission. PLoS One. 2015;10:e0133511. doi: 10.1371/journal.pone.0133511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jurgeit A., McDowell R., Moese S., Meldrum E., Schwendener R., Greber U.F. Niclosamide is a proton carrier and targets acidic endosomes with broad antiviral effects. PLoS Pathog. 2012;8:e1002976. doi: 10.1371/journal.ppat.1002976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempf C., Michel M.R., Kohler U., Koblet H. A novel method for the detection of early events in cell-cell fusion of Semliki Forest virus infected cells growing in monolayer cultures. Arch. Virol. 1987;95:283–289. doi: 10.1007/BF01310786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo S.C., Chen Y.J., Wang Y.M., Kuo M.D., Jinn T.R., Chen W.S., Chang Y.C., Tung K.L., Wu T.Y., Lo S.J. Cell-based analysis of Chikungunya virus membrane fusion using baculovirus-expression vectors. J. Virol. Methods. 2011;175:206–215. doi: 10.1016/j.jviromet.2011.05.015. [DOI] [PubMed] [Google Scholar]
- Kuo S.C., Chen Y.J., Wang Y.M., Tsui P.Y., Kuo M.D., Wu T.Y., Lo S.J. Cell-based analysis of Chikungunya virus E1 protein in membrane fusion. J. Biomed. Sci. 2012;19:44. doi: 10.1186/1423-0127-19-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Frazia S., Ciucci A., Arnoldi F., Coira M., Gianferretti P., Angelini M., Belardo G., Burrone O.R., Rossignol J.F., Santoro M.G. Thiazolides, a new class of antiviral agents effective against rotavirus infection, target viral morphogenesis, inhibiting viroplasm formation. J. Virol. 2013;87:11096–11106. doi: 10.1128/JVI.01213-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanzrein M., Kasermann N., Weingart R., Kempf C. Early events of Semliki Forest virus-induced cell-cell fusion. Virology. 1993;196:541–547. doi: 10.1006/viro.1993.1509. [DOI] [PubMed] [Google Scholar]
- Lee C.Y., Kam Y.W., Fric J., Malleret B., Koh E.G., Prakash C., Huang W., Lee W.W., Lin C., Lin R.T., Renia L., Wang C.I., Ng L.F., Warter L. Chikungunya virus neutralization antigens and direct cell-to-cell transmission are revealed by human antibody-escape mutants. PLoS Pathog. 2011;7:e1002390. doi: 10.1371/journal.ppat.1002390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macarron R., Banks M.N., Bojanic D., Burns D.J., Cirovic D.A., Garyantes T., Green D.V., Hertzberg R.P., Janzen W.P., Paslay J.W., Schopfer U., Sittampalam G.S. Impact of high-throughput screening in biomedical research. Nat. Rev. Drug Discov. 2011;10:188–195. doi: 10.1038/nrd3368. [DOI] [PubMed] [Google Scholar]
- Masrinoul P., Puiprom O., Tanaka A., Kuwahara M., Chaichana P., Ikuta K., Ramasoota P., Okabayashi T. Monoclonal antibody targeting chikungunya virus envelope 1 protein inhibits virus release. Virology. 2014;464–465:111–117. doi: 10.1016/j.virol.2014.05.038. [DOI] [PubMed] [Google Scholar]
- Mavalankar D., Shastri P., Raman P. Chikungunya epidemic in India: a major public-health disaster. Lancet Infect. Dis. 2007;7:306–307. doi: 10.1016/S1473-3099(07)70091-9. [DOI] [PubMed] [Google Scholar]
- Parashar D., Cherian S. Antiviral perspectives for chikungunya virus. Biomed. Res. Int. 2014;2014:631642. doi: 10.1155/2014/631642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parola P., de Lamballerie X., Jourdan J., Rovery C., Vaillant V., Minodier P., Brouqui P., Flahault A., Raoult D., Charrel R.N. Novel chikungunya virus variant in travelers returning from Indian Ocean islands. Emerg. Infect. Dis. 2006;12:1493–1499. doi: 10.3201/eid1210.060610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezza G., Nicoletti L., Angelini R., Romi R., Finarelli A.C., Panning M., Cordioli P., Fortuna C., Boros S., Magurano F., Silvi G., Angelini P., Dottori M., Ciufolini M.G., Majori G.C., Cassone A., group, C.s. Infection with chikungunya virus in Italy: an outbreak in a temperate region. Lancet. 2007;370:1840–1846. doi: 10.1016/S0140-6736(07)61779-6. [DOI] [PubMed] [Google Scholar]
- Rossignol J.F. Nitazoxanide: a first-in-class broad-spectrum antiviral agent. Antivir. Res. 2014;110:94–103. doi: 10.1016/j.antiviral.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossignol J.F., La Frazia S., Chiappa L., Ciucci A., Santoro M.G. Thiazolides, a new class of anti-influenza molecules targeting viral hemagglutinin at the post-translational level. J. Biol. Chem. 2009;284:29798–29808. doi: 10.1074/jbc.M109.029470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sane J., Kurkela S., Levanov L., Nikkari S., Vaheri A., Vapalahti O. Development and evaluation of a real-time RT-PCR assay for Sindbis virus detection. J. Virol. Methods. 2012;179:185–188. doi: 10.1016/j.jviromet.2011.10.021. [DOI] [PubMed] [Google Scholar]
- Schwartz O., Albert M.L. Biology and pathogenesis of chikungunya virus. Nat. Rev. Microbiol. 2010;8:491–500. doi: 10.1038/nrmicro2368. [DOI] [PubMed] [Google Scholar]
- Shi Z., Wei J., Deng X., Li S., Qiu Y., Shao D., Li B., Zhang K., Xue F., Wang X., Ma Z. Nitazoxanide inhibits the replication of Japanese encephalitis virus in cultured cells and in a mouse model. Virol. J. 2014;11:10. doi: 10.1186/1743-422X-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staples J.E., Breiman R.F., Powers A.M. Chikungunya fever: an epidemiological review of a re-emerging infectious disease. Clin. Infect. Dis. 2009;49:942–948. doi: 10.1086/605496. [DOI] [PubMed] [Google Scholar]
- van Duijl-Richter M.K., Hoornweg T.E., Rodenhuis-Zybert I.A., Smit J.M. Early events in chikungunya virus infection-from virus cell binding to membrane fusion. Viruses. 2015;7:3647–3674. doi: 10.3390/v7072792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voss J.E., Vaney M.C., Duquerroy S., Vonrhein C., Girard-Blanc C., Crublet E., Thompson A., Bricogne G., Rey F.A. Glycoprotein organization of Chikungunya virus particles revealed by X-ray crystallography. Nature. 2010;468:709–712. doi: 10.1038/nature09555. [DOI] [PubMed] [Google Scholar]
- Weaver S.C., Forrester N.L. Chikungunya: evolutionary history and recent epidemic spread. Antivir. Res. 2015;120:32–39. doi: 10.1016/j.antiviral.2015.04.016. [DOI] [PubMed] [Google Scholar]
- Weaver S.C., Lecuit M. Chikungunya virus and the global spread of a mosquito-borne disease. N. Engl. J. Med. 2015;372:1231–1239. doi: 10.1056/NEJMra1406035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.