Abstract
Although considerable progress has been made in improving the blood service system in China over the last 2 decades, many challenges remain. A number of issues have received public attentions; however, others continue to be underacknowledged and controversial. This article describes 3 of these important and less emphasized issues: first, the ambiguity of the definition of voluntary nonremunerated blood donation and its relationship to an adequate blood supply; second, the current inadequacies of cost recovery from the blood service system; and third, the lack of a universally implemented program of hemovigilance. Currently, there is controversy regarding these challenges. Open recognition and discussion offers the prospect of bringing solutions closer to reality.
Keywords: Donor motivation, Cost recovery, Cost assessment, Hemovigilance
Highlights
-
•
Current annual blood donations in China have not kept pace with growing demand.
-
•
Blood donor motivation is based on a system that is not entirely altruistic or entirely incentive based.
-
•
Financial reimbursement systems for blood centers in China have not kept pace with the cost of technical advancements.
-
•
A nationwide hemovigilance system in China has yet to be established.
Until the 1990s, the blood supply in China was based on donations from voluntary nonremunerated blood donors (VNRBDs), paid blood donors, family replacement donors, and an in-between type called employer-organized donors [1]. In 1998, China enacted the Blood Donation Law, prohibiting paid donation. By 2011, the proportion of all blood donations from VNRBD was reported to be 100%, up from slightly greater than 5% in 1988. During the same period, the total volume of blood collected annually increased 4-fold, from less than 5 million units to more than 20 million units [2]. In 2015, the total number of units donated in China exceeded 22 million [3]. By the end of the year, routine nucleic acid testing of all donations for major transfusion transmissible viruses was fully implemented [3].
Progress has not only been made in the quantity of blood donated and the proportion of donations obtained by VNRBD, but also in blood collection–based legislation and regulation. The infrastructure of blood services has become more coordinated and consolidated, and performance has improved. In China, there are 3 types of facilities exclusively collecting blood and supplying hospitals in their localities. According to their range of functions undertaken and services provided, administration level, and locality, blood establishments are categorized as provincial blood centers, prefectural regional blood banks, or small county blood banks usually located in remote areas. All blood establishments are public, independent of each other, and under the supervision of local government and health authorities. There were approximately 430 blood establishments in 2015, the number being half that present in the year 2000. Improvements in both the number of blood donations collected each year and in overall geographic coverage in the collection program indicate that the overall accessibility of blood service provision in China has improved.
Despite 15 years of achievement, there are still many challenges facing blood services in China. There are some long-existing problems that are well recognized, such as the unmet clinical demand for blood despite increasing blood donation rates and the high prevalence of transfusion-transmitted viral infections in the general population [2], [4], [5], [6]. This article focuses on 3 additional challenges that have received less attention: the sustainability of voluntary donations, blood service cost assessment and recovery, and systematic and objective evaluation of blood service safety. These challenges center on the determinants for sustainable motivation of blood donors, the means to financially secure the operation of blood establishments, and the implementation of systematic methods to improve the quality and safety of the entire blood service. Understanding these issues is important to gain a better understanding of China's current blood collection service, predict future trends, and plan a long-term strategy for sustainable and affordable blood services that can adequately meet clinical needs.
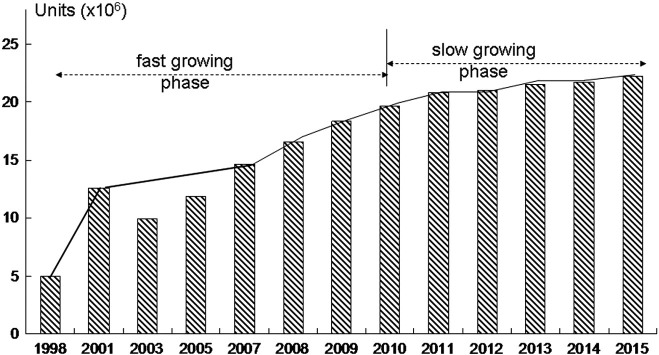
Defining Voluntary Nonremunerated Blood Donation
When the Blood Donation Law was put into effect in October 1998 [7], the total number of units donated that calendar year barely reached 5 million, or 4 units per 1000 population. Annual donations reached 12.6 million in 2001, more than a 3-fold increase in less than 3 years, with an average rate of increase of 51% as shown in Figure 1 [2], [8]. Despite the negative impact of severe acute respiratory syndrome on blood donations and transfusions in 2003, and the slow recovery in the following year, overall donations continued to increase by more than 10% during the next 5 years. This phase of rapid growth in donations ended in 2010. In the years since, units obtained by donation have remained relatively constant, but the rate of annual increase has fallen sharply, down to 1% to 2.4% since 2012.
Fig. 1.
Annual blood donations in China (1998-2015). The pattern of donations shows an initial fast-growth phase followed by a plateau phase, a pattern believed to consistent with an incentive-based system for blood collections. See Figure 2.
Although insufficient supply of blood challenges many countries, the situation in China is particularly concerning. The World Health Organization estimates that a gross donation rate of no less than 1% to 3% of a population is required to meet their basic clinical transfusion demands [9]. However, the donation rate in China was barely 1% in 2015. Given the already low donation rate and the slow growth rate, the number of available blood units must continue to increase by at least 10% to meet the increasing demand for blood. According to the Year Books of Chinese Health released by the National Health and Family Planning Commission (equivalent to a Ministry of Health in other nations), the number of inpatient admissions to hospitals has been increasing at an annual rate of 11.48% or more since 2008 [2]. There is no doubt that the most urgent priority for blood services is to motivate new potential donors and to stimulate those who have historically donated to continue to donate on a regular basis. At the same time, researchers, policy makers, and practitioners of blood service society need to understand the underlying cause of the current slow rate of growth in annual blood collections.
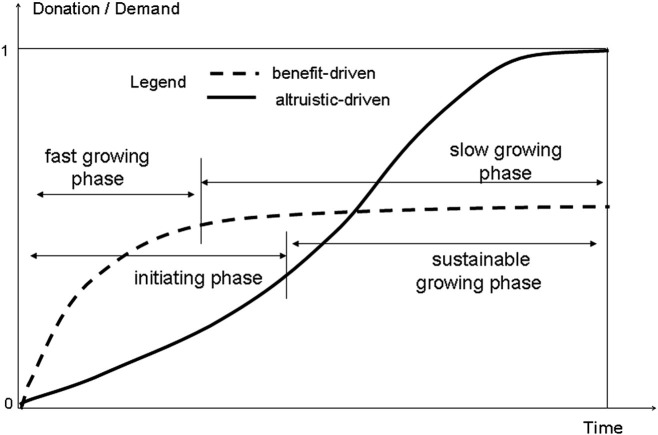
Since the World Health Assembly released its resolution WHA 28.72 in 1975, which calls for member states to promote the development of national blood services based on VNRBD, this altruistically motivated form of donation has been proven to be the cornerstone for both safety and adequacy of blood supply globally (WHA Resolution 58.13, 2005) [10]. The World Health Organization defines VNRBD as a donation in which “a person gives blood, plasma, or cellular components of his/her own free will and receives no payment for it, either in the form of cash, or in kind which could be considered a substitute for money. This would include time off work other than that reasonably needed for the donation and travel. Small tokens, refreshments, and reimbursements of direct travel costs are compatible with voluntary non-remunerated donation” [11]. This definition has been adopted by almost all international organizations devoted to transfusion medicine and by most of national authorities. With this principle, donors do not receive direct benefits or repayment for blood donation in monetary form or its substitutes; the motivation is altruistic. Because of the deeply rooted traditional belief in the personal value of blood to one's own health, the general public in China does not intrinsically see benefit in taking time and effort to donate blood for unknown others without personal return. As a result, it was predictable that implementation of a system of blood donation based on altruistic motivation in China would result in an initial slow growth phase. It takes considerable effort to disseminate information on the importance of blood donation and transfusion and to build a case for altruistic donation practices. Once people have accepted the altruistic principle and become donors, naturally there will be high chances that they will remain regular donors. With more people accepting the altruistic principle, blood collection is expected to enter a sustainable growth phase with a steady increase in the number of blood donations. The authors believe this 2 phase growth pattern to be inevitable: a slowly growing initial phase followed by a sustainable growing phase. Time is also needed for blood services to become more efficient, and to eliminate spurious altruism or nonmonetary forms of compensation, which harm efforts to increase altruistic and voluntary donation [12]. In the long term, as has been proven globally, altruistic blood donation is expected to meet the demands of hospitals and patients. In contrast, blood donation based on personal incentives may be less sustainable and studies have suggested that personal incentives may reduce the number of blood donors in the long term [13], [14]. The anticipated effects of a blood donation system based on either altruistic motivation or on motivation by personal incentives are illustrated in Figure 2 .
Fig. 2.
Two theories of blood donation rates based on motivations. The solid line represents donations over time in a system based on altruistic motivation for donation. It begins with a gradually increasing phase when volunteer nonremunerated blood donations are implemented. With greater adoption of the principle, it leads to a sustainable development phase. Eventually, the rate of donations will reach or exceed demand and the growth rate will plateau. The dotted line represents donations based on an incentive system. Personal benefits or monetary incentives are strong and direct forces. There is a very fast initial growth phase. These driving forces may not have a sustained effect, however, and over time, the donation rate will flatten or decline. It is not possible for this theoretical example for the incentive-based system to recruit sufficient donors to meet demand.
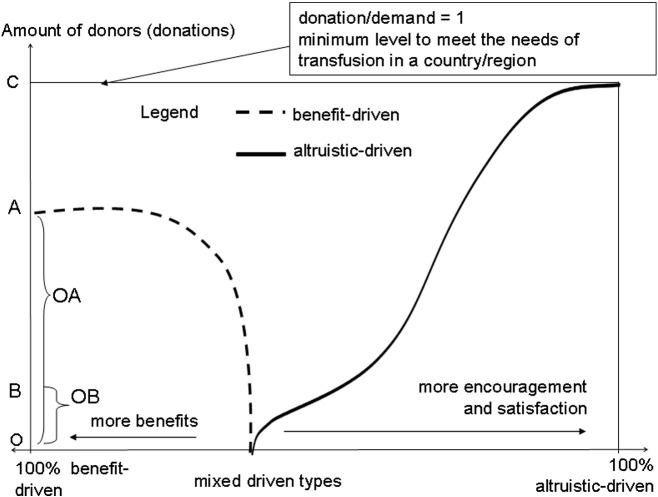
The Blood Donation Law of China accepts and provides for the existence of VNRBD, but it does not adhere to its specific and rigorous definition. The Law banned monetary compensations (previously termed “nutrition fees”) to donors by either the agencies collecting the blood or the patients receiving blood transfusion. The Blood Donation Law does allow some form of compensation for donors, however, in exchange for donation. For example, the law ensures that the donors, their spouses, and their immediate family members can receive blood transfusion at no cost. In cases where blood is in a short supply, donors and their families may be prioritized to receive blood that is available should they require transfusion. These privileges are referred to as the “Give Blood Voluntarily and Use Blood for Free” provision. The amount of blood that one shall donate to receive these benefits differs by regional regulations. In some places, a single unit donated enables the donor unlimited free transfusions throughout their lifetime. The waived costs are borne by the blood service facility that collected their blood originally. As shown in Figure 1, the rate of donation increased substantially over the initial 12 years of implementation, but has since slowed substantially. This trend is consistent with the biphasic trajectory of the benefit-driven mode of blood donation depicted with the predications by the authors as shown in Fig. 2, Fig. 3 .
Fig. 3.
Hypothetic model of the effects of 2 different models of blood donor motivation. The number of donations or donors is shown on the y-axis and time is indicated on the x-axis. Point C indicates the level of donations required to meet demand. Point A indicates the initial level of donors or donations in an incentive-based donor system. Under the assumption that the incentive-based system is not sustainable, donation rates decline (dotted line). Point B indicates the initial portion of donors who may accept altruistic principles and become volunteer non-remunerated donors. An incentive-based (benefit-driven) program may show a successful initial phase, but may fail to reach demands, and may ultimately delay the growth of altruistic donors.
The current motto of voluntary donation in China, Give Blood Voluntarily and Use Blood for Free, has proven to be a great leap forward. It has led to the eradication of paid donation, while increasing donations 4-fold in less than 13 years (1998-2011). However, the free transfusions obtained in exchange by donations represent personal benefits and thus are inconsistent with the altruistic principles of VNRBD. It is apparent, by both theoretical analysis and the very real stagnation of blood donations China currently faces, that the Give Blood Voluntarily and Use Blood for Free model is not sustainable. The ability to provide sufficient blood will become increasingly constrained and will not keep pace with increasing demand for blood. The consequent impact on health services will be visible more often, from cases of surgery cancellations to the restriction on the overall development of health care system.
When considering solutions to China's current inadequate blood supply, many authorities and practitioners propose more direct incentives to encourage greater donor participation. Proposed benefits include quicker reimbursement for the costs of free transfusions prepaid by patients and extending the policy coverage of one donation for lifelong unlimited free transfusions [15], [16], [17]. It is not clear yet whether these proposals will bring in more donors, or whether any long-term increases in donation will be seen. Additional incentives will create a substantial new fiscal commitment by blood establishments that cannot be honored without a proportional commitment from Health authorities. Increasing the effectiveness of VNRBD requires disseminating the right messages, building cultural consciousness and societal awareness around voluntary donation, and eliminating any pretense that a donation system based on direct personal benefit is a viable strategy for meeting China's long-term blood unit needs [17], [18].
Cost Assessment and Recovery
Cost recovery could be the greatest challenge to maintaining a functioning blood collection system. Currently, blood collecting and processing facilities in China are financed through the revenues from the services they offer, although some local governments allocate partial subsidies from their annual budgets. Occasionally, higher government departments may provide funding for specific purposes, but neither these nor the local government subsidies should be counted on for routine revenue or to cover substantial expenditures. Donations from industry or individuals are negligible in China. One of the direct consequences of restricted resources has been the inability to hire qualified staff in sufficient numbers with competitive salaries. Continued inadequacies of financing will inevitably constrain the ability of blood collecting and processing facilities to maintain their services, let alone improve their performance.
In China, revenues for blood service establishments almost entirely come from hospitals, referred to as cost recovery. By law, costs may only be recovered for blood collection, storage, screening, and component separation. Costs for these services are nationally fixed, last set in 2006. There has never been any official statement as why only these 4 services are reimbursable, nor how these reimbursement costs have been assessed nationwide. There is also no instruction regarding how any other costs are to be assessed or recovered. It is generally assumed that local governments shall be responsible for these, which in practice makes cost recovery dependent on the financial capacity and political will of local authorities. In reality, some blood collection and processing facilities cannot balance their income with actual expenditures, despite subsidies and substantial efforts to contain costs [19], [20], [21].
On September 11, 2012, the Committee of Blood Establishment Management of the Chinese Society of Blood Transfusion (CSBT) reported the results of a survey at its annual meeting in Haerbing, China. The survey collected data on operations and services in 2011 from 174 blood establishments across the country. According to this report, for many blood establishments, funding received for provision of services was significantly less than the cost of providing them. For example, a blood service facility bears a net loss of 52.33 RMB (US $8.18) when collecting and supplying a standard unit (200 mL) of whole blood, or the packed red cells and plasma separated from it (Table 1 ).
Table 1.
Average income and cost for a standard of whole blood or components from it
| Revenue | Government subsidy | Total income | Total cost | Net income | |
|---|---|---|---|---|---|
| RMB | 250 | 98.60 | 348.6 | 400.93 | −52.33 |
| US$a | 39.06 | 15.41 | 54.47 | 62.65 | −8.18 |
Calculated with the rough annual average rate of exchange of 6.4 in 2011.
In China, whole blood donations can be made either for 200 or 400 mL, as defined by the Blood Donation Law. Although the 200-mL collection volume is not favored by blood collection agencies, until the law is amended, the collection volume remains the decision of the donor. When a donation is made for a double unit (400 mL), the revenues to be collected will be doubled too. More double-unit donations will also save indirect expenses that cannot be attributed to a specific unit of blood, such as the expense of public education and donor recruitment, as well as fixed running costs such as human resource, electricity, water, and so on. Among the 174 institutions that participated in the survey, 38% of the blood collected was in double units. This may partially explain how a blood service could remain functional in spite of an unbalanced financial sheet. Another explanation was the significant indebtedness of these institutions. The survey indicated an average debt-to-fixed assets ratio of 21%, ranging from 0 to 180%, which was equivalent to an average debt of RMB 71400 (US $11156) per employee. It should be noted that debts are not allowed for government-sponsored establishments in China. These debts and increasing financial burden threaten the viability of organizations providing vital blood services. It could be a significant concern if these establishments are suddenly required to pay off these debts.
The way that cost recovery standards were set with payments lower than real costs likely reflects the expectation that local governments would provide subsidies to affiliated blood establishments. Nevertheless, subsidies are not mandated, being left to local decisions and fiscal capacities. By law, blood service establishments are required to deposit all revenues to designated government-supervised accounts. As for the expenditures, they should have their budgets approved first by supervising agencies of the government. After budget approval, the actual expenses can be reimbursed from the deposited revenues. Governments may add subsidies if the amount of depositions cannot balance the approved expenses. The survey showed that two-thirds of the institutions that participated in the survey were permitted to use up all revenues they collected, and some were granted subsidies from local governments. However, for one-third of institutions, only 70% to 85% of revenues were returned to cover costs. The balance of funds was retained in the accounts under supervision. In these cases, no local subsidies will be given under normal conditions.
A blood service will not remain viable under such unfavorable financial conditions as suppressed budget, incomplete reimbursement of costs, and insufficient subsidies. The natural consequence is that the capacity to plan for quality and service improvement is very limited. The implementation of nuclear acid testing is a practical example of how new screening assays could be impaired if real costs cannot be properly assessed and covered. Although nuclear acid testing pilot studies were conducted in China as early as in 2002, it took 9 years before its adoption in some developed regions on the eastern coast in 2011 [22]. Nationwide adoption was achieved at the end of 2015, nearly 12 years behind the United States. In comparison, the HIV and HCV antibody tests were adopted in 1992 in eastern coast regions, only 7 and 2 years behind the very first assays adopted in the developed world. The entire country followed the leading institutions and made these 2 antibody tests routine in 1993. At that time, costs were being fully recovered based on local assessments.
Hemovigilance and Decision-Making Processes
Cash payment to blood donors has been banned since the enforcement of the Donation Law, the proportion of VNRBD has increased, and collection and supply have increased several fold. The logical expectation is that this progress should have been accompanied by improvements in blood safety and the capacity to meet clinical demand. To monitor, evaluate, and continuously improve blood supply adequacy and safety, it is important to collect relevant data through standardized and systemic data collection and reporting. Such tools, usually referred to as either hemovigilance or biovigilance, have been applied in China since 2003; however, no national or local data are generally available.
Despite the wide recognition of the importance of a hemovigilance system, there is hesitation as to whether it is the right time to implement a hemovigilance program in China. A major concern for implementing such a plan is that, given the deteriorating status of the doctor-patient relationship and violence against health care workers at present in China [23], the self-revelations of originally unknown events and the investigation of their causes may precipitate more violence and penalties. It may be worth undertaking some pilot hemovigilance studies that may facilitate evidence-based decision making on key issues such as the effectiveness of donor history questionnaires [24], the justified needs and cost-effectiveness of alanine transaminase and novel marker testing (eg, human T-cell lymphotropic virus) [25], [26], and strategies for donor reentry [27]. In addition, any implementation of hemovigilance will require a decision on whether hemovigilance reporting should be voluntary or required.
Despite unfavorable conditions and mounting concerns, advances have been made through individual efforts, and preliminary studies have been published. In 2013, the Blood Quality Management Committee of the Chinese Society of Blood Transfusion released the Guideline on Hemovigilance, since revised in 2015 [28]. For blood establishments and hospitals looking for help with setting up new plans or further improving existing plans, the guideline provides ample information on definitions, methodologies, and documentation protocols.
Conclusion
Blood safety and availability in China has significantly improved since the Blood Donation Law came into effect in October 1998. The central health authority expects to reach a donor/population rate of 1.5% by 2020, an ambitious increase of 50% over the next 5 years. Challenges are likely to be encountered, particularly related to meeting ever-increasing clinical demands for blood products while maintaining the safety, integrity, and sustainability of the service. Most of these challenges are already being addressed, including but not limited to inappropriate blood utilization [29], the high prevalence of transfusion-transmitted infections [30], restrictions on eligible donation ages and intervals, regional differences in development, and isolated information management systems. There are other challenges, however, that are not linked directly to any specific issues, but that are of more strategic significance and have greater long-term implications. Identifying and resolving these challenges will lay the groundwork for an effective and reliable blood service system.
This article has identified a number of concerns facing the blood services industry in China that have thus far received inadequate attention. First, the amount of blood donated annually has not kept pace with demand. Second, blood services are being impaired by cost-assessment standards that were inadequate from the very beginning. Third and finally, there is not enough performance measurement in the blood collection and processing system. A number of questions on these issues remain: shall the current mode of donation motivation remain driven by personal incentives, or would it be appropriate to embrace a major change and reaffirm the original principle of VNRBD? Shall blood establishments remain fiscally squeezed, or will cost recovery and government subsides be reassessed and revised regularly? Is it time to implement hemovigilance programs, and if so, shall they be made mandatory or voluntary? The authors believe that highlighting such matters is of primary importance for a sustainable blood program in China.
Acknowledgment
We thank Heather Harker Ryan, MS, RN (lecturer in the Department of Nursing at University of Massachusetts Boston), for editing the manuscript.
Footnotes
Conflict of interest: None.
References
- 1.Tison G.H., Liu C., Ren F., Nelson K., Shan H. Influences of general and traditional Chinese beliefs on the decision to donate blood among employer organized and volunteer donors in Beijing, China. Transfusion. 2007;47:1871–1879. doi: 10.1111/j.1537-2995.2007.01410.x. [DOI] [PubMed] [Google Scholar]
- 2.Yin Y., Li C., Liu Z. Blood donation in China: sustaining efforts and challenges in achieving safety and availability. Transfusion. 2015;55(10):2523–2530. doi: 10.1111/trf.13130. [DOI] [PubMed] [Google Scholar]
- 3.News release of National Health and Family Planning Commission of PRC, 2/24/2016. Available at: http://www.nhfpc.gov.cn/xcs/s3578/201602/1be8bf864c1e455fa99ac34c2dc2b4e4.shtml
- 4.Shi L., Wang J.X., Stevens L., Ness P., Shan H. Blood safety and availability: continuing challenges in China's blood banking system. Transfusion. 2013;54(2):471–482. doi: 10.1111/trf.12273. [DOI] [PubMed] [Google Scholar]
- 5.Yu X., Chen W., Liu Z., Huang Y. Safety and current status of blood transfusion in China: an update. Lancet Haematol. 2016;3(2):e60–e62. doi: 10.1016/S2352-3026(16)00010-7. [DOI] [PubMed] [Google Scholar]
- 6.Shi L., Wang J., Liu Z., Stevens L., Sadler A., Ness P. Blood donor management in China. Transfus Med Hemother. 2014;41(4):273–282. doi: 10.1159/000365425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Standing Committee of the National People's Congress Blood Donation Law. 1997. http://www.npc.gov.cn/wxzl/wxzl/2000-12/05/content_4698.htm
- 8.2011. Report of Medical Administration Dept. MoH. National Conference on Blood Safety. [Haerbin] [Google Scholar]
- 9.World Health Organization. WHO global database of blood safety summary report 2008. 2008. Available at: http://www.who.int/bloodsafety/global_database/GDBS_Summary_Report_2008.pdf
- 10.World Health Organization. WHA58.13. Blood safety: proposal to establish World Blood Donor Day. 2005. Available at: http://www.who.int/worldblooddonorday/resources/WHA58_13-en.pdf?ua=1
- 11.WHO Expert Group. Expert consensus statement on achieving self-sufficiency in safe blood and blood products, based on voluntary non-remunerated blood donation (VNRBD). 2012. Available at: http://www.who.int/bloodsafety/Expert_Consensus_Statement_Self-Sufficiency.pdf?ua=1 [DOI] [PubMed]
- 12.Fernández-Montoya A. Altruism and payment in blood donation. Transfus Sci. 1997;18(3):379–386. doi: 10.1016/S0955-3886(97)00026-X. [DOI] [PubMed] [Google Scholar]
- 13.Abolghasemi H., Hosseini-Divkalayi N.S., Seighali F. Blood donor incentives: a step forward or backward. Asian J Transfus Sci. 2010;4(1):9–13. doi: 10.4103/0973-6247.59385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kasraian L., Maghsudlu M. Blood donors' attitudes towards incentives: influence on motivation to donate. Blood Transfus. 2012;10(2):186–190. doi: 10.2450/2011.0039-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li H. To implement the policy of using blood for free by increasing government investment. J Clin Transfus Lab Med. 2007;9(2):172–173. [In Chinese] [Google Scholar]
- 16.Gao Y., An W., Liang X., Wang N., Meng Q., Bi M. Investigation and analysis of the reimbursement for blood donors in 357 blood banks nationwide. Inter J Blood Transfus Haematol. 2013;36(5):401–402. [In Chinese] [Google Scholar]
- 17.Tao H., Guo S. Analysis of the factors affecting voluntary blood donation. Chin J Pub Health. 2008;24(1):90–91. [In Chinese] [Google Scholar]
- 18.Meng Y., Zhu Y. Voluntary non-remunerate blood donation is the base of blood safety. Chin J Blood Transfus. 2014;27(5):566–568. [In Chinese] [Google Scholar]
- 19.Shun M. Costs of blood transfusion ought be assessed. Health News. 2011;P2 [ http://www.iiyi.com/d-09-14002.html. In Chinese] [Google Scholar]
- 20.Liu K., Shi R., Zhang Z. Discussion on voluntary blood donation and the fee of clinical use of blood. Chin Health Econ. 2004;23(9):28. [In Chinese] [Google Scholar]
- 21.Zhao T. Analysis of current status of blood charging. Chin Med Herald. 2011;08(6):111–112. [In Chinese] [Google Scholar]
- 22.Zou Z., Zhou G., Zhu Y. Implementation of centralized blood screening in blood stations and reflection. Chin J Blood Transfus. 2014;27(11):1085–1087. [In Chinese] [Google Scholar]
- 23.Editorial. Violence against doctors: why China? Why now? What next?Lancet. 2014;383(9922):1013. doi: 10.1016/S0140-6736(14)60501-8. [DOI] [PubMed] [Google Scholar]
- 24.Meng Y., Xie D., Shen Y., Zhu Y. Having a correct recognition and practice of blood history questionnaire. Chin J Blood Transfus. 2014;27(7):797–799. [In Chinese] [Google Scholar]
- 25.Xie J., Ge S., Zhang Y., Lin Y., Ni H., Zhang J. Prevalence of HTLV among blood donors in Southeast China, 2004-2013. PLoS Negl Trop Dis. 2015;9(4):e3685. doi: 10.1371/journal.pntd.0003685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ren F.R., Wang J.X., Huang Y., Yao F.Z., Lv Y.L., Li J.L. HBV NAT in Chinese blood donors with normal and elevated ALT. Transfusion. 2011;51:2588–2595. doi: 10.1111/j.1537-2995.2011.03215.x. [DOI] [PubMed] [Google Scholar]
- 27.Zhou G., Xie Y., Wang X., Ren Y., Zhu Y. Obligatory blood services in conducting re-entry of blood donors with false-reactive results. Chin J Blood Transfus. 2014;27(10):1079–1082. [In Chinese] [Google Scholar]
- 28.The Blood Quality Management Committee Chinese Society of Blood Transfusion. Guideline on Haemovigilance, 2nd edition. http://download.sbc.org.cn/column/xuezhiwei/download.php?dw_filename=20151027-3.pdf Released on 2015–10-21. Available at:
- 29.Yu X., Pang H., Xu Z., Yan H., Xu L., Du J. Multicentre evaluation of perioperative red blood cells transfusion in China. Br J Anaesth. 2014;113:1055–1056. doi: 10.1093/bja/aeu392. [DOI] [PubMed] [Google Scholar]
- 30.Wang J., Liu J., Yao F., Wen G., Li J., Huang Y. Prevalence, incidence, and residual risks for tr-HIV1+ 2 among Chinese blood donors. Transfusion. 2013;53:1240–1249. doi: 10.1111/j.1537-2995.2012.03940.x. [DOI] [PMC free article] [PubMed] [Google Scholar]