Abstract
This study aimed to identify optimal high-temperature indices to predict risks of all-cause mortality and outpatient visits for subtropical islanders in warm seasons (May to October). Eight high-temperature indices, including three single measurements (average, maximum and minimum temperature) and five composite indices (heat index, humidex, temperature humidity index, apparent temperature and wet-bulb globe temperature), and their standardized Z scores, were used in distributed lag non-linear models. Cumulative 8-day (lag zero to seven days) relative risks (RRs) and 95% confidence intervals were estimated, 1 and 2 standardized deviations above the medium (i.e., at 84.1th and 97.7th percentile, respectively), by comparing with Z scores for the lowest risks of mortality and outpatient visits as references. Analyses were performed for Taipei in north, Central Taiwan and Southern Taiwan. Results showed that standardized Z-values of high-temperature indices associated with the lowest health risk were approximately 0 in Taipei and Central Taiwan, and − 1 in Southern Taiwan. As the apparent temperature was at Z = 2, the cumulative 8-day mortality risk increased significantly, by 23% in Taipei and 28% in Southern Taiwan, but not in Central Taiwan. The maximum temperature displayed consistently a high correlation with all-cause outpatient visits at Z = 1; with the cumulative 8-day RRs for outpatient visits increased by 7%, 3%, and 4% in the three corresponding areas. In conclusion, this study has demonstrated methods to compare multiple high-temperature indices associated with all-cause mortality and outpatient visits for population residing in a subtropical island. Apparent temperature is an optimal indicator for predicting all-cause mortality risk, and maximum temperature is recommended to associate with outpatient visits. The impact of heat varied with study areas, evaluated health outcomes, and high-temperature indices. The increased extreme heat is associated with stronger risk for all-cause mortality than for outpatient visits.
Abbreviations: AIC, Akaike's information criterion; AT, apparent temperature; CI, confidence interval; CWB, Central Weather Bureau; DLNM, distributed lag non-linear model; Flu, influenza; HI, heat index; NHRI, National Health Research Institute; PM10, particulate matter less than 10 μm in aerodynamic diameter; RR, relative risk; RH, relative humidity; TCDC, Taiwan Centers for Disease Control; THI, temperature humidity index; TEPA, Taiwan Environmental Protection Administration; WBGT, wet-bulb globe temperature; WS, wind speed; WVP, water vapor pressure
Keywords: High-temperature indices, Mortality, Outpatient visits, Standardization, Taiwan
Highlights
► Apparent temperature was the optimal high-temperature index in temperature–all-cause mortality study. ► Maximum temperature was the optimal high-temperature index in temperature–all-cause outpatient visits study. ► Extreme heat is associated with stronger risk for all-cause mortality than for outpatient visits.
1. Introduction
The association between temperature and mortality has been depicted with U-, V-, or J-shaped curves among various climate regions (Curriero et al., 2002, Gouveia et al., 2003, McMichael et al., 2008). The climate in recent decades is characterized with increased frequency and intensity of extreme temperatures (Meehl and Tebaldi, 2004). Health effects of global warming are now considered a critical issue (Anderson and Bell, 2011, Kovats and Hajat, 2008, Kovats and Kristie, 2006, O'Neill and Ebi, 2009). Most studies used ambient temperatures (i.e., average, maximum, and minimum temperature) to evaluate heat-related health effects (Hajat et al., 2010, Kim et al., 2006, Knowlton et al., 2007, Kovats et al., 2004, Lin et al., 2011, Yu et al., 2010, Wang et al., 2012). However, other weather indicators, such as relative humidity (RH), wind speed (WS), water vapor pressure (WVP) and thermal radiation, also affect the perception of temperature to humans. Several composite indices, including heat index (HI) (Hartz et al., 2012, Metzger et al., 2009), apparent temperature (AT) (Anderson and Bell, 2009, Chung et al., 2009), humidex (Smoyer-Tomic and Rainham, 2001) and wet-bulb globe temperature (WBGT) (Epstein and Moran, 2006, Kjellstrom et al., 2009), have been used to evaluate health events associated with heat waves or extremely high temperatures.
Various high-temperature indices and approaches have been used to assess the association between mortality and heat waves or high temperature. But, no study has determined which index is optimal to predict mortality (Hajat et al., 2010, Vaneckova et al., 2011, Yu et al., 2011). Anderson et al. have indicated that, after adjusting for humidity, the temperature–mortality associations are not significantly different among using average, maximum and apparent temperature metrics (Anderson and Bell, 2009). Barnett et al. (2010) suggested that no temperature index can be considered optimal because all indices are highly correlated with temperature measurements. The applied temperature measurement should be chosen according to practical concerns, i.e. the measure may provide comprehensive information (Barnett et al., 2010). Thus, studies addressing the determination of an optimal high-temperature index to predict health outcomes were still far from being conclusive.
Most studies on the high temperature (i.e., heat wave) impact focus on mortality, and only some consider morbidity (Kovats and Hajat, 2008, Ye et al., 2012). Moreover, most studies on heat effects are performed in areas with temperate climate rather than subtropical climate (Basu, 2009, Kovats and Kristie, 2006, Ye et al., 2012). Therefore, the present study was to report high-temperature indices optimal to evaluate the all-cause mortality and outpatient visits associated with temperatures in Taiwan, a subtropical island, located on the west of the Pacific Ocean. We evaluated models among eight standardized high-temperature indices: average, maximum, and minimum temperature, HI, temperature humidity index (THI), humidex, AT, and WBGT. Relative risks of all-cause mortality and outpatient visits associated with these indices were evaluated for three areas, Taipei in the north, Central Taiwan and Southern Taiwan.
2. Materials and methods
2.1. Data sources
Data used in this study included vital statistics obtained from the Department of Health (DOH), universal health insurance claims data from the National Health Research Institute (NHRI), daily meteorological data from the Central Weather Bureau (CWB), and daily air pollution monitoring data from the Taiwan Environmental Protection Administration (TEPA), all from 2000 to 2008. Data representative for population structure, climate and air pollution in Taiwan were collected from three major metropolitan areas: Taipei, Central Taiwan (Taichung, Zhanghua and Nantou), and Southern Taiwan (Kaohsiung and Pingtung), comprising 63.7% of the total 23 million population in Taiwan.
Daily area-specific all-cause deaths (ICD9 codes 000–999) were retrieved from the vital statistics dataset with underlying cause of death coded with the 9th revision of International Classification of Diseases (ICD-9). The NHRI has established a cohort of one million residents to represent all insured residents in Taiwan with their electronic reimbursement claim records accessible for research purposes. Disease diagnoses were coded with the 9th revision of International Classification of Diseases with Clinical Modification (ICD-9-CM). Daily area-specific all-cause outpatient visits (ICD9 CM 000–999) were retrieved from the electronic records.
CWB provided 24-hour data from 25 real-time weather monitoring stations in Taiwan Central Weather Bureau (2011). Weather conditions measured using three stations in Taipei, four stations in Central Taiwan and four stations in Southern Taiwan were available for determining daily mean, maximum, and minimum temperatures, RH, dew point temperature, WVP, and WS. The TEPA established Air Quality Monitoring Network in 1993 with 74 stationary monitoring stations throughout the island (Taiwan Environmental Protection Administration, 2011, Taiwan Governmental Information Office, 2008). Concentrations of ambient air pollutants, including particulate matter smaller than 10 μm in aerodynamic diameter (PM10), nitrogen dioxides (NO2) and ozone (O3), were measured and recorded hourly at each station. We analyzed daily levels of PM10, O3, and NO2, monitored by 14, 10 and 13 general ambient environment stations in Taipei, Central Taiwan, and Southern Taiwan, respectively. Locations of the weather and ambient environment stations are shown in Fig. 1 .
Fig. 1.
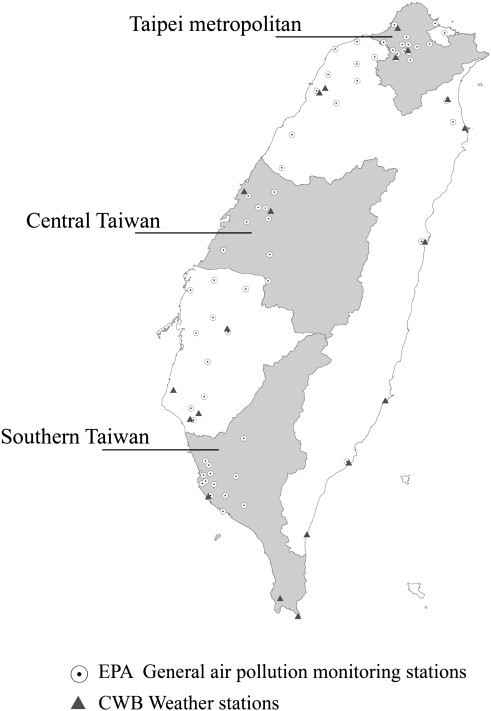
Locations of general air monitoring stations and weather stations in Taipei, Central Taiwan and Southern Taiwan.
2.2. High-temperature indices
The eight high-temperature indices used in this study including single temperature measurements and composite temperature indices that have been widely used in heat–health association studies are detailed in Table 1 . Briefly, average, maximum, and minimum temperatures were monitored hourly at the regional representative weather stations. The HI based on dry bulb temperature and RH was used in environments with temperatures above 80 °F (26.7 °C) and with RH above 40% (Steadman, 1979). The humidex developed by Environment Canada was used as the measure of subjectively perceived temperature and humidity (Masterton and Richardson, 1979). To assess the temperature perception in study population (Rosenberg et al., 1983), we used the Taiwan CWB adopted THI index. It is similar to the thermal discomfort index developed by the U.S. Weather Bureau, widely used in Europe as well to assess heat discomfort (Pantavou et al., 2011). The AT was used as an alternative measure of perceived temperature, which combines several environmental and physiological variables, including temperature, clothing cover, physical activity, WS and WVP (Steadman, 1984). The WBGT developed by the American Conference of Governmental Industrial Hygienists was used to estimate heat stress in the working environment.
Table 1.
Composite high-temperature indices summarized for the study.
| Index name | Abbreviation | Variables used | Equation/definition |
|---|---|---|---|
| Daily average temperature | Tavg. | Air temperature (°C) | Daily 24 h average |
| Daily maximum temperature | Tmax. | Air temperature (°C) | The maximum hourly temperature in a day |
| Daily minimum temperature | Tmin. | Air temperature (°C) | The minimum hourly temperature in a day |
| Heat index (Steadman, 1979) | HI | 1. Ta: dry bulb temperature (°F) 2. RH: Relative Humidity (%) |
HI = − 42.379 + 2.04901523(Ta) + 10.14333127(RH) − 0.22475541(Ta)(RH) − 6.83787 × 10− 3(Ta2) − 5.481717 × 10− 2(RH2) + 1.22874 × 10− 3(Ta2)(RH) + 8.5282 × 10− 4(Ta)(RH2) − 1.99 × 10− 6(Ta2) (RH2) |
| Humidex (Environment Canada, 2012, Masterton and Richardson, 1979) | – | 1. T: Air Temperature (°C) 2. e: Water vapor pressure (hPa) |
Humidex = T + (0.5555) × (e − 10) e = 6.11 × exp(5417.7530 × ((1/273.16) − (1/dew point))) |
| Temperature humidity index (Rosenberg et al., 1983) |
THI | 1. T: Air Temperature (°C) 2. tb: dew point temperature (°C) |
|
| Apparent temperature (Steadman, 1984) | AT | 1. Ta = Ambient dry bulb temperature (°C) 2. e = water vapor pressure (KPa) 3. v = wind speed (m/s) |
AT = − 2.7 + 1.04×Ta + 2e − (0.65v) |
| Wet-bulb globe temperature (Medicine ACoS, 1984) | WBGT | 1. Ta = dry bulb temperature (°C) 2. e = water vapor pressure (hPa) |
WBGT = 0.567 × Ta + 0.393e + 3.94 e = RH / 100 × 6.105 × exp (17.27 × Ta/(237.7 + Ta)) |
2.3. Statistical analysis
Data analyses first transformed the study area (c)-specific temperature index X i (i = 1–8 for eight different high-temperature indices) on day (t) into a standardized value (Z i, t c) based on the following equation:
where μ i c is the mean and σ i c is the standard deviation for high-temperature index i in warm seasons of 2000–2008.
Locally weighted least square regression smoother (LOESS) was used to test each high-temperature index (original measurements and their standardized values — Z score) for associations with all-cause mortality and outpatient visits. The span was set to 1, and degree was set to 2 under lag 0 day (present day).
For each high-temperature index, data analysis further calculated area-specific cumulative 8-day (from lag 0 to lag 7 days) relative risks (RR) and 95% confidence intervals (CI) to determine associations with daily deaths and outpatient visits, using distributed lag non-linear model (DLNM) (Armstrong, 2006, Gasparrini et al., 2010). The model used to measure expected deaths and outpatient visits at day (t) in each area (c) would be:
where Y t c is the expected deaths or outpatient visits for area c on day t. A linear relationship was assumed between deaths and outpatient visits, and air pollutants — PM10, O3, and NO2 with zero thresholds and 5-day lag maximum. The X j, t c represents the air pollutants (j = 1–3 for PM10, O3, and NO2) for area c on day t; NS(T i, t c or Z i, t c, 5 ; lag, 3) are natural cubic splines of measurements or Z-scores for each high-temperature index i = 1–8. Five degrees of freedom (df) for high-temperature indices and Z-score were set, and the effect was accumulated for 8 days (lag 0 to 7 days) under 3 df lag stratification (also set as natural cubic splines). The smoother term of time (“time” in the model) was set to 3 df per warm seasons. Moreover, year was treated as an extra categorical variable in models to control for annual variation in health outcomes (e.g. the sudden drop of outpatient visits due to epidemic of severe acute respiratory syndrome in 2003). Other covariates, such as daily deaths and outpatient visits due to pneumonia and influenza (Flu t c, ICD9 CM codes 480–487), public holiday and day of the week (Dow) were also included in the models for adjustment. We used the Akaike's information criterion (AIC) to measure the relative goodness of fit of statistical models. A lower AIC value indicates a better model fit (Akaike, 1973).
Because values and ranges of the high-temperature index varied dramatically, and we were unable to report the risk estimates per 1 degree change under natural cubic spline function for high-temperature indices. The area-specific cumulative 8-day relative risks for deaths and outpatient visits were reported at standardized deviations of 1 and 2 above mean (i.e., at 84.1th and 97.7th percentile, respectively), and were compared with the standardized score of the lowest health risk for each high-temperature index. Basically, the standardized score for the lowest health risk was inspected from each plot of standardized high-temperature index–health association. This method was similar to estimate relative risks of various temperature indices at the 95th, 96th, 97th, 98th, 99th, and 99.5th percentiles, which had been used previously in the Australian study (Vaneckova et al., 2011). Data management and all statistical analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA) and Statistical Environment R 2.12.
3. Results
3.1. Ambient environmental characteristics
Table 2 depicts the descriptive statistics for climatic factors, high-temperature indices and air pollutants in the three study areas during May–October in 2000–2008. Both the highest and lowest average temperatures appeared in Taipei. Average RH ranged from 53% to 98%, and average WS ranged from 0.60 to 12.0 m/s in study areas. Air pollutant concentrations were similar among areas except that average PM10 and O3 concentrations were higher in Southern Taiwan. The correlation coefficients between each pairs of the eight high-temperature indices ranged from 0.61 to 0.99, the lowest correlation was between maximum and minimum temperature, and the higher correlations were among the composite high-temperature (r2 = 0.89 to 0.99) (data not shown).
Table 2.
Characteristics of climatic factors, high-temperature indices and air pollutants among study areas in May–October of 2000–2008 in Taiwan.
| Variable | Min | Q1 | Q2 | Q3 | Max | Mean | S.D. |
|---|---|---|---|---|---|---|---|
| Taipei | |||||||
| Tavg. | 19.0 | 25.5 | 27.4 | 29.2 | 33.0 | 27.1 | 2.56 |
| Tmax. | 20.0 | 29.1 | 32.0 | 33.9 | 38.2 | 31.3 | 3.35 |
| Tmin. | 15.8 | 22.8 | 24.6 | 25.8 | 30.0 | 24.1 | 2.31 |
| HI | 16.5 | 26.6 | 30.4 | 33.9 | 39.8 | 30.1 | 4.43 |
| THI | 18.8 | 24.2 | 26.0 | 27.2 | 29.0 | 25.5 | 2.09 |
| Humidex | 23.4 | 34.0 | 38.0 | 40.2 | 44.4 | 36.7 | 4.34 |
| AT | 18.9 | 27.4 | 30.3 | 32.3 | 35.6 | 29.5 | 3.41 |
| WBGT | 21.6 | 28.3 | 30.9 | 32.2 | 34.8 | 30.1 | 2.73 |
| PM10, μg/m3 | 14.7 | 30.9 | 40.6 | 50.9 | 151 | 42.7 | 16.4 |
| NO2, ppb | 3.50 | 16.2 | 20.7 | 24.6 | 41.0 | 20.5 | 6.44 |
| O3 of 24 h, ppb | 4.82 | 18.3 | 25.3 | 32.1 | 74.7 | 25.7 | 10.0 |
| Relative humidity, % | 52.7 | 71.0 | 76.0 | 81.5 | 97.7 | 76.2 | 7.49 |
| Water pressure, hPa | 15.3 | 25.3 | 28.4 | 30.0 | 33.7 | 27.3 | 3.68 |
| Wind speed, m/s | 0.60 | 1.47 | 1.95 | 2.80 | 6.67 | 2.19 | 0.94 |
| Central Taiwan | |||||||
| Tavg. | 19.5 | 26.2 | 27.6 | 28.9 | 31.7 | 27.4 | 1.95 |
| Tmax. | 20.7 | 29.8 | 31.6 | 32.6 | 38.4 | 31.1 | 2.08 |
| Tmin. | 16.3 | 23.4 | 24.8 | 26.0 | 28.7 | 24.5 | 2.05 |
| HI | 18.2 | 27.9 | 30.8 | 33.5 | 38.5 | 30.6 | 3.65 |
| THI | 19.2 | 24.8 | 26.1 | 27.0 | 28.6 | 25.7 | 1.70 |
| Humidex | 24.4 | 35.3 | 38.0 | 40.0 | 43.6 | 37.2 | 3.68 |
| AT | 18.8 | 27.8 | 30.0 | 31.7 | 34.8 | 29.4 | 2.96 |
| WBGT | 22.1 | 29.1 | 30.9 | 32.1 | 34.4 | 30.4 | 2.34 |
| PM10, μg/m3 | 11.0 | 33.1 | 46.8 | 65.4 | 142 | 51.6 | 23.2 |
| NO2, ppb | 3.33 | 11.3 | 14.1 | 18.1 | 35.6 | 15.1 | 5.07 |
| O3 of 24 h, ppb | 4.26 | 19.8 | 26.8 | 34.2 | 71.7 | 27.4 | 10.3 |
| Relative humidity, % | 54.5 | 73.0 | 76.0 | 79.5 | 97.5 | 76.3 | 6.26 |
| Water pressure, hPa | 14.5 | 26.1 | 28.8 | 30.1 | 34.1 | 27.7 | 3.46 |
| Wind speed, m/s | 0.90 | 2.00 | 2.60 | 3.45 | 11.9 | 2.87 | 1.20 |
| Southern Taiwan | |||||||
| Tavg. | 22.4 | 27.1 | 28.2 | 29.0 | 31.0 | 28.0 | 1.35 |
| Tmax. | 24.1 | 30.6 | 31.9 | 32.8 | 35.1 | 31.6 | 1.68 |
| Tmin. | 20.2 | 24.5 | 25.4 | 26.3 | 28.8 | 25.3 | 1.32 |
| HI | 21.0 | 29.7 | 32.0 | 34.3 | 38.9 | 31.9 | 3.01 |
| THI | 21.9 | 25.7 | 26.6 | 27.3 | 28.8 | 26.4 | 1.22 |
| Humidex | 28.9 | 37.0 | 39.1 | 40.7 | 44.0 | 38.6 | 2.77 |
| AT | 21.6 | 29.3 | 30.9 | 32.2 | 34.5 | 30.6 | 2.12 |
| WBGT | 24.9 | 30.2 | 31.6 | 32.6 | 34.6 | 31.3 | 1.80 |
| PM10, μg/m3 | 16.5 | 33.9 | 46.9 | 70.4 | 154 | 54.2 | 25.7 |
| NO2, ppb | 4.43 | 10.5 | 12.9 | 15.8 | 40.1 | 13.6 | 4.36 |
| O3 of 24 h, ppb | 4.74 | 18.0 | 27.5 | 39.3 | 71.9 | 29.3 | 13.4 |
| Relative humidity, % | 56.5 | 73.5 | 77.0 | 81.0 | 98.5 | 77.3 | 6.63 |
| Water pressure, hPa | 17.8 | 27.6 | 30.0 | 31.3 | 35.1 | 29.2 | 3.06 |
| Wind speed, m/s | 0.75 | 1.85 | 2.40 | 3.05 | 12.0 | 2.59 | 1.02 |
Note: Tavg.: daily average temperature; Tmax.: daily maximum temperature; Tmin.: daily minimum temperature; HI: heat index; THI: temperature humidity index; AT: apparent temperature; WBGT: wet-bulb globe temperature; and S.D.: standard deviation.
3.2. Association between current temperatures and mortality/outpatient visits
Fig. 2 shows the association between high-temperature indices (lag 0 day) and daily all-cause deaths measured using LOESS. The high-temperature indices varied among areas, with wider ranges for original high-temperature indices in Taipei. After standardization for these indices, the regression lines showed a similar pattern of association for Z scores ranged within ± 2 standard deviation. A U-shaped temperature–mortality association was observed in Taipei. An observed positive linear relationship between mortality and high temperatures was identified in Southern Taiwan. No significant association with high temperature was detected in Central Taiwan. Fig. 3 shows the association between high-temperature indices and outpatient visits on lag 0 day measured using LOESS. There were larger variations at Z scores lower than − 2 (i.e., extremely low percentiles in warm seasons). In contrast with all-cause mortality, the outpatient visits were not significantly associated with extreme high temperatures in any of the study areas.
Fig. 2.
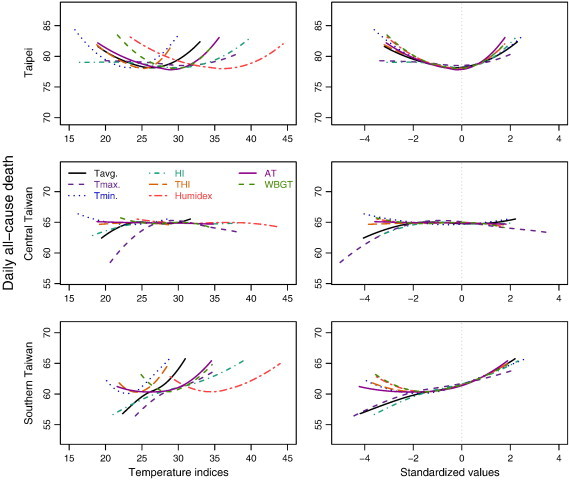
Locally weighted least square regression smoother (LOESS) between all-cause mortality and (standardized) high-temperature indices.
Fig. 3.
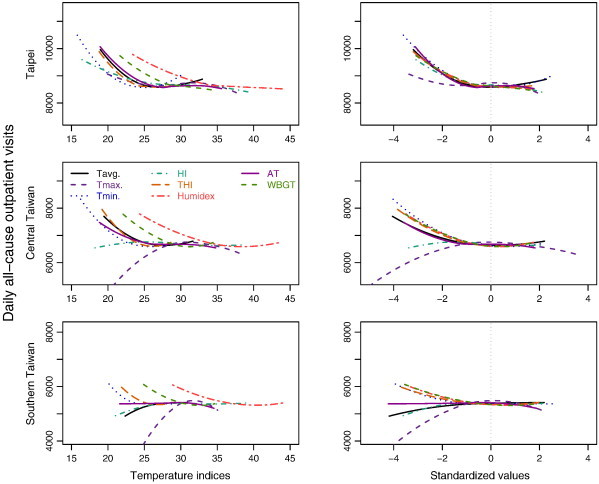
Locally weighted least square regression smoother (LOESS) between all-cause outpatient visits and (standardized) high-temperature indices.
3.3. Cumulative relative risk for various high-temperature indices
The AIC values among various models for associations between high-temperature indices and all-cause models were similar (Table 3 ). Based on the selection criteria for modeling, AT was the most optimal index in Taipei and Southern Taiwan, but humidex or WBGT was most optimal in Central Taiwan. Fig. S1, Fig. S2, Fig. S3 show the cumulative 8-day relatively risk of all-cause mortality associated with high-temperature indices and their transformed standardized values. The lowest mortality risks were identified at Z = 0 for Taipei and Central Taiwan, and at Z = − 1 for Southern Taiwan. Therefore, these transformed standardized scores were used as reference values in further analyses. At the transformed high-temperature index of Z = 1 (84.1th percentile of high-temperature indices), the mortality risk approximately increased by 3%, 1% and 9% in Taipei, Central Taiwan and Southern Taiwan, respectively. As of Z = 2 (97.7th percentile of high-temperature indices) for AT, the cumulative relative risks for mortality significantly increased by 23% in Taipei and by 28% in Southern Taiwan. There was no significant increase in Central Taiwan. Comparing the risk estimates for the eight high-temperature indices, the RRs were similar at Z = 1, but the risk estimates at Z = 2 were higher for composite high-temperature indices than for single high-temperature indices.
Table 3.
Summary for high-temperature indices associated with the lowest mortality risk in locally weighted least square regression smoother (LOESS) and distributed lag non-linear model (DLNM).
| Area/temperature index | LOESS at lag 0 day (Fig. 2) |
DLNM (cumulative lag 0 to lag 7 days) |
||||
|---|---|---|---|---|---|---|
| Z score⁎ | Value of temperature indices | Reference temperature indices⁎⁎ | Relative risk (95% CI)⁎⁎⁎ |
AIC | ||
| At + 1 S.D. | At + 2 S.D. | |||||
| Taipei | ||||||
| Tavg. | − 0.29 | 26 | 26 | 1.04 (1.01–1.08) | 1.11 (0.96–1.28) | 12,132 |
| Tmax. | − 0.17 | 31 | 31 | 1.03 (0.99–1.07) | 1.13 (0.96–1.33) | 12,148 |
| Tmin. | − 0.29 | 23 | 21 | 1.02 (0.99–1.06) | 1.17 (1.03–1.33) | 12,131 |
| HI | − 0.04 | 30 | 29 | 1.03 (1.00–1.06) | 1.13 (1.03–1.23) | 12,132 |
| THI | − 0.17 | 25 | 25 | 1.04 (1.00–1.07) | 1.19 (1.00–1.43) | 12,132 |
| Humidex | − 0.16 | 36 | 35 | 1.03 (1.00–1.07) | 1.20 (1.02–1.42) | 12,132 |
| AT | − 0.20 | 29 | 28 | 1.03 (1.00–1.07) | 1.23 (1.05–1.43) | 12,129 |
| WBGT | − 0.16 | 30 | 28 | 1.03 (1.00–1.07) | 1.22 (1.03–1.46) | 12,132 |
| Central Taiwan | ||||||
| Tavg. | − 4.05 | 19 | 27 | 1.02 (0.99–1.06) | 1.07 (0.93–1.23) | 11,866 |
| Tmax. | − 5.01 | 21 | 36 | 1.03 (0.99–1.07) | 0.98 (0.87–1.10) | 11,862 |
| Tmin. | − 0.51 | 23 | 24 | 1.00 (0.96–1.04) | 1.16 (1.03–1.32) | 11,858 |
| HI | − 3.38 | 18 | 29 | 1.01 (0.98–1.05) | 1.07 (0.98–1.17) | 11,860 |
| THI | 1.71 | 29 | 27 | 1.00 (0.96–1.04) | 1.13 (0.94–1.35) | 11,857 |
| Humidex | 1.75 | 44 | 40 | 0.99 (0.96–1.03) | 1.13 (0.94–1.36) | 11,855 |
| AT | 1.82 | 35 | 35 | 1.01 (0.98–1.05) | 0.90 (0.73–1.12) | 11,858 |
| WBGT | 1.74 | 34 | 32 | 0.99 (0.96–1.03) | 1.13 (0.93–1.38) | 11,855 |
| Southern Taiwan | ||||||
| Tavg. | − 4.19 | 22 | 27 | 1.05 (1.01–1.10) | 1.22 (1.12–1.32) | 11,548 |
| Tmax. | − 4.44 | 24 | 31 | 1.08 (1.03–1.13) | 1.15 (1.01–1.32) | 11,550 |
| Tmin. | − 1.80 | 23 | 24 | 1.07 (1.03–1.12) | 1.13 (1.06–1.20) | 11,555 |
| HI | − 3.61 | 21 | 27 | 1.07 (1.02–1.11) | 1.18 (1.10–1.27) | 11,557 |
| THI | − 1.73 | 24 | 25 | 1.09 (1.04–1.14) | 1.25 (1.11–1.40) | 11,554 |
| Humidex | − 1.50 | 34 | 34 | 1.11 (1.05–1.16) | 1.24 (1.10–1.41) | 11,557 |
| AT | − 2.11 | 26 | 27 | 1.09 (1.05–1.14) | 1.28 (1.13–1.45) | 11,546 |
| WBGT | − 1.46 | 29 | 28 | 1.11 (1.05–1.17) | 1.24 (1.09–1.41) | 11,559 |
Note: Tavg.: daily average temperature; Tmax.: daily maximum temperature; Tmin.: daily minimum temperature; HI: heat index; THI: temperature humidity index; AT: apparent temperature; WBGT: wet-bulb globe temperature; S.D.: standard deviation; and AIC represents Akaike's information criterion values.
Z score of high-temperature indices for lowest predicted all-cause deaths in LOESS regression (Fig. 2).
High-temperature indices' value with lowest mortality risk in DLNM model.
Risk estimated based on reference equals to Z = 0 in Taipei and Central Taiwan, and Z = − 1 in Southern Taiwan (Supplement Figs. 1–3).
Compared with the association with mortality, there was a greater variation in relationships between selected high-temperature indices and all-cause outpatient visits (Table 4 ). Based on AIC values, the maximum temperature was the most optimal predictor among associations between outpatient visits and temperatures. The lowest outpatient visit risk was observed at Z = 0 in Taipei and Central Taiwan, but at Z = − 1 in Southern Taiwan (Fig. S4, Fig. S5, Fig. S6). Thus, these standardized scores were used as reference values for further analyses. At Z = 1, the cumulative 8-day relative risks for outpatient visits increased by approximately 7%, 3%, and 4% in Taipei, Central Taiwan and Southern Taiwan, respectively. At Z = 2, the estimated cumulative relative risks for these three areas decreased dramatically and were no longer statistically significant.
Table 4.
Summary for high-temperature indices associated with the lowest outpatient visit risk in locally weighted least square regression smoother (LOESS) and distributed lag non-linear model (DLNM).
| Area/temperature index | LOESS at lag 0 day (Fig. 3) |
DLNM (cumulative lag 0 to lag 7 days) |
||||
|---|---|---|---|---|---|---|
| Z score⁎ | Value of temperature indices | Reference temperature indices⁎⁎ | Relative risk (95% CI)⁎⁎⁎ |
AIC | ||
| At + 1 S.D. | At + 2 S.D. | |||||
| Taipei | ||||||
| Tavg. | − 0.11 | 27 | 19 | 1.07 (1.07–1.07) | 1.05 (1.03–1.06) | 294,133 |
| Tmax. | 2.06 | 38 | 20 | 1.07 (1.06–1.07) | 1.02 (1.01–1.04) | 293,412 |
| Tmin. | 0.39 | 25 | 25 | 1.05 (1.04–1.05) | 1.02 (1.00–1.03) | 296,599 |
| HI | 2.19 | 40 | 29 | 1.06 (1.06–1.07) | 1.07 (1.06–1.08) | 294,306 |
| THI | 0.41 | 26 | 26 | 1.06 (1.05–1.06) | 1.03 (1.01–1.05) | 295,944 |
| Humidex | 1.76 | 44 | 37 | 1.04 (1.04–1.05) | 1.03 (1.02–1.05) | 296,988 |
| AT | 1.78 | 36 | 28 | 1.07 (1.07–1.08) | 1.01 (1.00–1.03) | 294,251 |
| WBGT | 1.75 | 35 | 30 | 1.04 (1.03–1.04) | 1.04 (1.02–1.06) | 297,643 |
| Central Taiwan | ||||||
| Tavg. | 0.18 | 28 | 19 | 1.04 (1.03–1.04) | 1.03 (1.01–1.04) | 144,296 |
| Tmax. | − 5.01 | 21 | 20 | 1.03 (1.02–1.03) | 1.00 (0.99–1.01) | 142,948 |
| Tmin. | 0.66 | 26 | 25 | 1.02 (1.01–1.02) | 1.02 (1.00–1.03) | 147,765 |
| HI | − 3.38 | 18 | 29 | 1.03 (1.03–1.04) | 1.02 (1.01–1.03) | 144,018 |
| THI | 0.26 | 26 | 25 | 1.03 (1.03–1.04) | 1.01 (0.99–1.03) | 144,018 |
| Humidex | 0.33 | 38 | 35 | 1.03 (1.03–1.03) | 1.00 (0.98–1.01) | 146,606 |
| AT | 1.82 | 35 | 26 | 1.04 (1.04–1.05) | 0.93 (0.92–0.95) | 143,834 |
| WBGT | 0.38 | 31 | 29 | 1.03 (1.02–1.03) | 0.99 (0.97–1.01) | 146,939 |
| Southern Taiwan | ||||||
| Tavg. | − 4.19 | 22 | 22 | 1.03 (1.02–1.03) | 1.07 (1.06–1.08) | 112,884 |
| Tmax. | − 4.44 | 24 | 24 | 1.04 (1.03–1.04) | 1.01 (1.00–1.03) | 112,040 |
| Tmin. | − 0.55 | 25 | 25 | 1.02 (1.01–1.02) | 1.02 (1.01–1.02) | 116,159 |
| HI | − 3.61 | 21 | 30 | 1.02 (1.02–1.03) | 1.03 (1.02–1.04) | 113,894 |
| THI | 0.44 | 27 | 25 | 1.03 (1.03–1.04) | 1.03 (1.01–1.04) | 114,760 |
| Humidex | 0.68 | 41 | 39 | 1.03 (1.02–1.04) | 0.99 (0.97–1.00) | 115,572 |
| AT | 1.88 | 35 | 27 | 1.05 (1.04–1.05) | 1.07 (1.06–1.09) | 112,513 |
| WBGT | 0.80 | 33 | 32 | 1.03 (1.02–1.03) | 0.97 (0.95–0.98) | 115,970 |
Note: Tavg.: daily average temperature; Tmax.: daily maximum temperature; Tmin.: daily minimum temperature; HI: heat index; THI: temperature humidity index; AT: apparent temperature; WBGT: wet-bulb globe temperature; S.D.: standard deviation; and AIC represents Akaike's information criterion values.
Z score of high-temperature indices for lowest predicted all-cause outpatient visits in LOESS regression (Fig. 3).
High-temperature indices' value with lowest outpatient visit risk in DLNM model.
Risk estimated based on DLNM set as centered value equals to Z = 0 in Taipei and Central Taiwan, and Z = − 1 in Southern Taiwan (Supplement Figs. 4–6).
4. Discussion
Associations between high-temperature indices and mortality and outpatient visits differ among areas and enable to further compare the capacity of prediction. The index of temperature measurement used in the study is as simple as possible. For example, daily average temperature is a simple indicator that the general population can easily understand. Average temperature is the most common measurement used for studying the impact of temperature on health outcomes. However, to account for the changes in temperature perceived by humans, recent studies have introduced comprehensive weather variables as composite high-temperature indices such as HI, AT, humidex and WBGT to study the temperature-related health outcomes (Anderson and Bell, 2009, Chung et al., 2009, Epstein and Moran, 2006, Kjellstrom et al., 2009, Smoyer-Tomic and Rainham, 2001).
The present study evaluated whether all-cause mortality and outpatient visits are associated with the eight high-temperature indices in warm seasons for population in a subtropical island. We found that the association may vary by the study area, evaluated health outcomes and selected high-temperature indices. Apparent temperature is the most optimal high-temperature index associated with all-cause mortality. However, the eight temperature indices performed similarly in models fitting for predicting all-cause mortality. Besides, the maximum temperature is consistently the most optimal high-temperature index for predicting all-cause outpatient visits.
Temperature indices vary based on demographic and geographic status. A Korean study suggested that HI and mean temperature performed comparably for predicting mortality (Kim et al., 2006). A Toronto study concluded that humidex and AT are both effective for predicting excess mortality associated with hot and humid weather (Smoyer-Tomic and Rainham, 2001). Some research teams have used AT as the high-temperature index of interest and have found significant association between temperature and mortality (Chung et al., 2009). On the other hand, a study conducted in New York city showed that maximum HI is a better goodness of fit than maximum, minimum or average temperature in estimating the mortality risk during hot weather (Metzger et al., 2009). A Chinese study showed that, based on model fitting, the mean temperature was a better predictor of mortality than maximum and minimum temperatures (Guo et al., 2011). Yu et al. revealed that mean temperature was an accurate index of all-cause death in Brisbane, Australia (Yu et al., 2011).
In contrast, Anderson et al. reported that temperature-related mortality assessments did not significantly differ among average, maximum and apparent temperature metrics. They found that the association with apparent temperature is nearly identical to that with the mean daily temperature after controlling for humidity (Anderson and Bell, 2009). Vaneckova et al. also found that average temperature and composite high-temperature indices perform similarly in estimating mortality risk (Vaneckova et al., 2011). Likewise, all high-temperature indices are significantly associated with mortality in this study because temperature indices are highly correlated with each other. The cumulative mortality risks associated with the composite indices are also relatively similar. In subtropical regions, the consistent high temperature and humidity, and other weather characteristics such as WS and WVP result in a relatively smaller effect on perceived temperature. Barnett et al. (2010) have concluded that no high-temperature index can be considered superior to others, because an optimal high-temperature index is also associated with age groups, seasons, and areas analyzed. They suggest selecting high-temperature index based on practical concerns such as the accessibility of climate measurements, public familiarity with the index, and data available (Barnett et al., 2010).
In terms of morbidity, some studies have reported that HI is an optimal heat index for predicting inpatient cares and heat-related dispatches (Hartz et al., 2012, Semenza et al., 1999). The mean apparent temperature is also an indicator that may well predict hospital admissions for several diseases in nine California counties (Green et al., 2010). However, Khalaj et al. found that emergency hospital admissions were more likely correlated with maximum temperature (Khalaj et al., 2010). Our study found similar results that maximum temperature is an optimal high-temperature index for predicting heat-related outpatient visits. The weather associated morbidity may be different between clinical visits and emergency room visits. The choice of high-temperature indices may thus produce subtle differences in assessing possible health-related effects of heat. This study also showed that the optimal high-temperature index for predicting mortality is different from predicting outpatient visits.
No standard methodology has been developed to evaluate the capacity of high-temperature indices for predicting health effects. A common choice is to measure the change in relative risk of mortality associated with one degree temperature increase or decrease. However, this approach complicates comparisons among different high-temperature indices with different scales and ranges. In this study, we standardize the indices to unify the measurement scale and improve the capacity of prediction.
Most studies assume a linear association between temperatures and health outcomes, which might not be plausible with practical data (Metzger et al., 2009). Armstrong et al. (2011) found that a linear relationship seems to fit well above the threshold temperature without controlling other climate status. Although, some evidences have shown non-linearity association as the temperature is above the thresholds, with quadratic or larger relationships at the highest temperatures. The present study proposed an alternative method to estimate the cumulative RR using DLMN and presented non-linear associations between high temperature indices and mortality, and outpatient visits as well. Standardization assures the comparability among various high-temperature indices (Armstrong et al., 2011).
The cumulative 8-day RRs of health outcomes vary among high temperatures. In summary, our study observes higher cumulative RRs for mortality than for outpatient visits in association with high temperature. The area-specific RRs of mortality associated with observed and standardized high-temperature indices are clearly non-linear with index values (Fig. S1, Fig. S2, Fig. S3). The corresponding RRs of outpatient visits are more fluctuated and inconsistent (Fig. S4, Fig. S5, Fig. S6). These findings support the study in England that high temperatures have a larger effect on mortality than on morbidity (Kovats et al., 2004). We found the mortality risk increased dramatically as standardized high-temperature indices increased from Z = 1 to 2. Nonetheless, the standardized high-temperature indices have higher RRs at Z = 1 than at Z = 2 for all-cause outpatient visits. A possible explanation is that people who have mild illness may take immediate action in response to remit the symptoms. They may stay in air conditioned environment or drink more fluids against the outdoor high temperature.
An island located in a subtropical region, separated from the Asian continent, with an area of 144 km wide and 394 km long, the weather in Taiwan varied from north to south. Therefore, the health risks associated with these high-temperature indices are evaluated only for the population residing in the area-specific environment. Studies with similar methodologies are thus suggested for populations located in different climates. In addition, this study also found that the risks associated with heat are significant in Taipei and Southern Taiwan rather than in Central Taiwan. Compared with the other two areas, Central Taiwan has lower income and higher portion of the elders (Directorate-General of Budget, Accounting and Statistics, Executive Yuan, R.O.C. (Taiwan), 2012). However, due to limited detail information for social economics, this study may not conclude any effects related with these factors. Interactions among these variables are recommended to assess in future study. Moreover, this ecological study focused only on all-cause mortality and outpatient visits. Further studies of temperature effects on human physical responses, clinical symptoms of heat exposure, and identification of the most vulnerable groups are needed to establish a comprehensive heat wave warning system in the future.
5. Conclusion
The associations between high temperature and all-cause mortality and outpatient visits varied by region, health outcomes and selected high-temperature indices. Apparent temperature is the most optimal among high-temperature indices for predicting all-cause mortality. Maximum temperature is highly correlated with all-cause outpatient visits. Standardized high-temperature indices provided an effective platform for comparing these indices on heat related health association study.
The following are the supplementary data related to this article.
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause mortality associated with (standardized) temperature indices in Taipei. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily mortality from pneumonia and influenza, holiday effects, day of the week, and long-term trends.
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause mortality associated with (standardized) temperature indices in Central Taiwan. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily mortality from pneumonia and influenza, holiday effects, day of the week, and long-term trends.
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause mortality associated with (standardized) temperature indices in Southern Taiwan. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily mortality from pneumonia and influenza, holiday effects, day of the week, and long-term trends.
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause outpatient visits associated with (standardized) temperature indices in Taipei. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily outpatient visits of pneumonia and influenza, holiday effects, day of the week, and long-term trends.
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause outpatient visits associated with (standardized) temperature indices in Central Taiwan. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily outpatient visits of pneumonia and influenza, holiday effects, day of the week, and long-term trends.
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause outpatient visits associated with (standardized) temperature indices in Southern Taiwan. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily outpatient visits of pneumonia and influenza, holiday effects, day of the week, and long-term trends.
Acknowledgments
We appreciate the authorities of Department of Health, Taiwan National Health Research Institute, Taiwan Environmental Protection Administration, and Taiwan Central Weather Bureau for providing research data. Interpretations and conclusions herein do not represent those of these agencies. Dr. Fung-Chang Sung and Ted Knoy are appreciated for their editorial assistance. This study was supported in part by Taiwan National Science Council (NSC 96-3111-B-033-001, NSC 99-2621-M-039-001 and NSC 99-2221-E-033-052), the China Medical University Hospital (1MS1), and the Taiwan Department of Health (DOH100-TD-B-111-004, DOH100-TD-C-111-005).
Footnotes
Authors' contribution: All the authors participated in this study and contributed remarkable part of it. YK Lin, CK Chang, MH Li and YC Wang designed the study methods and obtained the research data. YC Wang and YC Wu performed statistical analyses. YK Lin, CK Chang and YC Wang drafted and finalized the manuscript. All the authors have read and approved the final version of the manuscript.
Conflicts of interest: All the authors declare that this study involves no conflict of interest.
References
- Akaike H. 2nd international symposium on information theory. 1973. Information theory and an extension of the maximum likelihood principle; pp. 267–281. [Google Scholar]
- Anderson B.G., Bell M.L. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20:205–213. doi: 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson G.B., Bell M.L. Heat waves in the United States: mortality risk during heat waves and effect modification by heat wave characteristics in 43 U.S. communities. Environ Health Perspect. 2011;119:210–218. doi: 10.1289/ehp.1002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong B. Models for the relationship between ambient temperature and daily mortality. Epidemiology. 2006;17:624–631. doi: 10.1097/01.ede.0000239732.50999.8f. [DOI] [PubMed] [Google Scholar]
- Armstrong B.G., Chalabi Z., Fenn B., Hajat S., Kovats S., Milojevic A. Association of mortality with high temperatures in a temperate climate: England and Wales. J Epidemiol Community Health. 2011;65:340–345. doi: 10.1136/jech.2009.093161. [DOI] [PubMed] [Google Scholar]
- Barnett A.G., Tong S., Clements A.C. What measure of temperature is the best predictor of mortality? Environ Res. 2010;110:604–611. doi: 10.1016/j.envres.2010.05.006. [DOI] [PubMed] [Google Scholar]
- Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health. 2009;8:40. doi: 10.1186/1476-069X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung J.Y., Honda Y., Hong Y.C., Pan X.C., Guo Y.L., Kim H. Ambient temperature and mortality: an international study in four capital cities of East Asia. Sci Total Environ. 2009;408:390–396. doi: 10.1016/j.scitotenv.2009.09.009. [DOI] [PubMed] [Google Scholar]
- Curriero F.C., Heiner K.S., Samet J.M., Zeger S.L., Strug L., Patz J.A. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155:80–87. doi: 10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
- Directorate-General of Budget, Accounting and Statistics, Executive Yuan, R.O.C. (Taiwan) National Statistics. 2012. http://www.dgbas.gov.tw/mp.asp?mp=1 Available at. Accessed date: 2012.02.25.
- Environment Canada Calculation of the 1971 to 2000 climate normals for Canada. 2012. http://climate.weatheroffice.gc.ca/prods_servs/normals_documentation_e.html Available at. Accessed date: 2012.02.25.
- Epstein Y., Moran D.S. Thermal comfort and the heat stress indices. Ind Health. 2006;44:388–398. doi: 10.2486/indhealth.44.388. [DOI] [PubMed] [Google Scholar]
- Gasparrini A., Armstrong B., Kenward M.G. Distributed lag non-linear models. Stat Med. 2010;29:2224–2234. doi: 10.1002/sim.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gouveia N., Hajat S., Armstrong B. Socioeconomic differentials in the temperature–mortality relationship in Sao Paulo, Brazil. Int J Epidemiol. 2003;32:390–397. doi: 10.1093/ije/dyg077. [DOI] [PubMed] [Google Scholar]
- Green R.S., Basu R., Malig B., Broadwin R., Kim J.J., Ostro B. The effect of temperature on hospital admissions in nine California counties. Int J Public Health. 2010;55:113–121. doi: 10.1007/s00038-009-0076-0. [DOI] [PubMed] [Google Scholar]
- Guo Y., Barnett A.G., Pan X., Yu W., Tong S. The impact of temperature on mortality in Tianjin, China: a case-crossover design with a distributed lag nonlinear model. Environ Health Perspect. 2011;119:1719–1725. doi: 10.1289/ehp.1103598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat S., Sheridan S.C., Allen M.J., Pascal M., Laaidi K., Yagouti A. Heat-health warning systems: a comparison of the predictive capacity of different approaches to identifying dangerously hot days. Am J Public Health. 2010;100:1137–1144. doi: 10.2105/AJPH.2009.169748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartz D.A., Golden J.S., Sister C., Chuang W.C., Brazel A.J. Climate and heat-related emergencies in Chicago, Illinois (2003–2006) Int J Biometeorol. 2012;56(1):71–83. doi: 10.1007/s00484-010-0398-x. [Electronic publication ahead of print 2011 Jan 27] [DOI] [PubMed] [Google Scholar]
- Khalaj B., Lloyd G., Sheppeard V., Dear K. The health impacts of heat waves in five regions of New South Wales, Australia: a case-only analysis. Int Arch Occup Environ Health. 2010;83:833–842. doi: 10.1007/s00420-010-0534-2. [DOI] [PubMed] [Google Scholar]
- Kim H., Ha J.S., Park J. High temperature, heat index, and mortality in 6 major cities in South Korea. Arch Environ Occup Health. 2006;61:265–270. doi: 10.3200/AEOH.61.6.265-270. [DOI] [PubMed] [Google Scholar]
- Kjellstrom T., Holmer I., Lemke B. Workplace heat stress, health and productivity — an increasing challenge for low and middle-income countries during climate change. Glob Health Action. 2009:2. doi: 10.3402/gha.v2i0.2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowlton K., Lynn B., Goldberg R.A., Rosenzweig C., Hogrefe C., Rosenthal J.K. Projecting heat-related mortality impacts under a changing climate in the New York City region. Am J Public Health. 2007;97:2028–2034. doi: 10.2105/AJPH.2006.102947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovats R.S., Hajat S. Heat stress and public health: a critical review. Annu Rev Public Health. 2008;29:41–55. doi: 10.1146/annurev.publhealth.29.020907.090843. [DOI] [PubMed] [Google Scholar]
- Kovats R.S., Kristie L.E. Heatwaves and public health in Europe. Eur J Public Health. 2006;16:592–599. doi: 10.1093/eurpub/ckl049. [DOI] [PubMed] [Google Scholar]
- Kovats R.S., Hajat S., Wilkinson P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. Occup Environ Med. 2004;61:893–898. doi: 10.1136/oem.2003.012047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y.-K., Ho T.-J., Wang Y.-C. Mortality risk associated with temperature and prolonged temperature extremes in elderly populations in Taiwan. Environ Res. 2011;111:1156–1163. doi: 10.1016/j.envres.2011.06.008. [DOI] [PubMed] [Google Scholar]
- Masterton J.M., Richardson F.A. Report CLI 1-79. Environment Canada, Ontario, Downsview. 1979. Humidex: a method of quantifying human discomfort due to excessive heat and humidity. [Google Scholar]
- McMichael A.J., Wilkinson P., Kovats R.S., Pattenden S., Hajat S., Armstrong B. International study of temperature, heat and urban mortality: the ‘ISOTHURM’ project. Int J Epidemiol. 2008;37:1121–1131. doi: 10.1093/ije/dyn086. [DOI] [PubMed] [Google Scholar]
- Medicine ACoS Prevention of thermal injuries during distance running — position stand. Med J Aust. 1984:876. [PubMed] [Google Scholar]
- Meehl G.A., Tebaldi C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science. 2004;305:994–997. doi: 10.1126/science.1098704. [DOI] [PubMed] [Google Scholar]
- Metzger K.B., Ito K., Matte T.D. Summer heat and mortality in New York City: how hot is too hot? Environ Health Perspect. 2009;118:80–86. doi: 10.1289/ehp.0900906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neill M.S., Ebi K.L. Temperature extremes and health: impacts of climate variability and change in the United States. J Occup Environ Med. 2009;51:13–25. doi: 10.1097/JOM.0b013e318173e122. [DOI] [PubMed] [Google Scholar]
- Pantavou K., Theoharatos G., Mavrakis A., Santamouris M. Evaluating thermal comfort conditions and health responses during an extremely hot summer in Athens. Build and Environ. 2011;46:339–344. [Google Scholar]
- Rosenberg N.J., Verma S.B., Blad B.L. Human and animal biometeorology. Microclimate: The Biol Environ. 1983:425–467. [Google Scholar]
- Semenza J.C., McCullough J.E., Flanders W.D., McGeehin M.A., Lumpkin J.R. Excess hospital admissions during the July 1995 heat wave in Chicago. Am J Prev Med. 1999;16:269–277. doi: 10.1016/s0749-3797(99)00025-2. [DOI] [PubMed] [Google Scholar]
- Smoyer-Tomic K.E., Rainham D.G. Beating the heat: development and evaluation of a Canadian hot weather health-response plan. Environ Health Perspect. 2001;109:1241–1248. doi: 10.1289/ehp.011091241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steadman R.G. The assessment of sultriness. Part I: a temperature–humidity index based on human physiology and clothing science. J Appl Meteorol. 1979;18:861–873. [Google Scholar]
- Steadman R.G. A universal scale of apparent temperature. J Clim Appl Meteorol. 1984:1674–1687. [Google Scholar]
- Taiwan Central Weather Bureau The Central Weather Bureau online information. 2011. http://www.cwb.gov.tw/eng/index.htm Available at. Accessed Date: 2011/05/12.
- Taiwan Environmental Protection Administration Taiwan Air Quality Monitoring Network. 2011. http://taqm.epa.gov.tw/taqm/en/PsiAreaHourly.aspx Available at. Accessed date: 2011/05/12.
- Taiwan Governmental Information Office The Republic of China year book 2008: Chapter 12. Environmental protection. Taipei. 2008. http://www.gio.gov.tw/taiwan-website/5-gp/yearbook/2008/ch12.html Available at. Accessed Date: 2011/05/12.
- Vaneckova P., Neville G., Tippett V., Aitken P., Fitzgerald G., Tong S. Do biometeorological indices improve modeling outcomes of heat-related mortality? J Appl Meteorol Clim. 2011;50:1165–1176. [Google Scholar]
- Wang Y.C., Lin Y.K., Chuang C.Y., Li M.H., Chou C.H., Liao C.H. Associating emergency room visits with first and prolonged extreme temperature event in Taiwan: a population-based cohort study. Sci Total Environ. 2012;416:97–104. doi: 10.1016/j.scitotenv.2011.11.073. [DOI] [PubMed] [Google Scholar]
- Ye X., Wolff R., Yu W., Vaneckova P., Pan X., Tong S. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect. 2012;120:19–28. doi: 10.1289/ehp.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu W., Vaneckova P., Mengersen K., Pan X., Tong S. Is the association between temperature and mortality modified by age, gender and socio-economic status? Sci Total Environ. 2010;408:3513–3518. doi: 10.1016/j.scitotenv.2010.04.058. [DOI] [PubMed] [Google Scholar]
- Yu W., Guo Y., Ye X., Wang X., Huang C., Pan X. The effect of various temperature indicators on different mortality categories in a subtropical city of Brisbane, Australia. Sci Total Environ. 2011;409:3431–3437. doi: 10.1016/j.scitotenv.2011.05.027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause mortality associated with (standardized) temperature indices in Taipei. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily mortality from pneumonia and influenza, holiday effects, day of the week, and long-term trends.
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause mortality associated with (standardized) temperature indices in Central Taiwan. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily mortality from pneumonia and influenza, holiday effects, day of the week, and long-term trends.
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause mortality associated with (standardized) temperature indices in Southern Taiwan. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily mortality from pneumonia and influenza, holiday effects, day of the week, and long-term trends.
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause outpatient visits associated with (standardized) temperature indices in Taipei. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily outpatient visits of pneumonia and influenza, holiday effects, day of the week, and long-term trends.
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause outpatient visits associated with (standardized) temperature indices in Central Taiwan. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily outpatient visits of pneumonia and influenza, holiday effects, day of the week, and long-term trends.
Cumulative 8-day (lag 0 to lag 7 days) relative risk for all-cause outpatient visits associated with (standardized) temperature indices in Southern Taiwan. Relative risks were estimated using DLNM that included daily city-specific averages of PM10, NO2, O3, daily outpatient visits of pneumonia and influenza, holiday effects, day of the week, and long-term trends.


