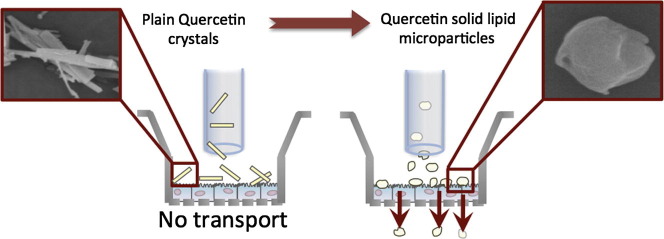
Graphical abstract
Keywords: Quercetin, Anti-asthmatic, Solid–lipid particle, Inhalation, Dry powder
Abstract
Purpose
The aim of the present work was to develop solid lipid microparticles (SLMs), as dry powders containing quercetin for direct administration to the lung.
Methods
Quercetin microparticles were prepared by o/w emulsification via a phase inversion technique, using tristearin as the lipid component and phosphatidylcholine as an emulsifier. The quercetin SLMs were characterised for morphology, drug loading (15.5% ± 0.6, which corresponded to an encapsulation efficiency of 71.4%), particle size distribution, response to humidity, crystallinity, thermal behaviour and in vitro respirable fraction. Furthermore, the toxicity and the in vitro transport of the SLMs on an air liquid interface model of the Calu-3 cell line were also investigated using a modified twin-stage impinger apparatus.
Results
Results showed that quercetin SLMs could be formulated as dry powder suitable for inhalation drug delivery (20.5 ± 3.3% fine particle fraction ⩽4.46 μm) that was absorbed, via a linear kinetic model across the Calu-3 monolayer (22.32 ± 1.51% over 4 h). In addition, quercetin SLMs were shown to be non-toxic at the concentrations investigated. Interestingly, no apical to basolateral transport of the micronised quercetin was observed over the period of study.
Conclusions
These observations suggest quercetin diffusion was enhanced by the presence of the lipid/emulsifying excipients in the SLMs; however further studies are necessary to elucidate the exact mechanisms.
1. Introduction
Quercetin is a flavonoid, a natural substance with a phenolic structure. Flavonoids can be divided into various classes on the basis of their molecular structure with quercetin belonging to the flavone class, which has a planar structure due to the double bond in the central ring of the 2-phenylchromen-4-one (2-phenyl-1-benzopyran-4-one) backbone. This flavonoid group can be found in abundance in onions, apples, broccoli, and berries (Nijveldt et al., 2001, Formica and Regelson, 1995). Quercetin pharmacokinetics and bioavailability in humans has previously been studied (Moon et al., 2008, Graefe et al., 2001). An important effect of quercetin is its ability to scavenge for oxygen-derived free radicals (Heijnen et al., 2001), given its antioxidant properties at low concentrations (Robaszkiewicz et al., 2007). Furthermore, in vitro and in vivo experiments have also shown that flavonoids possess potential anti-inflammatory, anti-allergic, antiviral, anti-carcinogenic and anti-asthmatic properties (Pettinari et al., 2006, Wu et al., 2004, Li et al., 2001, Davis et al., 2008, Gang et al., 2012, Moon et al., 2008).
Specifically, for the lungs, cell culture studies have shown that quercetin can reduce infectivity of target cells and replication against a wide variety of respiratory viruses, including herpes simplex virus and adenovirus (Chiang et al., 2003), coronavirus (Debiaggi et al., 1990), parainfluenza and respiratory syncytial virus (Kaul et al., 1985), rhinovirus (Dimova et al., 2003), and severe acute respiratory syndrome (Chen et al., 2006). Furthermore, there is evidence that quercetin plays a critical role in the amelioration of the pathogenic process of asthma in a murine model (mice) (Park et al., 2009), due to the alteration of specific cytokine production (Th1/Th2) and transcriptor factors (T-bet and GATA-3) gene expression in OVA-induced asthma model mice, suggesting quercetin could be used as a new therapeutic approach to allergic airway diseases. More recently, when given orally to guinea pigs, quercetin has been found to reduce hyper-reactivity of airways, one of the main attributes of allergic asthma (Joskova et al., 2011); causing significant broncodilation.
Furthermore, a report suggests that flavonoids such as quercetin and luteolin could stimulate Cl− secretion by activating an entry step of Cl− across the basolateral membrane through Na+/K+/2Cl− co-transporter; contributing to maintenance and/or production of airway surface liquid by regulating Cl− secretion in airway epithelial cells (Asano et al., 2009), very important in chronic obstructive pulmonary disease.
Quercetin is sparingly soluble in water and has poor bioavailability. As a result, the clinical application of the drug is greatly restricted. Previous studies have tried to resolve this issue by producing nanocrystals with enhanced dissolution (Kakran et al., 2012, Li et al., 2009). An alternative approach would be to incorporate the drug into a lipid matrix (Li et al., 2009). The production of solid lipid microparticles (SLMs) has been previously studied as a respiratory drug delivery vehicle for both poorly water-soluble drugs, such as budesonide (Mezzena et al., 2009) and for more water-soluble drugs, such as salbutamol (Scalia et al., 2012). There are many advantages in using SLMs (Jaspart et al., 2005), with the most significant being the ability to control release after deposition. Furthermore, SLMs should be well tolerated in vivo since they are made of physiological compounds. Of course, the toxicity of the surfactants and other excipients, used for their manufacture, needs to be considered.
While solid lipid nanoparticles are currently attracting a lot of attention in the research community, solid lipid micropatrticles have been rather unexploited, especially for inhalation drug delivery (Mezzena et al., 2009, Scalia et al., 2012, Jaspart et al., 2005), where particles should have an optimum aerodynamic diameter between 1 and 6 μm (Patton, 1999). Mezzena et al., 2009, Scalia et al., 2012 used this concept to deliver budesonide and salbutamol, two anti-asthma drugs, respectively, using glycerol behenate as the solid lipid component. In other studies, Dellamary et al. (2004), used dipalmitoylphosphatidylcholine, a biocompatible lipid and component of normal lung surfactant, to modulate immunoglobulin release while Sanna et al. (2004) applied the same concept for the formulation of SLMs to be used as carrier for lung delivery, using Compritol 888 as lipophilic component and Poloxamer as emulsifying agent.
The aim of this study was to investigate the potential use of solid lipid microparticles containing quercetin delivered as a dry powder for inhalation. The physicochemical characteristics of this formulation was investigated together with aerosol performance, in vitro cell toxicity and transport studies, using a Calu-3 adenocarcinoma cell line grown using an air-interface model.
2. Materials and methods
2.1. Materials
Micronised quercetin hydrate (referred to as quercetin hereafter) and tristearin were supplied by Sigma Aldrich (Steinheim, Germany). Phosphatidylcholine was supplied by Cargill (Hamburg, Germany). Ammonium acetate was supplied by Ajax Finechem Pty Ltd. (Sydney, Australia). Acetic acid was purchased from AnalaR VWR International (Poole, England) and EDTA di-sodium salt was supplied by APS Finechem (Sydney, Australia).
The Calu-3 cell line (HTB-55) was purchased from the American Type Cell Culture Collection (ATTC, Rockville, USA). Dulbecco’s modified Eagle’s medium, fetal bovine serum, Hanks balanced salt solution, phosphate buffer saline, HEPES, trypsin–EDTA solution (2.5 g/L trypsin, 0.5 g/L EDTA), l-glutamine solution (200 mM), nonessential amino acids solution and CelLytic M Cell Lysis (50 mM Tris–HCl, pH 8, 150 mM NaCl, 1% NP-40, 0.5% sodium deoxycholate, 0.1% SDS) were supplied by Invitrogen (Sydney, Australia). Transwell cell culture supports (0.33 cm2 polyester, 0.4 μm pore size) were obtained from Corning Costar (Lowell, MA, USA).
All solvents were analytical grade and were obtained from Sigma (Sydney, Australia).
Water was purified by Milli-Q reverse Osmosis (Molsheim, France).
2.2. Methods
2.2.1. Preparation of the solid lipid microparticles
For the development of SLMs loaded with quercetin, melt o/w emulsification technique was employed, since it circumvents the use of organic solvents (Mezzena et al., 2009, Jaspart et al., 2005). This approach is environmentally friendly, but also eliminates the potential for residual solvent in the final dosage form. Quercetin (1 g) was dissolved into a melted (70–75 °C) lipid phase (3.6 g tristearin) and the phase inversion was obtained adding hot (70–75 °C) MilliQ water (50 mL), containing 0.7 g of phosphatidylcholine as surfactant. The mixture was maintained at 75 °C and was subjected to high-shear mixing (21,500 rpm for 2 min, using a T-25 Ultra-Turrax; IKA-Werk, Staufen, Germany). Additionally, the o/w emulsion was sonicated at a constant duty cycle (22 kHz) for 2 min, using a probe (Microson XL2000 Ultrasonic Cell Disruptor, Misonix, Farmingdale, NY) at a power input of 80 W. The emulsion was quickly cooled to a room temperature, using an ice bath and the formed microparticles recovered by freeze-drying at −50 °C (Hetosicc, Heto Lab Equipment, Saint-Julie, Canada).
The amount of quercetin entrapped in the SLMs was determined by heating (75°C for 2 min) and sonication (10 min) of the microparticles (20–25 mg) in ethanol in sealed glass vials. The obtained sample was diluted to volume (50 mL) with methanol, filtered and assayed by high performance liquid chromatography (HPLC).
2.2.2. Physical and chemical characterisation
2.2.2.1. Particle size analysis
The particle size distribution of the SLMs was analysed using laser diffraction (Malvern Mastersizer 2000, Malvern Instruments Ltd., UK). Samples of powder (ca. 10 mg) were dispersed using the Scirocco dry dispersion unit (Malvern, UK) with a feed pressure of 4 Bar and feed rate of 50%. Samples were analysed in triplicate, with an obscuration value between 0.3% and 10% and a reference refractive index of 1.553.
2.2.2.2. Scanning electron microscopy
The morphology of SLMs particles was studied using a field emission scanning electron microscope (Zeiss Ultra plus, Carl Zeiss Pty Ltd., Sydney, Australia). The samples were sputter coated with gold to a thickness of 15 nm, under an argon atmosphere prior to analysis. Samples were dispersed onto carbon sticky tabs and images were taken at random locations.
2.2.2.3. Differential scanning calorimetry
The thermal response of quercetin raw material and SLM powders were studied using differential scanning calorimetry (DSC 823e; Mettler-Toledo, Schwerzenbach, Switzerland).
Samples (3–5 mg) were crimp-sealed in DSC sample pans and exposed to a 10 °C min−1 temperature ramp between 40 and 400 °C. Exothermal and endothermic peak temperatures, onset temperature and heat of enthalpy (ΔH) for each peak were determined using STARe software V.9.0x (Mettler Toledo, Greifensee, Switzerland).
2.2.2.4. X-ray powder diffraction
The X-ray powder diffraction (XRPD) pattern for the SLMs was analysed using a D5000 X-ray powder diffractometer (Siemens, Munich, Germany). Measurements were conducted at 25 °C, using Cu Kα radiation at 30 mA and 40 kV, with angular increment of 0.04° s−1.
2.2.2.5. Dynamic Vapour Sorption
Dynamic Vapour Sorption (DVS) was used to investigate the relative moisture sorption and stability of the quercetin raw material and SLMs, with respect to humidity. Samples (ca. 15 mg) were added to glass sample pans, which were placed in the sample chamber of a DVS (DVS-1, Surface Measurement Systems Ltd., London, UK). Each sample was dried at 0% RH before being exposed to 10% RH increments for two 0–90% RH cycles (25 °C). Equilibrium moisture content at each humidity step was determined by a dm/dt of 0.0005% min−1.
2.2.3. HPLC method of quercetin quantification
Chemical analysis of quercetin was performed by High-Performance Liquid Chromatography (HPLC) using a Shimadzu Prominence UFLC system equipped with an SPD-20 A UV–Vis detector, LC-20AT solvent delivery unit, SIL-20A HT autosampler (Shimadzu Corporation, Japan) and NovaPak C18 column (5 μm, 150 × 3.9 mm, Waters, Ireland). The HPLC settings were as follow: detection wavelength 370 nm, flow rate 0.4 mL min−1, injection volume 100 μL, and retention time of 4.5 min. The mobile phase was a mixture of acetate buffer and acetonitrile (55: 45, v/v) and 1 mM EDTA. Standard linearity was obtained between 0.2 and 20 μg mL−1.
2.2.4. In vitro aerosol studies
The aerosolisation of quercetin SLMs were analysed using an Aerolizer® dry powder inhalation (DPI) device (Novartis, Surrey, UK) and a next generation impactor (NGI) (Copley Scientific, Nottingham, UK) according to the method specified for dry powder inhalers in the pharmacopoeia (British Pharmacopoeia, 2012). Briefly, prior to testing, all eight NGI collection cups were coated with silicon oil to eliminate particle bounce. 10 mg ± 0.1 mg of quercetin SLMs were weighed and filled in size 3 gelatine capsules (Capsugel, Sydney, Australia) and placed in the Aerolizer®. A mouthpiece adaptor fitted into a United States Pharmacopeia (USP) throat was used to connect the Aerolizer® to the NGI. The particles were aerolised at 60 L min−1 for 4 s. The device containing the capsule, throat and the stages were then washed separately with methanol and the samples were analysed using HPLC. The mass balance was calculated as the recovery from the stage deposition, capsule and device. In addition, the fine particle dose (FPD) (drug recovered from stages 3 to filter) (⩽4.46 μm) and the fine particle fraction (FPF) (FPD/Total dose × 100) were calculated.
2.2.5. Cell viability assay after exposure to quercetin SLMs
The toxicity of quercetin SLMs was assessed by measuring the viability of Calu-3 cells in a liquid covered culture, following 3 days drug exposure to increasing drug concentrations, as previously described (Haghi et al., 2010).
Briefly, 5 × 104 cells were seeded per well in a volume of 100 μL into a 96 well plate. Cells were incubated overnight at 37 °C in 5% CO2 atmosphere. After 24 h, 100 μL of increasing concentrations of quercetin SLMs were added to each well, and the drug was dissolved in ethanol and added to complete medium in a final ethanol concentration of ⩽1%. Untreated controls and solvent controls were included for each experiment. Plates were incubated for 72 h at 37 °C in a humidified atmosphere with 5% CO2. Cells were then analysed for cell viability. Briefly, 20 μL of CellTiter 96® Aqueous assay (MTS reagent) (Promega, USA) was added to each well and the plates incubated for 3 h at 37 °C in humidified 5% CO2 atmosphere. Absorbance was measured at 492 nm using a POLARstar Optima (BMG Labtech, Offenburg, Germany). The absorbance value was directly proportional to cell viability (%). Data were expressed as % cell viability [(average absorbance of treated wells/average absorbance of control wells) × 100]. The half maximal inhibitory concentration (IC50) values were defined as the drug concentration that produces a decrease of 50% in cell viability compared to the untreated control. IC50 values were calculated by plotting (%) cell viability against the concentrations (ng mL−1) on a logarithmic scale. Data was fitted to the Hill equation using the General Fit function of KaleidaGraph 4.1 software. Each experiment was performed in triplicate.
In addition, measurement of the transepithelial electrical resistance (TEER) was performed using EVOM voltohmmeter (World Precision Instrument, USA) connected to STX-2 chopstick electrodes. 10 measurements were taken per well after the experiment to confirm the maintenance of barrier integrity over 4 h of experiment. Subtracting the resistance of a cell-free insert and correcting the value for the surface area of the Transwell calculated the resistance.
2.2.6. In vitro drug diffusion/transport studies using air interface Calu-3 cell culture
The transport of quercetin from the SLMs was studied using a Calu-3 lung epithelial model. The culture conditions for the Calu-3 cell air interface model were as previously described (Haghi et al., 2010). Briefly, Calu-3 cells were grown and subcultured in Dulbecco’s Modified Eagle’s medium (F-12 containing 10% (v/v) fetal calf serum, 1% (v/v) non essential amino acid solution and 1% (v/v) L-glutamine solution). Cells were then seeded on Transwell polyester inserts at a density of 5 × 105 cells cm−2. After 24 h, medium was removed from the apical chamber and the basolateral medium replaced every alternate day with fresh medium to establish an air-interface model over 12–14 days. Prior to transport studies the viability and integrity of the cell monolayer with respect to quercetin SLMs was evaluated.
A modified in vitro aerosol testing apparatus (twin stage impinger TSI, Radleys, Essex, UK) that allows the attachment of a Transwell containing Calu-3 epithelial cells was used to study the mechanism of drug deposition, dissolution and diffusion/transport (Haghi et al., 2010, Haghi et al., 2012). Before the drug transport studies, the TSI flow rate was set to 60 L min−1 using a rotary vein pump and a calibrated flow meter. The quercetin SLM sample was weighed (1 mg ± 0.05 mg) into a size 3 gelatine capsules, which was then insert into an Aerolizer® device and the pump activated for 4 s to disperse the powder. The TSI was then disassembled and the Transwell removed. After deposition of the powder, the Transwell was placed into a 24 well plate containing 300 μL modified buffer (HBSS supplemented with HEPES (1% v/v), and ethanol 97% (1% v/v) at pH 7.4) to measure the quercetin transport.
At 30 min time points the Transwells were moved to new well containing fresh modified buffer. After 4 h the surface of the monolayer was washed with transport buffer to account for the drug remaining on cell surface and the cells were lysed with Cell Lytic solution to allow the measurement of the drug in the cells. The lysates were centrifuged at 10,000 rpm for 10 min at 4 °C. The supernatant was collected and diluted to an appropriate volume. All the samples were analysed by HPLC. The initial amount deposited on the cell layer was calculated from the sum of the drug passed through the cell monolayer, the mass retained on the monolayer at the end of the experiment and the mass of drug inside the cells. Experiments were randomised for dose and repeated three times.
2.2.7. Statistical analysis
Data was subjected to statistical analysis (SPSS 17.0), using ANOVA one-way analysis to examine for significant difference. Significant differences between formulations were analysed using multiple comparisons (Tukeys post hoc test) and P values of <0.05 were considered to be significant.
3. Results
3.1. Physicochemical characteristics of quercetin solid lipid microparticles
For the preparation of the SLMs, tristearin and hydrogenated phosphatidylcholine were selected respectively as lipidic material and surfactant, based on a previous study on the development of quercetin-loaded lipid microparticles for dermal application (Scalia and Mezzena, 2009). In addition, phosphatidylcholine is a physiological compatible emulsifier (phosphatidylcholine is the major component of lung endogenous surfactant). The quercetin content of the SLMs was 15.5% w/v ± 0.6, which corresponded to an encapsulation efficiency of 71.4% (encapsulation efficiency is based on the recovered amount of quercetin in the microparticles as a function of the theoretical amount present in the powder when taking into account the excipients content) .
3.1.1. Particle size analysis
The particle size distribution of the as supplied micronised quercetin and quercetin SLMs are shown in Fig. 1 with analysis of the data indicating median volume diameters (d 0.5) of 2.28 ± 0.03 μm and 2.90 ± 0.30 μm, respectively. Further analysis suggested 90% of the SLMs had a diameter ⩽11.08 ± 1.09 μm.
Fig. 1.
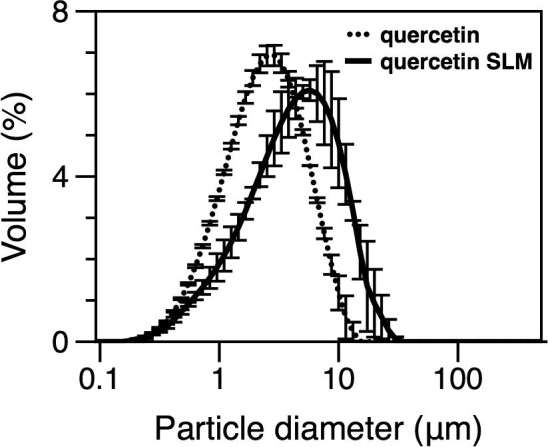
Particle size distribution of raw quercetin and quercetin SLM measured using dry dispersion system of laser diffraction. Data represent mean ± SD (n = 3).
3.1.2. Scanning electron microscopy
Scanning electron microscopy images of the SLMs and as-supplied quercetin are shown in Fig. 2 A and B, respectively. In general the SLMs particles had a spherical morphology and a size in line with particle size analysis, while raw quercetin was columnar in shape and larger than 10 μm. It is important to note that particle size data is represented as volume distribution and makes a series of assumptions (i.e. uniform spheres), while SEM is a ‘morphological’ technique. This is reflected by the differences observed in particle size when compared with SEM images, where particles appear to have an elongated or plate-like morphology. Particle size distribution for the SLMs was of an appropriate size for respiratory delivery (Patton, 1999) and similar to that measured using laser diffraction.
Fig. 2.
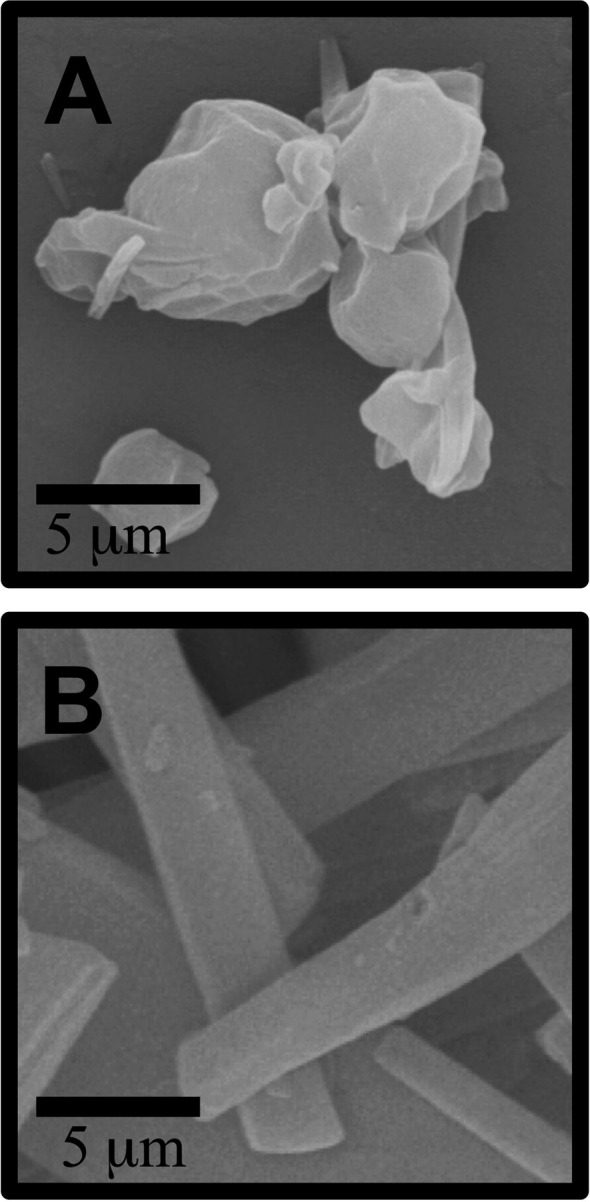
Scanning electron micrographs of quercetin SLMs (A) and raw quercetin (B).
3.1.3. Differential scanning calorimetry
The thermal response of the SLM components; tristearin, phosphatidylcholine and quercetin, as well as the prepared SLMs are displayed in Fig. 3 . Tristearin is a commercial monoacid triglyceride. Generally, triglycerides exhibit three different polymorphic forms characterised by particular chain packing and thermal stability: alpha (α), beta-prime (β′), and beta (β) (Hernqvist, 1990). In this specific experiment, tristearin presented an endotherm corresponding to the melting of the β phase at 63.75 °C, similar to previous literature (Lutton, 1945). Phosphatidylcholine is a surface-active molecule. Its transition temperature from crystalline to mesomorphic (liquid crystalline) was visible at around 84.22 °C, in agreement with previously reported values (Rutven and McElhaney, 2011).
Fig. 3.
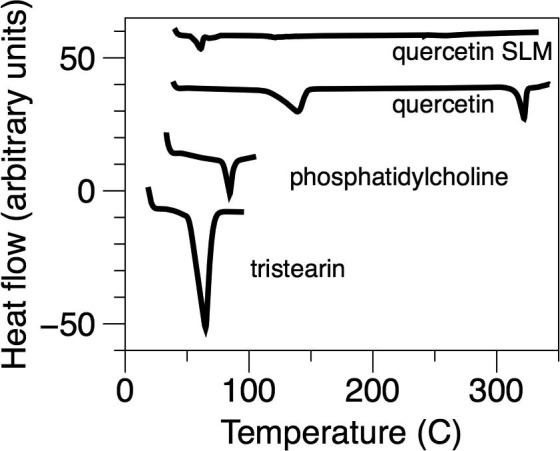
Differential scanning calorimetric thermograms of quercetin SLM, quercetin raw material, phosphatidylcholine and tristearin.
The DSC thermogram of quercetin raw material exhibited an endothermic peak at 321 °C, typical of melting, in line with literature data (Borghetti et al., 2009). Another smaller endothermic peak is visible at around 137 °C related to a decomposition process with water loss (Da Costa et al., 2002).
The DSC thermogram of the prepared SLMs showed a noticeable reduction in the melting point in comparison with quercetin raw material, followed by an endothermic response. These results are supported by various previous studies conducted on the phospholipid complexes of some phytoconstituents such as silybin, puerarin curcumin, naringenin and gallic acid (Maiti et al., 2007, Semalty et al., 2010). It is hypothesised that the main exothermic event is due to the melting of the primary excipient, tristearin and the simultaneous dissolution of the drug and phospholipid in the melt. The significance of the DSC data is that the quercetin appears incorporated into the matrix; an essential requirement with respect to stability and release profile modification.
3.1.4. X-ray powder diffraction
The diffractogram of raw quercetin and quercetin SLMs measured using XRPD is shown in Fig. 4 . The XRPD pattern of the starting material indicated a highly crystalline structure, as evident from the sharp peaks observed at 14, 16, and 27 of 2θ values. This was in good agreement with a previous study of quercetin (Sri et al., 2007). In comparison, the SLMs had no characteristic peaks of a crystalline structure suggesting the particles to be amorphous. The incorporation of the drug into the lipid matrix is likely to enhance stability of the drug and control release after deposition. This is reflected in the DVS and in vitro experiments presented in Sections 3.1.5, 3.4, respectievely.
Fig. 4.
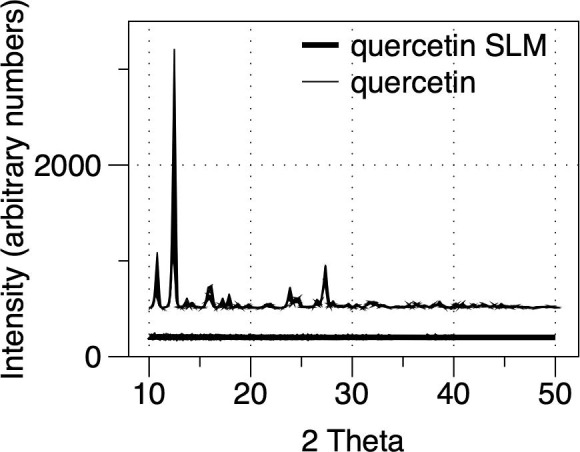
The X-ray powder diffractogram of raw quercetin and quercetin SLMs.
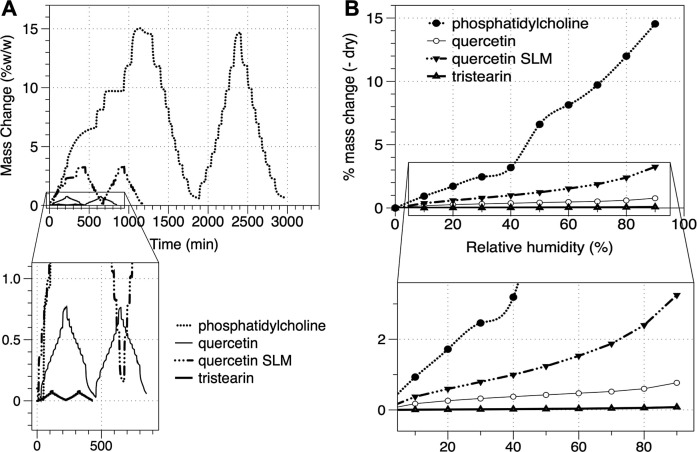
3.1.5. Dynamic Vapour Sorption
Dry powder inhalers are inherently susceptible to moisture sorption and thus elevated relative humidity (RH). To further study the SLMs, the powders were exposed to two 0–90% RH cycles using a DVS. Time vs. mass plots as a function of humidity are shown in Fig. 5 A while the moisture sorption isotherm for the first humidity ramp (cycle 1) is shown in Fig. 5B. In general, all of the formulation components were reversible in terms of moisture sorption/desorption suggesting no irreversible polymorphic change or crystalisation phenomena. The moisture sorption was highest for phosphatidylcholine (14.5% at 90% RH) compared with 0.8% and 0.1% for quercetin and tristearin, respectively. The moisture sorption of the SLMs was 3.3% at 90% RH. The reduction in moisture sorption for the SLMs in comparison to the phosphatidylcholine (which equates for ∼13% of the SLM particle mass) is most likely due to the contributing effects of the drug and tristearin (which make up the majority of the particle) and the presence of phosphatidylcholine on the surface of the particles (contributing to the high humidity sorption of SLMs).
Fig. 5.
Mass change as a function of time for quercetin SLM, quercetin, phosphatidylcholine and tristearin (A) DVS isotherm of the first cycle sorption for quercetin SLM, quercetin, phosphatidylcholine and tristearin (B). Zoomed in area in front view.
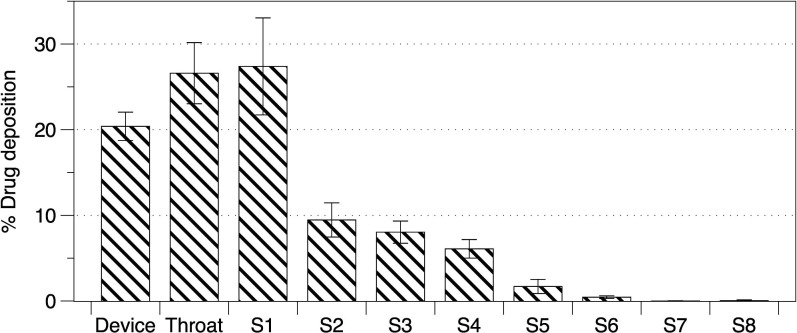
3.2. In vitro aerosolisation studies
The aerosolisation performance of quercetin SLMs was studied using the NGI and the data is presented in Fig. 6 . Analysis of the stage deposition data, capsule and device recovery indicated that 96.87% ± 1.51% of the loaded dose was recovered across all stages (indicating good mass balance). In addition, the fine particle dose (FPD) and fine particle fraction (FPF) were calculated to be 316.2 ± 52.3 μg and 20.5 ± 3.3%. The FPD and FPF represented the dose and percentage drug concentrations with an aerodynamic diameter less than 4.46 μm, suitable for inhalation delivery.
Fig. 6.
Quercetin SLMs aerosol deposition by next generation impaction. S1–S8 represents NGI stages cut off diameters: S1 > 8.06; S2 > 4.46; S3 > 2.82; S4 > 1.66; S5 > 0.94; S6 > 0.55; S7 > 0.34; S8 > 0.34 μm, respectively.
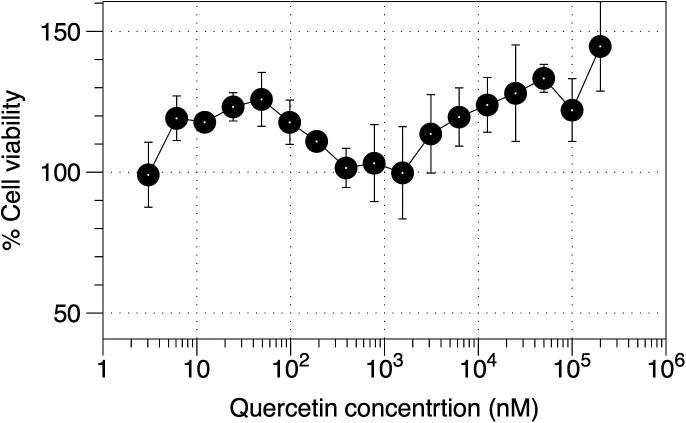
3.3. Cell viability assay
The dose response cytotoxicity profile of quercetin SLMs on Calu-3 cells was established and is shown in Fig. 7 . Calu-3 cell cultures were exposed to a range of SLMs concentrations (from a minimum of 0.15 nM to a maximum of 200,000 nM) over a 72 h treatment period. Cells viability was calculated with reference to the untreated cells, where average absorbance was normalised to 100% viability. The viability assay demonstrated that Calu-3 cells could tolerate a wide range of quercetin concentrations. The IC50 value could not be determined across the concentration range and thus, the SLMs should be considered non-toxic for Calu-3 cells.
Fig. 7.
The effect of quercetin SLMs on Calu-3 cell viability after 72 h drug treatment. Data represent mean ± SD (n = 3).
TEER of the Calu-3 monolayer was measured after 240 min of exposure to quercetin, quercetin SLMs, tristearin and phosphatidylcholine. This was performed to determine if any of the components in the formulation could change the integrity of the epithelial cells. It was found that there was no significant difference (P > 0.05) between the control cells and cells treated with quercetin (550 ± 40 Ω cm2), quercetin SLMs (550 ± 30 Ω cm2), tristearin (580 ± 30 Ω cm2), phosphatidylcholine (600 ± 55 Ω cm2) or co-deposition of tristearin and phosphatidylcholine (560 ± 23 Ω cm2).
Although to the authors’ knowledge, no previous viability studies have used Calu-3 epithelial cells, flavonoids are ubiquitous in the human diet, are highly bioavailable, and have been extensively studied with regard to their pharmacology and toxicology (Rossand and Kasum, 2002).
Furthermore, multiple laboratory clinical trials point to an excellent safety profile of quercetin, including studies using systemic, oral, and intravenous administration (Hard et al., 2007). Consequently in this study it could safely be assumed that quercetin SLMs are not toxic for the concentrations studied.
3.4. In vitro drug diffusion/transport studies using an air interface Calu-3 cell culture
The percentage of drug transported through the Calu-3 cell grown on the Transwell in the AIC configuration and attached to the modified TSI apparatus is shown in Fig. 8 . Drug concentrations were measured and expressed in terms of percent total recovery throughout the experiments and data was plotted as mean cumulative percentage (±standard deviation) of drug transport over 4 h. Data analysis demonstrates a linear kinetic profile, with a maximum of 22.32 ± 1.51% drug transported after 4 h from SLM formulation. Importantly, quercetin was not detectable in the basal chamber 4 h after deposition of the micronised quercetin micro particles. Such observations suggest that the rate-limiting step in uptake of quercetin SLMs was linked to the solubility, presumably due to the amorphous nature of quercetin trapped within the solid lipid matrix, since the flux is independent of quercetin concentration remaining on the cell monolayer.
Fig. 8.
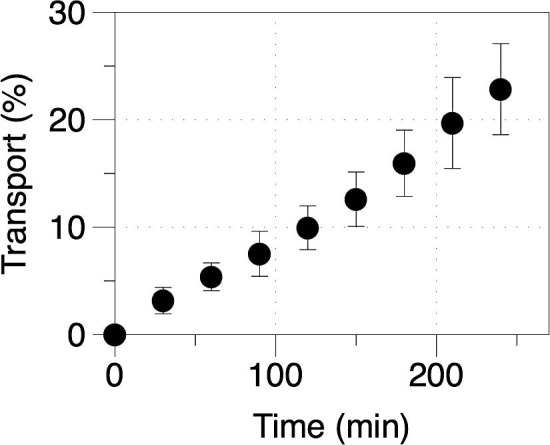
Release profiles of quercetin SLMs using a modified TSI air-interface Calu-3 cell model. Data represent mean ± SD (n = 3).
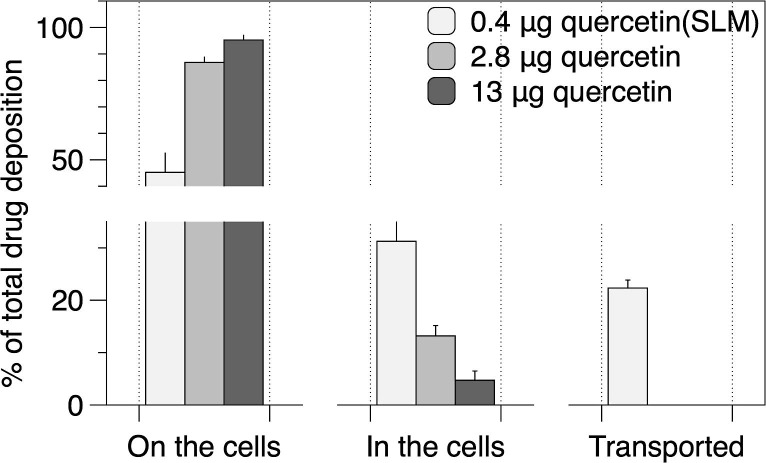
After deposition of SLMs on the Calu-3 cells grown in the AIC model, the concentration of quercetin transported into the basal compartment at set time points was measured and the cumulative mass and percentage transport calculated. Fig. 9 depicts the percentage of drug transported, remaining on the cells and trapped within the cells, from the single quercetin and quercetin SLMs.
Fig. 9.
Percentage of total drug remaining on the cell surface, inside the cells or transported to the basal chamber after 4 hours. Data represent mean ± SD (n = 3).
After 240 min 45.26 ± 7.23% of quercetin SLMs and >86.79 ± 1.96% of quercetin alone was still found to be on the cells surface, while 31.25 ± 7.40% and 13.20 ± 1.96% (from SLM formulation and quercetin alone, respectively) was found ‘trapped’ inside the cells. Only 22.32 ± 1.51% of drug from the SLM formulation was transported across the Calu-3 and was found in the basal compartment. No quercetin raw material was transported to the basal compartment.
4. Discussion
Phosphatidylcholine has previously been shown to have skin penetration enhancing characteristics in other studies (Saija et al., 1998). Specifically, a previous study has also shown that didecanoyl-l-alpha-phosphatidylcholine enhances the nasal absorption of insulin, in an in vitro rabbit nasal mucosa model, by facilitating a paracellular passage through a reversible opening of tight junctions (Carstens et al., 1993). Here we studied the deposition and transport of both quercetin SLM and micronised quercetin, alone. The quantities deposited were different between the SLM (0.4 μg) and micronised material (2.8 μg) since we attempted to achieve equivalent deposited masses of powder at the epithelia (i.e. including the lipid components). In addition, the higher mass of micronised sample was additionally tested to study if micronised material would be transported at all.
Only quercetin from SLM produced any epithelial transport across the cell line (although some internalization of quercetin was observed for the micronized samples). The enhancement effect achieved by the lipid microparticles could be traced to a more effective delivery of quercetin to the cells due to increased contact surface between the encapsulated substance and the cells. In addition, since the lipid microparticles enable slow release of quercetin at the cell surface over time, the extent of decomposition/oxidative degradation is reduced compared to the free drug, which is immediately available.
Lipid carrier with incorporated drugs has been demonstrated to increase the absorption and circulation in the body versus stand-alone compounds (Maeda, 2001). For nontoxic enhancers that have proven successful in in vivo studies, additional mechanisms to paracellular enhancement have been suggested (Gizurarson and Bechgaard, 1991). For instance, increased cell membrane permeability caused by enhancer incorporation into the luminal cell membrane has been suggested (Muranishi, 1990), but how this could induce drug transcellular absorption is unclear.
Although this study indicates that the absorption of quercetin is enhanced by the presence of phosphatidylcholine or tristearin, the real mechanism is still unclear. It is possible that the phospholipid may be incorporated into the luminal cell membrane, and this may constitute the primary step in the mechanism by which phosphatidylcholine affects tight junction permeability. Furthermore, changes in the lipid environment of the cell membrane may affect the basic transport properties of the Calu-3 epithelium. Additional studies are needed to evaluate this possibility.
5. Conclusions
This study has investigated the formulation and aerosol delivery to the lung of solid lipid quercetin microparticles as a potential active pharmaceutical ingredient for asthma therapy. We have demonstrated SLM particle technology can be used to deliver this naturally derived flavonoid for the treatment of range of respiratory diseases. The effect of the absorption enhancing non-toxic excipients in increasing the permeability of quercetin has also been highlighted; making this approach significant, since the raw micronised quercetin was not transported across epithelia. To the authors knowledge no previous studies have investigated quercetin transport mechanism using Calu-3 cell epithelial monolayer. This is an important aspect of the study since the lung epithelia will be the first barrier after deposition in the airways. Further studies are necessary to elucidate the exact mechanism.
Due to the natural physiological composition of the quercetin and its components in the final SLMs, this system has the potential to be used as a ‘bio-compatible’ delivery system to modulate the release of inhaled dry powder formulations.
References
- Asano J., Niisato N., Nakajima K., Miyazaki H., Yasuda M., Iwasaki Y., Hama T., Dejima K., Hisa Y., Marunaka Y. Quercetin stimulates Na+/K+/2Cl− cotransport via PTK-dependent mechanisms in human airway epithelium. Am. J. Respir. Cell Mol. Biol. 2009;41:688–695. doi: 10.1165/rcmb.2008-0338OC. [DOI] [PubMed] [Google Scholar]
- Borghetti G.S., Lula I.S., Sinisterra R.D., Bassani V.L. Quercetin/beta-cyclodextrin solid complexes prepared in aqueous solution followed by spray-drying or by physical mixture. AAPS PharmSciTech. 2009;10:235–242. doi: 10.1208/s12249-009-9196-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstens S., Danielsen G., Guldhammer B., Frederiksen O. Transport of insulin across rabbit nasal mucosa in vitro induced by didecanoyl-l-alpha-phosphatidylcholine. Diabetes. 1993;42:1032–1040. doi: 10.2337/diab.42.7.1032. [DOI] [PubMed] [Google Scholar]
- Chen L., Li J., Luo C., Liu H., Xu W., Chen G., Liew O.W., Zhu W., Puah C.M., Shen X., Jiang H. Binding interaction of quercetin-3-beta-galactoside and its synthetic derivatives with SARS-CoV 3CL(pro): structure-activity relationship studies reveal salient pharmacophore features. Bioorgan. Med Chem. 2006;14:8295–8306. doi: 10.1016/j.bmc.2006.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang L.C., Chiang W., Liu M.C., Lin C.C. In vitro antiviral activities of Caesalpinia pulcherrima and its related flavonoids. J. Antimicrob. Chemother. 2003;52:194–198. doi: 10.1093/jac/dkg291. [DOI] [PubMed] [Google Scholar]
- Da Costa E.M., Barbosa J.M., Do Nascimento T.G., Macedo R.O. Thermal characterization of the quercetin and rutin flavonoids. Thermochim. Acta. 2002;392:79–84. [Google Scholar]
- Davis J.M., Murphy E.A., McClellan J.L., Carmichael M.D., Gangemi J.D. Quercetin reduces susceptibility to influenza infection following stressful exercise. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008;295:R505–R509. doi: 10.1152/ajpregu.90319.2008. [DOI] [PubMed] [Google Scholar]
- Debiaggi M., Tateo F., Pagani L., Luini M., Romero E. Effects of propolis flavonoids on virus infectivity and replication. Microbiologica. 1990;13:207–213. [PubMed] [Google Scholar]
- Dellamary L., Smith D.J., Bloom A., Bot S., Guo G.R., Deshmuk H., Costello M., Bot A. Rational design of solid aerosols for immunoglobulin delivery by modulation of aerodynamic and release characteristics. J. Control. Release. 2004;95:489–500. doi: 10.1016/j.jconrel.2003.12.013. [DOI] [PubMed] [Google Scholar]
- Dimova S., Mugabowindekwe R., Willems T., Brewster M.E., Noppe M., Ludwig A., Jorissen M., Augustijns P. Safety-assessment of 3-methoxyquercetin as an antirhinoviral compound for nasal application: effect on ciliary beat frequency. Int. J. Pharm. 2003;263:95–103. doi: 10.1016/s0378-5173(03)00363-6. [DOI] [PubMed] [Google Scholar]
- Formica J.V., Regelson W. Review of the biology of Quercetin and related bioflavonoids. Food Chem. Toxicol. 1995;33:1061–1080. doi: 10.1016/0278-6915(95)00077-1. [DOI] [PubMed] [Google Scholar]
- Gang W., Jie W.J., Ping Z.L., Ming du S., Ying L.J., Lei W., Fang Y. Liposomal quercetin: evaluating drug delivery in vitro and biodistribution in vivo. Expert Opin. Drug Deliv. 2012;9:599–613. doi: 10.1517/17425247.2012.679926. [DOI] [PubMed] [Google Scholar]
- Gizurarson S., Bechgaard E. Intranasal administration of insulin to humans. Diabetes Res. Clin. Pract. 1991;12:71–84. doi: 10.1016/0168-8227(91)90083-p. [DOI] [PubMed] [Google Scholar]
- Graefe E.U., Wittig J., Mueller S., Riethling A.K., Uehleke B., Drewelow B., Pforte H., Jacobasch G., Derendorf H., Veit M. Pharmacokinetics and bioavailability of quercetin glycosides in humans. J. Clin. Pharmacol. 2001;41:492–499. doi: 10.1177/00912700122010366. [DOI] [PubMed] [Google Scholar]
- Haghi M., Young P.M., Traini D., Jaiswal R., Gong J., Bebawy M. Time- and passage-dependent characteristics of a Calu-3 respiratory epithelial cell model. Drug Dev. Ind. Pharm. 2010;36:1207–1214. doi: 10.3109/03639041003695113. [DOI] [PubMed] [Google Scholar]
- Haghi M., Traini D., Bebawy M., Young P.M. Deposition, diffusion and transport mechanism of dry powder microparticulate salbutamol, at the respiratory epithelia. Mol. Pharm. 2012;9:1717–1726. doi: 10.1021/mp200620m. [DOI] [PubMed] [Google Scholar]
- Hard G.C., Seely J.C., Betz L.J., Hayashi S.M. Re-evaluation of the kidney tumors and renal histopathology occurring in a 2-year rat carcinogenicity bioassay of quercetin. Food Chem. Toxicol. 2007;45:600–608. doi: 10.1016/j.fct.2006.10.018. [DOI] [PubMed] [Google Scholar]
- Heijnen C.G., Haenen G.R., van Acker F.A., van der Vijgh W.J., Bast A. Flavonoids as peroxynitrite scavengers: the role of the hydroxyl groups. Toxicol. In Vitro. 2001;15:3–6. doi: 10.1016/s0887-2333(00)00053-9. [DOI] [PubMed] [Google Scholar]
- Hernqvist L. Polymorphism of Triglycerides – a Crystallographic review. Food Struct. 1990;9:39–44. [Google Scholar]
- Jaspart S., Piel G., Delattre L., Evrard B. Solid lipid microparticles: formulation, preparation, characterisation, drug release and applications. Expert Opin. Drug Deliv. 2005;2:75–87. doi: 10.1517/17425247.2.1.75. [DOI] [PubMed] [Google Scholar]
- Joskova M., Franova S., Sadlonova V. Acute bronchodilator effect of quercetin in experimental allergic asthma. Bratisl. Lek. Listy. 2011;112:9–12. [PubMed] [Google Scholar]
- Kakran M., Shegokar R., Sahoo N.G., Shaal L.A., Li L., Muller R.H. Fabrication of quercetin nanocrystals: comparison of different methods. Eur. J. Pharm. Biopharm. 2012;80:113–121. doi: 10.1016/j.ejpb.2011.08.006. [DOI] [PubMed] [Google Scholar]
- Kaul T.N., Middleton E., Ogra P.L. Antiviral effect of flavonoids on human viruses. J. Med. Virol. 1985;15:71–79. doi: 10.1002/jmv.1890150110. [DOI] [PubMed] [Google Scholar]
- Li W.G., Zhang X.Y., Wu Y.J., Tian X. Anti-inflammatory effect and mechanism of proanthocyanidins from grape seeds. Acta Pharmacol. Sin. 2001;22:117–1120. [PubMed] [Google Scholar]
- Li H., Zhao X., Ma Y., Zhai G., Li L., Lou H. Enhancement of gastrointestinal absorption of quercetin by solid lipid nanoparticles. J. Control. Release. 2009;133:238–244. doi: 10.1016/j.jconrel.2008.10.002. [DOI] [PubMed] [Google Scholar]
- Lutton E.S. The polymorphism of tristearin and some of its homologs. J. Am. Chem. Soc. 1945;67:524–527. [Google Scholar]
- Maeda H. The enhanced permeability and retention (EPR) effect in tumor vasculature: the key role of tumor-selective macromolecular drug targeting. Adv. Enzyme Regul. 2001;41:189–207. doi: 10.1016/s0065-2571(00)00013-3. [DOI] [PubMed] [Google Scholar]
- Maiti K., Mukherjee K., Gantait A., Saha B.P., Mukherjee P.K. Curcumin-phospholipid complex: Preparation, therapeutic evaluation and pharmacokinetic study in rats. Int. J. Pharmaceut. 2007;330:155–163. doi: 10.1016/j.ijpharm.2006.09.025. [DOI] [PubMed] [Google Scholar]
- Mezzena M., Scalia S., Young P.M., Traini D. Solid lipid budesonide microparticles for controlled release inhalation therapy. AAPS J. 2009;11:771–778. doi: 10.1208/s12248-009-9148-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon H., Choi H.H., Lee J.Y., Moon H.J., Sim S.S., Kim C.J. Quercetin inhalation inhibits the asthmatic responses by exposure to aerosolized-ovalbumin in conscious guinea-pigs. Arch. Pharm. Res. 2008;31:771–778. doi: 10.1007/s12272-001-1225-2. [DOI] [PubMed] [Google Scholar]
- Moon Y.J., Wang L., DiCenzo R., Morris M.E. Quercetin pharmacokinetics in humans. Biopharm. Drug Dispos. 2008;29:205–217. doi: 10.1002/bdd.605. [DOI] [PubMed] [Google Scholar]
- Muranishi S. Absorption enhancers. Crit. Rev. Ther. Drug Carrier Syst. 1990;7:1–33. [PubMed] [Google Scholar]
- Nijveldt R.J., Van Nood E., Van Hoorn D.E., Boelens P.G., Van Norren K., Van Leeuwen P.A. Flavonoids: a review of probable mechanisms of action and potential applications. Am. J. Clin. Nutr. 2001;74:418–425. doi: 10.1093/ajcn/74.4.418. [DOI] [PubMed] [Google Scholar]
- Park H.J., Lee C.M., Jung I.D., Lee J.S., Jeong Y.I., Chang J.H., Chun S.H., Kim M.J., Choi I.W., Ahn S.C., Shin Y.K., Yeom S.R., Park Y.M. Quercetin regulates Th1/Th2 balance in a murine model of asthma. Int. Immunopharmacol. 2009;9:261–267. doi: 10.1016/j.intimp.2008.10.021. [DOI] [PubMed] [Google Scholar]
- Patton J.S. Inhalation delivery of therapeutic peptides and proteins. J. Aerosol Med. 1999;12:45–46. doi: 10.1089/jam.1999.12.45. [DOI] [PubMed] [Google Scholar]
- Pettinari A., Amici M., Cuccioloni M., Angeletti M., Fioretti E., Eleuteri A.M. Effect of polyphenolic compounds on the proteolytic activities of constitutive and immuno-proteasomes. Antioxid. Redox Signal. 2006;8:121–129. doi: 10.1089/ars.2006.8.121. [DOI] [PubMed] [Google Scholar]
- B. Pharmacopoeia, British Pharmacoloeia 2012, Online: vol. III, TSO, Information & publishing solutions, Norwich, UK, 2012.
- Robaszkiewicz A., Balcerczyk A., Bartosz G. Antioxidative and prooxidative effects of quercetin on A549 cells. Cell Biol. Int. 2007;31:1245–1250. doi: 10.1016/j.cellbi.2007.04.009. [DOI] [PubMed] [Google Scholar]
- Rossand J.A., Kasum C.M. Dietary flavonoids: bioavailability, metabolic effects, and safety. Ann. Rev. Nutr. 2002;22:19–34. doi: 10.1146/annurev.nutr.22.111401.144957. [DOI] [PubMed] [Google Scholar]
- N.A.H. Rutven, R. McElhaney, The mesomorphic phase behaviour of lipid bilayers, The structure of biological membranes, vol. 1, CRC Press, 2011, p. 19–89.
- Saija A., Tomaino A., Trombetta D., Giacchi M., De Pasquale A., Bonina F. Influence of different penetration enhancers on in vitro skin permeation and in vivo photoprotective effect of flavonoids. Int. J. Pharm. 1998;175:85–94. [Google Scholar]
- Sanna V., Kirschvink N., Gustin P., Gavini E., Roland I., Delattre L., Evrard B. Preparation and in vivo toxicity study of solid lipid microparticles as carrier for pulmonary administration. AAPS PharmSciTech. 2004;5:e27. doi: 10.1208/pt050227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scalia S., Salama R., Young P.M., Traini D. Preparation and in vitro evaluation of salbutamol-loaded lipid microparticles for sustained release pulmonary therapy. J. Microencapsul. 2012;29:225–233. doi: 10.3109/02652048.2011.646326. [DOI] [PubMed] [Google Scholar]
- Scalia S., Mezzena M. Incorporation of quercetin in lipid microparticles: effect on photo- and chemical-stability. J. Pharm. Biomed. Anal. 2009;49:90–94. doi: 10.1016/j.jpba.2008.10.011. [DOI] [PubMed] [Google Scholar]
- Semalty A., Semalty M., Singh D., Rawat M.S.M. Preparation and characterization of phospholipid complexes of naringenin for effective drug delivery. J. Incl. Phenom. Macro. 2010;67:253–260. [Google Scholar]
- Sri K.V., Kondaiah A., Ratna J.V., Annapurna A. Preparation and characterization of quercetin and rutin cyclodextrin inclusion complexes. Drug Dev. Ind. Pharm. 2007;33:245–253. doi: 10.1080/03639040601150195. [DOI] [PubMed] [Google Scholar]
- Wu M.J., Wang L., Ding H.Y., Weng C.Y., Yen J.H. Glossogyne tenuifolia acts to inhibit inflammatory mediator production in a macrophage cell line by downregulating LPS-induced NF-kappa B. J. Biomed. Sci. 2004;11:186–199. doi: 10.1007/BF02256562. [DOI] [PubMed] [Google Scholar]