Abstract
Rhinitis is often seen as posing a small burden. However, rhinitis is a complex disease that is underpinned by a plethora of different mechanisms and causes. Rhinitis is frequently associated with other comorbid conditions but, by itself, is a source of considerable morbidity for patients and creates a significant financial burden on health systems worldwide. This article approaches this condition from both a phenotypic and mechanistic standpoint, focusing on the complexity of characterizing these subtypes. Developing a clearer demarcation of the currently obscure rhinitis phenotypes and endotypes will substantially improve their future prevention and treatment.
Keywords: Rhinitis, Endotypes, Phenotypes, Pathophysiology, Symptoms
Key points
-
•
Rhinitis endotypes are as numerous and diverse as the disease’s phenotypes and are largely overlapping, making a clear demarcation challenging.
-
•
Some rhinitis phenotypes previously considered important are now thought to be less relevant because of advances that have been made in understanding rhinitis subtypes.
-
•
Consensus classification of rhinitis subsets is still an unmet need.
-
•
Chronic rhinitis is a far more complex and burdensome condition than is generally acknowledged, and there is considerable need for research to better understand the pathobiology of nonallergic rhinitis and its interaction with allergic rhinitis.
Introduction
Chronic rhinitis (CR) is defined as an inflammation of the nasal mucosa, characterized by 2 or more symptoms of nasal congestion/obstruction, anterior or posterior rhinorrhea, and sneezing and itching for at least 1 hour daily and for more than 2 weeks.1 CR is a prevalent pathologic condition with widespread morbidity associated with a considerable financial burden on health care systems.2, 3 Its economic impact is further magnified because it is a risk factor for other comorbidities in adults, such as sinusitis and asthma, and also a precursor to serious conditions in children, such as learning disabilities, behavioral deviation, and psychological impairment.3, 4 Nevertheless, it is an underestimated and often trivialized disease, often viewed as no more than a mere annoyance. Furthermore, the high variability in both underlying pathophysiologic mechanisms (endotypes) and clinical presentations (phenotypes) of CR has hindered efforts to develop clear guidelines for its diagnosis and treatment. Even the term rhinitis has been criticized because it connotes inflammation, whereas certain rhinitis endotypes seem to be devoid of an inflammatory component.5
The 3 most widely accepted rhinitis subgroups thus far are allergic rhinitis (AR), infectious rhinitis, and nonallergic noninfectious rhinitis (NAR).1 However, this classification may be an oversimplification, because a combined (mixed) phenotype exists in many patients.3, 6 In addition, there are numerous, mostly overlapping classification systems based on independent criteria such as age of onset, disease severity, symptoms, symptom pattern/frequency, causative agents, and underlying pathophysiology. For instance, from a clinical perspective, patients are classified as blockers, with nasal congestion as the prominent symptom, and runners, with rhinorrhea being predominant. Also, rhinitis caused by mechanical/structural abnormalities is included in the NAR subgroup by some investigators7, 8 and excluded by others.9 Furthermore, occupational rhinitis can be either allergic or nonallergic, blurring the boundaries between the 3 widely accepted categories.10 Characterization of rhinitis phenotypes is further hampered by the scarcity of distinct biomarkers. Even for allergic rhinitis, for which the immunopathogenesis is more clearly delineated, clinical classification as proposed by Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines are frequently not adhered to by treating physicians who still do not prescribe or modify treatment based on phenotypic characteristics (eg, frequency or disease severity), contrary to the ARIA guidelines.11, 12, 13, 14 These studies underscore the difficulty of using only the phenotype concept to classify CR and highlight the importance of developing a classification system that focuses on rhinitis endotypes.15
Subtypes, endotypes, and definitions
Rhinosinusitis and Overlapping Subtypes
Rhinitis frequently coexists with sinusitis because the nose and sinuses share vascular, neuronal, and anatomic pathways. Therefore, the term rhinosinusitis is preferred in patients with symptomatic sinus inflammation.16 Rhinosinusitis can be acute or chronic.1
The acute form of rhinosinusitis is infectious and predominantly of viral origin (around 90% of cases17, 18), with the usual causes being rhinovirus (common cold), coronavirus, adenovirus, parainfluenza virus, respiratory syncytial virus, or enterovirus. It is common that an acute viral rhinosinusitis is complicated by secondary bacterial superinfection that establishes a bacterial rhinosinusitis endotype (eg, Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis).
The chronic rhinosinusitis phenotype is more complicated for establishing a defined endotype because infection has a minor, if any, role. Chronic rhinosinusitis is characterized by nasal and sinus symptoms, such as nasal congestion, purulent discharge, facial pain, and impaired olfaction, which last longer than 12 weeks. Specifically, diagnosis requires:
-
1.
The existence of 2 or more symptoms, one of which must be either nasal blockage or discharge and the other facial pain/pressure or impaired olfaction
-
2.
Either endoscopic signs (polyps, mucopurulent discharge, and/or edema/mucosal obstruction primarily in the middle meatus) and/or computed tomography findings (sinus mucosal changes)19
Importantly, chronic rhinosinusitis is further classified into chronic rhinosinusitis without nasal polyps and chronic rhinosinusitis with nasal polyps.16 Both conditions are discrete phenotypes defined by the presence or absence of nasal polyps. However, this characteristic can also be endotype defining, because the presence of polyps indicates a different underlying pathophysiologic mechanism compared with when they are absent. Chronic rhinosinusitis without polyps seems to mechanistically involve Th1 mucosal inflammation resulting in tissue remodeling caused by overexpression of transforming growth factor beta.20, 21, 22 The role of infection in this endotype, if any, is not clear.21, 23 In contrast, the endotype for chronic rhinosinusitis with polyps seems to be Th2 skewed and characterized by increased levels of interleukin (IL)-4, IL-5, and IL-13 manifested as significant mucosal eosinophilia.24 A different endotype for chronic rhinosinusitis with polyps characterized by preponderance of neutrophils may be seen in patients with cystic fibrosis,25 or in Asian populations, in which TH17 cytokines and interferon gamma may be predominant.26
The eosinophilic endotype (chronic rhinosinusitis with polyps) may be further associated with increased levels of total and specific immunoglobulin E (IgE).27 In addition, a role for Staphylococcus aureus toxins and other microbial superantigens has been suggested28 through various pathways, including mediation of basophil degranulation, interaction with the T-cell receptor, and antienterotoxin IgE.27, 29, 30 Defective epithelial barrier caused by disruption of tight junctions could also play a role in this endotype.31 One particular phenotype/endotype that is important is aspirin-exacerbated respiratory disease, characterized by concomitant asthma and aspirin hypersensitivity and present in up to 40% of patients with nasal polyps.32, 33 This condition is also encompassed in the local inflammatory drug-induced rhinitis endotype, because it is defined by hypersensitivity to aspirin that leads to upper and lower airway inflammation, resulting in severe rhinitis and asthma symptoms.34 Additional chronic rhinosinusitis endotypes could be characterized based on their variable responsiveness to different treatments. For example, there exist good responders, weak responders, and nonresponders to any given therapeutic agent (eg, anti–IL-5–responsive and anti-IgE–responsive endotypes).16 However, it should be emphasized that poor treatment response may simply reflect an incorrect phenotypic/endotypic diagnosis, further emphasizing the need for better understanding of the pathogenesis of CR and chronic rhinosinusitis subtypes.
Allergic Rhinitis
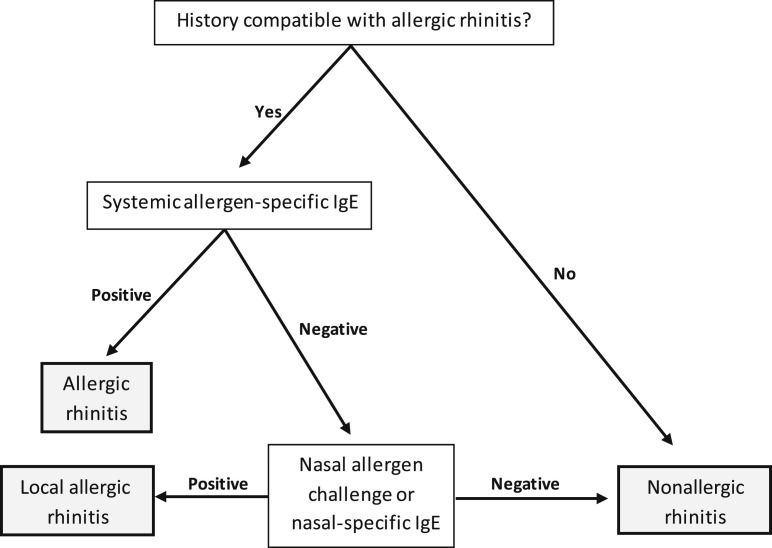
Allergic rhinitis, as defined by ARIA, is a well-defined endotype. It is an inflammatory condition caused by an IgE-mediated response to a spectrum of environmental allergens, including pollens, dust mite, cockroach frass, animal dander, rodents, and molds.35 Therefore, the diagnosis is established by skin-prick testing or specific IgE serologic testing to show IgE-mediated sensitization that corresponds with the patient’s medical history of symptoms induced by exposure to 1 or more specific sensitizing allergens (Fig. 1 ). Nasally inhaled sensitizing allergens are processed by antigen-presenting cells in the nasal mucosa and presented to CD4+ T lymphocytes.36 During this sensitization phase, T lymphocytes produce cytokines (eg, IL-3, Il-4, IL-5, IL-13, granulocyte-macrophage colony-stimulating factor), which lead to differentiation of B lymphocytes to plasma cells, which in turn produce antigen-specific IgE, which binds to high-affinity IgE receptors (Fc epsilon receptor I [FcERI]) on the surface of mast cells and basophils. On allergen reexposure, specific allergenic peptides are recognized by antigen-binding sites of specific IgE bound to these mast cells or basophils, resulting in cross-linking of IgE molecules and activation of signaling cascades that lead to granule exocytosis (also called degranulation) of preformed and newly formed bioactive mediators (eg, histamine, leukotrienes, prostaglandins, platelet-activating factor).35, 37 A late-phase reaction typically follows up to 4 to 12 hours later, as a result of the release of chemokines and other chemoattractants that cause Th2 cells, activated eosinophils, and mast cells to migrate into the nasal epithelium where they release additional cytokines, enzymes, and mediators that perpetuate allergic inflammation,38, 39 causing delayed or persistent AR symptoms.
Fig. 1.
Algorithm for allergic rhinitis, local allergic rhinitis, and nonallergic rhinitis.
Although AR as an endotype seems to be fairly straightforward, the variety of AR phenotypes is much more complicated. Clinically, AR has traditionally been characterized as seasonal, attributed to seasonal allergens (pollens); perennial, associated with year-round allergens (dust mites, mold spores, and animal dander)3, 9; or episodic, caused by sporadic exposures. However, this phenotyping approach is often inconsistent and overlapping.9 Therefore, ARIA guidelines11, 12 have categorized AR by duration, either as intermittent (<4 days per week or <4 weeks) or persistent (>4 days per week and >4 weeks) and by severity as mild, characterized by normal sleep, no impairment of daily activities/work/leisure/sport/school, and no troublesome symptoms; and moderate/severe, associated with any of the characteristics listed earlier. Further AR phenotyping may include pattern of sensitization (monosensitized vs polysensitized). It was recently suggested in a Practical Allergy (PRACTALL) document that more attention should be paid to the underlying mechanisms related to aeroallergen sensitization even if such sensitization does not seem to drive symptoms, because this patient profile could potentially define a novel phenotype and/or endotype.40
Nonallergic Rhinitis
Noninfectious nonallergic rhinitis (NAR) is a heterogeneous group of nasal conditions in which the diagnosis requires negative systemic IgE testing (see Fig. 1).7, 41 The NAR subtypes are common, affecting as many as 200 million individuals worldwide,42, 43 with a prevalence of 20% to 70% among adult patients.44 However, their heterogeneity, the different criteria used for classification, and the often conflicting terminology across studies impedes uncovering of the exact prevalence of this disorder.
For instance, from nasal mucosal eosinophilia (endotype-wise), NAR variants have historically been divided into 2 groups: NAR with eosinophilia syndrome (NARES) (which was long thought to be a distinct phenotype/endotype45) and all the other noneosinophilic subtypes (non-NARES); NARES was originally defined by the presence of more than 20% eosinophils in nasal smears.46, 47 However, there is currently no consensus on the eosinophilic threshold required for diagnosis, because any amount from greater than 5% to greater than 20% has been reported to indicate this condition.2, 8, 48 However, recent research scrutinizing NARES mechanics has raised questions regarding whether this is a distinct condition or whether it mostly overlaps with other conditions.40 The value of this histologic-based classification is further reduced because the methodologies used to obtain nasal cytology by swabbing or scraping the inferior turbinate or nasal lavage are variable and burdensome, making it impractical to routinely perform in the clinical setting.10 Furthermore, because NARES pathophysiology is obscure it has often been equated to idiopathic rhinitis (IR),45, 49 local AR,40 a local inflammatory response induced by irritants,50 or as a precursor to aspirin triad because NARES patients frequently have eosinophilic nasal polyps, bronchial hyperreactivity, and nonallergic asthma.2, 51, 52 Regardless of whether any or all of these different endotypes are relevant, it is clear that eosinophilia contributes to direct mucosal damage, protracted mucociliary clearance, and nasal hyperresponsiveness.50 Other studies have reported different inflammatory profiles in the nasal mucosa in patients with NAR, including mast cells and neutrophils, further complicating the utility of nasal histology as a biomarker for establishing reliable NAR endotypes.53
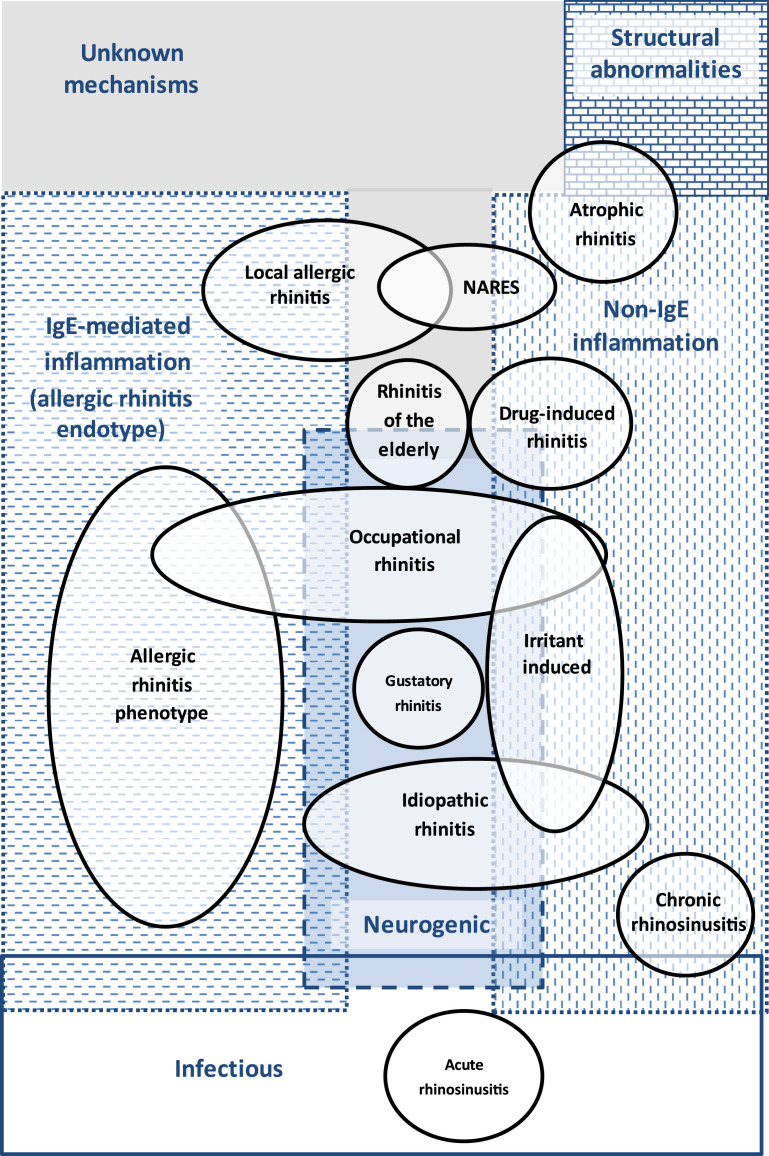
In addition to NARES, at least 6 other clinical entities are included in the NAR classification: drug-induced rhinitis, gustatory rhinitis, hormone-induced rhinitis, atrophic rhinitis, rhinitis of the elderly, and IR (Fig. 2 , Table 1 ).10
Fig. 2.
The rhinitis universe. Overlapping phenotypes (black circles) and endotypes (background).
Table 1.
Rhinitis phenotypes and characteristics
| Phenotype | Characteristic |
|---|---|
| Rhinitis by structural/systemic causes | Systematic disease/structural causes |
| Acute infectious rhinosinusitis | Infection |
| Chronic Rhinosinusitis | Duration >12 wk and paranasal sinuses involvement/polyps |
| Allergic rhinitis | IgE-mediated inflammation |
| Nonallergic rhinitis | — |
| Local allergic rhinitis | Topical IgE mechanism |
| NARES | Nasal smear with >5%–20% of eosinophils |
| Gustatory rhinitis | Symptoms elicited by ingestion of foods |
| Rhinitis of pregnancy | Pregnancy >36 wk |
| Drug-induced rhinitis | Symptoms elicited by medication intake |
| Rhinitis medicamentosa | Prolonged use of nasal decongestants |
| Occupational rhinitis | Symptoms only at workplace |
| Many surgeries/granulomatous disease | Atrophic rhinitis |
| Rhinitis of the elderly | Old-age onset |
| Idiopathic rhinitis | All other phenotypes excluded |
Idiopathic rhinitis
IR is the most prevalent subtype of the NAR group,54 and is also a diagnosis requiring exclusion of AR.44, 54, 55 Its terminology has been variable across studies,7, 10 including intrinsic rhinitis, IR, vasomotor rhinitis,55, 56 and nonallergic rhinopathy.6 Its pathophysiologic mechanism is unrelated to allergy, structural defects, or underlying systemic disease, and it is typically not associated with nasal eosinophilia.51, 57
Idiotypic rhinitis endotypes are not well elucidated. However, it is likely that the underlying mechanism is neurogenically mediated. The absence of a distinct consistent cellular inflammatory pattern in the nasal mucosa provides further indirect support for a neurogenic mechanism. Triggers for this form of NAR typically include noxious odorants or chemical irritants like tobacco smoke, perfumes/fragrance, and cleaning agents, but also changes in temperature, humidity, and barometric pressure. Other triggers may include positional changes, alcohol, or the act of eating.
Nonspecific irritants and alcohol9, 54, 58 were thought to induce tachykinin release and inhibition of sympathetic mediators, enhancing the parasympathetic response and culminating in nasal congestion and/or rhinorrhea.59 However, such a neural/vascular pathophysiologic mechanism has not been clearly documented,3 and it is now thought that some forms of IR may be disorders of the nonadrenergic noncholinergic (NANC) or peptidergic neural system.60, 61 Nasal peptidergic neurons (mainly sensory C fibers) are activated by these nonspecific stimuli, resulting in antidromic and orthodromic release of inflammatory neuropeptides, which can exert effects on the blood vasculature and mucus-secreting glands, leading to symptoms of IR. These fibers are thought to be primarily activated by transient response potential (TRP) calcium ion channels whose ligands have been shown to be affected by temperature, mechanical or osmotic stimuli, or a spectrum of chemical irritants. For example, TPRV1, for which capsaicin has been shown to be a specific ligand, is activated by hot temperatures. An acute exposure to capsaicin can activate TRPV1, whereas continuous exposure to capsaicin can desensitize this receptor40 (for a discussion of the mechanisms for NAR, see Baroody FM: Non-Allergic Rhinitis: Mechanism of Action, in this issue).
However, these pathways could define a novel umbrella endotype, the neurogenic rhinitis endotype, which can be distinguished from healthy controls by provocation to stimuli like cold dry air,62 a challenge that stimulates TRPA1 and TRPM8 channels, which are attenuated by capsaicin.63 Similar TRP pathways could explain gustatory rhinitis, which is another subtype with a strong neurologic basis,64 as well as other rhinitis subtypes to a variable degree (ie, acute viral rhinosinusitis, which is known to be responsive to cold air provocation65, 66; rhinitis of the elderly; or even AR, which may have a neural hypersensitivity facet63). Further support for a neurologic mechanism is that these conditions seem to be responsive to treatment with capsaicin or anticholinergic drugs.3, 67, 68
Further endotypes of IR could be defined by the trigger type; for example, irritant-sensitive IR.8 An irritant-induced umbrella phenotype that includes not only IR but other entities such as occupational rhinitis subphenotypes has been proposed (see Fig. 2).40 These novel groupings warrant further research.
Hormonal rhinitis
Hormonal rhinitis subtypes include rhinitis of pregnancy and menstrual cycle–related rhinitis.6, 69 Rhinitis of pregnancy is a common condition that affects up to 20% to 30% of pregnant women. Rhinitis of pregnancy typically begins in the last 6 weeks of pregnancy (after 34 weeks of gestation) and resolves spontaneously within 2 weeks postpartum,70 whereas menstrual cycle–related rhinitis consists of premenstrual symptoms on a cyclical basis. These phenotypes are probably based on similar pathophysiologic mechanisms primarily mediated through increased levels of estrogen, which cause nasal congestion through vascular engorgement.71 This assumption was based mainly on reports from women taking contraceptive pills containing high estrogen levels, which caused rhinitis as a side effect. Assuming that estrogen does cause nasal obstruction, increased congestion would be expected during the preovulatory phase of the menstrual cycle, when the levels of estrogen are highest, but this is not always the case.71 Therefore, other mechanisms have also been suggested, including increased circulating blood volume caused by a vasodilating effect of progesterone, increased production of human growth hormone (which is also the basis of a proposed acromegaly-related rhinitis subtype), as well as enhanced production of a placental growth hormone variant, of an insulinlike growth factor-I, or of prolactin. Other key players could include beta-estradiol, which has been shown to increase the expression of histamine H1 receptors on mucosal epithelial and microvascular endothelial cells72 and to induce eosinophil migration and/or degranulation.71, 73 Other suggested forms of hormonal rhinitis, such as those linked with thyroid disorders, are not currently supported by a high level of scientific evidence.2, 33
Gustatory rhinitis
Gustatory rhinitis is defined by the acute onset of profuse watery rhinorrhea immediately after ingestion of certain spicy foods but can occur after the act of eating in general.74, 75 Recent studies suggest that it is a direct neurogenic event, thought to be associated with overstimulation of the parasympathetic system. Regulation of vascular and glandular processes in the nose includes complex interactions between sensory, sympathetic, and parasympathetic nerves.76 Ingestion of the food could act as a mechanical stimulus that activates nociceptive sensory nerves, resulting in overactivation of parasympathetic fibers, as shown by the blunting of this effect by intranasal atropine.74, 77 However, the role of a hyperactive, NANC, or peptidergic neural system is still not well elucidated and remains under debate.64 Gustatory rhinitis has various endotypes/subtypes, including idiopathic gustatory rhinitis and posttraumatic, postsurgical, and cranial nerve neuropathy–associated endotypes.64, 78 Idiopathic gustatory rhinitis, the most common of these entities, is prevalent in the general population.64 However, up to 45% of patients consider it no more than an annoyance, probably leading to an underestimation of its prevalence.75
Drug-induced rhinitis
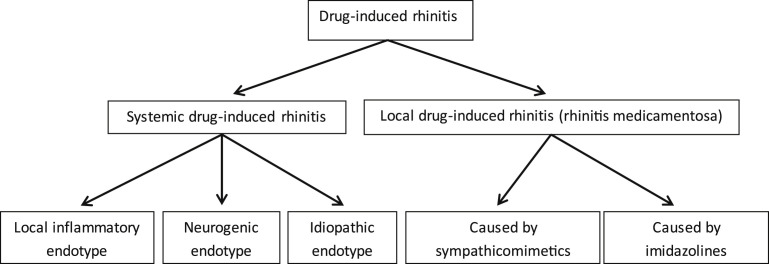
Systemic drug-induced rhinitis may be classified into 3 subtypes: local inflammatory type, neurogenic type, and idiopathic (unknown) type (Fig. 3 ).
Fig. 3.
Classification of drug-induced rhinitis.
The local inflammatory endotype commonly occurs after ingestion of aspirin and other nonsteroidal antiinflammatory drugs.8, 79 Although various pathogenic mechanisms have been proposed, it is thought that the inhibition of cyclooxygenase-1 shifts the metabolism of arachidonic acid to the lipooxygenase pathway, resulting in decreased production of prostaglandin E2 and increased cysteinyl leukotriene release (ie, leucotriene C4) precipitating local inflammation.79
The neurogenic endotype of drug-induced rhinitis can occur with sympatholytic drugs such as alpha-adrenergic and beta-adrenergic antagonists, including clonidine, guanethidine, doxazocin, and methyldopa.8, 79 Downregulation of the sympathetic tone leads to vascular engorgement, nasal congestion, and rhinorrhea. Other drug classes that could cause neurogenic-type rhinitis are phosphodiesterase-5 selective inhibitors such as sildenafil, tadalafil, and vardenafil, which act through their vasodilating properties. This group of medications is thought to affect the erectile tissue of the nasal turbinates (capacitance venous vessels) causing nasal congestion.51, 79, 80 This concept is the same as that underlying the so-called honeymoon rhinitis subtype, in which sexual activities are thought to cause nasal blockade.
The idiopathic endotype of drug-induced rhinitis is caused by several different drug classes, some of which seem to have no pathophysiologic similarities (eg, β-blockers, angiotensin-converting enzyme inhibitors,81 calcium channel blockers, antipsychotics8, 79). Although some assumptions can be made related to underlying mechanisms causing rhinitis for some of these agents (eg, ACE inhibitors resulting in increased release of bradykinin, which is a potent vasodilator), the pathophysiologic basis of the idiopathic endotype is largely obscure79 and no specific subendotypes have yet been defined.
Rhinitis medicamentosa is a distinct drug-induced rhinitis subtype.79 It is defined as rebound nasal congestion following excessive local (rather than systemic) use of decongestant sprays. Physical examination in patients with rhinitis medicamentosa often reveals swollen, red nasal mucous membranes with minimal discharge. Two different endotypes can be discerned depending on the classes of nasal decongestants used that can cause this condition: sympathomimetics and imidazolines (Box 1 ). Sympathomimetic amines activate sympathetic nerves and cause vasoconstriction. Imidazolines cause vasoconstriction primarily through alpha2-adrenoreceptors. Cocaine (which is a potent vasoconstrictor) can also cause rhinitis medicamentosa, although usually symptoms are significantly more severe.82 Histologic changes consistent with rhinitis medicamentosa include ciliary loss, squamous cell metaplasia, epithelial edema, goblet cell hyperplasia, and inflammatory cell accumulation.83 When used briefly (<3–5 days consecutively), these medications provide significant relief of nasal congestion; however, prolonged use may lead to rhinitis medicamentosa. The mechanisms underlying this condition are variable and could be secondary to decreased production of endogenous norepinephrine through negative feedback84; the result of sympathomimetic amines with activity at both alpha and beta sites but a beta effect that outlasts the alpha effect causing rebound swelling84; or edema formation by altering vasomotor tone and vascular permeability through increased parasympathetic activity. Alongside rebound congestion, tachyphylaxis85 and, rarely, nasal septal perforation86 may also occur, although recent findings suggest that long-term use of these medications may be much safer when coadministered with intranasal steroids.87, 88
Box 1. Classes of drugs that cause rhinitis medicamentosa.
Sympathomimetics
Pseudoephedrine
Amphetamine
Benzedrine
Mescaline
Phenylephrine
Ephedrine
Phenylpropanolamine
Imidazolines
Xylometazoline
Naphazoline
Clonidine
Oxymetazoline
Rhinitis of the elderly
Rhinitis of the elderly is possibly underpinned by nasal hyperresponsiveness of the parasympathetic system and exemplifies the neurogenic rhinitis endotype, because it commonly presents with profuse rhinorrhea and is responsive to anticholinergic treatment. A causal role of other age-related factors, such as changes in nasal physiology or body water content, decrease in nasal blood flow, degeneration of mucous glands, collagen atrophy, and weakening of the septal cartilage, is still under debate.3, 51, 67, 89 It is likely that such issues can result in drying and increased nasal congestion regardless of the underlying pathophysiology of rhinitis, and hence may magnify or bring about a more complicated endotype of rhinitis of the elderly.51
Atrophic rhinitis
Atrophic rhinitis is characterized by symptoms of crusting, purulent discharge, nasal obstruction, and halitosis.90 It has a primary and secondary endotype that, symptom-wise, are fairly similar. A thorough medical history coupled with typical endoscopic findings are sufficient to diagnose both entities. Signs of sequelae (eg, atrophic pharyngitis) and of complications (eg, septal perforation and saddle nose deformity) may be seen in long-standing cases of both subtypes.91
The primary (idiopathic) subtype of atrophic rhinitis is defined by nasal mucosal and glandular atrophy.6 It primarily affects people from areas with warm climates who present with nasal inflammation, dryness, crusting, a sense of severe congestion, and epistaxis.8, 91 The underlying pathophysiology is unclear but it is either caused by a lack of mucus, thereby facilitating bacterial growth, leading to mucosal colonization (usually with Klebsiella ozaenae, S aureus, Proteus mirabilis, and Escherichia coli 92) or, vice versa, microbial colonization may be the primary cause of this condition. In any case, characteristic findings include crusting of nasal mucosa, a foul-smelling nasal discharge, and a reported sense of severe congestion, paradoxically in spite of considerably wide and unobstructed nasal cavities.8
The secondary subtype has a similar presentation, with the triad of fetor, crusting, and spacious nasal cavities with perceived congestion.93 However, because this form of atrophic rhinitis is caused by extensive surgical removal of mucus-secreting tissue, trauma, or chronic granulomatous disorders,6 signs of these underlying causes may be evident on physical examination. Aggressive resection of the turbinates often causes the empty nose syndrome, in which the patient exhibits severe nasal obstruction and inability to sense airflow despite complete nasal patency.94
Local allergic rhinitis
Local AR (also called entopic rhinitis) cannot easily fit into the 3-arm classification of rhinitis by formal criteria (see Campo P, Salas M, Blanca-López N, et al: Local Allergic Rhinitis, in this issue). Resent research has been scrutinizing this phenotype, which is a form of CR with symptoms similar to AR without systemic but with localized antigen-specific IgE (see Fig. 1).41, 95, 96 Local IgE to common aeroallergens such as house dust mite and grass/olive pollen confirmed by specific provocation has previously been reported.49, 95, 96 The mechanism for LAR seems to be similar to that of AR, in which allergen exposure causes nasal mucosal production of specific IgE, which gives rise to a localized Th2 inflammatory response.41, 95, 96, 97, 98 The localized allergic response observed with this endotype has led some clinicians to term this condition “entopy.”99 Studies have uncovered leukocyte-lymphocyte similarities in the nasal lavage of patients with AR and LAR, with increased numbers of eosinophils, basophils, mast cells, CD3+, and CD4+ T cells.95, 96 It has also been suggested that LAR could be an early AR condition rather than a distinct phenotype,41, 57 although this has been contested by more recent findings.100 It has also been suggested that LAR could overlap with NARES.40 However, more research is needed to further define this entity.
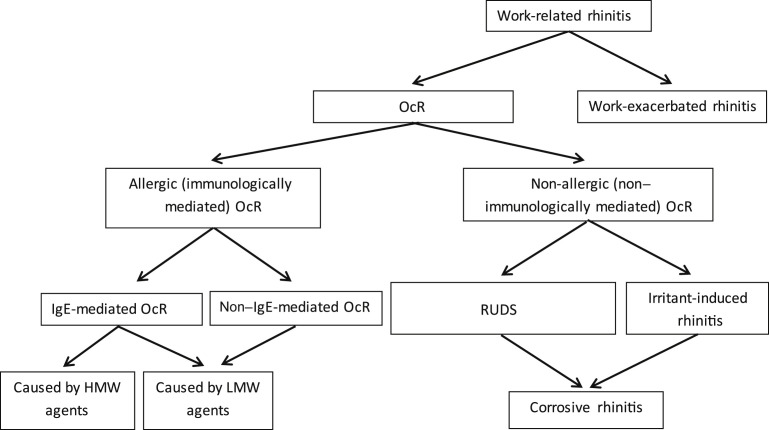
Occupational rhinitis
Classification of occupational rhinitis (see Grammer LC: Occupational Rhinitis, in this issue) is complex and there is currently no complete consensus (Fig. 4 ). Work-related-rhinitis is essentially an umbrella phenotype including occupational rhinitis, caused by factors in the work environment, and work-exacerbated rhinitis, in which a preexisting or concurrent rhinitis is worsened by occupational factors. Occupational rhinitis has been defined as “an inflammatory disease of the nose, which is characterized by intermittent or persistent symptoms (i.e., nasal congestion, sneezing, rhinorrhea, itching), and/or variable nasal airflow limitation and/or hypersecretion due to causes and conditions attributable to a particular work environment and not to stimuli encountered outside the workplace.”101 Occupational rhinitis includes conditions with similar characteristics to allergic, nonallergic,51 and irritant-induced phenotypes and to the neurogenic endotype. The nature of the workplace airborne agent exposures further defines the classification of occupational rhinitis into subvariants50:
-
•
Sensitizer-induced (allergic) occupational rhinitis is an IgE immunologically mediated condition that can be induced by high-molecular-weight and low-molecular-weight antigens. High-molecular-weight agents such as plant/animal proteins and some low-molecular-weight agents like platinum salts act as complete antigens to elicit a specific IgE-mediated response, whereas low-molecular-weight agents such as some diisocyanates (hexamethylene diisocyanate) and acid anhydrides (trimellitic acid) act as haptens to bind endogenous proteins to form new allergenic peptides capable of eliciting a specific IgE-mediated response.
-
•
The non–IgE-mediated immunologic-mediated endotype is primarily caused by low-molecular-weight agents, including reactive chemicals, transition metals, and wood dusts, and is less common.50, 102, 103
-
•
Nonallergic occupational rhinitis, also termed reactive upper airways dysfunction syndrome, is caused by a single exposure to high chemical irritant concentrations or multiple exposures to lower chemical irritant concentrations over time, the latter form also being termed irritant-induced rhinitis.50, 104 Both of these subforms can lead to significant inflammatory and even structural damage, resulting in so-called corrosive rhinitis, which is the severe end-stage form of the irritant-induced endotype, and is most often caused by potent toxic irritants such as chlorine, sulfur dioxide, and ammonia.105
Fig. 4.
Work-related rhinitis classification. OcR, occupational rhinitis; RUDS, reactive upper airways dysfunction syndrome. HMW, High molecular weight; LMW, Low molecular weight.
Rhinitis by structural/mechanical abnormalities
There are several structural abnormalities that predispose to and cause rhinitis. Different investigators have different views of whether these phenotypes are part of the NAR category or a stand-alone category. The most common symptom of these phenotypes is a sense of congestion either because of true blockage of the air passages or because of perceived congestion caused by a disturbance of normal airflow resistance and the development of a turbulent flow pattern.51 Septal deviation, commonly accompanied by contralateral compensatory turbinate hypertrophy, may cause nasal obstruction. Severe septal deviations may occur and impair nasal breathing, often unilaterally.1 Adenoidal hypertrophy typically manifests with nasal congestion, mouth breathing, nasal speech, and sleep apneic episodes/snoring.33 It is the most common acquired anatomic cause of nasal obstruction in infants and children,51 and is often associated with chronic allergic inflammation,1 which causes lymphoid hypertrophy leading to prominence of the adenoidal tissue and could therefore be postulated to represent a mechanical abnormality endotype, given its association with this defined mechanism. Choanal atresia, a rare congenital disorder involving blockage of the nose–lower airways passage can go unnoticed for years if unilateral,106 but when bilateral presents with conspicuous symptoms caused by difficulty in breathing.107 Nasal tumors are comparably uncommon,108 whereas nasal trauma/foreign objects are fairly common and may lead to nasal obstruction easily discernable by history or endoscopy.109 Cerebrospinal fluid rhinorrhea, which is drainage of cerebrospinal fluid from an abnormal subarachnoid space–nasal cavity pathway, is mainly a complication of surgery or trauma110 but can also be caused by benign intracranial hypertension or pseudotumor cerebri.51 It is characterized by clear watery secretion occasionally accompanied by headaches and olfactory impairment.16, 111
Rhinitis as a sign of systemic disease
Ciliary dysfunction impairs mucus clearance and can be primary or secondary (caused by viral infections and/or pollutants).112, 113 Primary ciliary dysfunction is a rare autosomal disorder that commonly manifests with recurrent respiratory infections that may manifest as Kartagener syndrome, characterized by the triad of situs inversus, chronic rhinosinusitis, and bronchiectasis. Cystic fibrosis causes recurrent nasal infections because of impaired microbial clearance and blocking of the sinus passages. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome) and granulomatosis with polyangiitis (formerly known as Wegener granulomatosis) are vasculitis conditions characterized by nasal symptoms. Granulomatous inflammation causes rhinitis in sarcoidosis, a chronic syndrome that may manifest with obstruction, nasal crusting, anosmia, and epistaxis.114, 115 Amyloid deposition can occur in the sinonasal cavities in amyloidosis, causing obstruction, nasal discharge, epistaxis, and postnasal drainage.116, 117
Summary
It is likely that rhinitis phenotypes will continue to be identified clinically until the underlying mechanisms of CR subtypes are better understood, which will lead to well-defined endotypes. In view of the clinical spectrum and complexity of these conditions, this will be a major undertaking. However, it is likely that better definition of CR endotypes will greatly improve treatment and reduce symptoms, and will also reduce associated comorbidities and health care costs related to these highly prevalent and burdensome conditions.
Footnotes
Conflicts of interest: Dr N.G. Papadopoulos has received grants from GSK, Nestle, and Merck, fees for development of educational presentations from AbbVie, Sanofi, Menarini, Meda, consultancy fees from GSK, AbbVie, Novartis, Menarini, ALK-Abello, and Meda, and fees for lectures by Novartis, Allergopharma, Uriach, GSK, Stallergenes, and MSD; Dr G.V. Guibas declares no relevant conflict of interest.
References
- 1.Roberts G., Xatzipsalti M., Borrego L.M. Paediatric rhinitis: position paper of the European Academy of Allergy and Clinical Immunology. Allergy. 2013;68(9):1102–1116. doi: 10.1111/all.12235. [DOI] [PubMed] [Google Scholar]
- 2.Bachert C. Persistent rhinitis - allergic or nonallergic? Allergy. 2004;59:11–15. doi: 10.1111/j.0108-1675.2004.00389.x. [DOI] [PubMed] [Google Scholar]
- 3.Tran N.P., Vickery J., Blaiss M.S. Management of rhinitis: allergic and non-allergic. Allergy Asthma Immunol Res. 2011;3:148–156. doi: 10.4168/aair.2011.3.3.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ledford D. Inadequate diagnosis of nonallergic rhinitis: assessing the damage. Allergy Asthma Proc. 2003;24:155–162. [PubMed] [Google Scholar]
- 5.Mastin T. Recognizing and treating non-infectious rhinitis. J Am Acad Nurse Pract. 2003;15:398–409. doi: 10.1111/j.1745-7599.2003.tb00414.x. [DOI] [PubMed] [Google Scholar]
- 6.Kaliner M. Classification of nonallergic rhinitis syndromes with a focus on vasomotor rhinitis, proposed to be known henceforth as nonallergic rhinopathy. World Allergy Organ J. 2009;2:98–101. doi: 10.1097/WOX.0b013e3181a9d55b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burns P., Powe D.G., Jones N.S. Idiopathic rhinitis. Curr Opin Otolaryngol Head Neck Surg. 2012;20:1–8. doi: 10.1097/MOO.0b013e32834e8ef7. [DOI] [PubMed] [Google Scholar]
- 8.Schroer B., Pien L.C. Nonallergic rhinitis: common problem, chronic symptoms. Cleve Clin J Med. 2012;79:285–293. doi: 10.3949/ccjm.79a11099. [DOI] [PubMed] [Google Scholar]
- 9.Greiner A.N., Meltzer E.O. Overview of the treatment of allergic rhinitis and nonallergic rhinopathy. Proc Am Thorac Soc. 2011;8:121–131. doi: 10.1513/pats.201004-033RN. [DOI] [PubMed] [Google Scholar]
- 10.Scarupa M.D., Kaliner M.A. Nonallergic rhinitis, with a focus on vasomotor rhinitis: clinical importance, differential diagnosis, and effective treatment recommendations. World Allergy Organ J. 2009;2:20–25. doi: 10.1097/WAO.0b013e318196ca1e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brozek J.L., Bousquet J., Baena-Cagnani C.E. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010;126:466–476. doi: 10.1016/j.jaci.2010.06.047. [DOI] [PubMed] [Google Scholar]
- 12.Bousquet J., Van Cauwenberge P., Khaltaev N., Aria Workshop Group, World Health Organization Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. 2001;108:S147–S334. doi: 10.1067/mai.2001.118891. [DOI] [PubMed] [Google Scholar]
- 13.Demoly P., Concas V., Urbinelli R. Spreading and impact of the World Health Organization's Allergic Rhinitis and its Impact on Asthma guidelines in everyday medical practice in France. Ernani survey. Clin Exp Allergy. 2008;38:1803–1807. doi: 10.1111/j.1365-2222.2008.03085.x. [DOI] [PubMed] [Google Scholar]
- 14.Ramirez L.F., Urbinelli R., Allaert F.A. Combining H1-antihistamines and nasal corticosteroids to treat allergic rhinitis in general practice. Allergy. 2011;66:1501–1502. doi: 10.1111/j.1398-9995.2011.02682.x. [DOI] [PubMed] [Google Scholar]
- 15.Demoly P., Calderon M.A., Casale T. Assessment of disease control in allergic rhinitis. Clin Transl Allergy. 2013;3:7. doi: 10.1186/2045-7022-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akdis C.A., Bachert C., Cingi C. Endotypes and phenotypes of chronic rhinosinusitis: a PRACTALL document of the European Academy of Allergy and Clinical Immunology and the American Academy of Allergy, Asthma & Immunology. J Allergy Clin Immunol. 2013;131:1479–1490. doi: 10.1016/j.jaci.2013.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fendrick A.M., Saint S., Brook I. Diagnosis and treatment of upper respiratory tract infections in the primary care setting. Clin Ther. 2001;23:1683–1706. doi: 10.1016/s0149-2918(01)80137-5. [DOI] [PubMed] [Google Scholar]
- 18.Gwaltney J.M., Jr. Acute community-acquired sinusitis. Clin Infect Dis. 1996;23:1209–1223. doi: 10.1093/clinids/23.6.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fokkens W.J., Lund V.J., Mullol J. European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl. 2012;(23) 3 p preceding table of contents, 1–298. [PubMed] [Google Scholar]
- 20.Hekiert A.M., Kofonow J.M., Doghramji L. Biofilms correlate with TH1 inflammation in the sinonasal tissue of patients with chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2009;141:448–453. doi: 10.1016/j.otohns.2009.06.090. [DOI] [PubMed] [Google Scholar]
- 21.Van Bruaene N., Derycke L., Perez-Novo C.A. TGF-beta signaling and collagen deposition in chronic rhinosinusitis. J Allergy Clin Immunol. 2009;124:253–259. doi: 10.1016/j.jaci.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 22.Li X., Meng J., Qiao X. Expression of TGF, matrix metalloproteinases, and tissue inhibitors in Chinese chronic rhinosinusitis. J Allergy Clin Immunol. 2010;125:1061–1068. doi: 10.1016/j.jaci.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 23.Tatar E.C., Tatar I., Ocal B. Prevalence of biofilms and their response to medical treatment in chronic rhinosinusitis without polyps. Otolaryngol Head Neck Surg. 2012;146:669–675. doi: 10.1177/0194599811434101. [DOI] [PubMed] [Google Scholar]
- 24.Patadia M., Dixon J., Conley D. Evaluation of the presence of B-cell attractant chemokines in chronic rhinosinusitis. Am J Rhinol Allergy. 2010;24:11–16. doi: 10.2500/ajra.2010.24.3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Zele T., Claeys S., Gevaert P. Differentiation of chronic sinus diseases by measurement of inflammatory mediators. Allergy. 2006;61:1280–1289. doi: 10.1111/j.1398-9995.2006.01225.x. [DOI] [PubMed] [Google Scholar]
- 26.Zhang N., Liu S., Lin P. Remodeling and inflammation in Chinese versus white patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2010;125:8. doi: 10.1016/j.jaci.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 27.Bachert C., Gevaert P., Holtappels G. Total and specific IgE in nasal polyps is related to local eosinophilic inflammation. J Allergy Clin Immunol. 2001;107:607–614. doi: 10.1067/mai.2001.112374. [DOI] [PubMed] [Google Scholar]
- 28.Van Zele T., Gevaert P., Watelet J.B. Staphylococcus aureus colonization and IgE antibody formation to enterotoxins is increased in nasal polyposis. J Allergy Clin Immunol. 2004;114:981–983. doi: 10.1016/j.jaci.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 29.Penn R., Mikula S. The role of anti-IgE immunoglobulin therapy in nasal polyposis: a pilot study. Am J Rhinol. 2007;21:428–432. doi: 10.2500/ajr.2007.21.3060. [DOI] [PubMed] [Google Scholar]
- 30.Bachert C., Zhang N. Chronic rhinosinusitis and asthma: novel understanding of the role of IgE ‘above atopy’. J Intern Med. 2012;272:133–143. doi: 10.1111/j.1365-2796.2012.02559.x. [DOI] [PubMed] [Google Scholar]
- 31.Soyka M.B., Wawrzyniak P., Eiwegger T. Defective epithelial barrier in chronic rhinosinusitis: the regulation of tight junctions by IFN-gamma and IL-4. J Allergy Clin Immunol. 2012;130(5):1087–1096.e10. doi: 10.1016/j.jaci.2012.05.052. [DOI] [PubMed] [Google Scholar]
- 32.Meltzer E.O., Hamilos D.L., Hadley J.A. Rhinosinusitis: establishing definitions for clinical research and patient care. J Allergy Clin Immunol. 2004;114:155–212. doi: 10.1016/j.jaci.2004.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bernstein I.L., Li J.T., Bernstein D.I. Allergy diagnostic testing: an updated practice parameter. Ann Allergy Asthma Immunol. 2008;100:S1–S148. doi: 10.1016/s1081-1206(10)60305-5. [DOI] [PubMed] [Google Scholar]
- 34.Szczeklik A., Nizankowska E. Clinical features and diagnosis of aspirin induced asthma. Thorax. 2000;55:42–44. doi: 10.1136/thorax.55.suppl_2.S42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sin B., Togias A. Pathophysiology of allergic and nonallergic rhinitis. Proc Am Thorac Soc. 2011;8:106–114. doi: 10.1513/pats.201008-057RN. [DOI] [PubMed] [Google Scholar]
- 36.KleinJan A., Willart M., van Rijt L.S. An essential role for dendritic cells in human and experimental allergic rhinitis. J Allergy Clin Immunol. 2006;118:1117–1125. doi: 10.1016/j.jaci.2006.05.030. [DOI] [PubMed] [Google Scholar]
- 37.Creticos P.S., Peters S.P., Adkinson N.F., Jr. Peptide leukotriene release after antigen challenge in patients sensitive to ragweed. N Engl J Med. 1984;310:1626–1630. doi: 10.1056/NEJM198406213102502. [DOI] [PubMed] [Google Scholar]
- 38.Bentley A.M., Jacobson M.R., Cumberworth V. Immunohistology of the nasal mucosa in seasonal allergic rhinitis: increases in activated eosinophils and epithelial mast cells. J Allergy Clin Immunol. 1992;89:877–883. doi: 10.1016/0091-6749(92)90444-7. [DOI] [PubMed] [Google Scholar]
- 39.Varney V.A., Jacobson M.R., Sudderick R.M. Immunohistology of the nasal mucosa following allergen-induced rhinitis. Identification of activated T lymphocytes, eosinophils, and neutrophils. Am Rev Respir Dis. 1992;146:170–176. doi: 10.1164/ajrccm/146.1.170. [DOI] [PubMed] [Google Scholar]
- 40.Papadopoulos N.G., Bernstein J.A., Demoly P. Phenotypes and endotypes of rhinitis and their impact on management: a PRACTALL report. Allergy. 2015;70:474–494. doi: 10.1111/all.12573. [DOI] [PubMed] [Google Scholar]
- 41.Rondon C., Dona I., Torres M.J. Evolution of patients with nonallergic rhinitis supports conversion to allergic rhinitis. J Allergy Clin Immunol. 2009;123:1098–1102. doi: 10.1016/j.jaci.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 42.Settipane R.A., Charnock D.R. Epidemiology of rhinitis: allergic and nonallergic. Clin Allergy Immunol. 2007;19:23–34. [PubMed] [Google Scholar]
- 43.Bousquet J., Fokkeins W., Burney P. Important research questions in allergy and related diseases: nonallergic rhinitis: a GA2LEN paper. Allergy. 2008;63:842–853. doi: 10.1111/j.1398-9995.2008.01715.x. [DOI] [PubMed] [Google Scholar]
- 44.Molgaard E., Thomsen S.F., Lund T. Differences between allergic and nonallergic rhinitis in a large sample of adolescents and adults. Allergy. 2007;62:1033–1037. doi: 10.1111/j.1398-9995.2007.01355.x. [DOI] [PubMed] [Google Scholar]
- 45.Settipane R.A. Rhinitis: a dose of epidemiological reality. Allergy Asthma Proc. 2003;24:147–154. [PubMed] [Google Scholar]
- 46.Settipane R.A., Lieberman P. Update on nonallergic rhinitis. Ann Allergy Asthma Immunol. 2001;86:494–507. doi: 10.1016/S1081-1206(10)62896-7. [DOI] [PubMed] [Google Scholar]
- 47.Bachert C., Van Bruaene N., Toskala E. Important research questions in allergy and related diseases: 3-chronic rhinosinusitis and nasal polyposis - a GALEN study. Allergy. 2009;64:520–533. doi: 10.1111/j.1398-9995.2009.01964.x. [DOI] [PubMed] [Google Scholar]
- 48.Ellis A.K., Keith P.K. Nonallergic rhinitis with eosinophilia syndrome. Curr Allergy Asthma Rep. 2006;6:215–220. doi: 10.1007/s11882-006-0037-0. [DOI] [PubMed] [Google Scholar]
- 49.Rondon C., Fernandez J., Lopez S. Nasal inflammatory mediators and specific IgE production after nasal challenge with grass pollen in local allergic rhinitis. J Allergy Clin Immunol. 2009;124:1005–1011.e1. doi: 10.1016/j.jaci.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 50.Nozad C.H., Michael L.M., Betty Lew D. Non-allergic rhinitis: a case report and review. Clin Mol Allergy. 2010;8:1. doi: 10.1186/1476-7961-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wallace D.V., Dykewicz M.S., Bernstein D.I. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol. 2008;122:S1–S84. doi: 10.1016/j.jaci.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 52.Moneret-Vautrin D.A., Hsieh V., Wayoff M. Nonallergic rhinitis with eosinophilia syndrome a precursor of the triad: nasal polyposis, intrinsic asthma, and intolerance to aspirin. Ann Allergy. 1990;64:513–518. [PubMed] [Google Scholar]
- 53.Gelardi M., Iannuzzi L., Tafuri S. Allergic and non-allergic rhinitis: relationship with nasal polyposis, asthma and family history. Acta Otorhinolaryngol Ital. 2014;34:36–41. [PMC free article] [PubMed] [Google Scholar]
- 54.Settipane G. Epidemiology of vasomotor rhinitis. World Allergy Organ J. 2009;2:115–118. doi: 10.1097/WOX.0b013e3181ac91ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rondon C., Canto G., Blanca M. Local allergic rhinitis: a new entity, characterization and further studies. Curr Opin Allergy Clin Immunol. 2010;10:1–7. doi: 10.1097/ACI.0b013e328334f5fb. [DOI] [PubMed] [Google Scholar]
- 56.Salib R.J., Harries P.G., Nair S.B. Mechanisms and mediators of nasal symptoms in non-allergic rhinitis. Clin Exp Allergy. 2008;38:393–404. doi: 10.1111/j.1365-2222.2007.02926.x. [DOI] [PubMed] [Google Scholar]
- 57.Rondon C., Campo P., Togias A. Local allergic rhinitis: concept, pathophysiology, and management. J Allergy Clin Immunol. 2008;129:1460–1467. doi: 10.1016/j.jaci.2012.02.032. [DOI] [PubMed] [Google Scholar]
- 58.Shusterman D., Balmes J., Murphy M.A. Chlorine inhalation produces nasal airflow limitation in allergic rhinitic subjects without evidence of neuropeptide release. Neuropeptides. 2004;38:351–358. doi: 10.1016/j.npep.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 59.Jaradeh S.S., Smith T.L., Torrico L. Autonomic nervous system evaluation of patients with vasomotor rhinitis. Laryngoscope. 2000;110:1828–1831. doi: 10.1097/00005537-200011000-00012. [DOI] [PubMed] [Google Scholar]
- 60.van Rijswijk J.B., Blom H.M., Fokkens W.J. Idiopathic rhinitis, the ongoing quest. Allergy. 2005;60:1471–1481. doi: 10.1111/j.1398-9995.2005.00975.x. [DOI] [PubMed] [Google Scholar]
- 61.Van Gerven L., Boeckxstaens G., Hellings P. Up-date on neuro-immune mechanisms involved in allergic and non-allergic rhinitis. Rhinology. 2012;50:227–235. doi: 10.4193/Rhino.11.152. [DOI] [PubMed] [Google Scholar]
- 62.Braat J.P., Mulder P.G., Fokkens W.J. Intranasal cold dry air is superior to histamine challenge in determining the presence and degree of nasal hyperreactivity in nonallergic noninfectious perennial rhinitis. Am J Respir Crit Care Med. 1998;157:1748–1755. doi: 10.1164/ajrccm.157.6.9701016. [DOI] [PubMed] [Google Scholar]
- 63.Sarin S., Undem B., Sanico A. The role of the nervous system in rhinitis. J Allergy Clin Immunol. 2006;118:999–1016. doi: 10.1016/j.jaci.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 64.Georgalas C., Jovancevic L. Gustatory rhinitis. Curr Opin Otolaryngol Head Neck Surg. 2012;20:9–14. doi: 10.1097/MOO.0b013e32834dfb52. [DOI] [PubMed] [Google Scholar]
- 65.Piedimonte G. Pathophysiological mechanisms for the respiratory syncytial virus-reactive airway disease link. Respir Res. 2002;3:S21–S25. doi: 10.1186/rr185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Doyle W.J., Skoner D.P., Seroky J.T. Effect of experimental rhinovirus 39 infection on the nasal response to histamine and cold air challenges in allergic and nonallergic subjects. J Allergy Clin Immunol. 1994;93:534–542. doi: 10.1016/0091-6749(94)90364-6. [DOI] [PubMed] [Google Scholar]
- 67.Tan R., Corren J. Optimum treatment of rhinitis in the elderly. Drugs Aging. 1995;7:168–175. doi: 10.2165/00002512-199507030-00002. [DOI] [PubMed] [Google Scholar]
- 68.Platt M. Pharmacotherapy for allergic rhinitis. Int Forum Allergy Rhinol. 2014;4:S35–S40. doi: 10.1002/alr.21381. [DOI] [PubMed] [Google Scholar]
- 69.Kaliner M. Recognizing and treating nonallergic rhinitis. Female Patient. 2002;27:20–32. [Google Scholar]
- 70.Ellegard E., Karlsson G. Nasal congestion during pregnancy. Clin Otolaryngol Allied Sci. 1999;24:307–311. doi: 10.1046/j.1365-2273.1999.00264.x. [DOI] [PubMed] [Google Scholar]
- 71.Ellegard E.K. Clinical and pathogenetic characteristics of pregnancy rhinitis. Clin Rev Allergy Immunol. 2004;26:149–159. doi: 10.1385/CRIAI:26:3:149. [DOI] [PubMed] [Google Scholar]
- 72.Hamano N., Terada N., Maesako K. Expression of histamine receptors in nasal epithelial cells and endothelial cells – the effects of sex hormones. Int Arch Allergy Immunol. 2008;115:220–227. doi: 10.1159/000023904. [DOI] [PubMed] [Google Scholar]
- 73.Hamano N., Terada N., Maesako K. Effect of sex hormones on eosinophilic inflammation in nasal mucosa. Allergy Asthma Proc. 1998;19:263–269. doi: 10.2500/108854198778557773. [DOI] [PubMed] [Google Scholar]
- 74.Raphael G.D., Raphael M.H., Kaliner M.A. Gustatory rhinitis: a syndrome of food-induced rhinorrhea. J Allergy Clin Immunol. 1989;13:110–115. doi: 10.1016/0091-6749(89)90484-3. [DOI] [PubMed] [Google Scholar]
- 75.Waibel K.H., Chang C. Prevalence and food avoidance behaviors for gustatory rhinitis. Ann Allergy Asthma Immunol. 2008;100:200–205. doi: 10.1016/S1081-1206(10)60443-7. [DOI] [PubMed] [Google Scholar]
- 76.Lacroix J.S., Landis B.N. Neurogenic inflammation of the upper airway mucosa. Rhinology. 2008;46:163–165. [PubMed] [Google Scholar]
- 77.Malik V., Ghosh S., Woolford T.J. Rhinitis due to food allergies: fact or fiction? J Laryngol Otol. 2007;121:526–529. doi: 10.1017/S0022215106005147. [DOI] [PubMed] [Google Scholar]
- 78.Jovancevic L., Georgalas C., Savovic S. Gustatory rhinitis. Rhinology. 2010;48:7–10. doi: 10.4193/Rhin07.153. [DOI] [PubMed] [Google Scholar]
- 79.Varghese M., Glaum M.C., Lockey R.F. Drug-induced rhinitis. Clin Exp Allergy. 2010;40:381–384. doi: 10.1111/j.1365-2222.2009.03450.x. [DOI] [PubMed] [Google Scholar]
- 80.Vitezic D., Pelcic J.M. Erectile dysfunction: oral pharmacotherapy options. Int J Clin Pharmacol Ther. 2002;40:393–403. doi: 10.5414/cpp40393. [DOI] [PubMed] [Google Scholar]
- 81.Materson B.J. Adverse effects of angiotensin-converting enzyme inhibitors in antihypertensive therapy with focus on quinapril. Am J Cardiol. 1992;69:46–53. doi: 10.1016/0002-9149(92)90281-3. [DOI] [PubMed] [Google Scholar]
- 82.Goodger N.M., Wang J., Pogrel M.A. Palatal and nasal necrosis resulting from cocaine misuse. Br Dent J. 2005;198:333–334. doi: 10.1038/sj.bdj.4812171. [DOI] [PubMed] [Google Scholar]
- 83.Lin C.Y., Cheng P.H., Fang S.Y. Mucosal changes in rhinitis medicamentosa. Ann Otol Rhinol Laryngol. 2004;113:147–151. doi: 10.1177/000348940411300213. [DOI] [PubMed] [Google Scholar]
- 84.Graf P. Rhinitis medicamentosa: a review of causes and treatment. Treat Respir Med. 2005;4:21–29. doi: 10.2165/00151829-200504010-00003. [DOI] [PubMed] [Google Scholar]
- 85.Knipping S., Holzhausen H.J., Goetze G. Rhinitis medicamentosa: electron microscopic changes of human nasal mucosa. Otolaryngol Head Neck Surg. 2007;136:57–61. doi: 10.1016/j.otohns.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 86.Keyserling H.F., Grimme J.D., Camacho D.L. Nasal septal perforation secondary to rhinitis medicamentosa. Ear Nose Throat J. 2006;85:8–9. [PubMed] [Google Scholar]
- 87.Baroody F.M., Brown D., Gavanescu L. Oxymetazoline adds to the effectiveness of fluticasone furoate in the treatment of perennial allergic rhinitis. J Allergy Clin Immunol. 2011;127(4):927–934. doi: 10.1016/j.jaci.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 88.Vaidyanathan S., Williamson P., Clearie K. Fluticasone reverses oxymetazoline-induced tachyphylaxis of response and rebound congestion. Am J Respir Crit Care Med. 2010;182:19–24. doi: 10.1164/rccm.200911-1701OC. [DOI] [PubMed] [Google Scholar]
- 89.Edelstein D.R. Aging of the normal nose in adults. Laryngoscope. 1996;106:1–25. doi: 10.1097/00005537-199609001-00001. [DOI] [PubMed] [Google Scholar]
- 90.Chhabra N., Houser S.M. The diagnosis and management of empty nose syndrome. Otolaryngol Clin North Am. 2009;42:311–330. doi: 10.1016/j.otc.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 91.Dutt S.N., Kameswaran M. The aetiology and management of atrophic rhinitis. J Laryngol Otol. 2005;119:843–852. doi: 10.1258/002221505774783377. [DOI] [PubMed] [Google Scholar]
- 92.Moore E.J., Kern E.B. Atrophic rhinitis: a review of 242 cases. Am J Rhinol. 2001;15:355–361. [PubMed] [Google Scholar]
- 93.deShazo R.D., Stringer S.P. Atrophic rhinosinusitis: progress toward explanation of an unsolved medical mystery. Curr Opin Allergy Clin Immunol. 2011;11:1–7. doi: 10.1097/ACI.0b013e328342333e. [DOI] [PubMed] [Google Scholar]
- 94.Houser S.M. Empty nose syndrome associated with middle turbinate resection. Otolaryngol Head Neck Surg. 2006;135:972–973. doi: 10.1016/j.otohns.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 95.Rondon C., Romero J.J., Lopez S. Local IgE production and positive nasal provocation test in patients with persistent nonallergic rhinitis. J Allergy Clin Immunol. 2007;119:899–905. doi: 10.1016/j.jaci.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 96.Rondon C., Dona I., Lopez S. Seasonal idiopathic rhinitis with local inflammatory response and specific IgE in absence of systemic response. Allergy. 2008;63:1352–1358. doi: 10.1111/j.1398-9995.2008.01695.x. [DOI] [PubMed] [Google Scholar]
- 97.Powe D.G., Huskisson R.S., Carney A.S. Evidence for an inflammatory pathophysiology in idiopathic rhinitis. Clin Exp Allergy. 2001;31:864–872. doi: 10.1046/j.1365-2222.2001.01106.x. [DOI] [PubMed] [Google Scholar]
- 98.Powe D.G., Huskisson R.S., Carney A.S. Mucosal T-cell phenotypes in persistent atopic and nonatopic rhinitis show an association with mast cells. Allergy. 2004;59:204–212. doi: 10.1046/j.1398-9995.2003.00315.x. [DOI] [PubMed] [Google Scholar]
- 99.Powe D.G., Jagger C., Kleinjan A. 'Entopy': localized mucosal allergic disease in the absence of systemic responses for atopy. Clin Exp Allergy. 2003;33:1374–1379. doi: 10.1046/j.1365-2222.2003.01737.x. [DOI] [PubMed] [Google Scholar]
- 100.Rondon C., Campo P., Zambonino M.A. Follow-up study in local allergic rhinitis shows a consistent entity not evolving to systemic allergic rhinitis. J Allergy Clin Immunol. 2014;133:1026–1031. doi: 10.1016/j.jaci.2013.10.034. [DOI] [PubMed] [Google Scholar]
- 101.Moscato G., Vandenplas O., Gerth Van Wijk R. Occupational rhinitis. Allergy. 2008;63:969–980. doi: 10.1111/j.1398-9995.2008.01801.x. [DOI] [PubMed] [Google Scholar]
- 102.Palczynski C., Walusiak J., Ruta U. Nasal provocation test in the diagnosis of natural rubber latex allergy. Allergy. 2000;55:34–41. doi: 10.1034/j.1398-9995.2000.00037.x. [DOI] [PubMed] [Google Scholar]
- 103.Archambault S., Malo J.L., Infante-Rivard C. Incidence of sensitization, symptoms, and probable occupational rhinoconjunctivitis and asthma in apprentices starting exposure to latex. J Allergy Clin Immunol. 2001;107:921–923. doi: 10.1067/mai.2001.114116. [DOI] [PubMed] [Google Scholar]
- 104.Meggs W.J. RADS and RUDS–the toxic induction of asthma and rhinitis. J Toxicol Clin Toxicol. 1994;32:487–501. doi: 10.3109/15563659409011053. [DOI] [PubMed] [Google Scholar]
- 105.Graham D., Henderson F., House D. Neutrophil influx measured in nasal lavages of humans exposed to ozone. Arch Environ Health. 1988;43:228–233. doi: 10.1080/00039896.1988.9934938. [DOI] [PubMed] [Google Scholar]
- 106.Assanasen P., Metheetrairut C. Choanal atresia. J Med Assoc Thai. 2009;92:699–706. [PubMed] [Google Scholar]
- 107.Sadek S.A. Congenital bilateral choanal atresia. Int J Pediatr Otorhinolaryngol. 1998;42:247–256. doi: 10.1016/s0165-5876(97)00142-0. [DOI] [PubMed] [Google Scholar]
- 108.Baumgartner B.J., Ladd T., Esquivel C. Low-grade adenocarcinoma of the nasal cavity–an unusual presentation: case report and review of the literature. Ear Nose Throat J. 2007;86:97–100. [PubMed] [Google Scholar]
- 109.Alvi A., Doherty T., Lewen G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope. 2003;113:102–106. doi: 10.1097/00005537-200301000-00019. [DOI] [PubMed] [Google Scholar]
- 110.Clark D., Bullock P., Hui T. Benign intracranial hypertension: a cause of CSF rhinorrhoea. J Neurol Neurosurg Psychiatry. 1994;57:847–849. doi: 10.1136/jnnp.57.7.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ryall R.G., Peacock M.K., Simpson D.A. Usefulness of beta 2-transferrin assay in the detection of cerebrospinal fluid leaks following head injury. J Neurosurg. 1992;77:737–739. doi: 10.3171/jns.1992.77.5.0737. [DOI] [PubMed] [Google Scholar]
- 112.Carson J.L., Collier A.M., Hu S.S. Acquired ciliary defects in nasal epithelium of children with acute viral upper respiratory infections. N Engl J Med. 1985;312:463–468. doi: 10.1056/NEJM198502213120802. [DOI] [PubMed] [Google Scholar]
- 113.Pedersen M. Ciliary activity and pollution. Lung. 1990;168:368–376. doi: 10.1007/BF02718154. [DOI] [PubMed] [Google Scholar]
- 114.Reed J., deShazo R.D., Houle T.T. Clinical features of sarcoid rhinosinusitis. Am J Med. 2010;123:856–862. doi: 10.1016/j.amjmed.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 115.Qazi F.A., Thorne J.E., Jabs D.A. Scleral nodule associated with sarcoidosis. Am J Ophthalmol. 2003;136:752–754. doi: 10.1016/s0002-9394(03)00454-9. [DOI] [PubMed] [Google Scholar]
- 116.Panda N.K., Saravanan K., Purushotaman G.P. Localized amyloidosis masquerading as nasopharyngeal tumor: a review. Am J Otolaryngol. 2007;28:208–211. doi: 10.1016/j.amjoto.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 117.Tsikoudas A., Martin-Hirsch D.P., Woodhead C.J. Primary sinonasal amyloidosis. J Laryngol Otol. 2001;115:55–56. doi: 10.1258/0022215011906803. [DOI] [PubMed] [Google Scholar]