Abstract
Ethnopharmacological relevance
Pelargonium sidoides DC. (Geraniaceae), a popular medicinal plant used in traditional medicine in the treatment of gastrointestinal ailments has been transformed into a phytopharmaceutical (EPs® 7360) for treating respiratory tract infections. The increasing international demand for Pelargonium sidoides has led to localised overexploitation of its wild populations in southern Africa. The aim of the review is to provide a synthesis of the current state of scientific knowledge on the phytochemical, pharmacological and toxicological properties of Pelargonium sidoides as well as the potential role of plant biotechnology in its conservation. The review highlights knowledge gaps in these research areas.
Materials and Methods
A comprehensive literature search involving mainly electronic and library sources of information were used to collate and synthesise published data.
Results
Experimental results from in vitro studies indicate that bioactive phytochemical constituents of Pelargonium sidoides may not possess a direct antimicrobial effect, but instead act by interfering with microbial binding to host cell receptors, inhibition of key enzymes and the production of antimicrobial effector molecules such as nitric oxide and interferons (IFNs) by the host cells. Furthermore, clinical evaluations in randomised, double-blind, placebo-controlled trials have demonstrated the beneficial effect of Pelargonium sidoides in the treatment of respiratory tract infections with few side effects. However, there is lack of adequate information on the safety evaluation of the plant. On the other hand, the increasing demand for Pelargonium sidoides has led to localised illegal harvesting of wild plants.
Conclusions
Pharmacological data reported in literature suggest that Pelargonium sidoides shows a beneficial effect in the treatment of respiratory tract infections. However, more studies are required to elucidate the mode of action of the active constituents exhibited in the treatment of respiratory tract infections and other health conditions caused by microbial attack. Furthermore, the pharmacological usefulness of Pelargonium sidoides must take cognisance of the broader context involving the need for conservation-friendly approaches in its utilisation. In this regard, plant biotechnology applications can play a meaningful role in a holistic conservation strategy.
Keywords: Conservation, Pelargonium sidoides, Pharmacological activity, Plant biotechnology, Umckaloabo
Graphical abstract
1. Introduction
Pelargonium sidoides DC. (Synonym: Pelargonium sidaefolium (Thunb.) R. Knuth; Common names: Umckaloabo, Uvendle, Kalwerbossie, Khoaara e nyenyane; Family: Geraniaceae) is a perennial geophyte predominantly found in the Eastern Cape Province of South Africa and the Lesotho highlands. The plant is adapted to a wide altitudinal range, spanning from near sea level in the Eastern Cape to 2746 m in the Lesotho highlands (Newton et al., 2013). The plant is widely used by local communities as a traditional medicine for curing various ailments, including diarrhoea, colic, gastritis, tuberculosis, cough, hepatic disorders, menstrual complaints and gonorrhoea (Brendler and van Wyk, 2008, Colling et al., 2010). The roots are also the main ingredient in a remedy used to treat a stomach ailment known as instila in infants (Hutchings et al., 1996). Powdered plant materials which are soaked in water are used as a facial cream in the treatment of skin pimples (Lewu et al., 2007). This indicates that Pelargonium sidoides may exhibit antibacterial properties. Probably the most compelling ethnobotanical use of Pelargonium sidoides has been in the treatment of tuberculosis, which subsequently led to its introduction in Europe in the late 1890s (Bladt and Wagner, 2007, Brendler and van Wyk, 2008). The traditional ethno-veterinary applications of Pelargonium sidoides include the use of root decoctions as an anthelmintic remedy in calves (Hutchings et al., 1996); boiled leaves to protect wounds against maggots; and the prevention of purging in horses (Brendler and van Wyk, 2008). An extract obtained by soaking the roots in water is administered orally in the treatment of dysentery in cattle (Lewu et al., 2007). Based on its medicinal properties in the treatment of respiratory-related ailments, Pelargonium sidoides has been formulated into phytopharmaceuticals, namely EPs® 7630 (Umckaloabo®, Dr. Willmar Schwabe GmbH & Co. KG Pharmaceuticals, Germany) and Linctagon® (Nativa, South Africa). The commercial success of Umckaloabo® is attributed to numerous factors, including >15 years of extensive scientific and clinical research (Gericke, 2011). On the other hand, only negligible research (Bourdette, 2012, Motsamai, 2012) has been done to evaluate the efficacy and safety of Linctagon® (which mainly contains 350 mg Pelargonium sidoides, 500 mg Vitamin C, 50 mg bromelain, 80 mg quercetin, 5 mg zinc). This review provides a synthesis of the state of scientific knowledge on the pharmacology and safety evaluation of Pelargonium sidoides as well as exploring the potential of plant biotechnology applications in its conservation.
2. Phytochemistry
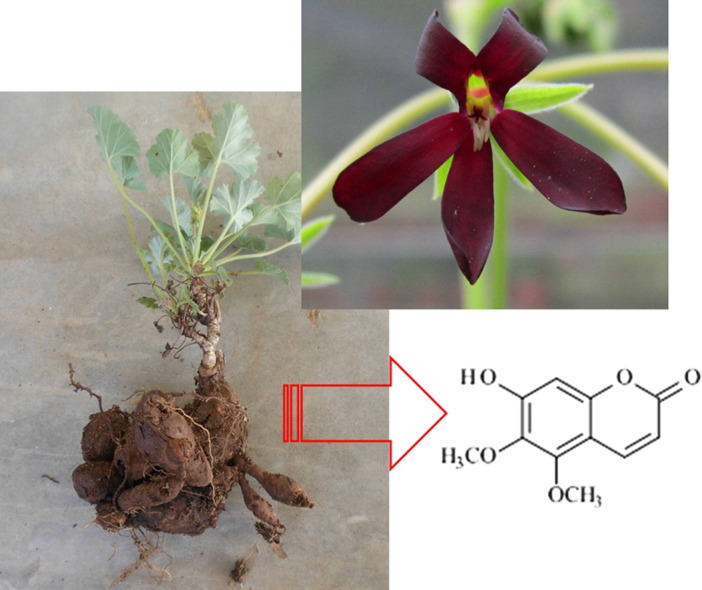
The extensive use of Pelargonium sidoides in traditional medicine coupled with its popularisation in modern medical systems in Europe have led to an upsurge in scientific exploration of its chemical composition in an effort to identify the active principles. This has resulted in a considerable body of literature exploring the phytochemical properties of Pelargonium sidoides (Gödecke et al., 2003, Gödecke et al., 2005, Hauer et al., 2010, Kayser and Kolodziej, 1995, Latté et al., 2000, Schoetz et al., 2008). Details of the phytochemistry of the plant were comprehensively summarised in an excellent review by Kolodziej (2007). However, identification of individual chemical constituents responsible for specific pharmacological activities has remained largely elusive. The chemical constituents of the root ethanolic extract of the plant consist largely of oligo- and polymeric proanthocyanidins, which are based on gallocatechin and epigallocatechin moieties (Theisen and Muller, 2012). The pharmacological efficacy of Pelargonium sidoides has been partly attributed to the biological activity of highly oxygenated coumarins (7-hydroxy-5,6-di-methoxycoumarin; 6,8-dihydroxy-5,7-dimethoxycoumarin), gallic acid-derivatives, flavonoids, phenolic and hydroxycinnamic acid-derivatives (Kayser and Kolodziej, 1995, Kolodziej, 2007, Colling et al., 2010). Recently, 6-Methoxy-7-(sulfooxy)-2H-1-benzopyran-2-one and 6,8-Bis(sulfooxy)-7-methoxy-2H-1-benzopyran-2-one were identified in Pelargonium sidoides for the first time (Hauer et al., 2010). Most significantly, Hauer et al. (2010) characterised two novel compounds, 7-Hydroxy-6-methoxy-8-(sulfooxy)-2H‑1-benzopyran-2-one and 8-Hydroxy-7-methoxy-6-(sulfooxy)-2H‑1-benzopyran-2-one (Fig. 2). These novel compounds have to be screened for pharmacological activity as they may represent the individual active constituents that have so far remained elusive.
Fig. 2.
Chemical structures of signature constituents found in Pelargonium sidoides DC.: Gallic acid (1); 7-hydroxy-5,6-dimethoxycoumarin (2); and 6,8-dihydroxy-5,7-dimethoxycoumarin (3); 6-Methoxy-7-(sulfooxy)-2H‑1-benzopyran-2-one (4); 6,8-Bis(sulfooxy)-7-methoxy-2H-1-benzopyran-2-one (5); 7-Hydroxy-6-methoxy-8-(sulfooxy)-2H-1-benzopyran-2-one (6); 8-Hydroxy-7-methoxy-6-(sulfooxy)-2H-1-benzopyran-2-one (7).
3. Pharmacological properties
It is interesting to note that the repertoire of health conditions for which Pelargonium sidoides is used has expanded beyond the original traditional uses against gastrointestinal disorders to include respiratory tract infections such as acute bronchitis, asthma, sinusitis and tonsilllopharyngitis. Accordingly, most of the experimental and clinical research has focused on the treatment of respiratory tract infections in line with the development of the phytopharmaceutical, EPs® 7630 (Umckaloabo®). In this regard, a wide array of pharmacological studies involving in vitro ( Table 1), in vivo ( Table 2) and randomised, double-blind, placebo-controlled clinical trials ( Table 3) has been conducted. Concomitantly, a diverse range of test systems has been used to evaluate the pharmacological properties of Pelargonium sidoides. The approaches, which are characterised by different levels of complexity, including the antimicrobial microdilution assay, anti-adhesion assay using HEp-2 cells, penicillin/gentamicin-protection assay, neuraminidase inhibition assay, fibroblast-virus protection assay and reverse transcription-polymerase chain reaction (RT-PCR) assay have helped in deciphering the pharmacological efficacies as well as the possible modes of action involved in the healing processes.
Table 1.
Evaluation of the pharmacological activities of Pelargonium sidoides DC. using in vitro methods.
| Biological activity (Test assay) | Extract/formulation | Test organism | Observed activity and effective concentration | Possible mode of action | Control | Reference |
|---|---|---|---|---|---|---|
| Antiviral activity (Neuraminidase inhibition assay) | aEPs® 7630 | H1N1 A/Puerto Rico/8/34 | EPs® 7630=5.4 µg/ml (EC50); EPs® 7630 (121.7 µg/ml) reduced neuraminidase activity by 50% | Interference with virus binding to host cell receptors | – | Theisen and Muller (2012) |
| Oligo-/polymeric fraction=2.8 µg/ml (EC50) | ||||||
| Gallocatechin-(4β→8)_gallocatechin=7.3 µg/ml (EC50) | ||||||
| Epigallocatechin-(4β→8)_gallocatechin=6.3 µg/ml (EC50) | ||||||
| Epigallocatechin=42.5 µg/ml (EC50) | ||||||
| Gallocatechin=28.4 µg/ml (EC50) | ||||||
| H3N2 A/Luxembourg/ 01/2005 | EPs® 7630=50 µg/ml (EC50) | |||||
| Anti-viral activity (Cytopathogenic effect reduction assay) | EPs® 7630 | H1N1 A/New Caledonia/20/99 | IC50=9.45 µg/ml | Inhibition of viral replication | – | Michaelis et al. (2011) |
| H3N2 A/California/7/2004 | IC50=8.66 µg/ml | Inhibition of viral replication | ||||
| RSV ATCC-No. VR-1540 | IC50=19.65 µg/ml | Inhibition of viral replication | ||||
| Human coronavirus HCo-229E | IC50=44.50 µg/ml | Inhibition of viral replication | ||||
| Parainfluenza virus 3 ATCC-No. VR-93 | IC50=74.35 µg/ml | Inhibition of viral replication | ||||
| Coxsackie A9 virus (isolated from a patient) | IC50=14.80 µg/ml | Inhibition of viral replication | ||||
| H5N1 A/Thailand/1(Kan-)/04 | IC50>100 µg/ml | – | ||||
| Adenovirus 3 GB ATCC-No. VR-3 | IC50>100 µg/ml | – | ||||
| Adenovirus 7 strain Gomen ATCC-No. VR-7 | IC50>100 µg/ml | – | ||||
| Human rhinovirus | IC50>100 µg/ml | – | ||||
| Antiviral activity (Fibroblast/EMCV protection assay) | EPs® 7630 | Encephalomyocarditis virus (EMCV) | EPs® 7630 (10 µg/ml)=80 U/ml | Inhibition of Cytopathic effect | LPS (1.0 ng/ml)=80 U/ml | Thäle et al. (2011) |
| Anti-viral activity (Plaque reduction assay) | Aqueous root extract | HSV-1 strain KOS | IC50=0.00006% | Inhibition of virus replication | Acyclovir | Schnitzler et al. (2008) |
| HSV-2 strain HG52 | IC50=0.000005% | Inhibition of virus replication | Acyclovir | |||
| Anti-viral activity (Fibroblast/EMCV protection assay) | Crude root extract | Encephalomyocarditis virus (EMCV) | EPs® 7630 (1.6 µg/ml)=100% inhibition | Inhibition of cytopathic effect; Modulation of IFN system | IFN-γ (100 U/ml) | Kolodziej et al. (2003) |
| Antibacterial activity (Microdilution assay) | 80% methanol tuber extract | Staphylococcus aureus ATCC 12600 | MIC=0.683 mg/ml | Inhibition of bacterial growth | Neomycin (MIC=1.302 mg/ml) | Moyo et al. (2013) |
| 80% methanol leaf extract | Enterococcus faecalis ATCC 19433 | MIC=0.097 mg/ml | Inhibition of bacterial growth | Neomycin (MIC=625 mg/ml) | ||
| Antibacterial activity (Microdilution assay) | Hairy root clones | Bacillus subtilis ATCC 6051 | Hairy root clone A4T-C (MIC=390 µg/ml) | Inhibition of bacterial growth | Streptomycin (MIC=1.56 µg/ml) | Colling et al. (2010) |
| Staphylococus aureus ATCC 12600 | A4T-C (MIC=780 µg/ml) | |||||
| Escherichia coli ATCC 11775 | A4T-C (MIC=780 µg/ml) | |||||
| Antibacterial activity (microdilution assay) | Root extract | Streptococcus pneumoniae; Streptococcus pyogenes; Streptococcus viridians; Staphylococcus aureus; Staphylococcus epidermidis; Neisseriae spp.; Haemophilus influenza (Clinical strains) | MIC=200–1600 μg/ml | Inhibition of bacterial growth | – | Uslu et al. (2009) |
| Antibacterial activity (Microdilution broth method) | Aqueous acetone root extract | Staphylococcus aureus ATCC 25923 incl. multi-resistant strains (1150.93; 1583.93; 999.93; 134.93; 1000.93) | MIC=3.3 mg/ml | Inhibition of bacterial growth | Bacterial starins resistant to antibiotics e.g. ciprofloxacin, erythromycin | Kolodziej et al. (2003) |
| Proteus mirabilis ATCC 14153 | MIC=3.3 mg/ml | |||||
| Antibacterial activity (Anti-adhesion assay using human HEp-2 cells) | EPs® 7630 (aqueous ethanolic extract) | Streptococcus pyogenes DSM 2071 (serogroup A) | 45% inhibition (@ 30 µg/ml) | Interaction with binding sites | Untreated group | Janecki et al. (2011) |
| Antibacterial activity (Anti-adhesive assay; substrate – gastric epithelial (AGS) cells) | EPs® 7630 | Helicobacter pylori (Clinical strains) | EPs® 7630 (50; 100 µg/ml) reduced bacterial attachment to AGS cells by 77% and 91%, respectively | Prevention of bacterial adhesion to AGS-cell membranes | Amoxicillin=no activity | Beil and Kilian (2007) |
| Antibacterial activity (Anti-adhesive assay; substrate human stomach epithelial tissue) | EPs® 7630 | Helicobacter pylori type I, strain G27 | Dose-dependent reduction in Helicobacter pylori adhesion to human gastric AGS-cell membranes (100% inhibition @ 10 mg/ml) | Inactivation of host (mucosal glycoproteins and epithelial mucins) bacterial adhesins interaction | 3'-/6'-Sialyllactose=100% inhibition; Abelmoschus Esculentus >90% inhibition | Wittschier et al. (2007) |
| Antibacterial activity (Flow cytometric adhesion assay with human HEp-2 cells and as substrate) | EPs® 7630 | Streptococcus pyogenes (Group A streptococci-GAS) DSM 2071 (serogroup A) | GAS adhesion to HEp-2 cells reduced by 46% @ 30 µg/ml | EPs® 7630 reduces bacterial adhesion to HEp-2 cells by targeting adhesion factors of GAS | Control (Samples without EPs® 7630): adhesion=80% HEp-2 cells | Conrad et al. (2007b) |
| Antibacterial activity (Flow cytometric adhesion assay with BEC as substrate) | EPs® 7630 | Streptococcus pyogenes (GAS) DSM 2071 (serogroup A) | EPs® 7630 (30 µg/ml): bacterial attachment was7-folder>control | Enhances attachment of bacteria to decaying BEC | Control: bacterial attachment to BEC=12.8% | Conrad et al. (2007b) |
| Antimycobacterial activity (Microdilution assay) | Butanol root extract | Mycobacterium smegmatis MC2 155 | MIC 0.156 µg/ml | Inhibition of bacterial growth | Ciprofloxacin (MIC=0.125 µg/ml) | Mativandlela et al.(2007) |
| Scopoletin | Mycobacterium smegmatis MC2 155 | MIC=7.81 µg/ml | Inhibition of bacterial growth | |||
| Umckalin | Mycobacterium smegmatis MC2 155 | MIC=62.5 µg/ml | Inhibition of bacterial growth | |||
| Catechin | Mycobacterium smegmatis MC2 155 | MIC=31.25 µg/ml | Inhibition of bacterial growth | |||
| Epigallocatechin | Mycobacterium smegmatis MC2 155 | MIC=7.81 µg/ml | Inhibition of bacterial growth | |||
| Antimycobacterial activity (BACTEC 460-radiometric assay) | Scopoletin; Umckalin; Catechin; Epigallocatechin | Mycobacterium tuberculosis ATCC 27294 | No activity @ 200 µg/ml | N/A | Isoniazid (@ 0.02 µg/ml | Mativandlela et al. (2007) |
| Antimycobacterial activity (Microdilution susceptibility assay) | EPs® 7630 fatty acids | Mycobacterium aurum A+ | Oleic acid (MIC-4 µg/ml); linoleic acid (MIC-2 µg/ml) | Inhibition of mycobacterial growth | Isoniazid (MIC=0.06 µg/ml) | Seidel and Taylor (2004) |
| Mycobacterium smegmatis ATCC 14468 | Linoleic acid (MIC-4 mg/ml) | Inhibition of mycobacterial growth | Isoniazid (MIC=1.0 mg/ml) | |||
| Antimycobacterial activity (Microdilution assay) | EPs® 7630 fatty acids (n-hexane extract) | Mycobacterium Aurum (Clinical strain) | Oleic acid (MIC-2 µg/ml); linoleic acid (MIC-2 µg/ml) | Inhibition of mycobacterial growth | – | Taylor (2003) |
| Antimycobacterial activity (Microplate Alamar blue assay) | Crude root extract | Mycobacterium tuberculosis H37Rv ATCC 27294 | Extract=100 μg/ml (MIC) | Inhibition of mycobacterial growth | Rifampicin (MIC=0.06 μg/ml) | Kolodziej et al. (2003) |
| Antimycobacterial activity (BACTEC 460-radiometric assay) | Crude root extract | Mycobacterium tuberculosis H37Rv ATCC 27294 | 96% Inhibition (@12.5 µg/ml) | Inhibition of mycobacterial growth | Kolodziej et al. (2003) | |
| Antifungal activity | 80% methanol leaf extract | Candida albicans ATCC 10231 | 0.781 mg/ml (MIC) | Inhibition of fungal growth | Amphotericin B (MIC=0.488 mg/ml) | Moyo et al. (2013) |
| Antifungal activity (Microbiological killing assay) | EPs® 7630 (aqueous ethanolic extract) | Candida albicans DSM 1386 ATCC 10231 | EPs® 7630 (30 µg/ml)=31% reduction in viable C. albicans cells | Intracellular killing is caused by a positive effect EPs® 7630 on the PBP killing activity | – | Conrad et al. (2007a) |
| Antifungal activity (Flow cytometry-based, whole blood method) | EPs® 7630 (aqueous ethanolic extract) | Candida albicans DSM 1386 ATCC 10231 | EPs® 7630 (30 µg/ml)=increased burst-active PBP to 120% after 4 min | Quick release of PBP to fight pathogens | – | Conrad et al. (2007a) |
| Antiparasitic activity (Intracellular leishmanicidal activity) | EPs® 7630 | Leishmania major strain LT 52, clone CC-1pXG-GFP | EPs® 7630 (0.1–10 μg/ml) Dose-dependent antileishmanial activity | Stimulation of NO release | Amphotericin B=1.0 μM | Thäle et al. (2011) |
| Antiparasitic activity (Intracellular leishmanicidal activity) | Methanol extract | Leishmania donovani | EC50=2.7 µg/ml | Activation of leishmanicidal macrophage functions | Pentostam (EC50=7.9 µg/ml) | Kayser et al. (2001) |
| Petroleum ether extract | Leishmania donovani | EC50=<0.1 µg/ml | ||||
| Ethyl acetate | Leishmania donovani | EC50=<0.1 µg/ml | ||||
| n-Butanol | Leishmania donovani | EC50=<3.3 µg/ml | ||||
| Gallic acid | Leishmania donovani | EC50=<4.4 µg/ml | ||||
| Gallic acid methyl ester | Leishmania donovani | EC50=<12.5 µg/ml | ||||
| Coumarims | Leishmania donovani | EC50=>25 µg/ml | ||||
| Immunomodulatory activity (Griess assay) | EPs® 7630 (1–30 μg/ml) | Listeria monocytogenes strain EGD serotype 1/2b | EPs®7630 (1–30 μg/mL) increased levels of NO; production of IL-1, IL-12, TNF-α | Bacterial inhibition through the antimicrobial effector molecule – NO | LPS (10 ng/ml)/IFN-γ (100 U/ml) | Thäle et al. (2008) |
| Immunomodulatory activity (Fluorescence-activated cell sorter analysis - FACS) | EPs® 7630 (30 μg/ml) | Listeria monocytogenes strain EGD serotype 1/2b | Concentration dependent increase in IL-1, IL-12 and TNF-α | Cytokine-induced macrophage activation | LPS (10 ng/ml)/IFN-γ (100 U/ml) | Thäle et al. (2008) |
| Immunomodulatory activity (Enzyme-linked immunosorbent assay - ELISA) | EPs® 7630 (1–30 μg/ml) | Listeria monocytogenes strain EGD serotype 1/2b | TNF-α (Listeria-infected BMMΦ)=(11.4–16.0 ng/mL) | Cytokine-induced macrophage activation | LPS (10 ng/ml)/IFN-γ (100 U/ml)=(9.8±1.1 ng/mL) | Thäle et al. (2008) |
| Immunomodulatory activity (Fibroblast-lysis assay-TNF activity) | EPs® 7630 | Leishmania donovani | Ethyl acetate fraction (25 µg/ml)=20.2 U/ml | Cytokine-induced macrophage activation | LPS (10 ng/ml)=184 U/ml | Kayser et al. (2001) |
| n-Butanol fraction (25 µg/ml)=18.9 U/ml | Cytokine-induced macrophage activation | |||||
| Gallic acid (25 µg/ml)=39 U/ml | Cytokine-induced macrophage activation | |||||
| Gallic acid methyl ester (25 µg/ml)=25.1 U/ml | Cytokine-induced macrophage activation | |||||
| Immunomodulatory activity (Fibroblast-virus protection assay-IFN activity) | EPs® 7630 | EMCV | Gallic acid: 12.5 µg/ml=0.4 U/ml; 25 µg/ml=3.7 U/ml; 50 µg/ml=17.9 U/ml | Inhibition of cytopathic effect; Modulation of IFN system | LPS (10 ng/ml) | Kayser et al. (2001) |
| Immunomodulatory activity (Greiss assay) | EPs® 7630 | Leishmania donovani | Gallic acid=54 µM (nitric oxide) | Induction of anti-infective effector molecule (=NO) | LPS 10 ng/ml)=119 µM | Kayser et al. (2001) |
| 7-Hydroxy-5,6-dimethoxycoumarin=40.8 µM (nitric oxide) | Induction of anti-infective effector molecule (=NO) | |||||
| 6,8-Dihydroxy-5,7-dimethoxycoumarin=46 µM (nitric oxide) | Induction of anti-infective effector molecule (=NO) | |||||
| Immunomodulatory activity (Reverse transcription-polymerase chain reaction: RT-PCR) | EPs® 7630 | Leishmania major LV9 | EPs® 7630 (50 μg/ml) up-regulation of iNOS, IL-12 and IL-18 mRNA levels | Molecular activation of cytokine gene expression | IFN-γ (100 U/ml)/LPS (10 ng/ml) | Trun et al. (2006) |
| Immunomodulatory activity (RT-PCR) | EPs® 7630 | Leishmania major LV9 | EPs® 7630 (50 μg/ml) up-regulation of iNOS and cytokine mRNA levels | Molecular activation of cytokine gene expression | IFN-γ (100 U/ml)/LPS (10 ng/ml) | Kolodziej et al. (2005) |
AGS=gastric epithelial cells; BEC=buccal epithelial cells; BMMΦ=Murine bone marrow-derived macrophages; ELISA=enzyme-linked immunosorbent assay; EMCV=Encephalomyocarditis virus; FACS=fluorescence-activated cell sorter analysis; GAS=Group A-streptococci; GFP=green fluorescent protein; Hep=Human epithelial cells; H1N1, H3N2=Influenza A virus strains; HSV=Herpes simplex virus type; IFN=interferon; IL=interleukin; LPS=Lipopolysaccharides; MIC=minimum inhibitory concentration; NO=inorganic nitric oxide; iNOS=inducible nitric oxide synthase; RSV=Respiratory syncytial virus; PBP=human peripheral blood phagocytes; RT-PCR=reverse transcription-polymerase chain reaction; TNF=tumour necrosis factor.
EPs® 7630=liquid herbal drug preparation of the root of Pelargonium sidoides (drug/extract ratio of 1:8–10) using aqueous ethanol (11% (m/m)) as extraction solvent (Conrad et al., 2007a,b).
Table 2.
In vivo studies in the pharmacological evaluation of Pelargonium sidoides DC.
| Biological activity | Extract/formulation | Experimental organism | Test organism | Administration | Dose range | Active concentration | Response | Control | Reference |
|---|---|---|---|---|---|---|---|---|---|
| Antiviral activity | EPs® 7630 | Female BALB/c mice | A/Puerto Rico/8/34H1N1 virus | Inhalation | 5 mg/kg | 5 mg/kg | Increased survival of virus-infected mice | Mice treated with vehicle | Theisen and Muller (2012) |
| Anticoagulant activity | EPs® 7630 | Male Sprague–Dawley rats | N/A | Oral | 10, 75, 500 mg/kg | 500 mg/kg p.o. | No effect on blood coagulation | Warfarin (0.05 mg/kg p.o.) | Koch and Biber (2007) |
| Central nervous system activity | Epigallo- and gallocatechin based oligomers of EPs® 7630 | Male NMRI mice | N/A | – | 200 mg/kg | 200 mg/kg | None to moderate effect on behavioural activity | Mice treated with vehicle | Schötz and Nöldner (2007) |
| Lipopolysaccharide (LPS) induced sickness behaviour | EPs® 7630 | Male NMRI-mice | N/A | Oral | 100, 200, 400 mg/kg | 400 mg/kg | Complete counteraction of LPS-induced sickness-behaviour | Mice treated with vehicle | Nöldner and Schötz (2007) |
EMCV=encephalomyocarditis virus; LPS=lipopolysaccarides; N/A=not applicable; NO=nitric oxide; Warfarin=3-(a-acetonylbenzyl)-4-hydroxy-coumarin.
Table 3.
Clinical studies on Pelargonium sidoides DC. and its related pharmaceutical products.
| Disease | Study design | No. of patients | Age (years) | Group size | Dosage /day | Duration | Outcomes measures | Result | Observed adverse events | Safety | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Acute bronchitis | Double-blind, placebo-controlled clinical trial with one adaptive interim analysis | 220 | 1–18 | EPs® 7630=111 vPlacebo=109 | 3×10 Drops (1–6 years) 3×20 drops (6–12 years) 3×30 drops (12–18 years) | 7 Days | Change in BBS score | EPs® 7630 (4.4); Placebo (2.9) (p<0.0001) | Gastrointestinal | All adverse events were non-serious | Kamin et al. (2012) |
| Acute bronchitis | Randomized, double-blind, placebo-controlled clinical dose-finding study with 4 parallel treatment groups | 400 | 6–18 | EPs® 7630 (30 mg/day)=100 EPs® 7630 (60 mg/day)=99 EPs® 7630 (90 mg/day)=99 Placebo=101 | 30, 60, 90 mg EPs® 7630 | 7 Days | Change in BBS score | EPs® 7630 (30 mg/day)=3.6 EPs® 7630 (60 mg/day)=4.4 EPs® 7630 (90 mg day)=5.5 Placebo=3.3 (p<0.0001) | Gastrointestinal | All adverse events were non-serious | Kamin et al. (2010) |
| Acute bronchitis | Randomised, double-blind, placebo-controlled, multicentre trial | 217 | ≥18 | EPs® 7630=108 Placebo=109 | 3×30 Drops | 7 Days | Change in BBS score | EPs® 7630 (7.6); Placebo (5.3) (p<0.0001) EPs® 7630-strong antitussive and “anti-fatigue” effects | Increased erythrocyte sedimentation rate | No serious adverse events recorded | Matthys and Funk (2008) |
| Acute bronchitis | Randomised, double-blind, placebo-controlled, multicentre study | 205 | 18–66 | EPs® 7630=108 Placebo=109 Adults: 18–66 years | 3×30 Drops | 7 Days | Change in BBS score | Decrease in BBS by: EPs® 7630 (7.6) Placebo (5.3); p<0.0001 | Gastrointestinal | No serious adverse events occurred during the study | Matthys and Heger (2007a) |
| Acute bronchitis | Prospective, open, multicentre outcomes study | N=205 | Mean total score of 5 typical bronchitis symptoms | Score decrease 6.1 (baseline)-2.8 (day 7) | Not specified | No serious adverse effects | Matthys and Heger (2007b) | ||||
| Acute bronchitis | multi-centre, prospective, open observational study | 2099 | 0–93 | All patients (n=2099); Children (3–18 years, n=498); infants (<2 years, N=78) | 3×10 Drops (<6 years) 3×20 drops (6–12 years) 3×30 drops (>12 years) | 14 Days | Change in BBS score | BSS decreased from a median of 7.1 at baseline to 1.0 at the 3rd follow-up | Gastrointestinal | All adverse events were non-serious | Matthys et al. (2007) |
| Acute bronchitis | Open and uncontrolled study | 742 | 0–12 | Children (upto 12 years old, N=742) | 3×5 Drops (0–2 years) 3×10 drops (2–6 years) 3×20 drops (>6 years) | 14 Days | Change in BBS score | Decrease in BBS score from 6.0 (baseline) to 1.4 (end of study) (p<0.001) | Exanthema; dyspnoea; diarrhoea | Adverse events-minor and transitory; disorders disappeared in 2 days | Haidvogl and Heger (2007) |
| Acute bronchitis | Randomised, Double-blind, placebo-controlled trial | 124 | ≥18 | EPs® 7630=64 Placebo=60 | 3×30 Drops | 7 Days | Change in BBS score | EPs® 7630 (7.2); Placebo (4.9) (p<0.0001) | Not specified | All adverse events were non-serious | Chuchalin et al. (2005) |
| Acute bronchitis | Double-blind, placebo-controlled trial | 468 | ≥18 | EPs® 7630=233 Placebo=235 | 3×30 Drops | 7 Days | Change in BBS score | EPs® 7630 (5.9); Placebo (3.2) (p<0.0001) | Gastrointenstinal; nervous system; respiratory and mediastinal; ear and labyrinth compliants | All adverse events were non-serious | Matthys et al. (2003) |
| Transient hypogammaglobulinemia of infancy (THI) | Double-blind, placebo controlled, prospective, monocentric pilot study | 28 | 1–5 | EPs® 7630=14Placebo=14 | 3×30 Drops | 7 Days | Symptom scoring | EPs® 7630 and placebo-no significant difference in symptom scores | Not specified | No adverse events | Patiroglu et al. (2012) |
| Immunomodulatory effect | Double-blind; Placebo-controlled trial | 25 | 26–56 | Pelargonium sidoides extract=11Placebo=14 | 3×30 Drops | 28 Days | Level of increase in salivary sIgA concentration | Herbal extract-213 µg/ml; Placebo-41.16 µg/ml | Not specified | No safety evaluation done | Luna et al. (2011) |
| Common cold | Randomised, double-blind, parallel group, placebo-controlled trial | 103 | 18–55 | EPs® 7630=52 Placebo=51 | 3×30 drops | 10 Days | Change in SSID | SSID values: EPs® 7630 (14.6); Placebo (7.6) (p<0.0001) | Tracheitis;epistaxis | All adverse events were non-serious | Lizogub et al. (2007) |
| Acute rhinosinusitis (of presumably bacterial origin) | Randomised; Double-blind, parallel group, placebo-controlled trial | 103 | 18–60 | EPs® 7630=51 Placebo=52 | 3×60 Drops | 22 Days | Change in SSS | SSS mean decrease: EPs® 7630 (5.5); Placebo (2.5)(p<0.00001) | Gastrointestinal; allergic skin reaction | All adverse events were non-serious | Bachert et al. (2009) |
| Asthma attacks during viral infections | Asthmatic children in randomised study | 61 | 1–14 | EPs® 7630=30 Control=31 | 3×10 drops (1–5 years) 3×20 drops (6–12 years) 3×30 drops (>12 years) | 5 Days | Symptom score | EPs® 7630 group had less frequency of asthma attacks (p<0.05) | Not specified | No safety evaluation done | Tahan and Yaman (2013) |
| Chronic obstructive pulmonary disease (COPD) | Double-blind, parallel group, placebo-controlled clinical trial | 200 | ≥18 | EPs® 7630=99 Placebo=101 | 3×30 Drops | 24 Weeks | Time to first exacerbation of COPD | EPs® 7630=57 days; Placebo=43 days (p=0.005) EPs® 7630: 37.8% needed antibiotic treatment vs 73.3% for placebo (p<0.0001) | Gastrointestinal | All adverse events were non-serious | Matthys et al. (2013) |
| Acute non-group A beta-hemolytic streptococcus tonsillopharyngitis | Randomized, double-blind, placebo-controlled trial | 143 | 6–10 | EPs® 7630=73 Placebo=70; Children (6–10 years) | 3×20 Drops | 6 Days | Change in TSS score from baseline | TSS mean decrease: EPs® 7630 (7.1 points); Placebo (2.5 points); (p<0.0001) | Not specified | Adverse events were independent of investigational medication | Bereznoy et al. (2003) |
BBS=Bronchitis Symptom Score; COPD=Chronic obstructive pulmonary disease; sIgA=secretory immunoglobulin A; SSID=Symptom Intensity Differences; SSS=Sinusitis Severity Score; THI=Transient hypogammaglobulinemia of infancy; TSS=Tonsillopharyngitis Severity Score.
3.1. In vitro studies
Pelargonium sidoides extracts have been tested and exhibited good activity against a number of viruses, including influenza A viruses (H1N1, H3N2), coxsackie A9 virus, human coronavirus, respiratory syncytial virus (RSV), parainfluenza virus 3 and herpes simplex viruses (HSV-1, HSV-2) (Table 1). However, the EPs® 7630 phytopharmaceutical had poor activity (IC50=>100 µg/ml) against the highly pathogenic avian influenza A virus (H5N1) (Michaelis et al., 2011). Notably, the EPs® 7630 extract had high in vitro activity against H1N1 (IC50=5.4 µg/ml) (Theisen and Muller, 2012) and H3N2 (IC50=8.66 µg/ml) (Michaelis et al., 2011) attesting to its use in respiratory health conditions. The authors noted that the EPs® 7630 extract was more active against enveloped viruses compared to non-enveloped viruses (adenovirus 3, adenovirus 7 and human rhinovirus). Interestingly, antiviral bioactivity (EC50) of isolated phenolic constituents against H1N1 increased in the order of complexity of their chemical chain structure as follows: epigallocatechin (42.5 µg/ml)>gallocatechin (28.4 µg/ml)>gallocatechin-(4β→8)-gallocatechin (7.3 µg/ml)>epigallocatechin-(4β→8)-gallocatechin (6.3 µg/ml)>oligo-/polymeric fraction (2.8 µg/ml) (Theisen and Muller, 2012). The study reported a poor direct virucidal activity of EPs® 7630 (250 µg/ml). Instead the authors discovered that the extract and its phenolic constituents imparted anti-viral activity by interfering with virus binding to host cell receptors and through inhibition of the neuraminidase enzyme. Furthermore, the control of viral infections may occur through the production of interferons (IFNs) by the host cells, suggesting that therapy by Pelargonium sidoides may be through the stimulation of the innate immune system (Kolodziej, 2007). Based on the current state of research using in vitro models it is clear that the mode of action of Pelargonium sidoides in antiviral activity may involve several mechanisms. The mode of action of the antiviral constituents in Pelargonium sidoides has also not been explained using in vivo models, for example Theisen and Muller (2012) only showed that EPs® 7630 increased survival of H1N1 virus-infected mice, but did not explain the underlying mechanisms involved (Table 2). Further studies incorporating molecular approaches may help to understand the mechanism of action of the antiviral active constituents.
In traditional medicine, extracts of Pelargonium sidoides are used to treat bacterial-related conditions such as diarrhoea, dysentery and tuberculosis (Hutchings et al., 1996). In South Africa, many plant species are used to alleviate symptoms of tuberculosis caused by Mycobacterium tuberculosis, the fifth largest cause of mortality in the country (McGaw et al., 2008). Pelargonium sidoides plant extracts have been tested against Mycobacterium species as well as several Gram-positive (Bacillus subtilis, Enterococcus faecalis, Staphylococcus aureus, Streptococcus pyogenes) and Gram-negative (Escherichia coli, Proteus mirabilis, Helicobacter pylori) bacteria. Most notably, EPs® 7630 had moderate in vitro activity against multi-resistant Staphylococcus aureus with a minimum inhibitory concentration (MIC) of 3.3 mg/ml (Kolodziej et al., 2003). The same bacterial strains were resistant to common antibiotics such as ciprofloxacin and erythromycin. This study provided a significant finding and highlighted the importance of Pelargonium sidoides as a potential alternative antibacterial remedy at a time when resistance to antibiotics is fast becoming a medical challenge. However, there is need of a paradigm shift towards experimentation that provides more biological insights on the molecular mechanisms involved in the observed in vitro activity. A Pelargonium sidoides butanol extract had higher activity (MIC=0.156 µg/ml) compared to that of its isolated chemical entities such as umckalin (MIC=62.5 µg/ml) against Mycobacterium smegmatis possibly due to synergistic effects (Mativandlela et al., 2007). The efficacy of a natural product may be due to two or more constituents acting synergistically, whereby their respective bioactivities often diminish or disappear upon separation into individual chemical entities (Li and Vederas, 2009). Synergism of bioactive compounds in phytopharmaceuticals is normally claimed to account for their therapeutic effectiveness (Wagner and Ulrich-Merzenich, 2009). In particular, polyphenolic compounds in plant extracts are known to increase the pharmacokinetic rate of anti-infective constituents in phytopharmaceuticals thereby enhancing their bioavailability (Wagner, 2011). In addition, these natural products can also work synergistically with antibiotics thereby improving their overall pharmacokinetic properties against resistant bacterial strains (Schmidt et al., 2007). However, the moderate MICs suggest that Pelargonium sidoides constituents have no direct effect on the bacteria. Thus, further studies have attempted to elucidate the modes of action of its active constituents. Beil and Kilian (2007) and Conrad et al. (2007b) working on Helicobacter pylori and Streptococcus pyogenes, demonstrated that EPs® 7630 prevents the bacteria from adhering to gastric AGS-cell membranes and HEp-2 cells, respectively. These studies showed that the possible mode of action of the bioactive constituents is through modulation of host-bacteria interactions and phagocytosis, which prevent bacterial attachment to the substrate (gastric and human epithelial cells) thereby rendering the pathogens ineffective. The bioactive constituents of Pelargonium sidoides have been shown to specifically target adhesion factors of the bacteria rather than those of the epithelial cell membranes (Conrad and Frank, 2008).
Immunomodulatory activities of Pelargonium sidoides and its related phytopharmaceutical medicine may also account for the observed moderate bioactivity against bacteria associated with respiratory diseases through activation of the host cells macrophage machinery. Kayser et al. (2001) demonstrated that murine macrophages infected with Leishmania parasites induced the production of the reactive nitrogen intermediary, inorganic nitric oxide (NO), a known antimicrobial effector molecule. The study showed that gallic acid and the highly oxygenated coumarins, 7-hydroxy-5,6-dimethoxycoumarin (umckalin) and 6,8-dihydroxy-5,7-dimethoxycoumarin were the most potent NO-inducers. Thäle et al. (2008) further proved that activated macrophages obtained from C57BL/6 WT mice were key components of the antimicrobial immune response against Listeria monocytogenes through the production of NO. Compared to the control (2.2 µM), infected cells treated with EPs® 7630 significantly increased release of NO in a dose-dependent response from 1.0 µg/ml (2.8 µM) to 30 µg/ml (5.5 µM). In both models, infected macrophages had a higher NO-inducing effect compared to non-infected macrophages indicating that the nonspecific immune response was triggered under disease attack (Kayser et al., 2001, Thäle et al., 2008). In Leishmania major-infected macrophage-like RAW 264.7 cells exposed to EPs® 7630, there was a marked up-regulation of inducible nitric oxide synthase (iNOS) gene expression evaluated by reverse transcription-polymerase chain reaction (RT-PCR) (Kolodziej et al., 2005, Trun et al., 2006). In diseased cells, the molecular expression of iNOS in activated macrophages stimulates the production of high levels of NO, which is an antimicrobial effector molecule (Nathan and Hibbs, 1991). In particular, gallic acid, one of the constituents of the EPs® 7630 (Kayser et al., 2001) has been shown to induce prolonged iNOS mRNA expression in Leishmania-infected cells. In addition, release of tumour necrosis factor (TNF-α) and interferons (IFN) provided further evidence for cytokine-induced macrophage activation and plays a crucial role in immune defence mechanisms in infected cells (Reiner and Locksley, 1995). Experimental data has shown that the TNF-inducing potential of Pelargonium sidoides is strongly associated with its phenolic constituents (Kolodziej and Kiderlen, 2007). The methanol extract of Pelargonium sidoides (25 µg/ml) exhibited negligible TNF-inducing potential (<0.1 U/ml) compared to the moderate activity of the ethyl acetate (20.2 U/ml) and n-butanol (18.9 U/ml) fractions (Kayser et al., 2001). Most significantly, gallic acid (6.25–50 µg/ml) led to a high dose-dependent increase in TNF-inducing potency (21–43.7 U/ml) of infected cells. Radtke et al. (2004) also demonstrated the concomitant TNF-α mRNA gene expression in infected cells. On the other hand, gallic acid was shown to increase IFN-α level in Leishmania-infected cells (Kolodziej et al., 2005) coupled with the up-regulation of IFN-γ mRNA transcripts (Radtke et al., 2004, Kolodziej et al., 2005). Most notably, umckalin, the signature chemical entity in Pelargonium sidoides exhibited poor cytokine gene expression profiles.
3.2. In vivo studies
Table 2 presents a summary of pharmacological evaluations using in vivo animal models. Despite the importance of animal models in the evaluation of pharmacological efficacy, only a few studies have utilised this system for Pelargonium sidoides and/or its related formulations. Good research practice for plant-derived medicines dictates that in vitro tests should be backed up with in vivo and ultimately clinical studies (Houghton et al., 2007). More studies on Pelargonium sidoides should adopt this approach so as to avoid the pitfalls associated with extrapolating in vitro test results to claim in vivo activity and efficacy. Cos et al. (2006) argued that animal models are indispensable in validating in vitro activity because they take into account pharmacokinetic, metabolic and toxicological phenomena. Based on this approach, Yu et al. (2010), Tian et al. (2011) and Li et al. (2013) used in vitro and in vivo antiviral models thereby obtaining comprehensive pharmacological data including efficacy and toxicology of several Chinese herbal medicines. Recently, Theisen and Muller (2012) confirmed in vitro antiviral activity of EPs® 7630 using an in vivo animal model system. Therefore, both in vitro and in vivo models should be considered in future Pelargonium sidoides anti-infective research. In addition, the research can also focus on developing better in vivo model systems to elucidate the actual mechanisms involved in the therapeutic processes of Pelargonium sidoides, which have so far remained unclear.
3.3. Clinical studies
The phytopharmaceutical, EPs® 7630 has undergone numerous clinical evaluations in randomised, double-blind, placebo-controlled trials. Incidentally, it has been clinically evaluated against respiratory-related conditions, namely acute bronchitis, acute rhinosinusitis, common cold, chronic obstructive pulmonary disease and asthma (Table 3). The clinical trials conducted for EPs® 7630 have included patients of all ages. The reported results suggest that the Pelargonium sidoides herbal medicine may be effective in the treatment of respiratory infections caused by bacteria and viruses. Among the common respiratory tract infections, most of the clinical studies have evaluated the phytopharmaceutical against acute bronchitis in placebo-controlled studies. Acute bronchitis is characterised by acute inflammation of the respiratory tract and is caused by viral infections in 95% of the cases (Matthys and Heger, 2007b). However, more clinical studies have to be done to determine its efficacy in the treatment of other common respiratory diseases. Despite the limited benefit of antibiotic therapy for acute bronchitis, they are prescribed in 60–80% of the cases (Matthys and Heger, 2007a). Against this background, more appropriate treatment options are required so as to prevent the overuse and/or abuse of antibiotics. In this regard, phytopharmaceuticals such as Pelargonium sidoides-based products may provide an alternative therapeutic option in the treatment of respiratory tract infections and related ailments.
3.4. Safety evaluation
It is of paramount importance that medicinal plants and phytopharmaceuticals are safe and do not cause undesirable side effects in patients. However, despite its long history of use in traditional medicine, there is a dearth of scientific information pertaining to the safety evaluation of Pelargonium sidoides. The Pelargonium sidoides extract, EPs® 7630, did not cause obvious toxic effects in mice as there were no significant differences in body weight, body temperature as well as organ weight (lungs, liver, spleen, kidneys) between the treatment and control groups (Theisen and Muller, 2012). Based on clinical data, the tolerability of treatment with EPs® 7630 has been shown to be good in both adults and children (Table 3). Nevertheless, some of the commonly reported adverse events included gastrointestinal complaints such as diarrhoea (Matthys et al., 2003, Matthys et al., 2007, Matthys et al., 2013, Haidvogl and Heger, 2007, Matthys and Heger, 2007a, Bachert et al., 2009, Kamin et al., 2010, Kamin et al., 2012), nervous system complaints (Matthys et al., 2003), respiratory and mediastinal ailments (Matthys et al., 2003), ear and labyrinth complaints (Matthys et al., 2003), exanthema (Haidvogl and Heger, 2007), tracheitis and epistaxis (Lizogub et al., 2007) and allergic skin reactions (Bachert et al., 2009). Recently, a clinical study by Teschke et al. (2012) concluded that Pelargonium sidoides did not reveal evidence of hepatotoxicity. However, even though the adverse events in most clinical studies have been reported as non-serious, more rigorous studies are still required to ascertain the safety of Pelargonium sidoides and its related formulations. In addition, further toxicological studies involving toxicity and mutagenic tests need to be done to evaluate the safety of this plant. Although the benefits of medicinal plants are widely acknowledged, the need for safety evaluation remains critical so as to distinguish between toxic effects and pharmacological efficacy of plant extracts (Aremu and van Staden, 2013). Based on the numerous studies reported in the current review, there is compelling experimental and clinical evidence to suggest that Pelargonium sidoides may be efficacious against respiratory tract infections and may be safe for both adults and children, but more stringent toxicological studies are required. Verschaeve and Van Staden (2008) have comprehensively discussed the various methods that are used in evaluating the safety of medicinal plants.
4. Commercial potential and world marketing
Besides its local use as a multipurpose traditional remedy, Pelargonium sidoides has evolved into an international phytopharmaceutical. The commercialisation of Pelargonium sidoides dates back to the early 1900s when the plant was introduced in Europe as a tuberculosis remedy by Charles Henry Stevens after being reportedly cured by a traditional healer in Lesotho (Bladt and Wagner, 2007, Brendler and van Wyk, 2008, Wynberg et al., 2012). The growing international demand for the Pelargonium sidoides root extract has led to an increase in the number of gatherers as well as the volume of harvested plant materials. Its evolution from a traditional medicine exclusive to southern Africa, mainly South Africa and Lesotho, into a successful phytopharmaceutical (Umckaloabo®) has created ‘the Pelargonium industry’ involving a network of harvesters, local buyers and processors and international pharmaceutical manufacturers, such as Dr. Willmar Schwabe GmbH & Co., KG Pharmaceuticals (Karlsruhe, Germany). Pelargonium trade has evolved from a largely unregulated to a more formalised industry over the past 20 years (Wynberg et al., 2012). An unknown number of harvesters in the Eastern Cape (South Africa) and Lesotho collect and sell the plant materials to local intermediary buyers (Van Niekerk and Wynberg, 2012, Newton et al., 2013). The organisation of trade in medicinal plants normally involves a chain of local dealers buying plant materials from local collectors and eventually selling to larger trading and export companies (Lubbe and Verpoorte, 2011). In the Eastern Cape, Gowar Enterprises collects and supplies the Pelargonium sidoides tuberous roots to another intermediary, BZH Import and Export, responsible for drying, shredding, packaging and onward routing to Parceval Pharmaceuticals, which exports the materials to the end-product manufacturer in Germany (Van Niekerk and Wynberg, 2012). In Lesotho, Bophelo Processing is responsible for collecting, processing and supplying of the tubers to Parceval Pharmaceuticals (Wynberg et al., 2012). The processing of the raw materials obtained from developing economies involved in the medicinal plant trade is still predominantly undertaken in European countries by end-product manufacturers (Lubbe and Verpoorte, 2011) and this also applies to Pelargonium sidoides.
The commercial success of Umckaloabo® provides a good example of what can be achieved with a well-directed research and development initiative and astute marketing (Gericke, 2011). Most of the harvesters mainly rely on wild collection of Pelargonium sidoides for their livelihoods due to limited alternative economic opportunities in these communities. Amidst the overall commercial success of the Pelargonium trade, questions have been asked about the possible vulnerability of the harvesters and their lack of bargaining power arising from the monopolistic marketing chain (Van Niekerk and Wynberg, 2012). Large trading companies have significant control over the pricing system due to their central role in the medicinal plant trade coupled to large scale purchases and ownership of critical infrastructure to perform several functions including quality control (Lubbe and Verpoorte, 2011). However, despite these challenges related to beneficiation equity from medicinal resources, lessons arising from the Pelargonium sidoides case study are clearly invaluable for future natural product research and development programmes in developing countries. An increasing number of medicinal plant suppliers in China, India, Mexico and Malaysia are now exporting processed products to end-product manufacturers in Western countries (Lubbe and Verpoorte, 2011). The ‘Pelargonium industry’ may have to evolve in tandem to this growing trend in the medicinal plant trade.
5. Biotechnology applications in Pelargonium sidoides conservation
The increasing commercial demand for Pelargonium sidoides on the international market has led to localised uncontrolled, indiscriminate and sometimes illegal harvesting of wild plants (Lewu et al., 2006, Lewu et al., 2007, Wynberg et al., 2012). The escalation in demand can cause irreparable reductions to wild populations (Colling et al., 2010), which may result in a biodiversity threat to Pelargonium sidoides. However, the conservation status of Pelargonium sidoides was recently revised from ‘declining’ (Red Data List of South African Plants, 2009) to ‘least concern’ (Red Data List of South African Plants, 2013). In Lesotho, the conservation status of Pelargonium sidoides has not been evaluated. In addition, the plant is not listed on either the International IUCN Red List of Threatened Species or Convention on International Trade in Endangered Species (CITES) database (Newton et al., 2013). There is a conspicuous lack of comprehensive data on annual harvested and traded volumes of Pelargonium sidoides. Varying estimates derived from data collected through interviews have been reported in literature. The estimates of annual harvested fresh material range from 9 to 45 t (Newton et al., 2013) and 26–440 t (Van Niekerk and Wynberg, 2012). Despite this lack of accurate data, tight conservation regulations have been formulated to curb uncontrolled harvesting in South Africa (Newton et al., 2013). Notwithstanding the occasional financial returns obtained by the local communities, the overexploitation of the resource may affect its availability in the future. In the Eastern Cape, the plants had a slow regeneration rate, which was significantly lower than the initial harvest after the second year (Lewu et al., 2007). To meet the ever-expanding demand in international trade of raw materials, Pelargonium sidoides may have to be cultivated on a large scale. Currently, the plant is only cultivated on a small, negligible scale (Colling et al., 2010). There are also limitations in the use of seed propagation, due to their low viability coupled with low germination (Lewu et al., 2006).
Alternatively, biotechnology tools such as plant tissue culture ( Fig. 1D) may play a critical role in the provision of genetically uniform clones for the Pelargonium industry (Moyo et al., 2013). Recently, Kotzé (2011), Moyo et al. (2012) and Moyo et al. (in press) reported on micropropagation and acclimatisation procedures with the capacity to produce millions of uniform Pelargonium sidoides clones throughout the year. There is a long history of the commercial production of high-value phytochemicals using tissue culture systems (Canter et al., 2005). However, a major challenge with the cultivation of medicinal plants is the perception that such plants do not produce a similar quality of bioactive compounds as wild plants. White et al. (2008) and Moyo et al. (2013) showed that greenhouse produced plants had similar bioactive compounds as wild plants in terms of the umckalin (6-hydroxy-5,7-dimethoxycoumarin) and phenolic compounds, respectively. In addition, extracts of greenhouse and wild plants exhibited comparable antimicrobial and antioxidant properties (Moyo et al., 2013). In the long term, the production of Umckaloabo® may have to be based on plant material produced under consistent cultivation practices. Such cultivated material produced under controlled environmental conditions is preferred for the phytopharmaceutical industry as it minimises qualitative and quantitative variations in the composition of natural products (Lubbe and Verpoorte, 2011). In addition, the quality of phytopharmaceuticals can be improved by the use of genetically uniform clones, which eliminates problems associated with product adulteration (Schmidt et al., 2007).
Fig. 1.
Pelargonium sidoides. (a) Young tuberous roots; (b) a flowering plant; (c) cross section of a tuberous root; and (d) high shoot multiplication in a plant tissue culture system.
On the other hand, the future pharmaceutical production of Umckaloabo® may also eventually depend on the application of bioreactor technology in the synthesis of Pelargonium sidoides bioactive compounds. Colling et al. (2010) demonstrated the ability of transgenic Pelargonium sidoides hairy root cultures, transformed using Agrobacterium rhizogenes, to produce the desired bioactive pharmaceutical compounds. The authors concluded that the system has immense potential as a conservation strategy for this medicinally important plant. However, there is a possibility that phytotherapeutics produced using biotechnology may not be readily acceptable by consumers of ‘natural’ medicines. Notwithstanding these concerns, it may be inevitable that biotechnology will play a key role in the production of plant-derived pharmaceutical compounds in the future. Hairy root cultures which are transformed using Agrobacterium rhizogenes often sustain stable and high productivity in plant growth regulator-free medium (Canter et al., 2005). Thus, the use of biotechnology approaches can allow for ease of standardisation of the chemical constituents of the phytopharmaceutical thereby guaranteeing consistent quality of the end-product. Overall, this will help to avert the current plant biodiversity conservation dilemma arising from overharvesting practices of wild populations.
6. Conclusions
Despite the emergence, in recent times, of high-throughput screening of synthetic chemical libraries as an alternative technology for the pharmaceutical industry, natural products remain a vital component in drug discovery. In particular, medicinal plants offer several advantages as potential sources of both novel chemical entities and phytopharmaceuticals. The pharmacological activities that have been demonstrated in various in vitro, in vivo and clinical studies indicate that Pelargonium sidoides possesses moderate direct anti-infective properties but highly notable immunomodulatory activity. In addition, Pelargonium sidoides root extract is effective and well tolerated in the treatment of respiratory-related infections. Based on both experimental and clinical pharmacological evidence, the transformation of Pelargonium sidoides from a traditional medicine to a successful phytopharmaceutical provides a compelling argument for the continued exploration of medicinal plants and indigenous medical systems for the next generation of phytopharmaceuticals. Even though significant milestones have been achieved in Pelargonium sidoides pharmacological research, further studies are still needed to fully elucidate the mechanisms of action and the biological principles underlying its therapeutic capacity. Most notably, the bulk of the pharmacological research on Pelargonium sidoides has been skewed towards respiratory tract infections at the expense of ailments for which the plant is used in Traditional African Medicine. Clinical research should also focus on other respiratory tract infections besides acute bronchitis, which has so far attracted the most attention. Furthermore, there is lack of conclusive data on the toxicological properties of Pelargonium sidoides despite having been used in traditional medicine for a long time. Stringent evaluation of the toxicological properties of Pelargonium sidoides is of paramount importance given its extensive use in medicinal formulations.
In the long term, the successful commercialisation of this southern African medicinal plant must be viewed in a much wider and holistic context that includes conservation-friendly practices and the sustainable supply of raw materials. In that context, the sustenance of the Pelargonium sidoides phytopharmaceutical industry will require innovative approaches, which utilise biotechnology tools such as plant tissue culture and bioreactors for the production of genetically uniform clones and therapeutic secondary metabolites, respectively.
Acknowledgements
Financial support from the University of KwaZulu-Natal (South Africa) for a Postdoctoral Fellowship for MM is gratefully acknowledged. We thank Dr Adeyemi O. Aremu for his critical evaluation of the manuscript.
References
- Aremu A.O., van Staden J. The genus Tulbaghia (Alliaceae)—A review of its ethnobotany, pharmacology, phytochemistry and conservation needs. J. Ethnopharmacol. 2013;149:387–400. doi: 10.1016/j.jep.2013.06.046. [DOI] [PubMed] [Google Scholar]
- Bachert C., Schapowal A., Funk P., Kieser M. Treatment of acute rhinosinusitis with the preparation from Pelargonium sidoides EPs® 7630: a randomized, double-blind, placebo-controlled trial. Rhinology. 2009;47:51–58. [PubMed] [Google Scholar]
- Beil W., Kilian P. EPs® 7630, an extract from Pelargonium sidoides roots inhibits adherence of Helicobacter pylori to gastric epithelial cells. Phytomedicine. 2007;14:5–8. doi: 10.1016/j.phymed.2006.11.024. [DOI] [PubMed] [Google Scholar]
- Bereznoy V.V., Riley D.S., Wasmer G., Heger M. Efficacy of extract of Pelargonium sidoides in children with acute non-group A beta-hemolytic streptococcus tonsillopharyngitis: a randomized, double-blind, placebo-controlled trial. Altern.Ther. Health Med. 2003;9:68–79. [PubMed] [Google Scholar]
- Bladt S., Wagner H. From Zulu traditional medicine to European phytomedicne Umckaloabo®. Phytomedicine. 2007;14:2–4. doi: 10.1016/j.phymed.2006.11.030. [DOI] [PubMed] [Google Scholar]
- Bourdette, F.M.R., 2012. The efficacy of Linctagon® spray for the prevention of colds and influenza in female soccer team players of the University of Johannesburg (MTech dissertation). University of Johannesburg.
- Brendler T., van Wyk B.-E. A historical, scientific and commercial perspective on the medicinal use of Pelargonium sidoides (Geraniaceae) J. Ethnopharmacol. 2008;119:420–433. doi: 10.1016/j.jep.2008.07.037. [DOI] [PubMed] [Google Scholar]
- Canter P.H., Thomas H., Ernst E. Bringing medicinal plants into cultivation: opportunities and challenges for biotechnology. Trends Biotechnol. 2005;23:180–185. doi: 10.1016/j.tibtech.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Chuchalin A.G., Berman B., Lehmacher W. Treatment of acute bronchitis in adults with a Pelargonium sidoides preparation (EPs® 7630): a randomised, double-blind controlled trial. Explore. 2005;1:437–445. doi: 10.1016/j.explore.2005.08.009. [DOI] [PubMed] [Google Scholar]
- Colling J., Groenewald J.-H., Makunga N.P. Genetic alterations for increased courmarin production lead to metabolic changes in the medicinally important Pelargonium sidoides DC. (Geraniaceae) Metab. Eng. 2010;12:561–572. doi: 10.1016/j.ymben.2010.08.001. [DOI] [PubMed] [Google Scholar]
- Conrad A., Frank U. Extract of Pelargonium sidoides (EPs® 7630) displays anti-infective properties by enhanced phagocytosis and differential modulation of host–bacteria interactions. Planta Med. 2008;74:682–685. doi: 10.1055/s-2008-1034287. [DOI] [PubMed] [Google Scholar]
- Conrad A., Hansmann C., Engels I., Daschner F.D., Frank U. Extract of Pelargonium sidoides (EPs® 7630) improves phagocytosis, oxidative burst, and intracellular killing of human peripheral blood phagocytes in vitro. Phytomedicine. 2007;14:46–51. doi: 10.1016/j.phymed.2006.11.016. [DOI] [PubMed] [Google Scholar]
- Conrad A., Jung I., Tioua D., Lallemand C., Carrapatoso F., Engels I., D. Daschner F.D., Frank U. Extract of Pelargonium sidoides (EPs® 7630) inhibits the interactions of group A-streptococci and host epithelia in vitro. Phytomedicine. 2007;14:52–59. doi: 10.1016/j.phymed.2006.11.018. [DOI] [PubMed] [Google Scholar]
- Cos P., Vlietinck A.J., Van den Berghe D., Maes L. Anti-infective potential of natural products: how to develop a stronger in vitro ‘proof-of-concept’. J. Ethnopharmacol. 2006;106:290–302. doi: 10.1016/j.jep.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Gericke N. Muthi to medicine. South Afr. J. Bot. 2011;77:850–856. [Google Scholar]
- Gödecke, T., Kaloga, M., Kolodziej, H., 2003. Unusual coumarins and antitubercular activity of the aerial parts of Pelargonium sidoides. In: Proceedings of the 51st Annual Congress of Medicinal Plant Research, Kiel.
- Gödecke T., Kaloga M., Kolodziej H. A phenol glucoside, uncommon coumarins and flavonoides from Pelargonium sidoides DC. Z. Naturforsch. 2005;60b:677–682. [Google Scholar]
- Haidvogl M., Heger M. Treatment effect and safety of EPs® 7630-solution in acute bronchitis in childhood: report of a multicentre observational study. Phytomedicine. 2007;14:60–64. doi: 10.1016/j.phymed.2006.11.014. [DOI] [PubMed] [Google Scholar]
- Hauer H., Germer S., Elsäßer J., Ritter T. Benzopyranones and their sulfate esters from Pelargonium sidoides. Planta Med. 2010;76:350–352. doi: 10.1055/s-0029-1186167. [DOI] [PubMed] [Google Scholar]
- Houghton P.J., Howes M.-J., Lee C.C., Steventon G. Uses and abuses of in vitro tests in ethnopharmacology: visualising an elephant. J. Ethnopharmacol. 2007;110:391–400. doi: 10.1016/j.jep.2007.01.032. [DOI] [PubMed] [Google Scholar]
- Hutchings A., Scott A.H., Lewis G., Cunningham A. Natal University Press; Pietermaritzburg: 1996. Zulu Medicinal Plants. [Google Scholar]
- Janecki A., Conrad A., Engels I., Frank U., Kolodziej H. Evaluation of an aqueous-ethanolic extract from Pelargonium sidoides (EPs® 7630) for its activity against group A-streptococci adhesion to human HEp-2 epithelial cells. J. Ethnopharmacol. 2011;133:147–152. doi: 10.1016/j.jep.2010.09.018. [DOI] [PubMed] [Google Scholar]
- Kamin W., Ilyenko L.I., Malek F.A., Kieser M. Treatment of acute bronchitis with EPs® 7630: randomized, controlled trial in children and adolescents. Pediatr. Int. 2012;54:219–226. doi: 10.1111/j.1442-200X.2012.03598.x. [DOI] [PubMed] [Google Scholar]
- Kamin W., Maydannik V.G., Malek F.A., Kieser M. Efficacy and tolerability of EPs® 7630 in patients (aged 6–18 years old) with acute bronchitis: a randomized, double-blind, placebo-controlled clinical dose-finding study. Acta Paediatr. 2010;99:537–543. doi: 10.1111/j.1651-2227.2009.01656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayser O., Kolodziej H. Highly oxygenated coumarins from Pelargonium sidoides. Phytochemistry. 1995;39:1181–1185. [Google Scholar]
- Kayser O., Kolodziej H., Kiderlen A.F. Immunomodulatory principles of Pelargonium sidoides. Phytother. Res. 2001;15:122–126. doi: 10.1002/ptr.785. [DOI] [PubMed] [Google Scholar]
- Koch E., Biber A. Treatment of rats with the Pelargonium sidoides extract EPs® 7630 has no effect on blood coagulation parameters or on the pharmacokinetics of warfarin. Phytomedicine. 2007;14:40–45. doi: 10.1016/j.phymed.2006.11.026. [DOI] [PubMed] [Google Scholar]
- Kolodziej H. Fascinating metabolic pools of Pelargonium sidoides and Pelargonium reniforme, traditional and phytomedicinal sources of the herbal medicine Umckaloabo. Phytomedicine. 2007;14:9–17. doi: 10.1016/j.phymed.2006.11.021. [DOI] [PubMed] [Google Scholar]
- Kolodziej H., Burmeister A., Trun W., Radtke O.A., Kiderlen A.F., Ito H., Hatano T., Yoshida T., Foo L.L. Tannins and related compounds induce nitric oxide synthase and cytokines gene expressions in Leishmania major-infected macrophage-like RAW 264.7 cells. Bioorg. Med. Chem. 2005;13:6470–6476. doi: 10.1016/j.bmc.2005.07.012. [DOI] [PubMed] [Google Scholar]
- Kolodziej H., Kayser O., Radtke O.A., Kiderlen A.F., Koch E. Pharmacological profile of extracts of Pelargonium sidoides and their constituents. Phytomedicine. 2003;10:18–24. doi: 10.1078/1433-187x-00307. [DOI] [PubMed] [Google Scholar]
- Kolodziej H., Kiderlen A.F. In vitro evaluation of antibacterial and immnomodulatory activities of Pelargonium reinforme, Pelargonium sidoides and the related herbal drug preparation EPs® 7630. Phytomedicine. 2007;14:18–26. doi: 10.1016/j.phymed.2006.11.020. [DOI] [PubMed] [Google Scholar]
- Kotzé, D., 2011. Production and pharmacological analysis of microcultures of Pelargonium sidoides DC. and Pelargonium reniforme Curtis (MSc thesis). University of Stellenbosch.
- Latté K.P., Kayser O., Tan N., Kaloga M., Kolodziej H. Unusual coumarin patterns of Pelargonium species forming the origin of the traditional herbal medicine Umckaloabo. Z. Naturforsch. 2000;55c:528–533. [Google Scholar]
- Lewu F.B., Adebola P.O., Afolayan A.J. Commercial harvesting of Pelargonium sidoides in the Eastern Cape, South Africa: striking a balance between resources conservation and livelihoods. J. Arid Environ. 2007;70:380–388. [Google Scholar]
- Lewu F.B., Grierson D.S., Afolayan A.J. The leaves of Pelargonium sidoides may substitute for its roots in the treatment of bacterial infections. Biol. Conserv. 2006;128:582–584. [Google Scholar]
- Li J.W.-H., Vederas J.C. Drug discovery and natural products: End of an era or an endless frontier? Science. 2009;325:161–165. doi: 10.1126/science.1168243. [DOI] [PubMed] [Google Scholar]
- Li L., Yu C.-H., Ying H.-Z., Yu J.-M. Antiviral effects of modified Dingchuan decoction against respiratory syncytial virus infection in vitro and an immunosuppressive mouse model. J. Ethnopharmacol. 2013;147:238–244. doi: 10.1016/j.jep.2013.03.012. [DOI] [PubMed] [Google Scholar]
- Lizogub V.G., Riley D.S., Heger M. Efficacy of a Pelargonium sidoides preparation in patients with common cold: a randomised, double-blind, placebo-controlled clinical trial. Explore. 2007;3:573–584. doi: 10.1016/j.explore.2007.09.004. [DOI] [PubMed] [Google Scholar]
- Lubbe A., Verpoorte R. Cultivation of medicinal and aromatic plants for speciality industrial materials. Ind. Crops Prod. 2011;34:785–801. [Google Scholar]
- Luna L.A., Jr., Bachib A.L.L., Novaes e Brito R.R., Eid R.G., Suguri V.M., Oliveira P.W., Gregorio L.C., Vaisberg M. Immune responses induced by Pelargonium sidoides extract in serum and nasal mucosa of athletes after exhaustive exercise: modulation of secretory IgA, IL-6 and IL-15. Phytomedicine. 2011;18:303–308. doi: 10.1016/j.phymed.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Mativandlela S.P.N., Meyer J.J.M., Hussein A.A., Lall N. Antitubercular activity of compounds isolated from Pelargonium sidoides. Pharm. Biol. 2007;45:645–650. [Google Scholar]
- Matthys H., Heger M. Treatment of acute bronchitis with a liquid herbal drug preparation from Pelargonium sidoides (EPs® 7630): a randomised, double-blind, placebo-controlled, multicentre study. Curr. Med. Res. Opin. 2007;23:323–331. doi: 10.1185/030079906X167318. [DOI] [PubMed] [Google Scholar]
- Matthys H., Eisebitt R., Seith B., Heger M. Efficacy and safety of an extract of Pelargonium sidoides (EPs® 7630) in adults with acute bronchitis. Phytomedicine. 2003;10:7–17. doi: 10.1078/1433-187x-00308. [DOI] [PubMed] [Google Scholar]
- Matthys H., Funk P. EPS® 7630 improves acute bronchitic symptoms and shortens time to remission: Results of a randomised, double-blind, placebo-controlled, multicentre trial. Planta Med. 2008;74:686–692. doi: 10.1055/s-2008-1074519. [DOI] [PubMed] [Google Scholar]
- Matthys H., Heger M. EPs® 7630-solution – an effective therapeutic option in acute and exacerbating bronchitis. Phytomedicine. 2007;14:65–68. doi: 10.1016/j.phymed.2006.11.017. [DOI] [PubMed] [Google Scholar]
- Matthys H., Kamin W., Funk P., Heger M. Pelargonium sidoides preparation (EPs® 7630) in the treatment of acute bronchitis in adults and children. Phytomedicine. 2007;14:69–73. doi: 10.1016/j.phymed.2006.11.015. [DOI] [PubMed] [Google Scholar]
- Matthys H., Pliskevich D.A., Bondarchuk O.M., Malek F.A., Tribanek M., Kieser M. Randomised, double-blind, placebo-controlled trial of EPs® 7630 in adults with COPD. Resp. Med. 2013;107:691–701. doi: 10.1016/j.rmed.2013.02.011. [DOI] [PubMed] [Google Scholar]
- McGaw L.J., Lall N., Meyer J.J.M., Eloff J.N. The potential of South African plants against Mycobacterium infections. J. Ethnopharmacol. 2008;119:482–500. doi: 10.1016/j.jep.2008.08.022. [DOI] [PubMed] [Google Scholar]
- Michaelis M., Doerr H.W., Cinatl J., Jr. Investigation of the influence of EPs® 7630, a herbal drug preparation from Pelargonium sidoides, on replication of a broad panel of respiratory viruses. Phytomedicine. 2011;18:384–386. doi: 10.1016/j.phymed.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motsamai, G.I., 2012. The Efficacy of Linctagon® Forte Capsules on the Symptoms of Colds and Influenza in Female Resident Students at the University of Johannesburg (MTech dissertation). University of Johannesburg.
- Moyo M., Aremu A.O., Gruz J., Šubrtová M., Szüčová L., Dolezal K., Van Staden J. Vol. 149. 2013. Conservation strategy for Pelargonium sidoides DC.: phenolic profile and pharmacological activity of acclimatized plants derived from tissue culture; pp. 557–561. (J. Ethnopharmacol.). [DOI] [PubMed] [Google Scholar]
- Moyo M., Finnie J.F., Van Staden J. Topolins in Pelargonium sidoides micropropagation: do the new brooms sweep cleaner? Plant Cell Tissue Organ Culture. 2012;110:319–327. [Google Scholar]
- Moyo, M., Koetle, M.J., Van Staden, J., Photoperiod and plant growth regulator combinations influence growth and physiological responses in Pelargonium sidoides DC. In Vitro Cell. Dev. Biol.-Plant, 10.1007/s11627-014-9594-4, in press [DOI]
- Nathan C.F., Hibbs J. Role of nitric oxide synthesis in macrophage antimicrobial activity. Curr. Opin. Immunol. 1991;3:65–70. doi: 10.1016/0952-7915(91)90079-g. [DOI] [PubMed] [Google Scholar]
- Newton, D., Raimondo, D., Motjotji, L., Lippai, C., 2013. Biodiversity management plan for Pelargonium sidoides DC. Notice 433 of 2013. Department of Environmental Affairs. Republic of South Africa.
- Nöldner M., Schötz K. Inhibition of lipopolysaccharide-induced sickness behavior by a dry extract from the roots of Pelargonium sidoides (EPs® 7630) in mice. Phytomedicine. 2007;14:27–31. doi: 10.1016/j.phymed.2006.11.013. [DOI] [PubMed] [Google Scholar]
- Patiroglu T., Tunc A., Gungor H.E., Unal E. The efficacy of Pelargonium sidoides in the treatment of upper respiratory tract infections in children with transient hypogammaglobulinemia of infancy. Phytomedicine. 2012;19:958–961. doi: 10.1016/j.phymed.2012.06.004. [DOI] [PubMed] [Google Scholar]
- Radtke O.A., Kiderlen A.F., Kayser O., Kolodziej H. Gene expression profiles of inducible nitric oxide synthase and cytokines in Leishmania major-infected macrophage-like RAW 264.7 cells treated with gallic acid. Planta Med. 2004;70:924–928. doi: 10.1055/s-2004-832618. [DOI] [PubMed] [Google Scholar]
- Red Data List of South African plants version 2013.1. 〈http://redlist.sanbi.org/〉, 2013 (accessed 09.12.13)
- Red Data List of South African plants. 〈http://redlist.sanbi.org/〉, 2009 (accessed 29.03.11).
- Reiner T.I., Locksley R.M. The regulation of immunity to Leishmania major. Ann. Rev. Immunol. 1995;13:151–177. doi: 10.1146/annurev.iy.13.040195.001055. [DOI] [PubMed] [Google Scholar]
- Schmidt B.M., Ribnicky D.M., Lipsky P.E., Raskin I. Revisiting the ancient concept of botanical therapeutics. Nat. Chem. Biol. 2007;3:360–366. doi: 10.1038/nchembio0707-360. [DOI] [PubMed] [Google Scholar]
- Schnitzler P., Schneider S., Stintzing F.C., Carle R., Reichling J. Efficacy of an aqueous Pelargonium sidoides extract against herpes virus. Phytomedicine. 2008;15:1108–1116. doi: 10.1016/j.phymed.2008.06.009. [DOI] [PubMed] [Google Scholar]
- Schoetz K., Erdelmeier C., Germer S., Hauer H. A detailed view on the constituents of EPs® 7630. Planta Med. 2008;74:667–674. doi: 10.1055/s-2008-1074515. [DOI] [PubMed] [Google Scholar]
- Schötz K., Nöldner M. Mass spectroscopic characterisation of oligomeric proanthocyanidins derived from an extract of Pelargonium sidoides roots (EPs® 7630) and pharmacological screening in CNS models. Phytomedicine. 2007;14:32–39. doi: 10.1016/j.phymed.2006.11.019. [DOI] [PubMed] [Google Scholar]
- Seidel V., Taylor P.W. In vitro activity of extracts and constituents of Pelagonium against rapidly growing mycobacteria. Int. J. Antimicrob. Agents. 2004;23:613–619. doi: 10.1016/j.ijantimicag.2003.11.008. [DOI] [PubMed] [Google Scholar]
- Tahan F., Yaman M. Can the Pelargonium sidoides root extract EPs® 7630 prevent asthma attacks during viral infections of the upper respiratory tract in children? Phytomedicine. 2013;20:148–150. doi: 10.1016/j.phymed.2012.09.022. [DOI] [PubMed] [Google Scholar]
- Taylor P.W. Antimycobacterial activity of indigenous South African plants. South Afr. Med. J. 2003;93:904–907. [PubMed] [Google Scholar]
- Teschke R., Frenzel C., Schulze J., Eickhoff A. Spontaneous reports of primarily suspected herbal hepatotoxicity by Pelargonium sidoides: was causality adequately ascertained? Regul. Toxicol. Pharmacol. 2012;63:1–9. doi: 10.1016/j.yrtph.2012.02.009. [DOI] [PubMed] [Google Scholar]
- Thäle C., Kiderlen A., Kolodziej H. Anti-infective mode of action of EPS® 7630 at the molecular level. Planta Med. 2008;74:675–681. doi: 10.1055/s-2008-1034324. [DOI] [PubMed] [Google Scholar]
- Thäle C., Kiderlen A.F., Kolodziej H. Anti-infective activities of Pelargonium sidoides (EPs® 7630): effects of induced NO production on Leishmania major in infected macrophages and antiviral effects as assessed in a fibroblast-virus protection assay. Planta Med. 2011;77:718–725. doi: 10.1055/s-0030-1250567. [DOI] [PubMed] [Google Scholar]
- Theisen L.L., Muller C.P. EPs® 7630 (Umckaloabo®), an extract from Pelargonium sidoides roots, exerts anti-influenza virus activity in vitro and in vivo. Antiviral Res. 2012;94:147–156. doi: 10.1016/j.antiviral.2012.03.006. [DOI] [PubMed] [Google Scholar]
- Tian L., Wang Z., Wu H., Wang S., Wang Y., Wang Y., Xu J., Wang L., Qi F., Fang M., Yu D., Fang X. Evaluation of the anti-neuraminidase activity of the traditional Chinese medicines and determination of the anti-influenza A virus effects of the neuraminidase inhibitory TCMs in vitro and in vivo. J. Ethnopharmacol. 2011;137:534–542. doi: 10.1016/j.jep.2011.06.002. [DOI] [PubMed] [Google Scholar]
- Trun W., Kiderlen A.F., Kolodziej H. Nitric oxide synthase and cytokines gene expression analyses in Leishmania-infected RAW 264.7 cells treated with an extract of Pelargonium sidoides (EPs® 7630) Phytomedicine. 2006;13:570–575. doi: 10.1016/j.phymed.2005.07.004. [DOI] [PubMed] [Google Scholar]
- Uslu H., Yoruk O., Ayyıldız A., Aktan B. Antibacterial spectrum of Umckaloabo (Pelargonium sidoides) on upper airway infection agents. Eur. J. Gen. Med. 2009;6:245–248. [Google Scholar]
- Van Niekerk J., Wynberg R. The trade in Pelargonium sidoides: rural livelihood relief or bounty for the ‘bio-bauccaneers’? Dev. South. Afr. 2012;29:530–547. [Google Scholar]
- Verschaeve L., Van Staden J. Mutagenic and antimutagenic properties of extracts from South African traditional medicinal plants. J. Ethnopharmacol. 2008;119:575–587. doi: 10.1016/j.jep.2008.06.007. [DOI] [PubMed] [Google Scholar]
- Wagner H. Synergy research: approaching a new generation of phytopharmaceuticals. Fitoterapia. 2011;82:34–37. doi: 10.1016/j.fitote.2010.11.016. [DOI] [PubMed] [Google Scholar]
- Wagner H., Ulrich-Merzenich G. Synergy research: approaching a new generation of phytopharmaceuticals. Phytomedicine. 2009;16:97–110. doi: 10.1016/j.phymed.2008.12.018. [DOI] [PubMed] [Google Scholar]
- White A.G., Davies-Coleman M.T., Ripley B.S. Measuring and optimising umckalin concentration in wild-harvested and cultivated Pelargonium sidoides (Geraniaceae) South Afr. J. Bot. 2008;74:260–267. [Google Scholar]
- Wittschier N., Faller G., Hensel A. An extract of Pelargonium sidoides (EPs 7630) inhibits in situ adhesion of Helicobacter pylori to human stomach. Phytomedicine. 2007;14:285–288. doi: 10.1016/j.phymed.2006.12.008. [DOI] [PubMed] [Google Scholar]
- Wynberg, R., van Niekerk, J., Kozanayi, W., Laird, S., 2012. Formalisation and the non-timber forest product sector: experiences from southern Africa. Report. Centre for International Forestry Research, Bogor, Indonesia, pp. 1–64.
- Yu C., Yan Y., Wu X., Zhang B., Wang W., Wu Q. Anti-influenza virus effects of the aqueous extract from Mosla scabra. J. Ethnopharmacol. 2010;127:280–285. doi: 10.1016/j.jep.2009.11.008. [DOI] [PubMed] [Google Scholar]




