Abstract
It is self-evident that infection and inflammation in the reproductive tract can inhibit male fertility, but the observation that fertility may also be compromised by systemic inflammation and disease is more difficult to explain. Recent studies implicating microbial pattern-recognition receptors, such as the Toll-like receptors (TLRs), as well as inflammatory cytokines and their signalling pathways, in testicular function have cast new light on this mysterious link between infection/inflammation and testicular dysfunction. It is increasingly evident that signalling pathways normally involved in controlling inflammation play fundamental roles in regulating Sertoli cell activity and responses to reproductive hormones, in addition to promoting immune responses within the testis. Many of the negative effects of inflammation on spermatogenesis may be attributed to elevated production of inflammation-related gene products within the circulation and the testis, which subsequently exert disruptive effects on spermatogenic cell development and survival, as well as the ability of the Sertoli cells to provide support for spermatogenesis. These interactions have important implications for testicular dysfunction and disease, and may eventually provide new opportunities for therapeutic interventions.
Keywords: Toll-like receptor, Lipopolysaccharide, Inflammation, Sertoli cell, Spermatogenesis, Infertility
1. Background
Infection and inflammation within the male reproductive tract have detrimental effects on reproduction, which usually manifest as reduced androgen production, lowered sperm counts and temporary loss of fertility, as well as discomfort and pain (Carlsen et al., 2003, Nariculam et al., 2007). It is not difficult to understand these negative consequences, since the inflammatory process is fundamentally destructive in nature. Infection and inflammation induce generation of highly toxic reactive oxygen species (ROS) and other cytotoxins, and production of cytokines, bioactive lipids and enzymes with profound effects on cellular and vascular function, eventually leading to the activation of immune cells with various damaging activities. The principal outcomes of a local inflammatory response are widespread apoptosis, vascular disruption, tissue remodelling and fibrosis, all of which are harmful for the tissues involved. However, it is increasingly evident that male reproductive function also can be compromised by systemic inflammation and disease, including many inflammatory conditions that do not involve infection or overt damage to the reproductive tissues (Baker, 1998, Dong et al., 1992). This observation represents one of the basic conundrums of male reproductive biology, and the underlying mechanisms involved are poorly understood.
In order to investigate the mechanisms whereby inflammation inhibits male reproduction, a rat model of systemic inflammation induced by lipopolysaccharide (LPS) was established in our laboratory over 10 years ago (O’Bryan et al., 2000b). A component of the cell wall of gram-negative bacteria, LPS is a well-characterised activator of the inflammatory response without the complication of infectious particles. Although LPS had been widely used to study inflammation in other systems, at the time there were only a small number of papers on the specific effects of LPS on male reproduction in several different species, and these studies provided only limited, and sometimes inconsistent, pieces of the puzzle.
2. The effects of systemic LPS administration on testicular function in the rat
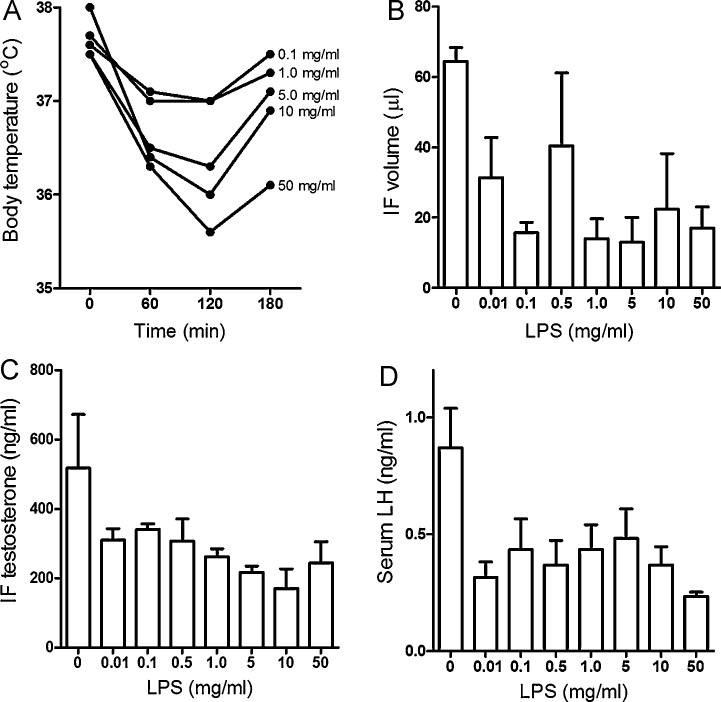
At the time these studies commenced, the activity of LPS preparations even from a single bacterial species and serotype was known to be quite variable and contained critical impurities, most notably bacterial lipopeptides, which could produce inconsistent results (Hirschfeld et al., 2000). Initial studies were undertaken whereby adult male rats were injected (i.p.) with a standardised stock of LPS from Escherichia coli (serotype 0127:B8) to establish the optimal range of dose and response (Fig. 1 ). These studies were also necessary to identify and eliminate doses of LPS that were liable to cause death through endotoxic shock (Galanos and Freudenberg, 1993).
Fig. 1.
LPS dose–response data in adult male rats. Adult male rats were injected with varying doses of LPS (E. coli, serotype 0128:B8). Body temperature (A) was measured every hour for 3 h, at which time the rats were killed and blood and testes taken for analysis of testicular function. Testis weights were unaffected, but even at relatively low does of LPS, testicular interstitial fluid (IF) formation (B), intratesticular steroidogenesis (IF testosterone) (C) and pituitary secretion of luteinising hormone (LH) (D) was inhibited. All values are mean and SEM (n = 3–6 animals), except in panel A, where the error bars and some dose data have been removed for clarity (data previously unpublished). Note that subsequent experiments established that doses above 5 mg/kg frequently caused death through endotoxic shock within 12–24 h after administration.
It was established that administration of LPS across a very broad range of doses inhibited the formation of testicular interstitial fluid and suppressed intratesticular and circulating levels of testosterone (Gow et al., 2001, Liew et al., 2007, O’Bryan et al., 2000b). This suppression of steroidogenesis was due to inhibition of both luteinising hormone (LH) secretion by the anterior pituitary and a reduced capacity of the Leydig cells in the interstitial tissue to produce testosterone. There have been many studies on the effects of inflammation and inflammatory mediators on the hypothalamic–pituitary–Leydig cell axis, and the interested reader is directed towards previous reviews on this topic (Hales, 2002, Hedger and Hales, 2006). Briefly, loss of steroidogenesis during inflammation is due to inhibitory actions of LPS and inflammatory mediators induced by LPS action, such as the pro-inflammatory cytokines interleukin 1β (IL1β) and tumour necrosis factor α (TNFα), ROS, nitric oxide and prostaglandins, on hypothalamic LH-releasing hormone secretion, production of LH in the pituitary, and Leydig cell cholesterol mobilisation and steroidogenic enzyme activity. Inflammation-activated neural pathways and corticosteroids, which are induced in response to inflammation, exert inhibitory effects on Leydig cell steroidogenic function as well (Gow et al., 2001, Monder et al., 1994, Ogilvie et al., 1999).
Spermatogenesis is a complex, organized and highly regulated process involving intimate, cyclical interactions between the developing spermatogenic cells and supporting Sertoli cells, and is dependent upon hormonal support of the Sertoli cells by both follicle-stimulating hormone (FSH) from the anterior pituitary and testosterone (McLachlan et al., 1996). A crucial observation was that lower doses of LPS, which caused maximal inhibition of steroidogenesis, had minimal effects on spermatogenesis, at least in the short term, but LPS administered as a single sub-lethal dose also caused significant spermatogenic disruption for a period of several weeks (Liew et al., 2007, O’Bryan et al., 2000a). A transient increase in circulating macrophages within the interstitial tissue and intravascular neutrophils followed treatment with either low or high doses of LPS, but no substantial leukocytic infiltration of either testicular compartment was observed (Gerdprasert et al., 2002a, Gerdprasert et al., 2002b). Detailed stereological analysis of the response to the high dose of LPS over a period of 4 weeks showed that the effects on spermatogenesis were quite specific (Liew et al., 2007). At 24 h after treatment, there was a significant delay of spermatocyte development at the leptotene/zygotene phase of meiosis (i.e. stages XI–XIII of the cycle of the seminiferous epithelium in the rat), followed within 6 days by premature release of these cells and the adjacent, but more luminally located, generation of round spermatids. There was also an increase in apoptosis of spermatocytes and spermatids at stages IX–XIII within the same time-frame (Liew et al., 2007). This led to the question: why were the spermatogenic cells at stages IX–XIII so specifically affected?
Notably, these rats did not develop a fever. In fact, body temperature actually fell in rats given high doses of LPS (Fig. 1), indicating that elevated testicular temperature, a mechanism that is commonly invoked by clinicians to explain fertility decline in men with infections, was not responsible for the damage to spermatogenesis observed. Moreover, although intratesticular testosterone was dramatically reduced there are several reasons why androgen deficiency could not account for the damage either. Firstly, lower doses of LPS resulted in a similar degree of inhibition of intratesticular testosterone levels to that caused by high dose LPS, without causing evident spermatogenic damage (O’Bryan et al., 2000b). Second, even at the high dose of LPS, the levels of intratesticular testosterone were only reduced by about 70%, whereas normal spermatogenesis can continue in the presence of intratesticular levels that are as low as 20% of normal in the rat (Sharpe et al., 1988). Third, the pattern of damage was not consistent with androgen deficiency, which specifically leads to loss of elongating and late spermatids at stages VII–VIII (O’Donnell et al., 1996). Nor was the pattern of spermatogenic damage caused by high doses of LPS consistent with vascular interruption, which leads to oxidative stress due to reperfusion injury and results in rapid apoptosis of spermatogonia and early spermatocytes followed by progressive depopulation of the seminiferous epithelium (Turner et al., 2004, Turner et al., 1997).
However, it should be noted that the two studies undertaken in our laboratory to address the effects of high dose LPS on spermatogenesis produced some significant differences in the pattern of early damage. In the initial study, there was substantial disruption of the testicular vasculature and this was accompanied by a more rapid and pronounced epithelial damage, including focal spermatogonial/spermatocyte apoptosis, within 3 days after LPS administration (O’Bryan et al., 2000b). This was also associated with a significantly higher mortality rate. These early damage events were not observed in the subsequent, more detailed, study, even though the doses of LPS employed were ostensibly the same (Liew et al., 2007). Significantly, studies by Reddy, Reddanna and colleagues using a similar high dose LPS treatment model in rats have demonstrated an association between these earlier, more severe, damage events and testicular oxidative stress responses (Metukuri et al., 2010, Reddy et al., 2006). These responses included induction of the stress proteins, heat shock protein 60 (HSP-60), high mobility group box chromosomal proteins 1 and 2 (HMGB1 and HMGB2), as well as increased lipid peroxidation, reduced antioxidant activities, mitochondrial dysfunction and spermatogenic cell apoptosis.
When considered together, these observations indicated that the effects of LPS-induced inflammation on spermatogenesis involve several mechanisms, as dictated by the severity of the resulting inflammatory response. Obviously, inhibition of Leydig cell function, vascular disturbance and oxidative stress can all contribute to spermatogenic damage during inflammation, but there is another mechanism that also should be considered, one that preferentially affects spermatogenic cells at stages XI–XIII. If all other mechanisms can be put to one side, the possibility that the seminiferous epithelium responds to inflammatory stimuli directly must be considered. This would not necessarily have to involve LPS itself acting directly on the epithelium, as there are large numbers of macrophages within the interstitial tissue that respond to LPS stimulation by producing various inflammatory mediators (Hales, 2002). Moreover, inflammatory mediators and inflammatory cells from the circulation can also enter the testis during systemic inflammation, infection or other disease states.
One also needs to consider why even relatively low doses of LPS inhibited the hypothalamic–pituitary–Leydig cell axis and interstitial fluid formation (Fig. 1), but very high doses of LPS were required to exert significant effects on spermatogenesis using the rat model. This differential sensitivity might have been due to actual differences in sensitivity to LPS at the cellular level, or the probability that circulating LPS may have variable access to the various compartments of the testis. Accordingly, direct effects on the pituitary, vasculature, and even the testicular macrophages and Leydig cells could occur at lower doses, but much higher doses could be necessary to allow sufficient LPS to traverse both the vascular and lymphatic endothelium of the interstitial tissue as well as the peritubular basement membrane and peritubular cell layer to directly affect seminiferous epithelial function. Curiously, one of the few studies to employ a model of direct injection of LPS into the mouse seminiferous tubules (via the efferent ducts) seemed to imply that this treatment caused minimal damage to the seminiferous epithelium (Nagaosa et al., 2009). This implication was not supported by the histology, which clearly showed extensive spermatogenic disruption, although not as extensive as the damage caused by injection of live E. coli. One should be very careful not to equate the damage to the seminiferous epithelium caused by LPS treatment alone with the very extensive and prolonged testicular damage that that occurs when live E. coli are introduced into the seminiferous tubules via retrograde injection (Demir et al., 2007, Lucchetta et al., 1983, Nagaosa et al., 2009).
3. The Toll-like receptors and their expression in the testis
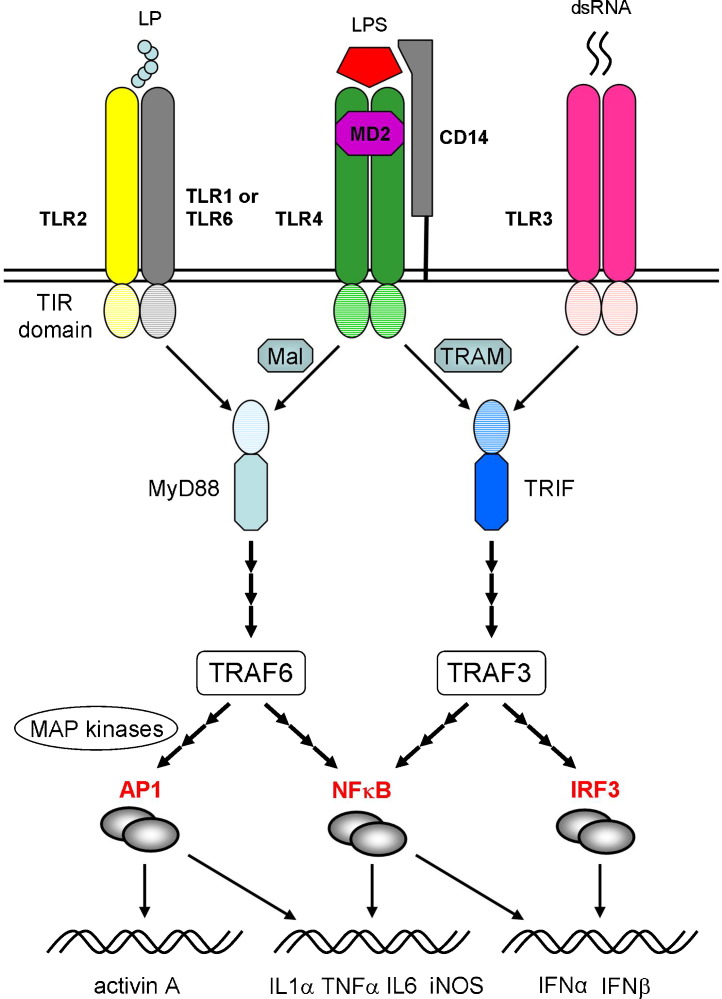
How might LPS or other inflammatory mediators affect the seminiferous epithelium directly? Inflammation is the host response to trauma or infection, and a mechanism to rapidly activate the innate arm of the immune system, while setting in train the necessary processes that will recruit the adaptive immune response. A major activator arm of inflammation and innate immunity involves recognition by specific pattern-recognition receptors of specific motifs, or pathogen-associated molecular patterns (PAMPs), found on bacterial, viral, fungal and protozoan pathogens. The best characterised of the pattern-recognition receptors are the Toll-like receptors (TLRs), which recognise bacterial and viral nucleic acids and other molecules unique to various pathogens, such as bacterial lipopeptides, peptidoglycans and LPS (O’Neill and Bowie, 2007, Roach et al., 2005). The TLRs are members of a larger family of transmembrane (cell-surface or endosomal) proteins that includes the interleukin 1 receptor (IL1R), and which share a conserved cytoplasmic domain called the Toll/IL1R (TIR) domain (Fig. 2 ).
Fig. 2.
Toll-like receptors (TLRs) and signalling pathway interactions. The TLRs respond to a variety of pathogen-related molecules, usually forming homo- or heterodimers during signalling. TLR2 can self-associate or combine with either TLR1 or TLR6 to mediate responses to various bacterial lipoprotein (LP) classes. TLR4 forms a complex with the co-receptor proteins, MD2 and CD14, to facilitate binding of bacterial LPS. The TLRs are sub-divided into cell surface receptors (e.g. TLR2 and 4), which largely respond to bacterial proteins, lipoproteins and lipopolysaccharides, and intracytoplasmic endosomal receptors (e.g. TLR3), which recognise bacterial and viral nucleic acids, such as viral double-stranded RNA (dsRNA). Most TLRs signal via the adaptor protein, MyD88 (myeloid differentiation primary response protein 88), except TLR3, which acts through the adaptor protein TRIF (TIR domain-containing adaptor-inducing interferon β). Uniquely, TLR4 can interact with either MyD88 or TRIF, through engagement of the adaptor proteins, Mal (MyD88 adaptor-like) or TRAM (TRIF-related adaptor molecule). Downstream signalling involves the tumour necrosis factor receptor-associated factors 3 and 6 (TRAF3 and TRAF6), activation of the transcription factors, NFκB (nuclear factor kappaB) and IRF3 (interferon regulatory factor 3), or induction of the mitogen-activated protein kinases (MAP kinases) Jnk (Jun N-terminal kinase) and p38 and production of the Fos/Jun transcription factor AP1 (activated protein 1). These transcription factors interact to induce the expression of multiple pro-inflammatory genes, including interleukin (IL) 1α, tumour necrosis factor α (TNFα), inducible nitric oxide (iNOS), or the type 1 interferons (IFNα, IFNβ). Note that many details of the signalling pathways have been omitted or truncated for the sake of simplicity.
In humans, ten functional TLRs (TLR1–10) have been identified, and a further 3 mammalian TLRs (TLR11–13) have been found in laboratory rodent species (Roach et al., 2005). They are particularly associated with cells of the monocyte lineage (i.e. macrophages and dendritic cells), but are also expressed by fibroblastic and epithelial cells, including those found within the male reproductive tract (Lauw et al., 2005, Zhang et al., 2004). Signalling from TLR activation relies upon interaction between the TIR domain of the receptor and various adaptor proteins. In the case of most TLRs, the adapter protein involved is MyD88 (myeloid differentiation primary-response protein 88), but TLR3 and TLR4 engage the adapter protein TRIF (TIR domain-containing adaptor protein inducing interferon β) (Fig. 2). Interaction between the TLR and its adapter protein activates tumour necrosis factor (TNF) receptor-associated factor 3 and/or 6 (TRAF3, TRAF6), leading to activation and nuclear translocation of the inflammatory transcription factors, nuclear factor kappa B (NFκB) and activated protein 1 (AP1), activation of the Jnk (Jun N-terminal kinase) and p38 mitogen-activated protein (MAP) kinases, and induction of various critical inflammatory genes (O’Neill and Bowie, 2007, Takeuchi and Akira, 2010) or activation of the interferon regulatory factors (IRFs) and induction of type 1 interferons (IFNα and IFNβ) (Hertzog et al., 2003, O’Neill and Bowie, 2007). The TLR responsible for detecting bacterial LPS is TLR4, which is actually a protein complex that includes the co-receptor proteins myeloid differentiation (MD) 2, essential for LPS recognition and signalling, and CD14, which enhances LPS responsiveness by facilitating the transfer of LPS to the TLR4/MD2 complex (Fig. 2) (Jiang et al., 2005, O’Neill and Bowie, 2007). Uniquely among the TLRs, TLR4 signalling can occur through either MyD88 or TRIF, depending upon the engagement of the adapter proteins, TIRAP/MAL (TIR-containing adapter or MyD88-adapter-like protein) and TRAM (TRIF-related adapter molecule), respectively. Consequently, the LPS/TLR4 interaction is an ideal model for investigating the effects of TLR signalling in various cell systems, and has been widely studied.
Other major pattern-recognition receptors include the nucleotide binding and oligomerisation domain (Nod)-like receptor (NLR) family and the retinoic acid-inducible gene (RIG)-like receptor (RLR) family (Takeuchi and Akira, 2010). Nod-like receptors detect bacterial PAMPs within the cytosol. Some of these receptors, such as Nod1 and Nod2, act via NFκB and MAP kinase activation, while other NLRs work through induction of the cysteine protease caspase 1, which activates the pro-inflammatory cytokines IL1β and IL18 and initiates caspase-mediated pro-apoptotic pathways within the target cell. The RLRs, which detect the presence of viral RNA in the cytosol, activate both NFκB and production of type 1 interferons. However, the pattern-recognition receptor family continues to expand, and now includes the C-type lectin receptors (CLR), which recognise fungi (Takeuchi and Akira, 2010).
In addition to their predictable expression on testicular macrophages and dendritic cells, TLR mRNA, protein and/or ligand responses have been described in several testicular cell types (Table 1 ). Accordingly, the Sertoli cells of rats and mice express TLR2, 3, 4 and 5 (Bhushan et al., 2008, Riccioli et al., 2006, Starace et al., 2008, Winnall et al., 2011, Wu et al., 2008). In the rat, expression of the essential TLR4 co-receptor proteins MD2 and CD14 have been confirmed as well (Winnall et al., 2011). In addition, TLR1, 10 and 11 mRNA expression has been observed in rat Sertoli cells (Bhushan et al., 2008), and low levels of TLR6 and 7 and 13 mRNA have been detected in mouse Sertoli cells (Riccioli et al., 2006, Wu et al., 2008). To date, responses to TLR1-6 ligands have also been confirmed using either rat or mouse Sertoli cells (Bhushan et al., 2008, Riccioli et al., 2006, Starace et al., 2008, Sun et al., 2010, Winnall et al., 2011, Wu et al., 2008). In the rat, spermatogenic cells express mRNA for TLR2, 3 and 4 in a stage specific manner, peritubular cells express TLR3 and 11, along with low levels of TLR2, 4 and 6, and Leydig cells express TLR2 mRNA and low levels of TLR4, MD2, CD14 and TLR10 (Bhushan et al., 2008, Winnall et al., 2011). Data indicate that Leydig cells, as well as peritubular cells, can respond to LPS preparations (Aubry et al., 2000, Cudicini et al., 1997, Wang et al., 1991), although direct effects of the relevant TLR ligands on spermatogenic cells have yet to be established. The intracytoplasmic receptors, TLR8 and TLR9, have not been observed in any non-myeloid testicular cell type. Of the other pattern-recognition receptors, Nod1 mRNA has been detected in rat Sertoli cells, peritubular cells and spermatogonia, while Nod2 was detected in spermatogonia only (Bhushan et al., 2008).
Table 1.
Toll-like receptor expression in rat and mouse Sertoli cells.
| Receptor | Principal ligands | Rat | Mouse | Ligand response |
|---|---|---|---|---|
| TLR1 | Triacyl lipopeptides | Yes | No | Confirmed |
| TLR2 | Lipoproteins | Yes | Yes | Confirmed |
| TLR3 | dsRNA | Yes | Yes | Confirmed |
| TLR4 | Lipopolysaccharides | Yes | Yes | Confirmed |
| TLR5 | Flagellin | Yes | Yes | Confirmed |
| TLR6 | Diacyl lipopeptides | No | Yes | Confirmed |
| TLR7 | ssRNA | No | Weak | ND |
| TLR8a | ssRNA | No | No | ND |
| TLR9 | CpG DNA | No | No | ND |
| TLR10b | Unknown | Weak | No | ND |
| TLR11 | Profilin | Yes | No | ND |
| TLR12 | Unknown | ND | No | ND |
| TLR13 | Unknown | ND | Weak | ND |
TLR not active in rodents.
TLR not expressed in the mouse. ND: no data.
Data derived from: Bhushan et al. (2008), Riccioli et al. (2006), Starace et al. (2008), Sun et al. (2010), Winnall et al. (2011), and Wu et al. (2008).
4. The response of Sertoli cells to TLR ligands and inflammatory mediators
Expression of pattern recognition receptors by the Sertoli cell, in particular, suggests a mechanism whereby inflammation can directly regulate spermatogenesis. Predictably, exposure of the Sertoli cell in vitro to LPS has been shown to directly inhibit lactate production and plasminogen activator activity, which are important for supporting spermatogenic cell development, and induces oxidative stress in these cell by increasing ROS production and reducing anti-oxidant activity (Aly et al., 2010, Bourdon et al., 1999). However, the story is actually more complicated. Numerous studies have established that LPS stimulates Sertoli cells to produce a select panel of inflammatory gene products, including IL1α (the cell-associated variant of IL1β), IL6 and inducible nitric oxide synthase (iNOS), as well as immunoregulatory cytokines, such as activin A (Gérard et al., 1992, Okuma et al., 2005a, Riccioli et al., 2006, Stéphan et al., 1995, Syed et al., 1995, Winnall et al., 2009, Wu et al., 2008). The contributions of these inflammatory mediators must also be considered in any model of intratesticular inflammation.
Although the obvious conclusion would be that these responses to LPS are mediated via the TLR4 complex expressed by the Sertoli cell, most (if not all) studies have employed crude LPS preparations, which are generally contaminated by other bacterial products (Hirschfeld et al., 2000, Takeuchi et al., 1999). Crucially, bacterial lipopeptides act specifically via TLR2 and bacterial peptidoglycans interact with other pattern-recognition receptor family members (Travassos et al., 2004, Zähringer et al., 2008). Careful examination of rat Sertoli cells showed that the level of expression of TLR4 and its co-receptor MD2 was similar in Sertoli cells and testicular macrophages, but that Sertoli cells displayed low basal or LPS-induced expression of the TLR4 accessory protein, CD14 and of TLR2 (Winnall et al., 2011). However, the response of these cells to crude LPS produced much stronger responses in terms of magnitude and duration compared with their response to highly purified LPS, which acts exclusively through TLR4. Moreover, the Sertoli cells responded to the synthetic lipopeptide, Pam3Cys (a specific TLR2 ligand), with a similar pattern of prolonged gene expression. In fact, Sertoli cells were more than 10-fold less sensitive to highly purified LPS than testicular macrophages, but expressed similar levels of IL1α and IL6, and much greater levels of activin A, when maximally stimulated. These data demonstrated that Sertoli cells respond to bacterial ligands acting through both TLR2 and TLR4, although they are less sensitive to these ligands in comparison with local macrophages, and display a Sertoli cell-specific pattern of gene expression in response. The data are also consistent with the need for relatively high doses of LPS to affect spermatogenesis in vivo, as mentioned previously. One further point to be made is that this review focuses upon the role of bacterial ligands and inflammation, but Sertoli cells also express pattern-recognition receptors that mediate responses to other pathogens, particularly viruses (Bhushan et al., 2008, Riccioli et al., 2006, Starace et al., 2008). Accordingly, viral ligands have effects on Sertoli cell function that are analogous, although not identical, to those observed following exposure to LPS.
In addition to pathogenic ligands, Sertoli cells respond to several inflammatory mediators, most notably IL1α and IL1β, TNFα, NO, TGFβ3 and IFNγ (Bauché et al., 1998, Lee and Cheng, 2003, Lui et al., 2003, Mauduit et al., 1993, Nehar et al., 1997, Okuda et al., 1995, Okuma et al., 2005b, Saito et al., 2011, Stéphan et al., 1995). The Sertoli cell itself is a potential source of several of these inflammatory mediators: for example, IL1α produced by the Sertoli cell in vitro stimulates IL6 production through an autocrine mechanism (Syed et al., 1995). Of course, cells of the monocyte/macrophage lineage, and particularly macrophages, within the adjacent testicular interstitial tissue would also provide an additional source of inflammatory mediators. Testicular macrophages have the capacity for inflammatory activity, although they express much lower levels of pro-inflammatory gene products when stimulated than do macrophages from other sites (Gerdprasert et al., 2002a, Hayes et al., 1996, Kern et al., 1995, O’Bryan et al., 2005). Equally significant is the fact that spermatogenic cells themselves also express several pro-inflammatory genes, including iNOS and TNFα (De et al., 1993, O’Bryan et al., 2000a), although this expression appears not to be responsive to LPS (Hedger and Winnall, unpublished data).
Another issue that merits consideration is the fact that Sertoli cells derived from sexually immature rats (around 20 days of age), which are most commonly used in studies on Sertoli cell function, may display significant differences from Sertoli cells that have been isolated from mature rats, in terms of their inflammatory responses. It appears that the majority of IL1α produced in response to LPS stimulation by Sertoli cells from immature rats remains within the cell, and is not secreted (Winnall et al., 2009). By contrast, Sertoli cells from adult rats secrete bioactive IL1α into the culture medium in response to LPS across a similar range of LPS doses (Gérard et al., 1992, Okuma et al., 2005a). These data suggest that intracellular and secreted forms of IL1α may play different autocrine roles in Sertoli cell biology at different stages of maturation, and raises the potential for inflammatory mediators to influence established maturation-specific changes in Sertoli cell function, such as the decline of sensitivity to FSH (Fakunding et al., 1976).
5. Inflammatory signalling and the cycle of the seminiferous epithelium
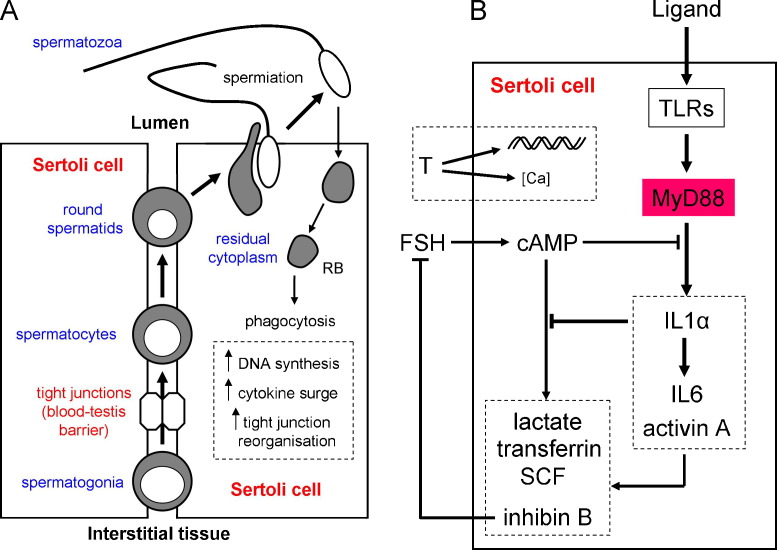
There is increasing evidence that the production by the Sertoli cells and spermatogenic cells of molecules that are otherwise normally associated with inflammation plays an important role in the fine regulation of the seminiferous epithelium (see O’Bryan and Hedger, 2008, for a more detailed review). In order to maintain the organisation of the seminiferous epithelium, spermatogenic and Sertoli cells must engage in continuous communication. Throughout the cycle of the seminiferous epithelium, the production of IL1α, IL6 and activin A by the Sertoli cell is regulated by changes in the developing spermatogenic cells, and production is rapidly and dramatically elevated following the release of the spermatozoa into the lumen of the seminiferous tubule (spermiation) at stage VIII of the cycle (Gérard et al., 1992, Hakovirta et al., 1995, Jonsson et al., 1999, Okuma et al., 2006, Söder et al., 1991, Syed et al., 1995, Wang et al., 1998). This increase in inflammatory cytokine production has been attributed to the effect of the residual cytoplasm and its phagocytosis by the Sertoli cell (Fig. 3A). Moreover, there is a corresponding increase in nuclear NFκB levels and expression of the inflammatory proteins, TNFα and iNOS, in spermatogenic cells at this time (De et al., 1993, Delfino and Walker, 1998, O’Bryan et al., 2000a). This surge of inflammatory cytokines and other mediators in the seminiferous epithelium not only coincides with the release of the spermatozoa, but also with a burst of spermatogonial and spermatocyte DNA synthesis and reorganisation of the tight junctions between adjacent Sertoli cells that constitute the blood–testis barrier, in order to allow the developing spermatocytes to pass into the luminal compartment of the seminiferous epithelium (Cheng and Mruk, 2002, Hakovirta et al., 1993a, Hakovirta et al., 1995, Russell, 1977, Söder et al., 1991). This is not a simple coincidence of events.
Fig. 3.
Communication networks in the Sertoli cell. (A) Spermatogenesis and intraepithelial responses at the time of spermiation. Spermatogonia enter meiosis to become spermatocytes and pass through the tight junctions between adjacent Sertoli cells. At the end of meiosis, the resulting haploid spermatids undergo major structural differentiation and are released from the seminiferous epithelium as spermatozoa (spermiation), leaving behind most of their cytoplasm, which is phagocytosed by the Sertoli cells as a residual body (RB). Release and phagocytosis of the RBs coincides with a surge of DNA synthesis among the nearby spermatogonia and spermatocytes, reorganisation of the tight junctions to allow spermatocytes to pass into the luminal compartment, and increased inflammatory gene expression in the Sertoli cells and spermatogenic cells. (B) Hormonal and inflammatory signalling pathways in control of Sertoli cell function. Sertoli cell function is regulated by androgens, specifically testosterone (T) produced by the nearby Leydig cells and FSH from the anterior pituitary. Testosterone exerts direct genomic effects on target genes mediated via the androgen receptor (classical mechanism), and non-classical effects mediated through intracellular calcium mobilisation. FSH acts via a membrane receptor linked to adenylate cyclase, which produces cAMP and activates protein kinase A to stimulate production of Sertoli cell molecules, including lactate, transferrin, stem cell factor (SCF) and the FSH-regulating hormone, inhibin B. Sertoli cell Toll-like receptors (TLRs) respond to activation by appropriate ligands, which may be pathogen-derived or endogenous, and signal via a number of pathways, most critically the MyD88-dependent pathway to increase expression of inflammatory genes, including IL1α, IL6 and activin A. Although these separate signalling pathways control some functional outcomes in common, there is clear evidence for reciprocal inhibitory regulation between the two signalling pathways as well.
Importantly, inflammatory mediators have effects on several functions of the seminiferous epithelium. Interleukin 1α stimulates the proliferation of both spermatogonia (mitosis) and early spermatocytes (meiosis) (Hakovirta et al., 1993b, Parvinen et al., 1991, Söder et al., 1991), but IL1α also stimulates production of IL6 and activin A by the Sertoli cell (Okuma et al., 2005b, Syed et al., 1995), both of which inhibit meiotic proliferation and/or progression (Hakovirta et al., 1995, Meinhardt et al., 2000). Activin A has complex effects on spermatogonial proliferation, which may be either stimulatory or inhibitory under different experimental conditions and at different developmental stages (Mather et al., 1990, Meehan et al., 2000). Adding a further level of complexity, studies on inflammation and immunity have shown that activin A has the capacity to inhibit the production and activity of IL1 and IL6 as well (Phillips et al., 2009). It is therefore likely that the sequential production of these cytokines immediately following spermiation plays a crucial role in regulating the subsequent burst of spermatogonial and spermatocyte proliferation and activity. Likewise, less dramatic variations in the level of expression of these cytokines at other stages of the cycle of the may regulate other aspects of Sertoli cell and spermatogenic cell activity. In addition, IL1α, IL6, activin A and TNFα stimulate a number of Sertoli cell activities that are necessary to support spermatogenesis, including the production of lactate and transferrin (de Winter et al., 1994, Hoeben et al., 1997, Huleihel et al., 2002, Nehar et al., 1997, Nehar et al., 1998, Saito et al., 2011, Sigillo et al., 1999, Simon et al., 2007), while TNFα promotes spermatogenic cell survival in cultured human and rat seminiferous tubules, an effect that is probably mediated through the Sertoli cell (Pentikäinen et al., 2001, Suominen et al., 2004).
Conversely, there is evidence that activation of inflammatory pathways in the Sertoli cell inhibits or modulates the response of the Sertoli cell to trophic stimulation by FSH and androgens (Fig. 3B). The Sertoli cell is subjected to more or less constant exposure to these two hormones, which are consequently unable to regulate the changes in Sertoli cell function across the cycle of the seminiferous epithelium on their own. There is a clear reciprocal inhibitory relationship between FSH, which acts via the production of 3′,5′-cyclic adenosine monophosphate (cAMP) and activation of protein kinase A, and inflammatory signalling via LPS, IL1α and TNFα in the control of production of activin A and the FSH-regulating hormone, inhibin B, in particular (Okuma et al., 2005a, Okuma et al., 2005b, Saito et al., 2011). However, this inhibitory interaction is not confined to activin and inhibin: IL1α, IL1β and TNFα have been shown to inhibit the ability of FSH to stimulate aromatase activity and stem cell factor (SCF) expression, and TNFα also inhibits the effects of FSH on lactate production by the Sertoli cell (Khan and Nieschlag, 1991, Mauduit et al., 1993, Saito et al., 2011). It also needs to be recognised that studies have shown synergistic actions of IL1 and FSH on some Sertoli cell functions in culture (Huleihel et al., 2002), further highlighting the complexity in the interactions involved.
The full details of this interaction between inflammatory signalling and FSH signalling in the Sertoli cell are unclear at present. While LPS and IL1α normally act via the adapter protein MyD88 and its downstream signalling pathways involving the transcription factors NFκB and AP1, and the MAP kinases p38 and Jnk, these inflammatory mediators also activate several other signalling pathways, most notably the sphingomyelinase/ceramide pathway, the phospholipase A2/arachidonic acid metabolite pathway and the phosphoinositide-specific phospholipase C pathway involving diacyglycerol and inositol trisphosphate (Dinarello, 1996). Moreover, TNFα does not act via MyD88 at all, but activates the TRAFs via a separate mechanism entirely (Chung et al., 2002). Critically, studies have shown that IL1 and TNFα activate the MAP kinases, p38 and Jnk, in Sertoli cells (De Cesaris et al., 1998, Ishikawa et al., 2005, Ishikawa and Morris, 2006, Petersen et al., 2005, Riccioli et al., 2006), and inhibitory interactions between these MAP kinase pathways and cAMP signalling has been reported in other cell types (Park et al., 2010, Zhang et al., 2006). Furthermore, there is evidence for interaction between inflammatory signalling and androgen action in the Sertoli cell: for example, TNFα stimulates androgen receptor expression in rat Sertoli cells by activating NFκB, which binds to enhancer motifs in the androgen receptor promoter (Delfino et al., 2003). However, TNFα also inhibits at least some porcine Sertoli cell responses to androgens in vitro (Benbrahim-Tallaa et al., 2002). Regardless of the specific mechanisms underlying these interactions, the data indicate that stage-specific production of inflammatory gene products by the Sertoli cells and spermatogenic cells have the potential to modulate the response of the Sertoli cell towards the constant influence of its trophic hormones.
Finally, IL1α, TNFα and NO all cause disassembly of the Sertoli cell junctions that constitute the blood–testis barrier, as well as the junctional complexes involved in Sertoli-spermatogenic cell adhesion (Lee and Cheng, 2003, Li et al., 2006, Sarkar et al., 2008, Siu et al., 2003). This involves the inhibition of essential junctional proteins, regulation of matrix metalloprotease and protease inhibitor activity, and disruption of the Sertoli cell actin cytoskeleton. Consequently, production of these inflammatory mediators by either the Sertoli cell or spermatogenic cells, or both, in the stages immediately following spermiation (i.e. stages IX–XIII) may play a central role in the opening of the blood–testis barrier to facilitate the movement of the early spermatocytes into the luminal compartment of the seminiferous epithelium at this time.
6. Implications for testicular physiology and pathology
In summary, the surge of inflammatory events within the seminiferous epithelium subsequent to sperm release (at stage VIII) may be responsible for regulating (at subsequent stages IX–XIII) a wave of spermatogonial proliferation, the timing of critical events in meiosis among early spermatocytes, modulating Sertoli cell activity and hormonal responsiveness, and opening of the Sertoli tight junctions to allow the spermatocytes to pass through into the luminal compartment where they can complete their development and differentiation into mature spermatozoa. The trigger for these events appears to be the phagocytosis of the residual bodies by the Sertoli cell (Gérard et al., 1992, Syed et al., 1995). Since phagocytosis alone is not usually a sufficient trigger for inflammation, it may be speculated that the contents of the discarded sperm cytoplasm serve to activate the response, possibly by engaging pattern recognition receptors, such as the TLRs, expressed by the Sertoli cells. Although the TLRs evolved to recognise pathogen-derived molecules, such as LPS and bacterial lipoproteins, recent data show that they are also activated by endogenous molecules (once microbial contamination has been excluded). For example, HMGB1, found in both spermatogonia and Sertoli cells and increased in the testis following treatment with LPS (Metukuri et al., 2010, Zetterström et al., 2006), is a ligand for TLR2, 4 and 9 (Park et al., 2006, Tian et al., 2007), while mammalian mRNA is a ligand for TLR3 and 7, and mammalian CpG DNA can activate TLR9 (Barrat et al., 2005, Karikó et al., 2004, Tsan and Gao, 2004, Yasuda et al., 2005). Since individual TLR null mice have apparently normal fertility, such communication probably involves more than one receptor/ligand interaction. It can further be proposed that activation of the spermatogenic cells to express iNOS and TNFα occurs secondarily to the activation of the Sertoli cells, by a mechanism that is yet to be identified. Moreover, since a large proportion of developing spermatogenic cells do not develop to maturity, but undergo spontaneous apoptosis, phagocytosis of these senescent cells may drive expression of inflammatory genes, such as IL1α, at other stages of the cycle of the seminiferous epithelium as well (Hakovirta et al., 1993b, Jonsson et al., 1999). Consequently, signalling through inflammation-related pathways can provide both a mechanism for communication between cell types in the seminiferous epithelium, and an explanation for how the development of the successive generations of spermatogenic cells remains co-ordinated and highly organised.
One other implication arising from the ongoing production of inflammatory genes within the seminiferous epithelium is that this may be responsible for regulating adaptive immune responses in the interstitial tissue, leading to the ability of the testis to support extended graft survival (i.e. testicular immune privilege). This could involve the production by the Sertoli cell of activin A, which has profound regulatory effects on antigen-presenting cell and lymphocyte functions in addition to its pro-inflammatory activities (Phillips et al., 2009).
It must be conceded that, although there is evidence from other systems that TLR signalling plays a role in non-pathogenic and physiological process (Rakoff-Nahoum et al., 2004), the evidence that TLRs play a critical role in normal spermatogenesis is largely circumstantial. More work is required to establish if this hypothesis is sustainable. On the other hand, there is no doubt that expression of TLRs and other pattern-recognition receptors by the Sertoli cell has considerable significance for testicular pathology. Presumably, TLRs expressed by the Sertoli cells, and possibly by the spermatogenic cells, are necessary to detect pathogens that ascend the reproductive tract and, as a consequence, lie behind the blood–testis barrier (Demir et al., 2007, Lucchetta et al., 1983, Nagaosa et al., 2009). The close relationship between inflammatory signalling in the seminiferous epithelium and spermatogenesis provides a mechanism to account for the link between systemic infection/inflammation and testicular dysfunction. Data from the LPS-treated rat model discussed at the start of this review pointed towards a specific sensitivity to acute inflammation that is most pronounced at stages IX–XIII of the cycle of the seminiferous epithelium, i.e. immediately following spermiation. These are the same stages of spermatogenic development that display the most dramatic inflammation-like responses during normal spermatogenesis. It is reasonable to assume that at least some of the negative effects of inflammation on spermatogenesis may be attributable to elevated production of inflammatory mediators within the circulation and the testis during infection and inflammation, regardless of its origin, which subsequently exert disruptive effects on spermatogenic cell development and survival at this critical time in the spermatogenic process. However, it should also be recognised that the presence of intact pathogens within the testicular environment will have much more severe consequences for spermatogenesis than those activated through TLR signalling alone, due to the influence of multiple bacterial products on other arms of the immune system (Bhushan et al., 2008, Nagaosa et al., 2009).
7. Significance and conclusions
Male infertility, reproductive tract infections, and chronic scrotal or perineal pain due to non-pathogenic inflammation cause enormous misery for a significant number of men and their partners, and place substantial burdens on the health care system. Approximately 1/20 men are infertile, and the largest cohort of male factor infertility of known aetiology have a suspected inflammatory or autoimmune involvement. This relationship is underscored by a recent microarray analysis of genes expressed in human spermatogenic failure, which show a skewing towards genes involved in inflammation (Spiess et al., 2007). Furthermore, testicular inflammation, caused by urogenital bacterial infections, sexually transmitted diseases, or even some non-reproductive infections such as mumps, severe acute respiratory syndrome (SARS) and tuberculosis, frequently leads to temporary or permanent loss of fertility (Aratchige et al., 2008, Xu et al., 2006). The WHO estimates that reproductive tract infections account for about 3% of the global burden of ill-health among men (AbouZahr and Vaughan, 2000). The discovery that pattern-recognition receptors and inflammatory signalling pathways appear to play a central role in the Sertoli cell's ability to support spermatogenesis provides a potential explanation why inflammation frequently plays such a central role in male reproductive dysfunction. Further investigation of these processes has the potential to considerably expand our understanding of testicular dysfunction and disease, and eventually provide new opportunities for therapeutic interventions.
Acknowledgements
This work was supported by a Fellowship Award from the National Health and Medical Research Council (NHMRC Grant number 143788) and an NHMRC Program Grant (143786).
References
- AbouZahr C., Vaughan J.P. Assessing the burden of sexual and reproductive ill-health: questions regarding the use of disability-adjusted life years. Bull. World Health Org. 2000;78:655–666. [PMC free article] [PubMed] [Google Scholar]
- Aly H.A., Lightfoot D.A., El-Shemy H.A. Bacterial lipopolysaccharide-induced oxidative stress in adult rat Sertoli cells in vitro. Toxicol. In Vitro. 2010;24:1266–1272. doi: 10.1016/j.tiv.2010.01.009. [DOI] [PubMed] [Google Scholar]
- Aratchige P.E., McIntyre P.B., Quinn H.E., Gilbert G.L. Recent increases in mumps incidence in Australia: the “forgotten’ age group in the 1998 Australian Measles Control Campaign. Med. J. Aust. 2008;189:434–437. doi: 10.5694/j.1326-5377.2008.tb02115.x. [DOI] [PubMed] [Google Scholar]
- Aubry F., Habasque C., Satie A.P., Jégou B., Samson M. Expression and regulation of the CC-chemokine monocyte chemoattractant protein-1 in rat testicular cells in primary culture. Biol. Reprod. 2000;62:1427–1435. doi: 10.1095/biolreprod62.5.1427. [DOI] [PubMed] [Google Scholar]
- Baker H.W. Reproductive effects of nontesticular illness. Endocrinol. Metab. Clin. North Am. 1998;27:831–850. doi: 10.1016/s0889-8529(05)70043-8. [DOI] [PubMed] [Google Scholar]
- Barrat F.J., Meeker T., Gregorio J., Chan J.H., Uematsu S., Akira S., Chang B., Duramad O., Coffman R.L. Nucleic acids of mammalian origin can act as endogenous ligands for Toll-like receptors and may promote systemic lupus erythematosus. J. Exp. Med. 2005;202:1131–1139. doi: 10.1084/jem.20050914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauché F., Stéphan J.P., Touzalin A.M., Jégou B. In vitro regulation of an inducible-type NO synthase in the rat seminiferous tubule cells. Biol. Reprod. 1998;58:431–438. doi: 10.1095/biolreprod58.2.431. [DOI] [PubMed] [Google Scholar]
- Benbrahim-Tallaa L., Boussouar F., Rey C., Benahmed M. Tumor necrosis factor-α inhibits glutathione S-transferase-α expression in cultured porcine Sertoli cells. J. Endocrinol. 2002;175:803–812. doi: 10.1677/joe.0.1750803. [DOI] [PubMed] [Google Scholar]
- Bhushan S., Tchatalbachev S., Klug J., Fijak M., Pineau C., Chakraborty T., Meinhardt A. Uropathogenic Escherichia coli block MyD88-dependent and activate MyD88-independent signaling pathways in rat testicular cells. J. Immunol. 2008;180:5537–5547. doi: 10.4049/jimmunol.180.8.5537. [DOI] [PubMed] [Google Scholar]
- Bourdon V., Defamie N., Fenichel P., Pointis G. Regulation of tissue-type plasminogen activator and its inhibitor (PAI-1) by lipopolysaccharide-induced phagocytosis in a Sertoli cell line. Exp. Cell Res. 1999;247:367–372. doi: 10.1006/excr.1998.4369. [DOI] [PubMed] [Google Scholar]
- Carlsen E., Andersson A.M., Petersen J.H., Skakkebaek N.E. History of febrile illness and variation in semen quality. Hum. Reprod. 2003;18:2089–2092. doi: 10.1093/humrep/deg412. [DOI] [PubMed] [Google Scholar]
- Cheng C.Y., Mruk D.D. Cell junction dynamics in the testis: Sertoli-germ cell interactions and male contraceptive development. Physiol. Rev. 2002;82:825–874. doi: 10.1152/physrev.00009.2002. [DOI] [PubMed] [Google Scholar]
- Chung J.Y., Park Y.C., Ye H., Wu H. All TRAFs are not created equal: common and distinct molecular mechanisms of TRAF-mediated signal transduction. J. Cell Sci. 2002;115:679–688. doi: 10.1242/jcs.115.4.679. [DOI] [PubMed] [Google Scholar]
- Cudicini C., Lejeune H., Gomez E., Bosmans E., Ballet F., Saez J., Jégou B. Human Leydig cells and Sertoli cells are producers of interleukins-1 and -6. J. Clin. Endocrinol. Metab. 1997;82:1426–1433. doi: 10.1210/jcem.82.5.3938. [DOI] [PubMed] [Google Scholar]
- De Cesaris P., Starace D., Riccioli A., Padula F., Filippini A., Ziparo E. Tumor necrosis factor-α induces interleukin-6 production and integrin ligand expression by distinct transduction pathways. J. Biol. Chem. 1998;273:7566–7571. doi: 10.1074/jbc.273.13.7566. [DOI] [PubMed] [Google Scholar]
- De S.K., Chen H.L., Pace J.L., Hunt J.S., Terranova P.F., Enders G.C. Expression of tumor necrosis factor-α in mouse spermatogenic cells. Endocrinology. 1993;133:389–396. doi: 10.1210/endo.133.1.8319585. [DOI] [PubMed] [Google Scholar]
- de Winter J.P., Vanderstichele H.M., Verhoeven G., Timmerman M.A., Wesseling J.G., de Jong F.H. Peritubular myoid cells from immature rat testes secrete activin-A and express activin receptor type II in vitro. Endocrinology. 1994;135:759–767. doi: 10.1210/endo.135.2.8033824. [DOI] [PubMed] [Google Scholar]
- Delfino F., Walker W.H. Stage-specific nuclear expression of NF-κB in mammalian testis. Mol. Endocrinol. 1998;12:1696–1707. doi: 10.1210/mend.12.11.0194. [DOI] [PubMed] [Google Scholar]
- Delfino F.J., Boustead J.N., Fix C., Walker W.H. NF-κB and TNF-α stimulate androgen receptor expression in Sertoli cells. Mol. Cell. Endocrinol. 2003;201:1–12. doi: 10.1016/s0303-7207(03)00005-4. [DOI] [PubMed] [Google Scholar]
- Demir A., Türker P., Önol F.F., Sirvanci S., Findik A., Tarcan T. Effect of experimentally induced Escherichia coli epididymo-orchitis and ciprofloxacin treatment on rat spermatogenesis. Int. J. Urol. 2007;14:268–272. doi: 10.1111/j.1442-2042.2007.01682.x. [DOI] [PubMed] [Google Scholar]
- Dinarello C.A. Biologic basis for interleukin-1 in disease. Blood. 1996;87:2095–2147. [PubMed] [Google Scholar]
- Dong Q., Hawker F., McWilliam D., Bangah M., Burger H., Handelsman D.J. Circulating immunoreactive inhibin and testosterone levels in men with critical illness. Clin. Endocrinol. 1992;36:399–404. doi: 10.1111/j.1365-2265.1992.tb01466.x. [DOI] [PubMed] [Google Scholar]
- Fakunding J.L., Tindall D.J., Dedman J.R., Mena C.R., Means A.R. Biochemical actions of follice-stimulating hormone in the Sertoli cell of the rat testis. Endocrinology. 1976;98:392–402. doi: 10.1210/endo-98-2-392. [DOI] [PubMed] [Google Scholar]
- Galanos C., Freudenberg M.A. Mechanisms of endotoxin shock and endotoxin hypersensitivity. Immunobiology. 1993;187:346–356. doi: 10.1016/S0171-2985(11)80349-9. [DOI] [PubMed] [Google Scholar]
- Gérard N., Syed V., Jégou B. Lipopolysaccharide, latex beads and residual bodies are potent activators of Sertoli cell interleukin-1α production. Biochem. Biophys. Res. Commun. 1992;185:154–161. doi: 10.1016/s0006-291x(05)80969-6. [DOI] [PubMed] [Google Scholar]
- Gerdprasert O., O’Bryan M.K., Muir J.A., Caldwell A.M., Schlatt S., de Kretser D.M., Hedger M.P. The response of testicular leukocytes to lipopolysaccharide-induced inflammation: further evidence for heterogeneity of the testicular macrophage population. Cell Tissue Res. 2002;308:277–285. doi: 10.1007/s00441-002-0547-6. [DOI] [PubMed] [Google Scholar]
- Gerdprasert O., O’Bryan M.K., Nikolic-Paterson D.J., Sebire K., de Kretser D.M., Hedger M.P. Expression of monocyte chemoattractant protein-1 and macrophage colony-stimulating factor in normal and inflamed rat testis. Mol. Hum. Reprod. 2002;8:518–524. doi: 10.1093/molehr/8.6.518. [DOI] [PubMed] [Google Scholar]
- Gow R.M., O’Bryan M.K., Canny B.J., Ooi G.T., Hedger M.P. Differential effects of dexamethasone treatment on lipopolysaccharide-induced testicular inflammation and reproductive hormone inhibition in adult rats. J. Endocrinol. 2001;168:193–201. doi: 10.1677/joe.0.1680193. [DOI] [PubMed] [Google Scholar]
- Hakovirta H., Kaipia A., Söder O., Parvinen M. Effects of activin-A, inhibin-A, and transforming growth factor-β1 on stage-specific deoxyribonucleic acid synthesis during rat seminiferous epithelial cycle. Endocrinology. 1993;133:1664–1668. doi: 10.1210/endo.133.4.8404607. [DOI] [PubMed] [Google Scholar]
- Hakovirta H., Pentitilä T.L., Pöllänen P., Fröysa B., Söder O., Parvinen M. Interleukin-1 bioactivity and DNA synthesis in X-irradiated rat testes. Int. J. Androl. 1993;16:159–164. doi: 10.1111/j.1365-2605.1993.tb01170.x. [DOI] [PubMed] [Google Scholar]
- Hakovirta H., Syed V., Jégou B., Parvinen M. Function of interleukin-6 as an inhibitor of meiotic DNA synthesis in the rat seminiferous epithelium. Mol. Cell. Endocrinol. 1995;108:193–198. doi: 10.1016/0303-7207(95)03475-m. [DOI] [PubMed] [Google Scholar]
- Hales D.B. Testicular macrophage modulation of Leydig cell steroidogenesis. J. Reprod. Immunol. 2002;57:3–18. doi: 10.1016/s0165-0378(02)00020-7. [DOI] [PubMed] [Google Scholar]
- Hayes R., Chalmers S.A., Nikolic-Paterson D.J., Atkins R.C., Hedger M.P. Secretion of bioactive interleukin 1 by rat testicular macrophages in vitro. J. Androl. 1996;17:41–49. [PubMed] [Google Scholar]
- Hedger M.P., Hales D.B. Immunophysiology of the male reproductive tract. In: Neill J.D., editor. Knobil and Neill's Physiology of Reproduction. Elsevier; Amsterdam: 2006. pp. 1195–1286. [Google Scholar]
- Hertzog P.J., O’Neill L.A., Hamilton J.A. The interferon in TLR signaling: more than just antiviral. Trends Immunol. 2003;24:534–539. doi: 10.1016/j.it.2003.08.006. [DOI] [PubMed] [Google Scholar]
- Hirschfeld M., Ma Y., Weis J.H., Vogel S.N., Weis J.J. Cutting edge: repurification of lipopolysaccharide eliminates signaling through both human and murine Toll-like receptor 2. J. Immunol. 2000;165:618–622. doi: 10.4049/jimmunol.165.2.618. [DOI] [PubMed] [Google Scholar]
- Hoeben E., Wuyts A., Proost P., Van Damme J., Verhoeven G. Identification of IL-6 as one of the important cytokines responsible for the ability of mononuclear cells to stimulate Sertoli cell functions. Mol. Cell. Endocrinol. 1997;132:149–160. doi: 10.1016/s0303-7207(97)00132-9. [DOI] [PubMed] [Google Scholar]
- Huleihel M., Zeyse D., Lunenfeld E., Zeyse M., Mazor M. Induction of transferrin secretion in murine Sertoli cells by FSH and IL-1: the possibility of different mechanism(s) of regulation. Am. J. Reprod. Immunol. 2002;47:112–117. doi: 10.1034/j.1600-0897.2002.0o054.x. [DOI] [PubMed] [Google Scholar]
- Ishikawa T., Hwang K., Lazzarino D., Morris P.L. Sertoli cell expression of steroidogenic acute regulatory protein-related lipid transfer 1 and 5 domain-containing proteins and sterol regulatory element binding protein-1 are interleukin-1β regulated by activation of c-Jun N-terminal kinase and cyclooxygenase-2 and cytokine induction. Endocrinology. 2005;146:5100–5111. doi: 10.1210/en.2005-0567. [DOI] [PubMed] [Google Scholar]
- Ishikawa T., Morris P.L. Interleukin-1β signals through a c-Jun N-terminal kinase-dependent inducible nitric oxide synthase and nitric oxide production pathway in Sertoli epithelial cells. Endocrinology. 2006;147:5424–5430. doi: 10.1210/en.2006-0643. [DOI] [PubMed] [Google Scholar]
- Jiang Z., Georgel P., Du X., Shamel L., Sovath S., Mudd S., Huber M., Kalis C., Keck S., Galanos C., Freudenberg M., Beutler B. CD14 is required for MyD88-independent LPS signaling. Nat. Immunol. 2005;6:565–570. doi: 10.1038/ni1207. [DOI] [PubMed] [Google Scholar]
- Jonsson C.K., Zetterström R.H., Holst M., Parvinen M., Söder O. Constitutive expression of interleukin-1α messenger ribonucleic acid in rat Sertoli cells is dependent upon interaction with germ cells. Endocrinology. 1999;140:3755–3761. doi: 10.1210/endo.140.8.6900. [DOI] [PubMed] [Google Scholar]
- Karikó K., Ni H., Capodici J., Lamphier M., Weissman D. mRNA is an endogenous ligand for Toll-like receptor 3. J. Biol. Chem. 2004;279:12542–12550. doi: 10.1074/jbc.M310175200. [DOI] [PubMed] [Google Scholar]
- Kern S., Robertson S.A., Mau V.J., Maddocks S. Cytokine secretion by macrophages in the rat testis. Biol. Reprod. 1995;53:1407–1416. doi: 10.1095/biolreprod53.6.1407. [DOI] [PubMed] [Google Scholar]
- Khan S.A., Nieschlag E. Interleukin-1 inhibits follitropin-induced aromatase activity in immature rat Sertoli cells in vitro. Mol. Cell. Endocrinol. 1991;75:1–7. doi: 10.1016/0303-7207(91)90238-n. [DOI] [PubMed] [Google Scholar]
- Lauw F.N., Caffrey D.R., Golenbock D.T. Of mice and man: TLR11 (finally) finds profilin. Trends Immunol. 2005;26:509–511. doi: 10.1016/j.it.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Lee N.P., Cheng C.Y. Regulation of Sertoli cell tight junction dynamics in the rat testis via the nitric oxide synthase/soluble guanylate cyclase/3′,5′-cyclic guanosine monophosphate/protein kinase G signaling pathway: an in vitro study. Endocrinology. 2003;144:3114–3129. doi: 10.1210/en.2002-0167. [DOI] [PubMed] [Google Scholar]
- Li M.W., Xia W., Mruk D.D., Wang C.Q., Yan H.H., Siu M.K., Lui W.Y., Lee W.M., Cheng C.Y. Tumor necrosis factor α reversibly disrupts the blood-testis barrier and impairs Sertoli-germ cell adhesion in the seminiferous epithelium of adult rat testes. J. Endocrinol. 2006;190:313–329. doi: 10.1677/joe.1.06781. [DOI] [PubMed] [Google Scholar]
- Liew S.H., Meachem S.J., Hedger M.P. A stereological analysis of the response of spermatogenesis to an acute inflammatory episode in adult rats. J. Androl. 2007;28:176–185. doi: 10.2164/jandrol.106.000752. [DOI] [PubMed] [Google Scholar]
- Lucchetta R., Clavert A., Meyer J.M., Bollack C. Acute experimental E. coli epididymitis in the rat and its consequences on spermatogenesis. Urol. Res. 1983;11:117–120. doi: 10.1007/BF00257715. [DOI] [PubMed] [Google Scholar]
- Lui W.Y., Wong C.H., Mruk D.D., Cheng C.Y. TGF-β3 regulates the blood-testis barrier dynamics via the p38 mitogen activated protein (MAP) kinase pathway: an in vivo study. Endocrinology. 2003;144:1139–1142. doi: 10.1210/en.2002-0211. [DOI] [PubMed] [Google Scholar]
- Mather J.P., Attie K.M., Woodruff T.K., Rice G.C., Phillips D.M. Activin stimulates spermatogonial proliferation in germ-Sertoli cell cocultures from immature rat testis. Endocrinology. 1990;127:3206–3214. doi: 10.1210/endo-127-6-3206. [DOI] [PubMed] [Google Scholar]
- Mauduit C., Jaspar J.M., Poncelet E., Charlet C., Revol A., Franchimont P., Benahmed M. Tumor necrosis factor-α antagonizes follicle-stimulating hormone action in cultured Sertoli cells. Endocrinology. 1993;133:69–76. doi: 10.1210/endo.133.1.8319591. [DOI] [PubMed] [Google Scholar]
- McLachlan R.I., Wreford N.G., O’Donnell L., de Kretser D.M., Robertson D.M. The endocrine regulation of spermatogenesis: independent roles for testosterone and FSH. J. Endocrinol. 1996;148:1–9. doi: 10.1677/joe.0.1480001. [DOI] [PubMed] [Google Scholar]
- Meehan T., Schlatt S., O’Bryan M.K., de Kretser D.M., Loveland K.L. Regulation of germ cell and Sertoli cell development by activin, follistatin, and FSH. Dev. Biol. 2000;220:225–237. doi: 10.1006/dbio.2000.9625. [DOI] [PubMed] [Google Scholar]
- Meinhardt A., McFarlane J.R., Seitz J., de Kretser D.M. Activin maintains the condensed type of mitochondria in germ cells. Mol. Cell. Endocrinol. 2000;168:111–117. doi: 10.1016/s0303-7207(00)00308-7. [DOI] [PubMed] [Google Scholar]
- Metukuri M.R., Reddy C.M., Reddy P.R., Reddanna P. Bacterial LPS mediated acute inflammation-induced spermatogenic failure in rats: role of stress response proteins and mitochondrial dysfunction. Inflammation. 2010;33:235–243. doi: 10.1007/s10753-009-9177-4. [DOI] [PubMed] [Google Scholar]
- Monder C., Miroff Y., Marandici A., Hardy M.P. 11β-Hydroxysteroid dehydrogenase alleviates glucocorticoid-mediated inhibition of steroidogenesis in rat Leydig cells. Endocrinology. 1994;134:1199–1204. doi: 10.1210/endo.134.3.8119160. [DOI] [PubMed] [Google Scholar]
- Nagaosa K., Nakashima C., Kishimoto A., Nakanishi Y. Immune response to bacteria in seminiferous epithelium. Reproduction. 2009;137:879–888. doi: 10.1530/REP-08-0460. [DOI] [PubMed] [Google Scholar]
- Nariculam J., Minhas S., Adeniyi A., Ralph D.J., Freeman A. A review of the efficacy of surgical treatment for and pathological changes in patients with chronic scrotal pain. BJU Int. 2007;99:1091–1093. doi: 10.1111/j.1464-410X.2006.06733.x. [DOI] [PubMed] [Google Scholar]
- Nehar D., Mauduit C., Boussouar F., Benahmed M. Tumor necrosis factor-α-stimulated lactate production is linked to lactate dehydrogenase A expression and activity increase in porcine cultured Sertoli cells. Endocrinology. 1997;138:1964–1971. doi: 10.1210/endo.138.5.5098. [DOI] [PubMed] [Google Scholar]
- Nehar D., Mauduit C., Boussouar F., Benahmed M. Interleukin 1α stimulates lactate dehydrogenase A expression and lactate production in cultured porcine Sertoli cells. Biol. Reprod. 1998;59:1425–1432. doi: 10.1095/biolreprod59.6.1425. [DOI] [PubMed] [Google Scholar]
- O’Bryan M.K., Gerdprasert O., Nikolic-Paterson D.J., Meinhardt A., Muir J.A., Foulds L.M., Phillips D.J., de Kretser D.M., Hedger M.P. Cytokine profiles in the testes of rats treated with lipopolysaccharide reveal localized suppression of inflammatory responses. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2005;288:R1744–R1755. doi: 10.1152/ajpregu.00651.2004. [DOI] [PubMed] [Google Scholar]
- O’Bryan M.K., Hedger M.P. Inflammatory networks in the control of spermatogenesis. Chronic inflammation in an immunologically privileged tissue? Adv. Exp. Med. Biol. 2008;636:92–114. doi: 10.1007/978-0-387-09597-4_6. [DOI] [PubMed] [Google Scholar]
- O’Bryan M.K., Schlatt S., Gerdprasert O., Phillips D.J., de Kretser D.M., Hedger M.P. Inducible nitric oxide synthase in the rat testis: evidence for potential roles in both normal function and inflammation-mediated infertility. Biol. Reprod. 2000;63:1285–1293. doi: 10.1095/biolreprod63.5.1285. [DOI] [PubMed] [Google Scholar]
- O’Bryan M.K., Schlatt S., Phillips D.J., de Kretser D.M., Hedger M.P. Bacterial lipopolysaccharide-induced inflammation compromises testicular function at multiple levels in vivo. Endocrinology. 2000;141:238–246. doi: 10.1210/endo.141.1.7240. [DOI] [PubMed] [Google Scholar]
- O’Donnell L., McLachlan R.I., Wreford N.G., de Kretser D.M., Robertson D.M. Testosterone withdrawal promotes stage-specific detachment of round spermatids from the rat seminiferous epithelium. Biol. Reprod. 1996;55:895–901. doi: 10.1095/biolreprod55.4.895. [DOI] [PubMed] [Google Scholar]
- O’Neill L.A., Bowie A.G. The family of five: TIR-domain-containing adaptors in Toll-like receptor signalling. Nat. Rev. Immunol. 2007;7:353–364. doi: 10.1038/nri2079. [DOI] [PubMed] [Google Scholar]
- Ogilvie K.M., Held Hales K., Roberts M.E., Hales D.B., Rivier C. The inhibitory effect of intracerebroventricularly injected interleukin 1β on testosterone secretion in the rat: role of steroidogenic acute regulatory protein. Biol. Reprod. 1999;60:527–533. doi: 10.1095/biolreprod60.2.527. [DOI] [PubMed] [Google Scholar]
- Okuda Y., Bardin C.W., Hodgskin L.R., Morris P.L. Interleukins-1α and -1β regulate interleukin-6 expression in Leydig and Sertoli cells. Rec. Prog. Horm. Res. 1995;50:367–372. doi: 10.1016/b978-0-12-571150-0.50022-6. [DOI] [PubMed] [Google Scholar]
- Okuma Y., O’Connor A.E., Hayashi T., Loveland K.L., de Kretser D.M., Hedger M.P. Regulated production of activin A and inhibin B throughout the cycle of the seminiferous epithelium in the rat. J. Endocrinol. 2006;190:331–340. doi: 10.1677/joe.1.06706. [DOI] [PubMed] [Google Scholar]
- Okuma Y., O’Connor A.E., Muir J.A., Stanton P.G., de Kretser D.M., Hedger M.P. Regulation of activin A and inhibin B secretion by inflammatory mediators in adult rat Sertoli cell cultures. J. Endocrinol. 2005;187:125–134. doi: 10.1677/joe.1.06266. [DOI] [PubMed] [Google Scholar]
- Okuma Y., Saito K., O’Connor A.E., Phillips D.J., de Kretser D.M., Hedger M.P. Reciprocal regulation of activin A and inhibin B by interleukin-1 (IL-1) and follicle-stimulating hormone (FSH) in rat Sertoli cells in vitro. J. Endocrinol. 2005;185:99–110. doi: 10.1677/joe.1.06053. [DOI] [PubMed] [Google Scholar]
- Park C.H., Moon Y., Shin C.M., Chung J.H. Cyclic AMP suppresses matrix metalloproteinase-1 expression through inhibition of MAPK and GSK-3beta. J. Invest. Dermatol. 2010;130:2049–2056. doi: 10.1038/jid.2010.62. [DOI] [PubMed] [Google Scholar]
- Park J.S., Gamboni-Robertson F., He Q., Svetkauskaite D., Kim J.Y., Strassheim D., Sohn J.W., Yamada S., Maruyama I., Banerjee A., Ishizaka A., Abraham E. High mobility group box 1 protein interacts with multiple Toll-like receptors. Am. J. Physiol. Cell Physiol. 2006;290:C917–C924. doi: 10.1152/ajpcell.00401.2005. [DOI] [PubMed] [Google Scholar]
- Parvinen M., Söder O., Mali P., Fröysa B., Ritzén E.M. In vitro stimulation of stage-specific deoxyribonucleic acid synthesis in rat seminiferous tubule segments by interleukin-1α. Endocrinology. 1991;129:1614–1620. doi: 10.1210/endo-129-3-1614. [DOI] [PubMed] [Google Scholar]
- Pentikäinen V., Erkkilä K., Suomalainen L., Otala M., Pentikäinen M.O., Parvinen M., Dunkel L. TNFα down-regulates the Fas ligand and inhibits germ cell apoptosis in the human testis. J. Clin. Endocrinol. Metab. 2001;86:4480–4488. doi: 10.1210/jcem.86.9.7861. [DOI] [PubMed] [Google Scholar]
- Petersen C., Svechnikov K., Fröysa B., Söder O. The p38 MAPK pathway mediates interleukin-1-induced Sertoli cell proliferation. Cytokine. 2005;32:51–59. doi: 10.1016/j.cyto.2005.07.014. [DOI] [PubMed] [Google Scholar]
- Phillips D.J., de Kretser D.M., Hedger M.P. Activin and related proteins in inflammation: not just interested bystanders. Cytokine Growth Factor Rev. 2009;20:153–164. doi: 10.1016/j.cytogfr.2009.02.007. [DOI] [PubMed] [Google Scholar]
- Rakoff-Nahoum S., Paglino J., Eslami-Varzaneh F., Edberg S., Medzhitov R. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004;118:229–241. doi: 10.1016/j.cell.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Reddy M.M., Mahipal S.V., Subhashini J., Reddy M.C., Roy K.R., Reddy G.V., Reddy P.R., Reddanna P. Bacterial lipopolysaccharide-induced oxidative stress in the impairment of steroidogenesis and spermatogenesis in rats. Reprod. Toxicol. 2006;22:493–500. doi: 10.1016/j.reprotox.2006.03.003. [DOI] [PubMed] [Google Scholar]
- Riccioli A., Starace D., Galli R., Fuso A., Scarpa S., Palombi F., De Cesaris P., Ziparo E., Filippini A. Sertoli cells initiate testicular innate immune responses through TLR activation. J. Immunol. 2006;177:7122–7130. doi: 10.4049/jimmunol.177.10.7122. [DOI] [PubMed] [Google Scholar]
- Roach J.C., Glusman G., Rowen L., Kaur A., Purcell M.K., Smith K.D., Hood L.E., Aderem A. The evolution of vertebrate Toll-like receptors. Proc. Natl. Acad. Sci. U.S.A. 2005;102:9577–9582. doi: 10.1073/pnas.0502272102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell L. Movement of spermatocytes from the basal to the adluminal compartment of the rat testis. Am. J. Anat. 1977;148:313–328. doi: 10.1002/aja.1001480303. [DOI] [PubMed] [Google Scholar]
- Saito, K., Winnall, W.R., Muir, J.A., Hedger, M.P., 2011. Regulation of Sertoli cell activin A and inhibin B by tumour necrosis factor α and interleukin 1α: interaction with follicle-stimulating hormone/adenosine 3′,5′-cyclic phosphate signalling. Mol. Cell. Endocrinol., doi:10.1016/j.mce.2011.01.014. [DOI] [PubMed]
- Sarkar O., Mathur P.P., Cheng C.Y., Mruk D.D. Interleukin 1 alpha (IL1A) is a novel regulator of the blood-testis barrier in the rat. Biol. Reprod. 2008;78:445–454. doi: 10.1095/biolreprod.107.064501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpe R.M., Donachie K., Cooper I. Re-evaluation of the intratesticular level of testosterone required for quantitative maintenance of spermatogenesis in the rat. J. Endocrinol. 1988;117:19–26. doi: 10.1677/joe.0.1170019. [DOI] [PubMed] [Google Scholar]
- Sigillo F., Guillou F., Fontaine I., Benahmed M., Le Magueresse-Battistoni B. In vitro regulation of rat Sertoli cell transferrin expression by tumor necrosis factor α and retinoic acid. Mol. Cell. Endocrinol. 1999;148:163–170. doi: 10.1016/s0303-7207(98)00199-3. [DOI] [PubMed] [Google Scholar]
- Simon L., Ekman G.C., Tyagi G., Hess R.A., Murphy K.M., Cooke P.S. Common and distinct factors regulate expression of mRNA for ETV5 and GDNF, Sertoli cell proteins essential for spermatogonial stem cell maintenance. Exp. Cell Res. 2007;313:3090–3099. doi: 10.1016/j.yexcr.2007.05.002. [DOI] [PubMed] [Google Scholar]
- Siu M.K., Lee W.M., Cheng C.Y. The interplay of collagen IV, tumor necrosis factor-α, gelatinase B (matrix metalloprotease-9), and tissue inhibitor of metalloproteases-1 in the basal lamina regulates Sertoli cell-tight junction dynamics in the rat testis. Endocrinology. 2003;144:371–387. doi: 10.1210/en.2002-220786. [DOI] [PubMed] [Google Scholar]
- Söder O., Syed V., Callard G.V., Toppari J., Pöllänen P., Parvinen M., Fröysa B., Ritzén E.M. Production and secretion of an interleukin-1-like factor is stage-dependent and correlates with spermatogonial DNA synthesis in the rat seminiferous epithelium. Int. J. Androl. 1991;14:223–231. doi: 10.1111/j.1365-2605.1991.tb01084.x. [DOI] [PubMed] [Google Scholar]
- Spiess A.N., Feig C., Schulze W., Chalmel F., Cappallo-Obermann H., Primig M., Kirchhoff C. Cross-platform gene expression signature of human spermatogenic failure reveals inflammatory-like response. Hum. Reprod. 2007;22:2936–2946. doi: 10.1093/humrep/dem292. [DOI] [PubMed] [Google Scholar]
- Starace D., Galli R., Paone A., Cesaris P.D., Filippini A., Ziparo E., Riccioli A. Toll-like receptor 3 activation induces antiviral immune responses in mouse Sertoli cells. Biol. Reprod. 2008;79:766–775. doi: 10.1095/biolreprod.108.068619. [DOI] [PubMed] [Google Scholar]
- Stéphan J.P., Guillemois C., Jégou B., Bauché F. Nitric oxide production by Sertoli cells in response to cytokines and lipopolysaccharide. Biochem. Biophys. Res. Comm. 1995;213:218–224. doi: 10.1006/bbrc.1995.2119. [DOI] [PubMed] [Google Scholar]
- Sun B., Qi N., Shang T., Wu H., Deng T., Han D. Sertoli cell-initiated testicular innate immune response through toll-like receptor-3 activation is negatively regulated by Tyro3, Axl, and mer receptors. Endocrinology. 2010;151:2886–2897. doi: 10.1210/en.2009-1498. [DOI] [PubMed] [Google Scholar]
- Suominen J.S., Wang Y., Kaipia A., Toppari J. Tumor necrosis factor-alpha (TNF-α) promotes cell survival during spermatogenesis, and this effect can be blocked by infliximab, a TNF-α antagonist. Eur. J. Endocrinol. 2004;151:629–640. doi: 10.1530/eje.0.1510629. [DOI] [PubMed] [Google Scholar]
- Syed V., Stéphan J.P., Gérard N., Legrand A., Parvinen M., Bardin C.W., Jégou B. Residual bodies activate Sertoli cell interleukin-1α (IL-1α) release, which triggers IL-6 production by an autocrine mechanism, through the lipoxygenase pathway. Endocrinology. 1995;136:3070–3078. doi: 10.1210/endo.136.7.7789334. [DOI] [PubMed] [Google Scholar]
- Takeuchi O., Akira S. Pattern recognition receptors and inflammation. Cell. 2010;140:805–820. doi: 10.1016/j.cell.2010.01.022. [DOI] [PubMed] [Google Scholar]
- Takeuchi O., Hoshino K., Kawai T., Sanjo H., Takada H., Ogawa T., Takeda K., Akira S. Differential roles of TLR2 and TLR4 in recognition of gram-negative and gram-positive bacterial cell wall components. Immunity. 1999;11:443–451. doi: 10.1016/s1074-7613(00)80119-3. [DOI] [PubMed] [Google Scholar]
- Tian J., Avalos A.M., Mao S.Y., Chen B., Senthil K., Wu H., Parroche P., Drabic S., Golenbock D., Sirois C., Hua J., An L.L., Audoly L., La Rosa G., Bierhaus A., Naworth P., Marshak-Rothstein A., Crow M.K., Fitzgerald K.A., Latz E., Kiener P.A., Coyle A.J. Toll-like receptor 9-dependent activation by DNA-containing immune complexes is mediated by HMGB1 and RAGE. Nat. Immunol. 2007;8:487–496. doi: 10.1038/ni1457. [DOI] [PubMed] [Google Scholar]
- Travassos L.H., Girardin S.E., Philpott D.J., Blanot D., Nahori M.A., Werts C., Boneca I.G. Toll-like receptor 2-dependent bacterial sensing does not occur via peptidoglycan recognition. EMBO Rep. 2004;5:1000–1006. doi: 10.1038/sj.embor.7400248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsan M.F., Gao B. Endogenous ligands of Toll-like receptors. J. Leuk. Biol. 2004;76:514–519. doi: 10.1189/jlb.0304127. [DOI] [PubMed] [Google Scholar]
- Turner T.T., Bang H.J., Lysiak J.L. The molecular pathology of experimental testicular torsion suggests adjunct therapy to surgical repair. J. Urol. 2004;172:2574–2578. doi: 10.1097/01.ju.0000144203.30718.19. [DOI] [PubMed] [Google Scholar]
- Turner T.T., Tung K.S., Tomomasa H., Wilson L.W. Acute testicular ischemia results in germ cell-specific apoptosis in the rat. Biol. Reprod. 1997;57:1267–1274. doi: 10.1095/biolreprod57.6.1267. [DOI] [PubMed] [Google Scholar]
- Wang D.L., Nagpal M.L., Calkins J.H., Chang W.W., Sigel M.M., Lin T. Interleukin-1β induces interleukin-1α messenger ribonucleic acid expression in primary cultures of Leydig cells. Endocrinology. 1991;129:2862–2866. doi: 10.1210/endo-129-6-2862. [DOI] [PubMed] [Google Scholar]
- Wang J.E., Josefsen G.M., Hansson V., Haugen T.B. Residual bodies and IL-1α stimulate expression of mRNA for IL-1α and IL-1 receptor type I in cultured rat Sertoli cells. Mol. Cell. Endocrinol. 1998;137:139–144. doi: 10.1016/s0303-7207(97)00246-3. [DOI] [PubMed] [Google Scholar]
- Winnall, W.R., Muir, J.A., Hedger, M.P., 2011. Differential responses of epithelial Sertoli cells of the rat testis to Toll-Like receptor 2 and 4 ligands: implications for studies of testicular inflammation using bacterial lipopolysaccharides. Innate Immun., doi:10.1177/1753425909354764. [DOI] [PubMed]
- Winnall W.R., Okuma Y., Saito K., Muir J.A., Hedger M.P. Regulation of interleukin 1α, activin and inhibin by lipopolysaccharide in Sertoli cells from prepubertal rats. Mol. Cell. Endocrinol. 2009;307:169–175. doi: 10.1016/j.mce.2009.02.007. [DOI] [PubMed] [Google Scholar]
- Wu H., Wang H., Xiong W., Chen S., Tang H., Han D. Expression patterns and functions of toll-like receptors in mouse Sertoli cells. Endocrinology. 2008;149:4402–4412. doi: 10.1210/en.2007-1776. [DOI] [PubMed] [Google Scholar]
- Xu J., Qi L., Chi X., Yang J., Wei X., Gong E., Peh S., Gu J. Orchitis: a complication of severe acute respiratory syndrome (SARS) Biol. Reprod. 2006;74:410–416. doi: 10.1095/biolreprod.105.044776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasuda K., Yu P., Kirschning C.J., Schlatter B., Schmitz F., Heit A., Bauer S., Hochrein H., Wagner H. Endosomal translocation of vertebrate DNA activates dendritic cells via TLR9-dependent and -independent pathways. J. Immunol. 2005;174:6129–6136. doi: 10.4049/jimmunol.174.10.6129. [DOI] [PubMed] [Google Scholar]
- Zähringer U., Lindner B., Inamura S., Heine H., Alexander C. TLR2 -promiscuous or specific? A critical re-evaluation of a receptor expressing apparent broad specificity. Immunobiology. 2008;213:205–224. doi: 10.1016/j.imbio.2008.02.005. [DOI] [PubMed] [Google Scholar]
- Zetterström C.K., Strand M.L., Söder O. The high mobility group box chromosomal protein 1 is expressed in the human and rat testis where it may function as an antibacterial factor. Hum. Reprod. 2006;21:2801–2809. doi: 10.1093/humrep/del256. [DOI] [PubMed] [Google Scholar]
- Zhang D., Zhang G., Hayden M.S., Greenblatt M.B., Bussey C., Flavell R.A., Ghosh S. A toll-like receptor that prevents infection by uropathogenic bacteria. Science. 2004;303:1522–1526. doi: 10.1126/science.1094351. [DOI] [PubMed] [Google Scholar]
- Zhang J., Bui T.N., Xiang J., Lin A. Cyclic AMP inhibits p38 activation via CREB-induced dynein light chain. Mol. Cell. Biol. 2006;26:1223–1234. doi: 10.1128/MCB.26.4.1223-1234.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]