Highlights
-
•
Foreign viral genes can be inserted into the AMPV genome.
-
•
Resultant recombinant viruses express the inserted genes and are stable in cell culture.
-
•
Both S1 and N genes from IBX QX induced protection against QX challenge.
-
•
Induced seroconversion after recombinant inoculation was minimal.
Keywords: Avian metapneumovirus, Infectious bronchitis, QX genotype, Recombinant vaccine, S1, Nucleocapsid protein, GFP
Abstract
The study investigates the ability of subtype A Avian metapneumovirus (AMPV) to accept foreign genes and be used as a vector for delivery of Infectious bronchitis virus (IBV) QX genes to chickens. Initially the GFP gene was added to AMPV at all gene junctions in conjunction with the development of cassetted full length DNA AMPV copies. After recombinant virus had been recovered by reverse genetics, GFP positions supporting gene expression while maintaining virus viability in vitro, were determined. Subsequently, either S1 or nucleocapsid (N) genes of IBV were positioned between AMPV M and F genes, while later a bivalent recombinant was prepared by inserting S1 and N at AMPV MF and GL junctions respectively. Immunofluorescent antibody staining showed that all recombinants expressed the inserted IBV genes in vitro and furthermore, all recombinant viruses were found to be highly stable during serial passage. Eyedrop inoculation of chickens with some AMPV-IBV recombinants at one-day-old induced protection against virulent IBV QX challenge 3 weeks later, as assessed by greater motility of tracheal cilia from chickens receiving the recombinants. Nonetheless evidence of AMPV/IBV seroconversion, or major recombinant tracheal replication, were largely absent.
1. Introduction
Avian metapneumovirus (AMPV) is a major endemic respiratory pathogen of global domestic poultry [1], and secondary infections can exacerbate the disease [2]. AMPV belongs to the subfamily Pneumovirinae, genus Metapneumovirus [3] of which four subtypes have been recognized (A, B, C and D) [4], [5], [6]. The genome has 8 genes, with genome sizes typically close to 13.5 kb [7]. Reverse genetics (RG) systems for subtypes A and C have allowed their rational mutation [8], [9]. To date RG has produced viruses with deletions, gene modifications and reporter gene insertions [8], [10], [11], [12]. Some studies have considered the replicative ability of recombinants in vivo [11], [12] but not foreign viral gene insertion, nor the genetic stability of expanded genomes.
Avian infectious bronchitis (IBV) is the major worldwide endemic respiratory pathogen of chickens (family coronavirus, genus gammacoronavirus) which, like AMPV primarily infects the respiratory tract but can also infect the kidneys, intestine and reproductive system [13]. IBV epidemiology is characterized by the emergence of virulent variants which evade prevailing IBV immunity. In the last decade the QX genotype [14] has emerged, which predominantly affects the respiratory tract and kidneys [15]. It was first recognised in China and has continued to spread to much of Europe and Asia. In this study, novel QX candidate vaccines based on AMPV vectors were constructed and tested.
The major IBV surface protein spike S0 becomes cleaved into the outer, antigenically important S1, and inner membrane bound, S2 section [13]. Previously inoculation of S1 expressed in baculovirus was shown to induce protection [16]. The internal nucleocapsid (N) protein can also induce protective immunity [17], [18] involving both T and B lymphocyte epitopes [18], [19]. Here two different QX S1 genes and a QX N gene were inserted into AMPV, both to assess the vector's acceptance of foreign genes, and its suitability for delivery of IBV genes to chickens.
Three AMPV genomes acted as vectors. Prior to introduction of S1 or N genes, a cloning site flanked by a transcription start and stop sequence, was added to intergenic regions of full length (FL) DNA genome copies. To aid IBV recombinant optimization, green fluorescent protein (GFP) was initially added to these sites and recombinant viruses recovered; then AMPV S1 and N recombinant viruses were constructed. The two S1 genes used differed by a 15 nucleotide deletion present in a proportion of the donor virus.
Recombinant viruses were tested in chickens in two experiments to determine their protective capacity. IBV inoculation of chickens leads to infection of and damage to the tracheal ciliated epithelium [20]. Loss of cilial motility is readily observed [21] and protection is considered best assessed by the maintenance of motility following challenge [22], as also adopted in European Pharmacopoeia, IBV vaccine monographs. To assess replication of recombinants, real time RT PCR was performed on material from choanal swabs while induced specific antibody to IBV and AMPV was measured by ELISA and haemaglutination inhibition (HI).
2. Materials and methods
2.1. Addition of GFP to AMPV
Three subtype A AMPV viruses were employed as vectors for GFP and later IBV genes. First was a German field isolate (Virus A) passaged in Vero cells [9] and found avirulent in turkeys [12], second was Virus AvF which contained an F gene modification found to better induce protection in turkeys [12] and third was 309/04, a virulent field isolate deriving from a subtype A vaccine and arising in field conditions [23].
Seven versions of virus A [12] FL cDNA were made by site directed mutagenesis, as outlined in Fig. 1 . An Xho1 restriction endonuclease (RE) site was added to each intergenic region, following the preceding gene stop signal and prior to the downstream gene start signal. A cloning cassette flanked by cut Sal 1 RE sites, allowing gene insertion and transcription, was ligated into each cut Xho1 RE site of the seven FLs. After cloning into STB12 cells (Invitrogen, according to manufacturer's recommendation (AMR)), the seven FLs were cut with Sal 1. GFP genes flanked by Xho1 sites were produced by high fidelity PCR using primers GFP ins+ and GFP ins neg (Table 1 ) and these were added to the seven FL cDNAs by ligation after Xho1 digestion. Colonies containing DNA of correct orientation and sequence were selected by sequencing. FLs containing GFP were recovered by RG [9]. GFP expression was assessed by fluorescence microscopy. Virus viabilities were evaluated as maximum titres obtained following three Vero passages.
Fig. 1.
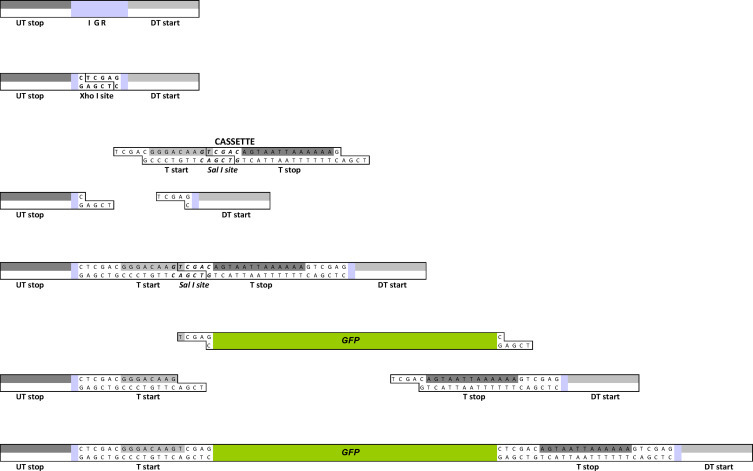
Schematic representation of the strategy used for adding genes to cloned AMPV genome copies. An Xho1 RE site, then standardized cassette and finally chosen gene for expression (illustrated by GFP) were added to intergenic regions (IGR) between upstream gene transcriptional stops (UT stop) and the downstream gene transcriptional starts (DT start).
Table 1.
Oligonucleotide primer sequences used.
| Name | Primers (5′… 3′) | Function | |
|---|---|---|---|
| 1 | GFP ins+ | GGGACCTCGAGTATGGTGAGCAAGGGCGAGGAGC | GFP amplification adding XhoI sites |
| 2 | GFP ins neg | CCACTCCTCGAGATTTTACTTGTACAGCTCGTCC | GFP amplification adding XhoI sites |
| 3 | N all b neg | ACTAATGAGAATCACAATAATAAAAAGCACAG | N RT and PCR amplification |
| 4 | N 200+ | GCAGCATGGATACTGGAGACG | N sequencing |
| 5 | N 300 neg | GGTCAGCGGCTGGTCCTGTTCC | N sequencing |
| 6 | N 560+ | GGTTCACGTGGTCGTAGGAG | N sequencing |
| 7 | N 750+ | CCAGGTTATAGAGTAGATCAAGTATTTGGC | N sequencing |
| 8 | N 920+ | CTGTGGTGCCTAGAGATGACC | N primer for mRNA PCR |
| 9 | N all+ | CCAAGGGAAAACTTGTGAGGAACAC | N PCR amplification |
| 10 | N start xho+ | GGAACACTATTATAATAACAATCCTCGAGCATGGCAAGCAGTAAGG | N amplification adding sticky ends |
| 11 | N stop xho neg | TGTAGCAAGTCCTTACTCGAGTCAAAGTTCATTTTCACCAAG | N amplification adding sticky ends |
| 12 | QX 1210 neg | ACATTCAAAATTCATGCTTAA | Diagnostic RT-PCR for QX IBV |
| 13 | QX 860+ | TGTTAATACTACTCTGGCG | Diagnostic RT-PCR for QX IBV |
| 14 | QX S1 1050+ | GGTTTAATTCCTTGTCAGTTTCTCTTACTTATGG | S1 sequencing |
| 15 | QX S1 1380+ | GCTGCTAATTTTAGTTATTTAGCAGATGGTGG | S1 sequencing |
| 16 | QX S1 270 neg | CCTGAAGAGGTGCTGTCATAGC | S1 sequencing |
| 17 | QX S1 400+ | GGCATGATTCCACGTGATCATATTCG | S1 sequencing |
| 18 | QX S1 550 neg | CAGTAGTTTTGTTGGAAGTAAAAACAAGATCACC | S1 sequencing |
| 19 | QX S1 end neg | CGAACCATCTGGTTCAATACAAAATCTGC | S1 PCR amplification |
| 20 | QX S1 start+ | CCAGTTGTGAATTTGAAGAAAGAACAAAAGACCGACTTAG | S1 PCR amplification |
| 21 | RT QX S1 neg | CATCTTTAACGAACCATCTGG | S1 RT amplification |
| 22 | S1 1380+ | GCTGCTAATTTTAGTTATTTAGCAGATGGTGG | S1 primer for mRNA PCR |
| 23 | S1 start xho+ | GGTAAATTATTGCTCGAGGATGTTGGTGAAGTCACTGTTTTTAGTG | S1 amplification adding XhoI sites |
| 24 | S1 stop xho neg | GTTACGTTTTGCTCGAGTTAACGCCTACGACGATGTGAGCTATTGG | S1 amplification adding XhoI sites |
| 25 | SX 3+ | TAATACTGGYAATTTTTCAGA | S1 sequencing |
2.2. Analysis of IBV QX genes prior to insertion into AMPV
An IBV QX virus isolated in Germany was grown in eggs, titrated in tracheal organ cultures (TOC) and stored in aliquots at -80 °C. As the genome sequence was unknown, a range of IBV genomes were aligned to identify conserved regions within, and flanking, S1 and N genes. These were used for the design of RT-PCR and sequencing primers, as detailed in Table 1. Sequencing of the S1 gene amplicon revealed two populations, one of which showed a 15 nucleotide deletion (del) (5′-UGUUUGAUUCUGAUA-3′) between bases 59 and 73.
2.3. Predictive computational comparison of S1 populations
S1 genes with and without the deletion were compared. The Protean program of the DNASTAR multiple program package (Lasergene Inc., USA) was used to estimate physicochemical properties, composition of the proteins and prediction of secondary structures. Order–disorder prediction used the VL-XT predictor on the PONDR server [24]. Prediction of immunodominant helper T-lymphocyte antigenic sites from primary sequence data was by analysis of the occurrence of amphipathic fragments using the AMPHI algorithm [25]. The predictive algorithms had been previously shown correct in more than 75% of cases.
2.4. IBV S1 and N amplification for insertion
For gene insertion, Xho I RE sites were added to S1 and N gene extremities by RT-PCR using modifying primers S1 start xho+ S1 stop xho neg, N start xho+ and N stop xho neg (Table 1).
2.5. IBV gene insertion into AMPV cDNAs
IBV genes were inserted into FLs A, AvF [12] and FL 309/04 [23] with the cassette at the MF intergenic region. For insertion of a second gene, the cloning cassette was additionally added between G and L genes. After cloning into STB12 cells, seven recombinant cDNAs were produced as detailed in Table 2 .
Table 2.
Details of the constructed recombinant cloned FL cDNAs.
| Clone name | Source virus | IBV QX insert | Intergenic regione |
|---|---|---|---|
| Adel S1 MF | Aa | Deleted S1d | MF |
| Afull S1 MF | A | Full S1 | MF |
| AvFdel S1 MF | AvFb | Deleted S1d | MF |
| AvFfull S1 MF | AvF | Full S1 | MF |
| AvFN MF | AvF | N | MF |
| AvFfull S1 MF + N GL | AvF | Full S1 + N | MF + GL |
| 309full S1 MF | 309/04c | Full S1 | MF |
Subtype A virus isolated in Germany.
Virus A with F gene modifications increasing induced protection in turkeys.
Field virus deriving from an subtype A type registered vaccine.
IBV QX S1 containing a 15 base deletion between nucleotides 59 to 73.
Location in cloned AMPV of the inserted gene(s).
2.6. Recovery of virus
Recombinant viruses were rescued from FLs [9] then passaged in Vero cells to produce sufficient virus for protection studies. Viruses were titrated in 48 well plates containing Vero cell monolayers. Cytopathic effect end points were observed using low power microscopy and titres were calculated [26]. Virus stocks of 1.5 ml aliquots were stored at −80 °C.
2.7. S1 and N gene messenger RNA RT-PCRs
To verify the transcription of inserted S1 and N genes in Vero cell grown virus, a previously reported protocol [10] was used, except that primers within those genes were S1 1380+ and N 920+ for S1 and N genes respectively (Table 1).
2.8. Expression of inserted genes
S1 and N protein expression were assessed using immunofluorescence (IF) on AMPV recombinant infected Vero monolayers, using a polyclonal chicken antiserum (GD) anti QX for S1 expression and a monoclonal mouse antibody (Biozol) for N gene expression. Appropriate FITC conjugated antibodies were used to visualize specific S1/N proteins (AMR).
2.9. Chicken experiment 1
Approximately 70 one-day-old SPF chickens were divided into seven groups, each containing ten animals. In groups one to four, birds were inoculated by eyedrop with 4 log10 TCID50 Afull S1 MF, AvFfull S1 MF, Adel S1 MF and AvFdel S1 MF respectively. The AMPV control group was inoculated with AvF. At 21 days post vaccination (dpv), all birds, and half the unvaccinated control (C+) were challenged with 4 log10 TCID50 QX IBV strain by eyedrop, while the other controls remained unvaccinated (C−). For sampling, of tracheas and kidneys, half the chickens per group were humanely killed at 4 days post challenge (dpc) and the remainder at 6 dpc.
2.10. Chicken experiment 2
Approximately 60 one-day-old SPF chickens were divided into six groups of ten birds, of which four were inoculated with 4 log10 TCID50 of viruses 309full S1 MF, AvFfull S1 MF + N GL, AvFN MF and AvFfull S1 MF virus by eyedrop. The remaining groups acted as controls. At 21 dpv, all vaccinated birds and half the unvaccinated controls (C+) were challenged with 4 log10 TCID50 of IBV QX by eyedrop, while the other controls remained unvaccinated (C−). In each group, five birds were humanely killed at 4 dpc and five at 6 dpc and tracheas and kidneys were collected.
2.11. Serology
Chickens from each group were bled at 18 dpv for IBV and AMPV serology. Sera from birds receiving S1 recombinant AMPVs were tested using an IBV QX HI test, while those receiving either recombinant containing the N gene were tested by IBV HI and ELISA (Biochek, AMR). AMPV ELISA (IDEXX, AMR).
2.12. Assessment of replication of recombinants by AMPV real time RT-PCR
Ten choanal swabs were collected from all groups at 3, 6 and 9 days post vaccination (dpv) for AMPV real time RT-PCR [27] to assess recombinant replication.
2.13. Determination of tracheal cilial activity
At 4 and 6 dpc in both chicken experiments, tracheas were collected and cut into 1 mm transverse sections. For each trachea, ten sections were collected (three upper, four middle and three lower) and examined under low power microscopy to determine activity of cilia. Individual sections were classified as either containing beating cilia or beating being entirely absent.
2.14. Statistical analysis
Statistical analysis of cilial motility was performed using the Chi-square test. A p value < 0.05 was considered statistically significant.
2.15. Clinical signs
Birds were examined daily for the presence of nasal exudate and generally for overall health.
3. Results
3.1. Recombinant AMPV GFP construction
The GFP gene was added to modified FL AMPV copies and viruses were recovered. Maximum TCID50 titres per ml of Vero cell lysate, following three Vero cells passages, were low when the inserted gene was positioned at a gene junction close to the virus leader. Hence with GFP placed between N and P genes, the titre was 2.1 while in all other positions it exceeded 4.0. At the MF position it was 5.0. For all constructs, strong fluorescence was observed when infected Vero cells were viewed by UV microscopy for all constructs as illustrated for recombinant GFP MF (Fig. 2 ).
Fig. 2.
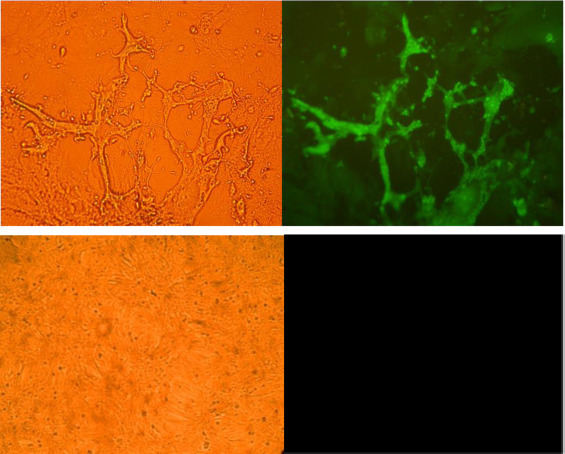
TOP Vero cell monolayer infected with virus expressing GFP between MF viewed under white (left) and ultraviolet illumination (right) BELOW Uninfected Vero cell monolayer under white (left) and ultraviolet illumination (right).
3.2. Computational analysis
Protean suite software analysis predicted S1 proteins to share the same physicochemical properties and PONDR predicted no differences to the disordered region. The Protean suite predicted the proportion of alpha helix to remain constant while a difference of beta pleated sheets was evident. The AMPHI program predicted a T cell epitope present only in the complete S1 protein, at amino acid positions 15-19. However S1 containing the deletion possessed two additional predicted T cell epitope regions (amino acids 264-268 and 383-388).
3.3. IBV recombinant AMPV construction
Virus was rescued from AMPV FL cDNAs containing IBV genes as confirmed by cytopathic effect typical of AMPV on Vero cell monolayers. Viruses were sequenced to after three passages. RT-PCR of virus mRNAs confirmed transcription of the inserted IBV genes (data not shown). Expression of IBV proteins was confirmed in all recombinant viruses by IF (Fig. 3 ).
Fig. 3.

Vero cell monolayers infected with AMPV recombinant viruses viewed by UV microscopy. Viruses 1 to 3 used IBV N monoclonal serum and 4 to 10 used IBV polyclonal chicken serum.
3.4. Serology
IBV and AMPV antibody responses were not generally detectable (Table 3 ). For IBV in experiment 1, a single bird in group AvFdel S1 MF and two birds in group AvFfull S1 MF had detectably seroconverted by HI. For AMPV ELISA serology, two seroconversions were detected in the AvF control group (experiment 1) and three in the 309full S1 MF group (experiment 2).
Table 3.
Chickens experiments 1 and 2: post vaccination virus detection by real time RT-PCR, pre challenge serology and cilial activity post challenge.
| Groups | AMPV real time RT PCR (dpv)a | Serology (18 dpv)a |
% TOC beating (dpc)b | ||||||
|---|---|---|---|---|---|---|---|---|---|
| AMPV |
IBV |
||||||||
| Day 3 | Day 6 | Day 9 | ELISA | HI | ELISA | Day 4 | Day 6 | ||
| Experiment 1 | Adel S1 MF | 4/10 | 0/10 | 0/10 | 0/10 | 0/10 | n.d.c | 0 | 20 |
| Afull S1 MF | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | n.d.c | 0 | 24 | |
| AvFdel S1 MF | 0/10 | 0/10 | 1/10 | 0/10 | 1/10 | n.d.c | 0 | 0 | |
| AvFfull S1 MF | 0/10 | 0/10 | 0/10 | 0/10 | 2/10 | n.d.c | 0 | 0 | |
| AvF | 0/10 | 0/10 | 5/10 | 2/10 | 0/10 | n.d.c | 0 | 0 | |
| C+ | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | n.d.c | 0 | 0 | |
| C− | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | n.d.c | 100 | 98 | |
| Experiment 2 | AvFN MF | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0 | 32 |
| AvFfull S1 MF + N GL | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0 | 40 | |
| 309full S1 MF | 6/10 | 8/10 | 6/10 | 3/10 | 0/10 | 0/10 | 0 | 8 | |
| AvFfull S1 MF | 0/10 | 1/10 | 1/10 | 0/10 | 0/10 | 0/10 | 0 | 2 | |
| C+ | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0 | 4 | |
| C− | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 100 | 100 | |
50 rings prepared from 5 birds from each group, each sampling day.
Days post vaccination.
Days post challenge.
Not done.
3.5. AMPV real time RT-PCR
Except for 309full S1 MF, real time RT-PCR showed minimal AMPV recombinant replication (Table 3).
3.6. Tracheal motility following challenge
At 4 dpc, sections from all birds challenged with IBV were ciliostatic. At 6 dpc, some sections from birds previously inoculated with AMPV QX recombinants showed cilial motility, with those birds given AvFfull S1 MF + N GL showing most, followed by AvFN MF and with the least for AvF viruses expressing only the S1 gene. In all cases the distribution of beating rings within any group was even. No differences were observed between recombinant AMPVs expressing the full and deleted S1. Comparing AMPV vectors with identically positioned inserts, A led to greater cilial recovery than either 309/04 or AvF. See Table 3 for details.
3.7. Statistical analysis
Significantly increased cilial activity, calculated by comparing each group to the respective positive control, was found for birds vaccinated with Afull S1 MF (p = 0.0002), Adel S1 MF (p = 0.0008), AvFfull S1 + N GL (p = 0.00001) and AvFN MF (p = 0.0002) and analysis between these groups did not reveal any significant differences.
3.8. Clinical signs and gross lesions
No signs were detected after vaccination. In experiment 1, clinical signs were observed in three birds at 6 dpc. One positive control bird and two AvF control birds were humanly killed after displaying lethargy, ruffled feathers and reduced response to external stimuli. Gross kidney lesions, typical of QX IBV infection, were detected at post-mortem examination in the same birds. No signs or lesions were seen in experiment 2.
4. Discussion
When IBV MF recombinants were used to inoculate one-day-old chickens, many induced IBV protection of the trachea, yet serology and real time RT PCR virus detection indicated poor tracheal replication. Surprisingly, recombinants replicating least induced most protection whereby recombinants based on virus A protected best while virus 309/04 induced no detectable protection. Despite computer analysis predicting T cell epitopes differences concerning the S1 15 nucleotide deletion, no protection differences were observed.
The primary site of AMPV and IBV replication in chickens is the upper respiratory tract, hence an AMPV based IBV recombinant might be predicted to be ideal for inducing IBV protection. Conventional wisdom suggests that the minimal levels of upper respiratory tract replication detected in our study, led to the observed protection. Therefore any AMPV recombinant replicating better might yield greater protection. Growing worldwide commercial field evidence is indicating that subtype B AMPV better infects commercial chickens than subtype A. If a subtype B RG system becomes available, protection afforded by any resultant IBV recombinants will be keenly compared to the current study, which counter-intuitively suggests that recombinant AMPVs inducing the best protection replicate least well. If more protection inducing recombinants are found not to appreciably replicate in the respiratory tract or produce generalised seroconversion, it will become necessary to investigate whether replication might occur at another site or alternatively protection may result from a yet unrecognized mechanism. There is already some evidence that, AMPV replication in the respiratory tract of turkeys does not imply induction of AMPV protection [12], protection following live vaccination does not require initial replication in the trachea [28] and AMPV vaccination can lead to apparent protection without AMPV seroconversion [29], [30].
For the first time, AMPV recombinants are reported carrying foreign viral genes. Previously AMPVs were shown highly stable both in cell culture and during natural passage [20] as has also been reported for other members of the Mononegavirales such as vesicular stomatitis and rabies viruses [31], [32]. This contrasts with single strand positive viruses such as IBV and feline calicivirus where minimal passage readily results in consensus sequence mutations [13], [33]. Furthermore, the recombinant AMPV genome carrying more than 3000 extra nucleotides (IBV S1 and N genes) was stable with respect to functionally irrelevant inserted genes, and their presence did not appreciably reduce virus viability, if distanced beyond the phosphoprotein gene.
Our study suggests that a range of AMPV vectored candidate vaccines could be readily prepared. For IBV, this is in marked contrast to conventional attenuation where more than 100 egg passages is typically required. Such AMPV recombinants would have greater genetic stability in two key respects. Firstly instability on simple passage implies that any live vaccine will be genetically heterogeneous. Of greater significance is the ability of IBV live vaccines to recombine with other IBV genotypes during co-infection, via homologous recombination, thus potentially leading to new field genotypes. In contrast, AMPV has been shown to be stable with respect to multiple passage while the absence (or extremely low frequency) of homologous recombination avoids recombinant generation.
The nature of the protective immune response to IBV is not well understood [13]. While virus AvF containing N gene alone or N + S1 genes together protected tracheas better than AvF containing the S1 gene alone, the expression of the inserted genes would need to be quantified, before conclusions about the relative contribution of each gene to protection, could be drawn. Previous studies indicate that the internal N protein is able to stimulate a cell mediated immune response (CMI) [18] whereas the exposed S1 protein would be more likely to stimulate antibody production [34], [35], [36], hence our study adds weight to the notion that both a CMI and antibody response are important in protection.
In conclusion, we report for the first time that AMPV is able to accept genes from, express proteins of, and confer protection against, foreign viruses. Those recombinant AMPV-IBV viruses are genetically stable and able to incorporate inserted genes totalling at least 3000 nucleotides; though the upper limit is yet to be established. It is likely that further developments will lead to flexible vaccines of greater efficacy as well as providing a better understanding of the essential components for induction of effective protection against IBV as well as other avian viruses.
Conflict of interest
There is no conflict of interest.
References
- 1.Bell I.G., Alexander D.J. Failure to detect antibody to turkey rhinotracheitis virus in Australian poultry flocks. Aust Vet J. 1990;67(June, 6):232–233. doi: 10.1111/j.1751-0813.1990.tb07772.x. [DOI] [PubMed] [Google Scholar]
- 2.Cook J.K. Avian rhinotracheitis. Rev Sci Tech. 2000;19(2):602–613. doi: 10.20506/rst.19.2.1233. [DOI] [PubMed] [Google Scholar]
- 3.Pringle C.R. Virus taxonomy – San Diego 1998. Arch Virol. 1998;143(7):1449–1459. doi: 10.1007/s007050050389. [DOI] [PubMed] [Google Scholar]
- 4.Bayon-Auboyer M.H., Arnauld C., Toquin D., Eterradossi N. Nucleotide sequences of the F, L and G protein genes of two non-A/non-B avian pneumoviruses (APV) reveal a novel APV subgroup. J Gen Virol. 2000;81(November, Pt 11):2723–2733. doi: 10.1099/0022-1317-81-11-2723. [DOI] [PubMed] [Google Scholar]
- 5.Juhasz K., Easton A.J. Extensive sequence variation in the attachment (G) protein gene of avian pneumovirus: evidence for two distinct subgroups. J Gen Virol. 1994;75(Pt 11):2873–2880. doi: 10.1099/0022-1317-75-11-2873. [DOI] [PubMed] [Google Scholar]
- 6.Seal B.S. Avian pneumovirus and emergence of a new type in the United States of America. Anim Health Res Rev. 2000;1:67–72. doi: 10.1017/s1466252300000062. [DOI] [PubMed] [Google Scholar]
- 7.Easton A.J., Domachowske J.B., Rosenberg H.F. Animal pneumoviruses: molecular genetics and pathogenesis. Clin Microbiol Rev. 2004;17(April, 2):390–412. doi: 10.1128/CMR.17.2.390-412.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Govindarajan D., Buchholz U.J., Samal S.K. Recovery of avian metapneumovirus subgroup C from cDNA: cross-recognition of avian and human metapneumovirus support proteins. J Virol. 2006;80(June, 12):5790–5797. doi: 10.1128/JVI.00138-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Naylor C.J., Brown P.A., Edworthy N., Ling R., Jones R.C., Savage C.E. Development of a reverse-genetics system for Avian pneumovirus demonstrates that the small hydrophobic (SH) and attachment (G) genes are not essential for virus viability. J Gen Virol. 2004;85(November):3219–3227. doi: 10.1099/vir.0.80229-0. [DOI] [PubMed] [Google Scholar]
- 10.Brown P.A., Lupini C., Catelli E., Clubbe J., Ricchizzi E., Naylor C.J. A single polymerase (L) mutation in avian metapneumovirus increased virulence and partially maintained virus viability at an elevated temperature. J Gen Virol. 2011;92(February, Pt 2):346–354. doi: 10.1099/vir.0.026740-0. [DOI] [PubMed] [Google Scholar]
- 11.Ling R., Sinkovic S., Toquin D., Guionie O., Eterradossi N., Easton A.J. Deletion of the SH gene from avian metapneumovirus has a greater impact on virus production and immunogenicity in turkeys than deletion of the G gene or M2-2 open reading frame. J Gen Virol. 2008;89(February, Pt 2):525–533. doi: 10.1099/vir.0.83309-0. [DOI] [PubMed] [Google Scholar]
- 12.Naylor C.J., Lupini C., Brown P.A. Charged amino acids in the AMPV fusion protein have more influence on induced protection than deletion of the SH or G genes. Vaccine. 2010;28(September, 41):6800–6807. doi: 10.1016/j.vaccine.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 13.Cavanagh D. Coronavirus avian infectious bronchitis virus. Vet Res. 2007;38(March–April, 2):281–297. doi: 10.1051/vetres:2006055. [DOI] [PubMed] [Google Scholar]
- 14.Worthington K.J., Currie R.J., Jones R.C. A reverse transcriptase-polymerase chain reaction survey of infectious bronchitis virus genotypes in Western Europe from 2002 to 2006. Avian Pathol. 2008;37(June, 3):247–257. doi: 10.1080/03079450801986529. [DOI] [PubMed] [Google Scholar]
- 15.Terregino C., Toffan A., Beato M.S., De Nardi R., Vascellari M., Meini A. Pathogenicity of a QX strain of infectious bronchitis virus in specific pathogen free and commercial broiler chickens, and evaluation of protection induced by a vaccination programme based on the Ma5 and 4/91 serotypes. Avian Pathol. 2008;37(October, 5):487–493. doi: 10.1080/03079450802356938. [DOI] [PubMed] [Google Scholar]
- 16.Song C.S., Lee Y.J., Lee C.W., Sung H.W., Kim J.H., Mo I.P. Induction of protective immunity in chickens vaccinated with infectious bronchitis virus S1 glycoprotein expressed by a recombinant baculovirus. J Gen Virol. 1998;79(April):719–723. doi: 10.1099/0022-1317-79-4-719. (Pt 4) [DOI] [PubMed] [Google Scholar]
- 17.Yu L., Liu W., Schnitzlein W.M., Tripathy D.N., Kwang J. Study of protection by recombinant fowl poxvirus expressing C-terminal nucleocapsid protein of infectious bronchitis virus against challenge. Avian Dis. 2001;45(April–June (2)):340–348. [PubMed] [Google Scholar]
- 18.Seo S.H., Wang L., Smith R., Collisson E.W. The carboxyl-terminal 120-residue polypeptide of infectious bronchitis virus nucleocapsid induces cytotoxic T lymphocytes and protects chickens from acute infection. J Virol. 1997;71(October, 10):7889–7894. doi: 10.1128/jvi.71.10.7889-7894.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu D., Han Z., Xu J., Shao Y., Li H., Kong X. A novel B-cell epitope of avian infectious bronchitis virus N protein. Viral Immunol. 2010;23(April, 2):189–199. doi: 10.1089/vim.2009.0094. [DOI] [PubMed] [Google Scholar]
- 20.Cubillos A., Ulloa J., Cubillos V., Cook J.K.A. Characterization of strains of infectious-Bronchitis Virus isolated in Chile. Avian Pathol. 1991;20(1):85–99. doi: 10.1080/03079459108418744. [DOI] [PubMed] [Google Scholar]
- 21.Cavanagh D., Ellis M.M., Cook J.K.A. Relationship between sequence variation in the S1 spike protein of infectious bronchitis virus and the extent of cross-protection in vivo. Avian Pathol. 1997;26(March 1):63–74. doi: 10.1080/03079459708419194. [DOI] [PubMed] [Google Scholar]
- 22.Frangipani J.A., Jungback C. Immunigenicity testing of vaccines against Avian Bronchitis Virus – comparison of several methods to demonstrate experimental infection. In: Heffels-Redman U., Kaleta E.F., editors. International Symposium on avian Corona-and Pneumovirus Infections; 2004; Rauischholzhausen: VVB Laufersweiler Verlag; 2004. pp. 202–212. [Google Scholar]
- 23.Catelli E., Cecchinato M., Savage C.E., Jones R.C., Naylor C.J. Demonstration of loss of attenuation and extended field persistence of a live avian metapneumovirus vaccine. Vaccine. 2006;24(July, 14):6476–6482. doi: 10.1016/j.vaccine.2006.06.076. [DOI] [PubMed] [Google Scholar]
- 24.Romero P., Obradovic R Z., Dunker A.K. Sequence data analysis for long disordered regions prediction in the Calcineurin family. Genome Inform Ser Workshop Genome Inform. 1997;8:110–124. [PubMed] [Google Scholar]
- 25.Margalit H., Spouge J.L., Cornette J.L., Cease K.B., Delisi C., Berzofsky J.A. Prediction of immunodominant helper T cell antigenic sites from the primary sequence. J Immunol. 1987;138(April, 7):2213–2229. [PubMed] [Google Scholar]
- 26.Reed L.J., Muench H. A simple method of estimating fifty percent end points. Am J Public Health N. 1938;27:493–497. [Google Scholar]
- 27.Cecchinato M, Lupini C, Munoz Pogoreltseva OS, Listorti V, Mondin A, Drigo M, et al. Development of a real time RT-PCR assay for the simultaneous identification, quantitation and differentiation of Avian Metapneuomovirus subtype A and B. Avian Pathol, http://dx.doi.org/10.1080/03079457.2013.788130, in press. [DOI] [PubMed]
- 28.Naylor C.J., Jones R.C. Demonstration of a virulent subpopulation in a prototype live attenuated turkey rhinotracheitis vaccine. Vaccine. 1994;12(October, 13):1225–1230. doi: 10.1016/0264-410x(94)90248-8. [DOI] [PubMed] [Google Scholar]
- 29.Cook J.K.A., Ellis M.M., Dolby C.A., Holmes H.C., Finney P.M., Huggins M.B. A live attenuated turkey rhinotracheitis virus vaccine I. Stability of the attenuated strain. Avian Pathol. 1989;18:511–522. doi: 10.1080/03079458908418623. [DOI] [PubMed] [Google Scholar]
- 30.Williams R.A., Savage C.E., Jones R.C. Further studies on the development of a live attenuated vaccine against turkey rhinotracheitis. Avian Pathol. 1991;20:585–596. doi: 10.1080/03079459108418798. [DOI] [PubMed] [Google Scholar]
- 31.Schnell M.J., Buonocore L., Whitt M.A., Rose J.K. The minimal conserved transcription stop-start signal promotes stable expression of a foreign gene in vesicular stomatitis virus. J Virol. 1996;70(April, 4):2318–2323. doi: 10.1128/jvi.70.4.2318-2323.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mebatsion T., Schnell M.J., Cox J.H., Finke S., Conzelmann K.K. Highly stable expression of a foreign gene from rabies virus vectors. Proc Natl Acad Sci USA. 1996;93(July, 14):7310–7314. doi: 10.1073/pnas.93.14.7310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Radford A.D., Dawson S., Coyne K.P., Porter C.J., Gaskell R.M. The challenge for the next generation of feline calicivirus vaccines. Vet Microbiol. 2006;117(October, 1):14–18. doi: 10.1016/j.vetmic.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 34.Cavanagh D., Davis P.J., Darbyshire J.H., Peters R.W. Coronavirus IBV: virus retaining spike glycopolypeptide S2 but not S1 is unable to induce virus-neutralizing or haemagglutination-inhibiting antibody, or induce chicken tracheal protection. J Gen Virol. 1986;67(July):1435–1442. doi: 10.1099/0022-1317-67-7-1435. (Pt 7) [DOI] [PubMed] [Google Scholar]
- 35.Moore K.M., Jackwood M.W., Hilt D.A. Identification of amino acids involved in a serotype and neutralization specific epitope within the s1 subunit of avian infectious bronchitis virus. Arch Virol. 1997;142(11):2249–2256. doi: 10.1007/s007050050239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mockett A.P., Cavanagh D., Brown T.D. Monoclonal antibodies to the S1 spike and membrane proteins of avian infectious bronchitis coronavirus strain Massachusetts M41. J Gen Virol. 1984;65(December):2281–2286. doi: 10.1099/0022-1317-65-12-2281. Pt 12. [DOI] [PubMed] [Google Scholar]


