Graphical abstract

Keywords: HCMV, Uracil derivatives, Antiviral, Nonnucleoside, Nucleobase
Abstract
HCMV infection represents a life-threatening condition for immunocompromised patients and newborn infants and novel anti-HCMV agents are clearly needed. In this regard, a series of 1-[ω-(phenoxy)alkyl]uracil derivatives were synthesized and examined for antiviral properties. Compounds 17, 20, 24 and 28 were found to exhibit highly specific and promising inhibitory activity against HCMV replication in HEL cell cultures with EC50 values within 5.5–12 μM range. Further studies should be undertaken to elucidate the mechanism of action of these compounds and the structure–activity relationship for the linker region.
1. Introduction
Human cytomegalovirus (HCMV) belongs to the viral family known as Herpesviridae, and is also known as human herpesvirus-5 (HHV-5). Within Herpesviridae, HCMV belongs to the Betaherpesvirinae subfamily.1 One characteristic feature of the herpesviruses, including HCMV, is the ability to remain latent within the body after infection.2 Latent HCMV is present in approximately 90% of adults aged over 80 in the U.S.,3 and typically goes unnoticed in healthy people, but can be life-threatening for the immunocompromised person. In this regard, HIV-infected persons,4, 5 organ transplant recipients,6 or newborn infants are all at high risk of infection. Transplacental HCMV transmission can lead to congenital abnormalities and stillbirth, thus represents one of the most common viral causes of birth defects.7 HCMV infection may also cause mucoepidermoid carcinoma and possibly other malignancies.8 Moreover, a number of studies have revealed that HCMV is associated with autoimmune diseases,9 atherosclerosis,10 coronary restenosis11, 12 and increased risk of diabetes.13, 14
To date only three anti-HCMV agents, ganciclovir,15 cidofovir,16 and foscarnet,17 have been approved for clinical use. They exhibit their effects by inhibiting the activity of the HCMV polymerase, thus reducing viral replication in patients with recognized HCMV infection symptoms. The use of these drugs however has been severely limited by their toxicity.18 In addition, due to their inherent poor oral bioavailability, they must be administered intravenously to reach appropriate therapeutic levels. The exception to this limitation is valganciclovir, the orally administered prodrug for ganciclovir.19 Unfortunately, as is typical for many nucleoside drugs, the development of drug-resistant viral strains has emerged.20, 21, 22 Thus, there is an urgent need for new and more effective anti-HCMV agents with improved activity and pharmacokinetic profiles.
Recently a new class of nonnucleoside HCMV polymerase inhibitors has attracted interest.23 As a result of the BioChem Pharm screening campaign, a series of 1,6-naphthiridine-based HCMV inhibitors were identified. The highest activity was exhibited by compound 1 (Fig. 1 ) which possesses an ortho-substituted benzyl moiety.24 Subsequent design modifications led to the macrocyclic analogues represented by 2.25 These compounds exhibited potent activity against HCMV and other herpesviruses, however were accompanied by significant cytotoxicity. Potent anti-HCMV and anti-VZV activity was also noted for other heterocyclic-based inhibitors including imidazo[1,2-a]pyridine derivatives 3 26, 27, 28 and benzothiadiazines 4.29, 30 Other examples of broad-spectrum herpesvirus inhibitors are represented by derivatives of fused heterocyclic systems including the quinolones,31 thieno[2,3-b]-,32 thieno[3,2-b]-,33 furo[2,3-b]pyridines34 (5) and pyrrolo[3,2,1-ij]quinolones35 (6), all developed by Pfizer (Fig. 1). It should be noted that all of these compounds possess a common structural feature: an N-heterocycle linked to a benzene ring.
Figure 1.

HCMV inhibitors.
Previously we have reported the synthesis and antiviral properties for a number of different classes of nucleobase derivatives. Specifically, the anti-HIV and anti-HCMV activity for a series of 9-[2-(phenoxy)ethyl]- and 9-[2-(benzyloxy)ethyl]-derivatives of adenine have been described.36 The 1-{[2-(phenoxy)ethoxy]methyl}uracils were found to be moderately active against HIV,37 while 1-[2-(2-benzoylphenoxy)ethyl]-derivatives exhibited strong inhibitory properties.38 In addition, several derivatives of 3-benzyl-1-(cinnamyl)uracil demonstrated significant activity against HIV and HCMV replication in cell culture.39 As a result, these observations provided strong impetus to further explore the antiviral activity spectrum of 1-[ω-(phenoxy)alkyl]uracils, as well as to investigate the structural requirements for the linker between the aromatic moieties, since this scaffold is common to many known inhibitors of HCMV polymerase.
2. Results and discussion
2.1. Chemistry
A series of novel uracil derivatives was synthesized in a similar manner as previously described by our group.38, 40 Condensation of equimolar amounts of 2,4-bis(trimethylsilyl)pyrimidines 7 with bromides 8 was performed at 160–170 °C in the absence of solvent to afford target compounds 9–28 in 70–88% yield (Scheme 1 ).
Scheme 1.

General approach for the synthesis of the target compounds.
Compound 29 was obtained in an 81% yield by alkaline hydrolysis of 18 in refluxing water–ethanol for 8 h (Scheme 2 ), while reduction of compound 21 was accomplished with SnCl2 in mild acid-free conditions41, 42 to produce the amino-substituted compound 30 in 59% yield.
Scheme 2.
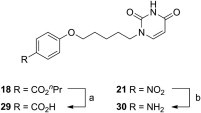
Reagents and conditions: (a) aq. NaOH, EtOH, reflux, 8 h; (b) SnCl2·H2O, EtOH, reflux, 3 h.
2.2. Antiviral activity
The anti-HCMV properties of target compounds 9–30 were evaluated against HCMV (AD-169 and Davis strains) in HEL cell cultures and the results are shown in Table 1 . Most of the compounds proved to be inhibitory against HCMV. In examining the structure activity relationship for the compounds, it appears that the activity is strongly dependent upon the substituent at the para-position of the benzene core. Polar groups proved unfavorable and resulted in a loss of activity (compounds 18, 21, 29). Activity for alkyl substituted compounds increased with the size of the substituent: EC50 for H (9) = Me (12) < i-Pr (14) < t-Bu (15), however, introduction of a bulky phenyl group led to poor activity for 16, thus there appears to be a steric limit. The 4-cyano- (17) and 4-bromo- (20) substituted compounds were found to exhibit the highest activity, which was comparable to ganciclovir. Interestingly, the 4-chloro-substituted compound 19 was essentially inactive. One possible rationale for these observations could be complementary polar interactions between the halogen- or cyano-substituents and an appropriate protein functionality, for example, a carbonyl group, since the oxygen-containing compound 29 was inactive. This assumption is partially supported by the fact that reduction of NO2-group in inactive compound 21 led to 4-amino substituted compound 30 which exhibited slight anti-HCMV activity.
Table 1.

| Compd | R1 | R2 | n | mp (°C) | Yield (%) | EC50 (μМ)a |
Cytotoxicity (μМ) |
||
|---|---|---|---|---|---|---|---|---|---|
| AD-169 | Davis | Cell morphology (MCC)b | Cell growth (CC50)c | ||||||
| 9 | H | H | 3 | 151–153 | 88 | >100 | >100 | >100 | >100 |
| 10 | H | 2-Me | 3 | 147–149 | 72 | >100 | >100 | >100 | >100 |
| 11 | H | 3-Me | 3 | 101–103 | 75 | 45.0 | 55.0 | >100 | >100 |
| 12 | H | 4-Me | 3 | 146–147 | 87 | >20 | >20 | 100 | >100 |
| 13 | H | 3,5-Me2 | 3 | 96–98 | 85 | >100 | >100 | >100 | >100 |
| 14 | H | 4-iPr | 3 | 139–140 | 78 | 25.0 | 15.0 | 100 | >100 |
| 15 | H | 4-tBu | 3 | 125–127 | 77 | 14.0 | 12.0 | 100 | 40 |
| 16 | H | 4-Ph | 3 | 174–175 | 76 | >20 | 54 | 100 | ND |
| 17 | H | 4-CN | 3 | 185–186 | 84 | 8.9 | 5.5 | 100 | 100 |
| 18 | H | 4-CO2nPr | 3 | 131–132 | 76 | 45.0 | 45.0 | ⩾100 | >100 |
| 19 | H | 4-Cl | 3 | 168–169 | 84 | >100 | >100 | >100 | ND |
| 20 | H | 4-Br | 3 | 125–127 | 76 | 9.4 | 12.0 | 100 | >100 |
| 21 | H | 4-NO2 | 3 | 197–199 | 78 | >4 | >4 | 20 | ND |
| 22 | Br | 4-Br | 3 | 160–162 | 77 | 36.0 | 67.0 | >100 | >100 |
| 23 | I | 4-Br | 3 | 166–168 | 78 | 13.0 | 20.0 | ⩾100 | >100 |
| 24 | Me | 4-Br | 3 | 169–171 | 82 | 8.9 | 9.0 | 100 | >100 |
| 25 | H | 4-Br | 1 | 179–181 | 79 | >100 | >100 | >100 | ND |
| 26 | H | 4-Br | 2 | 143–144 | 80 | >20 | >20 | 100 | ND |
| 27 | H | 4-Br | 4 | 121–122 | 70 | >4 | >4 | 20 | ND |
| 28 | H | 4-Br | 6 | 145–147 | 76 | 12.0 | 8.9 | ⩾100 | >100 |
| 29 | H | 4-CO2H | 3 | 225–227 | 81 | >100 | >100 | >100 | ND |
| 30 | H | 4-NH2 | 3 | 190–192 | 59 | 55.0 | 55.0 | >100 | >100 |
| Ganciclovir | 7.0 | 8.3 | 394 | 200 | |||||
| Cidofovir | 1.3 | 1.1 | 317 | 161 | |||||
Effective concentration required to reduce virus plaque formation by 50%. Virus input was 100 plaque forming units (PFU).
Minimum cytotoxic concentration that causes a microscopically detectable alteration of cell morphology.
Cytotoxic concentration required to reduce cell growth by 50%.
Substitutions at position five of the uracil ring were also examined. In that regard, while thymine analogue 24 was slightly more active than uracil derivative 20, for halogen-substituted 22 and 23 activity was notably diminished. As a result, this modification was not investigated further.
Initially, 20 was selected to investigate optimal length of the linker chain between the uracil and the benzene moieties. Compounds 25–27, containing three, four and six methylenes, respectively, were found to be inactive against HCMV at subtoxic concentrations. In contrast, compound 28, which has eight methylene units, demonstrated the same level of activity as 20.
In addition, target compounds 9–30 were screened against a large panel of other DNA and RNA viruses. No activity was observed for HSV-1, HSV-2, VZV, Vaccinia virus, Vesicular stomatitis virus, Coxsackie virus B4, Respiratory syncytial virus, Influenza A virus H1N1 subtype, Influenza A virus H3N2 subtype, Influenza B virus, Parainfluenza-3 virus, Reovirus-1, Sindbis virus, Punta Toro virus, Feline Corona Virus, HIV-1 and HIV-2. The only exception was noted for compound 13, which demonstrated a 50% reduction of HIV-1-induced cytopathogenesis at 24 μM concentration with a 50% cytotoxic concentration of 154 μM.
3. Conclusions
A series of novel 1-[ω-(phenoxy)alkyl]uracil derivatives was synthesized and shown to have promising and highly specific inhibitory properties against HCMV replication in cell culture. Notably, the substitution pattern in the benzene core appears to be of importance for activity. The EC50 values for the most active compounds in the series (compounds 17, 20, 24 and 28) lie within the range of 5.5–12.0 μM and are accompanied with low cytotoxicity (CC50 ⩾ 100 μM). Additional efforts are currently underway to elucidate the mechanism of action of these compounds and further explore the structure-activity relationship for the linker region.
4. Materials and methods
4.1. General
All reagents were obtained at highest grade available from Sigma and Acros Organics and used without further purification unless otherwise noted. Anhydrous DMF and isopropanol were purchased from Sigma–Aldrich Co. Anhydrous acetone, 1,2-dichloroethane, and ethyl acetate were obtained by distillation over P2O5. NMR spectra were registered on a Bruker Avance 400 spectrometer (400 MHz for 1H and 100 MHz for 13C) in DMSO-d 6 with tetramethylsilane as an internal standard. Data are reported in the following order: multiplicity (br, broad; s, singlet; d, doublet; dd, doublet of doublets; t, triplet; m, multiplet; q, quartet; qu, quintet). TLC was performed on Merck TLC Silica gel 60 F254 plates eluted with ethyl acetate or chloroform/MeOH (10:1) and developed with UV-lamp VL-6.LC (France). Acros Organics (Belgium) silica gel (Kieselgur 60–200 μm, 60A) was used for column chromatography. Melting points were determined in glass capillaries on a Mel-Temp 3.0 (Laboratory Devices Inc., U.S.). Yields refer to spectroscopically (1H and 13C NMR) homogeneous materials. High resolution mass spectra were measured on Bruker micrOTOF II instruments using electrospray ionization (HRESIMS). The measurements were done in a positive ion mode (interface capillary voltage −4500 V) in a mass range from m/z 50–3000 Da; external or internal calibration was done with ESI Tuning Mix™ (Agilent Technologies). A syringe injection was used for solutions in acetonitrile (flow rate 3 μl/min). Nitrogen was applied as a dry gas; interface temperature was set at 180 °C. Bromides 8 were synthesized as per known procedures.43, 44
4.2. Synthesis
4.2.1. General procedure for the synthesis of 1-[5-(phenoxy)-pentyl]uracils (9–24)
A mixture of uracil, 5-bromouracil, 5-iodouracil or thymine (5.60 mmol) and ammonium chloride (0.3 g, 5.60 mmol) in HMDS (15 mL) was refluxed for 10 h with exclusion of moisture until a clear solution was obtained. Excess silylating reagent was removed under vacuum. To the residual clear oil of 2,4-bis(trimethylsilyloxy)pyrimidine 7, an equimolar amount of bromide 8 was added, the reaction mixture heated at 160–170 °C for 1 h, then the resulting amber oil was dissolved in 40 mL of EtOAc, treated with 10 mL of i-PrOH and evaporated. The residue was dissolved in 10 mL of CHCl3 and purified by column chromatography, eluting with CHCl3/MeOH, 10:1. Subsequent recrystallization from i-PrOH/DMF mixture provided the desired products.
4.2.1.1. 1-[5-(Phenoxy)pentyl]uracil (9)
Yield 88%, mp 151–153 °C, R f 0.53 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.39 (2H, qu, J = 5.3 Hz, CH2), 1.63 (2H, qu, J = 7.2 Hz, CH2), 1.72 (2H, qu, J = 7.2 Hz, CH2), 3.67 (2H, t, J = 7.2 Hz, NCH2), 3.93 (2H, t, J = 6.5 Hz, OCH2), 5.55 (1H, dd, J = 7.7 and 2.1 Hz, H-5), 6.89–6.92 (3H, m, aromatic H), 7.26 (2H, t, J = 8 Hz, H-3′, H-5′), 7.64 (1H, d, J = 7.8 Hz, H-6), 11.25 (1H, s, NH). 13C NMR (DMSO-d 6): δ 22.9, 28.6, 28.7, 47.8, 67.5, 101.2, 114.8, 120.8, 129.9, 146.2, 151.4, 159.3, 164.3. HRESIMS: found m/z 275.1394, calcd for C15H18N2O3 [M+H]+ 275.1390; m/z 297.1214, calcd for C15H18N2O3 [M+Na]+ 297.1210.
4.2.1.2. 1-[5-(2-Methylphenoxy)pentyl]uracil (10)
Yield 72%, mp 147–149 °C, R f 0.51 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.41 (2H, qu, J = 7 Hz, CH2), 1.64 (2H, qu, J = 7.3 Hz, CH2), 1.74 (2H, qu, J = 7.3 Hz, CH2), 2.12 (3H, s, CH3), 3.68 (2H, t, J = 7 Hz, NCH2), 3.92 (2H, t, J = 6.3 Hz, OCH2), 5.55 (1H, dd, J = 7.8 and 2 Hz, H-5), 6.80 (1H, t, J = 7.5 Hz, aromatic H), 6.87 (1H, d, J = 8 Hz, aromatic H), 7.09–7.13 (2H, m, aromatic H), 7.64 (1H, d, J = 7.9 Hz, H-6), 11.25 (1H, s, NH). 13C NMR (DMSO-d 6): δ 16.4, 22.9, 28.6, 28.8, 47.8, 67.5, 101.2, 111.6, 120.4, 126.9, 127.4, 130.8, 146.2, 151.4, 157.1, 164.3. HRESIMS: found m/z 289.1541, calcd for C16H20N2O3 [M+H]+ 289.1547; m/z 311.1359, calcd for C16H20N2O3 [M+Na]+ 311.1366.
4.2.1.3. 1-[5-(3-Methylphenoxy)pentyl]uracil (11)
Yield 75%, mp 101–103 °C, R f 0.49 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.38 (2H, qu, J = 7 Hz, CH2), 1.64 (2H, qu, J = 7.3 Hz, CH2), 1.71 (2H, qu, J = 7.5 Hz, CH2), 2.25 (3H, s, CH3), 3.67 (2H, t, J = 7.2 Hz, NCH2), 3.90 (2H, t, J = 6.5 Hz, OCH2), 5.55 (1H, dd, J = 7.7 and 2 Hz, H-5), 6.68–6.72 (2H, m, aromatic H), 7.09–7.15 (2H, m, aromatic H), 7.63 (1H, d, J = 7.9 Hz, H-6), 11.23 (1H, s, NH). 13C NMR (DMSO-d 6): δ 21.1, 22.5, 28.2, 28.3, 47.4, 67.0, 100.8, 111.4, 115.1, 121.1, 129.2, 138.9, 145.7, 151.0, 158.7, 163.8. HRESIMS: found m/z 289.1552, calcd for C16H20N2O3 [M+H]+ 289.1547; m/z 311.1372, calcd for C16H20N2O3 [M+Na]+ 311.1366.
4.2.1.4. 1-[5-(4-Methylphenoxy)pentyl]uracil (12)
Yield 87%, mp 146–147 °C, R f 0.56 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.42 (2H, qu, J = 8 Hz, CH2), 1.66 (2H, qu, J = 7.1 Hz, CH2), 1.73 (2H, qu, J = 7.8 Hz, CH2), 2.21 (3H, s, CH3), 3.67 (2H, t, J = 7.3 Hz, NCH2), 3.88 (2H, t, J = 6.5 Hz, OCH2), 5.49 (1H, dd, J = 7.8 and 2 Hz, H-5), 6.73 (2H, d, J = 8.7 Hz, H-3′, H-5′), 7.01 (2H, d, J = 8.3 Hz, H-2′, H-6′), 7.47 (1H, d, J = 7.8 Hz, H-6), 11.07 (1H, s, NH). 13C NMR (DMSO-d 6): δ 20.1, 22.5, 28.3, 28.4, 47.5, 67.1, 101.0, 114.1, 129.0, 129.6, 145.0, 150.9, 156.5, 163.8. HRESIMS: found m/z 289.1542, calcd for C16H20N2O3 [M+H]+ 289.1547; m/z 311.1361, calcd for C16H20N2O3 [M+Na]+ 311.1366.
4.2.1.5. 1-[5-(3,5-Dimethylphenoxy)pentyl]uracil (13)
Yield 85%, mp 96–98 °C, R f 0.58 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.37 (2H, qu, J = 6.8 Hz, CH2), 1.62 (2H, qu, J = 7.2 Hz, CH2), 1.67 (2H, qu, J = 7.2 Hz, CH2), 2.21 (6H, s, CH3), 3.66 (2H, t, J = 7.1 Hz, NCH2), 3.88 (2H, t, J = 6.4 Hz, OCH2), 5.55 (1H, dd, J = 7.9 and 2.2 Hz, H-5), 6.51 (2H, s, H-2′, H-6′), 6.53 (1H, s, H-4′), 7.64 (1H, d, J = 7.8 Hz, H-6), 11.25 (1H, s, NH). 13C NMR (DMSO-d 6): δ 21.1, 22.5, 28.2, 28.4, 47.4, 66.9, 100.8, 112.1, 122.0, 138.6, 145.7, 151.0, 158.7, 163.8. HRESIMS: found m/z 303.1709, calcd for C17H22N2O3 [M+H]+ 303.1703; m/z 325.1526, calcd for C17H22N2O3 [M+Na]+ 325.1523.
4.2.1.6. 1-[5-(4-i-Propylphenoxy)pentyl]uracil (14)
Yield 78%, mp 139–140 °C, R f 0.50 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.15 (6H, d, J = 7.0 Hz, CH3), 1.39 (2H, qu, J = 7.0 Hz, CH2), 1.63 (2H, qu, J = 7.6 Hz, CH2), 1.71 (2H, qu, J = 7.6 Hz, CH2), 2.80 (1H, m, J = 6.9 Hz, CH2), 3.67 (2H, t, J = 7.2 Hz, NCH2), 3.90 (2H, t, J = 6.4 Hz, OCH2), 5.55 (1H, dd, J = 7.8 and 2.2 Hz, H = 5), 6.82 (1H, d, J = 8.7 Hz, H-3′, H-5′), 7.11 (2 H, d, J = 8.7 Hz, H-2′, H-6′), 7.65 (1H, d, J = 7.8 Hz, H-6), 11.24 (1H, d, J = 1.3 Hz, H-3). 13C NMR (DMSO-d 6): δ 22.5, 24.1, 28.2, 28.4, 32.6, 39.1, 39.3, 39.5, 39.7, 39.9, 47.4, 67.1, 100.8, 114.2, 127.1, 140.2, 145.7, 151.0, 156.7, 163.8. HRESIMS: found m/z 317.1863, calcd for C18H24N2O3 [M+H]+ 317.1860; m/z 339.1677, calcd for C18H24N2O3 [M+Na]+ 339.1679.
4.2.1.7. 1-[5-(4-tert-Butylphenoxy)pentyl]uracil (15)
Yield 77%, mp 125-127 °C, R f 0.50 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.23 (9H, s, CH3), 1.38 (2H, qu, J = 7.2 Hz, CH2), 1.62 (2H, qu, J = 7.2 Hz, CH2), 1.70 (2H, qu, J = 7.5 Hz, CH2), 3.67 (2H, t, J = 7.1 Hz, NCH2), 3.90 (2H, t, J = 6.7 Hz, OCH2), 5.55 (1H, dd, J = 7.8 and 2.2 Hz, H-5), 6.81 (2H, d, J = 8.9 Hz, H-3′, H-5′), 7.25 (2H, d, J = 8.9 Hz, H-2′, H-6′), 7.64 (1H, d, J = 7.8 Hz, H-6), 11.25 (1H, s, NH). 13C NMR (DMSO-d 6): δ 22.9, 28.7, 28.8, 31.8, 47.8, 67.5, 101.3, 114.3, 126.4, 142.9, 146.1, 151.4, 156.8, 164.3. HRESIMS: found m/z 331.2012, calcd for C19H26N2O3 [M+H]+ 331.2016; m/z 353.1824, calcd for C19H26N2O3 [M+Na]+ 353.1836.
4.2.1.8. 1-[5-(4-Phenylphenoxy)pentyl]uracil (16)
Yield 76%, mp 174–175 °C, R f 0.54 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.41 (2H, qu, J = 7.4 Hz, CH2), 1.64 (2H, qu, J = 7.4 Hz, CH2), 1.74 (2H, qu, J = 7.3 Hz, CH2), 3.68 (2H, t, J = 7.2 Hz, NCH2), 3.98 (2H, t, J = 6.4 Hz, OCH2), 5.56 (1H, dd, J = 7.8 and 2.2 Hz, H-5), 7.00 (2H, d, J = 8.8 Hz, H-2′, H-6′), 7.30 (1H, t, J = 7.4 Hz, H-4′′), 7.42 (2H, t, J = 7.6 Hz, H-3′′, H-5′′), 7.54-7.63 (4H, m, H-3′, H-5′, H-2′′, H-6′′), 7.66 (1H, d, J = 7.8 Hz, H-6), 11.26 (1H, s, H-3). 13C NMR (DMSO-d 6): δ 22.4, 28.2, 28.3, 39.1, 39.3, 39.5, 39.7, 40.0, 47.4, 67.3, 100.8, 114.9, 126.2, 126.7, 127.8, 128.9, 132.4, 139.9, 145.7, 151.0, 158.3, 163.8. HRESIMS: found m/z 351.1708, calcd for C21H22N2O3 [M+H]+ 351.1703; m/z 373.1526, calcd for C21H22N2O3 [M+Na]+ 373.1523.
4.2.1.9. 1-[5-(4-Cyanophenoxy)pentyl]uracil (17)
Yield 84%, mp 185–186 °C, R f 0.33 (chloroform/MeOH, 10: 1); 1H NMR (DMSO-d 6): δ 1.40 (2H, qu, J = 7.9 Hz, CH2), 1.64 (2H, qu, J = 6.4 Hz, CH2), 1.75 (2H, qu, J = 7.4 Hz, CH2), 3.67 (2H, t, J = 7.2 Hz, NCH2), 4.05 (2H, t, J = 6.3 Hz, OCH2), 5.54 (1H, dd, J = 7.8 and 2.1 Hz, H-5), 7.07 (2H, d, J = 8.8 Hz, H-3′, H-5′), 7.62 (1H, d, J = 7.9 Hz, H-6), 7.72 (2H, d, J = 9 Hz, H-2′, H-6′), 11.14 (1H, s, NH). 13C NMR (DMSO-d 6): δ 22.3, 28.0, 28.1, 47.3, 67.9, 100.9, 102.8, 115.6, 119.1, 134.1, 145.6, 151.0, 162.2, 163.7. HRESIMS: found m/z 300.1353, calcd for C16H17N3O3 [M+H]+ 300.1343; m/z 322.1163, calcd for C16H17N3O3 [M+Na]+ 322.1162.
4.2.1.10. 1-[5-(4-n-Propoxycarbonylphenoxy)pentyl]uracil (18)
Yield 76%, mp 131–132 °C, R f 0.35 (ethyl acetate); 1H NMR (DMSO-d 6): δ 0.94 (3H, t, J = 7.4 Hz, CH3) 1.39 (2H, qu, J = 7.5 Hz, CH2) 1.57–1.81 (6H, m, CH2) 3.67 (2H, t, J = 7.1 Hz, NCH2) 4.02 (2H, t, J = 6.4 Hz, OCH2) 4.17 (2H, t, J = 6.6 Hz, OCH2) 5.55 (1H, dd, J = 7.8 and 2.1 Hz, H-5) 7.01 (2H, d, J = 8.8 Hz, H-2′, H-6′) 7.65 (1H, d, J = 7.8 Hz, H-6) 7.89 (2H, d, J = 8.7 Hz, H-3′, H-5′) 11.24 (1H, s, H-3). 13C NMR (CDCl3): δ 10.4, 21.7, 22.3, 28.1, 28.2, 39.0, 39.3, 39.5, 39.7, 39.9, 47.3, 65.7, 67.6, 100.8, 114.4, 122.0, 131.2, 145.7, 151.0, 162.5, 163.8, 165.5. HRESIMS: found m/z 361.1758, calcd for C19H24N2O5 [M+H]+ 361.1758; m/z 383.1568, calcd for C19H24N2O5 [M+Na]+ 383.1577.
4.2.1.11. 1-[5-(4-Chlorophenoxy)pentyl]uracil (19)
Yield 84%, mp 168–169 °C, R f 0.41 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.38 (2H, qu, J = 6.1 Hz, CH2), 1.62 (2H, qu, J = 7.4 Hz, CH2), 1.71 (2H, qu, J = 7.6 Hz, CH2), 3.67 (2H, t, J = 7.3 Hz, NCH2), 3.92 (2H, t, J = 6.3 Hz, OCH2), 5.55 (1H, dd, J = 7.8 and 2.2 Hz, H-5), 6.92 (2H, d, J = 8.7 Hz, H-3′, H-5′), 7.29 (2H, d, J = 8.7 Hz, H-2′, H-6′), 7.64 (1H, d, J = 7.9 Hz, H-6), 11.23 (1H, s, NH). 13C NMR (DMSO-d 6): δ 22.4, 28.2, 47.4, 67.6, 100.8, 116.1, 124.1, 129.2, 145.7, 151.0, 157.5, 163.8. HRESIMS: found m/z 309.1003, calcd for C15H17ClN2O3 [M+H]+ 309.1000; m/z 331.0816, calcd for C15H17ClN2O3 [M+Na]+ 331.0820.
4.2.1.12. 1-[5-(4-Bromophenoxy)pentyl]uracil (20)
Yield 76%, mp 125–127 °C, R f 0.50 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.39 (2H, qu, J = 8.3 Hz, CH2), 1.62 (2H, qu, J = 7.2 Hz, CH2), 1.71 (2H, qu, J = 7.2 Hz, CH2), 3.66 (2H, t, J = 7.2 Hz, NCH2), 3.92 (2H, t, J = 6.3 Hz, OCH2), 5.55 (1H, dd, J = 7.8 and 2.2 Hz, H-5), 6.87 (2H, d, J = 9 Hz, H-3′, H-5′), 7.41 (2H, d, J = 8.9 Hz, H-2′, H-6′), 7.64 (1H, d, J = 7.8 Hz, H-6), 11.23 (1H, s, NH). 13C NMR (DMSO-d 6): δ 22.8, 28.6, 47.8, 68.0, 101.3, 112.2, 117.1, 132.5, 146.2, 151.4, 158.3, 164.3. HRESIMS: found m/z 375.0310, calcd for C15H17BrN2O3 [M+Na]+ m/z 375.0315.
4.2.1.13. 1-[5-(4-Nitrophenoxy)pentyl]uracil (21)
Yield 78%, mp 197–199 °C, R f 0.43 (chloroform/MeOH, 10:1); 1H NMR (DMSO-d 6): δ 1.39 (2H, qu, J = 7.6 Hz, CH2) 1.64 (2H, qu, J = 7.4 Hz, CH2) 1.76 (2H, qu, J = 7.2 Hz, CH2) 3.67 (2H, t, J = 7.2 Hz, NCH2) 4.10 (2H, t, J = 6.4 Hz, OCH2) 5.54 (1H, dd, J = 7.8 and 2.2 Hz, H-5) 7.11 (2H, d, J = 9.2 Hz, H-2′, H-6′) 7.65 (1H, d, J = 7.8 Hz, H-6) 8.17 (2H, d, J = 9.2 Hz, H-3′, H-5′) 11.21 (1H, s, H-3). 13C NMR (DMSO-d 6): δ 22.3, 28.0, 28.1, 39.1, 39.3, 39.5, 39.7, 40.0, 47.3, 68.4, 100.8, 115.0, 125.9, 145.7, 151.0, 163.8, 164.0. HRESIMS: found m/z 320.1234, calcd for C15H17N3O5 [M+H]+ 320.1241; m/z 342.1048, calcd for C15H17N3O5 [M+Na]+ 342.1060.
4.2.1.14. 1-[5-(4-Bromophenoxy)pentyl]-5-bromouracil (22)
Yield 77%, mp 160–162 °C, R f 0.50 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.38 (2H, qu, J = 8.1 Hz, CH2), 1.64 (2H, qu, J = 7.2 Hz, CH2), 1.72 (2H, qu, J = 7.4 Hz, CH2), 3.69 (2H, t, J = 7.4 Hz, NCH2), 3.94 (2H, t, J = 6.5 Hz, OCH2), 6.89 (2H, d, J = 8.9 Hz, H-3′, H-5′), 7.42 (2H, d, J = 9 Hz, H-2′, H-6′), 8.24 (1H, s, H-6), 11.74 (1H, s, NH). 13C NMR (DMSO-d 6): δ 22.3, 28.1, 47.8, 67.5, 94.6, 111.8, 116.7, 132.1, 145.4, 150.4, 157.9, 159.7. HRESIMS: found m/z 430.9603, calcd for C15H16Br2N2O3 [M+H]+ 430.9600; m/z 452.9426, calcd for C15H16Br2N2O3 [M+Na]+ 452.9420.
4.2.1.15. 1-[5-(4-Bromophenoxy)pentyl]-5-iodouracil (23)
Yield 78%, mp 166–168 °C, R f 0.82 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.37 (2H, qu, J = 7.9 Hz, CH2), 1.62 (2H, qu, J = 7.4 Hz, CH2), 1.71 (2H, qu, J = 7.7 Hz, CH2), 3,67 (2H, t, J = 7.3, NCH2), 3.93 (2H, t, J = 6.4 Hz, OCH2), 6.88 (2H, d, J = 9 Hz, H-3′, H-5′), 7.40 (2H, d, J = 9 Hz, H-2′, H-6′), 8.20 (1H, s, H-6), 11.57 (1H, s, NH). 13C NMR (DMSO-d 6): δ 25.7, 31.5, 31.6, 51.0, 70.9, 71.3, 115.1, 120.1, 135.4, 153.3, 154.0, 161.3, 164.4. HRESIMS: found m/z 478.9445, calcd for C15H16BrIN2O3 [M+H]+ 478.9462; m/z 500.9274, calcd for C15H16BrIN2O3 [M+Na]+ 500.9281.
4.2.1.16. 1-[5-(4-Bromophenoxy)pentyl]thymine (24)
Yield 82%, mp 169–171 °C, R f 0.60 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.38 (2H, qu, J = 8.1 Hz, CH2), 1.62 (2H, qu, J = 7.1 Hz, CH2), 1.72 (2H, qu, J = 7.6 Hz, CH2), 1.75 (3Н, s, СН3), 3.63 (2H, t, J = 7.3 Hz, NCH2), 3.94 (2H, t, J = 6.4 Hz, OCH2), 6.89 (2H, d, J = 9 Hz, H-3′, H-5′), 7.42 (2H, d, J = 9.1 Hz, H-2′, H-6′), 7.53 (1H, s, H-6), 11.21 (1H, s, NH). 13C NMR (DMSO-d 6): δ 12.0, 22.4, 28.2, 47.0, 67.5, 108.4, 111.8, 116.7, 132.1, 141.5, 150.9, 157.9, 164.3. HRESIMS: found m/z 367.0638, calcd for C16H19BrN2O3 [M+H]+ 367.0652; m/z 389.0460, calcd for C16H19BrN2O3 [M+Na]+ 389.0471.
4.2.1.17. 1-[3-(4-Bromophenoxy)propyl]uracil (25)
Yield 79%, mp 179–181 °C, R f 0.46 (ethyl acetate); 1H NMR (DMSO-d 6), δ 2.04 (2H, qu, J = 6.3 Hz, CH2), 3.83 (2H, t, J = 6.8 Hz, NCH2), 3.99 (2H, t, J = 6.8 Hz, OCH2), 5.53 (4H, dd, J = 7.8 and 2.3 Hz, H-5), 6.87 (2H, d, J = 9.0 Hz, H-3′, H-5′), 7.43 (2H, d, J = 8.9 Hz, H-2′, H-6′), 7.62 (1H, d, J = 7.8 Hz, H-6), 11.22 (1H, s, H-3). 13C NMR (DMSO-d 6): δ 27.9, 39.1, 39.3, 39.5, 39.7, 40.0, 45.4, 65.4, 100.9, 112.0, 116.7, 132.1, 145.9, 151.0, 157.7, 163.8. HRESIMS: found m/z 325.0193, calcd for C13H13BrN2O3 [M+H]+ 325.0182; m/z 347.0007, calcd for C13H13BrN2O3 [M+Na]+ 347.0002.
4.2.1.18. 1-[4-(4-Bromophenoxy)butyl]uracil (26)
Yield 80%, mp 143–144 °C, R f 0.40 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.67–1.72 (4H, m, CH2), 3.72 (2H, t, J = 6.6 Hz, CH2), 3.97 (2H, t, J = 5.8 Hz, CH2), 5.56 (1Н, dd, J = 7.8 and 2.2 Hz, Н-5), 6.90 (2H, d, J = 9.1 Hz, H-3′, H-5′), 7.43 (2H, d, J = 9 Hz, H-2′, H-6′), 7.67 (1H, d, J = 7.9 Hz, H-6), 11.23 (1H, s, NH). 13C NMR (DMSO-d 6): δ 25.2, 25.6, 47.2, 67.4, 100.9, 111.9, 116.8, 132.1, 145.7, 151.0, 157.9, 163.8. HRESIMS: found m/z 361.0160, calcd for C14H15BrN2O3 [M+Na]+ 361.0158.
4.2.1.19. 1-[6-(4-Bromophenoxy)hexyl]uracil (27)
Yield 70%, mp 121–122 °C, R f 0.51 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.30 (2H, qu, J = 6.9 Hz, CH2), 1.42 (2Н, qu, J = 6.8 Hz, СН2), 1.59 (2Н, qu, J = 7.1 Hz, СН2), 1.70 (2Н, qu, J = 6.8 Hz, СН2), 3.65 (2H, t, J = 7.2 Hz, CH2), 3.93 (2H, t, J = 6.5 Hz, CH2), 5.53 (1Н, dd, J = 7.8 and 2.2 Hz, Н-5), 6.89 (2H, d, J = 9 Hz, H-3′, H-5′), 7.42 (2H, d, J = 8.9 Hz, H-2′, H-6′), 7.64 (1H, d, J = 7.8 Hz, H-6), 11.19 (1H, s, NH). 13C NMR (DMSO-d 6): δ 25.1, 25.5, 28.4, 47.467.7, 100.8, 111.8, 116.8, 132.1, 145.7, 151.0, 158.0, 163.8. HRESIMS: found m/z 389.0465, calcd for C16H19BrN2O3 [M+Na]+ 389.0471.
4.2.1.20. 1-[8-(4-Bromophenoxy)octyl]uracil (28)
Yield 76%, mp 145–147 °C, R f 0.54 (ethyl acetate); 1H NMR (DMSO-d 6): δ 1.16-1.43 (8H, m, CH2), 1.56 (2H, qu, J = 7.1 Hz, CH2), 1.67 (2H, qu, J = 7.0 Hz, CH2), 3.63 (2H, t, J = 7.2 Hz, NCH2), 3.92 (2H, t, J = 6.5 Hz, OCH2), 5.54 (1H, dd, J = 7.8 and 2.2 Hz, H-5), 6.88 (2H, d, J = 8.9 Hz, H-3′, H-5′), 7.41 (2H, d, J = 8.9 Hz, H-2′, H-6′), 7.64 (1H, d, J = 7.8 Hz, H-6), 11.22 (1 H, s, H-3). 13C NMR (DMSO-d 6): δ 25.4, 25.8, 28.4, 28.5, 28.6, 28.6, 39.1, 39.3, 39.5, 39.7, 40.0, 47.4, 67.7, 100.8, 111.7, 116.7, 132.1, 145.7, 151.0, 158.0, 163.8. HRESIMS: found m/z 395.0964, calcd for C18H23BrN2O3 [M+H]+ 395.0965; m/z 417.0781, calcd for C18H23BrN2O3 [M+Na]+ 417.0784.
4.2.2. 4-[5-(2,4-Dioxo-3,4-dihydropyrimidin-1(2H)-yl)pentyloxy]benzoic acid (29)
A solution of 1-[5-(4-n-propoxycarbonylphenoxy)pentyl]uracil 18 (1.60 g, 4.44 mmol) in 40 mL of EtOH and 20 mL of 2.5% aqueous NaOH was refluxed for 8 h and EtOH was evaporated. The residue was cooled to rt, treated dropwise with 2% HCl and stored in a refrigerator overnight. The resulting precipitate was filtered and recrystallized from aqueous EtOH to yield 1.15 g of 25 as white crystals. Yield 81%, mp 225–227 °C, R f 0.69 (chloroform/MeOH, 10:1); 1H NMR (DMSO-d 6): δ 1.38 (2H, qu, J = 7.3 Hz, CH2), 1.63 (2H, qu, J = 7.3 Hz, CH2), 1.74 (2H, qu, J = 7.3 Hz, CH2), 3.66 (2H, t, J = 7.2 Hz, NCH2), 4.01 (2H, t, J = 6.3 Hz, OCH2), 5.54 (1H, d, J = 7.8 Hz, H-5), 6.98 (2H, d, J = 8.8 Hz, H-2′, H-6′), 7.64 (1H, d, J = 7.8 Hz, H-6), 7.87 (2H, d, J = 8.8 Hz, H-3′, H-5′), 11.22 (1H, br s, H-3). 13C NMR (DMSO-d 6): δ 22.4, 28.1, 28.2, 39.1, 39.3, 39.5, 39.7, 39.9, 47.3, 67.6, 100.8, 114.2, 122.9, 131.4, 145.7, 151.0, 162.3, 163.8, 167.1. HRESIMS: found m/z 341.1108, calcd for C16H18N2O5 [M+Na]+ 341.1108; m/z 363.0928, calcd for C16H17NaN2O5 [M+Na]+ 363.0927.
4.2.3. 1-[5-(4-Aminophenoxy)pentyl]uracil (30)
To the solution of 1-[5-(4-nitrophenoxy)pentyl]uracil 21 (1.17 g, 3.36 mmol) in 20 ml of abs EtOH SnCl2·2H2O (4.2 g, 18.61 mmol) was added. Resulting mixture was refluxed for 3 h and poured into 200 ml of cold distilled water. Resulting precipitate was filtered off, air-dried and recrystallized from i-PrOH/DMF 2:1 mixture to yield 0.63 g of 26 as small yellow crystals. Yield 59%, mp 190–192 °C, R f 0.55 (chloroform/MeOH, 10:1); 1H NMR (DMSO-d 6): δ 1.36 (2H, qu, J = 7.4 Hz, CH2), 1.51–1.74 (4H, m, CH2), 3.66 (2H, t, J = 7.1 Hz, NCH2), 3.80 (2H, t, J = 6.4 Hz, OCH2), 4.53 (2H, br s, NH2), 5.53 (1H, d, J = 7.8 Hz, H-5), 6.50 (2H, d, J = 8.7 Hz, H-2′, H-6′), 6.62 (2H, d, J = 8.8 Hz, H-3′, H-5′), 7.63 (1H, d, J = 7.8 Hz, H-6), 11.17 (1H, br s, H-3). 13C NMR (DMSO-d 6): δ 22.5, 28.2, 28.5, 39.2, 39.4, 39.6, 39.8, 40.0, 47.4, 67.8, 100.8, 115.0, 115.4, 142.3, 145.7, 151.0, 163.8. HRESIMS: found m/z 290.1507, calcd for C15H19N3O3 [M+H]+ 290.1499; m/z 312.1325, calcd for C15H19N3O3 [M+Na]+ 312.1319.
4.3. Biological assays
4.3.1. Antiviral activity assays other than HIV
The compounds were evaluated against the following viruses: herpes simplex virus type 1 (HSV-1) strain KOS, thymidine kinase-deficient (TK−) HSV-1 KOS strain resistant to ACV (ACVr), herpes simplex virus type 2 (HSV-2) strains Lyons and G, human cytomegalovirus (HCMV) (strains AD-169 and Davis), varicella–zoster virus (strains OKA and YS), vaccinia virus Lederle strain, respiratory syncytial virus (RSV) strain Long, vesicular stomatitis virus (VSV), Coxsackie B4, Parainfluenza 3, Influenza virus A (subtypes H1N1, H3N2), influenza virus B, Reovirus-1, Sindbis and Punta Toro. The antiviral assays were based on inhibition of virus-induced cytopathicity or plaque formation in human embryonic lung (HEL) fibroblasts, African green monkey cells (Vero), human epithelial cells (HeLa) or Madin–Darby canine kidney cells (MDCK). Confluent cell cultures in microtiter 96-well plates were inoculated with 100 CCID50 of virus (1 CCID50 being the virus dose to infect 50% of the cell cultures) or 10 or 100 plaque forming units (PFU) (for VZV and HCMV) in the presence of varying concentrations of the test compounds. Viral cytopathicity or plaque formation was recorded as soon as it reached completion in the control virus-infected cell cultures that were not treated with the test compounds. Antiviral activity was expressed as the EC50 or compound concentration required to reduce virus-induced cytopathogenicity or viral plaque formation by 50%.
4.3.2. Anti-HIV activity assays
Inhibition of HIV-1(IIIB)- and HIV-2(ROD)-induced cytopathicity in CEM cell cultures was measured in microtiter 96-well plates containing ∼3 × 105 CEM cells/mL infected with 100 CCID50 of HIV per milliliter and containing appropriate dilutions of the test compounds. After 4−5 days of incubation at 37 °C in a CO2-controlled humidified atmosphere, CEM giant (syncytium) cell formation was examined microscopically. The EC50 (50% effective concentration) was defined as the compound concentration required to inhibit HIV-induced giant cell formation by 50%.
4.3.3. Cytostatic activity assays
All assays were performed in 96-well microtiter plates. To each well were added (5−7.5) × 104 tumor cells and a given amount of the test compound. The cells were allowed to proliferate for 48 h (murine leukemia L1210 cells) or 72 h (human lymphocytic CEM and human cervix carcinoma HeLa cells) at 37 °C in a humidified CO2-controlled atmosphere. At the end of the incubation period, the cells were counted in a Coulter counter. The IC50 (50% inhibitory concentration) was defined as the concentration of the compound that inhibited cell proliferation by 50%.
Acknowledgments
This work was supported by grant of Russian Foundation For Basic Research (13-04-01391). The antiviral work was supported by KU Leuven (GOA 10/14). The authors thank Lies Van den Heurck, Anita Camps, Steven Carmans, Leentje Persoons, Frieda De Meyer, Leen Ingels and Lizette van Berckelaer for their help in performing the antiviral and cytostatic assays.
Footnotes
Supplementary data (NMR spectra for all of the synthesized compounds) associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.bmc.2013.05.009.
Supplementary data
NMR spectra for all of the synthesized compounds.
References and notes
- 1.Ryan K.J., Ray C.G., editors. Sherris Medical Microbiology. 4th ed. McGraw Hill; 2004. p. 556. [Google Scholar]
- 2.Reeves M., Sinclair J. Springer; Berlin Heidelberg: 2008. Human Cytomegalovirus; pp. 297–313. [Google Scholar]
- 3.Staras S.A.S., Dollard S.C., Radford K.W., Flanders W.D., Pass R.F., Cannon M. J. Clin. Infect. Dis. 2006;43:1143. doi: 10.1086/508173. [DOI] [PubMed] [Google Scholar]
- 4.Baroco A.L., Oldfield E.C. Curr. Gastroent. Rep. 2008;10:409. doi: 10.1007/s11894-008-0077-9. [DOI] [PubMed] [Google Scholar]
- 5.Jackson S.E., Mason G.M., Wills M.R. Virus Res. 2011;157:151. doi: 10.1016/j.virusres.2010.10.031. [DOI] [PubMed] [Google Scholar]
- 6.Nashan B., Gaston R., Emery V., Säemann M.D., Mueller N.J., Couzi L., Dantal J., Shihab F., Mulgaonkar S., Seun Kim Y., Brennan D.C. Transplantation. 2012;93:1075. doi: 10.1097/TP.0b013e31824810e6. [DOI] [PubMed] [Google Scholar]
- 7.Pereira L. J. Infect. Dis. 2011;203:1510. doi: 10.1093/infdis/jir126. [DOI] [PubMed] [Google Scholar]
- 8.Melnick M., Sedghizadeh P.P., Allen C.M., Jaskoll T. Exp. Mol. Pathol. 2012;92:118. doi: 10.1016/j.yexmp.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 9.Toyoda-Akui M., Yokomori H., Kaneko F., Shimizu Y., Takeuchi H., Tahara K., Yoshida H., Kondo H., Motoori T., Ohbu M., Oda M., Hibi T. Int. J. Gen. Med. 2011;4:397. doi: 10.2147/IJGM.S19245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caposio P., Orloff S.L., Streblow D.N. Virus Res. 2011;157:204. doi: 10.1016/j.virusres.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pandey J.P., LeRoy E.C. Arthritis Rheum. 1998;41:10. doi: 10.1002/1529-0131(199801)41:1<10::AID-ART2>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 12.Zhou Y.F., Leon M.B., Waclawiw M.A., Popma J.J., Yu Z.X., Finkel T., Epstein S.E. N. Eng. J. Med. 1996;335:624. doi: 10.1056/NEJM199608293350903. [DOI] [PubMed] [Google Scholar]
- 13.Hjelmesaeth J., Sagedal S., Hartmann A., Rollag H., Egeland T., Hagen M., Nordal K.P., Jenssen T. Diabetologia. 2004;47:1550. doi: 10.1007/s00125-004-1499-z. [DOI] [PubMed] [Google Scholar]
- 14.Van der Werf N., Kroese F.G.M., Rozing J., Hillebrands J.-L. Diabetes Metab. Res. Rev. 2007;23:169. doi: 10.1002/dmrr.695. [DOI] [PubMed] [Google Scholar]
- 15.Faulds D., Heel R.C. Drugs. 1990;39:597. doi: 10.2165/00003495-199039040-00008. [DOI] [PubMed] [Google Scholar]
- 16.De Clercq E. Rev. Med. Virol. 1993;3:85. [Google Scholar]
- 17.Chrisp P., Clissold S.P. Drugs. 1991;41:104. doi: 10.2165/00003495-199141010-00009. [DOI] [PubMed] [Google Scholar]
- 18.Bedard J., May S., Lis M., Tryphonas L., Drach J., Huffman J., Sidwell R., Chan L., Bowlin T., Rando R. Antimicrob. Agents Chemother. 1999;43:557. doi: 10.1128/aac.43.3.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sugawara M., Huang W., Fei Y.J., Leibach F.H., Ganapathy V., Ganapathy M.E. J. Pharm. Sci. 2000;89:781. doi: 10.1002/(SICI)1520-6017(200006)89:6<781::AID-JPS10>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 20.Smith I.L., Taskintuna I., Rahhal F.M., Powell H.C., Ai E., Mueller A.J., Spector S.A., Freeman W.R. Arch. Ophthalmol. 1998;116:178. doi: 10.1001/archopht.116.2.178. [DOI] [PubMed] [Google Scholar]
- 21.Limaye A.P., Corey L., Koelle D.M., Davis C.L., Boeckh M. Lancet. 2000;356:645. doi: 10.1016/S0140-6736(00)02607-6. [DOI] [PubMed] [Google Scholar]
- 22.Weinberg A., Jabs D.A., Chou S., Martin B.K., Lurain N.S., Forman M.S., Crumpacker C. J. Infect. Dis. 2003;187:777. doi: 10.1086/368385. [DOI] [PubMed] [Google Scholar]
- 23.Mercorelli B., Sinigalia E., Loregian A., Palù G. Rev. Med. Virol. 2008;18:177. doi: 10.1002/rmv.558. [DOI] [PubMed] [Google Scholar]
- 24.Chan L., Jin H., Stefanac T., Lavallée J.F., Falardeau G., Wang W., Bédard J., May S., Yuen L. J. Med. Chem. 1999;42:3023. doi: 10.1021/jm9902483. [DOI] [PubMed] [Google Scholar]
- 25.Falardeau G., Lachance H., St-Pierre A., Yannopoulos C.G., Drouin M., Bédard J., Chan L. Bioorg. Med. Chem. Lett. 2005;15:1693. doi: 10.1016/j.bmcl.2005.01.050. [DOI] [PubMed] [Google Scholar]
- 26.Gueiffier A., Lhassani M., Elhakmaoui A., Snoeck R., Andrei G., Chavignon O., Teulade J.C., Kerbal A., Essassi E.M., Debouzy J.C., Witvrouw M., Blache Y., Balzarini J., De Clercq E., Chapat J.P. J. Med. Chem. 1996;39:2856. doi: 10.1021/jm9507901. [DOI] [PubMed] [Google Scholar]
- 27.Véron J.-B., Allouchi H., Enguehard-Gueiffier C., Snoeck R., Andrei G., De Clercq E., Gueiffier A. Bioorg. Med. Chem. 2008;16:9536. doi: 10.1016/j.bmc.2008.09.027. [DOI] [PubMed] [Google Scholar]
- 28.Véron J.-B., Enguehard-Gueiffier C., Snoeck R., Andrei G., De Clercq E., Gueiffier A. Bioorg. Med. Chem. 2007;15:7209. doi: 10.1016/j.bmc.2007.03.061. [DOI] [PubMed] [Google Scholar]
- 29.Martinez A., Gil C., Perez C., Castro A., Prieto C., Otero J., Andrei G., Snoeck R., Balzarini J., De Clercq E. J. Med. Chem. 2000;43:3267. doi: 10.1021/jm000118q. [DOI] [PubMed] [Google Scholar]
- 30.Martinez A., Gil C., Castro A., Pérez C., Prieto C., Otero J. Bioorg. Med. Chem. 2003;11:2395. doi: 10.1016/s0968-0896(03)00148-2. [DOI] [PubMed] [Google Scholar]
- 31.Oien N.L., Brideau R.J., Hopkins T.A., Wieber J.L., Knechtel M.L., Shelly J.A., Anstadt R.A., Wells P.A., Poorman R.A., Huang A., Vaillancourt V.A., Clayton T.L., Tucker J.A., Wathen M.W. Antimicrob. Agents Chemother. 2002;46:724. doi: 10.1128/AAC.46.3.724-730.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schnute M.E., Cudahy M.M., Brideau R.J., Homa F.L., Hopkins T.A., Knechtel M.L., Oien N.L., Pitts T.W., Poorman R.A., Wathen M.W., Wieber J.L. J. Med. Chem. 2005;48:5794. doi: 10.1021/jm050162b. [DOI] [PubMed] [Google Scholar]
- 33.Larsen S.D., Zhang Z., DiPaolo B.A., Manninen P.R., Rohrer D.C., Hageman M.J., Hopkins T.A., Knechtel M.L., Oien N.L., Rush B.D., Schwende F.J., Stefanski K.J., Wieber J.L., Wilkinson K.F., Zamora K.M., Wathen M.W., Brideau R.J. Bioorg. Med. Chem. Lett. 2007;17:3840. doi: 10.1016/j.bmcl.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 34.Schnute M.E., Brideau R.J., Collier S.A., Cudahy M.M., Hopkins T.A., Knechtel M.L., Oien N.L., Sackett R.S., Scott A., Stephan M.L., Wathen M.W., Wieber J.L. Bioorg. Med. Chem. Lett. 2008;18:3856. doi: 10.1016/j.bmcl.2008.06.060. [DOI] [PubMed] [Google Scholar]
- 35.Nieman J.A., Nair S.K., Heasley S.E., Schultz B.L., Zerth H.M., Nugent R.A., Chen K., Stephanski K.J., Hopkins T.A., Knechtel M.L., Oien N.L., Wieber J.L., Wathen M.W. Bioorg. Med. Chem. Lett. 2010;20:3039. doi: 10.1016/j.bmcl.2010.03.115. [DOI] [PubMed] [Google Scholar]
- 36.Petrov V.I., Ozerov A.A., Novikov M.S., Pannecouque C., Balzarini J., De Clercq E. Chem. Heterocycl. Compd. 2003;39:1218. [Google Scholar]
- 37.Novikov M.S., Ozerov A.A., Orlova Y.A., Buckheit R.W. Chem. Heterocycl. Compd. 2005;41:625. [Google Scholar]
- 38.Novikov M.S., Ivanova O.N., Ivanov A.V., Ozerov A.A., Valuev-Elliston V.T., Temburnikar K., Gurskaya G.V., Kochetkov S.N., Pannecouque C., Balzarini J., Seley-Radtke K.L. Bioorg. Med. Chem. 2011;19:5794. doi: 10.1016/j.bmc.2011.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Novikov M.S., Valuev-Elliston V.T., Babkov D.A., Paramonova M.P., Ivanov A.V., Gavryushov S.A., Khandazhinskaya A.L., Kochetkov S.N., Pannecouque C., Andrei G., Snoeck R., Balzarini J., Seley-Radtke K.L. Bioorg. Med. Chem. 2013 doi: 10.1016/j.bmc.2012.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Novikov M.S., Ozerov A.A. Chem. Heterocycl. Compd. 2005;41:905. [Google Scholar]
- 41.Bellamy F.D., Ou K. Tetrahedron Lett. 1984;25:839. [Google Scholar]
- 42.Tona M., Sánchez-Baeza F., Messeguer A. Tetrahedron. 1994;50:8117. [Google Scholar]
- 43.Kikumoto R., Tobe A., Tonomura S. J. Med. Chem. 1981;24:145. doi: 10.1021/jm00134a004. [DOI] [PubMed] [Google Scholar]
- 44.Kikumoto R., Tobe A., Fukami H., Egawa M. J. Med. Chem. 1983;26:246. doi: 10.1021/jm00356a024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
NMR spectra for all of the synthesized compounds.


