Abstract
Anemia is present in over two-thirds of patients with malignant hematological disorders. The etiology of anemia predominates from ineffective erythropoiesis from marrow infiltration, cytokine related suppression, erythropoietin suppression, and vitamin deficiency; ineffective erythropoiesis is further exacerbated by accelerated clearance due to antibody mediated hemolysis and thrombotic microangiopathy. As the anemia is chronic in nature, symptoms are generally well tolerated and often non-specific. Transfusion of red blood cells (RBCs) is a balance between providing benefit for patients while avoiding risks of transfusion. Conservative/restrictive RBC transfusion practices have shown equivalent patient outcomes compared to liberal transfusion practices, and meta-analysis has shown improved in-hospital mortality, reduced cardiac events, re-bleeding, and bacterial infections. The implications for a lower threshold for transfusion in patients with malignancies are therefore increasingly being scrutinized. Alternative management strategies for anemia with IV iron and erythropoietin stimulating agents (ESAs) should be considered in the appropriate settings.
Keywords: Anemia, Red blood cell transfusion, Restrictive vs liberal transfusion practices
1. Introduction
Blood transfusion therapy is a key component of supportive care for adults and children with malignant hematologic disorders such as leukemia and recipients of hematopoietic stem cell transplants (HSCT). Over two-thirds of patients with a hematologic malignancy develop anemia [1], with the highest prevalence in children with leukemia (over 97%) and lymphoma (over 93%) [2]. The transfusion of red blood cells (RBC) is a balance between the benefits of maintaining oxygen delivery and the inherent risks from blood transfusion. We have previously published reviews of blood transfusion practices in adults [3] and in the elderly [4]; and here, we update blood transfusion therapy in adults and children. We summarize the pathophysiology of anemia in this setting, indications for red blood cell (RBC) transfusion, current blood risks, special situations in RBC transfusion, and alternative or adjunct therapy for anemia management such as erythropoietic stimulating agents (ESAs) and iron therapy. Where possible, we provide evidence-based guidelines for best practices.
2. Pathophysiology of anemia in patients with malignant hematologic disorders
The anemia in this setting is multifactorial and includes production defects, accelerated clearance, and hemorrhage. Causes of anemia include leukemic infiltration of the bone marrow at diagnosis or relapse, chemotherapy and radiation therapies, suppression of the erythropoietin response to anemia, infection/inflammation, shortened RBC survival, or hemorrhage secondary to thrombocytopenia and/or consumptive coagulopathies such as disseminated intravascular coagulation [5].
Anemia in patients with leukemia is most often due to underproduction of erythropoietic precursors, because of direct tumor infiltration of the bone marrow or chemotherapies [6]. In patients undergoing HSCT, radiotherapy and preparative myeloablative chemotherapy regimens further challenge RBC precursor production. Ninety six percent of adult patients receiving myeloablative chemotherapy preparations require RBC support, compared to only 63% of patients receiving non-myeloablative preparations [7].
Reduced and ineffective erythropoiesis in the form of renal dysfunction (reduced erythropoietin) and cytokine mediated anemia of chronic disease (ACD) also contribute to anemia in patients with hematologic malignancies. Tumor-released cytokines upregulate hepcidin [8], [9] which leads to sequestration of body iron stores in bone marrow macrophages and reduced iron absorption from the alimentary tract. Hepcidin degrades ferroportin receptors, which are responsible for making iron available for erythropoiesis, through iron transport from enterocytes and marrow macrophages into plasma [10].
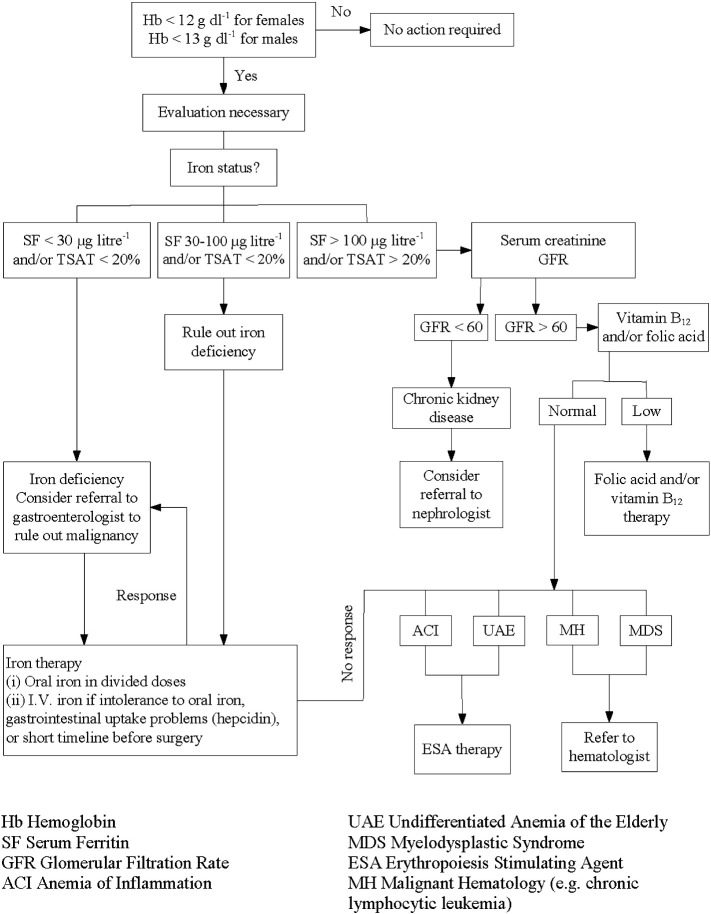
Red cell precursors may also selectively be reduced: i.e. pure red cell aplasia, due to ABO-incompatible HST [11], underlying lymphoproliferative disorder [12], certain drugs [13], and formation of antibodies to erythropoietin [14]. Less frequent contributing causes of erythropoiesis suppression include viral suppression of erythropoiesis as occurs with various infections including parvovirus B19. Renal insufficiency and vitamin deficiencies such as iron, folate or vitamin B12 may also contribute to anemia in adult patients, as illustrated in Fig. 1 [4].
Fig. 1.
Evaluation and management of anemia.
Once the blood count demonstrates anemia, an evaluation should begin with an assessment of iron status. When ferritin and/or iron saturation levels indicate absolute iron deficiency, iron therapy is indicated. When ferritin and/or iron saturation values rule out absolute iron deficiency, serum creatinine and glomerular filtration rate (GFR) determination may indicate chronic kidney disease (CKD). When ferritin and/or iron saturation values are in determinant, further evaluation to rule out absolute iron deficiency versus inflammation/chronic disease is necessary. A clinical response to a therapeutic trial of iron would confirm absolute iron deficiency. No response to iron therapy would indicate the anemia of chronic disease, suggesting that ESA therapy be considered.
Reproduced with permission From Goodnough LT, Schrier A. Am J Hematol 2014;89:88–96 [4].
Shortened RBC survival can also accompany the anemia of underproduction in malignancy. Lymphoproliferative conditions such as chronic lymphocytic leukemia, Hodgkin's and non-Hodgkin's lymphoma, and lymphoplasmacytic lymphoma are associated with warm and cold reactive autoantibodies to RBCs [15]. Fludarabine and other purine analogs also increase the frequency of autoimmune hemolytic anemias (AHA) [16]. Laboratory findings in AHA typically include a low hemoglobin, high lactate dehydrogenase (LDH), high bilirubin (typically indirect), low haptoglobin, hemoglobinuria and positive direct antiglobulin test (DAT) for IgG classically in a warm AHA and complement (or C3d) in a cold AHA.
Malignancies and targeted therapies have also been associated with microangiopathic hemolytic anemia (MAHA) and disseminated intravascular coagulation (DIC). While acute DIC is uncommon presentation for most hematologic malignancies, urokinase-like plasminogen activator has been found in blasts of acute promyelocytic leukemia (APL) which often lead to DIC prior to widespread treatment with all-trans retinoic acid [17], [18]. Chemotherapy agents such as cisplatin, bleomycin, daunorubicin, and calcineurin inhibitors used in HSCT patients such as cyclosporine and tacrolimus have been shown to independently lead to drug-induced MAHA [19].
3. Clinical manifestations of anemia
The signs and symptoms of anemia vary based on the acuity of the anemia, the compensatory change in blood volume and the compensatory change in the patient's cardiovascular system. Chronic anemia is generally well tolerated due to compensatory expansion of intravascular plasma volume, increased cardiac output, vasodilatation, increased blood flow due to decreased viscosity, and not least, increased RBC 2,3 diphosphoglycerate (DPG) with a right shift of the oxygen dissociation curve. Symptoms of anemia are often non-specific and can include fatigue, pallor, dizziness, headaches, vertigo, tinnitus, dyspnea, faintness, and inactivity. Fatigue specifically has been linked to poor quality of life [20]. Children can additionally experience poor feeding, irritability, change in behavior and poor school performance. Cardiac enlargement and evidence of congestive heart failure may present with bruits, flow murmurs, and a gallop rhythm in severe anemia.
The traditional therapy for cancer-related anemia has been RBC transfusions. However, blood transfusions have been identified as one of the most over-used (and inappropriate) therapeutic interventions by national accreditation (Joint Commission) and medical societies such as the American Board of Internal Medicine [21], the American Medical Association and the American Society of Hematology.i Guidelines have been published by the AABB [22] and the National Cancer Center Network (NCCN) [23] for RBC transfusion therapy as well as alternative anemia therapies such as IV iron and ESA therapy [24]. Additional guidelines specific to pediatric [25] and adult [3] clinical settings have been published, and will be reviewed.
4. Blood transfusion risks
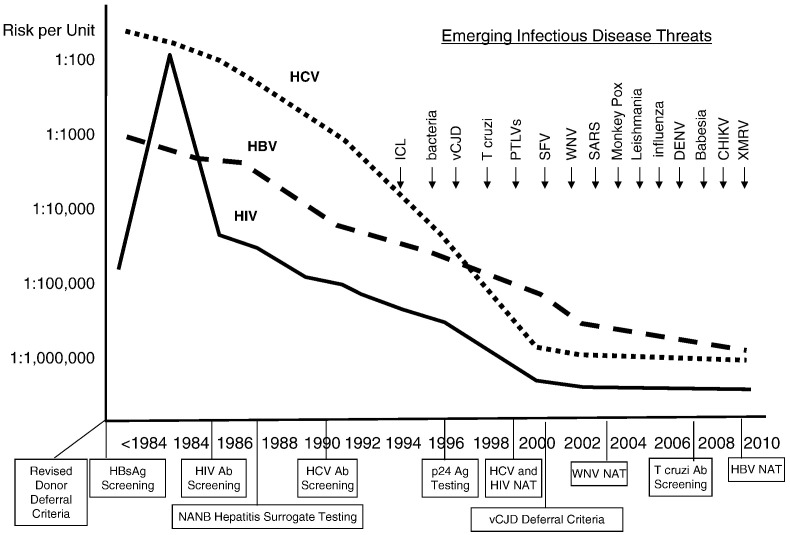
Transfusion-transmitted infections prompted concern by patients and healthcare providers since the 1980s, with the recognition of transfusion–transmission of HIV and hepatitis C virus (HCV) [26]. These risks have decreased substantially and responses to emerging pathogens transmitted by blood transfusion have been rapid (Fig. 2 ). Between 2007 and 2011, transfusion-related acute lung injury (TRALI) caused the highest percentage (43%) of fatalities reported to the FDA, followed by hemolytic transfusion reactions (23%) caused by non-ABO (13%) or ABO (10%) incompatible blood transfusions [27].
Fig. 2.
Risks of major TTVs linked to interventions, and accelerating rate of EIDs of concern to blood safety.
Evolution of the risks of transmission by blood transfusion for HIV, HBV, and HCV. Major interventions to reduce risks are indicated below the time line on the X axis. Emerging infectious disease threats over the past 20 years are indicated above in the top right quadrant of the figure. Ab = antibody; Ag = antigen; CHIKV = Chikungunya virus; DENV = dengue virus; ICL = idiopathic CD4 + T-lymphocytopenia; SARS = severe acute respiratory syndrome; SFV = simian foamy virus; XMRV = xenotropic murine leukemia virus-related virus.
Reproduced with permission, from Perkins, et al. Transfusion 2010;50:2080–2099.
RBC transfusion is associated with a number of potential side effects including common one such as febrile non-hemolytic and mild allergic reactions, HLA and RBC antigen alloimmunization, bacterial and viral infection transmission, and transfusion associated graft vs. host disease (TA-GVHD). The morbidity and mortality risks associated with transfusion-transmitted CMV infection and TA-GVHD in the immunocompromised patient are beyond the scope of this review, and the interested reader in adverse outcomes specific to immunocompromised hosts can reference relevant reviews [28], [29].
Increasing evidence suggests that a far greater number of patients now have adverse clinical outcomes (increased morbidity and mortality) associated with unnecessary blood transfusions [30], [31], [32]. Table 1 lists risks that include not only known transmissible pathogens for infectious disease, transfusion reactions, TRALI, errors in blood administration, and circulatory overload; but also potential, as yet undefined risks such as immunomodulation (e.g., peri-operative infection or tumor progression), unknown risks (such as the recently-emerging pathogen of new variant Creutzfeldt-Jakob disease); [33] and potential risks associated with storage lesions from blood transfusions to patients in clinical settings such as cardiac surgery [34], [35].
Table 1.
Transfusion-associated adverse events.
| I. Infectious agents | |
|---|---|
| Transfusion-transmitted disease routinely tested | Estimated risk per unit |
| Hepatitis B virus (HBV; 1970 [surface antigen]; 1986–1987 | |
| [core antibody]); 2009 [nucleic acid] | 1:1,000,000 |
| Human immunodeficiency virus (HIV; 1985 [antibody]; | |
| 200 [nucleic acid]) | 1:2,000,000 |
| Hepatitis C virus (HCV; 1986–1987 [alanine aminotransferase]; | |
| 1990 [antibody]; 1999 [nucleic acid]) | 1:2,000,000 |
| Human T-cell lymphotropic virus (HTLV; 1988 [antibody]) | Very rare |
| West Nile virus (WNV; 2003 [nucleic acid]) | Very rare |
| Bacteria (in platelets only; 2004) | 1:20,000 |
| Trypanosomacruzi (2007 [antibody]) | Very rare |
| Syphilis | Very rare |
| Cytomegalovirus (CMV) (for patients at risk) | Rare |
| Transfusion-transmitted disease not routinely tested | Very rare |
| Hepatitis A virus (HAV) | |
| Parvovirus B19 | |
| Dengue fever virus (DFV) | |
| Malaria | |
| Hepatitis E | |
| Babesia sp | |
| Plasmodium sp | |
| Leishmania sp | |
| Brucella sp | |
| New variant Creutzfeldt-Jakob disease (nvCJD) prions | |
| Unknown Pathogens | |
| II. Transfusion-associated adverse reactions events | |
| ABO incompatible blood transfusions | 1 in 60,000 |
| Symptoms | 40% |
| Fatalities | 1 in 600,000 |
| Delayed serologic reactions | 1 in 1600 |
| Delayed hemolytic reactions | 1 in 6700 |
| Transfusion-related acute lung injury (TRALI) | 1 in 20,000 |
| Graft-versus-host disease | Very rare |
| Post-transfusion purpura | Very rare |
| Febrile, nonhemolytic transfusion | |
| reactions | |
| Red blood cells | 1 in 200 |
| Platelets | 1 in 5–20 |
| Allergic reactions | 1 in 30–100 |
| Transfusion-associated circulatory overload (TACO) | 1 in 12 |
| Anaphylactic reactions (IgA deficiency) | 1 in 150,000 |
| Iron overload | Estimated 80–100 U for adults |
| Transfusion-related immunosuppression (TRIM) | Unestablished |
| Storage Lesions | Unestablished |
| Modified From Goodnough LT. Lancet 2013;391:1791–2. | |
Awareness of blood risks and costs has led providers to institution-based initiatives in Patient Blood Management, with the adoption of guidelines that limit the use of blood transfusion [3]. Patient Blood Management encompasses an evidence-based approach that is multidisciplinary (transfusion medicine specialists, surgeons, anesthesiologists, and critical care specialists) and multiprofessional (physicians, nurses, pump technologists and pharmacists) [36]. Preventative strategies are emphasized: to identify, evaluate, and manage anemia in medical [4], [37] and surgical [38] patients, use of pharmacologic interventions [24] and the avoidance of unnecessary diagnostic testing to minimize iatrogenic blood loss; [39] and to establish clinical practice guidelines for blood transfusions.
5. Red blood cell (RBC) transfusion therapy
5.1. Pediatric patients
5.1.1. Level 1 evidence
A single randomized, prospective multi-center trial to evaluate a hemoglobin ‘trigger’ in children was performed by Lacroix et al. in 2007 [40]. In this study, over 600 children admitted to the pediatric intensive care units (ICU) at 19 centers in four countries were randomized to either a restrictive-strategy group where hemoglobin threshold was set at 7 g/dl or a liberal-strategy transfusion group where hemoglobin threshold was set at 9 g/dl. The authors found that the restrictive strategy resulted in a 44% decrease in the number of RBC transfusions without increasing rates of new or progressive multi-organ dysfunction, the primary outcome of the study. A number of secondary outcomes, including sepsis, transfusion reactions, nosocomial respiratory infections, catheter-related infections, adverse events, length of stay in the ICU and hospital and morality were no different between the groups. The authors recommend a restrictive RBC transfusion strategy in pediatric patients who are stable in the ICU [40].
Other randomized trials investigating hemoglobin thresholds have been completed or are underway in neonates [41], [42], [43]. The Prematures in Need of Transfusion (PINT) study suggested that liberal RBC transfusions were beneficial to neurocognitive outcomes of premature infants at 18–22 months, in contrast to Bell's randomized clinical trial in Iowa which showed poorer neurologic outcomes at 7–10 year follow-up for those premature infants who were transfused liberally [40], [41]. The Transfusion of Prematures (TOP) trial is underway to address these conflicting results [42].
Evidence from robust randomized controlled trials is otherwise lacking in children with hematologic malignancies, leading to heterogeneity in practice between different centers and those among patient groups [5], [44]. In a survey of pediatric centers from Children's Oncology Group, 60% of centers used a transfusion trigger of hemoglobin 8 g/dl, whereas 25% of centers used 7 g/dl [44]. Clinicians should consider RBC transfusion for children prior to radiation therapy.
5.2. Directed donation
A patient's family may seek out alternatives to transfusions from volunteer community blood donors due to concerns about blood safety. A directed blood donor is an individual, usually a relative, or friend who donates blood specifically for a patient in advance of a scheduled transfusion or procedure. Directed donor units are no safer than allogeneic RBC units, with similar rates of infectious disease marker positivity compared to volunteer community donor units when controlling for first time blood donor status [45]. Several potential risks must be considered when a biologic family member wishes to serve as a directed donor to a child who may later need a hematopoietic stem cell transplant from a family member, including TRALI and RBC and HLA alloimmunization. These risks should be adequately explained to families wishing to proceed with directed donation. In addition, the practitioner must discuss cost, timing of donation, and special needs of the patient such as ABO/Rh blood type compatibility and CMV seronegative status, which may not be met by the directed donor/family member. Cellular blood components from blood relatives should be irradiated to prevent TA-GVHD.
5.3. Dosage of and rate of RBC transfusion in children
The standard dose for RBC therapy in children is 10 to 15 ml per kg of child's actual body weight infused over 3 to 4 h, taking care to maximize the use of each blood unit entered. The hemoglobin should increase by 2 g/dl for each 10 ml per kg of packed RBCs transfused of units stored in additive solution (AS) [46]. The rate of RBC transfusion has not been well studied in children, but practitioners should take into consideration the severity of anemia, its onset, any ongoing blood loss and their cardiovascular health. Traditionally, children with gradual onset of severe anemia should be transfused at a slow rate (i.e. 1 ml/kg/h) to prevent transfusion associated circulatory overload (TACO). A recent randomized clinical trial showed that in 43 children without evidence of cardiac failure with severe anemia, none developed signs of circulatory overload with RBC transfusion at rates of 1 ml/kg/h or 3 ml/kg/h [47]. In children with evidence of cardiac failure, practitioners should transfuse slowly and prescribe diuretics if necessary [48].
5.4. End-of-life management of anemia
Patients receiving palliative care also have anemia, but there is no good evidence about best transfusion practice in children. Commonly, children with advanced cancer in the last month of life complain of fatigue, and their families report significant suffering because of this fatigue [49]. The cause of fatigue is multifactorial, and can include physiological, psychological and situational factors, including anemia and disrupted sleep [50]. Studies in adults have shown that treatment of anemia with either RBC transfusion or erythropoietin reduced fatigue and enhanced quality of life [49]. In children, erythropoietin improved anemia but failed to improve quality of life [51]. Further studies are needed in pediatric palliative care to address best treatment of anemia.
5.5. Adult patients
5.5.1. Reassessment of the transfusion trigger
Moderate anemia has few associated symptoms, due to significant compensatory mechanisms that preserve oxygen transport in the setting of a reduced Hb. Important physiological compensatory mechanisms include increased blood flow due to decreased blood viscosity, increased oxygen unloading to tissues due to increased red cell diphosphoglycerate (DPG), maintenance of blood volume due to increased plasma volume, and redistribution of blood flow [52]. Symptomatic manifestations occur only when the Hb is below two-thirds of normal (i.e., less than 9 to 10 g/dl) as basal cardiac output increases in the anemic patient and is manifested clinically by symptoms of increased cardiac work [53]. The historical practice was to correct moderate anemia with red blood cell transfusions in order to treat these signs and symptoms or to transfuse blood prophylactically. Subsequently, reflected in one publication that stated ‘when the concentration of hemoglobin is less than 8 to 10 g/dl, it is wise to give a blood transfusion before operation’ [54].
This re-adjustment of the transfusion trigger from a Hb of 10 g/dl to a somewhat lower threshold was accompanied by the realization that in populations such as Jehovah's Witness patients that decline blood transfusions because of religious beliefs, morbidity and mortality do not occur until the hemoglobin is very low [55]. Data from Jehovah's Witness patients indicate that the critical level of hemodilution, defined as the point at which oxygen consumption (VO2) starts to decrease because insufficient oxygen delivery (DO2), is achieved at a Hb level of approximately 4 g/dl [56].
For patients known to have cardiovascular disease (CVD) who are anemic, postoperative mortality has been reported to be increased significantly, when compared with patients not known to have CVD [57]. Management of anemia and the transfusion trigger should therefore be different for these patients. A post-hoc analysis of one study [58] was accompanied by an editorial observing that “survival tended to decrease for patients with pre-existing heart disease in the restrictive transfusion strategy group, suggesting that critically ill patients with heart and vascular disease may benefit from higher Hb” [59]. A previously published clinical practice set of guidelines concluded “the presence of coronary artery disease likely constitutes an important factor in determining a patient's tolerance to low Hb” [60]. A retrospective, analysis on 79,000 elderly patients (> 65 years of age) hospitalized with acute myocardial infarction in the United States found that blood transfusion in patients whose admission hematocrit values were less than 33% were associated with significantly lower mortality rates [61]. A more aggressive use of blood transfusion in the management of anemia in elderly patients with cardiac disease is warranted [4], [62].
5.5.2. Level 1 evidence
There are an increasing number of controlled, randomized trials providing Level I evidence for blood transfusion practices. A previous systematic review of the literature to year 2000 identified 10 trials [63]. The authors concluded at that time that the existing evidence supported the use of restrictive transfusion triggers in patients who were free of serious cardiac disease. A Cochrane systematic review of prospective randomized trials to 2012 [31] compared “high” versus “low” Hb thresholds of 19 trials involving a total of 6264 patients. The authors found that 1) “low” Hb thresholds were well tolerated; 2) red blood cell transfusions were reduced by 34% (CI 24 to 45%) in patients randomized to the “low” Hb cohorts; and 3) the number of red blood cell transfusions was reduced by 1.2 units (CI 0.5 to 1.8 units) in the “low” Hb cohorts. A more recent meta-analysis found that a restrictive red blood cell transfusion strategy aiming to allow a hemoglobin concentration as low as 7 g/dl reduced cardiac events, re-bleeding, bacterial infections, and mortality [32].
There are six key randomized, clinical trials in adult patients that compare ‘restrictive’ vs. ‘liberal’ RBC transfusion strategies in various clinical settings (Table 2 ). The Transfusion Requirements in Critical Care (TRICC) trial [64] found that intensive care patients could tolerate a restrictive transfusion strategy (Hb range 7 to 9 g/dl, 8.2 g/dl on average) as well as patients transfused more liberally (Hb range 10 to 12 g/dl, 10.5 g/dl on average), with no differences in 30 day mortality rates. In contrast, a retrospective study of 2393 patients [65] consecutively admitted to the ICU found that an admission hematocrit < 25%, in the absence of transfusion, was associated with long-term mortality; so that there may be hematocrit levels below which the transfusion risk to benefit imbalance reverses.
Table 2.
Six key clinical trials of blood transfusion in adults.
| Clinical setting (Ref) |
Hemoglobin threshold (g/dl) | Age (years) | Patients transfused | Deviation from transfusion protocol | Mean hemoglobin at transfusion (g/dl) | Participation of eligible patients |
|---|---|---|---|---|---|---|
| Intensive care [64] | 7 vs 10 | 57.1 ± 18.1 58.1 ± 18.3 |
67% 99% |
1.4% 4.3% |
8.5 ± 0.7a 10.7 ± 0.7a |
41% |
| CT surgery [66] | 8 vs 10 | 58.6 ± 12.5 vs 60.7 ± 12.5 | 47% 78% |
1.6% 0.0% |
9.1 (9.0–9.2) 10.5 (10.4–10.6) |
75% |
| Hip fracture repair [67] | 8 vs 10 | 81.5 ± 9.0 vs 81.8 ± 8.8 | 41% 97% |
9.0% 5.6% |
7.9 ± 0.6 9.2 ± 0.5 |
56% |
| Acute upper GI bleeding [68] | 7 vs 9 | NA |
49% 86% |
9.0% 3.0% |
7.3 ± 1.4 8.0 ± 1.5 |
93% |
| Symptomatic coronary artery disease [69] | 8 vs 10 | 74.3 ± 11.1 vs 67.3 ± 13.6 | 28.3% NAb |
1.8% 9.1% |
7.9 ± 0.8 9.3 ± 7.9 |
12.2% |
| Sepsis trial [70] | 7 vs 9 | 67 vs 67 | 64% vs 99% | 5.9% vs 2.2% | 7.7 vs 9.3 | 82% |
Updated From Goodnough LT, Schrier A. Am J Hematol 2014;89:88–96 [4].
Average daily hemoglobin.
NA: not available.
The TRACS (Transfusion Requirements after Cardiac Surgery) trial [66] was a large, single center study of patients randomized to receive either restrictive (hematocrit > 24%) or liberal (hematocrit > than 30%) red blood cell transfusions postoperatively. Thirty day all-cause mortality was not different (10% vs. 11%, respectively) between the two cohorts. The FOCUS trial found that elderly (mean > 80 years of age) patients who underwent repair of hip fracture surgery, tolerated a Hb trigger without red blood cell transfusions postoperatively to as low as 8 g/dl (or higher with transfusions, if symptomatic) [67]. More recently, a single center prospective study [68] of patients with upper gastrointestinal (UGI) bleeding demonstrated that patients randomized to a restrictive (Hb < 7 g/dl) vs. a liberal (Hb < 9 g/dl) Hb threshold for blood transfusions, had significantly improved outcomes, including mortality at 45 days and rates of re-bleeding.
The MINT trial [69] was a pilot, feasibility study of liberal (hemoglobin ≥ 10 g/dl) versus restrictive (hemoglobin < 8 g/dl) transfusion thresholds, was initiated for a planned enrollment of 200 patients with symptomatic coronary artery disease (acute coronary syndrome or stable angina undergoing cardiac catheterization), but was terminated at the end of 18 months after enrollment of only 110 patients; of eligible screened patients, only 12% were enrolled (Table 2). The primary, composite outcome (death, myocardial infarction or revascularization) occurred in 10.9% of the liberal transfusion cohort, compared to 25.9% of the restrictive cohort (p = 0.054); and mortality occurred in 1.8% and 13.0%, respectively (p = 0.032). The MINT trial [69] provides evidence that a more liberal transfusion practice to maintain hemoglobin thresholds above 10 g/dl represents prudent management of high risk patients with symptomatic coronary artery disease. Finally, a most recently published trial [70] of lower (< 7 g/dl) vs. higher (< 9 g/dl) hemoglobin thresholds for transfusion in patients with septic shock, found equivalent 90 day mortalities (43 vs 45%, respectively) for patients in the two cohorts.
One of the important limitations of prospectively, randomized clinical trials is that patients who are both eligible and who agree to participate in the study may not be particularly reflective of all patients in these clinical settings. Only 41% of the patients who were determined to be eligible for the TRICC trial [64] and 56% of patients eligible for the FOCUS trial [67] were actually enrolled in the studies, leading to concerns over selection bias; did the treating physicians accurately predict which patients would survive the study, and not enroll the others, thereby ensuring that no differences in survival outcomes would be found between treatment groups?
Another limitation is the interpretation of the ‘transfusion trigger’ in these studies. The mean pretransfusion Hb for patients in the ‘restrictive’ red cell transfusion arm of the TRACS trial was 9.1 g/dl (Table 2). Similarly, the mean Hb for patients in the ‘restrictive’ arm of the TRICC trial was 8.5 g/dl, yet some have interpreted this study to advocate that a Hb of 7 g/dl is appropriate for use as the transfusion trigger in critical care patients.
5.6. Clinical practice guidelines
The number of published clinical practice guidelines for red blood cell [5], [22], [60], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86] transfusions attests to the increasing interest and importance of appropriate blood utilization by professional societies and health care institutions (Table 3 ). The selection of a discrete Hb as a ‘trigger’ for RBC transfusion has been controversial. The guidelines generally acknowledge the necessity of considering patient co-variables or other patient-specific criteria for making transfusion decisions. Among published guidelines, it is generally agreed that transfusion is not of benefit when the Hb is greater than 10 g/dl, but may be beneficial when the Hb is less than 6–7 g/dl [22], [74], [75], [76], [79], [80], [81], [82], [83], [84].
Table 3.
Clinical practice guidelines.
| Red blood cell transfusion | |||
|---|---|---|---|
| Year | Society | Recommendations | Reference |
| 1988 | NIH Consensus Conference | < 7 g/dl (acute) | JAMA 1988;260:2700 [71] |
| 1992 | Am Coll Physicians (ACP) | No number | Ann Int Med 1992;116:393–402 [72] |
| 1996/2006 | AmerSocAnesth (ASA) | < 6 g/dl (acute) No number |
Anesth 1996;84:732–747 [73] Anesth 2006;105:198–208 [74] |
| 1997/1998 | Can Med Assoc (CMA) | No number | Can Med Assoc J 1997;156: S1–24 [60] J Emerg Med 1998;16:129–31 [75] |
| 1998 | Coll Amer Path (CAP) | 6 g/dl (acute) | Arch Path Lab Med 1998;122:130–8 [76] |
| 2001/2012 | Br Com Stand Haematol | No number 7–8 g/dla |
Br J Haematol 2001;113:24–31 [77] http://www.bcshguidelines.com/documents/BCSH_Blood_Admin_-_addendum_August_2012.pdf[78] |
| 2001 | Australasian Soc Blood Trans | 7 g/dl | http://www.nhmrc.health.gov.au[79] |
| 2007/2011 | Soc Thor Surg (STS) SocCardvascAnesth (CVA) |
7 g/dl or 8 g/dla |
Ann ThoracSurg 2007;83:S27–86 [80] Ann ThoracSurg 2011;91:944–82 [81] |
| 2009 | ACCM SCCM |
7 g/dl 7 g/dl |
Crit Care Med 2009;37:3124–57 [82] J Trauma 2009;67:1439–42 [83] |
| 2011 | SABM | 8 g/dl | Trans Med Rev 2011;232–246 [84] |
| 2012 | National Blood Authority, Australia | No number | http://www.nba.gov.au/guidelines/review.html[86] |
| 2012 | AABB | 7–8 g/dl or 8 g/dlb | Ann Int Med 2012;157:49–58 [22] |
| 2012 | KDIGOc | No number | Kid Int 2012;2:311–316 [85] |
| 2012 | National Cancer Center Network (NCCN) | 7–9 g/dl | JNCCN 2012;10:628–53 [5] |
From Goodnough LT. Lancet 2013;391:1845–54 [3].
For patients with acute blood loss.
For patients with symptoms of end-organ ischemia.
An editorial [87] recently summarized the implications of these trials and meta-analyses with a call for a target Hb level for transfusion, stating that ‘it is no longer acceptable to recommend that we transfuse using vague approaches such as clinical judgment or in the hope of alleviating symptoms’. However, this approach would use transfusion to treat laboratory numbers, rather than patients; and would risk over-interpreting available evidence for a ‘transfusion trigger’ and risk under-estimating both the heterogeneity of anemias (e.g., acute versus chronic) and the heterogeneity of patients (i.e., co-morbidities). Given the increasing evidence that shows that blood transfusions are poorly effective and possibly harmful, the guiding principle for transfusion therapy should be that ‘Less is More’. The AABB recently published recommendations for the American Board of Internal Medicine's Choosing Wisely campaign advocating single unit RBC transfusions for nonbleeding hospitalized patients [88]. Additional units should only be prescribed after reassessment of the patient.
5.7. Blood utilization
Both the pediatric [89] and adult hospital [36] at Stanford University Medical Center have reduced blood use by using computerized physician order entry process for blood transfusions [90], [91]. The hemoglobin concentration threshold for blood transfusions decreased after clinical effectiveness teams instituted physician education and clinical decision support in July 2010, via best practices alerts (BPA) at the time of electronic physician order entry (POE) [90]. Fig. 3 shows a subsequent analysis of trends in blood use at Stanford Health Center (SHC). Overall blood component transfusions increased yearly until 2009; after the (BPA) was implemented in July, 2010; however, RBC transfusions have decreased 29% through 2013, importantly, over this same interval [92]. Clinical patient outcomes (length of stay, 30 day readmission rate, mortality) were associated with hospital-wide and particularly in medical and surgical patients receiving RBC transfusion support following clinical decision support (CDS) for restrictive transfusion practice.
Fig. 3.
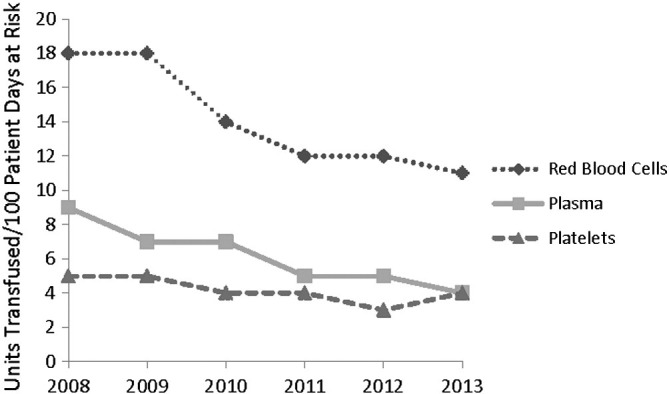
Blood components issued to patients at Stanford Hospital & Clinics (SHC).
Transfusion of red blood cells, plasma, and platelets decreased by 24%, 10%, and 12% respectively, from 2009 through 2013.
Reproduced with permission, From Goodnough LT, Shah N. The Next Chapter in Patient Blood Management: Real-time Clinical Decision Support. Am J Clin Path 2014;142:741–747.
6. Special considerations for transfusion of red blood cells
6.1. Adjunct or alternative therapies: erythropoietin simulating agent (ESA) and iron therapy
The hemoglobin threshold at which to transfuse RBCs or consider adjunct therapies such as erythropoietic stimulating agents (ESAs) should be individualized as different patients tolerate varying degrees of anemia differently. While even moderate chronic anemia is well tolerated by some patients, interval increases in hemoglobin lead to decreased fatigue and improvements in quality of life in adults [93]. ESAs were considered a safe therapeutic option to improve functional status as they were shown to reduce transfusion requirement and improve response. In early 2000s, however, studies began to show that ESA therapy in experimental trials designed to target normal or high-normal hemoglobin levels, were linked to tumor progression and shortened survival [24]. Later trials failed to confirm these detrimental effects and potentially showed a survival benefit [93], [94]. A large meta-analysis concluded that ESA therapy increased the baseline rate of thrombosis present in cancer patients. The use of ESA versus RBC transfusion in selected cancer patients such as those with chronic kidney disease and those on palliative treatment continues under a FDA Risk Evaluation and Mitigation and Strategy [5]. Current risk mitigation strategies include using ESA therapy only for patients with hemoglobin less than 10 g/dl [95]. Anemia can and should be treated at higher Hgb levels if there are available alternative to RBC that are safer.
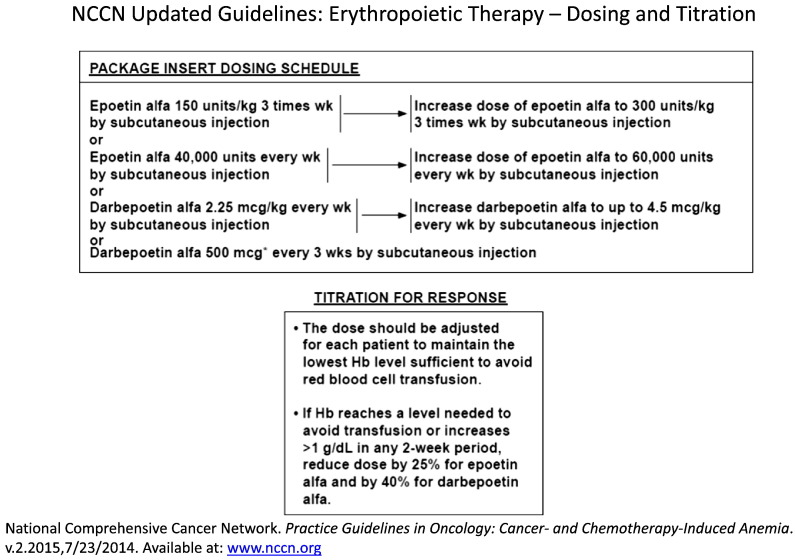
Optimization of iron status should be considered prior to ESA treatment and simultaneously as iron works synergistically with ESA to achieve an optimal biological response by increasing bioavailable iron for erythropoiesis [94]. As illustrated in Fig. 4 , NCCN guidelines recommend iron therapy independent of ESA with those with absolute IDA (ferritin < 30 ng/ml and transfusion saturation < 20%) benefiting from iron alone while those with functional IDA (ferritin 30–800 ng/ml and transfusion saturation 20–50%) benefitting from a combination of iron and ESA.
Fig. 4.
NCCN guidelines.
NCCN guidelines recommend iron therapy independent of ESA with those with absolute IDA (ferritin < 30 ng/ml and transfusion saturation < 20%) benefiting from iron alone while those with functional IDA (ferritin 30–800 ng/ml and transfusion saturation 20–50%) benefitting from a combination of iron and ESA.
In children, there are few randomized studies on the use of ESAs to prevent or treat cancer associated anemia. These studies are difficult to interpret given most have small patient cohorts, variable patient populations, variable study designs and treatment dosing. Shankar reviewed nine randomized trials in pediatrics and concluded that the role of ESAs in treatment or prevention of anemia in children with cancer remains unclear [96]. The existing pediatric data suggests that use of ESAs can significantly decrease the need for RBC transfusions and side effects are mild. However, there are no data to show improvement of quality of life or cost-effectiveness of ESAs and their potential role in promoting cancer cells' growth remains a significant concern in children.
7. Conclusion
Level 1 evidence and meta-analysis of studies comparing restrictive vs. liberal transfusion practices have demonstrated that clinical patient outcomes are improved when fewer red cell transfusions are administered. Future research is needed for the optimal management of anemia in patients with serious comorbidities such as cardiac disease and whether fresh blood is associated with better clinical outcomes than stored blood.
Conflict of interest
NS and JA state no conflicts of interest. LTG is a consultant for American Regent.
Practice points
-
•
Anemia is common in patients with hematologic malignancies, with multifactorial etiologies.
-
•
Level 1 evidence for transfusion “triggers” based on hemoglobin levels have moved to a restrictive over liberal strategies such that RBC transfusion is unlikely to be of benefit when the Hb is greater than 10 g/dl, but may be beneficial when the Hb is less than 6–7 g/dl.
-
•
While treatment of moderate anemia has been shown to improve quality of life, beneficial effects on clinical patient outcomes are unknown.
-
•
Iron restricted erythropoiesis should be identified and treated.
-
•
Erythropoietin stimulating agents should be used cautiously in adults with hematologic malignancies, in accordance with FDA boxed warnings on label and the REMS program.
Research agenda
-
•
Randomized controlled trails between restrictive versus liberal RBC transfusion comparing outcomes in the hematology–oncology population, particularly pediatric.
-
•
Safety profile of ESA use in different subsets of oncology patients.
-
•
Select patients who may have the biggest improvement in quality of life (QOL) while investigating if ones with highest QOL changes have identifiable improvement in clinical patient outcomes.
Footnotes
References
- 1.Ludwig H., Van Belle S., Barrett-Lee P., Birgegard G., Bokemeyer C., Gascon P. The European Cancer Anaemia Survey (ECAS): a large, multinational, prospective survey defining the prevalence, incidence, and treatment of anaemia in cancer patients. Eur J Cancer. 2004;40:2293–2306. doi: 10.1016/j.ejca.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 2.Michon J. Incidence of anemia in pediatric cancer patients in Europe: results of a large, international survey. Med Pediatr Oncol. 2002;39:448–450. doi: 10.1002/mpo.10183. [DOI] [PubMed] [Google Scholar]
- 3.Goodnough L.T., Levy J.H., Murphy M.F. Concepts of blood transfusion in adults. Lancet. 2013;381:1845–1854. doi: 10.1016/S0140-6736(13)60650-9. [DOI] [PubMed] [Google Scholar]
- 4.Goodnough L.T., Schrier S.L. Evaluation and management of anemia in the elderly. Am J Hematol. 2014;89:88–96. doi: 10.1002/ajh.23598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodgers G.M., III, Becker P.S., Blinder M. Cancer- and chemotherapy-induced anemia. J Natl Compr Canc Netw. 2012;10:628–653. doi: 10.6004/jnccn.2012.0064. [DOI] [PubMed] [Google Scholar]
- 6.Hockenberry M.J., Hinds P.S., Barrera P., Billups C., Rodriguez-Galindo C., Tan M. Incidence of anemia in children with solid tumors or Hodgkin disease. J Pediatr Hematol Oncol. 2002;24:35–37. doi: 10.1097/00043426-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Weissinger F., Sandmaier B.M., Maloney D.G., Bensinger W.I., Gooley T., Storb R. Decreased transfusion requirements for patients receiving nonmyeloablative compared with conventional peripheral blood stem cell transplants from HLA-identical siblings. Blood. 2001;98:3584–3588. doi: 10.1182/blood.v98.13.3584. [DOI] [PubMed] [Google Scholar]
- 8.Roy C.N., Andrews N.C. Anemia of inflammation: the hepcidin link. Curr Opin Hematol. 2005;12:107–111. doi: 10.1097/00062752-200503000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Ruggiero A., Riccardi R. Interventions for anemia in pediatric cancer patients. Med Pediatr Oncol. 2002;39:451–454. doi: 10.1002/mpo.10184. [DOI] [PubMed] [Google Scholar]
- 10.Weiss G., Goodnough L.T. Anemia of chronic disease. N Engl J Med. 2005;352:1011–1023. doi: 10.1056/NEJMra041809. [DOI] [PubMed] [Google Scholar]
- 11.Gajewski J.L., Johnson V.V., Sandler S.G., Sayegh A., Klumpp T.R. A review of transfusion practice before, during, and after hematopoietic progenitor cell transplantation. Blood. 2008;112:3036–3047. doi: 10.1182/blood-2007-10-118372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vlachaki E., Diamantidis M.D., Klonizakis P., Haralambidou-Vranitsa S., Ioannidou-Papagiannaki E., Klonizakis I. Pure red cell aplasia and lymphoproliferative disorders: an infrequent association. Sci World J. 2012;2012:475313. doi: 10.1100/2012/475313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Engelen W., Verpooten G.A., Van der Planken M., Helbert M.F., Bosmans J.L., De Broe M.E. Four cases of red blood cell aplasia in association with the use of mycophenolate mofetil in renal transplant patients. Clin Nephrol. 2003;60:119–124. doi: 10.5414/cnp60119. [DOI] [PubMed] [Google Scholar]
- 14.Rossert J., Casadevall N., Eckardt K.U. Anti-erythropoietin antibodies and pure red cell aplasia. J Am Soc Nephrol. 2004;15:398–406. doi: 10.1097/01.asn.0000107561.59698.42. [DOI] [PubMed] [Google Scholar]
- 15.Gehrs B.C., Friedberg R.C. Autoimmune hemolytic anemia. Am J Hematol. 2002;69:258–271. doi: 10.1002/ajh.10062. [DOI] [PubMed] [Google Scholar]
- 16.Paydas S. Fludarabine-induced hemolytic anemia: successful treatment by rituximab. Hematol J. 2004;5:81–83. doi: 10.1038/sj.thj.6200339. [DOI] [PubMed] [Google Scholar]
- 17.Franchini M., Di Minno M.N., Coppola A. Disseminated intravascular coagulation in hematologic malignancies. Semin Thromb Hemost. 2010;36:388–403. doi: 10.1055/s-0030-1254048. [DOI] [PubMed] [Google Scholar]
- 18.Langer F., Spath B., Haubold K., Holstein K., Marx G., Wierecky J. Tissue factor procoagulant activity of plasma microparticles in patients with cancer-associated disseminated intravascular coagulation. Ann Hematol. 2008;87:451–457. doi: 10.1007/s00277-008-0446-3. [DOI] [PubMed] [Google Scholar]
- 19.Zakarija A. Thrombotic microangiopathy syndromes. Cancer Treat Res. 2009;148:115–136. doi: 10.1007/978-0-387-79962-9_8. [DOI] [PubMed] [Google Scholar]
- 20.Straus D.J., Testa M.A., Sarokhan B.J., Czuczman M.S., Tulpule A., Turner R.R. Quality-of-life and health benefits of early treatment of mild anemia: a randomized trial of epoetin alfa in patients receiving chemotherapy for hematologic malignancies. Cancer. 2006;107:1909–1917. doi: 10.1002/cncr.22221. [DOI] [PubMed] [Google Scholar]
- 21.Choosing Wisely An initiative of the ABIM foundation. http://www.choosingwisely.org/ (Accessed: 1/12/2015)
- 22.Carson J.L., Grossman B.J., Kleinman S., Tinmouth A.T., Marques M.B., Fung M.K. Red Blood Cell Transfusion: A Clinical Practice Guideline From the AABB. Ann Intern Med. 2012;157:49–58. doi: 10.7326/0003-4819-157-1-201206190-00429. [DOI] [PubMed] [Google Scholar]
- 23.NCCN Clinical Practice Guidelines in Oncology NCCN guidelines: cancer-and chemotherapy-induced anemia. www.nccn.org/professionals/physician_gls/PDF/anemia.pdf Version2.2012. (Accessed 10/10/2014)
- 24.Goodnough L.T., Shander A. Current status of pharmacologic therapies in patient blood management. Anesth Analg. 2013;116:15–34. doi: 10.1213/ANE.0b013e318273f4ae. [DOI] [PubMed] [Google Scholar]
- 25.Roseff S.D., Luban N.L., Manno C.S. Guidelines for assessing appropriateness of pediatric transfusion. Transfusion. 2002;42:1398–1413. doi: 10.1046/j.1537-2995.2002.00208.x. [DOI] [PubMed] [Google Scholar]
- 26.Perkins H.A., Busch M.P. Transfusion-associated infections: 50 years of relentless challenges and remarkable progress. Transfusion. 2010;50:2080–2099. doi: 10.1111/j.1537-2995.2010.02851.x. [DOI] [PubMed] [Google Scholar]
- 27.US Food and Drug Administration Center for Biologics Evaluation and Research Fatalities reported to FDA following blood collection and transfusion. Annual summary for fiscal year 2011. http://www.fda.gov/downloads/BiologicsBloodVaccines/SafetyAvailability/ReportaProblem/TransfusionDonationFatalities/UCM300764.pdf (accessed Sept 2, 2014)
- 28.Vamvakas E.C. Is white blood cell reduction equivalent to antibody screening in preventing transmission of cytomegalovirus by transfusion? A review of the literature and meta-analysis. Transfus Med Rev. 2005;19:181–199. doi: 10.1016/j.tmrv.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 29.Anderson K.C., Weinstein H.J. Transfusion-associated graft-versus-host disease. N Engl J Med. 1990;323:315–321. doi: 10.1056/NEJM199008023230506. [DOI] [PubMed] [Google Scholar]
- 30.Goodnough L.T., Murphy M.F. Do liberal blood transfusions cause more harm than good? BMJ. 2014;349:g6897. doi: 10.1136/bmj.g6897. [DOI] [PubMed] [Google Scholar]
- 31.Carson J.L., Carless P.A., Hebert P.C. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2012;4 doi: 10.1002/14651858.CD002042.pub3. CD002042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salpeter S.R., Buckley J.S., Chatterjee S. Impact of more restrictive blood transfusion strategies on clinical outcomes: a meta-analysis and systematic review. Am J Med. 2014;127:124–131.e3. doi: 10.1016/j.amjmed.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 33.Goodnough L.T. Blood management: Transfusion Medicine comes of age. Lancet. 2013;381:1791–1792. doi: 10.1016/S0140-6736(13)60673-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang D., Sun J., Solomon S.B., Klein H.G., Natanson C. Transfusion of older stored blood and risk of death: a meta-analysis. Transfusion. 2012;52:1184–1195. doi: 10.1111/j.1537-2995.2011.03466.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Steiner M.E., Triulzi D.J., Assmann S.F., Sloan S.R., Delaney M., Blajchman M.A. Randomized trial results: red cell storage is not associated with a significant difference in multiple-organ dysfunction score or mortality in transfused cardiac surgery patients. Transfusion. 2014;54:15A. [Google Scholar]
- 36.Goodnough L.T., Shander A. Patient blood management. Anesthesiology. 2012;116:1367–1376. doi: 10.1097/ALN.0b013e318254d1a3. [DOI] [PubMed] [Google Scholar]
- 37.Goodnough L.T., Nemeth E., Ganz T. Detection, evaluation, and management of iron-restricted erythropoiesis. Blood. 2010;116:4754–4761. doi: 10.1182/blood-2010-05-286260. [DOI] [PubMed] [Google Scholar]
- 38.Goodnough L.T., Maniatis A., Earnshaw P., Benoni G., Beris P., Bisbe E. Detection, evaluation, and management of preoperative anaemia in the elective orthopaedic surgical patient: NATA guidelines. Br J Anaesth. 2011;106:13–22. doi: 10.1093/bja/aeq361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salisbury A.C., Reid K.J., Alexander K.P., Masoudi F.A., Lai S.M., Chan P.S. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171:1646–1653. doi: 10.1001/archinternmed.2011.361. [DOI] [PubMed] [Google Scholar]
- 40.Lacroix J., Hebert P.C., Hutchison J.S., Hume H.A., Tucci M., Ducruet T. Transfusion strategies for patients in pediatric intensive care units. N Engl J Med. 2007;356:1609–1619. doi: 10.1056/NEJMoa066240. [DOI] [PubMed] [Google Scholar]
- 41.Kirpalani H., Whyte R.K., Andersen C., Asztalos E.V., Heddle N., Blajchman M.A. The Premature Infants in Need of Transfusion (PINT) study: a randomized, controlled trial of a restrictive (low) versus liberal (high) transfusion threshold for extremely low birth weight infants. J Pediatr. 2006;149:301–307. doi: 10.1016/j.jpeds.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 42.Bell E.F., Strauss R.G., Widness J.A., Mahoney L.T., Mock D.M., Seward V.J. Randomized trial of liberal versus restrictive guidelines for red blood cell transfusion in preterm infants. Pediatrics. 2005;115:1685–1691. doi: 10.1542/peds.2004-1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kirpalani H, Bell E, D'Angio C, Hintz S, Kennedy K, Ohls R. Transfusion of prematures (TOP) trial: does a liberal red blood cell transfusion strategy improve neurologically-intact survival of extremely-low-birth-weight infants as compared to a restrictive strategy? http://www.nichd.nih.gov/about/Documents/TOP_Protocol.pdf (Accessed: 10/16/2014)
- 44.Bercovitz R.S., Quinones R.R. A survey of transfusion practices in pediatric hematopoietic stem cell transplant patients. J Pediatr Hematol Oncol. 2013;35:e60–e63. doi: 10.1097/MPH.0b013e3182707ae5. [DOI] [PubMed] [Google Scholar]
- 45.Dorsey K.A., Moritz E.D., Steele W.R., Eder A.F., Stramer S.L. A comparison of human immunodeficiency virus, hepatitis C virus, hepatitis B virus, and human T-lymphotropic virus marker rates for directed versus volunteer blood donations to the American Red Cross during 2005 to 2010. Transfusion. 2013;53:1250–1256. doi: 10.1111/j.1537-2995.2012.03904.x. [DOI] [PubMed] [Google Scholar]
- 46.Fasano R., Luban N.L. Blood component therapy. Pediatr Clin North Am. 2008;55:421–445. doi: 10.1016/j.pcl.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 47.Olgun H., Buyukavci M., Sepetcigil O., Yildirim Z.K., Karacan M., Ceviz N. Comparison of safety and effectiveness of two different transfusion rates in children with severe anemia. J Pediatr Hematol Oncol. 2009;31:843–846. doi: 10.1097/MPH.0b013e3181b27073. [DOI] [PubMed] [Google Scholar]
- 48.Alam A., Lin Y., Lima A., Hansen M., Callum J.L. The prevention of transfusion-associated circulatory overload. Transfus Med Rev. 2013;27:105–112. doi: 10.1016/j.tmrv.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 49.Ullrich C.K., Mayer O.H. Assessment and management of fatigue and dyspnea in pediatric palliative care. Pediatr Clin North Am. 2007;54:735–756. doi: 10.1016/j.pcl.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 50.Yennurajalingam S., Bruera E. Palliative management of fatigue at the close of life: “it feels like my body is just worn out”. JAMA. 2007;297:295–304. doi: 10.1001/jama.297.3.295. [DOI] [PubMed] [Google Scholar]
- 51.Razzouk B.I., Hord J.D., Hockenberry M., Hinds P.S., Feusner J., Williams D. Double-blind, placebo-controlled study of quality of life, hematologic end points, and safety of weekly epoetin alfa in children with cancer receiving myelosuppressive chemotherapy. J Clin Oncol. 2006;24:3583–3589. doi: 10.1200/JCO.2005.03.4371. [DOI] [PubMed] [Google Scholar]
- 52.Goodnough L.T., Despotis G.J., Hogue C.W., Jr., Ferguson T.B., Jr. On the need for improved transfusion indicators in cardiac surgery. Ann Thorac Surg. 1995;60:473–480. doi: 10.1016/0003-4975(95)98960-3. [DOI] [PubMed] [Google Scholar]
- 53.Finch C.A., Lenfant C. Oxygen transport in man. N Engl J Med. 1972;286:407–415. doi: 10.1056/NEJM197202242860806. [DOI] [PubMed] [Google Scholar]
- 54.Adams R.C., Lundy J.S. Anesthesia in cases of poor surgical risk: some suggestions for decreasing the risk. Surg Gynecol Obstet. 1941;71:1011–1014. [Google Scholar]
- 55.Carson J.L., Noveck H., Berlin J.A., Gould S.A. Mortality and morbidity in patients with very low postoperative Hb levels who decline blood transfusion. Transfusion. 2002;42:812–818. doi: 10.1046/j.1537-2995.2002.00123.x. [DOI] [PubMed] [Google Scholar]
- 56.van Woerkens E.C., Trouwborst A., van Lanschot J.J. Profound hemodilution: what is the critical level of hemodilution at which oxygen delivery-dependent oxygen consumption starts in an anesthetized human? Anesth Analg. 1992;75:818–821. doi: 10.1213/00000539-199211000-00029. [DOI] [PubMed] [Google Scholar]
- 57.Carson J.L., Duff A., Poses R.M., Berlin J.A., Spence R.K., Trout R. Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet. 1996;348:1055–1060. doi: 10.1016/S0140-6736(96)04330-9. [DOI] [PubMed] [Google Scholar]
- 58.Hebert P.C., Yetisir E., Martin C., Blajchman M.A., Wells G., Marshall J. Is a low transfusion threshold safe in critically ill patients with cardiovascular diseases? Crit Care Med. 2001;29:227–234. doi: 10.1097/00003246-200102000-00001. [DOI] [PubMed] [Google Scholar]
- 59.Parrillo J.E. Journal supplements, anemia management, and evidence-based critical care medicine. Crit Care Med. 2001;29(Supplement):S139–S140. [Google Scholar]
- 60.Expert Working Group Guidelines for red blood cell and plasma transfusion for adults and children. Can Med Assoc J. 1997;156(Suppl. 11):S1–S24. [Google Scholar]
- 61.Wu W.C., Rathore S.S., Wang Y., Radford M.J., Krumholz H.M. Blood transfusion in elderly patients with acute myocardial infarction. N Engl J Med. 2001;345:1230–1236. doi: 10.1056/NEJMoa010615. [DOI] [PubMed] [Google Scholar]
- 62.Goodnough L.T., Bach R.G. Anemia, transfusion, and mortality. N Engl J Med. 2001;345:1272–1274. doi: 10.1056/NEJM200110253451711. [DOI] [PubMed] [Google Scholar]
- 63.Carson J.L., Hill S., Carless P., Hebert P., Henry D. Transfusion triggers: a systematic review of the literature. Transfus Med Rev. 2002;16:187–199. doi: 10.1053/tmrv.2002.33461. [DOI] [PubMed] [Google Scholar]
- 64.Hebert P.C., Wells G., Blajchman M.A., Marshall J., Martin C., Pagliarello G. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340:409–417. doi: 10.1056/NEJM199902113400601. [DOI] [PubMed] [Google Scholar]
- 65.Mudumbai S.C., Cronkite R., Hu K.U., Wagner T., Hayashi K., Ozanne G.M. Association of admission hematocrit with 6-month and 1-year mortality in intensive care unit patients. Transfusion. 2011;51:2148–2159. doi: 10.1111/j.1537-2995.2011.03134.x. [DOI] [PubMed] [Google Scholar]
- 66.Hajjar L.A., Vincent J.L., Galas F.R., Nakamura R.E., Silva C.M., Santos M.H. Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA. 2010;304:1559–1567. doi: 10.1001/jama.2010.1446. [DOI] [PubMed] [Google Scholar]
- 67.Carson J.L., Terrin M.L., Noveck H., Sanders D.W., Chaitman B.R., Rhoads G.G. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365:2453–2462. doi: 10.1056/NEJMoa1012452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Villanueva C., Colomo A., Bosch A., Concepcion M., Hernandez-Gea V., Aracil C. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368:11–21. doi: 10.1056/NEJMoa1211801. [DOI] [PubMed] [Google Scholar]
- 69.Carson J.L., Brooks M.M., Abbott J.D., Chaitman B., Kelsey S.F., Triulzi D.J. Liberal versus restrictive transfusion thresholds for patients with symptomatic coronary artery disease. Am Heart J. 2013;165:964–971. doi: 10.1016/j.ahj.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Holst L.B., Haase N., Wetterslev J., Wernerman J., Guttormsen A.B., Karlsson S. Lower versus higher hemoglobin threshold for transfusion in septic shock. N Engl J Med. 2014;371:1381–1391. doi: 10.1056/NEJMoa1406617. [DOI] [PubMed] [Google Scholar]
- 71.Consensus conference Perioperative red blood cell transfusion. JAMA. 1988;260:2700–2703. [PubMed] [Google Scholar]
- 72.Welch H.G., Meehan K.R., Goodnough L.T. Prudent strategies for elective red blood cell transfusion. Ann Intern Med. 1992;116:393–402. doi: 10.7326/0003-4819-116-5-393. [DOI] [PubMed] [Google Scholar]
- 73.Practice guidelines for blood component therapy: a report by the American Society of Anesthesiologists Task Force on Blood Component Therapy. Anesthesiology. 1996;84:732–747. [PubMed] [Google Scholar]
- 74.Practice guidelines for perioperative blood transfusion and adjuvant therapies: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Anesthesiology. 2006;105:198–208. doi: 10.1097/00000542-200607000-00030. [DOI] [PubMed] [Google Scholar]
- 75.Innes G. Guidelines for red blood cells and plasma transfusion for adults and children: an emergency physician's overview of the 1997 Canadian blood transfusion guidelines. Part 1: red blood cell transfusion. Canadian Medical Association Expert Working Group. J Emerg Med. 1998;16:129–131. doi: 10.1016/s0736-4679(97)00253-9. [DOI] [PubMed] [Google Scholar]
- 76.Simon T.L., Alverson D.C., AuBuchon J., Cooper E.S., DeChristopher P.J., Glenn G.C. Practice parameter for the use of red blood cell transfusions: developed by the Red Blood Cell Administration Practice Guideline Development Task Force of the College of American Pathologists. Arch Pathol Lab Med. 1998;122:130–138. [PubMed] [Google Scholar]
- 77.Murphy M.F., Wallington T.B., Kelsey P., Boulton F., Bruce M., Cohen H. Guidelines for the clinical use of red cell transfusions. Br J Haematol. 2001;113:24–31. doi: 10.1046/j.1365-2141.2001.02701.x. [DOI] [PubMed] [Google Scholar]
- 78.British Committee for Standards in Haematology (BCSH) Guideline on the administration of blood components. http://www.bcshguidelines.com/documents/BCSH_Blood_Admin_-_addendum_August_2012.pdf (Accessed: 1/20/2015)
- 79.Australasian Society of Blood Transfusion Clinical practice guidelines: appropriate use of red blood cells. http://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/cp78.pdf Accessed: 1/20/2015.
- 80.Ferraris V.A., Ferraris S.P., Saha S.P., Hessel E.A., 2nd, Haan C.K., Royston B.D. Perioperative blood transfusion and blood conservation in cardiac surgery: the Society of Thoracic Surgeons and The Society of Cardiovascular Anesthesiologists clinical practice guideline. Ann Thorac Surg. 2007;83:S27–86. doi: 10.1016/j.athoracsur.2007.02.099. [DOI] [PubMed] [Google Scholar]
- 81.Ferraris V.A., Brown J.R., Despotis G.J., Hammon J.W., Reece T.B., Saha S.P. 2011 update to the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists blood conservation clinical practice guidelines. Ann Thorac Surg. 2011;91:944–982. doi: 10.1016/j.athoracsur.2010.11.078. [DOI] [PubMed] [Google Scholar]
- 82.Napolitano L.M., Kurek S., Luchette F.A., Corwin H.L., Barie P.S., Tisherman S.A. Clinical practice guideline: red blood cell transfusion in adult trauma and critical care. Crit Care Med. 2009;37:3124–3157. doi: 10.1097/CCM.0b013e3181b39f1b. [DOI] [PubMed] [Google Scholar]
- 83.Napolitano L.M., Kurek S., Luchette F.A., Anderson G.L., Bard M.R., Bromberg W. Clinical practice guideline: red blood cell transfusion in adult trauma and critical care. J Trauma. 2009;67:1439–1442. doi: 10.1097/TA.0b013e3181ba7074. [DOI] [PubMed] [Google Scholar]
- 84.Shander A., Fink A., Javidroozi M., Erhard J., Farmer S.L., Corwin H. Appropriateness of allogeneic red blood cell transfusion: the international consensus conference on transfusion outcomes. Transfus Med Rev. 2011;25:232–246. doi: 10.1016/j.tmrv.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 85.KDIGO Clinical practice guideline for anemia in chronic kidney disease. Kidney Int Suppl. 2012;2:311–316. [Google Scholar]
- 86.National Blood Authority, Australia Patient blood management guidelines. http://www.nba.gov.au/guidelines/review.html (Accessed 1/20/2015)
- 87.Carson J.L., Hebert P.C. Should we universally adopt a restrictive approach to blood transfusion? It's all about the number. Am J Med. 2014;127:103–104. doi: 10.1016/j.amjmed.2013.10.026. [DOI] [PubMed] [Google Scholar]
- 88.Callum J.L., Waters J.H., Shaz B.H., Sloan S.R., Murphy M.F. The AABB recommendations for the Choosing Wisely campaign of the American Board of Internal Medicine. Transfusion. 2014;54:2344–2352. doi: 10.1111/trf.12802. [DOI] [PubMed] [Google Scholar]
- 89.Adams E.S., Longhurst C.A., Pageler N., Widen E., Franzon D., Cornfield D.N. Computerized physician order entry with decision support decreases blood transfusions in children. Pediatrics. 2011;127:1112–1119. doi: 10.1542/peds.2010-3252. [DOI] [PubMed] [Google Scholar]
- 90.Goodnough L.T., Shieh L., Hadhazy E., Cheng N., Khari P., Maggio P. Improved blood utilization using real-time clinical decision support. Transfusion. 2014;54:1358–1365. doi: 10.1111/trf.12445. [DOI] [PubMed] [Google Scholar]
- 91.Goodnough LT, Maggio P, Hadhazy E, Shieh L, Hernandez-Boussard T, Khari P. Restrictive blood transfusion practices are associated with improved patient outcomes. Transfusion Epub. 7/4/2014 doi: 10.1111/trf.12723. [DOI] [PubMed] [Google Scholar]
- 92.Goodnough L.T., Shah N. The next chapter in patient blood management: real-time clinical decision support. Am J Clin Pathol. 2014;142:741–747. doi: 10.1309/AJCP4W5CCFOZUJFU. [DOI] [PubMed] [Google Scholar]
- 93.Birgegard G. Managing anemia in lymphoma and multiple myeloma. Ther Clin Risk Manag. 2008;4:527–539. doi: 10.2147/tcrm.s1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gilreath J.A., Stenehjem D.D., Rodgers G.M. Diagnosis and treatment of cancer-related anemia. Am J Hematol. 2014;89:203–212. doi: 10.1002/ajh.23628. [DOI] [PubMed] [Google Scholar]
- 95.Bohlius J., Weingart O., Trelle S., Engert A. Cancer-related anemia and recombinant human erythropoietin—an updated overview. Nat Clin Pract Oncol. 2006;3:152–164. doi: 10.1038/ncponc0451. [DOI] [PubMed] [Google Scholar]
- 96.Shankar A.G. The role of recombinant erythropoietin in childhood cancer. Oncologist. 2008;13:157–166. doi: 10.1634/theoncologist.2007-0126. [DOI] [PubMed] [Google Scholar]